protocol to distribute... · Web viewUtilizing the muscles of mastication and guide planes one can...
Transcript of protocol to distribute... · Web viewUtilizing the muscles of mastication and guide planes one can...
A Protocol for the Treatment of Temporomandibular Disorder James E Metz, DDS, Diplomate ABDSM
Mickey C Harrison, DDS
The Metz Center for Sleep Apnea
1271 East Broad Street
Columbus, Ohio 43205
©2015, The Metz Center; Unauthorized reproduction or distribution will be prosecuted. Requests for reproduction should be directed to Dr. James Metz at [email protected].
1
Primary Site Stimulation (Stress Test)
The answer to differentiating temporomandibular dysfunction (TMD) from other head pain, even with the complexities of cranial nerve V, may be a simple technique utilized by medical practitioners. Primary Site Stimulation is a pressure technique that can be useful in the diagnosis of TM issues1 2. If the clinician puts pressure on a specific structure and it creates the chief complaint, then one has usually found the problem. The complexities and anatomic deviations of the system are not an issue here; the goal is to find and reproduce the pain.
A simple example is that of a patient with “arm pain.” If they cannot tell the origin of the pain, the practitioner must test. If the arm is examined by the use of primary site stimulation, then pressure is applied by the clinician to various structures located in the arm. If the patient’s chief complaint is “stimulated” while applying pressure to a specific structure, the diagnosis is complete, and whatever was stimulated to hurt is the source of the pain. Realize that this test cannot predictably be accomplished with palpation3 or jaw manipulation to diagnosis a TMD problem. The inaccessibility of some muscles to palpation and the complexity of the system create the need for a different type of testing.
The protocol is similar to the medical standard of care for distinguishing between local, projected, referred and central pain and tenderness1. The stress test should become the standard of care for dentistry, as it is in medicine. The test should always be a part of the complete TMD examination.Two methods can be employed:
1. Anterior Deprogrammer (Figures 6, 7, 8) 2. Anterior Appliance (Figure 9)
Fig. 6 Anterior Deprogrammer, Retruded position Fig. 7 Anterior Deprogrammer, Protruding mandible
Fig. 8 Ant. Deprogrammer, Checking posterior contact Fig. 9 Anterior Appliance, Note: Excellent esthetics
2
The reliability of the stress test by either method has a high degree of confidence. Each of the tests will give a yes or no to the diagnosis of TMD, but with a different urgency. Stress testing by either means will minimize inconvenience, pain, misery or cost to the patient. However, if the practitioner wants a true understanding of this TMD protocol with all of its ramifications, a complete knowledge of the anterior deprogrammer must be gained prior to the use of the anterior appliance as a stress test method. At least twenty-five patients should be diagnosed with the anterior deprogrammer stress test before the anterior appliance is substituted.
It must be realized that sometimes there is no substitute for the expediency of the anterior deprogrammer. This is especially true with a doubtful patient, or if a yes/no answer is urgently required. The anterior deprogrammer stress test shows, vividly, the character and distribution of the pain related to TMD4.
Once the anterior deprogrammer is understood, the anterior appliance is the most reliable diagnostic tool available. However, the cost to the patient is greater. The anterior deprogrammer gives a quicker diagnosis but does not separate TM joint patients from muscle patients as accurately as does the anterior appliance. Testing with the anterior deprogrammer is completed during one office visit. If the anterior appliance is used, a period of two weeks will be required for diagnosis.
The patient is asked to keep a record of their symptoms until they are pain free and the diary is reviewed at each check appointment. The joint will sometimes remain somewhat painful (anti-inflammatory medications can be utilized as needed) for a period of one week with the anterior appliance. Approximately 60% of the time this pain will disappear during the first week. However, TMJ pain should never be allowed to continue beyond the two week check. If the joint is still painful after the initial two weeks, a pivotal appliance is indicated, and will be discussed in subsequent sections.
The stress testing with the anterior deprogrammer causes, among other things, an eccentric (lengthening) contraction of the lateral pterygoid muscle5 6; an isometric contraction of the masseter, medial pterygoid, and temporalis muscles; and pressure on the temporomandibular joint. Centric relation occlusion and habitual occlusion will not normally be coincidental7. The doctor will usually be able to demonstrate a “slide in occlusion” very conclusively after the test.
There are variations on the anterior deprogrammer. Huffman numbered leaf gauge (originally proposed by Hart Long8): mylar film 10 mm wide
and .1 mm in thickness attached together in book form, total thickness with all “leaves” 5.5 mm. (Huffman Leaf Gauges, 853 Sylvan Shores Drive, South Vienna, OH, 45369-9517, phone 937.624.6101)9.
Woelfel sliding guide: made from hard plastic, which is calibrated, and varies in thickness from .5 mm to 16 mm. The Woelfel sliding guide is the simplest to use and most sterilizable of the anterior deprogrammers. (Girrbach Dental GmbH, Durrenweg 40, D-75177 Pforzheim, Germany, phone 0049.723.1957000; see website at www.girrbach.de)10 11.
Lucia jig: custom molded plastic which can be modified with an acrylic bur to any thickness desired. The jig is generally molded over maxillary centrals for retention and has point contact on a mandibular central10 12.
NTI-tss (NTI-TSS Inc.) appliance: A modified Lucia jig, which can be used for a short time as an appliance. The deficiency is the small number of teeth contacted in the lower arch. The increased pressure on such few teeth is problematic, especially as compared to the anterior appliance described in this paper13.
