Presentation1.pptx, ultrasound study of the spleen and pancreas.
-
Upload
abdellah-nazeer -
Category
Documents
-
view
1.749 -
download
4
Transcript of Presentation1.pptx, ultrasound study of the spleen and pancreas.
Dr ABD ALLAH NAZEER MD
Ultrasound study of the spleen and pancreas
ULTRASOUND OF THE SPLEEN - Normal
Intercostal scan plane Normal Spleen
The size of the spleen can be extremely variable ranging from 7cm- 14cm
Accessory spleens or splenunculi are common
Ultrasound appearanceThe spleen has a homogeneous inverted comma appearance When it becomes enlarged it loses this shape and as it expands it becomes very rounded and sometimes appears as an egg shape extending beyond the Left kidneyMeasurementNormal Spleen Sizelt14 cm superior to inferior axis 6-7cm in the medial to lateral axis 5 to 6cm in the anterior to posterior plane Average volume is approximately 350mls
Normal VariantsAnd congenital anomalies
1-Small spleen2- Asplenia3- Polysplenia4- Splenunculus5- Splenic artery 6- Calcification7- Wandering spleen
Common PathologySplenomegally gt13-14 cm (or Volume gt500cc)and becomes roundedInfection- multiple echogenic foci (granulomata)HaemangiomaCystsMetastasesLymphomaVarices - portal hypertensionHaematomas-intraparenchymal subcapsular and pericapsularAbscessSplenic infarction
Normal spleen Homogenous moderately echogenic Less visible vessels than the liver(No
second set of veins equivalent to portal vein
An accessory spleen (supernumerary spleen splenule or
splenunculus) is a small nodule of splenic tissue found apart from the main body of the spleen Accessory spleens are found in approximately 10 percent of the population and are typically around 1 centimeter in diameter They form either by the result of developmental anomalies or trauma More common with splenomegally Usually solitary and may be multiple
Splenosis is one type of ectopic splenic tissue and spontaneous
transplantation of the splenic tissue at unusual site after splenic traumarupture It is an acquired condition and is defined as autoimplantation one or more focal deposits of splenic tissue in various compartments of the body Nodules of ectopic splenic tissue develop on peritoneal mesenteric surfaces similar to endometriosis deposits
Wandering spleen (Pelvic spleen ectopic ptotic aberrant) is a rare medical disease caused by the loss or weakening of the ligaments that help to hold the spleen stationary They susceptible to torsion around the vascular pedicle
Splenomegaly is a term which refers to enlargement of the spleen The normal adult splenic length upper limit is usually around 12-15 cm The thickness must be less than 6 cm and the spleen is much longer than the left kidney
Splenic pathology
Splenic cyst is either congenital (true cyst) inflammatory (abscesses hydatid cyst) vascular (infarction peliosis) posttraumatic (hematoma false cyst) and neoplastic (hemangioma lymphangioma lymphoma metastasis)
Post traumatic splenic pseudocyst
Echinococcal cyst Hydatid disease is endemic area usually sheep raising areas
Splenic Hydatid Disease
Intraparenchymal splenic hematoma
Subcapsular splenic hematoma
Peri-splenic hematoma
Splenic abscessUsually result of bacterial endocarditis or septicemia IV drug abuse Immunocompromised patients
Splenic abscess with poorly defined hypoechoic and isoechoic area at US images CT show multiple hypodense area at enlarged spleen
Splenic fungal abscess with poorly defined hypoechoic and hypodense area at US and CT images
Splenic artery aneurysmSplenic artery aneurysms are rare but still the third most common abdominal aneurysm after aneurysms of the abdominal aorta and iliac arteries They may occur in pregnant women in the third trimester and rupture carries a maternal mortality of greater than 50 and a fetal mortality of 70 - 90 Risk factors include smoking and hypertension
A splenic artery pseudoaneurysmis rare situation of a pseudoaneurysm forming in relation to the splenic artery It occur after trauma or post-pancreatitis
Spleen infarction - hypoechogenic bearing marked with a white arrow Duplex color sonography was used as well there is no color signal from the ischemic area
Splenic infarct with a wedge shaped non vascularized splenic lesion
Splenic granulomaUS shows hyperechoic foci with posterior tiny shadowSplenic granuloma as a result from previous exposure to histoplasmosis TB and sarcoidosis
Splenic granuloma
Splenic hemangiomas (also known as splenic venous malformations) while being rare lesions are considered the second commonest focal lesion involving the spleen after simple splenic cysts
Splenic hemangioma with a small hyperechoic lesion
Large complex hyperechoic solid hemangioma with scattered hypoechoic foci
Cystic hemangioma
Asymptomatic Splenic Hamartoma with Rapidly Expansive Growth
Hamartomas is a benign primary neoplasm of spleen they are
normally an incidental finding at imaging surgery or autopsy They can occur in any age group Symptoms occur from mass effect if they grow large Most splenic hamartomas are hyperechoic solid masses with or without cystic changes at ultrasound examination
Lymphangioma
Lymphoma with Splenomegally and hypoechoic splenic masses
Splenic lymphoma is often a manifestation of the diffuse dissemination
characteristic of Hodgkins and non-Hodgkins lymphoma Splenic lymphoma may be single or multiple and appears hypoechoic or hyperechoic masses and they are usually associated with hilar lymphadenopathy
Splenic lymphoma with hypoechoic splenic masses
Splenic angiosarcoma is exceedingly rare but it is the most common primary non-hematolymphoid malignant neoplasm of the spleen It is a highly aggressive malignancy with a poor prognosis The majority of patients present with abdominal pain or a palpable abdominal mass
Angiosarcoma of the Spleen
Cystic splenic metastasis Primary tumour is cystic Secondary changes are -Degeneration- Hemorrhage- Necrosis- Infection
Splenic metastasis
ULTRASOUND OF THE PANCREAS ndash Normal
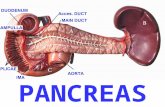
Pancreas Scan Plane Normal Pancreas and surrounding anatomy
Sagittal Scan Plane Pancreatic Head Head of pancreas
Scanning TechniqueTechniqueBegin transversely high in the epigastrumYou may need to apply enough pressure to help displace bowel gasAdjust image depth so the aorta is at the bottom of the screen
Head of pancreas - Use both transverse amp sagittal planes as the head can be quite long and continue left caudally for several centimeters
Body of Pancreas - Transverse probe Use the splenic vein to help identify the pancreas superficial to this
Tail of pancreas - Start with the probe transverse then angle the heel of the probe cephalad and left as the tail can be sitting up under the spleen Thus the spleen can be used as a window and a left intercostal coronal approach can also be utilized
Ultrasound AppearancesNormal appearance is usually homogeneous and almost isoechoic with the liverIt is frequently hyperechoic compared to the liver because of fatty infiltrationSizeVaries with age and historyApproximate normal measurements areHead 35mm (anterior to posterior)Neck 10-15mmTail 20mm
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
ULTRASOUND OF THE SPLEEN - Normal
Intercostal scan plane Normal Spleen
The size of the spleen can be extremely variable ranging from 7cm- 14cm
Accessory spleens or splenunculi are common
Ultrasound appearanceThe spleen has a homogeneous inverted comma appearance When it becomes enlarged it loses this shape and as it expands it becomes very rounded and sometimes appears as an egg shape extending beyond the Left kidneyMeasurementNormal Spleen Sizelt14 cm superior to inferior axis 6-7cm in the medial to lateral axis 5 to 6cm in the anterior to posterior plane Average volume is approximately 350mls
Normal VariantsAnd congenital anomalies
1-Small spleen2- Asplenia3- Polysplenia4- Splenunculus5- Splenic artery 6- Calcification7- Wandering spleen
Common PathologySplenomegally gt13-14 cm (or Volume gt500cc)and becomes roundedInfection- multiple echogenic foci (granulomata)HaemangiomaCystsMetastasesLymphomaVarices - portal hypertensionHaematomas-intraparenchymal subcapsular and pericapsularAbscessSplenic infarction
Normal spleen Homogenous moderately echogenic Less visible vessels than the liver(No
second set of veins equivalent to portal vein
An accessory spleen (supernumerary spleen splenule or
splenunculus) is a small nodule of splenic tissue found apart from the main body of the spleen Accessory spleens are found in approximately 10 percent of the population and are typically around 1 centimeter in diameter They form either by the result of developmental anomalies or trauma More common with splenomegally Usually solitary and may be multiple
Splenosis is one type of ectopic splenic tissue and spontaneous
transplantation of the splenic tissue at unusual site after splenic traumarupture It is an acquired condition and is defined as autoimplantation one or more focal deposits of splenic tissue in various compartments of the body Nodules of ectopic splenic tissue develop on peritoneal mesenteric surfaces similar to endometriosis deposits
Wandering spleen (Pelvic spleen ectopic ptotic aberrant) is a rare medical disease caused by the loss or weakening of the ligaments that help to hold the spleen stationary They susceptible to torsion around the vascular pedicle
Splenomegaly is a term which refers to enlargement of the spleen The normal adult splenic length upper limit is usually around 12-15 cm The thickness must be less than 6 cm and the spleen is much longer than the left kidney
Splenic pathology
Splenic cyst is either congenital (true cyst) inflammatory (abscesses hydatid cyst) vascular (infarction peliosis) posttraumatic (hematoma false cyst) and neoplastic (hemangioma lymphangioma lymphoma metastasis)
Post traumatic splenic pseudocyst
Echinococcal cyst Hydatid disease is endemic area usually sheep raising areas
Splenic Hydatid Disease
Intraparenchymal splenic hematoma
Subcapsular splenic hematoma
Peri-splenic hematoma
Splenic abscessUsually result of bacterial endocarditis or septicemia IV drug abuse Immunocompromised patients
Splenic abscess with poorly defined hypoechoic and isoechoic area at US images CT show multiple hypodense area at enlarged spleen
Splenic fungal abscess with poorly defined hypoechoic and hypodense area at US and CT images
Splenic artery aneurysmSplenic artery aneurysms are rare but still the third most common abdominal aneurysm after aneurysms of the abdominal aorta and iliac arteries They may occur in pregnant women in the third trimester and rupture carries a maternal mortality of greater than 50 and a fetal mortality of 70 - 90 Risk factors include smoking and hypertension
A splenic artery pseudoaneurysmis rare situation of a pseudoaneurysm forming in relation to the splenic artery It occur after trauma or post-pancreatitis
Spleen infarction - hypoechogenic bearing marked with a white arrow Duplex color sonography was used as well there is no color signal from the ischemic area
Splenic infarct with a wedge shaped non vascularized splenic lesion
Splenic granulomaUS shows hyperechoic foci with posterior tiny shadowSplenic granuloma as a result from previous exposure to histoplasmosis TB and sarcoidosis
Splenic granuloma
Splenic hemangiomas (also known as splenic venous malformations) while being rare lesions are considered the second commonest focal lesion involving the spleen after simple splenic cysts
Splenic hemangioma with a small hyperechoic lesion
Large complex hyperechoic solid hemangioma with scattered hypoechoic foci
Cystic hemangioma
Asymptomatic Splenic Hamartoma with Rapidly Expansive Growth
Hamartomas is a benign primary neoplasm of spleen they are
normally an incidental finding at imaging surgery or autopsy They can occur in any age group Symptoms occur from mass effect if they grow large Most splenic hamartomas are hyperechoic solid masses with or without cystic changes at ultrasound examination
Lymphangioma
Lymphoma with Splenomegally and hypoechoic splenic masses
Splenic lymphoma is often a manifestation of the diffuse dissemination
characteristic of Hodgkins and non-Hodgkins lymphoma Splenic lymphoma may be single or multiple and appears hypoechoic or hyperechoic masses and they are usually associated with hilar lymphadenopathy
Splenic lymphoma with hypoechoic splenic masses
Splenic angiosarcoma is exceedingly rare but it is the most common primary non-hematolymphoid malignant neoplasm of the spleen It is a highly aggressive malignancy with a poor prognosis The majority of patients present with abdominal pain or a palpable abdominal mass
Angiosarcoma of the Spleen
Cystic splenic metastasis Primary tumour is cystic Secondary changes are -Degeneration- Hemorrhage- Necrosis- Infection
Splenic metastasis
ULTRASOUND OF THE PANCREAS ndash Normal
Pancreas Scan Plane Normal Pancreas and surrounding anatomy
Sagittal Scan Plane Pancreatic Head Head of pancreas
Scanning TechniqueTechniqueBegin transversely high in the epigastrumYou may need to apply enough pressure to help displace bowel gasAdjust image depth so the aorta is at the bottom of the screen
Head of pancreas - Use both transverse amp sagittal planes as the head can be quite long and continue left caudally for several centimeters
Body of Pancreas - Transverse probe Use the splenic vein to help identify the pancreas superficial to this
Tail of pancreas - Start with the probe transverse then angle the heel of the probe cephalad and left as the tail can be sitting up under the spleen Thus the spleen can be used as a window and a left intercostal coronal approach can also be utilized
Ultrasound AppearancesNormal appearance is usually homogeneous and almost isoechoic with the liverIt is frequently hyperechoic compared to the liver because of fatty infiltrationSizeVaries with age and historyApproximate normal measurements areHead 35mm (anterior to posterior)Neck 10-15mmTail 20mm
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
The size of the spleen can be extremely variable ranging from 7cm- 14cm
Accessory spleens or splenunculi are common
Ultrasound appearanceThe spleen has a homogeneous inverted comma appearance When it becomes enlarged it loses this shape and as it expands it becomes very rounded and sometimes appears as an egg shape extending beyond the Left kidneyMeasurementNormal Spleen Sizelt14 cm superior to inferior axis 6-7cm in the medial to lateral axis 5 to 6cm in the anterior to posterior plane Average volume is approximately 350mls
Normal VariantsAnd congenital anomalies
1-Small spleen2- Asplenia3- Polysplenia4- Splenunculus5- Splenic artery 6- Calcification7- Wandering spleen
Common PathologySplenomegally gt13-14 cm (or Volume gt500cc)and becomes roundedInfection- multiple echogenic foci (granulomata)HaemangiomaCystsMetastasesLymphomaVarices - portal hypertensionHaematomas-intraparenchymal subcapsular and pericapsularAbscessSplenic infarction
Normal spleen Homogenous moderately echogenic Less visible vessels than the liver(No
second set of veins equivalent to portal vein
An accessory spleen (supernumerary spleen splenule or
splenunculus) is a small nodule of splenic tissue found apart from the main body of the spleen Accessory spleens are found in approximately 10 percent of the population and are typically around 1 centimeter in diameter They form either by the result of developmental anomalies or trauma More common with splenomegally Usually solitary and may be multiple
Splenosis is one type of ectopic splenic tissue and spontaneous
transplantation of the splenic tissue at unusual site after splenic traumarupture It is an acquired condition and is defined as autoimplantation one or more focal deposits of splenic tissue in various compartments of the body Nodules of ectopic splenic tissue develop on peritoneal mesenteric surfaces similar to endometriosis deposits
Wandering spleen (Pelvic spleen ectopic ptotic aberrant) is a rare medical disease caused by the loss or weakening of the ligaments that help to hold the spleen stationary They susceptible to torsion around the vascular pedicle
Splenomegaly is a term which refers to enlargement of the spleen The normal adult splenic length upper limit is usually around 12-15 cm The thickness must be less than 6 cm and the spleen is much longer than the left kidney
Splenic pathology
Splenic cyst is either congenital (true cyst) inflammatory (abscesses hydatid cyst) vascular (infarction peliosis) posttraumatic (hematoma false cyst) and neoplastic (hemangioma lymphangioma lymphoma metastasis)
Post traumatic splenic pseudocyst
Echinococcal cyst Hydatid disease is endemic area usually sheep raising areas
Splenic Hydatid Disease
Intraparenchymal splenic hematoma
Subcapsular splenic hematoma
Peri-splenic hematoma
Splenic abscessUsually result of bacterial endocarditis or septicemia IV drug abuse Immunocompromised patients
Splenic abscess with poorly defined hypoechoic and isoechoic area at US images CT show multiple hypodense area at enlarged spleen
Splenic fungal abscess with poorly defined hypoechoic and hypodense area at US and CT images
Splenic artery aneurysmSplenic artery aneurysms are rare but still the third most common abdominal aneurysm after aneurysms of the abdominal aorta and iliac arteries They may occur in pregnant women in the third trimester and rupture carries a maternal mortality of greater than 50 and a fetal mortality of 70 - 90 Risk factors include smoking and hypertension
A splenic artery pseudoaneurysmis rare situation of a pseudoaneurysm forming in relation to the splenic artery It occur after trauma or post-pancreatitis
Spleen infarction - hypoechogenic bearing marked with a white arrow Duplex color sonography was used as well there is no color signal from the ischemic area
Splenic infarct with a wedge shaped non vascularized splenic lesion
Splenic granulomaUS shows hyperechoic foci with posterior tiny shadowSplenic granuloma as a result from previous exposure to histoplasmosis TB and sarcoidosis
Splenic granuloma
Splenic hemangiomas (also known as splenic venous malformations) while being rare lesions are considered the second commonest focal lesion involving the spleen after simple splenic cysts
Splenic hemangioma with a small hyperechoic lesion
Large complex hyperechoic solid hemangioma with scattered hypoechoic foci
Cystic hemangioma
Asymptomatic Splenic Hamartoma with Rapidly Expansive Growth
Hamartomas is a benign primary neoplasm of spleen they are
normally an incidental finding at imaging surgery or autopsy They can occur in any age group Symptoms occur from mass effect if they grow large Most splenic hamartomas are hyperechoic solid masses with or without cystic changes at ultrasound examination
Lymphangioma
