Prevalence of Onychomycosis in and around Karwar, Uttara ...Prevalence of Onychomycosis in and...
Transcript of Prevalence of Onychomycosis in and around Karwar, Uttara ...Prevalence of Onychomycosis in and...

DOI: https://doi.org/10.18320/JIMD/201603.03126
Journal of International Medicine and Dentistry 2016; 3(3): 126-133
JOURNAL OF INTERNATIONAL MEDICINE AND DENTISTRY
To search……………..to know………..…….to share
p-ISSN: 2454-8847
e-ISSN: 2350-045X
Original article
Prevalence of Onychomycosis in and around Karwar, Uttara Kannada
Venkatesh V N1, Swapna Kotian2
Abstract: Onychomycosis, one of the most common nail infections caused by dermatophytes, yeast and non-dermatophytic moulds accounts for about half of all nail abnormalities and about a third of all fungal infections of the skin. The study aimed to determine the prevalence of onychomycosis and fungal aetiology in this area. A total of 168 samples suspected to be having nail infection were collected and processed. Fungal culture was positive in 119(70.83%) while direct microscopy showed a positivity of 86(51.19%). Distal Lateral Subungual Onychomycosis (DLSO) was the most common clinical condition observed in 102(60.71%) participants and least 14(8.33%) were seen in candidal onychomycosis (CO). Trichophyton rubrum 36(30.25%) was the most common isolate among the dermatophytes whereas among non-dermatophytic moulds, Aspergillus niger 4(3.36%) was the predominant isolate. Clinical evaluation, direct microscopy and culture are important for proper diagnosis.
Key words: Onychomycosis, Trichophyton rubrum, Distal Lateral Subungual Onychomycosis
Introduction:
Onychomycosis, a denomination used to describe nail infection usually caused by dermatophytes, yeast and non-dermatophytic moulds, represents upto 20% of all nail disorders. 1, 2 Until the late 1990’s, onychomycosis was a poorly discussed topic of medical science. Even in the financially more advanced Asian countries, onychomycosis has been highlighted only in the last decade.3 The worldwide incidence of onychomycosis is increasing and a number of factors contribute to this risk. First, as the population ages, there are corresponding increases in chronic health problems, such as diabetes and poor peripheral circulation. Second, the number of persons who are immunocompromised because of infection with human immunodeficiency virus and the use of immunosuppressive therapies, cancer chemotherapy or antibiotics continue to expand. Third, avid sports participation is increasing the use of health clubs,
communal swimming pools and occlusive footwear for exercise.4 Onychomycosis affects approximately 5 % of the population worldwide5 and represents 20-40% of onychopathies and about 30% of mycotic cutaneous infections6. Although onychomycosis is rarely life threatening, its high incidence and prevalence and the associated morbidity makes it an important public health problem. Inspite of improved personal hygiene and living environment, onychomycosis continues to spread and persist. Unlike in western countries where it is the frequent cause of nail disorders, in South-East Asia the prevalence of onychomycosis is relatively low. This was partially confirmed by a large scale survey in Asia in the late 1990’s in which the prevalence of onychomycosis was lower in tropical countries in the temperate zone (18%).7 In India, higher priorities in socioeconomic concerns and health issues for other diseases have resulted in low awareness of onychomycosis by physicians and the general public alike.

Venkatesh VN et al: Prevalence of onychomycosis www.jimd.in
127
Journal of International Medicine and Dentistry 2016; 3(3): 126-133
The epidemiology of onychomycosis has been well-studied in some countries, but few data are available in tropical countries. Very few studies have been reported from this region of Karnataka. Therefore, we undertook a study to improve the knowledge of the epidemiology and the mycological features of onychomycosis.
Materials and Methods:
A total of 168 samples were collected from patients with clinically suspected fungal nail infections who have attended dermatology outpatient department of our tertiary care hospital. The duration of the study was from November 2014 to October 2015. After the approval from Institutional Ethical committee and obtaining a written informed consent from the patients, the samples were collected. At the time of collection, a detailed history in relation to age, sex, address, occupation, duration of illness, medication and clinical appearance and location of onychomycosis were documented.. Patients who were undergoing treatment with systemic or topical anti-fungal agents 4 weeks preceding the study period were excluded.