3
The claims of NTI-tss for the treatment of migraine are based on a 19 person study conducted in 1996 by Lamey, Steele, and Aitchison at Queen’s University of Belfast and reported in the British Dental Journal14. The Lamey study was conducted with full centric relation splints and not the NTI. The FDA granted the acceptance for migraine because of the similarity of the NTI to the centric relation splint, and the CR splints decreased migraine by 40%. Therefore, by this logic the NTI would also have this effect. As stated previously, there is great confusion as to the diagnosis of migraine or TMD. Splints are for TMD and may benefit some true migraine patients because TMD can be a secondary symptom. Controlling a secondary symptom may decrease the frequency of the migraine, but true migraine will not be controlled with an anterior splint. This leaves the claims of others subject to judgment.
The test with the anterior deprogrammer begins by: Placing it between the patient’s maxillary and mandibular central incisors. The patient must first protrude and then retrude the mandible to its most posterior position. They then bite with “substantial” pressure on the deprogrammer. The doctor or auxiliary must sit with the patient, making sure that they stay retruded and
continue to bite with substantial pressure. It is necessary that the test be conducted for at least 7 minutes; muscles sometimes take that long to spasm. Many times the patient will feel nothing prior to the onset of the painful spasm.
No posterior teeth can touch (see figure 8). It is also important that the patient be comforted if the test produces a painful result, and
duplication of the symptoms is successful. The patient is never asked to continue beyond their endurance. Place warm moist towels on affected area for comfort. The Key: Once the patient reproduces the chief complaint, the test does not need to continue. The diagnosis of TMD has been made, and an appliance (anterior or pivotal) is appropriate. The following steps are physical therapy (refer to page 19 for more information). If the pain is minor or the patient does not desire an appliance the following technique may be used to control symptoms.
Once the pain begins, the patient should alternately bite for six seconds and relax for six seconds.
Test continues for 7 but no longer than 10 minutes, measured from the beginning of testing. The test is stopped prior to the 10 minutes if pain subsides. This is referred to as cycling the muscle, which is a stretching of the muscle until the myospasm subsides.
A true joint patient will be in pain from the onset of the test, and seven minutes is long enough for them to tolerate the discomfort. The Key: If stressing a structure reproduces the chief complaint, then the source of the pain has been diagnosed with the stress test.
A phenomenon occurs when a patient first complains of joint symptoms at the onset of the test. The joint pain will sometimes go away after 2 to 3 minutes and is then replaced by the typical muscle spasm related to TMD. It is hypothesized that a muscle spasm of the lateral pterygoid repositions the disc (through the stretched TMJ capsule) in a more forward position than normal; once the disc is in this forward position, it is sensitive to the initial testing15 (see figure 10). However, it will then reposition to a more normal posture when the muscle starts to release. If the test is stopped prior to the 7 minutes the clinician may incorrectly conclude that the patient has a joint problem, which is a more involved treatment than that for a muscle spasm.
4
Figure 10: Left side, disc out of position; Right side, normal disc position.
The test is simple, but very telling because of the neurologic principle of primary site stimulation1 16. Primary site simulation, as previously discussed, is the premise that if one presses on a structure that is truly causing the pain, the pain will change. If the practitioner presses on a structure that is aching because of referred pain, the pain will not change. If the stress test causes or changes the chief complaint, the diagnosis of TMD is appropriate. It is important that the clinician asks the patient, “Is this the same pain as your headache or just part of the headache?” The question can also be asked, “Is this the pain for which you are seeking treatment?”
Patients can be both a TMD and headache sufferer. One of the conditions will be more significant. If they are mainly a headache patient with a lesser amount of TMD, treating the TMD successfully will not get rid of the headache. However, if the dentist is able to eliminate the TMD component, the headache may decrease in either intensity and/or frequency17. Remember, the trigeminal nerve is the major sensory nerve of the head and neck. Beware of referred pain18.
Advanced Understanding: Another condition that may be associated with TMD deals with patients having otologic complaints, such as otalgia, tinnitus, vertigo, and hearing loss. These individuals have a higher incidence of otologic complaint than do control subjects without TMD signs or symptoms19. The overlap of symptoms is most likely due to convergence. It is probable that other muscles can also be affected by the phenomenon. Possibly, the tensor tympani, which dampens and stabilizes the inner ear to vibration, could also be affected. Taking one more step, the tensor veli palatine may also be affected by convergence. Loughner hypothesizes that the closing of the Eustachian tube, the responsibility of this muscle, creates a sensation similar to a sea shell over the ear20. The sensation created may be the otologic symptom for which the patient has a complaint.
5
TMD SPLINTS – WHEN, WHY, AND HOW21
Potential Sources of Headache and Orofacial Pain: Vascular, Myofascial, Neurologic, and Intracapsular / Joint Pain
6
JointSplint of choice: Pivotal Appliance (Always Bilateral)
Wear time: 24/7 for one month but Never while eating. After first month gradually reduce daytime wear until symptoms abate (6 months to 1 year).Splint will require an adjustment each month. Stress test by loading the TMJs to confirm healing (10 Minutes).
Mechanics: Unloads and decompresses TMJ.
MuscleSplint of choice: Anterior Appliance
Wear time: Only at night
Mechanics: Physical therapy for the lateral pterygoids. Ensures Anterior Disclusion!