Lymphoma with Splenomegally and hypoechoic splenic masses
Splenic lymphoma is often a manifestation of the diffuse dissemination
characteristic of Hodgkins and non-Hodgkins lymphoma Splenic lymphoma may be single or multiple and appears hypoechoic or hyperechoic masses and they are usually associated with hilar lymphadenopathy
Splenic lymphoma with hypoechoic splenic masses
Splenic angiosarcoma is exceedingly rare but it is the most common primary non-hematolymphoid malignant neoplasm of the spleen It is a highly aggressive malignancy with a poor prognosis The majority of patients present with abdominal pain or a palpable abdominal mass
Angiosarcoma of the Spleen
Cystic splenic metastasis Primary tumour is cystic Secondary changes are -Degeneration- Hemorrhage- Necrosis- Infection
Splenic metastasis
ULTRASOUND OF THE PANCREAS ndash Normal
Pancreas Scan Plane Normal Pancreas and surrounding anatomy
Sagittal Scan Plane Pancreatic Head Head of pancreas
Scanning TechniqueTechniqueBegin transversely high in the epigastrumYou may need to apply enough pressure to help displace bowel gasAdjust image depth so the aorta is at the bottom of the screen
Head of pancreas - Use both transverse amp sagittal planes as the head can be quite long and continue left caudally for several centimeters
Body of Pancreas - Transverse probe Use the splenic vein to help identify the pancreas superficial to this
Tail of pancreas - Start with the probe transverse then angle the heel of the probe cephalad and left as the tail can be sitting up under the spleen Thus the spleen can be used as a window and a left intercostal coronal approach can also be utilized
Ultrasound AppearancesNormal appearance is usually homogeneous and almost isoechoic with the liverIt is frequently hyperechoic compared to the liver because of fatty infiltrationSizeVaries with age and historyApproximate normal measurements areHead 35mm (anterior to posterior)Neck 10-15mmTail 20mm
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Ultrasound appearanceThe spleen has a homogeneous inverted comma appearance When it becomes enlarged it loses this shape and as it expands it becomes very rounded and sometimes appears as an egg shape extending beyond the Left kidneyMeasurementNormal Spleen Sizelt14 cm superior to inferior axis 6-7cm in the medial to lateral axis 5 to 6cm in the anterior to posterior plane Average volume is approximately 350mls
Normal VariantsAnd congenital anomalies
1-Small spleen2- Asplenia3- Polysplenia4- Splenunculus5- Splenic artery 6- Calcification7- Wandering spleen
Common PathologySplenomegally gt13-14 cm (or Volume gt500cc)and becomes roundedInfection- multiple echogenic foci (granulomata)HaemangiomaCystsMetastasesLymphomaVarices - portal hypertensionHaematomas-intraparenchymal subcapsular and pericapsularAbscessSplenic infarction
Normal spleen Homogenous moderately echogenic Less visible vessels than the liver(No
second set of veins equivalent to portal vein
An accessory spleen (supernumerary spleen splenule or
splenunculus) is a small nodule of splenic tissue found apart from the main body of the spleen Accessory spleens are found in approximately 10 percent of the population and are typically around 1 centimeter in diameter They form either by the result of developmental anomalies or trauma More common with splenomegally Usually solitary and may be multiple
Splenosis is one type of ectopic splenic tissue and spontaneous
transplantation of the splenic tissue at unusual site after splenic traumarupture It is an acquired condition and is defined as autoimplantation one or more focal deposits of splenic tissue in various compartments of the body Nodules of ectopic splenic tissue develop on peritoneal mesenteric surfaces similar to endometriosis deposits
Wandering spleen (Pelvic spleen ectopic ptotic aberrant) is a rare medical disease caused by the loss or weakening of the ligaments that help to hold the spleen stationary They susceptible to torsion around the vascular pedicle
Splenomegaly is a term which refers to enlargement of the spleen The normal adult splenic length upper limit is usually around 12-15 cm The thickness must be less than 6 cm and the spleen is much longer than the left kidney
Splenic pathology
Splenic cyst is either congenital (true cyst) inflammatory (abscesses hydatid cyst) vascular (infarction peliosis) posttraumatic (hematoma false cyst) and neoplastic (hemangioma lymphangioma lymphoma metastasis)
Post traumatic splenic pseudocyst
Echinococcal cyst Hydatid disease is endemic area usually sheep raising areas
Splenic Hydatid Disease
Intraparenchymal splenic hematoma
Subcapsular splenic hematoma
Peri-splenic hematoma
Splenic abscessUsually result of bacterial endocarditis or septicemia IV drug abuse Immunocompromised patients
Splenic abscess with poorly defined hypoechoic and isoechoic area at US images CT show multiple hypodense area at enlarged spleen
Splenic fungal abscess with poorly defined hypoechoic and hypodense area at US and CT images
Splenic artery aneurysmSplenic artery aneurysms are rare but still the third most common abdominal aneurysm after aneurysms of the abdominal aorta and iliac arteries They may occur in pregnant women in the third trimester and rupture carries a maternal mortality of greater than 50 and a fetal mortality of 70 - 90 Risk factors include smoking and hypertension
A splenic artery pseudoaneurysmis rare situation of a pseudoaneurysm forming in relation to the splenic artery It occur after trauma or post-pancreatitis
Spleen infarction - hypoechogenic bearing marked with a white arrow Duplex color sonography was used as well there is no color signal from the ischemic area
Splenic infarct with a wedge shaped non vascularized splenic lesion
Splenic granulomaUS shows hyperechoic foci with posterior tiny shadowSplenic granuloma as a result from previous exposure to histoplasmosis TB and sarcoidosis
Splenic granuloma
Splenic hemangiomas (also known as splenic venous malformations) while being rare lesions are considered the second commonest focal lesion involving the spleen after simple splenic cysts
Splenic hemangioma with a small hyperechoic lesion
Large complex hyperechoic solid hemangioma with scattered hypoechoic foci
Cystic hemangioma
Asymptomatic Splenic Hamartoma with Rapidly Expansive Growth
Hamartomas is a benign primary neoplasm of spleen they are
normally an incidental finding at imaging surgery or autopsy They can occur in any age group Symptoms occur from mass effect if they grow large Most splenic hamartomas are hyperechoic solid masses with or without cystic changes at ultrasound examination
Lymphangioma
Lymphoma with Splenomegally and hypoechoic splenic masses
Splenic lymphoma is often a manifestation of the diffuse dissemination
characteristic of Hodgkins and non-Hodgkins lymphoma Splenic lymphoma may be single or multiple and appears hypoechoic or hyperechoic masses and they are usually associated with hilar lymphadenopathy
Splenic lymphoma with hypoechoic splenic masses
Splenic angiosarcoma is exceedingly rare but it is the most common primary non-hematolymphoid malignant neoplasm of the spleen It is a highly aggressive malignancy with a poor prognosis The majority of patients present with abdominal pain or a palpable abdominal mass
Angiosarcoma of the Spleen
Cystic splenic metastasis Primary tumour is cystic Secondary changes are -Degeneration- Hemorrhage- Necrosis- Infection
Splenic metastasis
ULTRASOUND OF THE PANCREAS ndash Normal
Pancreas Scan Plane Normal Pancreas and surrounding anatomy
Sagittal Scan Plane Pancreatic Head Head of pancreas
Scanning TechniqueTechniqueBegin transversely high in the epigastrumYou may need to apply enough pressure to help displace bowel gasAdjust image depth so the aorta is at the bottom of the screen
Head of pancreas - Use both transverse amp sagittal planes as the head can be quite long and continue left caudally for several centimeters
Body of Pancreas - Transverse probe Use the splenic vein to help identify the pancreas superficial to this
Tail of pancreas - Start with the probe transverse then angle the heel of the probe cephalad and left as the tail can be sitting up under the spleen Thus the spleen can be used as a window and a left intercostal coronal approach can also be utilized
Ultrasound AppearancesNormal appearance is usually homogeneous and almost isoechoic with the liverIt is frequently hyperechoic compared to the liver because of fatty infiltrationSizeVaries with age and historyApproximate normal measurements areHead 35mm (anterior to posterior)Neck 10-15mmTail 20mm
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Normal VariantsAnd congenital anomalies
1-Small spleen2- Asplenia3- Polysplenia4- Splenunculus5- Splenic artery 6- Calcification7- Wandering spleen
Common PathologySplenomegally gt13-14 cm (or Volume gt500cc)and becomes roundedInfection- multiple echogenic foci (granulomata)HaemangiomaCystsMetastasesLymphomaVarices - portal hypertensionHaematomas-intraparenchymal subcapsular and pericapsularAbscessSplenic infarction
Normal spleen Homogenous moderately echogenic Less visible vessels than the liver(No
second set of veins equivalent to portal vein
An accessory spleen (supernumerary spleen splenule or
splenunculus) is a small nodule of splenic tissue found apart from the main body of the spleen Accessory spleens are found in approximately 10 percent of the population and are typically around 1 centimeter in diameter They form either by the result of developmental anomalies or trauma More common with splenomegally Usually solitary and may be multiple
Splenosis is one type of ectopic splenic tissue and spontaneous
transplantation of the splenic tissue at unusual site after splenic traumarupture It is an acquired condition and is defined as autoimplantation one or more focal deposits of splenic tissue in various compartments of the body Nodules of ectopic splenic tissue develop on peritoneal mesenteric surfaces similar to endometriosis deposits
Wandering spleen (Pelvic spleen ectopic ptotic aberrant) is a rare medical disease caused by the loss or weakening of the ligaments that help to hold the spleen stationary They susceptible to torsion around the vascular pedicle
Splenomegaly is a term which refers to enlargement of the spleen The normal adult splenic length upper limit is usually around 12-15 cm The thickness must be less than 6 cm and the spleen is much longer than the left kidney
Splenic pathology
Splenic cyst is either congenital (true cyst) inflammatory (abscesses hydatid cyst) vascular (infarction peliosis) posttraumatic (hematoma false cyst) and neoplastic (hemangioma lymphangioma lymphoma metastasis)
Post traumatic splenic pseudocyst
Echinococcal cyst Hydatid disease is endemic area usually sheep raising areas
Splenic Hydatid Disease
Intraparenchymal splenic hematoma
Subcapsular splenic hematoma
Peri-splenic hematoma
Splenic abscessUsually result of bacterial endocarditis or septicemia IV drug abuse Immunocompromised patients
Splenic abscess with poorly defined hypoechoic and isoechoic area at US images CT show multiple hypodense area at enlarged spleen
Splenic fungal abscess with poorly defined hypoechoic and hypodense area at US and CT images
Splenic artery aneurysmSplenic artery aneurysms are rare but still the third most common abdominal aneurysm after aneurysms of the abdominal aorta and iliac arteries They may occur in pregnant women in the third trimester and rupture carries a maternal mortality of greater than 50 and a fetal mortality of 70 - 90 Risk factors include smoking and hypertension
A splenic artery pseudoaneurysmis rare situation of a pseudoaneurysm forming in relation to the splenic artery It occur after trauma or post-pancreatitis
Spleen infarction - hypoechogenic bearing marked with a white arrow Duplex color sonography was used as well there is no color signal from the ischemic area
Splenic infarct with a wedge shaped non vascularized splenic lesion
Splenic granulomaUS shows hyperechoic foci with posterior tiny shadowSplenic granuloma as a result from previous exposure to histoplasmosis TB and sarcoidosis
Splenic granuloma
Splenic hemangiomas (also known as splenic venous malformations) while being rare lesions are considered the second commonest focal lesion involving the spleen after simple splenic cysts
Splenic hemangioma with a small hyperechoic lesion
Large complex hyperechoic solid hemangioma with scattered hypoechoic foci
Cystic hemangioma
Asymptomatic Splenic Hamartoma with Rapidly Expansive Growth
Hamartomas is a benign primary neoplasm of spleen they are
normally an incidental finding at imaging surgery or autopsy They can occur in any age group Symptoms occur from mass effect if they grow large Most splenic hamartomas are hyperechoic solid masses with or without cystic changes at ultrasound examination
Lymphangioma
Lymphoma with Splenomegally and hypoechoic splenic masses
Splenic lymphoma is often a manifestation of the diffuse dissemination
characteristic of Hodgkins and non-Hodgkins lymphoma Splenic lymphoma may be single or multiple and appears hypoechoic or hyperechoic masses and they are usually associated with hilar lymphadenopathy
Splenic lymphoma with hypoechoic splenic masses
Splenic angiosarcoma is exceedingly rare but it is the most common primary non-hematolymphoid malignant neoplasm of the spleen It is a highly aggressive malignancy with a poor prognosis The majority of patients present with abdominal pain or a palpable abdominal mass
Angiosarcoma of the Spleen
Cystic splenic metastasis Primary tumour is cystic Secondary changes are -Degeneration- Hemorrhage- Necrosis- Infection
Splenic metastasis
ULTRASOUND OF THE PANCREAS ndash Normal
Pancreas Scan Plane Normal Pancreas and surrounding anatomy
Sagittal Scan Plane Pancreatic Head Head of pancreas
Scanning TechniqueTechniqueBegin transversely high in the epigastrumYou may need to apply enough pressure to help displace bowel gasAdjust image depth so the aorta is at the bottom of the screen
Head of pancreas - Use both transverse amp sagittal planes as the head can be quite long and continue left caudally for several centimeters
Body of Pancreas - Transverse probe Use the splenic vein to help identify the pancreas superficial to this
Tail of pancreas - Start with the probe transverse then angle the heel of the probe cephalad and left as the tail can be sitting up under the spleen Thus the spleen can be used as a window and a left intercostal coronal approach can also be utilized
Ultrasound AppearancesNormal appearance is usually homogeneous and almost isoechoic with the liverIt is frequently hyperechoic compared to the liver because of fatty infiltrationSizeVaries with age and historyApproximate normal measurements areHead 35mm (anterior to posterior)Neck 10-15mmTail 20mm
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Normal spleen Homogenous moderately echogenic Less visible vessels than the liver(No
second set of veins equivalent to portal vein
An accessory spleen (supernumerary spleen splenule or
splenunculus) is a small nodule of splenic tissue found apart from the main body of the spleen Accessory spleens are found in approximately 10 percent of the population and are typically around 1 centimeter in diameter They form either by the result of developmental anomalies or trauma More common with splenomegally Usually solitary and may be multiple
Splenosis is one type of ectopic splenic tissue and spontaneous
transplantation of the splenic tissue at unusual site after splenic traumarupture It is an acquired condition and is defined as autoimplantation one or more focal deposits of splenic tissue in various compartments of the body Nodules of ectopic splenic tissue develop on peritoneal mesenteric surfaces similar to endometriosis deposits
Wandering spleen (Pelvic spleen ectopic ptotic aberrant) is a rare medical disease caused by the loss or weakening of the ligaments that help to hold the spleen stationary They susceptible to torsion around the vascular pedicle
Splenomegaly is a term which refers to enlargement of the spleen The normal adult splenic length upper limit is usually around 12-15 cm The thickness must be less than 6 cm and the spleen is much longer than the left kidney
Splenic pathology
Splenic cyst is either congenital (true cyst) inflammatory (abscesses hydatid cyst) vascular (infarction peliosis) posttraumatic (hematoma false cyst) and neoplastic (hemangioma lymphangioma lymphoma metastasis)
Post traumatic splenic pseudocyst
Echinococcal cyst Hydatid disease is endemic area usually sheep raising areas
Splenic Hydatid Disease
Intraparenchymal splenic hematoma
Subcapsular splenic hematoma
Peri-splenic hematoma
Splenic abscessUsually result of bacterial endocarditis or septicemia IV drug abuse Immunocompromised patients
Splenic abscess with poorly defined hypoechoic and isoechoic area at US images CT show multiple hypodense area at enlarged spleen
Splenic fungal abscess with poorly defined hypoechoic and hypodense area at US and CT images
Splenic artery aneurysmSplenic artery aneurysms are rare but still the third most common abdominal aneurysm after aneurysms of the abdominal aorta and iliac arteries They may occur in pregnant women in the third trimester and rupture carries a maternal mortality of greater than 50 and a fetal mortality of 70 - 90 Risk factors include smoking and hypertension
A splenic artery pseudoaneurysmis rare situation of a pseudoaneurysm forming in relation to the splenic artery It occur after trauma or post-pancreatitis
Spleen infarction - hypoechogenic bearing marked with a white arrow Duplex color sonography was used as well there is no color signal from the ischemic area
Splenic infarct with a wedge shaped non vascularized splenic lesion
Splenic granulomaUS shows hyperechoic foci with posterior tiny shadowSplenic granuloma as a result from previous exposure to histoplasmosis TB and sarcoidosis
Splenic granuloma
Splenic hemangiomas (also known as splenic venous malformations) while being rare lesions are considered the second commonest focal lesion involving the spleen after simple splenic cysts
Splenic hemangioma with a small hyperechoic lesion
Large complex hyperechoic solid hemangioma with scattered hypoechoic foci
Cystic hemangioma
Asymptomatic Splenic Hamartoma with Rapidly Expansive Growth
Hamartomas is a benign primary neoplasm of spleen they are
normally an incidental finding at imaging surgery or autopsy They can occur in any age group Symptoms occur from mass effect if they grow large Most splenic hamartomas are hyperechoic solid masses with or without cystic changes at ultrasound examination
Lymphangioma
Lymphoma with Splenomegally and hypoechoic splenic masses
