Presentation1.pptx, radiological imaging of peri natal acute ischemia and hypoxic ischemic...
-
Upload
abdellah-nazeer -
Category
Documents
-
view
556 -
download
0
Transcript of Presentation1.pptx, radiological imaging of peri natal acute ischemia and hypoxic ischemic...

Radiological imaging of peri-natal acute ischemia
and hypoxic ischemic encephalopathy
Dr ABD ALLAH NAZEER MD
Perinatal acute Stroke similar to a stroke which occurs
in adults is defined as a disturbance to the blood supply of the developing brain This description includes both ischemicevents which results from a blockage of vessels and hypoxicevents which results from a lack of oxygen to the brain tissue as well as some combination of the two A neonatal stroke occurs in approximately 1 in 4000 births but is likely much higher due to the lack of noticeable symptoms One treatment with some proven benefits is hypothermia but may be most beneficial in conjunction with pharmacological agents Neonatal strokes may lead to cerebral palsy learning difficulties or other disabilities Well-designed clinical trialsfor stroke treatment in neonates are lacking but some current studies involve the transplantation of neural stem cells and umbilical cord stem cells it is not yet known if this therapy is likely to be successful
Risk FactorsMany different risk factors play a role in causing a neonatal stroke Some maternal disorders that may contribute to neonatal strokes include autoimmune disorders coagulation disorders prenatal cocaine exposure infection congenital heart disease diabetes and trauma Placental disorders that increase the risk of stroke include placental thrombosis placental abruption placental infection and chorioamnionitis Other disorders that may increase the risk of a neonatal stroke are blood homocysteine and lipid disorders such as polycythemia disseminated intravascular coagulopathy prothrombinmutation lipoprotein (a) deficiency Factor VIII deficiency and Factor V Leiden mutation Infectious disorders such as central nervous system (CNS) infection or systemic infection may also contributeMany infants who suffer a neonatal stroke also follow an uncomplicated pregnancy and delivery without identifiable risk factors which exemplifies the necessity for further research on this subject
Perinatal arterial ischemic stroke (PAIS) has an estimated incidence
of 1 in 2300 live births Most often PAIS presents with convulsions Initial assessment is performed with (Doppler) ultrasound and amplitude-integrated electroencephalography (aEEG) Magnetic resonance imaging (MRI) is used to confirm PAIS Although neonatal MRI enables prediction of motor outcome in PAIS patients by localizing the stroke area according to the posterior limb of the internal capsule or by visualizing pre-Wallerian degeneration it remains difficult to determine the viability of brain tissue after stroke In adults it has been shown that
arterial spin labeling (ASL) perfusion MRI a noninvasive technique is
valuable for the assessment of acute stroke Perfusion deficits and perfusionndashdiffusion mismatches as visualized on the ASL images have been proven to correspond with dynamic susceptibility contrast-enhanced images Furthermore a relation between perfusion in the affected hemisphere and outcome has been shown Although noninvasive ASL perfusion imaging seems to be a promising tool in the neonatal population experience is still limited and only one study has described the use of ASL MRI in the evaluation of PAIS ASL MRI could demonstrate areas of hypo- and hyperperfusion in patients with PAIS However ASL has not yet been used to assess changes in perfusion (abnormalities) over time in neonates with stroke In addition regional cerebral oxygenation (rScO2) was monitored compared with reported rScO2 values in neonates (63thinspplusmnthinsp12 and analyzed as a function of the perfusion signal as visualized on the ASL MR images
Radiographic features
CTdiffuse edema with effacement of the CSF-containing spacesdecreased cortical gray matter attenuation with loss of normal gray-white differentiationdecreased bilateral basal ganglia attenuationreversal sign reversal of the normal CT attenuation of grey and white matter demonstrated within the first 24 hours in a small number of these patients
it has been proposed that this finding is due to the distention of deep medullary veins secondary to partial obstruction of venous outflow from the elevated intracranial pressure caused by diffuse edemathe end result is that the cerebral white matter is of higher attenuation than the cortical gray matter