NO PAIN – NOT
STOP BITINGPAIN LINGERS OVER JOINT COMPARTMENT (TMJ) (Capsulitis, Synovitis, Arthritides, or Nonreduceable Disc)
STOP BITINGPAIN SUBSIDES (MUSCLE) Educate the patient and cycle the muscle (Home Care Instructions)
Stress Test by Loading, Resulting in Primary Site Stimulation (“A Basic Orthopedic Principle for Diagnosis”)
Technique: Anterior Deprogramming DeviceTime: .5-7 minutesMuscle Activity: Temporalis contracts (Bilaterally) Superior head of lateral pterygoid contracts (Bilaterally) Inferior head of lateral pterygoid stretched to relaxed length (Bilaterally) TMJ Impact: Compression/Loading of the condyle disc assembly and joint structures
PAIN – TMD STARTS WITHIN .5 – 7 MINUTES
Anterior Deprogrammer Stress Test Technique22 23
1. Place the anterior deprogrammer at midline between the maxillary and mandibular central incisors22 23 24.
2. The patient first protrudes, then retrudes the mandible to its most posterior position. The patient bites with constant, substantial pressure on the anterior deprogrammer.
3. During the entire test, no posterior tooth can touch. An excessive number of leaves should not be added to accomplish the separation of the posterior teeth. If 5 to 10 additional leaves (beyond first contact) are used, that should be sufficient.
4. Most TMD patients exhibit symptoms from the damaged tissue within .5 to 7 minutes24.5. During the test, ask the patient, “Is this a familiar pain?” It must be similar to their “headache,”
for which they are seeking treatment, to qualify as a familiar pain. The intensity of the headache may not be the same but the character will be familiar.
6. The familiar pain must be the patient’s chief complaint.7. The stress test changes to alternately biting for 6 seconds and resting for 6 seconds after pain
develops.8. The pattern continues for several minutes or until the pain subsides. Generally, the pain will
subside within the ten minutes.9. If pain starts in the joint and remains in that area after seven minutes the pain will only get
worse. Stop the test. The pain will not subside. 10. Never ask a patient to continue beyond their endurance. Place warm, moist towels on affected
area for comfort.
The Key: Once the patient reproduces the chief complaint, the test does not need to be continued. The diagnosis of TMD has been made, and an appliance is appropriate.
Advanced Understanding:
Steps 7-10 are physical therapy. If the TMD complaint is minor muscle pain or if the patient does not desire an anterior appliance, the stress test technique may be used at home by the patient two times each day to control symptoms (early AM and late PM). The therapy technique will only make the TM joint patients more uncomfortable, therefore it is only recommended for muscle patients.
7
ANTERIOR APPLIANCE
STRESS TEST TECHNIQUE
The Anterior Appliance is both a diagnostic and therapeutic modality. The appliance must be adjusted properly for the test to be valid. The chief advantage of the Anterior Appliance over the Anterior Deprogrammer is that the patient does not have to be subjected to the “creation of the headache,” but the practitioner must first understand the anterior deprogrammer concept. The appliance stretches the lateral pterygoid (both superior and inferior heads) over a longer period; and, normally, the patient does not experience the pain of cramping.
Three outcomes are possible with the Anterior Appliance, worn for diagnostic purposes, after two weeks of wear:
a. The patient feels no difference – TMD is not the patient’s source of pain.b. The patient experiences pain in or around the ear, which does not go away after two weeks –
switch to Pivotal Appliance. c. The patient feels significantly better after a two-week period of wearing the Anterior
Appliance – great!
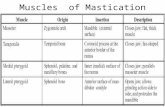
Mechanics of the Anterior Deprogramming Device and Appliance:Utilizing the muscles of mastication and guide planes one can take advantage of force vectors to stretch the lateral pterygoid (superior and inferior head) and seat the condyle. These actions can be done with either the anterior deprogrammer or anterior appliance. If either is placed between the central incisors with no posterior tooth contact and the patient bites -- an anterior superior movement of the condyle must occur25 26. The anterior deprogrammer does this quite easily but the anterior appliance must be adjusted properly to achieve this goal. Refer to anterior appliance adjustment.
Please note the force vectors, if the anterior teeth are brought into contact without posterior tooth contact.
Superior head of lateral pterygoid is stretched.
Inferior head of lateral pterygoid is stretched.
The condoyle is forced to assume a more superior, anterior position.
The disc is compressed.
The anterior appliance decreases the mechanical stress on the masticatory system. However, if the TMJ is the source of the pain, the anterior appliance will increase the pain in or around the ear. If the joint is
8
STOP BITINGPAIN SUBSIDES (MUSCLE)
Educate the patient and cycle (refer to page 21) the muscle
MuscleSplint of choice: Anterior Appliance
Wear time: Only at night
Mechanics: Physical therapy for the lateral pterygoids. Ensures Anterior
the problem, the use of the anterior appliance should be discontinued. The use of the pivotal appliance is indicated.
A Review of the Flow Chart
Refer patient or find a cause other than TMD.
The patient will only feel tired and no duplication of pain will happen. No pain is a sure indication that TMD is most likely not the problem.
Exception – If the test is negative, ask the patient if he/she is in a headache cycle now? If not, the test should be attempted again during a headache cycle. The variable nature of the bruxism can cause muscle pain to come and go.
TMD is the diagnosis
Pain (chief complaint) is duplicated within 3 to 7 minutes, and stops if the patient releases. Most TMD patients fall into this category27 28.
Treatment: Anterior Appliance
The chief complaint starts in 3 to 7 minutes, and if biting pressure is released – the pain will go away. It can radiate into the joint, temples, back of the neck, sinus area, top of head, or just about anywhere else in the head and neck region
The chief complaint will be duplicated (not intensity but character)
Patient comfort is always of the utmost importance Fabricate the anterior appliance Give patient home care instructions Have patient keep pain diary Recall in two weeks
A supportive nature is very helpful during the procedure. The stress test can really hurt. An excellent idea is for the practitioner to experience the test, before administering it to patients. The physical therapy technique
9
NO PAIN – NOT
PAIN – TMD STARTS WITHIN .5 – 7 MINUTES
D
of applying warm, moist heat to the painful area makes the contraction more bearable. The painful muscles are probably the lateral pterygoid complex and/or the temporalis29 30. The deep masseter may also play a role.
