REVIEW ARTICLE - Stanford Medicinemed.stanford.edu/.../Periop_Mgt_Emphysema.pdfFig 1. A model of the...
Transcript of REVIEW ARTICLE - Stanford Medicinemed.stanford.edu/.../Periop_Mgt_Emphysema.pdfFig 1. A model of the...

REVIEW ARTICLEMartin J. London, MD
Section Editor
The Perioperative Management of Patients With Severe Emphysema
Katherine P. Grichnik, MD, and Steven E. Hill, MD
SEVERE EMPHYSEMA IS A frequent coexistent conditionin surgical patients. It is a chronic obstructive pulmonary
disease (COPD), part of a heterogenous group of diseases thatalso includes chronic bronchitis and asthma; COPD is charac-terized by airflow obstruction and hyperinflation.1 Specifically,emphysema is anatomically defined by “abnormal, permanentenlargement of airspaces distal to the terminal bronchiole,accompanied by the destruction of their walls, and withoutobvious fibrosis.”2 More than 2.9 million people in the UnitedStates are affected by emphysema, and 13,000 people die eachyear.3,4 Patients are more likely to be older, male, and at thetime of diagnosis have commonly lost 50% to 70% of their lungfunction.4-7 Optimal perioperative anesthetic care requires re-view of the anatomy and pathophysiology of emphysema,knowledge of the therapeutic options, understanding the reac-tions of emphysema patients to surgical and anesthetic proce-dures, and an awareness of common perioperative problems.
ANATOMY AND PHYSIOLOGY OF PULMONARYEMPHYSEMA
Definitions/Anatomy
Anatomically, the bronchiole is divided into the lobularbronchiolus, the terminal bronchiolus, and the respiratory bron-chiolus8 (Fig 1). Emphysema is limited to the gas exchangingacinus consisting of the respiratory bronchiolus, the alveolarduct, and the alveolus itself. Pathologically, there are 5 recog-nized types of emphysema (Table 1).1,8-10
Primary etiologies for emphysema include tobacco use and�-1 antitrypsin deficiency. However, industrial exposure totoxins, air pollution, and recurrent prior respiratory illnessesmay also lead to emphysema.11 Pathologically, lung tissue may
be injured by proteinases12 (elastases) released from neutro-phils and alveolar macrophages, which are normally neutral-ized by antielastase inhibitors such as �-1 antitrypsin. Animbalance of elastase release (stimulated by smoking, infec-tion, and industrial exposure) to antielastase inhibitor produc-tion (�-1 antitrypsin deficiency or oxidative damage to �-1antitrypsin from smoke inhalation) can lead to lung tissueinjury and subsequent emphysema. Animal studies support thistheory as the experimental inhalation of exogenous elastase andcollagenase result in acinar destruction, remarkably similar tohuman emphysema.13
Other evidence suggests that a more intricate process ofpulmonary remodeling also occurs.14 Pathologic loss of tissuetensile strength because of bioengineering or structural fatiguein repetitively stressed tissues is postulated.15 Chronic inflam-mation may also play a role, mediated by different pathwayscompared with asthma.16,17 Macrophages, cytotoxic T cells, andneutrophils are found in bronchial biopsies and bronchoalveo-lar lavage; they can release proteases to break down connectivetissue in lung parenchyma.18-20 Additionally, COPD patientshave increased hydrogen peroxide concentrations in exhaledbreath condensates and increased breath and urinary concen-trations of 8-isoprostane, a marker for oxidative stress,21-23
which can promote COPD through enhancement of inflamma-tion and proteolytic injury.24,25
Physiology
The pathophysiology of emphysema is based on airflowobstruction9,10,26 because of decreased elastic recoil from lossof elastin, collagen, and surfactant at the level of the alveolus.Loss of structural protein from small airways produces dy-namic airway collapse on expiration. Airway inflammation,bronchospasm, and increased secretions additionally increaseairway resistance. The end result is delayed lung emptyingleading to increased lung volumes, mechanical compromise ofthe diaphragm, and markedly increased work of breathing. Theclinical consequence is incomplete exhalation with resultingintrinsic positive end-expiratory pressure (auto-PEEP) or dy-namic pulmonary hyperinflation (DPH) caused by retained gasvolume in the lungs. These phenomena can happen in patientswith normal lungs when mechanically ventilated at high rates,but are especially characteristic of patients with emphysemaduring mechanical ventilation.27
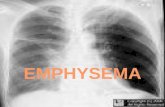
Patients with emphysema have chest radiographs character-ized by hyperinflated lungs, a flattened diaphragm, an increasedanterior-to-posterior diameter, an elevated rib cage, and a small
From the Department of Anesthesiology, Division of CardiothoracicAnesthesia, Duke Heart Center, Duke University Health Care Systems,Durham, NC.
Presented in part at the 23rd Annual Society of CardiovascularAnesthesiologist Meeting, Vancouver, British Columbia, Canada, May5-8, 2001.
Address reprint requests to Katherine P. Grichnik MD, Departmentof Anesthesiology, Duke University Health Care Systems, Box 3094,Durham, NC 27710, 919-681-6893. E-mail: [email protected]
© 2003 Elsevier Inc. All rights reserved.1053-0770/03/1703-0001$30.00/0doi:10.1016/S1053-0770(03)00059-4Key words: emphysema, anesthesia, lung volume reduction surgery,
dynamic pulmonary hyperinflation, barotrauma, pulmonary edema
364 Journal of Cardiothoracic and Vascular Anesthesia, Vol 17, No 3 (June), 2003: pp 364-387

vertical heart (Fig 2).28 Emphysema is often heterogenouslydistributed with asymmetric bullae formation or lobar predom-inance of emphysematous tissue (Fig 3). Clinically, pulmonaryfunction tests are characterized by a ratio of forced expiratoryvolume in 1 second (FEV1) to forced vital capacity (FVC) of�70%, a decreased diffusion capacity for carbon monoxide
(DLCO), an increased residual volume (RV), an increased func-tional residual capacity (FRC), and an increased total lungcapacity (TLC).29,30 Gas exchange is typically impaired withdecreased arterial oxygen tension and increased arterial carbondioxide tension. Etiologies for abnormal gas exchange includeventilation-to-perfusion mismatch, increased physiologic dead-
Fig 1. A model of the lung illustrating the types of emphysema. A�centriacinar emphysema, B�paraseptal emphysema, C�panacinar
emphysema, D�irregular or scar emphysema. Reprinted with permission.8
Table 1. The Characteristics of the Types of Emphysema
Type ofEmphysema Airway Location
Upper VersusLower Lung Heterogeneity Miscellaneous
Centrilobular Proximal Upper Heterogenous Associated with tobaccoPanacinar Throughout Lower Uniform Associated with alpha-1 antitrypsin
deficiencyParaseptal Periphery Both Heterogenous Increased spontaneous pneumothoraxIrregular Periphery primarily arises
in scar tissueBoth Heterogenous Arises in scar tissue
Bullous Peripheral Both Heterogenous Abnormally large airspace enlargement(�1 cm) in focal areas
365SEVERE EMPHYSEMA

space, increased work of breathing, decreased diaphragmaticfunction, and diminished diffusion capacity between the alve-olus and the microvasculature. Physiologically, patients mayhave pulmonary hypertension, elevated right ventricular (RV)dimensions, elevated RV diastolic pressures, and depressed RVejection fractions.31
Expected declines in pulmonary function occur over timeincluding decreases in FEV1 (average of 15-30 mL/yr), DLCO,and arterial oxygen and carbon dioxide tensions.32-34 Determi-nants of survival include age, arterial oxygen tension, andpostbronchodilator FEV1 at the time of diagnosis.33-38 Longi-tudinal studies report a 60% 10-year mortality after the diag-nosis of emphysema (Fig 4).33,35,39
MEDICAL AND SURGICAL THERAPIES
Medical Treatment
The goals of medical therapy for emphysema are to retardchronic disease progression, treat acute exacerbations40 andcontrol symptoms to improve quality of life (QOL).20,41 Med-ical management includes patient education and risk factoridentification,42 avoidance of environmental toxins or causativeagents (tobacco),43 prevention of infection, graded exercise andpulmonary toilet instruction,44 and pharmacologic treatment.45
Effective medications include bronchodilators (�-adrenergicagonists and anticholinergics),46 but the role of methylxan-thines is unclear with conflicting evidence for efficacy.47-51
Corticosteroid therapy is commonly used to treat acute diseaseexacerbations;52 there is no role for chronic inhaled adminis-tration to reduce disease progression as initially postulated.53-56
Antibiotic therapy is also indicated for acute disease exacerba-tion with purulent sputum production,57,58 and vaccinationagainst pneumococcal disease and influenza is recommended.59
Psychoactive drugs such as bupropion hydrochloride may aidin smoking cessation.60 Intravenous �-1 antitrypsin supplemen-tation is used to replace intravascular levels in the �-1 anti-trypsin-deficient patient, but it is unclear if this therapy pre-vents disease progression.61-63 Low-flow oxygen can improveexercise tolerance and quality of life and is the only medicaltherapy shown to improve survival in hypoxemic patients.64
New agents include leukotriene-receptor antagonists, drugswith anti-inflammatory and bronchodilating properties.65 Theyare currently indicated for asthma but may become useful foremphysema as well. Potential future therapy includes the de-velopment of antagonists to postulated cellular mediators ofemphysema, increased types of protease inhibitor agents, andmore specific anti-inflammatory drugs.66,67
Surgical Treatment: Lung Volume Reduction Surgery
Because medical therapy has been relatively ineffective inhalting the progression of emphysema, others have turned tosurgical attempts to both palliate and treat this disease.68-72
Early maneuvers included costrochondrectomy and transversesternotomy to improve thoracic mobility.73 With the under-standing that thoracic distention was the result of and not thecause of emphysema, others attempted to limit lung expansionwith thoracoplasty and phrenectomy or elevate the diaphragmwith pneumoperitoneum and abdominal constrictive belts.74-77
Procedures such as tracheal stents to stabilize the posteriormembranous trachea in expiration and denervation to relievebronchospasm and mucus formation have also been tried.78-83
These procedures were associated with high morbidity andunpredictable results.
The concept of anatomic surgical resection of nonfunctionallung tissue was introduced in the 1940s70 but was not com-monly performed until 1957, when Brantigan and Mueller
Fig 3. Chest computed tomography of a patient with severe em-
physema demonstrating peripheral bullous disease, right greater
than left.
Fig 2. Chest radiograph of a patient with severe emphysema
demonstrating lung hyperinflation, flattened diaphragms and a small
vertical heart.
366 GRICHNIK AND HILL

advocated bullectomy to treat emphysema.84,85 Although 75%of patients derived a clinical benefit from the procedure, therewas also a high mortality (18%) and a lack of objective data,preventing wide acceptance. Thirty years later, Cooper, Wak-abayashi, and Eugene86-89 revitalized this procedure with anoperation now known as lung volume reduction surgery(LVRS). The operation involves resection of 20% to 30% ofhyperinflated lung that should be noncontributory to effectiveventilation. Proposed benefits are improvement in elastic recoil,lung compliance, and chest wall conformation to reduce hyper-inflation and allow the resumption of a more normal diaphrag-matic position. Additionally, enhanced ventilation-to-perfusionmatching should occur in the remaining lung tissue to result inclinical improvements in pulmonary function.87-97
Initial studies reported significantly positive clinical re-sults,87,98 which led to LVRS being performed by many sur-geons worldwide.99 Short-term results from many nonrandom-ized studies and case series have been reported, most showingreduced hyperinflation and improved pulmonary function, ven-tilatory mechanics and exercise tolerance at 3 to 6 months afterprocedure.91,100-105 (Outcomes from 180 studies [1995-1999]have been well reviewed by Flaherty and Martinez.106) How-ever, only 4 randomized trials of lung volume reduction surgeryversus medical management have been reported and are pre-sented in Table 2.107-110
Others reported less significant clinical benefit and consid-erable morbidity including prolonged postoperative air leaks(greater than 7 days with some requiring reoperation), subcu-taneous emphysema (Fig 5A and B), pneumonia, pneumotho-rax, prolonged mechanical ventilation because of respiratoryfailure (reintubation rate of 19%-33%), arrhythmias, and gas-trointestinal dysfunction.111-115 Cardiac and cerebrovascularcomplications have also been reported.116,117
Mortality from this procedure may also be high. Initial30-day mortalities were reported to be 0% to 15% and causes
Fig 4. Comparison of 10-year survival rates in three groups of
subjects with chronic airway obstruction. Group I subjects had asth-
matic bronchitis, Group II subjects had mixed features of various
disease states including chronic bronchitis, asthma and emphysema,
Group III subjects had the emphysematous form of COPD. Copyright
© 1987 Massachusetts Medical Society. All rights reserved. Repro-
duced with permission.33
Table 2. Selected Controlled Studies of LVRS Versus Medical Therapy
BaselineValues 30 Day 3 Months to 6 Months 12 Months 24 Months
36Months
Study Variable No. Age FEV1
WalkTest
Mortality%
No.F/U FEV1
WalkTest
Mortality%
No.F/U FEV1
WalkTest
Mortality%
No.F/U FEV1
WalkTest
Mortality%
Mortality%
Criner108 BilateralMS
19 59 0.69 260 6* 15/19 0.85 321 9.4*
Medical 18 58.8 0.72 273 N/R 15/18 0.82 303 N/R
Geddes107 BilateralMS
23 62 0.74 210 17/6† 19/23 0.91 260 21 13/23 0.84 290 N/R
Medical 24 60 0.75 220 N/R 23/24 0.7 230 12 19/24 0.74 205 N/R
Meyers109 BilateralMS
65 66 0.58 249 N/R 51/65 0.87 11 45/65 0.91 15 17
Medical 22 65 0.62 264 N/R 22/22 0.52 0 17/22 0.57 20 46
Pompeo110 Uni- orbilateralMS
30 61.9 0.86 380 3.3 30/30 1.32 473 6.6 28/30 13.3
Medical 30 64.1 0.83 376 0 30/30 0.84 407 3.3 27/30 14.8
Abbreviations: LVRS, lung volume reduction surgery; No., number of patients; FEV1, forced vital capacity in 1 second; Walk test, 6-minute walktest or shuttle-walk test in meters; No. F/U, number of patients followed up as a fraction of the number of patients at baseline; bilateral MS,bilateral median sternotomy lung volume reduction surgery; Uni, unilateral; medical, medical management; N/R, not reported.
*In this crossover study, 1 patient died before surgery, and 13 patients crossed over to surgery after completion of the medical arm†Initial high mortality noted (5/15) with patients with very low DLCO and walk distance. Inclusion criteria were subsequently modified to exclude
these patients. 17% includes these patients and 6% does not.Adapted with permission.104
367SEVERE EMPHYSEMA

