proefschrift jashvant poeran Virender... · 2016. 3. 10. · Virender Jashvant John Poeran....
Transcript of proefschrift jashvant poeran Virender... · 2016. 3. 10. · Virender Jashvant John Poeran....

PERINATAL MORTALITY-System Related and Environmental Factors-
Virender Jashvant John Poeran

Perinatal Mortality
– System Related and Environmental Factors –
Virender Jashvant John Poeran

Perinatal Mortality – System Related and Environmental Factors –
PhD thesis, Erasmus University Rotterdam, The Netherlands
Cover design Joseph Mallchok | Maaike van der Staal, YourThesis
Layout Renate Siebes, Proefschrift.nu
Printing Ridderprint, Ridderkerk
Publisher Medix Publishers BV, Keizersgracht 317A, 1016 EE Amsterdam
ISBN/EAN 978-94-91487-08-8
Acknowledgements
The board of The Netherlands Perinatal Registry kindly provided permission to use the
Registry for research purposes.
The research presented in this dissertation was performed at the department of Obstetrics
and Gynaecology, division of Obstetrics and Prenatal Medicine, Erasmus MC, Rotterdam,
The Netherlands
Financial support for this dissertation was kindly provided by:
The department of Obstetrics and Gynaecology Erasmus MC, The Rotterdam municipal
authorities and the ‘Ready for a Baby’ programme (www.klaarvooreenkind.nl), J.E. Jurriaanse
Stichting, Medical Dynamics, Mpluz, Danone, BMA-Mosos, Goodlife Pharma, AbbVie BV,
Nutricia, Vasa Previa Foundation (www.vasaprevia.nl).
“The Dutch Vasa Previa Foundation is a non-profit organization whose primary objective is
the reduction of infant mortality or permanent injury due to vasa previa. Some activities to
achieve this are drawing attention to the risk of vasa previa within the relevant professional
groups and aiming for adjustment of medical protocols, which are important for diagnosis and
management of vasa previa. In addition, the foundation offers support and advice to anyone
who is experiencing or has experienced vasa previa.”
Copyright © 2013
Virender Jashvant John Poeran, Rotterdam, The Netherlands, [email protected]
All rights reserved. No part of this thesis may be reproduced in any form or by any means
without written permission from the author.

Perinatal Mortality
– System Related and Environmental Factors –
Perinatale sterfte: systeem gerelateerde
en omgevingsgebonden factoren
PROEFSCHRIFT
ter verkrijging van de graad van doctor aan de
Erasmus Universiteit Rotterdam
op gezag van de rector magnificus
Prof.dr. H.G. Schmidt
en volgens besluit van het College voor Promoties.
De openbare verdediging zal plaatsvinden op
woensdag 18 september 2013 om 11:30 uur
door
Virender Jashvant John Poeran
geboren te Paramaribo (Suriname)

PROMOTIECOMMISSIE
Promotoren Prof.dr. G.J. Bonsel
Prof.dr. E.A.P. Steegers
Overige leden Prof.dr.ir. A. Burdorf
Prof.dr. A.J. van der Heijden
Prof.dr. A.P. Verhoeff
Copromotoren Dr. E. Birnie
Dr. S. Denktaş
Paranimfen Drs. Jacoba van der Kooy
Drs. Martijn Wagemans

CONTENTSChapter 1 Introduction 7
Part I: Perinatal health in Rotterdam
Chapter 2 Urban perinatal health inequalities 17
Chapter 3 Pregnancy and birth in Rotterdam: a local health report 25
Chapter 4 Social deprivation and adverse perinatal outcomes among Western and non-Western pregnant women in a Dutch urban population
41
Part II: Perinatal health in The Netherlands
Chapter 5 Population attributable risks of patient, child and organisational risk factors for perinatal mortality
61
Chapter 6 The ‘Healthy Pregnancy 4 All’ Study: design and cohort profile 83
Chapter 7 The effectiveness of risk selection in the Dutch obstetric care system
111
Chapter 8 Planned home compared with planned hospital births in The Netherlands: intrapartum and early neonatal death in low-risk pregnancies
129
Chapter 9 Does centralisation of acute obstetric care reduce perinatal mortality? An empirical study of over 1 million births in The Netherlands
149
Chapter 10 The impact of extremes in outdoor temperature and sunshine exposure on birthweight
171
Chapter 11 General discussion 191
Chapter 12 English and Dutch summary 207
Chapter 13 Authors and affiliations 215
Manuscripts 217
About the author 220
PhD portfolio 222
Word of thanks 224


1Introduction

8
INTRO
DU
CTION
1 In The Netherlands perinatal mortality rates exceed the European average.1-3 On a second
geographic level of comparison, i.e., within The Netherlands, adverse perinatal outcome
rates are much higher in the four largest cities (‘G4’, i.e., Amsterdam, Rotterdam, The Hague,
Utrecht).4,5 Again, on a third level, i.e., within the G4-cities, adverse perinatal outcomes are
overrepresented in socially deprived areas on the borough- and neighbourhood level.6-9
For long, population factors such as the high age of mothers at first childbirth, the high
prevalence of multiple pregnancies (as a consequence of either assisted reproduction or
high maternal age), and the increasing prevalence of non-Western pregnant women were
held responsible for the high perinatal mortality.1,2 However, these explanations were
challenged as perinatal mortality remains high in analyses after exclusion of these risk
groups.10 Recent studies have thus addressed the potential role of other factors, in particu-
lar healthcare related factors and geographic (e.g., neighbourhood, environment) factors.
Healthcare related factors put forward the unique system of Dutch obstetric care with
independently practicing community midwives11,12, travel time to hospital13, and organi-
sational characteristics of hospitals14. Candidate environmental factors are physical factors
(e.g., air pollution15,16 and ambient noise pollution17), and aggregate social factors like urban
deprivation4,7,8,18.
As stated, three geographic levels of inequalities in perinatal health are present, i.e., (1) The
Netherlands vs. Europe, (2) regions and G4-cities vs. the remainder of the Netherlands, and
(3) deprived vs. non-deprived neighbourhoods and boroughs within these G4-cities. The
causal factors of perinatal inequalities may differ between the three geographic levels. An
important cause (e.g., social deprivation) at one level may play an insignificant role at another
level. Furthermore, as the majority of studies only deliver relative effect measures5,6,8,11-14,19
with or without adjustment such as odds ratios, there is insufficient information on the
importance of risk factors for perinatal mortality in absolute terms on the population level
(e.g., population attributable risks), and the effect size of interdependence (interaction)
between these risk factors. An estimate of attribution, including interaction, is critical to
prioritise among options available to tackle perinatal mortality.
Finally, the definition of perinatal mortality has to be taken into account: death from 22
weeks of gestational age until 7 days postpartum. This definition combines stillbirth and
neonatal mortality; hence, perinatal mortality differences may rest on different underlying
patterns of these two components. Organisational studies within the Netherlands focus on
intrapartum and neonatal mortality14, but international comparison shows that in particular
(term) stillbirth mainly contributes to the poor Dutch position on perinatal health.1-3

9
INTRO
DU
CTION
1In response to the high perinatal mortality, the Dutch Minister of Health issued several
measures20 in 2008, of which two were deemed most important: (1) the appointment of an
advisory board on pregnancy and birth, and (2) the request for a national report on priority
setting of perinatal research. The advisory board proposed several recommendations in their
final report (‘A good beginning’) in 2010.20,21 Two important recommendations refer to (1)
targeting pregnancy and deprivation (particularly in urban areas), and (2) universal access
within 15 minutes to ‘qualified professionals’ (midwives, gynaecologists, paediatricians,
anaesthesiologists, and operating theatre staff ) to guarantee the quality of 24*7 acute
obstetric care.
Most recommendations from the advisory group report were also mentioned in the research
topics proposed in the ZonMw (The Netherlands Organisation for Health Research and
Development) Signalement study, which provided the quantitative background to some of
the aforementioned recommendations.22 In this study, the unique Dutch system of obstetric
care was addressed on patient, environment and healthcare related risk factors of perinatal
mortality and morbidity. Also, the concept of ‘Big4’ was introduced; ‘Big4’ refers to four
adverse pregnancy outcomes (perinatal morbidities) which precede perinatal mortality
in 85% of cases.22 ‘Big4’ morbidities were defined as the presence (single or combined)
of congenital anomalies (list defined), preterm birth (<37th week of gestation), small
for gestational age (SGA, birthweight below the 10th percentile for gestational age23) or
low Apgar score (<7, 5 minutes after birth). Mostly, the first three ‘Big4’ morbidities offer
some interventional opportunities in terms of diagnosis, preventive actions or treatments
when timely detected. Figure 1.1 illustrates in a Venn diagram the relationship between
(combinations of ) ‘Big4’ morbidities and perinatal mortality. Mainly, the presence of more
than one ‘Big4’ morbidity poses a significant risk for perinatal mortality, e.g., a low Apgar
score combined with preterm birth occurs in 30.3% of all cases of perinatal mortality.22
The Signalement study proposed a ‘stepwise’ model to represent the causal chain to
perinatal mortality.22,24 The occurrence of ‘Big4’ morbidities (‘step 1’) and their progression
to perinatal mortality (‘step 2’) is influenced by the accumulation18 and interaction of
patient, environment and healthcare related risk factors. This ‘stepwise’ model not only offers
different windows for intervention, but also implies different ways to intervene in each step.
In addition to national policy measures to increase perinatal health, local and regional
projects were launched. One comprehensive regional project is the ‘Ready for a Baby’
programme in the multi-ethnic city of Rotterdam.25,26 This public health programme was
instituted by the municipal council of Rotterdam, with collaboration of the local public health

10
INTRO
DU
CTION
1
authorities (GGD Rotterdam Rijnmond), the university medical centre (Erasmus MC) and
the healthcare professionals (e.g., gynaecologists, midwives, youth healthcare physicians).
The main object of this 10-year programme is to improve perinatal health and to reduce
perinatal mortality in all districts of Rotterdam to at least the current national average.25,26
Key elements include: (1) better understanding of the large health differences between
women living in deprived and non-deprived urban areas5,6, (2) improving cooperation
between healthcare professionals in the chain of obstetric healthcare27, (3) developing
improved methods for risk selection before and during pregnancy, and (4) methods to reach
low educated and immigrant groups. Baseline measurement and continuous monitoring
of the effect of interventions in the ‘Ready for a Baby’ programme are vital in this process.
Figure 1.1 Venn diagram with the prevalence per 1,000 births (¶) of separate and combined ‘Big4’ morbidities and their contribution to all cases of perinatal mortality († in %); this adds up to 85% of all cases of perinatal mortality.
¶ 0.3† 1.9%
CONGENITALANOMALY
PRETERMBIRTH
SMALL FORGESTATIONAL AGE
LOW APGARSCORE
¶ 0.7† 6.7%
¶ 3.1† 0.9%
¶ 54.8† 1.5%
¶ 0.6† 2.3%
¶ 62.9† 0.2%
¶ 3.2† 0.2%
¶ 18.0† 1.2%
¶ 6.4† 3.2%
¶ 1.5† 5.6%
¶ 1.0† 7.0%
¶ 2.5† 23.4%
¶ 0.4† 0.2%
¶ 5.1† 30.3%
¶ 2.2† 0.4%

11
INTRO
DU
CTION
1AIM OF THIS THESISThe aim of this thesis is to investigate the main contributing factors in adverse perinatal
outcomes on the three geographic levels. In particular the relative role of patient-,
environment- and healthcare related risk factors is studied in order to select rational health
policies and to decrease gaps in perinatal health.
This thesis has two parts, each of which draws evidence from different sources. Part I
describes results from the regional ‘Ready for a Baby’ programme, and part II contains
studies on the national level, either ordered by ‘ZonMw’ (The Netherlands Organisation
for Health Research and Development) concerning the ‘Signalement’ study, ‘SAZ’ hospitals
(a co-operative institution of circa 40 small general hospitals in The Netherlands), or the
Ministry of Health, Welfare and Sport (regarding the national programme ‘Healthy Pregnancy
4 All’). These studies will guide the reader through the eight research questions, the first
two questions being addressed in part I (Rotterdam), and questions three to eight being
addressed in part II (The Netherlands).
Part I. Rotterdam
1. How are perinatal mortality and morbidity distributed within the city of Rotterdam?
2. To what extent are determinants of social deprivation pertinent to differences in perinatal
mortality and morbidity?
Part II. The Netherlands
3. What is the contributing role of patient (maternal and child) and non-patient (healthcare
organisation, environment) risk factors in perinatal mortality on the population level?
4. What is a rational method to select priority areas for improved prevention of adverse
perinatal outcome?
5. Is the Dutch system of risk selection adequate in separating low risk pregnancies from
high risk pregnancies?
6. Can the unique feature of home birth in Dutch obstetric care still be offered as a safe
option to a selected group of women?
7. Is centralisation of acute obstetric care an effective intervention, on the healthcare
organisational level, to improve perinatal outcome?
8. Do climatological factors provide an additional explanation for inequalities in perinatal
outcome?

12
INTRO
DU
CTION
11. Buitendijk SE, Nijhuis JG. High perinatal mortal-
ity in the Netherlands compared to the rest of Europe. Ned Tijdschr Geneeskd. 2004;148:1855-1860.
2. Mohangoo AD, Buitendijk SE, Hukkelhoven CW, et al. Higher perinatal mortality in The Netherlands than in other European countries: the Peristat-II study. Ned Tijdschr Geneeskd. 2008;152:2718-2727.
3. The EURO-PERISTAT project in collaboration with SCPE EE. European perinatal health report, 2008. (online: www.europeristat.com).
4. Tromp M, Eskes M, Reitsma JB, et al. Regional perinatal mortality differences in the Netherlands; care is the question. BMC Public Health. 2009;9: 102.
5. de Graaf JP, Ravelli AC, Wildschut HI, et al. Perinatal outcomes in the four largest cities and in deprived neighbourhoods in The Netherlands. Ned Tijdschr Geneeskd. 2008;152(50):2734-2740.
6. de Graaf JP, Ravelli AC, de Haan MA, Steegers EA, Bonsel GJ. Living in deprived urban districts increases perinatal health inequalities. J Matern Fetal Neonatal Med. 2012 (in press).
7. Poeran J, Denktas S, Birnie E, Bonsel GJ, Steegers EA. Urban perinatal health inequalities. J Matern Fetal Neonatal Med. 2011;24:643-646.
8. Ravelli AC, Steegers EA, Rijninks-van Driel GC, et al. Differences in perinatal mortality between districts of Amsterdam. Ned Tijdschr Geneeskd. 2011;155:A3130.
9. Poeran J, Denktas S, Birnie E, et al. Pregnancy and birth in Rotterdam: a local health report (in Dutch: Zwangerschap en geboorte in Rotterdam: een lokale gezondheidsrapportage). Tijdschrift voor gezondheidswetenschappen. 2012;90:496-503.
10. Anthony S, Jacobusse GW, van der Pal-de Bruin KM, Buitendijk S, Zeitlin J. Factors E-PWGoR. Do differences in maternal age, parity and multiple births explain variations in fetal and neonatal mortality rates in Europe?--Results from the EURO-PERISTAT project. Paediatr Perinat Epide-miol. 2009;23:292-300.
11. van der Kooy J, Poeran J, de Graaf JP, et al. Planned home compared with planned hospital births in the Netherlands: intrapartum and early neonatal death in low-risk pregnancies. Obstet Gynecol. 2011;118:1037-1046.
12. Evers AC, Brouwers HA, Hukkelhoven CW, et al. Perinatal mortality and severe morbidity in low and high risk term pregnancies in the Netherlands: prospective cohort study. BMJ. 2010; 341:c5639.
13. Ravelli AC, Jager KJ, de Groot MH, et al. Travel time from home to hospital and adverse perinatal outcomes in women at term in the Netherlands. BJOG. 2011;118:457-465.
14. de Graaf JP, Ravelli AC, Visser GH, et al. Increased adverse perinatal outcome of hospital delivery at night. BJOG. 2010;117:1098-1107.
15. de Medeiros AP, Gouveia N, Machado RP, et al. Traffic-related air pollution and perinatal mortal-ity: a case-control study. Environ Health Perspect. Jan 2009;117(1):127-132.
16. Wilhelm M, Ritz B. Residential proximity to traffic and adverse birth outcomes in Los Angeles county, California, 1994-1996. Environ Health Perspect. Feb 2003;111(2):207-216.
17. Hartikainen AL, Sorri M, Anttonen H, Tuimala R, Laara E. Effect of occupational noise on the course and outcome of pregnancy. Scand J Work Environ Health. Dec 1994;20(6):444-450.
18. Timmermans S, Bonsel GJ, Steegers-Theunissen RP, et al. Individual accumulation of heterogene-ous risks explains perinatal inequalities within deprived neighbourhoods. Eur J Epidemiol. 2011;26:165-180.
19. Ravelli AC, Tromp M, van Huis M, et al. Decreas-ing perinatal mortality in The Netherlands, 2000-2006: a record linkage study. J Epidemiol Community Health. 2009;63:761-765.
20. Sheldon T. Prompt access to expert care is among advice to reduce perinatal deaths in Netherlands. BMJ. 2010;340:c277.
21. Van der Velden J. Dutch report: Een goed begin. Veilige zorg rond zwangerschap en geboorte. Advies Stuurgroep Zwangerschap en Geboorte. The Hague: 2009.
REFERENCES

13
INTRO
DU
CTION
122. Bonsel GJ, Birnie E, Denktas S, Poeran J, Steegers
EAP. Dutch report: Lijnen in de Perinatale Sterfte, Signalementstudie Zwangerschap en Geboorte 2010. Rotterdam: Erasmus MC; 2010.
23. Kloosterman GJ. Intrauterine growth and in-trauterine growth curves. Maandschr Kinderge-neeskd. 1969;37:209-225.
24. Poeran J, Steegers EA, Bonsel GJ. Approach to perinatal mortality in the Netherlands: outcomes of a systematic expert study. Ned Tijdschr Geneeskd. 2012;155:A4499.
25. Denktas S, Bonsel GJ, Steegers EA. Perinatal health in Rotterdam, the Netherlands--experiences after 2 years of ‘Ready for a baby’. Ned Tijdschr Geneeskd. 2012;156:A4289.
26. Denktas S, Bonsel GJ, Van der Weg EJ, et al. An urban perinatal health programme of strategies to improve perinatal health. Matern Child Health J. 2011;16:1553-1558.
27. Posthumus AG, Scholmerich VL, Waelput AJ, et al. Bridging Between Professionals in Perinatal Care: Towards Shared Care in The Netherlands. Matern Child Health J. 2012 (in press).

14
INTRO
DU
CTION
1

PART I
Perinatal health in Rotterdam

16

2
Journal of Maternal-Fetal and Neonatal Medicine. 2011;24:643-646.
Urban perinatal health inequalities
J. Poeran, S. Denktaş, E. Birnie, G.J. Bonsel, E.A.P. Steegers

18
URBA
N PERIN
ATAL H
EALTH
INEQ
UA
LITIES
2
ABSTRACTObjective Large urban areas have higher perinatal mortality rates. In attaining a better
understanding, we conducted an analysis on a neighbourhood level in Rotterdam, the
second largest city of The Netherlands.
Methods Perinatal outcome of all single pregnancies (50,000) was analysed for the period of
2000-2006. The prevalences of perinatal mortality and perinatal morbidity were determined
for every neighbourhood.
Results Large perinatal health inequalities exist between neighbourhoods in the city of
Rotterdam with perinatal mortality rates as high as 37 per 1,000 births. The highest risks
were observed in deprived neighbourhoods.
Conclusion We observed high levels of perinatal health inequalities in the city of Rotterdam
which have not been previously described in the Western world. Accumulation of medical
risk factors as well as socio-economic and urban risk factors seems to be a likely contributor.

19
URBA
N PERIN
ATAL H
EALTH
INEQ
UA
LITIES
2
INTRODUCTIONHealth inequalities pose a complex problem in the field of public health, consisting of
medical, social and socio-economic aspects. Considering the substantial long term effects,
adverse perinatal health outcomes, along with perinatal health inequalities, are of particular
interest.1,2
In The Netherlands, perinatal mortality exceeds the European average despite a high
standard of mother and child healthcare.3,4 A recent national study showed an increased
risk of 12% on adverse perinatal outcomes in large urban areas; for non-Western women
this additional risk was 26%.3 The largest risk was observed in deprived neighbourhoods
where ethnicity was expected to be a key etiologic factor.3 However, the effect of living in
deprived neighbourhoods, as compared to living elsewhere, was most prominent among
Western women with an increased risk of 24%.3 In attaining a better understanding of this
complicated matter, we conducted an analysis on the neighbourhood level in the second
largest city of The Netherlands, i.e., the city of Rotterdam where socio-economic inequalities
are most obvious.
METHODSThe Netherlands Perinatal Registry contains population-based information of 96% of all
pregnancies in The Netherlands. Source data are collected by 95% of midwives, 99% of
gynaecologists and 68% of paediatricians (including 100% of Neonatal Intensive Care
Unit paediatricians).5 From this registry we selected perinatal outcome data of the city of
Rotterdam (587,161 inhabitants in 2009) for the period of 2000-2006 (50,000 singleton
pregnancies). The prevalence of adverse perinatal outcomes was determined for every
neighbourhood using the 4-digit zip codes as recorded in The Netherlands Perinatal Registry,
and municipal neighbourhood boundaries. Adverse perinatal outcome was defined as
the occurrence of either perinatal mortality or perinatal morbidity. Perinatal mortality
was defined as death from 22 weeks of gestational age until 7 days postpartum; perinatal
morbidity was defined as the presence (single or combined) of congenital anomalies
(list defined), small for gestational age (SGA, birthweight below the 10th percentile for
gestational age6), preterm birth (<37th week of gestation) or low Apgar score (< 7, 5 minutes
after birth). The prevalences of adverse perinatal outcomes were illustrated on a map of
Rotterdam making use of separate colours per stratum.

20
URBA
N PERIN
ATAL H
EALTH
INEQ
UA
LITIES
2
Table 2.1 Socio-demographic characteristics of the Rotterdam population (2009, top) and characteristics of the Rotterdam pregnant population along with perinatal outcomes (2000-2006, bottom)
Absolute number Percentage
General population
EthnicityWestern 373,115 64%Non-Western
Surinamese 52,206 9%Antillean 20,261 3%Turkish 46,203 8%Moroccan 38,158 6%Cape Verdean 15,103 3%Non-Western, other 42,115 7%
Socioeconomic characteristicsHaving a job 300,236 51%Dependent on social security 29,504 5%Debt settlement 4,747 1%
Composition of householdLiving alone 139,367 24%Couple without children 133,681 23%Couple with children 216,874 37%One-parent household 80,543 14%Other 16,696 3%
RESULTSTable 2.1 shows recent socio-demographic characteristics of the Rotterdam population in
2009 along with characteristics of the pregnant population from 2000-2006. During the
study period (2000-2006) there were 50,000 singleton pregnancies in the city of Rotterdam.
In almost half of these cases (49%) the mother had a non-Western background; almost
half (48%) of women were primiparous. Teenage pregnancies accounted for 4% of all
pregnancies. The geographic distribution of prevalences of perinatal mortality and perinatal
morbidity is illustrated in figure 2.1. The neighbourhood-specific perinatal mortality rates
varied from 2 to 34 per 1,000 births, for congenital anomalies from 10 to 91 per 1,000 births,
for SGA from 38 to153 per 1,000 births, for preterm birth from 34 to 157 per 1,000 births
and for low Apgar score from 4 to 37 per 1,000 births. The highest mortality rates were
observed in deprived neighbourhoods.
Table 2.1 continues on next page.

21
URBA
N PERIN
ATAL H
EALTH
INEQ
UA
LITIES
2
DISCUSSIONImpressive geographic perinatal health inequalities between neighbourhoods were
observed in the second largest city of The Netherlands. In several neighbourhoods perinatal
mortality and morbidity exceeded national levels observed well before the 1960s. The
highest risks of adverse perinatal outcomes were seen in deprived neighbourhoods,
supporting the theory of neighbourhood context as an individual risk factor for adverse
Table 2.1 Continued
Absolute number Percentage
Pregnant population
Total number of single pregnancies 50,000 100%
Neighbourhoods with <500 births 32 40%Neighbourhoods with 500-1,000 births 27 33%Neighbourhoods with >1,000 births 22 27%
EthnicityWestern 25,544 51%Non-Western 24,456 49%
General characteristicsPrimiparity 24,050 48%Teenage pregnancy 2,231 4%Maternal age >36 years 1,548 3%
Absolute number Per 1,000 births
Perinatal outcomes
Perinatal mortality 600 12Top 5 best neighbourhoods 2 2Top 5 worst neighbourhoods 53 23
Congenital abnormalities 1,333 27Top 5 best neighbourhoods 44 13Top 5 worst neighbourhoods 80 63
Small for gestational age 4,704 94Top 5 best neighbourhoods 92 47Top 5 worst neighbourhoods 378 118
Preterm birth 3,865 77Top 5 best neighbourhoods 84 47Top 5 worst neighbourhoods 204 119
Apgar score <7, 5 minutes after birth 1,221 24Top 5 best neighbourhoods 9 5Top 5 worst neighbourhoods 145 36

22
URBA
N PERIN
ATAL H
EALTH
INEQ
UA
LITIES
2
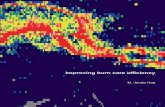
Figure 2.1 Neighbourhood inequalities in perinatal health in Rotterdam: perinatal mortality rates (top) and adverse perinatal outcome rates (bottom), both per 1000 births (2000-2006); yellow lines indicate highways.

23
URBA
N PERIN
ATAL H
EALTH
INEQ
UA
LITIES
2
perinatal outcomes. This may be due to various reasons (single or combined), e.g., stress
due to unsafety or noise, environmental hazards (petrochemical industry, traffic pollution),
and/or healthcare deficits (restricted healthcare access and insufficient healthcare
performance).3,7,8
Ethnicity is an important risk factor for adverse perinatal outcomes.9,10 However, to under-
stand perinatal health patterns in large cities, urban and socio-economic risk factors should
also be considered.7 In particular, the accumulation of risk factors in urban communities
may explain such perinatal health inequalities as studied in large cohort studies in the cities
of Rotterdam (‘Generation R’)10 and Amsterdam (‘ABCD’)7,9. Medical and non-medical risk
factors may synergistically increase the risk of adverse perinatal outcomes to a far greater
extent than can be explained by their individual etiologic contributions.
Some methodological issues should be discussed. The high number of pregnancies in the
7-year study period minimises the effect of yearly fluctuation of neighbourhood prevalences
of adverse perinatal outcomes. As the risk of perinatal outcomes differs significantly
between multiple and singleton pregnancies, only singleton pregnancies were studied.
The Netherlands Perinatal Registry has a high degree of coverage of all pregnancies in The
Netherlands (96% of all pregnancies are registered), another factor which augments the
validity of our findings.
The usage of 4-digit zip codes allowed a clear illustration of the perinatal health inequalities
between neighbourhoods. The disadvantage of using 4-digit zip codes is the great variety
in neighbourhood size, expressed in geographical size as well as the number of inhabitants.
Consequently, there is a risk of overestimating or underestimating the prevalence of rare
adverse perinatal outcomes in small neighbourhoods. To minimise this effect we aggregated
neighbourhood prevalences into two large groups of outcomes: perinatal mortality and
perinatal morbidity.
To our knowledge, the observed degree of perinatal health inequalities has not been
previously described in other Western cities. Considering the substantial long term health
effects of perinatal morbidity for individuals and generations to come, we feel that these
findings warrant further investigation and also should be given priority on the public health
agenda as it is very likely that similar problems exist in comparable settings.

24
URBA
N PERIN
ATAL H
EALTH
INEQ
UA
LITIES
2
REFERENCES1. Barker DJ. Adult consequences of fetal growth
restriction. Clin Obstet Gynecol. 2006;49:270-83.
2. Moster D, Lie RT, Markestad T. Long-term medical and social consequences of preterm birth. N Engl J Med. 2008;359:262-73.
3. Graaf JP de, Ravelli AC, Wildschut HI, et al. Perinatal outcomes in the four largest cities and in deprived neighbourhoods in The Netherlands. Ned Tijdschr Geneeskd. 2008;152:2734-40.
4. Mohangoo AD, Buitendijk SE, Hukkelhoven CW, et al. Higher perinatal mortality in The Netherlands than in other European countries: the Peristat-II study. Ned Tijdschr Geneeskd. 2008;152:2718-27.
5. Perinatal care in The Netherlands 2006 (in Dutch: Perinatale zorg in Nederland 2006). Utrecht: The Netherlands Perinatal Registry; 2008.
6. Kloosterman GJ. On intrauterine growth. Int J Gynaecol Obstet. 1970;8:895-912.
7. Agyemang C, Vrijkotte TG, Droomers M, van der Wal MF, Bonsel GJ, Stronks K. The effect of neighbourhood income and deprivation on pregnancy outcomes in Amsterdam, The Netherlands. J Epidemiol Community Health. 2009;63:755-60.
8. de Medeiros AP, Gouveia N, Machado RP, et al. Traffic-related air pollution and perinatal mortality: a case-control study. Environ Health Perspect. 2009;117:127-32.
9. Goedhart G, van Eijsden M, van der Wal MF, Bonsel GJ. Ethnic differences in preterm birth and its subtypes: the effect of a cumulative risk profile. BJOG. 2008;115:710-9.
10. Troe EJ, Raat H, Jaddoe VW, et al. Explaining differences in birthweight between ethnic populations. The Generation R Study. BJOG. 2007;114:1557-65.

3
Tijdschrift voor Gezondheidswetenschappen. 2012;90:496-503. (Article in Dutch, translated into English for this thesis)
Pregnancy and birth in Rotterdam: a local health report
J. Poeran, S. Denktaş, E. Birnie, H.J. van der Weg, A.J.J. Voorham, E.A.P. Steegers, G.J. Bonsel

26
PREGN
AN
CY AN
D BIRTH
IN RO
TTERDA
M: A
LOCA
L HEA
LTH REPO
RT
3
ABSTRACTWithin The Netherlands, the city of Rotterdam has high rates of perinatal mortality and
morbidity (congenital anomalies, preterm birth, small for gestational age, low Apgar score:
so-called ‘Big4’ morbidities). Following this observation, the municipality of Rotterdam
initiated an elaborate public health initiative to reduce perinatal mortality and morbidity.
This initiative, ‘Ready for a Baby’, is a collaboration between the municipality, the academic
medical centre (Erasmus MC) and the local public health authorities (GGD Rotterdam
Rijnmond). The main target is to decrease perinatal mortality and ‘Big4’ morbidities in
Rotterdam. An important first step was the measuring of baseline perinatal health in the
city of Rotterdam. Data were derived from The Netherlands Perinatal Registry for the period
2000-2007 (n=56,443 singleton pregnancies). We looked at prevalences, absolute and
standardised (for parity, maternal age, ethnicity and socioeconomic status), of perinatal
mortality and ‘Big4’ morbidities within the several boroughs of Rotterdam. Additionally,
we looked at socio-demographics and healthcare related factors. Large differences in
perinatal mortality and morbidity exist between boroughs in the city of Rotterdam, with
most likely different causes per borough. In some boroughs healthcare related factors
and environmental factors play an important role while in other boroughs characteristics
of the pregnant women, e.g., lifestyle or ethnicity are more important causes. These data
are crucial in the development of policies specifically targeted to the several boroughs to
decrease perinatal morbidity and mortality within the city of Rotterdam.

27
PREGN
AN
CY AN
D BIRTH
IN RO
TTERDA
M: A
LOCA
L HEA
LTH REPO
RT
3
INTRODUCTIONA recent Dutch study showed women in the four largest cities of The Netherlands to be
at increased risk for perinatal mortality and related perinatal morbidity.1,2 In particular,
Rotterdam has high rates of perinatal mortality and preceding perinatal morbidity, the
most important being congenital anomalies, preterm birth (<37 weeks’ gestation), small for
gestational age (SGA, birthweight <p10) and a so-called low Apgar score, 5 minutes after
birth.3 Due to their importance in perinatal mortality (they precede 85% of perinatal mortality)
we refer to these four precursor morbidities as ‘Big4’. In 2008, following the observations in
the city of Rotterdam, the municipal authorities started an elaborate public health initiative
in collaboration with the academic medical centre (Erasmus MC) and the local public health
authority (GGD Rotterdam Rijnmond): the ‘Ready for a Baby’ programme (in Dutch: Klaar
voor een Kind, see www.klaarvooreenkind.nl). The aim of this 10-year initiative is to reduce
perinatal mortality and perinatal morbidity in the city of Rotterdam to the national level.4,5
The first step in this initiative was to thoroughly record perinatal mortality, morbidity, and
their attributing factors in Rotterdam. These attributing factors can pertain to the pregnant
women (e.g., smoking, folic acid use or ethnicity), their environment (e.g., neighbourhood
social quality or environmental pollution), or they can be related to healthcare (e.g., access
to care or availability of facilities). However, as these factors are not registered as such, we
defined several indicators (which could be derived from existing data) to approximate
the separate role of patient, healthcare and environment related risk factors for adverse
perinatal outcome.3 Depending on the role of these specific indicators, neighbourhood- and
risk factor-specific policy will be possible within the city of Rotterdam.6,7 This approach is
analogous to the national ‘Public Health Forecast’ reports (‘VTV’) by the National Institute for
Public Health and the Environment (‘RIVM’).8 This manuscript describes the used methods
and includes a small selection from the Rotterdam borough reports on perinatal health.
These reports have been discussed in the Rotterdam municipal council in 2011 as well as
the borough councils, and are now publicly available.6
METHODS
The Netherlands Perinatal Registry
Data regarding the indicators (socio-demographics, healthcare related and perinatal
outcome) were derived from The Netherlands Perinatal Registry (www.perinatreg.nl),

28
PREGN
AN
CY AN
D BIRTH
IN RO
TTERDA
M: A
LOCA
L HEA
LTH REPO
RT
3
containing complete population-based information of >97% of all pregnancies in The
Netherlands. Source data are routinely collected by 94% of midwives, 99% of gynaecologists
and 68% of paediatricians including 100% of Neonatal Intensive Care Unit paediatricians.
Data were available for 2000-2007; only singleton pregnancies were included.
Indicators
Perinatal outcome
The most important outcome indicators were perinatal morbidity and perinatal mortality.
The former comprised the ‘Big4’ morbidities (congenital anomalies, SGA, preterm birth
and low Apgar score). Congenital anomalies are recorded postpartum and classified
through a standard coding system by organ system (8 categories, 71 subcategories, see
www.perinatreg.nl). Preterm birth is defined as birth before 37 weeks of gestational age;
small for gestational age (SGA) is defined as a birthweight below the 10th percentile for
gestational age. An Apgar score is a 0-10 score based on complexion, pulse rate, reflex
irritability, muscle tone and breathing; a low Apgar score is defined as <7, 5 minutes after
birth. Perinatal mortality is the sum of fetal mortality (intrauterine death from 22 weeks of
gestational age) and early neonatal mortality (death in the first 7 days after birth).
Healthcare related indicators
Healthcare related indicators included in the borough reports refer to: (1) the proportion
of women with a late first antenatal booking visit (after 14 weeks of gestational age), and
(2) the level of care at start of labour (primary care under supervision of a community
midwife, or secondary/tertiary care under supervision of an obstetrician). Women with
a late antenatal booking visit will not fully benefit from healthy lifestyle advices during
pregnancy, concerning an optimal pregnancy outcome. Moreover, due to their gestational
age, these women are not able to participate in first trimester screening for chromosomal
anomalies, mainly Down syndrome. Also, ultrasound determination of gestational age is less
precise after the first trimester; this will result in a less precise due date and the definition
of a possible preterm birth.3,9 The second indicator refers to the unique system of obstetric
care in The Netherlands. This system is characterised by risk-based levels of care: primary
care for low risk pregnancies, provided by independently practicing community midwives,
and secondary/tertiary care for high risk pregnancies provided by obstetricians. Through
risk selection, this distinction between assumed low risk and high risk pregnancies is
made by primary care community midwives. Therefore, the proportion of women starting
labour in primary care (supposedly low risk) is an important healthcare related indicator.

29
PREGN
AN
CY AN
D BIRTH
IN RO
TTERDA
M: A
LOCA
L HEA
LTH REPO
RT
3
We used the prevalence of ‘Big4’ as an indicator of high risk pregnancy. Based on the ‘Big4’
prevalence per borough, an estimation can be made on the expected proportion of women
starting labour in primary care and the degree to which high risk pregnancies are detected
and referred, e.g., high ‘Big4’ prevalence with low proportion of women starting labour in
primary care may refer to adequate risk selection.
Demographics
Demographic indicators pertain to ethnicity (Western, non-Western), and maternal age
(<20 years, >35 years). Non-Western women are at increased risk for adverse pregnancy
outcome including perinatal mortality.1 This increased risk also regards pregnant women
outside the range of maternal age 20-35 years.10,11
Other
The other indicators refer to parity (primiparous / multiparous) and the environment of the
pregnant woman (neighbourhood social quality as measured by a composite indicator).
Both indicators are associated with perinatal outcome, including perinatal mortality.1,3
‘Deprived neighbourhood’ was defined as having a ‘Social Index’ score of <6. The ‘Social
Index’ (SI) is a composite 0-10 measure indicating neighbourhood social quality as annually
determined by the Rotterdam Centre for Research and Statistics (see www.cos.rotterdam.
nl). The SI is only available for the city of Rotterdam, but is preferred over the less refined
national ‘yes / no deprived neighbourhood’ variable based on 4-digit zip codes and an
official public list of 40 deprived zip code based neighbourhoods.12,13 Moreover, this national
variable indicates some Rotterdam neighbourhoods as ‘non-deprived’ while their Social
Index score indicates otherwise.
Geographics
In the study period, the city of Rotterdam consisted of 13 boroughs (in March 2010, a 14th
was added, Rozenburg). These boroughs were defined based on 4-digit postal code areas, the
lowest level of aggregation in The Netherlands Perinatal Registry. Next to using crosstabs,
we also illustrated outcomes per borough on a map of Rotterdam, using shades of red to
indicate outcome levels (figure 3.1, the darker the shade the more negative the outcome).
Maps were constructed using ESRI® ArcGIS version 9.3 (Environmental Systems Research
Institute, Inc., USA). Geographic information was obtained from the Rotterdam municipal
services. Due to the availability of data from 8 years (2000-2007) we could avoid too small
numbers of pregnancies per geographic area.

30
PREGN
AN
CY AN
D BIRTH
IN RO
TTERDA
M: A
LOCA
L HEA
LTH REPO
RT
3
Standardisation
In comparing indicators between the 13 boroughs, differences in socio-demographics have
to be taken into account as they have an effect on perinatal outcome, e.g., a borough with
a high number of non-Western women, a high number of teenage pregnancies, or women
from neighbourhoods with a low Social Index, will generally have a higher prevalence
of adverse perinatal outcomes. To make an ‘honest’ comparison between the boroughs,
differences in socio-demographics have to be accounted for. Standardisation is a method to
account for this. With ‘direct standardisation’ the ‘expected’ outcome levels per borough are
calculated for the scenario that the concerning borough has the same socio-demographic
composition (by maternal age, parity, Social Index and ethnicity) as the whole city of
Rotterdam. Persisting differences in outcome after standardisation, may be attributable to
Figure 3.1 Perinatal mortality (per 1,000 births) in the 13 boroughs of Rotterdam. Rotterdam average 11.5 per 1,000 births. National average 9.7 per 1,000 births. Names of boroughs are abbreviated: HH Hoek van Holland, OV Overschie, HS Hillegersberg-Schiebroek, AL Prins Alexander, NO Noord, DE Delfshaven, CE Stadscentrum, KR Kralingen-Crooswijk, HO Hoogvliet, PE Pernis, CH Charlois, FE Feijenoord, YS IJsselmonde.
HH
OVHS AL
DE
NOKR
CE
YSFECH
CH
HO
PE
HARBOUR OFROTTERDAM

31
PREGN
AN
CY AN
D BIRTH
IN RO
TTERDA
M: A
LOCA
L HEA
LTH REPO
RT
3
other factors (than socio-demographics) such as quality of healthcare or local health policies.
The most important limitation of standardisation is that it implies that the standardisation
factors (in this case maternal age, parity, Social Index and ethnicity) are non-modifiable. In
other words: the effect of these four standardisation factors is disregarded when looking
only at standardised figures. Another important limitation refers to boroughs differing
greatly (compared to the whole city of Rotterdam) in socio-demographic composition, with
accompanying large expected differences in perinatal outcomes. Standardisation might
moderate these significant differences seen in absolute outcomes. Therefore, both crude and
standardised outcomes are important to observe. The technique of direct standardisation
is described in more detail elsewhere.14
Selection from the borough reports
As the borough reports are extensive we included only a selection in this manuscript to
illustrate the most important conclusions. Both crude and standardised rates are included
in the borough reports.6 The selection for this manuscript pertains to:
• crude (absolute, unstandardised) perinatal mortality and ‘Big4’ prevalence per borough
(table 3.1);
• crude perinatal mortality per borough visualised on a map of Rotterdam (figure 3.1);
• crude and standardised indicator rates compared for two boroughs (Hoogvliet and
Overschie, table 3.2). These boroughs were chosen to illustrate that factors attributing to
perinatal mortality (increased in both boroughs) are thought to differ for each borough.
RESULTS
Overview
There were 56,443 singleton pregnancies in the study period (2000-2007) in the city of
Rotterdam. Table 3.1 and figure 3.1 illustrate crude perinatal mortality (per 1,000 births) for
each borough. Additionally, table 3.1 shows crude ‘Big4’ prevalence per borough. Perinatal
mortality varies from 3.4 (Hoek van Holland) per 1,000 births to 21.1 (Pernis) per 1,000 births.
‘Big4’ prevalence varied from 140.6 (Hillegersberg-Schiebroek) per 1,000 births to 205.7
(Charlois) per 1,000 births.

32
PREGN
AN
CY AN
D BIRTH
IN RO
TTERDA
M: A
LOCA
L HEA
LTH REPO
RT
3
Rotterdam compared to The Netherlands
Table 3.2 provides an overview of the indicators for The Netherlands, Rotterdam, and two
boroughs (Hoogvliet and Overschie). The first two columns (‘A’ and ‘B’) compare the indicators
for The Netherlands with Rotterdam. Columns 3 to 6 refer to the borough of Hoogvliet;
columns 7 to 10 refer to the borough of Overschie.
The first two columns illustrate a higher perinatal mortality for Rotterdam compared to The
Netherlands (11.5 compared to 9.7 per 1,000 births, respectively). Also, ‘Big4’ prevalence
is higher in Rotterdam (181.1 compared to 152.7 per 1,000 births in The Netherlands).
Rotterdam also has a higher proportion of women with a late antenatal booking visit (36.1%
compared to 20.7% for The Netherlands), and a higher proportion of non-Western women
(48.7% compared to 16.2%).
Comparing boroughs: Hoogvliet
Column 3 (‘C’) from table 3.2 shows crude rates for the borough of Hoogvliet. The proportional
change compared to the crude rates for Rotterdam (‘B’) is shown in the 4th column (‘C-B’).
In particular preterm birth (+38.3%) and low Apgar score (+34.0%) are increased in the
Table 3.1 Perinatal mortality (†) and ‘Big4’ per 1,000 births, for The Netherlands, Rotterdam and the Rotterdam boroughs
Geographic area † ‘Big4’
The Netherlands 9.7 152.7Rotterdam 11.5 181.1
BoroughsCharlois 13.3 205.7Delfshaven 13.3 192.8Feijenoord 11.3 181.1Hillegersberg-Schiebroek 7.6 140.6Hoek van Holland 3.4 181.8Hoogvliet 12.5 203.5IJsselmonde 10.3 184.4Kralingen-Crooswijk 12.0 178.6Noord 8.9 174.3Overschie 16.3 185.7Pernis 21.1 165.7Prins Alexander 12.8 168.6Stadscentrum 13.1 171.3

33
PREGN
AN
CY AN
D BIRTH
IN RO
TTERDA
M: A
LOCA
L HEA
LTH REPO
RT
3
Ta
ble
3.2
In
dica
tors
list
ed fo
r tw
o bo
roug
hs, H
oogv
liet a
nd O
vers
chie
. Str
ongl
y de
viat
ing
leve
ls a
re c
olou
red
to e
nhan
ce in
terp
reta
tion*
.
Boro
ugh
of H
oogv
liet
Boro
ugh
of O
vers
chie
NLD
SRD
AM
ABS
CRU
Δ%
STN
STN
Δ%
ABS
ABS
Δ%
STN
STN
Δ%
Indi
cato
rA
BC
C-B
DC-
DE
E-B
FE-
F
Pe
rin
ata
l o
utc
om
e (
pe
r 1
,00
0)
Cong
enita
l ano
mal
ies
27.0
26.4
21.4
-19.
0%25
.8-1
7.1%
27.6
4.8%
27.0
2.2%
Pret
erm
birt
h61
.569
.295
.738
.3%
67.9
41.0
%75
.89.
5%70
.57.
6%Sm
all f
or g
esta
tiona
l age
71.5
93.1
89.9
-3.4
%82
.68.
9%93
.60.
5%91
.12.
6%Lo
w A
pgar
sco
re11
.515
.020
.034
.0%
13.0
54.5
%14
.2-5
.2%
14.6
-2.7
%To
tal '
Big4
' mor
bidi
ties
152.
718
1.1
203.
512
.4%
169.
320
.2%
185.
72.
5%18
0.9
2.7%
Perin
atal
mor
talit
y9.
711
.512
.58.
4%10
.320
.9%
16.3
41.8
%11
.344
.2%
Feta
l mor
talit
y6.
98.
38.
52.
5%7.
316
.6%
13.5
63.1
%8.
166
.5%
Early
neo
nata
l mor
talit
y2.
83.
24.
023
.6%
3.1
31.3
%2.
8-1
2.6%
3.2
-11.
8%
He
alt
hca
re r
ela
ted
(%
)
Ant
enat
al b
ooki
ng a
t >14
wee
ks20
.7%
36.1
%36
.0%
-0.3
%27
.5%
31.0
%23
.8%
-34.
1%32
.6%
-27.
1%St
art l
abou
r in
prim
ary
care
49.0
%47
.6%
20.3
%-5
7.4%
46.1
%-5
6.0%
57.4
%20
.4%
47.0
%22
.1%
Pre
gn
an
t p
op
ula
tio
n (
%)
Non
-Wes
tern
wom
en16
.2%
48.7
%36
.6%
-24.
9%N
/AN
/A36
.8%
-24.
4%N
/AN
/AW
este
rn te
ens
1.2%
2.9%
2.9%
-0.5
%N
/AN
/A1.
7%-4
0.6%
N/A
N/A
Non
-Wes
tern
teen
s4.
3%5.
8%6.
9%18
.7%
N/A
N/A
5.2%
-11.
1%N
/AN
/AW
este
rn 3
5+ y
ears
old
20.4
%22
.0%
17.8
%-1
9.1%
N/A
N/A
22.9
%3.
8%N
/AN
/AN
on-W
este
rn 3
5+ y
ears
old
16.6
%14
.8%
15.1
%2.
3%N
/AN
/A12
.5%
-15.
1%N
/AN
/A
Oth
er
(%)
Prim
ipar
ous
wom
en46
.1%
48.0
%44
.6%
-7.1
%N
/AN
/A49
.2%
2.4%
N/A
N/A
Nei
ghbo
urho
od S
ocia
l Ind
ex <
6.0
N/A
58.3
%0.
0%-1
00.0
%N
/AN
/A49
.7%
-14.
8%N
/AN
/A
-5
% to
-10%
m
ore
than
-10%
+5
% to
+10
%
+10%
to +
15%
m
ore
than
+10
%
* Sh
ades
of g
reen
repr
esen
t a p
ositi
ve d
evia
tion;
yel
low
, ora
nge
and
red
repr
esen
t a n
egat
ive
devi
atio
n. C
olou
r cod
ing
is n
ot u
sed
for ‘
the
prop
ortio
n of
wom
en st
artin
g la
bour
in p
rimar
y ca
re’ a
s th
ere
is n
o ne
gativ
e or
pos
itive
judg
men
t pos
sibl
e w
ithou
t tak
ing
into
acc
ount
oth
er fa
ctor
s su
ch a
s an
tena
tal r
isk
load
(‘Bi
g4’).

34
PREGN
AN
CY AN
D BIRTH
IN RO
TTERDA
M: A
LOCA
L HEA
LTH REPO
RT
3
borough of Hoogvliet (compared to Rotterdam). On the other hand, congenital anomalies
are decreased (-19.0%). The perinatal mortality rate (12.5 per 1,000 births) is increased
compared to Rotterdam (+8.4%); mainly due to an increase in early neonatal mortality
(+23.6%). Another notable finding is that there is a smaller proportion of women starting
labour in primary care under the supervision of a primary care community midwife (-57.4%).
Also, the Hoogvliet population differs greatly from the Rotterdam population with less
non-Western pregnant women (-24.9%) in Hoogvliet, but an increased proportion of non-
Western pregnant teens (+18.7%). There are no neighbourhoods with a low Social Index
score (<6) in this borough.
Column 5 (‘D’) shows standardised rates for Hoogvliet; column 6 (‘C-D’) shows the comparison
between the crude (‘C’) and standardised (‘D’) rates. Except for congenital anomalies
(-17.1%) all adverse perinatal outcomes have a higher prevalence than expected based on
standardisation, in particular preterm birth (+41.0%), low Apgar score (+54.5%) and early
neonatal mortality (+31.3%). Furthermore, the proportion of women with a late antenatal
first booking is higher (+31.0%) than would be expected based on standardisation. By
contrast, the proportion of women starting labour in primary care is lower (-56.0%) than
expected.
Comparing boroughs: Overschie
Analogous to the rates for Hoogvliet, columns 7 (‘E’) and 8 (‘E-B’) from table 3.2 show crude
rates for the borough of Overschie (column 7) and the proportional difference with the
crude Rotterdam rates (column 8). Crude differences with Rotterdam are relatively small
for separate ‘Big4’ prevalences with a maximum difference of +9.5% for preterm birth.
However, relative perinatal mortality is increased (+41.8%), mainly due to an increased fetal
mortality (+63.1%). The proportion of women with a late antenatal booking visit is lower
(-34.1%) compared to Rotterdam. However, a greater proportion of women start labour in
primary care (+20.4%). Also notable is the decreased proportion of non-Western pregnant
women in Overschie (-24.4%), and also less pregnant women living in a neighbourhood
with a low Social Index (<6, -14,8%). Columns 9 (‘F’) and 10 (‘E-F’) show standardised rates
and their comparison with crude rates, respectively. Standardised ‘Big4’ rates do not differ
much compared to the crude rates for this borough, similar to the crude differences with
Rotterdam as shown in the ‘E-B’ column. Again, perinatal mortality is higher (+44.2%), the
proportion of women with a late antenatal booking is lower (-27.1%), and the proportion
of women starting labour in primary care is higher (+22,1%).

35
PREGN
AN
CY AN
D BIRTH
IN RO
TTERDA
M: A
LOCA
L HEA
LTH REPO
RT
3
DISCUSSIONIn Rotterdam, large differences exist in crude and standardised perinatal mortality and ‘Big4’
rates between boroughs. Next to differences in outcome, there are also large differences
in socio-demographics and healthcare related factors. The Rotterdam borough reports
on perinatal health provide possible explanations on borough-specific backgrounds on
increased perinatal mortality or ‘Big4’ prevalence, e.g., maternal or child factors such as
primiparity or having a SGA baby, healthcare related factors such as a suboptimal selection
(and referral) of high risk pregnancies, or environment related factors such as living in a
deprived neighbourhood.
The comparison between the boroughs of Hoogvliet and Overschie showed an increased
perinatal mortality in both boroughs, however, with large differences in ‘Big4’ prevalence,
healthcare related factors and the proportion of non-Western pregnant women. What
particularly stands out is the highly increased perinatal mortality without an expected
increased ‘Big4’ prevalence (as precursors of perinatal mortality) in Overschie. This suggests
a small role of ‘Big4’ morbidities in the increased perinatal mortality shifting the focus to
other causes such as healthcare related factors or environment related factors. The borough
of Hoogvliet has relatively high ‘Big4’ rates accompanied by a strongly increased perinatal
mortality. This suggests a high antenatal risk level, caused by precursors of ‘Big4’, e.g.,
smoking during pregnancy. In addition, the high early neonatal mortality (death after a
live birth) suggests suboptimal healthcare related factors around birth.
The differences between crude and standardised rates indicate different backgrounds
on perinatal health per borough. These differences are more pronounced in the borough
reports on perinatal health as all boroughs are described and compared.6 In some boroughs
healthcare related factors and environment are the main contributors, while in other
boroughs mainly characteristics of the pregnant women are the main contributors (e.g.,
ethnicity or lifestyle factors such as smoking).
Comparable initiatives
‘Urban perinatal health’ is a relatively new field within Obstetrics and Public Health, gaining
a lot of attention in The Netherlands. This is readily illustrated by a comparable urban
perinatal health report for the city of Amsterdam.15 The Amsterdam report also concludes
that effects of risk factors for perinatal mortality differ per borough, advising differential
policies per borough. An important difference, compared to the Rotterdam report, is the
absence of standardisation.

36
PREGN
AN
CY AN
D BIRTH
IN RO
TTERDA
M: A
LOCA
L HEA
LTH REPO
RT
3
International initiatives pertaining to urban or inner-city perinatal health also exist.16-18
Even though these initiatives are comparable on some points with the Rotterdam and
Amsterdam initiatives, there are mostly large differences. In the United Kingdom, for
example, there are more (reliable) data available on smoking during pregnancy, one of the
most important lifestyle factors in the context of adverse perinatal outcome.19 Data from
The Netherlands Perinatal Registry underestimate the actual smoking prevalence as this
is poorly registered by the caregivers. In addition, the UK studies use larger geographical
areas, with also outcomes being studied per practice or hospital.16-18 Another important to
mention difference refers to the unique system of obstetric care in The Netherlands which
significantly differs from systems in other Western countries.
Cumulation of risks
An important subject in the UK reports is the connection between adverse perinatal
outcome and social deprivation, a specific characteristic of large urban areas.16-18 Indeed, a
large body on literature exists on the association between social deprivation and adverse
perinatal outcome.20-22 Mostly, the effect of social deprivation on low birthweight / SGA,
preterm birth and perinatal mortality is described.20-22 Also, de Graaf et al. describe an
increased perinatal mortality and ‘Big4’ in socially deprived neighbourhoods in the context
of The Netherlands.1 A particular finding in this study is that specifically Western women
appeared at increased risk in socially deprived neighbourhoods. In Rotterdam, this translated
into a 24% increased risk for adverse perinatal outcome for Western women compared to
non-Western women in socially deprived neighbourhoods.1
Another Dutch study in this context was conducted by Timmermans and colleagues.22
They used data from the Rotterdam ‘Generation R’ cohort and concluded that deprived
neighbourhoods are characterised by a cumulation of risk factors which drives the adverse
perinatal outcomes in these neighbourhoods.22 Numerous risk factors may be responsible
for affecting perinatal health, specific for deprived areas are factors such as feelings of stress
due to unsafety or noise pollution, physical environment (e.g., industry, traffic), or problematic
(access to) healthcare.7,20,22-25 In order to gain insight in the background of urban perinatal
health and specific intervention policies in this context, the full range of urban perinatal
risk factors has to be taken into account; medical as well as non-medical (deprivation,
psychosocial, etc.) risk factors.20,26 Large cohort studies such as ‘Generation R’ in Rotterdam27
and ‘ABCD’ in Amsterdam20,28 have resulted in knowledge on numerous risk factors. Outcomes
of these studies are crucial in understanding perinatal health in the city of Rotterdam.