Splenic lymphoma is often a manifestation of the diffuse dissemination
characteristic of Hodgkins and non-Hodgkins lymphoma Splenic lymphoma may be single or multiple and appears hypoechoic or hyperechoic masses and they are usually associated with hilar lymphadenopathy
Splenic lymphoma with hypoechoic splenic masses
Splenic angiosarcoma is exceedingly rare but it is the most common primary non-hematolymphoid malignant neoplasm of the spleen It is a highly aggressive malignancy with a poor prognosis The majority of patients present with abdominal pain or a palpable abdominal mass
Angiosarcoma of the Spleen
Cystic splenic metastasis Primary tumour is cystic Secondary changes are -Degeneration- Hemorrhage- Necrosis- Infection
Splenic metastasis
ULTRASOUND OF THE PANCREAS ndash Normal
Pancreas Scan Plane Normal Pancreas and surrounding anatomy
Sagittal Scan Plane Pancreatic Head Head of pancreas
Scanning TechniqueTechniqueBegin transversely high in the epigastrumYou may need to apply enough pressure to help displace bowel gasAdjust image depth so the aorta is at the bottom of the screen
Head of pancreas - Use both transverse amp sagittal planes as the head can be quite long and continue left caudally for several centimeters
Body of Pancreas - Transverse probe Use the splenic vein to help identify the pancreas superficial to this
Tail of pancreas - Start with the probe transverse then angle the heel of the probe cephalad and left as the tail can be sitting up under the spleen Thus the spleen can be used as a window and a left intercostal coronal approach can also be utilized
Ultrasound AppearancesNormal appearance is usually homogeneous and almost isoechoic with the liverIt is frequently hyperechoic compared to the liver because of fatty infiltrationSizeVaries with age and historyApproximate normal measurements areHead 35mm (anterior to posterior)Neck 10-15mmTail 20mm
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
An accessory spleen (supernumerary spleen splenule or
splenunculus) is a small nodule of splenic tissue found apart from the main body of the spleen Accessory spleens are found in approximately 10 percent of the population and are typically around 1 centimeter in diameter They form either by the result of developmental anomalies or trauma More common with splenomegally Usually solitary and may be multiple
Splenosis is one type of ectopic splenic tissue and spontaneous
transplantation of the splenic tissue at unusual site after splenic traumarupture It is an acquired condition and is defined as autoimplantation one or more focal deposits of splenic tissue in various compartments of the body Nodules of ectopic splenic tissue develop on peritoneal mesenteric surfaces similar to endometriosis deposits
Wandering spleen (Pelvic spleen ectopic ptotic aberrant) is a rare medical disease caused by the loss or weakening of the ligaments that help to hold the spleen stationary They susceptible to torsion around the vascular pedicle
Splenomegaly is a term which refers to enlargement of the spleen The normal adult splenic length upper limit is usually around 12-15 cm The thickness must be less than 6 cm and the spleen is much longer than the left kidney
Splenic pathology
Splenic cyst is either congenital (true cyst) inflammatory (abscesses hydatid cyst) vascular (infarction peliosis) posttraumatic (hematoma false cyst) and neoplastic (hemangioma lymphangioma lymphoma metastasis)
Post traumatic splenic pseudocyst
Echinococcal cyst Hydatid disease is endemic area usually sheep raising areas
Splenic Hydatid Disease
Intraparenchymal splenic hematoma
Subcapsular splenic hematoma
Peri-splenic hematoma
Splenic abscessUsually result of bacterial endocarditis or septicemia IV drug abuse Immunocompromised patients
Splenic abscess with poorly defined hypoechoic and isoechoic area at US images CT show multiple hypodense area at enlarged spleen
Splenic fungal abscess with poorly defined hypoechoic and hypodense area at US and CT images
Splenic artery aneurysmSplenic artery aneurysms are rare but still the third most common abdominal aneurysm after aneurysms of the abdominal aorta and iliac arteries They may occur in pregnant women in the third trimester and rupture carries a maternal mortality of greater than 50 and a fetal mortality of 70 - 90 Risk factors include smoking and hypertension
A splenic artery pseudoaneurysmis rare situation of a pseudoaneurysm forming in relation to the splenic artery It occur after trauma or post-pancreatitis
Spleen infarction - hypoechogenic bearing marked with a white arrow Duplex color sonography was used as well there is no color signal from the ischemic area
Splenic infarct with a wedge shaped non vascularized splenic lesion
Splenic granulomaUS shows hyperechoic foci with posterior tiny shadowSplenic granuloma as a result from previous exposure to histoplasmosis TB and sarcoidosis
Splenic granuloma
Splenic hemangiomas (also known as splenic venous malformations) while being rare lesions are considered the second commonest focal lesion involving the spleen after simple splenic cysts
Splenic hemangioma with a small hyperechoic lesion
Large complex hyperechoic solid hemangioma with scattered hypoechoic foci
Cystic hemangioma
Asymptomatic Splenic Hamartoma with Rapidly Expansive Growth
Hamartomas is a benign primary neoplasm of spleen they are
normally an incidental finding at imaging surgery or autopsy They can occur in any age group Symptoms occur from mass effect if they grow large Most splenic hamartomas are hyperechoic solid masses with or without cystic changes at ultrasound examination
Lymphangioma
Lymphoma with Splenomegally and hypoechoic splenic masses
Splenic lymphoma is often a manifestation of the diffuse dissemination
characteristic of Hodgkins and non-Hodgkins lymphoma Splenic lymphoma may be single or multiple and appears hypoechoic or hyperechoic masses and they are usually associated with hilar lymphadenopathy
Splenic lymphoma with hypoechoic splenic masses
Splenic angiosarcoma is exceedingly rare but it is the most common primary non-hematolymphoid malignant neoplasm of the spleen It is a highly aggressive malignancy with a poor prognosis The majority of patients present with abdominal pain or a palpable abdominal mass
Angiosarcoma of the Spleen
Cystic splenic metastasis Primary tumour is cystic Secondary changes are -Degeneration- Hemorrhage- Necrosis- Infection
Splenic metastasis
ULTRASOUND OF THE PANCREAS ndash Normal
Pancreas Scan Plane Normal Pancreas and surrounding anatomy
Sagittal Scan Plane Pancreatic Head Head of pancreas
Scanning TechniqueTechniqueBegin transversely high in the epigastrumYou may need to apply enough pressure to help displace bowel gasAdjust image depth so the aorta is at the bottom of the screen
Head of pancreas - Use both transverse amp sagittal planes as the head can be quite long and continue left caudally for several centimeters
Body of Pancreas - Transverse probe Use the splenic vein to help identify the pancreas superficial to this
Tail of pancreas - Start with the probe transverse then angle the heel of the probe cephalad and left as the tail can be sitting up under the spleen Thus the spleen can be used as a window and a left intercostal coronal approach can also be utilized
Ultrasound AppearancesNormal appearance is usually homogeneous and almost isoechoic with the liverIt is frequently hyperechoic compared to the liver because of fatty infiltrationSizeVaries with age and historyApproximate normal measurements areHead 35mm (anterior to posterior)Neck 10-15mmTail 20mm
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Splenosis is one type of ectopic splenic tissue and spontaneous
transplantation of the splenic tissue at unusual site after splenic traumarupture It is an acquired condition and is defined as autoimplantation one or more focal deposits of splenic tissue in various compartments of the body Nodules of ectopic splenic tissue develop on peritoneal mesenteric surfaces similar to endometriosis deposits
Wandering spleen (Pelvic spleen ectopic ptotic aberrant) is a rare medical disease caused by the loss or weakening of the ligaments that help to hold the spleen stationary They susceptible to torsion around the vascular pedicle
Splenomegaly is a term which refers to enlargement of the spleen The normal adult splenic length upper limit is usually around 12-15 cm The thickness must be less than 6 cm and the spleen is much longer than the left kidney
Splenic pathology
Splenic cyst is either congenital (true cyst) inflammatory (abscesses hydatid cyst) vascular (infarction peliosis) posttraumatic (hematoma false cyst) and neoplastic (hemangioma lymphangioma lymphoma metastasis)
Post traumatic splenic pseudocyst
Echinococcal cyst Hydatid disease is endemic area usually sheep raising areas
Splenic Hydatid Disease
Intraparenchymal splenic hematoma
Subcapsular splenic hematoma
Peri-splenic hematoma
Splenic abscessUsually result of bacterial endocarditis or septicemia IV drug abuse Immunocompromised patients
Splenic abscess with poorly defined hypoechoic and isoechoic area at US images CT show multiple hypodense area at enlarged spleen
Splenic fungal abscess with poorly defined hypoechoic and hypodense area at US and CT images
Splenic artery aneurysmSplenic artery aneurysms are rare but still the third most common abdominal aneurysm after aneurysms of the abdominal aorta and iliac arteries They may occur in pregnant women in the third trimester and rupture carries a maternal mortality of greater than 50 and a fetal mortality of 70 - 90 Risk factors include smoking and hypertension
A splenic artery pseudoaneurysmis rare situation of a pseudoaneurysm forming in relation to the splenic artery It occur after trauma or post-pancreatitis
Spleen infarction - hypoechogenic bearing marked with a white arrow Duplex color sonography was used as well there is no color signal from the ischemic area
Splenic infarct with a wedge shaped non vascularized splenic lesion
Splenic granulomaUS shows hyperechoic foci with posterior tiny shadowSplenic granuloma as a result from previous exposure to histoplasmosis TB and sarcoidosis
Splenic granuloma
Splenic hemangiomas (also known as splenic venous malformations) while being rare lesions are considered the second commonest focal lesion involving the spleen after simple splenic cysts
Splenic hemangioma with a small hyperechoic lesion
Large complex hyperechoic solid hemangioma with scattered hypoechoic foci
Cystic hemangioma
Asymptomatic Splenic Hamartoma with Rapidly Expansive Growth
Hamartomas is a benign primary neoplasm of spleen they are
normally an incidental finding at imaging surgery or autopsy They can occur in any age group Symptoms occur from mass effect if they grow large Most splenic hamartomas are hyperechoic solid masses with or without cystic changes at ultrasound examination
Lymphangioma
Lymphoma with Splenomegally and hypoechoic splenic masses
Splenic lymphoma is often a manifestation of the diffuse dissemination
characteristic of Hodgkins and non-Hodgkins lymphoma Splenic lymphoma may be single or multiple and appears hypoechoic or hyperechoic masses and they are usually associated with hilar lymphadenopathy
Splenic lymphoma with hypoechoic splenic masses
Splenic angiosarcoma is exceedingly rare but it is the most common primary non-hematolymphoid malignant neoplasm of the spleen It is a highly aggressive malignancy with a poor prognosis The majority of patients present with abdominal pain or a palpable abdominal mass
Angiosarcoma of the Spleen
Cystic splenic metastasis Primary tumour is cystic Secondary changes are -Degeneration- Hemorrhage- Necrosis- Infection
Splenic metastasis
ULTRASOUND OF THE PANCREAS ndash Normal
Pancreas Scan Plane Normal Pancreas and surrounding anatomy
Sagittal Scan Plane Pancreatic Head Head of pancreas
Scanning TechniqueTechniqueBegin transversely high in the epigastrumYou may need to apply enough pressure to help displace bowel gasAdjust image depth so the aorta is at the bottom of the screen
Head of pancreas - Use both transverse amp sagittal planes as the head can be quite long and continue left caudally for several centimeters
Body of Pancreas - Transverse probe Use the splenic vein to help identify the pancreas superficial to this
Tail of pancreas - Start with the probe transverse then angle the heel of the probe cephalad and left as the tail can be sitting up under the spleen Thus the spleen can be used as a window and a left intercostal coronal approach can also be utilized
Ultrasound AppearancesNormal appearance is usually homogeneous and almost isoechoic with the liverIt is frequently hyperechoic compared to the liver because of fatty infiltrationSizeVaries with age and historyApproximate normal measurements areHead 35mm (anterior to posterior)Neck 10-15mmTail 20mm
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Wandering spleen (Pelvic spleen ectopic ptotic aberrant) is a rare medical disease caused by the loss or weakening of the ligaments that help to hold the spleen stationary They susceptible to torsion around the vascular pedicle
Splenomegaly is a term which refers to enlargement of the spleen The normal adult splenic length upper limit is usually around 12-15 cm The thickness must be less than 6 cm and the spleen is much longer than the left kidney
Splenic pathology
Splenic cyst is either congenital (true cyst) inflammatory (abscesses hydatid cyst) vascular (infarction peliosis) posttraumatic (hematoma false cyst) and neoplastic (hemangioma lymphangioma lymphoma metastasis)
Post traumatic splenic pseudocyst
Echinococcal cyst Hydatid disease is endemic area usually sheep raising areas
Splenic Hydatid Disease
Intraparenchymal splenic hematoma
Subcapsular splenic hematoma
Peri-splenic hematoma
Splenic abscessUsually result of bacterial endocarditis or septicemia IV drug abuse Immunocompromised patients
Splenic abscess with poorly defined hypoechoic and isoechoic area at US images CT show multiple hypodense area at enlarged spleen
Splenic fungal abscess with poorly defined hypoechoic and hypodense area at US and CT images
Splenic artery aneurysmSplenic artery aneurysms are rare but still the third most common abdominal aneurysm after aneurysms of the abdominal aorta and iliac arteries They may occur in pregnant women in the third trimester and rupture carries a maternal mortality of greater than 50 and a fetal mortality of 70 - 90 Risk factors include smoking and hypertension
A splenic artery pseudoaneurysmis rare situation of a pseudoaneurysm forming in relation to the splenic artery It occur after trauma or post-pancreatitis
Spleen infarction - hypoechogenic bearing marked with a white arrow Duplex color sonography was used as well there is no color signal from the ischemic area
Splenic infarct with a wedge shaped non vascularized splenic lesion
Splenic granulomaUS shows hyperechoic foci with posterior tiny shadowSplenic granuloma as a result from previous exposure to histoplasmosis TB and sarcoidosis
Splenic granuloma
Splenic hemangiomas (also known as splenic venous malformations) while being rare lesions are considered the second commonest focal lesion involving the spleen after simple splenic cysts
Splenic hemangioma with a small hyperechoic lesion
Large complex hyperechoic solid hemangioma with scattered hypoechoic foci
Cystic hemangioma
Asymptomatic Splenic Hamartoma with Rapidly Expansive Growth
Hamartomas is a benign primary neoplasm of spleen they are
normally an incidental finding at imaging surgery or autopsy They can occur in any age group Symptoms occur from mass effect if they grow large Most splenic hamartomas are hyperechoic solid masses with or without cystic changes at ultrasound examination
Lymphangioma
Lymphoma with Splenomegally and hypoechoic splenic masses
Splenic lymphoma is often a manifestation of the diffuse dissemination
characteristic of Hodgkins and non-Hodgkins lymphoma Splenic lymphoma may be single or multiple and appears hypoechoic or hyperechoic masses and they are usually associated with hilar lymphadenopathy
Splenic lymphoma with hypoechoic splenic masses
Splenic angiosarcoma is exceedingly rare but it is the most common primary non-hematolymphoid malignant neoplasm of the spleen It is a highly aggressive malignancy with a poor prognosis The majority of patients present with abdominal pain or a palpable abdominal mass
Angiosarcoma of the Spleen
Cystic splenic metastasis Primary tumour is cystic Secondary changes are -Degeneration- Hemorrhage- Necrosis- Infection
Splenic metastasis
ULTRASOUND OF THE PANCREAS ndash Normal
Pancreas Scan Plane Normal Pancreas and surrounding anatomy
Sagittal Scan Plane Pancreatic Head Head of pancreas
Scanning TechniqueTechniqueBegin transversely high in the epigastrumYou may need to apply enough pressure to help displace bowel gasAdjust image depth so the aorta is at the bottom of the screen
Head of pancreas - Use both transverse amp sagittal planes as the head can be quite long and continue left caudally for several centimeters
Body of Pancreas - Transverse probe Use the splenic vein to help identify the pancreas superficial to this
Tail of pancreas - Start with the probe transverse then angle the heel of the probe cephalad and left as the tail can be sitting up under the spleen Thus the spleen can be used as a window and a left intercostal coronal approach can also be utilized
Ultrasound AppearancesNormal appearance is usually homogeneous and almost isoechoic with the liverIt is frequently hyperechoic compared to the liver because of fatty infiltrationSizeVaries with age and historyApproximate normal measurements areHead 35mm (anterior to posterior)Neck 10-15mmTail 20mm
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Splenomegaly is a term which refers to enlargement of the spleen The normal adult splenic length upper limit is usually around 12-15 cm The thickness must be less than 6 cm and the spleen is much longer than the left kidney
Splenic pathology
Splenic cyst is either congenital (true cyst) inflammatory (abscesses hydatid cyst) vascular (infarction peliosis) posttraumatic (hematoma false cyst) and neoplastic (hemangioma lymphangioma lymphoma metastasis)
Post traumatic splenic pseudocyst
Echinococcal cyst Hydatid disease is endemic area usually sheep raising areas
Splenic Hydatid Disease
Intraparenchymal splenic hematoma
Subcapsular splenic hematoma
Peri-splenic hematoma
Splenic abscessUsually result of bacterial endocarditis or septicemia IV drug abuse Immunocompromised patients
Splenic abscess with poorly defined hypoechoic and isoechoic area at US images CT show multiple hypodense area at enlarged spleen
Splenic fungal abscess with poorly defined hypoechoic and hypodense area at US and CT images
