Review Article Transcultural Diabetes Nutrition Algorithm...
Transcript of Review Article Transcultural Diabetes Nutrition Algorithm...

Hindawi Publishing CorporationInternational Journal of EndocrinologyVolume 2013, Article ID 679396, 7 pageshttp://dx.doi.org/10.1155/2013/679396
Review ArticleTranscultural Diabetes Nutrition Algorithm:A Malaysian Application
Zanariah Hussein,1 Osama Hamdy,2 Yook Chin Chia,3 Shueh Lin Lim,4
Santha Kumari Natkunam,5 Husni Hussain,6 Ming Yeong Tan,7 Ridzoni Sulaiman,8
Barakatun Nisak,9 Winnie Siew Swee Chee,10 Albert Marchetti,11
Refaat A. Hegazi,12 and Jeffrey I. Mechanick13
1 Department of Medicine, Hospital Putrajaya, Pusat Pentadbiran Kerajaan Persekutuan, Presint 7, 62250 Putrajaya, Malaysia2 Division of Endocrinology, Diabetes and Metabolism, Joslin Diabetes Center, Harvard Medical School, Boston, MA 02215, USA3Department of Medicine, University Malaya Medical Centre, Kuala Lumpur, Malaysia4Department of Medicine, Hospital Pulau Pinang, Penang, Malaysia5 Department of Medicine, Hospital Tengku Ampuan Rahimah, Selangor, Malaysia6 Family Medicine, Putrajaya Health Clinic, Putrajaya, Malaysia7 Department of Health Care, International Medical University, Kuala Lumpur, Malaysia8Department of Dietetics and Food Services, Hospital Kuala Lumpur, Kuala Lumpur, Malaysia9Department of Nutrition and Dietetics, University Putra Malaysia, Selangor, Malaysia10Department of Nutrition and Dietetics, International Medical University, Kuala Lumpur, Malaysia11Preventive Medicine and Community Health, University of Medicine and Dentistry of New Jersey, Newark, NJ 07101, USA12Abbott Nutrition, Columbus, OH 43219, USA13Division of Endocrinology, Diabetes, and Bone Disease, Icahn School of Medicine at Mount Sinai, New York, NY 10029, USA
Correspondence should be addressed to Zanariah Hussein; [email protected]
Received 27 June 2013; Accepted 27 September 2013
Academic Editor: Patrizio Tatti
Copyright © 2013 Zanariah Hussein et al. This is an open access article distributed under the Creative Commons AttributionLicense, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properlycited.
Glycemic control among patients with prediabetes and type 2 diabetes mellitus (T2D) inMalaysia is suboptimal, especially after thecontinuous worsening over the past decade. Improved glycemic control may be achieved through a comprehensive managementstrategy that includes medical nutrition therapy (MNT). Evidence-based recommendations for diabetes-specific therapeutic dietsare available internationally. However, Asian patients with T2D, including Malaysians, have unique disease characteristics andrisk factors, as well as cultural and lifestyle dissimilarities, which may render international guidelines and recommendations lessapplicable and/or difficult to implement. With these thoughts in mind, a transcultural Diabetes Nutrition Algorithm (tDNA) wasdeveloped by an international task force of diabetes and nutrition experts through the restructuring of international guidelines forthe nutritional management of prediabetes and T2D to account for cultural differences in lifestyle, diet, and genetic factors. Theinitial evidence-based global tDNA template was designed for simplicity, flexibility, and cultural modification. This paper reportstheMalaysian adaptation of the tDNA,which takes into account the epidemiologic, physiologic, cultural, and lifestyle factors uniqueto Malaysia, as well as the local guidelines recommendations.
1. Introduction
Globally, the prevalence of prediabetes and type 2 diabetes(T2D) is increasing as a consequence of social, epidemiologic,
and demographic shifts, such as population aging and urban-ization [1, 2]. The majority of people with these conditionsnow live in low- and middle-income countries, includingmany Asian nations, where substantial increases in incidence

2 International Journal of Endocrinology
rates are anticipated by the year 2030 [2]. According tothe fourth Malaysian National Health and Morbidity Survey(NHMS IV) carried out in 2011, the prevalence of T2D inMalaysian adults≥30 years of age had risen to 20.8%, affectingan estimated 2.8 million individuals [3] as compared withthe third National Health andMorbidity Survey (NHMS III),which reported a prevalence of 14.9% in 2006 [4].The hetero-geneous nature of Asian populations gives rise to unique T2Dfeatures. For example, Asians tend to develop T2D at a lowerbody mass index (BMI), at younger age, and with a lowerwaist circumference than Caucasians [5, 6], and their courseof illness is punctuatedwith earlier chronic complications [7–9] and frequent postprandial hyperglycemia [10]. These andother clinical features must be recognized and factored intolifestyle recommendations in order to tailor management toindividual needs and improve the effectiveness of preventiveand therapeutic efforts at the primary care level.