37
PREGN
AN
CY AN
D BIRTH
IN RO
TTERDA
M: A
LOCA
L HEA
LTH REPO
RT
3
The ‘Ready for a Baby’ programme
The large differences in borough profiles suggest borough-specific policies in which
collaborations between caregivers are crucial. Spread out across the country there are
currently numerous regional ‘obstetric collaborations’ between midwives and obstetricians
in the same region. At-risk pregnant women are systematically discussed in these
collaborations. Next to just midwives and obstetricians, it is also crucial to collaborate with
other caregivers in the chain of obstetric healthcare (e.g., youth healthcare physicians,
paediatricians or maternity care professionals).
In the municipal public health programme ‘Ready for a Baby’ experiments in healthcare
are conducted aimed to improve communication and collaboration between caregivers
in the chain of obstetric healthcare (see www.klaarvooreenkind.nl).4,5,29 One of the most
important projects is the so called ‘R4U’ project. ‘R4U’ stands for Rotterdam Reproductive
Risk Reduction; it is a scorecard which scores medical and non-medical (e.g., psychosocial)
risk factors in a standardised way at first antenatal booking visit. This project goes beyond
just screening and subsequently links care pathways to specific risk factors, thus enhancing
collaboration. Other initiatives within the ‘Ready for a Baby’ programme are:
• implementation of and research with a new instrument (‘GyPsy’)29 to screen for psycho-
pathology during pregnancy;
• the construction of within-hospital birth centres (opening in October 2009 and March
2011), a place where women can deliver in a safe home-like primary care setting under
supervision of a primary care community midwife;
• extensive education on preconception care aimed at specific groups at risk, e.g., ethnic
minorities;
• strategies to improve communication in the transfer of care from obstetric care to youth
healthcare.
The effect of these initiatives will become apparent in the coming years by continuous
monitoring of perinatal health in the city of Rotterdam.
Conclusion
Within the city of Rotterdam, large differences in perinatal mortality and morbidity (‘Big4’)
exist between boroughs in the city of Rotterdam, with most likely different causes per
borough. In some boroughs healthcare related factors and environmental factors play

38
PREGN
AN
CY AN
D BIRTH
IN RO
TTERDA
M: A
LOCA
L HEA
LTH REPO
RT
3
an important role while in other boroughs characteristics of the pregnant women, e.g.,
lifestyle or ethnicity are more important causes. These data are crucial in the development
of policies specifically targeted to the several boroughs and aimed at decreasing perinatal
morbidity and mortality within the city of Rotterdam.
REFERENCES1. de Graaf JP, Ravelli AC, Wildschut HI, et al. Perinatal
outcomes in the four largest cities and in deprived neighbourhoods in The Netherlands. Ned Tijdschr Geneeskd. 2008;152:2734-40.
2. Steegers EAP, De Graaf JP, Laudy JAM, et al. Recht op een goede start. Medisch Contact. 2008;63:100-1.
3. Bonsel GJ, Birnie E, Denktas S, Poeran J, Steegers EAP. Lijnen in de Perinatale Sterfte, Signale-mentstudie Zwangerschap en Geboorte 2010. Rotterdam: Erasmus MC, 2010. (Dutch report on perinatal research prioritisation).
4. Denktas S, Voorham T, Bonsel GJ, et al. Grootste-delijke perinatale gezondheid. Programmatische aanpak van perinatale sterfte in Rotterdam. TSG, 2009; 87: 199-202.
5. Denktas S, Bonsel GJ, Van der Weg EJ, et al. An Urban Perinatal Health Programme of Strategies to Improve Perinatal Health. Matern Child Health J. 2011;16:1553-8.
6. Poeran J, Birnie E, Denktaş S, Steegers EAP, Bonsel GJ. Perinatale gezondheid in Rotterdam. Rotterdam: Erasmus MC, 2011. (Online: http://www.bds.rotterdam.nl/dsresource?objectid=214373) (Rotterdam borough reports on perinatal health).
7. Poeran J, Denktas S, Birnie E, Bonsel GJ, Steegers EA. Urban perinatal health inequalities. J Matern Fetal Neonatal Med. 2011;24:643-6.
8. Van der Lucht F, Polder JJ. Van gezond naar beter: Kernrapport van de Volksgezondheid Toekomst Verkenning 2010. Rijksinstituut voor Volksgezondheid en Milieu; Bilthoven 2010. (online: http://www.vtv2010.nl/object_binary/o9196_RIVM-01-Kernrapport-Van-gezond-naar-beter-VTV-2010.pdf).
9. Chote AA, Koopmans GT, Redekop WK, et al. Explaining ethnic differences in late antenatal care entry by predisposing, enabling and need factors in The Netherlands. The Generation R Study. Matern Child Health J. 2011;15:689-99.
10. Olausson PM, Cnattingius S, Goldenberg RL. Determinants of poor pregnancy outcomes among teenagers in Sweden. Obstet Gynecol. 1997;89:451-7.
11. Cleary-Goldman J, Malone FD, Vidaver J, et al. Impact of maternal age on obstetric outcome. Obstet Gynecol. 2005;105:983-90.
12. Website Ministry of Housing, Spatial Planning and the Environment. Subject ‘Aandachtswijken’ (on-line: http://www.rijksoverheid.nl/onderwerpen/aandachtswijken?#ref-vrom).
13. Gent, van WPC. Realistic regeneration -housing contexts and social outcomes of neighbourhood interventions in Western European cities-; chapter 4. Thesis 2009, University of Amsterdam. (online available: http://dare.uva.nl/document/153004).
14. Roalfe AK, Holder RL, Wilson S. Standardisation of rates using logistic regression: a comparison with the direct method. BMC Health Serv Res. 2008;8:275.
15. Ravelli AC, Steegers EA, Rijninks-van Driel GC, et al. Perinatale sterfteverschillen in Amsterdam. Ned Tijdschr Geneeskd. 2011;155:A3130.
16. Improving maternity care in London: A framework for developing services. National Health Service: London 2011. (online: http://www.londonhp.nhs.uk/wp-content/uploads/2011/03/Improving-maternity-care-in-London_A-framework-for-developing-services.pdf ).
17. Elsheikh A, Malik A, Gardosi J. West Midlands Perinatal & Infant Mortality 2008/9. West Midlands Perinatal Institute; Birmingham 2010. (online: http://www.perinatal.nhs.uk/pnm/KHD_2008-9.pdf ).

39
PREGN
AN
CY AN
D BIRTH
IN RO
TTERDA
M: A
LOCA
L HEA
LTH REPO
RT
3
18. Martin T, Gardosi J. Birmingham and The Black Country: Reducing Perinatal Mortality Project, interim report. National Health Service; Birmingham 2007. (online: http://www.perinatal.nhs.uk/rpnm/B&BC_RPM_Project_Interim_Report.pdf ).
19. Andres RL, Day MC. Perinatal complications associated with maternal tobacco use. Semin Neonatol. 2000;5:231-41.
20. Agyemang C, Vrijkotte TG, Droomers M, van der Wal MF, Bonsel GJ, Stronks K. The effect of neighbourhood income and deprivation on pregnancy outcomes in Amsterdam, The Netherlands. J Epidemiol Community Health. 2009;63:755-60.
21. Auger N, Giraud J, Daniel M. The joint influence of area income, income inequality, and immigrant density on adverse birth outcomes: a population-based study. BMC Public Health. 2009;9:237.
22. Timmermans S, Bonsel GJ, Steegers-Theunissen RP, et al. Individual accumulation of heterogeneous risks explains perinatal inequalities within deprived neighbourhoods. Eur J Epidemiol. 2011;26:165-80.
23. de Medeiros AP, Gouveia N, Machado RP, et al. Traffic-related air pollution and perinatal mortality: a case-control study. Environ Health Perspect. 2009;117:127-32.
24. Hartikainen AL, Sorri M, Anttonen H, Tuimala R, Laara E. Effect of occupational noise on the course and outcome of pregnancy. Scand J Work Environ Health. 1994;20:444-50.
25. Wilhelm M, Ritz B. Residential proximity to traf-fic and adverse birth outcomes in Los Angeles county, California, 1994-1996. Environ Health Perspect. 2003;111:207-16.
26. Kramer MS, Seguin L, Lydon J, Goulet L. Socio-economic disparities in pregnancy outcome: why do the poor fare so poorly? Paediatr Perinat Epidemiol. 2000;14:194-210.
27. Troe EJ, Raat H, Jaddoe VW, et al. Explaining differ-ences in birthweight between ethnic populations. The Generation R Study. BJOG. 2007;114:1557-65.
28. Goedhart G, van Eijsden M, van der Wal MF, Bonsel GJ. Ethnic differences in preterm birth and its subtypes: the effect of a cumulative risk profile. BJOG. 2008;115:710-9.
29. Quispel C, Schneider TA, Bonsel GJ, Lambregtse-van den Berg MP. An innovative screen-and-advice model for psychopathology and psychosocial problems among urban pregnant women: an exploratory study. J Psychosom Obstet Gynaecol. 2012;33:7-14.

40
PREGN
AN
CY AN
D BIRTH
IN RO
TTERDA
M: A
LOCA
L HEA
LTH REPO
RT
3

4
Social Science and Medicine. 2013;83:42-9.
Social deprivation and adverse perinatal outcomes among Western and non-Western pregnant women
in a Dutch urban population
J. Poeran, A.F.G. Maas, E. Birnie, S. Denktaş, E.A.P. Steegers, G.J. Bonsel

42
SOCIA
L DEPRIVATIO
N A
ND
AD
VERSE PERINATA
L OU
TCOM
ES
4
ABSTRACTSocial deprivation is considered a key factor in adverse perinatal outcomes. Rotterdam,
the second largest city in The Netherlands, has large inequalities in perinatal health and a
high number of deprived neighbourhoods. Social deprivation is measured here through
a composite variable: ‘Social Index’ (SI). We studied the impact of the SI (2008-2009; 5
categories) in terms of perinatal mortality, congenital anomalies, preterm birth, small
for gestational age (SGA) and low 5-minute Apgar score as registered in The Netherlands
Perinatal Registry (Rotterdam 2000-2007, n=56,443 singleton pregnancies). We applied
ethnic dichotomisation as Western (European/North-American/Australian) vs. Non-Western
(all others) ethnicity was expected to interact with the impact of SI. Tests for trend and
multilevel regression analysis were applied. Gradually decreasing prevalence of adverse
perinatal outcomes was observed in Western women from the lowest SI category (low social
quality) to the highest SI category (high social quality). In Western women the low-high SI
gradient for prevalence of spontaneous preterm birth (per 1,000) changed from 57.2 to 34.1,
for iatrogenic preterm birth from 35.2 to19.0, for SGA from 119.6 to 59.4, for low Apgar score
from 10.9 to 8.2, and for perinatal mortality from 14.9 to 7.6. These trends were statistically
confirmed by Chi2-tests for trend (p<0.001). For non-Western women such trends were
absent. These strong effects for Western women were confirmed by significant odds ratios
for almost all adverse perinatal outcomes estimated from multilevel regression analysis.
We conclude social deprivation to play a different role among Western vs. non-Western
women. Our results suggest that improvements in social quality may improve perinatal
outcomes in Western women, but alternative approaches may be necessary for non-Western
groups. Suggested explanations for non-Western ‘migrant’ groups include the presence of
‘protective’ effects through knowledge systems or intrinsic resilience. Implications concern
both general and targeted policies.

43
SOCIA
L DEPRIVATIO
N A
ND
AD
VERSE PERINATA
L OU
TCOM
ES
4
INTRODUCTIONIn The Netherlands perinatal mortality exceeds the European average despite a high standard
of mother and child healthcare with free access.1 Perinatal health in the larger cities is even
worse, with the highest rates of perinatal mortality and morbidity being observed in deprived
neighbourhoods.2 The high prevalence of ethnic minority groups and disseminated social
deprivation in urban areas are generally put forward as key aetiologic factors.2-6 Social
deprivation is a very broad term and can be defined as ‘reduction or prevention of culturally
normal interaction with the rest of society’. Indeed, aspects of social deprivation such as
material poverty and lack of social cohesion are both related to ill health, and also strongly
connected; the combined reinforcing presence of these factors might be particularly important
for perinatal ill health.7-9 Numerous studies have shown ethnicity and social deprivation to be
strongly related to adverse perinatal outcomes such as preterm birth and small for gestational
age.3,4,10-14 However, many recent studies have been conducted in the United States and Canada
where ethnic minorities differ considerably from those in Europe and, more specifically, The
Netherlands.2-6,11,13,15,16 In the United States the majority of ethnic minorities either comprise
African-Americans or Hispanics; in Europe they mainly originate from former colonies (for
example in the United Kingdom or The Netherlands) or they result from the 1960’s labour
migration from countries such as Turkey or Morocco (for example in Germany and France,
respectively). Findings from these studies do not necessarily apply to European countries.
Another motivation for our study pertains to findings from a recent Dutch study
which showed Western (European/North-American/Australian) women in deprived
neighbourhoods to have an increased risk of adverse perinatal outcomes as opposed to
non-Western women.2
Rotterdam, the second largest city of The Netherlands, has the highest proportion of non-
Western inhabitants as well as the highest number of deprived neighbourhoods, and the
highest rate of adverse perinatal outcomes, creating a suitable population in which to study
the effect of social deprivation on perinatal outcomes.2 In continuation of previous work, we
investigated the background and the association of social deprivation with adverse perinatal
outcomes, for Western and non-Western women separately, as we hypothesise differential
effects. We used a composite variable, the so called ‘Social Index’ (SI) as deprivation indicator
at the neighbourhood level in the city of Rotterdam. As social deprivation is considered
an important metric of neighbourhood quality policy makers have created the SI and its
underlying domains to measure this. It is used to measure the effectiveness of efforts to
reduce area-based social deprivation. The SI conceptually resembles the less detailed

44
SOCIA
L DEPRIVATIO
N A
ND
AD
VERSE PERINATA
L OU
TCOM
ES
4
Scottish Carstairs index.17 We use the unaltered SI values to facilitate communication of
study results to policy-makers.
METHODS
Outcome data
Data from all single pregnancies in Rotterdam over the period 2000-2007 were derived from
The Netherlands Perinatal Registry. This registry contains population-based information of
97% of all pregnancies in The Netherlands.18 Source data are collected by 94% of midwives,
99% of gynaecologists and 68% of paediatricians, including 100% of Neonatal Intensive
Care Unit paediatricians.18 The mission of The Netherlands Perinatal Registry is to improve
the quality of healthcare by giving insight into the perinatal care process and outcomes
(see also www.perinatreg.nl).
The Netherlands Perinatal Registry provided individual-level information on adverse
perinatal outcomes, along with the four-digit zip codes of the mothers’ places of residence.
The number of pregnancies per zip code area (neighbourhood) ranged from 127 to 2,611.
Adverse perinatal outcome was defined as the occurrence of either perinatal mortality or
perinatal morbidity. Perinatal mortality was defined as death from 22 weeks of gestational
age until 7 days postpartum. We also defined four outcome variables of perinatal morbidity:
congenital anomalies (list defined), small for gestational age (SGA, birthweight below
the 10th percentile for gestational age19, preterm birth (<37th week of gestation) or low
5-minute Apgar-score (<7). As previously described4, preterm birth was subdivided into
spontaneous and iatrogenic preterm birth, the latter being defined as birth <37th week
of gestation and an elective caesarean section or induction of labour. The remainder of
births <37th week of gestation were classified as spontaneous preterm birth. We assume
iatrogenic preterm birth and low Apgar score to be related to both maternal factors as well
as peripartum healthcare factors, whereas the remaining morbidity conditions are assumed
to be primarily related to individual (maternal) characteristics.
Social Index
Neighbourhood social quality was assessed making use of a combined variable, the so-called
‘Social Index’ (SI). This index was created in 2008 and is calculated annually for the Rotterdam
municipal authorities by the Centre for Research and Statistics Rotterdam (COS-Rotterdam,

45
SOCIA
L DEPRIVATIO
N A
ND
AD
VERSE PERINATA
L OU
TCOM
ES
4
www.cos.nl) as a policy measure. All underlying data are empirical. The SI is a composite
multidimensional variable indicating neighbourhood social quality on a 1-10 scale. As is
depicted in figure 4.1 the SI sum score combines scores from 4 ‘domains’: (1) (personal)
capacities, (2) living environment, (3) participation and (4) neighbourhood commitment
(‘social cohesion’). In turn, these ‘domain’ scores are a sum of ‘item’ scores which are based
on a combination of registration data and questionnaire data. The questionnaire data
are obtained from respondents from a random sample of the Rotterdam population. Per
neighbourhood 900 persons were sampled, proportionally stratified for age group, sex and
ethnicity. The number of inhabitants per neighbourhood ranged from 1,579 to 21,200. The
aim was to have 175 respondents (who completed the questionnaire) per neighbourhood.
The initial format was an online questionnaire; if response was not sufficient, respondents
were approached with a paper and pencil questionnaire or by telephone. Overall, response
was 52% online, 21% by paper and pencil, and 27% by telephone.
Figure 4.1 Composition of the SI: four SI ‘domains’ with corresponding ‘items’ extracted from questionnaire data (*) and from registration data (†).
SOCIAL INDEX
(Personal) Capacities Living Environment Participation NeighbourhoodCommitment
EDUCATION-school drop-outs†
-starting qualification / educational level†
(PERCEIVED) HEALTH-perceived health*-filed reports at local(public) health initiatives†
-filed reports of domestic violence†
INCOME-low income households*-social welfare receivers†
-insufficient incomehouseholds*
PROFICIENCY-Dutch proficiency*
DISCRIMINATION-perceived discrimination*-perceived social inter-course between ethnicgroups*
HOUSING QUALITY-overcrowded housing†
-satisfactory housing*
NEIGHBOURHOOD FACILITIES-satisfactoryneighbourhood (health/social) facilities*-knowledge ofneighbourhood socialfacilities*
NUISANCES-neighbourhood pollution*-neighbourhoodvandalism*-neighbourhoodnuisances from speedingcars, traffic noise,rumours, drugs andhang-around youths*-perceived safety*
SCHOOL, WORK AND YOUTHS-job applicants†
-school going youth†
SOCIAL CONTACTS-contacts with family andfriends*-social isolation*
SOCIALPARTICIPATION-sports, social and cultural activities, going out*
DEDICATION TO SOCIETAL ACTIVITIES-dedication to informalcare*-dedication to voluntarywork*-active participation to neighbourhood liveability*
NEIGHBOURHOOD MIGRATION-neighbourhood migrationrate† -neighbourhood newresident rate†-length of residency†
PERCEIVED NEIGH-BOURHOOD BINDING-perceived neighbour-hood binding*-dedication to neighbour-hood (activities)*-trust in local authorities*

46
SOCIA
L DEPRIVATIO
N A
ND
AD
VERSE PERINATA
L OU
TCOM
ES
4
The SI and its underlying domains are considered important metrics of the effectiveness of
policy makers’ efforts to reduce area-based social deprivation. More in-depth information
on the Social Index and its construction is provided in the online appendix file. In this study,
we used the average SI for 2008 and 2009 as a proxy for neighbourhood social quality,
both as a continuous measure and as an ordinal measure (5 categories) with the following
‘COS-Rotterdam’ thresholds:
<3.9 highest social deprivation (I);
3.9-4.9 problematic social deprivation (II);
5.0-5.9 moderate social deprivation (III);
6.0-7.0 adequate social quality (IV);
>7.0 high social quality (V).
Ethnicity
Dutch law does not permit the routine utilisation or registration of ethnicity data. As yet,
The Netherlands Perinatal Registry is exempt from this restriction. The ethnic classification
in this professional-based registry recognises seven possible categories: Western Dutch,
Western other (including women from other European countries, Australia and the US),
Mediterranean, (East) Asian, African, South Asian, or other non-Western. The African and
South Asian group mainly comprises women from the former Dutch colonies Suriname and
The Netherlands Antilles. The group of East Asian women mainly originate from Indonesia,
also a former Dutch colony.
Classification of clients is done by the healthcare professional with an absence of strict
coding rules in applying the category labels. Current classification is therefore crudely based
on a mixture of self-declared ethnicity, race and known country of birth of the woman or
her parents. The registry does not contain information on first/second generation migrants,
nor on their length of stay in Rotterdam or The Netherlands.
Therefore, the current system as devised by the professional organisations may introduce
some classification error, in particular within ‘migrant’ (non-Western) categories. We
dichotomised ethnic groups as Western vs. non-Western for two reasons: (1) to compare
our results with previous studies, and (2) in view of the hypothesis generating nature of
our study which may lead to more detailed investigation of specific ethnic groups in future
studies. The first two classes of the original classification were combined into Western and
the remainder into non-Western women.2

47
SOCIA
L DEPRIVATIO
N A
ND
AD
VERSE PERINATA
L OU
TCOM
ES
4
Analysis
Individual-level data on pregnancy outcomes as registered in The Netherlands Perinatal
Registry were linked to the 2008-2009 neighbourhood SI making use of 4-digit zip codes.
Simple crosstabs were created illustrating the proportion of Western and non-Western
women, mean age, and prevalence rates of adverse perinatal outcomes for each SI category.
Mean age and adverse outcome were separately illustrated for Western and non-Western
pregnant women. One-way tests for trend were carried out for the association of ethnicity,
age and adverse perinatal outcomes and the SI categories (ANOVA for age, Chi-square for
dichotomous variables).
Analogous to the above, we also compared average SI domain scores for Western women
with scores from non-Western women in each SI category. A one-way ANOVA test was used
to test for the difference in mean SI domain scores.
Multilevel logistic regression models were used to estimate adjusted odds ratios (aOR) to
further asses the association between the 2008-2009 mean neighbourhood SI (continuous
measure) and adverse perinatal outcomes (dichotomous outcomes) for Western and non-
Western women. We specified hierarchical random-intercept models that allow for the
incorporation of both individual-level and neighbourhood-level characteristics, as well as
the adjustment for clustering of individuals within their neighbourhoods. SAS version 9.2
(SAS Institute Inc., Cary, NC) was used to run the random intercept multilevel models with
the GLIMMIX procedure. Crude and aORs (for parity; primiparous/multiparous) are reported.
The significance was set at alpha=0.05, two tailed.
RESULTSA total of 56,443 singleton pregnancies were analysed. Characteristics of the study
population are shown in table 4.1.
Patient characteristics per SI category
The association of ethnicity and mean maternal age with SI category is described in table
4.2 (upper part). There are no neighbourhoods in Rotterdam in category I (SI <3.9). The
proportions of Western women and non-Western women respectively increase (from 24.0
to 89.5%) and decrease (from 76.0 to 10.5%) with increasing SI (a higher SI stands for a
neighbourhood with higher social quality). Mean maternal age increases for both Western

48
SOCIA
L DEPRIVATIO
N A
ND
AD
VERSE PERINATA
L OU
TCOM
ES
4
Table 4.1 Characteristics of the study population and perinatal outcomes (Rotterdam, 2000-2007)
N Percentage
No. of singleton pregnancies during study period 56,443 100.0%
Paritya
Primiparous 27,105 48.0%Multiparous 29,333 52.0%
Gestational agea
< 37 weeks 3,900 7.0%37-42 weeks 51,591 92.9%> 42 weeks 71 0.1%
Maternal agea
≤ 19 years 2,445 4.3%20-24 years 10,378 18.4%25-29 years 15,800 28.0%30-34 years 17,368 30.8%≥ 35 years 10,437 18.5%
EthnicityWestern 28,972 51.3%Non-Western 27,471 48.7%
Social Index>3.9 0 0.0%3.9-4.9 6,138 10.9%5.0-5.9 26,760 47.4%6.0-7.0 16,611 29.4%>7.0 6,934 12.3%
Absolute number Per 1,000 births
Perinatal outcomesb
Congenital anomalies 1,489 26.4Preterm birth 3,908 69.3Small for gestational age 5,255 93.1Apgar score <7 (5 minutes after birth) 844 15.0
Any Big4b 10,222 181.2
Fetal mortalityc 466 8.3
Early neonatal mortalityd 183 3.2
Perinatal mortalitye 649 11.5a Totals do not add up due to missing values (parity 5 missings, gestational age 881 missings, maternal age 15 missings).b Number and proportion of pregnant women with at least one ‘Big4’ morbidity.c From 22 weeks of gestational age.d 0-7 days postpartum.e Total of fetal, intrapartum and neonatal mortality.

49
SOCIA
L DEPRIVATIO
N A
ND
AD
VERSE PERINATA
L OU
TCOM
ES
4
Ta
ble
4.2
M
ean
age,
eth
nici
ty a
nd p
reva
lenc
e ra
tes
of a
dver
se p
erin
atal
out
com
es fo
r Wes
tern
and
non
-Wes
tern
wom
en p
er S
I cat
egor
y
Et
hnic
ityTo
tal
SI c
ateg
ory
pa
III
IIIIV
V
n=
56,4
43n=
0n=
6,13
8n=
26,7
60n=
16,6
11n=
6,93
4
Preg
nanc
ies
(%)
Wes
tern
51.3
024
.038
.067
.089
.5<0
.001
Non
-Wes
tern
48.7
076
.062
.023
.010
.5
Mea
n ag
e (y
ears
)W
este
rn30
.30
27.7
29.7
30.3
32.1
<0.0
01N
on-W
este
rn28
.00
27.4
28.0
28.3
30.0
<0.0
01
Cong
enita
l ano
mal
ies
(per
1,0
00)
Wes
tern
25.9
023
.826
.423
.530
.00.
249
Non
-Wes
tern
26.9
020
.828
.826
.424
.60.
219
Pret
erm
birt
h (p
er 1
,000
)Sp
onta
neou
sW
este
rn44
.50
57.2
49.1
44.4
34.1
<0.0
01N
on-W
este
rn45
.20
46.6
44.8
45.9
42.0
0.75
7Ia
trog
enic
Wes
tern
26.4
035
.225
.330
.319
.00.
009
Non
-Wes
tern
24.5
023
.623
.427
.533
.60.
056
Smal
l for
ges
tatio
nal a
ge (p
er 1
,000
)W
este
rn84
.20
119.
699
.179
.959
.4<0
.001
Non
-Wes
tern
103.
40
103.
310
2.5
106.
010
6.1
0.59
3
Low
Apg
ar s
core
(per
1,0
00)
Wes
tern
12.5
010
.913
.514
.38.
20.
050
Non
-Wes
tern
17.5
018
.618
.015
.513
.70.
139
Perin
atal
mor
talit
y (p
er 1
,000
)W
este
rn10
.30
14.9
11.1
10.5
7.6
0.00
8N
on-W
este
rn12
.70
12.0
13.3
12.4
6.8
0.57
6
a Chi
-squ
are
test
for t
rend
was
use
d fo
r eth
nici
ty a
nd p
reva
lenc
e ra
tes
of a
dver
se o
utco
mes
. For
the
mea
n ag
e a
one-
way
AN
OVA
was
use
d.

50
SOCIA
L DEPRIVATIO
N A
ND
AD
VERSE PERINATA
L OU
TCOM
ES
4
and non-Western women with increasing SI (27.7-32.1 and 27.4-30.0 years, respectively).
Both mean age (for Western and non-Western women) and ethnicity show significant
p-values (p<0.001) when testing for trend.
Outcomes in Western women per SI category
The lower part of table 4.2 shows a decreasing trend for rates of spontaneous and iatrogenic
preterm birth (range: 57.2-34.1 and 35.2-19.0 per 1,000, respectively), small for gestational
age (119.6-59.4 per 1,000) and perinatal mortality (14.9-7.6 per 1,000) with better SI values.
This is also verified by the significant p-values when testing for trend (range: <0.001-0.009).
When comparing SI category II with category V, the congenital anomaly rate increases (23.8-
30.0 per 1,000), and the low Apgar score rate decreases (10.9-8.2 per 1,000).
Outcomes in non-Western women per SI category
When comparing SI category II with category V, congenital anomalies, iatrogenic preterm
birth and small for gestational age increase (from 20.8 to 24.6, 23.6-33.6 and 103.3-106.1
per 1,000, respectively). Conversely, rates of spontaneous preterm birth, low Apgar score
and perinatal mortality decrease (46.6-42.0, 18.6-13.7 and 12.0-6.8 per 1,000, respectively).
Trends, however, were not statistically significant.
SI domains
Table 4.3 depicts mean SI domain scores per SI category for Western and non-Western women.
Western women almost always have significantly higher mean SI domain scores compared
with non-Western women, except for SI domains ‘participation’ and ‘neighbourhood
commitment’ in SI category II. The latter being the only domain score for which non-Western
women have a significantly higher score compared with Western women.
Multilevel logistic regression models
Table 4.4 shows the crude and adjusted odds ratio (OR and aOR adjusted for parity) of
the impact of the mean 2008-2009 neighbourhood SI (on a continuous 1-10 scale) on
adverse perinatal outcomes, for Western and non-Western women. For Western as well as
non-Western women congenital anomalies show non-significant effects of SI. For Western
women significant negative associations with SI were shown for spontaneous and iatrogenic
preterm birth, small for gestational age, low Apgar score and perinatal mortality. For non-

51
SOCIA
L DEPRIVATIO
N A
ND
AD
VERSE PERINATA
L OU
TCOM
ES
4
Western women a positive association was demonstrated for iatrogenic preterm birth and
a negative association for low Apgar score. The largest protective effect of higher SI was
seen in Western women for small for gestational age (aOR 0.78; CI 0.73-0.83).
Table 4.3 Mean SI domain scores per SI category for Western and non-Western women
SI category
I II III IV VDomain Ethnicity n=0 n=6,138 n=26,760 n=16,611 n=6,934
Capacities Western 0 3.94a 4.86a 6.44a 8.13a
Non-Western 0 3.93a 4.69a 6.33a 8.03a
Living environment Western 0 5.13a 5.88a 6.71a 7.61a
Non-Western 0 5.10a 5.78a 6.64a 7.55a
Participation Western 0 5.03 5.77a 6.34a 7.37a
Non-Western 0 5.04 5.72a 6.29a 7.32a
Neighbourhood commitment Western 0 4.85a 5.71b 6.62a 7.41a
Non-Western 0 4.93a 5.72b 6.56a 7.32a
a Western vs. non-Western women, ANOVA p<0.001.b Western vs. non-Western women, ANOVA p<0.05.
Table 4.4 Multilevel hierarchical random-intercept logistic regression models: crude (OR) as well as adjusted (aOR, adjusted for parity) odds ratios including 95% confidence intervals (CI) of the associations between mean 2008-2009 neighbourhood SI and adverse perinatal outcomes for Western and non-Western women
Ethnicity ORa (CIc) aORb (CIc)
Congenital anomalies Western 1.02 (0.90-1.16) 1.02 (0.90-1.17)Non-Western 1.02 (0.91-1.15) 1.02 (0.91-1.15)
Preterm birthSpontaneous Western 0.86 (0.80-0.92)d 0.87 (0.80-0.93)d
Non-Western 1.01 (0.92-1.11) 1.00 (0.91-1.10)Iatrogenic Western 0.88 (0.78-0.98)e 0.88 (0.78-0.99)e
Non-Western 1.15 (1.03-1.28)e 1.15 (1.03-1.28)e
Small for gestational age Western 0.77 (0.72-0.82)d 0.78 (0.73-0.83)d
Non-Western 1.02 (0.96-1.08) 1.01 (0.95-1.07)
Low Apgar score Western 0.83 (0.73-0.95)e 0.84 (0.74-0.96)e
Non-Western 0.87 (0.75-1.00) 0.86 (0.74-1.00)e
Perinatal mortality Western 0.83 (0.72-0.96)e 0.84 (0.72-0.97)e
Non-Western 0.96 (0.82-1.13) 0.96 (0.82-1.12)a OR: crude odds ratiob aOR: adjusted odds ratio (for parity)c CI: confidence intervald p-value <0.001e p-value <0.05

52
SOCIA
L DEPRIVATIO
N A
ND
AD
VERSE PERINATA
L OU
TCOM
ES
4
DISCUSSION
Principal fi ndings
This study is one of the few European studies to address the effect of a combined social
deprivation measure on adverse perinatal outcomes and applying multilevel modelling.20 In
the large, multi-ethnic city of Rotterdam the impact of social deprivation on adverse perinatal
outcomes plays a key role with a striking ethnicity-related effect. In the most deprived
neighbourhoods, perinatal outcomes were universally poor with a tendency for even worse
figures for Western women compared to non-Western women. With decreasing deprivation, a
strong gradient for improvement exists for almost all perinatal outcomes in Western women.
For every point increase of the Social Index (higher is better), adjusted perinatal mortality
in Western women shows a 16% decrease. As a similar gradient in perinatal outcomes is
absent in non-Western women, an ethnicity related perinatal outcome gap emerges, with
impressive perinatal health inequalities in neighbourhoods with the lowest deprivation.
Other studies
Our finding that social deprivation has a stronger negative effect on Western women than
non-Western women has been sparsely described in the literature.13,21 Fang et al. used New
York City birth records to show that foreign born women of African and Caribbean descent
had more favourable birth outcomes compared with that for whites, particularly in the
poorest neighbourhoods.21 O’Campo et al. studied the effect sizes for non-Hispanic whites
and non-Hispanic blacks for the relation between neighbourhood deprivation and preterm
birth.13 For whites, the effect size was larger compared to blacks indicating that this group
appears to be less affected by neighbourhood deprivation than whites.13 Furthermore, one
previous study by De Graaf et al., conducted in The Netherlands also supports the current
findings.2 They found that the effect of living in deprived neighbourhoods, as compared
to living elsewhere, was most prominent among Western women with an increased risk of
adverse perinatal outcomes of 24%.2
Possible underlying mechanisms
It is challenging to interpret the observed ethnicity-related effect by one underlying
mechanism. A first explanation takes into account the density of migrant subgroups in the
neighbourhood population.22 Previous studies have suggested that the risk of poor health

53
SOCIA
L DEPRIVATIO
N A
ND
AD
VERSE PERINATA
L OU
TCOM
ES
4
outcomes for a minority individual is inversely related to the density of his or her racial/ethnic
group in the local community, i.e., greater numbers of migrants/non-Western populations in
deprived neighbourhoods, and that living in neighbourhoods with a high migrant density
may be beneficial specifically for migrant (here non-Western) women, such that fewer
negative effects of deprivation in these neighbourhoods may be experienced. This hypothesis
has been validated for various adverse health outcomes ranging from psychiatric conditions
to rates of heart disease.7,8,23,24 The presumed mechanisms include health protection through
increased participation in social networks or knowledge systems, and a more extensive
repertoire of positive coping behaviours.7,8,23,24 When applied to our study context, these
protective effects may result in less feelings of stress during pregnancy and may stimulate
healthy behaviour. In Rotterdam, this could be valid for the non-Western women in deprived
areas (lowest SI) as they generally tend to have better outcomes than Western women in these
areas. However, we also observed a lack of improvement in adverse perinatal outcomes with
increasing SI for non-Western women. This ‘net neutral effect’ may be (partly) explained by
the combination of a decrease in potentially protective migrant/non-Western density when
SI and its positive effects increase. A second explanation may rest on lifestyle epidemiology
concerning factors such as smoking which is known to have a profound effect on perinatal
outcome.25 Previous studies have shown that smoking behaviour differs among ethnic and
socio-economic groups.26 Our data could reflect healthier lifestyle behaviour for Western
women with increasing SI, this gradient may be absent in non-Western women.
Another explanation of our study results pertains to healthcare related factors. This may
pertain to general thresholds to healthcare or density of facilities which is lower in deprived
areas. Western women might profit more from this effect due to better health literacy and
informal networks.9 We assumed iatrogenic preterm birth and low Apgar score to be partially
related to peripartum healthcare factors. However, different patterns were observed for
low Apgar score and iatrogenic preterm birth in Western and non-Western women. Thus,
it is unclear to what extent healthcare related factors have affected the observed ethnic
disparities. The perinatal healthcare process still needs careful analysis as little is known on
its dynamics in a multicultural setting.27
A sociobiological explanation of our study results may involve the presence of epigenetic
effects in some groups of non-Western women, particularly those of African descent, that
limit the potential for positive effects on perinatal outcomes when SI increases.28,29 This
phenomenon has been demonstrated by Collins et al. in a three generation linked dataset of
African Americans in Illinois.30 Their study showed rates of low birthweight to be associated
with worsening maternal grandmothers’ residential environments during her pregnancy

54
SOCIA
L DEPRIVATIO
N A
ND
AD
VERSE PERINATA
L OU
TCOM
ES
4
with her daughter that years later delivered a low birthweight neonate. This association
was independent of the living conditions of the daughter during her pregnancy with the
infant with low birthweight.30 Further research is needed to investigate if this phenomenon
among African Americans also applies to other non-Western populations.
Finally, instead of the above so-called ‘causation’ options, one may think of ‘selection’. Western
and non-Western women may differ in their motive to move to a deprived neighbourhood
or differ in the potential for ‘upward mobility’. As previously described, ethnic minorities
tend to cluster, usually in poor urban areas. This ‘ethnic concentration’ may be maintained by
both its residents and newly arriving migrants because of the amenities and organisations
feeding on this ethnic concentration. That is why residents stay in these neighbourhoods
even when they have the financial means to move out.31,32 Western women in deprived
neighbourhoods are thought to represent a negative selection as the above mechanism
may not apply to them.31,32 The latter is supported by our finding that the only SI domain
for which Western women have a significantly lower score than non-Western women is for
‘neighbourhood commitment’ (social cohesion) in the lowest SI category in Rotterdam, i.e.,
Western women are thought to have less commitment to these neighbourhoods.32
Strengths and weaknesses
The major strengths of the current study include the use of a validated registry with a high
coverage over a long period of time; The Netherlands Perinatal Registry, currently 2000-
2007.18 As social quality and social deprivation are multidimensional concepts, the usage
of a neighbourhood-specific combined social deprivation variable adds strength to the
estimates and, in case of the Social Index, it also allows to draw conclusions regarding a
more specific dimension of social deprivation.33 Neighbourhood-specific social deprivation
indices are generally constructed with factor or principal component analysis.16,33 Such an
approach rests on selecting the most efficient items to represent 1 or more underlying
constructs. The SI intentionally was composed by municipal policymakers, selecting items
which in their view represented best observable and direct interpretable information
on social deprivation; herewith, statistical overlap was accepted to allow for political
communication. Hence, the Social Index was designed for policy monitoring purposes as
an outcome in the first place, rather than for research purposes as a determinant. What also
adds strength to our findings is that initial results were cross-validate d by additional analyses
of the effect of neighbourhood house price quintiles on adverse perinatal outcomes (data
available in the online appendix file). A particular strength of the current study pertains to

55
SOCIA
L DEPRIVATIO
N A
ND
AD
VERSE PERINATA
L OU
TCOM
ES
4
the differentiation between iatrogenic and spontaneous preterm birth as they may differ in
aetiological or causal pathways.34 The majority of previous retrospective studies on the effect
of social deprivation and preterm birth do not take this difference into account.10,12,15,20,34,35
The limitations associated with this study should also be noted. Firstly, area based indices
such as the SI may not correspond to individual socioeconomic status (‘ecological fallacy’)
and do not reflect heterogeneity among the individuals within a neighbourhood. A
possible way to triangulate would be to interview a sample of the women. However, the
strict national privacy regulations which apply to The Netherlands Perinatal Registry,
do not allow identification of individuals for subsequent active approach. Multilevel
modelling to estimate effects based on a neighbourhood-level measure may partially
bypass this problem. The advantage of this approach is that it allows for the incorporation
of both individual-level and neighbourhood-level characteristics. Moreover, it adjusts for
clustering of individuals within neighbourhoods, thereby increasing the validity of the
effect sizes compared to conventional logistic regression analysis.36 As parity was one of
the few individual-level factors we could adjust for, and as we did not have information
on individual-level socioeconomic status, we could not fully benefit from the theoretical
advantages of multilevel modelling over conventional logistic regression. An advantage
of the usage of neighbourhood specific indices is that they provide complementary
information to individual measures of social quality and may be particularly useful in studies
concerning pregnancy outcomes. Determination of social class is known to be problematic
in such studies as not only the mother’s socioeconomic characteristics have to be taken
into account, but also the father’s.37 Additionally, the use of area based deprivation indices
is well supported in the literature.3,10-13,15,16,20,37
Another limitation refers to the use of the mean 2008-2009 SI in assessing the effect on
perinatal outcomes from 2000-2007. This discrepancy was due to the unavailability of data.
Consequently, our analysis does not take into account the variability of neighbourhood SI
between 2000 and 2007. The variability between 2008 and 2009 was small (data available
in the online appendix file). Moreover, it is generally expected to take a long period of time
for possible changes in neighbourhood social quality to take effect (data available in the
online appendix file). Therefore, the discrepancy in the years of available data between
the exposure variable and outcome variables is expected to play a marginal role. Also, the
current study lacks data on lifestyle, in particular smoking, one of the main risk factors for
adverse perinatal outcomes.25 This could have resulted in possible overestimation of the
impact of SI on adverse pregnancy outcomes. However, previous studies have shown that
socioeconomic status remains significantly associated with adverse perinatal outcomes

56
SOCIA
L DEPRIVATIO
N A
ND
AD
VERSE PERINATA
L OU
TCOM
ES
4
such as preterm birth, even after taking smoking into account.13,20 Finally, one could argue
against the grouping of all non-Western women as this is a very heterogeneous group,
disregarding among others any differences in races, cultures, first or second generations, or
migrants’ length of stay. However, the main objective of our study follows from a previous
study which suggested that specifically Western women were at risk for adverse pregnancy
outcomes in deprived areas.2 To further study and reconfirm this effect, we chose to group
non-Western women as we were specifically interested in Western women.
Possible implications
The SI is associated with adverse perinatal outcomes to the extent that both general and
targeted policies seem relevant. In the context of social deprivation, social policy should
continue to aim to serve Western as well as non-Western women equally. General policies,
in particular preventive policies, show higher average benefits (compared to targeted
policies) if applied on the population level. However, they do so while increasing health
gaps as their effects rely on competences and resources which are unequally distributed,
this is called the ‘prevention paradox’.38 Therefore, complementary priority programs are
justified, dedicated to specific ‘worst off’ subgroups.
The observed increased risk of adverse perinatal outcomes in Western women in the most
deprived neighbourhoods justifies additional attention in antenatal care. This approach could
include intensified prevention from existing health promoting programs in combination
with targeted social welfare. It is, however, difficult to extend this recommendation to non-
Western women, as our data and those of others do not show a straightforward relation
between social deprivation and perinatal outcome beyond the effect of being an ethnic
minority itself. Perhaps the ‘Western’ conventional deprivation indicators do not cover the
subtle ethnic specific pathways for adverse perinatal outcomes.
Non-Western women did not improve in perinatal outcome with increasing SI, but showed
an advantage over Western women in deprived neighbourhoods, possibly due to ‘protective’
knowledge systems. Future research could tap into these knowledge systems to evaluate
whether they can contribute to improvement in outcome with increasing SI in non-Western
women.
In addition, we also recommend more studies on this subject in European settings as most
studies on social deprivation and adverse perinatal outcomes have been conducted in
either the US or Canada which makes it unclear to what extent observations are valid for
European populations.

57
SOCIA
L DEPRIVATIO
N A
ND
AD
VERSE PERINATA
L OU
TCOM
ES
4
REFERENCES1. Mohangoo AD, Buitendijk SE, Hukkelhoven CW, et
al. Higher perinatal mortality in The Netherlands than in other European countries: the Peristat-II study. Ned Tijdschr Geneeskd. 2008;152:2718-27.
2. de Graaf JP, Ravelli AC, Wildschut HI, et al. Perinatal outcomes in the four largest cities and in deprived neighbourhoods in The Netherlands. Ned Tijdschr Geneeskd. 2008;152:2734-40.
3. Agyemang C, Vrijkotte TG, Droomers M, van der Wal MF, Bonsel GJ, Stronks K. The effect of neighbourhood income and deprivation on pregnancy outcomes in Amsterdam, The Netherlands. J Epidemiol Community Health. 2009;63:755-60.
4. Goedhart G, van Eijsden M, van der Wal MF, Bonsel GJ. Ethnic differences in preterm birth and its subtypes: the effect of a cumulative risk profile. BJOG. 2008;115:710-9.
5. Goedhart G, van Eijsden M, van der Wal MF, Bonsel GJ. Ethnic differences in term birthweight: the role of constitutional and environmental factors. Paediatr Perinat Epidemiol. 2008;22:360-8.
6. Poeran J, Denktas S, Birnie E, Bonsel GJ, Steegers EA. Urban perinatal health inequalities. J Matern Fetal Neonatal Med. 2011;24:643-6.
7. Fang J, Madhavan S, Bosworth W, Alderman MH. Residential segregation and mortality in New York City. Soc Sci Med. 1998;47:469-76.
8. Halpern D, Nazroo J. The ethnic density effect: results from a national community survey of England and Wales. Int J Soc Psychiatry. 2000;46:34-46.
9. Jonkers M, Richters A, Zwart J, Ory F, van Roos-malen J. Severe maternal morbidity among im-migrant women in the Netherlands: patients’ per-spectives. Reprod Health Matters. 2011;19:144-53.
10. Auger N, Giraud J, Daniel M. The joint influence of area income, income inequality, and immigrant density on adverse birth outcomes: a population-based study. BMC Public Health. 2009;9:237.
11. Elo IT, Culhane JF, Kohler IV, et al. Neighbourhood deprivation and small-for-gestational-age term births in the United States. Paediatr Perinat Epidemiol. 2009;23:87-96.
12. Farley TA, Mason K, Rice J, Habel JD, Scribner R, Cohen DA. The relationship between the neighbourhood environment and adverse birth outcomes. Paediatr Perinat Epidemiol. 2006;20:188-200.
13. O’Campo P, Burke JG, Culhane J, et al. Neighbor-hood deprivation and preterm birth among non-Hispanic Black and White women in eight geographic areas in the United States. Am J Epidemiol. 2008;167:155-63.
14. Timmermans S, Bonsel GJ, Steegers-Theunissen RP, et al. Individual accumulation of heterogeneous risks explains perinatal inequalities within deprived neighbourhoods. Eur J Epidemiol. 2011;26:165-80.
15. Genereux M, Auger N, Goneau M, Daniel M. Neighbourhood socioeconomic status, maternal education and adverse birth outcomes among mothers living near highways. J Epidemiol Community Health. 2008;62:695-700.
16. Janevic T, Stein CR, Savitz DA, Kaufman JS, Mason SM, Herring AH. Neighborhood deprivation and adverse birth outcomes among diverse ethnic groups. Ann Epidemiol. 2010;20:445-51.
17. Carstairs V, Morris R. Deprivation and health in Scotland. Health Bull (Edinb). 1990;48:162-75.
18. Perinatal care in The Netherlands 2007 (in Dutch: Perinatale zorg in Nederland 2007). Utrecht: The Netherlands Perinatal Registry; 2009. (online: http://www.perinatreg.nl/uploads/150/116/Jaarboek_Perinatale_Zorg_2007.pdf).
19. Kloosterman GJ. On intrauterine growth. Int J Gynaecol Obstet. 1970;8:895-912.
20. Gray R, Bonellie SR, Chalmers J, Greer I, Jarvis S, Williams C. Social inequalities in preterm birth in Scotland 1980-2003: findings from an area-based measure of deprivation. BJOG. 2008;115:82-90.
21. Fang J, Madhavan S, Alderman MH. Low birth weight: race and maternal nativity--impact of community income. Pediatrics. 1999;103:E5.
22. Grady SC. Racial disparities in low birthweight and the contribution of residential segregation: a multilevel analysis. Soc Sci Med. 2006;63:3013-29.
23. Neeleman J, Wessely S. Ethnic minority suicide: a small area geographical study in south London. Psychol Med. 1999;29:429-36.

58
SOCIA
L DEPRIVATIO
N A
ND
AD
VERSE PERINATA
L OU
TCOM
ES
4
24. Rabkin JG. Ethnic density and psychiatric hos-pitalization: hazards of minority status. Am J Psychiatry. 1979;136:1562-6.
25. Andres RL, Day MC. Perinatal complications associated with maternal tobacco use. Semin Neonatol. 2000;5:231-41.
26. Barnett R, Moon G, Kearns R. Social inequality and ethnic differences in smoking in New Zealand. Soc Sci Med. 2004;59:129-43.
27. Denktas S, Bonsel GJ, Van der Weg EJ, et al. An urban perinatal health programme of strategies to improve perinatal health. Matern Child Health J. 2011;16:1553-8.
28. Burris HH, Collins JW, Jr. Race and preterm birth--the case for epigenetic inquiry. Ethn Dis. 2010;20:296-9.
29. Kramer MR, Hogue CR. What causes racial disparities in very preterm birth? A biosocial perspective. Epidemiol Rev. 2009;31:84-98.
30. Collins JW, Jr., David RJ, Rankin KM, Desireddi JR. Transgenerational effect of neighborhood poverty on low birth weight among African Americans in Cook County, I llinois. Am J Epidemiol. 2009;169:712-7.
31. Crowder K, South SJ. Spatial Dynamics of White Flight: The Effects of Local and Extralocal Racial Conditions on Neighborhood out-Migration. Am Sociol Rev. 2008;73:792-812.
32. Schaake K, Burgers J, Mulder CH. Ethnicity at the Individual and Neighborhood Level as an Explanation for Moving Out of the Neighborhood. Popul Res Policy Rev. 2010;29:593-608.
33. Messer LC, Laraia BA, Kaufman JS, et al. The development of a standardized neighborhood deprivation index. J Urban Health. 2006;83:1041-62.
34. Moutquin JM. Classification and heterogeneity of preterm birth. BJOG. 2003;110 Suppl 20:30-3.
35. Aveyard P, Cheng KK, Manaseki S, Gardosi J. The risk of preterm delivery in women from different ethnic groups. BJOG. 2002;109:894-9.
36. Twisk JWR. Applied Multilevel Analysis. 4 ed. Cambridge: Cambridge University Press; 2010.
37. Rajaratnam JK, Burke JG, O’Campo P. Maternal and child health and neighborhood context: the selection and construction of area-level variables. Health Place. 2006;12:547-56.
38. Allebeck P. The prevention paradox or the inequal-ity paradox? Eur J Public Health. 2008;18:215.

PART II
Perinatal health in The Netherlands

60

5
Manuscript submitted for publication.
Population attributable risks of patient, child and organisational
risk factors for perinatal mortality
J. Poeran, G.J.J.M. Borsboom, J.P. De Graaf, E. Birnie, E.A.P. Steegers, G.J. Bonsel

62
POPU
LATION
ATTRIBUTA
BLE RISKS FOR PERIN
ATAL M
ORTA
LITY
5
ABSTRACTObjective Estimate the contributing role of maternal, child, and organisational risk factors
in perinatal mortality by calculating their population attributable risks (PAR).
Methods The primary dataset comprised all (n=1,020,749) singleton hospital births from
≥22 weeks’ gestation (The Netherlands Perinatal Registry 2000-2008). PARs for single and
grouped risk factors were estimated in four stages: (1) creating a duplicate dataset for each
PAR analysis in which risk factors of interest were set to the most favourable value (e.g.,
all women assigned ‘Western’ for PAR calculation of ethnicity); (2) in the primary dataset
an elaborate multilevel logistic regression model was fitted from which (3) the obtained
coefficients were used to predict perinatal mortality in each duplicate dataset; (4) PARs were
then estimated as the proportional change of predicted- compared to observed perinatal
mortality. Additionally, PARs for grouped risk factors were estimated by using incremental
values in two orders: after PAR estimation of grouped maternal risk factors, the resulting
PARs for grouped child, and grouped organisational factors were estimated, and vice versa.
Results The combined PAR of maternal, child and organisational factors is 94.4%, i.e., when
all factors are set to the most favourable value perinatal mortality is expected to be reduced
with 94.4%. Depending on the order of analysis, the PAR of maternal risk factors varies from
1.4-13.1%, and for child- and organisational factors 58.7-74.0% and 7.3-34.3%, respectively.
Conclusion The PAR of maternal, child and organisational factors combined is 94.4%.
Optimisation of organisational factors may achieve a 34.3% decrease in perinatal mortality.

63
POPU
LATION
ATTRIBUTA
BLE RISKS FOR PERIN
ATAL M
ORTA
LITY
5
INTRODUCTIONIn The Netherlands perinatal mortality rates exceed the European average.1,2 For long,
population factors such as the high maternal age at first childbirth, the high number of
multiple pregnancies, and the increasing proportion of non-Western pregnant women were
held responsible.1,2 These explanations were challenged as perinatal mortality remains high
after exclusion of these risk groups.3 Recent studies have thus addressed the contribution
of non-patient factors like the system of Dutch obstetric care with independently practicing
community midwives4, travel time to a hospital5, organisational characteristics of hospitals6,
and geographic factors, in particular urban deprivation7-9. However, of these studies neither
established the relative importance of the patient and non-patient risk factors, nor the
magnitude of the effect when unfavourable patient and non-patient risks coincide. A valid
estimate of attribution of these is essential to prioritise among available policy options
to reduce perinatal mortality. Our study aims to disentangle the contribution of patient
and non-patient risk factors to perinatal mortality, applying the population attributable
risk (PAR) concept to a comprehensive (2000-2008) national perinatal dataset. The PAR
concept is attractive as it generally quantifies the separate impact of a risk factor in
terms of proportion of total mortality (or other relevant outcome) accounted for by that
factor. The standard PAR approach assumes risk factors to act independently, and applies
straightforward formulae.10 The concept is considerably more complex if risk factors interact,
in a non-additive, conditional or time-dependent fashion. For convenience such interaction
effects are often ignored, or risk groups are excluded11, at the cost of conflicting or invalid
estimations of the impact of risk factors (in the perinatal context).
Our approach particularly accounts for interactions between the organisational features
of care provision and the fetal-maternal risk level. E.g., we account for the effect that travel
time to hospital5 for women referred during parturition may strongly depend on fetal
morbidity and maternal features: under perfect fetal-maternal conditions, travel time effects
may be minimal, while the effect may be sizable if the rate of unexpected transfers is high.
Likewise, we account for interaction between staffing level during out-of-office hours and
fetal-maternal characteristics.
We introduce a four-stage computational framework to estimate the relative importance
of interacting patient- and non-patient risk factors for perinatal mortality.

64
POPU
LATION
ATTRIBUTA
BLE RISKS FOR PERIN
ATAL M
ORTA
LITY
5
METHODS
Patient data
In this retrospective cohort study we derived data on maternal factors, child factors
and outcomes from The Netherlands Perinatal Registry. This registry contains complete
population-based information of >97% of all pregnancies in the Netherlands.12 On behalf
of the respective professional societies, source data are routinely collected by 94% of
midwives, 99% of gynaecologists and 68% of paediatricians including 100% of Neonatal
Intensive Care Unit paediatricians.12 (See website for detailed description: www.perinatreg.
nl). The registry contains 1,620,126 birth records for the period of 2000-2008.
We excluded multiple pregnancies (n=35,326), births with unknown gestational age
(n=17,768), births with unknown or erroneous zip code (n=20,804), and births supervised
exclusively by primary care midwives (n=525,479) as we assume hospital organisational
features to be of little or no importance in births under the exclusive supervision of primary
care midwives. Intra-uterine deaths (stillbirths, n=7,661) were excluded as their delivery
differs from normal cases.13
The final patient database consisted of 1,013,088 records.
Geographical data
Travel time to hospital was calculated as the travel time between a pregnant woman’s 4-digit
zip code and the hospital’s zip code; zip code covers an average of 4,000 inhabitants. Travel
time data were derived from a commercially available geographic information system
package acquired from the Geodan company (www.geodan.nl). We assume travel time to
hospital only to have an impact on women with unplanned births who were transferred
from home to hospital during parturition. Thus, hospital travel time was set to zero for
women with planned births, i.e., induction of labor (n=467,071) or a planned (primary)
caesarean section (n=98,135).
Hospital data
Hospital organisational data were collected separately from this study by one of the
investigators (JPDG), with the full support of the Dutch Society of Obstetricians and
Gynaecologists using a standardised (structured) interview for all (n=99) maternity units.
Response was 100%.6 Collected data consisted of 24 variables (table 5.1) with inevitable

65
POPU
LATION
ATTRIBUTA
BLE RISKS FOR PERIN
ATAL M
ORTA
LITY
5
Table 5.1 Overview of hospitals’ organisational data
Organisational feature Remarks
General teaching hospital categorised into yes / no
Gynaecology departmentduration of daytime shifts categorised into durations of 10-12 hours and 7-9
hoursduration of evening / night shifts and the highest level of the professional who is attending these shifts
categorised into durations of ≤14 hours and ≥15 hours with professional levels categorised into two groups: (1) gynaecologist / gynaecologist in training and (2) non-in-training physician / midwife / nurse
the highest level of the professional who is attending the evening and night shifts during the week
categorised into five groups: (1) gynaecologist, (2) in-training and non-in-training resident gynaecology, (3) general emergency physician, (4) midwife and (5) nurse
the highest level of the professional who is attending the daytime shifts during weekends
categorised into five groups: (1) gynaecologist, (2) in-training and non-in-training resident gynaecology, (3) general emergency physician, (4) midwife and (5) nurse
the highest level of the professional who is attending the evening and night shifts during weekends
categorised into five groups: (1) gynaecologist, (2) in-training and non-in-training resident gynaecology, (3) general emergency physician, (4) midwife and (5) nurse
permitted to sleep during attending shifts categorised into yes / nogynaecologist on backup call during shifts categorised into yes / noprofessional doing rounds during weekends categorised into four groups: (1) gynaecologist,
(2) in-training and non-in-training resident gynaecology, (3) general emergency physician, (4) midwife and (5) nurse
in-hospital presence of the emergency operating theatre team
categorised into three groups: in-hospital presence during (1) 24 hours, (2) presence during daytime and evening and on-call during the night, (3) presence during daytime and on-call during the evening and night
in-hospital presence of an anesthaesiologist categorised into three groups: in-hospital presence during (1) 24 hours, (2) presence during daytime and evening and on-call during the night, (3) presence during daytime and on-call during the evening and night
the total number of obstetric caregivers (specialists, physicians, midwives, nurses)
a continuous number
annual number of deliveries continuous as well as grouped into three categories: (1) <1000, (2) 1000-2000, (3) >2000
combination of the annual number of deliveries with the gynaecologist:other obstetric caregiver ratio
categorised into six groups: (1) <1000 and ≤1:4, (2) <1000 and 1:4-1:6, (3) <1000 and >1:6, (4) 1000-2000 and ≤1:4, (5) 1000-2000 >1:4, (6) >2000 and all ratios
minimum duration of attending shift during weekends
a continuous number (range 12-72 hours)
Table 5.1 continues on next page.

66
POPU
LATION
ATTRIBUTA
BLE RISKS FOR PERIN
ATAL M
ORTA
LITY
5
Table 5.1 Continued
Organizational feature Remarks
average travel time in minutes from home to hospital for an on-call gynaecologist
a continuous number
maximum travel time in minutes from home to hospital for an on-call gynaecologist
a continuous number
number of caregivers present during attending shifts on weekday evenings and nights
a continuous number
number of caregivers present during attending shifts on weekends during the day
a continuous number
number of caregivers present during attending shifts on weekends during the evening and the night
a continuous number
Paediatrics departmentlevel of care for newborns categorised into four groups: (1) Neonatal Intensive
Care Unit (NICU), (2) post-NICU or incubator from 30 weeks of gestational age, (3) incubator from 32 weeks of gestational age, (4) initially first aid for neonate with suboptimal start with subsequent referral to a hospital with a higher level of care
the highest level of the professional at the paediatrics department who is attending the shifts outside office hours
categorised into six groups: (1) fellow neonatologist, (2) paediatrician, (3) in-training paediatrician, (4) non-in-training resident paediatrics, (5) general emergency physician, (6) no professional present but on-call
the lowest level of the professional at the paediatrics department who is attending the shifts outside office hours
categorised into six groups: (1) fellow neonatologist, (2) paediatrician, (3) in-training paediatrician, (4) non-in-training resident paediatrics, (5) general emergency physician, (6) no professional present but on-call
professional on-call at the paediatrics department
categorised into four groups: (1) no one on-call, (2) paediatrician on-call, (3) fellow neonatologist on-call, (4) other professional on-call
partial overlap. For that reason we used principal component analysis (PCA) as an accepted
technique to reduce the high number of interrelated explanatory variables to a limited
number of so-called principal components. PCA summarises the net information content
of overlapping data into a small number of independent, non-overlapping constructed
variables. Such a constructed variable consists of a weighted sum of the scores of the
observed variables, where each weight reflects the added informative value of each
observed variable to the constructed variable. The background and the technique itself
are described in more depth elsewhere.14 In the best case, 50% or more of all variability in
the original variables is covered by a limited number of (usually two or three) constructed
variables. The removal of overlap increases the power of the constructed variables as

67
POPU
LATION
ATTRIBUTA
BLE RISKS FOR PERIN
ATAL M
ORTA
LITY
5
determinants in explanatory regression analysis. Note that the PCA technique is descriptive
only: it can not be used for predictive analysis.
In our analysis the 24 organisation variables were summarised into two principal
components, factor 1 and factor 2, with a computed numerical score for each hospital.
Factor 1 can be interpreted as ‘scale size of the hospital’ as it primarily combines original
variables pointing to hospital size and the number of obstetric caregivers: the lower the
factor value, the larger the hospital and the higher the number of obstetric caregivers.
Factor 2 can be interpreted as ‘24-hour equality of service level’. This factor combines original
variables pointing to around-the-clock availability of qualified professionals from various
backgrounds. The two factors together cover about 70% of the information (variability)
contained in the original 24 variables.
We additionally computed a ‘hospital-specific intervention policy’ variable defined as the
hospital-specific percentage of primary caesarean sections for term breech presentation.
A low ‘primary-caesarean-section- for-term-breech’ percentage represents hospitals with
a more expectative approach in obstetric policy whereas a high percentage stands for
hospitals with a more proactive obstetric policy.
Outcome measures and risk factors
The main outcome was intrapartum or early neonatal death within 7 days after live birth,
for convenience further referred to as perinatal mortality.6 Risk factors were grouped into
maternal and child factors (patient factors) and organisational factors (non-patient factors).
Maternal factors were ethnicity (Western / non-Western of African descent / other non-
Western), parity (0 / 1-2 / >2) and maternal age (<25 / 25-29 / 30-34 / 35-39 / ≥40 years).
Child factors were gestational age (thirteen categories)6, congenital anomalies (yes / no),
small for gestational age (SGA: birthweight >10th / 2.3-10th / <2.3rd percentile)15,16 and fetal
presentation (cephalic / breech / transverse or other / unknown). Congenital anomalies are
recorded postpartum and classified through a standard coding system by organ system (8
categories, 71 subcategories).17
Travel time to the hospital was expressed in minutes (continuous). Other organisational
factors were: day and time of delivery (Saturday / Sunday / weekday, each subdivided
into three time slots 00:00-07:59 / 08:00-17:59 / 18:00-00:00), emergency referral during
parturition (yes / no), the two principal component factors, and the ‘primary-caesarean-
section-for-term-breech’ percentage. Emergency referral during parturition was defined
according to the caregiver providing delivery information in the registry.