Splenic artery aneurysmSplenic artery aneurysms are rare but still the third most common abdominal aneurysm after aneurysms of the abdominal aorta and iliac arteries They may occur in pregnant women in the third trimester and rupture carries a maternal mortality of greater than 50 and a fetal mortality of 70 - 90 Risk factors include smoking and hypertension
A splenic artery pseudoaneurysmis rare situation of a pseudoaneurysm forming in relation to the splenic artery It occur after trauma or post-pancreatitis
Spleen infarction - hypoechogenic bearing marked with a white arrow Duplex color sonography was used as well there is no color signal from the ischemic area
Splenic infarct with a wedge shaped non vascularized splenic lesion
Splenic granulomaUS shows hyperechoic foci with posterior tiny shadowSplenic granuloma as a result from previous exposure to histoplasmosis TB and sarcoidosis
Splenic granuloma
Splenic hemangiomas (also known as splenic venous malformations) while being rare lesions are considered the second commonest focal lesion involving the spleen after simple splenic cysts
Splenic hemangioma with a small hyperechoic lesion
Large complex hyperechoic solid hemangioma with scattered hypoechoic foci
Cystic hemangioma
Asymptomatic Splenic Hamartoma with Rapidly Expansive Growth
Hamartomas is a benign primary neoplasm of spleen they are
normally an incidental finding at imaging surgery or autopsy They can occur in any age group Symptoms occur from mass effect if they grow large Most splenic hamartomas are hyperechoic solid masses with or without cystic changes at ultrasound examination
Lymphangioma
Lymphoma with Splenomegally and hypoechoic splenic masses
Splenic lymphoma is often a manifestation of the diffuse dissemination
characteristic of Hodgkins and non-Hodgkins lymphoma Splenic lymphoma may be single or multiple and appears hypoechoic or hyperechoic masses and they are usually associated with hilar lymphadenopathy
Splenic lymphoma with hypoechoic splenic masses
Splenic angiosarcoma is exceedingly rare but it is the most common primary non-hematolymphoid malignant neoplasm of the spleen It is a highly aggressive malignancy with a poor prognosis The majority of patients present with abdominal pain or a palpable abdominal mass
Angiosarcoma of the Spleen
Cystic splenic metastasis Primary tumour is cystic Secondary changes are -Degeneration- Hemorrhage- Necrosis- Infection
Splenic metastasis
ULTRASOUND OF THE PANCREAS ndash Normal
Pancreas Scan Plane Normal Pancreas and surrounding anatomy
Sagittal Scan Plane Pancreatic Head Head of pancreas
Scanning TechniqueTechniqueBegin transversely high in the epigastrumYou may need to apply enough pressure to help displace bowel gasAdjust image depth so the aorta is at the bottom of the screen
Head of pancreas - Use both transverse amp sagittal planes as the head can be quite long and continue left caudally for several centimeters
Body of Pancreas - Transverse probe Use the splenic vein to help identify the pancreas superficial to this
Tail of pancreas - Start with the probe transverse then angle the heel of the probe cephalad and left as the tail can be sitting up under the spleen Thus the spleen can be used as a window and a left intercostal coronal approach can also be utilized
Ultrasound AppearancesNormal appearance is usually homogeneous and almost isoechoic with the liverIt is frequently hyperechoic compared to the liver because of fatty infiltrationSizeVaries with age and historyApproximate normal measurements areHead 35mm (anterior to posterior)Neck 10-15mmTail 20mm
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Splenic pathology
Splenic cyst is either congenital (true cyst) inflammatory (abscesses hydatid cyst) vascular (infarction peliosis) posttraumatic (hematoma false cyst) and neoplastic (hemangioma lymphangioma lymphoma metastasis)
Post traumatic splenic pseudocyst
Echinococcal cyst Hydatid disease is endemic area usually sheep raising areas
Splenic Hydatid Disease
Intraparenchymal splenic hematoma
Subcapsular splenic hematoma
Peri-splenic hematoma
Splenic abscessUsually result of bacterial endocarditis or septicemia IV drug abuse Immunocompromised patients
Splenic abscess with poorly defined hypoechoic and isoechoic area at US images CT show multiple hypodense area at enlarged spleen
Splenic fungal abscess with poorly defined hypoechoic and hypodense area at US and CT images
Splenic artery aneurysmSplenic artery aneurysms are rare but still the third most common abdominal aneurysm after aneurysms of the abdominal aorta and iliac arteries They may occur in pregnant women in the third trimester and rupture carries a maternal mortality of greater than 50 and a fetal mortality of 70 - 90 Risk factors include smoking and hypertension
A splenic artery pseudoaneurysmis rare situation of a pseudoaneurysm forming in relation to the splenic artery It occur after trauma or post-pancreatitis
Spleen infarction - hypoechogenic bearing marked with a white arrow Duplex color sonography was used as well there is no color signal from the ischemic area
Splenic infarct with a wedge shaped non vascularized splenic lesion
Splenic granulomaUS shows hyperechoic foci with posterior tiny shadowSplenic granuloma as a result from previous exposure to histoplasmosis TB and sarcoidosis
Splenic granuloma
Splenic hemangiomas (also known as splenic venous malformations) while being rare lesions are considered the second commonest focal lesion involving the spleen after simple splenic cysts
Splenic hemangioma with a small hyperechoic lesion
Large complex hyperechoic solid hemangioma with scattered hypoechoic foci
Cystic hemangioma
Asymptomatic Splenic Hamartoma with Rapidly Expansive Growth
Hamartomas is a benign primary neoplasm of spleen they are
normally an incidental finding at imaging surgery or autopsy They can occur in any age group Symptoms occur from mass effect if they grow large Most splenic hamartomas are hyperechoic solid masses with or without cystic changes at ultrasound examination
Lymphangioma
Lymphoma with Splenomegally and hypoechoic splenic masses
Splenic lymphoma is often a manifestation of the diffuse dissemination
characteristic of Hodgkins and non-Hodgkins lymphoma Splenic lymphoma may be single or multiple and appears hypoechoic or hyperechoic masses and they are usually associated with hilar lymphadenopathy
Splenic lymphoma with hypoechoic splenic masses
Splenic angiosarcoma is exceedingly rare but it is the most common primary non-hematolymphoid malignant neoplasm of the spleen It is a highly aggressive malignancy with a poor prognosis The majority of patients present with abdominal pain or a palpable abdominal mass
Angiosarcoma of the Spleen
Cystic splenic metastasis Primary tumour is cystic Secondary changes are -Degeneration- Hemorrhage- Necrosis- Infection
Splenic metastasis
ULTRASOUND OF THE PANCREAS ndash Normal
Pancreas Scan Plane Normal Pancreas and surrounding anatomy
Sagittal Scan Plane Pancreatic Head Head of pancreas
Scanning TechniqueTechniqueBegin transversely high in the epigastrumYou may need to apply enough pressure to help displace bowel gasAdjust image depth so the aorta is at the bottom of the screen
Head of pancreas - Use both transverse amp sagittal planes as the head can be quite long and continue left caudally for several centimeters
Body of Pancreas - Transverse probe Use the splenic vein to help identify the pancreas superficial to this
Tail of pancreas - Start with the probe transverse then angle the heel of the probe cephalad and left as the tail can be sitting up under the spleen Thus the spleen can be used as a window and a left intercostal coronal approach can also be utilized
Ultrasound AppearancesNormal appearance is usually homogeneous and almost isoechoic with the liverIt is frequently hyperechoic compared to the liver because of fatty infiltrationSizeVaries with age and historyApproximate normal measurements areHead 35mm (anterior to posterior)Neck 10-15mmTail 20mm
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Splenic cyst is either congenital (true cyst) inflammatory (abscesses hydatid cyst) vascular (infarction peliosis) posttraumatic (hematoma false cyst) and neoplastic (hemangioma lymphangioma lymphoma metastasis)
Post traumatic splenic pseudocyst
Echinococcal cyst Hydatid disease is endemic area usually sheep raising areas
Splenic Hydatid Disease
Intraparenchymal splenic hematoma
Subcapsular splenic hematoma
Peri-splenic hematoma
Splenic abscessUsually result of bacterial endocarditis or septicemia IV drug abuse Immunocompromised patients
Splenic abscess with poorly defined hypoechoic and isoechoic area at US images CT show multiple hypodense area at enlarged spleen
Splenic fungal abscess with poorly defined hypoechoic and hypodense area at US and CT images
Splenic artery aneurysmSplenic artery aneurysms are rare but still the third most common abdominal aneurysm after aneurysms of the abdominal aorta and iliac arteries They may occur in pregnant women in the third trimester and rupture carries a maternal mortality of greater than 50 and a fetal mortality of 70 - 90 Risk factors include smoking and hypertension
A splenic artery pseudoaneurysmis rare situation of a pseudoaneurysm forming in relation to the splenic artery It occur after trauma or post-pancreatitis
Spleen infarction - hypoechogenic bearing marked with a white arrow Duplex color sonography was used as well there is no color signal from the ischemic area
Splenic infarct with a wedge shaped non vascularized splenic lesion
Splenic granulomaUS shows hyperechoic foci with posterior tiny shadowSplenic granuloma as a result from previous exposure to histoplasmosis TB and sarcoidosis
Splenic granuloma
Splenic hemangiomas (also known as splenic venous malformations) while being rare lesions are considered the second commonest focal lesion involving the spleen after simple splenic cysts
Splenic hemangioma with a small hyperechoic lesion
Large complex hyperechoic solid hemangioma with scattered hypoechoic foci
Cystic hemangioma
Asymptomatic Splenic Hamartoma with Rapidly Expansive Growth
Hamartomas is a benign primary neoplasm of spleen they are
normally an incidental finding at imaging surgery or autopsy They can occur in any age group Symptoms occur from mass effect if they grow large Most splenic hamartomas are hyperechoic solid masses with or without cystic changes at ultrasound examination
Lymphangioma
Lymphoma with Splenomegally and hypoechoic splenic masses
Splenic lymphoma is often a manifestation of the diffuse dissemination
characteristic of Hodgkins and non-Hodgkins lymphoma Splenic lymphoma may be single or multiple and appears hypoechoic or hyperechoic masses and they are usually associated with hilar lymphadenopathy
Splenic lymphoma with hypoechoic splenic masses
Splenic angiosarcoma is exceedingly rare but it is the most common primary non-hematolymphoid malignant neoplasm of the spleen It is a highly aggressive malignancy with a poor prognosis The majority of patients present with abdominal pain or a palpable abdominal mass
Angiosarcoma of the Spleen
Cystic splenic metastasis Primary tumour is cystic Secondary changes are -Degeneration- Hemorrhage- Necrosis- Infection
Splenic metastasis
ULTRASOUND OF THE PANCREAS ndash Normal
Pancreas Scan Plane Normal Pancreas and surrounding anatomy
Sagittal Scan Plane Pancreatic Head Head of pancreas
Scanning TechniqueTechniqueBegin transversely high in the epigastrumYou may need to apply enough pressure to help displace bowel gasAdjust image depth so the aorta is at the bottom of the screen
Head of pancreas - Use both transverse amp sagittal planes as the head can be quite long and continue left caudally for several centimeters
Body of Pancreas - Transverse probe Use the splenic vein to help identify the pancreas superficial to this
Tail of pancreas - Start with the probe transverse then angle the heel of the probe cephalad and left as the tail can be sitting up under the spleen Thus the spleen can be used as a window and a left intercostal coronal approach can also be utilized
Ultrasound AppearancesNormal appearance is usually homogeneous and almost isoechoic with the liverIt is frequently hyperechoic compared to the liver because of fatty infiltrationSizeVaries with age and historyApproximate normal measurements areHead 35mm (anterior to posterior)Neck 10-15mmTail 20mm
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Post traumatic splenic pseudocyst
Echinococcal cyst Hydatid disease is endemic area usually sheep raising areas
Splenic Hydatid Disease
Intraparenchymal splenic hematoma
Subcapsular splenic hematoma
Peri-splenic hematoma
Splenic abscessUsually result of bacterial endocarditis or septicemia IV drug abuse Immunocompromised patients
Splenic abscess with poorly defined hypoechoic and isoechoic area at US images CT show multiple hypodense area at enlarged spleen
Splenic fungal abscess with poorly defined hypoechoic and hypodense area at US and CT images
Splenic artery aneurysmSplenic artery aneurysms are rare but still the third most common abdominal aneurysm after aneurysms of the abdominal aorta and iliac arteries They may occur in pregnant women in the third trimester and rupture carries a maternal mortality of greater than 50 and a fetal mortality of 70 - 90 Risk factors include smoking and hypertension
A splenic artery pseudoaneurysmis rare situation of a pseudoaneurysm forming in relation to the splenic artery It occur after trauma or post-pancreatitis
Spleen infarction - hypoechogenic bearing marked with a white arrow Duplex color sonography was used as well there is no color signal from the ischemic area
Splenic infarct with a wedge shaped non vascularized splenic lesion
Splenic granulomaUS shows hyperechoic foci with posterior tiny shadowSplenic granuloma as a result from previous exposure to histoplasmosis TB and sarcoidosis
Splenic granuloma
Splenic hemangiomas (also known as splenic venous malformations) while being rare lesions are considered the second commonest focal lesion involving the spleen after simple splenic cysts
Splenic hemangioma with a small hyperechoic lesion
Large complex hyperechoic solid hemangioma with scattered hypoechoic foci
Cystic hemangioma
Asymptomatic Splenic Hamartoma with Rapidly Expansive Growth
Hamartomas is a benign primary neoplasm of spleen they are
normally an incidental finding at imaging surgery or autopsy They can occur in any age group Symptoms occur from mass effect if they grow large Most splenic hamartomas are hyperechoic solid masses with or without cystic changes at ultrasound examination
Lymphangioma
Lymphoma with Splenomegally and hypoechoic splenic masses
Splenic lymphoma is often a manifestation of the diffuse dissemination
characteristic of Hodgkins and non-Hodgkins lymphoma Splenic lymphoma may be single or multiple and appears hypoechoic or hyperechoic masses and they are usually associated with hilar lymphadenopathy
Splenic lymphoma with hypoechoic splenic masses
Splenic angiosarcoma is exceedingly rare but it is the most common primary non-hematolymphoid malignant neoplasm of the spleen It is a highly aggressive malignancy with a poor prognosis The majority of patients present with abdominal pain or a palpable abdominal mass
Angiosarcoma of the Spleen
Cystic splenic metastasis Primary tumour is cystic Secondary changes are -Degeneration- Hemorrhage- Necrosis- Infection
Splenic metastasis
ULTRASOUND OF THE PANCREAS ndash Normal
Pancreas Scan Plane Normal Pancreas and surrounding anatomy
Sagittal Scan Plane Pancreatic Head Head of pancreas
Scanning TechniqueTechniqueBegin transversely high in the epigastrumYou may need to apply enough pressure to help displace bowel gasAdjust image depth so the aorta is at the bottom of the screen
Head of pancreas - Use both transverse amp sagittal planes as the head can be quite long and continue left caudally for several centimeters
Body of Pancreas - Transverse probe Use the splenic vein to help identify the pancreas superficial to this
Tail of pancreas - Start with the probe transverse then angle the heel of the probe cephalad and left as the tail can be sitting up under the spleen Thus the spleen can be used as a window and a left intercostal coronal approach can also be utilized
Ultrasound AppearancesNormal appearance is usually homogeneous and almost isoechoic with the liverIt is frequently hyperechoic compared to the liver because of fatty infiltrationSizeVaries with age and historyApproximate normal measurements areHead 35mm (anterior to posterior)Neck 10-15mmTail 20mm
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Echinococcal cyst Hydatid disease is endemic area usually sheep raising areas
Splenic Hydatid Disease
Intraparenchymal splenic hematoma
Subcapsular splenic hematoma
Peri-splenic hematoma
Splenic abscessUsually result of bacterial endocarditis or septicemia IV drug abuse Immunocompromised patients
Splenic abscess with poorly defined hypoechoic and isoechoic area at US images CT show multiple hypodense area at enlarged spleen
Splenic fungal abscess with poorly defined hypoechoic and hypodense area at US and CT images
Splenic artery aneurysmSplenic artery aneurysms are rare but still the third most common abdominal aneurysm after aneurysms of the abdominal aorta and iliac arteries They may occur in pregnant women in the third trimester and rupture carries a maternal mortality of greater than 50 and a fetal mortality of 70 - 90 Risk factors include smoking and hypertension
A splenic artery pseudoaneurysmis rare situation of a pseudoaneurysm forming in relation to the splenic artery It occur after trauma or post-pancreatitis
Spleen infarction - hypoechogenic bearing marked with a white arrow Duplex color sonography was used as well there is no color signal from the ischemic area
Splenic infarct with a wedge shaped non vascularized splenic lesion
Splenic granulomaUS shows hyperechoic foci with posterior tiny shadowSplenic granuloma as a result from previous exposure to histoplasmosis TB and sarcoidosis
Splenic granuloma
Splenic hemangiomas (also known as splenic venous malformations) while being rare lesions are considered the second commonest focal lesion involving the spleen after simple splenic cysts
Splenic hemangioma with a small hyperechoic lesion
Large complex hyperechoic solid hemangioma with scattered hypoechoic foci
Cystic hemangioma
Asymptomatic Splenic Hamartoma with Rapidly Expansive Growth
Hamartomas is a benign primary neoplasm of spleen they are
normally an incidental finding at imaging surgery or autopsy They can occur in any age group Symptoms occur from mass effect if they grow large Most splenic hamartomas are hyperechoic solid masses with or without cystic changes at ultrasound examination
