Review of the Evidence: Clostridium difficile Prevention · 1. Clostridium difficile is … • An...
Transcript of Review of the Evidence: Clostridium difficile Prevention · 1. Clostridium difficile is … • An...

Healthcare Associated Infections Program
Center for Healthcare Quality California Department of Public Health
Patient Safety First Conference April 22, 2016
1
Review of the Evidence: Clostridium difficile Prevention
Terry Nelson MBA RN CIC Liaison Infection Preventionist

Objectives
1. Understand the scope of the Clostridium difficile infection (CDI) problem
2. Describe the factors that contribute to C. difficile transmission and CDI incidence
3. Understand the basis for infection prevention and antimicrobial stewardship interventions to reduce CDI
4. Identify opportunities for CDI prevention across the continuum of care
2

1. What is Clostridium difficile ?
3

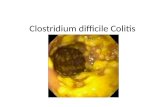
1. Clostridium difficile is …
• An anaerobic, gram-positive, spore-forming, toxin-producing bacillus
• Transmitted among humans via fecal-oral route
• The cause of Clostridium difficile infection (CDI); severity ranges from mild to moderate diarrhea to fulminant pseudomembranous colitis; death in up to 9%
• The leading cause of antibiotic-associated colitis in adults, in both acute and long-term care settings
4
Lessa, et al. New Engl J Med 2015;372:825-34
Leffler and Lamont. New Engl J Med 2015;372:1539-48
Laffan, et al. J Am Geriatr Soc 2006;54(7):1068-73

2. Is CDI a problem?
5

2. CDI is a substantial and increasing problem nationally, and in California • Clostridium difficile caused an estimated • 450,000 illnesses and 29,000 deaths in US in 2011 • 112,800 cases of nursing-home onset CDIs in
United States in 2012
• C. difficile is the most frequently reported healthcare-associated pathogen in hospitals • 10,588 healthcare facility onset-CDI cases reported
in CA in 2014 • 9% increase since 2011
6
Lessa, et al. New Engl J Med 2015;372:825-34
http://www.cdph.ca.gov/programs/hai/Documents/2014-HAI-in-CA-Hospitals-Annual-Report-2014.pdf. Hunter, et al. OFID 2015

7
Leffler and Lamont. New Engl J Med 2015;372:1539-48.

3. How does someone get CDI?
8

3. C. difficile infection requires two events
The following events may occur separately and in any order, but both are required for infection to occur:
1. The C.difficile bacterium or spore must be ingested
2. The normal intestinal flora must be compromised allowing for C.difficile to establish itself and proliferate
9
Sunenshine et al. Cleve Clin J Med. 2006;73:187-97

Clostridium difficile Pathogenesis
10
Sunenshine et al. Cleve Clin J Med. 2006;73:187-97
4. Toxin A & B production leads to colon damage
1. Ingestion of spores transmitted to patients via the hands of healthcare personnel and environment
2. Germination into growing (vegetative) form
3. Changes in lower intestinal flora due to antimicrobial use allows proliferation of C. difficile in colon

4. If both conditions occur (intestinal flora is compromised and C. difficile is ingested), what is the incubation period for CDI?
11

4. The incubation period for CDI is brief
• Incubation period between exposure to C. difficile and occurrence of CDI has been estimated in multiple studies to be a median of 2–3 days • Molecular typing suggests incubation periods are
most commonly a few days to 4 weeks
• Increased risk of CDI can persist many weeks after cessation of predisposing antimicrobial therapy, resulting from prolonged perturbation of normal intestinal flora
12
Cohen et al. Infect Contr Hosp Epidemiol. 2010;31(5):431-55
Walker et al. PLoS Medicine. 2012;9(2):e1001172

5. Are normal healthy people in the community colonized with C. difficile?
13

5. Clostridium difficile is not a common inhabitant of the healthy human adult gastrointestinal tract
• Only 2-7% of the healthy adult population have been found to be colonized with C. difficile
14
Gladys et al. J Clin Microbiol. 2014;52(7):2406-9
Cohen et al. Infect Contr Hosp Epidemiol. 2010;31(5):431-55

