Ribbleton Medical Centre NewApproachComprehensive Report ... · •...
Transcript of Ribbleton Medical Centre NewApproachComprehensive Report ... · •...

This report describes our judgement of the quality of care at this service. It is based on a combination of what we foundwhen we inspected, information from our ongoing monitoring of data about services and information given to us fromthe provider, patients, the public and other organisations.
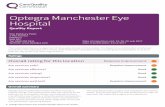
Ratings
Overall rating for this service Good –––
Are services safe? Good –––
Are services effective? Good –––
Are services caring? Good –––
Are services responsive to people’s needs? Good –––
Are services well-led? Good –––
RibbleRibblettonon MedicMedicalal CentrCentreeQuality Report
243 Ribbleton AvenueRibbletonPrestonPR26RDTel: 01772 792512Website: www.ribbletonmedicalcentre.co.uk
Date of inspection visit: 08 April 2015Date of publication: 08/05/2015
1 Ribbleton Medical Centre Quality Report 08/05/2015

Contents
PageSummary of this inspectionOverall summary 2
The five questions we ask and what we found 4
The six population groups and what we found 6
What people who use the service say 8
Areas for improvement 8
Detailed findings from this inspectionOur inspection team 9
Background to Ribbleton Medical Centre 9
Why we carried out this inspection 9
How we carried out this inspection 9
Detailed findings 0
Overall summaryLetter from the Chief Inspector of GeneralPracticeWe had previously undertaken an inspection at thispractice in July 2014 as part of our pilot inspectionstesting our new methodology. We found one area forimprovement and we issued a compliance action inrelation to this at that time.
We carried out an inspection of Ribbleton Medical Centreon 8 April 2015 as part of our new comprehensiveinspection programme and to determine the actionstaken since the last inspection.
Overall the practice is rated as Good.
Our key findings were as follows:
• Improvements had been implemented for the safe andeffective recruitment and employment of staff.
• Staff understood and fulfilled their responsibilities toraise concerns, and to report incidents and nearmisses. Information about safety was recorded,monitored, appropriately reviewed and addressed.
• Patients’ needs were assessed and care was plannedand delivered following best practice guidance. Staffhad received training appropriate to their roles.
• Patients we spoke with said the GPs and nurses werevery good and caring. Out of 106 responses to theFriends and Family test between December 2014 andMarch 2015, 94 respondents said they were eitherextremely likely or likely to recommend the practice tofriends and family.
• Information about services and how to complain wasavailable and the practice responded appropriately tothese.
• Patients said they found it easy to make anappointment with a named GP. The practice wascommitted to providing continuity of care. Urgentappointments were available each day.
• The practice had good facilities and was well equippedto treat patients and meet their needs.
Summary of findings
2 Ribbleton Medical Centre Quality Report 08/05/2015

• There was a clear leadership structure and staff feltsupported by management. The practice proactivelysought feedback from staff and patients, which it actedon.
However, there were also areas of practice where theprovider needs to make improvements
The provider should:
• Ensure that all clinical staff receive training in theprinciples of the Mental Capacity Act 2005.
• Ensure staff who perform chaperoning duties aretrained to undertake this role.
• Ensure that staff training is effectively recorded andmonitored and copies of training certificates kept.
• Ensure an accessible record of clinical staffprofessional registration numbers are kept, so thatthese can be checked more efficiently.
• Ensure regular checks on infection control are carriedout and ensure disposable curtains are changedappropriately.
• Ensure a clear documentary record is maintained ofthe staff recruitment processes including whenreferences are requested and the actions taken whenthese are not provided.
• Ensure a Legionella risk assessment is carried out forthe premises.
Professor Steve Field (CBE FRCP FFPH FRCGP)Chief Inspector of General Practice
Summary of findings
3 Ribbleton Medical Centre Quality Report 08/05/2015

The five questions we ask and what we foundWe always ask the following five questions of services.
Are services safe?The practice is rated as good for providing safe services. Staffunderstood and fulfilled their responsibilities to raise concerns, andto report incidents and near misses. Lessons were learned andcommunicated widely to support improvement. Information aboutsafety was recorded, monitored, appropriately reviewed andaddressed. Staff were knowledgeable about what constituted asafeguarding concern and how to respond to this type of concern.Recruitment checks highlighted as not being followed in a previousinspection were conducted for all staff. There were enough staff tokeep patients safe.
Good –––
Are services effective?The practice is rated as good for providing effective services. Datashowed patient outcomes were at or above average for the locality.Staff referred to guidance from National Institute for Health and CareExcellence and used it routinely. Patient’s needs were assessed andcare was planned and delivered in line with current legislation. Thisincluded assessing capacity and promoting good health. Writtenconsent was obtained for minor surgical procedures. Staff hadreceived training appropriate to their roles. Staff had receivedannual appraisals.The practice regularly met with other healthprofessionals and commissioners in the local area in order to reviewareas for improvement and share good practice.
Good –––
Are services caring?The practice is rated as good for providing caring services. Datashowed that patients rated the practice higher than others forseveral aspects of care. Patients said they were treated withcompassion, dignity and respect and they were involved in decisionsabout their care and treatment. Information to help patientsunderstand the services available was easy to understand. We alsosaw that staff treated patients with kindness and respect, andmaintained confidentiality.
Good –––
Are services responsive to people’s needs?The practice is rated as good for providing responsive services. Itreviewed the needs of its local population and engaged with theNHS England Area Team and Clinical Commissioning Group (CCG) tosecure improvements to services where these were identified.Patients reported good access to the practice and that there wascontinuity of care, with urgent appointments available the sameday. The practice was committed to providing continuity of care. Thepractice sought to gain patient feedback and had an active virtual
Good –––
Summary of findings
4 Ribbleton Medical Centre Quality Report 08/05/2015

Patient Reference Group (PRG) who provided ideas and suggestionsto help improve the service. The practice had good facilities and waswell equipped to treat patients and meet their needs. Informationabout how to complain was available and easy to understand andevidence showed that the practice responded quickly to issuesraised. Learning from complaints with staff and other stakeholderswas evidenced.
Are services well-led?The practice is rated as good for being well-led. The practice had aclear vision which had quality patient care as its top priority. Highstandards were promoted and owned by all practice staff withevidence of team working across all roles. Governance andperformance management arrangements were proactivelyreviewed. We found there was a high level of staff engagement withan open door policy for access to all senior staff. Staff told us theywere very satisfied with their roles. The practice sought feedbackfrom patients and acted upon it where possible.
Good –––
Summary of findings
5 Ribbleton Medical Centre Quality Report 08/05/2015