included respiratory failure, cardiac failure, sepsis, multiorganfailure, pneumonia, acute respiratory distress syndrome, andaspiration.113 There are limited long-term mortality data, withthe few studies reporting 18% to 68% mortality at 3 to 5 years(Table 3); causes additionally include cancer, suicide, gastro-intestinal bleeding, and pulmonary embolus.118
A review of 711 Medicare claims in 1995 revealed LVRSpatients suffered from prolonged hospital length of stay, a highreadmission rate, and high use of rehabilitation services.119,120
Review of the published data and data requested from centersperforming the surgery determined that the reported results
were compromised by small patient numbers, inadequate con-trols with variability in patient selection, baseline assessments,perioperative care, the type of surgery performed, definitions ofadverse outcomes, and duration of follow-up.120 In 1 study,60% of LVRS patients did not return for follow-up after sur-gery; it was discovered that 27% of the nonreturn patients haddied as compared with 3% of the patients who returned.120,121
The cost of LVRS was also considered. At a reimbursementrate of $31,398 per procedure, it was estimated that if LVRSwere performed on every eligible Medicare beneficiary thatalmost 1 billion dollars would be spent.122 Thus, the role andexpenses of LVRS were questioned, and, in January 1996,Medicare stopped funding for this procedure, citing inadequateevidence for efficacy and long-term benefit.123
Subsequently, a multicenter randomized prospective clinicaltrial has been designed and supported by the National Heart,Lung and Blood Institute, the Health Care and Finance Orga-nization (now known as the Centers for Medicare and MedicaidServices), and the Agency for Health Care Policy and Re-search.120,124,125 The purpose of the National Emphysema Treat-ment Trial (NETT) is to determine (1) whether surgical ormedical therapy is more efficacious for patients with emphy-sema with respect to short- and long-term improvement ofpulmonary function and quality of life, (2) whether differentsurgical approaches (median sternotomy or thoracoscopy) areassociated with different outcomes, (3) the costs associatedwith this procedure over time.126 This trial was designed todefine who would and who would not benefit from LVRS.127-129
Similar studies are underway in Massachusetts (Overholt-BlueCross Emphysema Surgery Trial), Canada, and Great Brit-ain.104,130
Important concepts are emerging from the study of emphy-sema and the widely variable responses of patients to LVRS.The first NETT results examined 1033 patients and identified agroup of 69 patients at high risk of death compared withmedical management (relative risk [RR] � 3.9, 95%confidenceinterval [95%CI] � 1.9-9.0).131 They were patients with a lowpreoperative FEV1 and a uniform pattern of emphysema or alow DLCO. Others have also identified poor outcomes with ahomogenous distribution of emphysema,132,133 lower-lobeLVRS,118 a low DLCO, higher age, limited initial walk test,134
and pleural adhesions.107,114,116,135,136 In contrast, improved out-comes have been associated with emphysema heterogene-ity,133,137 upper- versus lower-lobe LVRS,118,137,138 bilateral ver-sus unilateral LVRS,103,139 and the use of buttressed staples forresection versus laser resection.140,141
Of concern is the finding that pulmonary function appears toimprove to maximal levels at 3 to 6 months and then re-gresses107,136,142,143 (Fig 6); in some, there was a correlationbetween the magnitude of short-term incremental improvementand the rate of deterioration in FEV1.144 When long-term datawere averaged, the rate of decline in FEV1 was 163 mL/y; itcould then be predicted that an average patient would return tobaseline FEV1 approximately 2 to 5 years postoperatively.These data suggest that surgery produced a one-time benefit butdid not modify the natural history of the disease. However, ithas been argued that the improved QOL with reduced dyspneais a long-lasting benefit of LVRS.103,145-148 QOL and dyspnea
Fig 5B. Subcutaneous emphysema after pulmonary surgery. Note
the prominent subcutaneous emphysema, especially on the right, in
the axillary tissue.
Fig 5A. Mechanism of soft-tissue emphysema following alveolar
disruption. Air from a torn alveolus (A) first enters perivascular in-
terstitium (B), dissection proximally within brochovascular sheath
toward the mediastinum (C). As mediastinal pressure rises, decom-
pression occurs in the cervical (D), subcutaneous and retroperitoneal
(E) soft-tissue spaces and may even cause pleural rupture producing
pneumothorax (F). Arrows indicate the direction of air movement.
Reprinted with permission.318
368 GRICHNIK AND HILL

may be independent of FEV1 changes and more dependent onimprovements in other domains of the respiratory system.26,149
Other findings have included the development of pulmonaryhypertension in some patients,150 the observation that the con-tralateral lung function can improve after unilateral lung reduc-tion,151 the finding of variable arterial blood gas effects,152 anda lack of difference between a sternotomy versus video-assistedthoracoscopic approach.153,154 Still controversial is the amountof lung to resect.155 Severe hypercapnea may not be a contra-indication as initially determined.93,156
Independent of the NETT trial, others have sought reliablepredictors of who will benefit from LVRS. Preoperativeimaging techniques have been used for risk assessment butare variable among surgical centers.133,157,158 Highly quan-titative assessment of computed tomography scans can mea-sure volume and severity of emphysema versus normallung;136,159-162 scoring systems to assess the heterogeneityof emphysema distribution are proposed to correlate withLVRS outcome variables.163 The radiologic pattern of emphy-sema may also be prognostic as patients with centrilobular
Fig 6. Change in forced expiratory volume in one second (mL) over time. The median changes in FEV1 were obtained by comparing the
responses of each subject with his or her baseline values. Twenty-four patients underwent LVRS (surgical group) and 24 patients underwent
medical rehabilitation (medical group). P values are for comparison of the surgical group to the medical group at each point. The bars show 95
percent confidence intervals. Note the initial improvement in FEV1 at 3 months for the surgical group, which subsequently declines at
approximately the same rate as the medical group. Reprinted with permission.108
Table 3. Selected Studies of Long-Term Survival After LVRS
Study Population TechniquePerioperative
Survival % 2 Year % 3 Year % 4 Year % 5 Year %
Flaherty136 89 from 1994-1998 Bilateral MS 30 day � 94.4 89 82Gelb111 26 patients in 1995 Bilateral
VATS180 day � 96 81 69 54 42
Naunheim113 330, from 1993-1998 UnilateralVATS
30 day � 94.8 75 69
343, from 1993-1998 BilateralVATS
30 day � 93 81 74
Yusen118 200 patients, from1993-1998
Bilateral MS 90 day � 95.5 87 82 74 71
Abbreviations: MS, median sternotomy; VATS, video-assisted thoracic surgery.
369SEVERE EMPHYSEMA

emphysema may benefit more than patients with panacinaremphysema.164
Mechanical lung function may be prognostic. Dueck et al166
examined the improvement of preoperative flow limitation afterLVRS as an indicator of reduced dynamic pulmonary hyperin-flation (DPH) and correlated it to postoperative reductions inFRC and FRC/TLC.165 Similarly, preoperative auto-PEEP wasfound to correlate with postoperative FEV1.166 Improved post-operative workload was associated with reductions in pulmo-nary resistance, auto-PEEP, and WOB.167 However, Ingenito etal168 found that only preoperative inspiratory resistance corre-lated inversely with improved FEV1 after surgery.
The use of LVRS in patients with undiagnosed pulmonarynodules and/or isolated lung cancer is controversial.169 Inpathologic analysis of tissue from LVRS patients, a wide rangeof abnormal tissue including adenocarcinoma, bronchoalveolarmetaplasia, and carcinoid tumorlets has been found in tissuefrom LVRS patients.170,171 DeRose et al advocated LVRS com-bined with nodule resection and reported recurrent cancer inonly 1 of 14 patients at 1 year.172
Although the role of LVRS is not firmly established, it is alsobeing used in combination with other procedures to allowsurgery for patients deemed inoperable because of the severityof emphysema. LVRS has been performed in conjunction withcoronary artery bypass surgery, cardiac valvular surgery, andaortic aneurysm surgery.173-175
Future results from the NETT trial and similar trials in othercountries will clarify the questions of safety, efficacy, and costof LVRS surgery with emphasis on prognostic markers toidentify patients most able to benefit from the procedure.
Surgical Treatment: Lung Transplantation
The only other surgical alternative for treatment of severeemphysema is lung transplantation (LT), usually reserved forpatients not expected to live more than 2 years.13,176-178 Ingeneral, patients considered for LT have similar expiratory flowvolumes (FEV1 less than 30% predicted) to LVRS candidates;patients with relative contraindications to LVRS (such as ho-mogenous lung disease) may be considered for LT.178 Optimalcandidate selection criteria are presented in Table 4.
Thirty-nine percent of the total lung transplants performedfrom 1995 to 2001 were to treat COPD/emphysema using bothsingle and bilateral lung transplants (SLT, BLT).179-181 SLT isperformed most frequently to allocate the precious resource ofdonor lungs.176 However, BLT for emphysema may have anadvantage of preventing the remaining native emphysematouslung from “crowding out” the newly transplanted normal lungand may have better long-term outcomes.181
The major benefit of LT is that a patient can achieve near-normal lung function posttransplant, especially for BLT.181,182
Maximal gains in FVC and FEV1 occur 6-12 months afterLT181 in contrast to LVRS, at which time decline in lungfunction may be occurring. If lung function does decline, it isusually related to infection or rejection, not native diseaseprogression.183 BLT is characterized by normal spirometry,oxygenation, and ventilation with resolution of thoracic hyper-inflation; a mild restrictive defect may remain.184,185 SLT pul-monary function differs because of the physiologic interactionwith the native diseased lung; acutely, mediastinal shift mayoccur with hemodynamic compromise. Chronically, a biphasicexpiratory flow pattern is observed with high initial flow fromthe transplanted lung followed by slower terminal flow fromthe native diseased lung;178,186 hyperinflation of the thorax mayremain.187,188 Interestingly, the curvature of the diaphragm onthe transplanted side may return to normal with abnormalitiesremaining on the contralateral side.189 Despite these limitations,marked clinical and spirometric improvements (FEV1 im-proved from 0.49 L, 16% predicted to 1.6 L, 54% predicted) in1 study190 are seen; SLT recipients perform as well as BLTrecipients in some exercise testing.191
Potential complications of LT are multiple including acuteand chronic rejection, infection, primary organ dysfunction,development of bronchial strictures, gastroparesis, and thegradual development of obliterative bronchiolitis.192-195 Uniqueto SLT are (1) unchanged hyperinflation of the nativelung,196,197 (2) large ventilation-to-perfusion defect if severereperfusion injury of the transplanted lung occurs,198 and (3)lesions from the native lung (carcinoma, tuberculosis reactiva-tion, and infectious contamination) affecting the transplantedlung.178,179
Table 4. Selection Criteria for Lung Transplantation in Patients With Emphysema
Indications Contraindications Relative Contraindications
Severe emphysema, distribution less important Unresolved substance abuse Coronary artery diseaseFEV1 �30% predicted Severe coronary artery disease Mild renal insufficiencyRapid decline in oxygenation, ventilation Left ventricular dysfunction OsteoporosisDevelopment of secondary pulmonary hypertension Severe renal insufficiencySLT �65 years Hepatic dysfunctionBLT �60 years Active or recent cancer (except skin cancer)Ambulatory Viral infection with HIV, Hep B, Hep CBody weight 70-130% of ideal Acute illnessSix minute walk test �300 meters Mechanical ventilation*Global psychosocial risk assessment adequate
Abbreviations: FEV1, forced expiratory volume in 1 second; SLT, single-lung transplant; BLT, bilateral lung transplant; HIV, human immuno-deficiency virus; Hep B, hepatitis B virus; Hep C, hepatitis C virus; BiPAP, biphasic positive airway pressure. Data in table from Schulman.177
*Ambulatory patients with tracheotomy for nocturnal ventilation and patients using noninvasive ventilation such as BiPAP masks areacceptable candidates.
370 GRICHNIK AND HILL

Perioperative mortality is 7% to 10%,178 and overall survivalfor lung transplantation in COPD/emphysema patients isgreater than 25% at 7 years with patients receiving bilaterallungs having a survival advantage (Fig 7).179 Early mortality isusually from infection or primary graft failure,179 and latemortality is usually from bronchiolitis obliterans or infec-tion.179,200 As with LVRS, the relative survival risk of LT foremphysema versus medical therapy has been questioned.Hosenpud et al201 compared survival after LT (65% at 3 years)versus survival of patients on the waiting list for LT (70% at 3years) and found that the relative risk of LT for emphysemanever dropped below the risk of waiting. However, the analysismay be confounded by the common practice of placing patientson a lung transplant waiting list in anticipation of needing atransplant after a long waiting period.178 The health-relatedQOL was also not examined; similar to LVRS, patients aftertransplant report significant improvements in wellbeing.202
Because organ supply is limited and waiting time for LTcandidates continues to increase, LVRS versus LT has beenexamined. In a comparison of SLT, BLT, and LVRS, superiorpulmonary function was found with LT: 79% improvement inFEV1 after LVRS versus 231% after SLT and 498% after BLT;similar results in exercise tests and oxygenation were reported.203
LVRS was performed on 20 patients awaiting LT; 95% sur-vived at 32 months and 75% improved enough not to need
LT.204 Similarly, Meyers et al performed LVRS on 99 patientspotentially eligible for LT; 59% of survivors did not need to belisted for LT.205 Cost must also be considered: LVRS costsapproximately $31,000 with few postprocedural expenses,whereas lung transplantation costs $108,000 with an estimated$1000/month medication cost.206 Other considerations forLVRS versus LT include the age of the patient, the risks ofimmunosuppression and comorbid conditions that could ex-clude a patient from transplantation but not from LVRS (eg,pulmonary nodule);204,207 LVRS has been performed before LTas a bridge to transplant208 or at the time of SLT to prevent/treathyperinflation of the remaining native lung.209,210 Salvage ofrespiratory function by LVRS has been attempted in patientswith SLT who are incapacitated by bronchiolitis obliterans.211
ANESTHETIC, HEMODYNAMIC AND VENTILATORYMANAGEMENT OF THE PATIENT WITH EMPHYSEMA
Preoperative Evaluation
Initial preoperative inspection should assess the adequacy ofprior medical management as determined by optimization ofmedications, pulmonary toilet, and pulmonary rehabilitation.Absence of concurrent infection will augment a limited abilityto clear secretions postoperatively. Review of prior steroid usemay determine the need for use of steroids intraoperatively.
Fig 7. Survival after lung transplantation for COPD/emphysema: Adapted from the International Society for Heart and Lung Transplantation
1994-2001 data.178
371SEVERE EMPHYSEMA

Preoperative arterial blood gas analysis and pulmonary func-tion testing with and without bronchodilators can both deter-mine the sufficiency of medical therapy and assist in riskassessment.
Patients with severe COPD are at higher risk of seriouspostoperative pulmonary complications compared to patientswith mild COPD or no COPD (relative risk from 2.7 to 4.7).212-216
Additionally, upper abdominal and thoracic surgery are inde-pendently associated with decline in pulmonary function with a10% to 40% risk of postoperative pulmonary complica-tions.212,217 The value of spirometry, split lung function testsand mimicry of postoperative conditions have also been used toassess perioperative respiratory risk, as promulgated in manyanesthesia textbooks (Table 5).218,219 It has been suggested thatincreased risk is associated with an FEV1 or FVC less than 50%to 70% of predicted value or a ratio of FEV1 to FVC of lessthan 65%.220,221 However, such risk tables were constructedfrom methodologically flawed studies,222 use data acquiredabout thoracic surgical outcomes before improvements in an-esthetic care and surgical technique,223 and do not address therole of exercise tolerance in risk assessment.
Spirometry has been found to have a variable predictivevalue (RR of an abnormal finding from 0.9 to 4.0)212 and is notbetter than clinical findings in the prediction of respiratorycomplications.213,224-226 The use of a “risk score” such as thecardiorespiratory risk index is also not reliable.227 However, thecalculation of a predicted postoperative (ppo) FEV1 based onthe amount of lung to be resected may correlate with pulmo-
nary complications.228 Some also found preoperative partialpressure of arterial carbon dioxide (PACO2) �45 mmHg to bea predictor of risk.229,230 Exercise tolerance has been advocatedas one of the best predictors of pulmonary outcomes aftersurgical procedures.231-235
Slinger and Johnston236 have addressed the above concernsin a novel approach to risk stratification. They propose evalu-ation in three domains: respiratory mechanical function, car-diopulmonary reserve, and lung parenchymal function, anddescribe the most valid test(s) for prediction of respiratory riskin each.
Respiratory mechanical function is most accurately evalu-ated by the predicted postoperative FEV1 (ppo FEV1 in L �preop FEV1 in L [% lung resected � preop FEV1 in L]).Nakahara et al228 found that a ppo FEV1 40% of the predictednormal for a particular patient resulted in no postoperativerespiratory complications, whereas a ppo FEV1 �30% of nor-mal resulted in all patients needing postoperative mechanicalventilatory support.228
Cardiopulmonary function can be assessed simply by a6-minute walk test with oximetry and more completely with anassessment of maximal oxygen consumption and ppo maximaloxygen consumption (calculated as for FEV1).237 In 1 study of25 thoracic patients, patients with complications had a ppomaximal oxygen consumption of 10.6 mL/kg/min comparedwith patients without complications who had 14.8 mL/kg/min(p � 0.1); all patients with a ppo maximal oxygen consumptionof less than 10 mL/kg/min died.238 A 6-minute walk test of lessthan 2,000 feet correlated with an oxygen consumption of lessthan 15 mL/kg/min239 and thus may be associated with in-creased perioperative morbidity.
Lung parenchymal function is best assessed by a ppo DLCO
(calculated as for ppo FEV1). In a multivariate analysis of 376thoracic surgical patients, a ppo DLCO of �40% was associatedwith increased respiratory complications (p � 0.004); DLCO andFEV1 were largely unrelated indicators of risk and should beassessed independently.236,240
Should a patient fall into a high-risk category based on ppoFEV1, surgery does not need to be cancelled but additionaltesting, precautions and perioperative care may be indicated asin Table 6.236
Table 5. Assessment of Operative Risk Using Pulmonary Function
Tests
Testing PhasePulmonary Function
TestIncreased Operative Risk
Result
Whole-lung tests Arterial blood gas(room air)
PaCO2 �45 mmHgPaO2 �60 mmHg
Spirometry FVC �1.5 mL/kgFEV1 �50% of FVC
Lung volume VC �2LMVV �50% predictedRV/TLC �50%
Single-lung tests Right and leftindividual lungfunction testsof perfusionand ventilationusingradioisotopes
Predicted postoperativeFEV1 �0.85 L or �70%blood flow todiseased lung
Mimicpostoperativeconditions
Unilateral balloonocclusion of aright or leftpulmonaryartery
Mean PAP �40 mmHg,PaCO2 �60 mmHg, orPaO2 �45 mmHg
Abbreviations: PaCO2, partial pressure of arterial carbon dioxide;PaO2, partial pressure of arterial oxygen; FVC, forced vital capacity;FEV1, forced expiratory volume in 1 second; VC, vital capacity; MVV,maximum voluntary ventilation; RV/TLC, residual volume to totallung capacity; PAP, pulmonary artery pressure.
Data from.217,218,220
Table 6. A Suggested Approach to Anesthetic Management Based
on Preoperative Assessment of Risk
Predicted Postoperative FEV1
�40% 30%-40% �30%
Extubate in the ORif clinicallyindicated
Consider extubationbased on:
Staged weaning frommechanicalventilation
1. Exercise tolerance2. Assess ppo DLCO
3. V/Q scan4. Associated diseases
Establish effectivethoracic epiduralanalgesia
Abbreviations: FEV1, forced expiratory volume in 1 second; OR,operating room; DLCO, diffusion capacity for carbon monoxide; ppo,predicted postoperative; V/Q, ventilation to perfusion.
Reprinted with permission.235
372 GRICHNIK AND HILL