6. So if normal healthy people in the community aren’t typically colonized with C. difficile, why are we seeing so much community-onset CDI?
15

6. Most patients with community-onset CDI had a previous hospitalization
• In a prospective study at a university hospital, of 136 patients with CDI, 28% had onset in the community, however the majority (87%) were previously hospitalized
• In a multicenter study, the majority (81%) of community-onset CDI was associated with a previous hospital stay
16
Johal et al. Gut. 2004;53(5):673-77
Dubberke et al. Infect Contr Hosp Epidemiol. 2010;31(10):1030-7

7. How frequent is C. difficile colonization among patients admitted to healthcare facilities?
17

7. C. difficile colonization among patients admitted to healthcare facilities increases with prior healthcare exposure • 10% of asymptomatic adult patients upon admission to a tertiary care hospital were positive for toxigenic C. difficile; colonized patients were significantly more likely to have had a recent hospitalization
• 15% of asymptomatic adult patients upon admission to a large teaching hospital with or without prior healthcare exposure
• Up to 30% of asymptomatic residents of long-term care facilities; higher in facilities with a prior CDI outbreak
18
Alasmari, et al. Clin Infect Dis. 2014;59(2):216-222
Laffan, et al. J Am Geriatr Soc 2006;54(7):1068-73
Ziakas, et al. PLoS One 2015;10(2),e0117195.
Leekha, et al. Am J Infect Contr. 2013;41(5):390-3

8. Is C. difficile transmitted in healthcare facilities?
19

8. Person-to-person transmission of C. difficile within healthcare facilities is well documented • Patients can spread C.difficile to other patients
through direct or indirect contact via hands of healthcare workers or the environment
• Molecular typing confirmed up to 37% of CDIs resulted from in-ward patient-to-patient transmission despite established proper infection control practices • Transmissions most commonly observed during
1st week following the first C. difficile positive sample from a newly diagnosed patient
• Patients/Residents with suspected CDI should be placed on contact precautions promptly
20
Curry, et al. Clin Infect Dis. 2013;57(8):1094-102. Walker et al. PLoS Medicine. 2012;9(2):e1001172

Early detection and isolation of patients with suspected CDI is a strategy to prevent transmission • Focus on testing patients/residents with
clinically significant diarrhea without other identified causes • ≥3 liquid bowel movements (Type 7 on Bristol Stool
Chart) in 24 hours • Stool conforms to shape of container
• Use presumptive contact precautions until CDI ruled out
21
Dubberke et al. Infect Contr Hosp Epidemiol. 2014;35(6):628-45

22
Bristol Stool Chart

9. What role does the environment play in C. difficile transmission?
23

9. The environment is an important source of C. difficile transmission
• C.difficile spores are shed in high numbers, are resistant to desiccation and some disinfectants, and can live on surfaces for up to 5 months
• Admission to a room previously occupied by a CDI patient is a significant risk factor for C.difficile acquisition • 11% of ICU patients admitted to a room previously
occupied by a CDI patient developed CDI, versus 4.6% of ICU patients admitted to a room without a prior CDI positive occupant
24
Kramer, et al. BMC Infect Dis. 2006;6:130
Shaughnessy, et al. Infect Contr Hosp Epidemiol. 2011;32(3):201-206

25

10. Do we need to worry about C. difficile transmission in outpatient settings too?
26

10. The outpatient setting may also be a source for C. difficile transmission • Among community-associated CDI patients cultured
during outpatient visits: • The skin of 32% of patients tested positive for C.difficile • 27% of patients shed spores to one or more high-
touch surfaces in the examination room
• Among ~1000 community-associated CDI cases with no inpatient overnight stay within 12 weeks: • 41% had high-level outpatient healthcare exposure
(surgery, dialysis, ED visit, inpatient visit not overnight) • 41% had low-level outpatient healthcare exposure (doctor
or dentist office, pharmacy)
27
Jury et al. PLoS One. 2013;8(7):e70175.
Chitnis et al JAMA Intern Med. 2013;173:1359-67.