The six population groups and what we foundWe always inspect the quality of care for these six population groups.
Older peopleThe practice is rated as good for the care of older people. Nationallyreported data showed that outcomes for patients were good forconditions commonly found in older people. For example theQuality and Outcomes Framework (QOF) information indicated thepercentage of patients aged 65 and older who had received aseasonal flu vaccination reflected the national average. The practicesafeguarded older vulnerable patients from the risk of harm orabuse. There were policies in place, staff had been trained and wereknowledgeable regarding vulnerable older people and how tosafeguard them. The practice was responsive to the needs of olderpeople, and offered home visits and rapid access appointments forthose with enhanced needs. One GP had protected time specificallyto focus on the health needs of people living in care homes withinthe local community.
Good –––
People with long term conditionsThe practice is rated as good for the care of people with long-termconditions. The practice had a higher than average number ofpatients with long standing health conditions compared to the localClinical Commissioning Group (CCG) area. Patients with long termconditions were supported by a healthcare team that cared for themusing good practice guidelines and were attentive to their changingneeds. Patients had health reviews at regular intervals depending ontheir health needs and condition. Patients who did not respond totheir annual invite to review their healthcare condition were offereda telephone consultation with a GP. The practice maintained andmonitored registers of patients with long term conditions includingcardiovascular disease and diabetes. These registers enabled thepractice to monitor and review patients with long term conditionseffectively. The Quality and Outcomes Framework (QOF) informationindicated that patients with long term health conditions receivedcare and treatment in line with national averages. One of the homesvisited regularly by the GP with protected time catered for patientswith brain damage and therefore tended to be a younger age group.
Good –––
Families, children and young peopleThe practice is rated as good for the care of families, children andyoung people. Staff demonstrated a good understanding and wereproactive in safeguarding and protecting children from the risk ofharm or abuse. The practice had a clear means of identifying inrecords those children (together with their parents and siblings) whowere subject to a child protection plan. The practice had
Good –––
Summary of findings
6 Ribbleton Medical Centre Quality Report 08/05/2015

appropriate child protection policies in place to support staff andstaff were trained to a level relevant to their role. The practiceoffered a full range of childhood vaccinations and had systems inplace to follow up children who did not attend for these.
Working age people (including those recently retired andstudents)The practice is rated as good for the care of working-age people(including those recently retired and students). The needs of theworking age population, those recently retired and students hadbeen identified and the practice had adjusted the services it offeredto ensure these were accessible, flexible and offered continuity ofcare. The practice was proactive in offering online services as well asa full range of health promotion and screening that reflects theneeds for this age group.
Good –––
People whose circumstances may make them vulnerableThe practice is rated as good for the care of people whosecircumstances may make them vulnerable. The practice was awareof, and identified their vulnerable patients. This was highlightedwithin patient records. The practice discussed any concerningpatients as a team, safeguarding policies and protocols were inplace and staff were trained in safeguarding vulnerable adults andchildren. The safeguarding lead was a GP who had receivedappropriate training. The practice held a register of patients living invulnerable circumstances including those with a learning disability.They carried out annual health checks for people with a learningdisability and offered longer appointments and offered home visits ifrequired.
Good –––
People experiencing poor mental health (including peoplewith dementia)The practice is rated as good for the care of people experiencingpoor mental health (including people with dementia). The practicemaintained a register of patients who experienced poor mentalhealth. The register supported clinical staff to offer patients anannual appointment for a health check and a medication review.The practice monitored patients with poor mental health accordingto clinical quality indicators and in line with good practiceguidelines. A psychologist worked at the practice one day per weekand offered referred patients cognitive behavioural therapy (CBT)which is a talking therapy commonly used to treat anxiety anddepression. The practice worked with multi-disciplinary teams andother mental health services in the case management of patientsexperiencing poor mental health, including those with dementia.
Good –––
Summary of findings
7 Ribbleton Medical Centre Quality Report 08/05/2015

What people who use the service sayDuring our visit, we spoke with five patients and onecarer. They told us that the GPs and nurses working at thepractice were very good. They said they usually could getto see a preferred GP and that on occasion when theyhad to wait they did not mind. They said the practice wasalways clean and tidy.
A member of the practice’s patient representation group(PRG) told us that the practice consulted with them,listened to them and acted on their suggestions.
Although prominently displayed and readily available topatients, we did not receive any feedback through ourCQC comment cards. We therefore reviewed some of therecent feedback the practice had received through theirFriends and Family test. The practice had received 106
responses between December 2014 and March 2015. Intotal 94 respondents said they were either extremelylikely or likely to recommend the practice to friends andfamily.
The results of the National GP Patient Survey published inJanuary 2015 demonstrated the practice performed wellwith 83% of respondents stating they were satisfied withthe surgery's opening hours; 92% of respondentsdescribed their overall experience of this surgery as goodand 79% of respondents described their experience ofmaking an appointment as good. These percentageswere all above the average results for the local ClinicalCommissioning Group (CCG).
Areas for improvementAction the service SHOULD take to improveEnsure that all clinical staff receive training in theprinciples of the Mental Capacity Act 2005
Ensure staff who perform chaperoning duties are trainedto undertake this role.
Ensure that staff training is effectively recorded andmonitored and copies of training certificates kept.
Ensure an accessible record of clinical staff professionalregistration numbers are kept, so that these can bechecked more efficiently.
Ensure regular checks on infection control are carried outand ensure disposable curtains are changedappropriately.
Ensure a clear documentary record is maintained of thestaff recruitment processes including when referenceswere requested and the actions taken when these are notprovided.
Ensure a Legionella risk assessment is carried out for thepremises.
Summary of findings
8 Ribbleton Medical Centre Quality Report 08/05/2015

