Pulmonary hypertension in infants with congenital heart...
Transcript of Pulmonary hypertension in infants with congenital heart...
Research Paper
Mediators of In� ammation, 6, 323±326 (1997)
© 1997 Rapid Science Publishers
Pulmonary hypertension in infantswith congenital heart defects: areleukotrienes involved?
A. Serraf1, J-P. Gascard2, J. Bruniaux1, C. Labat2,C. Planche1 and C. Brink2,CA
1Service de Chirurgie et Re animation CardiaquesPe diatriques, and 2CNRS ERS 566, Centre ChirurgicalMarie-Lannelongue, 133, avenue de la Re sistance,92350 Le Plessis-Robinson, France
CACorresponding AuthorTel: (+33) 1 40 94 28 00 ext. 3015Fax: (+33) 1 46 30 12 08Email: [email protected]
The circulating levels of leukotriene E4 in infantswith congenital heart defects, increased pulmon-ary blood � ow and pulmonary arterial hyper-tension, were determined and compared withinfants with decreased pulmonary blood � ow(Tetralogy of Fallot). There was no correlation(r = 0·38) between the pulmonary arterial pres-sure (56 4 mmHg) and the leukotriene E4 levels(1·37 0·67 ng/ml blood) measured in peripheralblood samples from the hypertensive group priorto surgery. There was considerable variation inthe detectable leukotriene E4 levels in bloodsamples from different patients. The levels de-tected in the blood samples between the twogroups of patients was similar. These data suggestthat neither the surgical repair during cardiopul-monary bypass nor the pulmonary hypertensionappeared to modify the leukotriene E4 bloodlevels in the small number of patients studied.
Key words: Pulmonary hypertension, Cardiovascularsurgery, Congenital heart defects, Leukotrienes,Extracorporeal circulation
Introduction
The hypothesis that metabolites of the arachi-donic acid cascade, speci�cally products of the5-lipoxygenase pathway, may be involved inpulmonary hypertension was based on twolines of evidence. First, injection of cysteinyl-leukotrienes signi�cantly increased pulmonaryvascular resistance in neonatal lambs1 as well asin mature guinea-pigs and rats.2 Furthermore, inthe monkey, transient pulmonary hypertensionwas also observed following leukotriene admin-istration.3 The second line of evidence wasprovided by Stenmark and coworkers4 whodetected the presence of cysteinyl-leukotrienesin newborns with persistent pulmonary hyper-tension. These latter observations were basedon analysis of bronchoalveolar lavage �uidderived from infants with pulmonary hyper-tension. Such data suggested indirectly thatcysteinyl-leukotrienes which are potent vaso-constrictor agents in the human lung5 may beassociated with elevated pulmonary arterialpressure in children.
Previous surgical reports have shown thatthere are acute transitory episodes of increasedpulmonary arterial pressure in patients follow-ing open heart surgery for correction of con-genital heart lesions.6 Unfortunately, thecirculating levels of leukotrienes in this subsetof patients is not known. In this study, the
levels of LTE4 in blood samples derived frominfants with congenital heart defects, increasedpulmonary blood �ow and pulmonary hyper-tension were determined during the surgicalintervention for correction of the heart defectand compared with infants with decreasedpulmonary blood �ow. Since LTE4 is known tobe produced by the human lung in vitro7,8 andis a stable product of the 5-lipoxygenase path-way, the aim of the present study was toestablish whether or not circulating LTE4 wascorrelated with pulmonary arterial pressure andto determine whether the human lung in situreleased this 5-lipoxygenase pathway metabo-lite.
Methods
Subjects
Eighteen patients with congenital heart defects(2±25 months of age) were studied. Six werediagnosed to have regular form of Tetralogy ofFallot, seven patients had complete atrioventri-cular septal defect, three had truncus arteriosusand two had ventricular septal defect. All pa-tients with pulmonary hypertension (n = 12)presented with heart failure despite medicaltherapy support. None of them received medi-cation that could interfere with the arachidonicacid cascade. Haemodynamic measurements
Mediators of In¯ ammation ´ Vol 6 ´ 1997 323
(pulmonary, systemic and atrial pressures) werecontinuously recorded for each patient usingthe Hewlett Packard 78354A monitor. Openheart repair was performed with the aid ofhypothermic cardiopulmonary bypass. Aorticcross-clamping with injection of blood cardio-plegia was used during the intracardiac repair.The mean duration of the cardiopulmonarybypass in Fallot patients was 69 4 min and114 9 min in pulmonary hypertension sub-jects. None of the patients had cardiac repairunder deep hypothermic circulatory arrest.After sternal and pericardial opening, bloodsamples were drawn from the main pulmonaryartery and the left atrium. Surgery was thenconducted as usual. Prior to weaning fromcardiopulmonary bypass, monitoring lines (Sel-dicath 3 Fr. Plastimed) were introduced in theleft atrial cavity and in the main pulmonaryartery. Whilst in the intensive care unit, bloodsamples were collected from the patients viathese catheter lines.