2. Methods and MaterialsThe universal tDNA template for patients with prediabetesand T2D was established by an international task force ofexperts during a two-year process that included planningand developmental meetings, evidence collection and review,consensus building, and algorithm construction and facevalidation [11]. The initial global template was designed forsimplicity, flexibility, and cultural modification. A compara-ble process was used by an appointed Malaysian task forceto adapt the algorithm to meet the needs of practitionersand patients in Malaysia. The regional version emergedthrough themodification of general tDNA recommendationsto account for cultural, lifestyle, food, diet, and geneticdifferences that exist among the Malaysian people.
2.1. Perspectives Unique toMalaysia. Among themajor ethnicgroups inMalaysia, Indians (24.9% in 2011 and 19.9% in 2006)had the highest prevalence of T2D, followed byMalays (16.9%in 2011 and 11.9% in 2006) and Chinese (13.8% in 2011 and11.4% in 2006) [3, 4]. These epidemiologic differences couldbe due to the genetic makeup, diet, and cultural variantsamong these major ethnic groups.
The overall prevalence of abdominal obesity in Malaysia,measured by waist circumference, has been reported between55.6% and 57.4% [13, 14]. Epidemiologic studies investigatingabdominal obesity in Malaysia have consistently shown anethnic trend similar to that seen inT2Dwith prevalence beinghighest among Indians (65.5–68.8%), followed by Malays(55.1–60.6%), Chinese (49.5–51.1%), and other indigenousgroups (44.9–48.3%) [13, 14]. The prevalence of abdominalobesity is increased among patients with T2D and is observedin 75% of T2D patients in Malaysia. Moreover, in theDiabCare Malaysia 2008 study, the most recent study in anongoing initiative to monitor diabetes control in Malaysia,undesirable waist circumference was reported in a higherproportion of women (≥80 cm in 89.4%) than men (≥90 cmin 73.7%) with T2D [15].The study patients with T2D, 72% ofwhom were obese, had a mean BMI of 27.8 kg/m2.
Glycemic control in Malaysia continues to deterioratedespite initiatives by the Ministry of Health to increase
awareness and also expanded accessibility of glycosylatedhemoglobin (A1c) testing across the country. The DiabCareMalaysia 2008 study reported ameanA1c of 8.66%, comparedwith 8.0% [16] in 2003, a mean fasting glucose of 8.0mmol/L,and an elevated mean postprandial glucose of 12.7mmol/L inMalaysians with T2D. Furthermore, only 22% of the patientsachieved the glycemic target of A1c <7%, the lowest ratesince 1998 [15]. Data from the online registry database AdultDiabetes Control andManagement (ADCM) revealed ethnicdifferences in glycemic control and complication profilesamongMalaysians. Chinese patients had the lowestmeanA1clevels, while Malaysian Indians had the highest [17].
Only 16.4%of theMalaysian patients adhere to the dietaryregimen provided by dietitians [20]. Interestingly, patientswere found to adhere to the advice of “eat lots of food high indietary fiber such as vegetables or oats” but found it difficultto eat five or more servings of fruits and vegetables perday. Self-care practices among the majority of patients withsuboptimal glycemic control are obviously inadequate. Alarge proportion of Malaysian T2D patients consume four ormore meals a day and more than two carbohydrate portionsper snack [21].
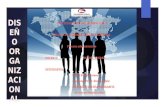
The currentMalaysia Clinical PracticeGuidelines (CPGs)for the management of T2D contain recommendations with-out any specific reference to glycemia-targeted specializednutrition (GTSN), that is, oral nutritional products thatfacilitate glycemic control and may be used as meal and/orsnack replacements or supplements as part of the medicalnutrition therapy (MNT) [18].With the increasing prevalenceof prediabetes and T2D and the continued deterioration ofglycemic control among patients in Malaysia, there is a clearneed for a simple MNT algorithmic decision-making tool toaddress these issues. This paper summarizes the Malaysianadaptation of the universal tDNA template [11]. See Figure 1.Specific Southeast Asian and Asian Indian tDNA versionshave also been published [22, 23].
3. Results: Transcultural Factors for Malaysia
3.1. Assessment of Body Composition and Risk of DiseaseProgression. The World Health Organization (WHO) West-ern Pacific Regional Office and the International DiabetesFoundation (IDF) define overweight and obesity in Asiansas BMI greater than 23 kg/m2 and 25 kg/m2, respectively[24]. Lower cutoff values are required for Asian populationsbecause Asians generally have a higher percentage of intra-abdominal fat compared with Caucasians of the same age,sex, and BMI [25]. Furthermore, Asian populations havehigher cardiovascular and T2D risk factors than Caucasiansat any BMI level [25, 26], thereby highlighting the rationalefor defining Asian-specific cutoff values for anthropometricmeasures.
The Malaysian CPG for the management of obesitycategorizes overweight as BMI of 23.0–27.4 kg/m2 and obesityas BMI of 27.5 kg/m2 and above [28]. Waist circumferencecutoff values for abdominal obesity are 90 cm for men and80 cm for women [24]. Similarly, these cutoff values are alsofound in the CPG for the management of T2D in Malaysia[12] and are used as the standard throughout this paper.