white cerebellum sign has been described in at least one study as a component of the reversal sign and in which there is diffuse edema and hypoattenuation of the cerebral hemispheres with sparing of the cerebellum and brainstem resulting in apparent high attenuation of the cerebellum and brainstem relative to the cerebral hemisphereslinear hyperdensity outlining the cortex as well as linear cortical enhancement (later and less evident signs) correspond to cortical laminar necrosis
MRIDiffusion-weighted MR imaging is the earliest imaging modality to become positive usually within the first few hours after a hypoxic-ischemic event due to early cytotoxic edema During the first 24 hours there may be restricted diffusion in the cerebellar hemispheres basal ganglia or cerebral cortex (in particular the perirolandic and occipital cortices) The thalami brainstem or hippocampi may also be involved Diffusion-weighted imaging abnormalities usually pseudo-normalize by the end of the 1st week As in younger patients conventional T1 and T2 weighted images are often normal or demonstrate only very subtle abnormalities In the early subacute period (24 hoursndash2 weeks) conventional T2 weighted images typically become positive and demonstrate increased signal intensity and swelling of the injured gray matter structures T1 hyperintensities signaling cortical laminar necrosis become evident after two weeks This hyperintense signal does not represent hemorrhage its believed to be caused by the accumulation of denatured proteins in dying cells This hyperintensity can be seen also within a few days on FLAIR
Acute Ischemic Stroke NECT and Axial DWI-diffusion
CT of a 7 day old with history of perinatal asphyxia shows diffuse low attenuating supratentorial brain parenchyma with relatively hyperdense Cerebellum - CT Reversal sign of Global hypoxia
CT scan show bilateral hypodensity involving the basal ganglia and the thalami Axial T1WI show hyperintensity of the basal gangliaAxial T2WI shows corresponding hypointensity DWI reveals hyperintensity at the basal ganglia hippocampi and occipital lobes consistent with restricted diffusion of acute ischemic injury
CT without and with iv contrast Axial T2 with bilateral thalamic infarct
Global hypoxic-ischemic brain injury
Hypoxic-ischemic brain injury
Images show the temporal evolution of a right-sided main branch MCA territory infarction (patient 1) on T1-weighted images (top row) and T2-weighted images (bottom row) obtained on days 2 5 12 42 and 75 post-delivery
Graph shows DWIs of a patient with an infarction within the PCA territory showing severe HSI on day 3 (A) and mild-to-moderate HSI on day 10 (B)
MRI Diffusion show bilateral fronto parietal and parieto occipital cortical restricted diffusion Similar restricted diffusion in caudate nuclei Area of involvement corresponds to cortical as well as internal border zone infarcts Imaging wise Bilateral border infarcts
A Axial T2-weighted fast spin-echo image (3200851) with an echo train length of 8 obtained at 13 hours of life shows no abnormality B Trace LSDI image (15206251) with a b max of 750 secondsmm2 obtained at 13 hours of life shows no abnormality C Corresponding ADC map D Axial T2-weighted fast spin-echo image obtained at 5 days of life shows very subtle hyperintensity in the posterior putamen bilaterally (arrows) E Trace LSDI image obtained at 5 days of life shows decreased diffusion in corresponding areas (arrows) F Corresponding ADC map G T1-weighted axial spin-echo image (600202) obtained at 6 weeks of life shows hyperintensity within the posterior putamen and ventrolateral thalamus bilaterally (arrows)
The neonatal mean diffusion-weighted image (mDWI) shows an ischemic area in the middle cerebral artery territory which resulted in a cyst observed at 3 and 24 mo The neonatal Z map shows normal Z values in all regions At 3 mo low Z values representing abnormal fractional anisotropy (FA) values were observed in the affected corticospinal tract which corresponded with the subsequent development of unilateral motor deficits The Z map at 24 mo was essentially identical Interestingly FA values in the fornix continued to decrease from the time of the neonatal scan to 24 mo suggesting delayed degeneration in this tract
Restricted diffusion signal in the DCST Left middle cerebral artery infarction (A) results in DWI signal changes throughout the DCST PLIC and cerebral peduncle involvement are evident on coronal (B) and sagittal images (C) Signal in the basis pontis and medullary pyramids can be seen on left (D) but not right (E) parasagittal sections
Neonate with left middle cerebral artery stroke and chronic hemiparesis DWI signal is appreciated throughout the DCST including PLIC (A) peduncle (B C) pons (D E) and pontomedullary junction (F)