BENEFITS OF THE ANTERIOR APPLIANCE:
1. The anterior appliance with shallow anterior guidance is the least invasive definitive therapy. 2. Anterior appliance is much easier to adjust than the typical centric relation splint. 3. The number of adjustment appointments is considerably less than with full occlusal splints. The
design allows for more healing between appointments and retains its adjustment longer, because the posterior occlusion is not involved.
4. The breakage problem is significantly reduced (without posterior tooth contact the masseter and the medial pterygoid do not contract nearly as forcefully30).
5. Patient compliance is higher. Because of the design, saliva makes the appliance almost disappear.
TWO CONCERNS WITH THE ANTERIOR APPLIANCE EXPRESSED BY MANY PRACTITIONERS:
Many practitioners have asked if this lack of posterior contact causes a problem. The answer is clear -- it does not cause teeth to shift, when the appliance is used as described.
o The appliance should not be used for eating or during the day after the first two weeks. o No change in the occlusion has been evident from the pretreatment casts. It is
important, however, to include the two “C” clasps, which are retentive, on the first premolars. Otherwise movement may possibly occur between the maxillary first premolar and maxillary canine.
Since the appliance is small – will the patient swallow it and is the appliance stable? If made correctly, stability will not be a problem. After fabrication, place the appliance and ask the patient to try and “knock it loose” without using their hands. If the retention is not sufficient, reline or use Biostar (pressure forming unit) from Great Lakes Orthodontics for fabrication.
Advanced understanding:
Not all patients who have TMD symptoms are aggressive bruxers. The anterior appliance is very successful for muscle patients – except for one group. The group that will not have success is made up of the patients who do not aggressively brux. They will come to the office for their two week check, and not one mark on the anterior appliance can be found. The management of this group must include home care instructions, the utilization of the anterior deprogrammer for exercise, and the anterior appliance. The anterior deprogrammer stress test (all steps) is used prior to sleep and when the patient wakes in the morning. It is recommended to leave the anterior appliance in place during the exercise. The anterior appliance along with the exercise utilizing the anterior deprogrammer will generally control the muscle symptoms. It has been observed that this group is structurally the smallest of the female patients31; they are the group that holds their mandible forward in protrusion instead of bruxing.
It is important to note that the design of the appliance may impact how the patient sleeps and breathes at night. It has been shown by Gagnon and also Nikolopoulou that in subjects with sleep apnea, an occlusal splint may cause an elevation in AHI32 33 34. The advantage of the anterior appliance is the
10
minimal thickness of acrylic. It is designed to allow for as much tongue space as possible. If an occlusal guard is too bulky, it will crowd the tongue and force it to the posterior, which aggravates the person’s airway while they are attempting to breathe during sleep, potentially contributing to an increase in respiratory disturbances, hypopneas or apneas.
Advanced Understanding:
Q: What comes after the successful use of the Anterior Appliance?A: For a true TMD patient with no airway issues, no further treatment is needed, unless the patient desires a more definitive answer.
If the patient feels encumbered by the appliance or the amount of wear time, what should be done? An excellent set of casts are mounted on an Arcon articulator to determine the person’s occlusal
and skeletal relationships. Time is saved by making the maxillary posterior segments removable. A careful and complete diagnostic work-up (including radiographs, consultations, testing, etc.)
must be accomplished before any irreversible treatment is rendered. The methods available to clinicians, as dentists, are limited. A well planned occlusal adjustment
that satisfies the mechanics of the anterior appliance may be the best option. Care must be taken that the adjustment is not overly damaging to the system. All options need to be considered!
The Key: If the mechanics of the anterior appliance can be duplicated, then the success should be replicated. The correction, if completed and goals are met, gives a very similar situation to that of the centric relation splint. The reduction of painful symptoms with appliance therapy is very well documented35 36 37.
If the individual is a sleep patient with airway concerns and TMD symptoms, it is appropriate to screen them with a high resolution pulse oximeter once their TMD symptoms have been addressed. They can
11
The test for occlusal change is quite simple: An accurate pretreatment impression is taken, poured immediately in die stone, and filed for future reference.
It is imperative that the cast be accurate and meticulously cleaned of inaccuracies. Another impression is taken and poured six months to a year later with equal care. The patient cannot wear
the anterior appliance to this appointment! The pretreatment cast is pressed into soft red compound to leave cusp tip impressions and excess compound is
removed. The second cast is then tried into the compound impression – there should be no discrepancy.
then be referred for a polysomnogram as needed and treated with a mandibular advancement device. This will be further discussed in subsequent sections.
THE ANTERIOR SPLINT DIAGNOSTIC TECHNIQUEPotential Sources of Headache and Orofacial Pain:
Vascular, Myofascial, Neurologic, and Intracapsular / Joint Pain
12
JointSplint of choice: Pivotal Appliance (Always Bilateral)
Wear time: 24/7 for one month but Never while eating. After first month gradually reduce daytime wear until symptoms abate (6 months to 1 year).Splint will require an adjustment each month. Stress test by loading the TMJs to confirm healing (10 Minutes)
Mechanics: Unloads and decompresses TMJ
MuscleSplint of choice: Anterior Appliance
Wear time: Only at night
Mechanics: Physical therapy for the lateral pterygoids Ensures Anterior Disclusion!