International Journal of Endocrinology 3
(1) Ethnocultural lifestyle input:Geographic location and ethnocultural classifications
(2) Individual risk assessment:Family history of high-risk dietary patterns and premature cardiovascular disease, less than recommended physical activity,abnormal anthropometrics (BMI/WC/WHR over normal ranges for locale), hypertension, dyslipidemia, any cardiovascular event,any liver disease, microalbuminuria over normal range, risky alcohol intake, and any sleep disturbance, and any chronic illness
Low risk High risk
(3) General recommendations:Counseling, physical activity, and healthy eating consistent with
(4) Overweight/obesity (5) Hypertension (6) DyslipidemiaLipid-modifying diet
(7) Chronic kidney diseaseProtein restricted diet:
-Stage 3–5 or greater: 0.6–0.8 g/kgwith adequate energy intake(30–35 kcal/kg/day)
Antihypertensive diet consistentwith sodium restriction
At goal(9) Maintain physical activity and MNT
Not at goal(10) Intensify physical activity and MNT
(8) Follow-up evaluation (1–3 months):History, physical (anthropometrics, blood pressure); chemistries(glucose, A1c, lipids, urinary albumin/creatinine, and liver enzymes);
urinalysis
-Sodium
current clinical practice guidelines or evidence
Physical activity consistent with guidelines;weight loss consistent with guidelines;MNT consistent with guidelines;GTSN caloric supplementation orreplacement consistent with options andstrategies
<2.4 g/day <2, 400mg/day
See text and tables throughout this report for additional information and clarifications
Figure 1: Transcultural Diabetes Nutrition Algorithm (tDNA): Malaysian application.
3.2. Physical Activity in T2D Management. Physical activityand exercise have been shown to lower blood glucose levels,improve glucose and insulin utilization, and improve carbo-hydratemetabolism [29, 30]. Benefits of physical activity havebeen demonstrated in both Caucasian and Asian patientswith T2D [31–34]. The Malaysian CPG for the managementof T2D recommends physical activity as an integral featurein every stage of T2Dmanagement [12]. These recommenda-tions are echoed in theMalaysian tDNA application (Table 1).
3.3. MNT and Weight Loss in T2D Management. MNT playsan integral role in T2D management and indeed is rec-ommended by the American Diabetes Association as animportant component of individual weight loss programs forT2D patients [35]. The benefits of MNT on glycemic controlin Asians with prediabetes and T2D have been demonstratedin clinical trials [36–39]. On-site registered dietitian-ledmanagement of MNT has been shown to improve glycemiccontrol in poorly-managed patients with T2D in primary careclinics in Taiwan. Patients with A1c levels ≥7% who receivedon-site diabetic self-management education had significantlygreater improvements in fasting plasma glucose and A1clevels after one year than control subjects or subjects with
A1c levels <7% [36]. A lifestyle intervention that includesMNT was found to be effective in preventing or delaying thedevelopment of T2D in middle-aged Japanese patients withimpaired glucose tolerance [40, 41].
TheMalaysianDietitians’ Association (MDA) has formedan expert committee, comprising dietitians from primarycare, hospitals, and academia, to compose MNT recommen-dations for T2D.The first version was published in 2005 [42]and updated in 2013 [43]. Building on the MNT guidelinesrecommended by the MDA, the Malaysian CPG for themanagement of T2D, and taking into consideration similarMalaysian CPGs for hypertension and dyslipidemia, thispanel recommends the nutritional considerations outlined inTable 2 [12, 18, 19].
Weight loss is an important therapeutic objective forT2D patients to reduce insulin resistance. Moderate weightloss of just 5–10% of body weight in patients with T2Dhas been shown to decrease insulin resistance and improveother metabolic risk factors [38, 44, 45]. GTSN formulaeare a component of MNT that contain nutrients to facilitateweight management and glycemic control. These formulaeare available in Malaysia and may be utilized with nutritionalcounseling asmeal and/or snack replacements for overweightand obese patients and those with suboptimal glycemic

4 International Journal of Endocrinology
Table 1: Physical activity guidelines for the management of type 2diabetesa [12].
Frequency
Exercise 5 days a week withno more than 2 consecutivedays without physicalexercise
All patients Intensity andtype
(i) Moderate-intensityactivities include walkingdown stairs, cycling, fastwalking, doing heavylaundry, ballroom dancing(slow), noncompetitivebadminton, andlow-impact aerobics(ii) Vigorous activitiesinclude jogging, climbingstairs, football, squash,tennis, swimming, jumpingrope, and basketball
Duration
150min per week ofmoderate-intensity aerobicphysical activity and/or atleast 90min per week ofvigorous aerobic physicalactivity
Overweight or obese patients(BMI > 23)
Gradually increase physicalactivity to 60–90minutesdaily for long-term majorweight loss
BMI: body mass index.aPatients should be assessed for complications that may preclude vigorousexercise. Age and previous physical activity level should be considered.