Axial diffusion weighted images from a neonate (A) with a modified pediatric ASPECTS of eight (involvement of left internal capsule insula M3 M5 M6 P1 P2 and thalamus) and a child (B) with a modified pediatric ASPECTS of 10 (involvement of left caudate lentiform internal capsule insula and middle cerebral artery territories M1ndashM6)
(A) Axial diffusion-weighted image showing hyperintensity in the territory of left middle cerebral artery (B) MR angiography demonstrates loss of flow distal to the left middle cerebral artery bifurcation
A B
Perinatal asphyxia more appropriately known as hypoxic-
ischemic encephalopathy (HIE) is characterized by clinical and laboratory evidence of acute or subacute brain injury due to asphyxia The primary causes of this condition are systemic hypoxemia andor reduced cerebral blood flow (CBF) Birth asphyxia causes 840000 or 23 of all neonatal deaths worldwideHIE- Acute brain injury that occur before during or after birth
Signs and symptomsMild hypoxic-ischemic encephalopathybullMuscle tone may be slightly increased and deep tendon reflexes may be brisk during the first few daysbullTransient behavioral abnormalities such as poor feeding irritability or excessive crying or sleepiness (typically in an alternating pattern) may be observed bullTypically resolves in 24h
Moderately severe hypoxic-ischemic encephalopathyThe infant is lethargic with significant hypotonia and diminished deep tendon reflexesThe grasping Moro and sucking reflexes may be sluggish or absentThe infant may experience occasional periods of apneaSeizures typically occur early within the first 24 hours after birthFull recovery within 1-2 weeks is possible and is associated with a better long-term outcome
Severe hypoxic-ischemic encephalopathySeizures can be delayed and severe and may be initially resistant to conventional treatments The seizures are usually generalized and their frequency may increase during the 24-48 hours after onset correlating with the phase of reperfusion injury As the injury progresses seizures subside and the electroencephalogram becomes isoelectric or shows a burst suppression pattern At that time wakefulness may deteriorate further and the fontanelle may bulge suggesting increasing cerebral edema
Other symptoms include the following Stupor or coma is typical the infant may not respond to any physical stimulus except the most noxiousBreathing may be irregular and the infant often requires ventilatory support Generalized hypotonia and depressed deep tendon reflexes are common Neonatal reflexes (eg sucking swallowing grasping Moro) are absent Disturbances of ocular motion such as a skewed deviation of the eyes nystagmus bobbing and loss of dolls eye (ie conjugate) movements may be revealed by cranial nerve examination Pupils may be dilated fixed or poorly reactive to lightIrregularities of heart rate and blood pressure are common during the period of reperfusion injury as is death from cardiorespiratory failure An initial period of well-being or mild hypoxic-ischemic encephalopathy may be followed by sudden deterioration suggesting ongoing brain cell dysfunction injury and death during this period seizure intensity may increase
Imaging of neonatal hypoxic-ischemic encephalopathy
Ultrasonography is the first-line imaging technique for the evaluation of the newborn brain These past few years have seen an increasing role of MRI in the investigation of HIE because of greater sensitivity and specificity Electro-encephalogram(EEG)Computed Tomography(CT)MRI MRS and DWI
MRI sequencesT1 WI T2 WI++ FLAIR are not very useful to detect lesion in young infant less than 24 months due to brain maturation IR T1-weighted Has been very helpful in the last two decades before generalization of high fields MRI as it gives excellent images of brain anatomy and maturation It also shows accurately the differentiation between myelinated and unmyelinated WM Three-dimensional GE T1 weighted sequence (3DT1) bullallow 1 mm contiguous slices which can be reconstructed in any anatomic plane T2 to detect hemorrhagic lesions DWI It is now recommended that DWI should be performed between 2 days and 8 days of life Multiple studies have shown DWI are more sensitive in the detection of HIE lesions than conventional MRI especially for early diagnosis
MRI ProtocolSagittal and axial T1 WI Axial and coronal T2 WI Axial T2 3D T1 FLAIR (older child) DWI MRSLactate peak bulldue to anaerobic glycolysis bullfound within 24 h of life Subsequently a reduction in N-acetyl aspartate (NAA) is evident due to neuronal loss
Advanced technique Perfusion