NO CHANGE – NOT TMD
AFTER 2 WEEKS – PAIN PRESENT IN TMJ AREAPAIN HAS INTENSIFIED OR STAYED THE SAME OVER JOINT COMPARTMENT (Arthritides or Nonreduceable Disc)
AFTER 2 WEEKS -- PATIENT IMPROVED
PAIN HAS DEFINITELY IMPROVED AND PATIENT FEELS THAT THEY ARE RECOVERING (Muscle Pain, Capsulitis, or Synovitis)
Stress Test by Progressive Loading
Technique: Anterior ApplianceTime: 2 weeks / 24 hour wear, except when eatingMuscle activity: Temporalis contracts (Bilaterally)
Superior head of lateral pterygoid contracts (Bilaterally)Inferior head of lateral pterygoid stretched to relaxed length (Bilaterally)
TMJ Impact: Compression / Loading of the condyle disc assembly and joint structures
AFTER TWO WEEKS IF …. MUSCLE PAIN - RESOLVES / IMPROVING
ORTMJ - PAIN PRESENT IN TMJ AREA
Requirements of Anterior Appliance
1. Appliance must be stable – Cover entire facial and lingual surfaces of teeth numbers 5 through 12 and cut off occlusals on 5 and 12. To reduce retention, prior to fabrication, the deep undercuts on the cast should be blocked out. Less desirable solutions are to decrease the facial coverage and/or cut through the appliance’s facial interproximals with a fine disc to separate the teeth. Remember, the more esthetic the appliance – the greater the compliance. If the retention is not sufficient, reline or use Biostar pressure forming unit from Great Lakes Orthodontics for fabrication.
2. The appliance is adjusted until the mandibular six anterior teeth touch. A smooth arc of contact is desired and if a mandibular anterior tooth is severely out of alignment – it should be ignored.
3. The anterior deprogrammer should be used to adjust the appliance after two weeks of wear; this should never be done at the delivery appointment. The technique is to add leaves until no tooth touches and then take away one leaf at a time, while adjusting contact, until no leaves remain. Even contact of all teeth with the TMJs seated is the goal.
4. Anterior guidance must be very shallow and as flat as possible but retain some angle in order to separate the posterior teeth.
5. At least 3mm of “slide area” required from centric point to edge of splint.
6. Posterior teeth cannot touch – if they do, the appliance will not work! The patient returns in approximately 2 weeks for check. They must wear their appliance to the appointment. The check is to refine the appliance. If a posterior tooth touches, one must add to the splint. Adjust contacts with the anterior deprogrammer.
A Key: if the patient complains of joint symptoms after two weeks with this type of splint, one should not continue. One must change to a pivotal appliance.
7. Patient instructions – wear appliance at night only and follow home care instructions (Page 19). If for the first two weeks the patient is having significant problems, daytime wear is permissible. After patient symptoms are relieved, the patient should use as needed.
8. Patients should always be prescribed Colgate Prevident Fluoride Gel (not Colgate Prevident 5000 Paste), and they should place a “pea size” amount of the Gel in the splint before bed (Colgate Palmolive, www.colgate.com).
13
JointSplint of choice: Pivotal Appliance (Always Bilateral)
Wear time: 24/7 for one month but Never while eating. After first month gradually reduce daytime wear until symptoms abate (6 months to 1 year).Splint will require an adjustment each month. Stress test by loading the TMJs to confirm healing (10 Minutes)
Mechanics: Unloads and decompresses TMJ
STOP BITINGPAIN LINGERS OVER JOINT COMPARTMENT (TMJ)(Capsulitis, Synovitis, Arthritides, or Nonreduceable Disc)
Joint Pain and the Pivotal Appliance
Indications for the pivot appliance defined 38 :
1. Non-reducible dislocated articular disc, confirmed by MRI.2. Systemic disease entities that cause arthrogenous pain in TMJ during the stress test (e.g., arthralgia, osteoarthritis, osteoarthrosis).3. Post-surgical involvement of the TMD.4. Intracapsular pain -- determined to be the TMJ by either stress test.
Utilizing the anterior deprogrammer to stress the system, the patient will begin to exhibit symptoms within the first minute. The pain will only intensify as the test continues.
After the patient exhibits symptoms, the test changes to alternately biting for 6 seconds and resting for 6 seconds. The pain will only increase in intensity, and does not diminish. Stop test after 7 minutes. A diagnosis is evident, and nothing will be gained by continuing. Joint derangements are highly probable39 40. Many times the patient will relate that they cannot chew anything hard (bagel, pizza crust, chips, tough meat, etc.) without causing a headache.
A Key: Experience has shown that approximately 60% of patients initially reporting pain in the joint while chewing are not joint patients but are actually muscle patients41.
If there is ever a question of joint involvement with the anterior deprogrammer test the practitioner has two choices:
1. Place cotton rolls on both the left and right sides between the first and second premolars, then tell the patient to bite hard42. The placement here is very important. Too far back on the molars and you will unload the joint; and too far forward on the anterior teeth, the lateral pterygoid, and temporalis are stimulated.
Joint patients will have pain Muscle patients will not have pain
2. Fabricate an anterior appliance and prescribe an anti-inflammatory medication. Seat appliance and wait two weeks. Sixty percent of the time, after 1 – 2 weeks the joint symptoms will disappear. If they do not resolve – make a pivotal appliance.