Monitoring and Sedation
Monitoring selected for the patient with severe emphysemashould be tailored to the type and extent of the procedure whileaccounting for the severity of the pulmonary disease. In addi-tion to the usual American Society of Anesthesiologists mon-itors, an arterial cannula should be considered for most patients.Frequent arterial blood gases and the ability to rapidly identifyhemodynamic compromise are crucial. Central venous accessshould be considered for procedures with significant potentialfor third-space volume shifting or blood loss. However, caremust be taken to avoid unintentional pneumothorax as a com-plication of line insertion (ipsilateral internal jugular vein can-nulation for thoracotomy is preferred). Foley catheterizationshould be used for any operation that may require significantfluid administration.
While placing catheters, sedation should be given cautiouslyas patients may be very susceptible to respiratory depressionfrom sedatives241 and residual effects may create difficulty withemergence from anesthesia. The relationship between CO2
retention and lung mechanics in 311 patients with COPD andvarying degrees of hypercapnea was examined.242 At rest,patients with more hypercapnea (PaCO2 �55) had greaterhyperinflation, airflow obstruction, and respiratory pump dys-function that resulted in a significantly lower minute ventilationthan normocapnic patients, mostly because of a reduction intidal volume. Gross et al examined the effect of midazolam onchanges in minute ventilation in response to hypercapnea inpatients with and without COPD (Fig 8).241 Although bothgroups had a diminished minute ventilation response to hyper-capnea with midazolam, the patients with COPD had a moreprofound decrease, which lasted for a longer period of time. Alow-dose infusion of the short-acting agent propofol may be
advantageous over bolus administration of benzodiazepines inthis setting.
Choices of Anesthesia and Analgesia
Although the type of anesthetic administered is probably notas important as the expertise with which it is administered,every plan must take into account the difficulties of ventilationin this patient population. Regional anesthesia can and shouldbe considered when appropriate. Avoidance of high spinal orepidural block levels is desirable for patients who rely onintercostal muscles for ventilation to prevent dyspnea and car-bon dioxide retention. A combined regional and light generalanesthetic approach can be effective. Regional techniques (eg,epidural, intercostal, paravertebral blocks) can facilitate re-duced intraoperative opioid use and minimization of inhalationagents to decrease prolonged anesthetic effects.243
In developing a strategy for postoperative analgesia, consid-eration should be given to the expected duration of chest tubedrainage and/or the intensity of the postsurgical pain. Theepidural route is especially effective for procedures expected torequire more than 1 day of analgesia and procedures in whichdelayed return of gastrointestinal function may prevent oralanalgesic administration. In general, placement of the epiduralclose to the dermatomal level of the surgical incision canincrease the efficacy of the analgesics administered.244-246 Localanesthetic use in the epidural can minimize the need for opioidsand their respiratory depressant effects; it has been suggestedthat the combination of local anesthetic and opioids for syner-gism is most effective.247,248 Adequate inspiratory and expira-tory muscle function must be assured with local anesthetic usein a regional analgesic technique.
Paravertebral blocks,249 intercostal blocks,250,251 and intrathe-cal opioids252-254 are alternative techniques, especially usefulfor short-stay procedures. Paravertebral blocks can provideunilateral analgesia with local anesthetic, to allow avoidance ofopioids, less hypotension, and less urinary retention than epi-dural analgesia.255,256 Single administration paravertebralblocks provide effective analgesia for only 9 to 12 hours, butcatheter techniques can be used to extend the duration of theblock.257,258 Similarly, single administration intercostal blocksmay last 6 to 12 hours, although intercostal catheters can beused for a longer duration of analgesia.259,260 Intrathecal opioidsmay provide analgesia for up to 24 hours and intrathecalcatheters for prolonged analgesia have been used.261,262 Theoptimal technique for postoperative analgesia in the patientwith severe emphysema is not known.
Should parenteral and/or epidural opioids be administered,care must be taken to meticulously monitor respiratory func-tion, as patients may be uniquely susceptible to carbon dioxideretention from the ventilatory depressant effects of the opi-oids.263-267 Supplemental analgesics devoid of respiratory de-pression such as nonsteroidal antiinflammatory agents shouldbe considered if not contraindicated to limit the respiratoryeffects of opioid administration.268
A theoretical concern about thoracic epidural analgesia is thepotential to cause increases in bronchial tone and reactivitythrough pulmonary sympathetic blockade and respiratory mus-cle weakness, with adverse effects on ventilation.269 To inves-
Fig 8. The slope of the fall in the minute ventilation response to
carbon dioxide after midazolam administration over time.
Slope�difference in minute ventilation between normocapnea and
hypercapnea divided by the difference in carbon dioxide tensions,
min�minutes. At time 0, midazolam was administered. Figure de-
rived from data from Gross et al, with permission.240
373SEVERE EMPHYSEMA

tigate these concerns, Gruber et al270 examined 12 patients withsevere emphysema presenting for LVRS. Preoperative thoracicepidural anesthesia with bupivacaine was found to improvetidal volume, peak inspiratory flow rates and decrease pulmo-nary resistance as compared with baseline values. Similarly,Groeben et al269 found no increase in airway obstruction in 20patients with severe COPD undergoing breast surgery withhigh thoracic epidural blockade as the sole anesthetic.
Two large analyses support the use of regional analgesia forpatients to preserve pulmonary function in the perioperativeperiod. Richardson et al271 examined 55 studies using epiduralanalgesia, paravertebral, or extrapleural analgesia (grouped to-gether); intercostal block, cryoablation; intrapleural analgesia;and transcutaneous nerve stimulation. Spirometric function wasreported as the percentage of preoperative pulmonary functionthat was preserved. Paravertebral blockade preserved spiromet-ric function to 75% of preoperative values, whereas intercostalblockade and epidural analgesia preserved spirometric functionto 52% and 47%, respectively, of preoperative values. Statis-tical analysis was not attempted because of variable studymethods, and no comparison to intravenous analgesia wasmade.
In a more rigorous analysis, Ballantyne et al272 examined 65studies using epidural analgesia, intercostal blockade, localwound infiltration, and interpleural and intravenous analgesiaas compared with systemic opioid analgesia. They examinedrelevant clinical outcomes of atelectasis incidence, pulmonaryinfections, pulmonary complications, and postoperative arterialpartial pressure of oxygen (PaO2). Secondarily, spirometricfunction was assessed. Epidural opioid analgesia comparedwith systemic opioids reduced the incidence of atelectasis(relative risk [RR] � 0.53, 95% confidence interval [CI] �0.33-0.85, p � 0.01). Epidural local anesthetic analgesia com-pared with systemic opioids decreased the incidence of pulmo-nary infections (RR � 0.36, 95% CI � 0.21-0.65, p � 0.001),pulmonary complications (RR � 0.58, 95% CI � 0.42-0.80,p � 0.001) and resulted in a greater postoperative PaO2 (dif-ference at 25% correlation � 4.56, 95% CI � �9.0757 to0.0585, p � 0.047). In contrast to the findings of Richardson etal, no differences in spirometric function were evident with anyof the therapies. It can be concluded that regional analgesictechniques can improve pulmonary outcomes perioperatively,as compared with conventional intravenous analgesia. It hasbeen suggested that the recent trend of improved outcome inhigh-risk thoracic patients after pulmonary resection seems tobe related to the use of epidural analgesia.273 Thoracic epiduraladministration of bupivacaine has also been shown to attenuatesupraventricular tachyarrhythmias after pulmonary resection ascompared with epidural morphine alone.274
Anesthetic Induction
Induction must be carefully undertaken when general anes-thesia with endotracheal intubation is necessary. Initially, anextended period of denitrogenation is required. COPD patientsmay need 9 to 10 minutes to achieve an end-tidal fractionaloxygen concentration of 90% after breathing 100% oxygen,whereas patients with normal lung function take only 2 to 3minutes (Fig 9).275 This is likely because of ventilation-to-
perfusion and diffusion abnormalities in patients with severeemphysema.
Hemodynamic instability is commonly observed in thesepatients during induction. Severe hypotension has been re-ported (and perhaps underreported) on induction of anesthe-sia.13,276-281 This may be because of the occurrence of DPH;institution of positive-pressure ventilation (PPV); the inadver-tent application of positive end-expiratory pressure (PEEP);pneumothorax; vasodilatation from anesthetic agents; and/orsympathetic blockade from regional anesthesia, hypovolemia,and myocardial ischemia. It is important to avoid excessiveventilation immediately after induction as can occur with maskventilation or when confirming endotracheal tube placement byauscultation as overventilation can lead to pulmonary gas trap-ping (Fig 10). Hypoventilation with ventilator timing set for aprolonged expiratory phase after induction may be advanta-geous until the degree of pulmonary dysfunction under anes-thesia is determined.
The properties of the ventilator used may influence theintraoperative course of the patient. A volume-controlled ven-tilator will deliver a preset volume without regard for thepressure necessary to deliver that volume. Use of a pressure-limited ventilator has been advocated in the literature.282 Ifauto-PEEP or breath stacking should occur, the pressure-lim-ited ventilator will sense the accumulating pressure and re-spond by reducing the volume of the next breath; an alarm forlow minute ventilation will alert the anesthesiologist if thisphenomenon compromises minute ventilation. In the absenceof a pressure-limited ventilator, use of an ICU ventilator withan intravenous anesthesia technique may be used. Close mon-itoring of peak and mean airway pressures is important becausethese are surrogate measures for retained volume in the lungs.Flow-volume loops available on selected ventilators can di-rectly display breath stacking by observation of continuedexpiratory flow at the point of starting the next inspiration(Fig 11).
The risk of bronchospasm during an anesthetic in a popula-tion with obstructive lung disease has been estimated to be7.7/1,000 as compared with the overall rate of 1.7/1,000 pa-tients based on a retrospective analysis of 156,064 patients.283
There was a lower incidence with regional versus generalanesthesia, but bronchoscopy and mediastinoscopy were asso-ciated with more bronchospasm. Although many have recom-mended intravenous lidocaine to prevent intraoperative bron-chospasm,284,285 its efficacy remains to be proven.286-288 Upperairway reactivity is also important to control; inhalation agentsat various minimum alveolar concentration levels and nebu-lized bronchodilators can facilitate this goal.289
The modes of ventilation used may be critically important.Maintenance of a short I:E ratio has been shown to reducepulmonary hyperinflation auto-PEEP.290,291 Slinger et al292
showed the importance of I:E time management as the appli-cation of external PEEP to patients with auto-PEEP duringone-lung ventilation (OLV) did not increase the total PEEP ifexpiratory flow time was increased. Further, use of an end-expiratory pause (as is common for many operating roomventilators) will shorten the expiratory time period; increasedauto-PEEP and decreased arterial oxygenation can occur.293 A
374 GRICHNIK AND HILL

Fig 9. End-tidal oxygraphy over time in patients with and without chronic obstructive pulmonary disease (COPD). FEO2 tidal fractional
oxygen concentration, ��patients without COPD, o�patients with COPD. Reprinted with permission.274
Fig 10. The development of dynamic pulmonary hyperinflation during mechanical ventilation and a representation of lung deflation during
apnea. FRC�functional residual capacity. Adapted with permission.308
375SEVERE EMPHYSEMA

simple maneuver is to intermittently disconnect from the ven-tilator to allow expiration of trapped pulmonary gas.
Intraoperative anesthesia may be achieved with short-dura-tion drugs and inhalation agents to facilitate rapid emergenceand reduce the possibility of excessive sedation or inadequateventilation.294 Nitrous oxide should be avoided because of therisk of expansion of a closed gas space within diseased lungsand to allow for changing fraction of inspiratory oxygen (FIO2)without changing anesthetic depth.295 The use of short- tointermediate-duration nondepolarizing neuromuscular block-ade agents can avert ill-timed coughing during the surgicalprocedure, reducing the risk of barotrauma and yet allowing fora rapid recovery of neuromuscular function.
Treatment of intraoperative hypoxemia with OLV may needto be carefully considered. Application of continuous positiveairway pressure (CPAP) to the nondependent lung may lead tolung expansion because of increased compliance in emphy-sema.291 A useful first maneuver is to do fiberoptic bronchos-copy to confirm correct dual-lumen endotracheal tube positionand remove secretions. Careful application of CPAP and PEEPmay then be considered with attention to lung hyperinflation;nondependent lung re-expansion is the ultimate treatment.More common is intraoperative hypercarbia with increasedventilation-to-perfusion mismatch, significant deadspace venti-lation, and the need for caution with ventilatory patterns.296
Extrathoracic endoscopic procedures using insufflation of car-bon dioxide (CO2) may also result in impaired CO2 excre-tion.297 Hypercarbia in the absence of severe acidosis andhypoxia is usually well tolerated but may require inotropicsupport or lidocaine treatment.115,298,299
Prolonged emergence and return to adequate respiratoryfunction may occur. Volatile agents in concentrations as low as0.1 minimum alveolar concentration can depress the ventilatoryresponse to hypoxia in normal patients and may have a more
profound effect in the patient with emphysema.300,301 It hasbeen shown that patients with COPD have a higher volume ofdeadspace and that PaCO2 is higher for spontaneously breath-ing patients under anesthesia using volatile agents comparedwith patients without COPD.241 The importance of successfullyextubating the patient with severe emphysema should bestressed.87,302 Spontaneous ventilation improves preload, avoidsincreased afterload, minimizes DPH, and should decrease stresson pulmonary suture lines in the setting of lung surgery.
Parenchymal air leaks are a common perioperative prob-lem,303 first encountered with initial lung re-expansion; highgas flows may be required to adequately ventilate the patient.291
Excessive air leak can compromise the ability to extubate thepatient and may lead to the need for prolonged chest tubedrainage.141 Experience from care of the LVRS patient suggeststhat hypercarbia may be expected in the postoperative period,with elevations of PaCO2 noted to 48 hours after sur-gery.291,296,304 PaCO2 greater than 70 mmHg may be treatedwith a short period of CPAP.
A period of postoperative ICU care or intensive postanes-thetic care unit observation should be considered for the patientwith severe emphysema to assure adequate pulmonary functionpostoperatively, assess the chest X-ray, optimize analgesia, andassess any issues related to the operation. ICU care shouldalways be considered after any major surgery, especially tho-racic or upper abdominal procedures, because these procedurescan cause significant pulmonary dysfunction (reduction inFRC, depression of respiratory drive, impaired mechanics ofventilation, impaired gas exchange) even in the absence ofemphysema.305 A longer than usual hospital length of stay canbe anticipated with an increased need for postoperative oxygenadministration.296
COMMON PERIOPERATIVE PROBLEMS
Dynamic Pulmonary Hyperinflation and Intrinsic PEEP
DPH and auto-PEEP, which occur as more ventilation isinspired than is expired, may occur with increased expiratoryairflow resistance (Fig 10). Three factors determine DPH andauto-PEEP: (1) the patient’s intrinsic respiratory system resis-tance and compliance, (2) added external resistance (endotra-cheal tube diameter, ventilator tubing, and devices), and (3)ventilatory pattern (frequency, tidal volume, inspiration-to-ex-piration time ratios, inflation volume, and end-inspiratorypause).292,306,309 These conditions are particularly dangerouswith OLV for thoracic surgery as the entire ventilatory demandis placed on a single dependent diseased lung. Hemodynamicconsequences include impaired venous return, a tamponade-like effect on the RV from hyperinflated lungs, compression ofthe alveolar blood vessels by elevated intra-alveolar pressures,and septal shift causing left ventricle dysfunction.281,310 Exces-sive DPH or auto-PEEP may cause cardiac arrest characterizedby electromechanical dissociation.276-281
DPH or auto-PEEP can be particularly challenging to man-age because most standard anesthesia machines or ICU venti-lator monitors do not readily detect progressively increasingintrathoracic volume;278 use of a flowmeter may allow detec-tion of interrupted expiratory flow (Fig 11). Bardoczky et al311
have correlated interrupted expiratory flow with the develop-
Fig 11. A flow-volume loop from a mechanically ventilated pa-
tient with emphysema. Flow is in liters/minute and pulmonary vol-
ume is in liters. Note that expiratory flow does not return to baseline
prior to inspiration, creating a situation in which dynamic hyperin-
flation or auto-PEEP could occur.
376 GRICHNIK AND HILL