Arterial Spin-Labeled (ASL) Perfusion bullRecent advances in novel research imaging modalitybullallows noninvasive evaluation of CBF (cerebral blood flow) using electromagnetically labeled arterial blood water as an endogenous contrast agent bullDemonstrates low CBF in neonates who have suffered HIE and in infants and children after stroke
Imaging RecommendationCranial sonography (US) bullFirst between 7 and 14 days bullRepeat before discharge from the hospital MRI DWI MRS bullWhen US is abnormal MRI precise lesion extension and aide in prognosticating bull Defining injury in VLBW neonates with normal US
PrognosisPoor outcome if bullIVH plus PVL bullPVL with volume loss widespread infarction or seizures bullPVL with enlarged cysts
It is necessary to bullknow the normal cerebral appearance before interpret pathological aspect bulldistinguish hypoxic-ischemic brain damage from normal myelination Brain compositionChanges in brain composition Changes in cellular density increase in complex lipids content due to the evolving process of myelination decrease in water content mostly in the WM
Shortening of T1 Shortening of T2
Imaging PatternThe imaging patterns of HIE can be classified into 3 types Lesions predominantly located in the PVWM Lesions predominantly located in the basal ganglia or thalamus Multicystic encephalomalcia The pattern of injury is postulated to depend on bull The type of hypoxiandashischaemia (acute and profound or prolonged and partial) bullThe gestational age (term or pre-term)
HIE in preterm infantRisk FactorsPregnancy Gestational ageweight previous preterm birth spontaneous preterm labor Intrapartum Abruption pre-eclampsia premature rupture of membranes chorioamnionitis group B Strep Peri amp postnatal factors Respiratory distress sepsis anemia apnea bradycardia cardiac arrest
General Features++ PVL +- associated to Germinal matrix and IVH PV hemorrhagic infarction Cerebellar infarction Definition bullPVL is the HIE driven periventricular white matter (PVWM) necrosis seen in very low birth weight premies (lt1500g) EpidemiologybullBirth weight lt 1500 g 45 incidence of PVL (higher if associated with IVH) bullGestational age lt 33 weeks 38 incidence of PVL bullgt 50 of patients with PVL or grade III IVH develop cerebral palsy
Cranial ultrasound coronal view day 1 showing severe echogenicity in the white matter MRI (T2SE (TR 6284TE 120) and ADC) performed on day 3 showing increased signal intensity in the white matter on T2SE and low signal intensity in the deep white matter on the ADC map with sparing of the anterior periventricular white matter and asymmetrical distribution in the parieto-occipital white matter The child died and was subsequently diagnosed to have molybdenum cofactor deficiency
Cranial sonography in 5-day old term with HIE with increase in echogenicity of white matter consistent with edemaCD ultrasound shows reversal of diastolic flow reflecting increased vascular resistance secondary to edema
PVL in a preterm infant (a) Coronal head US image obtained in the 1st week of life shows increased echogenicity in the periventricular white matter (arrows) (b) Follow-up US image obtained 2 months later shows development of cystic changes in these regions and dilatation of the adjacent lateral ventricles findings that are consistent with PVL
CT images show decrease In basal ganglia density related to Cytotoxic edemaSubtle loss of the normally sharp Transition from grey matter to White matter at the corticomedullary Junction Cerebral edema seen with effacementof the cortical sulci and the sylvian Fissures
PVL in a preterm neonate Axial T1-weighted (a) and T2-weighted (b) MR images obtained on day 4 of life demonstrate T1 hypointensity and T2 hyperintensity in the periventricular whitematter Note the punctate foci of high signal intensity on the T1-weighted image (arrows in a) These foci should be distinguished from foci of hemorrhage whichwould demonstrate greater T2 shortening on the corresponding T2-weighted image
28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
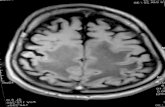
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

Perinatal acute Stroke similar to a stroke which occurs
in adults is defined as a disturbance to the blood supply of the developing brain This description includes both ischemicevents which results from a blockage of vessels and hypoxicevents which results from a lack of oxygen to the brain tissue as well as some combination of the two A neonatal stroke occurs in approximately 1 in 4000 births but is likely much higher due to the lack of noticeable symptoms One treatment with some proven benefits is hypothermia but may be most beneficial in conjunction with pharmacological agents Neonatal strokes may lead to cerebral palsy learning difficulties or other disabilities Well-designed clinical trialsfor stroke treatment in neonates are lacking but some current studies involve the transplantation of neural stem cells and umbilical cord stem cells it is not yet known if this therapy is likely to be successful