68
POPU
LATION
ATTRIBUTA
BLE RISKS FOR PERIN
ATAL M
ORTA
LITY
5
Population attributable risk
The aim of this study is to estimate the population attributable risk (PAR) of maternal, child
and organisational risk factors for perinatal mortality. The PAR of a risk factor is the amount
of perinatal mortality that can be attributed to that particular risk factor among individuals
with the risk factor compared to those without.10 The standard PAR calculation is as follows:
PAR%=[(P*(RR−1))/(1+(P*(RR−1)))]*100. From this formula PAR estimations are expressed
as ‘the percentage or proportion of outcome accounted for’ by the risk factor involved. RR
stands for relative risk, and P for the prevalence of the risk factor in the studied population.
As said, PAR estimates from the above formula are subject to limitations if risk factors or
their effects interact. First, the formula is not additive if multiple risk factors act depend-
ently: a simple one-factor-at-a-time computation then leads to an unrealistic sum of PARs
being >100%. Second, computational complexity increases rapidly with more independent
factors, e.g., requiring simulation studies. Confounding adds to the complexity.
Logistic regression analysis enables to address several risk factors at a time, and indeed
has been used in some PAR studies.18 The resulting adjusted odds ratios (OR) are, however,
difficult to interpret, as the reference risk is unclear, and as this approach has no solution
for conditionally dependent factors.18 The method we present in this study addresses the
interaction problem. It only requires the researcher to be explicit on the presumed causal
priority of the related explanatory variables under study.11
Estimation of PARs
The PAR for single risk factors and groups of risk factors were estimated with a four-stage
approach (figure 5.1). In stage one, multiple duplicate datasets were created. In the duplicate
dataset the risk factor(s) of interest were eliminated by setting their values uniformly to
the most favourable value in terms of outcome. E.g., in the duplicate dataset used for the
PAR analysis of the single risk factor ‘ethnicity’, all women were assigned ‘Western’. The most
favourable value (categorical or continuous) was obvious in most variables. E.g., in case of
travel time to hospital, this value was zero; for the principal component factors 1 and 2, we
used the average value of the academic hospitals as optimum. For the primary-caesarean-
section-for-term-breech’ policy we replaced the observed percentage of primary caesarean
sections in term breech in a specific hospital by the national average, in those hospitals
where the observed percentage was lower than this average. Thus, a specific duplicate
dataset underlies each specific PAR estimate.

69
POPU
LATION
ATTRIBUTA
BLE RISKS FOR PERIN
ATAL M
ORTA
LITY
5
In stage two, a multilevel multivariable logistic regression model with perinatal mortality
as dependent variable was fitted using the original (unchanged) dataset. All determinants
mentioned above (=independent variables) were forced into the model, including
predefined interactions. Because of the multilevel structure of the data (individuals are
grouped per hospital) we used a multilevel logistic regression model which adjusts for the
possible clustering of particular individuals within hospitals (random intercept).
In stage three, the estimated beta-coefficients obtained in the multilevel model with the
original dataset, were used to predict -on the individual level- the probability of perinatal
mortality (‘PRED’ in figure 5.1) once a specific factor was eliminated. In each duplicate dataset
Figure 5.1 Four-stage procedural scheme for the estimation of PARs.
SUMMATION ofobserved cases of perinatal mortality
(‘OBS’)
SUMMATION ofpredicted individual perinatal mortality probabilities (‘PRED’)
PAR CALCULATION(in %) for eliminated risk factors
OBS - PREDOBS
X 100%
ORIGINAL DATASET
DUPLICATE DATASET
MULTIPLE DUPLICATEdatasets with risk factors ELIMINATED by setting the risk factors of interest to the most favourable value(s)
MULTILEVELREGRESSION MODEL
(forced inclusion of maternal, child and organisational factors
PREDICTING PERINATAL MORTALITY with defined risk factors eliminated
12 3
4

70
POPU
LATION
ATTRIBUTA
BLE RISKS FOR PERIN
ATAL M
ORTA
LITY
5
the role of one or more risk factors was eliminated by setting the value to the optimum. The
individual perinatal mortality probabilities were then summed to obtain a total predicted
perinatal mortality for each duplicate dataset with one or more risk factors eliminated. For
example, the predicted number of cases of perinatal mortality in a hypothetical world with
Western mothers only, all other factors equal, was estimated by applying the parameter
estimates from the multilevel model to the duplicate dataset in which all women were
assigned ‘Western’.
In stage four, PARs were calculated. The total predicted (by definition: lower) perinatal mortality
of each duplicate dataset was compared to the observed (‘OBS’ in figure 5.1) total mortality of
the original dataset. The PAR was then conventionally calculated as the proportional change
of the perinatal mortality (in %): e.g., if predicted mortality was 78% of the observed mortality,
the PAR was 22%. We did so for all single risk factors and groups of risk factors (maternal, child,
and organisational factors). If sets of risk factors were defined cumulative, this allowed for an
incremental analysis. E.g., if we start with estimating the PAR of ethnicity, followed by the PAR
of ethnicity and maternal age combined, the difference between these two PARs provides a
PAR of maternal age conditional on a population with only Western women.
The magnitude of the contribution of risk factors to perinatal mortality as computed by
this four-stage approach is presented in three ways:
1. the ‘univariable contribution’, where only the risk factor(s) at stake are set to the most
favourable values, leaving all other variables to their original level;
2. a ‘descending order contribution’, where we used a cumulative approach starting with
maternal, followed by child, and organisational factors, respectively. Note that in this
case the organisational PAR is estimated, assuming both maternal and child factors to
be optimal. For this method of calculation, the PAR of maternal factors is the same as
the ‘univariable contribution’ PAR.
3. ‘ascending order’ contribution’ with the reversed order of appearance of risk factors:
first organisational, then child, and finally maternal factors.
It can be expected that starting with organisational factors (‘ascending order’), leaving
the original level of mother and child risks unaltered, provides an equal or higher PAR,
compared to estimating the PAR of organisational factors conditional on a hypothetically
perfect mother-child population (‘descending order’). The comparison of results from (2) the
descending vs. (3) ascending order may thus be thought of as a policy choice to start with
either improvement of maternal and child factors vs. improvement of organisational factors.

71
POPU
LATION
ATTRIBUTA
BLE RISKS FOR PERIN
ATAL M
ORTA
LITY
5
SAS version 9.2 (SAS Institute Inc., Cary, NC) was used, with the GLIMMIX procedure to run
the random intercept multilevel models which were also used to calculate the predicted
values of perinatal mortality. Syntax can be obtained from the authors.
RESULTSIn our study population (table 5.2) most women are of Western origin (83.3%), primiparous
(52.9%) and 30-34 years old (38.3%). Preterm birth (<37 weeks’ gestation) was seen in 8.6%,
congenital anomaly in 3.0%, SGA in 10.6%, and a non-cephalic presentation was seen in 8.1%
of cases. Almost 15% of women had to travel 15 minutes or more to the hospital where they
gave birth, most children (42.4%) were born on a weekday between 08:00 and 17:59, 32.4%
of women were referred during parturition, and 12.5% of women gave birth in a hospital
with a ‘primary-caesarean-section- for-term-breech’ percentage of 75% or more. All academic
hospitals showed principal component factor values in the ‘best’ quartile (data not shown).
Table 5.2 Characteristics of the study population
N Percentage
Study population 1,013,088 100,0%
Maternal factors
EthnicityWestern 844,340 83.3%Non-Western African descent 27,617 2.7%Non-Western other 141,131 13.9%
ParityPrimiparous (P0) 535,641 52.9%Multiparous (P1-P2) 425,288 42.0%Multiparous (P>2) 52,159 5.1%
Maternal age< 25 years 122,769 12.1%25-29 years 290,524 28.7%30-34 years 387,942 38.3%35-39 years 181,738 17.9%≥ 40 years 30,115 3.0%
Child factors
Gestational age22-27.6 weeks 4,876 0.5%28-31.6 weeks 8,417 0.8%32 weeks 4,238 0.4%
Table 5.2 continues on next page.

72
POPU
LATION
ATTRIBUTA
BLE RISKS FOR PERIN
ATAL M
ORTA
LITY
5
Table 5.2 Continued
N Percentage
33 weeks 6,733 0.7%34 weeks 11,157 1.1%35 weeks 18,119 1.8%36 weeks 33,707 3.3%37 weeks 63,848 6.3%38 weeks 155,400 15.3%39 weeks 212,947 21.0%40 weeks 242,565 23.9%41 weeks 176,094 17.4%≥ 42 weeks 74,987 7.4%
Congenital anomaliesNo 982,273 97.0%Yes 30,815 3.0%
Small for gestational age (SGA)No SGA 905,919 89.4%Birthweight P2.3-P10 80,697 8.0%Birthweight < P2.3 26,472 2.6%
Fetal presentationCephalic 930,785 91.9%Breech 72,313 7.1%Transverse or other 9,036 0.9%Unknown 954 0.1%
Organisational factors
Travel time to hospital< 15 minutes 865,105 85.4%≥ 15 minutes 147,983 14.6%
Day and time of deliverySaturday 00:00-07:59 33,625 3.3%Saturday 08:00-17:59 55,509 5.5%Saturday 18:00-23:59 28,743 2.8%Sunday 00:00-07:59 33,750 3.3%Sunday 08:00-17:59 54,880 5.4%Sunday 18:00-23:59 28,434 2.8%Weekdays 00:00-07:59 173,463 17.1%Weekdays 08:00-17:59 429,398 42.4%Weekdays 18:00-23:59 175,286 17.3%
Referral during parturitionNo 684,495 67.6%Yes 328,593 32.4%
Hospital ‘elective-caesarean-section- for-term-breech’ percentage< 75% 886,893 87.5%≥ 75% 126,195 12.5%

73
POPU
LATION
ATTRIBUTA
BLE RISKS FOR PERIN
ATAL M
ORTA
LITY
5
Multivariable multilevel logistic regression model using the original dataset
Effect estimates from the multivariable multilevel logistic regression model are shown
in table 5.3. For maternal factors, only parity is significantly associated with perinatal
mortality, with the highest risk for multiparous (P>2) women (OR 1.57; CI 1.38-1.78). All
child factors are significantly associated with perinatal mortality. Gestational ages <37
weeks have the highest risks for perinatal mortality (OR range 3.71 to >1,000); the highest
risk for term pregnancies is seen for 37 weeks of gestation (OR 2.35; CI 2.01-2.75). Infants
with congenital anomalies have an 11 times increased risk (OR 11.05; CI 10.25-11.91),
and a birthweight < P2.3 has an almost 7 times increased risk (OR 6.79; CI 6.10-7.56) for
perinatal mortality. Increased risks are also observed for non-cephalic fetal presentations
(OR range 1.53-2.20). For organisational factors only the principal component factors are
Table 5.3 Multivariable multilevel logistic regression model
aOR CI P-value
Maternal factors
Ethnicity 0.083Western [ref] 1.00Non-Western African descent 1.10 0.94 1.28Non-Western other 1.10 1.01 1.20
ParityPrimiparous (P0) [ref] 1.00 <.0001Multiparous (P1-P2) 1.31 1.23 1.40Multiparous (P>2) 1.57 1.38 1.78
Maternal age 0.085< 25 years 1.05 0.95 1.1625-29 years [ref] 1.0030-34 years 1.07 0.99 1.1635-39 years 1.13 1.03 1.24≥ 40 years 0.96 0.81 1.15
Child factors
Gestational age <.000122-27.6 weeks >1,000 >1,000 >1,00028-31.6 weeks 43.38 37.28 50.4832 weeks 16.68 13.52 20.5933 weeks 12.42 10.22 15.0934 weeks 7.35 6.07 8.91
Table 5.3 continues on next page.

74
POPU
LATION
ATTRIBUTA
BLE RISKS FOR PERIN
ATAL M
ORTA
LITY
5
Table 5.3 Continued
aOR CI P-value
35 weeks 5.54 4.64 6.6236 weeks 3.71 3.14 4.3737 weeks 2.35 2.01 2.7538 weeks 1.36 1.18 1.5739 weeks 1.05 0.91 1.2140 weeks [ref] 1.0041 weeks 1.34 1.16 1.54≥ 42 weeks 1.35 1.12 1.63
Congenital anomalies <.0001No [ref] 1.00Yes 11.05 10.25 11.91
Small for gestational age (SGA)No SGA [ref] 1.00 <.0001Birthweight P2.3-P10 2.41 2.18 2.65Birthweight < P2.3 6.79 6.10 7.56
Fetal presentation <.0001Cephalic [ref] 1.00Breech 1.53 1.41 1.66Transverse or other 1.54 1.29 1.83Unknown 2.20 1.26 3.86
Organisational factors
Travel time to hospital 1.00 0.99 1.00 <.0001
Day and time of delivery <.0001Saturday 00:00-07:59 1.49 1.27 1.75Saturday 08:00-17:59 1.11 0.97 1.29Saturday 18:00-23:59 1.34 1.12 1.60Sunday 00:00-07:59 1.40 1.19 1.64Sunday 08:00-17:59 1.31 1.14 1.50Sunday 18:00-23:59 1.16 0.96 1.39Weekdays 00:00-07:59 1.42 1.31 1.55Weekdays 08:00-17:59 [ref] 1.00Weekdays 18:00-23:59 1.29 1.19 1.41
Referral during parturition <.0001No [ref] 1.00Yes 1.24 1.14 1.34
Hospital ‘elective-caesarean-section-for-term-breech’ percentage
0.99 0.98 0.99 <.0001
Hospital organisational featuresPrincipal component (factor 1) 1.01 0.91 1.11 0.915Principal component (factor 2) 0.98 0.89 1.09 0.752Principal component (factor 1) ^2 0.86 0.77 0.97 0.012Principal component (factor 2) ^2 0.99 0.95 1.04 0.746

75
POPU
LATION
ATTRIBUTA
BLE RISKS FOR PERIN
ATAL M
ORTA
LITY
5
not significantly associated with perinatal mortality (OR 1.01; CI 0.91-1.11 and OR 0.98; CI
0.89-1.09 for factor 1 and 2, respectively). Births on Saturday nights and weekday nights
have a >40% increased risk for perinatal mortality (OR 1.49; CI 1.27-1.75 and OR 1.42; CI
1.31-1.55, respectively), referral during parturition has an almost 25% increased risk (OR 1.24;
CI 1.14-1.34). The hospital ‘primary-caesarean-section- for-term-breech’ percentage is also
significantly associated with perinatal mortality (0.99; CI 0.98-0.99). For every percentage
increase in ‘primary-caesarean-section- for-term-breech’, perinatal mortality decreases with
1%. Thus, a hospital with a higher percentage of primary caesarean sections on average
has a lower rate of perinatal mortality adjusted for other factors.
PAR results
Table 5.4 lists PARs of single risk factors (upper part) and groups of risk factors (‘univariable
contribution’; lower part). Of all maternal factors, parity has the highest univariable PAR
(8.9%). In other words: if all women in our dataset would be primiparous perinatal mortality
would be reduced by 8.9%, all other things equal. Of all child factors, gestational age (72.2%)
and congenital anomalies (22.7%) have the highest univariable PAR. Hospital organisational
factors captured in the ‘primary-caesarean-section- for-term-breech’ percentage and
the principal component factors have the highest univariable PAR (13.2% and 16.4%,
respectively) of the organisational factors. If every hospital is set to the between-hospital
average ‘primary-caesarean-sections-for-term-breech’ percentage, perinatal mortality would
decline with 13.2%. If all hospitals are set to the most favourable principal component
Table 5.4 Observed and predicted perinatal mortality with subsequent PAR estimations of single risk factors (upper part) and groups of risk factors (lower part)
N OBS-PRED PAR (%)
Observed cases of perinatal mortality 6,269 - 100,0%
Predicted cases of perinatal mortality
Maternal factors
EthnicityEveryone Western 6,184 85 1.4%
ParityEveryone nulliparous 5,711 558 8.9%
Maternal ageEveryone 25-29 years 6,047 222 3.5%
Table 5.4 continues on next page.

76
POPU
LATION
ATTRIBUTA
BLE RISKS FOR PERIN
ATAL M
ORTA
LITY
5
Table 5.4 Continued
N OBS-PRED PAR (%)
Child factors
Gestational ageEveryone 40 weeks 1,740 4,529 72.2%
Congenital anomaliesNo congenital anomalies 4,848 1,421 22.7%
Small for gestational age (SGA)No SGA 5,554 715 11.4%
Fetal presentationEveryone cephalic 5,881 388 6.2%
Organisational factors
Travel time to hospitalEveryone no travel time 6,458 -189* *
Day and time of deliveryEveryone on weekdays 08:00-17:59 5,564 705 11.2%
Referral during parturitionNo referrals 6,076 193 3.1%
Hospital ‘elective-caesarean-section- for-term-breech’ percentageEvery hospital the average % 5,444 825 13.2%
Principal component factorsAll principal component factors set to the most favorable value 5,240 1,029 16.4%
Groups of factors
All maternal factors set to the most favorable value 5,450 819 13.1%
All child factors set to the most favorable value 1,004 5,265 84.0%
All organisational factors set to the most favorable value 4,120 2,149 34.3%
All mother and child factors set to the most favorable value 811 5,458 87.1%
All child and organisational factors set to the most favorable value 438 5,831 93.0%
All maternal, child and organisational factors set to the most favorable value
352 5,917 94.4%
* In table 5.3 ‘travel time to hospital’ has an OR of 0.995 representing a 0.5% decreased risk of perinatal mortality for every minute of extra travel time. Therefore, predicted mortality > observed mortality when everyone in the duplicate dataset is assigned a 0 for travel time. This would result in a negative PAR according to our calculation method.
factor value, perinatal mortality would be reduced with 16.4%. According to the ‘univariable
contribution’ estimation method, the estimated PAR of all maternal factors combined is
13.1%. Univariable contribution of the child factors combined and the organisational factors
combined is 84.0% and 34.3%, respectively. The PAR of all maternal, child and organisational
factors together is 94.4%. In other words: when all factors are set to the most favourable

77
POPU
LATION
ATTRIBUTA
BLE RISKS FOR PERIN
ATAL M
ORTA
LITY
5
value the perinatal mortality is expected to be reduced with 94.4%, pointing to a high
explanatory power of the complete set of variables in this analysis.
Table 5.5 compares results from the ‘descending order contribution’ vs. the ‘ascending order
contribution’. The former estimation method results in a PAR of 13.1%, 74.0% and 7.3% for
maternal, child and organisational factors, respectively. The latter estimation method results
in a PAR of 34.3%, 58.7% and 1.4% for organisational, child and maternal factors, respectively.
Hence, depending on the estimation method, the PAR of maternal factors varies from 1.4 to
13.1%; for child factors from 58.7 to 74.0%, and for organisational factors from 7.3 to 34.3%.
DISCUSSION
Principal fi ndings
Combining a multilevel logistic regression approach with a specific ‘what-if’ framework,
we were able to estimate the impact of maternal, child and organisational risk factors
on perinatal mortality. We estimated the combined population attributable risk (PAR) of
Table 5.5 PARs of groups of risk factors estimated by two methods: ‘descending order contribution’ (left) and ‘ascending order contribution’ (right)
↓
MATERNAL FACTORS 13.1% 94.4% MATERNAL FACTORS
↓ +74.0% +1.4% ↑CHILD FACTORS 87.1% 93.0% CHILD FACTORS
↓ +7.3% +58.7% ↑ORGANISATIONAL FACTORS 94.4% 34.3% ORGANISATIONAL FACTORS
↑

78
POPU
LATION
ATTRIBUTA
BLE RISKS FOR PERIN
ATAL M
ORTA
LITY
5
patient- (maternal and child) and non-patient (organisational) factors to be 94.4%. Thus,
almost all perinatal mortality could be explained statistically. Gestational age showed the
highest single contribution (PAR of 72.2%), but also organisational factors as single factors
ranked high (PAR of 34.3%). In estimating the risk attributions for combined maternal, child
and organisational factors, results depended on the causal priority given on the various
risk groups. By selecting a ‘descending order’ the PARs of maternal, child and organisational
factors are 13.1%, 74.0% and 7.3%, respectively. The reverse order provides PARs of 34.3%,
58.7% and 1.4%, which can be translated into the following: optimising organisational
factors with the current pregnant population has a potential of a one third decrease in
perinatal mortality.
Also, our data showed the overriding importance of decreasing preterm births, and a
distinct >200% risk of a birth at 37.0-37.6 weeks of gestation (table 5.3, OR 2.35), considered
‘at term’6. This finding suggests reconsidering the threshold of ‘term’ pregnancy from 37
weeks to 38 weeks.19,20
Other PAR studies
Previous studies describing PARs for perinatal mortality have used multivariable regression
models with the resulting adjusted odds ratio (OR) replacing the relative risk (RR) in the
conventional PAR formula (depicted in the methods section).18,21-23 Two previous studies have
used data from The Netherlands Perinatal Registry to calculate PARs for perinatal mortality,
however with each a different approach.11,22 Ravelli and colleagues calculated adjusted PARs
for perinatal mortality (stillbirths included) through multivariable regression and adjusted
odds ratios (see above). Focusing on maternal factors only, they showed nulliparity to have
the highest PAR for perinatal mortality (14.8%), considerably more than e.g. maternal age
(PAR 1.4-3.6%), ethnicity (PAR 6.6%), and gender of the child (PAR 3.6%).22 The difference
with our PARs arises from the absence of child and organisational factors, the different
computational procedure (see Methods), and the inclusion of stillbirths. Gijsen et al. used
a method comparable to our multilevel and ‘observed-expected’ method in estimating
perinatal mortality attributable to the effect of an off-hours delivery.11 They found an overall
PAR of 12.5% of evening and night time deliveries for intrapartum and early neonatal
mortality. A limitation of this study is the exclusion of several groups at risk for intrapartum
and early neonatal mortality, e.g., small for gestational age infants and severe congenital
anomalies which most likely are more vulnerable to suboptimal care.

79
POPU
LATION
ATTRIBUTA
BLE RISKS FOR PERIN
ATAL M
ORTA
LITY
5
Strengths and weaknesses
An important strength of our study is the usage of a validated national database (The
Netherlands Perinatal Registry) with complete coverage of all deliveries over a long period
of time (2000-2008). Second, compared to previous studies, our explanatory model included
more detailed information on organisational factors from all Dutch hospitals, built on a
previous study on hospital related effects.6,11,22 Third, we used a novel method to calculate
PARs in a multivariable context, and demonstrated a strong effect of the researcher’s choice
of explanatory variables (‘ascending and ‘descending order contribution’) and on the order
of including these variables in computing PARs.
Provided that appropriate choices are made, we assume the resulting multivariable PARs
to be more accurate compared to PAR estimations from the conventional PAR-formula
which is unsuitable in case of interacting variables.18 Generally, a multivariable PAR provides
additional information beyond measures on the strength of association.4-6,8,9,24-26 For example:
a placental abruption may have a high OR for perinatal mortality; however, on the population
level its attributable risk is limited as the condition is very rare; PARs account for this.10
This study also has limitations. First, the lack of detailed data on maternal lifestyle factors
in The Netherlands Perinatal Registry, in particular smoking, may contribute to a too small
PAR of maternal factors.27 By including SGA and gestational age in our study model part
of this maternal smoking effect is switched to these child factors. Still, in view of the low
PAR of maternal factors, our study suggests that in the perinatal mortality context, casemix
adjustment for maternal factors is of less value than often assumed.1-3 A second limitation
refers to the modifiability of risk factors, which is not addressed by our method. In public
health, PARs are generally calculated for modifiable risk factors only as the concept is used
to judge priorities for intervention programs. Some risk factors in our study obviously are
non-modifiable (e.g., parity or ethnicity), and others only partially. Still, the small PARs
on parity and ethnicity may serve the discussion on relevance and prioritisation. Finally,
we by intent excluded births under supervision of independently practicing midwives
(n=525,479 from a total of 1,620,126). Our results only pertain to hospital births; as in most
Western countries births take place in hospital this selection may account for international
generalisability of our results.
Possible implications
In assuming organisational factors to be modifiable at least partially on the long term, our
study suggests a major decrease in perinatal mortality (PAR of 34%) after these factors have

80
POPU
LATION
ATTRIBUTA
BLE RISKS FOR PERIN
ATAL M
ORTA
LITY
5
been optimised. Possible policies include ensuring (e)quality of obstetric care during off-
hours, and a proactive approach in obstetric policy. Centralisation of obstetric care may be
deemed necessary in optimising organisational factors ensuring 24-hour high level obstetric,
anaesthesia, and optimal neonatal resuscitation coverage.28 Next to organisational factors,
the PAR estimations of child factors suggest substantial reduction of perinatal mortality on
the population level through measures decreasing preterm birth rates. Foremost, methods
to improve detection of (risks for) preterm are needed which may be achieved through
standardised antenatal risk scoring systems, or prediction algorithms for preterm birth.29,30
The threshold of term may be shifted to 38 weeks gestational age.
Conclusion
We quantified the overall impact on in-hospital perinatal mortality of maternal, child, and
organisational risk factors, adjusting for their mutual dependencies. The so-called population
attributable risk (PAR) of these three groups of factors combined is 94.4%, where gestational
age has the highest single impact. The PARs of risk factors separately vary by the method
of estimation, in particular the order of adjustment which in turn depends on the intended
use. Focusing on the role of hospital organisational factors, the PAR results suggest that
a change towards the theoretical organisation optimum with an otherwise unchanged
pregnant population provides a 34.3% decrease in in-hospital perinatal mortality.
REFERENCES1. Buitendijk SE, Nijhuis JG. High perinatal mortality
in the Netherlands compared to the rest of Europe. Ned Tijdschr Geneeskd. 2004;148:1855-1860.
2. Mohangoo AD, Buitendijk SE, Hukkelhoven CW, et al. Higher perinatal mortality in The Netherlands than in other European countries: the Peristat-II study. Ned Tijdschr Geneeskd. 2008;152:2718-2727.
3. Anthony S, Jacobusse GW, van der Pal-de Bruin KM, Buitendijk S, Zeitlin J, Factors E-PWGoR. Do differences in maternal age, parity and multiple births explain variations in fetal and neonatal mortality rates in Europe?--Results from the EURO-PERISTAT project. Paediatr Perinat Epide-miol. 2009;23:292-300.
4. Evers AC, Brouwers HA, Hukkelhoven CW, et al. Perinatal mortality and severe morbidity in low and high risk term pregnancies in the Netherlands: prospective cohort study. BMJ. 2010;341:c5639.
5. Ravelli AC, Jager KJ, de Groot MH, et al. Travel time from home to hospital and adverse perinatal outcomes in women at term in the Netherlands. BJOG. 2011;118:457-465.
6. de Graaf JP, Ravelli AC, Visser GH, et al. Increased adverse perinatal outcome of hospital delivery at night. BJOG. 2010;117:1098-1107.
7. Poeran J, Denktas S, Birnie E, Bonsel GJ, Steegers EA. Urban perinatal health inequalities. J Matern Fetal Neonatal Med. 2011;24:643-646.

81
POPU
LATION
ATTRIBUTA
BLE RISKS FOR PERIN
ATAL M
ORTA
LITY
5
8. Ravelli AC, Steegers EA, Rijninks-van Driel GC, et al. Differences in perinatal mortality between districts of Amsterdam. Ned Tijdschr Geneeskd. 2011;155:A3130.
9. Timmermans S, Bonsel GJ, Steegers-Theunissen RP, et al. Individual accumulation of heterogeneous risks explains perinatal inequalities within deprived neighbourhoods. Eur J Epidemiol. 2011; 26:165-180.
10. Altman DG. Strategies for community health intervention: promises, paradoxes, pitfalls. Psy-chosom Med. 1995;57:226-233.
11. Gijsen R, Hukkelhoven CW, Schipper CM, Ogbu UC, de Bruin-Kooistra M, Westert GP. Effects of hospital delivery during off-hours on perinatal outcome in several subgroups: a retrospective cohort study. BMC Pregnancy Childbirth. 2012;12:92.
12. Perinatal care in The Netherlands 2008 (in Dutch: Perinatale zorg in Nederland 2008). Utrecht: The Netherlands Perinatal Registry; 2011.
13. Stillbirth Collaborative Research Network Writing G. Causes of death among stillbirths. JAMA. 2011;306:2459-2468.
14. Burstyn I. Principal component analysis is a powerful instrument in occupational hygiene inquiries. Ann Occup Hyg. 2004;48:655-661.
15. Manning, FA. Intrauterine growth retardation. In: Manning, FA, ed. Fetal medicine: Principles and practice. Appleton and Lange, Norwalk, CT 1995.
16. Mikolajczyk RT, Zhang J, Betran AP, et al. A global reference for fetal-weight and birthweight percentiles. Lancet. 2011;377:1855-1861.
17. Rietberg CCT. Term breech delivery in The Netherlands; chapter 7. Thesis 2006, University of Utrecht. (online available: http://igitur-archive.library.uu.nl/dissertations/2006-1031-200813/c7.pdf ).
18. Benichou J. A review of adjusted estimators of attributable risk. Stat Methods Med Res. 2001; 10:195-216.
19. Fleischman AR, Oinuma M, Clark SL. Rethinking the definition of “term pregnancy”. Obstet Gynecol. 2010;116:136-139.
20. Reddy UM, Bettegowda VR, Dias T, Yamada-Kushnir T, Ko CW, Willinger M. Term pregnancy: a period of heterogeneous risk for infant mortality. Obstet Gynecol. 2011;117:1279-1287.
21. Hutcheon JA, McNamara H, Platt RW, Benjamin A, Kramer MS. Placental weight for gestational age and adverse perinatal outcomes. Obstet Gynecol.119:1251-1258.
22. Ravelli AC, Tromp M, van Huis M, et al. Decreasing perinatal mortality in The Netherlands, 2000-2006: a record linkage study. J Epidemiol Community Health. 2009;63:761-765.
23. Cruz-Anguiano V, Talavera JO, Vazquez L, et al. The importance of quality of care in perinatal mortality: a case-control study in Chiapas, Mexico. Arch Med Res. 2004;35:554-562.
24. de Graaf JP, Ravelli AC, Wildschut HI, et al. Perinatal outcomes in the four largest cities and in deprived neighbourhoods in The Netherlands. Ned Tijdschr Geneeskd. 2008;152:2734-2740.
25. Tromp M, Eskes M, Reitsma JB, et al. Regional perinatal mortality differences in the Netherlands; care is the question. BMC Public Health. 2009;9: 102.
26. van den Hooven EH, Pierik FH, de Kluizenaar Y, et al. Air pollution exposure during pregnancy, ultrasound measures of fetal growth, and adverse birth outcomes: a prospective cohort study. Environ Health Perspect. 2012;120:150-156.
27. Andres RL, Day MC. Perinatal complications associated with maternal tobacco use. Semin Neonatol. 2000;5:231-241.
28. Heller G, Richardson DK, Schnell R, Misselwitz B, Kunzel W, Schmidt S. Are we regionalized enough? Early-neonatal deaths in low-risk births by the size of delivery units in Hesse, Germany 1990-1999. Int J Epidemiol. 2002;31:1061-1068.
29. Davey MA, Watson L, Rayner JA, Rowlands S. Risk scoring systems for predicting preterm birth with the aim of reducing associated adverse outcomes. Cochrane Database Syst Rev. 2011:CD004902.
30. Schaaf JM, Ravelli AC, Mol BW, Abu-Hanna A. Development of a prognostic model for predict-ing spontaneous singleton preterm birth. Eur J Obstet Gynecol Reprod Biol. 2012;164:150-155.

82
POPU
LATION
ATTRIBUTA
BLE RISKS FOR PERIN
ATAL M
ORTA
LITY
5

6The ‘Healthy Pregnancy 4 All’ Study:
design and cohort profile
S. Denktaş, J. Poeran, L.C. de Jong-Potjer, S.F. van Voorst, A.A. Vos, A.J.M. Waelput, E. Birnie, G.J. Bonsel, E.A.P. Steegers
Manuscript submitted for publication.

84
THE ‘H
EALTH
Y PREGN
AN
CY 4 ALL’ STU
DY
6
ABSTRACTThe design of a national study designated as ‘Healthy Pregnancy 4 All’ (HP4All) is presented.
This study combines epidemiologic and health services research to evaluate the effectiveness
of two obstetric interventions: (1) programmatic preconception care (PCC) provision to
reduce the risks and risk load related adverse pregnancy outcome in a population-based
prospective cohort study; (2) a score card-based antenatal risk assessment in a cluster
randomised controlled trial for medical and non-medical risks related to adverse pregnancy
outcome, followed by patient-tailored multidisciplinary care pathways. Altogether, 14
municipalities/regions were selected to participate according to socio-demographic data
(high risk load), perinatal outcome data (high adverse outcome prevalence), and some
specific data for either PCC or antenatal risk assessment. In total, 839 women need to be
included in the preconception care study and 7,000 women need to be included in the
antenatal risk assessment study. Data are collected by physical examinations, questionnaires,
interviews, and biological samples. Preparations started in the spring of 2011. Participant
recruitment and complete data collection started in the fall of 2012.

85
THE ‘H
EALTH
Y PREGN
AN
CY 4 ALL’ STU
DY
6
INTRODUCTIONPerinatal mortality rates in the Netherlands are high and decline slowly compared to other
European countries.1-3 More risks and a higher risk load for adverse outcomes were found
for women living in socially deprived areas.4 With the support of the Ministry of Health
and Welfare a nationwide study, called ‘Healthy Pregnancy 4 All’ (HP4All), was developed
to provide evidence based strategies at an early stage to improve pregnancy outcome.
Several municipal pilot studies in the city of Rotterdam provided the framework for this
national study.5
Main objectives
The main HP4All study objective is to evaluate the effectiveness of two interventions and
their associated preventive strategies in either the preconception period or the antenatal
period to reduce adverse pregnancy outcome. Accordingly, two sub-studies are specified:
a population-based prospective cohort study focusing on the effectiveness of customised
preconception care (PCC) and a cluster randomised trial focusing on the early identification
of groups at risk for adverse pregnancy outcomes (in particular, preterm birth and small
for gestational age) and the related effectiveness of score-card based early antenatal risk
assessment with the so-called ‘R4U’ (Rotterdam Reproductive Risk Reduction) score card.
Rationale
The rationale of the PCC sub-study originates from increasing evidence showing the
critical influence of embryonic development and placentation during early pregnancy on
pregnancy outcome.6-8 Risks influencing this early pregnancy phase are optimally modified
in the preconception period.6,9,10 The Dutch Health Council recommended (2007) to integrate
general PCC in the health care system.11 The Minister of Health, however, advised to first
evaluate the utilisation and effectiveness of PCC for high risk groups in the HP4All study,
before the nationwide implementation of PCC in Dutch obstetric care can be considered.
The rationale of the second sub-study on early antenatal risk assessment originates from the
unique Dutch system of obstetric care which has three risk-based levels of care: primary care
for low risk pregnancies and deliveries, provided by independently practicing community
midwives, and secondary/tertiary care for high risk pregnancies provided by obstetricians.12
As the level of care depends on the distinction between assumed low risk and high risk
pregnancies, antenatal risk assessment by primary care community midwives is an important

86
THE ‘H
EALTH
Y PREGN
AN
CY 4 ALL’ STU
DY
6
part of Dutch obstetric care.12 Although social deprivation has been shown to contribute to
adverse perinatal health in the Netherlands, standard risk assessment does not include the
assessment of social risks of perinatal health.4,5,13,14 In addition, subsequent patient-tailored
social care pathways are lacking. Therefore, in the new antenatal risk assessment tool (‘R4U’)
explicitly social and medical risk factors are taken into account as part of the HP4All study.
Population-based cohort studies, e.g., the Generation R15 and ABCD16 studies have
contributed to our knowledge of various health problems in pregnancy and childhood
and their lasting impact on health in later life. Moreover, studies using a large national
Dutch database (The Netherlands Perinatal Registry) showed increased adverse pregnancy
outcome in large urban areas, in particular in deprived neighbourhoods.13,17 Also, four
specific morbidities appear to precede perinatal mortality in 85% of cases, the so-called ‘Big4’
morbidities.18,19 These are: congenital anomalies (list defined), preterm birth (<37th week
of gestation), small for gestational age (SGA, birth weight <10th percentile for gestational
age) or low Apgar score (<7, 5 minutes after birth). Taking advantage of knowledge from
these cohort studies, the HP4All study will study the effectiveness of newly introduced
evidence-based care strategies for early identification and customised care provision to
women at risk.
Below, we first describe the selection of geographical areas most suitable for the
interventions. Next, we describe the designs of the preconception care and the antenatal
risk assessment studies.
SELECTION OF THE PARTICIPATING MUNICIPALITIES/REGIONSThe first step in HP4All was the identification of the geographical unit in which the
aforementioned sub-studies would preferably be carried out. We used a national geographic
information system (GIS) to divide The Netherlands into 62 municipalities/regions, being
the 50 cities with > 70,000 inhabitants and the 12 provinces (excluding the 50 previously
selected cities). The second step involved the selection of municipalities/regions in which
to carry out the sub-studies, based on multiple criteria which are relevant to either the
preconception care sub-study, to the enhanced antenatal risk assessment sub-study,
or to both. The final step dealt with additional conditions and the final selection of the
participating municipalities/regions which is elaborated on below.

87
THE ‘H
EALTH
Y PREGN
AN
CY 4 ALL’ STU
DY
6
Selection criteria
Initially, we selected municipalities/regions according to socio-demographic parameters
associated with high risk load (maternal age, parity, ethnicity, and socioeconomic status)
and perinatal outcome data (overall ‘Big4’ and perinatal mortality prevalence). Before the
municipalities/regions could be selected, specific parameters relevant to either sub-study
PCC or antenatal risk assessment were added.
For the PCC sub-study these criteria were (1) proportion of women having their first antenatal
booking visit at ≥14 weeks of gestational age, and prevalences of (2) congenital anomalies
and of (3) SGA. A timely first antenatal booking is important because the opportunities
for prenatal screening and interventions (i.e., lifestyle advice and changes) as well as the
effectiveness of those interventions are larger in an early fetal stage. Congenital anomaly and
SGA prevalences are considered to be indicative for a region’s periconceptional health status.
For the antenatal risk assessment sub-study, additional criteria were (1) overall perinatal
mortality rates, (2) perinatal mortality amongst women with ‘Big4’ pregnancies, and (3)
prevalence of SGA and prematurity.
Data sources
The division of The Netherlands into 62 municipalities/regions was based on 4-digit postal
codes areas. Data were provided by the Falk company (www.falk.nl), the National Public
Health Authority, and the Statistics Netherlands organisation (CBS, www.cbs.nl). Information
on socioeconomic status (SES, determined in 2006) per postal code area was obtained from
the Social and Cultural Planning Office (SCP, www.scp.nl). Data on pregnancy and perinatal
outcome were derived from The Netherlands Perinatal Registry (2000-2008), containing
information of more than 97% of all pregnancies in The Netherlands.20 These data are
routinely collected by 94% of midwives, 99% of gynaecologists and 68% of paediatricians
including 100% of Neonatal Intensive Care Unit paediatricians.20 Table 6.1 shows the
demographic characteristics of the so-called ‘G4-cities’, i.e., the four largest cities: Amsterdam,
Rotterdam, The Hague, Utrecht, and the rest of the Netherlands. Compared to the rest of The
Netherlands, the ‘G4’-cities have a larger proportion of non-Western women (43% vs. 11.3%),
more teenage pregnancies (2.8% vs. 1.5%), and more women in low SES neighbourhoods
(59.2% vs. 19.0%). Considerably more women live in deprived neighbourhoods (32.5% vs.
1.3%) and the overall adverse perinatal outcome is worse in ‘G4-cities’, as illustrated by a
‘Big4’ prevalence of 20.5% compared to 18.1%.

88
THE ‘H
EALTH
Y PREGN
AN
CY 4 ALL’ STU
DY
6
Table 6.1 Demographic characteristics of the study population by yes/no ‘G4-cities’ (the four largest cities) with percentages in brackets
G4-cities Netherlands minus G4-cities
Total
No. of pregnancies during study period 245,445 (100.0) 1,338,420 (100.0) 1,583,865 (100.0)
ParityPrimiparous 121,592 (49.5) 607,953 (45.4) 729,545 (46.1)Multiparous 123,853 (50.5) 730,467 (54.6) 854,320 (53.9)
EthnicityWestern 139,786 (57.0) 1,186,772 (88.7) 1,326,558 (83.8)Non-Western 105,659 (43.0) 151,648 (11.3) 257,307 (16.2)
Maternal age< 20 years 6,987 (2.8) 19,861 (1.5) 26,848 (1.7)20-24 years 34,864 (14.2) 127,013 (9.5) 161,877 (10.2)25-29 years 61,354 (25.0) 395,138 (29.5) 456,492 (28.8)30-34 years 85,444 (34.8) 535,927 (40.0) 621,371 (39.2)≥ 35 years 56,796 (23.1) 260,481 (19.5) 317,277 (20.0)
Socioeconomic 'status score'<p20 145,367 (59.2) 254,607 (19.0) 399,974 (25.3)p20-p80 58,641 (23.9) 853,074 (63.7) 911,715 (57.6)>p80 41,437 (16.9) 230,739 (17.2) 272,176 (17.2)
NeighbourhoodNon-deprived 165,658 (67.5) 1,320,392 (98.7) 1,486,050 (93.8)Deprived 79,787 (32.5) 18,028 (1.3) 97,815 (6.2)
Perinatal outcomes**Congenital anomalies 5,233 (2.1) 33,159 (2.5) 38,392 (2.4)Preterm birth 15,673 (6.4) 81,646 (6.1) 97,319 (6.1)Small for gestational age 27,724 (11.3) 125,175 (9.4) 152,899 (9.7)Apgar score <7 (5 minutes after birth) 3,385 (1.4) 14,818 (1.1) 18,203 (1.1)
Any Big4** 50,267 (20.5) 242,697 (18.1) 292,964 (18.5)
Fetal mortality† 1,478 (0.6) 6,718 (0.5) 8,196 (0.5)
Intrapartum mortality 458 (0.2) 2,126 (0.2) 2,584 (0.2)
Neonatal mortality†† 761 (0.3) 3,547 (0.3) 4,308 (0.3)
Perinatal mortality‡ 2,697 (1.1) 12,391 (0.9) 15,088 (1.0)
** Individual 'Big4' morbidities do not add up to 'any Big4' as women can have >1 'Big4' morbidity.† From 22 weeks of gestational age.†† 0-7 days postpartum.‡ Total of fetal, intrapartum and neonatal mortality.

89
THE ‘H
EALTH
Y PREGN
AN
CY 4 ALL’ STU
DY
6
Perinatal mortality and ‘Big4’ prevalence
Figures 6.1 and 6.2 illustrate the geographical distribution of perinatal mortality rates, and
the prevalence rate of ‘Big4’ (per 1,000) respectively. Various shades of red represent the
different prevalence classes, the darker the shade the more prevalent the adverse outcome.
The classes are based on the distribution of the rates: the middle three classes comprise 95%
(2 standard deviations) of the outcome levels; the middle class comprises 68%. Both figures
show large geographical inequalities in adverse perinatal outcomes on the national level.
Figure 6.1 Absolute prevalence of perinatal mortality per 1,000 births.

90
THE ‘H
EALTH
Y PREGN
AN
CY 4 ALL’ STU
DY
6
Comparison municipalities/regions
We additionally compared these outcomes across regions after direct standardisation21 for
population differences by maternal age, parity, ethnicity, and SES. Standardisation is needed
because a region with, e.g., a high number of non-Western women or a high number of
teenage pregnancies will generally have a higher prevalence of adverse perinatal outcomes.
Tables 6.2 and 6.3 show the socio-demographic parameters and the specific criteria for the
PCC and the antenatal risk assessment sub-studies. For each specific indicator we present
Figure 6.2 Absolute prevalence of ‘Big4’ morbidities per 1,000 births.

91
THE ‘H
EALTH
Y PREGN
AN
CY 4 ALL’ STU
DY
6
Ta
ble
6.2
Se
lect
ion
crite
ria*
for t
he p
reco
ncep
tion
care
exp
erim
ent w
ith s
corin
g in
dec
iles;
the
high
er d
ecile
s re
pres
ent a
mor
e lik
ely
qual
ifica
tion
for i
nclu
sion
Dem
ogra
phic
s1s
t ant
enat
al b
ooki
ng
≥14W
Cong
enita
l ano
mal
ies
SGA
Rank
#%
PR
EGAG
E <2
0N
W
ETH
NLO
W
SES
ABS
STN
DIN
EQA
BSST
ND
INEQ
ABS
STN
DIN
EQ
Cit
ies
1A
mst
erda
m10
810
1010
103
32
78
69
962
Rott
erda
m10
1010
1010
103
67
410
96
105
3D
en H
aag
910
1010
1010
29
84
109
810
94
Utr
echt
93
106
1010
410
107
32
791
5Ei
ndho
ven
87
97
99
68
98
99
510
36
Tilb
urg
88
99
54
104
45
1010
389
7A
lmer
e8
710
310
91
77
69
88
938
Gro
ning
en c
ity7
95
92
25
22
45
35
609
Bred
a7
66
53
19
99
36
74
7510
Nijm
egen
75
69
33
94
56
88
679
11En
sche
de6
88
104
42
55
39
76
7712
Ape
ldoo
rn6
53
26
74
11
95
410
6313
Haa
rlem
73
76
87
31
27
44
766
14A
rnhe
m6
99
88
57
66
37
75
8615
Zaan
stad
64
86
77
12
32
54
863
16A
mer
sfoo
rt7
27
49
97
56
63
24
7117
Haa
rlem
mer
mee
r7
14
14
54
11
22
27
4118
's-H
erto
genb
osch
53
34
12
109
94
88
470
19Zo
eter
mee
r5
68
31
16
44
17
610
6220
Zwol
le6
73
42
37
21
72
110
5521
Maa
stric
ht4
94
64
310
1010
1010
101
91
Tabl
e 6.
2 co
ntin
ues o
n ne
xt p
age.

92
THE ‘H
EALTH
Y PREGN
AN
CY 4 ALL’ STU
DY
6
Ta
ble
6.2
Co
ntin
ued
Dem
ogra
phic
s1s
t ant
enat
al b
ooki
ng
≥14W
Cong
enita
l ano
mal
ies
SGA
Rank
#%
PR
EGAG
E <2
0N
W
ETH
NLO
W
SES
ABS
STN
DIN
EQA
BSST
ND
INEQ
ABS
STN
DIN
EQ
22D
ordr
echt
610
97
98
32
13
77
880
23Le
iden
54
76
88
68
710
65
383
24Em
men
46
110
45
102
27
64
970
25Ed
e5
63
55
66
78
21
15
6026
Venl
o3
78
73
28
66
59
101
7527
Wes
tland
41
11
57
610
108
11
1065
28D
even
ter
56
68
78
77
72
77
279
29D
elft
37
99
75
710
1010
55
693
30Si
ttar
d-G
elee
n3
83
71
210
54
49
81
6531
Leeu
war
den
410
49
54
88
82
53
1080
32A
lkm
aar
44
65
66
85
510
22
265
33H
eerle
n2
105
103
48
1010
310
102
8734
Hel
mon
d5
57
66
54
88
59
101
7935
Hilv
ersu
m1
55
39
91
11
83
51
5236
Súdw
est F
rysl
ân3
51
82
29
22
101
13
4937
Am
stel
veen
21
82
88
11
110
21
1055
38H
enge
lo4
64
75
61
43
14
45
5439
Purm
eren
d2
46
49
101
35
14
69
6440
Roos
enda
al2
59
12
18
99
88
101
7341
Oss
22
43
11
75
49
1010
260
42Sc
hied
am1
1010
1010
102
76
410
97
9643
Spijk
enis
se1
97
43
25
33
16
94
57

93
THE ‘H
EALTH
Y PREGN
AN
CY 4 ALL’ STU
DY
6
44Le
idsc
hend
am-V
oorb
urg
22
73
87
55
49
35
565
45A
lphe
n a/
d Ri
jn1
25
14
49
78
14
46
5646
Alm
elo
38
58
23
11
19
76
155
47Vl
aard
inge
n1
810
57
48
65
98
84
8348
Gou
da3
38
83
19
13
34
33
5249
Mid
delb
urg
19
47
66
48
66
43
367
50Vl
issi
ngen
110
65
86
56
81
89
376
Pro
vin
ces
51G
roni
ngen
87
29
79
53
28
56
778
52Fr
iesl
and
94
18
99
310
108
23
985
53D
rent
he9
31
56
86
44
23
58
6454
Ove
rijss
el9
11
25
72
33
61
29
5155
Gel
derla
nd10
22
21
33
109
92
36
6256
Utr
echt
101
31
23
59
95
11
757
57N
oord
-Hol
land
101
22
78
26
65
11
859
58Zu
id-H
olla
nd10
22
14
54
87
71
29
6259
Zeel
and
83
13
1010
24
51
35
459
60N
oord
-Bra
bant
101
21
11
97
75
67
259
61Li
mbu
rg9
42
21
110
910
67
82
7162
Flev
olan
d8
95
46
66
33
96
67
78
10%
HIG
EST
SCO
RE
10%
-20%
H
IGH
EST
SCO
RE
10%
LO
WES
T SC
ORE
* ‘%
PRE
G’:
% p
regn
ant w
omen
in th
e ge
nera
l pop
ulat
ion
/ ‘AG
E <2
0’: %
teen
age
preg
nanc
ies
/ ‘N
W E
THN
’: %
non
-Wes
tern
pre
gnan
t wom
en /
‘LO
W S
ES’:
% w
omen
in
neig
hbou
rhoo
ds w
ith a
soci
oeco
nom
ic st
atus
scor
e <p
20 /
‘ABS
’: A
bsol
ute
% /
‘STN
D’:
Stan
dard
ised
% /
‘INEQ
’: In
equa
lity
as m
easu
red
by th
e re
lativ
e ris
k of
pre
vale
nces
be
twee
n w
omen
from
nei
ghbo
urho
ods
with
soc
ioec
onom
ic s
tatu
s sc
ore
<p20
com
pare
d to
>p8
0.

94
THE ‘H
EALTH
Y PREGN
AN
CY 4 ALL’ STU
DY
6
Ta
ble
6.3
Se
lect
ion
crite
ria* f
or th
e ris
k se
lect
ion
expe
rimen
t with
scor
ing
in d
ecile
s; th
e hi
gher
dec
iles r
epre
sent
a m
ore
likel
y qu
alifi
catio
n fo
r inc
lusi
on
Dem
ogra
phic
sPe
rinat
al m
orta
lity
/ al
l wom
enPe
rinat
al m
orta
lity
/ BI
G4
mor
bidi
ties
Perin
atal
mor
talit
y /
star
t lab
our i
n pr
imar
y ca
re
Rank
#%
PR
EGAG
E <2
0PR
IMI
NW
ET
HN
LOW
SE
SA
BSST
ND
INEQ
ABS
STN
DIN
EQA
BSST
ND
INEQ
Cit
ies
1A
mst
erda
m10
810
1010
86
98
77
75
811
32
Rott
erda
m10
107
1010
1010
36
73
109
511
03
Den
Haa
g9
107
1010
98
76
74
108
911
44
Utr
echt
93
910
69
92
910
27
65
965
Eind
hove
n8
79
97
55
42
22
98
683
6Ti
lbur
g8
87
99
88
64
58
99
310
17
Alm
ere
87
410
38
103
58
36
77
898
Gro
ning
en7
910
59
79
18
93
21
787
9Br
eda
76
66
53
47
24
67
83
7410
Nijm
egen
75
86
910
104
1010
26
67
100
11En
sche
de6
85
810
99
48
63
98
396
12A
peld
oorn
65
43
28
88
98
83
410
8613
Haa
rlem
73
97
64
68
56
93
27
8214
Arn
hem
69
109
89
49
96
85
28
102
15Za
anst
ad6
46
86
21
12
14
56
456
16A
mer
sfoo
rt7
26
74
1010
510
107
11
888
17H
aarle
mm
erm
eer
71
54
14
37
76
71
16
6018
's-H
erto
genb
osch
53
103
46
53
44
56
75
7019
Zoet
erm
eer
56
68
31
12
11
16
710
5820
Zwol
le6
76
34
62
58
42
41
1068
21M
aast
richt
49
84
68
78
32
610
96
9022
Dor
drec
ht6
104
97
21
32
15
74
1071

95
THE ‘H
EALTH
Y PREGN
AN
CY 4 ALL’ STU
DY
6
23Le
iden
54
107
64
29
32
94
53
7324
Emm
en4
64
110
22
13
31
86
1061
25Ed
e5
61
35
74
99
510
13
270
26Ve
nlo
37
58
73
210
31
1010
102
8127
Wes
tland
41
11
11
28
11
88
79
5328
Dev
ente
r5
66
68
99
37
54
910
390
29D
elft
37
89
91
15
11
110
108
7430
Sitt
ard-
Gel
een
38
93
73
17
11
99
91
7131
Leeu
war
den
410
94
95
510
55
105
55
9132
Alk
maa
r4
47
65
22
104
310
34
165
33H
eerle
n2
1010
510
78
61
28
1010
493
34H
elm
ond
55
47
65
48
43
108
82
7935
Hilv
ersu
m1
510
53
75
210
86
33
472
36Sú
dwes
t Fry
slân
35
21
87
710
1010
101
17
8237
Am
stel
veen
21
38
21
110
75
91
110
6138
Hen
gelo
46
34
75
75
66
74
44
7239
Purm
eren
d2
48
64
23
95
49
79
577
40Ro
osen
daal
25
59
12
52
12
59
101
5941
Oss
22
54
33
47
12
78
76
6142
Schi
edam
110
910
1010
109
64
85
14
9743
Spijk
enis
se1
98
74
108
69
84
67
794
44Le
idsc
hend
am-V
oorb
urg
22
77
31
110
43
102
38
6345
Alp
hen
a/d
Rijn
12
85
110
101
1010
54
35
7546
Alm
elo
38
35
81
32
25
16
61
5447
Vlaa
rdin
gen
18
710
57
103
610
310
102
9248
Gou
da3
31
88
63
107
69
22
371
49M
idde
lbur
g1
91
47
13
13
42
22
242
50Vl
issi
ngen
110
46
56
91
47
18
101
73
Tabl
e 6.
3 co
ntin
ues o
n ne
xt p
age.

96
THE ‘H
EALTH
Y PREGN
AN
CY 4 ALL’ STU
DY
6
Ta
ble
6.3
Co
ntin
ued
Dem
ogra
phic
sPe
rinat
al m
orta
lity
/ al
l wom
enPe
rinat
al m
orta
lity
/ BI
G4
mor
bidi
ties
Perin
atal
mor
talit
y /
star
t lab
our i
n pr
imar
y ca
re
Rank
#%
PR
EGAG
E <2
0PR
IMI
NW
ET
HN
LOW
SE
SA
BSST
ND
INEQ
ABS
STN
DIN
EQA
BSST
ND
INEQ
#P
rov
ince
s
51G
roni
ngen
87
32
99
86
109
65
54
9152
Frie
slan
d9
42
18
109
59
94
46
989
53D
rent
he9
32
15
66
28
82
45
970
54O
verij
ssel
91
11
25
74
89
11
39
6155
Gel
derla
nd10
21
22
56
45
74
34
661
56U
trec
ht10
12
31
45
46
73
34
659
57N
oord
-Hol
land
101
32
24
67
79
61
28
6858
Zuid
-Hol
land
102
22
14
61
58
12
29
5559
Zeel
and
83
21
38
78
1010
52
31
7160
Noo
rd-B
raba
nt10
13
21
33
63
37
78
259
61Li
mbu
rg9
45
22
34
52
36
89
163
62Fl
evol
and
89
15
46
76
79
55
510
87
10%
HIG
EST
SCO
RE
10%
-20%
H
IGH
EST
SCO
RE
10%
LO
WES
T SC
ORE
* ‘%
PRE
G’:
% p
regn
ant w
omen
in th
e ge
nera
l pop
ulat
ion
/ ‘AG
E <2
0’: %
teen
age
preg
nanc
ies
/ ‘PR
IMI’:
% p
rimip
arou
s w
omen
/ ‘N
W E
THN
’: %
non
-Wes
tern
pre
gnan
t w
omen
/ ‘L
OW
SES
’: %
wom
en in
nei
ghbo
urho
ods
with
a s
ocio
econ
omic
sta
tus
scor
e <p
20 /
‘ABS
’: A
bsol
ute
% /
‘STN
D’:
Stan
dard
ised
% /
‘INEQ
’: In
equa
lity
as m
easu
red
by th
e re
lativ
e ris
k of
pre
vale
nces
bet
wee
n w
omen
from
nei
ghbo
urho
ods
with
soc
ioec
onom
ic s
tatu
s sc
ore
<p20
com
pare
d to
>p8
0.