ment of auto-PEEP (sensitivity 0.78, specificity 0.91, predictivevalue 0.92) facilitating monitoring for DPH.311 On recognitionof this problem, the patient should be immediately discon-nected from the ventilator and allowed to exhale. Depending onthe amount of accumulated air, this may take many seconds tominutes. Hemodynamic parameters should improve with exha-lation, but resuscitative medications may be required.
Ducros et al312 evaluated the incidence of auto-PEEP in thissetting (Fig 12). They found that lung transplant candidateswith severe emphysema had high levels of auto-PEEP imme-diately after induction of anesthesia, which increased withOLV; they also maintained high levels of trapped air. Con-versely, patients with restrictive lung disease did not developsignificant auto-PEEP or trapped air at any time.
Barotrauma
Pulmonary barotrauma is defined as extra-alveolar air inlocations in which it is not normally found and can occur as theresult of a sustained increase in intramural pulmonary pressure,secondary to alveolar overdistention.306 In patients with highlevels of DPH and auto-PEEP, conventional ventilatory settings(such as a tidal volume of 10-12 mL/kg) may shift ventilationto the upper, less-compliant portion of a volume-pressurecurve, thus risking alveolar rupture with overdistention.306 Therisk of barotrauma increases with high intrapleural pressure,increased expiratory resistance because of an endotrachealtube, coughing, or “bucking” against the ventilator and highlevels of extrinsic PEEP. The hemodynamic effects of baro-trauma are similar to hemodynamic effects of DPH and mayinclude mediastinal shift toward the nontraumatized lung. In-creased inflation pressures in the nontraumatized lung canoccur because it is compressed by the volume of gas in thecontralateral intrapleural space.
Avoidance of barotrauma may be aided by the use of musclerelaxants, intermittent disconnection from the ventilator, a longexpiratory time, and close monitoring. Minimization of peakinspiratory and plateau airway pressures have been recom-mended,27,313 although others have found no correlation ofthese pressures to the incidence of barotrauma in acute respi-ratory distress syndrome (ARDS) patients.314 Ventilation withsmaller tidal volumes than traditionally used (6 mL/kg v 10-12mL/kg) is beneficial.315 The addition of a small amount ofexternal PEEP to prevent distal airway collapse in a sheepmodel also resulted in less inflammation and histologic in-jury,316 factors thought to predispose to barotrauma. Improvedclinical outcomes have been shown in patients with ARDS
Table 7. Lung-Protective Strategy for Reduction of Barotrauma in
Patients With Acute Lung Injury
Maneuver Recommended Value
Limit inspiratory drivingpressure (PPLAT-PEEPTOTAL)
�20 cm H2O pressure
Limit peak airway pressure �40 cm H2O pressurePressure-limited or
pressure-supportventilation
Pressure-controlled inverseratio ventilation if FIO2 �
0.5Relatively high PEEP (If
PEEPAUTO occurs, thenPEEPTOTAL � PEEPEXT �
PEEPAUTO)
PEEPTOTAL 2 cm H2Opressure � PFLEX
Frequent lung recruitmentmeasures
Hold continuous positiveairway pressure at 30-40cm H2O pressure for 40sec
Respiratory rate �30
Abbreviations: cm H2O pressure, centimeters of water pressure;FIO2, fraction of inspired oxygen; PPLAT, plateau pressure after inspira-tory pause; PFLEX, the inflection point corresponding to the upwardshift in the slope of the pressure-volume curve; PEEPAUTO, the differ-ence between alveolar pressure at end-expiration and airway pres-sure; PEEPEXT, PEEP applied externally to the respiratory circuit,PEEPTOTAL, PEEPEXT � PEEPAUTO.
Data from.315
Fig 12. Auto-PEEP and trapped air volume in patients during
two-lung supine, two-lung lateral, and one-lung lateral ventilation.
Group 1 patients had mild obstructive airways disease; they only
developed auto-PEEP with OLV and had minimal air trapping. Group
2 had severe emphysema; they had high levels of auto-PEEP after
induction of anesthesia, which increased with OLV; they also main-
tained high levels of trapped air. Group 3 had severe restrictive lung
disease (pulmonary fibrosis); they generated minimal auto-PEEP and
trapped air. Patients with severe obstructive disease are prone to
pulmonary air trapping unlike those with restrictive disease. Re-
printed with permission.310
377SEVERE EMPHYSEMA

using such “lung-protective strategies” based on individualpatient lung mechanics (Table 7).317
Intraoperative pneumothorax in the dependent ventilatedlung may be difficult to detect and can quickly become atension pneumothorax with positive-pressure ventilation.318,319
Emergent treatment includes resuscitative vasoactive medica-tions and relief of intrapleural pressure can be accomplishedrapidly by chest tube thoracostomy or a large-gauge IV cath-eter. It may be necessary to turn the patient supine for adequateresuscitation. Barotrauma can also manifest as pneumomedia-stinum, pneumoperitoneum, and subcutaneous emphysema(Fig 5A and B).320,321
Post–Lung Resection Pulmonary Edema
Pulmonary edema is a perioperative problem of significanceto anesthesiologists.322,323 The syndrome of post–lung resectionpulmonary edema (PLRPE) has been reported after 2% to 4%of pneumonectomy procedures (right � left), after 1% oflobectomies and after 0.1% to 0.2% of thoracoscopic surger-ies.322-324 Radiologic signs may appear before symptoms, withsymptoms most commonly occurring on postoperative days 2to 4. The syndrome is resistant to treatment, with a 30% to 50%mortality. Histologically, PLRPE is similar to the ARDS.PLRPE can occur with normal pulmonary capillary wedgepressure (PCWP),322,325 although the measurement of PCWPmay be difficult postpneumonectomy326 or in mechanicallyventilated patients with COPD.327 The physiology of PLRPE isunclear. The volume of fluid given to the patient has beenimplicated, with most authors citing Zeldin et al.328 However,this study examined only 10 pneumonectomy patients withPLRPE, and adequate fluid data were available on only 40% ofthe patients. Two other studies support the concept that peri-operative fluid administration greater that 2 L is associated withthe syndrome.329,330
However, the pathophysiology may not entirely rest on thefluid balance because postpneumonectomy pulmonary edemaalso occurs in patients without high perioperative fluidload.324,331,332 A comprehensive review by Slinger322 suggeststhat fluid therapy is only one of the contributing factors to thissyndrome; other potential mechanisms are presented in Table8.322,324,325,333-336
Risk factors that predispose the patient to PLRPE include aright pneumonectomy (because of disruption of differentiallymphatic drainage with R�L),337 increased perioperative pul-monary arterial pressures (in part because of hypoxemia, hy-percarbia, pain),322,338 perioperative volotrauma (large tidal vol-ume during OLV, mediastinal shift, and lung hyperinflation
postsurgery),339,340-343 prior radiation therapy,330 and resectionof normally perfused lung (acutely shunting that blood flow toremaining lung tissue).330
Perioperative fluid loading could aggravate the above mech-anisms and patient risk factors. Increased cardiac output, in-creased pulmonary artery pressures, and increased net filtrationpressure across the pulmonary capillary bed can result in fluidtranslocation to the pulmonary interstitial space. These princi-ples may also be important in nonthoracic surgery.344 Pulmo-nary edema correlated with patients who received more than 67mL/kg/d for various surgical procedures,345 and a 10% inci-dence of respiratory failure was documented in a study ofperipheral vascular patients, in which patients received morethan 6 L of fluid in 24 hours.346
Debate also exists about the type of fluid, especially colloidversus crystalloid. Among the proposed benefits of colloids areslower and perhaps less translocation of the fluid from theintravascular (IVC) space to the extravascular space(EVC).347,348 Improved tissue microperfusion with less endo-thelial swelling, resulting in improved tissue oxygen tension,has been presented.349 However, conflicting data exist becausesome investigators have found increased long-term mortalitywith colloid use in sepsis patients.350,351 Ernest et al348 foundthat colloid agents, once translocated to the EVC space, actu-ally increased the volume of that space in excess of the amountof colloid given in septic patients. Others found that colloidadministration can promote lung water retention in burn pa-tients.352 A meta-analysis of randomized clinical trials of iso-tonic crystalloid versus colloid fluid therapy found no differ-ence in pulmonary edema or mortality.353
The total volume of fluid seems to be a critical contributoryfactor for PLRPE. In the absence of a leaky capillary syndrome(as in sepsis or burns), a combination of crystalloid and colloidis one strategy to attempt to prevent PLRPE. A minimal amountof crystalloid can be initially administered with the understand-ing that much of this fluid will translocate to the EVC space.Further fluids can be administered as colloids to replace intra-vascular volume because less total fluid volume is needed. Thetotal amount of intravenous fluid to be given can be guided byindices of adequate volume status, such as urine output andCVP. Mild hypotension may not need to be treated with fluidboluses as positional changes and vasoactive agents can beused to support hemodynamics if urine output and CVP areadequate.
Other Potential Problems
Perioperative supraventricular arrhythmias are common(18%-25%); increased age, increased intraoperative blood loss,and extent of resection are risk factors.354-356 Atrial fibrillationwas found to be the most common arrhythmia; 80% convertedto normal rhythm by 3 days.354 Postoperative SVT is associatedwith a higher rate of ICU admission, longer hospital LOS, anda higher 30-day mortality.356 Although infrequent, cardiac isch-emia or infarction can occur as well.117
Pulmonary hypertension or right ventricular dysfunctionmay also occur after pulmonary resection.150,356,358 Postulatedmechanisms include an increase in pulmonary vascular resis-tance with a decrease in lung cross-sectional area, reactivevasoconstriction, an alteration of vasodilatory to vasoconstric-
Table 8. Postulated Mechanisms for Post–Lung Resection
Pulmonary Edema
Lymphatic disruption and surgical traumaAcute inflammatory reaction to operative lung collapse and re-
expansionLung capillary endothelial damageRelative oxygen toxicityIschemia/reperfusion injury of operative lungMicroembolizationRestricted pulmonary capillary volume in emphysema patients
378 GRICHNIK AND HILL

tive mediators, and kinking of the pulmonary blood vessels.150
Pulmonary infection remains a devastating complication andmay be related to ability to mobilize secretions postopera-tively.20,40 Malignant hyperinflation of a nondependent lung hasbeen reported during chest surgery, thought to be because ofairway secretions and a noncompliant dependent lung.359 Thiscondition may also occur postoperatively with mechanical ven-tilation. In contradistinction, mediastinal shift and cardiac her-niation have also been reported, usually after pneumonectomy,usually because of an imbalance of intrathoracic pressure be-tween the operative and nonoperative thoracic cavities.360,361
SUMMARY
Emphysema may be commonly encountered in many surgi-cal populations. The pathophysiology rests on airspace enlarge-ment and obstruction to airflow, especially expiratory airflow.Medical therapy can ameliorate symptoms and improve exer-cise tolerance but not cure the disease. Surgical attempts to treatemphysema with LVRS remain investigational and lung trans-plantation is limited by donor availability. Unique anestheticconsiderations include the potential for dynamic pulmonaryhyperinflation, barotrauma, and pulmonary edema.
REFERENCES
1. Sobonya RE: Emphysema, in Saldana M, (ed): Pathology ofPulmonary Disease. Philadelphia, PA, J.B. Lippincott Company, 1994,275-286
2. Snider GL, Kleinerman J, Thurlbeck WM, et al: Report of aNational Heart, Lung, and Blood Institute, Division of Lung DiseasesWorkshop. The definition of emphysema. Am Rev Respir Dis 132:182-185, 1985
3. American Lung Association—Emphysema. Available at:http://www.lungusa.org/diseases/lungemphysema.html. Accessed Oc-tober 27, 2002
4. American Lung Association—Trends in Chronic Bronchitisand Emphysema: Morbidity and Mortality. Available at: http://www.lungusa.org/data/copd/COPD1.pdf. Accessed date October 27, 2002
5. Viegi G, Scognamiglio A, Baldacci S, et al: Epidemiology ofchronic obstructive pulmonary disease (COPD). Respiration 68:4-19,2001
6. Sobonya RE, Burrows B: The epidemiology of emphysema.Clin Chest Med 4:351-358, 1983
7. Data Fact Sheet: Chronic Obstructive Pulmonary Disease(COPD). Available at: http://www.nhlbi.nih.gov/health/public/lung/other/copd_fact.htm#em. Accessed October 27, 2002
8. Reid LM: Chronic Obstructive Pulmonary Diseases, in Fish-man AP, (ed): Pulmonary Diseases and Disorders. New York, NY,McGraw-Hill, 1988, pp 1247-1272
9. Turato G, Zuin R, Saetta M: Pathogenesis and pathology ofCOPD. Respiration 68:117-128, 2001
10. Hogg JC: Chronic obstructive pulmonary disease: An overviewof pathology and pathogenesis. Novartis Found Symp 234:4-26, 2001
11. Gurney JW: Pathophysiology of obstructive airways disease.Rad Clin North Am 36:15-27, 1998
12. Evans MD, Pryor WA: Cigarette smoking, emphysema anddamage to alpha-1 proteinase inhibitor. Am J Physiol 266:L593-611,1994
13. Sienge PW, Hartigan PM, Body SC: Anesthetic considerationsfor patients with severe emphysematous lung disease. Int AnesthesiolClin 38:1-23, 2000
14. Pardo A, Selman M: Proteinase-antiproteinase imbalance in thepathogenesis of emphysema: the role of metalloproteinases in lungdamage. Histol Histopathol 14:227-233, 1999
15. Stebbens WE: Proteinase imbalance versus biomechanicalstress in pulmonary emphysema 69:46-62, 2000
16. Barnes PJ: Mechanisms in COPD: Differences from asthma.Chest 117:10S-12S (suppl), 2000
17. Finkelstein R, Fraser RS, Ghezzo H, et al: Alveolar inflamma-tion and its relation to emphysema in smokers. Am J Respir Crit CareMed 152:1666-1672, 1995
18. O’Shaughnessy TC, Ansari TW, Barnes NC, et al: Inflamma-tion in bronchial biopsies of subjects with chronic bronchitis: Inverserelationship of CD8�T lymphocytes with FEV1. Am J Respir Crit CareMed 155:852-857, 1997
19. Peci A, Balbi B, Majori M, et al: Inflammatory cells andmediators in bronchial lavage of patients with chronic obstructivepulmonary disease. Eur Respir J 12:380-386, 1998
20. Barnes PJ: Chronic obstructive pulmonary disease. N EnglJ Med 343:269-280, 2000
21. Repine JE, Bast A, Lankhorst I: Oxidative stress in chronicobstructive pulmonary disease. Am J Respir Care Med 156:341-357,1997
22. Dekhuijzen PNR, Aben KK, Dekker I, et al: Increased exha-lation of hydrogen peroxide in patients with stable and unstable chronicobstructive pulmonary disease. Am J Respir Crit Care Med 154:813-816, 1996
23. Practico D, Basili S, Vieri M, et al: Chronic obstructive pul-monary disease is associated with an increase in urinary levels ofisoprotane F2alpha-III, an index of oxidant stress. Am J Respir CritCare Med 158:1709-1714, 1998
24. Barnes PJ, Karin M: Nuclear factor kappa-beta—A pivotaltranscription factor in chronic inflammatory diseases. N Engl J Med336:1066-1071, 1997
25. Rahman I, Morrison D, Donaldson K, et al: Systemic oxidativestress in asthma, COPD, and smokers. Am J Respir Crit Care Med154:1055-1060, 1996
26. deCastro MA: Current controversies in surgical therapy foremphysema. Semin Cardiothorac Vasc Anesth 4:26-30, 2000
27. Slutsky AS: Mechanical ventilation. American College ofChest Physicians’ Consensus Conference. Chest 104:1833-59, 1993(erratum Chest 106:656, 1994)
28. Foster WL Jr, Gimenez EI, Roubidouz MA, et al: The emphy-sema: radiologic-pathologic correlations. Radiographics 13:311-328,1993
29. American Thoracic Society: Standardization of spirometry:1994 update. Am J Respir Crit Care Med 152:1107-1136, 1995
30. Zarins LP, Clausen JL: Body Plethysmography, in Clausen JL,(ed): Pulmonary function testing guidelines and controversies, equip-ment, methods and normal values. New York, NY, Academic Press,1982, pp 141-153
31. Scraf SM, Iqbal M, Keller C, et al: Hemodynamic character-ization of patients with severe emphysema. Am J Respir Crit Care Med166:314-322, 2002
32. Kanner RE, Renzetti AD Jr, Stanish WM, et al: Predictors ofsurvival in subjects with chronic airflow limitation. Am J Med 74:249-255, 1983
33. Burrows B, Bloom JW, Traver GA, et al: The course andprognosis of different forms of airways obstruction in a sample fromthe general population. N Eng J Med 317:1309-1314, 1987
34. Anthonisen NR: Prognosis in chronic obstructive pulmonarydisease: Results from multicenter clinical trials. Am Rev Respir Dis140:S95-99, 1989
379SEVERE EMPHYSEMA