Table 2: Nutrition guidelines for themanagement of type 2 diabetes[12, 18, 19].
Calories
For overweight and obese individuals, a reducedcalorie diet of 20–25 kcal/kg body weight isrecommended to achieve a weight loss of 5–10%of initial body weight over a 6-month period
Carbohydrate 45–60% daily energy intakeProtein 15–20% daily energy intakeFat 25–35% daily energy intakeSaturated fat Less than 7% of total caloriesCholesterol Less than 200mg/dayFiber∗ 20–30 g/daySodium <2,400mg/day∗Should be derived predominantly from foods rich in complex carbohy-drates including grains (especially whole grains), fruits and vegetables.
control, including persons with high insulin requirements.These formulae are also indicated as a supplementary nutri-tion for patients with diabetes and acute concurrent illnesswho are unable to maintain optimal nutrition due to reducedappetite and calorie intake. Recommendations for the use ofmeal replacements will be incorporated in the revised MNTguidelines from the MDA.
3.4. Nutritional Management of Patients with ConcomitantHypertension, Dyslipidemia, and/or Chronic Kidney Disease(CKD). Data from the ADCM’s online registry databaseshowed that as many as 57% of the Malaysian patients withT2D experience concomitant hypertension [46]. Among theethnic groups in Malaysia, more Malay patients (62.3%)have concomitant hypertension than Chinese (19.6%) orIndian (17.0%) patients. In patients with T2D, hypertension isdefined as blood pressure >130/80mmHg on two readings 2-3 weeks apart [12]. Pharmacotherapy for hypertension shouldbe initiated in patients with T2D when the blood pressure ispersistently >130mmHg systolic and/or >80mmHg diastolic[12]. For patients with concomitant hypertension, salt intakeshould be restricted to <6 g/day (sodium 2 g) [18].
The ADCM also revealed that as many as 38% of thepatients with T2D in Malaysia suffer from concomitant dys-lipidemia [47]. Malays were more likely to have uncontrolledlow-density lipoprotein cholesterol (LDL-C) and triglyc-erides compared with Chinese and Indians; however, Indianswere twice as likely to have inadequate high-density lipopro-tein cholesterol compared with Malays [47]. A recent studythat investigated the ethnic differences in lipid metabolismamong Malaysian patients with T2D demonstrated thatMalays had significantly higher serum levels of glycoxidationand lipoxidation products compared with those of Chineseand Indian patients [48]. For T2D patients with dyslipidemia,lifestyle modification focusing on the reduction of saturatedfat (<7% of total calories), trans fat (avoid), and choles-terol (<200mg/day) intake has been recommended [12, 19].In accordance with the Malaysian CPG for dyslipidemia,patients over the age of 40 without overt cardiovasculardisease (CVD) should be treated with lipid lowering drugs,regardless of the baseline LDL-C levels, while all patients withovert CVD, irrespective of age, should be treated with lipidlowering drugs [19].
For T2D patients with concomitant CKD, limited proteinintake and daily sodium <2400mg are recommended. Forthose with CKD stages 3–5, daily protein should be limitedto 0.6–0.8 g/kg in a diet with adequate energy intake (30–35kcal/kg/day) [49].
4. Conclusions
The following recommendations, statements, figures, tables,and graphs represent the conclusions of the Malaysian tran-scultural Diabetes Nutrition Algorithm (tDNA) task forceand constitute the current Malaysian tDNA application,which accommodates local differences in lifestyle, foods, andcustoms and incorporates established local Clinical PracticeGuidelines (CPGs) to meet the needs and preferences of type2 diabetes (T2D) patients in Malaysia.
Recommendation 1. Medical nutrition therapy (MNT) is anintegral component of the management of T2D and mustbe prioritized in view of poor glycemic control amongpatients in Malaysia. Individualized care plans are essential

International Journal of Endocrinology 5
Table 3: Glycemia-targeted specialized nutrition (GTSN) for themanagement of prediabetes and type 2 diabetes.
