Renal Nursing
-
Upload
freenursingnotes -
Category
Documents
-
view
1.947 -
download
2
description
Transcript of Renal Nursing

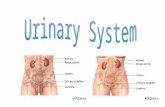
THE GENITOURINARY SYSTEM
Urological Assessment Key Signs and Symptoms of Urological Problems EDEMA - associated with fluid retention
- renal dysfunctions usually produce ANASARCAPAIN
Suprapubic pain= bladderColicky pain on the flank= kidney
HEMATURIAPainless hematuria may indicate URINARY CANCER!Early-stream hematuria - urethral lesionLate-stream hematuria - bladder lesion
DYSURIA - Pain with urination - lower UTI
POLYURIA - More than 2 Liters urine per day
OLIGURIA - Less than 400 mL per day
ANURIA - Less than 50 mL per day
Urinary Urgency
Urinary retention
Laboratory examination1. Urinalysis2. BUN and Creatinine levels of the serum3. Serum electrolytes
Diagnostic examination1. Radiographic2. IVP 3. KUB x-ray4. KUB ultrasound5. CT and MRI6. Cystography
Implementation Steps for selected problems
Provide PAIN relief● Assess the level of pain● Administer medications usually narcotic ANALGESICS
Maintain Fluid and Electrolyte Balance● Encourage to consume at least 2 liters of fluid per day
______________________________________________________________

● In cases of ARF, limit fluid as directed● Weigh client daily to detect fluid retention
Ensure Adequate urinary elimination● Encourage to void at least every 2-3 hours● Promote measures to relieve urinary retention:
1. Alternating warm and cold compress2. Bedpan3. Open faucet 4. Provide privacy5. Catheterization if indicated
Urinary Tract Infection (UTI)
Bacterial invasion of the kidneys or bladder (CYSTITIS) usually caused by Escherichia coli
Predisposing factors include1. Poor hygiene2. Irritation from bubble baths3. Urinary reflux4. Instrumentation5. Residual urine, urinary stasis6. Urinary Tract Infection (UTI)
PATHOPHYSIOLOGYThe invading organism ascends the urinary tract, irritating the mucosa and causing
characteristic symptomsUreter - ureteritisBladder - cystitisUrethra - urethritisPelvis - pyelonephritis
Assessment findings1. Low-grade fever2. Abdominal pain3. Enuresis4. Pain/burning on urination5. Urinary frequency6. Hematuria
Assessment findings: Upper UTI1. Fever and CHIILS2. Flank pain
______________________________________________________________

3. Costovertebral angle tenderness
Laboratory Examination1. Urinalysis2. Urine Culture
Nursing interventions1. Administer antibiotics as ordered.2. Provide warm baths and allow client to void in water to alleviate painful voiding.3. Force fluids. Nurses may give 3 liters of fluid per day.4. Encourage measures to acidify urine (cranberry juice, acid-ash diet).
Provide client teaching and discharge planning concerning1. Avoidance of tub baths 2. Avoidance of bubble baths that might irritate urethra3. Importance for girls to wipe perineum from front to back4. Increase in foods/fluids that acidify urine.
Pharmacology1. Sulfa drugs
Highly concentrated in the urineEffective against E. coli!
2. QuinolonesNephrolithiasis/Urolithiasis
Presence of stones anywhere in the urinary tract calciumoxalateuric acid
Nephrolithiasis/UrolithiasisPredisposing factors
1. Diet: large amounts of calcium and oxalate2. Increased uric acid levels3. Sedentary life-style, immobility4. Family history of gout or calculi5. Hyperparathyroidism
PathophysiologySupersaturation of crystals due to stasis
Stone formation
______________________________________________________________