Specimen collection and processing:
The specimens were obtained from clinically abnormal nails by vigorous scrapping of the nail bed, the underside of the nail plate and hyponychium and nail clippings after cleaning the affected area with 80% ethanol. The samples of each patient were placed in separate sterile petridish and transported to the mycology laboratory. All specimens were analyzed by direct microscopy and culture. Scraped scales and clippings from the nails were analyzed for fungal elements such as hyphae or blastoconidia by direct microscopic examination in potassium hydroxide (20 %). For fungal cultures, all samples were inoculated on each of two isolation media (1) Sabouraud Dextrose Agar (SDA, Hi Media Laboratories)(2)SDA with 5 % Chloramphenicol and
Cycloheximide(SCCA, Hi Media Laboratories) in duplicate. Along with these media, Dermatophyte Test Medium (DTM) was used (Hi Media Laboratories).The culture tubes were incubated at 25°C & 37°C and examined daily for a period of six weeks according to standard protocol (Larone).8
Identification:
Growth in the culture medium was viewed as confirmation of dermatophytes as aetiological agents; if no growth was found after 6 weeks, it was considered as negative. Pure isolates were generated by subculturing onto SCCA for both macroscopic and microscopic examination. Further identification was done by performing slide culture technique, hair perforation test and urea hydrolysis (Larone)8. The identification of non-dermatophytic fungal species was performed by following microscopic and macroscopic evaluation of the primary cultures and slide culture (Larone)8. When the light microscopy of a nail specimen showed filaments with only a non-dermatophytic growth in culture, a second nail specimen was examined again by light microscopy and culture to confirm non-dermatophytic mould infection. All the values were calculated and projected as percents. Chi -square statistics was carried out to check if it were statistically significant with significance set at p<0.01.
Results:
In a total of 168 clinically suspected cases of Onychomycosis, the study included 82(48.81%) males and 86 (51.19%) females. Distal Lateral Subungual Onychomycosis (DLSO) was the most common clinical condition observed in 102(60.71%) participants of which 48(47.06%) were males and 54(52.94%) were females. The next most prevalent clinical condition was Proximal Subungual Onychomycosis (PSO) seen in 30 (17.86%) participants with 14(46.67%)

Venkatesh VN et al: Prevalence of onychomycosis www.jimd.in
128
Journal of International Medicine and Dentistry 2016; 3(3): 126-133
males and 16(53.33%) females followed by Superficial White Onychomycosis (SWO) being noted in 22(13.1%) participants of which 12 (54.55%) were males and 10(45.45%) were females. A clinical pattern of candidal onychomycosis (CO) was also noted in 14 (8.33%) participants with 8(57.14%) being shown by males and 6(42.86%) by females as outlined in Table I. The study included participants belonging to all the age groups with highest prevalence being observed in 16-30 years age group people 73(43.45%) followed by participants in 31-45 years age group with prevalence of 58(34.52%). A lower incidence was noted in participants belonging to younger age group of 5-15 years i.e. 9(5.36%) and the elder age group above 60 years with 5(2.18%) as outlined in Table II. Highest prevalence was observed in participants who were fishermen 68(40.48%) by profession followed by other group which included agriculturists 39(23.21%), students 30(17.86%) as seen in Table II. History of disease varied from less than a month to more than a year at the time of first presentation. A hundred and seventeen (69.64%)had greater than 1 year history followed by 43(25.6%) having a 6 month- 1 year history; 5 (2.98%) had a history of 1-6 months while only 3 (1.79%) had a disease history of less than 1 month at presentation.
Table I: Clinical type and gender distribution
Clinical type
Male (%)
Female (%)
Total (%)
DLSO 48(47.06) 54(52.94) 102(60.71) PSO 14(46.67) 16(53.33) 30(17.86) SWO 12(54.55) 6(42.86) 14(8.33) CO 8(57.14) 10(45.45) 22(13.1) Total 82(48.81) 86(51.19) 168 Clinical diagnosis was confirmed by both direct microscopy and culture [Figure I]. Fungal culture was positive in 119(70.83%) while direct microscopy showed a positivity of 86(51.19%); 71(42.26%) were positive by direct
microscopy and culture while 15(8.93%) cases showed positive result by direct microscopy and negative in culture. Forty eight (28.57%) cases showed negative
Table II: Participants’ Demographics
Age Prevalence (% , n= 168)
5-15 years 9(5.36%) 16-30 years 73(43.45%) 31-45 years 58(34.52%) 46-60 years 23(13.69%) >60 years 5(2.98%)
Total 168
Occupation Agriculturist 39(23.21%) Fishermen 68(40.48%) Housewife 25(14.88%)
Student 30(17.86%) Office worker 6(3.57%)
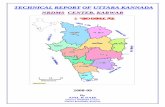
Total 168 Figure I: A. Case of onychomycosis showing nail dystrophy B. Direct microscopy showing fungal elements C. Trichophyton rubrum macroscopic appearance D. Lactophenol cotton blue tease mount – Trichophyton mentagrophytes
results in direct microscopy but positive culture. Of the total cases, 34(20.24%) were negative by both direct microscopy as well as culture as outlined in Table III.