14
Special Situation for Disc Displaced Less than Four Weeks:1. Time is of the essence and all treatment must be completed in 4 weeks or the joint begins to
fibrose, which will prevent the disc from repositioning.2. If the displacement is recent (less than 3 weeks), an anterior appliance is fabricated that day
for the patient. The patient is then placed on a Medrol (methylprednisone, Upjohn) Dosepak six (6) day regimen (4 mg, 21 tablets), provided there are no contraindications.
3. Patient should be seen after 3 days on Medrol and questioned about range of motion and symptoms.
4. If range of motion is back to normal and the symptoms are in remission, then wait another three days and reexamine.
5. If all normal – congratulations – if not proceed to step 6.6. If displacement has not reduced, consider having a capable specialist perform a TMJ
arthrocentesis, a nonarthroscopic lavage and lysis, which is highly efficient in this particular type of TMJ problem.
7. After the injection procedure, treat the patient with an anterior appliance to stabilize the disc.
8. Time is of the essence. The surgeon must perform this procedure immediately, within the 4 week deadline.
9. The use of the anterior appliance for stabilization has been very successful31. If joint symptoms persist a pivotal appliance is necessary.
Treatment for a Painful Joint:
The pivotal appliance is generally effective for the displaced disc. It has the ability to alter the mechanics
of the jaw at the joint level to an unloaded, uncompressed treatment position43 44. The appliance is perfectly flat, over the most distal tooth. Both left and right contact at the same time (refer to requirements of pivotal appliance handout). The pivotal appliance transfers the fulcrum from the TMJ to the teeth intentionally, until healing occurs.
The patient does not eat with the appliance in place, and the appliance is worn 24 hours each day. Generally, after 6 weeks the appliance is only worn at night. Treatment time is variable, but is generally at least 4 to as many as 18 months. Time must be given for healing to occur. Wear of the appliance continues until the loaded position is comfortable. One may test, as previously described, to assure healing of the TMJ has occurred. One of the true pleasures of dentistry is to see the positive change in the TMJ patient; sometimes, the personality change is dramatic.
How to determine if the loaded position is comfortable (Tests all previously described):
1. Anterior Deprogrammer2. Cotton rolls in the premolar area3. Anterior Appliance
15
Variation of the Cotton Roll Test One Can Perform To Validate the Idea of A Pivot: The concept of changing the mechanics at the joint level requires a careful analysis of the mechanics involved. A skull helps in the understanding of the pivot mechanics. Here is a test which may be performed in one’s own office, when the clinician has diagnosed a probable TMJ problem:1. Place cotton rolls bilaterally in the first and second premolar area.2. Instruct the patient to bite hard – the joint will be painful (The placement is critical to ensure
stimulation of the proper muscles; pressure on anterior teeth can cause contraction of the lateral pterygoid and temporalis muscles, which confuses the test due to referred pain).
3. Move back over the most posterior molar and bite hard – the joint will not hurt. What changed? The mechanics changed!
Photo of disc is taken from the middle cranial fossa, the floor of which has been removed45. It should be noted that the disc has been displaced but the retrodiscal tissue has “extended the disc.” Collagen makes up much of the retrodiscal tissue and can be remodeled into disc tissue.
Conditions must be such that healing can happen. It is the goal that the pivotal appliance will create these conditions. If the patient’s pain is relieved, it is extremely likely that this healing has occurred.
TWO CONCERNS WITH THE PIVOTAL APPLIANCE EXPRESSED BY MANY PRACTITIONERS:
1. Many practitioners have asked if this lack of anterior contact causes a problem. The answer is clear – it does not cause teeth to shift, when the appliance is used as described. The patient must understand they cannot eat with this or any appliance. Tooth movement can occur if this appliance is used for longer periods than described46.
2. Since the appliance is two unilateral, unconnected appliances, will the patient swallow them and are they stable? If made correctly, stability will not be a problem. After fabrication, place the two appliances and ask the patient to try and “knock them loose” without using their hands. If the retention is not sufficient, reline or use the Biostar (pressure forming unit) from Great Lakes Orthodontics for fabrication.
16
Medial
Lateral
Posterior
Anterior
Extended discSuperior head of Lateral Pterygoid
Deep Temporal Nerve
Requirements of Pivotal Appliance
1. Appliance must be stable – Cover entire buccal and lingual surfaces of mandibular molars and second premolar. The appliance is two separate pieces. If the retention is not sufficient, reline or use the Biostar pressure forming unit from Great Lakes Orthodontics for fabrication.
2. Add orthodontic acrylic to central fossa area of last mandibular molar, which has an opposing maxillary molar; make this addition as thin as possible and flat (If no molars exist, the dentist must supply
them; this can be done with a removable partial denture or implants. If more retention is needed, grooves can be cut in the RPD
for stabilization). At least 2mm of “slide area” is required from the centric point where the mesial lingual cusp of the last maxillary molar makes contact to edge of splint.
3. Adjust the splints so they both touch at the same time when the patient closes with the tongue pressed against the roof of their mouth. No attempt is made to achieve centric relation.
4. Teeth anterior to the last molar cannot touch – if they do, the appliance will not work! The patient must wear the appliance at all times, except when they eat, and return in approximately 2 weeks for a check. Examine, to be sure no teeth anterior to the contact point touch, and that the area where the posterior maxillary molar touches is perfectly flat. A relatively small depression in this area will prevent the appliance from functioning correctly.
5. If appliance is adjusted properly the joint symptoms will be nearly nonexistent or much improved after 3 to 5 days. (A temporal headache indicates the pivotal appliance is too thick. High Angle Class ll patients have this problem, due to lack of freeway space. A solution is to make the appliance thinner or move the pivot to the first molar area.)