Our inspection teamOur inspection team was led by:
Our inspection team was led by a CQC Lead Inspector.The team included a GP and a specialist advisor(practice manager).
Background to RibbletonMedical CentreRibbleton Medical Centre is in Preston and is part of theNHS Greater Preston Clinical Commissioning Group (CCG.)Services are provided under a general medical service(GMS) contract with NHS England. There are 8,036registered patients. The practice population includes ahigher number (9.2%) of children under the age of 4, and alower number (10.9%) of people over the age of 65, incomparison with the CCG average of 6% and 15.9%respectively.
There are high levels of deprivation in the practice area.Information published by Public Health England, rates thelevel of deprivation within the practice population group asone on a scale of one to ten. Level one represents thehighest levels of deprivation and level ten the lowest.
The practice opens from 8am to 6pm Monday to Fridays.Patients requiring a GP outside of normal working hoursare advised to contact an external out of hour’s serviceprovider Preston Primary Care Centre.
The practice has four GP partners (three male and onefemale) one salaried GP (female), three practice nurses, onehealth care assistant, a practice manager, reception andadministration staff. The practice is a GP training practice.
The practice offers a nurse triage service and urgentappointments are available each day with a GP once thepatient has spoken with the triage nurse.
On line services include appointment booking, orderingrepeat prescriptions and online access to medical records.
The premises are purpose built and offer access andfacilities for disabled patients and visitors.
Why we carried out thisinspectionWe inspected this service as part of our comprehensiveinspection programme and checked whetherimprovements had been achieved since our last inspectionin July 2014. In addition, we checked whether the providerwas meeting the legal requirements and regulationsassociated with the Health and Social Care Act 2008(Regulated Activities) Regulations 2014, and looked at theoverall quality of the service to provide a rating for theservice under the Care Act 2014.
Please note that when referring to information throughoutthis report, for example, any reference to the Quality andOutcomes (QOF) framework data, this relates to the mostrecent information available to the CQC at that time.
How we carried out thisinspectionTo get to the heart of patients’ experiences of care andtreatment, we always ask the following five questions:
Is it safe?
Is it effective?
Is it caring?
RibbleRibblettonon MedicMedicalal CentrCentreeDetailed findings
9 Ribbleton Medical Centre Quality Report 08/05/2015

Is it responsive to people’s needs?
Is it well-led?
We also looked at how well services are provided forspecific groups of people and what good care looks like forthem. The population groups are:
Older people
People with long-term conditions
Families, children and young people
Working age people (including those recently retired andstudents)
People living in vulnerable circumstances
People experiencing poor mental health (including peoplewith dementia)
Before visiting the practice we reviewed information weheld and asked other organisations and key stakeholdersto share what they knew about the practice. We alsoreviewed policies, procedures and other information thepractice manager provided before the inspection day. Wecarried out an announced visit on 8 April 2015.
We spoke with a range of staff including two GPs, a traineeGP, a psychologist, a practice nurse, a health care assistant,reception staff, administration staff, and the practicemanager. We sought views from patients andrepresentatives of the patient reference group, looked atcomment cards, and reviewed survey information.
Detailed findings
10 Ribbleton Medical Centre Quality Report 08/05/2015

Our findingsSafe track record
The practice used a range of information to identify risksand improve patient safety. This included investigatingreported incidents, checking national patient safety alertsand sharing comments and complaints received frompatients. The staff we spoke with were aware of theirresponsibilities to raise concerns, and knew how to reportincidents and near misses. Reports and data from NHSEngland indicated that the practice had a good track recordfor maintaining patient safety.
We reviewed safety records and incident reports. Thepractice manager, clinicians and any other relevant staffinvestigated and reported on the incidents and events.Interviews with staff confirmed that incidents wereappropriately reported and where improvements andactions were required these were responded toappropriately. Staff told us that they felt confident to reportadverse events and incidents.
Minutes of meetings provided clear evidence that incidents,events and complaints were discussed and whereappropriate actions and protocols were identified tominimise re-occurrence of the incident or complaint.Records were available that showed the practice hadconsistently reviewed and responded to significant events,incidents and complaints and so could show evidence of asafe track record over the long term.
Learning and improvement from safety incidents
The practice had a system in place for reporting, recordingand monitoring significant events, incidents and accidents.We reviewed records of significant events that had occurredduring the previous 12 months. Significant events were astanding item on the practice’s weekly clinical meetingagenda. There was evidence that the practice had learnedfrom these and that the findings were shared with relevantstaff.
We saw evidence to confirm that, as individuals and ateam, staff were actively reflecting on their practice andcritically looked at what they did to see if anyimprovements could be made. Significant events, incidentsand complaints were investigated and reflected on by theGPs and practice manager and learning disseminated to
the whole team where relevant. GPs told us they completedincident reports and carried out significant event analysisroutinely and as part of their ongoing professionaldevelopment.
We looked at significant events from April 2014 to January2015. These had been analysed, reported and discussedwith relevant staff. Following a small audit of safeguardingdocumentation action was taken to improve the quality ofinteragency communications, improve the quality ofrecorded information and to ensure Health Visitorattendance at multidisciplinary meetings. Another incidentreviewed as a significant event resulted in proceduresbeing reviewed and amended to make sure accuraterecords were maintained following a minor family planningprocedure.
National patient safety alerts were disseminated by thepractice manager to relevant staff. Staff confirmed theyreceived these by email. We saw clinical audits had beencarried out in response to these safety alerts.
Reliable safety systems and processes includingsafeguarding
The practice had systems to manage and review risks tovulnerable children, young people and adults. We lookedat training records, which showed that staff had receivedrelevant role specific training on safeguarding. We askedmembers of the medical, nursing and administrative staffabout their understanding of abuse and theirresponsibilities when they suspected a patient was at riskof abuse. Staff knew how to recognise signs of abuse inolder people, vulnerable adults and children. All staff hadaccess to the practice policy and procedure forsafeguarding children and adults. They knew how to shareinformation, properly record safeguarding concerns andhow to contact the relevant agencies in working hours andout of normal hours.
The practice had one GP partner as the lead forsafeguarding and another GP partner as the deputy lead.They had been trained to level 3 as required to fulfil thisrole. All staff we spoke with were aware who these leadswere and who to speak with in the practice if they had asafeguarding concern.
Are services safe?
Good –––
11 Ribbleton Medical Centre Quality Report 08/05/2015