Overweight (BMI > 23 kg/m2) orobese (BMI > 27.5 kg/m2)
Use meal and/or snackreplacementsa as part of ameal plan to reduce totalcalorie intake(i) Calorie reduction of500–1000 calories per day(to lose 0.5–1.0 kg perweek), using 1-2 servings ofa GTSN formulab to replace250–500 calories frommeals(ii) Reassess every1–3months
Normal weight(BMI 18–23 kg/m2)
Controlleddiabetes
(A1c ≤ 6.5%c)
The use of mealreplacements should bebased on clinical judgmentand individual assessmentd
Uncontrolleddiabetes
(A1c > 6.5%c)
Use 1-2 servings of a GTSNformula per day to beincorporated into a mealplan
Underweight (BMI < 18 kg/m2)
Use 1–3 servings of a GTSNformula per day assupplementation based onclinical judgment andindividual assessment ofdesired rate of weight gainand clinical tolerance
BMI: body mass index; A1c: glycosylated hemoglobin; GTSN: glycemia-targeted specialized nutrition.Recommendations were rated and assigned numerical and alphabeticaldescriptors according to levels of scientific substantiation provided by the2010 American Association of Clinical Endocrinologists protocol for thedevelopment of Clinical Practice Guidelines [27].aMeal and snack replacements are nutritional products used as replacementformeals or snacks to replace calories in the diet. It is suggested that productsused should meet the American Diabetes Association nutritional guidelines.bGlycemia-targeted specialized nutrition formulas are complete and bal-anced products with at least 200 calories per serving used as part of a mealplan to help control calorie intake and achieve glycemic control.cGlycemic (A1c) targets should be individualized for each patient based onlocal CPGs.dTo avoid hypoglycemia or postprandial hyperglycemia, individuals whomay have muscle mass and/or function loss and/or micronutrient deficiencymay benefit from a nutrition supplement. Individuals who need support withweight maintenance and/or a healthy meal plan could benefit from mealreplacement.
in order to increase adherence and compliance with MNTrecommendations.
Recommendation 2. Personalized nutrition counseling bya dietitian is recommended and should be individualizedaccording to personal nutritional needs, concomitant disease,severity of T2D, cultural preferences, and patient coopera-tion. If access to a dietitian is not possible, all newly diagnosedpatients should receive basic nutrition and dietary counselingfrom either doctors or diabetes educators.
Recommendation 3. Values for bodymass index (BMI) cutoffsin the Malaysian CPGs are recommended for use in theMalaysian tDNA.
Recommendation 4. TheMalaysian CPG for the managementof T2D recommends physical activity as an integral featurein every stage of T2Dmanagement [12]. These recommenda-tions are adopted in the Malaysian tDNA (Table 1).
Recommendation 5. Overweight and obese individuals shouldachieve a weight loss of 5–10% of the initial body weight overa 6-month period (Table 2).
Recommendation 6. The nutritional recommendations out-lined in Table 2 (adapted from the Malaysian Dietitians’Association’sMNT guidelines and theMalaysian CPG for themanagement of T2D) should be implemented as part of theMalaysian tDNA.
Recommendation 7. Patients with T2D and concomitanthypertension should limit salt intake to <6 g/day (sodium2 g). Those with concomitant chronic kidney disease (CKD)should limit protein intake, especially those with CKD stages3–5 (daily protein of 0.6–0.8 g/kgwith adequate energy intakeof 30–35 kcal/kg/day).
Recommendation 8. Lifestyle modification focusing on thereduction of saturated fat (<7% of total calories) and choles-terol (<200mg/day), as well as the avoidance of trans-fat,is recommended for patients with T2D and concomitantdyslipidemia.
Recommendation 9. The use of meal replacements should bebased on clinical judgment and individual assessment. Forpatients who are overweight,meal and/or snack replacementsare recommended as part of meal plans to reduce totalcalorie intake (Table 3). For patients of normal weight withuncontrolled T2D, 1-2 servings of a GTSN formula per day,incorporated into a meal plan as meal or snack replace-ment, are recommended. For underweight individuals, 1–3 servings of a GTSN formula per day are recommendedas supplementation based on the clinical judgment andindividual assessment of desired rate of weight gain andclinical tolerance.
Recommendation 10. To provide support and motivatepatients to comply with MNT, monthly follow-ups are rec-ommended for patients with poorly-controlled T2D and forthose who are at high risk of complications. For patientswith well-controlled T2D, regular follow-up every 3 monthsis recommended.
Disclosures
Zanariah Hussein has received consulting fees from AbbottNutrition, Novo Nordisk, AstraZeneca, and Boehringer In-gelheim. OsamaHamdy has served as a consultant for AbbottNutrition and a speaker for Amylin/Eli Lilly. Yook Chin Chiahas received honorarium for lectures from Pfizer, Servier,

6 International Journal of Endocrinology
AstraZeneca, Sanofi-Aventis, Reckitt Benckiser, GlaxoSmith-Kline, and Sandoz. Shueh Lin Lim has received honorariumfor lectures fromMerck SharpDohme, Eli Lilly, Abbott, NovoNordisk, Novartis, AstraZeneca, Merck Serono, and Sanofi-Aventis. Santha Kumari has no conflict of interests to declare.Husni Hussain has received honorarium for lectures fromMerck Serono, Sanofi-Aventis, and ASP Medical Clinic SdnBhd.MingYeongTanhas received consulting fee fromAbbottNutrition and honorarium for lectures from Roche Diag-nostics, Abbott Nutrition, Merck Sharp Dohme, and MerckSerono. Ridzoni Sulaiman, Barakatun Nisak, and WinnieSiew Swee Chee have received consulting fee or honorariumfrom Abbott Nutrition. Refaat A. Hegazi is employed byAbbottNutrition; thematerial presented in this paper is basedon the best-known clinical evidence and is not affected by thisfinancial relationship. Albert Marchetti has received financialsupport for research and the development of educationalmaterials from Eli Lilly, Takeda, GlaxoSmithKline, Bristol-Myers Squibb, and Abbott Nutrition. Jeffrey Mechanick hasreceived financial support for the development of educationalpresentations from Abbott Nutrition. He has received finan-cial support for consultancy and for writing and reviewingthe paper from Abbott Nutrition. He has received fees forparticipation in review activities such as data monitoringboards, statistical analysis, and endpoint committees fromAbbott Nutrition International. He has received funding fortravel and accommodations from Abbott Nutrition.