Leukotriene E4 measurements
All blood samples (0.5 ml) were collecteddirectly in tubes containing methanol at thebeginning (Start) of extracorporeal circulation(ECC), 5 min after lung reperfusion (RP) and atthe end of ECC. The tubes were stored over-night at - 208 C. The samples were then thawed,vortexed and centrifuged (5000 rpm for 20 minat 48 C). The supernatant was then removed andadded to tubes containing 40 ml of methanol at10%and this mixture was then passed througha column (Sep-Pak C-18). The extracts contain-ing lipids were collected on 3 ml of methanol.These samples were then separated into equalvolume aliquots and dried using a Speed-Vacevaporator. The residue was dissolved in mobilephase solution of HPLC (acetonitrile/water/acetic acid at pH 5.6). This solution (20 ml) wasinjected into an HPLC (Waters) for separation.The samples were collected and quanti�cationwas performed by EIA (Stallergens, Fresnes,France).
Due to the complexity of the surgical inter-vention, internal standards for LTE4 were notperformed. However, using a blood sampleobtained prior to surgery in one infant theanalytic recoveries for standard LTE4 were 78%for 0·5 ng/ml and 82%for 1 ng/ml, demonstrat-ing that collection of blood samples in tubescontaining methanol permitted adequate recov-eries of LTE4. The range of LTE4 levels detectedin the peripheral blood samples was 0 to0·76 ng/ml (Fallot patients) and 0 to 7·2 ng/ml(pulmonary hypertension patients).
Statistical analysis
Results are expressed as means SEM. Sincethe number of patients studied was limited andthe LTE4 range was large, no statistical analysiswas performed on the data. However, the datafor each patient are presented.
Results
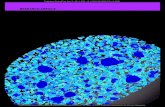
The pulmonary arterial pressure and the quan-tities of LTE4 detected in peripheral bloodsamples derived from patients without (Fallot)and with pulmonary hypertension (PH) prior tosurgery are shown in Table 1. There was nocorrelation between the elevated preoperativepulmonary arterial pressure and the levels ofcirculating LTE4 detected in the peripheralblood samples (r = 0·38). The LTE4 levelsdetected in the infants during the course of thesurgical intervention are presented in Tables 2and 3 as well as in Fig. 1. The LTE4 levelsmeasured in blood samples derived from thepulmonary artery for the different patients(Fallot vs. PH) were similar. Values obtained inthe samples from the left atrium in these twogroups of patients were also similar. In �vepatients (PH) who were studied over the courseof 12 h the LTE4 levels were not altered whencompared with those data obtained at thebeginning of ECC.
In � ve of the 18 patients examined (one Fallotand four PH), the LTE4 levels were below thethreshold level of detection. Of the 13 patientswhere LTE4 levels were detectable, eight sub-jects exhibited higher LTE4 levels in bloodsamples derived from the left atrium than thoselevels detected in blood samples from thepulmonary artery during the lung reperfusionperiod. In two subjects, the LTE4 levels in theleft atrium were lower than those measured inthe pulmonary artery blood samples. In twopatients no samples were obtained and inanother patient the values were the same. Inaddition, the total quantities of LTE4 detectedduring the surgical intervention were: Fallot,
Table 1. Pulmonary arterial pressure and circulating leuko-triene E4 levels in infant patients
Patients Age(months)
(n) PAP(mmHg)
LTE4(ng/ ml)
Fallot 11.9 3.2 6 NM 0.44 0.12PH 8.5 1.6 12 56 4 1.37 0.67
Values are means SEM from the number of patients studied (n).Age at time of surgery. PH = pulmonary hypertension; PAP =pulmonary arterial pressure (prior to surgery) and NM = notmeasured. The LTE4 levels were determined in peripheral bloodsamples prior to surgery.