Risk FactorsMany different risk factors play a role in causing a neonatal stroke Some maternal disorders that may contribute to neonatal strokes include autoimmune disorders coagulation disorders prenatal cocaine exposure infection congenital heart disease diabetes and trauma Placental disorders that increase the risk of stroke include placental thrombosis placental abruption placental infection and chorioamnionitis Other disorders that may increase the risk of a neonatal stroke are blood homocysteine and lipid disorders such as polycythemia disseminated intravascular coagulopathy prothrombinmutation lipoprotein (a) deficiency Factor VIII deficiency and Factor V Leiden mutation Infectious disorders such as central nervous system (CNS) infection or systemic infection may also contributeMany infants who suffer a neonatal stroke also follow an uncomplicated pregnancy and delivery without identifiable risk factors which exemplifies the necessity for further research on this subject
Perinatal arterial ischemic stroke (PAIS) has an estimated incidence
of 1 in 2300 live births Most often PAIS presents with convulsions Initial assessment is performed with (Doppler) ultrasound and amplitude-integrated electroencephalography (aEEG) Magnetic resonance imaging (MRI) is used to confirm PAIS Although neonatal MRI enables prediction of motor outcome in PAIS patients by localizing the stroke area according to the posterior limb of the internal capsule or by visualizing pre-Wallerian degeneration it remains difficult to determine the viability of brain tissue after stroke In adults it has been shown that
arterial spin labeling (ASL) perfusion MRI a noninvasive technique is
valuable for the assessment of acute stroke Perfusion deficits and perfusionndashdiffusion mismatches as visualized on the ASL images have been proven to correspond with dynamic susceptibility contrast-enhanced images Furthermore a relation between perfusion in the affected hemisphere and outcome has been shown Although noninvasive ASL perfusion imaging seems to be a promising tool in the neonatal population experience is still limited and only one study has described the use of ASL MRI in the evaluation of PAIS ASL MRI could demonstrate areas of hypo- and hyperperfusion in patients with PAIS However ASL has not yet been used to assess changes in perfusion (abnormalities) over time in neonates with stroke In addition regional cerebral oxygenation (rScO2) was monitored compared with reported rScO2 values in neonates (63thinspplusmnthinsp12 and analyzed as a function of the perfusion signal as visualized on the ASL MR images
Radiographic features
CTdiffuse edema with effacement of the CSF-containing spacesdecreased cortical gray matter attenuation with loss of normal gray-white differentiationdecreased bilateral basal ganglia attenuationreversal sign reversal of the normal CT attenuation of grey and white matter demonstrated within the first 24 hours in a small number of these patients
it has been proposed that this finding is due to the distention of deep medullary veins secondary to partial obstruction of venous outflow from the elevated intracranial pressure caused by diffuse edemathe end result is that the cerebral white matter is of higher attenuation than the cortical gray matter
white cerebellum sign has been described in at least one study as a component of the reversal sign and in which there is diffuse edema and hypoattenuation of the cerebral hemispheres with sparing of the cerebellum and brainstem resulting in apparent high attenuation of the cerebellum and brainstem relative to the cerebral hemisphereslinear hyperdensity outlining the cortex as well as linear cortical enhancement (later and less evident signs) correspond to cortical laminar necrosis
MRIDiffusion-weighted MR imaging is the earliest imaging modality to become positive usually within the first few hours after a hypoxic-ischemic event due to early cytotoxic edema During the first 24 hours there may be restricted diffusion in the cerebellar hemispheres basal ganglia or cerebral cortex (in particular the perirolandic and occipital cortices) The thalami brainstem or hippocampi may also be involved Diffusion-weighted imaging abnormalities usually pseudo-normalize by the end of the 1st week As in younger patients conventional T1 and T2 weighted images are often normal or demonstrate only very subtle abnormalities In the early subacute period (24 hoursndash2 weeks) conventional T2 weighted images typically become positive and demonstrate increased signal intensity and swelling of the injured gray matter structures T1 hyperintensities signaling cortical laminar necrosis become evident after two weeks This hyperintense signal does not represent hemorrhage its believed to be caused by the accumulation of denatured proteins in dying cells This hyperintensity can be seen also within a few days on FLAIR