There was a system to highlight or flag vulnerable patientson the practice’s electronic records. This includedinformation to make staff aware of any relevant issueswhen patients attended appointments; for examplechildren subject to child protection plans.
There was a chaperone policy, which was visible in bothwaiting rooms on the ground and first floor. (A chaperone isa person who acts as support and a safeguard and witnessfor a patient and health care professional during a medicalexamination or procedure). Nursing staff and the healthcare assistant usually carried out chaperone duties. Wewere told on rare occasions reception staff were used toprovide chaperoning duties. However, it was unclear whattraining reception staff had to undertake this role.
Medicines management
We checked medicines stored in the treatment rooms andfridges. We found that they were stored appropriately. Allmedicines that we checked were found to be in date.
There was a current policy and procedures in place formedicines management including cold storage ofvaccinations and other drugs requiring this. We saw thechecklist that was completed daily to ensure the fridgesremained at a safe temperature and staff told us of anincident where one of the pharmaceutical fridges failedover a weekend. The result was a failure of the cold chain.The cold chain refers to the process used to maintainoptimal conditions during the transport, storage, andhandling of vaccines so that they remain viable and safe touse. Following the breakdown of the fridge themanufacturers of each affected vaccine was contacted andtheir advice followed regarding the disposal of thesevaccines. A policy and procedure for the maintenance ofthe cold chain was available to staff.
GPs reviewed their prescribing practices as and whenmedication alerts or new guidance was received. Clinicalaudits had also been undertaken on the use of somemedicines in response to alerts and we saw examples ofthese. Examples included the use of Metoclopramide. Thisis used to relieve nausea and vomiting. The outcome of theaudit resulted in a change of prescribing practice andidentified areas for further improvement when prescribingthis medication.
Patient medicines were reviewed on a regular basis in linewith current guidance and legislation depending on thenature and stability of their condition. We saw from data
produced at Clinical Commission Group (CCG) level thataudits were carried out by the CCG medicines managementpharmacist to optimise the prescribing of certainmedicines such as antibiotics or medicines for patientswith long term conditions. Data indicated that the practicehad a higher than average antibiotic prescribing level. Wewere told that this was due to specific medical reasons, ahigher than average number of children on the practiceregister and the level of deprivation in the local community.
All prescriptions were reviewed and signed by a GP beforethey were given to the patient. The practice had recentlyinstalled electronic prescribing which meant that patientprescriptions could be sent automatically to the patient’spreferred pharmacist or chemist. This reduced the need touse paper prescriptions. Blank prescription forms werestored securely.
Medicines for use in medical emergencies were securelystored in the treatment rooms. One practice nurse had leadresponsibility for checking stocks of medicines and theirexpiry dates. We saw these regular checks were recorded.All staff knew where the emergency medicines were stored.There was oxygen kept by the practice for use in case of anemergency. This was checked regularly. The practice alsohad emergency medicine kits for anaphylaxis (a severe,potentially life-threatening allergic reaction that candevelop rapidly).
GPs did not routinely carry medicines in their doctors’ bags.Medicines were taken from the emergency stock for homevisits if the GP believed they might need this. There wassufficient stocks of medicines for the GPs to do this withoutcompromising the remaining medicines available at thepractice. We were told this protocol enabled the nurse tomonitor stocks and expiry dates more easily.
Cleanliness and infection control
We saw the premises were clean and tidy. There werecleaning schedules in place and cleaning records werekept. We saw audits to confirm that monthly monitoringchecks to ensure the practice cleanliness were carried out.Patients we spoke with told us the practice was alwaysclean and tidy. They told us that clinical staff washed theirhands and used gloves and aprons appropriately.
The practice had a lead for infection control who hadundertaken further training to enable them to provideadvice on the practice infection control policy. Staffreceived training about infection control specific to their
Are services safe?
Good –––
12 Ribbleton Medical Centre Quality Report 08/05/2015

role. We looked at an audit undertaken in 2014, whichidentified areas for improvement in the clinical roomswhere minor surgical procedures were undertaken. At ourvisit we could see the improvements to the environmentthat had had been made to ensure the risk of transmittinginfection was reduced. The lead for the infection controlwas not available at our visit but we were told that theychecked the practice regularly to ensure procedures werefollowed. However, the records of these checks were notavailable. We observed that some of the disposable privacycurtains had passed the planned date for renewal.
Staff understood their role in respect of preventing andcontrolling infection. For example reception staff coulddescribe the process for handling submitted specimens.
We inspected treatment and clinical rooms. We noted thatall consultation and treatment rooms had adequate handwashing facilities. Instructions about hand hygiene wereavailable throughout the practice with hand gels in clinicalrooms. We found protective equipment such as gloves andaprons were available in the treatment/consulting rooms.Couches were washable in the treatment rooms andcleaned following each use.
We were told the practice only used instruments that weresingle use. Procedures for the safe storage and disposal ofinstrumentation, sharps and waste products were evident.There was also a policy for needle stick injury and staffknew the procedure to follow in the event of an injury.
The practice had recently been assessed for asbestos;however, a policy for the management, testing andinvestigation of Legionella (a bacterium that can grow incontaminated water and can be potentially fatal) was notavailable. The practice manager confirmed they would takeimmediate action to address this.
Equipment
Staff we spoke with told us they had sufficient and suitableequipment to enable them to carry out diagnosticexaminations, assessments and treatments.
All equipment was tested and maintained regularly and wesaw equipment maintenance logs, contracts and otherrecords that confirmed this. Contracts were in place forannual checks of fire extinguishers and portable appliancetesting (PAT). We saw that annual calibration and servicing
of medical equipment was slightly out of date. We weretold that the servicing of the medical equipment had beenarranged; however, the appointment was cancelled andhad been rearranged.
Emergency drugs were stored in a separate cupboard.There was an oxygen cylinder, nebulisers and access to anautomated external defibrillator. These were maintainedand checked regularly.
Staffing and recruitment
At the last inspection, a requirement was made for thepractice to improve its recruitment procedures to ensurestaff were safely and effectively recruited.
Records we looked at contained evidence that appropriaterecruitment checks had been undertaken prior toemployment. This included application forms with fullwork histories, references, qualifications, registration withthe appropriate professional body and criminal recordschecks through the Disclosure and Barring Service (DBS).One older recruitment file, for a non clinical staff memberdid not have any references. Discussion with the practicemanager identified that they had requested references on anumber of occasions but none were supplied. The practicemanager stated that they contacted one of the referees andthey had advised it was not their company policy toprovide references. The practice manager confirmed that infuture they would record all attempts to obtainpre-employment references and develop a protocol of howto proceed if these were not forthcoming.
There was an informal system in place to record and checkprofessional registration of the GPs with the GeneralMedical Council (GMC) and the practices nurse with theNursing Midwifery Council (NMC). We saw evidence thatdemonstrated professional registration for clinical staff wasup to date and valid. However, an easily accessible recordof clinical staff professional registration numbers wouldenable monitoring checks to be carried out moreefficiently.
Staff told us there was enough staff to maintain the smoothrunning of the practice and there were always enough staffon duty to keep patients safe. Procedures were in place tomanage expected absences, such as annual leave, andunexpected absences through staff sickness. The staffworked well as a team and as such supported each other intimes of absence and unexpected increased need and
Are services safe?
Good –––
13 Ribbleton Medical Centre Quality Report 08/05/2015