324 Mediators of In¯ ammation ´ Vol 6 ´ 1997
A. Serr af et al.
0·64 0·17 ng/ml blood; and PH, 1·030·43 ng/ml blood.
Discussion
While LTE4 was detected in blood samples frominfants (72%) an increase in the circulatinglevels was not observed in those patients withpulmonary hypertension. These data, derivedfrom a limited number of patients, suggestedthat neither the surgical intervention nor thepulmonary hypertension were associated withan alteration in LTE4 blood levels.
There was considerable variation in the LTE4levels detected in blood samples obtained fromneonates with or without pulmonary hyper-tension. The range in the quantities of LTE4detected was similar to those reported by otherinvestigators when this metabolite was meas-ured in either urine,9 - 11 bronchoalveolarlavage12 or blood samples13 from patients with
Table 2. LTE4 levels (pg/ml) detected in blood samples obtained from infants (Fallot)
Patients Age (months) Peripheralblood
ECC
Start Lung reperfusion End
PA LA PA LA PA LA
1 8 590 660 750 432 470 327 4402 3.2 366 421 471 2010 1850 582 18803 15.8 700 1040 565 525 780 635 6654 25.7 755 835 765 500 1105 1170 13205 10.4 0 0 0 0 0 0 06 8.5 246 224 632 NP 445 491 523
PA = pulmonary artery; LA = left atrium; 0 = below level of assay detection; NP = no sample; ECC = extracorporeal circulation; months = ageat surgery.
Table 3. LTE4 levels (pg/ml) detected in blood samples obtained from infants (PH)
Patients Age(months)
PAP(mmHg)
Peripheralblood
ECC
Start Lung reperfusion End
PA LA PA LA PA PA
1 13 83 406 188 746 149 340 138 2532 9 60 630 312 1180 550 542 551 5223 7.2 52 0 0 0 0 0 0 04 12 48 0 0 0 0 0 0 05 3.7 NM 155 209 603 NP NP 161 6816 15 70 570 1086 799 413 566 NP NP7 3.8 67 5090 6679 1610 7158 2317 2517 13898 4.8 NM 1217 244 1743 570 1832 206 14049 2.7 70 7172 5427 NP 532 6850 4350 5920
10 20.5 47 0 0 0 0 0 0 011 2.4 40 1170 1200 1310 801 1370 270 150012 7.8 50 0 0 0 0 0 0 0
PA = pulmonary artery; LA = left atrium; 0 = below level of assay detection; NP = no sample; ECC = extracorporeal circulation; NM = notmeasured; PAP = pulmonary arterial pressure (prior to surgery); months = age at surgery.
2
1
0
6 6
5 6
6
6
12
11
11
11
11
11
55
5 Pulmonary artery5 Left atrium
FALLOT
LTE
4 ng
/ml o
f blo
od
START LR END START LR END 12 hpost-ECC
ECC ECC
PH
FIG. 1. Circulating leukotriene E4 levels in infants duringopen heart surgery. Measurements of LTE4 were performedin blood samples obtained during surgery in a group ofinfants without (Fallot) and with pulmonary hypertension(PH). Blood samples were derived from either the pulmon-ary artery or the left atrium at the beginning (START) ofextracorporeal circulation (ECC), 5 min after lung reperfu-sion (LR) and at the END of ECC. In a limited number ofsubjects (n = 5) measurements were made at 12 h post-ECC. Values are means SEM and the number of infantsstudied is presented above each bar.
Mediators of In¯ ammation ´ Vol 6 ´ 1997 325
LT and pulmon ary hypertens ion in inf ants
different clinical pathologies. The reasons forthese variations are presently unknown but areprobably independent of the pathophysiologicalcondition, since control subjects (Fallot) exhibita similar range in LTE4 values, when comparedwith values obtained in infants with pulmonaryhypertension. Furthermore, the LTE4 levels de-tected were not correlated with the high pul-monary arterial pressure observed in PHinfants.These data are similar to a previous report inadult pulmonary hypertensive patients whereother metabolites of the arachidonic acid cas-cade were measured.14 These authors found nocorrelation between the pulmonary arterial pres-sure and thromboxane (TxB2) levels in urinesamples. These data suggest that the circulatingpotent vasoconstrictor metabolites of the arachi-donic acid pathway (TxA2 and LTE4) which aredetected in pulmonary hypertension may not berelated to the in vivo pressure modulationsreported in the pulmonary artery.