May pass through the urinary tract
OBSTRUCTION, INFECTION and HYDRONEPHROSIS
Assessment findings1. Abdominal or flank pain2. Renal colic radiating to the groin3. Hematuria4. Cool, moist skin5. Nausea and vomiting
Diagnostic tests 1. KUB Ultrasound and X-ray: pinpoints location, number, and size of stones 2. IVP: identifies site of obstruction and presence of non-radiopaque stones 3. Urinalysis: indicates presence of bacteria, increased protein, increased WBC and RBC (hematuria)
Medical management1. Surgery
a. Percutaneous nephrostomy: tube is inserted through skin and underlying tissues into renal pelvis to remove calculi.b. Percutaneous nephrostolithotomy: delivers ultrasound waves through a probe placed on the calculus.
2. Extracorporeal shock-wave lithotripsy: delivers shock waves from outside the body to the stone, causing pulverizationa. Pain management : Morphine or Meperidineb. Diet modification
Nursing interventions1. Strain all urine through gauze to detect stones and crush all clots.2. Force fluids (3000—4000 cc/day).3. Encourage ambulation to prevent stasis.4. Relieve pain by administration of analgesics as ordered and application of moist
heat to flank area.5. Monitor intake and output6. Provide modified diet, depending upon stone consistency: Calcium, Oxalate and
Uric acid stones
Calcium stones- limit milk/dairy products; provide acid-ash diet to acidify urine (cranberry or prune juice, meat, eggs, poultry, fish, grapes, and whole grains)
Oxalate stones______________________________________________________________

- avoid excess intake of foods/ fluids high in oxalate (tea, chocolate, rhubarb, spinach); maintain alkaline-ash diet to alkalinize urine (milk; vegetables; fruits except prunes, cranberries, and plums)
Uric acid stones- educe foods high in purine (liver, beans, kidneys, venison, shellfish, meat soups, gravies, legumes); maintain alkaline urine
7. Administer allopurinol (Zyloprim) as ordered, to decrease uric acid production.8. Provide client teaching and discharge planning concerning:
● Prevention of Urinary stasis by maintaining increased fluid intake especially in hot weather and during illness; mobility; voiding whenever the urge is felt and at least twice during the night
● Adherence to prescribed diet● Need for routine urinalysis (at least every 3—4 months)● Need to recognize and report signs/ symptoms of recurrence
(hematuria, flank pain).
Acute Renal FailureSudden interruption of kidney function to regulate fluid and electrolyte balance and remove toxic products from the body
PATHOPHYSIOLOGY● Pre-renal failure● Intra-renal failure● Post-renal failure
Prerenal CAUSE: Factors interfering with perfusion and resulting in diminished blood flow and
glomerular filtrate, ischemia, and oliguria; include CHF, cardiogenic shock, acute vasoconstriction, hemorrhage, burns, septicemia, hypotension, anaphylaxis
Intrarenal CAUSE:Conditions that cause damage to the nephrons; include acute tubular necrosis
(ATN), endocarditis, diabetes mellitus, malignant hypertension, acute glomerulonephritis, tumors, blood transfusion reactions, hypercalcemia, nephrotoxins (certain antibiotics, x-ray dyes, pesticides, anesthetics)
Postrenal CAUSE: Mechanical obstruction anywhere from the tubules to the urethra; includes
calculi, BPH, tumors, strictures, blood clots, trauma, and anatomic malformation
Three phases of acute renal failure______________________________________________________________

1. Oliguric phase2. Diuretic phase3. Convalescence or recovery phase
Four phases of acute renal failure (Brunner and Suddarth)1. Initiation phase2. Oliguric phase3. Diuretic phase4. Convalescence or recovery phase
Assessment findings: The Three Phases of Acute Renal Failure1. Oliguric phase
Urine output less than 400 cc/24 hoursduration 1—2 weeksManifested by dilutional hyponatremia, hyperkalemia, hyperphosphatemia, hypocalcemia, hypermagnesemia, and metabolic acidosisDiagnostic tests: BUN and creatinine elevated
2. Diuretic phaseDiuresis may occur (output 3—5 liters/day) due to partially regenerated tubule’s inability to concentrate urineDuration: 2—3 weeks; manifested by hyponatremia, hypokalemia, and hypovolemiaDiagnostic tests: BUN and creatinine slightly elevated
3. Recovery or convalescent phaseRenal function stabilizes with gradual improvement over next 3—12 months
Laboratory findings:● Urinalysis: Urine osmo and sodium● BUN and creatinine levels increased● Hyperkalemia● Anemia● ABG: metabolic acidosis
Nursing interventions● Monitor fluid and Electrolyte Balance● Reduce metabolic rate● Promote pulmonary function● Prevent infection● Provide skin care● Provide emotional support
Nursing interventions1. Monitor and maintain fluid and electrolyte balance.
a. Measure l & O every hour. note excessive losses in diuretic phaseb. Administer IV fluids and electrolyte supplements as ordered.c. Weigh daily and report gains.d. Monitor lab values; assess/treat fluid and electrolyte and acid-base imbalances as needed
2. Monitor alteration in fluid volume.a. Monitor vital signs, PAP, PCWP, CVP as needed.
______________________________________________________________