Venkatesh VN et al: Prevalence of onychomycosis www.jimd.in
129
Journal of International Medicine and Dentistry 2016; 3(3): 126-133
It was statistically significant (p< 0.001). A total of 119(70.83%) culture positive cases were seen, dermatophytes being the
most common pathogen being isolated in 98(82.35%) participants.
Table III: Direct microscopy and culture correlation
Culture positive (%) Culture negative (%)
Total (n= 168) (%)
Direct microscopy positive 71(42.26) 15(18.93) 86(51.19)
Direct microscopy negative 48(28.57) 34(20.29) 82(48.81)
Total 119(70.83) 49(29.17) 168 *p=0.0006 Table IV: Spectrum of isolation
Isolate Percentage prevelance (n=119) (%) Trichophyton rubrum 36(30.25) Trichophyton mentagrophytes 24(20.17) Trichophyton mentegrophytes var interdigitale 24(20.17) Trichophyton tonsurans 8(6.72) Microsporum species 6(5.04) Non-dermatophyte mould 8(6.72) Candida species 13(10.92) Total 119
Among the non dermatophytes, Candida species 13(10.9%) was the most common isolate. The various dermatophytes in varying percentages, Candida species and non-dermatophyte moulds isolated in fungal culture are outlined in Table IV.
Discussion:
Onychomycosis is one of the most frequent nail diseases accounting for about half of all nail abnormalities and about a third of all fungal infections of the skin and can have a serious impact on patients’ quality of life. 9, 10 The total rate of isolation in our study was 119(70.83%) which was in accordance with various studies in India and other places around the world, which included 60% in Karnataka 11, 82.3% in Sikkim 12, 88 % in West Bengal 13, 86.9% in Turkey 14 and 66.5% in Brazil.15 However, some of the studies have shown contrary results having low rate of isolation- 39.5% in Central Delhi 16, 37.6% in Himachal 17, 45 % in New Delhi 3, 26.3% in Rome 2, 8% in Ontario 18 respectively. The difference in the rate of prevalence of onychomycosis
may be due to the fact that the fungi causing disease vary from one geographical area to other, primarily due to difference in climatic conditions. 19 Variation in the prevalence also depends on age, predisposing factors, social class, occupation, living environment and frequency of travel.20 One of the other reasons for variation in the prevalence may be due to the fact that many do not seek medical attention. 21 In our present study, of the total 168 total suspected cases of onychomycosis, 86(51.19%) were females and 82(48.81%) were males showing no significant difference in the occurrence based on the gender. Some of the previous studies have shown higher rate of incidence in males 14,
16, 17, 22, 23 and some showed increased incidence in the female population. 2, 24 The higher incidence in males could be due to common use of occlusive footwear, more exposure to outdoor conditions and increase in various outdoor physical activities.25 In females, finger nails were more involved because generally, work involved performing domestic chores thus

Venkatesh VN et al: Prevalence of onychomycosis www.jimd.in
130
Journal of International Medicine and Dentistry 2016; 3(3): 126-133
hands remained wet for a long time in the day.3 The most common clinical condition type observed in our study was DLSO 102 (60.71%) which is characterized by invasion of nail bed and underside of nail plate 20 and is comparable to other reports. 26, 27 The second most common clinical condition observed was PSO in 30 (17.86%) participants. Some of the previous studies have reported greater incidence28, 29 while some other researchers have reported lower incidence of PSO.30, 31 The other clinical types observed were SWO in 22[13.1%] of cases and CO in 14 [8.33%]. The prevalence of onychomycosis varies by age; in our study, higher rate of prevalence was noted in participants ranging in age between 16-30 years- 73(43.45%) followed by 31-45 years participants i.e. 58(34.52%) which is in accordance with other studies having reported higher prevalence in younger adults.16, 26, 31 Nail infection being a cosmetic problem with physical morbidity causing destruction and disfigurement of nail plate leads to self-consciousness thus seeking medical help as well as due to increased physical activity and different shoe wearing habits.23 Lower incidence was noted in children belonging to 5-15 years age group- 9(5.36%) which may be due to less exposure to fungus , faster nail growth and smaller nail surface for invasion of fungus.32 Five (2.98%) participants belonging to age group greater than 60 years in age showed nail infection which may be attributed to poor peripheral circulation, repeated nail trauma over a period of time, longer exposure to pathogenic fungi, suboptimal immune function, less physical activity and poor personal hygiene. 