Lymphangioma
Lymphoma with Splenomegally and hypoechoic splenic masses
Splenic lymphoma is often a manifestation of the diffuse dissemination
characteristic of Hodgkins and non-Hodgkins lymphoma Splenic lymphoma may be single or multiple and appears hypoechoic or hyperechoic masses and they are usually associated with hilar lymphadenopathy
Splenic lymphoma with hypoechoic splenic masses
Splenic angiosarcoma is exceedingly rare but it is the most common primary non-hematolymphoid malignant neoplasm of the spleen It is a highly aggressive malignancy with a poor prognosis The majority of patients present with abdominal pain or a palpable abdominal mass
Angiosarcoma of the Spleen
Cystic splenic metastasis Primary tumour is cystic Secondary changes are -Degeneration- Hemorrhage- Necrosis- Infection
Splenic metastasis
ULTRASOUND OF THE PANCREAS ndash Normal
Pancreas Scan Plane Normal Pancreas and surrounding anatomy
Sagittal Scan Plane Pancreatic Head Head of pancreas
Scanning TechniqueTechniqueBegin transversely high in the epigastrumYou may need to apply enough pressure to help displace bowel gasAdjust image depth so the aorta is at the bottom of the screen
Head of pancreas - Use both transverse amp sagittal planes as the head can be quite long and continue left caudally for several centimeters
Body of Pancreas - Transverse probe Use the splenic vein to help identify the pancreas superficial to this
Tail of pancreas - Start with the probe transverse then angle the heel of the probe cephalad and left as the tail can be sitting up under the spleen Thus the spleen can be used as a window and a left intercostal coronal approach can also be utilized
Ultrasound AppearancesNormal appearance is usually homogeneous and almost isoechoic with the liverIt is frequently hyperechoic compared to the liver because of fatty infiltrationSizeVaries with age and historyApproximate normal measurements areHead 35mm (anterior to posterior)Neck 10-15mmTail 20mm
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Splenic Hydatid Disease
Intraparenchymal splenic hematoma
Subcapsular splenic hematoma
Peri-splenic hematoma
Splenic abscessUsually result of bacterial endocarditis or septicemia IV drug abuse Immunocompromised patients
Splenic abscess with poorly defined hypoechoic and isoechoic area at US images CT show multiple hypodense area at enlarged spleen
Splenic fungal abscess with poorly defined hypoechoic and hypodense area at US and CT images
Splenic artery aneurysmSplenic artery aneurysms are rare but still the third most common abdominal aneurysm after aneurysms of the abdominal aorta and iliac arteries They may occur in pregnant women in the third trimester and rupture carries a maternal mortality of greater than 50 and a fetal mortality of 70 - 90 Risk factors include smoking and hypertension
A splenic artery pseudoaneurysmis rare situation of a pseudoaneurysm forming in relation to the splenic artery It occur after trauma or post-pancreatitis
Spleen infarction - hypoechogenic bearing marked with a white arrow Duplex color sonography was used as well there is no color signal from the ischemic area
Splenic infarct with a wedge shaped non vascularized splenic lesion
Splenic granulomaUS shows hyperechoic foci with posterior tiny shadowSplenic granuloma as a result from previous exposure to histoplasmosis TB and sarcoidosis
Splenic granuloma
Splenic hemangiomas (also known as splenic venous malformations) while being rare lesions are considered the second commonest focal lesion involving the spleen after simple splenic cysts
Splenic hemangioma with a small hyperechoic lesion
Large complex hyperechoic solid hemangioma with scattered hypoechoic foci
Cystic hemangioma
Asymptomatic Splenic Hamartoma with Rapidly Expansive Growth
Hamartomas is a benign primary neoplasm of spleen they are
normally an incidental finding at imaging surgery or autopsy They can occur in any age group Symptoms occur from mass effect if they grow large Most splenic hamartomas are hyperechoic solid masses with or without cystic changes at ultrasound examination
Lymphangioma
Lymphoma with Splenomegally and hypoechoic splenic masses
Splenic lymphoma is often a manifestation of the diffuse dissemination
characteristic of Hodgkins and non-Hodgkins lymphoma Splenic lymphoma may be single or multiple and appears hypoechoic or hyperechoic masses and they are usually associated with hilar lymphadenopathy
Splenic lymphoma with hypoechoic splenic masses
Splenic angiosarcoma is exceedingly rare but it is the most common primary non-hematolymphoid malignant neoplasm of the spleen It is a highly aggressive malignancy with a poor prognosis The majority of patients present with abdominal pain or a palpable abdominal mass
Angiosarcoma of the Spleen
Cystic splenic metastasis Primary tumour is cystic Secondary changes are -Degeneration- Hemorrhage- Necrosis- Infection
Splenic metastasis
ULTRASOUND OF THE PANCREAS ndash Normal
Pancreas Scan Plane Normal Pancreas and surrounding anatomy
Sagittal Scan Plane Pancreatic Head Head of pancreas
Scanning TechniqueTechniqueBegin transversely high in the epigastrumYou may need to apply enough pressure to help displace bowel gasAdjust image depth so the aorta is at the bottom of the screen
Head of pancreas - Use both transverse amp sagittal planes as the head can be quite long and continue left caudally for several centimeters
Body of Pancreas - Transverse probe Use the splenic vein to help identify the pancreas superficial to this
Tail of pancreas - Start with the probe transverse then angle the heel of the probe cephalad and left as the tail can be sitting up under the spleen Thus the spleen can be used as a window and a left intercostal coronal approach can also be utilized
Ultrasound AppearancesNormal appearance is usually homogeneous and almost isoechoic with the liverIt is frequently hyperechoic compared to the liver because of fatty infiltrationSizeVaries with age and historyApproximate normal measurements areHead 35mm (anterior to posterior)Neck 10-15mmTail 20mm
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Intraparenchymal splenic hematoma
Subcapsular splenic hematoma
Peri-splenic hematoma
Splenic abscessUsually result of bacterial endocarditis or septicemia IV drug abuse Immunocompromised patients
Splenic abscess with poorly defined hypoechoic and isoechoic area at US images CT show multiple hypodense area at enlarged spleen
Splenic fungal abscess with poorly defined hypoechoic and hypodense area at US and CT images
Splenic artery aneurysmSplenic artery aneurysms are rare but still the third most common abdominal aneurysm after aneurysms of the abdominal aorta and iliac arteries They may occur in pregnant women in the third trimester and rupture carries a maternal mortality of greater than 50 and a fetal mortality of 70 - 90 Risk factors include smoking and hypertension
A splenic artery pseudoaneurysmis rare situation of a pseudoaneurysm forming in relation to the splenic artery It occur after trauma or post-pancreatitis
Spleen infarction - hypoechogenic bearing marked with a white arrow Duplex color sonography was used as well there is no color signal from the ischemic area
Splenic infarct with a wedge shaped non vascularized splenic lesion
Splenic granulomaUS shows hyperechoic foci with posterior tiny shadowSplenic granuloma as a result from previous exposure to histoplasmosis TB and sarcoidosis
Splenic granuloma
Splenic hemangiomas (also known as splenic venous malformations) while being rare lesions are considered the second commonest focal lesion involving the spleen after simple splenic cysts
Splenic hemangioma with a small hyperechoic lesion
Large complex hyperechoic solid hemangioma with scattered hypoechoic foci
Cystic hemangioma
Asymptomatic Splenic Hamartoma with Rapidly Expansive Growth
Hamartomas is a benign primary neoplasm of spleen they are
normally an incidental finding at imaging surgery or autopsy They can occur in any age group Symptoms occur from mass effect if they grow large Most splenic hamartomas are hyperechoic solid masses with or without cystic changes at ultrasound examination
Lymphangioma
Lymphoma with Splenomegally and hypoechoic splenic masses
Splenic lymphoma is often a manifestation of the diffuse dissemination
characteristic of Hodgkins and non-Hodgkins lymphoma Splenic lymphoma may be single or multiple and appears hypoechoic or hyperechoic masses and they are usually associated with hilar lymphadenopathy
Splenic lymphoma with hypoechoic splenic masses
Splenic angiosarcoma is exceedingly rare but it is the most common primary non-hematolymphoid malignant neoplasm of the spleen It is a highly aggressive malignancy with a poor prognosis The majority of patients present with abdominal pain or a palpable abdominal mass
Angiosarcoma of the Spleen
Cystic splenic metastasis Primary tumour is cystic Secondary changes are -Degeneration- Hemorrhage- Necrosis- Infection
Splenic metastasis
ULTRASOUND OF THE PANCREAS ndash Normal
Pancreas Scan Plane Normal Pancreas and surrounding anatomy
Sagittal Scan Plane Pancreatic Head Head of pancreas
Scanning TechniqueTechniqueBegin transversely high in the epigastrumYou may need to apply enough pressure to help displace bowel gasAdjust image depth so the aorta is at the bottom of the screen
Head of pancreas - Use both transverse amp sagittal planes as the head can be quite long and continue left caudally for several centimeters
Body of Pancreas - Transverse probe Use the splenic vein to help identify the pancreas superficial to this
Tail of pancreas - Start with the probe transverse then angle the heel of the probe cephalad and left as the tail can be sitting up under the spleen Thus the spleen can be used as a window and a left intercostal coronal approach can also be utilized
Ultrasound AppearancesNormal appearance is usually homogeneous and almost isoechoic with the liverIt is frequently hyperechoic compared to the liver because of fatty infiltrationSizeVaries with age and historyApproximate normal measurements areHead 35mm (anterior to posterior)Neck 10-15mmTail 20mm
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Subcapsular splenic hematoma
Peri-splenic hematoma
Splenic abscessUsually result of bacterial endocarditis or septicemia IV drug abuse Immunocompromised patients
Splenic abscess with poorly defined hypoechoic and isoechoic area at US images CT show multiple hypodense area at enlarged spleen
Splenic fungal abscess with poorly defined hypoechoic and hypodense area at US and CT images
Splenic artery aneurysmSplenic artery aneurysms are rare but still the third most common abdominal aneurysm after aneurysms of the abdominal aorta and iliac arteries They may occur in pregnant women in the third trimester and rupture carries a maternal mortality of greater than 50 and a fetal mortality of 70 - 90 Risk factors include smoking and hypertension
A splenic artery pseudoaneurysmis rare situation of a pseudoaneurysm forming in relation to the splenic artery It occur after trauma or post-pancreatitis
Spleen infarction - hypoechogenic bearing marked with a white arrow Duplex color sonography was used as well there is no color signal from the ischemic area
Splenic infarct with a wedge shaped non vascularized splenic lesion
Splenic granulomaUS shows hyperechoic foci with posterior tiny shadowSplenic granuloma as a result from previous exposure to histoplasmosis TB and sarcoidosis
Splenic granuloma
Splenic hemangiomas (also known as splenic venous malformations) while being rare lesions are considered the second commonest focal lesion involving the spleen after simple splenic cysts
Splenic hemangioma with a small hyperechoic lesion
Large complex hyperechoic solid hemangioma with scattered hypoechoic foci
Cystic hemangioma
Asymptomatic Splenic Hamartoma with Rapidly Expansive Growth
Hamartomas is a benign primary neoplasm of spleen they are
normally an incidental finding at imaging surgery or autopsy They can occur in any age group Symptoms occur from mass effect if they grow large Most splenic hamartomas are hyperechoic solid masses with or without cystic changes at ultrasound examination
Lymphangioma
Lymphoma with Splenomegally and hypoechoic splenic masses
Splenic lymphoma is often a manifestation of the diffuse dissemination
characteristic of Hodgkins and non-Hodgkins lymphoma Splenic lymphoma may be single or multiple and appears hypoechoic or hyperechoic masses and they are usually associated with hilar lymphadenopathy
Splenic lymphoma with hypoechoic splenic masses
Splenic angiosarcoma is exceedingly rare but it is the most common primary non-hematolymphoid malignant neoplasm of the spleen It is a highly aggressive malignancy with a poor prognosis The majority of patients present with abdominal pain or a palpable abdominal mass
Angiosarcoma of the Spleen
Cystic splenic metastasis Primary tumour is cystic Secondary changes are -Degeneration- Hemorrhage- Necrosis- Infection
Splenic metastasis
ULTRASOUND OF THE PANCREAS ndash Normal
Pancreas Scan Plane Normal Pancreas and surrounding anatomy
Sagittal Scan Plane Pancreatic Head Head of pancreas
Scanning TechniqueTechniqueBegin transversely high in the epigastrumYou may need to apply enough pressure to help displace bowel gasAdjust image depth so the aorta is at the bottom of the screen
Head of pancreas - Use both transverse amp sagittal planes as the head can be quite long and continue left caudally for several centimeters
Body of Pancreas - Transverse probe Use the splenic vein to help identify the pancreas superficial to this
Tail of pancreas - Start with the probe transverse then angle the heel of the probe cephalad and left as the tail can be sitting up under the spleen Thus the spleen can be used as a window and a left intercostal coronal approach can also be utilized
Ultrasound AppearancesNormal appearance is usually homogeneous and almost isoechoic with the liverIt is frequently hyperechoic compared to the liver because of fatty infiltrationSizeVaries with age and historyApproximate normal measurements areHead 35mm (anterior to posterior)Neck 10-15mmTail 20mm
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Peri-splenic hematoma
Splenic abscessUsually result of bacterial endocarditis or septicemia IV drug abuse Immunocompromised patients
Splenic abscess with poorly defined hypoechoic and isoechoic area at US images CT show multiple hypodense area at enlarged spleen
Splenic fungal abscess with poorly defined hypoechoic and hypodense area at US and CT images
Splenic artery aneurysmSplenic artery aneurysms are rare but still the third most common abdominal aneurysm after aneurysms of the abdominal aorta and iliac arteries They may occur in pregnant women in the third trimester and rupture carries a maternal mortality of greater than 50 and a fetal mortality of 70 - 90 Risk factors include smoking and hypertension
A splenic artery pseudoaneurysmis rare situation of a pseudoaneurysm forming in relation to the splenic artery It occur after trauma or post-pancreatitis
Spleen infarction - hypoechogenic bearing marked with a white arrow Duplex color sonography was used as well there is no color signal from the ischemic area
Splenic infarct with a wedge shaped non vascularized splenic lesion
Splenic granulomaUS shows hyperechoic foci with posterior tiny shadowSplenic granuloma as a result from previous exposure to histoplasmosis TB and sarcoidosis
Splenic granuloma
Splenic hemangiomas (also known as splenic venous malformations) while being rare lesions are considered the second commonest focal lesion involving the spleen after simple splenic cysts
Splenic hemangioma with a small hyperechoic lesion
Large complex hyperechoic solid hemangioma with scattered hypoechoic foci
Cystic hemangioma
Asymptomatic Splenic Hamartoma with Rapidly Expansive Growth
Hamartomas is a benign primary neoplasm of spleen they are
normally an incidental finding at imaging surgery or autopsy They can occur in any age group Symptoms occur from mass effect if they grow large Most splenic hamartomas are hyperechoic solid masses with or without cystic changes at ultrasound examination
Lymphangioma
Lymphoma with Splenomegally and hypoechoic splenic masses
Splenic lymphoma is often a manifestation of the diffuse dissemination
characteristic of Hodgkins and non-Hodgkins lymphoma Splenic lymphoma may be single or multiple and appears hypoechoic or hyperechoic masses and they are usually associated with hilar lymphadenopathy
Splenic lymphoma with hypoechoic splenic masses
Splenic angiosarcoma is exceedingly rare but it is the most common primary non-hematolymphoid malignant neoplasm of the spleen It is a highly aggressive malignancy with a poor prognosis The majority of patients present with abdominal pain or a palpable abdominal mass
Angiosarcoma of the Spleen
Cystic splenic metastasis Primary tumour is cystic Secondary changes are -Degeneration- Hemorrhage- Necrosis- Infection
Splenic metastasis
ULTRASOUND OF THE PANCREAS ndash Normal
Pancreas Scan Plane Normal Pancreas and surrounding anatomy
Sagittal Scan Plane Pancreatic Head Head of pancreas
Scanning TechniqueTechniqueBegin transversely high in the epigastrumYou may need to apply enough pressure to help displace bowel gasAdjust image depth so the aorta is at the bottom of the screen
Head of pancreas - Use both transverse amp sagittal planes as the head can be quite long and continue left caudally for several centimeters
Body of Pancreas - Transverse probe Use the splenic vein to help identify the pancreas superficial to this
Tail of pancreas - Start with the probe transverse then angle the heel of the probe cephalad and left as the tail can be sitting up under the spleen Thus the spleen can be used as a window and a left intercostal coronal approach can also be utilized
Ultrasound AppearancesNormal appearance is usually homogeneous and almost isoechoic with the liverIt is frequently hyperechoic compared to the liver because of fatty infiltrationSizeVaries with age and historyApproximate normal measurements areHead 35mm (anterior to posterior)Neck 10-15mmTail 20mm
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Splenic abscessUsually result of bacterial endocarditis or septicemia IV drug abuse Immunocompromised patients
Splenic abscess with poorly defined hypoechoic and isoechoic area at US images CT show multiple hypodense area at enlarged spleen
Splenic fungal abscess with poorly defined hypoechoic and hypodense area at US and CT images