35. Piccioni P, Caria E, Bigamini E, et al: Predictors of survival ina group of patients with chronic airflow obstruction. J Clin Epidemiol51:547-555, 1998
36. Traver GA, Cline MG, Burrows B: Predictors of mortality inpatients with chronic airways obstruction. Am Rev Respir Dis 119:895-902, 1979
37. Snider GL: Chronic obstructive pulmonary disease: Risk fac-tors, pathophysiology and pathogenesis. Ann Rev Med 40:411-429,1989
38. Hodgkin JE: Prognosis in chronic obstructive pulmonary dis-ease. Clin Chest Med 11:555-569, 1990
39. Hansen EF, Pharareth K, Laursen LC, et al: Reversible andirreversible airflow obstruction as a predictor of overall mortality inasthma and chronic obstructive pulmonary disease. Am J Respir CritCare Med 159:1267-1271, 1999
40. Stoller JK: Acute exacerbations of chronic obstructive pulmo-nary disease. N Engl J Med 346:988-994, 2002
41. American Thoracic Society: Standards for the diagnosis andcare of patients with chronic obstructive pulmonary disease. Am RevRespir Crit Care Med 152:S77-S121, 1995
42. American College of Chest Physicians and the American As-sociation of Cardiovascular and Pulmonary Rehabilitation GuidelinesPanel: Pulmonary Rehabilitation: Joint ACCP/AACVPR evidence-based guidelines. Chest 112:1363-1396, 1997
43. Anthonisen NR, Connett JE, Kiley JP, et al: Effects of smokingintervention and the use of an inhaled anticholinergic bronchodilator onthe rate of decline of FEV1. JAMA 272:1497-1505, 1996
44. Lacasse Y, Wong E, Guyatt GH, et al: Meta-analysis of respi-ratory rehabilitation in chronic obstructive pulmonary disease. Lancet348:1115-1119, 1996
45. Pauwels RA, Buist AS, Calverley PMA, et al: Global strategyfor the diagnosis, management and prevention of chronic obstructivepulmonary disease: NHLBI/WHO Global Initiative for Chronic Ob-structive Lung Disease (GOLD) Workshop Summary. Am J Respir CritCare 163:1256-1276, 2001
46. Skordin MS: Pharmacotherapy for asthma and chronic obstruc-tive pulmonary disease: current thinking, practices and controversies.Arch Intern Med 153:814-828, 1993
47. Sherk PA, Grossman RF: The chronic obstructive pulmonarydisease exacerbation. Clin Chest Med 21:705-721, 2000
48. McCrory DC, Brown C, Gelfand SE, et al: Management ofexacerbations of COPD: A summary and appraisal of the publishedevidence: Chest 117(suppl):23S-28S, 2001
49. Wrenn K, Slovis CM, Murphy F, et al: Aminophylline therapyfor acute bronchospastic disease in the emergency room. Ann InternMed 115:241-247, 1991
50. Rice KL, Leatherman JW, Duan PG, et al: Aminophylline foracute exacerbations of chronic obstructive pulmonary disease: A con-trolled trial. Ann Intern Med 107:305-309, 1987
51. Seidenfeld JJ, Jones WN, Moss RE, et al: Intravenous ami-nophylline in the treatment of acute bronchospastic exacerbations ofchronic obstructive pulmonary disease. Ann Emerg Med 13:248-252,1984
52. Niewoehner DE, Erbland ML, Deupree RH, et al: Effect ofsystemic glucocorticoids on exacerbations of chronic obstructive pul-monary disease. N Engl Med 340:1941-1947, 1999
53. Paulwels RA, Lofdahl CG, Pride NB, et al: European Respi-ratory Society Study of Chronic Obstructive Pulmonary Disease (EU-ROSCOP): Hypothesis and design. Eur Respir J 5:1254-1261, 1992
54. Pauwels RA, Lofdahl C-G, Laitinen LA, et al: Long-termtreatment with inhaled budesonide in persons with mild chronic ob-structive pulmonary disease who continue smoking. N Engl J Med340:1948-1953, 1999
55. Vesbo J, Sorensen T, Lange P, et al: Long-term effect ofinhaled budesonide in mild and moderate chronic obstructive pulmo-nary disease: A randomized controlled trial. Lancet 353:1819-1823,1999
56. Burge PS, Calverley PMA, Jones PW, et al: Randomized,double-blind, placebo-controlled trial of inhaled fluticasone propionatein patients with moderate-to-severe chronic obstructive pulmonarydisease: the ISOLDE trial. BMJ 320:1297-1303, 2000
57. Saint S, Bent S, Vittinghoff E, Grady D: Antibiotics in chronicobstructive pulmonary disease exacerbations: A meta-analysis. JAMA273:957-960, 1995
58. Anthonisen NR, Manfreda J, Warren CW, et al: Antibiotictherapy in exacerbations of chronic obstructive pulmonary disease. AnnIntern Med 106:196-204, 1987
59. Centers for Disease Control and Prevention: Prevention ofpneumococcal disease. Recommendations of the Advisory Committeeon Immunization Practices (ACIP): MMWR 46(RR-8):1-24, 1997
60. Hurt RD, Sachs DP, Glover ED, et al: A comparison ofsustained release bupropion and placebo for smoking cessation. N EnglJ Med 337:1195-1202, 1997
61. Alpha-1-Antitrypsin Deficiency Registry Study Group: Sur-vival and FEV1 decline in individuals with severe deficiencies ofalpha-1-antitrypsin. Am J Crit Care Med 158:49-59, 1998
62. Lieberman J: Augmentation therapy reduces frequency of lunginfections in antitrypsin deficiency: A new hypothesis with supportingdata. Chest 118:1480-1485, 2000
63. Dirksen A, Dijkman JH, Madsen F, et al: A randomized clin-ical trial of alpha-1-antitrypsin augmentation therapy. Am J Respir CritCare Med 160:1468-1472, 1999
64. Tarpy SP, Celli BR: Long-term oxygen therapy. N Engl J Med333:710-714, 1995
65. Lipworth BJ: Leukotriene-receptor antagonists. Lancet 353:57-62, 1999
66. Barnes PJ: New therapies for chronic obstructive pulmonarydisease. Thorax 53:137-147, 1998
67. Barnes PJ: Novel approaches and targets for treatment ofchronic obstructive pulmonary disease. Am J Respir Crit Care Med160:S72-S79, 1999
68. Gaensler EA, Cugell DW, Knudson RJ, et al: Surgical man-agement of emphysema. Clin Chest Med 4:443-463, 1983
69. Deslauiers J: History of surgery for emphysema. Semin ThoracCardiovasc Surg 8:43-51, 1996
70. Knudsen RJ, Gaensler EA: Surgery for emphysema. Ann ThorSurg 1:332, 1965
71. Abbott AO, Hopkins WA, Van Fleit WE, et al: A new ap-proach to pulmonary emphysema. Thorax 8:116-132, 1953
72. Miller JI Jr: The history of surgery of empyema, thoracoplasty,Eloesser flap, and muscle flap transposition. Chest Surg Clin North Am10:45-53, 2000
73. Freund WA: Zur operativen behandlung gewisser lungen-krankheiten insbesondere des auf starrer thorax dilatation beruhendenalveolaren emphysems. Z Exp Pathol Theap 3:479, 1906
74. Pearson EF: Cystic disease of the lungs. Ill Med J 67:28, 193575. Allison PR: Giant bullous cysts of the lung. Thorax 2:169,
194776. Reich L: Der einfluss des pneumperitoneums auf das lun-
genemphysema. Wien Arc Intern Med 8:245, 192477. Carter MG, Gaensler EA, Kyllonen A: Pneumoperitoneum in
the treatment of pulmonary emphysema. N Eng J Med 243:549, 195078. Herzog H: Erschlaffung und expiratoische invangination der
membranosen teile der intrathorakalen luftrohre und der haupbronchienals ursache der asphyktischen anfalle beim asthma bronchiale und beider chronischen asthmoiden brochitis des lungenemphysems. SchweizMed Wochenschr 84:217, 1954
380 GRICHNIK AND HILL

79. Nissen R: Tracheoplastik zur beseitigung der erschlaffung desmembranosen teils der intrathorakalen luftrohre. Schweiz MedWochenschr 84:219, 1954
80. Ranier WG, Hutchinson D, Newby JP, et al: Major airwaycollapsibility in the pathogenesis of obstructive emphysema. J ThoracCardiovasc Surg 22:45, 1951
81. Kummell H: Zur chirurgischen behandlung des asthma bron-chiale. Arch Klin Chir 127:716, 1923
82. Rienhoff WM, Gay LN: Treatment of intractable bronchialasthma by bilateral resection of posterior pulmonary plexus. Arch Surg37:456, 1938
83. Abbott OA, Hopkins WA, Van Fleit WE, et al: A new ap-proach to pulmonary emphysema. Thorax 8:116, 1953
84. Brantigan OC, Mvellee E, Kress MB: A surgical approach topulmonary emphysema. Am Rev Respir Dig 80:194-202, 1959
85. Brantigan OC, Mueller E: Surgical treatment of pulmonaryemphysema. Am Surg 23:789-804, 1957
86. Wakabayashi A, Brenner M, Kayaleh RA, et al: Thoracoscopiccarbon dioxide laser treatment of bullous emphysema. Lancet 337:881-883, 1991
87. Cooper JD, Trulock EF, Triantafillou AN, et al: Bilateralpneumonectomy (volume reduction) for chronic obstructive pulmonarydisease. J Thorac Cardiovasc Surg 109:106-119, 1995
88. Wakabayashi A: Thoracoscopic laser pneumoplasty in thetreatment of diffuse bullous emphysema. Ann Thorac Surg 60:936-942,1995
89. Eugene J, Ott RA, Gogia HS, et al: Video-thoracic surgery fortreatment of end-stage bullous emphysema and chronic obstructivepulmonary disease. Am Surg 61:943-946, 1995
90. Hoppin FG: Theoretical basis for improvement following re-duction pneumoplasty in emphysema. Am J Respir Crit Care Med155:520-525, 1997
91. Bellemare E, Cordeau M-P, Couture J, et al: Effects of em-physema and lung volume reduction surgery on transdiaphragmaticpressure and diaphragm length. Chest 121:1898-1910, 2002
92. Cassart M, Hamacher J, Verbandt Y, et al: Effects of lungvolume reduction surgery for emphysema on diaphragm dimensionsand configuration. Am J Respir Crit Care Med 163:1171-1175, 2001
93. Shade D Jr, Cordova F, Lando Y, et al: Relationship betweenresting hypercapnea and physiologic parameters before and after lungvolume reduction surgery in severe chronic obstructive pulmonarydisease. Am J Respir Crit Care Med 159:1405-1411, 1999
94. Martinez FJ, Montes de Oce M, Whyte RI, et al: Lung volumereduction improves dyspnea, dynamic hyperinflation, and respiratorymuscle function. Am J Respir Crit Care Med 155:1984-1990, 1997
95. Benditt JO, Wood DE, McCool FD, et al: Changes in breathingand ventilatory muscle recruitment patterns induced by lung volumereduction surgery. Am J Respir Crit Care Med 155:279-284, 1997
96. Gelb AF, Zamel N, McKenna RJ Jr, et al: Mechanism ofshort-term improvement in lung function after emphysema resection.Am J Respir Crit Care Med 154:945-951, 1996
97. Barnas GM, Gilbert TB, Krasna MJ, et al: Acute effects ofbilateral lung volume reduction surgery on lung and chest wall me-chanical properties. Chest 114:61-68, 1998
98. Sciurba FC, Rogers RM, Keenan RJ: Improvement in pulmo-nary function and elastic recoil after lung-reduction surgery for diffuseemphysema. N Eng J Med 334:1095-1099, 1996
99. Hamacher J, Russi EW, Weder W: Lung volume reductionsurgery: A survey of the European experience. Chest 117:1560-1567,2000
100. Pierce RJ, Snell G: Lung volume reduction surgery (LVRS) foremphysema—Early Australian experience. Aust N Z J Med 30:194,2000
101. Porter SH, Ruffin RE, Pfitzner J, et al: Videoscopic lungvolume reduction surgery in an Australian public teaching hospital.Aust N Z Med 30:202-208, 2000
102. Malthaner RA, Miller JD: Lung volume reduction surgery:Results of a Canadian pilot study. Canadian Lung Volume ReductionSurgery Study Group. Can J Surg 43:377-383, 2000
103. Lowdermilk GA, Keenan RJ, Landreneau RJ, et al: Compari-son of clinical results for unilateral and bilateral thoracoscopic lungvolume reduction. Ann Thorac Surg 69:1670-1674, 2000
104. Stirling GR, Babidge WJ, Peacock MJ, et al: Lung volumereduction surgery in emphysema: A systematic review. Ann ThoracSurg 72:641-648, 2001
105. Wilkens H, Demertizis DS, Konig J, et al: Lung volumereduction surgery versus conservative treatment in severe emphysema.Eur Respir J 16:1043-1049, 2000
106. Flaherty KR, Martinez FJ: Lung volume reduction surgery foremphysema. Clin Chest Med 21:819-848, 2000
107. Geddes D, Davies M, Koyama H, et al: Effect of lung volumereduction surgery in patients with severe emphysema. N Eng J Med343:239-245, 2000
108. Criner GJ, Cordova FC, Furukawa S, et al: Prospective ran-domized trial comparing bilateral lung volume reduction surgery topulmonary rehabilitation in severe chronic obstructive pulmonary dis-ease. Am J Respir Crit Care Med 160:2018-2027, 1999
109. Meyers BF, Yusen RD, Lefrak SS, et al: Outcome of Medicarepatients with emphysema selected for, but denied, a lung volumereduction operation. Ann Thorac Surg 66:331-336, 1998
110. Pompeo E, Marino M, Nofroni I, et al: Reduction pneumo-plasty versus respiratory rehabilitation in severe emphysema: A ran-domized study. Ann Thorac Surg 70:948-953, 2000
111. Gelb AF, McKenna RJ, Brenner M, et al: Lung function 4years after lung volume reduction surgery for emphysema. Chest 116:1608-1615, 1999
112. Scharf SM, Rossoff K, McKeon LM: Changes in pulmonarymechanics after lung volume reduction surgery. Lung 176:191-204,1998
113. Naunheim KS, Kaiser LR, Bavaria JE, et al: Long-term sur-vival after thoracoscopic lung volume reduction: A multi-institutionalreview. Ann Thorac Surg 68:2026-2031, 1999
114. Glaspole IN, Gabbay E, Smith JA, et al: Predictors of periop-erative morbidity and mortality in lung volume reduction surgery. AnnThorac Surg 69:1711-1716, 2000
115. Buettner AU, McRae R, Myles P, et al: Anaesthesia andpostoperative pain management for bilateral lung volume reductionsurgery. Anaesth Intensive Care 27:503-508, 1999
116. Naunheim KS, Hazelrigg SR, Kaiser LR, et al: Risk analysisfor thoracoscopic lung volume reduction: a multi-institutional experi-ence. Eur J Cardiothorac Surg 17:673-679, 2000
117. Hogue CW Jr, Stamos T, Winters KJ, et al: Acute myocardialinfarction during lung volume reduction surgery. Anesth Analg 88:332-334, 1999
118. Yusen RD, Meyers BF, Lefrak SS, et al: Outcomes of 200consecutive patients after lung volume reduction surgery. Chest 118:102S-103S, 2000
119. Health Care Financing Administration Report to Congress:Lung volume reduction surgery and Medicare coverage policy; impli-cations of recently published evidence. Washington DC, Department ofHealth and Human Services, 1998
120. The National Emphysema Treatment Trial Research Group:Rationale and Design of the National Emphysema Treatment Trial.Chest 116:1750-1761, 1999
121. Butler CW, Snyder M, Wood DE, et al: Underestimation ofmortality following lung volume reduction surgery resulting fromincomplete follow-up. Chest 119:1056-1060, 2001
381SEVERE EMPHYSEMA