b. Weigh client daily.c. Maintain strict I & O records.
3. Assess every hour for hypervolemiaa. Maintain adequate ventilation.b. Restrict FLUID intakec. Administer diuretics and antihypertensives
4. Promote optimal nutritional status.a. Weigh daily.b. Administer TPN as ordered.c. With enteral feedings, check for residual and notify physician if residual volume increases.d. Restrict protein intake to 1 g/kg/daye. Restrict POTASSIUM intaked. HIGH CARBOHYDRATE DIET, calcium supplements
5. Prevent complications from impaired mobility (pulmonary embolism, skin breakdown, and atelectasis)
6. Prevent fever/infection.a. Assess for signs of infection.b. Use strict aseptic technique for wound and catheter care.
7. Support client/significant others and reduce/ relieve anxiety.a. Explain pathophysiology and relationship to symptoms.b. Explain all procedures and answer all questions in easy-to-understand termsc. Refer to counseling services as needed
8. Provide care for the client receiving dialysis.9. Provide client teaching and discharge planning concerning
a. Adherence to prescribed dietary regimenb. Signs and symptoms of recurrent renal diseasec. Importance of planned rest periodsd. Use of prescribed drugs onlye. Signs and symptoms of UTI or respiratory infection need to report to physician immediately
Chronic Renal FailureGradual, Progressive irreversible destruction of the kidneys causing severe renal dysfunction. The result is azotemia to UREMIAPredisposing factors:
a. DM= worldwide leading causeb. Recurrent infectionsc Exacerbations of nephritisd. urinary tract obstructione. hypertension
PathophysiologySTAGE 1= reduced renal reserve, 40-75% loss of nephron functionSTAGE 2= renal insufficiency, 75-90% loss of nephron function
______________________________________________________________

STAGE 3= end-stage renal disease, more than 90% loss. DIALYSIS IS THE TREATMENT!
Assessment findings1. Nausea, vomiting; diarrhea or constipation; decreased urinary output2. Dyspnea3. Stomatitis4. Hypertension (later), lethargy, convulsions, memory impairment, pericardial friction rub
Diagnostic tests: a. 24 hour creatinine clearance urinalysisb. Protein, sodium, BUN, Crea and WBC elevatedc. Specific gravity, platelets, and calcium decreasedD. CBC= anemia
Medical management1. Diet restrictions2. Multivitamins3. Hematinics and erythropoietin4. Aluminum hydroxide gels5. Anti-hypertensive6. Anti-seizures7. DIALYSIS
Nursing interventions1. Prevent neurological complications.
a. Assess every hour for signs of uremia (fatigue, loss of appetite, decreased urine output, apathy, confusion, elevated blood pressure, edema of face and feet, itchy skin, restlessness, seizures).b. Assess for changes in mental functioning.c. Orient confused client to time, place, date, and persons; institute safety measures to protect client from falling out of bed.d. Monitor serum electrolytes, BUN, and creatinine as ordered
2. Promote optimal GI function.a. Assess/provide care for stomatitisb. Monitor nausea, vomiting, anorexiac. Administer antiemetics as ordered.
3. Monitor/prevent alteration in fluid and electrolyte balance4. Assess for hyperphosphatemia (paresthesias, muscle cramps, seizures, abnormal
reflexes), and administer aluminum hydroxide gels (Amphojel) as ordered5. Promote maintenance of skin integrity.
a. Assess/provide care for pruritus.b. Assess for uremic frost (urea crystallization on the skin) and bathe in plain water
6. Monitor for bleeding complications, prevent injury to client.______________________________________________________________