Splenic artery aneurysmSplenic artery aneurysms are rare but still the third most common abdominal aneurysm after aneurysms of the abdominal aorta and iliac arteries They may occur in pregnant women in the third trimester and rupture carries a maternal mortality of greater than 50 and a fetal mortality of 70 - 90 Risk factors include smoking and hypertension
A splenic artery pseudoaneurysmis rare situation of a pseudoaneurysm forming in relation to the splenic artery It occur after trauma or post-pancreatitis
Spleen infarction - hypoechogenic bearing marked with a white arrow Duplex color sonography was used as well there is no color signal from the ischemic area
Splenic infarct with a wedge shaped non vascularized splenic lesion
Splenic granulomaUS shows hyperechoic foci with posterior tiny shadowSplenic granuloma as a result from previous exposure to histoplasmosis TB and sarcoidosis
Splenic granuloma
Splenic hemangiomas (also known as splenic venous malformations) while being rare lesions are considered the second commonest focal lesion involving the spleen after simple splenic cysts
Splenic hemangioma with a small hyperechoic lesion
Large complex hyperechoic solid hemangioma with scattered hypoechoic foci
Cystic hemangioma
Asymptomatic Splenic Hamartoma with Rapidly Expansive Growth
Hamartomas is a benign primary neoplasm of spleen they are
normally an incidental finding at imaging surgery or autopsy They can occur in any age group Symptoms occur from mass effect if they grow large Most splenic hamartomas are hyperechoic solid masses with or without cystic changes at ultrasound examination
Lymphangioma
Lymphoma with Splenomegally and hypoechoic splenic masses
Splenic lymphoma is often a manifestation of the diffuse dissemination
characteristic of Hodgkins and non-Hodgkins lymphoma Splenic lymphoma may be single or multiple and appears hypoechoic or hyperechoic masses and they are usually associated with hilar lymphadenopathy
Splenic lymphoma with hypoechoic splenic masses
Splenic angiosarcoma is exceedingly rare but it is the most common primary non-hematolymphoid malignant neoplasm of the spleen It is a highly aggressive malignancy with a poor prognosis The majority of patients present with abdominal pain or a palpable abdominal mass
Angiosarcoma of the Spleen
Cystic splenic metastasis Primary tumour is cystic Secondary changes are -Degeneration- Hemorrhage- Necrosis- Infection
Splenic metastasis
ULTRASOUND OF THE PANCREAS ndash Normal
Pancreas Scan Plane Normal Pancreas and surrounding anatomy
Sagittal Scan Plane Pancreatic Head Head of pancreas
Scanning TechniqueTechniqueBegin transversely high in the epigastrumYou may need to apply enough pressure to help displace bowel gasAdjust image depth so the aorta is at the bottom of the screen
Head of pancreas - Use both transverse amp sagittal planes as the head can be quite long and continue left caudally for several centimeters
Body of Pancreas - Transverse probe Use the splenic vein to help identify the pancreas superficial to this
Tail of pancreas - Start with the probe transverse then angle the heel of the probe cephalad and left as the tail can be sitting up under the spleen Thus the spleen can be used as a window and a left intercostal coronal approach can also be utilized
Ultrasound AppearancesNormal appearance is usually homogeneous and almost isoechoic with the liverIt is frequently hyperechoic compared to the liver because of fatty infiltrationSizeVaries with age and historyApproximate normal measurements areHead 35mm (anterior to posterior)Neck 10-15mmTail 20mm
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Splenic abscess with poorly defined hypoechoic and isoechoic area at US images CT show multiple hypodense area at enlarged spleen
Splenic fungal abscess with poorly defined hypoechoic and hypodense area at US and CT images
Splenic artery aneurysmSplenic artery aneurysms are rare but still the third most common abdominal aneurysm after aneurysms of the abdominal aorta and iliac arteries They may occur in pregnant women in the third trimester and rupture carries a maternal mortality of greater than 50 and a fetal mortality of 70 - 90 Risk factors include smoking and hypertension
A splenic artery pseudoaneurysmis rare situation of a pseudoaneurysm forming in relation to the splenic artery It occur after trauma or post-pancreatitis
Spleen infarction - hypoechogenic bearing marked with a white arrow Duplex color sonography was used as well there is no color signal from the ischemic area
Splenic infarct with a wedge shaped non vascularized splenic lesion
Splenic granulomaUS shows hyperechoic foci with posterior tiny shadowSplenic granuloma as a result from previous exposure to histoplasmosis TB and sarcoidosis
Splenic granuloma
Splenic hemangiomas (also known as splenic venous malformations) while being rare lesions are considered the second commonest focal lesion involving the spleen after simple splenic cysts
Splenic hemangioma with a small hyperechoic lesion
Large complex hyperechoic solid hemangioma with scattered hypoechoic foci
Cystic hemangioma
Asymptomatic Splenic Hamartoma with Rapidly Expansive Growth
Hamartomas is a benign primary neoplasm of spleen they are
normally an incidental finding at imaging surgery or autopsy They can occur in any age group Symptoms occur from mass effect if they grow large Most splenic hamartomas are hyperechoic solid masses with or without cystic changes at ultrasound examination
Lymphangioma
Lymphoma with Splenomegally and hypoechoic splenic masses
Splenic lymphoma is often a manifestation of the diffuse dissemination
characteristic of Hodgkins and non-Hodgkins lymphoma Splenic lymphoma may be single or multiple and appears hypoechoic or hyperechoic masses and they are usually associated with hilar lymphadenopathy
Splenic lymphoma with hypoechoic splenic masses
Splenic angiosarcoma is exceedingly rare but it is the most common primary non-hematolymphoid malignant neoplasm of the spleen It is a highly aggressive malignancy with a poor prognosis The majority of patients present with abdominal pain or a palpable abdominal mass
Angiosarcoma of the Spleen
Cystic splenic metastasis Primary tumour is cystic Secondary changes are -Degeneration- Hemorrhage- Necrosis- Infection
Splenic metastasis
ULTRASOUND OF THE PANCREAS ndash Normal
Pancreas Scan Plane Normal Pancreas and surrounding anatomy
Sagittal Scan Plane Pancreatic Head Head of pancreas
Scanning TechniqueTechniqueBegin transversely high in the epigastrumYou may need to apply enough pressure to help displace bowel gasAdjust image depth so the aorta is at the bottom of the screen
Head of pancreas - Use both transverse amp sagittal planes as the head can be quite long and continue left caudally for several centimeters
Body of Pancreas - Transverse probe Use the splenic vein to help identify the pancreas superficial to this
Tail of pancreas - Start with the probe transverse then angle the heel of the probe cephalad and left as the tail can be sitting up under the spleen Thus the spleen can be used as a window and a left intercostal coronal approach can also be utilized
Ultrasound AppearancesNormal appearance is usually homogeneous and almost isoechoic with the liverIt is frequently hyperechoic compared to the liver because of fatty infiltrationSizeVaries with age and historyApproximate normal measurements areHead 35mm (anterior to posterior)Neck 10-15mmTail 20mm
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Splenic fungal abscess with poorly defined hypoechoic and hypodense area at US and CT images
Splenic artery aneurysmSplenic artery aneurysms are rare but still the third most common abdominal aneurysm after aneurysms of the abdominal aorta and iliac arteries They may occur in pregnant women in the third trimester and rupture carries a maternal mortality of greater than 50 and a fetal mortality of 70 - 90 Risk factors include smoking and hypertension
A splenic artery pseudoaneurysmis rare situation of a pseudoaneurysm forming in relation to the splenic artery It occur after trauma or post-pancreatitis
Spleen infarction - hypoechogenic bearing marked with a white arrow Duplex color sonography was used as well there is no color signal from the ischemic area
Splenic infarct with a wedge shaped non vascularized splenic lesion
Splenic granulomaUS shows hyperechoic foci with posterior tiny shadowSplenic granuloma as a result from previous exposure to histoplasmosis TB and sarcoidosis
Splenic granuloma
Splenic hemangiomas (also known as splenic venous malformations) while being rare lesions are considered the second commonest focal lesion involving the spleen after simple splenic cysts
Splenic hemangioma with a small hyperechoic lesion
Large complex hyperechoic solid hemangioma with scattered hypoechoic foci
Cystic hemangioma
Asymptomatic Splenic Hamartoma with Rapidly Expansive Growth
Hamartomas is a benign primary neoplasm of spleen they are
normally an incidental finding at imaging surgery or autopsy They can occur in any age group Symptoms occur from mass effect if they grow large Most splenic hamartomas are hyperechoic solid masses with or without cystic changes at ultrasound examination
Lymphangioma
Lymphoma with Splenomegally and hypoechoic splenic masses
Splenic lymphoma is often a manifestation of the diffuse dissemination
characteristic of Hodgkins and non-Hodgkins lymphoma Splenic lymphoma may be single or multiple and appears hypoechoic or hyperechoic masses and they are usually associated with hilar lymphadenopathy
Splenic lymphoma with hypoechoic splenic masses
Splenic angiosarcoma is exceedingly rare but it is the most common primary non-hematolymphoid malignant neoplasm of the spleen It is a highly aggressive malignancy with a poor prognosis The majority of patients present with abdominal pain or a palpable abdominal mass
Angiosarcoma of the Spleen
Cystic splenic metastasis Primary tumour is cystic Secondary changes are -Degeneration- Hemorrhage- Necrosis- Infection
Splenic metastasis
ULTRASOUND OF THE PANCREAS ndash Normal
Pancreas Scan Plane Normal Pancreas and surrounding anatomy
Sagittal Scan Plane Pancreatic Head Head of pancreas
Scanning TechniqueTechniqueBegin transversely high in the epigastrumYou may need to apply enough pressure to help displace bowel gasAdjust image depth so the aorta is at the bottom of the screen
Head of pancreas - Use both transverse amp sagittal planes as the head can be quite long and continue left caudally for several centimeters
Body of Pancreas - Transverse probe Use the splenic vein to help identify the pancreas superficial to this
Tail of pancreas - Start with the probe transverse then angle the heel of the probe cephalad and left as the tail can be sitting up under the spleen Thus the spleen can be used as a window and a left intercostal coronal approach can also be utilized
Ultrasound AppearancesNormal appearance is usually homogeneous and almost isoechoic with the liverIt is frequently hyperechoic compared to the liver because of fatty infiltrationSizeVaries with age and historyApproximate normal measurements areHead 35mm (anterior to posterior)Neck 10-15mmTail 20mm
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Splenic artery aneurysmSplenic artery aneurysms are rare but still the third most common abdominal aneurysm after aneurysms of the abdominal aorta and iliac arteries They may occur in pregnant women in the third trimester and rupture carries a maternal mortality of greater than 50 and a fetal mortality of 70 - 90 Risk factors include smoking and hypertension
A splenic artery pseudoaneurysmis rare situation of a pseudoaneurysm forming in relation to the splenic artery It occur after trauma or post-pancreatitis
Spleen infarction - hypoechogenic bearing marked with a white arrow Duplex color sonography was used as well there is no color signal from the ischemic area
Splenic infarct with a wedge shaped non vascularized splenic lesion
Splenic granulomaUS shows hyperechoic foci with posterior tiny shadowSplenic granuloma as a result from previous exposure to histoplasmosis TB and sarcoidosis
Splenic granuloma
Splenic hemangiomas (also known as splenic venous malformations) while being rare lesions are considered the second commonest focal lesion involving the spleen after simple splenic cysts
Splenic hemangioma with a small hyperechoic lesion
Large complex hyperechoic solid hemangioma with scattered hypoechoic foci
Cystic hemangioma
Asymptomatic Splenic Hamartoma with Rapidly Expansive Growth
Hamartomas is a benign primary neoplasm of spleen they are
normally an incidental finding at imaging surgery or autopsy They can occur in any age group Symptoms occur from mass effect if they grow large Most splenic hamartomas are hyperechoic solid masses with or without cystic changes at ultrasound examination
Lymphangioma
Lymphoma with Splenomegally and hypoechoic splenic masses
Splenic lymphoma is often a manifestation of the diffuse dissemination
characteristic of Hodgkins and non-Hodgkins lymphoma Splenic lymphoma may be single or multiple and appears hypoechoic or hyperechoic masses and they are usually associated with hilar lymphadenopathy
Splenic lymphoma with hypoechoic splenic masses
Splenic angiosarcoma is exceedingly rare but it is the most common primary non-hematolymphoid malignant neoplasm of the spleen It is a highly aggressive malignancy with a poor prognosis The majority of patients present with abdominal pain or a palpable abdominal mass
Angiosarcoma of the Spleen
Cystic splenic metastasis Primary tumour is cystic Secondary changes are -Degeneration- Hemorrhage- Necrosis- Infection
Splenic metastasis
ULTRASOUND OF THE PANCREAS ndash Normal
Pancreas Scan Plane Normal Pancreas and surrounding anatomy
Sagittal Scan Plane Pancreatic Head Head of pancreas
Scanning TechniqueTechniqueBegin transversely high in the epigastrumYou may need to apply enough pressure to help displace bowel gasAdjust image depth so the aorta is at the bottom of the screen
Head of pancreas - Use both transverse amp sagittal planes as the head can be quite long and continue left caudally for several centimeters
Body of Pancreas - Transverse probe Use the splenic vein to help identify the pancreas superficial to this
Tail of pancreas - Start with the probe transverse then angle the heel of the probe cephalad and left as the tail can be sitting up under the spleen Thus the spleen can be used as a window and a left intercostal coronal approach can also be utilized
Ultrasound AppearancesNormal appearance is usually homogeneous and almost isoechoic with the liverIt is frequently hyperechoic compared to the liver because of fatty infiltrationSizeVaries with age and historyApproximate normal measurements areHead 35mm (anterior to posterior)Neck 10-15mmTail 20mm
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Spleen infarction - hypoechogenic bearing marked with a white arrow Duplex color sonography was used as well there is no color signal from the ischemic area
Splenic infarct with a wedge shaped non vascularized splenic lesion
Splenic granulomaUS shows hyperechoic foci with posterior tiny shadowSplenic granuloma as a result from previous exposure to histoplasmosis TB and sarcoidosis
Splenic granuloma
Splenic hemangiomas (also known as splenic venous malformations) while being rare lesions are considered the second commonest focal lesion involving the spleen after simple splenic cysts
Splenic hemangioma with a small hyperechoic lesion
Large complex hyperechoic solid hemangioma with scattered hypoechoic foci
Cystic hemangioma
Asymptomatic Splenic Hamartoma with Rapidly Expansive Growth
Hamartomas is a benign primary neoplasm of spleen they are
normally an incidental finding at imaging surgery or autopsy They can occur in any age group Symptoms occur from mass effect if they grow large Most splenic hamartomas are hyperechoic solid masses with or without cystic changes at ultrasound examination
Lymphangioma
Lymphoma with Splenomegally and hypoechoic splenic masses
Splenic lymphoma is often a manifestation of the diffuse dissemination
characteristic of Hodgkins and non-Hodgkins lymphoma Splenic lymphoma may be single or multiple and appears hypoechoic or hyperechoic masses and they are usually associated with hilar lymphadenopathy
Splenic lymphoma with hypoechoic splenic masses
Splenic angiosarcoma is exceedingly rare but it is the most common primary non-hematolymphoid malignant neoplasm of the spleen It is a highly aggressive malignancy with a poor prognosis The majority of patients present with abdominal pain or a palpable abdominal mass
Angiosarcoma of the Spleen
Cystic splenic metastasis Primary tumour is cystic Secondary changes are -Degeneration- Hemorrhage- Necrosis- Infection
Splenic metastasis
ULTRASOUND OF THE PANCREAS ndash Normal
Pancreas Scan Plane Normal Pancreas and surrounding anatomy
Sagittal Scan Plane Pancreatic Head Head of pancreas
Scanning TechniqueTechniqueBegin transversely high in the epigastrumYou may need to apply enough pressure to help displace bowel gasAdjust image depth so the aorta is at the bottom of the screen
Head of pancreas - Use both transverse amp sagittal planes as the head can be quite long and continue left caudally for several centimeters
Body of Pancreas - Transverse probe Use the splenic vein to help identify the pancreas superficial to this
Tail of pancreas - Start with the probe transverse then angle the heel of the probe cephalad and left as the tail can be sitting up under the spleen Thus the spleen can be used as a window and a left intercostal coronal approach can also be utilized
Ultrasound AppearancesNormal appearance is usually homogeneous and almost isoechoic with the liverIt is frequently hyperechoic compared to the liver because of fatty infiltrationSizeVaries with age and historyApproximate normal measurements areHead 35mm (anterior to posterior)Neck 10-15mmTail 20mm
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Splenic infarct with a wedge shaped non vascularized splenic lesion
Splenic granulomaUS shows hyperechoic foci with posterior tiny shadowSplenic granuloma as a result from previous exposure to histoplasmosis TB and sarcoidosis
Splenic granuloma
Splenic hemangiomas (also known as splenic venous malformations) while being rare lesions are considered the second commonest focal lesion involving the spleen after simple splenic cysts
Splenic hemangioma with a small hyperechoic lesion
Large complex hyperechoic solid hemangioma with scattered hypoechoic foci
Cystic hemangioma
Asymptomatic Splenic Hamartoma with Rapidly Expansive Growth
Hamartomas is a benign primary neoplasm of spleen they are
normally an incidental finding at imaging surgery or autopsy They can occur in any age group Symptoms occur from mass effect if they grow large Most splenic hamartomas are hyperechoic solid masses with or without cystic changes at ultrasound examination