The low levels of LTE4 (28% of patients,undetected) and the interpatient variation willnow require further investigation. First, theremay be a preferential metabolism of arachidonicacid in different individuals. A signi�cant mod-i� cation in the production/removal equilibriumof the 5-lipoxygenase metabolites could resultin alterations in detection of the more stablemetabolite (LTE4). Therefore, the measurementof only LTE4 in the biological samples may notbe an appropriate index of the 5-lipoxygenasepathway activity in all patients. Unfortunately,no data are available concerning LTC4 and LTD4levels in biological samples obtained from sub-jects where no LTE4 was detected. The consid-erable variation in the levels of LTE4 betweenpatients may also be related to the way LTE4 isbound in the circulation. Unfortunately, little isknown about the �xation of cysteinyl-leuko-trienes in the human circulation. Few studieshave been published dealing with the quantita-tion of leukotrienes in human blood samplesand analysis has been essentially based onresults derived from human plasma.15 Finally, anincrease in quantities of leukotrienes may occurin the tissue compartment rather than in thecirculation. Indeed, previous data have shownthat following an instillation of LT in the ratlung only a small percentage could be detectedin the lavage �uid16 suggesting that the lungtissue rather than the lung liquid was thedominant compartment. Whether or not lung
tissue from pulmonary hypertensive patientsexhibits elevated levels of LTE4 has not beenreported. In order to adequately understand therole of these potent in�ammatory mediators inpulmonary hypertension these issues will haveto be addressed not only in relation to thisdisease but also other pathologies where leuko-trienes have been implicated.
References1. Schreiber MD, Heymann MA, Soifer SJ. The differential effects of
leukotriene C4 and D4 on the pulmonary and systemic circulations onnewborn lambs. Pedi atr Res 1987; 21: 176 ±182.
2. Berkowitz BA, Zabko-Potapovich B, Valocik R, Gleason JG. Effects ofthe leukotrienes on the vasculature and blood pressure of differentspecies. J Pharmocol Exp Ther 1983; 229: 105 ±112.
3. Smedegard G, Hedqvist P, Dahlen SE, Revenas B, Hammarstrom S,Samuelsson B. Leukotriene C4 affects pulmonary and cardiovasculardynamics in monkey. Nature 1982; 295: 327 ±329.
4. Stenmark KR, James SL, Voelkel NF, Norbert F, Toews WH, Reeves JT,Murphy RC. Leukotriene C4 and D4 in neonates with hypoxemia andpulmonary hypertension. N Eng l J Med 1983; 309: 77 ±80.
5. Labat C, Ortiz JL, Norel X, Gorenne I, Verley J, Abram TS, Cuthbert NJ,Tudhope SR, Norman P, Gardiner PJ, Brink C. A second cysteinylleukotriene receptor in human lung. J Ph arm acol Exp Ther 1992; 63:800 ±805.
6. Serraf A, Bruniaux J, Lacourt-Gayet F, Chambran P, Binet JP, Lecronier G,Demontoux S, Planche C. Obstructed total anomalous pulmonaryvenous return. J Tho r ac Cardiov asc Surg 1991; 101: 601 ±606.
7. Kumlin M, Dahlen S-E. Characte ristics of formation and furthermetabolism of leukotrienes in the chopped human lung. Bio chimic a etBiophys ic a Acta 1990; 1044: 201 ±210.
8. Gorenne I, Labat C, Gascard JP, Norel X, Muller-Peddinghaus R, MohrsKH, Taylor WA, Gardiner PJ, Brink C. ®-2-[4-(Quinolin-2-yl-methoxy)-phenyl-2-cyclopentyl Acetic acid] (BAY x1005) a potent leukotrienesynthesis inhibitor: effects on anti-IgE challenge in human airways.J Pharm aco l Exp Ther 1994; 268: 868 ±872.
9. Manning PJ, Rokach J, Malo JL, Ethier D, Cartier A, Girard Y, CharlesonS, O’Byrne PM. Urinary leukotriene E4 levels during early and lateasthmatic responses. J Allergy Clin Immunol 1990; 86: 211 ±220.