97
THE ‘H
EALTH
Y PREGN
AN
CY 4 ALL’ STU
DY
6
the absolute rate (ABS), the standardised rate (STND) and the inequality-rate (INEQ), the
latter being expressed as the relative risk of the outcome for low SES pregnant women
compared to high SES pregnant women, after direct standardisation for maternal age,
parity and ethnicity.17 Next, to facilitate comparisons, we assigned decile scores to regions,
varying from one (the region is one of the 10% areas with best outcomes) to 10 (the region
belongs to the 10% worst outcomes). The sum of the decile scores for the various indicators
by region is shown in the last column (‘RANK’); higher scores imply unfavourable ranking.
For clarity, colors are used to differentiate between favourable and unfavourable outcomes:
green represents the first decile (with the best outcome), pink the 10th decile (10% with
the most adverse outcomes), amber the 10th-20th decile. Based on the sum of the decile
scores for the PCC sub-study (table 6.2), the pink and amber municipalities/regions have
the most adverse outcomes, i.e., 1. The Hague; 2. Rotterdam; 3. Eindhoven; 4. Amsterdam; 5.
Schiedam; 6. Almere ; 7. Delft; 8. Utrecht; 9. Maastricht; 10. Tilburg; 11. Heerlen; 12. Arnhem;
13. Friesland. According to the sum of the decile score for the risk assessment sub-study
(table 6.3) the following municipalities/regions show the most adverse outcomes: 1. The
Hague; 2. Amsterdam; 3. Rotterdam; 4. Arnhem; 5. Tilburg; 6. Nijmegen; 7. Schiedam; 8.
Utrecht; 9. Enschede; 10. Spijkenisse; 11. Heerlen; 12. Vlaardingen; 13. Groningen; 14.
Leeuwarden.
Additional to the identified municipalities, the province of Friesland best qualified for the
PCC sub-study and the province of Groningen for the risk assessment sub-study.
Final selection municipalities/regions
After the theoretical selection of the candidate municipalities/regions in the previous step,
the next step elaborated on the practical aspects of sub-study implementation in candidate
municipalities/regions, e.g., willingness to participate of local authorities and caregivers.
The candidate municipalities/regions were first presented to the Ministry of Health, after
which the Aldermen of these candidate municipalities/regions were consulted, which
resulted in a final selection. The participating municipalities/regions are (figure 6.3): in the
province of Groningen Appingedam/Delfzijl/Menterwolde/Pekela and Groningen city, the
municipalities of Enschede, Nijmegen, Heerlen, Tilburg, Schiedam, Utrecht, The Hague,
Amsterdam, and Almere.
All municipalities decided to participate in both sub-studies either as study or control. As a
separate municipal program on reducing perinatal mortality was already being carried out
in Rotterdam5, this city was not selected for participation in the HP4All study.

98
THE ‘H
EALTH
Y PREGN
AN
CY 4 ALL’ STU
DY
6
DESIGN OF THE PRECONCEPTION CARE SUBSTUDYIn this population-based prospective cohort study with a pre-post design for the
measurement of effectiveness of PCC, we approach all women in the fertile age (18-42
years) and invite them to visit Preconception Care Consultations if they contemplate
pregnancy. This sub-study consists of two consultations provided by midwives or general
practitioners (GP), the second consultation takes place three months after the first. During
Figure 6.3 Participating municipalities in the ‘Healthy Pregnancy 4 All’ project.
AppingedamDelfzijl
GroningenMenterwolde
Pekela
Enschede
Heerlen
Nijmegen
Tilburg
Schiedam
Utrecht
AlmereAmsterdam
The Hague

99
THE ‘H
EALTH
Y PREGN
AN
CY 4 ALL’ STU
DY
6
the first consultation, PCC risks are assessed and a tailored management plan is composed.
At the second consultation, reduction of the PCC risk load is measured, and if required, the
management plan is adapted.
Sample size calculation
The statistical design is based on a pre-post comparison with paired data. The primary
outcomes used for the sample size calculation are overall preconceptional folic acid
supplementation use and smoking cessation amongst smokers, as changes in these
behavioral risk factors have a major impact on perinatal health and can be measured by
biomarkers.22-24
The sample size was based on the following criteria:
1. Self-reported folic acid supplementation use. To reject the null hypothesis (H0: Δ ≤ 20%,
defined as the PCC program leading to a ≤ 20% increase of folic acid users in women
that were not already using folic acid supplements at baseline) a total sample size of
n= 839 is needed. Assumptions for the power calculation were (1) the smallest clinically
relevant difference (‘Δ’) is a 20% increase of folic acid use in non-users at baseline, (2) the
proportion of women using folic acid at baseline is 30% (π0=30%), (3) a-select drop-out
rate of 10%, (4) results are pairwise analysed, (5) a statistical significance level α <0.025
(1-sided, correction for multiple testing due to two primary outcome measures), and
(6) a power (1-β) of 0.80.
2. Smoking cessation. (1) To reject the null hypothesis (H0: Δ ≤ 5%, defined as smoking
cessation occurring in ≤ 5% of women that smoked at baseline) a total sample size of
n=687 is needed. Assumptions for the power calculation were (2) the smallest clinically
relevant difference (‘Δ’) is a 5% decrease of smoking compared to baseline, (3) the
proportion of smoking women at baseline is 30% (π0=30%), (4) the a-select drop-out
rate is 10%, (5) the results are pairwise analysed, (5) the significance level is α <0.025
(1-sided, correction for multiple testing due to two primary outcome measures), and
(6) the power (1-β) is 0.80.
Enrollment
Women are actively approached by: (1) an invitational letter from the municipal public health
service or municipality, and/or (2) an invitational letter from their GP, and/or (3) referral by
a youth healthcare physician or nurse, and/or (4) referral by a peer educator in perinatal

100
THE ‘H
EALTH
Y PREGN
AN
CY 4 ALL’ STU
DY
6
health. The precise mode of approach depends on specific local collaborative agreements
with the municipal authorities, the local public health authorities and the local caregivers.
In addition, participating GPs and midwives can recruit women regularly attending their
care. Furthermore, women within the community are informed about the PCC consultations
by flyers and posters. Each woman, including the method that they were recruited by, is
registered when a PCC visit at participating GP or midwife practices is scheduled. Women
are sent participant information leaflets with an informed consent form before they are
approached by telephone for inclusion. If women agree to participate they hand in the
informed consent form before their consultation.
Logistics and data collection
The logistics of the PCC sub-study are carried out in close collaboration with local project
coordinators and certified clinical laboratories in the 14 participating municipalities. The
PCC risk assessment is performed by the client prior to each consultation individually at a
convenient moment using the web-based validated ‘ZwangerWijzer’ (translated ‘Preparing
for pregancy’) internet questionnaire (www.zwangerwijzer.nl).25 GPs and midwives during
the consultations are supported professionally by the ‘Preconceptiewijzer’ (translated
‘Preparing for preconception care’) tool (www.preconceptiewijzer.nl)., ‘Preconceptiewijzer’
presents identified risk factors from ‘ZwangerWijzer’.This tool further provides GPs and
midwives both with protocols on management of PCC risk factors and with information
leaflets to hand out to the client.
Before the first PCC visit takes place, additional information will be collected from partici-
pating women: data on basic characteristics (e.g., educational level), general health (e.g.,
medical history), details on risk factors and health behaviours (primarily: folic acid use,
alcohol consumption, smoking, drug use, diet, preventive behaviours regarding Listeria/
Toxoplasmosis prevention, weight) , and attitudes towards PCC are collected by a digital
or on request by a paper - questionnaire (table 6.4). This questionnaire also includes
a cardiovascular risk score (My Life Check, American Heart association, online: http://
mylifecheck.heart.org/) and a risk score for diabetes (FINDRISK).26 To measure alterations
after the first PC consultation, clients are sent a digital or paper questionnaire regarding
their health behaviours (risk reduction or elimination) 3 months after the first consultation.
The same health behaviours are addressed as in the first questionnaire.
Additionally, protocol-based anthropometric measurements are performed (BMI, blood
pressure, waist- and hip circumference), and biomarkers are collected at both consultations.

101
THE ‘H
EALTH
Y PREGN
AN
CY 4 ALL’ STU
DY
6
Ta
ble
6.4
Pl
anne
d as
sess
men
ts in
the
prec
once
ptio
n ca
re e
xper
imen
t: pa
ram
eter
s, bi
omar
kers
, que
stio
nnai
res
and
outc
ome
Para
met
er
Bio
mar
ker
Que
stio
nnai
re O
utco
me
Folic
aci
d su
pple
tion
Eryt
rocy
te fo
late
, aft
er b
oth
cons
ulta
tions
Self-
repo
rted
folic
aci
d us
e•
Prev
alen
ce: f
olic
aci
d us
e m
easu
red
at b
asel
ine
with
ery
troc
yte
fola
te a
nd s
elf-r
epor
ted
use.
• Ef
fect
iven
ess
of p
reco
ncep
tion
care
: inc
reas
e in
num
ber o
f wom
en
usin
g fo
lic a
cid
(sel
f-rep
orte
d an
d in
crea
se o
f ery
troc
yte
fola
te
com
pare
d to
bas
elin
e).
Smok
ing
cess
atio
nSe
rum
cot
inin
e le
vel,
afte
r bo
th c
onsu
ltatio
nsSe
lf-re
port
ed s
mok
ing,
sm
okin
g ce
ssat
ion
and
smok
ing
redu
ctio
n.
• Pr
eval
ence
: num
ber o
f sm
oker
s at
bas
elin
e ba
sed
on s
elf-r
epor
t an
d se
rum
cot
inin
e.
• Ef
fect
iven
ess
prec
once
ptio
n ca
re: n
umbe
r of w
omen
repo
rtin
g to
ha
ve s
topp
ed s
mok
ing
or h
ave
redu
ced
smok
ing.
Alc
ohol
inta
ke c
essa
tion
% C
DTa a
nd G
amm
a G
T,
afte
r bot
h co
nsul
tatio
nsSe
lf-re
port
ed a
lcoh
ol
cons
umpt
ion,
bef
ore
each
co
nsul
tatio
n.
• Pr
eval
ence
: num
ber o
f wom
en u
sing
alc
ohol
and
hav
e be
en b
inge
dr
inki
ng, o
r cla
ssifi
ed a
s he
avy
drin
kers
(sel
f-rep
orte
d us
e),%
CD
T an
d G
amm
a G
T at
bas
elin
e.
• Ef
fect
iven
ess
of p
reco
ncep
tion
care
: cha
nge
in n
umbe
r of w
omen
us
ing
alco
hol p
reco
ncep
tiona
lly (s
elf-r
epor
t). D
ecre
ase
in %
CD
T an
d G
amm
a G
T, n
orm
aliz
ing
for h
eavy
drin
kers
aft
er a
bstin
ence
/de
crea
sed
use.
Dru
gsTo
x sc
reen
ing
urin
eb , aft
er
both
con
sulta
tions
Que
stio
nnai
re a
nd m
easu
re
befo
re e
ach
cons
ulta
tion
• Pr
eval
ence
: num
ber o
f wom
en u
sing
har
d- a
nd s
oftd
rugs
at
base
line
base
d on
sel
f-rep
ort a
nd u
rine
scre
enin
g.•
Effe
ctiv
enes
s of
pre
conc
eptio
n ca
re: n
umbe
r of w
omen
who
st
oppe
d dr
ug u
se b
ased
on
self-
repo
rt a
nd u
rine
scre
enin
g
Tabl
e 6.
4 co
ntin
ues o
n ne
xt p
age.

102
THE ‘H
EALTH
Y PREGN
AN
CY 4 ALL’ STU
DY
6
Ta
ble
6.4
Co
ntin
ued
Para
met
er
Bio
mar
ker
Que
stio
nnai
re O
utco
me
Vita
min
e D
25-O
H C
alci
diol
, aft
er th
e fir
st c
onsu
ltatio
n –
•
Prev
alen
ce o
f vita
min
D d
efic
ienc
y ba
sed
on 2
5-O
H C
alci
diol
leve
l m
easu
red
at th
e st
art o
f the
pre
conc
eptio
n ca
re c
onsu
ltatio
n.•
Que
stio
ns re
gard
ing
prog
nost
ic fa
ctor
s
Nut
ritio
nN
ot a
pplic
able
Self
repo
rted
die
t, be
fore
eac
h co
nsul
tatio
n•
Avoi
danc
e of
vita
min
A, n
o ra
w p
rodu
cts
and
prop
erly
was
hed
vege
tabl
es: s
elf-r
epor
ted
at b
asel
ine.
• In
crea
se in
num
ber o
f wom
en w
ith a
hea
lthy
diet
, avo
idin
g vi
tam
in A
and
raw
pro
duct
s, ve
geta
bles
pro
perly
was
hed:
sel
f-re
port
ed d
urin
g se
cond
con
sulta
tion
com
pare
d to
bas
elin
e.
Adju
stm
ent m
edic
atio
n re
gim
eN
ot a
pplic
able
Self
repo
rted
med
icat
ion
use,
be
fore
eac
h co
nsul
tatio
n.•
Prev
alen
ce: p
reco
ncep
tiona
l med
icat
ion
use
and
type
s of
m
edic
atio
n.•
Effe
ctiv
enes
s: s
afe
med
icat
ion
polic
y ev
alua
tion
by th
e he
alth
car
e pr
ovid
er ([
1] re
ferr
al fr
om m
idw
ife to
GP
for m
edic
atio
n po
licy,
[2]
num
ber o
f cas
es in
whi
ch c
essa
tion/
repl
acem
ent/
no c
essa
tion/
cont
inua
tion
of m
edic
atio
n is
cho
sen,
bas
ed o
n 'T
erat
olog
y In
form
atio
n Se
rvic
e' a
dvic
e, [3
] pat
ient
adh
eren
ce to
med
icat
ion
polic
y
Purs
uing
a h
ealth
y bo
dyw
eigh
t–
Ant
hrop
omet
rics
in b
oth
cons
ulta
tions
•
Prev
alen
ce o
f ove
rwei
ght (
BMI 2
5-30
), ob
esity
(BM
I >30
), an
d un
derw
eigh
t (BM
I <18
.5)
• Ef
fect
iven
ess
of p
reco
ncep
tion
care
: num
ber o
f wom
en w
ith
over
wei
ght B
MI >
25 lo
sing
wei
ght,
and
unde
rwei
ght B
MI <
18.5
%
gain
ing
wei
ght.

103
THE ‘H
EALTH
Y PREGN
AN
CY 4 ALL’ STU
DY
6
Adhe
renc
e to
pe
rson
aliz
ed a
dvic
e–
• Ad
here
nce
to a
dvic
e re
gard
ing
spec
ific
dete
cted
risk
fact
ors
acco
rdin
g to
the
care
give
r.
Preg
nanc
y ou
tcom
e–
Retr
ospe
ctiv
e fr
om n
atio
nal
data
base
(The
Net
herla
nds
Perin
atal
Reg
istr
y)
• N
umbe
r of b
irths
adv
erse
out
com
es d
efin
ed a
s (1
) per
inat
al
mor
talit
y, (2
) con
geni
tal a
nom
alie
s, (3
) pre
term
birt
h (<
37th
wee
k of
pre
gnan
cy),
(4) s
mal
l for
ges
tatio
nal a
ge (b
irthw
eigh
t <10
th
perc
entil
e), (
5) lo
w A
pgar
sco
re (<
5, 5
min
utes
aft
er b
irth)
.
Book
ing
visi
t <12
th w
eek
of g
esta
tion
– Re
tros
pect
ive
from
The
N
ethe
rland
s Pe
rinat
al
Regi
stry
, sel
f-rep
orte
d at
firs
t co
nsul
tatio
n
• G
esta
tiona
l age
at f
irst a
nten
atal
boo
king
vis
it
Card
iova
scul
ar ri
sk s
core
ac
cord
ing
to 'M
y Li
fe
Chec
k'c
Chol
este
rol,
Glu
cose
Mea
sure
d bl
ood
pres
sure
, BM
I, qu
estio
nnai
re it
ems
rega
rdin
g di
etar
y ha
bits
and
phy
sica
l ac
tivity
• Pr
ogno
stic
val
ue o
f car
diov
ascu
lar r
isk
scor
e an
d pr
eval
ence
of:
hype
rten
sive
dis
ease
in p
regn
ancy
, con
geni
tal a
nom
alie
s, pr
eter
m
birt
h, s
mal
l for
ges
tatio
nal a
ge, l
ow A
pgar
sco
re.
FIN
DRI
SK d
iabe
tes
scor
eCh
oles
tero
l, G
luco
seBl
ood
pres
sure
, BM
I, w
aist
an
d hi
p ci
rcum
fere
nce,
qu
estio
nnai
re it
ems
rega
rdin
g fa
mily
his
tory
, abn
orm
al
gluc
ose
mea
sure
men
t
• Pr
ogno
stic
val
ue d
iabe
tes
risk
scor
e an
d pr
eval
ence
of:
gest
atio
nal
diab
etes
, hyp
erte
nsiv
e di
seas
e in
pre
gnan
cy, p
erin
atal
mor
talit
y,
mac
roso
mia
, con
geni
tal a
nom
alie
s, pr
eter
m b
irth,
sm
all f
or
gest
atio
nal a
ge, l
ow A
pgar
sco
re.
a CD
T: C
arbo
hydr
ate-
defic
ient
tran
sfer
rin, l
abor
ator
y te
st to
det
ect (
heav
y) a
lcho
hol c
onsu
mpt
ion.
b scr
eens
for a
mfe
tam
ines
, bar
bitu
rate
s, be
nzod
iaze
pine
s, c
ocai
ne, e
csta
sy,
met
amfe
tam
ine,
met
hado
n, o
piat
es, P
CP, c
anna
bis.
c htt
p://
myl
ifech
eck.
hear
t.org
.

104
THE ‘H
EALTH
Y PREGN
AN
CY 4 ALL’ STU
DY
6
Blood samples are collected either by the caregiver or by an outpatient-testing facility of
the local laboratory. Initial analysis of the samples (hemoglobin, mean corpuscular volume,
fasting glucose at baseline) and refrigeration (between -20 and -80 degrees Celsius) will
occur within 24 hours after sample collection at the local laboratory. Only deviant vitamin
D, glucose, cholesterol and hemoglobin results are communicated to the participant’s GP if
she has requested so in the informed consent form. Regarding primary outcomes: erytrocyte
folate – as biomarker for folic acid use), serum cotinin – as biomarker for cigarette smoking,
carbohydrate dehydrogenase (CDT) – as biomarker for outcome for heavy drinking and
urinary drugs tests – as biomarker for soft and hard-drug use; are measured.
Study preparation
Before study onset, the participating midwives and GPs receive training in PCC, including
implementation of the ‘Preconceptiewijzer’ tool. Additionally, the participating caregivers
and their staff are given a preparatory tutorial at baseline on relevant procedures within the
HP4All study. These procedures include anthropometric and blood pressure measurements
and paper and web-based data registration.
Recruitment for the PCC sub-study was set up to the extent that was agreed upon with
the local project coordinators. Firstly, the municipality or Municipal Health Service (which
ever was chosen locally) selected women by the municipal population registry to mail
the invitational letter. An invitational letter was provided by the project, and letters were
adapted locally to fit the local situation. Secondly, local youth service was provided with
flyers and posters- with local practices offering consultations - to disseminate amongst their
youth healthcare physicians and nurses. Furthermore, GPs were supported logistically in
selecting women registered in their practice. Women with evident contraindications for
such invitation, both medically (such as terminal illness, with a hysterectomy or sterilisation
in the past) or socially (widow, in detention) were excluded. They sent out a locally adapted
basic letter provided by the project. Perinatal Health Educators were trained and provide
perinatal health education sessions to self-recruited women contemplating pregnancy.
DESIGN OF THE ANTENATAL RISK ASSESSMENT SUBSTUDYIn this cluster randomised trial midwifery practices in participating municipalities (‘clusters’)
were randomly assigned to either the use of a score-card (‘R4U’) based antenatal risk

105
THE ‘H
EALTH
Y PREGN
AN
CY 4 ALL’ STU
DY
6
assessment, care pathways and multidisciplinary consultation (intervention group) or
conventional risk assessment (control group). Score-card based systematic risk assessment
will be performed with the ‘R4U’ score-card at the first antenatal booking visit followed
by, if necessary, a specific referral to, e.g., higher level obstetric care (gynaecologist),
psychosocial care in case of medical or non-medical high risk using risk-specific care
pathways. Additionally, these women at increased risk will be reviewed in a multidisciplinary
team of caregivers concerning tailored antenatal care. Exclusion criteria include a medical
emergency situation during the booking visit (e.g., ectopic pregnancy), or women being
in labour.
The 70-item ‘R4U’ score-card consists of six risk domains (social status, ethnicity, care, lifestyle,
medical history and obstetric history). Corresponding care pathways to both medical and
non-medical services will support health care professionals to encounter complex (non-)
medical risk factors. A predefined weighted sum risk threshold, based on weighted single
risk factors, is derived from the ‘R4U’ score-card. If a pregnant woman’s individual sum risk
score exceeds the threshold, her case will be assessed in a multidisciplinary setting with
community midwives, obstetricians, and other care providers.
Pregnant women’s risk status in the control group is assessed conventionally, i.e., according
to the elaborate so-called ‘List of Obstetric Indications’ (in Dutch: Verloskundige Indicatie
Lijst)12 which lists all conventional (>140) high risk indications (for referral or consultation). In
each control region care ‘as usual’ will be provided until 700 participants have been included
or until 2/3 of the study period (2 years) has passed. After that moment, the implementation
of the risk assessment intervention will start.
Primary outcomes are the prevalence of preterm birth and SGA, and the efficacy of ‘R4U’
implementation (measured by the number of ‘R4U’ score-cards completed by the health
care professional against the number of booking visits, the development and use of care
pathways following ‘R4U’ scores, actually performed multidisciplinary consultations,
and patient and healthcare professional satisfaction). Secondary outcomes are perinatal
mortality (from 22 weeks’ gestation until 7 days postpartum), undetected SGA and
unexpected preterm birth, measured as onset of childbirth in primary care, prevalence and
accumulation of medical and non-medical risk factors, and the number of women referred
to secondary care through either R4U score-card based or conventional risk assessment.

106
THE ‘H
EALTH
Y PREGN
AN
CY 4 ALL’ STU
DY
6
Randomisation procedure and sample size calculation
In January 2011 randomisation took place by an independent statistician. In order to study the
need for matching, we stratified the adverse perinatal outcomes (‘Big4’ and perinatal mortality)
in each cluster by SES and ethnicity. Since clusters were not considerably different in terms of
these characteristics, matching of clusters for SES and ethnicity was considered unnecessary.
Sample size in this study is based on the effectiveness of the ‘R4U’ risk assessment and
resulting care pathways intervention in early pregnancy on the likelihood of SGA and
preterm birth. In this cluster-randomised trial, sample size depends on: (1) the average
risk of SGA and preterm birth without the intervention (π0); (2) the expected effect of the
intervention (π1); (3) the inflation factor reflecting the partial similarity/dependency of
women’s outcomes or responses within the same cluster27); and (4) the α and (5) power (1-β)
of the test. Using data from the 2000-2008 Netherlands Perinatal Registry for the selected
postal code regions20, we estimated π0 at 16.7% (summation of preterm birth and SGA),
the expected effect of the intervention (π1) at 13% and the inflation factor at 2.06, based
on formulas on Donner et al.27 With 10 clusters, five municipalities in the control and five
in the intervention group, and an alpha of 0.05 (two-sided), 7,000 participants (3,500 per
arm) should provide power in excess of 80%. This means that 700 women per cluster should
be included in the analysis.
Logistics and data collection
As with the PCC sub-study, the logistics of this sub-study are carried out in close collaboration
with participating local project coordinators, midwives, obstetricians, and, if available, research
midwives in the 14 participating municipalities. Midwives and obstetricians inform pregnant
women about the HP4All study at the booking visit and hand out an information package.
All pregnant women at their first antenatal booking visit with a midwife or obstetrician
located in the areas are eligible if she meets the inclusion criteria. In intervention
municipalities, the ‘R4U’ score-card will be filled out during the first antenatal visit. For the
‘R4U’ score-card a web-based registration form is used in which women are registered, coded
with a study identification number. Depending on the detected risk factors, care pathways
can be used to modify these risk factors. If a pregnant woman’s weighted sum risk score
exceeds the predefined threshold, multidisciplinary consultation will be advised. In control
municipalities, pregnant women in the control group will receive regular antenatal health
care. Table 6.5 provides an overview of the planned assessments within the risk assessment
sub-study including variables, methods and outcomes.

107
THE ‘H
EALTH
Y PREGN
AN
CY 4 ALL’ STU
DY
6
Table 6.5 Planned assessments in the risk selection experiment: variables, methods and outcomes
Variables Methods Outcomes
Patients
1. INTERVENTION GROUP
Non-medical risk factors: 39 items from the risk score card, categorized into the domains social, ethnicity, care, and lifestyle.
Medical risk factors: 30 items from the risk score card, categorized into the domains general history and obstetric history
Baseline characteristics: Age, zip-code, ethnicity, onset of care, household composition, family income, employment, education level, smoking, alcohol, drugs, folic acid use, medication use, pre-existing chronic diseases, sexually transmitted diseases.
R4U score card + registration form ‘Obstetric history’
Questionnaire ‘Baseline characteristics’
Case Record Form ‘pregnancy and delivery data’
Primary outcomes: - Preterm birth - SGA
Secondary outcomes: - Undetected SGA and unexpected
preterm births (babies born in primary care)
- Prevalence of risk factors- Risk accumulation - Involved healthcare professionals
during pregnancy- Detection and prevention of impaired
growth and preterm birth during pregnancy
- Perinatal mortality - Congenital anomalies- Mode of delivery - Place of delivery - Asphyxia- Neonatal admission - Maternal morbidity (e.g., pre-
existing chronic disease, pregnancy complications), and maternal mortality.
2. CONTROL GROUP
Baseline characteristics: Age, zip-code, ethnicity, onset of care, household composition, family income, employment, education level, smoking, alcohol, drugs, folic acid use, medication use, pre-existing chronic diseases, sexually transmitted diseases.
Registration form ‘Obstetric history’
Questionnaire ‘Baseline characteristics’
Case Record Form ‘pregnancy and delivery data’
Patient satisfaction in both groups Questionnaire ‘Patient experiences during the first antenatal visit’
- Which topics were discussed (10 examples)?
- What was your experience? - Do you think this was important to ask?
Care providers
General characteristics participating midwifery practices and hospitals in both groups
Interview-based questionnaire
- Current number of patients and employees
- Use of risk selection instruments- Collaboration with hospitals and
(other) midwifery practices- Work processes (e.g., counselling for
prenatal screening, or ultrasound facilities).
Care provider satisfaction in both groups
Questionnaire - Feasibility - Efficacy of implementation- Collaboration - Continuation of intervention

108
THE ‘H
EALTH
Y PREGN
AN
CY 4 ALL’ STU
DY
6
Study preparation
In municipalities allocated to the intervention group, midwives and obstetricians will use
the ’R4U’ score-card during the first antenatal visit of all women (provided that informed
consent is given). Participating midwives and obstetricians receive personal instructions in
planned sessions by the project team for the practical use of the web-based ’R4U’ score-card.
Besides, an e-learning program is available for all caregivers. The project team has developed
28 templates of care pathways for all risk factors in the ‘R4U’ score-card. Together with local
healthcare professionals in perinatal care, municipal services, community health services,
and other services, these templates will be adapted in organised meetings to local setting,
taking the availability of local facilities, agreements, and guidelines into consideration.
We aim to assess 20% of all pregnant women in this multidisciplinary setting in order to
determine a cut-off score per municipality.
INFORMED CONSENT, DATA QUALITY, CONTROL, MANAGEMENT AND TIME SCHEDULE FOR BOTH SUBSTUDIES
Informed consent
The HP4All study has been approved by the Medical Ethical Committee of the Erasmus
Medical Centre Rotterdam (Preconception Care sub-study: MEC 2012-425; Antenatal risk
assessment trial: MEC 2012-322), and by the management of all participating care providers.
Pregnant and non-pregnant women, depending on the sub-study, will receive written and
oral information about the study.
Participation in either sub-study is voluntary and informed consent must be obtained. PCC
consultations are currently not covered by health care insurances; PCC providers will receive
reimbursement from the HP4All project. The participating practices in the antenatal risk
sub-study receive no financial compensation.
Data quality, control and management
For logistic reason, data are collected and coded with a study identification number.
Otherwise we will not be able to link data from the initial visit to birth records. The research
team and participating caregivers have access to the key that links study identification

109
THE ‘H
EALTH
Y PREGN
AN
CY 4 ALL’ STU
DY
6
number to record data. Data analysis and storage will take place on an anonymised
dataset. Access to this anonymised data is only available to the research team. All data and
biomaterials are stored 15 years after inclusion.
Time schedule
The HP4All study was initiated in April 2011. Full participant recruitment and complete
data collection started in December 2012. A cohort of 839 women for the PCC sub-study
is expected to be completed by the beginning of 2014. For the risk assessment sub-study,
7,000 women are also expected to be included by the beginning of 2014.
REFERENCES1. Buitendijk SE, Nijhuis JG. High perinatal mortality
in the Netherlands compared to the rest of Europe. Ned Tijdschr Geneeskd. 2004;148:1855-1860.
2. Mohangoo AD, Buitendijk SE, Hukkelhoven CW, et al. Higher perinatal mortality in The Netherlands than in other European countries: the Peristat-II study. Ned Tijdschr Geneeskd. 2008;152:2718-2727.
3. The EURO-PERISTAT project in collaboration with SCPE EE. European perinatal health report, 2008. (online: www.europeristat.com).
4. de Graaf JP, Ravelli AC, de Haan MA, Steegers EA, Bonsel GJ. Living in deprived urban districts increases perinatal health inequalities. J Matern Fetal Neonatal Med. 2013;26:473-481.
5. Denktas S, Bonsel GJ, Van der Weg EJ, et al. An urban perinatal health programme of strategies to improve perinatal health. Matern Child Health J. 2012;16:1553-1558.
6. Saravelos SH, Regan L. The importance of pre-conception counseling and early pregnancy monitoring. Seminars in reproductive medicine. 2011;29:557-568.
7. Barker DJ, Bagby SP, Hanson MA. Mechanisms of disease: in utero programming in the patho-genesis of hypertension. Nat Clin Pract Nephrol. 2006;2:700-707.
8. Mook-Kanamori DO, Steegers EA, Eilers PH, Raat H, Hofman A, Jaddoe VW. Risk factors and outcomes associated with first-trimester fetal growth restriction. JAMA. 2010;303:527-534.
9. Korenbrot CC, Steinberg A, Bender C, Newberry S. Preconception care: a systematic review. Matern Child Health J. 2002;6:75-88.
10. van der Zee B, de Beaufort I, Temel S, de Wert G, Denktas S, Steegers E. Preconception care: an essential preventive strategy to improve children’s and women’s health. J Public Health Policy. 2011;32:367-379.
11. Health Council of the Netherlands. Preconception care: a good beginning. The Hague: Health Council of the Netherlands, 2007; publication no. 2007/19E. ISBN 978-90-5549-678-5 (online: http://www.gezondheidsraad.nl/en/publications/prevention/preconception-care-good-beginning).
12. Amelink-Verburg MP, Buitendijk SE. Pregnancy and labour in the Dutch maternity care system: what is normal? The role division between midwives and obstetricians. J Midwifery Womens Health. 2010;55:216-225.
13. de Graaf JP, Ravelli AC, Wildschut HI, et al. Perinatal outcomes in the four largest cities and in deprived neighbourhoods in The Netherlands. Ned Tijdschr Geneeskd. 2008;152:2734-2740.

110
THE ‘H
EALTH
Y PREGN
AN
CY 4 ALL’ STU
DY
6
14. Poeran J, Maas AFG, Birnie E, Denktas S, Steegers EA, Bonsel GJ. Social deprivation and adverse perinatal outcomes among Western and non-Western pregnant women in a Dutch urban population. Soc Sci Med. 2013 (in press).
15. Jaddoe VW, Mackenbach JP, Moll HA, et al. The Generation R Study: Design and cohort profile. Eur J Epidemiol. 2006;21:475-484.
16. van Eijsden M, Vrijkotte TG, Gemke RJ, van der Wal MF. Cohort profile: the Amsterdam Born Children and their Development (ABCD) study. Int J Epidemiol. 2010;40:1176-1186.
17. de Graaf JP, Steegers EA, Bonsel GJ. Inequalities in perinatal and maternal health. Curr Opin Obstet Gynecol. 2013;25:98-108.
18. Bonsel GJ, Birnie E, Denktas S, Poeran J, Steegers EAP. Dutch report: Lijnen in de Perinatale Sterfte, Signalementstudie Zwangerschap en Geboorte 2010. Rotterdam: Erasmus MC; 2010.
19. van der Kooy J, Poeran J, de Graaf JP, et al. Planned home compared with planned hospital births in the Netherlands: intrapartum and early neonatal death in low-risk pregnancies. Obstet Gynecol. 2011;118:1037-1046.
20. Perinatal care in The Netherlands 2008 (in Dutch: Perinatale zorg in Nederland 2008). Utrecht: The Netherlands Perinatal Registry; 2011.
21. Roalfe AK, Holder RL, Wilson S. Standardisation of rates using logistic regression: a comparison with the direct method. BMC Health Serv Res. 2008;8:275.
22. Andres RL, Day MC. Perinatal complications associated with maternal tobacco use. Semin Neonatol. Aug 2000;5:231-241.
23. Lumley J, Watson L, Watson M, Bower C. Pericon-ceptional supplementation with folate and/or multivitamins for preventing neural tube defects. Cochrane Database Syst Rev. 2001:CD001056.
24. Salmasi G, Grady R, Jones J, McDonald SD. Environmental tobacco smoke exposure and perinatal outcomes: a systematic review and meta-analyses. Acta Obstet Gynecol Scand. 2010;89:423-441.
25. Landkroon AP, de Weerd S, van Vliet-Lachotzki E, Steegers EA. Validation of an internet question-naire for risk assessment in preconception care. Public Health Genomics. 2009;13:89-94.
26. Lindstrom J, Tuomilehto J. The diabetes risk score: a practical tool to predict type 2 diabetes risk. Diabetes care. 2003;26:725-731.
27. Donner A, Klar N. Design and analysis of cluster randomization trials in health research. 1st ed. London; 2000.

7
Manuscript submitted for publication.
The effectiveness of risk selection in the Dutch obstetric care system
J. Poeran, J. van der Kooy, E. Birnie, S. Denktaş, E.A.P. Steegers, G.J. Bonsel

112
RISK SELECTION
IN D
UTCH
OBSTETRIC CA
RE
7
ABSTRACTObjective To quantify if risk selection in Dutch obstetric care (by midwives) results in a
true low risk population in primary care at the end of pregnancy. This is an essential quality
of care indicator as a distinction is made between primary care for low risk pregnancies by
independently practicing community midwives, and secondary/tertiary care for high risk
pregnancies by obstetricians.
Methods All singleton pregnancies (≥22 weeks’ gestation, 2000-2007, n=1,407,387) from
The Netherlands Perinatal Registry were selected. We defined high risk pregnancy as the
presence of ≥1 ‘Big4’ morbidities, the main precursors of perinatal mortality: congenital
anomalies, preterm birth, small for gestational age (SGA), or low Apgar score. Referral
patterns of high risk pregnancies were studied during pregnancy and parturition; adequate
risk selection implies no high risk pregnancies in primary care. Additionally, we applied a
diagnostic test framework to study effectiveness of SGA selection (and referral) by defining
true positives (referral of SGA), false positives (referral of non-SGA), false negatives (non-
referral of SGA), and true negatives (non-referral of non-SGA). Sensitivity, specificity, negative
predictive value (NPV), negative likelihood ratio (LR-), and false negative rate (FN) were
determined for eight patient subgroups.
Results 59% of ‘Big4’ were referred during pregnancy, 19% during parturition; 22%
remained in primary care. SGA ‘test’ characteristics differed considerably for subgroups
(sensitivity 15%-59%, specificity 54%-87%, NPV 89%-97%, LR- 0.69-1.05, FN 3%-11%).
Conclusion Risk selection in Dutch obstetric care does not realise its aim of a true low risk
group in primary care at the end of pregnancy. Methods for improvement are warranted.

113
RISK SELECTION
IN D
UTCH
OBSTETRIC CA
RE
7
INTRODUCTIONIn The Netherlands perinatal mortality exceeds the European average.1 The unique Dutch
system of obstetric care has been regarded as a potential contributing factor.2-4 This system
is characterised by three risk-based levels of care. Primary care for low risk pregnancies is
provided by independently practicing community midwives and a small percentage of
general practitioners (GPs). Assumed low risk pregnant women can either opt for a home
birth or a short-stay hospital birth under supervision of a community midwife. Secondary/
tertiary care for assumed high risk pregnancies is provided by obstetricians in hospitals.
Currently, approximately 80% of pregnant women start antenatal care in primary care.5
Whenever risk factors (for adverse perinatal or maternal outcome) are present before
pregnancy or arise during pregnancy or parturition, women shift from low risk to high risk
and are referred to secondary care or from secondary to tertiary care, also during parturition.
This ongoing risk assessment during pregnancy and during parturition is called ‘risk selection’.
In formal terms, the aim of risk selection is to identify and refer high risk pregnancies in order
to obtain a true low risk group of pregnant women (expressed as high negative predictive
value of risk selection) in the primary care setting.5,6 Thus, risk selection adequacy is an
essential quality of care indicator of the Dutch obstetric care system.
Although the effectiveness of risk selection in Dutch primary obstetric care has been studied,
a nationwide systematic evaluation on the performance of the risk selection process is still
absent.3,4,6-11 The present nationwide retrospective study quantifies the performance of risk
selection (during pregnancy and during parturition) by community midwives in terms of its
ability to achieve a true low risk population at the end of pregnancy.
METHODS
Netherlands Perinatal Registry
We selected data from all singleton pregnancies for the period 2000-2007 as registered in
The Netherlands Perinatal Registry, which is subject to Dutch law regulations regarding
confidentiality. In agreement with the World Health Organization (WHO) reporting
guidelines, only pregnancies with a gestational age of ≥22 weeks were included.12
The registry contains population-based information of >97% of all pregnancies in The
Netherlands.13 Source data are collected by 94% of midwives, 99% of gynaecologists and
68% of paediatricians (including 100% of Neonatal Intensive Care Unit paediatricians) as part

114
RISK SELECTION
IN D
UTCH
OBSTETRIC CA
RE
7
of their routine medical dossier; see website for detailed description www.perinatreg.nl.13
The board of The Netherlands Perinatal Registry granted permission to use the anonymous
registry data for this study. The Netherlands Perinatal Registry has been extensively
described and used in several recent studies.1,2,4,10,13-15
Assignment of high risk
In Dutch obstetric care a pregnancy is considered a valid high risk, justifying referral, if an
adverse perinatal outcome, adverse maternal outcome or combination of both is present
or is to be expected. Indications for referral are listed in the so-called ‘List of Obstetric
Indications’ (in Dutch: Verloskundige Indicatie Lijst).5 Community midwives are trained in
the use of the ‘List of Obstetric Indications’ to detect (expected) high risks.
Judgment of adequacy of high and low risk assignment
As a retrospective measure to judge whether assumed low risk women truly were low risk,
we used the prevalence of so-called ‘Big4’ morbidities as an indicator of risk status (gold
standard).2,15 From a detailed analysis of The Netherlands Perinatal Registry we know that
four specific morbidities precede perinatal mortality in 85% of cases, the so-called ‘Big4’
morbidities.2,15 These are: congenital anomalies (list defined), preterm birth (<37th week
of gestation), small for gestational age (SGA, birthweight <10th percentile for gestational
age16) or low Apgar score (<7, 5 minutes after birth). Congenital anomalies are registered
postpartum through a standard coding system with eight different organ systems, and
further distinction into 51 specific and 20 more global categories. By using remnant ‘Big4’
morbidity among assumed low risk women as yard stick we focus on undetected risks which
are relevant to perinatal mortality. This focus by definition does not include any unexpected
adverse maternal outcome in low risk women.
Eff ectiveness of risk selection
The primary outcome in quantifying the effectiveness of risk selection is the ‘Big4’ (high
risk) prevalence at the end of pregnancy in primary care. In the theoretical perfect case
‘Big4’ morbidity is absent in assumed low risk pregnancies.
From this starting point, we utilise three methods to quantify effectiveness of risk selection:
Method 1. with a flow chart approach describing the proportional shift of women from
primary care to secondary/tertiary care over the course of pregnancy, distinguishing

115
RISK SELECTION
IN D
UTCH
OBSTETRIC CA
RE
7
between two referral moments (during pregnancy and during parturition); risk selection
should preferably take place during pregnancy;
Method 2. by comparing eight, mutually exclusive, patient subgroups in terms of the level
of care at first antenatal booking (primary, secondary/tertiary care) and subsequent referral,
where ‘Big4’ prevalence and perinatal mortality are observed in the various subgroups;
preferably, perinatal mortality is only increased in the secondary/tertiary care group with
referral of ‘Big4’ pregnancies during parturition being a rare event.
The eight subgroups were defined according to parity (primiparous/multiparous), ethnicity
(Western/non-Western), and living in a deprived neighbourhood (yes/no, based on 4-digit
zip codes and an official public list of 40 deprived zip code based neighbourhoods).17 The
eight groups presumably differ according to ‘Big4’ prevalence and care characteristics.
Method 3. by formal analysis of diagnostic performance of selection and referral of one
‘Big4’ category, i.e., SGA. The theoretical goal is to obtain a SGA-free population in the
primary care setting, which is studied for the same eight patient subgroups as before.
If the subgroup SGA prevalence matches the subgroup variation in test characteristics,
then, the selected patient subgroup factors (parity/ethnicity/neighbourhood) are likely
to be responsible for the between subgroup differences in test characteristics. However, if
there is a discrepancy, other factors may explain the subgroup test characteristics variation
factors, e.g., system related factors.
SGA was chosen as, together with congenital anomalies, it can be detected the easiest in
the antenatal phase. Moreover, there is general consensus on (improving) detection of SGA
because of the inherent increased risk for adverse outcome18, and most congenital anomalies
are now detected by routine ultrasound (introduced in 2007) at 20 weeks of gestational age.
Referral categories
To describe the referral process we defined five mutually exclusive categories:
I. First antenatal booking in secondary/tertiary care, no referral by definition, birth in
hospital in secondary/tertiary care.
II. First antenatal booking in primary care, referral during pregnancy, birth in hospital in
secondary/tertiary care;
III. First antenatal booking in primary care, referral during parturition, birth in hospital in
secondary/tertiary care;

116
RISK SELECTION
IN D
UTCH
OBSTETRIC CA
RE
7
IV. First antenatal booking in primary care, no referral, home birth in primary care;
V. First antenatal booking in primary care, no referral, short-stay hospital birth in primary
care.
Diagnostic performance of SGA referral and selection
For the third quantification of effectiveness of risk selection we applied a diagnostic test
framework in which SGA selection (and referral) during pregnancy and during parturition
are treated as a positive ‘test result’, whereas the presence of SGA at birth is regarded as
the ‘gold standard’ outcome. The related 2x2 table is illustrated in table 7.1: ‘A’ represents
true positives (referral of SGA), ‘B’ false positives (referral of non-SGA), ‘C’ false negatives
(non-referral of SGA), and ‘D’ true negatives (non-referral of non-SGA).
The following five diagnostic test characteristics were determined applying method 319-21:
• Sensitivity [A/(A+C)], the proportion of SGA cases referred;
• Specificity [D/(B+D)], the proportion of non-SGA cases which are not referred;
• Negative predictive value (NPV) [D/(C+D)], the proportion of non-referred women
without a SGA baby;
• Negative likelihood ratio (LR-), [1-sensitivity/specificity], determines whether a negative
‘test’ result, i.e., no referral, decreases the probability of having a SGA baby for women
who are not referred. A negative likelihood ratio ranging from 0 to <1 implies diagnostic
value of the test, a value of 1 represents a test without diagnostic value (‘similar to
flipping a coin’) regarding SGA selection and referral. The lower the LR-, the higher the
diagnostic value, i.e., non-referral being associated with absence of SGA;
• SGA false negative rate (FN) [1-NPV], i.e., the proportion of non-referred women with
a SGA baby (false negative).
Table 7.1 Main 2x2 table with actual referral to secondary/tertiary care treated as a positive ‘test result’ and the presence of SGA (small for gestational age) at birth treated as the ‘gold standard’ outcome
SGA present at birth
Yes No
ReferralYes A B
No C D
A: True positive / B: False positive / C: False negative / D: True negative

117
RISK SELECTION
IN D
UTCH
OBSTETRIC CA
RE
7
The NPV, LR- and FN can be considered the most important test characteristics. These
characteristics pertain to the least desirable situation, i.e., a woman with a high risk (e.g.,
SGA) pregnancy giving birth in primary care which is only intended for low risk pregnancies.
RESULTS
Process of risk selection
A total of 1,407,387 single pregnancies were analysed. Figure 7.1 displays the selection
and referral of ‘Big4’ pregnancies by referral category in a flowchart; 15% of all pregnancies
are ‘Big4’ pregnancies. The dark grey area represents the ‘Big4’ proportion in primary care
(above the dashed line) and in secondary/tertiary care (below the dashed line). The dark
grey area above the dashed line diminishes in width if ‘Big4’ pregnancies are referred from
primary care to secondary/tertiary care during pregnancy or during parturition. Over the
course of pregnancy, the proportion of ‘Big4’ pregnancies in primary care decreases from
14% at first antenatal booking to 6% in women giving birth at home and to 9% among
women with a short-stay hospital delivery under the supervision of a community midwife.
Table 7.2 displays demographics and outcomes in the overall study population by the referral
categories. Most women are multiparous (54%), between the ages of 20-35 years (84%),
of Western origin (84%) and living in a non-deprived neighbourhood (94%). The largest
referral group is the group of women referred during pregnancy (group II, n=466,415). In
the group referred during parturition (group III), 70% of women are primiparous compared
to 48% of women referred during pregnancy (group II). Group IV has the lowest risks, the
group with the highest risk is group I.
Method 2: ‘Big4’ and perinatal mortality prevalence by patient subgroup and referral category
Table 7.3 shows the ‘Big4’ and perinatal mortality (overall 9.8 per 1,000) prevalence for the
different subgroups in the five referral categories. Late ‘Big4’ referral, i.e., ‘Big4’ prevalence
in women referred during parturition is not rare with a range of 14-19%; perinatal mortality,
however, is relatively low ranging from 3.5 to 8.3 per 1,000 births.
Overall, there are large differences in perinatal mortality and ‘Big4’ prevalence between
subgroups and referral categories: in all referral categories, primiparous women have

118
RISK SELECTION
IN D
UTCH
OBSTETRIC CA
RE
7
Fig
ure
7.1
Re
ferr
al a
nd ri
sk s
elec
tion
in D
utch
obs
tetr
ic c
are
in a
bsol
ute
num
bers
; effe
ctiv
enes
s of
risk
sel
ectio
n is
illu
stra
ted
as th
e pr
opor
tion
of
‘Big
4’ p
regn
anci
es in
dar
k gr
ey. T
he d
iffer
ent r
efer
ral c
ateg
orie
s ar
e lig
ht g
rey;
from
left
to ri
ght r
efer
ral c
ateg
orie
s I t
o V.

119
RISK SELECTION
IN D
UTCH
OBSTETRIC CA
RE
7
Ta
ble
7.2
D
emog
raph
ics a
nd o
utco
me
in th
e st
udy
popu
latio
n by
the
five
diffe
rent
refe
rral
cat
egor
ies
Re
ferr
al c
ateg
orie
s
Refe
rral
cat
egor
yI
IIIII
IVV
Tota
l
Firs
t boo
king
Seco
ndar
y/Te
rtia
ry c
are
Prim
ary
care
Prim
ary
care
Prim
ary
care
Prim
ary
care
Birt
hSe
cond
ary/
Tert
iary
car
eSe
cond
ary/
Tert
iary
car
eSe
cond
ary/
Tert
iary
car
ePr
imar
y ca
re:
hom
ePr
imar
y ca
re:
hosp
ital
Refe
rral
No
refe
rral
Dur
ing
preg
nanc
yD
urin
g pa
rtur
ition
No
refe
rral
No
refe
rral
N25
3,86
746
6,41
519
0,34
533
6,28
216
0,47
81,
407,
387
Parit
y*Pr
imip
arou
s (%
)12
1,06
6 (4
8)22
6,13
3 (4
8)13
4,10
2 (7
0)10
44,8
8 (3
1)63
,567
(40)
649,
356
(46)
Mul
tipar
ous
(%)
132,
794
(52)
240,
121
(52)
56,1
93 (3
0)23
1,71
9 (6
9)96
,826
(60)
757,
653
(54)
Mat
erna
l age
*<2
0 ye
ars
(%)
4,72
5 (2
)**
7,53
9 (2
)4,
333
(2)
2,82
0 (1
)4,
637
(3)
24,0
54 (2
)
20-3
5 ye
ars
(%)
206,
984
(82)
**38
2,19
5 (8
2)16
6,93
8 (8
8)29
0,44
2 (8
6)13
6,41
8 (8
5)1,
182,
977(
84)
>35
year
s (%
)42
,158
(17)
**76
,681
(16)
19,0
74 (1
0)43
,020
(13)
19,4
23 (1
2)20
0,35
6 (1
4)
Ethn
icity
Wes
tern
(%)
214,
332
(84)
387,
985
(83)
157,
245
(83)
308,
425
(92)
112,
775
(70)
1,18
0,76
2 (8
4)
Non
-Wes
tern
(%)
39,5
35 (1
6)78
,430
(17)
33,1
00 (1
7)27
,857
(8)
47,7
03 (3
0)22
6,62
5 (1
6)
Tabl
e 7.
2 co
ntin
ues o
n ne
xt p
age.

120
RISK SELECTION
IN D
UTCH
OBSTETRIC CA
RE
7
Ta
ble
7.2
Co
ntin
ued
Re
ferr
al c
ateg
orie
s
Refe
rral
cat
egor
yI
IIIII
IVV
Tota
l
Firs
t boo
king
Seco
ndar
y/Te
rtia
ry c
are
Prim
ary
care
Prim
ary
care
Prim
ary
care
Prim
ary
care
Birt
hSe
cond
ary/
Tert
iary
car
eSe
cond
ary/
Tert
iary
car
eSe
cond
ary/
Tert
iary
car
ePr
imar
y ca
re:
hom
ePr
imar
y ca
re:
hosp
ital
Refe
rral
No
refe
rral
Dur
ing
preg
nanc
yD
urin
g pa
rtur
ition
No
refe
rral
No
refe
rral
Nei
ghbo
rhoo
dN
on-d
epriv
ed23
7,83
6 (9
4)43
7,35
8 (9
4)17
7,65
2 (9
3)32
4,47
7 (9
6)14
3,69
9 (9
0)1,
321,
022
(94)
Dep
rived
16,0
31 (6
)29
,057
(6)
12,6
93 (7
)11
,805
(4)
16,7
79 (1
0)86
,365
(6)
Cong
enita
l ano
mal
ies
No
(%)
245,
554
(97)
447,
192
(96)
185,
515
(97)
332,
647
(99)
158,
329
(99)
1,36
9,23
7 (9
7)
Yes
(%)
8,31
3 (3
)19
,223
(4)
4,83
0 (3
)3,
635
(1)
2,14
9 (1
)38
,150
(3)
Pret
erm
birt
hN
o (%
)22
3,94
6 (8
8)42
6,32
4 (9
1)17
7,40
4 (9
3)33
4,92
0 (1
00)
157,
945
(98)
1,32
0,53
9 (9
4)
Yes
(%)
29,9
21 (1
2)40
,091
(9)
12,9
41 (7
)1,
362
(0)
2,53
3 (2
)86
,848
(6)
Smal
l for
ges
tatio
nal a
geN
o (%
)23
1,49
4 (9
1)42
5,52
2 (9
1)17
8,06
2 (9
4)32
1,10
7 (9
5)15
0,53
2 (9
4)1,
306,
717
(93)
Yes
(%)
22,3
73 (9
)40
,893
(9)
12,2
83 (6
)15
,175
(5)
9,94
6 (6
)10
0,67
0 (7
)
* Tot
als
do n
ot a
lway
s ad
d up
due
to m
issi
ng v
alue
s (p
arity
378
mis
sing
s, m
ater
nal a
ge 2
84 m
issi
ngs)
.**
Per
cent
ages
add
up
to 1
01%
bec
ause
of r
ound
ing

121
RISK SELECTION
IN D
UTCH
OBSTETRIC CA
RE
7
Ta
ble
7.3
Pr
eval
ence
of ‘
Big4
’ mor
bidi
ties
and
perin
atal
mor
talit
y by
the
five
refe
rral
cat
egor
ies
in d
iffer
ent s
ubgr
oups
(bas
ed o
n pa
rity,
eth
nici
ty
and
neig
hbou
rhoo
d). T
otal
num
ber o
f pre
gnan
cies
(N=1
,407
,009
) doe
s no
t inc
lude
378
par
ity m
issi
ngs.
Refe
rral
cat
egor
ies
Refe
rral
cat
egor
yI
II
III
IV
V
To
tal
Firs
t boo
king
Seco
ndar
y/Te
rtia
ry
care
Prim
ary
care
Prim
ary
care
Prim
ary
care
Prim
ary
care
Birt
hSe
cond
ary/
Tert
iary
ca
reSe
cond
ary/
Tert
iary
ca
reSe
cond
ary/
Tert
iary
ca
rePr
imar
y ca
re: h
ome
Prim
ary c
are:
hos
pita
l
Refe
rral
No
refe
rral
D
urin
g pr
egna
ncy
D
urin
g pa
rtur
ition
N
o re
ferr
al
No
refe
rral
NBi
g4*
†**
NBi
g4*
†**
NBi
g4*
†**
NBi
g4*
†**
NBi
g4*
†**
NBi
g4*
†**
Su
bg
rou
ps
Prim
ipar
ous
Wes
tern
Non
-dep
rived
101,
876
25%
20.3
188,
323
24%
13.8
110,
669
16%
3.7
94,4
359%
0.8
44,8
8212
%5.
954
0,18
519
%10
.0
Dep
rived
3,28
428
%26
.56,
379
27%
16.3
3,71
918
%3.
52,
597
8%0.
82,
063
15%
3.4
18,0
4221
%11
.8
Non
-Wes
tern
Non
-dep
rived
12,2
9330
%34
.224
,570
27%
17.6
15,3
1618
%5.
35,
947
12%
1.7
12,3
0214
%5.
170
,428
22%
14.3
Dep
rived
3,61
330
%39
.66,
861
29%
18.4
4,39
819
%5.
51,
509
13%
2.7
4,32
014
%2.
820
,701
23%
14.9
Mul
tipar
ous
Wes
tern
Non
-dep
rived
106,
312
18%
19.6
188,
639
15%
11.7
41,7
2514
%6.
220
8,15
05%
0.6
63,8
006%
3.6
608,
626
11%
8.1
Dep
rived
2,85
827
%33
.94,
522
20%
13.0
1,09
716
%7.
33,
179
6%1.
91,
993
8%2.
013
,649
16%
12.7
Non
-Wes
tern
Non
-dep
rived
17,3
4823
%31
.535
,683
18%
15.6
9,89
715
%7.
015
,876
7%0.
622
,640
7%2.
510
1,44
415
%12
.2
Dep
rived
6,27
625
%33
.511
,277
20%
17.0
3,47
415
%8.
34,
514
6%0.
98,
393
8%1.
433
,934
15%
13.2
Tota
l25
3,86
022
%22
.346
6,25
420
%13
.519
0,29
516
%4.
733
6,20
76%
0.7
160,
393
9%4.
01,
407,
009
15%
9.8
* ‘Bi
g4’ m
orbi
ditie
s in
per
cent
age
of th
e to
tal a
mou
nt o
f pre
gnan
cies
in th
at s
ubgr
oup.
** P
erin
atal
mor
talit
y (fr
om 2
2 w
eeks
of g
esta
tiona
l age
unt
il 7
days
pos
tpar
tum
) per
1,0
00 b
irths
.

122
RISK SELECTION
IN D
UTCH
OBSTETRIC CA
RE
7
higher ‘Big4’ prevalences compared to multiparous women (range 8-30% versus 5-27% for
multiparous women). Perinatal mortality, however, is lower in primiparous women referred
during parturition compared to multiparous women (3.5-5.5 vs. 6.2-8.3 per 1,000 births,
respectively). In almost all subgroups and referral categories, non-Western women have
higher ‘Big4’ and perinatal mortality prevalences; outcome differences between living in a
non-deprived versus living in a deprived neighbourhood are smaller.
Method 3: SGA selection during pregnancy
Table 7.4 shows the SGA prevalence before and after selection (and subsequent referral),
and diagnostic test characteristics for SGA selection and referral during pregnancy and during
parturition. Of all women exposed to the selection and referral process during pregnancy
(referral categories II to V), non-Western primiparous women in deprived neighbourhoods
have the highest SGA prevalence (13%). For all subgroups, SGA prevalence is lower after
selection compared to before. Sensitivity and specificity of SGA selection during pregnancy
ranges from 49% to 59% and from 58% to 63% respectively. The range of NPV is 89-97%.
The negative likelihood ratio (LR-) ranges from 0.69 to 0.85, indicating that that the SGA
prevalence decreases (after the selection / ’test’) in the group of women who are not referred
during pregnancy. However, the values are close to 1 (which would imply a test without
diagnostic value) which implies a modest discriminating value. The FN ranges from 3-11%
depicting the percentage of non-referred women having SGA babies.
Method 3: SGA selection during parturition
Of all women exposed to the selection and referral process during parturition (referral
categories III to V) primiparous non-Western women have the highest SGA prevalence
(11%). For all subgroups, there is no difference in SGA prevalence before and after selection.
Sensitivity and specificity of SGA selection during parturition range from 15% to 45% and
from 54% to 87%, respectively. For primiparous women the sensitivity is higher than for
multiparous women. Specificity, on the other hand, is higher for multiparous women than
for primiparous women. The NPV is similar to that for the SGA selection process during
pregnancy 89-97%. The LR- ranges from 0.97 to 1.05 implying no diagnostic value of risk
selection for SGA during parturition. The FN ranges from 3-11%.

