Renal physiology in pregnancy
-
Upload
nandinii-ramasenderan -
Category
Health & Medicine
-
view
1.495 -
download
2
Transcript of Renal physiology in pregnancy

Renal PhysiologyNandinii Ramasenderan (K1)

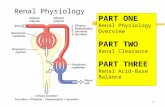
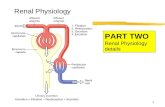
A. Renal Vein
B. Renal Artery
C. Ureter
D. Medulla
E. Renal Pelvis
F. Cortex
1. Ascending loop of Henle
2. Descending loop of Henle
3. Peritubular capillaries
4. Proximal tubule
5. Glomerulus
6. Distal tubule
The Kidney and the Nephron

•Glomerulus
•Afferent and Efferent arterioles
•Proximal Tubule
•Loop of Henle
•Distal Tubule
•Collecting Duct
Components of the nephron

Functions of the Kidney:Maintaining balance
• Regulation of body fluid volume and osmolality• Regulation of electrolyte balance• Regulation of acid-base balance• Excretion of waste products (urea, ammonia, drugs, toxins)• Production and secretion of hormones• Regulation of blood pressure

From http://www.emc.maricopa.edu/faculty/farabee/BIOBK/BioBookEXCRET.html
Overview of nephron function

Filtration

Reabsorption and secretion

Reabsorption
• Active Transport –requires ATP• Na+, K+ ATP pumps
• Passive Transport-• Na+ symporters (glucose, a.a., etc)• Na+ antiporters (H+)• Ion channels• Osmosis

What is Reabsorbed- Where?Proximal tubule - reabsorbs 65 % of filtered Na+ as well as Cl-, Ca2+, PO4, HCO3
-. 75-90% of H20. Glucose, carbohydrates, amino acids, and small proteins are also reabsorbed here.
Loop of Henle - reabsorbs 25% of filtered Na+.
Distal tubule - reabsorbs 8% of filtered Na+. Reabsorbs HCO3-.
Collecting duct - reabsorbs the remaining 2% of Na+ only if the hormone aldosterone is present. H20 depending on hormone ADH.

Secretion
• Proximal tubule – uric acid, bile salts, metabolites, some drugs, some creatinine
• Distal tubule – Most active secretion takes place here including organic acids, K+, H+, drugs, Tamm-Horsfall protein (main component of hyaline casts).

Hormones Produced by the Kidney
• Renin:• Released from juxtaglomerular apparatus when low blood flow or low Na+. Renin leads to
production of angiotensin II, which in turn ultimately leads to retention of salt and water.
• Erythropoietin: • Stimulates red blood cell development in bone marrow. Will increase when blood oxygen
low and anemia (low hemoglobin).
• Vitamin D3: • Enzyme converts Vit D to active form 1,25(OH)2VitD. Involved in calcium homeostasis.

Renin, Angiotensin, Aldosterone:
Regulation of Salt/Water Balance

Aldosterone
• Secreted by the adrenal glands in response to angiotensin II or high potassium
• Acts in distal nephron to increase resorption of Na+ and Cl- and the secretion of K+ and H+
• NaCl resorption causes passive retention of H2O

Anti-Diuretic Hormone (ADH)
• Osmoreceptors in the brain (hypothalamus) sense Na+ concentration of blood.
• High Na+ (blood is highly concentrated) stimulates posterior pituitary to secrete ADH.
• ADH upregulates water channels on the collecting ducts of the nephrons in the kidneys.
• This leads to increased water resorption and decrease in Na concentration by dilution

Anatomic Changes in Pregnancy
• Kidney’s increased size (can increase up to 2cm in length),• Increased vascular volume, • Increased interstitial space and increased glomerular size (not number). • The greatest changes are seen in the collecting system, where calyces, renal
pelvises and ureters dilate and elongate. • These changes are evident by the 3rd gestational month and persist until the
12th week post partum

• Pregnancy induces increased synthesis of prostaglandin E2 (PGE2) which inhibits ureteral peristalsis and may be responsible for the hypomotility and distension.
• Increased oestrogen and progesterone production causes muscular and hypertrophic changes in the urinary tract resulting in hypomotility of the urinary tract.
• Increased production of chorionic growth hormone may cause some renal hypertrophy.
• Mechanical obstruction by the enlarged uterus can contribute to ureteral distension as well as changes to surrounding structures.

Functional Changes
• Early in pregnancy increased RBF, secondary to increased CO and renal vasodilatation
• This has been shown to be up to 40% above nongravid values. • Usually a decrease in systolic pressure is seen, due to the decrease in
vascular resistance from vasodilation.• This increased RBF increased glomerular filtration rate (GFR). This
begins during the first few weeks after conception, is at its greatest at the beginning of the 2nd trimester and remains until after delivery.
• Creatinine, urea and uric acid clearances increase, therefore serum levels decrease during pregnancy.

• Acid base regulation altered decrease in the bicarbonate threshold. Early morning urine specimen is more alkaline.
• Pregnant women tend to hyperventilate and subsequently mild alkalosis is often present.
• Glucose, water-soluble vitamins, protein and amino acids are excreted during normal pregnancy (increase in GFR filtered load of nutrients to surpass the reabsorptive capacity of the kidney, therefore these substances spill into the urine)
• Intermittent glycosuria is normal and makes screening for diabetes more difficult. • Volume regulation ch. gradual accumulation and retention of water and sodium.• Most healthy women gain an average of 12.5 kilograms and most of this is fluid. • The plasma volume doubles and this results in a fall in the plasma sodium
concentration (dilution).