10. Bernard GR, Korley V, Chee P, Swindell B, Ford-Hutchinson AW, TagariP. Persistent generation of peptido leukotrienes in patients with theadult respiratory distress syndrome. Am Rev Re spir Dis 1991; 144:263 ±267.
11. Cook AJ, Yuksel B, Sampson AP, Greenough A, Price JF. Cysteinylleukotriene involvement in chronic lung disease in premature infants.Eur Re spir J 1996; 9: 1907 ±1912.
12. Lee TH, Crea AEG, Gant V, Spur BW, Marron BE, Nicolaou KC, ReardonE, Brezinski M, Serhan CN. Identi� cation of lipoxin A4 and its relation-ship to the sul� dopeptide leukotrienes C4, D4 and E4 in thebronchoalveolar lavage �uids obtained from patients with selectedpulmonary diseases. Am Rev Respir Dis 1990; 141: 1453 ±1458.
13. Sampson AP, Green CP, Spencer DA, Piper PJ, Price JF. Leukotrienes inthe blood and urine of children with acute asthma. Ann NY Acad Sci1991; 629: 437 ±439.
14. Christman BW, McPherson CD, Newman JH, King GA, Bernard GR,Groves BM, Loyd JE. An imbalance betw een the excretion ofthromboxane and prostacyclin metabolite s in pulmonary hypertension.N Engl J Med 1992; 327: 70 ±75.
15. Heavey DJ, Soberman RJ, Lewis RA, Spur B, Austen KF. Criticalconsiderations in the development of an assay for sul� dopeptideleukotrienes in plasma. Pros tag landins 1987; 33: 693 ±705.
16. Wescott JY, McDonnell TJ, Voekel NF. Alveolar transfer and metabolismof eicosanoids in the rat. Am Rev Res pir Dis 1989; 139: 80 ±87.
ACKNOWLEDGEMENT. The authors wish to thank Dr Serge Demontoux forexcellent support during the surgical intervention.
Received 4 August 1997;accepted in revised form 4 September 1997
326 Mediators of In¯ ammation ´ Vol 6 ´ 1997
A. Serr af et al.
Submit your manuscripts athttp://www.hindawi.com
Stem CellsInternational
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
MEDIATORSINFLAMMATION
of
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Behavioural Neurology
EndocrinologyInternational Journal of
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Disease Markers
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
BioMed Research International
OncologyJournal of
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Oxidative Medicine and Cellular Longevity
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
PPAR Research
The Scientific World JournalHindawi Publishing Corporation http://www.hindawi.com Volume 2014
Immunology ResearchHindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Journal of
ObesityJournal of
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Computational and Mathematical Methods in Medicine
OphthalmologyJournal of
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Diabetes ResearchJournal of
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Research and TreatmentAIDS
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Gastroenterology Research and Practice
Hindawi Publishing Corporationhttp://www.hindawi.com Volume 2014
Parkinson’s Disease
Evidence-Based Complementary and Alternative Medicine
Volume 2014Hindawi Publishing Corporationhttp://www.hindawi.com


















![Clinical Study Allopurinol, Benzbromarone, or a Combination ...InternationalJournalofRheumatology and in ammation [ , ]. Drugs such as colchicine, anti-in ammatories, and analgesics](https://static.fdocuments.net/doc/165x107/613d83b7e1ef621e9f2dc55a/clinical-study-allopurinol-benzbromarone-or-a-combination-internationaljournalofrheumatology.jpg)
![Research Article Correlation between Microleakage …downloads.hindawi.com/journals/ijd/2016/8084505.pdfplaque accumulation, secondary caries, and periodontal in ammation []. Factors](https://static.fdocuments.net/doc/165x107/5f71a0f4052a217f706115f8/research-article-correlation-between-microleakage-plaque-accumulation-secondary.jpg)

![Temporomandibular Disorders, Head · used to decrease TMJ in ammation[10 12]. Patients who are diagnosed with TMJ in ammation may have altered mandibular dynamics that are](https://static.fdocuments.net/doc/165x107/5bf6b42f09d3f20a768c5edc/temporomandibular-disorders-head-used-to-decrease-tmj-in-ammation10-12-patients.jpg)