22 In our study, higher prevalence of 68(40.48%) was observed in participants who were fishermen by profession; this could be due to feet being wet for a prolonged period of time thus providing a conducible condition for proliferation of
pathogenic fungi. The second group who showed higher prevalence of 39(23.22%) were agriculturists, who too are exposed to pathogens present in soil. This study also had 30(17.86%) students which may be related to increased use of sports shoes and socks retaining sweat and as well as vigorous physical activity resulting in frequent nail injuries among students. 23 The two important conventional methods for identification are direct microscopy by potassium hydroxide (KOH) and fungal culture and both are necessary for definitive identification of the aetiologic agents as direct microscopy serves as a screening test and culture helps in differentiating among the pathogens and identifying the agents. 20 Of the 168 suspected cases, 71(42.26%) were confirmed by showing positivity by both direct microscopy and culture, but 15(8.93%) showed positivity by direct microscopy and culture being negative which may be due to the fact that these culture negative results may reflect the administration of anti-fungal treatment initiated before sampling as some patients may have given incorrect information on their receipt of anti-fungal treatment. 33 In 48 (28.57%) cases, culture yielded a positive result with direct microscopy being negative which may be due to very less presence of fungal elements in the sample which could not be visualized by direct microscopy and false negative in direct microscopy is a ordinary practice. Fungal cultures provide information regarding the species involved in producing the disease. In our study, dermatophytes represent the most common isolate- 98(82.35%) which is comparable to other studies 11, 16, 17, 26, 30 followed by non-dermatophytes-21(17.65% ) which includes 13 (10.92) Candida species. T. rubrum- 36( 30.25%) was the most common isolate seen in our study which is in accordance with other studies. 13, 16, 26, 34,
35, 36 It has also been noted that T. rubrum is a common causative agent due to the ability of the fungus to invade deeper

Venkatesh VN et al: Prevalence of onychomycosis www.jimd.in
131
Journal of International Medicine and Dentistry 2016; 3(3): 126-133
tissue and nail keratin. In some studies 25,
16 , T. mentagrophytes has been reported as most prevalent dermatophyte, but we have identified T. mentagrophytes in 24 (20.17%), T. tonsurans in 8(6.72%) and Microsporum species in 6(3.57%) which are the other isolates commonly seen.37 This difference could be attributed to variation in epidemiology based on geographical location. Candida species have been isolated in 13(10.92%) cases involving Candida albicans, Candida parapsilosis and other Candida species which is in accordance with many studies. 16, 27, 30, 31 Non-dermatophytic moulds were isolated in 8(6.72%) cases which included 4(3.36%) Aspergillus niger, 2(1.68%) Fusarium species, 1(0.84%) Scytalidium species and 1(0.84%) Aspergillus flavus. Aspergillus species are known to spread from nails causing deep aspergillosis.38 These etiological agents have also been reported in other studies conducted worldwide to cause onychomycosis. 13, 16,
39
Conclusion:
The present study shows that T. rubrum was the common isolate from this region causing onychomycosis. To diagnose onychomycosis, clinical examination alone is not sufficient. 13, 19 It was seen that both mycological and clinical examination are important for establishing diagnosis. It is beneficial to do both direct microscopic examination and culture in order to improve diagnosis. A well rounded epidemiological research is needed in this region which covers all aspects of the society to know the actual prevalence.