122. Huizenga HF, Ramsey SD, Albert RK: Estimated growth oflung volume reduction surgery among Medicare enrollees. Chest 114:1583-1587, 1998
123. Medicare coverage policy. Statement of Bruce C. Vladeckbefore the House Ways and Means Committee, Subcommittee onHealth, April 17, 1997. Baltimore, MD, Health Care Financing Ad-ministration. Available from: http://cms.hhs.gov/testimony/1997/t970417a.asp. Accessed October 27, 2002
124. The National Emphysema Treatment Trial Research Group:Rationale and design of the National Emphysema Treatment Trial(NETT): A prospective randomized trial of lung volume reductionsurgery. J Thorac Cardiovasc Surg 118:518-528, 1999
125. National Emphysema Treatment Trial (NETT): Evaluation ofLung Volume Reduction Surgery for Emphysema. Available from:www.nhlbi.nih.gov/health/prof/lung/nett/lvrsweb.htm. Accessed Octo-ber 27, 2002
126. Ramsey SD, Sullivan SD, Kaplan RM, et al: Economic anal-ysis of lung volume reduction surgery as part of the national emphy-sema treatment trial. Ann Thorac Surg 71:995-1002, 2001
127. Drazen JM: Surgery for emphysema—Not for everyone.N Engl J Med 345:1126-1127, 2001
128. SoRelle R: Lung volume reduction surgery poses significantmortality risks to the sickest patients. Circulation 104:E9017-E9018,2001
129. Utz JP, Hubmayr RD, Deschamps C: Lung volume reductionsurgery for emphysema: out on a limb without a NETT. Mayo ClinProc 73:552-566, 1998
130. Miller JD, Malthaner RA, Goldsmith CH, et al: Lung volumereduction for emphysema and the Canadian Lung Volume ReductionSurgery (CLVR) Project. Can Respir J 6:26-32, 1999
131. National Emphysema Treatment Trial Research Group: Pa-tients at high risk of death after lung volume reduction surgery. N EnglJ Med 34:1075-1083, 2001
132. Hamacher J, Bloch KE, Stammberger U, et al: Two years’outcome of lung volume reduction surgery in different morphologicemphysema types. Ann Thorac Surg 68:1792-1798, 1999
133. Wisser W, Klepetko W, Kontrus M, et al: Morphologic gradingof the emphysematous lung and its relation to improvement after lungvolume reduction surgery. Ann Thorac Surg 65:793-799, 1998
134. Szekely LA, Oelberg DA, Wright C, et al: Preoperative pre-dictors of operative morbidity and mortality in patients undergoingbilateral lung volume reduction surgery. Chest 111:550-558, 1997
135. Mineo TC, Pompeo E, Togliani P, et al: Thoracoscopic reduc-tion pneumoplasty for severe emphysema: Do pleural adhesions affectoutcome? Thorac Cardiovasc Surg 47:288-292, 1999
136. Flaherty KR, Kazerooni EA, Curtis JL, et al: Short-term andlong-term outcomes after bilateral lung volume reduction surgery:Prediction by quantitative CT. Chest 119:1337-1346, 2001
137. McKenna RJ, Brenner M, Fischel RJ, et al: Patient selectioncriteria for lung volume reduction surgery. J Thorac Cardiovasc Surg114:957-967, 1997
138. Slone RM, Pilgram TK, Gierada DS, et al: Lung volumereduction surgery: comparison of preoperative radiological features andclinical outcome. Radiology 204:658-693, 1997
139. Serna DL, Brenner M, Osann KE, et al: Survival after unilat-eral versus bilateral lung volume reduction surgery for emphysema.J Thorac Cardiovasc Surg 118:1101-1109, 1999
140. Stammberger U, Klepetko W, Stamatis G, et al: Buttressing thestaple line in lung volume reduction surgery: A randomized three-center study. Ann Thorac Surg 70:1820-1825, 2000
141. McKenna RJ Jr, Brenner M, Gelb AF, et al: A randomized,prospective trial of stapled lung reduction versus laser bullectomy fordiffuse emphysema. J Thorac Cardiovasc Surg 111:317-322, 1996
142. Bloch KE, Georgescu CL, Russi EW, et al: Gain and subse-quent loss of lung function after lung volume reduction surgery in casesof severe emphysema with different morphological patterns. J ThoracCardiovasc Surg 123:845-854, 2002
143. Porter SH, Ruffin RE, Pfitzner J, et al: Videoscopic lungvolume reduction surgery in an Australian public teaching hospital.Aust N Z Med 30:202-208, 2000
144. Brenner M, McKenna RJ Jr, Gelb AF, et al: Rate of FEV1
change following lung volume reduction surgery. Chest 113:652-659,1998
145. Brenner M, McKenna RJ, Gelb AF: Dyspnea response follow-ing bilateral thoracoscopic staple lung volume reduction surgery. Chest112:916-923, 1997
146. Yusen RD, Pohl MS, Biggar DC, et al: Outcomes through 5years after lung volume reduction surgery. Chest 116:376S, 1999
147. Pohl MS, Yusen RD, Davin GE, et al: Quality of life in patients2 years and 3 years post-lung volume reduction surgery. Chest 114:351S-352S, 1998
148. Hamacher J, Buchi S, Georgescu CL, et al: Improved quality oflife after lung volume reduction surgery. Eur Respir J 19:54-60, 2002
149. Yusen RD, Anrecilla M, Pohl MS, et al: Change in lung anddiaphragmatic function and dyspnea following lung volume reductionsurgery. Chest 112:3S, 1997
150. Weg IL, Rossoff L, McKeon K, et al: Development of pulmo-nary hypertension after lung volume reduction surgery. Am J RespirCrit Care Med 159:552-556, 1999
151. Sugi K, Kaneda Y, Suga K, et al: Improvement of contralateralpulmonary function after unilateral lung volume reduction surgery(LVRS). Ann Thorac Cardiovasc Surg 6:363-368, 2000
152. Albert RK, Benditt JO, Hidelbrandt J, et al: Lung volumereduction surgery has variable effects on blood gases in patients withemphysema. Am J Respir Crit Care Med 158:71-76, 1998
153. Wisser W, Tschernka E, Senbaklavaci O: Functional improve-ment after volume reduction: Sternotomy versus videoendoscopic ap-proach. Ann Thorac Surg 63:822-828, 1997
154. Russi EW: Surgical lung volume reduction in emphysema:How much for how long? Chest 115:318-320, 1999
155. Brenner M, McKenna RJ Jr, Chen JC, et al: Relationshipbetween amount of lung resected and outcome after lung volumereduction surgery. Ann Thorac Surg 69:388-393, 2000
156. Mitsui K, Kurokawa Y, Kaiwa Y, et al: Thoracoscopic lungvolume reduction surgery for pulmonary emphysema patients withsevere hypercapnea. Jap J Thorac Cardiovasc Surg 49:481-488, 2001
157. Hunsaker A, Igenito E, Topal U, et al: Preoperative screeningfor lung volume reduction surgery: usefulness of combining thin sec-tion CT with physiological assessment. Am J Rad 170:309-314, 1998
158. Slone RM, Gierada DS, Yusen RD: Preoperative and postop-erative imaging in the surgical management of pulmonary emphysema.Rad Clin NA 36(1):57-89, 1998
159. Rogers RM, Coxson HO, Sciurba FC, et al: Preoperative se-verity of emphysema predictive of improvement after lung volumereduction surgery: Use of CT morphometry. Chest 118:1240-1247,2000
160. Gierada DS, Yusen RD, Villanueva IA, et al: Patient selectionfor lung volume reduction surgery: An objective model based on priorclinical decisions and quantitative CT analysis. Chest 117:991-998,2000
161. Cleverley JR, Hansell DM: Imaging of patients with severeemphysema considered for lung volume reduction surgery. Br J Radiol72:227-235, 1999
162. Coxson HO, Whittall KP, Rogers RM, et al: A cluster analysisof CT scans predicts patients who respond to lung volume reductionsurgery. Chest 117:247S-248S, 2000
382 GRICHNIK AND HILL

163. Russi EW, Bloch KE, Weder W: Functional and morphologicalheterogeneity of emphysema and its implication for selection of pa-tients for lung volume reduction surgery. Eur Respir J 14:230-236,1999
164. Sugi K, Kaneda Y, Murakami T, et al: The outcome of volumereduction surgery according to the underlying type of emphysema. SurgToday 31:580-585, 2001
165. Dueck R, Cooper S, Kapelanski D, et al: A pilot study ofexpiratory flow limitation and lung volume reduction surgery. Chest116:1762-1771, 1999
166. Tschernko EM, Kritzinger M, Gruber EM: Lung volume re-duction surgery: Preoperative functional predictors for postoperativeoutcome. Anesth Analg 88:28-33, 1999
167. Tschernko EM, Gruber EM, Jaksch P, et al: Ventilatory me-chanics and gas exchange during exercise before and after lung volumereduction surgery. Am J Respir Crit Care Med 158:1424-1431, 1998
168. Ingenito EP, Evans RB, Loring SH, et al: Relation betweenpreoperative inspiratory lung resistance and the outcome of lung vol-ume reduction surgery for emphysema. N Engl J Med 338:1181-1185,1998
169. McKenna RJ, Fischel RJ, Gelb AF: Combined operation forlung volume reduction surgery and lung cancer. Chest 110:885-888,1996
170. Duarte IG, Gal AA, Mansour KA, et al: Pathologic findings inlung volume reduction surgery. Chest 113:660-664, 1998
171. Pigula FA, Kennan RJ, Terson PF, et al: Unsuspected lungcancer found in work-up for lung reduction operation. Ann Thorac Surg61:174-176, 1996
172. DeRose JJ, Argenziano M, El-Amir N, et al: Lung reductionoperation and resection of pulmonary nodules in patients with severeemphysema. Ann Thorac Surg 65:314-318, 1998
173. Whyte RI, Bria W, Martinez FL, et al: Combined lung volumereduction surgery and mitral valve reconstruction. Ann Thorac Surg66:1414-1416, 1998
174. Zannini P, Caretta A, Chiesa R, et al: Combined lung volumereduction surgery and thoracic aortic aneurysm resection. J CardiovascSurg (Torino) 139:509-510, 1998
175. Schmid RA, Staminberger U, Hillinger S, et al: Lung volumereduction surgery combined with cardiac interventions. Eur J Cardio-thorac Surg 15:585-591, 1999
176. Arcsoy AM, Kotloff RM: Lung transplantation. N Engl J Med340:1081-1091, 1999
177. O’Brien GM, Criner GJ: Surgery for severe COPD: Lungvolume reduction and lung transplantation. Postgrad Med 103:179-80,1998
178. Schulman LL: Lung transplantation for chronic obstructivepulmonary disease. Clin Chest Med 21:849-865, 2000
179. ISHLT Nineteenth Annual Heart/Lung Registry 2002 Data2002 DATA. Available from: https://www.ishlt.org/regist_heart-lung_slide_toc.htm. Accessed September 19, 2002
180. Weill D, Keshavjee S: Lung transplantation for emphysema:Two lungs or one? J Heart Lung Transpl 20:739-742, 2001
181. Sundaresan S, Shiraishi Y, Trulock EP, et al: Single or bilaterallung transplantation for emphysema? J Thorac Cardiovasc Surg 112:1485-1495, 1996
182. Brunsting LA, Lupinetti FM, Cascade PN, et al: Pulmonaryfunction in single-lung transplantation for chronic obstructive pulmo-nary disease. J Thorac Cardiovasc Surg 107:1337-1345, 1994
183. Martinez JA, Paradis IL, Dauber JH, et al: Spirometry values instable lung transplant recipients. Am J Respir Crit Care Med 155:285-290, 1997
184. Arens R, McDonough JM, Zhao H, et al: Altered lung mechan-ics after double-lung transplantation. Am J Respir Crit Care Med158:1403-1409, 1998
185. Low DE, Trulock EP, Kaiser LR, et al: Morbidity, mortality,and early results of single versus bilateral lung transplantation foremphysema. J Thorac Cardiovasc Surg 103:1119-1126, 1992
186. Herlihy JP, Venegas JC, Systrom DM, et al: Expiratory flowpattern following single-lung transplantation in emphysema. Am JRespir Crit Care Med 150:1684-1689, 1994
187. Cheriyan AF, Garrity ER, Pifarre R, et al: Reduced transplantlung volumes after single-lung transplantation for chronic obstructivepulmonary disease. Am J Respir Crit Care Med 151:851-853, 1995
188. Estenne M, Cassart M, Poncelet P, et al: Volume of graft andnative lung after single-lung transplantation for emphysema. Am JRespir Crit Care Med 159:641-645, 1999
189. Cassart M, Verbandt Y, de Francquen P, et al: Diaphragmdimensions after single-lung transplantation for emphysema. Am JRespir Crit Care Med 159:1992-1997, 1999
190. Levine SM, Aznueto A, Peters JL, et al: Medium term func-tional results of single-lung transplantation for endstage obstructivelung disease. Am J Respir Crit Care Med 150:398-402, 1994
191. Orens JB, Becker FS, Lynch JP III, et al: Cardiopulmonaryexercise testing following allogeneic lung transplantation for differentunderlying disease states. Chest 107:144-149, 1995
192. Bando K, Paradis JL, Komastu K, et al: Analysis of time-dependent risks for infection, rejection, and deaths after pulmonarytransplantation. J Thorac Cardiovasc Surg 109:49-59, 1995
193. Arcasoy SM, Kotloff RM: Lung transplantation. N Engl J Med340:1081-1091, 1999
194. Christie JD, Bavaria JE, Palevsky HI, et al: Primary graftfailure following lung transplantation. Chest 114:51-60, 1998
195. Berkowitz N, Schulman LL, McGregor C, et al: Gastroparesisafter lung transplantation. Potential role in postoperative respiratorycomplications. Chest 108:1602-1607, 1995
196. Smiley RM: Postoperative independent ventilation in a single-lung transplant recipient. Anesthesiology 74:1144-1148, 1991
197. Weill D, Torres F, Hodges TN, et al: Acute native lung hyper-inflation is not associated with poor outcomes after single-lung trans-plant for emphysema. J Heart Lung Transplant 18:1080-1087, 1999
198. Schulman LL: Physiology of the transplanted lung, in NormanDJ, Suki WN, (eds): Primer on Transplantation. Chelsea, MI, Slack Inc,1998, 519-26
199. Frost AE, Keller CA, Noon GP, et al: Outcome of the nativelung after single-lung transplant. Chest 107:981-984, 1995
200. Hosenpud JD, Bennett LE, Keck BM, et al: The Registry of theInternational Society for Heart and Lung Transplantation: EighteenthOfficial Report-2001. J Heart Lung Transpl 20:805-815, 2001
201. Hosenpud JD: Effect of diagnosis on survival benefit of lungtransplantation for end-stage lung disease. Lancet 351:24-27, 1998
202. Gross CR, Savik K, Bolman RM, et al: Long-term health statusand quality of life outcomes of lung transplant recipients. Chest 108:1587-1593, 1995
203. Gassiert HA, Trulock EP, Cooper JD, et al: Comparison ofearly functional results after volume reduction or lung transplantationfor chronic obstructive pulmonary disease. J Thorac Cardiovasc Surg111:296-307, 1996
204. Zenati M, Keenan RJ, Courcoulas AP, et al: Lung volumereduction or lung transplantation for end-stage pulmonary emphysema?Eur J Cardiothorac Surg 14:27-32, 1998
205. Meyers BF, Yusen RD, Guthrie RJ, et al: Outcome of bilaterallung volume reduction in patients with emphysema potentially eligiblefor lung transplantation. J Thorac Cardiovasc Surg 122:10-17, 2001
206. Ramsey SD, Patrick DK, Albert RK, et al: The cost-effective-ness of lung transplantation: A pilot study. Chest 108:1594-1601, 1995
207. Meyer DM, Bennett LE, Norvick RJ, et al: Single versusbilateral, sequential lung transplantation for end-stage emphysema:
383SEVERE EMPHYSEMA

