Rheumatoid arthritis
-
Upload
julie-jane-testa -
Category
Health & Medicine
-
view
253 -
download
5
description
Transcript of Rheumatoid arthritis

RHEUMATOID ARTHRITIS

RHEUMATOID ARTHRITIS
Definition:-an autoimmune disease in which the
joint lining and occasionally other tissues become inflamed as a result of overactivity of the body’s immune system. RA is a chronic, systemic, inflammatory disorder that primarily involves the joints.

Epidemiology: 10 cases per 1000 people, or ~ 2.1
million adults in the United States Affects women two top four times
more often than men at all ages There is general increase in
prevalence for both sexes with increasing age
There is lower prevalence of RA in native Japanese and Chinese compared to whites

Etiology: like many other chronic diseases, the etiology
of RA is unknown Current research is based on a complex, but as
yet incomplete, appreciation of the functions of the immune system
Based on the fact that individuals with RA produce antibodies to their own immunoglobulins, there is some reason to believe that RA is an autoimmune disorder. It is not clear, however, whether this antibody production is a primary event or results as a response to a specific antigen from an external stimulus
A specific etiological agent for RA has not been identified

Etiology: Rheumatoid factors (RF) have received
considerable attention in the search for a causative agent in RA because they are found in the sera of approximately 70% of all patients with RA
Recent studies have also sought to establish a genetic predisposition to the development of RA. Human leukocyte antigens (HLAs)are found on the cell surface of most human cells and are capable of generating an immune response when genetically incompatible tissues are grafted to each other for example, during organ transplants.

Pathophysiology: Long-standing RA is characterized by
the grossly edematous appearance of the synovium with slender villous or hair-like projections into the joint cavity
There are distinctive vascular changes, including venous distention, capillary obstruction, neutrophilic infiltration of the arterial walls, and areas of thrombosis and hemorrhage

Pannus – synovial proliferation of vascular granulation tissue, dissolves collagen as it extends over the joint cartilage. Granulation tissue will eventually result in adhesions, fibrosis or bony ankylosis of the joint

Pathophysiology: Chronic inflammation can also
weaken the joint capsule and its supporting ligamentous structures, altering structure and function
Tendon rupture and fraying tendon sheaths may produce imbalance muscle pull resulting in deformities seen in advanced RA

Pathophysiology: Key features of a synovial joint that
differentiates it from other types of joints are the features that make it susceptible to persistent inflammation
High molecular weight substances such as macroglobulins and fibrinogens can pass through the synovial capillaries during periods of inflammation and are not easily cleared. Because the cartilage is avascular, antigen-antibody complexes may be sequestered within the joint cavity and may facilitate a process of phagocytosis and further development of pannus.

Pathophysiology: In established synovitis,
polymorphonuclear (PMN) leukocytes are chemotactically drawn into the joint cavity and contribute to the inflammatory destruction of the synovium. It is known that the lysosomal enzymes, which are released from these leukocytes, can directly injure synovial tissues

Clinical Manifestations:The 1987 Revised Criteria for the Classification of
Rheumatoid Arthritis1. Morning stiffness-Lasts at least an hour before maximal improvement2. Arthritis of three or more joint areas-at least three joint areas simultaneously have had
soft tissue swelling or fluid (not bony overgrowth alone)
3. Arthritis of hand joints-at least one area is swollen (wrist, MCP, or PIP
joints)4. Symmetric arthritis-simultaneous involvement of the same joint areas
on both sides of the body

5. Rheumatoid nodules-subcutaneous nodules over bony
prominences or extensor surfaces6. Serum rheumatoid factor-abnormal amount7. Radiographic changes-include erosions or unequivocal bony
decalcification localized in or most marked adjacent to the involved joint
The joint signs and symptoms described in criteria 1-4 must have lasted for at least 6 weeks.

Signs and symptoms: Systemic manifestations-morning stiffness, anorexia, weight loss, fatigue Joint involvement-marked bilateral and symmetrical patterns-arthralgia, crepitus Cervical spine-50% takes place at the atlanto-axial joint-ankylosing spondylitis Temporomandibular joints-results in an inability to open the mouth fully with normal side-to-side gliding-normal approximation of the upper and lower teeth may also be altered

Shoulder-involvement of GH, SC, and AC joints; scapulothoracic articulation-degeneration, pain, LOM-capsule and ligaments become distended with chronic inflammation Elbows-capsular and ligamentous distention, and joint surface erosion may lead to elbow instability-Flexion contractures may result from persistent spasm secondary to pain

Wrists-development of flexion contractures which ultimately diminishes the ability to execute power grasp-volar subluxation resulting from chronic inflammation of the proximal carpals-Stenosing tenosynovitis (deQuervain’s disease) may also occur

Hand jointsMCP joint:-soft-tissue swelling; volar subluxation; ulnar driftPIP joint:-swelling(sausage-like finger)-Swan-neck deformity-Boutonniere deformity-Bouchard’s nodesDIP joint:-Heberden’s nodes-mallet finger

Ulnar Deviation

Swan neck deformity

Boutonniere deformity

Thumb:-Type I deformity – MCP flex; IP hypext; without CMC involvement- Type II deformity – CMC is subluxed; IP hypext- Type III deformity – CMC subluxed; MCP hypext; more commonly found in RA Mutilans Deformity (Open-Glass Hand):-grossly unstable thumb and severely deformed phalanges-transverse folds of the skin resemble a folded telescope

Hip-less commonly involved in RA-severe inflammatory destruction of the femoral head and the acetabulum may push the acetabulum into the pelvic cavity (protrusio acetabuli) Knees-distention of the joint capsule and attenuation of ligaments-painful knees may be held in slightly flexed positions, ultimately resulting to flexion contractures