123
RISK SELECTION
IN D
UTCH
OBSTETRIC CA
RE
7
Ta
ble
7.4
Su
bgro
up S
GA
pre
vale
nce
befo
re (‘
SGA
% B
F’) a
nd a
fter
(‘SG
A%
AF’
) sel
ectio
n, a
nd d
iagn
ostic
test
cha
ract
eris
tics*
; bot
h fo
r sel
ectio
n an
d re
ferr
al o
f SG
A p
regn
anci
es d
urin
g pr
egna
ncy
and
durin
g pa
rtur
ition
Sele
ctio
n du
ring
preg
nanc
ySe
lect
ion
durin
g pa
rtur
ition
SGA
%
BFSG
A%
A
FSE
NS
SPEC
NPV
LR-
FNSG
A%
BF
SGA
%
AF
SEN
SSP
ECN
PVLR
-FN
Su
bg
rou
ps
Prim
ipar
ous
Wes
tern
Non
-dep
rived
9%7%
53%
58%
93%
0.82
7%7%
7%42
%56
%93
%1.
057%
Dep
rived
11%
9%53
%58
%91
%0.
809%
9%9%
44%
56%
91%
1.01
9%N
on-W
este
rnN
on-d
epriv
ed12
%11
%50
%59
%89
%0.
8511
%11
%11
%45
%54
%89
%1.
0111
%D
epriv
ed13
%11
%49
%61
%89
%0.
8311
%11
%11
%44
%57
%89
%0.
9911
%
Mul
tipar
ous
Wes
tern
Non
-dep
rived
4%3%
52%
63%
97%
0.76
3%3%
3%15
%87
%97
%0.
983%
Dep
rived
7%5%
59%
59%
95%
0.69
5%5%
5%18
%83
%95
%0.
995%
Non
-Wes
tern
Non
-dep
rived
6%5%
53%
58%
95%
0.81
5%5%
5%23
%80
%95
%0.
975%
Dep
rived
7%5%
52%
60%
95%
0.79
5%5%
5%21
%79
%95
%1.
005%
Tota
l7%
5%52
%60
%95
%0.
795%
5%5%
33%
73%
95%
0.93
5%
* SE
NS:
sen
sitiv
ity, S
PEC:
spe
cifi c
ity, N
PV: n
egat
ive
pred
ictiv
e va
lue,
LR-
: neg
ativ
e lik
elih
ood
ratio
, FN
: SG
A fa
lse
nega
tive
rate
.

124
RISK SELECTION
IN D
UTCH
OBSTETRIC CA
RE
7
DISCUSSION
Principal fi ndings
To our knowledge, this is the largest study on the effectiveness of risk selection in Dutch
primary obstetric care. The main focus was to examine whether risk selection realises its
aim of a true low risk group of pregnant women by identifying and referring high risk
pregnancies. Even though many ‘Big4’ pregnancies are referred, our results demonstrate that
a true low risk population is never attained, with a ‘Big4’ prevalence of up to 15% in primary
care (table 7.3), intended for low risk pregnancies only. Also, ‘Big4’ prevalence among late
referrals (during parturition) was still substantial, ranging from 14% to 19%.
We further observed a suboptimal discrimination of SGA and non-SGA pregnancies (low
sensitivity, LR- close to 1 in all subgroups) with a SGA prevalence of 3% to 11% still being
born in primary care.
Moreover, we observed a discrepancy in the subgroup SGA prevalence and the subgroup
variation in SGA selection test characteristics (table 7.4). This implies other factors to be
responsible for the suboptimal test characteristics instead of the selected patient factors,
e.g., system related factors. One may think of differences in availability of SGA screening
methods.
Home birth versus short-stay hospital birth
In primary care, short-stay hospital births showed higher ‘Big4’ prevalence compared to
home births (9% vs. 6%). This may reflect an unintentional selection process by either the
midwife or self-selection by pregnant women, i.e., more healthy women appear to opt for
home birth. This has also been observed in other studies.22
Preventability
From our results, the question arises whether the birth of a ‘Big4’ baby in a primary rather
than secondary care setting is a preventable situation. As stated, congenital anomalies
and SGA are better predictable than (spontaneous) preterm birth and a low Apgar score.
In accepting that a NPV of 100% is not attainable, we actually state that ‘Big4’ deliveries in
a primary care are to some extent inevitable in a system with different risk-based settings.

125
RISK SELECTION
IN D
UTCH
OBSTETRIC CA
RE
7
The subsequent question then refers to the observed ‘setting safety’ of a primary care
setting. Both general consensus and the ‘List of Obstetric Interventions’ agree that a neonate
with a ‘Big4’ morbidity is better off in a hospital setting under the care of an obstetrician/
paediatrician.23 The benefit of this so-called ‘setting safety’ may be related to availability of
neonatological expertise, continuous fetal heart rate monitoring or advanced resuscitation
equipment.4,10
As we showed less optimal SGA selection, and more referrals during parturition for
primiparous women, we believe that all primiparous women should deliver in a hospital
environment, either under supervision of a midwife (birth centre) or an obstetrician. This
also follows from unequivocal evidence from previous studies24-26, where others generally
waive the primary care option.24
Strengths and limitations
The strengths of the current study include the nationwide approach and high coverage of
pregnancies in The Netherlands Perinatal Registry over a long period of time. In addition,
the use of ‘Big4’ morbidities, as the major precursors of perinatal mortality, allows for an
easy-to-comprehend proxy measure of high risk pregnancy.2,15 Also, the application of a
diagnostic test framework allows the results to be interpreted objectively in a standardised
way; comparisons with other diagnostic test studies can be easily made. Another strength
pertains to the use of subgroups. It is interesting at the very least to see a discrepancy
between the level of subgroup differences for SGA prevalence compared to the smaller
subgroup differences in test characteristics.
This study also has limitations. Firstly, it is not possible to determine the exact indication for
why women were referred because of the retrospective nature of The Netherlands Perinatal
Registry. For our study objective, the effect of this limitation is limited as we focused on high
risk births taking place in primary care, which is intended for low risk births. Our estimate
of prevalence of high risk births in primary care is conservative as it is likely to be higher,
providing it would have been possible to take into account all referral indications. Another
possible limitation is that with the ‘Big4’ approach, maternal and other non-‘Big4’ related
risks are disregarded. This problem also appears to be limited as the majority of referral
indications according to the ‘List of Obstetric Interventions’ pertain to fetal/neonatal risks
alone.5 Finally, the impact of routine ultrasound examination at 20 weeks of gestational age
(introduced in 2007) on congenital abnormality rates and perinatal mortality rates due to
second trimester abortions cannot be evaluated in our 2000-2007 dataset.

126
RISK SELECTION
IN D
UTCH
OBSTETRIC CA
RE
7
Previous studies on risk selection in the Dutch system
Our findings contradict most previous studies on the effectiveness of risk selection in
Dutch primary obstetric care, stating that risk selection is effective.6-9 In contrast with our
study, these studies took into account maternal morbidity and obstetric interventions
(e.g., caesarean section). However, these studies have been conducted some time ago, are
restricted to smaller study groups, specific regions or did not evaluate the risk selection
process systematically.6-9 Another limitation of previous studies is that they defined the
effectiveness of risk selection not only as prevention of adverse perinatal outcomes
but also as prevention of obstetric interventions such as a caesarean section.7-9 While
we recognise that the assessment of risk selection must be weighed against the risk of
possibly unnecessary obstetric interventions, the primary goal of adequate risk selection
and subsequent referral is to prevent adverse perinatal and/or maternal outcomes, the
prevention of (unnecessary) obstetric interventions being an important secondary goal.6,9,27
Several reports have expressed concern on the effectiveness of risk selection in Dutch
primary obstetric care.2,4,10 A recent Dutch study revealed that in 43% of Neonatal Intensive
Care Unit (NICU) admissions the pregnancy had been indicated as low risk, and thus
parturition had started in primary obstetric care.10 Furthermore, infants of pregnant women
at supposedly low risk whose labor started in primary care had a significantly higher delivery
related perinatal mortality risk than the infants of assumed high risk women whose labor
started in secondary care (relative risk 2.33, confidence interval 1.12-4.83).4 Infants of women
who were referred during parturition had a 3.66 times higher risk of delivery related perinatal
mortality than infants of women who started labor in secondary care, and a 2.5-fold higher
risk of NICU admission.4 These studies emphasise that the level of healthcare provision
could be improved for a proportion of supposedly low risk pregnant women at the onset
of labor. Whether the delay in referral is related to late diagnosis (no continuous fetal heart
rate monitoring during parturition in primary care), transport to hospital or assessment
(‘primary care is supposedly low risk’), is yet unclear.4,10
Possible implications
Our results demonstrate that the aim of risk selection in Dutch primary obstetric care
is suboptimally attained. We propose some directions of improvement. As stated in the
‘List of Obstetric Interventions’, risk selection is currently exclusively done by primary
care community midwives. Possible improvements could be the increase of midwives’
competence and capabilities, or introduction of a checklist-based standardised risk

127
RISK SELECTION
IN D
UTCH
OBSTETRIC CA
RE
7
selection strategy at first antenatal booking. However, we believe that the required pace
of change is more likely to be achieved through a combination of the latter with ‘shared
care’: better cooperation between midwives and obstetricians who are jointly responsible
for the determination of a woman’s risk status, thereby joining their expertise which is either
physiology-based (midwives) or pathology-based (obstetricians).28 Shared obstetric care
has already been implemented in some form in other Western countries such as Australia
and the United Kingdom.29-31 One study demonstrated a 27% increase in the detection rate
of intrauterine growth restriction for women receiving shared obstetric care as opposed to
conventional obstetric care.32 For more generalisable results however, a study to evaluate
different shared care strategies has to be conducted in The Netherlands because of the
unique system of obstetric care. We believe that our recommendation for shared care also
applies to countries which are considering or already have an obstetric care system with
features similar to the Dutch system, such as Canada.33-36
REFERENCES1. Mohangoo AD, Buitendijk SE, Hukkelhoven CW, et
al. Higher perinatal mortality in The Netherlands than in other European countries: the Peristat-II study. Ned Tijdschr Geneeskd. 2008;152:2718-2727.
2. Bonsel GJ, Birnie E, Denktas S, Poeran J, Steegers EAP. Dutch report: Lijnen in de Perinatale Sterfte, Signalementstudie Zwangerschap en Geboorte 2010. Rotterdam: Erasmus MC; 2010.
3. Sheldon T. Obstetric care must change if Nether-lands is to regain reputation for safe childbirth. BMJ. 2008;336:c239.
4. Evers AC, Brouwers HA, Hukkelhoven CW, et al. Perinatal mortality and severe morbidity in low and high risk term pregnancies in the Netherlands: prospective cohort study. BMJ. 2010;341:c5639.
5. Amelink-Verburg MP, Buitendijk SE. Pregnancy and labour in the Dutch maternity care system: what is normal? The role division between mid-wives and obstetricians. J Midwifery Womens Health. 2010;55:216-225.
6. Bais JMJ, Pel M. The basis of the Dutch obstetric system: risk selection. Eur Clinics Obstet Gynaecol. 2007;2:209-212.
7. Eskes M. Het Wormerveeronderzoek. Meer-jarenonderzoek naar de kwaliteit van de verlos-kundige zorg rond een vroedvrouwenpraktijk. Thesis 1989, University of Amsterdam.
8. Berghs G, Spanjaards E. De normale zwanger-schap: bevalling en beleid. Thesis 1988, Catholic University Nijmegen.
9. Bais JMJ. Risk selection and detection. A critical appraisal of the Dutch obstetric system. Thesis 2004, University of Amsterdam.
10. Evers AC, van Leeuwen J, Kwee A, et al. Mortality and morbidity among full-term neonates in a neonatal intensive care unit in the Utrecht region, the Netherlands. Ned Tijdschr Geneeskd. 2010;154:118.
11. Sheldon T. Prompt access to expert care is among advice to reduce perinatal deaths in Netherlands. BMJ. 2010;340:c277.
12. World Health Organization. Neonatal and perinatal mortality. Country, regional and global estimates. Geneva: WHO, 2006. (online: http://whqlibdoc.who.int/publications/2006/9241563206_eng.pdf).
13. Perinatal care in The Netherlands 2007 (in Dutch: Perinatale zorg in Nederland 2007). Utrecht: The Netherlands Perinatal Registry; 2009.

128
RISK SELECTION
IN D
UTCH
OBSTETRIC CA
RE
7
14. Tromp M, Meray N, Ravelli AC, Reitsma JB, Bonsel GJ. Medical Record Linkage of Anonymous Registries without Validated Sample Linkage of the Dutch Perinatal Registries. Stud Health Technol Inform. 2005;116:125-130.
15. Van der Kooy J, Poeran J, de Graaf JP, et al. Planned home compared with planned hospital births in the Netherlands: intrapartum and early neonatal death in low-risk pregnancies. Obstet Gynecol. 2011;118:1037-1046.
16. Kloosterman GJ. On intrauterine growth. Int J Gynaecol Obstet. 1970;8:895-912.
17. Gent, van WPC. Realistic regeneration -housing contexts and social outcomes of neighbourhood interventions in Western European cities-; chapter 4. Thesis 2009, University of Amsterdam. (online: http://dare.uva.nl/document/153004).
18. Figueras F, Gardosi J. Intrauterine growth restric-tion: new concepts in antenatal surveillance, di-agnosis, and management. Am J Obstet Gynecol. Apr 2011;204:288-300.
19. Altman DG, Bland JM. Diagnostic tests 2: Predictive values. BMJ. 1994;309:102.
20. Altman DG, Bland JM. Diagnostic tests. 1: Sensitivity and specificity. BMJ. 1994;308:1552.
21. Deeks JJ, Altman DG. Diagnostic tests 4: likelihood ratios. BMJ. 2004;329:168-169.
22. Kennare RM, Keirse MJ, Tucker GR, Chan AC. Planned home and hospital births in South Aus-tralia, 1991-2006: differences in outcomes. Med J Aust. 2010;192:76-80.
23. National Institute for Health and Clinical Excellence (see Antenatal Care: Routine Care for the Healthy Pregnant Woman). (online: http://www.nice.org.uk/nicemedia/live/11947/40115/40115.pdf).
24. Chervenak FA, McCullough LB, Brent RL, Levene MI, Arabin B. Planned home birth: the professional responsibility response. Am J Obstet Gynecol. 2013;208:31-38.
25. Brocklehurst P, Hardy P, Hollowell J, et al. Perinatal and maternal outcomes by planned place of birth for healthy women with low risk pregnancies: the Birthplace in England national prospective cohort study. BMJ. 2011;343:d7400.
26. De Neef T, Hukkelhoven CW, Franx A, van Everhardt E. Uit de lijn der verwachting. Nederl Tijdschrift Obstet Gynaecol 2009;122:34-342.
27. National Institute for Health and Clinical Excel-lence. Intrapartum care: care of healthy women and their babies during childbirth. CG55. 2007. (online: www.nice.org.uk/nicemedia/pdf/IPC-NICEGuidance.pdf ).
28. Posthumus AG, Scholmerich VL, Waelput AJ, et al. Bridging Between Professionals in Perinatal Care: Towards Shared Care in The Netherlands. Matern Child Health J. 2012 (in press).
29. Halliday J. WUDWAW ‘Who Usually Delivers Whom and Where’, Perinatal Data Collection Unit. Victoria, Australia: Victorian Government Department of Human Services; 1999.
30. Hampson JP, Roberts RI, Morgan DA. Shared care: a review of the literature. Fam Pract. 1996;13:264-279.
31. Tucker J, Florey CD, Howie P, McIlwaine G, Hall M. Is antenatal care apportioned according to obstetric risk? The Scottish antenatal care study. J Public Health Med. 1994;16:60-70.
32. Chan FY, Pun TC, Tse LY, Lai P, Ma HK. Shared antenatal care between family health services and hospital (consultant) services for low risk women. Asia Oceania J Obstet Gynaecol. 1993;19:291-298.
33. De Vries R, Benoit C, Van Teijlingen E, Wrede S. Birth by design: pregnancy, maternity care and midwifery in North America and Northern Europe. New York: Routledge, 2001.
34. Hatem M, Sandall J, Devane D, Soltani H, Gates S. Midwife-led versus other models of care for childbearing women. Cochrane Database Syst Rev. 2008:CD004667.
35. Bick D. Enhancing safety in the maternity services: a greater role for midwife-led care? Midwifery. 2009;25:1-2.
36. Royal College of Obstetricians and Gynaecologists/Royal College of Midwives. Home births. Joint statement No.2; 2007 (online: http://www.rcog.org.uk/files/rcog-corp/uploaded-files/JointStatmentHomeBirths2007.pdf).

8
Obstetrics and Gynecology. 2011;118:1037-46.
Planned home compared with planned hospital births in The Netherlands: intrapartum and
early neonatal death in low-risk pregnancies
J. van der Kooy, J. Poeran, J.P. de Graaf, E. Birnie, S. Denktaş, E.A.P. Steegers, G.J. Bonsel

130
PLAN
NED
HO
ME CO
MPA
RED W
ITH PLA
NN
ED H
OSPITA
L BIRTHS
8
ABSTRACTObjective The purpose of our study was to compare the intrapartum and early neonatal
mortality rate of planned home birth vs. planned hospital birth in community midwife-led
deliveries, after case mix adjustment.
Methods Perinatal outcome of 679,952 low-risk women was obtained from the Dutch
Perinatal Registry (2000-2007). This group represents all women who had a choice between
home and hospital birth. Two different analyses were performed; natural prospective
approach (intention-to-treat like analysis) and perfect guideline approach (per-protocol like
analysis). Unadjusted and adjusted odds ratios were calculated. Case mix was based on the
presence of at least one of the following: congenital abnormalities, small for gestational age,
preterm birth, or low Apgar score. We also investigated the potential risk role of intended
place of birth. The technique used was multivariable stepwise logistic regression.
Results Intrapartum and neonatal death 0-7 days was observed in 0.15% of planned
home vs 0.18% in planned hospital births (crude RR 0.80 95%CI 0.71-0.91). After case mix
adjustment, the relation is reversed, showing non-significant increased mortality risk of
home birth (OR 1.05 95%CI 0.91-1.21). In certain subgroups additional mortality may arise
at home if risk conditions emerge at birth (up to 20% increase).
Conclusion Home birth, under routine conditions, is generally not associated with
increased intrapartum and early neonatal death, yet in subgroups additional risk cannot
be excluded.

131
PLAN
NED
HO
ME CO
MPA
RED W
ITH PLA
NN
ED H
OSPITA
L BIRTHS
8
INTRODUCTIONThe debate on the safety of home births continues in the literature as recently addressed
in the Lancet.1 In the Netherlands, approximately 50% of women give birth under the
supervision of a community midwife. The community midwives are independent health
care professionals in the Netherlands, operating either solely or in group practices. The
proportion of home birth deliveries in the Netherlands has steadily decreased over the
last decade but is currently stable at 25% of all births. Several Anglo-Saxon countries are
considering the reintroduction of home births, based on recent claims of sufficient safety.2
The reverse trend is observed in the Netherlands, where the debate has intensified since
the national perinatal mortality rate showed to be one of the highest in Europe.3
In the Dutch system, independently operating community midwives provide care for low-
and medium-risk pregnant women (primary healthcare). High-risk pregnant women are
referred to the gynaecologist for remaining ante- and intrapartum care. If no or only a few
risk factors are present, women can stay with the midwife and decide where the delivery
will take place: at home or in the hospital, both supervised by the community midwife.
For pregnant women with so called ‘medium-risk’ delivery in hospital is obligatory but can
still be under the supervision of the community midwife. A strict definition of medium
risk, created and agreed upon by midwives and gynaecologists together, is defined in the
Dutch guidelines.4 The claimed benefits of planned home births include the reduction of
maternal-fetal morbidity, a lower risk for unjustified medical interventions, and psychosocial
advantages for the mother. These benefits may be counterbalanced by the disadvantages
associated with a high intrapartum referral rate and an increased perinatal mortality,
morbidity and long term negative effects.5-11
This paper re-addresses the Dutch evidence focusing on two critical features of previous
analyses. First, previous studies compared outcomes after exclusion of pregnant women
who in view of the delivery guidelines should have been referred to a gynaecologist. Second,
previous studies did not apply case mix analysis, assuming risk equivalence of home and
hospital groups.5,9,12-18 Case mix may, however, differ across planned place of delivery, due
to self selection or due to the midwife’s proposal, with the healthiest and most affluent
women receiving home birth (confounding the comparison by indication bias).5 6,7,11,19-21
The purpose of our study was to compare the intrapartum and early neonatal mortality
rate of planned home birth vs. planned hospital birth in community midwife-led deliveries,
after case mix adjustment. We compared a natural prospective approach without ex post
exclusion of unsuitable midwife cases (intention-to-treat like), with the conventional

132
PLAN
NED
HO
ME CO
MPA
RED W
ITH PLA
NN
ED H
OSPITA
L BIRTHS
8
approach based on a theoretical midwife population under perfect guideline adherence
(per-protocol like). We hypothesised that while in general no difference may exist between
home and hospital outcomes, for specific risk groups the hospital setting is protective as
obstetrical and neonatal expertise and clinical facilities are directly available (so-called
“setting safety”).
METHODS
Data
The Netherlands Perinatal Registry (PRN) contains population-based information of 96%
of all pregnancies in The Netherlands. Source data are collected by 95% of midwives,
99% of gynaecologists and 68% of paediatricians (including 100% of Neonatal Intensive
Care Unit paediatricians).3,22 (See website for detailed description: www.perinatreg.nl). We
selected the records of all singleton pregnant women, under supervision of a community
midwife at the onset of labour between 2000-2007 (693,592 women). The onset of labour
was defined as spontaneous contractions or the spontaneous rupture of membranes by
the PRN. Two subsets of pregnant women were further excluded from the original set of
693,592 women. First, 13,384 women with so called ‘medium risk’, for example women with
a history of postpartum haemorrhage or obesity (BMI>30). Dutch guidelines prescribe a
hospital delivery for these women which may be supervised by the community midwife.
Secondly we excluded records were the data was incomplete (n=256).
The remaining women (n=679,952) were categorised according to intended place of birth,
which usually is concordant with the observed place of birth either home or hospital. For
some women the place was not decided until the onset of labour. This could be due to
indifference on the part of the woman; or delayed antepartum care. The intended place
was then coded ‘unknown’. This yielded 3 intention groups: home, hospital, and, unknown.
Outcome measures, maternal and neonatal risk factors
Outcome was defined as intrapartum and early neonatal mortality , i.e. (I) intrapartum
death, (II) neonatal death up to 24 hrs, and (III) neonatal death up from 1 day to 7 days post
partum. In our low risk group under midwife supervision, mortality beyond 8 days is rare,
and regarded to be unrelated to place of delivery. The PRN does not include long term child
outcomes for example psychomotor development and behavioural function.

133
PLAN
NED
HO
ME CO
MPA
RED W
ITH PLA
NN
ED H
OSPITA
L BIRTHS
8
Maternal risk factors were parity (nulliparous vs. multiparous), age, ethnicity (Western/non-
Western; based on a more refined classification in the registry), and living in a deprived
neighbourhood (yes/no, based on 4-digit zip-codes and a public list of deprived, zip-code
based, neighbourhoods issued by the Dutch government).
Detailed risk information is unavailable in national registries. Case mix of any defined
group of women was primarily represented by the prevalence (single or combined) of
‘Big4’ conditions (see below). From detailed analysis of the complete perinatal dataset of
the same Netherlands Perinatal Registry (PRN), years 2000-2007, (1.25 million records)23, it
appeared that the presence of any of 4 conditions preceded perinatal mortality in 85% of
cases. These conditions were defined as; congenital abnormalities (list defined), small for
gestational age (SGA, birth weight below the 10th percentile for gestational age, gender and
parity specific), preterm birth (< 37th week of gestation) or low Apgar score (< 7, measured
5 minutes after birth). We will continue to refer to these 4 conditions as the ‘Big4’. The main
results of this detailed analysis are found in figure 8.1.
In our current analysis these so called ‘Big4’ represent an objective estimate of the risk
challenge at birth. The preventability of their occurrence, either antenatally or during
delivery, is not at issue. Here we intentionally use it as a risk indicator, an explanatory
factor at onset. By doing so, we ignore differential management effects of setting on the
emergence of these Big4, in particular low Apgar, should they exist.
Data analysis
As primary analysis we present the results of the natural prospective approach (NPA), resem-
bling an intention-to-treat analysis. For comparison we added a perfect guideline approach
(PGA), resembling a per-protocol analysis. The NPA approach establishes, within observational
constraints, the intrapartum and early neonatal death of planned home versus planned hospital
births. It stems from the viewpoint of a pregnant woman starting birth under supervision of
a midwife (the denominator is n=679,952). The natural approach thus includes spontaneous
preterm labour since to some extent this group was not referred to the gynaecologist during
labour or was referred late during (home) delivery. Therefore a direct setting effect (admission
to hospital at the onset of labour) may be visible to the advantage of the hospital. Furthermore
indirect setting effects may be present, for example the timing of referral.
PGA includes the subset of women within the NPA population, who in retrospect were
compliant with the guidelines which define low risk at the onset of labour and therefore
allowed to choose between a home or hospital birth under supervision of a midwife.

134
PLAN
NED
HO
ME CO
MPA
RED W
ITH PLA
NN
ED H
OSPITA
L BIRTHS
8
Non-compliance exists if a high risk condition was already detectable at the onset of labour.
These conditions applied to women with a gestational age <37 or >41 weeks, prolonged
rupture of membranes (>24hr) and intrauterine death with unclear timing relative to onset
of labour (see figure 8.2). PGA (n=602,331) still included undetected SGA and congenital
malformations that emerge at birth, as detection failure cannot be regarded as non-
compliance from the viewpoint of current guidelines.
First we compared characteristics of the NPA and PGA populations by intended place of
birth (t-tests for comparisons). Then we investigated the potential risk role of intended place
Figure 8.1 Perinatogram illustrating in a Venn diagram the relationship between (combinations of ) Big 4 morbidities and perinatal mortality defined as death from 22 weeks of gestational age until 7 days postpartum. In 85% of all cases of perinatal mortality, one or more Big4 morbidities are present; for instance, a low Apgar score combined with preterm birth occurs in 30.3% of all cases of perinatal mortality. *Prevalence per 1,000 births of separate and combined Big 4 morbidities and their contribution to all cases of perinatal mortality (†percentage); this adds up to 85% of all cases of perinatal mortality. The dashed circles connect low Apgar score with preterm birth and congenital abnormality with intrauterine growth restriction.

135
PLAN
NED
HO
ME CO
MPA
RED W
ITH PLA
NN
ED H
OSPITA
L BIRTHS
8
of birth by a set of predefined nested multivariable logistic regression models (stepwise
analysis; inclusion p<0.05; exclusion p>0.10) where we added maternal and neonatal (case
mix) explanat ory variables. For these variables, hospital birth was set as the reference.
All stepwise analyses were repeated with a forward and backward approach, and finally
forced inclusion of predictive variables (p<0.05). Risk factor coefficients were only shown
Figure 8.2 Flow of women through the study.

136
PLAN
NED
HO
ME CO
MPA
RED W
ITH PLA
NN
ED H
OSPITA
L BIRTHS
8
in case of significance p<0.05. Results across the three approaches were similar unless
stated otherwise.
We graphically described the crude mortality of the planned home and planned hospital
population, for the series of populations which result from successive exclusion of women
meeting a criterion for non-compliance (figure 8.3; dotted lines). This successive exclusion
through non-compliance criteria gradually transforms the NPA population into the PGA
population. If the mortality rate of a non-compliance group is average, home and hospital
mortality rates do not change on its exclusion. If the rates decrease at a different gradient
(e.g. hospital steeper than home, as after exclusion of pregnancy duration < 36 weeks) this
may point to either differential prevalence of the non-compliance factor (as here), or to
differential case fatality by setting where the largest mortality decrease is observed in the
setting with the highest case fatality (interpretable as lowest setting safety).
To support this interpretation, we first divided the crude mortality of the home and hospital
group by the respective prevalence of Big4 conditions to obtain case mix adjustment. This
assumes Big4 prevalence to be a suitable risk indicator at the group level. Subsequent
division of the resulting home/Big4 mortality ratio by the hospital/Big4 mortality yields
an index (Big4 adjusted homebirth mortality index; figure 8.3; black line). If this index is
100%, then relative mortality in home births and hospital births is equal. If the index is for
example 120%, then home births have 20% excess mortality taking our case mix differences
into account. Combining crude mortality changes with index changes allows for tentative
interpretation of setting effects.
RESULTSTable 8.1 describes the baseline characteristics of both the NPA and PGA populations
(n=679,952 vs. 602,331).
In both the NPA and PGA populations about 60% of women planned a home delivery and
about 32% planned a hospital delivery. Compared to women who planned birth in the
hospital or with unknown location, the women with planned home birth were more likely to
be multiparous, 25 years or older, of Dutch origin and to live in a privileged neighbourhood
(all of which are favourable conditions). In home birth women, neonatal case mix compared
also favourably. Premature delivery was less common, as was the prevalence of a Big4
condition (NPA home birth 8.7% vs. hospital 10.8% vs. unknown 10.5%; PGA home birth
6.5% vs. hospital 8.2% vs. unknown 7.5%; p<0.001 in both cases).

137
PLAN
NED
HO
ME CO
MPA
RED W
ITH PLA
NN
ED H
OSPITA
L BIRTHS
8
Intrapartum and early neonatal mortality was 1099/679,952=1.62 ‰ in the NPA women and
551/602,331=0.91‰ in PGA women. Mortality was lower in women who were multiparous,
between 24-34 year, of Dutch origin, or living in a privileged neighbour hood (both NPA and
PGA), see table 8.1. Within the group with intrapartum and early neonatal mortality, Big4
conditions were found in 792 of the 1099 deaths (72.1%) in the NPA women, compared to
290 out of 551 deaths (52.6%) in the PGA group.
In the NPA population, crude mortality risk was significantly lower for women who planned
to give birth at home (RR 0.80 95%CI 0.71-0.91) and for women with unknown intention (RR
0.96 95%CI 0.77-1.19) compared to those who intended to give birth in hospital (P<0.05) (see
table 8.2). All maternal and neonatal risk factors, except living in a deprived neighbourhood,
showed significant effect sizes in agreement with the expected direction. Mortality was
significantly increased in infants with a Big4 outcome, especially in infants with multiple
Big4 conditions (RR 168.9 95%CI 148.9-191.4).
The nested multivariable logistic regression analysis showed that in the presence of
adjusting maternal factors only (model 2), the intended place of birth had no significant
impact on outcome. The maternal factors showed risks similar to the univariable (crude)
analysis. The addition of Big4 case mix adjustment (model 3) showed the intended place of
birth to be a significant co-variable, yet the contrast of planned home birth (OR 1.05 95%CI
0.91-1.21) vs. hospital birth (reference=1) turned out to be non-significant. The effect of
maternal risk factors was affected to a limited degree by the introduction of Big4 case mix.
We repeated the analysis for the PGA population (table 8.3). The results of the crude analysis
were close to the NPA analysis. However, the effect of ethnic background was considerably
stronger in the PGA population. In all analyses the intended place of birth showed a
consistent significant impact on intrapartum and early neonatal mortality, yet the contrast
between home and hospital birth never reached statistical difference. After Big4 case mix
adjustment home birth showed a non-significant increased risk (OR 1.11 95%CI 0.93-1.34).
Figure 8.3 describes the crude mortality risk (left Y-axis) and the Big4 adjusted home birth
mortality index (right Y-axis), where each dot represents the mortality risk results after the
group listed on the X-axis has been excluded from the population.
The crude mortality (dotted lines) initially shows a difference in favour of home delivery
(home: 0.18% vs. hospital: 0.22%), which converges towards a much lower average level if
premature births are excluded. Further exclusions lower the crude mortality rate, leaving the
small difference almost unaffected. The mortality index (black line) shows a distinct change
from an initial level of about 100% towards about 120% after exclusion of the pregnancy

138
PLAN
NED
HO
ME CO
MPA
RED W
ITH PLA
NN
ED H
OSPITA
L BIRTHS
8
Ta
ble
8.1
Ch
arac
teris
tics
and
outc
omes
of
wom
en in
prim
ary
care
at
the
onse
t of
labo
ur (n
atur
al p
rosp
ectiv
e ap
proa
ch a
nd p
erfe
ct g
uide
line
appr
oach
)*
Varia
ble
Plan
ned
hom
e bi
rth
Plan
ned
hosp
ital b
irth
Plan
ned
plac
e un
know
nIn
trap
artu
m a
nd e
arly
ne
onat
al d
eath
NPA
PG
A
NPA
PG
A
NPA
PGA
N
PA
PGA
Parit
y†40
2,91
2 (5
9.3)
363,
568
(60.
4)21
9,10
5 (3
2.2)
190,
098
(31.
6)57
,935
(8.5
)48
,665
(8.1
)67
9,95
260
2,33
1Pr
imip
arou
s17
1,98
6 (4
2.69
)14
8,08
2 (4
0.73
)10
4,24
9 (4
7.58
)88
,110
(46.
35)
26,2
54 (4
5.32
)21
,047
(43.
25)
614
(0.2
0)28
3 (0
.11)
Mul
tipar
ous
230,
926
(57.
31)
215,
486
(59.
27)
114,
856
(52.
42)
101,
988
(53.
65)
31,6
81 (5
4.68
)27
,618
(56.
75)
485
(0.1
3)26
8 (0
.08)
Mat
erna
l age
(y)†
Youn
ger t
han
194,
036
(1.0
0)3,
502
(0.9
6)6,
713
(3.0
6)5,
770
(3.0
4)1,
190
(2.0
5) 9
10 (1
.87)
42 (0
.35)
13 (0
.13)
20-2
534
,661
(8.6
0)30
,787
(8.4
7)32
,617
(14.
89)
28,6
69 (1
5.08
)6,
823
(11.
78)
5,61
1 (1
1.53
)13
3 (0
.18)
65 (0
.10)
25-3
429
6,12
8 (7
3.50
)26
7,40
8 (7
3.55
)14
2,59
7 (6
5.08
)12
4,07
1 (6
5.27
)39
,526
(68.
22)
33,5
83 (6
9.01
)69
3 (0
.14)
348
(0.0
8)O
lder
than
35
68,0
87 (1
6.90
)61
,871
(17.
02)
37,1
78 (1
6.97
)31
,588
(16.
62)
10,3
96 (1
7.94
)8,
559
(17.
59)
231
(0.2
0)12
5 (0
.12)
Ethn
ic b
ackg
roun
d†
Wes
tern
364,
796
(90.
54)
329,
677
(90.
68)
143,
677
(65.
57)
124,
144
(65.
31)
45,2
05 (7
8.03
)38
,508
(68.
80)
880
(0.1
6)45
2 (0
.09)
Non
Wes
tern
38,1
16 (9
.46)
33,8
91 (9
.32)
75,4
28 (3
4.43
)65
,954
(34.
69)
12,7
30 (2
1.97
)17
,461
(31.
20)
219
(0.1
7)99
(0.0
8)
Nei
ghbo
urho
od†
Priv
ilege
d ne
igh-
bour
hood
388,
089
(96.
32)
350,
346
(96.
36)
196,
659
(89.
76)
170,
366
(89.
62)
53,8
23 (9
2.90
)45
,425
(93.
34)
1,03
1 (0
.16)
518
(0.0
9)
Und
erpr
ivile
ged
neig
hbou
rhoo
d14
,823
(3.6
8)13
,222
(3.6
4)22
,446
(10.
24)
19,7
32 (1
0.38
)4,
112
(7.1
0)3,
240
(6.6
6)68
(0.1
6)33
(0.0
9)

139
PLAN
NED
HO
ME CO
MPA
RED W
ITH PLA
NN
ED H
OSPITA
L BIRTHS
8
Ges
tatio
nal a
ge (w
k)†
Less
than
34
2,40
9 (0
.60)
1,70
2 (0
.78)
583
(1.0
1)37
0 (7
.88)
35-3
66,
510
(1.6
2)4,
064
(1.8
5)1,
206
(2.0
8)65
(0.5
5)37
15,2
03 (3
.77)
13,6
22 (3
.75)
9,60
3 (4
.38)
8,46
8 (4
.45)
2,49
7 (4
.31)
2,18
7 (4
.49)
56 (0
.21)
51 (0
.21)
38-4
136
8,92
6 (9
1.56
)34
9,94
6 (9
6.25
)19
3,81
6 (8
8.46
)18
1,63
0 (9
5.55
)49
,585
(85.
59)
46,4
78 (9
5.51
)54
8 (0
.09)
500
(0.0
9)M
ore
than
41
9,86
4 (2
.45)
9,92
0 (4
.53)
4,06
4 (7
.01)
60 (0
.25)
Big4
†
Smal
l for
gest
atio
nal a
ge18
,786
(4.6
6)17
,089
(4.7
0)13
,114
(5.9
9)11
,604
(6.1
0)3,
081
(5.3
2)2,
665
(5.4
8)71
(0.2
0)59
(0.1
9)
Prem
atur
e8,
090
(2.0
1)5,
117
(2.3
4)1,
547
(2.6
7)92
(0.6
2)0.
00Lo
w A
pgar
scor
e1,
692
(0.4
2)1,
483
(0.4
1)1,
180
(0.5
4)95
9 (0
.50)
289
(0.5
0)22
8 (0
.47)
97 (3
.07)
86 (3
.22)
Cong
enita
l ab
nom
ality
4,87
4 (1
.21)
4,36
6 (1
.20)
2,94
1 (1
.34)
2,53
1 (1
.33)
778
(1.3
4)65
5 (1
.35)
74 (0
.86)
60 (0
.79)
Com
bina
tion
Big4
1,64
8 (0
.41)
693
(0.1
9)1,
279
(0.5
8)45
3 (0
.24)
391
(0.6
7)92
(0.1
9)45
8 (1
3.80
)85
(6.8
7)To
tal B
ig4
35,0
90 (8
.71)
23,6
31 (6
.50)
23,6
31 (1
0.79
)15
,547
(8.1
8)6,
086
(10.
50)
3,64
0 (7
.48)
792
(1.2
2)29
0 (0
.68)
NPA
, nat
ural
pro
spec
tive
appr
oach
; PG
A, p
erfe
ct g
uide
line
appr
oach
.D
ata
are
n (%
).* T
otal
s m
ay n
ot a
dd u
p to
100
bec
ause
of r
ound
ing
erro
r.† P
<.00
1.

140
PLAN
NED
HO
ME CO
MPA
RED W
ITH PLA
NN
ED H
OSPITA
L BIRTHS
8
Ta
ble
8.2
In
trap
artu
m a
nd n
eona
tal d
eath
0-7
day
s in
wom
en w
ho a
re in
prim
ary
care
at t
he o
nset
of l
abou
r (na
tura
l pro
spec
tive
appr
oach
)
Mod
el 1
Mod
el 2
Mod
el 3
Tota
lM
orta
lity
pCr
ude
RR
95%
CI
pAd
just
ed
OR
95%
CI
pAd
just
ed
OR
95%
CI
p
Inte
nded
pla
ce o
f birt
h<.
05<.
05<.
05H
ome
402,
912
594
(0.1
5)0.
800.
71–0
.91
nie
1.05
0.91
–1.2
1H
ospi
tal [
ref]
219,
105
403
(0.1
8)1
1U
nkno
wn
57,9
3510
2 (0
.18)
0.96
0.77
–1.1
9ni
e0.
770.
61–0
.97
Parit
y <
.001
<.0
01 <
.001
Prim
ipar
ous
302,
489
614
(0.2
0)1.
581.
40–1
.78
1.67
1.47
–1.8
9ni
eM
ultip
arou
s [r
ef]
377,
463
485
(0.1
3)1
1
Mat
erna
l age
(y)
<.0
01 <
.001
<.0
01 <.
001
Youn
ger t
han
1911
,939
42 (0
.35)
2.43
1.78
–3.3
11.
801.
31–2
.48
1.67
1.17
–2.3
820
-25
74,1
0113
3 (0
.18)
1.24
1.03
–1.4
91.
030.
85–1
.24
0.92
0.75
–1.1
325
-34
[ref]
478,
017
693
(0.1
4)1
11
Old
er th
an 3
511
5,66
123
1 (0
.20)
1.38
1.19
–1.6
01.
561.
34–1
.81
1.44
1.23
–1.6
8
Ethn
ic b
ackg
roun
d <
.001
<.0
01<.
05<.
05W
este
rn [r
ef]
571,
185
880
(0.1
5)1
11
Non
-Wes
tern
108,
767
219
(0.2
0)1.
311.
13–1
.52
1.32
1.14
–1.5
41.
211.
02–1
.45

141
PLAN
NED
HO
ME CO
MPA
RED W
ITH PLA
NN
ED H
OSPITA
L BIRTHS
8
Nei
ghbo
urho
od<.
05Pr
ivile
ged
neig
h-bo
urho
od [r
ef]
638,
571
1,03
1 (0
.16)
1
Und
erpr
ivile
ged
neig
hbou
rhoo
d41
,381
68 (0
.16)
1.02
0.80
–1.3
0ni
eni
e
Ges
tatio
nal a
ge (w
k) <
.001
<.0
01 <.
001
Less
than
34
4,69
437
0 (7
.88)
88.0
877
.44–
100.
1815
.74
12.5
6–19
.72
35-3
611
,780
65 (0
.55)
6.17
4.77
–7.9
72.
111.
56–2
.86
3727
,303
56 (0
.21)
2.29
1.74
–3.0
22.
261.
71–2
.99
38-4
1 [r
ef]
612,
327
548
(0.0
9)1
1M
ore
than
41
23,8
4860
(0.2
5)2.
812.
15–3
.67
2.10
1.60
–2.7
7
Big4
<.0
01 <
.001
<.00
1SG
A34
,910
71 (0
.20)
1.27
1.00
–1.6
23.
642.
82–4
.69
Prem
atur
ity14
,754
92 (0
.62)
12.4
99.
90–1
5.76
Low
apg
ar3,
161
97 (3
.07)
21.3
517
.28–
26.3
853
.41
42.5
5–67
.04
Cong
enita
l ab
nom
ality
8,59
374
(0.8
6)5.
684.
48–7
.20
14.5
311
.30–
18.6
7
Com
bina
tion
Big4
3,31
845
8 (1
3.80
)16
8.85
148.
94–1
91.4
168
.17
55.2
7–84
.08
No
Big4
615,
145
307
(0.0
5)1
RR, r
elat
ive
risk;
CI,
confi
den
ce in
terv
al; O
R, o
dds
ratio
; nie
, not
in e
quat
ion.
Dat
a ar
e n
or n
(%) u
nles
s ot
herw
ise
spec
ifi ed
.M
odel
1: c
rude
RR.
Mod
el 2
: adj
uste
d fo
r mat
erna
l fac
tors
incl
udin
g in
tend
ed p
lace
of b
irth,
par
ity, a
ge, e
thni
c ba
ckgr
ound
, and
nei
ghbo
rhoo
d. M
odel
3: a
djus
ted
for
mat
erna
l fac
tors
and
chi
ld fa
ctor
s; m
odel
2 +
ges
tatio
nal a
ge a
nd p
rese
nce
of B
ig4.

142
PLAN
NED
HO
ME CO
MPA
RED W
ITH PLA
NN
ED H
OSPITA
L BIRTHS
8
Ta
ble
8.3
In
trap
artu
m a
nd n
eona
tal d
eath
0-7
day
s in
wom
en w
ho a
re in
prim
ary
care
at t
he o
nset
of l
abou
r (pe
rfec
t gui
delin
e ap
proa
ch)
Mod
el 1
Mod
el 2
Mod
el 3
Tota
l (n)
Mor
talit
yCr
ude
RR
95%
CI
pAd
just
ed
OR
95%
CI
pAd
just
ed
OR
95%
CI
p
Inte
nded
pla
ce o
f birt
h<.
05<.
05<.
05H
ome
363,
568
344
(0.0
9)0.
990.
83–1
.18
1.02
0.85
–1.2
31.
110.
93–1
.34
Hos
pita
l [re
f]19
0,09
818
2 (0
.10)
11
1U
nkno
wn
48,6
6525
(0.0
5)0.
540.
35–0
.81
0.54
0.36
–0.8
30.
570.
37–0
.86
Parit
y <.
001
<.00
1Pr
imip
arou
s25
7,23
928
3 (0
.11)
1.42
1.20
–1.6
71.
521.
28–1
.82
nie
Mul
tipar
ous
[ref
]34
5,09
226
8 (0
.08)
11
Mat
erna
l age
(y)
<.00
1 <.
001
<.05
Youn
ger t
han
1910
,182
13 (0
.13)
1.56
0.90
–2.7
11.
310.
75–2
.30
1.29
0.73
–2.2
620
-25
65,0
6765
(0.1
0)1.
220.
94–1
.59
1.11
0.84
–1.4
51.
080.
83–1
.41
25-3
4 [r
ef]
424,
915
348
(0.0
8)1
11
Old
er th
an 3
510
2,01
812
5 (0
.12)
1.50
1.22
–1.8
41.
661.
34–2
.04
1.50
1.22
–1.8
5
Ethn
ic b
ackg
roun
dW
este
rn [r
ef]
507,
063
452
(0.0
9)1
Non
-Wes
tern
94,7
1799
(0.1
0)1.
170.
94–1
.46
nie
nie

143
PLAN
NED
HO
ME CO
MPA
RED W
ITH PLA
NN
ED H
OSPITA
L BIRTHS
8
Nei
ghbo
urho
odPr
ivile
ged
neig
h-bo
urho
od [r
ef]
566,
137
518
(0.0
9)1
Und
erpr
ivile
ged
neig
hbou
rhoo
d36
,194
33 (0
.09)
1.00
0.70
–1.4
2ni
eni
e
Ges
tatio
nal a
ge (w
k) <.
001
<.00
137
24,2
7751
(0.2
1)2.
431.
82–3
.24
2.51
1.87
–3.3
738
-41
[ref]
578,
054
500
(0.0
9)1
1
Big3
<.00
1 <.
001
SGA
31,3
5859
(0.1
9)4.
033.
04–5
.35
4.28
3.22
–5.6
8Lo
w a
pgar
2,67
086
(3.2
2)69
.05
54.2
8–87
.84
71.5
255
.87–
91.5
6Co
ngen
ital
abno
mal
ity7,
552
60 (0
.79)
17.0
312
.88–
22.5
316
.76
12.6
4–22
.23
Com
bina
tion
Big3
1,23
885
(6.8
7)14
7.19
115.
97–1
86.8
015
9.49
123.
86–2
05.3
8N
o Bi
g355
9,51
326
1 (0
.05)
11
RR, r
elat
ive
risk;
CI,
confi
den
ce in
terv
al; O
R, o
dds
ratio
; nie
, not
in e
quat
ion.
Mod
el 1
: cru
de R
R. M
odel
2: a
djus
ted
for m
ater
nal f
acto
rs in
clud
ing
inte
nded
pla
ce o
f birt
h, p
arity
, age
, eth
nic
back
grou
nd, a
nd n
eigh
borh
ood.
Mod
el 3
: adj
uste
d fo
r m
ater
nal f
acto
rs a
nd c
hild
fact
ors;
mod
el 2
+ g
esta
tiona
l age
and
pre
senc
e of
Big
4.

144
PLAN
NED
HO
ME CO
MPA
RED W
ITH PLA
NN
ED H
OSPITA
L BIRTHS
8
duration <36 weeks. Combined with the similar crude mortality rates of home and hospital
delivery from then onwards, this suggests setting safety for the risk groups still included i.e.
all groups right to the exclusion label ‘pregnancy duration <36 weeks’. For example after
exclusion of pregnancy duration > 41 weeks (PGA group), the adjusted mortality index is
120%, which is slightly larger than the non significant regression result of 111% (table 8.3).
DISCUSSIONPlanned home birth within the Dutch maternity care system has a lower crude mortality
rate compared to a community midwife led planned hospital birth. However, after case
mix adjustment, the relation is reversed, showing a non-significant increased perinatal
mortality rate of home birth. Excess setting dependent mortality may arise at home if
risk conditions are present or emerge at birth, yet remnant confounding by indication
effect (Big4 conditions are more prevalent in hospital) and low mortality prevalence limits
statistical proof. Authors favouring a comparison of settings among ‘suitable’ home births
only (PGA), usually exclude risk conditions with a potential setting effect. This mechanism
may explain the apparently contradictory results from previous studies.1,5,7,10-15,17,18
Figure 8.3 ‘Big4’ adjusted mortality index of home birth (hospital based birth under midwife supervision=100%).
PGANPA

145
PLAN
NED
HO
ME CO
MPA
RED W
ITH PLA
NN
ED H
OSPITA
L BIRTHS
8
A strength of this study was the size of the study population, which reflects the complete
Dutch experience from 2000-2007. The amount of missing explanatory data is negligible,
mortality data have been shown to be complete. No annual trends are observed in the
relations shown, except for a minimal gradual decrease in total perinatal mortality.3
Our case mix adjustment proved to be essential. The assumption of comparability across
home vs. hospital populations appeared not to be justifiable judging from the unequal
prevalence of Big4 conditions. These primarily have their origin in early negative fetal
conditions and disadvantaged genetic background of the parents. Only in the case of low
Apgar, one may argue that the midwifery management during labour might influence it’s
occurrence, while a management role in SGA, spontaneous prematurity, and congenital
anomalies at that stage is unlikely. We decided to include low Apgar cases assuming the
role of management to be small compared to the disadvantage of the home setting once
a child with persistent low Apgar is born. Thus, our point of departure starts from the risk
challenge represented by Big4 at the onset of labour, and investigates whether setting
matters in terms of prognosis. The mechanisms underlying the apparent favourable
selection for home birth are still to be elucidated. Self selection by the pregnant women
can coincide with implicit or explicit selection by the midwife who may tend to ‘refer’ to
hospital if she feels uncomfortable with the risk level at home. The difference in the ratio
home:hospital community midwifery led deliveries among the four largest Dutch cities
suggests the presence of substantial professional and setting effects. In Amsterdam and
Utrecht the ratio is 2:1, and in Rotterdam and the Hague it is 1:2.
Several study limitations merit discussion. While an improvement compared to previous
studies, our case mix control is still incomplete because Big4 is unrelated to 15% of deaths.
In the PGA population this proportion is even 48%. Thus we cannot rule out remnant
confounding by indication as little is known on the factors underlying choice of setting.
RCT would be the superior design to address our research question. However when home
birth was part of a trial, participation hampered24 and introduced selective participation
which limited generalis ability. Moreover if following one’s choice impacts outcome,
estimates of setting effects are also biased.24-26 Despite their shortcomings, in particular
when considering the difficulty to overcome the confounding by indication phenomenon,
observational studies as ours are therefore invaluable. A comparison with a 100%
gynaecologist hospital-based system is not included. The data from an otherwise very
similar country as Flanders27 suggest that more favourable results may be expected in low
risk women in general from a hospital-based system. In Flanders perinatal mortality is about
33% less than in the Netherlands, while the caesarean section rates show little difference.

146
PLAN
NED
HO
ME CO
MPA
RED W
ITH PLA
NN
ED H
OSPITA
L BIRTHS
8
This study primarily focuses upon the disadvantages and neglects the claimed benefits
when comparing planned home versus planned hospital births. However studies accessing
mother’s opinion show that preventing these disadvantages easily outweighs the claimed
benefits.28
Our results appear compatible with most other reports even though previous studies show
conflicting results. Planned home births attended by registered professional attendants are
not associated with an increased risk of adverse perinatal outcomes in cohort studies in
North America7,12, the United Kingdom14, Europe 5,11,15,17, Australia29 and New Zealand30. In
contrast, other cohort studies have shown a higher risk of perinatal mortality in planned
home births compared to planned hospital births.10,13,16,18,30 All studies are limited by
voluntary submission of data7,8,11-14,17,31,32, non representative sampling5,13, lack of appropriate
comparison groups7,12,15,29, or insufficient statistical power5,17,29,32. A critical factor, as our
study shows, is the in retrospect exclusion of unplanned and unsuitable home births from
analysis.18
Our results partly agree with those of Kennare at al.30 who found higher standardised
perinatal mortality ratios among planned home deliveries after limited adjustment (birth
weight, gestational age). Our results also partly agree with the meta-analysis by Wax et al.9:
differences in the prevalence of SGA, premature births and congenital anomalies seem
equally present in planned home vs. hospital births. They reported a twofold higher neonatal
mortality rate but no increase in perinatal mortality. These results are in agreement with
figure 8.3 where the fetal death subgroup does not benefit from setting safety. It should be
noted that the study of Wax et al. received methodological criticisms33-36 most notably the
inclusion of the study of Pang and the exclusion of the study of De Jonge. Our conclusions
apparently contradict those of De Jonge et al. who concluded equal intrapartum and
early neonatal outcome of planned home birth vs. hospital birth in apparently the same
population.15 However, the point of departure is not the same. Of our two comparisons of
home delivery vs. hospital delivery, one parallels the approach of De Jonge. Our principal
approach (NPA) compares neonatal mortality in the actual populations delivering at home
vs. hospital, while the approach of De Jonge compares neonatal mortality in a hypothetical
group resembling our PGA population. Our adjustment procedure however goes further
than the maternal factor adjustment of De Jonge.15
From our study we conclude that planned home birth, under routine conditions, is not
associated with a higher intrapartum and early neonatal mortality rate. However in
subgroups additional risk cannot be excluded.

147
PLAN
NED
HO
ME CO
MPA
RED W
ITH PLA
NN
ED H
OSPITA
L BIRTHS
8
REFERENCES1. Home birth--proceed with caution. Lancet. 2010;
376:303.
2. Royal College of Obstetricians and Gynaecologists/Royal College of Midwives. Home births. Joint statement No.2; 2007 (Online: http://www.rcog.org.uk/files/rcog-corp/uploaded-files/JointStatmentHomeBirths2007.pdf).
3. Ravelli AC, Tromp M, van Huis M, et al. Decreasing perinatal mortality in The Netherlands, 2000-2006: a record linkage study. J Epidemiol Community Health. 2009;63:761-5.
4. CVZ. List of Obstetric Indications (in Dutch: Ver-loskundig Vademecum) 2003. Diemen (online: http://www.knov.nl/docs/uploads/Verloskundig_Vademecum_2003.pdf).
5. Ackermann-Liebrich U, Voegeli T, Gunter-Witt K, et al. Home versus hospital deliveries: follow up study of matched pairs for procedures and outcome. Zurich Study Team. BMJ. 1996;313:1313-8.
6. Hutton EK, Reitsma AH, Kaufman K. Outcomes associated with planned home and planned hospital births in low-risk women attended by midwives in Ontario, Canada, 2003-2006: a retrospective cohort study. Birth. 2009;36:180-9.
7. Janssen PA, Saxell L, Page LA, Klein MC, Liston RM, Lee SK. Outcomes of planned home birth with registered midwife versus planned hospital birth with midwife or physician. CMAJ. 2009;181:377-83.
8. Johnson KC, Daviss BA. Outcomes of planned home births with certified professional midwives: large prospective study in North America. BMJ. 2005;330:1416.
9. Wax JR, Lucas FL, Lamont M, Pinette MG, Cartin A, Blackstone J. Maternal and newborn outcomes in planned home birth vs planned hospital births: a metaanalysis. Am J Obstet Gynaecol. 2010;203:243 e1-8.
10. Wax JR, Pinette MG, Cartin A, Blackstone J. Maternal and newborn morbidity by birth facil-ity among selected United States 2006 low-risk births. Am J Obstet Gynaecol. 2010;202:152 e1-5.
11. Wiegers TA, Keirse MJ, van der Zee J, Berghs GA. Outcome of planned home and planned hospital births in low risk pregnancies: prospective study in midwifery practices in The Netherlands. BMJ. 1996;313:1309-13.
12. Anderson RE, Murphy PA. Outcomes of 11,788 planned home births attended by certified nurse-midwives. A retrospective descriptive study. J Nurse Midwifery. 1995;40:483-92.
13. Bastian H, Keirse MJ, Lancaster PA. Perinatal death associated with planned home birth in Australia: population based study. BMJ. 1998;317:384-8.
14. Chamberlain G, Wraight A, Crowley P. Birth at home. Pract Midwife. 1999;2:35-9.
15. De Jonge A, van der Goes BY, Ravelli AC, et al. Perinatal mortality and morbidity in a nationwide cohort of 529,688 low-risk planned home and hospital births. BJOG. 2009;116:1177-84.
16. Evers AC, Brouwers HA, Hukkelhoven CW, et al. Perinatal mortality and severe morbidity in low and high risk term pregnancies in the Netherlands: prospective cohort study. BMJ. 2010;341:c5639.
17. Lindgren HE, Radestad IJ, Christensson K, Hild-ingsson IM. Outcome of planned home births compared to hospital births in Sweden between 1992 and 2004. A population-based register study. Acta Obstet Gynaecol Scand. 2008;87:751-9.
18. Pang JW, Heffelfinger JD, Huang GJ, Benedetti TJ, Weiss NS. Outcomes of planned home births in Washington State: 1989-1996. Obstet Gynaecol. 2002;100:253-9.
19. Hildingsson IM, Lindgren HE, Haglund B, Radestad IJ. Characteristics of women giving birth at home in Sweden: a national register study. Am J Obstet Gynaecol. 2006;195:1366-72.
20. Hogberg U. Homebirths in a modern setting - a cautionary tale. Acta Obstet Gynaecol Scand. 2008;87:797-9.
21. Neuhaus W, Piroth C, Kiencke P, Gohring UJ, Mall-man P. A psychosocial analysis of women plan-ning birth outside hospital. J Obstet Gynaecol. 2002;22:143-9.