6. Patient instructions – wear appliance except when eating and follow home care instructions (Page 19). After 6 weeks switch to nighttime wear only. Treatment time varies with age and magnitude of the problem. The normal length of time is from 6 to 18 months. The health of the joint can be determined by running a stress test with an anterior deprogramming device, anterior appliance or cotton rolls (described previously).
7. After the loaded position is no longer painful, discontinue use of the pivot and treat as a muscle problem only. If the anterior appliance is not painful, treatment is successful.
8. Patients should always be prescribed Colgate Prevident Fluoride Gel (not Colgate Prevident 5000 Paste), and they should place a “pea size” amount of the Gel in the splint before bed.
18
The Pivotal Appliance
Advanced UnderstandingMechanics of the Pivotal Appliance
Possible Axis:Condyle—CondyleCondyle-Fulcrum
19
Anterior Appliance
Perfectly Flat
In this area
Second Molar First Molar Second Premolar
Home Care Disciplines for Muscle and Joint SorenessJames E. Metz, DDS, 1271 East Broad Street, Columbus, Ohio, 43205
614-252-4444, [email protected]
The time it will take to gain comfort will depend, in part, upon you following these instructions.
1. MOST IMPORTANT DISCIPLINE – Preferred position of sleep Sleep on your side with the pillow high on your head, and with no pressure on the jaw. Speak with Dr. Metz if you have a
question, especially if you are abnormally tired during the day with a sufficient amount of sleep. Use a rolled up towel or pillow against the back to keep from changing to flat on the back. It is very hard to change sleep
habits, so do not give up! As long as 6 months is sometimes needed to change sleeping positions.
2. Avoid caffeine and sugar as much as possible, both are stimulants to the nervous system. Intake of coffee, Mountain Dew, cola, diet cola, tea, chocolate, etc. should be very carefully monitored and curtailed. The caffeine contained in one cup of coffee is the maximum amount a person should consume per day. Caffeine can get rid of a headache and can cause headache. Reducing your intake of caffeine “cold turkey” will bring on headaches in many people. You may need to take ibuprofen (400 mg. four times a day, read the warnings on the packaging) to control a withdrawal
headache from caffeine.
3. Eat a soft diet and avoid chewing as much as possible. Absolutely no gum chewing. Avoid clenching your teeth. No bagels, hard carrots, tough meats, or anything that requires “hard chewing.”
4. Avoid clenching your teeth during the day. Many people think they do not clench but most do at times. A good technique for catching yourself clenching is to program your brain to think, “Am I clenching my teeth?” You can use
every day events to “jog” your memory. Think! Every time you look at your watch (before you even think of the time) or walk through a door, try to catch yourself clenching. After practice, this technique is very effective in preventing TMD headache during your waking hours.
Small “sticky dots” from a stationary store can remind you not to clench. Put one wherever it will be a good reminder. If you see one, think “am I clenching my teeth?” (Technique from Dr. Gordon Douglass, San Francisco, CA)
If you catch yourself, place your tongue in the roof of your mouth and push hard while you move your jaw up and down.
5. Avoid over opening and stretching your jaw. A two and one-half finger width of opening is maximum distance allowed, especially when yawning; push up with a fist under your jaw when yawning to limit opening.
6. Take your medications. Medication helps to gain control of symptoms more rapidly by decreasing inflammation. Call the office or emergency (911) if you feel an allergic reaction is occurring, and discontinue medication use immediately.
7. Wear your appliance! You can decrease the wear time of the anterior appliance as soon as you start to feel better. The pivotal appliance needs a 6 to 18-month period to accomplish its goals and the wear time is variable. Never wear the
appliance after the initial 2 week period during the day. After the pivotal appliance healing period, the anterior appliance will follow. Never wear either appliance when eating.
8. It is your responsibility to maintain contact with the office. If you start to have pain, call the office. A regular check appointment is essential, especially for the pivotal. Initially the appointment time is every two weeks. After
control is gained, every three to six months is essential. Never wear the pivotal appliance singly because the appliance will cause harm. Never wear a broken appliance. Call if you have a problem or if your appliance is making the symptoms worse. Call immediately if the pain starts to center in or around your ear.