11. Does environmental cleaning and disinfection work to prevent C. difficile transmission?
28

11. Environmental cleaning with bleach can reduce CDI rates on high-incidence units
29
Mayfield et al. Clin Infect Dis 2000;31:995–1000.

30
Assess adequacy of environmental cleaning before switching disinfectant
Carling et al.Clin Infect Dis 2006;42:385-8.
Only 47% of high-touch surfaces in 3 hospitals had been cleaned.

12. How long do patients shed C. difficile into their environment?
31

12. A CDI patient can shed the bacterium and spores into their environment both during and after CDI therapy
• Even upon resolution of diarrhea, 37% continue to shed spores into their environment
• 50% shed C.difficile into their environment 1 to 4 weeks after CDI treatment, although asymptomatic
32
Sethi, et al. Infect Contr Hosp Epidemiol. 2010;31(1):21-27

33
Sethi, et al. Infect Contr Hosp Epidemiol. 2010;31(1):21-27

13. How many CDI patients have a recurrent episode?
34

13. CDI recurrence is common, and highly morbid
• Recurrence among community-associated CDI has been estimated around 14%, and mortality 1%.
• Recurrence among hospital-associated CDI has been
estimated around 21%, and mortality 9%.
35
Lessa, et al. New Engl J Med 2015;372:825-34

14. How easily is C. difficile carried on the hands of healthcare workers?
36

14. Healthcare worker hands are a source for C.difficile spores • 24% of healthcare workers who cared for a CDI
patient had C.difficile spores on their hands; spores found on • 44% of nursing assistants’ hands • 19% of nurses’ hands • 23% of physicians’ hands
• High-risk contact (i.e., exposure to fecal soiling) and
at least one contact without the use of gloves were significantly associated with healthcare worker hand contamination with C.difficile spores
37
Landelle, et al. Infect Contr Hosp Epidemiol. 2014;35(1):10-15

38
A. Frequency of C. difficile contamination of skin sites of patients with CDI
B. Frequency of C. difficile acquisition on sterile gloves after contact with skin sites of patients with CDI
C. Typical illustration of acquisition of C. difficile on sterile gloves after contact with a CDI-affected patient’s groin. *Of note, the patient had showered 1 h before collection of the specimen.
Bobulsky, et al. Clin Infect Dis. 2008;46:447-50

Skin and environmental C. difficile contamination from CDI patients and asymptomatic carriers supports universal glove use on units with high CDI rates
39
Riggs et al. Clin Infect Dis 2007;45:992–8.

15. What are the recommended hand hygiene practices for CDI?
40

15. Hand hygiene in compliance with CDC or WHO guidelines • C. difficile spores are resistant to alcohol
• During outbreaks or in settings with hyperendemic CDI, hand hygiene with soap and water is preferred • Be aware that hand hygiene adherence may decrease
when soap and water is preferred • Clinical studies have not found increase in CDI with
alcohol-based hand hygiene products, but several did find reductions in MRSA or VRE
• Gloves are effective at preventing C. difficile contamination of hands
41
Dubberke, et al. Infect Contr Hosp Epidemiol. 2014;35(6):628-645

16. What role do antibiotics play in CDI?
42

16. Antibiotic exposure is the major risk factor for CDI when a patient is also exposed to the C. difficile bacterium or spores • Increases in CDI risk are observed with increased
cumulative dose, number of antibiotics, and days of antibiotic therapy
43
Stevens, et al. Clin Infect Dis. 2011;53(1):42-48
Number of antibiotics 2 3-4 5+
Risk of CDI compared to patient on 1 antibiotic
2.5 times higher
3.3 times higher
9.6 times higher
Days of antibiotics 4-7 8-18 >18
Risk of CDI compared to patient on antibiotics <4 days
1.4 times higher
3.0 times higher
7.8 times higher