References:
1. Weitzman I, Summerbell RC. The dermatophytes. Clin Microbiol Rev 1995; 8: 240-59. 2. Mercantini R, Marsella R, Moretto D. Onychomycosis in Rome, Italy. Mycopathologia 1996; 136: 25-32; https://doi.org/10.1007/BF00436657
3. Kaur R, Kashyap B, Bhalla P. A Five-year survey of Onychomycosis in New Delhi, India: Epidemiological and Laboratory Aspects. Indian J Dermatol 2007; 52(1) 39-42; https://doi.org/10.4103/0019-5154.31923 4. Proceedings of the International summit on cutaneous Antifungal Therapy and Mycology Workshop. San Francisco. California, October 21-24, 1993. J Am Acad Dermat 1994; 31;S1-116 5. Murray SC, Dawber RP. Onychomycosis of toenails: orthopaedic and pediatric considerations. Australas J Dermatol 2002; 43: 105-12. 6. Achten G, Wanet RJ. Onychomycosis in the laboratory. Mykosen 1978; 21:125-7. 7. Bramono K. The Asian Achilles survey. Presented in the 6th Asian Dermatological Congress, Bangkok: November 2001. 8. Larone DH. Medically Important Fungi: A Guide to Identification. 4th ed. Washington, DC: American Society for Microbiology Press; 2002. 9. Baran R, Dawber RPR. Diseases of the Nails and Their Management. Oxford, England: Blackwell Science; 1994. 10. Sikora M, Pachołek T, Soter K, Szepietowski J. Analysis of fungal skin and skin appendages infections in the region of Wrocław in the years 1995-1999. Mikol Lek. 2000; 7:145-151. 11. Jain S, Sehgal VN. Commentary: onychomycosis: an epidemio-etiologic perspective. Int J Dermatol 2000; 39:100-103; https://doi.org/10.1046/j.1365-4362.2000.00808.x 12. Adhikari L, Gupta AD, Pal R, Singh TSK. Clinico-etiologic correlates of onychomycosis in Sikkim. Indian J Pathol Microbiol 2009; 52:194-197. 13. Das NK, Ghosh P, Das S, Bhattacharya S, Dutta RN, Sengupta SR. A study on the etiological agent and clinico-mycological correlation of fingernail onychomycosis in eastern India. Indian J Dermatol 2008; 53:75-79; https://doi.org/10.4103/0019-5154.41651 14. Yenişehirli G, Bulut Y, Sezer E, Günday E. Onychomycosis infections in the Middle Black Sea Region, Turkey. Int J Dermatol 2009; 48: 956-959; https://doi.org/10.1111/j.1365-4632.2009.04126.x 15. Pontes ZB, Lima Ede O, Oliveira NM, Dos Santos JP, Ramos AL, Carvalho MF.

Venkatesh VN et al: Prevalence of onychomycosis www.jimd.in
132
Journal of International Medicine and Dentistry 2016; 3(3): 126-133
Onychomycosis in João Pessoa city, Brazil. Rev Argent Microbiol 2002; 34: 95-9. 16. Sanjiv A, Shalini M, Charoo H. Etiological agents of onychomycosis from a tertiary care hospital in Central Delhi, India. Indian J Fund Appl Life Science. 2011; 1: 11-14. 17. Gupta M, Sharma NL, Kanga AK, Mahajan VK, Tegta GR. Onychomycosis: clinico-mycologic study of 130 patients from Himachal Pradesh, India. Indian J Dermatol Venereol Leprol 2007; 73: 389-392; https://doi.org/10.4103/0378-6323.37055 18. Gupta AK, Jain HC, Lynde CW, Macdonald P, Cooper EA, Summerbell RC. Prevalence and epidemiology of onychomycosis in patients visiting physicians offices: A multicentre Canadian survey of 15000 patients. J Am Acad Dermatol 2000; 43: 244-8; https://doi.org/10.1067/mjd.2000.104794 19. Sehgal VN, Srivastava G, Dogra S, Chaudhary A, Adhikari T. Onychomycosis: an Asian perspective. Skinmed 2010; 8: 37-45. 20. Kaur R, Kashyap B, Bhalla P. Onychomycosis – Epidemiology, diagnosis and management. Indian J Med Microbiol 2008; 26(2): 108-116; https://doi.org/10.4103/0255-0857.40522 21. Eleweski BE. Diagnostic techniques for confirming onychomycosis. J Am Acad Dermatol 1996; 35(3 pt 2): S6-S9. 22. Elewski BE, Charif MA. Prevalence of onychomycosis in patients attending a dermatology clinic in northeastern Ohio for the other conditions. Arch Dermatol. 1997; 133: 1172-1173; https://doi.org/10.1001/archderm.1997.03890450124022 23. Scher RK. Onychomycosis is more than a cosmetic problem. Br J Dermatol. 1994; 130(suppl 43): S15; https://doi.org/10.1111/j.1365-2133.1994.tb06087.x 24. Lopes JO, Alves SH, Mari CR, Oliveira LT, Brum LM, Westphalen JB, et al. A ten-year survey of onychomycosis in the central region of Rio Grande do Sul, Brazil. Rev Inst Med Trop Sao Paulo 1999; 41: 147-9; https://doi.org/10.1590/S0036-46651999000300002 25. Shankarnarayan SA, Pal S, Sharma N, Juyal D, Sharma MK, Dimri D. Incidence and epidemiology of onychomycosis in patients