demand. The practice manager and GP oversaw the rotafor clinicians and we saw they ensured that sufficient staffwere on duty to deal with expected demand includinghome visits and chaperoning.
The practice had developed clear lines of accountability forall aspects of care and treatment. Clinical staff had leadroles for which they were appropriately trained. Thediversity and skill mix of the staff was good; each personknew exactly what their role was and undertook this to ahigh standard. Staff were skilled and knowledgeable intheir field of expertise and were able to demonstrate howthey could support each other when the need arose.
As a teaching practice, the GPs had mentorship roles withthe doctors training in their practice. The second yeartraining GP doctor felt that they received good training andwas not being used as an extra pair of hands.
Monitoring safety and responding to risk
The practice had systems, processes and policies in placeto manage and monitor risks to patients, staff and visitorsto the practice. All new employees working in the buildingwere given induction information for the building, whichcovered health and safety and fire safety.
There was a staff handbook available for all staff and thiswas supported by a health and safety, general workplaceand clinical policies and procedures for staff follow.
There was a fire risk assessment in place and the practiceregularly had fire equipment tested. Records of fireequipment safety checks to ensure the safety of patients,staff or visitors were available.
Arrangements to deal with emergencies and majorincidents
Staff could describe how they would alert others toemergency situations by use of the panic button on thecomputer system.
An appropriate business continuity plan was in place. Thiscomprehensive plan covered business continuity, staffing,records/electronic systems, clinical and environmentalevents. Key contact numbers were included and paper andelectronic copies of the plan were kept in the practice. Staffwe spoke with were knowledgeable about the businesscontinuity plans and could describe what to do in the eventof a disaster or serious event occurring.
Staff had received training in dealing with medicalemergencies including cardiopulmonary resuscitation(CPR). This was updated annually. Emergency equipmentwas available including access to oxygen and anautomated external defibrillator (used to attempt to restarta person’s heart in an emergency). When we askedmembers of staff, they all knew the location of thisequipment and records confirmed that it was checkedregularly. Emergency medicines were available in a securearea of the practice and all staff knew of their location.These included those for the treatment of cardiac arrest,anaphylaxis and hypoglycaemia and suspected meningitis.Processes were also in place to check whether emergencymedicines were within their expiry date and suitable foruse. All the medicines we checked were in date and fit foruse.
There was a fire procedure policy in place, which identifiedkey personnel, such as fire marshals and their duties in theevent of a fire. Weekly fire alarm tests were carried out andequipment maintained by a contracted company.
Are services safe?
Good –––
14 Ribbleton Medical Centre Quality Report 08/05/2015

Our findingsEffective needs assessment
Patients told us clinicians listened to them and they wereconfident in the treatment they received. All the clinicianswe spoke with were familiar with, and using current bestpractice guidance. The staff we spoke with and evidencewe reviewed, confirmed that care and treatment deliveredwas aimed at ensuring each patient was given support toachieve the best health outcomes for them. Each clinicianconfirmed that they had online access to NICE guidance.
The local community where Ribbleton Medical Centre waslocated has been classified as having high levels of multipledeprivation. (Multiple deprivation is when different types ofdeprivation e.g. lack of education, poor health, high crimelevels, high unemployment are combined into one overallmeasure of deprivation, and are indicators of the quality oflife that the local population experience). We foundclinicians and staff were familiar with the needs of theirlocal population and the impact of the socio-economicenvironment on their health and wellbeing. National datashowed that the practice had 71.9% per 1000 patientsclaiming disability allowance compared with Englandaverage of 50.3%. The practice also had a lower percentageof patients in paid work and a higher percentage ofunemployed patients compared with the England average.
The practice had coding and alerts within the clinicalrecord system to ensure that patients with specific needswere highlighted to staff on opening the clinical record. Forexample, patients on the ‘at risk’ register and palliative careregister. The practice referred patients appropriately tosecondary care and other services. Test results and hospitalconsultation letters were received into the practice eitherelectronically or by paper. These were then scanned ontothe system daily.
New patient health checks were carried out by the healthcare assistant and cardiovascular and other regular healthchecks and screenings were ongoing in line with nationalexpectations.
People with long term conditions were helped andencouraged to self-manage, and checks for blood counts,blood pressure and general wellbeing had been combinedinto single appointments where possible to create a
holistic approach. One GP had responsibility to work withvulnerable patients who were at high risk of hospitaladmission and for carrying out planned weekly visits topatients living in care homes.
The GPs and practice nurses had completed accreditedtraining for checking patients’ physical health and themanagement of various specific diseases. The GPs told usthey had lead responsibilities in specialist clinical areassuch as diabetes, heart disease and asthma and thepractice nurses supported this work.
One practice nurse provided a daily triage service topatients to assess their health care needs and direct themto the most appropriate level of medical support. The otherpractice nurses, in the main, managed long-termconditions such as diabetes, heart disease and asthma.Nurses told us they were able to focus on specificconditions and provide patients with regular support basedon up to date information about each long-termconditions. The practice offered mixed clinics, whichprovided patients with flexibility to attend appointmentswhen it suited them. Systems were in place to identify andrecall patients who did not attend for follow upappointments.
Clinical staff told us the practice focused on learning anddeveloping to improve outcomes for patients. They saidthey were open about asking for and providing colleagueswith advice and support. GPs told us they supported allstaff to continually review and discuss new best practiceguidelines for the management of long-term healthconditions. In addition, the practice nurses received amonthly group tutorial on different clinical conditions withone of the GPs. A practice nurse told us that they weresupported by the GPs and they felt able to discuss anyconcerns they had about a patient or the management of apatient’s condition
We saw no evidence of discrimination when making careand treatment decisions. Interviews with GPs showed thatthe culture in the practice was that patients were referredon need and that age, sex and race was not taken intoaccount in this decision-making.
Management, monitoring and improving outcomes forpeople
The practice routinely collected information aboutpatients’ care and treatment. It used the Quality andOutcomes Framework (QOF) to assess its performance and
Are services effective?(for example, treatment is effective)
Good –––
15 Ribbleton Medical Centre Quality Report 08/05/2015