20
1 Mense M, Simons DG, Ressell IJ, Muscle Pain, Understanding Its Nature, Diagnosis and Treatment, Lippincott Williams and Wilkins, Philadelphia, 17-18, 20012 Okeson JP, Bell’s Orofacial Pain, 5th ed., Quintessence Publishers Inc., Chicago: 66, 19953 Johnstone DR, Templeton M, The feasibility of palpating the lateral pterygoid muscle, J Prosthetic Dentistry, 44(3):318-23, 19804 Mense M, Simons DG, Ressell IJ, Muscle Pain, Understanding Its Nature, Diagnosis and Treatment, Lippincott Williams and Wilkins, Philadelphia, 26, 20015 Fenlon MR, Woelfel JB, Condylar position recorded using leaf gauges and specific closure forces, Intl J Prosthodontics, 6(4):402-8, 19936 Wood DP, Floreani KJ, Galil KA, Teteruck WR, The effect of incisal bite force on condylar seating, Angle Orthodontist, 64(1):53-61, 19947 McHorris WH, Focus on anterior guidance, Journal Gnathology, 1:3-13, 19898 Long H, Locating centric relation with a leaf gauge, J Prosthetic Dentistry, 29:608-610, 19739 Rosenblum RH, Huffman RW, Leaf gauge with consecutively numbered leaves, J Prosthetic Dentistry, 54(5):652-654, 198510 Woelfel JB, New device for accurately recording centric relation, J Prosthetic Dentistry, 56(6):716-28, 198611 Carroll WJ, Woelfel JB, Huffman RW, Simple application of anterior jig or leaf gauge in routine clinical practice, J Prosthetic Dentistry, 59(5):611-618, 198812 Lucia VO, A technique for recording centric relation, J Prosthetic Dentistry, 14(3):492-505, 196413 Staplemann H, Turp JC, The NTI-tss device for the therapy of bruxism, temporomandibular disorders, and headache-where do we stand? A qualitative systematic review of the literature, BMC Oral Health, 8(22):1-23, 200814 Lamey PJ, Steele JG, Aitchison T, Migraine: the effect of acrylic appliance design on clinical response, British Dental J, 180(4):137-140, 199615 Metz, JE, personal communication 2003-201316 Sessle BJ, Bryant PS, Dionne RA, Temporomandibular Disorders and Related Pain Conditions, Seattle: IASP Press: 208, 199517 Magnusson T, Carlsson GE, Recurrent headaches in relation to temporomandibular joint pain dysfunction, Acta Odontologica Scandanavia, 36(6):333-8, 197818 Ehrlich R, Garlick D, Ninio M, The effect of jaw clenching on the electromyographic activities of two neck and two trunk muscles, J Orofacial Pain, 13(2):115-20, 199919 Tuz HH, Onder EM, Kisnisci RS, Prevalence of otologic complaints in patients with temporomandibular disorder, American J Orthodontics Dentofacial Orthopedics, 123(6):620-2, 200320 Loughner BA, personal communication 2003-201021 ©James E Metz, DDS, 1271 East Broad Street, Columbus, Ohio, 43205, 614-252-4444, www.ColumbusDentistry.com; Flowchart developed with Dr. William McHorris, Memphis, Tennessee22 McHorris WH, American Academy of Restorative Dentistry, 199523 McHorris WH, personal communication, 1982-200324 Dorland’s Illustrated Medical Dictionary, 28th ed., Philadelphia: WB Saunders: 1550, 199425 Downs DH, An investigation into condylar position with leaf gauge and bimanual manipulation, J Gnathology, 7 1:75-81, 198826 Downs DH, Albers MT, Boyle AG, Greer WT, Marker TJ, Parlet CR, Schulz KS, Wilson RL, Centric relation for diagnostic mountings, J Gnathology, 16 1:7-14, 198827 Gelb H, Tarte J, A two-year clinical dental evaluation of 200 cases of chronic headache: the craniocervical-mandibular syndrome, J American Dental Association, 91(6):1230-6, 197528 Forssell H, Kangasniemi P, Mandibular dysfunction in patients with muscle contraction headache. Proceedings Finnish Dental Society, 80(5-6):211-6, 198429 Williamson EH, Steinke RM, Morse PK, Swift TR, Centric Relation: A comparison of muscle determined position and operator guidance, American J Orthodontics, 77(2):133-45, 198030 Williamson and Lundquist, Anterior guidance: its effect on electromyographic activity of the temporal and masseter muscles, J Prosthetic Dentistry, 49(6):816-23, 198331Metz JE, Clinical experience and observation, 2003-201532Gagnon Y, Mayer P, Morisson F, Rompré PH, Lavigne GJ, Aggravation of respiratory disturbances by the use of an occlusal splint in apneic patients: a pilot study, International J Prosthodontics, 17(4):447-53, 200433Nikolopoulou M, Ahlberg J, Visscher CM, Hamburger HL, Naeije M, Lobbezoo F, Effects of occlusal stabilization splints on obstructive sleep apnea: a randomized controlled trial, J Orofacial Pain, 27:199-205, 201334 Nikolopoulou M, Naeije M, Aarab G, HL Hamburger, Visscher CM, Lobbezzo F, The effect of raising the bite without mandibular protrusion on obstructive sleep apnoea, J Oral Rehabilitation, 38:643-647, 201135 Clark GT, A critical evaluation of orthopedic interocclusal therapy: design, theory and overall effectiveness, J American Dental Association, 108(3):359, 198436 Sheikholeslam A, Holmgren K, Riise C, A clinical and electromyographic study of the long term effects of an occlusal splint on the temporal and masseter muscle in patients with functional disorders and nocturnal bruxism, J Oral Rehabilitation, 13:137-145, 198637 Manns A, Valdivia J, et al, The effect of different occlusal splints on the electromyographic activity of elevator muscles, J Gnathology, 7:61-73, 198838 “Indications for the pivot appliance” originally proposed by Dr. William H McHorris, Memphis, TN39 Blackwood H, Arthritis of the mandibular joint, British Dental J, 115:317-376, 196340 Toller P, Osteoarthritis of the mandibular condyle, British Dental J, 134(6):223-31, 197341 Metz, JE, Clinical experience and observation, 1998-201342 Cotton roll test developed by Drs. Downs and Wilson with the RAZA study group, Colorado Springs, CO43 Okeson, J.P., Bell’s Orofacial Pains Fifth Edition, Chicago: Quintessence Publishing, 301, 1995
44Jiang T, Condyle and mandibular bending deformation due to bite force, Kokubyo Gakkai Zasshi, J Stomatological Society, Japan, 59(1):142-59, 199245 Dissection courtesy of Loughner BA, 1990-200046 Dahl BL, Krogstad O, The effect of partial bite raising splint on the occlusal face height, an x-ray cephalometric study in human adults, Acta Odontologica Scandanavia, 40(1):17-24, 1982