Acknowledgments
The content of this paper was created and enriched solely bythe authors, tDNA task force members, through a processof the ongoing literature searches, independent contributionsand reviews, and group interactions for consensus. Financialsupport was provided by Abbott Nutrition Internationalthrough an educational grant. Editorial support was providedby Mediconnexions Consulting Sdn Bhd.
References
[1] J. E. Shaw, R. A. Sicree, and P. Z. Zimmet, “Global estimates ofthe prevalence of diabetes for 2010 and 2030,”Diabetes Researchand Clinical Practice, vol. 87, no. 1, pp. 4–14, 2010.
[2] D. R. Whiting, L. Guariguata, C. Weil, and J. Shaw, “IDFDiabetes Atlas: global estimates of the prevalence of diabetes for2011 and 2030,” Diabetes Research and Clinical Practice, vol. 94,no. 3, pp. 311–321, 2011.
[3] I. M. Feisul, “Current burden of diabetes in Malaysia,” in Pro-ceedings of the 1st National Institutes of Health (NIH) ScientificMeeting, Selangor, Malaysia, June 2012.
[4] G. R. Letchuman,W.M.WanNazaimoon,W. B.WanMohamadet al., “Prevalence of diabetes in the Malaysian National HealthMorbidity Survey III 2006,” The Medical Journal of Malaysia,vol. 65, no. 3, pp. 180–186, 2010.
[5] R. Huxley, W. P. T. James, F. Barzi et al., “Ethnic comparisons ofthe cross-sectional relationships betweenmeasures of body sizewith diabetes and hypertension,” Obesity Reviews, vol. 9, no. 1,pp. 53–61, 2008.
[6] K.-H. Yoon, J.-H. Lee, J.-W. Kim et al., “Epidemic obesity andtype 2 diabetes in Asia,”The Lancet, vol. 368, no. 9548, pp. 1681–1688, 2006.
[7] S.-C. Chiang, J.-K. Lee, C.-H. Chen et al., “Justifying the highprevalence of microalbuminuria for type 2 diabetic patients inTaiwan with conditional probability approach-a DEMAND IIStudy,” Journal of the Chinese Medical Association, vol. 74, no. 1,pp. 3–10, 2011.
[8] A. Y. T. Wu, N. C. T. Kong, F. A. De Leon et al., “An alarminglyhigh prevalence of diabetic nephropathy inAsian type 2 diabeticpatients: the MicroAlbuminuria Prevalence (MAP) Study,”Diabetologia, vol. 48, no. 1, pp. 17–26, 2005.
[9] L.-M. Chuang, S. T. Tsai, B. Y. Huang, and T. Y. Tai, “The statusof diabetes control in Asia—a cross-sectional survey of 24 317patients with diabetes mellitus in 1998,” Diabetic Medicine, vol.19, no. 12, pp. 978–985, 2002.
[10] J.-S. Wang, S.-T. Tu, I.-T. Lee et al., “Contribution of post-prandial glucose to excess hyperglycaemia in Asian type 2diabetic patients using continuous glucose monitoring,” Dia-betes/Metabolism Research and Reviews, vol. 27, no. 1, pp. 79–84,2011.
[11] J. I. Mechanick, A. E. Marchetti, C. Apovian et al., “Diabetes-specific nutrition algorithm: a transcultural program to opti-mize diabetes and prediabetes care,” Current Diabetes Reports,vol. 12, no. 2, pp. 180–194, 2012.
[12] Ministry of Health Malaysia, “Malaysian Clinical PracticeGuidelines for the Management of Type 2 Diabetes Mellitus,”2009, http://www.acadmed.org.my/.
[13] W. N. W. Mohamud, A. A.-S. Ismail, A. S. M. Khir et al.,“Prevalence of metabolic syndrome and its risk factors in adultMalaysians: results of a nationwide survey,” Diabetes Researchand Clinical Practice, vol. 96, no. 1, pp. 91–97, 2012.
[14] M. Zaki, Z. Robaayah, S. P. Chan, M. Vadivale, and T. O. Lim,“Malaysia Shape of the Nation (MySoN): a primary care basedstudy of abdominal obesity in Malaysia,”TheMedical Journal ofMalaysia, vol. 65, pp. 143–149, 2010.
[15] M. Mafauzy, Z. Hussein, and S. P. Chan, “The status of diabetescontrol in Malaysia: results of diabcare 2008,” Medical Journalof Malaysia, vol. 66, no. 3, pp. 175–181, 2011.