undertook regular clinical audits. QOF data showed thepractice performed above the national average for the localclinical commissioning group and the England average forthe last four years. The practice actively monitored itsperformance alongside the Clinical Commissioning Group(CCG) and bench marking against quality frameworks.
The practice had a system in place for completing clinicalaudit cycles. Following each clinical audit, changes totreatment or care were made where needed and the auditrepeated to ensure outcomes for patients had improved.For example, following an alert from the Medicines andHealthcare Products Regulatory Agency (MHRA) regarding amedicine used to reduce nausea and vomiting .The aim ofthe audit was to review dosage and duration ofadministration alongside the new guidance and to ensurethat all patients prescribed this medicine long term did notexperience neurological side effects. The outcome of theaudit was shared with the GPs so appropriate action wastaken.
Examples of other clinical audits included looking at asample of 19 patients who were triaged by the nurse toassess the quality of the assessment provided to thepatient and the written notes recorded following theconsultation. The audit identified a positive outcome withevidence of appropriate consultation and recording. Arecent audit of cytology smears showed that the practicehad a lower score on inadequate smears when comparedto the other locations, which used the Manchester Cytologycentre to analyse these. Therefore, patients did not need toreturn for a repeat procedure.
Minor surgical procedures and Intra Uterine DeviceImplants (IUD or coil) were undertaken at the practice inline with their registration and NICE guidance. We saw thatpatients consented to these procedures and the signedpaper consent forms were scanned into the patients’medical notes.
The practice also provided enhanced services such as theviolent patient scheme and ankle brachial pressure index(ABPI) monitoring. This is a diagnostic assessment of bloodpressure in a patient’s ankle where there is suspectedperipheral arterial disease. In addition, a cognitivebehavioural therapist worked at the practice for a day eachweek and saw between five and six patients each time.They told us that the service they provided was benefitingsome of the severely depressed patients they were seeing.
Regular meetings took place with multi-disciplinary teamattendance to share information and provide reflection andlearning to the benefit of the patients. We saw evidence ofcollaborative working with other healthcare professionals,which resulted in positive outcomes for the patientsconcerned.
Effective staffing
Practice staffing included medical, nursing, managerial andadministrative staff. We reviewed staff personnel files andthese contained evidence of the training they had received.However, the sample of staff files we saw did not havecopies of training certificates. In addition a staff trainingmatrix detailing what mandatory and other training staffhad received was not available. A staff training matrix orsimilar record would allow for gaps in a staff member’straining to be easily identified and assist in the forwardplanning of staff training.
All staff had access to a staff handbook which included arange of employment policies and procedures andincluded information on safeguarding and whistleblowing.Staff were up to date with attending mandatory coursessuch as annual basic life support. We noted a good skill mixamong the doctors with a number having additionaltraining certificates in children’s health, family planning,and minor surgery. Practice nurses had defined duties andwere able to demonstrate that they were trained to fulfilthese duties.
All GPs were up to date with their yearly continuingprofessional development requirements and all had beenrevalidated. (Every GP is appraised annually, andundertakes a fuller assessment called revalidation everyfive years. Only when revalidation has been confirmed bythe General Medical Council can the GP continue topractise and remain on the performers list with NHSEngland).
All staff undertook annual appraisals that identifiedlearning needs from which action plans were documented.As the practice was a training practice, doctors who weretraining to be qualified as GPs had access to a senior GPthroughout the day for support. One trainee GP spokepositively of the support they received at the practice. Theyfelt they were provided with opportunities to learn anddevelop and compared this favourably to another practicethey had been training at.
Are services effective?(for example, treatment is effective)
Good –––
16 Ribbleton Medical Centre Quality Report 08/05/2015

Staff told us they felt supported and trained to provide agood standard of service to patients.
Working with colleagues and other services
The practice worked with other service providers to meetpatient’s needs and manage those of patients withcomplex needs. It received blood test results, X-ray results,and letters from the local hospital including dischargesummaries, out-of-hours GP services both electronicallyand by post. The practice had a policy outlining theresponsibilities of all relevant staff in passing on, readingand acting on any issues arising from communications withother care providers on the day they were received. All staffwe spoke with understood their roles and felt the system inplace worked well.
The practice held monthly multidisciplinary team meetingsto discuss the needs of complex patients, patients on therisk register hospital admissions and discharges andattendance at A&E.
Minutes from meetings showed that a variety ofprofessionals attended the meetings including districtnurses, community matron, cancer nurse specialist andsocial services support. The practice had taken action to tryto get a health visitor to attend the meetings also.
Information sharing
The practice used electronic systems to communicate withother providers. They shared information with out of hour’sservices regarding patients with special needs. Theycommunicated and shared information regularly betweenthemselves, other practices and community health andsocial care staff at various regular meetings.
The practice had systems to provide staff with theinformation they needed. Staff used an electronic patientrecord to coordinate, document and manage patients’care. All staff were fully trained on the system, andcommented positively about the system’s safety and easeof use. This software enabled scanned papercommunications, such as those from hospital, to be savedin the system for future reference.
Consent to care and treatment
All clinical staff (GPs and nurses) we spoke withdemonstrated an awareness of the Mental Capacity Act2005 (MCA) and their duties in respect of this. However, staffwe spoke with said they had not had training specifically in
relation to the MCA. When interviewed, staff gave examplesof how a patient’s best interests were taken into account ifa patient did not have capacity to make a decision. Allclinical staff demonstrated a clear understanding of Gillickcompetencies. (These are used to help assess whether achild has the maturity to make their own decisions and tounderstand the implications of those decisions).
The practice on occasion carried out some minor surgicalprocedures. For these minor surgical procedures, writtenconsent was obtained and scanned into the patient’selectronic records.
Staff had access to an updated consent policy, whichreflected current guidance. Information about consent wasalso available on the practice’s website.
Patients we spoke with confirmed that consent was alwayssought before examinations or procedures wereundertaken.
Health promotion and prevention
There were health promotion and prevention adviceleaflets available in the waiting rooms at the practiceincluding information on strokes, meningitis, cancer andimmunisations. The practice web site had a range ofinformation and useful links for further supportinginformation for family health, long term conditions andminor illnesses. There was also information available abouttravel vaccinations with links to regions in the world toassist people in identifying what vaccinations theyrequired.
The practice nurses held a variety of mixed clinics includinga weekly baby clinic and for specific problems and generalhealth checks. There was a weekly diabetic clinic onTuesdays although appointments were flexible to assistpatients to attend when they were available. The healthcare assistant provided a lifestyle management support topatients. This included discussions about the patient’senvironment, family life, carer status, mental health andphysical wellbeing as well as checks on blood pressure,smoking, diet and alcohol and drug dependency ifappropriate.
The practice also operated NHS health checks for patientsbetween 40-74 years of age.
The practice used the coding of health conditions inpatients’ electronic records and disease registers to planand manage services. For example, patients on disease
Are services effective?(for example, treatment is effective)
Good –––
17 Ribbleton Medical Centre Quality Report 08/05/2015

registers were offered reviews with the nurse. The practicehad ways of identifying patients who needed additionalsupport, and it was pro-active in offering additional help.The practice kept a register of all patients with a learning
disability and they were all offered an annual health check.There were local health and support groups that theyaccessed and referred patients with mental health andlearning disabilities needs.
Are services effective?(for example, treatment is effective)
Good –––
18 Ribbleton Medical Centre Quality Report 08/05/2015