Lymphangioma
Lymphoma with Splenomegally and hypoechoic splenic masses
Splenic lymphoma is often a manifestation of the diffuse dissemination
characteristic of Hodgkins and non-Hodgkins lymphoma Splenic lymphoma may be single or multiple and appears hypoechoic or hyperechoic masses and they are usually associated with hilar lymphadenopathy
Splenic lymphoma with hypoechoic splenic masses
Splenic angiosarcoma is exceedingly rare but it is the most common primary non-hematolymphoid malignant neoplasm of the spleen It is a highly aggressive malignancy with a poor prognosis The majority of patients present with abdominal pain or a palpable abdominal mass
Angiosarcoma of the Spleen
Cystic splenic metastasis Primary tumour is cystic Secondary changes are -Degeneration- Hemorrhage- Necrosis- Infection
Splenic metastasis
ULTRASOUND OF THE PANCREAS ndash Normal
Pancreas Scan Plane Normal Pancreas and surrounding anatomy
Sagittal Scan Plane Pancreatic Head Head of pancreas
Scanning TechniqueTechniqueBegin transversely high in the epigastrumYou may need to apply enough pressure to help displace bowel gasAdjust image depth so the aorta is at the bottom of the screen
Head of pancreas - Use both transverse amp sagittal planes as the head can be quite long and continue left caudally for several centimeters
Body of Pancreas - Transverse probe Use the splenic vein to help identify the pancreas superficial to this
Tail of pancreas - Start with the probe transverse then angle the heel of the probe cephalad and left as the tail can be sitting up under the spleen Thus the spleen can be used as a window and a left intercostal coronal approach can also be utilized
Ultrasound AppearancesNormal appearance is usually homogeneous and almost isoechoic with the liverIt is frequently hyperechoic compared to the liver because of fatty infiltrationSizeVaries with age and historyApproximate normal measurements areHead 35mm (anterior to posterior)Neck 10-15mmTail 20mm
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Splenic granulomaUS shows hyperechoic foci with posterior tiny shadowSplenic granuloma as a result from previous exposure to histoplasmosis TB and sarcoidosis
Splenic granuloma
Splenic hemangiomas (also known as splenic venous malformations) while being rare lesions are considered the second commonest focal lesion involving the spleen after simple splenic cysts
Splenic hemangioma with a small hyperechoic lesion
Large complex hyperechoic solid hemangioma with scattered hypoechoic foci
Cystic hemangioma
Asymptomatic Splenic Hamartoma with Rapidly Expansive Growth
Hamartomas is a benign primary neoplasm of spleen they are
normally an incidental finding at imaging surgery or autopsy They can occur in any age group Symptoms occur from mass effect if they grow large Most splenic hamartomas are hyperechoic solid masses with or without cystic changes at ultrasound examination
Lymphangioma
Lymphoma with Splenomegally and hypoechoic splenic masses
Splenic lymphoma is often a manifestation of the diffuse dissemination
characteristic of Hodgkins and non-Hodgkins lymphoma Splenic lymphoma may be single or multiple and appears hypoechoic or hyperechoic masses and they are usually associated with hilar lymphadenopathy
Splenic lymphoma with hypoechoic splenic masses
Splenic angiosarcoma is exceedingly rare but it is the most common primary non-hematolymphoid malignant neoplasm of the spleen It is a highly aggressive malignancy with a poor prognosis The majority of patients present with abdominal pain or a palpable abdominal mass
Angiosarcoma of the Spleen
Cystic splenic metastasis Primary tumour is cystic Secondary changes are -Degeneration- Hemorrhage- Necrosis- Infection
Splenic metastasis
ULTRASOUND OF THE PANCREAS ndash Normal
Pancreas Scan Plane Normal Pancreas and surrounding anatomy
Sagittal Scan Plane Pancreatic Head Head of pancreas
Scanning TechniqueTechniqueBegin transversely high in the epigastrumYou may need to apply enough pressure to help displace bowel gasAdjust image depth so the aorta is at the bottom of the screen
Head of pancreas - Use both transverse amp sagittal planes as the head can be quite long and continue left caudally for several centimeters
Body of Pancreas - Transverse probe Use the splenic vein to help identify the pancreas superficial to this
Tail of pancreas - Start with the probe transverse then angle the heel of the probe cephalad and left as the tail can be sitting up under the spleen Thus the spleen can be used as a window and a left intercostal coronal approach can also be utilized
Ultrasound AppearancesNormal appearance is usually homogeneous and almost isoechoic with the liverIt is frequently hyperechoic compared to the liver because of fatty infiltrationSizeVaries with age and historyApproximate normal measurements areHead 35mm (anterior to posterior)Neck 10-15mmTail 20mm
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Splenic granuloma
Splenic hemangiomas (also known as splenic venous malformations) while being rare lesions are considered the second commonest focal lesion involving the spleen after simple splenic cysts
Splenic hemangioma with a small hyperechoic lesion
Large complex hyperechoic solid hemangioma with scattered hypoechoic foci
Cystic hemangioma
Asymptomatic Splenic Hamartoma with Rapidly Expansive Growth
Hamartomas is a benign primary neoplasm of spleen they are
normally an incidental finding at imaging surgery or autopsy They can occur in any age group Symptoms occur from mass effect if they grow large Most splenic hamartomas are hyperechoic solid masses with or without cystic changes at ultrasound examination
Lymphangioma
Lymphoma with Splenomegally and hypoechoic splenic masses
Splenic lymphoma is often a manifestation of the diffuse dissemination
characteristic of Hodgkins and non-Hodgkins lymphoma Splenic lymphoma may be single or multiple and appears hypoechoic or hyperechoic masses and they are usually associated with hilar lymphadenopathy
Splenic lymphoma with hypoechoic splenic masses
Splenic angiosarcoma is exceedingly rare but it is the most common primary non-hematolymphoid malignant neoplasm of the spleen It is a highly aggressive malignancy with a poor prognosis The majority of patients present with abdominal pain or a palpable abdominal mass
Angiosarcoma of the Spleen
Cystic splenic metastasis Primary tumour is cystic Secondary changes are -Degeneration- Hemorrhage- Necrosis- Infection
Splenic metastasis
ULTRASOUND OF THE PANCREAS ndash Normal
Pancreas Scan Plane Normal Pancreas and surrounding anatomy
Sagittal Scan Plane Pancreatic Head Head of pancreas
Scanning TechniqueTechniqueBegin transversely high in the epigastrumYou may need to apply enough pressure to help displace bowel gasAdjust image depth so the aorta is at the bottom of the screen
Head of pancreas - Use both transverse amp sagittal planes as the head can be quite long and continue left caudally for several centimeters
Body of Pancreas - Transverse probe Use the splenic vein to help identify the pancreas superficial to this
Tail of pancreas - Start with the probe transverse then angle the heel of the probe cephalad and left as the tail can be sitting up under the spleen Thus the spleen can be used as a window and a left intercostal coronal approach can also be utilized
Ultrasound AppearancesNormal appearance is usually homogeneous and almost isoechoic with the liverIt is frequently hyperechoic compared to the liver because of fatty infiltrationSizeVaries with age and historyApproximate normal measurements areHead 35mm (anterior to posterior)Neck 10-15mmTail 20mm
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Splenic hemangiomas (also known as splenic venous malformations) while being rare lesions are considered the second commonest focal lesion involving the spleen after simple splenic cysts
Splenic hemangioma with a small hyperechoic lesion
Large complex hyperechoic solid hemangioma with scattered hypoechoic foci
Cystic hemangioma
Asymptomatic Splenic Hamartoma with Rapidly Expansive Growth
Hamartomas is a benign primary neoplasm of spleen they are
normally an incidental finding at imaging surgery or autopsy They can occur in any age group Symptoms occur from mass effect if they grow large Most splenic hamartomas are hyperechoic solid masses with or without cystic changes at ultrasound examination
Lymphangioma
Lymphoma with Splenomegally and hypoechoic splenic masses
Splenic lymphoma is often a manifestation of the diffuse dissemination
characteristic of Hodgkins and non-Hodgkins lymphoma Splenic lymphoma may be single or multiple and appears hypoechoic or hyperechoic masses and they are usually associated with hilar lymphadenopathy
Splenic lymphoma with hypoechoic splenic masses
Splenic angiosarcoma is exceedingly rare but it is the most common primary non-hematolymphoid malignant neoplasm of the spleen It is a highly aggressive malignancy with a poor prognosis The majority of patients present with abdominal pain or a palpable abdominal mass
Angiosarcoma of the Spleen
Cystic splenic metastasis Primary tumour is cystic Secondary changes are -Degeneration- Hemorrhage- Necrosis- Infection
Splenic metastasis
ULTRASOUND OF THE PANCREAS ndash Normal
Pancreas Scan Plane Normal Pancreas and surrounding anatomy
Sagittal Scan Plane Pancreatic Head Head of pancreas
Scanning TechniqueTechniqueBegin transversely high in the epigastrumYou may need to apply enough pressure to help displace bowel gasAdjust image depth so the aorta is at the bottom of the screen
Head of pancreas - Use both transverse amp sagittal planes as the head can be quite long and continue left caudally for several centimeters
Body of Pancreas - Transverse probe Use the splenic vein to help identify the pancreas superficial to this
Tail of pancreas - Start with the probe transverse then angle the heel of the probe cephalad and left as the tail can be sitting up under the spleen Thus the spleen can be used as a window and a left intercostal coronal approach can also be utilized
Ultrasound AppearancesNormal appearance is usually homogeneous and almost isoechoic with the liverIt is frequently hyperechoic compared to the liver because of fatty infiltrationSizeVaries with age and historyApproximate normal measurements areHead 35mm (anterior to posterior)Neck 10-15mmTail 20mm
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Large complex hyperechoic solid hemangioma with scattered hypoechoic foci
Cystic hemangioma
Asymptomatic Splenic Hamartoma with Rapidly Expansive Growth
Hamartomas is a benign primary neoplasm of spleen they are
normally an incidental finding at imaging surgery or autopsy They can occur in any age group Symptoms occur from mass effect if they grow large Most splenic hamartomas are hyperechoic solid masses with or without cystic changes at ultrasound examination
Lymphangioma
Lymphoma with Splenomegally and hypoechoic splenic masses
Splenic lymphoma is often a manifestation of the diffuse dissemination
characteristic of Hodgkins and non-Hodgkins lymphoma Splenic lymphoma may be single or multiple and appears hypoechoic or hyperechoic masses and they are usually associated with hilar lymphadenopathy
Splenic lymphoma with hypoechoic splenic masses
Splenic angiosarcoma is exceedingly rare but it is the most common primary non-hematolymphoid malignant neoplasm of the spleen It is a highly aggressive malignancy with a poor prognosis The majority of patients present with abdominal pain or a palpable abdominal mass
Angiosarcoma of the Spleen
Cystic splenic metastasis Primary tumour is cystic Secondary changes are -Degeneration- Hemorrhage- Necrosis- Infection
Splenic metastasis
ULTRASOUND OF THE PANCREAS ndash Normal
Pancreas Scan Plane Normal Pancreas and surrounding anatomy
Sagittal Scan Plane Pancreatic Head Head of pancreas
Scanning TechniqueTechniqueBegin transversely high in the epigastrumYou may need to apply enough pressure to help displace bowel gasAdjust image depth so the aorta is at the bottom of the screen
Head of pancreas - Use both transverse amp sagittal planes as the head can be quite long and continue left caudally for several centimeters
Body of Pancreas - Transverse probe Use the splenic vein to help identify the pancreas superficial to this
Tail of pancreas - Start with the probe transverse then angle the heel of the probe cephalad and left as the tail can be sitting up under the spleen Thus the spleen can be used as a window and a left intercostal coronal approach can also be utilized
Ultrasound AppearancesNormal appearance is usually homogeneous and almost isoechoic with the liverIt is frequently hyperechoic compared to the liver because of fatty infiltrationSizeVaries with age and historyApproximate normal measurements areHead 35mm (anterior to posterior)Neck 10-15mmTail 20mm
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Asymptomatic Splenic Hamartoma with Rapidly Expansive Growth
Hamartomas is a benign primary neoplasm of spleen they are
normally an incidental finding at imaging surgery or autopsy They can occur in any age group Symptoms occur from mass effect if they grow large Most splenic hamartomas are hyperechoic solid masses with or without cystic changes at ultrasound examination
Lymphangioma
Lymphoma with Splenomegally and hypoechoic splenic masses
Splenic lymphoma is often a manifestation of the diffuse dissemination
characteristic of Hodgkins and non-Hodgkins lymphoma Splenic lymphoma may be single or multiple and appears hypoechoic or hyperechoic masses and they are usually associated with hilar lymphadenopathy
Splenic lymphoma with hypoechoic splenic masses
Splenic angiosarcoma is exceedingly rare but it is the most common primary non-hematolymphoid malignant neoplasm of the spleen It is a highly aggressive malignancy with a poor prognosis The majority of patients present with abdominal pain or a palpable abdominal mass
Angiosarcoma of the Spleen
Cystic splenic metastasis Primary tumour is cystic Secondary changes are -Degeneration- Hemorrhage- Necrosis- Infection
Splenic metastasis
ULTRASOUND OF THE PANCREAS ndash Normal
Pancreas Scan Plane Normal Pancreas and surrounding anatomy
Sagittal Scan Plane Pancreatic Head Head of pancreas
Scanning TechniqueTechniqueBegin transversely high in the epigastrumYou may need to apply enough pressure to help displace bowel gasAdjust image depth so the aorta is at the bottom of the screen
Head of pancreas - Use both transverse amp sagittal planes as the head can be quite long and continue left caudally for several centimeters
Body of Pancreas - Transverse probe Use the splenic vein to help identify the pancreas superficial to this
Tail of pancreas - Start with the probe transverse then angle the heel of the probe cephalad and left as the tail can be sitting up under the spleen Thus the spleen can be used as a window and a left intercostal coronal approach can also be utilized
Ultrasound AppearancesNormal appearance is usually homogeneous and almost isoechoic with the liverIt is frequently hyperechoic compared to the liver because of fatty infiltrationSizeVaries with age and historyApproximate normal measurements areHead 35mm (anterior to posterior)Neck 10-15mmTail 20mm
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Lymphangioma
Lymphoma with Splenomegally and hypoechoic splenic masses
Splenic lymphoma is often a manifestation of the diffuse dissemination
characteristic of Hodgkins and non-Hodgkins lymphoma Splenic lymphoma may be single or multiple and appears hypoechoic or hyperechoic masses and they are usually associated with hilar lymphadenopathy
Splenic lymphoma with hypoechoic splenic masses
Splenic angiosarcoma is exceedingly rare but it is the most common primary non-hematolymphoid malignant neoplasm of the spleen It is a highly aggressive malignancy with a poor prognosis The majority of patients present with abdominal pain or a palpable abdominal mass
Angiosarcoma of the Spleen
Cystic splenic metastasis Primary tumour is cystic Secondary changes are -Degeneration- Hemorrhage- Necrosis- Infection
Splenic metastasis
ULTRASOUND OF THE PANCREAS ndash Normal
Pancreas Scan Plane Normal Pancreas and surrounding anatomy
Sagittal Scan Plane Pancreatic Head Head of pancreas
Scanning TechniqueTechniqueBegin transversely high in the epigastrumYou may need to apply enough pressure to help displace bowel gasAdjust image depth so the aorta is at the bottom of the screen
Head of pancreas - Use both transverse amp sagittal planes as the head can be quite long and continue left caudally for several centimeters
Body of Pancreas - Transverse probe Use the splenic vein to help identify the pancreas superficial to this
Tail of pancreas - Start with the probe transverse then angle the heel of the probe cephalad and left as the tail can be sitting up under the spleen Thus the spleen can be used as a window and a left intercostal coronal approach can also be utilized
Ultrasound AppearancesNormal appearance is usually homogeneous and almost isoechoic with the liverIt is frequently hyperechoic compared to the liver because of fatty infiltrationSizeVaries with age and historyApproximate normal measurements areHead 35mm (anterior to posterior)Neck 10-15mmTail 20mm
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Lymphoma with Splenomegally and hypoechoic splenic masses
Splenic lymphoma is often a manifestation of the diffuse dissemination
characteristic of Hodgkins and non-Hodgkins lymphoma Splenic lymphoma may be single or multiple and appears hypoechoic or hyperechoic masses and they are usually associated with hilar lymphadenopathy
Splenic lymphoma with hypoechoic splenic masses
Splenic angiosarcoma is exceedingly rare but it is the most common primary non-hematolymphoid malignant neoplasm of the spleen It is a highly aggressive malignancy with a poor prognosis The majority of patients present with abdominal pain or a palpable abdominal mass
Angiosarcoma of the Spleen
Cystic splenic metastasis Primary tumour is cystic Secondary changes are -Degeneration- Hemorrhage- Necrosis- Infection
Splenic metastasis
ULTRASOUND OF THE PANCREAS ndash Normal
Pancreas Scan Plane Normal Pancreas and surrounding anatomy
Sagittal Scan Plane Pancreatic Head Head of pancreas
Scanning TechniqueTechniqueBegin transversely high in the epigastrumYou may need to apply enough pressure to help displace bowel gasAdjust image depth so the aorta is at the bottom of the screen
Head of pancreas - Use both transverse amp sagittal planes as the head can be quite long and continue left caudally for several centimeters
Body of Pancreas - Transverse probe Use the splenic vein to help identify the pancreas superficial to this