148
PLAN
NED
HO
ME CO
MPA
RED W
ITH PLA
NN
ED H
OSPITA
L BIRTHS
8
22. Perinatal care in The Netherlands 2006 (in Dutch: Perinatale zorg in Nederland 2006). Utrecht: The Netherlands Perinatal Registry; 2008.
23. Bonsel GJ, Birnie E, Denktas S, Poeran J, Steegers EAP. Dutch report: Lijnen in de Perinatale Sterfte, Signalementstudie Zwangerschap en Geboorte 2010. Rotterdam: Erasmus MC; 2010. (online: http://www.nvk.nl/Nieuws/Dossiers/DossierPerinatalezorg.aspx).
24. Hendrix M, Van Horck M, Moreta D, et al. Why women do not accept randomisation for place of birth: feasibility of a RCT in The Netherlands. BJOG. 2009;116:537-42; discussion 42-4.
25. Tyson H. Outcomes of 1001 midwife-attended home births in Toronto, 1983-1988. Birth. 1991;18: 14-9.
26. Dowswell T, Thornton JG, Hewison J, et al. Should there be a trial of home versus hospital delivery in the United Kingdom? BMJ. 1996;312:753-7.
27. Cammu H, Martens G, Landuyt J, De Coen K, Defoort P. Perinatale activiteiten in Vlaanderen 2009. Brussel: Studiecentrum voor Perinatale Epidemiologie; 2010.
28. Bijlenga D, Birnie E, Bonsel GJ. Feasibility, Reliability, and Validity of Three Health-State Valuation Methods Using Multiple-Outcome Vignettes on Moderate-Risk Pregnancy at Term. Value Health. 2009;12:821-7.
29. Woodcock HC, Read AW, Bower C, Stanley FJ, Moore DJ. A matched cohort study of planned home and hospital births in Western Australia 1981-1987. Midwifery. 1994;10:125-35.
30. Kennare RM, Keirse MJ, Tucker GR, Chan AC. Planned home and hospital births in South Australia, 1991-2006: differences in outcomes. Med J Aust. 2010;192:76-80.
31. Gulbransen G, Hilton J, McKay L, Cox A. Home birth in New Zealand 1973-93: incidence and mortality. N Z Med J. 1997;110:87-9.
32. Davies J, Hey E, Reid W, Young G. Prospective regional study of planned home births. Home Birth Study Steering Group. BMJ. 1996;313:1302-6.
33. Gyte GM, Dodwell MJ, Macfarlane AJ. Home birth metaanalysis: does it meet AJOG’s reporting re-quirements? Am J Obstet Gynaecol. 2011;204:e15; author reply e8-20, discussion.
34. Johnson KC, Daviss BA. International data demon-strate home birth safety. Am J Obstet Gynaecol. 2011;204:e16-7; author reply e8-20, discussion.
35. Kirby RS, Frost J. Maternal and newborn outcomes in planned home birth vs planned hospital births: a metaanalysis. Am J Obstet Gynaecol. 2011;204:e16; author reply e8-20, discussion.
36. Sandall J, Bewley S, Newburn M. “Home birth triples the neonatal death rate”: public commu-nication of bad science? Am J Obstet Gynaecol. 2011;204:e17-8; author reply e8-20, discussion.

9
Manuscript submitted for publication.
Does centralisation of acute obstetric care reduce perinatal
mortality? An empirical study of over 1 million births in
The Netherlands
J. Poeran, G.J.J.M. Borsboom, J.P. de Graaf, E. Birnie, E.A.P.Steegers, J.P. Mackenbach, G.J. Bonsel

150
CENTRA
LISATION
OF ACU
TE OBSTETRIC CA
RE IN TH
E NETH
ERLAN
DS
9
ABSTRACTObjective Estimating outcome of hypothetical closure of 10 small hospitals (out of 99)
and centralisation of acute obstetric care in larger hospitals in order to assess whether this
would lower perinatal mortality in The Netherlands.
Design Hypothetical analysis using retrospective cohort data.
Setting The Netherlands
Population Selected were all (n=1,160,708) singleton hospital births from ≥22 weeks’
gestation as recorded in The Netherlands Perinatal Registry 2000-2008 with exclusion of (1)
unknown gestational age, (2) unknown or no travel time to hospital and (3) fetal mortality.
Main outcome measures Predicted perinatal (intrapartum and first-week) mortality for
several patient subgroups for two simulated centralisation scenarios: (1) closure of the
10 smallest hospitals, and (2) closure of the 10 smallest hospitals, but avoiding adjacent
closures. Women who delivered in hypothetically closed hospitals were assigned the next-
nearest hospital with travel time and hospital features changed accordingly. Predictions
followed from regression coefficients from a multilevel logistic regression model with a
forced casemix control (maternal and child factors) and a set of hospital organisational
features with perinatal mortality as outcome.
Results Scenario 1 resulted in doubled travel time, and 10% increased mortality (0.34% vs.
0.38%). In scenario 2 perinatal mortality showed little change (0.33% vs. 0.32%) with less
effect on travel time. Heterogeneity in hospital organisational features caused simultaneous
improvement and deterioration of predicted perinatal mortality depending mainly on the
features of the newly assigned next-nearest hospital. Consequences vary for subgroups:
pregnant women at increased risk suffer more from increased travelling, and gain more if
a (specialised) ‘perinatal centre’ or a better performing hospital is nearby.
Conclusion In The Netherlands, centralisation of acute obstetric care according to the
‘closure-of-the-smallest-rule’ yields suboptimal outcomes. In order to develop an optimal
strategy for centralisation one would need to consider all positive and negative effects:
heterogeneity in organisational features of closed and surviving hospitals, financial aspects,
differential effects for patient subgroups, increased travel time and adequate antenatal
risk selection.

151
CENTRA
LISATION
OF ACU
TE OBSTETRIC CA
RE IN TH
E NETH
ERLAN
DS
9
INTRODUCTIONDutch perinatal mortality exceeds the European average.1,2 Structural inadequacies in the
provision of care were discovered as major contributors.3 In response, a national Steering
Group on Pregnancy and Birth -on behalf of the Dutch Ministry of Health-, issued several
recommendations.4 One recommendation addressed the observed inadequate availability
of 7*24h acute obstetric care stating availability within 15 minutes of ‘qualified professionals’
(midwives, gynaecologists, paediatricians, anaesthesiologists, and operating theatre staff;
‘qualified’ in terms of seniority).4,5 However, small hospitals reported to be unable to satisfy
these demands with existing on-call coverage schemes. Moreover, larger hospitals were
unwilling to do so as the current financial system explicitly excludes any reimburse ment of
so-called ‘availability (standby) costs’. Consequently, centralisation of acute obstetric care
services was considered, implying a reduction of acute services in about half of all hospitals
with a parallel redistri bution of qualified professionals from small local to nearby larger
hospitals. While the advantages are obvious (e.g., increase in continuity of care, and a likely
volume related performance improvement), the disadvantages of centralisation should
be acknowledged too (e.g., increased travel time and organisational disutilities regarding
non-obstetric services).4-9 Centralisation may also critically affect paediatric, emergency
room, and acute anaesthesia services in the reduced hospitals.8
The key question is whether direct effects of centralisation on patient outcomes are to be
expected. An overall positive outcome would more easily justify the above disutilities. In
this study we estimated the direct effects on intrapartum and first-week mortality when
10 small hospitals (out of 99 providing obstetric care) would hypothetically be closed
according to two plausible centralisation scenarios. The effects of closing were estimated by
a redistribution of patient flow (depending on their zip code of residency) to the next-nearest
hospital, taking into account (1) detailed information of maternal and child characteristics,
(2) acute referral status, (3) travel time in normal and (in retrospect) high risk cases, and
hospital related factors such as (4) day and time of birth, (5) the hospital’s organisational
7*24h characteristics, and (6) any additional non-specific hospital effects not accounted
for by the previously mentioned factors. The net consequences were then calculated for all
individual women redistributed from the hypothetically closed hospitals to the remaining
hospitals, to allow for a trade-off of positive and negative effects.

152
CENTRA
LISATION
OF ACU
TE OBSTETRIC CA
RE IN TH
E NETH
ERLAN
DS
9
METHODS
General approach
This study was issued by the so-called society of SAZ-hospitals, which represents the
interests of about 40 small general hospitals in The Netherlands. These hospitals are
located throughout The Netherlands, either within the ‘Randstad’ conurbation (the densely
populated western part of the Netherlands) or outside. Centralisation of care primarily will
affect SAZ hospitals.
Our general approach was as follows. In step 1, we estimated the impact of maternal,
child, and hospital’s organisational characteristics in terms of intrapartum and first-week
(perinatal) mortality, using multilevel logistic regression analysis. Next, in step 2, we
identified all pregnant women who would need to change hospital as the consequence of
a defined centralisation scenario. We distinguished two centralisation scenarios: closure of
the 10 smallest hospitals (scenario 1) and closure of the 10 smallest hospitals, while avoiding
simultaneous closure of two adjacent hospitals (scenario 2). The women involved were
assumed to deliver in the next-nearest hospital in terms of estimated travel time. In step
3, we estimated the individual intrapartum and first-week mortality risk after closure. We
did so by applying to each individual woman the regression coefficients (obtained in step
1) to the characteristics of her situation after centralisation. Finally, in step 4, we compared
the current observed total mortality among women affected by closure, with the expected
total mortality by adding the estimated probabilities.
Data collection
Data on maternal factors, child factors and outcomes were obtained from The Netherlands
Perinatal Registry. This registry contains population-based information of 97% of all
pregnancies in the Netherlands.10 On behalf of the respective professional societies,
source data are routinely collected by 94% of midwives, 99% of gynaecologists and 68%
of paediatricians including 100% of Neonatal Intensive Care Unit (NICU) paediatricians
(see website for detailed description: www.perinatreg.nl).10 The professional board of The
Netherlands Perinatal Registry granted permission to use the anonymous registry data for
this study. The registry contains 1,620,126 records for the period 2000-2008. We excluded
multiple pregnancies (n=35,326), births with unknown gestational age (n=17,278), births with
an unknown or erroneous zip code (n=23,736), births in hospitals which had not participated
in the registry >2 years (n=6,535), homebirths (n=368,672), and stillbirths (n=7,871).

153
CENTRA
LISATION
OF ACU
TE OBSTETRIC CA
RE IN TH
E NETH
ERLAN
DS
9
We excluded homebirths since centralisation of care, travel distance, and hospital’s
organisational features are of little or no importance in homebirths. Stillbirths were excluded
as delivery decisions are subject to different considerations.11
Analysed were 1,160,708 births which additionally were combined with data from two
sources: travel time data and individual hospital’s organisational characteristics. Travel
times to the closed and next-nearest hospitals were calculated making use of the hospital’s
zip code and pregnant women’s zip code (these 4-digit zip codes cover on average
4,000 inhabitants). Travel times (not: distances) between zip codes were derived from a
commercially available geographic information system (www.geodan.nl). We distinguished
planned from unplanned births as we assume travel time to hospital only to have an impact
on women with unplanned births who were transferred from home to hospital during
parturition. Thus, hospital travel time was set to zero for women with planned births, i.e.,
induction of labour or a planned (primary) caesarean section.
Data on hospital’s organisational characteristics including data pertinent to 7*24 hour
services were collected separately from this study, with the support of the Dutch Society of
Obstetricians and Gynaecologists using a standard questionnaire for all 99 Dutch maternity
units (response: 100%).3
Table 9.1 displays these collected 24 variables with inevitable overlap of data. We used
principal component analysis (PCA) to summarise the original 24 variables into two principal
components, factor 1 and factor 2, with a computed numerical score for each hospital.
Factor 1 can be interpreted as ‘hospital’s scale size’ as it primarily combines original variables
pointing to hospital size and the number of obstetric caregivers: the lower the factor value
the larger the hospital and the higher the number of obstetric caregivers. Factor 2 can be
interpreted as ‘24-hour equality of service level’. This factor combines original variables
pointing to around-the-clock availability of the various qualified professionals: the higher
the factor value the more the 24-hour equality of service level (in terms of seniority). These
two factors jointly explained almost 70% of variance of the original 24 variables, i.e., the
two constructed variables contain 70% of the available information.
PCA is a ‘data reduction’ technique commonly used in datasets with a high number of related
explanatory variables. It essentially summarises the net information content of overlapping
data into a small number of independent constructed variables. The background and the
technique itself are described in more depth elsewhere.12

154
CENTRA
LISATION
OF ACU
TE OBSTETRIC CA
RE IN TH
E NETH
ERLAN
DS
9
Ta
ble
9.1
O
verv
iew
of h
ospi
tals
’ org
anis
atio
nal d
ata
Org
anis
atio
nal f
eatu
reRe
mar
ks
Gen
eral
Teac
hing
hos
pita
lca
tego
rised
into
yes
/ no
Gyn
aeco
logy
dep
artm
ent
Dur
atio
n of
day
time
shift
sca
tego
rised
into
dur
atio
ns o
f 10-
12 h
ours
and
7-9
hou
rsD
urat
ion
of e
veni
ng /
nigh
t shi
fts
and
the
high
est l
evel
of t
he
prof
essi
onal
who
is a
tten
ding
thes
e sh
ifts
cate
goris
ed in
to d
urat
ions
of ≤
14 h
ours
and
≥15
hou
rs w
ith p
rofe
ssio
nal l
evel
s ca
tego
rised
in
to tw
o gr
oups
: (1)
gyn
aeco
logi
st /
gyna
ecol
ogis
t in
trai
ning
and
(2) n
on-in
-tra
inin
g ph
ysic
ian
/ mid
wife
/ nu
rse
The
high
est l
evel
of t
he p
rofe
ssio
nal w
ho is
att
endi
ng th
e ev
enin
g an
d ni
ght s
hift
s du
ring
the
wee
kca
tego
rised
into
fi ve
gro
ups:
(1) g
ynae
colo
gist
, (2)
in-t
rain
ing
and
non-
in-t
rain
ing
resi
dent
gy
naec
olog
y, (3
) gen
eral
em
erge
ncy
phys
icia
n, (4
) mid
wife
and
(5) n
urse
The
high
est l
evel
of t
he p
rofe
ssio
nal w
ho is
att
endi
ng th
e da
ytim
e sh
ifts
durin
g w
eeke
nds
cate
goris
ed in
to fi
ve g
roup
s: (1
) gyn
aeco
logi
st, (
2) in
-tra
inin
g an
d no
n-in
-tra
inin
g re
side
nt
gyna
ecol
ogy,
(3) g
ener
al e
mer
genc
y ph
ysic
ian,
(4) m
idw
ife a
nd (5
) nur
seTh
e hi
ghes
t lev
el o
f the
pro
fess
iona
l who
is a
tten
ding
the
even
ing
and
nigh
t shi
fts
durin
g w
eeke
nds
cate
goris
ed in
to fi
ve g
roup
s: (1
) gyn
aeco
logi
st, (
2) in
-tra
inin
g an
d no
n-in
-tra
inin
g re
side
nt
gyna
ecol
ogy,
(3) g
ener
al e
mer
genc
y ph
ysic
ian,
(4) m
idw
ife a
nd (5
) nur
sePe
rmitt
ed to
sle
ep d
urin
g at
tend
ing
shift
sca
tego
rised
into
yes
/ no
Gyn
aeco
logi
st o
n ba
ckup
cal
l dur
ing
shift
sca
tego
rised
into
yes
/ no
Prof
essi
onal
doi
ng ro
unds
dur
ing
wee
kend
sca
tego
rised
into
four
gro
ups:
(1) g
ynae
colo
gist
, (2)
in-t
rain
ing
and
non-
in-t
rain
ing
resi
dent
gy
naec
olog
y, (3
) gen
eral
em
erge
ncy
phys
icia
n, (4
) mid
wife
and
(5) n
urse
In-h
ospi
tal p
rese
nce
of th
e em
erge
ncy
oper
atin
g th
eatr
e te
amca
tego
rised
into
thre
e gr
oups
: in-
hosp
ital p
rese
nce
durin
g (1
) 24
hour
s, (2
) pre
senc
e du
ring
dayt
ime
and
even
ing
and
on-c
all d
urin
g th
e ni
ght,
(3) p
rese
nce
durin
g da
ytim
e an
d on
-cal
l du
ring
the
even
ing
and
nigh
t In
-hos
pita
l pre
senc
e of
an
anae
sthe
siol
ogis
tca
tego
rised
into
thre
e gr
oups
: in-
hosp
ital p
rese
nce
durin
g (1
) 24
hour
s, (2
) pre
senc
e du
ring
dayt
ime
and
even
ing
and
on-c
all d
urin
g th
e ni
ght,
(3) p
rese
nce
durin
g da
ytim
e an
d on
-cal
l du
ring
the
even
ing
and
nigh
t Th
e to
tal n
umbe
r of o
bste
tric
car
egiv
ers
(spe
cial
ists
, ph
ysic
ians
, mid
wiv
es, n
urse
s)a
cont
inuo
us n
umbe
r
Ann
ual n
umbe
r of d
eliv
erie
sco
ntin
uous
as
wel
l as
grou
ped
into
thre
e ca
tego
ries:
(1) <
1000
, (2)
100
0-20
00, (
3) >
2000

155
CENTRA
LISATION
OF ACU
TE OBSTETRIC CA
RE IN TH
E NETH
ERLAN
DS
9
Com
bina
tion
of th
e an
nual
num
ber o
f del
iver
ies
with
the
gyna
ecol
ogis
t:oth
er o
bste
tric
car
egiv
er ra
tioca
tego
rised
into
six
gro
ups:
(1) <
1000
and
≤1:
4, (2
) <10
00 a
nd 1
:4-1
:6, (
3) <
1000
and
>1:
6, (4
) 10
00-2
000
and
≤1:4
, (5)
100
0-20
00 >
1:4,
(6) >
2000
and
all
ratio
s
Min
imum
dur
atio
n of
att
endi
ng s
hift
dur
ing
wee
kend
sa
cont
inuo
us n
umbe
r (ra
nge
12-7
2 ho
urs)
Aver
age
trav
el ti
me
in m
inut
es fr
om h
ome
to h
ospi
tal f
or a
n on
-cal
l gyn
aeco
logi
sta
cont
inuo
us n
umbe
r
Max
imum
trav
el ti
me
in m
inut
es fr
om h
ome
to h
ospi
tal f
or a
n on
-cal
l gyn
aeco
logi
sta
cont
inuo
us n
umbe
r
Num
ber o
f car
egiv
ers
pres
ent d
urin
g at
tend
ing
shift
s on
w
eekd
ay e
veni
ngs
and
nigh
tsa
cont
inuo
us n
umbe
r
Num
ber o
f car
egiv
ers
pres
ent d
urin
g at
tend
ing
shift
s on
w
eeke
nds
durin
g th
e da
ya
cont
inuo
us n
umbe
r
Num
ber o
f car
egiv
ers
pres
ent d
urin
g at
tend
ing
shift
s on
w
eeke
nds
durin
g th
e ev
enin
g an
d th
e ni
ght
a co
ntin
uous
num
ber
Paed
iatr
ics
depa
rtm
ent
Leve
l of c
are
for n
ewbo
rns
cate
goris
ed in
to fo
ur g
roup
s: (1
) Neo
nata
l Int
ensi
ve C
are
Uni
t (N
ICU
), (2
) pos
t-N
ICU
or
incu
bato
r fro
m 3
0 w
eeks
of g
esta
tiona
l age
, (3)
incu
bato
r fro
m 3
2 w
eeks
of g
esta
tiona
l age
, (4
) ini
tially
fi rs
t aid
for n
eona
te w
ith s
ubop
timal
sta
rt w
ith s
ubse
quen
t ref
erra
l to
a ho
spita
l w
ith a
hig
her l
evel
of c
are
The
high
est l
evel
of t
he p
rofe
ssio
nal a
t the
pae
diat
rics
depa
rtm
ent w
ho is
att
endi
ng th
e sh
ifts
outs
ide
offi c
e ho
urs
cate
goris
ed in
to s
ix g
roup
s: (1
) fel
low
neo
nato
logi
st, (
2) p
aedi
atric
ian,
(3) i
n-tr
aini
ng
paed
iatr
icia
n, (4
) non
-in-t
rain
ing
resi
dent
pae
diat
rics,
(5) g
ener
al e
mer
genc
y ph
ysic
ian,
(6) n
o pr
ofes
sion
al p
rese
nt b
ut o
n-ca
ll Th
e lo
wes
t lev
el o
f the
pro
fess
iona
l at t
he p
aedi
atric
s de
part
men
t who
is a
tten
ding
the
shift
s ou
tsid
e offi
ce
hour
sca
tego
rised
into
six
gro
ups:
(1) f
ello
w n
eona
tolo
gist
, (2)
pae
diat
ricia
n, (3
) in-
trai
ning
pa
edia
tric
ian,
(4) n
on-in
-tra
inin
g re
side
nt p
aedi
atric
s, (5
) gen
eral
em
erge
ncy
phys
icia
n, (6
) no
prof
essi
onal
pre
sent
but
on-
call
Prof
essi
onal
on-
call
at th
e pa
edia
tric
s de
part
men
t ca
tego
rised
into
four
gro
ups:
(1) n
o on
e on
-cal
l, (2
) pae
diat
ricia
n on
-cal
l, (3
) fel
low
ne
onat
olog
ist o
n-ca
ll, (4
) oth
er p
rofe
ssio
nal o
n-ca
ll

156
CENTRA
LISATION
OF ACU
TE OBSTETRIC CA
RE IN TH
E NETH
ERLAN
DS
9
Outcome and determinants of hospital performance
The main outcome was intrapartum or first-week mortality after live birth, for convenience
further referred to as perinatal mortality. Determinants with their optimal categorisation
were selected for their proven effect on perinatal mortality.3,7,13-17 We distinguished maternal
and child factors (casemix) and organisational factors. Maternal factors were parity and
age category combined (primiparous / multiparous, <25 / 25-29 / 30-34 / 35-39 / ≥40
years), and ethnicity (Western / non-Western). Child factors were gestational age (thirteen
categories3), congenital anomalies (yes / no), small for gestational age (SGA: birthweight
>10th / 2.3-10th / <2.3rd percentile) and fetal presentation (cephalic / breech / transverse
or other / unknown). Congenital anomalies are recorded postpartum and classified through
a standard coding system by organ system (8 categories, 71 subcategories).18
Organisational factors were travel time to the hospital in minutes (continuous), the two
principal components (factor 1 and factor 2), day and time of delivery (Saturday / Sunday /
weekday, each subdivided into three time slots 00:00-07:59 / 08:00-17:59 / 18:00-00:00), and
emergency referral during parturition (yes / no). We assumed the hospitals’ performance
according to principal component factor 1 and 2 did not to change after the hypothetical
closure of the 10 small hospitals. Emergency referral during parturition was defined by
using information from both the caregiver during pregnancy (midwife, obstetrician) and
the caregiver responsible at start of labour (midwife or obstetrician).
Analysis
For presentational purposes only, we grouped hospitals into small size SAZ hospitals (1)
within and (2) outside the Randstad conurbation, (3) academic hospitals and (4) other
general hospitals.
The different steps in the analysis are illustrated in figure 9.1. First, a comprehensive
multilevel multivariable logistic regression model (‘hospital performance model’) was
fitted using the primary dataset (step 1). All determinants mentioned above were entered
into the model. The principal component factors were included in the model as both their
actual value as well as their quadratic value as we presumed linear effects as well as effects
of extremes (e.g., the largest hospitals’ performance to be comparable to the smallest
hospitals in which quality in the former is ensured by the total staffing levels [‘quantity’]
and in the latter by the level of obstetric staff [mostly gynaecologists, not residents on
duty, ‘quality’])

157
CENTRA
LISATION
OF ACU
TE OBSTETRIC CA
RE IN TH
E NETH
ERLAN
DS
9
We predefined an additional interaction term relating travel time to clinical condition of
the child, as previous studies have suggested a poorer condition to be associated with a
larger adverse impact of extended travel time.19 Clinical condition was represented by the
single or combined presence of so-called ‘Big4’20 morbidities: congenital anomalies, preterm
birth (<37th week of gestation), SGA (birthweight <10th percentile for gestational age) or
low Apgar score (<7, 5 minutes after birth). As the presence of any of the ‘Big4’ morbidities
precedes perinatal mortality in 85% of cases, we assume this to be an appropriate risk
indicator.20 Because of the multilevel structure of the data (individuals are grouped per
hospital) we used multilevel logistic regression analysis which adjusts for the possible
clustering of individuals within hospitals, and unspecified effects at the hospital level. In
step 2 women who delivered in the hypothetically closed hospitals were assigned the
next-nearest hospital. Finally, the estimated coefficients obtained from step 1 were used to
predict perinatal mortality for each scenario (step 3) taking into account (1) the features of
the new hospital, (2) the associated travel distance and (3) the specific interaction term of
‘Big4’*travel time for those referred. The overall observed and predicted mortality before
vs. after the closure of the hospitals were then compared. Predicted mortality was the sum
of all individually recalculated mortality probabilities for women affected by centralisation.
Figure 9.1 Overview of computational model.
PRIMARY DATASET DUPLICATE DATASETS
DATASET 1 / SCENARIO 1‘Closure of 10 smallest hospitals’
-women in closed hospitals assigned the next nearest hospital with corresponding travel time and hospital features
FITTING OF HOSPITAL PERFORMANCE MODEL
PREDICTING PERINATAL MORTALITYwith coefficients from hospital performance model
DATASET 2 / SCENARIO 2‘Closure of 10 smallest hospitals, avoiding adjacent closures’
-women in closed hospitals assigned the next nearest hospital with corresponding travel time and hospital features

158
CENTRA
LISATION
OF ACU
TE OBSTETRIC CA
RE IN TH
E NETH
ERLAN
DS
9
Presentation was for all women together, and for several subgroups based on planned
or unplanned birth, referral during parturition, deliveries within ‘office hours’, parity, and
presence of morbidities. The statistical software package SAS version 9.2 (SAS Institute Inc.,
Cary, NC) was used, with the GLIMMIX procedure to run random intercept multilevel models.
RESULTSTable 9.2 shows the study population characteristics by type of hospital. Most women are
multiparous and 30-34 years (20.2-22.8%), and of Western origin (79.0-90.4%). Preterm birth
(<37 weeks’ gestation) was observed in 0.6-3.8%, congenital anomalies in 1.8-5.0%, SGA
in 9.4-11.3%, and a non-cephalic presentation in 7.2-9.2%. Of all women 2.1-12.9% had to
travel more than 20 minutes to the hospital where they gave birth. SAZ hospitals all fell
in the ≥ P25 value range of factor 1 (‘hospital scale size, number of obstetric caregivers’,
a lower value represents larger hospitals) while academic hospitals all fell in the <P25
value range. This confirms the SAZ hospitals to be relatively small with smaller numbers of
obstetric caregivers compared to the larger academic hospitals. Factor 2 (‘24-hour equality
of service level’ a higher factor value represents more 24-hour equality of service level in
terms of seniority) was distributed more evenly across type of hospital. The majority of
women delivered in hospitals in the ≥ P25 value range illustrating most women to deliver
in hospitals with the highest level of 24-hour equality of service. Most deliveries were on a
weekday between 08:00 and 17:59 (37.9-43.9%); 22.2-29.9% of women were referred during
parturition. ‘Big4’ risk prevalence did not differ much between SAZ hospitals (17.3-19.2%)
and other non-academic hospitals (19.0%). For academic hospitals prevalence is 27.3%.
Hospital performance
Effect estimates from the multilevel multivariable logistic regression model (‘hospital
performance model’) are shown in table 9.3. All casemix variables are significantly associated
with perinatal mortality. The highest risks are seen for multiparous women of 35-39 years
(OR 1.51 CI 1.30-1.75), non-Western women (OR 1.15 CI 1.04-1.28), gestational ages <37 (OR
range 2.97->1000), congenital anomalies (OR 10.11 CI 9.14-11.19), birthweight <p2.3 (OR
6.46 CI 5.67-7.35), and transverse or other fetal presentation (OR 2.06 CI 1.60-2.65).
For organisational factors only principal component factor 1, 2 and quadratic factor 2 are
not significantly associated with perinatal mortality. Travel time (in minutes) to hospital has
an OR of 0.98, implying a 2% decreased risk of perinatal mortality for every extra minute of

159
CENTRA
LISATION
OF ACU
TE OBSTETRIC CA
RE IN TH
E NETH
ERLAN
DS
9
Ta
ble
9.2
Ch
arac
teris
tics
of th
e st
udy
popu
latio
n pe
r hos
pita
l gro
up
SAZ
hosp
itals
with
inRa
ndst
adco
nurb
atio
n
SAZ
hosp
itals
outs
ide
Rand
stad
conu
rbat
ion
Acad
emic
hos
pita
lsO
ther
hos
pita
ls
N%
N%
N%
N%
Ca
sem
ix v
ari
ab
les
Parit
y &
age
cat
egor
yPr
imip
arou
s &
<25
yea
rs9,
600
9.2%
22,7
379.
6%13
,654
9.0%
67,3
2410
.1%
Prim
ipar
ous
& 2
5-29
yea
rs18
,477
17.7
%47
,239
19.9
%23
,546
15.5
%11
8,19
717
,7%
Prim
ipar
ous
& 3
0-34
yea
rs19
,113
18.3
%37
,042
15.6
%25
,826
17.0
%11
6,58
917
.5%
Prim
ipar
ous
& ≥
35 y
ears
7,46
27.
1%10
,945
4.6%
11,7
557.
7%42
,888
6.4%
Mul
tipar
ous
& <
25 y
ears
2,58
22.
5%6,
805
2.9%
4,81
43.
2%21
,252
3.2%
Mul
tipar
ous
& 2
5-29
yea
rs10
,270
9.8%
29,1
4812
.3%
15,8
2910
.4%
71,6
3610
.7%
Mul
tipar
ous
& 3
0-34
yea
rs21
,067
20.2
%54
,102
22.8
%31
,184
20.5
%13
5,85
020
.4%
Mul
tipar
ous
& 3
5-39
yea
rs13
,551
13.0
%25
,978
10.9
%21
,153
13.9
%79
,350
11.9
%M
ultip
arou
s &
≥40
yea
rs2,
369
2.3%
3,63
11.
5%4,
232
2.8%
13,5
112.
0%
Ethn
icity
Wes
tern
83,8
6580
.3%
214,
887
90.4
%12
0,03
679
.0%
529,
076
79.4
%N
on-W
este
rn20
,626
19.7
%22
,740
9.6%
31,9
5721
.0%
137,
521
20.6
%
Ges
tatio
nal a
ge22
-27.
6 w
eeks
127
0.1%
348
0.1%
3,19
02.
1%1,
317
0.2%
28-3
1.6
wee
ks11
90.
1%39
30.
2%6,
605
4.3%
1,42
10.
2%32
wee
ks24
80.
2%71
30.
3%1,
296
0.9%
2,05
10.
3%33
wee
ks53
90.
5%1,
361
0.6%
1,28
00.
8%3,
653
0.5%
34 w
eeks
944
0.9%
2,36
31.
0%1,
804
1.2%
6,23
80.
9%
Tabl
e 9.
1 co
ntin
ues o
n ne
xt p
age.

160
CENTRA
LISATION
OF ACU
TE OBSTETRIC CA
RE IN TH
E NETH
ERLAN
DS
9
Ta
ble
9.2
Co
ntin
ued
SAZ
hosp
itals
with
inRa
ndst
adco
nurb
atio
n
SAZ
hosp
itals
outs
ide
Rand
stad
conu
rbat
ion
Acad
emic
hos
pita
lsO
ther
hos
pita
ls
N%
N%
N%
N%
35 w
eeks
1,55
61.
5%3,
967
1.7%
2,51
71.
7%10
,363
1.6%
36 w
eeks
2,94
92.
8%7,
255
3.1%
4,64
13.
1%19
,611
2.9%
37 w
eeks
6,77
16.
5%15
,563
6.5%
9,48
76.
2%39
,044
5.9%
38 w
eeks
16,3
4215
.6%
38,8
1416
.3%
21,7
8414
.3%
97,3
5714
.6%
39 w
eeks
23,1
5722
.2%
52,2
6222
.0%
30,9
1720
.3%
147,
476
22.1
%40
wee
ks27
,052
25.9
%58
,970
24.8
%35
,281
23.2
%17
0,67
225
.6%
41 w
eeks
18,5
8217
.8%
41,3
7017
.4%
24,1
7115
.9%
119,
727
18.0
%≥
42 w
eeks
6,10
55.
8%14
,248
6.0%
9,02
05.
9%47
,667
7.2%
Cong
enita
l ano
mal
ies
No
102,
648
98.2
%22
9,99
796
.8%
144,
320
95.0
%65
1,15
097
.7%
Yes
1,84
31.
8%7,
630
3.2%
7,67
35.
0%15
,447
2.3%
Smal
l for
ges
tatio
nal a
ge (S
GA
)N
o SG
A94
,585
90.5
%21
4,31
290
.2%
134,
787
88.7
%59
6,67
189
.5%
Birt
hwei
ght P
2.3-
P10
7,66
37.
3%17
,706
7.5%
12,9
368.
5%53
,289
8.0%
Birt
hwei
ght <
P2.
32,
243
2.1%
5,60
92.
4%4,
270
2.8%
16,6
372.
5%
Feta
l pre
sent
atio
nCe
phal
ic97
,009
92.8
%21
8,01
091
.7%
137,
933
90.7
%61
8,14
892
.7%
Bree
ch5,
873
5.6%
15,3
606.
5%10
,822
7.1%
40,0
996.
0%Tr
ansv
erse
or o
ther
720
0.7%
1,83
90.
8%1,
510
1.0%
5,03
30.
8%U
nkno
wn
889
0.9%
2,41
81.
0%1,
728
1.1%
3,31
70.
5%

161
CENTRA
LISATION
OF ACU
TE OBSTETRIC CA
RE IN TH
E NETH
ERLAN
DS
9
Org
an
isa
tio
na
l fa
cto
rs
Trav
el ti
me
to h
ospi
tal
≤ 20
min
utes
102,
320
97.9
%21
7,04
891
.3%
132,
426
87.1
%62
7,18
694
.1%
> 20
min
utes
2,17
12.
1%20
,579
8.7%
19,5
6712
.9%
39,4
115.
9%
Hos
pita
l org
anis
atio
nal f
eatu
res
Prin
cipa
l com
pone
nt (f
acto
r 1)
≥ P2
510
4,49
110
0.0%
237,
627
100.
0%0
0.0%
539,
523
80.9
%<
P25
00.
0%0
0.0%
151,
993
100.
0%12
7,07
419
.1%
Prin
cipa
l com
pone
nt (f
acto
r 2)
≥ P2
587
,162
83.4
%23
7,62
710
0.0%
151,
993
100.
0%40
0,36
860
.1%
< P2
517
,329
16.6
%0
0.0%
00.
0%26
6,22
939
.9%
Day
and
tim
e of
del
iver
ySa
turd
ay 0
0:00
-07:
593,
432
3.3%
7,70
43.
2%5,
985
3.9%
24,1
953.
6%Sa
turd
ay 0
8:00
-17:
595,
485
5.2%
13,1
775.
5%8,
248
5.4%
37,1
695.
6%Sa
turd
ay 1
8:00
-23:
592,
846
2.7%
6,45
82.
7%4,
397
2.9%
19,3
582.
9%Su
nday
00:
00-0
7:59
3,38
63.
2%7,
814
3.3%
5,97
73.
9%24
,464
3.7%
Sund
ay 0
8:00
-17:
595,
736
5.5%
12,8
465.
4%8,
259
5.4%
37,1
185.
6%Su
nday
18:
00-2
3:59
2,76
82.
6%6,
209
2.6%
4,44
72.
9%19
,329
2.9%
Wee
kday
s 00
:00-
07:5
917
,600
16.8
%39
,607
16.7
%30
,296
19.9
%12
5,36
318
.8%
Wee
kday
s 08
:00-
17:5
945
,837
43.9
%10
3,15
243
.4%
57,5
4437
.9%
266,
601
40.0
%W
eekd
ays
18:0
0-23
:59
17,4
0116
.7%
40,6
6017
.1%
26,8
4017
.7%
113,
000
17.0
%
Refe
rral
dur
ing
part
uriti
onN
o76
,046
72.8
%17
1,32
572
.1%
118,
186
77.8
%46
7,60
270
.1%
Yes
28,4
4527
.2%
66,3
0227
.9%
33,8
0722
.2%
198,
995
29.9
%
Big4
Cat
egor
yN
o Bi
g486
,454
82.7
%19
2,10
380
.8%
110,
463
72.7
%53
9,70
881
.0%
Onl
y on
e Bi
g416
,724
16.0
%41
,741
17.6
%33
,636
22.1
%11
6,16
017
.4%
Mor
e th
an o
ne B
ig4
1,31
31.
3%3,
783
1.6%
7,89
45.
2%10
,729
1.6%

162
CENTRA
LISATION
OF ACU
TE OBSTETRIC CA
RE IN TH
E NETH
ERLAN
DS
9
Table 9.3 Hospital performance model
aOR CI P
Casemix variables
Parity & age category <.0001Primiparous & <25 years 1.09 0.93 1.28Primiparous & 25-29 years [ref ] 1.00Primiparous & 30-34 years 1.09 0.95 1.26Primiparous & ≥35 years 1.32 1.11 1.58Multiparous & <25 years 0.88 0.68 1.14Multiparous & 25-29 years 1.32 1.13 1.55Multiparous & 30-34 years 1.45 1.27 1.65Multiparous & 35-39 years 1.51 1.30 1.75Multiparous & ≥25 years 1.51 1.16 1.97
Ethnicity 0,009Western [ref ] 1.00Non-Western 1.15 1.04 1.28
Gestational age <.000122-27.6 weeks >1,000 >1,000 >1,00028-31.6 weeks 68.41 55.92 83.6732 weeks 14.64 11,18 19.1733 weeks 11.94 9.52 14.9734 weeks 6.23 4.95 7.8435 weeks 4.88 3.96 6.0036 weeks 2.97 2.44 3.6137 weeks 2.16 1.82 2.5838 weeks 1.18 1.00 1.3939 weeks 1.05 0.90 1.2240 weeks [ref ] 1.0041 weeks 1.38 1.18 1.60≥ 42 weeks 1.37 1.11 1.69
Congenital anomalies <.0001No [ref ] 1.00Yes 10.11 9.14 11.19
Small for gestational age (SGA) <.0001No SGA [ref ] 1.00Birthweight P2.3-P10 2.51 2.24 2.83Birthweight < P2.3 6.46 5.67 7.35
Fetal presentation <.0001Cephalic [ref ] 1.00Breech 1.65 1.46 1.85Transverse or other 2.06 1.60 2.65Unknown 1.48 1.02 2.13
Table 9.3 continues on next page.

163
CENTRA
LISATION
OF ACU
TE OBSTETRIC CA
RE IN TH
E NETH
ERLAN
DS
9
Table 9.3 Continued
aOR CI P
Organisational factors
Travel time (to hospital, in minutes) 0.98 0.97 0.99 <.0001
Hospital organisational featuresPrincipal component (factor 1) 0.99 0.87 1.13 0,893Principal component (factor 2) 1.08 0.92 1.27 0,356Principal component (factor 1) ^2 0.85 0.72 1.00 0,048Principal component (factor 2) ^2 1.04 0.92 1.18 0,510
Day and time of delivery <0.001Saturday 00:00-07:59 1.50 1.22 1.85Saturday 08:00-17:59 1.17 0.97 1.40Saturday 18:00-23:59 1.41 1.12 1.78Sunday 00:00-07:59 1.31 1.06 1.63Sunday 08:00-17:59 1.46 1.24 1.73Sunday 18:00-23:59 1.33 1.05 1.68Weekdays 00:00-07:59 1.35 1.21 1.51Weekdays 08:00-17:59 [ref ] 1.00Weekdays 18:00-23:59 1.40 1.25 1.56
Referral during parturition <0.001No [ref ] 1.00Yes 1.28 1.17 1.41
Interaction <.0001No Big4*travel time [ref ] 1.00Only one Big4*travel time 0.99 0.98 0.99More than one Big4*travel time 1.02 1.01 1.02
aOR: adjusted odds ratio, CI: confi dence interval.
travel time. Deliveries on Saturday nights have a 50% increased risk for perinatal mortality
(OR 1.50; CI 1.22-1.85), referral during parturition has a 28% increased risk (OR 1.28; CI 1.17-
1.41). The interaction term Big4*travel time is ‘protective’ in case of one ‘Big4’ morbidity
(OR 0.99; CI 0.98-0.99), but complex ‘Big4’ morbidity adds to the travel risk (RR 1.02; CI 1.01-
1.02). The random coefficient for hospital varied (data not shown) which is suggestive of
differences in hospital performance in terms of perinatal mortality.
Eff ects of centralisation scenarios
Table 9.4 and table 9.5 list the predicted results of the centralisation scenarios 1 and 2. The
left side of the table (‘before closure’) depicts the observed situation while the right side
(‘after closure’) depicts the predicted effects for the defined subgroups.

164
CENTRA
LISATION
OF ACU
TE OBSTETRIC CA
RE IN TH
E NETH
ERLAN
DS
9
Scenario 1
Following scenario 1 (table 9.4), a total number of 61,578 (5.3%) women will have to deliver
in other hospitals as their hospital of (actual) delivery will be hypothetically closed. Perinatal
mortality is expected to increase with 21 (10%) cases: from 210 cases (0.34%) observed
before closure to 231 cases (0.38%) predicted after closure. In absolute numbers, expected
perinatal mortality after closure is higher than the observed mortality before closure for
almost all subgroups except for unplanned hospital births (from 124 to 116 mortality cases)
Table 9.4 Predicted results after hypothetical closure of 10 hospitals according to scenario 1
Group Before closure After closure
N † N † % N † N † %
All pregnant women 61,578 210 0.34% 61,578 231 0.38%
Planned hospital birth (primary caesarean section/induced labour)
26,431 86 0.33% 26,431 115 0.44%
Unplanned hospital birth 35,147 124 0.35% 35,147 116 0.33%
Referral during parturition from home
6,775 19 0.28% 6,775 22 0.32%
Referral during parturition from hospital
7,599 20 0.26% 7,599 25 0.33%
Deliveries within 'offi ce hours' 26,618 75 0.28% 26,618 79 0.30%Deliveries outside 'offi ce hours' 34,960 135 0.39% 34,960 152 0.43%
Primiparous women 30,664 102 0.33% 30,664 113 0.37%Multiparous women 30,914 108 0.35% 30,914 118 0.38%
No Big4 morbidities 49,247 30 0.06% 49,217 58 0.12%Only one Big4 morbidity 11,175 91 0.81% 11,175 89 0.80%More than one Big4 morbidities 1,156 89 7.70% 1,156 84 7.27%
Minutes 95% CI Minutes 95% CI
Average travel time in unplanned hospital births
12.7 3.2-22.2 23.7 12.5-34.9
Travel time >20 minutes in hospital births
6,077 9.9% 20,201 32.8%
Hospital size (deliveries per year) N N
<750 per year 61,578 23,884750-1,250 per year 0 28,2731,250-1,750 per year 0 9,400>1,750 per year 0 21
†: perinatal mortality.

165
CENTRA
LISATION
OF ACU
TE OBSTETRIC CA
RE IN TH
E NETH
ERLAN
DS
9
and the presence of one (from 91 to 89 mortality cases) or more (from 89 to 84 mortality
cases) ‘Big4’ morbidities. The largest difference in observed versus predicted perinatal
mortality is for the group of planned hospital births (from 86 to 115 mortality cases). In
addition, average travel time to hospital will increase from 12.7 to 23.7 minutes with almost
one third (32.8%) of women having to travel more than 20 minutes after closure. Less than
half of women (23,884 of 61,578) will deliver in an alternative hospital that is of the same
size group (<750 annual deliveries) as before closure.
Table 9.5 Predicted results after hypothetical closure of 10 hospitals according to scenario 2
Group Before closure After closure
N † N † % N † N † %
All pregnant women 81,852 268 0.33% 81,852 259 0.32%
Planned hospital birth (primary caesarean section/induced labour)
39,172 124 0.32% 39,172 122 0.31%
Unplanned hospital birth 42,680 144 0.34% 42,680 137 0.32%
Referral during parturition from home
11,113 28 0.25% 11,113 29 0.26%
Referral during parturition from hospital
11,037 22 0.20% 11,037 28 0.25%
Deliveries within 'offi ce hours' 36,285 95 0.26% 36,285 95 0.26%Deliveries outside 'offi ce hours' 45,567 173 0.38% 45,567 164 0.36%
Primiparous women 42,085 131 0.31% 42,085 119 0.28%Multiparous women 39,767 137 0.34% 39,767 140 0.35%
No Big4 morbidities 67,233 52 0.08% 67,233 86 0.13%Only one Big4 morbidity 13,488 99 0.73% 13,488 94 0.70%More than one Big4 morbidities 1,131 117 10.34% 1,131 79 6.98%
Minutes 95% CI Minutes 95% CI
Average travel time in unplanned hospital births
10.8 4.2-17.3 15.8 10.3-21.4
Travel time >20 minutes in hospital births
3,106 3.8% 9,167 11.2%
Hospital size (deliveries per year) N N
<750 per year 81,852 9,089750-1,250 per year 0 69,2041,250-1,750 per year 0 3,533>1,750 per year 0 26
†: perinatal mortality.

166
CENTRA
LISATION
OF ACU
TE OBSTETRIC CA
RE IN TH
E NETH
ERLAN
DS
9
Scenario 2
According to scenario 2 (table 9.5), a total number of 81,852 (7.1%) women will have to
deliver in other hospitals with the relocation resulting in a negligible effect on perinatal
mortality (from 268 to 259 cases). For most subgroups, expected perinatal mortality after
closure is lower than the observed mortality before closure, except for referral during
parturition from home (from 28 to 29 cases) or hospital (from 22 to 28 cases), deliveries
within ‘office hours’ (95 cases before and after closure), multiparous women (from 137 to
140 cases), and no ‘Big4’ morbidities (from 52 to 86 cases). In addition, average travel time
to hospital will increase from 10.8 to 15.8 minutes. Note that a minority of women (9,089
of 81,852, 11.1%) will deliver in an alternative hospital of the same size group (<750 annual
deliveries) as before closure.
DISCUSSION
Principal fi ndings
In this national study with retrospective cohort data we predicted outcome effects for two
centralisation scenarios for acute obstetrical care by using a comprehensive empirical model.
Combined with increased travel time to hospital for both scenarios, scenario 1 resulted
in a 10% overall increased perinatal mortality, while scenario 2 resulted in a negligible
effect on perinatal mortality. In scenario 2 >85% of women in hypothetically ‘closed’
hospitals were ‘transferred’ to higher volume hospitals. Rather than just increased travel
time, the effects of centralisation appear to be determined by heterogeneity of hospitals’
organisational characteristics which in turn increase or decrease predicted perinatal
mortality. These changes appeared to depend more on the features of the newly assigned
next-nearest hospital rather than that of the initial hypothetically closed hospital. Indirectly
and by their quality factor scores, the data demonstrate that small hospitals perform
reasonably well. The picture is subtle: risk groups, e.g., women with one or more ‘Big4’
morbidities benefit from both centralisation scenarios as their predicted perinatal mortality
is lower than observed perinatal mortality before closure, Conversely, centralisation
appears to be detrimental for the small subset of women who are referred during
parturition.

167
CENTRA
LISATION
OF ACU
TE OBSTETRIC CA
RE IN TH
E NETH
ERLAN
DS
9
Other studies
Centralisation of acute obstetric care services has been considered in other countries as
well, mostly relying on theoretical reasoning alone.21-23 Furthermore, previous studies at
best used an ecological study design, were descriptive rather than comparative, and were
heterogeneous in design and results.9,19,22-24 Most studies conclude a strong pro- or against-
centralisation policy comparing risk-adjusted outcome in small (low level care) hospitals
versus outcome in large (high level care) hospitals, without modelling hospital performance
itself.9,19,22-25 In Norway, Moster et al. performed a population-based study using data on
1.7 million births from The Norwegian Medical Birth Registry.24 Neonatal mortality was
compared between several geographical areas characterised by the volume of the majority
of the maternity units. Overall neonatal mortality was 1.2-2.2 times higher in areas with the
majority of women giving birth in small scale maternity units (500 or less births annually)
compared to areas with the majority of births in large scale units (>3,000 births annually).
As this study lacked risk and casemix adjustment, its conclusion in favour of centralisation
may be biased in the presence of area related risk differences as shown in other studies.24
Some studies focus on either high risk or low risk patient groups.9,19,23,25 Bartels et al.25 and
Phibbs et al.19 studied the effect of NICU level on neonatal mortality for high risk infants,
both showing (up to 94%) higher (adjusted) neonatal mortality in smaller and lower level
NICUs favouring centralisation. Finally, two studies which focused on low risk patients show
conflicting results.9,23
Strengths and weaknesses
An important strength of our study is the usage of a validated national database as
virtually all pregnancies over 9 years were included (2000-2008). Additionally, our analysis
included detailed information on organisational characteristics of all Dutch hospitals,
lacking in other studies.9,19,22-25 Other strengths include the detailed casemix adjustment
and the multilevel approach which adjusts for the possible clustering of individuals within
hospitals. The hospital performance model combined with our scenario approach enables
detailed effect estimations of different hypothetical centralisation scenarios going beyond
mortality impact estimations only.9,19,22-25 Studies based on reasoning can account less
easily for the mix of perinatal mortality effects, and the subdivision of effects into effects in
different patient groups. Based on these strengths, our study goes beyond similar previous
studies’ methodology providing empirical evidence on differential effects of centralisation
schemes. We believe our framework to be beneficial for other countries also considering

168
CENTRA
LISATION
OF ACU
TE OBSTETRIC CA
RE IN TH
E NETH
ERLAN
DS
9
centralisation of acute obstetric care. In the United Kingdom, for example, the Royal
College of Obstetricians and Gynaecologists recently cautioned the widespread belief
that centralisation will always result in better patient outcome by stating ‘localised where
possible, centralised where necessary’.21
This study has limitations. Maternal lifestyle factors, in particular smoking, were unavailable
and not included in the casemix adjustment26 By including SGA and gestational age in
the model the effects of this limitation (in the context of this study) are reduced as they, if
combined, act as a proxy for smoking. Smoking has little effect beyond its effect on birth
weight and gestational age at delivery. Furthermore, we based our estimations on the
assumption that women in the hypothetically closed hospitals would deliver in the next-
nearest hospital. While this strategy is generally valid, individual preferences may decide
otherwise.27 Also, we assumed no change in performance and organisational features of
remaining hospitals after centralisation. As conflicting study results illustrate9,19,22-24, it is
unclear in what direction these features will change after centralisation. Additional research
is needed.
Finally, we only included perinatal mortality, travel time and volume of destination hospitals
as effect measures of the centralisation scenarios to illustrate the differential effects of two
different centralisation scenarios. Future research with additional outcomes such as NICU-
admission or intervention rates may further specify the effects of centralisation.
Arguments pro and con centralisation
Common arguments in favour of centralisation are: volume-related better care provision,
access to rapid intervention during delivery, quick resuscitation of the newborn, and rapid
identification and management of newborn infants with unexpected morbidities (e.g.,
congenital anomalies) in large and higher level hospitals.24 An important reason opposing
centralisation is the increased travel time to hospital, with inherent increased risk for
adverse perinatal outcome, especially for high risk women or out-of-hospital delivery.22
Ravelli et al. showed a 17-52% increased risk for perinatal mortality with travel time to
hospital of 20 minutes or more.7 Another reason against centralisation is that in high risk
oriented hospitals, low risk births are expected to be less ‘natural’ with an increased risk for
(obstetric) interventions and corresponding increased costs.28 Moreover, financial aspects
of centralisation policy need to be considered, e.g., resource distribution costs or education
and salary costs for consultants (obstetrics, paediatrics, anaesthesiology, etc.).29 The inter-
dependency of acute obstetric care services with, e.g., paediatric / neonatal services and

169
CENTRA
LISATION
OF ACU
TE OBSTETRIC CA
RE IN TH
E NETH
ERLAN
DS
9
anaesthesiology services should also be considered. These services may be at risk of collapse
as the number of physicians required to sustain on-call coverage may be no longer available
in small hospitals after acute obstetric care has been centralised.8 Finally, particularly for The
Netherlands where about 20% of births still occur at home under supervision of a midwife10,
increased travel time to hospital will compromise these (low risk) women in their choice
to opt for a birth at home.
Conclusion
In The Netherlands, centralisation of obstetric care according to the ‘closure-of-the-smallest-
rule’ yields suboptimal outcomes in terms of perinatal mortality and increased travel time
to hospital. In order to develop an optimal strategy for centralisation one would need to
consider all positive and negative effects: heterogeneity in organisational features of closed
and surviving hospitals, financial aspects, differential effects for patient subgroups, increased
travel time and adequate antenatal risk selection. Current heterogeneity in organisational
features, where the smallest hospitals on average perform remarkably well, contradicts a
simple size related closure strategy. Differential effects of hospital quality, travel time and
antenatal risk selection should all be taken into account.
REFERENCES1. Buitendijk SE, Nijhuis JG. High perinatal mortality
in the Netherlands compared to the rest of Europe. Ned Tijdschr Geneeskd. 2004;148:1855-1860.
2. Mohangoo AD, Buitendijk SE, Hukkelhoven CW, et al. Higher perinatal mortality in The Netherlands than in other European countries: the Peristat-II study. Ned Tijdschr Geneeskd. 2008;152:2718-2727.
3. de Graaf JP, Ravelli AC, Visser GH, et al. Increased adverse perinatal outcome of hospital delivery at night. BJOG. 2010;117:1098-1107.
4. Sheldon T. Prompt access to expert care is among advice to reduce perinatal deaths in Netherlands. BMJ. 2010;340:c277.
5. Sheldon T. Netherlands drops plans to deliver acute obstetric care in 15 minutes. BMJ. 2012;344: e2302.
6. 24/7 acute obstetric hospital care (in Dutch: 24/7 acute verloskunde in het ziekenhuis), Dutch report on the effects of centralisation of acute obstetric care. Amstelveen: KPMG Advisory Plexus; 2012.
7. Ravelli AC, Jager KJ, de Groot MH, et al. Travel time from home to hospital and adverse perinatal outcomes in women at term in the Netherlands. BJOG. 2011;118:457-465.
8. Klein M, Johnston S, Christilaw J, Carty E. Mothers, babies, and communities. Centralizing maternity care exposes mothers and babies to complications and endangers community sustainability. Can Fam Physician. 2002;48:1177-1179, 1183-1175.
9. Tracy SK, Sullivan E, Dahlen H, Black D, Wang YA, Tracy MB. Does size matter? A population-based study of birth in lower volume maternity hospitals for low risk women. BJOG. 2006;113:86-96.

170
CENTRA
LISATION
OF ACU
TE OBSTETRIC CA
RE IN TH
E NETH
ERLAN
DS
9
10. Perinatal care in The Netherlands 2008 (in Dutch: Perinatale zorg in Nederland 2008). Utrecht: The Netherlands Perinatal Registry; 2011.
11. Stillbirth Collaborative Research Network Writ-ing G. Causes of death among stillbirths. JAMA. 2011;306:2459-2468.
12. Burstyn I. Principal component analysis is a powerful instrument in occupational hygiene inquiries. Ann Occup Hyg. 2004;48:655-661.
13. Anthony S, Jacobusse GW, van der Pal-de Bruin KM, Buitendijk S, Zeitlin J, Factors E-PWGoR. Do differences in maternal age, parity and multiple births explain variations in fetal and neonatal mortality rates in Europe?--Results from the EURO-PERISTAT project. Paediatr Perinat Epidemiol. 2009;23:292-300.
14. De Graaf JP, Ravelli AC, Wildschut HI, et al. Perinatal outcomes in the four largest cities and in deprived neighbourhoods in The Netherlands. Ned Tijdschr Geneeskd. 2008;152:2734-2740.
15. Evers AC, Brouwers HA, Hukkelhoven CW, et al. Perinatal mortality and severe morbidity in low and high risk term pregnancies in the Netherlands: prospective cohort study. BMJ. 2010;341:c5639.
16. Ravelli AC, Tromp M, van Huis M, et al. Decreasing perinatal mortality in The Netherlands, 2000-2006: a record linkage study. J Epidemiol Community Health. 2009;63:761-765.
17. Timmermans S, Bonsel GJ, Steegers-Theunissen RP, et al. Individual accumulation of heterogeneous risks explains perinatal inequalities within deprived neighbourhoods. Eur J Epidemiol. 2011;26:165-180.
18. Rietberg CCT. Term breech delivery in The Netherlands; chapter 7. Thesis 2006, University of Utrecht. (online available: http://igitur-archive.library.uu.nl/dissertations/2006-1031-200813/c7.pdf ).
19. Phibbs CS, Bronstein JM, Buxton E, Phibbs RH. The effects of patient volume and level of care at the hospital of birth on neonatal mortality. JAMA. 1996;276:1054-1059.
20. Bonsel GJ, Birnie E, Denktas S, Poeran J, Steegers EAP. Dutch report: Lijnen in de Perinatale Sterfte, Signalementstudie Zwangerschap en Geboorte 2010. Rotterdam: Erasmus MC; 2010.
21. Tomorrow’s specialist: working party report, September 2012. London: The Royal College of Obstetricians and Gynaecologists; 2012. (Online http://www.rcog.org.uk/files/rcog-corp/Tomorrow’s%20Specialist_FullReport.pdf ).
22. Hemminki E, Heino A, Gissler M. Should births be centralised in higher level hospitals? Experiences from regionalised health care in Finland. BJOG. 2011;118:1186-1195.
23. Heller G, Richardson DK, Schnell R, Misselwitz B, Kunzel W, Schmidt S. Are we regionalized enough? Early-neonatal deaths in low-risk births by the size of delivery units in Hesse, Germany 1990-1999. Int J Epidemiol. 2002;31:1061-1068.
24. Moster D, Lie RT, Markestad T. Neonatal mortality rates in communities with small maternity units compared with those having larger maternity units. BJOG. 2001;108:904-909.
25. Bartels DB, Wypij D, Wenzlaff P, Dammann O, Poets CF. Hospital volume and neonatal mortality among very low birth weight infants. Pediatrics. Jun 2006;117:2206-2214.
26. Andres RL, Day MC. Perinatal complications associated with maternal tobacco use. Semin Neonatol. 2000;5:231-241.
27. Phibbs CS, Mark DH, Luft HS, et al. Choice of hospital for delivery: a comparison of high-risk and low-risk women. Health Serv Res. 1993;28:201-222.
28. Tracy SK, Tracy MB. Costing the cascade: estimat-ing the cost of increased obstetric intervention in childbirth using population data. BJOG. 2003; 110:717-724.
29. Lemmens K, Janus J, van Schooten G, Vlieger E. 24/7 acute obstetric care in hospital (in Dutch: 24/7 acute verloskunde in het ziekenhuis). Amstelveen: KPMG Plexus; 2012. (Online http://www.rijksoverheid.nl/documenten-en-publicaties/rapporten/2012/03/01/24-7-acute-verloskunde-in-het-ziekenhuis.html).