Our findingsRespect, dignity, compassion and empathy
The results of the National GP Patient Survey published inJanuary 2015 demonstrated the practice performed wellwith 83% of respondents stating they were satisfied withthe surgery's opening hours; 92% of respondents describedtheir overall experience of this surgery as good and 79% ofrespondents described their experience of making anappointment as good. These percentages were all abovethe average results for the local Clinical CommissioningGroup (CCG). A further 98% of respondents stated they hadconfidence and trust in the last GP they saw or spoke to.
Although prominently displayed and readily available topatients, we did not receive any feedback through our CQCcomment cards. We therefore reviewed some of the recentfeedback the practice had received through their Friendsand Family test. The practice had received 106 responsesfrom between December 2014 and March 2015. In total 94respondents said they were either extremely likely or likelyto recommend the practice to friends and family.
Staff and patients told us that all consultations andtreatments were carried out in the privacy of a consultingroom. There were privacy curtains for use during physicaland intimate examinations and a chaperone service wasavailable. We noted that consultation / treatment roomdoors were closed during consultations and thatconversations taking place in these rooms could not beoverheard. Staff and patients informed us they were awarethere was a room available if patients or family membersrequested a private discussion.
The patient electronic recording system included flags onpatient records to alert staff to patient needs that mightrequire particular sensitivity. For example, where a patienthad a learning disability.
A member of the patient reference group (PRG) told us thatthe practice contacted them to seek their ideas andfeedback about different aspects of the service beingdelivered. Recently the PRG member said they had beenasked for ideas and suggestions to reduce the high numberof patients who did not attend for their bookedappointments. The PRG member said their suggestions
and ideas were listened to and gave an example of wherethey had identified information on the practice websitewhich required updating. This was responded to within aweek.
Care planning and involvement in decisions aboutcare and treatment
Patients we spoke with confirmed they felt involved indecisions about their care and treatment. Patients told usdiagnosis and treatment options were clearly explainedand they did not feel rushed in their appointment.Comments from patients included that they felt listened toand treated with respect, and options were alwaysdiscussed.
The National GP Patient Survey published in January 2015identified 88% of respondents said the last GP they saw orspoke to was good at listening to them; 85% ofrespondents said the last GP they saw or spoke to wasgood at explaining tests and treatments and 81% ofrespondents said the last GP they saw or spoke to wasgood at involving them in decisions about their care
GPs confirmed that all patients over 75 years had a namedGP. An electronic coding system maintained registers ofpatients with particular conditions or vulnerabilities, forexample, diabetes, mental health issues and learningdisabilities.
Staff told us that they used an internet search enginetranslation service to help communicate with people whodid not have English as a first language.
Patient/carer support to cope emotionally with careand treatment
Notices in the waiting room, and on the practice websitetold patients how to access a number of support groupsand organisations. The practice’s patient informationleaflet included details of support groups such as childbereavement services and Cruse bereavement care.
Reception staff knew that when patients wanted to discusssensitive issues or appeared distressed and they could offerthem a private room to discuss their needs.
Patients were positive about the care they received fromthe practice. Patients we spoke with told us they hadenough time to discuss things fully with the GP, patients feltlistened to and felt both the GP, practice nurses and mostreception staff were caring and compassionate.
Are services caring?
Good –––
19 Ribbleton Medical Centre Quality Report 08/05/2015

Our findingsResponding to and meeting people’s needs
The needs of the practice population were understood andsystems were in place to address identified needs in theway services were delivered. The practice held informationand registers about the prevalence of specific diseaseswithin their patient population. This information wasreflected in the services provided, for example screeningprogrammes, vaccination programmes and reviews forpatients with long term conditions and mental healthconditions.
A psychologist worked at the practice one day per weekand offered referred patients cognitive behavioural therapy(CBT) which is a talking therapy commonly used to treatanxiety and depression. A physiotherapist worked at thepractice three days per week and saw patients referred bythe GPs. In addition, Help Direct (a service to help peoplewith their socio-economic needs) was also based at thepractice. The patients could self refer to this service.
Patients with dementia, learning disabilities and enduringmental health conditions were reviewed annually. Theywere encouraged to bring carers with them to thesereviews. One GP had protected time to focus on the needsof patients living in nursing homes and care homes. Theobjective of this was to meet these patients’ needsproactively and prevent unnecessary hospital admissions.The practice was proactive in contacting patients whofailed to attend vaccination and screening programmes.Home visits could be arranged for children who missedtheir childhood immunisations.
The practice had an active Patient Reference Group (PRG).We spoke with a member of the group. They told us thatthe practice contacted them to seek their ideas andfeedback about different aspects of the service beingdelivered. The PRG member told us that they had beenrecently consulted on ideas to reduce the rate of patientswho did not attend for appointments. The member told usthat they were aware that the practice tried to activelyrecruit members to the PRG right from the point ofregistration with the practice.
Tackling inequity and promoting equality
The practice had consultation, treatment rooms andwaiting rooms both on the ground and first floor. Disabled
access into the building was available and a passenger liftwas available to the first floor for people with mobilityproblems and parents with prams. Corridors and doorwayswere wide enough for people who used mobility aides andprams. Disabled toilet facilities were accessible and aninduction hearing loop was available for people withhearing impairment. Consultation and treatment roomsdoors all had colour coded discs on them as well as thepracticing clinician’s name. This helped patients with visualimpairment and those who may have poor literacy skills.
The practice analysed its activity and monitored patientpopulation groups. They had tailored services and supportaround the practice populations needs and provided agood service to all patient population groups. The GPpartner explained that one of the challenges they facedwas finding solutions to reduce the number of patientswho did not attend for their planned appointments.
Between October 2014 and March 2015 the practice hadprovided three additional GP surgeries each week to helpcope with the winter pressures demand. These additionalsurgeries were provided through the working day. Thepractice had assessed that the patient demand and thesafety of staff influenced the decision to provide additionalsurgeries through the daytime. At our visit, we heard thatthe practice had received the go ahead to continue toprovide the additional GP surgeries each week. However,the practice manager stated that this service would only beprovided if they could secure the long term commitment ofa locum GP to ensure patients received continuity of care.
The practice population included a small group of patientswhose first language was not English. We were told that thepractice used a well known internet search enginetranslation service. Staff told us that this was effective.
The staff we spoke with demonstrated a goodunderstanding of how to meet the specific needs ofpatients with different religious or cultural backgrounds,however specific training in equality and diversity had notyet been undertaken.
Access to the service
The practice was open Monday to Friday 8 am until 6 pm.The practice did not offer late night or early morningappointments. The practice had assessed that the patientdemand and the safety of staff influenced the decision toprovide additional surgeries through the daytime asopposed to the evening or early morning. Information was
Are services responsive to people’s needs?(for example, to feedback?)
Good –––
20 Ribbleton Medical Centre Quality Report 08/05/2015