[16] M. Mohamed, “An audit on diabetes management in Asianpatients treated by specialists: the Diabcare-Asia 1998 and 2003studies,” Current Medical Research and Opinion, vol. 24, no. 2,pp. 507–514, 2008.
[17] B. H. Chew, I. Mastura, P. Y. Lee, T. Sri Wahyu, A. T. Cheong,and A. Zaiton, “Ethnic differences in glycaemic control andcomplications: the adult diabetes control and management(ADCM), Malaysia,” Medical Journal of Malaysia, vol. 66, no.3, pp. 244–248, 2011.
[18] Ministry of Health Malaysia, “Malaysian Clinical PracticeGuidelines for theManagement of Hypertension (3rd Edition),”2008, http://www.acadmed.org.my/.
[19] “Ministry of Health MalaysiaClinical Practice Guidelines onManagement of Dyslipidaemia 3rd Edition,” 2004, http://www.acadmed.org.my/.
[20] S. L. Tan, S. Juliana, andH. Sakinah, “Dietary compliance and itsassociationwith glycemic control among poorly controlled type2 diabetic outpatients in Hospital Universiti Sains Malaysia,”Malaysian Journal of Nutrition, vol. 17, no. 3, pp. 287–299, 2011.
[21] M. Y. Tan and J. Magarey, “Self-care practices of Malaysianadultswith diabetes and sub-optimal glycaemic control,”PatientEducation and Counseling, vol. 72, no. 2, pp. 252–267, 2008.

International Journal of Endocrinology 7
[22] S. R. Joshi, V. Mohan, S. S. Joshi, J. I. Mechanick, and A. Mar-chetti, “Transcultural diabetes nutrition therapy algorithm: theAsian indian application,” Current Diabetes Reports, vol. 12, no.2, pp. 204–212, 2012.
[23] H.-Y. Su, M.-W. Tsang, S.-Y. Huang, J. I. Mechanick, W. H.-H. Sheu, and A. Marchetti, “Transculturalization of a diabetes-specific nutrition algorithm: Asian application,” Current Dia-betes Reports, vol. 12, no. 2, pp. 213–219, 2012.
[24] World Health Organization, International Association for theStudy of Obesity, and International Obesity Taskforce. The Asia-Pacific Perspective: Redefining Obesity and Its Treatment, HealthCommunications, Sydney, Australia, 2000.
[25] WHO Expert Consultation, “Appropriate body-mass index forAsian populations and its implications for policy and interven-tion strategies,”TheLancet, vol. 363, no. 9403, pp. 157–163, 2004.
[26] S. Low, M. C. Chin, M. Stefan, D. Heng, and M. Deurenberg-Yap, “Rationale for redefining obesity in asians,” Annals of theAcademy of Medicine Singapore, vol. 38, no. 1, pp. 66–69, 2009.
[27] J. I. Mechanick, P. M. Camacho, R. H. Cobin et al., “AmericanAssociation of Clinical Endocrinologists protocol for standard-ized production of clinical practice guidelines—2010 update,”Endocrine Practice, vol. 16, no. 2, pp. 270–283, 2010.
[28] Ministry of Health Malaysia, “Clinical Practice Guidelines onManagement of Obesity,” 2004, http://www.acadmed.org.my/.
[29] M. Riddell and B. A. Perkins, “Exercise and glucose metabolismin persons with diabetes mellitus: perspectives on the role forcontinuous glucosemonitoring,” Journal of Diabetes Science andTechnology, vol. 3, no. 4, pp. 914–923, 2009.
[30] R. J. Sigal, G. P. Kenny, D. H. Wasserman, and C. Castaneda-Sceppa, “Physical activity/exercise and type 2 diabetes,”DiabetesCare, vol. 27, no. 10, pp. 2518–2539, 2004.
[31] N. G. Boule, E. Haddad, G. P. Kenny, G. A.Wells, and R. J. Sigal,“Effects of exercise on glycemic control and body mass in type2 diabetes mellitus: a meta-analysis of controlled clinical trials,”Journal of the AmericanMedical Association, vol. 286, no. 10, pp.1218–1227, 2001.
[32] G. Li, P. Zhang, J. Wang et al., “The long-term effect of lifestyleinterventions to prevent diabetes in theChinaDaQingDiabetesPrevention Study: a 20-year follow-up study,” The Lancet, vol.371, no. 9626, pp. 1783–1789, 2008.
[33] T. S. Church, S. N. Blair, S. Cocreham et al., “Effects of aerobicand resistance training on hemoglobin A1c levels in patientswith type 2 diabetes: a randomized controlled trial,” Journal ofthe American Medical Association, vol. 304, no. 20, pp. 2253–2262, 2010.
[34] D. Umpierre, P. A. B. Ribeiro, C. K. Kramer et al., “Physical ac-tivity advice only or structured exercise training and associationwith HbA1c levels in type 2 diabetes: a systematic review andmeta-analysis,” Journal of the AmericanMedical Association, vol.305, no. 17, pp. 1790–1799, 2011.