Influence of the recipient age on survival. J Heart Lung Transpl20:935-941, 2001
208. Zenati M, Keenan RJ, Landreneau RJ, et al: Lung reduction asa bridge to lung transplantation in pulmonary emphysema. Ann ThoracSurg 59:1581-1583, 1995
209. Kroshus TJ, Bolman RM, Kshettry VR: Unilateral volumereduction after single-lung transplantation for emphysema. Ann ThoracSurg 62:363-380, 1996
210. Yonan NA, el-Gamel A, Egan J, et al: Single-lung transplan-tation for emphysema: Predictors for native lung hyperinflation. J HeartLung Tranpl 17(2):192-201, 1998
211. Schulman LL, O’Hair DP, Cantu E, et al: Salvage by volumereduction of chronic allograft rejection in emphysema. J Heart LungTransplant 18:107-112, 1999
212. Smetana GW: Preoperative pulmonary evaluation. New EnglJ Med 340:937-944, 1999
213. Kroenke K, Lawrence VA, Theroux JF, et al: Postoperativecomplications after thoracic and major abdominal surgery in patientswith and without obstructive lung disease. Chest 104:1445-1451, 1993
214. Wightman JA: A prospective survey of the incidence of post-operative pulmonary complications. Br J Surg 55:85-91, 1968
215. Pedersen T, Eliasen K, Henriksen E: A prospective study ofrisk factors and cardiopulmonary complications associated with anaes-thesia and surgery: risk indicators of cardiopulmonary morbidity. ActaAnaesthesiol Scand 34:144-155, 1990
216. Tarhan S, Moffitt EA, Sessler AD, et al: Risk of anesthesia andsurgery in patients with chronic bronchitis and chronic obstructivepulmonary disease. Surgery 74:720-726, 1973
217. Sabanathan S, Eng J, Mearns AJ: Alteration in respiratorymechanics following thoracotomy. J R Coll Surg Edinb 35:144-150,1990
218. Eisenkraft JB, Cohen E, Neustein SM: Anesthesia for thoracicsurgery, in Barash PG, Cullen BF, Stoelting RK, (eds): Clinical Anes-thesia. (ed 3). Philadelphia, PA, Lippincott-Raven, 1997, 769-803
219. Benumof JL, Alfery DD: Anesthesia for thoracic surgery, inMiller RD, (ed): Anesthesia. (ed 3). New York, NY, Churchill Living-stone, 1990, 1521
220. Gass GD, Olsen GN: Preoperative pulmonary function testingto predict postoperative morbidity and mortality. Chest 89:127-135,1986
221. Boysen PG: Evaluation of the patient with pulmonary disease,in Rogers MC, Tinker JH, Covino BG, et al (eds): Principles andPractice of Anesthesiology (vol 1). St. Louis, MO, Mosby Year Book,1993, 238
222. Lawrence VA, Page CP, Harris GD: Preoperative spirometrybefore abdominal operations: A critical appraisal of its predictive value.Arch Intern Med 149:280-285, 1989
223. Olsen GN, Block AJ, Swenson EW, et al: Pulmonary functionevaluation of the lung resection candidate: A prospective study. AmRev Respir Dis 111:379-387, 1975
224. Lawrence VA, Dhanda R, Hilsenbeck SG, et al: Risk of pul-monary complications after elective abdominal surgery. Chest 110:744-750, 1996
225. Williams-Russo P, Charlson ME, MacKenzie CR, et al: Pre-dicting postoperative pulmonary complications: Is it a real problem?Arch Intern Med 152:1209-1213, 1992
226. Cain HD, Stevens PM, Adaniya R: Preoperative pulmonaryfunction and complications after cardiovascular surgery. Chest 76:130-135, 1979
227. Melendez JA, Carlon VA: Cardiopulmonary risk index doesnot predict complications after thoracic surgery. Chest 114:69-75, 1998
228. Nakahara K, Ohno K, Hashimoto J, et al: Prediction of post-operative respiratory failure in patients undergoing lung resection forlung cancer. Ann Thorac Surg 46:549-552, 1988
229. Milledge JS, Nunn JF: Criteria of fitness for anaesthesia inpatients with chronic obstructive lung disease. Brit Med J 13:670-673,1975
230. Stein M, Koota GM, Simon M, et al: Pulmonary evaluation ofsurgical patients. JAMA 181:765-770, 1962
231. Bollinger CT, Jordan P, Solar M, et al: Exercise capacity as apredictor of postoperative complications in lung resection candidates.Am J Respir Crit Care Med 151:1472-1480, 1995
232. Epstein SK, Faling LJ, Daly BD, et al: Inability to performbicycle ergometry predicts increased morbidity and mortality after lungresection. Chest 107:311-316, 1995
233. Jayr C, Matthay M, Goldstone J, et al: Preoperative and intra-operative factors associated with prolonged mechanical ventilation. Astudy in patients following major abdominal vascular surgery. Chest103:1231-1236, 1993
234. Nunn JF, Milledge JS, Chen D, et al: Respiratory criteria offitness for surgery and anaesthesia. Anaesthesia 43:543-551, 1988
235. Rao MK, Reilly TE, Schuller DE, et al: Analysis of risk factorsfor postoperative complication in head and neck surgery. Laryngoscope102:45-47, 1992
236. Slinger PD, Johnston MR: Preoperative assessment for pulmo-nary resection. J Cardiothorac Vasc Anesth 14:202-211, 2000
237. Walsh GL, Morice RC, Putnam JB, et al: Resection of lungcancer is justified in high-risk patients selected by exercise oxygenconsumption. Ann Thorac Surg 58:704-711, 1994
238. Bollinger CT, Wyser C, Roser H, et al: Lung scanning andexercise testing for the prediction of postoperative performance in lungresection candidates at increased risk of complications. Chest 108:341-348, 1995
239. Cahalin L, Pappagianapoulos P, Prevost S, et al: The relation-ship of the 6-minute walk test to maximal oxygen consumption intransplant candidates with end-stage lung disease. Chest 108:452-457,1995
240. Ferguson MK, Reeder LB, Mich R: Optimizing selection ofpatients for major lung resection. J Thorac Cardiovasc Surg 109:275-283, 1995
241. Gross JB, Zebrowski ME, Carel WD, et al: Time course ofventilatory depression after thiopental and midazolam in normal sub-jects and in patients with chronic obstructive pulmonary disease. An-esthesiology 58:540-544, 1983
242. Begin P, Grassino A: Inspiratory muscle dysfunction andchronic hypercapnea in chronic obstructive pulmonary disease. AmRev Respir Dis 143:905-912, 1991
243. Raghavendran S, Diwan R, Shah T, et al: Continuous caudalepidural analgesia for congenital lobar emphysema: A report of threecases. Anesth Analg 93:348-350, 2001
244. Guinard JP, Maurocordatos P, Chiolero R, et al: A randomizedcomparison of intravenous vs. lumbar and thoracic epidural fentanyl foranalgesia after thoracotomy. Anesthesiology 77:1108-1115, 1992
245. Kahn L, Baxter FJ, Dauphin A, et al: A comparison of thoracicand lumbar epidural techniques for post-thoracoabdominal esophagec-tomy analgesia. Can J Anaesth 46:415-422, 1999
246. Coe A, Sarginson R, Smith MW, et al: Pain following thora-cotomy: A randomized double-blind comparison of lumbar versusthoracic epidural fentanyl. Anaesthesia 46:918-921, 1991
247. Hansdottir V, Woestenborghs R, Nordberg G: The cerebrospi-nal fluid and plasma pharmcokinetics of sufentanil after thoracic orlumbar epidural administration. Anesth Analg 80:724-729, 1995
248. Tejwani GA, Rattan AK, McDonald JS: Role of spinal opioidreceptors in the antinociceptive interactions between intrathecal mor-phine and bupivacaine. Anesth Analg 74:726-734, 1992
249. Karmakar MK: Thoracic paravertebral block. Anesthesiology95:771-780, 2001
384 GRICHNIK AND HILL

250. Tschernko EM, Klepetko H, Gruber EM, et al: Clonidine addedto the anesthetic solution enhances analgesia and improves oxygenationafter intercostal nerve block for thoracotomy. Anesth Analg 87:107-111, 1998
251. Matsota P, Livanios S, Marinopoulou E: Intercostal nerveblock with bupivacaine for post-thoracotomy pain relief in children.Eur J Ped Surg 11:219-222, 2001
252. Liu N, Kuhlman G, Dalibon N, et al: A randomized, double-blinded comparison of intrathecal morphine, sufentanil and their com-bination versus IV morphine patient-controlled analgesia for post-thoracotomy pain. Anesth Analg 92:31-36, 2001
253. Cohen E, Neustein SM: Intrathecal morphine during thoracot-omy. Part I: Effect on intraoperative enflurane requirements. J Cardio-thorac Vasc Anesth 7:154-156, 1993
254. Neustein SM, Cohen E: Intrathecal morphine during thoracot-omy. Part II: Effect on postoperative meperidine requirements andpulmonary function tests. J Cardiothorac Vasc Anesth 7:157-159, 1993
255. Richardson J, Lonnqvist PA: Thoracic paravertebral block. Br JAnaesth 81:230-238, 1998
256. Lonnqvist PA, MacKenzie J, Soni AK, et al: Paravertebralblockade: Failure rate and complications. Anaesthesia 50:813-815,1995
257. Bimston DN, McGee JP, Liptay MJ, Fry WA: Continuousparavertebral extrapleural infusion for post-thoracotomy pain manage-ment. Surgery 126:650-656, 1999
258. Ganapathy S, Murkin JM, Boyd DW, et al: Continuous percu-taneous paravertebral block for minimally invasive cardiac surgery.J Cardiothorac Vasc Anesth 113:594-596, 1999
259. Barron DJ, Tolan MJ, Lea RE: A randomized controlled trial ofcontinuous extrapleural analgesia post-thoracotomy: Efficacy andchoice of local anaesthetic. Eur J Anaesthesiol 16:236-245, 1999
260. Watson DS, Panian S, Kendall V, et al: Pain control afterthoracotomy: Bupivacaine versus lidocaine in continuous extrapleuralintercostal nerve blockade. Ann Thorac Surg 67:825-828disc 828-829,1999
261. Michaloudias D, Petrou A, Bakos P, et al: Continuous spinalanaesthesia/analgesia for the perioperative management of high-riskpatients. Eur J Anaesth 17:239-247, 2000
262. Vercauteren MP, Geernaert K, Hoffmann VL, et al: Postoper-ative intrathecal patient-controlled analgesia with bupivacaine, sufen-tanil or a mixture of both. Anaesthesia 53:1022-1027, 1998
263. Shook JE, Watkins WD, Camporesi EM: Differential roles ofopioid receptors in respiration, respiratory disease, and opiate-inducedrespiratory depression. Am Rev Respir Dis 142:895-909, 1990
264. Ahuja BR, Strunin L: Respiratory effects of epidural fentanyl:Changes in end-tidal CO2 and respiratory rate following single dosesand continuous infusion of epidural fentanyl. Anaesthesia 40:949-955,1985
265. Renaud B, Brichant JF, Clergue F, et al: Ventilatory effects ofcontinuous epidural infusion of fentanyl. Anesth Analg 67:971-975,1988
266. Sandler AN, Chovaz P, Whiting W: Respiratory depressionfollowing epidural morphine: A clinical study. Can Anaesth Soc J33:542-549, 1986
267. Knill RL, Clement JL, Thompson WR: Epidural morphinecauses delayed and prolonged ventilatory depression. Can Anaesth SocJ 28:537-543, 1981
268. Moren J, Francois T, Blanloeil Y, et al: The effects of anonsteroidal antiinflammatory drug (ketoprofen) on morphine respira-tory depression: A double-blind, randomized study in volunteers.Anesth Analg 85:400-505, 1997
269. Groeben H, Schwalen A, Irsfeld S, et al: High thoracic epiduralanesthesia does not alter airway resistance and attenuates the response
to an inhalational provocation test in patients with bronchial hyperre-activity. Anesthesiology 81:868-874, 1994
270. Gruber EM, Tschernko EM, Kritzinger M, et al: The effects ofthoracic epidural analgesia with bupivacaine 0.25% on ventilatorymechanics in patients with severe chronic obstructive pulmonary dis-ease. Anesth Analg 92:1015-1019, 2001
271. Richardson J, Sabanthan S, Shah R: Post-thoracotomy spiro-metric lung function: The effect of analgesia: A review. J CardiovascSurg 40:445-446, 1999
272. Ballantyne JC, Carr DB, deFerranti S, et al: The comparativeeffects of postoperative analgesic therapies on pulmonary outcome:Cumulative meta-analyses of randomized controlled trials. AnesthAnalg 86:598-612, 1998
273. Cerfolio RJ, Allen MS, Trastek VF, et al: Lung resection inpatients with compromised pulmonary function. Ann Thorac Surg62:348-351, 1996
274. Oka T, Ozawa Y, Ohkubo Y: Thoracic epidural bupivacaineattenuates supraventricular tachydysrhythmias after pulmonary resec-tion. Anesth Analg 93:253-259, 2001
275. Samian E, Farah E, Delefosse D, et al: End-tidal oxygraphyduring preoxygenation in patients with severe diffuse emphysema.Anaesthesia 55:841-846, 2000
276. Lapinsky SE, Leung RS: Auto-PEEP and electromechanicaldissociation. New Engl J Med 335:674, 1996
277. Rosengarten PL, Tuxen DV, Dziukas L, et al: Circulatoryarrest induced by intermittent positive-pressure ventilation in a patientwith severe asthma. Anaesth Intensive Care 19:118-121, 1991
278. Rogers PL, Schlichtig R, Miro A, et al: Auto-PEEP duringCPR: an “occult” cause of electromechanical dissociation? Chest 99:492-493, 1991
279. Martens P, Vandekerckhove Y, Mullie A: Restoration of spon-taneous circulation after cessation of cardiopulmonary resuscitation.Lancet 341:841, 1993
280. Sprung J, Hunter K, Barnas GM, et al: Abdominal distention isnot always a sign of esophageal intubation: Cardiac arrest due to“auto-PEEP”. Anesth Analg 78:801-804, 1994
281. Connery LE, Deignan MJ, Gujer MW, et al: Cardiovascularcollapse associated with extreme iatrogenic PEEPi in patients withobstructive airways disease. Br J Anaesth 83:493-495, 1999
282. Tugrul M, Camci E, Karadeniz H, et al: Comparison of vol-ume-controlled with pressure-controlled ventilation during one-lunganaesthesia. Br J Anaesth 79:306-310, 1997
283. Olssen GL: Bronchospasm during anesthesia: A computer-aided incidence study of 136,929 patients. Acta Anaesthesiol Scand31:244-252, 1987
284. Groeben H, Schwalen A, Irsfeld S, et al: Intravenous lidocaineand bupivacaine dose dependently attenuate bronchial hyperreactivityin awake volunteers. Anesthesiology 84:533-539, 1996
285. Groeben H, Silvanus M-T, Beste M, et al: Combined intrave-nous lidocaine and inhaled salbutamol protect against bronchial hyper-reactivity more effectively than lidocaine or salbutamol alone. Anes-thesiology 89:862-868, 1998
286. Zemenick RB: Pretreatment intravenous lidocaine for intuba-tion of the asthmatic patient: More data are needed. Anesthesiology91:319(letter), 1999
287. Hirota K, Hashimoto Y, Sato T, et al: Lidocaine worsenshistamine-induced bronchoconstriction in dogs. Br J Anaesth 82:87-89,1999
288. Maslow AD, Regan MM, Israel E, et al: Inhaled albuterol, butnot intravenous lidocaine, protects against intubation-induced broncho-constriction in asthma. Anesthesiology 93:1198-204, 2000
289. Klock PA, Czeslick EG, Klafta JM, et al: The effect of sevoflu-rane and desflurane on upper airway reactivity. Anesthesiology 94:963-967, 2001
385SEVERE EMPHYSEMA