a. Monitor Hgb, hct, platelets, RBC.b. Hematest all secretions.c. Administer hematinics as ordered.d. Avoid lM injections
7. Promote/maintain maximal cardiovascular function.a. Monitor blood pressure and report significant changes.b. Auscultate for pericardial friction rub.c. Perform circulation checks routinely.
7. Promote/maintain maximal cardiovascular function.a. Administer diuretics as ordered and monitor output.b. Modify drug doses
8. Provide care for client receiving dialysis.
DIALYSISa procedure that is used to remove fluid and uremic wastes from the body when
the kidneys cannot function
Two methods1. Hemodialysis2. Peritoneal dialysis
Nursing management1. Meet the patient's psychosocial needs2. Remember to avoid any procedure on the arm with the fistula (HEMO)3. Monitor WEIGHT, blood pressure and fistula site for bleeding4. Monitor symptoms of uremia5. Detect complications like infection, bleeding (Hepatitis B/C and HIV infection in
Hemodialysis)6. Warm the solution to increase diffusion of waste products (PERITONEAL)7. Manage discomfort and pain8. To determine effectiveness, check serum creatinine, BUN and electrolytes
Male reproductive disordersDIGITAL RECTAL EXAMINATION- DRE
Recommended for men annually with age over 40 years Screening test for cancer Ask patient to BEAR DOWN
TESTICULAR EXAMINATION Palpation of scrotum for nodules and masses or inflammation BEGINS DURING ADOLESCENCE
Prostate specific antigen (PSA) Elevated in prostate cancer Normal is 0.2 to 4 nanograms/mL Cancer - over 4
BENIGN PROSTATIC HYPERPLASIA______________________________________________________________

- Enlargement of the prostate that causes outflow obstruction- Common in men older than 50 years old
Assessment findings1. DRE: enlarged prostate gland that is rubbery, large and NON-tender2. Increased frequency, urgency and hesitancy 3. Nocturia, DECREASE IN THE VOLUME AND FORCE OF URINE STREAM
Medical management1. Immediate catheterization2. Prostatectomy3. TRANSURETHRAL RESECTION of the PROSTATE (TURP)4. Pharmacology: alpha-blockers, alpha-reductase inhibitors. SAW palmetto
Nursing Intervention 1. Encourage fluids up to 2 liters per day2. Insert catheter for urinary drainage3. Administer medications – alpha adrenergic blockers and finasteride4. Avoid anticholinergics5. Prepare for surgery or TURP6. Teach the patient perineal muscle exercises. Avoid valsalva until healing
Nursing Intervention: TURP1. Maintain the three way bladder irrigation to prevent hemorrhage2. Only initially the drainage is pink-tinged and never reddish3. Administer anti-spasmodic to prevent bladder spasms
PROSTATE CANCER- a slow growing malignancy of the prostate gland- Usually an adenocarcinoma- This usualy spread via blood stream to the vertebraePredisposing factor
➢ AgeAssessment Findings
1. DRE: hard, pea-sized nodules on the anterior rectum2. Hematuria3. Urinary obstruction4. Pain on the perineum radiating to the leg
Diagnostic tests1. Prostatic specific antigen (PSA)2. Elevated SERUM ACID PHOSPHATASE indicates SPREAD or Metastasis
Medical and surgical management1. Prostatectomy2. TURP3. Chemotherapy: hormonal therapy to slow the rate of tumor growth4. Radiation therapy
______________________________________________________________

Nursing Interventions1. Prepare patient for chemotherapy2. Prepare for surgery
Nursing Interventions: Post-prostatectomy1. Maintain continuous bladder irrigation. Note that drainage is pink tinged w/in
24 hours2. Monitor urine for the presence of blood clots and hemorrhage3. Ambulate the patient as soon as urine begins to clear in color
______________________________________________________________