17. Are there particular antibiotics that are most associated with CDI?
44

17. Increased risk of CDI has been linked to specific antibiotics
45
High Risk Medium Risk Low Risk
Aminopenicillins Beta-lactam/beta-lactamase inhibitors
Macrolides
Clindamycin Carbapenems Trimethoprim/ sulfamethoxazole
Cephalosporins Tetracyclines
Fluoroquinolones
Dubberke, et al. Infect Contr Hosp Epidemiol. 2014;35(6):628-645
Price, et al. Clin Microbiol Infect. 2010;16(8):1297-302

18. Does antimicrobial stewardship targeting antibiotics associated with CDI reduce CDI incidence?
46

47
Valiquette, et al. Clin Infect Dis. 2007;45:S112-21
18. Antimicrobial stewardship targeting antimicrobials associated with CDI can reduce CDI incidence

48
Dancer, et al. Int J Antimicrobial Agents. 2013;41:137-42

19. Are there other antimicrobial stewardship interventions to reduce CDI incidence?
49

19. Both broad and targeted antimicrobial stewardship interventions can reduce CDI • Improved overall antimicrobial prescribing • Fewer patients on antimicrobials à
Fewer patients developing CDI à Fewer patients contributing to CDI transmission
• Stopping unnecessary antibiotics in patients with new CDI diagnoses • Improves clinical response of CDI to treatment and
reduces the risk of recurrent CDI à Fewer patients contributing to CDI transmission
50
Dubberke, et al. Infect Contr Hosp Epidemiol. 2014;35(6):628-645

Increased ward-level antibiotic exposure is associated with increased CDI incidence even in patients without direct antibiotic exposure
• Each 10% increase in ward-level antibiotic use was associated with significant increases in • Overall CDI incidence • CDI incidence among patients with direct recent
antibiotic exposure • CDI incidence among patients without direct recent
antibiotic exposure
51
Brown, et al. JAMA Int Med. 2015

Acid-suppressing therapies are another potential stewardship target to address CDI
52
Howell et al. Arch Intern Med. 2010;170(9):784-790

20. Why should we use a regional approach to CDI prevention?
53

20. Patient sharing among healthcare facilities is well documented in the Sacramento Metropolitan Area
54

CDI patients often cycle among multiple hospitals, long term acute care, and long term care facilities 26% of readmitted CDI patients were admitted to another hospital within 12 weeks of discharge Suspected or confirmed CDI status should be communicated to receiving facilities upon transfer
55
Huang, et al. Infect Contr Hosp Epidemiol. 2010;31(11):1160-1169

Patient Sharing Among Healthcare Facilities in Orange County
56
Huang, et al. Infect Contr Hosp Epidemiol. 2010;31(11):1160-1169

A coordinated response may be more effective than independent facility efforts
57
Figure from CDC Vitals Signs: http://www.cdc.gov/vitalsigns/stop-spread/index.html

58
Recap: Core and Supplemental CDI Prevention Strategies
Core Prevention Strategies Supplemental Prevention Strategies
q Contact precautions for duration of diarrhea q Extend use of Contact Precautions beyond duration of symptoms (e.g. 48 hours)
q Hand hygiene before, during, and after care of patient
q Presumptive isolation for patient with diarrhea pending confirmation of CDI
q Cleaning and disinfection of equipment and environment
q Hand washing (soap and water) before exiting room of CDI patient
q Laboratory-based alert system for immediate notification of positive test results
q Implement universal glove use on units with high CDI rates (e.g. in an outbreak setting)
q Educate HCW, housekeeping, administration, patients, families
q Use EPA sporicidal agents for environmental cleaning (as adjunct to core)
q Implement an antimicrobial stewardship program q Track use of antibiotics associated with CDI in the facility
q Perform CDI surveillance, analysis, and reporting q Evaluate and optimize testing for CDI

59
Questions?
For more information, please contact Erin Garcia, CDI Prevention Coordinator at
Terry Nelson, HAI Program Liaison at [email protected]
Or the HAI Program at
Thank you