[35] American Diabetes Association, “Standards of medical care indiabetes—2013,” Diabetes Care, vol. 36, supplement 1, pp. S11–S66, 2013.
[36] M.-C. Huang, C.-C. Hsu, H.-S. Wang, and S.-J. Shin, “Prospec-tive randomized controlled trial to evaluate effectiveness ofregistered dietitian-led diabetes management on glycemic anddiet control in a primary care setting in Taiwan,” Diabetes Care,vol. 33, no. 2, pp. 233–239, 2010.
[37] K.-W. Liang, W.-J. Lee, I.-T. Lee et al., “Persistent elevation ofparaoxonase-1 specific enzyme activity after weight reductionin obese non-diabetic men with metabolic syndrome,” ClinicaChimica Acta, vol. 412, no. 19-20, pp. 1835–1841, 2011.
[38] W. H.-H. Sheu, T.-M. Chang, W.-J. Lee et al., “Effect of weightloss on proinflammatory state of mononuclear cells in obesewomen,” Obesity, vol. 16, no. 5, pp. 1033–1038, 2008.
[39] H.-F. Lang, C.-Y. Chou, W. H.-H. Sheu, and J.-Y. Lin, “Weightloss increased serum adiponectin but decreased lipid levels inobese subjects whose bodymass index was lower than 30 kg/m2,” Nutrition Research, vol. 31, no. 5, pp. 378–386, 2011.
[40] N. Sakane, J. Sato, K. Tsushita et al., “Prevention of type 2diabetes in a primary healthcare setting: three-year results oflifestyle intervention in Japanese subjects with impaired glucosetolerance,” BMC Public Health, vol. 11, article 40, 2011.
[41] T. Saito, M. Watanabe, J. Nishida et al., “Lifestyle modificationand prevention of type 2 diabetes in overweight Japanese withimpaired fasting glucose levels: a randomized controlled trial,”Archives of InternalMedicine, vol. 171, no. 15, pp. 1352–1360, 2011.
[42] Malaysian Dietitians’ Association, “Medical Nutrition TherapyGuidelines for Type 2 Diabetes,” 2005.
[43] Malaysian Dietitians’ Association, “Medical Nutrition TherapyGuidelines for Type 2 Diabetes,” 2013.
[44] G. Mazzali, V. Di Francesco, E. Zoico et al., “Interrelationsbetween fat distribution, muscle lipid content, adipocytokines,and insulin resistance: effect of moderate weight loss in olderwomen,” American Journal of Clinical Nutrition, vol. 84, no. 5,pp. 1193–1199, 2006.
[45] K. Esposito, A. Pontillo, C. Di Palo et al., “Effect of weight lossand lifestyle changes on vascular inflammatory markers inobesewomen: a randomized trial,” Journal of theAmericanMed-ical Association, vol. 289, no. 14, pp. 1799–1804, 2003.
[46] B.H. Chew,M. Ismail, S. Shariff-Ghazali et al., “Determinants ofuncontrolled hypertension in adult type 2 diabetes mellitus: ananalysis of theMalaysian diabetes registry 2009,”CardiovascularDiabetology, vol. 11, no. 1, p. 54, 2012.
[47] B. H. Chew, M. Ismail, P. Y. Lee et al., “Determinants of uncon-trolled dyslipidaemia among adult type 2 diabetes in Malaysia:the Malaysian Diabetes Registry 2009,” Diabetes Research andClinical Practice, vol. 96, no. 3, pp. 339–347, 2012.
[48] K. A.-A. Ahmed, S. Muniandy, I. S. Ismail, R. S. Ali, and Z. H.Alhamodi, “Evaluation of N𝜀-(carboxymethyl)lysine and lipidperoxidation in multiethnic Malaysian subjects with type 2diabetes mellitus,” Scientific Research and Essays, vol. 6, no. 9,pp. 1957–1962, 2011.
[49] Ministry of Health Malaysia, “Clinical Practice Guidelines onManagement of Chronic Kidney Disease in Adults,” 2011.

Submit your manuscripts athttp://www.hindawi.com
Stem CellsInternational
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
MEDIATORSINFLAMMATION
of
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Behavioural Neurology
EndocrinologyInternational Journal of
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Disease Markers
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
BioMed Research International
OncologyJournal of
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Oxidative Medicine and Cellular Longevity
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
PPAR Research
The Scientific World JournalHindawi Publishing Corporation http://www.hindawi.com Volume 2014
Immunology ResearchHindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Journal of
ObesityJournal of
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Computational and Mathematical Methods in Medicine
OphthalmologyJournal of
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Diabetes ResearchJournal of
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Research and TreatmentAIDS
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Gastroenterology Research and Practice
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Parkinson’s Disease
Evidence-Based Complementary and Alternative Medicine
Volume 2014Hindawi Publishing Corporationhttp://www.hindawi.com