10
Manuscript submitted for publication.
The impact of extremes in outdoor temperature and sunshine
exposure on birthweight
J. Poeran, E. Birnie, E.A.P. Steegers, G.J. Bonsel

172
EXTREMES IN
OU
TDO
OR TEM
PERATURE A
ND
BIRTHW
EIGH
T
10
ABSTRACTBackground With the advent of the ‘fetal origins of adult disease’ hypothesis, environmental
determinants of birthweight regained interest. However, studies are heterogeneous in
design with conflicting results. We developed and applied a detailed spatial-time exposure
model for the most likely climatological factors affecting fetal growth: seasonality,
temperature and sunshine
Methods Daily climatological data (29 weather stations) were linked to all 1,460,401 term
singleton births (The Netherlands Perinatal Registry 2000-2008). An individual exposure
matrix for each pregnancy was computed for five exposure windows: (1) periconceptional,
(2) first / (3) second / (4) third trimester, and (5) day of delivery. Next, linear regression models
were specified with birthweight (in grams) as outcome and seasonality, minimum and
maximum ambient temperature, cumulative sunshine exposure, and maternal and child
factors as determinants. The final model enabled to quantify climatological contribution
to existing spatial variations in birthweight.
Results In The Netherlands, substantial regional differences exist in temperature extremes
and sunshine, with less temperature extremes and more sunshine in coastal areas. Our
exposure model explained existing irregular and modest seasonal birthweight effects
as a combined effect of season, temperature and sunshine with biologically plausible
exposure effects. A seasonal birthweight pattern emerged, modified by short and long
term temperature and sunshine effects. Summer is associated with an almost 20 gram
significantly decreased birthweight. Short term minimum and maximum temperature
exposures are significantly associated with higher and lower birthweight, respectively,
with effect sizes dependent on their timing during pregnancy. Also, higher cumulative
sunshine exposure during pregnancy increases birthweight. On the population level, we
demonstrated spatial differences in birthweight (range -11 to +25 grams) attributable to
the cumulative climatological effects, with lowest birthweights in inland areas.
Conclusion Birthweight is associated with the combined effect of season and exposure
to temperature extremes and cumulative exposure to sunshine, in particular during
critical reproductive exposure windows in pregnancy. The demonstrated negative
birthweight effects of maximum temperature exposure confirm results from animal studies.
Consequently, a climate footprint is visible in the regional birth weight differences.

173
EXTREMES IN
OU
TDO
OR TEM
PERATURE A
ND
BIRTHW
EIGH
T
10
INTRODUCTIONOver 2,000 years ago, Hippocrates already postulated effects of ‘warm and cold winds,
seasons and changes in weather’ on health.1 Indeed, a large body of evidence exists on
the effects of seasonality, ambient temperature and sunshine exposure on adult health.2-4
With the advent of the ‘fetal origins of adult disease’ hypothesis5, many studies have also
focused on exposure to climatological factors in the intrauterine period.6 In particular, the
determinants of birthweight are of renewed interest in the search to identify modifiable
factors which may prove useful for the development of strategies that prevent possible
disease in later life.6-10
Seasonality, ambient temperature and sunshine appear the most likely factors to influence
birthweight and have been previously studied.6-10 However, these studies show inconsistent
results, due to differences in methodology and study size, little or no adjustment for
known confounders, and considerable differences in exposure definitions.6-10 So far, no
universal exposure concept has emerged, distinguishing between peak exposure and
cumulative exposure effects, and taking varying exposure windows during pregnancy into
account. Most studies use mean temperature during pregnancy as exposure measure6-10,
while in particular extremes during heat and cold waves are of interest as they increase
cardiovascular mortality in adult deaths through blood flow changes.11 Regarding sunshine,
cumulative rather than peak exposure is of interest as it is thought that its effect runs mainly
through vitamin D.12
Here, we study the impact of peak temperature and cumulative sunshine on birthweight,
distinguishing between five exposure windows: periconceptionally, in the first, second
and third trimesters of pregnancy, and the day of delivery. We obtained geographically
detailed climatological data which permitted us to compute day-to-day individual exposure
patterns. The impact of climatological factors on birthweight was then studied using an
individual exposure model, taking into account the association between temperature and
sunshine exposure, and the competing impact of other known endogenous and exogenous
factors influencing birthweight.13 The resulting temporal-spatial relations were mapped,
to demonstrate the contribution of the selected climatological factors to existing regional
differences in birthweight.

174
EXTREMES IN
OU
TDO
OR TEM
PERATURE A
ND
BIRTHW
EIGH
T
10
METHODS
Patient data
In this retrospective cohort study we derived data on maternal factors, child factors and
birthweight from The Netherlands Perinatal Registry. This registry contains complete
population-based information of >97% of all pregnancies in the Netherlands.14 On behalf of
the respective professional societies, source data are routinely collected by 94% of midwives,
99% of gynaecologists and 68% of paediatricians including 100% of Neonatal Intensive
Care Unit paediatricians.14 (See website for detailed description: www.perinatreg.nl). The
board of The Netherlands Perinatal Registry granted permission to use the anonymous
registry data for this study. The registry contains data on 1,620,126 births for the period of
2000-2008. We excluded multiple pregnancies (n=35,326), births with gestational age < 37
weeks or unknown (n=116,139), births with unknown parity or neonate’s sex (n=353 and
n=433, respectively), and unknown or erroneous zip code (n=7,474). The final database
consisted of 1,460,401 births.
Climatological data
Daily maximum and minimum temperatures (in degrees Celsius) and sunshine (in hours)
were derived from 29 temperature stations throughout The Netherlands (figure 10.1). The
catchment area of each temperature station was based on 2-digit zip code with an average
population of 182,228 per zip code area. Data were obtained from the Royal Netherlands
Meteorological Institute (see website for detailed description: www.knmi.nl/index_en.html).
Exposure concept
From past evidence and biological considerations (critical reproductive windows) 6-10, we
derived five non-overlapping exposure windows (figure 10.2):
• from 3 days before to 3 days after conception, periconceptional (E1);
• from conception to 91 days after conception, first trimester (E2);
• from 92 days to 182 days after conception, second trimester (E3);
• from 183 days to 273 days after conception, third trimester (E4);
• day of birth (E5).

175
EXTREMES IN
OU
TDO
OR TEM
PERATURE A
ND
BIRTHW
EIGH
T
10
Climatological exposure was defined as follows: seasonality (captured by month of birth),
the minimum and maximum temperature, individually calculated for each exposure
window (E1-E5), and total sunshine exposure (in hours) individually calculated for windows
E2-E4.
The computation of exposure started with determining date of conception, which was
estimated from recorded information on gestational age at birth and date of delivery.
Figure 10.1 Map of The Netherlands with the 29 temperature stations and their catchment areas in shades of grey.

176
EXTREMES IN
OU
TDO
OR TEM
PERATURE A
ND
BIRTHW
EIGH
T
10
The climatological exposure information was subsequently projected on each pregnancy
individually for E1 to E5, providing an individual exposure profile for each woman. Climate
data were linked to individual records using the zip code. Date of delivery (a consecutive
number from 1 to 3,288 for every day in the study period) was used as variable to capture
the secular trend of increasing birthweight.8
Defi nition of outcome and maternal and child factors
The main outcome was birthweight in grams. Known maternal and child factors affecting
birthweight were also included. Maternal factors were parity (primiparous / multiparous),
ethnicity (Western / non-Western), maternal age (continuous), and socioeconomic status
(SES) score based on zip code of residence. Since the effect of maternal age on birthweight
appears to be inverse U-shaped (lower birthweight for the youngest and oldest mothers),
we used the quadratic value of maternal age as determinant. As a proxy for neighbourhood
Figure 10.2 Exposition model with different windows of exposure and the selection of exposure measures included the regression model. C = conception, C-3 = conception minus 3 days, C+91/182/273 = conception plus 91/182/273 days, E1-E5 = windows of exposure.
x xx x xx x xx x xx x
C+91 C+182 C+273
E2: from conception to 91 days after conceptionE3: from 92 days to 182 days after conceptionE4: from 183 days to 273 days after conception
C
E1E4
E5
C-3
E3E2
Total sunshine exposure in hours
MEASURE OF EXPOSURE
E5: day of birth
WINDOW OF EXPOSURE Minimum temperature
Maximum temperature
E1: 3 days before to 3 days after conception

177
EXTREMES IN
OU
TDO
OR TEM
PERATURE A
ND
BIRTHW
EIGH
T
10
SES we used zip code specific (publicly available) SES scores, which are made available by the
National Statistics Office (website in Dutch: www.scp.nl/Organisatie/Onderzoeksgroepen/
Wonen_Leefbaarheid_Veiligheid/Lopend_onderzoek_van_WLV/Statusscores). These SES
scores are zip code based and use individual data on e.g., income, taxes, hours of work, and
educational level. The scores are approximately normally distributed at the neighbourhood
level, where a negative score represents a high SES.
Child factors were gestational age (six categories), presence of congenital anomalies (yes
/ no), and neonate’s sex (male / female). In The Netherlands Perinatal Registry, congenital
anomalies are recorded postpartum and classified through a standard coding system by
organ system (8 categories, 71 subcategories).
Analysis
Linear regression models were specified in a predefined order. First, all maternal and child
factors and consecutive number of day of birth were included as determinants (model 0).
Next, season (month of birth) was added (model 1). In model 2 and 3, the temperature
and sunshine exposure measures were subsequently added. Models’ goodness of fit was
compared by the adjusted R-squared (R2) statistic.
Subsequently, we aimed to study regional differences in mean birthweight attributable to
our climatological exposure measures. We did so by studying the birthweight difference
between a dataset in which we allowed for the actual regional climatological differences
(original dataset) and a dataset in which we (hypothetically) ‘eliminated’ this regional
difference by substituting the minimum and maximum temperature, and sunshine
exposition by the national average, all other things equal (duplicate dataset). We used
coefficients obtained from model 3 to predict mean birthweight in this duplicate dataset.
The resulting regional differences (in grams) between observed mean weight (including
the effect of climatological factors) and predicted mean weight (excluding the effect of
climatological factors) are attributable to climatological factors and were illustrated on a
map of The Netherlands per 2-digit zip code. Because of the cancellation of the effect of
climatological factors in the duplicate dataset, the difference in mean weight between the
original and duplicate dataset represents the regional differences in birthweight attributable
to the selected climatological factors.
The linear regression models were fitted using SPSS version 20 (IBM Corporation, Somers,
NY, USA). SAS version 9.2 (SAS Institute Inc., Cary, NC) was used, with the GLM procedure
to run model 3 and use its coefficients to predict birthweight in a duplicate dataset. Maps

178
EXTREMES IN
OU
TDO
OR TEM
PERATURE A
ND
BIRTHW
EIGH
T
10
were constructed using ESRI ArcGIS version 9.3 (Environmental Systems Research Institute,
Inc., USA).
Table 10.1 Study group characteristics: subgroup sizes, subgroup mean birthweight differences with overall mean birthweight, and subgroup SGA prevalence (%)
N Mean subgroup BW-mean overall BWa
SD % SGA
Maternal factors
ParityPrimiparous 660,797 -88 485 9.7%Multiparous 799604 73 500 9.8%
Maternal age<20 years 23,594 -197 469 14.1%20-35 years 1,226,233 -2 497 9.6%>35 years 210,574 32 516 10.3%
EthicityWestern 1,225,392 18 500 9.0%Non-Western 235,009 -92 490 13.5%
Socioeconomic statusb
Low (<p20) 365,558 -56 504 12.2%Medium (p20-p80) 842,290 15 499 9.2%High (>p80) 252,553 33 490 8.2%
Child factors
Gestational age37 weeks 87,505 -473 488 9.8%38 weeks 221,349 -237 468 9.8%39 weeks 361,621 -67 450 9.8%40 weeks 428,778 85 453 9.7%41 weeks 281,509 210 466 9.8%≥42 weeks 79,639 282 476 9.7%
Congenital anomaliesNo 1,430,003 2 498 9.6%Yes 30,398 -97 581 16.1%
SexMale 746,603 67 505 9.7%Female 713,798 -70 485 9.8%
Year of birth2000-2002 501,459 -14 501 10.3%2003-2005 488,010 5 501 9.7%2006-2008 470,932 9 497 9.1%
a Mean overall BW = 3,522 gram, with SD = 500 gram.b Status scores were cut off at the 20th (low SES) and 80th percentile (high SES).

179
EXTREMES IN
OU
TDO
OR TEM
PERATURE A
ND
BIRTHW
EIGH
T
10
RESULTSTable 10.1 illustrates study population characteristics, differences between subgroup mean
birthweight and overall mean birthweight, and small for gestational age prevalence per
subgroup (SGA, birthweight <10th percentile). Subgroups with a significantly lower mean
birthweight are: (1) women who are primiparous (-88 grams), <20 years (-197 grams), non-
Western origin/background (-92 grams), with a low socioeconomic status (-56 grams); and
children who are born between 37 and 39 weeks of gestational age (-473 to -67 grams),
who have congenital anomalies (-97 grams), and are female (-70 grams). SGA prevalence
was highest in teenage pregnancies (maternal age <20 years, 14.1%), non-Western women
(13.5%), low socioeconomic status women (12.2%), and children born with a congenital
anomaly (16.1%).
Diff erences in temperature and sunshine exposure by region
Table 10.2 illustrates the regional and within-year variation in temperature and sunshine
exposure in The Netherlands. For convenience we listed temperature and sunshine exposure
overall, and for three temperature stations separately: ‘de Kooy’, ‘de Bilt’, and ‘Maastricht’
located in the north, middle and south of The Netherlands, respectively. As expected,
temperatures are highest in summer (peaks in July / August, average 17.9 and 17.7 degrees
Celsius), and lowest in winter (nadirs in December / January, average 4.0 and 4.2 degrees
Celsius). Sunshine exposure is highest in May / June (average 7.2 and 7.3 hours per day),
and lowest in December / January (average 2.2 and 1.9 hours per day).
There is a difference of 1 degree Celsius between the northern (higher in January) and the
southern temperature stations (higher in July). In the north, the temperature extremes
appear less, with more sunshine, particularly in July with a difference of almost an hour
per day (7.4 - 6.6 = 0.8 hours).
Linear regressions
Table 10.3 lists the linear regressions with beta coefficients, their 95% confidence intervals
(CI), and the adjusted R2 values for each model. In model 0 all determinants have a
significant contribution to the model with the largest beta coefficients for primiparous
women (-169.8, CI -171.3;-168.4), children born at 37 weeks (-552.3, CI -555.5;-549.1) and 38
weeks (-324.1, CI -326.4;-321.9), and female sex (-145.8, CI -147.2;-144.3). In model 1, month
of birth was added which did not alter the beta coefficients of maternal and child factors.

180
EXTREMES IN
OU
TDO
OR TEM
PERATURE A
ND
BIRTHW
EIGH
T
10
Most months showed significant, yet small effects on birthweight with beta coefficients
ranging from 3.7 (September) to 6.7 (May) compared to January. No clear pattern in beta
coefficients of month of birth was observed. Temperature exposure measures were added
in model 2. A clear pattern in months emerged with a highly significant birthweight nadir
in summer: >18 grams lower birthweight in July (-18.4) and August (-18.5). Beta coefficients
for temperature exposure measures were small. For minimum temperature only exposures
during first, second and third trimester were significant with beta coefficients ranging
Table 10.2 Monthly differences of temperature and sunshine; overall and for three temperature stations separately: ‘de Kooy’, ‘de Bilt’, and ‘Maastricht’ located in the north, middle and south of The Netherlands, respectively
Mean day temperature
Minimum day temperature
Maximum day temperature
Mean day sunshine hours
Temperature station: all
MonthJanuary 4.2 -16.8 15.9 2.2February 4.2 -15.4 18.0 3.5March 6.2 -20.7 22.2 4.4April 9.6 -7.9 29.7 6.4May 13.6 -1.5 32.6 7.2June 16.1 0.9 34.7 7.3July 17.9 3.7 37.1 6.8August 17.7 4.4 37.8 6.0September 15.3 0.5 31.3 5.3October 11.2 -8.5 24.0 4.0November 7.4 -7.2 19.4 2.2December 4.0 -17.0 16.3 1.9
Temperature station: 'De Kooy'
MonthJanuary 4.8 -8.5 12.2 2.3July 17.5 8.4 30.2 7.4
Temperature station: 'De Bilt'
MonthJanuary 4.3 -10.6 14.1 2.1July 18.1 6.4 35.7 6.6
Temperature station: 'Maastricht'
MonthJanuary 3.9 -11.7 15.5 2.2July 18.5 7.2 36.3 6.6

181
EXTREMES IN
OU
TDO
OR TEM
PERATURE A
ND
BIRTHW
EIGH
T
10
Ta
ble
10
.3
Line
ar re
gres
sion
mod
els
with
regr
essi
on c
oeffi
cien
ts w
ith (9
5% c
onfid
ence
inte
rval
s)
(adj
uste
d R2 )
Mod
el 0
(0.2
1)M
odel
1 (0
.21)
Mod
el 2
(0.2
1)M
odel
3 (0
.21)
Beta
coe
ffi ci
ent
Beta
coe
ffi ci
ent
Beta
coe
ffi ci
ent
Beta
coe
ffi ci
ent
Cons
tant
3903
.9 (3
900.
9;39
07.0
)*39
00.0
(389
6.1;
3903
.8)*
*40
49.2
(403
5.7;
4062
.6)*
4019
.0 (4
004.
0;40
33.9
)*
Ma
tern
al
fac
tors
Parit
yPr
imip
arou
s-1
69.8
(-17
1.3;
-168
.4)*
-169
.8 (-
171.
3;-1
68.3
)*-1
69.9
(-17
1.4;
-168
.4)*
-169
.9 (-
171.
4;-1
68.4
)*M
ultip
arou
sRe
fere
nce
Refe
renc
eRe
fere
nce
Refe
renc
e
Mat
erna
l age
^2-0
.17
(-0.1
8;-0
.16)
*-0
.17
(-0.1
8;-0
.16)
*-0
.17
(-0.1
8;-0
.16)
*-0
.17
(-0.1
8;-0
.16)
*
Ethi
city
Wes
tern
Refe
renc
eRe
fere
nce
Refe
renc
eRe
fere
nce
Non
-Wes
tern
-90.
0 (-9
2.1;
-87.
9)*
-90.
0 (-9
2.1;
-87.
9)*
-91.
0 (-9
3.1;
-88.
9)*
-91.
4 (-9
3.5;
-89.
3)*
Soci
oeco
nom
ic s
tatu
s sc
ore
-17.
9 (-1
8.6;
-17.
1)*
-17.
9 (-1
8.6;
-17.
1)*
-18.
1 (-1
8.8;
-17.
3)*
-18.
0 (-1
8.7;
-17.
2)*
Ch
ild
fa
cto
rs
Ges
tatio
nal a
ge37
wee
ks-5
52.3
(-55
5.5;
-549
.1)*
-552
.3 (-
555.
5;-5
49.0
)*-5
52.2
(-55
5.4;
-549
.0)*
-552
.2 (-
555.
4;-5
49.0
)*38
wee
ks-3
24.1
(-32
6.4;
-321
.9)*
-324
.1 (-
326.
4;-3
21.8
)*-3
24.1
(-32
6.4;
-321
.8)*
-324
.1 (-
326.
4;-3
21.8
)*39
wee
ks-1
52.5
(-15
4.4;
-150
.5)*
-152
.5 (-
154.
4;-1
50.5
)*-1
52.4
(-15
4.4;
-150
.4)*
-152
.4 (-
154.
4;-1
50.5
)*40
wee
ksRe
fere
nce
Refe
renc
eRe
fere
nce
Refe
renc
e41
wee
ks12
7.7
(125
.6;1
29.8
)*12
7.7
(125
.6;1
29.8
)*12
7.6
(125
.5;1
29.8
)*12
7.6
(125
.5;1
29.7
)*≥4
2 w
eeks
218.
4 (2
15.0
;221
.8)*
218.
4 (2
15.0
;221
.8)*
218.
5 (2
15.1
;221
.8)*
218.
4 (2
15.1
;221
.8)*
Cong
enita
l ano
mal
ies
No
Refe
renc
eRe
fere
nce
Refe
renc
eRe
fere
nce
Yes
-74.
6 (-7
9.6;
-69.
5)*
-74.
6 (-7
9.6;
-69.
5)*
-74.
3 (-7
9.4;
-69.
3)*
-74.
3 (-7
9.3;
-69.
2)*
Tabl
e 10
.3 co
ntin
ues o
n ne
xt p
age.

182
EXTREMES IN
OU
TDO
OR TEM
PERATURE A
ND
BIRTHW
EIGH
T
10
Ta
ble
10
.3
Cont
inue
d
(adj
uste
d R2
)M
odel
0 (0
.21)
Mod
el 1
(0.2
1)M
odel
2 (0
.21)
Mod
el 3
(0.2
1)
Beta
coe
ffi ci
ent
Beta
coe
ffi ci
ent
Beta
coe
ffi ci
ent
Beta
coe
ffi ci
ent
Sex M
ale
Refe
renc
eRe
fere
nce
Refe
renc
eRe
fere
nce
Fem
ale
-145
.8 (-
147.
2;-1
44.3
)*-1
45.8
(-14
7.2;
-144
.3)*
-145
.7 (-
147.
2;-1
44.3
)*-1
45.7
(-14
7.2;
-144
.3)*
Cli
ma
tolo
gic
al
fac
tors
Day
of b
irth:
con
secu
tive
num
ber i
n st
udy
perio
d0.
010
(0.0
09;0
.010
)*0.
010
(0.0
09;0
.010
)*0.
010
(0.0
10;0
.011
)*0.
009
(0.0
09;0
.010
)*
Mon
th o
f birt
hN
ot in
equ
atio
nJa
nuar
y-
Febr
uary
-2.
4 (-1
.2;6
.0)
-1.3
(-5.
4;2.
8)-0
.3 (-
4.4;
3.8)
Mar
ch-
4.0
(0.5
;7.5
)***
-4.4
(-9.
3;0.
6)-2
.0 (-
7.1;
3.1)
Apr
il-
5.6
(2.0
;9.1
)**
-6.0
(-12
.0;-0
.1)*
**-1
.5 (-
7.7;
4.7)
May
-6.
7 (3
.2;1
0.2)
*-8
.3 (-
15.0
;-1.6
)***
-1.3
(-8.
4;5.
7)Ju
ne-
5.2
(1.7
;8.8
)**
-16.
1 (-2
3.3;
-8.9
)*-7
.5 (-
15.2
;0.2
)Ju
ly-
6.2
(2.8
;9.7
)*-1
8.4
(-25.
5;-1
1.2)
*-9
.3 (-
17.0
;-1.5
)***
Augu
st-
3.0
(-0.5
;6.5
)-1
8.5
(-25.
5;-1
1.4)
*-1
1.1
(-18.
7;-3
.6)*
*Se
ptem
ber
-3.
7 (0
.2;7
.2)*
**-1
5.1
(-21.
6;-8
.6)*
-10.
5 (-1
7.3;
-3.6
)**
Oct
ober
-4.
1 (0
.6;7
.6)*
**-6
.1 (-
11.6
;-0.6
)***
-3.5
(-9.
3;2.
3)N
ovem
ber
-5.
9 (2
.3;9
.4)*
*3.
5 (-1
.3;8
.3)
5.4
(0.4
;10.
4)**
*D
ecem
ber
-0.
4 (-3
.1;4
.0)
-0.4
(-4.
6;3.
8)0.
3 (-4
.0;4
.5)

183
EXTREMES IN
OU
TDO
OR TEM
PERATURE A
ND
BIRTHW
EIGH
T
10
Min
imum
tem
pera
ture
: win
dow
of e
xpos
ure
Not
in e
quat
ion
Not
in e
quat
ion
E1: p
eric
once
ptio
nal
--
0.3
(0.0
;0.6
)0.
2 (-0
.1;0
.6)
E2: fi
rst t
rimes
ter
--
-0.6
(-1.
1;-0
.2)*
*-0
.3 (-
0.8;
0.1)
E3: s
econ
d tr
imes
ter
--
0.6
(0.3
;1.0
)**
0.4
(0.0
;0.8
)***
E4: t
hird
trim
este
r-
-1.
5 (1
.3;1
.8)*
1.5
(1.2
;1.7
)*E5
: day
of b
irth
--
0.1
(-0.2
;0.4
)0.
1 (-0
.2;0
.4)
Max
imum
tem
pera
ture
: win
dow
of e
xpos
ure
Not
in e
quat
ion
Not
in e
quat
ion
E1: p
eric
once
ptio
nal
--
-0.6
(-0.
9;-0
.3)*
-0.4
(-0.
8;-0
.1)*
*E2
: fi rs
t trim
este
r-
--1
.6 (-
1.9;
-1.2
)*-2
.1 (-
2.4;
-1.7
)*E3
: sec
ond
trim
este
r-
--2
.2 (-
2.5;
-1.9
)*-2
.4 (-
2.8;
-2.0
)*E4
: thi
rd tr
imes
ter
--
-2.0
(-2.
3;-1
.7)*
-2.1
(-2.
5;-1
.8)*
E5: d
ay o
f birt
h-
--0
.4 (-
0.7;
-0.2
)**
-0.4
(-0.
6;-0
.1)*
*
Cum
ulat
ive
suns
hine
in h
ours
: win
dow
of e
xpos
ure
Not
in e
quat
ion
Not
in e
quat
ion
Not
in e
quat
ion
E2: fi
rst t
rimes
ter
--
-0.
052
(0.0
39;0
.065
)*E3
: sec
ond
trim
este
r-
--
0.02
5 (0
.011
;0.0
38)*
*E4
: thi
rd tr
imes
ter
--
-0.
023
(0.0
10;0
.036
)**
* p<
0.00
01, *
* p>
0.00
01 a
nd p
<0.0
1, *
** p
>0.0
1 an
d p<
0.05
.

184
EXTREMES IN
OU
TDO
OR TEM
PERATURE A
ND
BIRTHW
EIGH
T
10
from -0.6 to 1.5. For maximum temperature all exposure windows had significant beta
coefficients ranging from -0.4 (day of birth) to -2.2 (second trimester). After adding sunshine
exposure to model 3, the summer nadir remained significant, but with moderation of beta
coefficients to -9.3 for July and -11.1 for August. Sunshine exposure demonstrated small,
yet significant effects with beta coefficients ranging from 0.023 to 0.052. As opposed to
Figure 10.3 Regional birthweight differences (per 2-digit zip code) attributable to difference in exposure to temperature extremes and sunshine (adjusted for maternal factors, child factors, and day and month of birth).

185
EXTREMES IN
OU
TDO
OR TEM
PERATURE A
ND
BIRTHW
EIGH
T
10
the emerging pattern of seasonality in model 2, there was no difference in adjusted R2
(0.21) between the models, implying combined (interacting) effects of temperature and
sunshine with seasonality.
Regional birthweight diff erences
The regional birthweight differences range from -11 to +25 grams due to the selected
climatological exposures, with moderation of these effects (i.e., higher birthweights) in
coastal areas (figure 10.3).
DISCUSSIONBirthweight is associated with the combined effect of season and exposure to temperature
extremes and cumulative exposure to sunshine, in particular during critical reproductive
exposure windows in pregnancy. We demonstrated small, yet consistent effects on top of
known maternal and child factors. The effects of seasonality alone were initially modest
(table 10.3, model 1) but most likely hided interacting effects of temperature and sunshine,
illustrated by the clear pattern in seasonality after inclusion of temperature and sunshine
in the model (table 10.3, model 2 and 3). The result was an almost 20 gram significantly
decreased birthweight in summer compared to January. We found minimum temperature
exposure in the second and third trimester to be associated with higher birthweight,
maximum temperature exposure for all exposure windows to be associated with lower
birthweight, and cumulative sunshine exposure to be associated with higher birthweight.
On the population level, there are significant regional differences in birthweight, attributable
to the selected climatological exposure measures, ranging from -11 to +25 grams (relative
to the observed birthweight). The detrimental effect of maximum temperature in particular,
appears to be moderated in coastal areas where there are less temperature extremes and
more sunshine hours. The superposition of the observed effects with differential timing of
exposure explains the hitherto unexplained or contradictory patterns in previous papers.6
Other studies
Previous studies on the relationship between climate and birthweight are heterogeneous
in design and outcome. 6-10 In an Australian large cohort study in the Perth region, Pereira et
al. investigated the effect of seasonal variation, temperature and sunshine on birthweight,
adjusted for sociodemographic, biological, and environmental exposures (e.g., air pollutants,

186
EXTREMES IN
OU
TDO
OR TEM
PERATURE A
ND
BIRTHW
EIGH
T
10
temperature and sunshine).7 Effects were studied separately by trimester. Analogous to
our findings, they report a 2% significantly increased risk of SGA by higher temperatures
sustained over pregnancy; this risk for lower birthweight was particularly observed for
exposition during the third trimester. The main differences compared to our study include
the use of only maximum temperature, exposure data from just two temperature stations,
and the inclusion of births from 33 weeks of gestational age, leading to incomplete exposure
windows for the third trimester.7
Although an inverse relation of heat stress on birthweight has been observed in several
studies7,9,15, the opposite (i.e., heat stress causing increased birthweight) has also been
demonstrated.8,9 Probably due to heterogeneity in study design, most of these studies
did not find consistent directions of effect measures for all exposure windows, e.g., one
study found a negative effect of first trimester temperature exposure on birthweight
(beta coefficient -5.4, 95% CI -7.9;-2.9), and a positive effect of third trimester temperature
exposure on birthweight (beta coefficient 1.3, 95% CI 0.5-2.1).9
Animal studies provide a biological explanation for part of our findings as they show
heat stress during pregnancy to be associated with reduced placental weight, decreased
uterine and umbilical blood flow and consequent reduction in offspring birthweight.16
Galan et al. exposed pregnant ewes to heat stress during pregnancy for 55 days (mean
birthweight 1,841 grams) and 80 days (mean birthweight 882 grams).17 They observed a
significant reduction in fetal and placental weights compared with a control group (mean
birthweight 3,391 grams).17 In terms of the ‘fetal origins of adult disease’ hypothesis5, our
findings, combined with findings from these animal studies may demonstrate some form
of adaptation mechanism regarding the expected outdoor climate after birth.
Possible mechanisms
Several theories exist on the background of our observed results. According to one, fetal
growth is influenced by the rate of uteroplacental blood flow. Extremes of temperature, in
particular heat, are known to affect human blood flow with excess cardiovascular deaths
occurring in heat waves.11 It is therefore plausible that maternal blood flow and, hence,
fetal nutrition will be affected by these extremes in different stages of pregnancy. It is also
possible that outdoor temperature during pregnancy or seasonality is linked to maternal
behaviours including smoking, diet and physical activity. In particular smoking may have
contributed to the summer decrease in birthweight as it has a profound negative effect on
birthweight, and tobacco consumption in general has been shown to peak in summer.18,19

187
EXTREMES IN
OU
TDO
OR TEM
PERATURE A
ND
BIRTHW
EIGH
T
10
Inherent to sunshine, vitamin D has also been mentioned as a possible causal factor. Its
production depends primarily on the action of sunlight on the skin, and therefore, it is
strongly associated with the duration of sunshine.12,20 A 2010 Dutch study found women
with deficient vitamin D levels in early pregnancy (median 13 weeks’ gestation) to be at
increased risk for an infant with lower birthweight (-114.4 gram, 95% CI -151.2;-77.6) and
SGA.20 Vitamin D deficiency is more prevalent during the winter months. Women with the
end of first trimester in winter will deliver during late spring and summer, and, according
to this hypothesis, will have lower birthweight children as demonstrated in our results.
Strengths and limitations
An important strength of our study is the usage of a validated national database (The
Netherlands Perinatal Registry) with an almost complete coverage of all pregnancies over
a long period of time (2000-2008), and detailed climatological data from a nationwide
network of 29 temperature stations, increasing the precision and generalisability of our
results. Additionally, in comparison with previous studies, our study model included an
individual exposition model covering the whole duration of pregnancy including the
periconceptional period.3,6-10 Other strengths include the use of sunshine exposure, as most
studies do not include this in their model, and the adjustment for socioeconomic status.
The latter is important because in current times it is relatively easy to keep a home and a
person in a temperate ambient, but this is less likely the case if socioeconomic status is low
and housing quality is poor.
One of the study limitations, similar to most previous studies, is that outdoor temperature
does not reflect the true exposition as a significant amount of time is spent indoors,
especially at time of extreme temperatures. Another potential source of error is a person’s
mobility as climatological data linked to a person’s zip code of residence may compromise
the exposure estimate. Inaccuracy resulting from the first underestimates the individual
exposure to temperature extremes with underestimation of the true peak temperature
effect. The second inaccuracy may yield an under- or overestimation on the individual
level without obvious systematic effect in general. Despite this error and the generally
temperate Dutch climate, a consistent effect remains. A last limitation is the lack of data
on maternal lifestyle factors, in particular smoking. However, by excluding preterm births
and taking into account socioeconomic status, both strongly related to maternal smoking,
we attempted to minimise the effects of this limitation.

188
EXTREMES IN
OU
TDO
OR TEM
PERATURE A
ND
BIRTHW
EIGH
T
10
Implications
Climatological factors impact birthweight on the individual level, the effect of which
emerges as regional differences in birthweight on the population level. For healthy babies
born at term the demonstrated differences appear small and effects on health later in life
are unlikely. More detrimental effects may emerge for vulnerable subgroups (e.g., women
carrying growth restricted babies) implying future research in these groups. The birthweight
effects on the population level may be also more sizeable in countries where the population
is truly exposed to extremes.
The World Health Organization recommends an indoor temperature of 18 degrees Celsius,
or 21 degrees Celsius for vulnerable people21; as it is impossible to change the climate,
improving housing quality to moderate exposure to extremes in temperature appears a
realistic implication for vulnerable subgroups.
Conclusion
Birthweight is associated with the combined effect of season and exposure to temperature
extremes and cumulative exposure to sunshine, in particular during critical reproductive
exposure windows in pregnancy. The effect of seasonality appears to be mediated by
interacting effects of temperature and sunshine, resulting in an almost average 20 gram
significantly decreased birthweight in summer compared to January. On the population
level, significant regional differences in birthweight exist, most likely attributable to
particularly maximum temperatures, with moderation of the effect in coastal areas. For
healthy babies born at term these differences in birthweight appear small; however, more
severe detrimental effects may emerge for vulnerable subgroups, e.g., women carrying
growth restricted babies.

189
EXTREMES IN
OU
TDO
OR TEM
PERATURE A
ND
BIRTHW
EIGH
T
10
1. Hippocrates. Airs, waters, places. In: Lloyd G, ed. Hippocratic writings. London: Penguin books; 1978:148-169.
2. Bhaskaran K, Armstrong B, Hajat S, Haines A, Wilkinson P, Smeeth L. Heat and risk of myocardial infarction: hourly level case-crossover analysis of MINAP database. BMJ. 2012;345:e8050.
3. Seretakis D, Lagiou P, Lipworth L, Signorello LB, Rothman KJ, Trichopoulos D. Changing seasonality of mortality from coronary heart disease. JAMA. 1997;278:1012-1014.
4. Lambert GW, Reid C, Kaye DM, Jennings GL, Esler MD. Effect of sunlight and season on serotonin turnover in the brain. Lancet. 2002;360:1840-1842.
5. Barker DJ. Adult consequences of fetal growth restriction. Clin Obstet Gynecol. 2006;49:270-283.
6. Strand LB, Barnett AG, Tong S. The influence of season and ambient temperature on birth out-comes: a review of the epidemiological literature. Environ Res. 2011;111:451-462.
7. Pereira G, Cook A, Haggar F, Bower C, Nassar N. Seasonal variation in fetal growth: accounting for sociodemographic, biological, and environmental exposures. Am J Obstet Gynecol. 2012;206:74 e71-77.
8. Murray LJ, O’Reilly DP, Betts N, Patterson CC, Davey Smith G, Evans AE. Season and outdoor ambient temperature: effects on birth weight. Obstet Gynecol. 2000;96:689-695.
9. Lawlor DA, Leon DA, Davey Smith G. The associa-tion of ambient outdoor temperature throughout pregnancy and offspring birthweight: findings from the Aberdeen Children of the 1950s cohort. BJOG. 2005;112:647-657.
10. Torche F, Corvalan A. Seasonality of birth weight in Chile: environmental and socioeconomic factors. Ann Epidemiol. 2010;20:818-826.
11. Huynen MMTE, Martens P, Schram D, Weijenberg MP, Kunst AE. The impact of heat waves and cold spells on mortality rates in the Dutch population. Environ Health Persp. 2001;109:463-470.
12. Urrutia RP, Thorp JM. Vitamin D in pregnancy: current concepts. Curr Opin Obstet Gynecol. 24: 57-64.
13. Wilcox AJ. Fertility and pregnancy: an epidemio-logic perspective. New York: Oxford University Press; 2010.
14. Perinatal care in The Netherlands 2008 (in Dutch: Perinatale zorg in Nederland 2008). Utrecht: The Netherlands Perinatal Registry; 2011.
15. Wells JC, Cole TJ. Birth weight and environmental heat load: a between-population analysis. Am J Phys Anthropol. 2002;119:276-282.
16. Wells JC. Thermal environment and human birth weight. J Theor Biol. 2002;214:413-425.
17. Galan HL, Hussey MJ, Barbera A, et al. Relationship of fetal growth to duration of heat stress in an ovine model of placental insufficiency. Am J Obstet Gynecol. 1999;180:1278-1282.
18. Andres RL, Day MC. Perinatal complications associated with maternal tobacco use. Semin Neonatol. 2000;5:231-241.
19. Warren CW, Erguder T, Lee J, et al. Effect of policy changes on cigarette sales: the case of Turkey. Eur J Public Health. 2012;22:712-716.
20. Leffelaar ER, Vrijkotte TG, van Eijsden M. Maternal early pregnancy vitamin D status in relation to fetal and neonatal growth: results of the multi-ethnic Amsterdam Born Children and their Development cohort. Br J Nutr.;104:108-117.
21. Health impact of low indoor temperatures: Report on a WHO meeting. Copenhagen: World Health Organization; 1985.
REFERENCES

190
EXTREMES IN
OU
TDO
OR TEM
PERATURE A
ND
BIRTHW
EIGH
T
10

11General discussion

192
GEN
ERAL D
ISCUSSIO
N
11
AIM OF THIS THESISThe aim of this thesis was to investigate the main contributing factors in adverse perinatal
outcomes on the three geographic levels (international, national, regional). The role of
patient, environmental, and healthcare related factors was studied, in particular their
relative importance. Such information may guide to select and to prioritise among policies
to decrease gaps in perinatal health.
Our results are presented in two parts. Part I contains three studies from the regional ‘Ready
for a Baby’ programme; part II contains six studies on the national level, either ordered
by ‘ZonMw’ (The Netherlands Organisation for Health Research and Development), ‘SAZ’
hospitals (a co-operative institution of about 40 small general hospitals in The Netherlands),
or the Ministry of Health, Welfare and Sport. All studies draw on data from The Netherlands
Perinatal Registry.
PRINCIPAL FINDINGS
Part I
We demonstrated that large differences exist in absolute perinatal mortality and morbidity
rates between neighbourhoods within the city of Rotterdam (chapter 2). The magnitude
of these inner-city inequalities in perinatal health had not been previously described in
developed countries. The inequalities were somewhat reduced by accounting for socio-
demographic population differences (‘standardisation’ for maternal age, parity, ethnicity,
neighbourhood social quality) between the Rotterdam boroughs, yet substantial differences
remained (chapter 3). The municipal report on perinatal health as described in chapter
3 shows how such an analysis allows to differentiate between patterns of possible causes
per borough, implying the necessity of different policy measures per borough. We believe
that the mechanisms in deprived neighbourhoods work through the accumulation of
heterogeneous risks (maternal, child, organisational, environmental). These risks are more
abundant in these neighbourhoods and underlie the generally high level of adverse
pregnancy outcomes.1
Another important factor influencing urban perinatal health is social deprivation (chapter
4). Deprivation points both to the above described higher risk level, and the lack of
personal and family resources to counter ill-health. We demonstrated differential effects
of social deprivation on Western and non-Western women in the city of Rotterdam. Better

193
GEN
ERAL D
ISCUSSIO
N
11
neighbourhood social quality (expressed in the Social Index) was clearly associated with
better perinatal outcomes for Western women. This trend was absent for non-Western
women as they showed small changes in prevalence of adverse pregnancy outcome with
better neighbourhood social quality. Policy recommendations in this context may refer
to (1) risk management and intensified care, and (2) empowerment, improving resources
and care access. For Western women, the latter is more important as our results show
that improved social quality is associated with perinatal outcome improvement in this
group. While this may also benefit non-Western women, tailored change requires better
understanding of the underlying patterns first. Suggested explanations for non-Western
‘migrant’ groups include the presence of ‘protective’ effects through knowledge systems
(‘resource availability’) or intrinsic resilience (‘high risk level’).2-4 The suggestion of knowledge
systems follows from the so-called ‘ethnic density’ hypothesis which suggests the risk of poor
health outcomes for a minority individual to be inversely related to the density of his or her
racial/ethnic group in the local community.5-8 The presumed mechanisms include health
protection through increased participation in social networks or knowledge systems, and a
more extensive repertoire of positive coping behaviours.5-9 Additional etiological research
in this multi-ethnic urban setting is mandatory. Possibly, risk assessment tools and social
measures such as the Social Index capture features through a ‘Western perspective’, e.g.,
rather than household income greater family income may be a more important measure
for non-Western groups.
Part II
The population attributable risks (PAR10) of maternal, child and organisational risk factors for
perinatal mortality are demonstrated in chapter 5. Adapting a new multivariable method
to compute PARs, the results showed to vary according to methodological choices. For
example, a PAR of maternal factors can be estimated with and without taking into account
the PAR of child and organisational factors. Maternal factors, long put forward as a crucial
determinant for the national perinatal mortality rate11-13, appeared to attribute to only 1.4%
to 13.1% of perinatal mortality in a multivariate context. PARs of child and organisational
factors were 58.7-74.0% and 7.3-34.3%, respectively, where the range reflects different
priority (for that factor) in the adjustment procedure. Focusing on the role of hospital organi-
sation factors, the PAR results suggest that a change towards the theoretical organisation
optimum, with an otherwise unchanged pregnant population, provides a 34.3% decrease
of in-hospital perinatal mortality.

194
GEN
ERAL D
ISCUSSIO
N
11
The highest PAR for a single risk factor was observed for gestational age (72.2%), i.e., if all
women would deliver at 40 weeks of gestational age - all other things equal - , the perinatal
mortality is expected to be reduced with 72.2%. Moreover, being born at 37-37.6 weeks
of gestation (considered at term) reflects a 200% increased risk for perinatal mortality
(compared to 40 weeks), which questions the definition of ‘term pregnancy’ and suggests
a change of the lower threshold from 37 weeks to 38 weeks of gestation.14,15
Results from the PAR study are in support of policy measures aimed at (1) improving organi-
sational factors in obstetric healthcare16-19, and (2) improved prevention of preterm birth.
Next to targeting specific risk factors, also regional policy measures may be implemented
to improve perinatal health. Chapter 6 reported on epidemiological methods to select
priority regions in which to study the implementation of intensified preconception care
and uniformal antenatal risk selection for the ‘Healthy Pregnancy 4 All’ project. Crude as
well as standardised rates are used in this selection process. Depending on the goal of the
intervention, i.e., improvement of preconception care or antenatal risk selection, different
indicators are needed to prioritise among regions. These indicators are related to perinatal
mortality, morbidity and healthcare factors. Both strategies of selection point out the four
largest cities (‘G4’, i.e., Amsterdam, Rotterdam, The Hague, Utrecht) as a priority region,
thus, illustrating the multifactorial effects on and the complexity of urban perinatal health.
Chapters 7, 8 and 9 address the unique Dutch system of obstetric care. This system is
characterised by three risk-based levels of care.20,21 Primary care for assumed low risk
pregnancies is provided by independently practicing community midwives. Assumed low
risk pregnant women can either opt for a home birth or a short-stay hospital birth under
supervision of a community midwife.20,21 Secondary/tertiary care for assumed high risk
pregnancies is provided by obstetricians in hospitals. Whenever risk factors of adverse
perinatal or maternal outcome are present before pregnancy or arise during pregnancy
or parturition, women shift from low risk to high risk and are referred to secondary care
or from secondary to tertiary care, also during parturition. This ongoing risk assessment
during pregnancy and during parturition is called ‘risk selection’, an essential quality of
care indicator of the Dutch obstetric care system.20-22 Risk selection in the Netherlands is
the exclusive responsibility of primary care community midwives.22 In formal terms, the
aim of risk selection is to identify and refer high risk pregnancies from an undifferentiated
group at onset of pregnancy, in order to obtain a true low risk group of pregnant women
(expressed as high negative predictive value of risk selection) for delivery in the primary
care setting.20,21

195
GEN
ERAL D
ISCUSSIO
N
11
Indications for referral and definitions of high and low risk pregnancy are listed in the ‘List of
Obstetric Indications’ (in Dutch: Verloskundige Indicatie Lijst).20,22 These indications, however,
are not fully registered as such in The Netherlands Perinatal Registry, and not always defined
unequivocally. For our analysis of risk selection effectiveness we therefore defined a high
risk pregnancy based on the presence of a ‘Big4’ morbidity.23
Our study showed that current risk selection does not result in a true low risk population
in primary care at the end of pregnancy. Furthermore, a considerable part of high risk
women is referred during parturition (chapter 7). Several mechanisms may be responsible
for suboptimal risk selection. First, primary care community midwives are oriented towards
low risk pregnancies. This ‘risk experience’ may cause high risk women not being detected
as such in primary care. By a similar mechanism low risk women who might deliver under
a midwife’s supervision may not always be detected in secondary/tertiary care. Second,
the availability of tools to detect high risk pregnancies in primary care may also play a role,
e.g., standardised checklist-based risk screen methods in the first trimester or ultrasound
examination in the second and third trimester. Standardised checklist-based antenatal risk
selection is currently evaluated in a national public health programme: ‘Health Pregnancy 4
All’ (HP4All).24 The instrument being used, the ‘R4U’ (Rotterdam Reproductive Risk Reduction),
screens on medical as well as social risk factors for adverse perinatal outcome.24
Financial incentives are a third mechanism which may influence risk selection effectiveness.
Assigning a high risk level implies referral, which directly affects professional income.
For example, midwives receive the full fee for delivery care, independent of the duration
of labour. If the patient is referred just after (artificial) rupture of membranes, this does
not affect the fee. Similarly, no surplus is provided in time consuming deliveries. This
incentive promotes a policy in which pregnant women stay under care of the primary care
community midwife until just after the start of delivery. Similarly, gynaecologists receive a
fee independent from the stage of delivery. The two aforementioned incentives together
may be responsible for high referral rates during parturition.
We believe that a successful effort in increasing risk selection effectiveness depends on
optimal collaboration between midwives and obstetricians with a joint responsibility for
the determination of a woman’s risk status, i.e., ‘shared care’. Shared obstetric care has
already been implemented in some form in other Western countries such as Australia and
the United Kingdom.25-27 One study demonstrated a 27% increase in the detection rate of
intrauterine growth restriction for women receiving shared obstetric care as opposed to
conventional obstetric care.28

196
GEN
ERAL D
ISCUSSIO
N
11
Chapter 8 addresses the safety of home birth. Under routine conditions, home birth is
generally not associated with increased intrapartum and early neonatal mortality. The
mortality risk of home birth compared to planned hospital birth in low risk pregnancies is
non-significantly increased (OR 1.05, 95% CI 0.91–1.21). In subgroups, additional risk cannot
be excluded. Moreover, a recent report, which presents an overview of evidence concerning
safety of home birth, advocates hospital based delivery for all women. The evidence in their
view supports professional responsibility to be more important than a consumer’s choice,
i.e., the home birth option for low risk women.29
In this thesis we frame the policy choice involving the home birth option along two key
questions. The first is whether risk selection is adequate, i.e., is the group starting delivery
under a midwife’s supervision truly a low risk group of women, who consequently can
be offered the choice to deliver at home? A 6% prevalence of perinatal morbidities in
home births - even after referral of high risks during parturition and pregnancy - suggests
a negative reply to this answer (chapter 7). The second question refers to the outcome
difference in the home environment vs. in the hospital environment in unanticipated
perinatal morbidities. We assume that neonates with morbidities are likely to benefit from
being in the hospital setting at onset, as this decreases delay in specialised care provision.30,31
In-hospital midwife-led birth centres provide a possible alternative to provide a home-like
environment during delivery without delay if referral to the hospital is deemed necessary.32
While home birth perhaps may be considered for a group of selected low risk multiparous
women, one can argue that all primiparous women should deliver in an in-hospital
environment, either under supervision of the midwife (birth centre) or a gynaecologist.29,33
The study in chapter 9 was set up because of current policy proposals in favour of cen-
tralisation acute obstetric care. The goal of centralisation is to ensure 7*24h availability of
‘qualified professionals’ (midwives, gynaecologists, paediatricians, anaesthesiologists, and
operating theatre staff; ‘qualified’ in terms of seniority) within 15 minutes.16,34
Centralisation is also under consideration in other countries.17-19 Recently, the Royal Col-
lege of Obstetricians and Gynaecologists (RCOG) stated in their ‘Working Party Report’ it
is adamant that obstetric care delivery has qualified specialists available at all times, 24
hours a day, 7 days a week as more than half of all births, after all, take place ‘out of hours’.17
However, also taking into account the possible drawbacks of centralisation they caution
this recommendation by stating ‘localised where possible, centralised where necessary’.17
The main reasons mentioned in the literature in favour of centralisation are: (1) better
care and access to rapid intervention during delivery, resuscitation of the newborn, and

197
GEN
ERAL D
ISCUSSIO
N
11
identification and management of newborn infants with unexpected morbidities (e.g.,
congenital anomalies) in large and higher level hospitals.35 However, this ‘bigger-is-better’
mantra is mainly based on theoretical reasoning, and empirical evidence from centralisation
studies in the context of (complex) surgical procedures.36 Moreover, in the context of
acute obstetric care, evidence-based data are scarce, and most studies on this subject are
ecological or of a descriptive nature, heterogeneous in design and have contradictory
results.18,19,35,37,38 One important argument against centralisation is increased travel time
to hospital, with inherent increased risk for adverse perinatal outcome (especially for high
risk women) or out-of-hospital delivery.39 Furthermore, as around 20% of births in The
Netherlands still occur at home under supervision of a midwife40, increased travel time to
hospital will compromise some low risk women in their choice to opt for a birth at home.
Finally, centralisation of acute obstetric care fits into a broader change of Dutch hospitals
towards merging, strongly advocated by health insurance companies who prefer larger
institutions for management reasons.
We provided an empirical framework to study the effects of centralisation of acute obstetric
care (chapter 9). Two hypothetical centralisation scenarios are defined, both representing
fairly small changes affecting 6-7% of patients: (1) closure of the 10 smallest hospitals,
and (2) closure of the 10 smallest hospitals, but avoiding adjacent closures. As only 10
small hospitals were hypothetically closed we assumed no system effects. Our results
demonstrated that closing the small hospitals (scenario 1 and 2) does not necessarily result
in distinct better outcomes on the population level. Outcome strongly depended on the
organisational features of the hospital receiving the patients from the closed hospitals.41
Multiple factors have to be taken into account regarding centralisation of acute obstetric
care, e.g., the organisational features of the closing hospital, the characteristics of the
women ‘shifting’ to the next nearest hospital (are they low risk or high risk), the quality of
risk selection (are there many ‘unexpected’ high risk women who need to be transferred);
thus, also additional travel time is an essential feature. Moreover, short term and long term
economic aspects of centralisation and ‘side’ effects on paediatric and anaesthesiology
services also need to be evaluated.
In line with the results from chapter 5, showing a 30% decrease in perinatal mortality to
be expected from optimising hospital organisational factors alone, we think centralisation,
on average, to be effective in improving perinatal health. However, centralisation should
be carried out bearing (organisational) information on the specific hospitals in mind. In
particular rural regions may not benefit at all from centralisation. We therefore support the
RCOG’s statement ‘localised where possible, centralised where necessary’.17

198
GEN
ERAL D
ISCUSSIO
N
11
In chapter 10 we studied the effect of climatological factors, i.e., seasonality, extremes
in temperature and cumulative sunshine exposure, on birthweight. For this purpose we
specified an elaborate exposition model taking into account the whole course of pregnancy
from conception to birth. Our aim was to identify critical phases and the type of exposure
to demonstrate the strongest effects on birthweight.
We found all measures of exposure to be significantly associated with birthweight, where
the modest effects of season alone hided interacting effects of temperature and sunshine.
In a multivariable context, we found minimum temperature exposure in the second and
third trimester to be associated with higher birthweight, maximum temperature exposure
for all exposure windows to be associated with lower birthweight, and cumulative sunshine
exposure to be associated with higher birthweight. The greatest single effect was observed
for seasonality, in particular after correction for temperature and sunshine effects. Unlike
most previous studies42, we demonstrated a regular seasonal pattern after this correction,
resulting in a spring/summer nadir with an almost 20 gram significantly decreased
birthweight in summer. Our results partially correspond with results from animal studies
in which maximum temperature exposures are consistently significantly associated with
lower birthweight.43,44
On the population level and combining all seasons, we demonstrated significant regional
differences in birthweight, attributable to the studied measures of minimum and maximum
temperature, and cumulative sunshine exposure. Maximum temperatures appear to
attribute most to these regional effects, with moderation in coastal areas. For healthy babies
born at term these differences appear small; however, more severe detrimental effects may
emerge for vulnerable subgroups, e.g., women carrying growth restricted babies. Regarding
the effect of climatologic factors on birthweight, the population level is too small to expect
a contribution to the national problem of increased perinatal mortality.
METHODOLOGICAL ISSUES
The Netherlands Perinatal Registry
In all studies described in this thesis data from The Netherlands Perinatal Registry are used.
This medical registry contains complete population-based information of >97% of all
pregnancies in The Netherlands.40 Source data are routinely collected by 94% of midwives,
99% of gynaecologists and 68% of paediatricians including 100% of Neonatal Intensive Care
Unit paediatricians.40 (See website for detailed description: www.perinatreg.nl).

199
GEN
ERAL D
ISCUSSIO
N
11
In general, medical registries such as The Netherlands Perinatal Registry try to capture
particular actions in healthcare systems (e.g., admissions, billing, drug prescriptions), while
research registries usually try to capture details on one specific disease or research question.
The use of medical registries for research purposes may be challenged by the limited amount
and the quality of the information. Quality concerns include the classification of the health
outcome, the limited amount of detailed clinical information (e.g., existing health status
of the patient), the limited amount of information on events occurring before the health
event (e.g., information on past exposures) and information on events after the health
event (e.g., follow-up information).45
While useful for the studies described in this thesis, The Netherlands Perinatal Registry’s
quality is challenged in different ways. Health events and disease states are not always
clearly classified, e.g., presence of pre-eclampsia. Its quality is also challenged by the limited
amount of information before and after birth (the health event), on former pregnancies,
on risk factors (such as smoking, educational level, etc.), on process information of hospital
admission and referrals (e.g., indication for referral and treatment in such cases). Secondly,
about 70% of the paediatricians and 100% of NICU paediatricians participate. While the
percentage of participating paediatricians is increasing, partial and selective participation
challenges completeness of short term neonatal outcome. Thirdly, the registry does
not contain long term follow up outcome of newborns. This information is registered
separately by, e.g., care providers in youth healthcare. While these shortcomings may be
true in general, our studies primarily suffer from the unavailability of detailed information
on former pregnancies and risk factors, since these may lead to residual confounding. To
some extent they also suffer from missing data on referrals and hospital admissions, since
these may provide insight in the possible underlying mechanisms of adverse outcome. Most
importantly, the legal environment and user costs should be evaluated to ensure access
to and continuing improvement of The Netherlands Perinatal Registry as our studies show
the value of this registry for our research purposes.
Adjustment techniques
In the observational context of the studies presented in this thesis different adjustment
techniques are indispensible. We used multivariable regression techniques and (direct)
standardisation techniques.46-49 Advantages of direct and indirect standardisation include
computational simplicity, and relatively fewer statistical assumptions. Standardisation can
be regarded as the preferred adjustment technique if one is more interested in the overall

200
GEN
ERAL D
ISCUSSIO
N
11
effect instead of the influence of separate determinants.46-48 Moreover, standardisation
requires a researcher’s selection of adjustment variables prior to outcome analysis, which
forces thought and plausible rationale from the researcher. In our research, standardised
rates provided useful summary measures, especially when outcomes are rare and specific
rates display wide random variability. However, any summary measure can hide patterns
that might have important public health implications. Standardisation rates put more
emphasis on less prevalent groups.46-48
Adjustment by regression (forced entry of adjusters), is more convenient for statistical tests
for interactions and group differences (the individual effect of different determinants).
Therefore, when many determinants are present, adjustment by means of multivariable
regression analysis is more convenient.47-49 However, when applying this technique more
statistical assumptions have to be made (particularly when continuous variables are used),
such as linear correlation of adjustment variables with outcome effects, equal effects
for everyone, and all combinations of parameters being possible (including biological
implausible combinations).47-49 Moreover, in regression adjustment variables are less
restricted as they can be, e.g., nominal, ordinal or interval variables; adjustment variables in
standardisation, however, require strata to be created. Adjusted rates in regression are based
on the most prevalent groups. Also, regression can either require a researcher’s selection of
adjustment variables (forced entry) or this can be determined statistically (stepwise) which
may compromise plausibility.
In chapters 4, 5, and 9 we use multilevel modelling to adjust for clustering of individuals
within their neighbourhoods (chapter 4) or hospitals (chapters 5, 9). The advantage of this
approach is that it allows for the incorporation of both individual-level and neighbourhood-
level or hospital-level characteristics. Moreover, it increases the validity of the effect sizes
compared to conventional logistic regression analysis.50 In chapter 9 we observed great
variation in random effects per hospital suggesting differences in hospital performance in
terms of perinatal mortality.
Due to lacking information in The Netherlands Perinatal Registry, in particular individual-
level socioeconomic status, we, however, could not fully benefit from the theoretical
advantages of multilevel modelling over conventional logistic regression.
‘Big4’ morbidities
From detailed analysis of the complete perinatal dataset of The Netherlands Perinatal
Registry, it appeared that the presence of a so-called ‘Big4’ morbidity precedes perinatal

201
GEN
ERAL D
ISCUSSIO
N
11
mortality in 85% of cases.23 These ‘Big4’ morbidities are: congenital anomalies, preterm
birth, small for gestational age, and low Apgar score. Risk status of pregnancies could be
insufficiently established due to lacking data in The Netherlands Perinatal Registry, especially
due to lacking registration of referral indications. Due to their attribution to perinatal
mortality, we used the presence of one or more ‘Big4’ morbidities as a proxy measure of
high risk pregnancy in several studies in this thesis.
A limitation from this proxy measure may refer to ‘preventability’. From this retrospective
dataset no conclusions can be drawn on the preventability of ‘Big4’ morbidities in primary
care would they have been referred to secondary/tertiary care. However, congenital
anomalies and SGA are the most predictable in the antenatal phase. Most congenital
anomalies are now detected by routine ultrasound (introduced in 2007) at 20 weeks of
gestational age. Furthermore, there is general consensus on (improving) detection of SGA
which holds an increased risk for adverse perinatal outcome.51
Most important, however, is that, again, both general consensus and the ‘List of Obstetric
Interventions’ agree that a neonate with a ‘Big4’ morbidity is better off in a hospital setting
under the care of an obstetrician/paediatrician.52 Thus, the more important issue concerns
the adequate level of care for a high risk pregnancy (optimal risk selection) and not the
preventability of ‘Big4’. Recent Dutch reports have expressed concerns on the effectiveness
of risk selection in Dutch primary obstetric care.23,30,31 Results from these studies emphasise
that the level of healthcare provision is inadequate for a proportion of supposedly low
risk pregnant women at the onset of labour. Whether the delay in referral is related to late
diagnosis (no continuous fetal heart rate monitoring during parturition in primary care),
transport to hospital or assessment (‘primary care is supposedly low risk’), is yet unclear
and needs to be additionally studied.30,31
RECOMMENDATIONSFrom the above discussion the following recommendations can be given.
Recommendations Part I
• Within the city of Rotterdam, neighbourhood and borough-specific policies are mandatory
on tackling the high degree of perinatal health inequalities between neighbourhoods
and boroughs. These recommendations most likely will extend to other large cities.