Tail of pancreas - Start with the probe transverse then angle the heel of the probe cephalad and left as the tail can be sitting up under the spleen Thus the spleen can be used as a window and a left intercostal coronal approach can also be utilized
Ultrasound AppearancesNormal appearance is usually homogeneous and almost isoechoic with the liverIt is frequently hyperechoic compared to the liver because of fatty infiltrationSizeVaries with age and historyApproximate normal measurements areHead 35mm (anterior to posterior)Neck 10-15mmTail 20mm
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Splenic lymphoma with hypoechoic splenic masses
Splenic angiosarcoma is exceedingly rare but it is the most common primary non-hematolymphoid malignant neoplasm of the spleen It is a highly aggressive malignancy with a poor prognosis The majority of patients present with abdominal pain or a palpable abdominal mass
Angiosarcoma of the Spleen
Cystic splenic metastasis Primary tumour is cystic Secondary changes are -Degeneration- Hemorrhage- Necrosis- Infection
Splenic metastasis
ULTRASOUND OF THE PANCREAS ndash Normal
Pancreas Scan Plane Normal Pancreas and surrounding anatomy
Sagittal Scan Plane Pancreatic Head Head of pancreas
Scanning TechniqueTechniqueBegin transversely high in the epigastrumYou may need to apply enough pressure to help displace bowel gasAdjust image depth so the aorta is at the bottom of the screen
Head of pancreas - Use both transverse amp sagittal planes as the head can be quite long and continue left caudally for several centimeters
Body of Pancreas - Transverse probe Use the splenic vein to help identify the pancreas superficial to this
Tail of pancreas - Start with the probe transverse then angle the heel of the probe cephalad and left as the tail can be sitting up under the spleen Thus the spleen can be used as a window and a left intercostal coronal approach can also be utilized
Ultrasound AppearancesNormal appearance is usually homogeneous and almost isoechoic with the liverIt is frequently hyperechoic compared to the liver because of fatty infiltrationSizeVaries with age and historyApproximate normal measurements areHead 35mm (anterior to posterior)Neck 10-15mmTail 20mm
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Splenic angiosarcoma is exceedingly rare but it is the most common primary non-hematolymphoid malignant neoplasm of the spleen It is a highly aggressive malignancy with a poor prognosis The majority of patients present with abdominal pain or a palpable abdominal mass
Angiosarcoma of the Spleen
Cystic splenic metastasis Primary tumour is cystic Secondary changes are -Degeneration- Hemorrhage- Necrosis- Infection
Splenic metastasis
ULTRASOUND OF THE PANCREAS ndash Normal
Pancreas Scan Plane Normal Pancreas and surrounding anatomy
Sagittal Scan Plane Pancreatic Head Head of pancreas
Scanning TechniqueTechniqueBegin transversely high in the epigastrumYou may need to apply enough pressure to help displace bowel gasAdjust image depth so the aorta is at the bottom of the screen
Head of pancreas - Use both transverse amp sagittal planes as the head can be quite long and continue left caudally for several centimeters
Body of Pancreas - Transverse probe Use the splenic vein to help identify the pancreas superficial to this
Tail of pancreas - Start with the probe transverse then angle the heel of the probe cephalad and left as the tail can be sitting up under the spleen Thus the spleen can be used as a window and a left intercostal coronal approach can also be utilized
Ultrasound AppearancesNormal appearance is usually homogeneous and almost isoechoic with the liverIt is frequently hyperechoic compared to the liver because of fatty infiltrationSizeVaries with age and historyApproximate normal measurements areHead 35mm (anterior to posterior)Neck 10-15mmTail 20mm
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Cystic splenic metastasis Primary tumour is cystic Secondary changes are -Degeneration- Hemorrhage- Necrosis- Infection
Splenic metastasis
ULTRASOUND OF THE PANCREAS ndash Normal
Pancreas Scan Plane Normal Pancreas and surrounding anatomy
Sagittal Scan Plane Pancreatic Head Head of pancreas
Scanning TechniqueTechniqueBegin transversely high in the epigastrumYou may need to apply enough pressure to help displace bowel gasAdjust image depth so the aorta is at the bottom of the screen
Head of pancreas - Use both transverse amp sagittal planes as the head can be quite long and continue left caudally for several centimeters
Body of Pancreas - Transverse probe Use the splenic vein to help identify the pancreas superficial to this
Tail of pancreas - Start with the probe transverse then angle the heel of the probe cephalad and left as the tail can be sitting up under the spleen Thus the spleen can be used as a window and a left intercostal coronal approach can also be utilized
Ultrasound AppearancesNormal appearance is usually homogeneous and almost isoechoic with the liverIt is frequently hyperechoic compared to the liver because of fatty infiltrationSizeVaries with age and historyApproximate normal measurements areHead 35mm (anterior to posterior)Neck 10-15mmTail 20mm
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Splenic metastasis
ULTRASOUND OF THE PANCREAS ndash Normal
Pancreas Scan Plane Normal Pancreas and surrounding anatomy
Sagittal Scan Plane Pancreatic Head Head of pancreas
Scanning TechniqueTechniqueBegin transversely high in the epigastrumYou may need to apply enough pressure to help displace bowel gasAdjust image depth so the aorta is at the bottom of the screen
Head of pancreas - Use both transverse amp sagittal planes as the head can be quite long and continue left caudally for several centimeters
Body of Pancreas - Transverse probe Use the splenic vein to help identify the pancreas superficial to this
Tail of pancreas - Start with the probe transverse then angle the heel of the probe cephalad and left as the tail can be sitting up under the spleen Thus the spleen can be used as a window and a left intercostal coronal approach can also be utilized
Ultrasound AppearancesNormal appearance is usually homogeneous and almost isoechoic with the liverIt is frequently hyperechoic compared to the liver because of fatty infiltrationSizeVaries with age and historyApproximate normal measurements areHead 35mm (anterior to posterior)Neck 10-15mmTail 20mm
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
ULTRASOUND OF THE PANCREAS ndash Normal
Pancreas Scan Plane Normal Pancreas and surrounding anatomy
Sagittal Scan Plane Pancreatic Head Head of pancreas
Scanning TechniqueTechniqueBegin transversely high in the epigastrumYou may need to apply enough pressure to help displace bowel gasAdjust image depth so the aorta is at the bottom of the screen
Head of pancreas - Use both transverse amp sagittal planes as the head can be quite long and continue left caudally for several centimeters
Body of Pancreas - Transverse probe Use the splenic vein to help identify the pancreas superficial to this
Tail of pancreas - Start with the probe transverse then angle the heel of the probe cephalad and left as the tail can be sitting up under the spleen Thus the spleen can be used as a window and a left intercostal coronal approach can also be utilized
Ultrasound AppearancesNormal appearance is usually homogeneous and almost isoechoic with the liverIt is frequently hyperechoic compared to the liver because of fatty infiltrationSizeVaries with age and historyApproximate normal measurements areHead 35mm (anterior to posterior)Neck 10-15mmTail 20mm
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Sagittal Scan Plane Pancreatic Head Head of pancreas
Scanning TechniqueTechniqueBegin transversely high in the epigastrumYou may need to apply enough pressure to help displace bowel gasAdjust image depth so the aorta is at the bottom of the screen
Head of pancreas - Use both transverse amp sagittal planes as the head can be quite long and continue left caudally for several centimeters
Body of Pancreas - Transverse probe Use the splenic vein to help identify the pancreas superficial to this
Tail of pancreas - Start with the probe transverse then angle the heel of the probe cephalad and left as the tail can be sitting up under the spleen Thus the spleen can be used as a window and a left intercostal coronal approach can also be utilized
Ultrasound AppearancesNormal appearance is usually homogeneous and almost isoechoic with the liverIt is frequently hyperechoic compared to the liver because of fatty infiltrationSizeVaries with age and historyApproximate normal measurements areHead 35mm (anterior to posterior)Neck 10-15mmTail 20mm
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Scanning TechniqueTechniqueBegin transversely high in the epigastrumYou may need to apply enough pressure to help displace bowel gasAdjust image depth so the aorta is at the bottom of the screen
Head of pancreas - Use both transverse amp sagittal planes as the head can be quite long and continue left caudally for several centimeters
Body of Pancreas - Transverse probe Use the splenic vein to help identify the pancreas superficial to this
Tail of pancreas - Start with the probe transverse then angle the heel of the probe cephalad and left as the tail can be sitting up under the spleen Thus the spleen can be used as a window and a left intercostal coronal approach can also be utilized
Ultrasound AppearancesNormal appearance is usually homogeneous and almost isoechoic with the liverIt is frequently hyperechoic compared to the liver because of fatty infiltrationSizeVaries with age and historyApproximate normal measurements areHead 35mm (anterior to posterior)Neck 10-15mmTail 20mm
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Ultrasound of the pancreas What to look for in pancreatic US Size Contour Texture Echogenicity Main pancreatic duct Common bile duct Major peripancreatic vessels(Portal vein superior mesenteric artery and vein Splenic artery and vein Aorta and inferior vena cava
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Pancreas and its proportions + neighboring anatomical structures in classic transverse epigastrial plain
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Pancreatic lipomatosis refers to fatty replacement of pancreatic parenchyma
This finding is most often associated with obesity and aging It tends to be commonest pathological condition involving the pancreas The condition may occasionally simulate a mass like lesion particularly when fatty replacement is uneven PathologySubtypeseven pancreatic lipomatosisuneven pancreatic lipomatosis
type 1a preferential fatty replacement of headtype 1b preferential fatty replacement of head neck and bodytype 2a preferential fatty replacement of head and uncinate processtype 2b fatty replacement of most of pancreas except peri biliary region
CausesSystemiccystic fibrosis (most common cause in childhood) metabolicendocrine hyperlipidemia diabetes mellitusstorage disease haemochromatosisdrugs steroidsinfectious viral infection sepsisLocalchronic pancreatitis
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Lipomatous pancreas - Pancreatic tissue brightness is much higher than the liver one
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Pancreas - Cystic LesionsPseudocyst - Think pseudocyst when there is a history of pancreatitis alcohol abuse stone disease or abdominal trauma and the lesion is unilocular or contains non-enhancing dependent debris Cystic neoplasm- Think of the possibility of a cystic neoplasm when there is no history of pancreatitis or trauma or when the cyst has internal septa a solid component central scar or wall calcification Mucinous cystic neoplasm - This is usually a unilocular cyst filled with mucin sometimes with wall calcification exclusively seen in womenSerous cystic neoplasm - This is a microcystic lesion that contains serous fluid with sometimes a characteristic scar which may calcify It can look like a branch-duct IPMN but SCN has no communication with the pancreatic duct The typical appearance makes a specific diagnosis possible which is important because SCN is the only tumor that is not premalignant Branch-duct IPMN - This tumor can look like a SCN but has no scar or calcifications MRCP or heavily weighted T2WI may show the connection to the pancreatic duct which is highly specific
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Benign cyst in the pancreatic tail
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Mucinous cystadenoma manifesting as a multiseptated cyst High-resolution endoscopic US image demonstrates the septated internal architecture of the cyst
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Mucinous cystic tumor Endoscopic US image shows a complex pancreatic cyst with internal septa
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Mucinous cystadenoma (MCA)
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Serous cystic adenoma Macroscopic type
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Acute pancreatitis refers to acute inflammation
of the pancreas The sonographic findings in acute pancreatitis include increased anteroposterior measurement of the pancreatic body at the level of the superior mesenteric artery Decreased pancreatic echogenicity compared with the liver heterogeneous echo pattern Focal intrapancreatic regions of abnormal echogenicity Focal massesHypoechoic peripancreatic areas of inflammation and acute peripancreatic fluid collections Diffuse decreased echogenicity focal contour and focal echogenicity changes within the pancreas are associated with extra-pancreatic disease is also noted
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Causes of Acute PancreatitisGallstones (45)
Alcohol (35)
Other (10)
Medications
Hypercalcemia
Hypertriglyceridemia
Obstruction
After endoscopic retrograde cholangiopancreatography
Heredity
Trauma
Viral infection
Vascular ischemia
Idiopathic (10)
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Pancreatic Diseases
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Acute pancreatitis - Pancreatic gland (P) is edematous and there is a fluid visible in front of the pancreas (Black anechogenic strip marked by arrows) From other anatomical structures we see splenic vein (SV) aorta (A) and inferior vena cava (IVC)
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Acute pancreatitis
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Pancreatitis with inhomogeneous swollen pancreas and extra-pancreaticsoft tissue edema caused by an obstructing bile duct stone
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Acute pancreatitis with area of inflammation localized to the at the pancreatic neck
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Pancreatitis with inhomogeneous pancreas and peripancreatic effusion
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Chronic pancreatitis - Granular structure of the gland with calcifications
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Chronic pancreatitis Transverse sonogram shows an echogenic enlarged pancreas with multiple small hyperechoic non-shadowing foci in the pancreas
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Chronic pancreatitis Longitudinal sonogram through the head of the pancreas (in the same patient as in the previous image) shows an echogenic pancreas with multiple small hyperechoic nonshadowing foci
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Chronic pancreatitis longitudinal US scan of pancreas head and part of body of pancreas is normal in size with regular borders a few small hyperechoicareas in pancreas parenchyma - calcification ndash non dilated pancreatic duct
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Pseudo-cyst - Big round object in a narrow contact with pancreatic headA tumour could be similar but it would not be probably so anechogenic
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Pseudo-cyst within the pancreatic head
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Pseudocyst at (a) conventional and (b) echo-enhanced ultrasound (a) Lesion with an echo-free pattern and a sharply delineated wall
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Chronic pancreatitis presented with moderate left upper quadrant pain Transverse sonogram through the pancreas
shows a 437-cm pseudocyst in the tail of the pancreas (arrow)
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Endoscopic US of small pancreatic head tumor obstructing the common bile duct
Pancreatic carcinoma
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Ultrasound image of the head of the pancreas of a mouse with a 4mm diameter tumor
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Endoscopic Ultrasound (EUS) of pancreatic head mass and liver metastasis
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Pancreatic tumour - Pancreatic head is enlarged by a hypoechogenic massThe tumour probably also blocks the pancreatic duct which seems to be dilated
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Cystic mass in the pancreatic head with a normal pancreatic corpus and tail and normal bile ducts Histology proved this to be a pancreatic adenocarcinoma
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Pancreatic adenocarcinoma with solid focal irregular hypoechoic mass
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Ultrasonographic examination of pancreatic carcinoma localized in the head of the pancreas
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Pancreatic endocrine islet cell tumors (PETs) are
predominantly well-differentiated pancreatic or peripancreatic tumors that demonstrate endocrine differentiation They include Insulinoma Gastrinoma Glucagonoma Somatostatinoma and VIP-Oma (vasoactive intestinal polypeptide) Endoscopic US is sensitive for diagnosis
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Islet cell tumor manifesting as a cyst with a solid component endoscopic US image obtained in a patient with a malignant primary neuroendocrine tumor of the pancreas show a cystic lesion in the pancreatic body with peripheral mural nodules (arrows)
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
EUS image of gastrinoma (TU) in the tail of the pancreas next to the pancreaticduct (P GANG) and splenic vein (VLIENALIS) measuring 1 cm in diameter
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Insulinoma of the pancreatic body US and CT images
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You
Burkitt lymphoma longitudinal US scan of pancreas globally enlarged pancreas with decreased non-homogenous echogenicity not dilated duct
Burkitt lymphoma longitudinal US scan of pancreas no increased blood flow in Doppler
Thank You