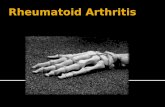
Ankles and feet-hindfoot pronation-flattening of the medial longitudinal arch-calcaneal exostoses-splayfoot-metatarsalgia-hallux valgus and bunion-hammer toes-cock-up or claw toes

Feet deformity

Muscle involvement-muscle weakness – may be due to either reflex inhibition secondary to pain or atrophy Tendons-tenosynovitis – may eventually lead to a tendon rupture-lag phenomenon – refers to a substantial difference between passive and active ROM

LAB TESTING FOR RA No single test is definitive in diagnosing RA. Typical laboratory findings in active disease
include: – Rheumatoid factor (see further detail
below) – Elevated acute phase reactants: ESR and C-
reactive protein (CRP) – CBC: thrombocytosis, hypochromic
microcytic anemia, eosinophilia – Synovial fluid analysis (see below) – Antibodies to cyclic citrullinated peptides
(CCP): specific for RA and correlated with aggressive disease

Synovial Fluid in RA • Low viscosity • WBC: 1,000–75,000/mm3 • > 70% PMNs • Transparent—cloudy • Hypergammaglobulinemia • HypocomplementemiaRheumatoid Factor (RF) in RA • 85% of the patients with RA are RF (+). • The other 15% of patients with RA are RF (–) A ACR
criteria are fulfilled with other positive findings (see above).
• Associated with increased severity of disease with increased systemic manifestations.
• Serial titers are of no value. • RF (+) can be seen in other diseases: rheumatic (SLE,
scleroderma, Sjogren’s), viral, parasitic, bacterial, neoplasms, hyperglobulinemic.

Increased ESR and CRP • Acute phase reactants • Markers for inflammation • Nonspecific and not used in diagnosis • Indicate inflammation/inflammatory
disorder: nonspecific for RA.

Impairments and Complications: Neurological Manifestations-mild neuropathies which result from nerve compression, such as carpal tunnel or tarsal tunnel syndromes Cardiopulmonary Complications-pericarditis (seen in 4% of the patients)-pleuritis Ocular manifestations-dry eyes, associated with Sjogren’s syndrome

Impairments and Complications: Deconditioning-compounded by inadequate levels of regular physical activity-Marked degree of cachexia and elevated resting energy expenditure-it appears that immune e system activity and inflammation creates increased metabolism Rheumatoid nodules-usually asymptomatic, although they can be tender and may cause skin breakdown or become infected Vascular complications-foot and wrist drop may occur as a result of vasculitis of the vasa arteriosum to the nerve supply of the radial or superficial peroneal nerves

Classification of Progression of Rheumatoid Arthritis Stage I, Early1. No destructive changes on radiographic
examination2. Radiographic evidence of osteoporosis may be
presentStage II, Moderate3. Radiographic evidence of osteoporosis, with or
without slight subchondral bone destruction; slight cartilage destruction may be present
4. No joint deformities, although limitation of joint mobility may be present
5. Adjacent muscle atrophy6. Extra-articular soft tissue lesions, such as nodules
and tenosynovitis may be present

Stage III, Severe1. Radiographic evidence of cartilage and
bone destruction, in addition to osteoporosis
2. Joint deformity, such as subluxation, ulnar deviation, or hyperextension, without fibrous or bony ankylosis
3. Extensive muscle atrophy4. Extra-articular soft tissue lesions, such as
nodules and tenosynovitis may be presentStage IV, Terminal5. Fibrous or bony ankylosis6. Criteria of Stage III

Medical Management:Treatment Options for Rheumatoid Arthritis
Medication DMARDs (disease-modifying
antirheumatic drugs) BRMs (Biologic response modifier) Corticosteroids NSAIDs Surgery Synovectomy Arthrodesis Tendon reconstruction

PT Management:
Exercise, Equipment, and Education Treatment Options in Rheumatoid Arthritis Passive treatments
Cold/heat Compression and elevation Massage TENS Acupuncture Orthosis

Exercises LE strengthening Walking Whole-body physical activity Jogging in water Combined LE strengthening, flexibility,
and mobility Aerobic exercises LE range of motion, mobility, or
flexibility Manual therapy with exercises

Equipment Adaptive for ADL Assistive for ambulation Appropriate footwear or insoles
Education Self-management Weight loss (if obese) Activity management or joint protection Social support Stress management/relaxation

Ring orthoses to correct Swan Neck and Boutonniere deformities

Orthosis to correct ulnar deviation of the fingers

Resting orthosis to decrease pain in acutely inflamed joints

Broad-handle utensilsto facilitate meal consumption and
opening of faucets

Extradepthshoes and molded insoles to accommodate rheumatic foot
deformities

Ankle–foot orthosis to provide mediolateral
ankle support or preventtripping

Knee brace to unload the medial knee compartment

ACR Revised Criteria for Classification of Functional Status in Rheumatoid ArthritisClass I Completely able to perform usual ADLs (self-
care, vocational, and avocational)Class II Able to perform usual self-care and vocational
activities, but limited in avocational activitiesClass III Able to perform usual self-care activities, but
limited in vocational and avocational activitiesClass IV Limited in ability to perform usual self-care,
vocational, and avocational activities

SOURCES:
O’Sullivan, S., Schmitz, T. (2007). Physical Rehabilitation (5th ed., pp. 1075-1083).Philadelphia, PA: F.A. Davis Company.
Braddom, R. (2011). Physical Medicine and Rehabilitation (4th ed., pp. 1419). Singapore: Saunders Elsevier