• Osmolarity levels decrease stimulate a diuresis by suppressing ADH. However, in pregnancy this does not appear to happen.
• It appears as though the osmoreceptors are ‘reset’ at a lower level to avoid a continuous diuresis.
• Mean BP decreases by around 10 mmHg in early pregnancy decrease in peripheral vascular resistance; effects of progesterone (smooth muscle relaxant).
• Renin concentration is 5 - 10 times greater in pregnancy, however the pregnant women is extremely resistant to the vasoconstriction effects of angiotensin II. Related to elevated levels of aminopeptidase which destroys angiotensin II.
• Erythropoietic activity increases during pregnancy. This is possibly due to an increase in erythropoietin levels from an increase in renal tissue

Normal Renal Alterations in Pregnancy

Normal Changes in Pregnancy
Systemic Vasodilation Lower BP Increased Aldosterone Volume expansion / edema Increased GFR / RBF Angiogenesis

Progesterone
Stimulates Nitric Oxide Synthase Decreased response to Angiotensin

Progesterone
Stimulates Nitric Oxide Synthase Leads to systemic Vasodilation Which causes lower BP, Which stimulates Aldosterone Which leads to volume expansion Which increases GFR/RBF
Decreased response to Angiotensin

Pregnancy in women with existing renal disease


Why don’t uremic women get pregnant?• Most beyond child bearing age• Libido/ frequency of intercourse reduced• Don’t ovulate• Absence of increase in basal body temperature during the luteal
phase of cycle• Elevated circulating prolactin concentrations• Elevated PRL impairs hypothalamic-pit function

Course of Renal Disease in Pregnancy
• Baseline azotemia = more rapid deterioration • As renal dz progresses, ability to maintain nl pregnancy deteriorates,
and presence of HTN incr likelihood of renal deterioration• Renal dysfunction - greater risk for complications incl preeclapsia,
premature delivery, IUGR

Chronic Renal Failure
• CRF is defined as a permanent reduction in glomerular filtration rate (GFR) sufficient to produce detectable alterations in well-being and organ function. This usually occurs at GFR below 25 ml/min.
Clinical practice Guidelines:Clinical practice Guidelines:•Pregnancy may be considered in women with chronic kidney disease (CKD) having mild renal impairment (serum creatinine <124 μmol/L) and well controlled blood pressure. (Grade C)•Women with moderate to severe renal impairment should be counselled to avoid pregnancy due to greater adverse maternal and fetal outcomes. (Grade C)•All pregnant women with CKD should be co-managed by a multidisciplinary team. (Grade C)

Stages of chronic kidney disease:
Cockroft Gault Formula: [(140-age) x weight] / [PCr x 72] x 0.75 (women)

Risk factor:• Family history of kidney disease
• Age - chronic kidney disease is much more common among people over 60 years of age
• Atherosclerosis
• Bladder obstruction
• Chronic glomerulonephritis
• Congenital kidney disease (kidney disease which is present at birth)
• Diabetes Hypertension
• Lupus erythematosus
• Overexposure to some toxins
• Sickle cell disease
• Some medications

Uremic Syndrome
• Uremia occurs in stage 3 & 4 of CRF:• Changes in mental status• Fever, Malaise• Anorexia, Nausea, vomiting, LOW• Mild neural dysfunction• Uremic pruritus (itching)

Associated problems with CRF
• Immunosuppression• Increased risk of infection• People with CFR should be vaccinated regularly
• Anemia• Due to reduced erythropoietin production by kidney. Usually doesn’t occur until 6-12
mos prior to dialysis
• Hyperuricemia (Gout)• Increased uric acid in system• Pain in joints, may contribute to renal dysfunction
• Hyperphosphatemia• Increased parathyroid hormone levels• Increased phosphate load from bone metabolism
• Hypertension
• Poor coagulation
• Proteinuria

How CKD should be managed in pregnancy?• All women with chronic kidney disease should be referred early in
pregnancy to an obstetrician and other specialist as necessary, to plan subsequent antenatal care.
• However, with a few exceptions, the most important aspects of managing chronic kidney disease in pregnancy relate to managing associated clinical features, rather than the type of kidney disease.
• Regular monitoring of maternal renal function (serum creatinine and serum urea), blood pressure, midstream urine (for infection), proteinuria, and when appropriate ultrasound (to detect urological obstruction) should identify pathological changes and allow timely intervention to optimise perinatal outcome and maternal renal outcome.

Before pregnancy:
• Ideally, all women with chronic kidney disease should be made aware of the risks to their long term renal function and to the fetus before they conceive.
• Women with chronic kidney disease often have amenorrhoea but may still occasionally ovulate and thus conceive.
• Contraceptive measures that consider clinical comorbidities should be taken by those who do not wish to become pregnant.
• Folic acid 400 μg daily should be given as usual before conception until 12 weeks’ gestation.
• Low dose aspirin (50-150 mg/day) should be started in early pregnancy to reduce the risk of pre-eclampsia and improve perinatal outcome.
• Fetotoxic drugs—such as ACE inhibitors and angiotensin II receptor blockers—should be stopped before pregnancy if equally effective drugs are available, or as soon as pregnancy is confirmed, if they are thought to be important for protecting maternal renal function.

During pregnancy:

Management:
• Dialysis• Kidney transplantation

Common Themes in Dialysing Pregnant Patients1. Keeping BUN < 502. Increasing dialysis time and frequency3. BP control4. Managing anemia with increasing doses of ESA5. Fetal monitoring once viability reached