290. Laghi F, Segal J, Choe WK, et al: Effect of imposed inflationtime on respiratory frequency and hyperinflation in patients withchronic obstructive pulmonary disease. Am J Respir Crit Care Med163:1365-1370, 2001
291. Krucylak PE, Naunheim KS, Keller CA, et al: Anestheticmanagement of patients undergoing unilateral video-assisted lung re-duction for treatment of end-stage emphysema. J Cardiothorac VascAnesth 10:850-853, 1996
292. Slinger PD, Hickey DR: The interaction between applied PEEPand auto-PEEP during one-lung ventilation. J Cardiothorac VascAnesth 12:133-136, 1998
293. Bardoczky GI, d’Hollander AA, Rocmans P, et al: Respiratorymechanics and gas exchange during one-lung ventilation for thoracicsurgery: The effects of end-expiratory pause in stable COPD patients.J Cardiothorac Vasc Anesth 12:137-141, 1998
294. Berg H, Viby-Mogensen J, Roed J, et al: Residual neuromus-cular block is a risk factor for postoperative pulmonary complications:A prospective, randomized, and blinded study of postoperative pulmo-nary complications after atracurium, vecuronium, and pancuronium.Acta Anaesthesiol Scand 41:1095-1103, 1997
295. Liu EH, Gillbe CE, Watson AC: Anaesthetic management ofpatients undergoing lung volume reduction surgery for treatment ofsevere emphysema. Anaesth Intensive Care 27:459-463, 1999
296. Zollinger A, Zaugg M, Weder W, et al: Video-assisted thora-coscopic volume reduction surgery in patients with diffuse pulmonaryemphysema: Gas exchange and anesthesiological management. AnesthAnalg 84:845-851, 1997
297. Sumpf E, Crozier TA, Ahrens D, et al: Carbon dioxide absorp-tion during extraperitoneal and transperitoneal endoscopic hernio-plasty. Anesth Analg 91:589-595, 2000
298. Morisaki H, Serita R, Innami Y, et al: Permissive hypercapniaduring thoracic anaesthesia. Acta Anaesthesiol Scand 43:845-849,1999
299. Slinger P, Blundell PE, Metcalf IR: Management of massivegrain aspiration. Anesthesiology 87:993-995, 1997
300. Knill R, Manninen P, Clement J: Ventilation and chemore-flexes during enflurane sedation and anesthesia in man. Can AnaesthSoc J 26:353-360, 1979
301. Pietak S, Weening CS, Hickey RF, et al: Anesthetic effects onventilation in patients with chronic obstructive pulmonary disease.Anesthesiology 42:160-166, 1975
302. Barker S, Clarke C, Trivedi N, et al: Anesthesia for thoraco-scopic laser ablation of bullous emphysema. Anesthesiology 78:44-50,1993
303. Triantafillou AN: Anesthetic management for bilateral volumereduction surgery. Semin Thorac Cardiovasc Surg 8:94-98, 1996
304. Liu EH, Gillbe CE, Watson AC: Anaesthetic management ofpatients undergoing lung volume reduction surgery for treatment ofsevere emphysema. Anaesth Intensive Care 27:459-463, 1999
305. Nunn JF: Effects of anaesthesia on respiration. Br J Anaesth65:54-62, 1990
306. Rossi A, Polese G, Brandi G, et al: Intrinsic positive end-expiratory pressure (PEEPi). Intensive Care Med 21:522-536, 1995
307. Slinger P, Leiuk L: Flow resistances of disposable double-lumen, single-lumen and univent tubes. J Cardiothorac Vasc Anesth12:142-144, 1998
308. Bardoczky GI, Yernault JC, Engelman E, et al: Intrinsic pos-itive end-expiratory pressure during one-lung ventilation for thoracicsurgery: The influence of preoperative pulmonary function. Chest 111:180-184, 1996
309. Yokota K, Toriumi T, Sari A, et al: Auto-positive end-expira-tory pressure during one-lung ventilation using a double-lumen endo-bronchial tube. Anesth Analg 82:1007-1010, 1996
310. Myles PS, Ryder IG, Weeks AM, et al: Diagnosis and man-agement of dynamic hyperinflation during lung transplantation. J Car-diothorac Vasc Anesth 11:100-104, 1997
311. Bardoczky G, d’Hollander A, Cappello M, et al: Interruptedexpiratory flow on automatically constructed flow-volume curves maydetermine the presence of intrinsic positive end-expiratory pressureduring one-lung ventilation. Anesth Analg 86:880-884, 1998
312. Ducros L, Moutafis M, Castlelain M-H, et al: Pulmonary airtrapping during two-lung and one-lung ventilation. J Cardiothorac VascAnesth 13:35-39, 1999
313. Idem Consensus Conference on Mechanical Ventilation—Jan-uary 28-30, 1993 at Northbrook, Illinois, USA. Part I. Intensive CareMed 20: 64-79, 1994
314. Eisner MD, Thompson BT, Schoenfeld D, et al: Airway pres-sures in patients with acute lung injury and acute respiratory distresssyndrome. Am J Respir Crit Care Med 165:978-982, 2002
315. The Acute Respiratory Distress Syndrome Network: Ventila-tion with lower tidal volumes as compared with traditional tidal vol-umes for acute lung injury and the acute respiratory distress syndrome.N Engl J Med 342:1301-1308, 2000
316. Takeuchi M, Goddon S, Dolhnikoff M, et al: Set positiveend-expiratory pressure during protective ventilation affects lung in-jury. Anesthesiology 97:682-692, 2002
317. Amato MB, Barbas CS, Medeiros DM, et al: Effect of aprotective ventilation strategy on mortality in the acute respiratorydistress syndrome. New Engl J Med 338:347-354, 1998
318. Malik S, Shapiro WA, Jablons D, et al: Contralateral tensionpneumothorax during one-lung ventilation for lobectomy: Diagnosisaided by fiberoptic bronchoscopy. Anesth Analg 95:570-572, 1995
319. Keller CA, Naunheim KS: Perioperative management of lungreduction patients. Clin Chest Med 18:285-300, 1997
320. Maunder RJ, Pierson DJ, Hudson LD: Subcutaneous and me-diastinal emphysema. Arch Intern Med 144:1447-1453, 1984
321. Sucato DJ, Girgis M: Bilateral pneumothoraces, pneumomedi-astinum, pneumoperitoneum, pneumoretroperitoneum and subcutane-ous emphysema following intubation with a double-lumen endotra-cheal tube for thoracoscopic anterior spinal release and fusion in apatient with idiopathic scoliosis. J Spinal Disord Tech 15:133-138,2002
322. Slinger PD: Perioperative fluid management for thoracic sur-gery: The puzzle of postpneumonectomy pulmonary edema. J Cardio-thorac Vasc Anesth 9:442-451, 1995
323. Krasna MJ, Deshmukh S, McLaughlin JS: Complications ofthoracoscopy. Ann Thorac Surg 61:1066-1069, 1996
324. Waller DA, Gebitekin C, Saunders NR, et al: Noncardiogenicpulmonary edema complicating lung resection. Ann Thorac Surg 55:140-143, 1993
325. Jordan S, Mitchell JA, Quinlan GJ, et al: The pathogenesis oflung injury following pulmonary resection. Eur Respir J 15:790-799,2000
326. Wittnich C, Trudel J, Zidulka A, et al: Misleading “pulmonarywedge pressure” after pneumonectomy: its importance in postoperativefluid therapy. Ann Thorac Surg 42:192-196, 1986
327. Hoyt JD, Leatherman JW: Interpretation of the pulmonaryartery occlusion pressure in mechanically ventilated patients with largerespiratory excursions in intrathoracic pressure. Intensive Care Med23:1125-1131, 1997
328. Zeldin RA, Normandin D, Landtwing D, et al: Postpneumo-nectomy pulmonary edema. J Thorac Cardiovasc Surg 87:359-365,1984
329. Verheijen-Breemharr L, Bogaard JM, van den Berg B: Non-cardiogenic pulmonary edema complicating lung resection. Ann Tho-rac Surg 43:323-326, 1988
386 GRICHNIK AND HILL

330. Parquin F, Marchal M, Meehiri S, et al: Post-pneumonectomypulmonary edema: Analysis and risk factors. Eur J Cardiothorac Surg10:929-933, 1996
331. Turnage WS, Lunn JJ: Postpneumonectomy pulmonary edema:A retrospective analysis of associated variables. Chest 103:1646-1650,1993
332. Alvarez JM, Bairstow BM, Tang C, et al: Post-lung resectionpulmonary edema: A case for aggressive management. J CardiothoracVasc Anesth 12:199-205, 1998
333. Satur CM, Gupta NK: Postpneumonectomy pulmonary edemaor microembolism? Ann Thorac Surg 57:523-524, 1994
334. Deslauriers J, Aucoin A, Gregoire J: Postpneumonectomy pul-monary edema. Chest Surg Clin North Am 8:611-631, 1998
335. Lases EC, Duurkens VA, Gerristen WB, et al: Oxidative stressafter lung resection therapy: A pilot study. Chest 117:999-1003, 2000
336. Caras WE: Postpneumonectomy pulmonary edema: Can it bepredicted? Chest 114:928-931, 1998
337. Nohl-Oser HC: An investigation of the anatomy of the lym-phatic drainage of the lungs as shown by the lymphatic spread ofbronchial carcinoma. Ann R Coll Surg 51:157-176, 1972
338. Kellow NH, Scott AD, Kaplan D, et al: Early changes in rightventricular function following lung resection. J Cardiothorac Vasc Surg8(suppl):124, 1994
339. van der Werff YD, van der Houwen HK, Jeijmans PJM, et al:Postpneumonectomy pulmonary edema. Chest 111:1278-1284, 1997
340. Jansen JP, Brutel del la Riviere A, Carpentier Alting MP, et al:Post-pneumonectomy syndrome in adulthood. Chest 101:1167-1170,1992
341. Amato MBP, Barbes CSU, Medicros DM: Beneficial effects ofthe ‘open lung approach’ with distending pressures in acute respiratorydistress. Am J Respir Crit Care Med 1523:1835-1846, 1995
342. Szagedi LL, Bardoczky GI, Engleman EE, et al: Airway pres-sure changes during one-lung ventilation. Anesth Analg 84:1034-1037,1997
343. Albert RK, Lakshminarayan S, Kirk W, et al: Lung inflationcan cause pulmonary edema in zone 1 of in situ dog lungs. J ApplPhysiol 49:815-819, 1980
344. Holte K, Sharrock NE, Kehlet H: Pathophysiology and clinicalimplications of perioperative fluid excess. Brit J Anaesth 89:622-632,2002
345. Arieff AI: Fatal postoperative pulmonary edema: pathogenesisand literature review. Chest 115:1371-1377, 1999
346. Christopherson RP, Beattie C, Frank SM, et al: Perioperativemorbidity in patients randomized to epidural or general anesthesia forlower extremity vascular surgery. Anesthesiology 79:422-434, 1993
347. Vaupshas HJ, Levy M: Distribution of saline following acutevolume loading: Postural effects. Clin Invest Med 13:165-177, 1990
348. Ernest D, Belzberg AS, Dodeck PM: Distribution of normalsaline and 5% albumin infusions in septic patients. Crit Care Med27:46-50, 1999
349. Lang K, Boldt J, Suttner S, et al: Colloids versus crystalloidsand tissue oxygen tension in patients undergoing major abdominalsurgery. Anesth Analg 93:405-409, 2001
350. Boldt J: The good, the bad, and the ugly: Should we completelybanish human albumin from our intensive care units? Anesth Analg91:887-895, 2000
351. Schierhout G, Roberts I: Fluid resuscitation with colloid orcrystalloid solutions in critically ill patients: A systematic review ofrandomized trials. Brit Med J 316:961-964, 1998
352. Goodwin CW, Dorethy J, Lam V, et al: Randomized trial ofefficacy of crystalloid and colloid resuscitation on hemodynamic re-sponse and lung water following thermal injury. Ann Surg 197:520-531, 1983
353. Choi PT-L, Yip G, Quinonez LG, Cook DJ: Crystalloids vs.colloids in fluid resuscitation: A systematic review. Crit Care Med27:200-210, 1999
354. Asamura H, Naruke T, Tsuchiya R, et al: What are the riskfactors for arrhythmias after thoracic operations? J Thorac CardiovascSurg 106:1104-1110, 1993
355. Benmof JL: Anesthesia for Thoracic Surgery. Philadelphia,PA, Saunders, 1995
356. Amar D, Roistacher N, Burt M, et al: Clinical and echocardio-graphic correlates of symptomatic tachydysrhythmias after noncardiacthoracic surgery. Chest 108:349-354, 1995
357. Haniuda M, Kubo K, Fujimoto K, et al: Different effects oflung volume reduction surgery and lobectomy on pulmonary circula-tion. Ann Surg 231:119-125, 2000
358. Reed CE, Dorman BH, Spinale FG: Mechanisms of rightventricular dysfunction after pulmonary resection. Ann Thorac Surg62:225-232, 1996
359. Yusim Y, Berkenstadt H, Keidan I, et al: Malignant hyperin-flation of the nondependent lung during chest surgery. Eur J Anaesth18:774-777, 2001
360. Temes RT, Talbot WA, Green DP, et al: Herniation of the lungafter video-assisted thoracic surgery. Ann Thorac Surg 72:606-607,2001
361. Miller JI Jr: Acute and delayed space problems followingpulmonary resection. Chest Surg Clin North Am 6:615-21, 1996
387SEVERE EMPHYSEMA








![Acute or chronic pulmonary emphysema? Or both?—A ......emphysema or acute alveolar dilation, respectively [3 , 5]. In some cases, an interstitial emphysema is described [, 636].](https://static.fdocuments.net/doc/165x107/6138f505a4cdb41a985b64ce/acute-or-chronic-pulmonary-emphysema-or-bothaa-emphysema-or-acute-alveolar.jpg)