202
GEN
ERAL D
ISCUSSIO
N
11
• In particular Western women in socially deprived neighbourhoods are entitled to
intensified antenatal care. This approach could include intensified prevention from
existing health promoting programs in combination with targeted social welfare. Also,
risk assessment should be modernised, regarding both the tools used for antenatal risk
screening and the approach of risks detected (‘shared care’). To enhance sustainability of
the joint responsibility of both obstetric and social caregivers in high risk pregnancies, a
combined financial remuneration system with adequate incentives should be advocated.
• Additional research is needed on (1) the differential effects of deprivation on Western
and non-Western pregnant women, (2) the risk accumulation phenomenon, and (3)
the consequences of adverse pregnancy outcomes in childhood. Concerning (1), the
sources of differential effects are important for tailored improvement programmes.
Concerning (2), the generalisability of the risk accumulation phenomenon is important
to support national antenatal screening instruments like the ‘R4U’ checklist. Concerning
(3), investigating long term consequences of adverse pregnancy outcomes is essential
in general, but more particular to check whether the same differential outcomes can be
observed (i.e., do the ethnicity related differential effects continue after birth). A remote
consequence of the research proposed under 1 to 3 could be different risk assessment
tools and strategies for different population strata.
• The financial remuneration structure should take into account the considerable regional
risk differences in the perinatal context; if regional budgeting is aimed at, adjusting for
maternal characteristics only is insufficient.
Recommendations Part II
• Improvement of hospital organisation deserves priority. Multiple factors appear
modifiable, e.g., 7*24h organisation including the timing of (planned) deliveries in a
fashion that problems most likely will emerge during daytime hours. Also, proactive
obstetric policy should be advocated, at least in the Dutch context. We expect policies
to already change towards a more proactive approach; however, no recent data are
available to substantiate this.
• Centralisation of acute obstetric care services should take local configuration and
measured hospital organisational features into account. Apart from the academic
perinatal centres, hospital size is not a decisive factor in this regard. Side effects of
centralisation may exceed the intended benefits.

203
GEN
ERAL D
ISCUSSIO
N
11
• Studies aimed at the prevention of preterm birth are expected to grossly affect perinatal
mortality. Rigorous anti-smoking policies combined with organisational and financial
support for active antenatal prevention are justified. Also, the ‘term’ threshold should
change from 37.0 to 38.0 weeks.
• In prioritising regions for public health interventions, crude and standardised outcome
both need to be made available.
• Home birth as an option should be restricted to low risk multiparous women, but is
only a sustained option if risk selection throughout pregnancy considerably improves.
General recommendations
• Risk factors should be detected in a consistent way (possibly through a standardised
checklist based approach) during antenatal risk selection preferably through a joint
effort by primary care community midwives and obstetricians.
• Mandatory information on lifestyle factors such as smoking should be incorporated in
detail in The Netherlands Perinatal Registry and the registration process.
• Data from medical and administrative registries should be conditionally made available
for research and care improving purposes, without prior individual consent, similar to,
e.g., the Nordic countries. Additionally, quality assurance should be a regular part, and
an intensive collaboration between registry authorities and hospitals and IT-stakeholders
for hospital administration systems is mandatory to respond to change.

204
GEN
ERAL D
ISCUSSIO
N
11
REFERENCES1. Timmermans S, Bonsel GJ, Steegers-Theunissen RP,
et al. Individual accumulation of heterogeneous risks explains perinatal inequalities within deprived neighbourhoods. Eur J Epidemiol. 2011; 26:165-80.
2. Burris HH, Collins JW, Jr. Race and preterm birth--the case for epigenetic inquiry. Ethn Dis. 2010 Summer;20:296-9.
3. Collins JW, Jr., David RJ, Rankin KM, Desireddi JR. Transgenerational effect of neighborhood pover-ty on low birth weight among African Americans in Cook County, Illinois. Am J Epidemiol. 2009 Mar 15;169(6):712-7.
4. Kramer MR, Hogue CR. What causes racial dispari-ties in very preterm birth? A biosocial perspective. Epidemiol Rev. 2009;31:84-98.
5. Fang J, Madhavan S, Bosworth W, Alderman MH. Residential segregation and mortality in New York City. Soc Sci Med. 1998 Aug;47:469-76.
6. Halpern D, Nazroo J. The ethnic density effect: results from a national community survey of England and Wales. Int J Soc Psychiatry. 2000 Spring;46:34-46.
7. Neeleman J, Wessely S. Ethnic minority suicide: a small area geographical study in south London. Psychol Med. 1999 Mar;29:429-36.
8. Rabkin JG. Ethnic density and psychiatric hos-pitalization: hazards of minority status. Am J Psychiatry. 1979 Dec;136:1562-6.
9. Grady SC. Racial disparities in low birthweight and the contribution of residential segregation: a multilevel analysis. Soc Sci Med. 2006 Dec;63: 3013-29.
10. Altman DG. Strategies for community health intervention: promises, paradoxes, pitfalls. Psy-chosom Med. 1995;57:226-33.
11. Buitendijk SE, Nijhuis JG. High perinatal mortality in the Netherlands compared to the rest of Europe. Ned Tijdschr Geneeskd. 2004;148:1855-60.
12. Mohangoo AD, Buitendijk SE, Hukkelhoven CW, et al. Higher perinatal mortality in The Netherlands than in other European countries: the Peristat-II study. Ned Tijdschr Geneeskd. 2008;152:2718-27.
13. Sheldon T. Perinatal mortality in Netherlands third worst in Europe. BMJ. 2008;337:a3118.
14. Fleischman AR, Oinuma M, Clark SL. Rethinking the definition of “term pregnancy”. Obstet Gy-necol. 2010;116:136-9.
15. Reddy UM, Bettegowda VR, Dias T, Yamada-Kushnir T, Ko CW, Willinger M. Term pregnancy: a period of heterogeneous risk for infant mortality. Obstet Gynecol. 2011;117:1279-87.
16. Sheldon T. Prompt access to expert care is among advice to reduce perinatal deaths in Netherlands. BMJ. 2010;340:c277.
17. Tomorrow’s specialist: working party report, September 2012. London: The Royal College of Obstetricians and Gynaecologists; 2012. (Online http://www.rcog.org.uk/files/rcog-corp/Tomor-row’s%20Specialist_FullReport.pdf ).
18. Heller G, Richardson DK, Schnell R, Misselwitz B, Kunzel W, Schmidt S. Are we regionalized enough? Early-neonatal deaths in low-risk births by the size of delivery units in Hesse, Germany 1990-1999. Int J Epidemiol. 2002;31:1061-8.
19. Hemminki E, Heino A, Gissler M. Should births be centralised in higher level hospitals? Experiences from regionalised health care in Finland. BJOG. 2011;118:1186-95.
20. Amelink-Verburg MP, Buitendijk SE. Pregnancy and labour in the Dutch maternity care system: what is normal? The role division between midwives and obstetricians. J Midwifery Womens Health. 2010;55:216-25.
21. Bais JMJ, Pel M. The basis of the Dutch obstetric system: risk selection. Eur Clinics Obstet Gynaecol. 2007;2:209-12.
22. Commisie Verloskunde CVZ. List Of Obstetric Indications (in Dutch: Verloskundig Vademecum) 2003. Diemen: 2003 (online http://www.knov.nl/docs/uploads/Verloskundig_Vademecum_2003.pdf).
23. Bonsel GJ, Birnie E, Denktas S, Poeran J, Steegers EAP. Dutch report: Lijnen in de Perinatale Sterfte, Signalementstudie Zwangerschap en Geboorte 2010. Rotterdam: Erasmus MC; 2010.

205
GEN
ERAL D
ISCUSSIO
N
11
24. Denktaş S, Waelput AJM, van Voorst S, et al. Healthy pregnancy 4 all: preconception care and risk selection during pregnancy (in Dutch: Precon-ceptiezorg en risicoselectie tijdens de zwanger-schap). Tijdschrift voor gezondheidswetenschap-pen. 2012;90:479-83.
25. Halliday J. WUDWAW ‘Who Usually Delivers Whom and Where’, Perinatal Data Collection Unit. Victoria, Australia: Victorian Government Department of Human Services; 1999.
26. Hampson JP, Roberts RI, Morgan DA. Shared care: a review of the literature. Fam Pract. 1996;13:264-79.
27. Tucker J, Florey CD, Howie P, McIlwaine G, Hall M. Is antenatal care apportioned according to obstetric risk? The Scottish antenatal care study. J Public Health Med. 1994;16:60-70.
28. Chan FY, Pun TC, Tse LY, Lai P, Ma HK. Shared antenatal care between family health services and hospital (consultant) services for low risk women. Asia Oceania J Obstet Gynaecol. 1993;19:291-8.
29. Chervenak FA, McCullough LB, Brent RL, Levene MI, Arabin B. Planned home birth: the professional responsibility response. Am J Obstet Gynecol. 2013;208:31-8.
30 . Evers AC, Brouwers HA, Hukkelhoven CW, et al. Perinatal mortality and severe morbidity in low and high risk term pregnancies in the Netherlands: prospective cohort study. BMJ. 2010;341:c5639.
31 . Evers AC, van Leeuwen J, Kwee A, et al. Mortality and morbidity among full-term neonates in a neonatal intensive care unit in the Utrecht region, the Netherlands. Ned Tijdschr Geneeskd. 2010;154:118.
32 . Gottvall K, Waldenstrom U, Tingstig C, Grunewald C. In-hospital birth center with the same medical guidelines as standard care: a comparative study of obstetric interventions and outcomes. Birth. 2011;38:120-8.
33 . de Neef T, Hukkelhoven CW, Franx A, van Ever-hardt E. Uit de lijn der verwachting. Nederl Tijdschrift Obstet Gynaecol 2009;122:34-342.
34 . Van der Velden J. Dutch report: Een goed begin. Veilige zorg rond zwangerschap en geboorte. Advies Stuurgroep Zwangerschap en Geboorte. The Hague: 2009.
35 . Moster D, Lie RT, Markestad T. Neonatal mortality rates in communities with small maternity units compared with those having larger maternity units. BJOG. 2001;108:904-9.
36 . Woo YL, Kyrgiou M, Bryant A, Everett T, Dickin-son HO. Centralisation of services for gynae-cological cancer. Cochrane Database Syst Rev. 2012;3:CD007945.
37 . Tracy SK, Sullivan E, Dahlen H, Black D, Wang YA, Tracy MB. Does size matter? A population-based study of birth in lower volume maternity hospitals for low risk women. BJOG. 2006;113:86-96.
38 . Phibbs CS, Bronstein JM, Buxton E, Phibbs RH. The effects of patient volume and level of care at the hospital of birth on neonatal mortality. JAMA. 1996;276:1054-9.
39 . Ravelli AC, Jager KJ, de Groot MH, et al. Travel time from home to hospital and adverse perinatal outcomes in women at term in the Netherlands. BJOG. 2011;118:457-65.
40 . Perinatal care in The Netherlands 2008 (in Dutch: Perinatale zorg in Nederland 2008). Utrecht: The Netherlands Perinatal Registry; 2011.
41 . Bonsel GJ, Poeran J, De Graaf JP, Borsboom GJJM, Birnie E, Steegers EAP, Mackenbach JP. Dutch report: Gevolgen van Concentratie van Perinatale Zorg. Rotterdam: Erasmus MC; 2012.
42 . Strand LB, Barnett AG, Tong S. The influence of season and ambient temperature on birth out-comes: a review of the epidemiological literature. Environ Res. 2011;111:451-62.
43 . Galan HL, Hussey MJ, Barbera A, et al. Relationship of fetal growth to duration of heat stress in an ovine model of placental insufficiency. Am J Obstet Gynecol. 1999;180(5):1278-82.
44 . Wells JC. Thermal environment and human birth weight. J Theor Biol. 2002;214(3):413-25.
45 . Reitsma JB. Registers in Cardiovascular Epide-miology. PhD thesis Academic Medical Center, University of Amsterdam ed; Amsterdam: 1999.
46 . Monson RR: Occupational Epidemiology. 2 edition. Boca Raton: CRC Press Inc; 1990, 72-74.
47 . Greenland S, Rothman KJ: Introduction to Cat-egorical Statistics in Modern Epidemiology. 2 edition. Philadelphia: Lippincott-Raven Publish-ers; 1998.

206
GEN
ERAL D
ISCUSSIO
N
11
48 . Bailit J, Garrett J. Comparison of risk-adjustment methodologies for cesarean delivery rates. Obstet Gynecol. 2003;102:45-51.
49 . Field A: Discovering Statistics Using SPSS. 3rd edition. London: Sage Publications; 2009.
50 . Twisk JWR. Applied Multilevel Analysis. 4 ed. Cambridge: Cambridge University Press; 2010.
51 . Figueras F, Gardosi J. Intrauterine growth restric-tion: new concepts in antenatal surveillance, di-agnosis, and management. Am J Obstet Gynecol. 2011 Apr;204:288-300.
52 . Commisie Verloskunde CVZ. List Of Obstetric Indications (in Dutch: Verloskundig Vademecum) 2003. Diemen: 2003 (online: http://www.knov.nl/docs/uploads/Verloskundig_Vademecum_2003.pdf).

12English and Dutch summary

208
12
ENG
LISH SU
MM
ARY
ENGLISH SUMMARYIn The Netherlands perinatal mortality rates exceed the European average. Also, within The
Netherlands inequalities in perinatal health are present, mainly in the four largest cities (‘G4’)
and deprived neighbourhoods. We state three levels of inequalities: (1) The Netherlands vs.
Europe, (2) regions and G4-cities vs. the remainder of The Netherlands, and (3) deprived vs.
non-deprived neighbourhoods and boroughs within these G4-cities. The causal factors for
perinatal inequalities may differ between the three geographic levels.
In response to the high perinatal mortality, the Dutch Minister for Health as well as the
municipality of Rotterdam issued several measures and research topics. This thesis reports
on local (PART I) and national (PART II) initiatives in the context of improving perinatal
health in The Netherlands. The aim is to investigate the main contributing factors in
adverse perinatal outcomes on the three geographic levels (international, national,
regional). Throughout this thesis, the concept of ‘Big4’ is applied. ‘Big4’ refers to four adverse
pregnancy outcomes (perinatal morbidities) which precede perinatal mortality in 85% of
cases: congenital anomalies, preterm birth (<37th week of gestation), small for gestational
age (SGA, birthweight below the 10th percentile for gestational age) or low Apgar score
(<7, 5 minutes after birth).
On the first geographic level, i.e., The Netherlands vs. Europe, the Dutch system of obstetric
care significantly differs from those in other Western countries, with a high percentage
of homebirths (around 20%), and an independent role for primary care community
midwives. Most important, however, is the risk-based level of care: primary care for low risk
pregnancies provided by independently practicing community midwives, and secondary/
tertiary care for high risk pregnancies provided by obstetricians in hospitals. Due to the
distinction between assumed low risk and high risk pregnancies, antenatal risk selection is
an essential indicator of the adequacy of the Dutch obstetric care system. We demonstrate
an insufficient separation of low risk pregnancies from a mix of low and high risk pregnancies
with a considerable part of this selection and subsequent referral taking place even during
parturition (chapter 7).
Home birth, as another unique feature, is generally not associated with increased intra-
partum and early neonatal mortality, under routine conditions (chapter 8). However, the
safety of home births is dependent on antenatal risk selection as only assumed low risk
women can be offered the choice of a birth at home. However, as antenatal risk selection
still results in 6% to 9% of high risk (‘Big4’) women in primary care, intended for low risk
pregnancies, improvement is mandatory (chapter 7).

209
12
ENG
LISH SU
MM
ARY
Chapters 5, 6, 9 and 10 pertain to perinatal health inequalities on the second geographic
level, i.e., regions and G4-cities vs. the remainder of the Netherlands. In chapter 5 we
demonstrate that an over 30% decrease in perinatal mortality is expected on the national
level through optimisation of (hospital) organisational features. This optimisation may be
achieved through centralisation of acute obstetric care services. However, hospitals appear
very heterogeneous in organisational features affecting perinatal outcome. Therefore, in
centralisation, these organisational features need to be taken into account as well as the
full scope of negatively (e.g., increased travel time) and positively (e.g., better 7*24h access
to specialised care) influencing factors (chapter 9). Due to the complexity of this matter
we agree with the statement from the Royal College of Obstetricians and Gynaecologists:
‘localised where possible, centralised where necessary’.
Chapter 6 reports on the selection of priority regions in which to implement intensified
preconception care and uniform antenatal risk selection. This selection was based on
indicators related to perinatal mortality, morbidity and healthcare factors. Both selecting
strategies (regarding to risk selection and preconception care) point out the four largest
cities (‘G4’, i.e., Amsterdam, Rotterdam, The Hague, Utrecht) as a priority region, thus
illustrating the increased risk for adverse perinatal outcome in large urban areas. G4-cities
surfacing in both selecting strategies emphasises the multifactorial effects on and the
complexity of urban perinatal health.
In chapter 10 we demonstrate the effect of climatological factors, i.e., seasonality, extremes
in temperature and cumulative sunshine exposure, on birthweight. Minimum tempera-
ture exposure in the second and third trimester was associated with higher birthweight,
maximum temperature exposure for all exposure windows was associated with lower
birthweight, and cumulative sunshine exposure was associated with higher birthweight.
On the population level, significant regional differences in birthweight exist, most likely
attributable to particularly maximum temperatures, with moderation of the effect in coastal
areas. For healthy babies born at term these differences in birthweight appear small; how-
ever, more severe detrimental effects may emerge for vulnerable subgroups, e.g., women
carrying growth restricted babies.
Chapters 2, 3 and 4 pertain to perinatal health inequalities on the third geographic level,
i.e., deprived vs. non-deprived neighbourhoods and boroughs within G4-cities, in particular
Rotterdam. We demonstrate large differences in absolute perinatal mortality and perinatal
morbidity rates between neighbourhoods within the city of Rotterdam with perinatal
mortality rates as high as 37 per 1,000 births (chapter 2). These inequalities remain after

210
12
ENG
LISH SU
MM
ARY
standardisation, also implying differences in possible causes per borough with subsequent
different policy measures per borough (chapter 3). Common mechanisms of adverse
perinatal outcome in deprived neighbourhoods are thought to be social deprivation and
accumulation of risks for perinatal mortality and morbidity. In chapter 4 we demonstrate
differential effects of social deprivation on Western and non-Western women in Rotterdam.
Improvement in neighbourhood social quality causes improvement in perinatal outcomes
for Western women only. Policy measures aimed at improving social quality for Western
women may improve outcome in Western women, however, alternative approaches may
be necessary for non-Western groups.
The most important recommendations for improvement of perinatal health on the first
geographic level include improvement of risk selection (possibly through a standardised
checklist based approach) and ‘shared care’ as the success of improvement strategies
depends on a joint collaboration of midwives and obstetricians. Important recommendations
on the second geographic level of perinatal health inequalities include a sensible policy
on centralisation of acute obstetric care and additional research and more public health
awareness for the complex issue of urban perinatal health. On the third geographic
level of perinatal health, we propose additional research on the differential effects of
social deprivation on Western and non-Western women. Our results imply strategies to
improve social quality for in particular for Western women and more focus on alternative
approaches for non-Western groups; these alternative approaches may be based on results
from additional research. Furthermore, neighbourhood, and borough specific policies are
mandatory on tackling urban perinatal health inequalities.

211
12
NED
ERLAN
DSE SA
MEN
VATTING
NEDERLANDSE SAMENVATTINGNederland kent een van de hoogste perinatale sterftecijfers in Europa met ook binnen
Nederland ongelijkheid in perinatale gezondheid waarbij de meest ongunstige uitkomsten
gezien worden in de vier grootste steden (G4: Amsterdam, Rotterdam, Den Haag, Utrecht) en
achterstandswijken. De ongelijkheid in perinatale gezondheid kan onderverdeeld worden
naar drie niveaus gebaseerd op geografie: (1) Nederland tegenover Europa, (2) de G4 en
regio’s binnen Nederland, en (3) achterstandswijken tegenover niet-achterstandswijken. De
oorzaken voor de ongelijkheid in perinatale gezondheid verschillen hoogstwaarschijnlijk
per niveau.
De hoge perinatale sterfte in Nederland werd zowel voor de landelijke als regionale poli-
tiek een prioriteit met voorstellen van de minister van Volksgezondheid en de gemeente
Rotterdam tot onderzoek en beleidsmaatregelen. Dit proefschrift rapporteert over regio-
nale (DEEL I) en landelijke initiatieven (DEEL II) ter verbetering van de perinatale sterfte in
Nederland. Hoofddoel van het proefschrift is dan ook de belangrijkste factoren te iden-
tificieren die bijdragen aan de slechte perinatale gezondheid in Nederland betreffende
de drie geografische niveaus (internationaal, nationaal, regionaal). Het concept van ‘Big4’
aandoeningen speelt een belangrijke rol in de stukken behorend bij dit proefschrift. ‘Big4’
staat voor de vier ongunstige zwangerschapsuitkomsten die voorafgaan aan 85% van alle
gevallen van perinatale sterfte: aangeboren afwijkingen, vroeggeboorte (vóór 37 weken
zwangerschap), te laag geboortegewicht voor de zwangerschapsduur (geboortegewicht
<p10), en een lage Apgarscore (<7, 5 minuten na de geboorte).
Voor de vergelijking op het eerste geografische niveau (Nederland tegenover de rest van
Europa) speelt het unieke systeem van verloskundige zorg in Nederland een belangrijke
rol; uniek in die zin dat, in vergelijking met andere Westerse landen, in Nederland een hoog
percentage van de zwangere vrouwen thuis bevalt (rond de 20%). Een ander verschil met
andere Westerse landen is de belangrijke rol van de eerstelijns verloskundige. Het belang-
rijkste verschil is echter het intrinsieke verschil tussen hoogrisico- en laagrisicozwanger-
schappen met daarbij behorende risicogeleide zorg in de verloskunde: eerstelijns zorg voor
laagrisicozwangerschappen verleend door verloskundigen, en tweede-/derdelijns zorg
voor hoogrisicozwangerschappen in ziekenhuizen verleend door gynaecologen. Door dit
onderscheid en de specifieke bijbehorende zorgconsequenties speelt antenatale risicose-
lectie een belangrijke rol in het Nederlandse systeem en kan dan ook gezien worden als
een belangrijke kwaliteitsindicator: ‘hoe goed worden laagrisico- en hoogrisicozwanger-
schappen van elkaar onderscheiden’. In dit proefchrift tonen wij aan dat deze twee groepen

212
12
NED
ERLAN
DSE SA
MEN
VATTING
suboptimaal kunnen worden onderscheiden van elkaar in de periode vóór de bevalling.
Daarnaast wordt ook een substantieel deel van de zwangere vrouwen gedurende de baring
aangeduid zijnde hoogrisico en daarop doorverwezen naar het ziekenhuis (hoofdstuk 7).
De thuisbevalling is een ander uniek kenmerk van het Nederlandse verloskundige systeem.
Onder normale omstandigheiden is deze niet geassocieerd met een verhoogde sterftekans
tijdens de baring of in de eerste week na de bevalling (hoofdstuk 8). Echter, de veiligheid
van thuisbevallingen hangt sterk af van herkenning en selectie van risico’s vóór de start
van de baring omdat alleen vrouwen die geacht worden laagrisico te zijn de keus wordt
geboden om thuis te bevallen. Door suboptimale risicoselectie bevalt nog steeds een niet
onbelangrijk deel van de hoogrisico (‘Big4’) vrouwen in de eerste lijn: 6% tot 9%. Het is van
cruciaal belang dit percentage omlaag te krijgen aangezien eerstelijns zorg uitsluitend
toegerust is op een laagrisicozwangerschap en -bevalling (hoofdstuk 7).
Hoofdstukken 5, 6, 9 en 10 behandelen verschillen in perinatale gezonheid op het tweede
geografische niveau: de G4 en regio’s binnen Nederland. In hoofdstuk 5 tonen wij aan dat
door optimalisatie van ziekenhuisorganisatie de perinatale sterfte met mogelijk meer dan
30% zou kunnen dalen. Een veelgenoemde beleidsmaatregel in dit kader is centralisatie
van acute verloskundige zorg, wat geacht wordt organisatieaspecten van ziekenhuizen
te verbeteren door het aantal ziekenhuizen dat acute verloskundige zorg biedt sterk te
verminderen. Dit impliceert sluiting van kleinere ziekenhuizen waarbij er een geringer
aantal grotere ziekenhuizen overblijft. Er bestaan echter grote verschillen tussen zieken-
huizen voor wat betreft organisatieaspecten met op hun beurt een positief of negatief
effect op de perinatale sterfte. Dit is een belangrijke factor waar rekening mee gehouden
moet worden bij een beleid van centralisatie van acute verloskundige zorg. Een verstandig
centralisatiebeleid houdt verder rekening met het hele spectrum van factoren die zowel
een positief (bijvoorbeeld 7*24 toegang tot specialistische zorg) als negatief (bijvoorbeeld
een toegenomen reistijd naar het ziekenhuis) effect kunnen hebben op de perinatale ge-
zondheid (hoofdstuk 9). Het centralisatievraagstuk is erg complex; wij ondersteunen dan
ook het standpunt van de Britse Royal College of Obstetricians and Gynaecologists: ‘localised
where possible, centralised where necessary’.
In hoofdstuk 6 wordt ingegaan op twee selectiestrategieën ter identificatie van hoogrisico-
gebieden in Nederland met als doel hier intensieve preconceptiezorg of uniforme antena-
tale risicoselectie toe te passen. Deze selectie is gebaseerd op indicatoren gerelateerd aan
perinatale sterfte, morbiditeit en zorgfactoren. De selectiestrategieën identificeerden de G4
als hoogrisico voor zowel preconceptiezorg als antenatale risicoselectie; hierbij werd nog

213
12
NED
ERLAN
DSE SA
MEN
VATTING
eens bevestigd dat er een verhoogd risico bestaat op ongunstige zwangerschapsuitkom-
sten in de G4. Daarnaast was dit ook een bevestiging van de complexiteit en multifactoriële
oorzaken van perinatale gezondheid in de grote steden.
In hoofdstuk 10 tonen wij effecten van het klimaat, te weten seizoen, temperatuurextremen
en cumulatieve blootstelling aan zonlicht, op geboortegewicht. Blootstelling aan minimum
temperaturen in het tweede en derde trimester van de zwangerschap was geassocieerd
met een hoger geboortegewicht; blootstelling aan maximum temperaturen gedurende de
periconceptionele periode, alle trimesters van de zwangerschap en op de dag van geboorte
was geassocieerd met een lager geboortegewicht; cumulatieve blootstelling aan zonlicht
gedurende alle trimesters was geassocieerd met een hoger geboortegewicht. Ook bleken
er binnen Nederland substantiële klimaatgerelateerde regionale verschillen te bestaan in
geboortegewicht die waarschijnlijk voor het belangrijkste deel toegeschreven kunnen wor-
den aan de blootstelling aan maximum temperaturen. Voor gezonde á terme zuigelingen
lijken deze verschillen klein; echter, de effecten kunnen ernstiger zijn voor risicogroepen
zoals vrouwen die zwanger zijn van groeivertraagde baby’s.
Hoofdstukken 2, 3 en 4 omvatten verschillen in perinatale gezondheid op het derde
geografische niveau: achterstandswijken tegenover niet-achterstandswijken binnen de
G4, in het bijzonder Rotterdam. Er bestaan grote verschillen in absolute perinatale sterfte
en perinatale morbiditeit tussen verschillende wijken binnen de stad Rotterdam met peri-
natale sterftecijfers oplopend tot 37 per 1.000 geboorten (hoofdstuk 2). Dat deze verschil-
len ook na standaardisatie aanhouden impliceert dat er verschillende oorzaken bestaan
per deelgemeente waarbij deelgemeente-specifiek beleid is geïndiceerd (hoofdstuk 3).
Veelgenoemde mechanismen van ongunstige zwangerschapsuitkomsten in achterstands-
wijken zijn sociale achterstand en cumulatie van risico’s gerelateerd aan perinatale sterfte
en morbiditeit. In hoofdstuk 4 tonen wij differentiële effecten van sociale achterstand op
Westerse en niet-Westerse zwangere vrouwen in Rotterdam. Met verbetering van sociale
kwaliteit in de buurt verbetert ook de perinatale gezondheid van Westerse vrouwen; een
verband dat niet gezien werd voor niet-Westerse vrouwen. Beleidsmaatregelen gericht op
verbetering van sociale kwaliteit, in het bijzonder gericht op Westerse vrouwen in achter-
standssituaties, zal waarschijnlijk ook de perinatale gezonheid in deze groep ten goede
komen. Voor niet-Westerse vrouwen is waarschijnlijk een alternatieve aanpak nodig.
Verbetering van perinatale gezondheid op het eerste geografische niveau zal waarschijn-
lijk vooral bewerkstelligd kunnen worden door verbetering van antenatale risicoselectie
(mogelijk door een checklist-gebaseerde aanpak) en zogenaamde shared care waarbij

214
12
NED
ERLAN
DSE SA
MEN
VATTING
risicoselectie een gemeenschappelijke verantwoordelijkheid is van zowel verloskundigen
als gynaecologen. Belangrijke aanbevelingen op het tweede geografische niveau omvatten
een verstandig beleid van centralisatie van acute verloskundige zorg, en nader onderzoek
naar het complexe thema van grootstedelijke perinatale gezondheid met meer focus op
de maatschappelijke gezondheidszorg. Voor wat betreft het derde geografische niveau is
de belangrijkste aanbeveling het nader onderzoek naar differentiële effecten van sociale
achterstand op Westerse en niet-Westerse vrouwen. Onze studieresultaten impliceren een
beleid ter verbetering van sociale kwaliteit voor met name Westerse vrouwen met een focus
op alternatieve maatregelen voor niet-Westerse vrouwen. Deze alternatieve maatregelen
zullen moeten volgen uit resultaten van nader onderzoek. Een andere belangrijke aanbeve-
ling op dit niveau is buurt- en deelgemeente-specifiek beleid voor wat betreft verbetering
van grootstedelijke perinatale gezondheid.

13Authors and affiliations
Manuscripts About the author
PhD portfolioWord of thanks

216
13AU
THO
RS AN
D A
FFILIATION
S
AUTHORS AND AFFILIATIONSFrom the Department of Obstetrics and Gynaecology, Division of Obstetrics and Prenatal
Medicine, Erasmus MC, University Medical Centre Rotterdam, The Netherlands
Semiha Denktaş, Eric A.P. Steegers, Gouke J. Bonsel, Arno F.G. Maas, Johanna (Hanneke)
P. de Graaf, Adja J.M. Waelput, Lieke C. de Jong-Potjer, Sabine F. van Voorst, Amber A. Vos,
Jacoba van der Kooy
From the Department of Public Health, Erasmus MC, University Medical Centre Rotterdam,
The Netherlands
Gouke J. Bonsel, Gerard J.J.M. Borsboom, Johan P. Mackenbach
From the Midwifery Academy, Rotterdam University of Applied Sciences, Rotterdam, The
Netherlands
Gouke J. Bonsel
From the Institute of Health Policy and Management, Erasmus University, Rotterdam, The
Netherlands
Erwin Birnie
From the Municipal Public Health Authority ‘GGD Rotterdam Rijnmond’, Rotterdam, The
Netherlands
H.J. (Ernie) van der Weg, A.J.J. (Toon) Voorham

217
13
MA
NU
SCRIPTS
MANUSCRIPTS
Manuscripts related to this thesis
Chapter 2
J. Poeran, S. Denktaş, E. Birnie, G.J. Bonsel, E.A.P. Steegers. Urban perinatal health inequalities.
Journal of Maternal-Fetal and Neonatal Medicine 2011;24:643-6.
Chapter 3
J. Poeran, S. Denktaş, E. Birnie, H.J. van der Weg, A.J.J. Voorham, E.A.P. Steegers, G.J.
Bonsel. Pregnancy and birth in Rotterdam: a local health report. Tijdschrift voor
gezondheidswetenschappen. 2012;90:496-503. (Article in Dutch, translated into English
for this thesis.)
Chapter 4
J. Poeran, A.F.G. Maas, E. Birnie, S. Denktaş, E.A.P. Steegers, G.J. Bonsel. Social deprivation
and adverse perinatal outcomes among Western and non-Western pregnant women in a
Dutch urban population. Social Science and Medicine;2013;83:42-49.
Chapter 5
J. Poeran, G.J.J.M. Borsboom, J.P. de Graaf, E. Birnie, E.A.P. Steegers, G.J. Bonsel. Population
attributable risks of patient, child and organisational risk factors for perinatal mortality.
Manuscript submitted for publication.
Chapter 6
S. Denktaş, J. Poeran, A.J.M. Waelput, L.C. de Jong-Potjer, S.F. van Voorst, A.A. Vos, G.J. Bonsel,
E.A. P. Steegers. The ‘Healthy Pregnancy 4 All’ Study: Design and cohort profile. Manuscript
submitted for publication.
Chapter 7
J. Poeran, J. van der Kooy, E. Birnie, S. Denktaş, E.A.P. Steegers, G.J. Bonsel. The effectiveness
of risk selection in the Dutch obstetric care system. Manuscript submitted for publication.

218
13M
AN
USCRIPTS
Chapter 8
J. van der Kooy, J. Poeran, J.P. de Graaf, E. Birnie, S. Denktaş, E.A.P. Steegers, G.J. Bonsel.
Planned home compared with planned hospital births in The Netherlands: intrapartum and
early neonatal death in low-risk pregnancies. Obstetrics and Gynecolology 2011;118:1037-
46.
Chapter 9
J. Poeran, G.J.J.M. Borsboom, J.P. de Graaf, E. Birnie, E.A.P.Steegers, J.P. Mackenbach, G.J.
Bonsel. Does centralisation of acute obstetric care reduce perinatal mortality? An empirical
study on pros and cons in The Netherlands. Manuscript submitted for publication.
Chapter 10
J. Poeran, E. Birnie, E.A.P. Steegers, G.J. Bonsel. The impact of extremes in outdoor
temperature and sunshine exposure on birthweight. Manuscript submitted for publication.
Other manuscripts
Scientifi c journals
S.J.A.L. Hemelaar, J. Poeran, E.A.P. Steegers, W.I. van der Meijden. Neonatal herpes infections
in The Netherlands in the period 2006-2011. Manuscript submitted for publication.
J. de Graaf, J. Schutte, J. Poeran, J. Van Roosmalen, G.J. Bonsel, E.A.P. Steegers. Regional
differences in Dutch maternal mortality. BJOG. 2012;119:582-8.
J.P. de Graaf, J.M. Schutte, J. Poeran, J. Van Roosmalen, G.J. Bonsel, E.A. Steegers. Regional
differences in maternal mortality in the Netherlands. Ned Tijdschr Geneeskd. 156:A4952.
(in Dutch with English abstract)
J. Poeran, E.A.P. Steegers, G.J. Bonsel. Approach to perinatal mortality in the Netherlands:
outcomes of a systematic expert study. Ned Tijdschr Geneeskd. 2012;155:A4499. (in Dutch
with English abstract)
J. Poeran, H. Wildschut, M. Gaytant, J. Galama, E.A.P. Steegers, W. van der Meijden. The
incidence of neonatal herpes in The Netherlands. J Clin Virol. 2008;42:321‐5.

219
13
MA
NU
SCRIPTS
Health reports
G.J. Bonsel, J. Poeran, G.J.J.M. Borsboom, J.P. de Graaf, E. Birnie, E.A.P. Steegers. ‘Populatie
attributieve risico’s van moeder-, kind- en organisatie factoren voor perinatale sterfte’ The
population attributable risk of mother-, child- and organisational factors for the perinatal
mortality in The Netherlands 2000‐2008. Rotterdam: Erasmus MC, 2012. (Report for ‘ZonMw’
The Netherlands Organisation for Health Research and Development, report in Dutch with
English abstract)
G.J. Bonsel, J. Poeran, J.P. de Graaf, G.J.J.M. Borsboom, E. Birnie, E.A.P. Steegers, J.P. Macken-
bach. ‘De effecten van concentratie van verloskundige zorg’ Merging hospitals with acute
obstetric care in The Netherlands: effects on perinatal mortality in a system with high
intrapartum referral rates and heterogeneous hospitals. Rotterdam: Erasmus MC, 2012.
(Report for a group of 40 small and medium sized hospitals in The Netherlands which was
presented to the Dutch Minister for Health, report in Dutch with English abstract)
J. Poeran, E. Birnie, S. Denktaş, E.A.P. Steegers, G.J. Bonsel. ‘Zwangerschap en geboorte in
Rotterdam: deelgemeenterapportage’ Perinatal health in Rotterdam 2000-2007. Rotterdam:
Erasmus MC, 2011. (Report for the Rotterdam city Council, report in Dutch with English
abstract)
G.J. Bonsel, E. Birnie, S. Denktaş, J. Poeran, E.A.P. Steegers. ‘Signalementstudie: lijnen in de
perinatale sterfte’ National report on priority topics in perinatal health improvement in The
Netherlands. Rotterdam: Erasmus MC, 2010. (Report for ‘ZonMw’ The Netherlands Organi-
sation for Health Research and Development, presented to the Dutch Minister for Health,
report in Dutch with English abstract)

220
13A
BOU
T THE AU
THO
R
ABOUT THE AUTHORAs the mother of the author, I am very honoured in helping him write this piece for his PhD-
thesis. Virender Jashvant John Poeran was born at a gestational age of 38 weeks on March
21st, 1983 in the Diakonessen hospital in Paramaribo, Suriname. Labour progressed fast, and
early in the morning at exactly 06:40 AM he came into this world in vertex presentation with
a birthweight of 3,560 grams, over 500 grams heavier than his older brother. His height was
49 centimetres with a head circumference of 36.5 centimetres. Right after birth, this already
attention seeking baby started crying loudly after which the midwife gave him an Apgar
score of 10/10. During my whole pregnancy I had expected a girl and I even came up with
the name ‘Sheila’. Having the nurse yelling ‘it’s a boy!’ made me adjust my reality a bit, but I
soon fell in love with that beautiful smile. The most important thing I remember about his
childhood is that he was the naughtiest of my three children. I could not leave him alone for
one second. He was always up to doing something and always busy bullying his little sister.
Jashvant’s first career choices involved being a magician, a pilot and an astronaut. It wasn’t
until his late teens he started thinking of going to medical school for which he was accepted
in the summer of 2001. During his medical training he stumbled upon the path of research
in which he was guided by professor Steegers from the department of Obstetrics and dr.
van der Meijden from the department of Dermatology. At the end of medical school he
more or less made the decision to pursue a career in Obstetrics and Gynaecology. He
finished two clinical internships abroad (Thailand and Suriname) and one in the Albert
Schweitzer hospital in Dordrecht. After obtaining his medical degree in 2008 he worked
a short period as a physician at the department of Obstetrics and Gynaecology at the
Albert Schweitzer hospital in Dordrecht.
Six months later Jashvant was accepted for a PhD-program in Perinatal Epidemiology
under guidance of professors Bonsel and Steegers at Erasmus MC. This municipal
program in the city of Rotterdam had been initiated to reduce the high perinatal mortality
in the city. He was additionally granted the possibility to obtain a Master’s degree in
Epidemiology, which he finished in August 2012. It was during his PhD-period that Jashvant
was extensively re-thinking his career choices and decided to pursue a career in Psychiatry
instead of Obstetrics and Gynaecology. At the end of his PhD-research he therefore worked
as an emergency physician in Psychiatry at the Parnassia Bavo Group, a large suburban
mental hospital in the Rotterdam area.
Always the adventurer and a big traveller, at the end of his PhD-period Jashvant fell in
love with the city of New York. After several meetings with his future boss and mentor dr.

221
13
ABO
UT TH
E AUTH
OR
Mazumdar he decided to pursue his career in the United States instead of The Netherlands.
In April 2013 he started working as a postdoctoral associate of Epidemiology at
Weill Cornell Medical College in New York under guidance of dr. Mazumdar and dr.
Memtsoudis. He is currently studying for his medical degree to be recognised in the
United States and may someday enter clinical medicine again. Being in New York, he has
also signed up to run the New York City Marathon on November 3, 2013, for which he
will raise money for charity. Although I sometimes cannot follow his choices in life I try to
support him wherever I can; in the end, I truly can say I am a proud mother.
Chandra Kirpal, Jashvant’s mother

222
13PH
D PO
RTFOLIO
PHD PORTFOLIO
Summary of PhD training and teaching activities
Name PhD candidate:
Erasmus MC Department:
Research school:
PhD period:
Promotors:
Copromotors:
Virender Jashvant John PoeranObstetrics & GynaecologyNetherlands Institute for Health Sciences (NIHES)August 2009 - December 2012Prof. dr. Gouke J. BonselProf. dr. Eric A.P. SteegersDr. Erwin BirnieDr. Semiha Denktaş
Year Workload
(ECTS)
1. PHD TRAINING
General and specific courses
Master of Science in Epidemiology, Netherlands Institute for Health Sciences, Rotterdam, The Netherlands (NIHES)
2010-2012 35
Introduction in ‘R’ programming 2012 0.1Introduction in SPSS Data Entry 2010 0.3
International conferences
Symposium ‘How Maternity Care Develops in a Multi-Ethnic Urban Society’, Rotterdam, The Netherlands: oral presentation Urban perinatal health in Rotterdam
2012 1.5
59th Annual Meeting of the Society for Gynecologic Investigation, San Diego, USA: poster presentation Social deprivation and adverse perinatal outcomes among Western and non-Western pregnant women in a Dutch urban population
2012 1
58th Annual Meeting of the Society for Gynecologic Investigation, Miami, USA: poster
presentation The effectiveness of risk selection in the Dutch obstetric care system2011 1
11th Congress of the European Society of Contraception and Reproductive Health, The Hague, The Netherlands: oral presentation Unexpected large perinatal health inequalities in an urban, multi‐ethnic population in the Netherlands
2010 1.5
57th Annual Meeting of the Society for Gynecologic Investigation, Orlando, USA: poster presentation Unexpected high levels of perinatal health inequalities in an urban multi‐ethnic population in The Netherlands
2010 1
National conferences
Symposium ‘Urban Perinatal Health’ (in Dutch: ‘Grootstedelijke Perinatale Gezondheid’), Rotterdam, The Netherlands: oral presentation The Social Index and Urban Perinatal Health in Rotterdam (Assisted in organising this symposium)
2011 3
NCVGZ Dutch Annual Public Health Conference (In Dutch: ‘Nationaal Congres Volksgezondheid’), Amsterdam, The Netherlands: oral presentation The Social index and perinatal outcomes in the city of Rotterdam
2011 2
NCVGZ Dutch Annual Public Health Conference (In Dutch: ‘Nationaal Congres Volksgezondheid’), Rotterdam, The Netherlands: oral presentation Large perinatal health inequalities within the city of Rotterdam
2010 2

223
13
PHD
PORTFO
LIO
Year Workload
(ECTS)
Seminars, workshops, research meetings
The Netherlands Perinatal Registry Annual Meetings (‘PRN Contactdag’), Utrecht, The Netherlands
2009-2012 0.8
Attending weekly and quarterly research meetings of the Department of Obstetrics and Gynaecology (and Urology) with three oral presentations, Rotterdam, The Netherlands
2009-2012 5
Attending the annual meetings of the Collaboration of Rotterdam Regional Gynaecologists’ Teaching Hospitals (in Dutch: RGOC) ‘Wladimiroff Symposium with one oral presentation, Rotterdam, The Netherlands
2010-2012 2
Attending the symposium on behalf of the 2.5 year anniversary of the ‘Sophia Birth Centre’, Rotterdam, The Netherlands
2012 0.2
Attending the symposium ‘Home Birth or Hospital Birth’, Maastricht, The Netherlands 2012 0.3Visit from professor Eileen Hutton and staff, VU Medical Centre, Amsterdam, The Netherlands; oral presentation
2012 0.5
Visit from professor Lucilla Poston and staff, King’s College, London, United Kingdom; oral presentation
2011 0.5
Regional Obstetric Collaboration meeting (‘VSV’), Schiedam, The Netherlands with one oral presentation
2010 1
Other: Grant proposal assistance
Assisted in the writing of several grant proposals for ‘ZonMw’ The Netherlands Organisation for Health Research and Development
2009-2012 5
Other: writing of municipal and national (public) health reports
(Assisted in) writing of several national and municipal health reports for local and national (health) authorities: (1) ‘ZonMw’, (2) a collaboration of 40 small hospitals, (3) the Ministry of Health, (4) the Municipality of Rotterdam
2009-2012 15
2. TEACHING ACTIVITIES
Lecturing
Lectures and practicals on ‘Perinatal Health’ in The Netherlands and Rotterdam for Medical students; minor ‘Circle of Life’
2011-2012 5
Lectures on ‘Perinatal Health and Policy Implications’ for Clinical Midwives aspiring to obtain a Master’s degree as Physician Assistant
2011-2012 2
Lecture on ‘Ethnicity and Perinatal Health’ for NIHES Master’s candidates; course ‘Urban Perinatal Health and Health Care’
2012 1
Lecture for students doing their research electives from the Rotterdam University of Applied Sciences on ‘The Dutch System of Obstetric Healthcare’
2011 1
Tutoring
Tutoring first-year Medical students in the first four months of their studies, also preparing them for an academic environment
2012 1
Supervising (Master’s) theses
Medical student Arno F.G. Maas, title: ‘The Social Index and Adverse Perinatal Outcomes in Rotterdam’
2010 2
Medical student Elva Hinborch, title: ‘Environmental Factors Influencing Perinatal Health’ 2010 1Medical student Rénuka S. Birbal, title: ‘Congenital Anomalies in the Borough of Hoek van Holland’
2011 2
Medical student Steffannie J.A.L. Hemelaar, title: ‘The Incidence of Neonatal Herpes in The Netherlands 2005-2012’
2012 2

224
13W
ORD
OF TH
AN
KS
WORD OF THANKSDat ik hier vandaag sta, de laatste dag als promovendus, heb ik aan meerdere personen
te danken. Ik heb mijn promotie-onderzoek ervaren als een tijd waarin ik een enorme
persoonlijke en professionele groei heb doorgemaakt. Wetenschap bleek mij meer te
trekken dan ik aanvankelijk had durven denken, en ik kreeg er nog betaald voor ook.
Ondanks dat ik mijn toekomst al langere tijd zag als gynaecoloog, heb ik meerdere moeilijke
keuzes durven nemen met een enorme impact op mijn toekomstbeeld, maar die mij
uiteindelijk wel gelukkiger hebben gemaakt.
Allereerst wil ik iedereen bedanken die in een bepaalde vorm heeft bijgedragen aan de
totstandkoming van dit proefschrift, in het bijzonder mijn promotoren prof. dr. Gouke
Bonsel en prof. dr. Eric Steegers.
Gouke, ik herinner me onze eerste ontmoeting nog heel goed, je had heel wat te vertellen
over ene ‘Signalementstudie’, omdat ik net uit een nachtdienst kwam is het meeste langs me
heen gegaan. Dat was gelukkig niet het geval toen ik ook daadwerkelijk onder jouw hoede
op de afdeling kwam. Het is niet te meten hoeveel ik van je heb geleerd over epidemiologie,
statistiek, algemene wetenschap, en de meest actuele (maar ook de minder actuele)
roddels. De manier waarop je altijd het onderste uit de kan wil halen, altijd nieuwsgierig
bent naar hoe dingen in elkaar zitten, heeft erg inspirerend gewerkt. Ik ben erg blij dat jij
mijn promotor bent geweest, dank voor de inspirerende jaren.
Beste Eric, na mijn onderzoek als student geneeskunde bleef ik je per e-mail stalken omdat
ik graag gynaecoloog wilde worden en wilde promoveren op jouw afdeling. Dat laatste heb
ik inmiddels bereikt en voor wat betreft dat eerste heb ik een van de moeilijkste gesprekken
uit mijn leven met jou gevoerd. Dank voor de voortdurende steun, het begrip, maar vooral
ook het getoonde vertrouwen. Ik hoop dat we in de toekomst nog zullen samenwerken.
Mijn eerste copromotor dr. Erwin Birnie. Beste Erwin, een man van initieel weinig woorden,
maar wel de juiste. Jouw altijd scherpe commentaren op mijn manuscripten waren altijd
een motivator om mezelf te blijven verbeteren en altijd kritisch te blijven; dit waardeer
ik enorm. Iets waar ik altijd aan zal terugdenken zijn de ‘soep-momenten’ en later de ‘vis-
momenten’ waar altijd weer de nieuwste roddels werden uitgewisseld.
Mijn tweede copromotor dr. Semiha Denktaş. Beste Semiha, ook met jou is het altijd
prettig samenwerken geweest; met name de informele sfeer heb ik erg gewaardeerd.
Ik kon met alles naar je toe komen, je bood altijd een luisterend oor en je gaf ook altijd
advies hoe te handelen in moeilijke situaties. Ik heb erg veel respect voor hoe jij bent

225
13
WO
RD O
F THA
NKS
gepromoveerd, een groot gemeentelijk programma hebt geleid, een groot landelijk
programma leidt en daarnaast nog eens een moeder van twee kinderen bent. Ook aan
jouw doorzettingsvermogen en multifunctionaliteit hoop ik me eens te meten.
Dit hele promotietraject was niet mogelijk geweest zonder financiële ondersteuning van
de Gemeente Rotterdam in de vorm van het initialiseren van het programma ‘Klaar voor
een Kind’. Rotterdam heeft met dit project nog maar eens bewezen vooral te ‘doen’ en te
‘durven’ in plaats van te ‘dralen’. In dit kader ben ik ook de GGD Rotterdam Rijnmond erg
erkentelijk voor de samenwerking binnen dit programma, in het bijzonder drs. H.J. (Ernie)
van der Weg en dr. A.J.J. (Toon) Voorham.
Bij de realisatie van dit proefschrift is voornamelijk gebruik gemaakt van gegevens uit de
Perinatale Registratie Nederland (PRN). Graag wil ik dan ook bedanken het PRN bestuur,
drs. G. de Winter en natuurlijk dr. ir. C.W.P.M. (Chantal) Hukkelhoven.
Graag wil ik ook bedanken de overige leden van de leescommissie voor hun kritische blik
op mijn proefschrift: prof. dr. ir. A. Burdorf, prof. dr. A.J. van der Heijden en prof. dr.
A.P. Verhoeff.
Ook de leden van de grote commissie wil ik hierbij bedanken voor hun tijd, hun kritische
blik en de discussie over de inhoud van mijn proefschrift.
De ‘Klaar voor een Kind(eren)’ en de ‘Healthy Pregnancies’: Sevilay Temel, Chantal Quispel,
Ingrid Peters, Daniëlle van Veen, Mieke van Veen, Hanneke Torij, Kirsten Heetkamp, Isabel
Fino Dos Santos Boialvo, Mijke van den Berg, Tom Schneider, Anke Posthumus, Amber Vos,
Sabine van Voorst, Vera Schölmerich, Adja Waelput, Lieke de Jong-Potjer, prof. Merkus en de
rest van de twee teams die ik misschien nog vergeten ben. Dank voor de fijne samenwerking,
maar vooral ook de gezelligheid!
In het bijzonder wil ook bedanken Jolanda Claessens en Brenda Karsan die me altijd
wisten te helpen als ik even niet meer wist hoe ik iets geregeld moest krijgen.
Ook ben ik dr. J.P. (Hanneke) de Graaf erg erkentelijk voor het altijd brengen van een (niet
bescheiden) lach. Daarnaast heb ik een erg fijne tijd gehad in die hele mooie kamer in het
Hs-gebouw die je toch maar weer even voor ons geregeld had.
Drs. G.J.J.M. (Gerard) Borsboom; ik zal niet gauw die beruchte vrijdagavond vergeten
toen we kort voor een deadline een analysefout ontdekten. Ik weet zeker dat ik er een paar
grijze haren aan heb overgehouden. Ik heb mijn tijd met jou als erg prettig ervaren, je hebt
me leren programmeren in SAS en je hebt was nooit te beroerd om me te helpen als ik
weer eens wat statistiekvraagjes had. Dank voor de gezellige, en vooral ook leerzame tijd.

226
13W
ORD
OF TH
AN
KS
De eerste helft van ‘Babsvant’, Babs, mijn steun en toeverlaat zowel tijdens werk maar ook
ver daarbuiten. Wie had gedacht dat we het zo goed met elkaar zouden vinden, ik niet
in ieder geval. Je hebt me kritisch leren kijken naar mijzelf, we hebben veel filosfofische
gesprekken gevoerd over het geloof en van alles en nog wat. Ik weet nog steeds niet precies
wat ons nou zo bindt maar ik hoop dat we nog een heleboel in de toekomst samen zullen
doen.
Mijn vrienden, mijn rotsen in de branding: David (en Aukje), Martijn (en Altia), Reza (en
Caroline), Marloes, Ben, Strelitzia en Babs voor de tweede keer. Jullie hebben allen gemeen
wat ik het belangrijkst vind in het leven: lekker eten en lekker lachen met op zijn tijd een
serieus gesprek. Dank voor jullie fantastische vriendschap, jullie maken mij tot de persoon
die ik ben.
Mijn paranimfen Martijn en Babs, dank dat jullie op deze belangrijke dag in deze rol naast
mij staan.
De soon-to-be New York crew Marijana, Fatima, Babs (alweer?!); dank voor de altijd heerlijk
luchtige humor en de gezelligheid. Met wie anders rijd ik via de stoep om slagbomen heen
of breng ik een hele dag in een Starbucks door met zelf meegenomen eten.
Mijn overige collega-onderzoekers op de afdeling Verloskunde en Gynaecologie: Wendy,
Yvonne, Kim, Babette, Evelyne, Sylvia, Nienke, Emilie, Nicole, John, Sam, Marieke, Melek,
Averil, Nina, Manon en iedereen die ik vergeten ben. Bedankt voor de zeer geslaagde
congressen (Miami 2011!), de woensdagochtendkoffies, de borrels (ook al was ik er niet
vaak) en natuurlijk die fantastische ski-trip!
Als laatste wil ik mijn familie bedanken, mijn broer Jashvier, mijn zusje Renu en mijn moeder
voor hun niet aflatende steun.

227

228
Het drukken van dit proefschrift is mede mogelijk gemaakt door sponsoring van de vol-
gende partijen:
• de afdeling Verloskunde en Gynaecologie, Erasmus MC
• de Gemeente Rotterdam en het ‘Klaar voor een Kind’ programma
(www.klaarvooreenkind.nl)
• J.E. Jurriaanse Stichting
• Medical Dynamics
• Mpluz
• Danone
• BMA-Mosos
• Goodlife Pharma
• AbbVie BV
• Nutricia
• Vasa Previa Foundation (www.vasaprevia.nl)
“De Nederlandse Vasa Previa Foundation is een non-profit organisatie met als hoofddoel het
terugbrengen van babysterfte of blijvend letsel als gevolg van vasa previa. Enkele activiteiten
om dit te bereiken zijn het onder de aandacht brengen van het gevaar van vasa previa binnen
de relevante beroepsgroepen en het aansturen op aanpassing van de medische protocollen, die
belangrijk zijn voor diagnose en management van vasa previa. Daarnaast biedt de stichting
een luisterend oor en advies voor iedereen die vasa previa meemaakt of heeft meegemaakt.”

Virender Jashvant John Poeran was born at a gestational age of 38 weeks on March 21st, 1983 in the Diakonessen hospital in Paramaribo, Suriname, at exactly 6:40
AM. He came into this world in vertex presentation with a birthweight of 3560 grams, a height of 49 centimetres and a head circumference of 36.5 centimetres. The attending midwife granted him an Apgar score of 10/10.
At the age of 8 he moved to The Netherlands where he finished middle and high school. In the summer of 2001 he was accepted for medical school at Erasmus University, Rotterdam. During his medical training he stumbled upon the path of research in which he was guided by professor Steegers from the department of Obstetrics and dr. van der Meijden from the department of Dermatology. After obtaining his medical degree in 2008 he worked as a physician at the department of Obstetrics and Gynaecology at the Albert Schweitzer hospital in Dordrecht.
In 2009 he was accepted for a PhD-program in Perinatal Epidemiology under guidance of professors Bonsel and Steegers at Erasmus MC. He was additionally granted the possibility to obtain a Master’s degree in Epidemiology, which he finished in August 2012, the same year in which he decided to pursue a career in Psychiatry instead of Obstetrics and Gynaecology. At the end of his PhD-research he therefore worked as an emergency physician in Psychiatry at the Parnassia Bavo Group. However, in the fall of 2012 he fell in love with the city of New York and is currently working as a postdoctoral associate of Epidemiology at Weill Cornell Medical College in New York.