visiting a tertiary care hospital in India. Cutis 2015; 95: E20-E25. 26. Ahmad M, Gupta S, Gupte S. A clinico-mycological study of onychomycosis. EDOJ 2010; 6: 1-9. 27. Garg A, Venkatesh V, Singh M, Pathak KP, Kaushal GP, Agrawal SK. Onychomycosis in central India: a clinicoetiologic correlation. Int J Dermatol 2004; 43: 498-502; https://doi.org/10.1111/j.1365-4632.2004.02125.x 28. Veer P, Patwardhan NS, Damle AS. Study of onychomycosis: prevailing fungi and pattern of infection. Indian J Med Microbiol 2007; 25: 53-56; https://doi.org/10.4103/0255-0857.31063 29. Sujatha V, Grover S, Dash K, Singh G. A clinico-mycological evaluation of onychomycosis. Indian J Dermatol Venereol Leprol 2000; 66: 238-240. 30. Bokhari MA, Hussain I, Jahangir M, Haroon TS, Aman S, Khurshid K. Onychomycosis in Lahore, Pakistan. Int J Dermatol 1999; 38: 591-595; https://doi.org/10.1046/j.1365-4362.1999.00768.x 31. Jesudanam TM, Rao GR, Lakshmi DJ, Kumari GR. Onychomycosis: a significant medical problem. Indian J Dermatol Venereol Leprol 2002; 68: 326-329. 32. Havu V, Brandt H, Heikkilä H, HollmenA, Oksman R, Rantanen T, et al. A double-blind, randomized study comparing itraconazole pulse therapy with continuous dosing for the treatment of toe-nail onychomycosis. Br J Dermatol 1997; 136: 230-4; https://doi.org/10.1046/j.1365-2133.1997.d01-1175.x 33. Fulgence KK, Abibatou K, Vincent D, Henriette V, Etienne AK, Kiki-Barro PC, et al. Tinea capitis in schoolchildren in southern Ivory Coast. Int J Dermatol 2013; 52: 456-460; https://doi.org/10.1111/j.1365-4632.2012.05733.x 34. Ogasawara Y, Hiruma M, Muto M, Ogawa H. Clinical and mycological study of occult tinea pedis and tinea unguium in dermatological patients from Tokyo. Mycoses 2003; 46: 114-119. 35. Foster KW, Ghannoum MA, Elewski BE. Epidemiologic surveillance of cutaneous fungal infection in the United States from 1999 to 2002. J Am Acad Dermatol 2004; 50:

Venkatesh VN et al: Prevalence of onychomycosis www.jimd.in
133
Journal of International Medicine and Dentistry 2016; 3(3): 126-133
748-752; https://doi.org/10.1016/S0190-9622(03)02117-0 36. Cheng S, Chong L. A prospective epidemiological study on tinea pedis and onychomycosis in Hong Kong. Chin Med J (Engl) 2002; 115: 860-865. 37. Havlickova B, Czaika V A, Friedrich M. Epidemiological trends in skin mycoses worldwide. Mycoses 2008; 51(4): 2-15; https://doi.org/10.1111/j.1439-0507.2008.01606.x
38. Colin K Campbell and Elizabeth M Johnson. Topley and Wilson’s Microbiology and Microbial Infection. 10th ed. UK: John Wiley and sons Ltd; 2007. 39. Bassiri-Jahromi S, Khaksar AA. Nondermatophytic moulds as a causative agent of onychomycosis in Teheran. Indian J Dermatol 2010; 55: 140-143; https://doi.org/10.4103/0019-5154.62743
*************************************************** ******************************* Conflict of interests: Nil Date of submission: 24-09-2016 Source of funding: Nil Date of acceptance: 19-10-2016
Authors details:
1. Corresponding author: Associate Professor, Department of Microbiology, Karwar Institute of Medical Sciences, Karwar- 581301, Karnataka, India; E-mail: [email protected] 2. Tutor, Department of Microbiology, Karwar Institute of Medical Sciences.
Karwar, Karnataka.