available to patients about appointments on the practicewebsite and in the practice information leaflet. Thisincluded information on who to contact for advice andappointments out of normal working hours and thecontact details for the out of hours medical provider. Thepractice offered pre bookable and urgent (on the day)appointments and home visits. Appointments could bemade in person, by phone or online. Priority was given tochildren; babies and vulnerable patients. These patientswere always offered a same day or urgent appointment.
Appointments were tailored to meet the needs of patients,for example those with long term conditions and thosewith learning disabilities were given longer appointments.Home visits were made to care homes, older patients andthose vulnerable housebound patients. The practiceoffered mixed clinics for patients with long term conditionsas this provided flexibility to attend appointments at timesconvenient to them.
Patients we spoke with, and patient survey results told uspatients were satisfied with the service they received fromthe practice. The results of the National GP Patient Surveypublished in January 2015 recorded that 97% ofrespondents said the last appointment they got wasconvenient. 79% of respondents described their experience
of making an appointment as good; 82% of respondentswere able to get an appointment to see or speak tosomeone the last time they tried and 72% said they foundit easy to get through to this surgery by phone.
Listening and learning from concerns and complaints
The practice had a system in place for handling complaintsand concerns. Its complaints policy was in line withrecognised guidance and contractual obligations for GPs inEngland and there was a designated responsible personwho handled all complaints in the practice.
We looked at the audit of complaints received by thepractice between March 2014 and February 2015. Thepractice had received six complaints. Complaints werebroken down into different categories, none contained anyclinical care elements. We saw the practice responded tocomplaints proactively investigating the concern,responding appropriately to the complainant, identifyingimprovements in service quality, sharing learning andadapting practice.
Information for patients on how to make a complaint wasdisplayed in the waiting room and in their informationleaflet available at the ground floor reception.
Are services responsive to people’s needs?(for example, to feedback?)
Good –––
21 Ribbleton Medical Centre Quality Report 08/05/2015

Our findingsVision and strategy
Ribbleton Medical Centre did not have a formal writtenvision and strategy. Staff reported an open culture wherethey felt safe to report incidents and mistakes knowing theywould be treated as a learning opportunity. Staff told us thepractice put the patient at the centre of everything they did.
All staff we spoke with demonstrated a commitment andenthusiasm and were engaged in providing a high qualityservice. Each member of staff had a clear role within thestructure of the practice and it was evident that there was astrong culture of teamwork and supporting each other.
Governance arrangements
The practice had a number of policies and procedures inplace to govern activity and these were available to staff onthe computer shared drive. Policies and procedures weviewed were dated and reviewed appropriately and wereup to date. Staff confirmed they had read them and wereaware of how to access them. Staff could describe in detailsome of the policies that governed how they worked forexample the safeguarding children’s policy and procedures.
There was a clear organisational and leadership structurewith named members of staff in lead roles. We spoke withstaff of varying roles and they were all clear about their ownroles and responsibilities. They all told us there was afriendly, open culture within the practice and they felt partof a team. They all felt valued, well supported and knewwho to go to in the practice with any concerns.
The practice used the Quality and Outcomes Framework(QOF) to measure its performance. The QOF data for thispractice showed the practice performed above the nationalaverage for the local clinical commissioning group and theEngland average for the last four years.
The practice had a programme of clinical audits which itused to monitor quality and systems to identify whereaction should be taken. Audits undertaken by the clinicalstaff were decided on either by the local ClinicalCommission Group (CCG) or national priorities but also inresponse to complaints and significant events. Minutes ofmeeting provided clear evidence that the outcome of theaudits were discussed at meetings and training anddevelopment days.
The practice had arrangements in place for identifying andmanaging risks.
Leadership, openness and transparency
There was a well-established clearly identifiedmanagement structure with clear lines of responsibility. Wespoke to staff with differing roles within the service andthey were clear about the lines of accountability andleadership. They all spoke of good clear leadership whicharticulated vision and motivated staff to provide a goodservice.
Staff felt well supported in their role. They felt confident inthe senior team’s ability to deal with any issues, includingserious incidents and concerns regarding clinical practice.All the staff we spoke with told us they felt they were valuedand their views about how to develop the service wereacted upon.
The practice held a number of various meetings at regularintervals that were documented. These included clinical,administrative and organisational meetings. Samples ofrecords we viewed demonstrated information wasexchanged about improvements to the service, practicedevelopments and the identified learning from complaintsand significant events.
Practice seeks and acts on feedback from its patients,the public and staff
We reviewed complaints and found they were wellmanaged. The practice investigated and responded tothem in a timely manner. They were discussed at staffmeetings and were used to ensure staff learned from theissues raised.
There was an active Patient Reference Group (PRG). Thepractice manager told us it was challenging trying to getthe local patient population to participate in sharing theirviews about the practice. One member of the PRGconfirmed that they were consulted on issues and that thepractice responded to their comments and suggestions.
The practice manager was actively promoting the Friendsand Family Test. The practice had received 106 responsesfrom between December 2014 and March 2015. In total 94respondents said they were either extremely likely or likelyto recommend the practice to friends and family
There was a whistleblowing policy in place. Staff told usthey had no concerns about reporting any issues internally.
Are services well-led?(for example, are they well-managed and do senior leaders listen, learnand take appropriate action)
Good –––
22 Ribbleton Medical Centre Quality Report 08/05/2015

Management lead through learning and improvement
GPs were all involved in revalidation, appraisal schemesand continuing professional development. We saw thatstaff were up to date with annual appraisals which includedlooking at their performance and development needs. Stafftold us appraisals were useful and provided an opportunityto share their views and opinions about the practice.
The practice had an induction programme for new staff.Staff undertook training relevant to their role andresponsibilities. Records of some training staff had received
was available. However, a matrix to easily identify whattraining each staff member (including all clinicians) hadhad and when refresher training was due was not availablenor were copies of all training certificates available.
The staff had protected education training (PET) eachmonth. The practice nurses had a monthly tutorial with oneof the GPs and a trainee GP commented positively on thesupport they received and compared this to other locationsthey had received training.
The practice had completed reviews of significant events,complaints and other incidents and shared the learningfrom these with staff at meetings to ensure the practiceimproved outcomes for patients.
Are services well-led?(for example, are they well-managed and do senior leaders listen, learnand take appropriate action)
Good –––
23 Ribbleton Medical Centre Quality Report 08/05/2015