Acute Ischemic Stroke NECT and Axial DWI-diffusion
CT of a 7 day old with history of perinatal asphyxia shows diffuse low attenuating supratentorial brain parenchyma with relatively hyperdense Cerebellum - CT Reversal sign of Global hypoxia
CT scan show bilateral hypodensity involving the basal ganglia and the thalami Axial T1WI show hyperintensity of the basal gangliaAxial T2WI shows corresponding hypointensity DWI reveals hyperintensity at the basal ganglia hippocampi and occipital lobes consistent with restricted diffusion of acute ischemic injury
CT without and with iv contrast Axial T2 with bilateral thalamic infarct
Global hypoxic-ischemic brain injury
Hypoxic-ischemic brain injury
Images show the temporal evolution of a right-sided main branch MCA territory infarction (patient 1) on T1-weighted images (top row) and T2-weighted images (bottom row) obtained on days 2 5 12 42 and 75 post-delivery
Graph shows DWIs of a patient with an infarction within the PCA territory showing severe HSI on day 3 (A) and mild-to-moderate HSI on day 10 (B)
MRI Diffusion show bilateral fronto parietal and parieto occipital cortical restricted diffusion Similar restricted diffusion in caudate nuclei Area of involvement corresponds to cortical as well as internal border zone infarcts Imaging wise Bilateral border infarcts
A Axial T2-weighted fast spin-echo image (3200851) with an echo train length of 8 obtained at 13 hours of life shows no abnormality B Trace LSDI image (15206251) with a b max of 750 secondsmm2 obtained at 13 hours of life shows no abnormality C Corresponding ADC map D Axial T2-weighted fast spin-echo image obtained at 5 days of life shows very subtle hyperintensity in the posterior putamen bilaterally (arrows) E Trace LSDI image obtained at 5 days of life shows decreased diffusion in corresponding areas (arrows) F Corresponding ADC map G T1-weighted axial spin-echo image (600202) obtained at 6 weeks of life shows hyperintensity within the posterior putamen and ventrolateral thalamus bilaterally (arrows)
The neonatal mean diffusion-weighted image (mDWI) shows an ischemic area in the middle cerebral artery territory which resulted in a cyst observed at 3 and 24 mo The neonatal Z map shows normal Z values in all regions At 3 mo low Z values representing abnormal fractional anisotropy (FA) values were observed in the affected corticospinal tract which corresponded with the subsequent development of unilateral motor deficits The Z map at 24 mo was essentially identical Interestingly FA values in the fornix continued to decrease from the time of the neonatal scan to 24 mo suggesting delayed degeneration in this tract
Restricted diffusion signal in the DCST Left middle cerebral artery infarction (A) results in DWI signal changes throughout the DCST PLIC and cerebral peduncle involvement are evident on coronal (B) and sagittal images (C) Signal in the basis pontis and medullary pyramids can be seen on left (D) but not right (E) parasagittal sections
Neonate with left middle cerebral artery stroke and chronic hemiparesis DWI signal is appreciated throughout the DCST including PLIC (A) peduncle (B C) pons (D E) and pontomedullary junction (F)
Axial diffusion weighted images from a neonate (A) with a modified pediatric ASPECTS of eight (involvement of left internal capsule insula M3 M5 M6 P1 P2 and thalamus) and a child (B) with a modified pediatric ASPECTS of 10 (involvement of left caudate lentiform internal capsule insula and middle cerebral artery territories M1ndashM6)
(A) Axial diffusion-weighted image showing hyperintensity in the territory of left middle cerebral artery (B) MR angiography demonstrates loss of flow distal to the left middle cerebral artery bifurcation
A B
Perinatal asphyxia more appropriately known as hypoxic-
ischemic encephalopathy (HIE) is characterized by clinical and laboratory evidence of acute or subacute brain injury due to asphyxia The primary causes of this condition are systemic hypoxemia andor reduced cerebral blood flow (CBF) Birth asphyxia causes 840000 or 23 of all neonatal deaths worldwideHIE- Acute brain injury that occur before during or after birth
Signs and symptomsMild hypoxic-ischemic encephalopathybullMuscle tone may be slightly increased and deep tendon reflexes may be brisk during the first few daysbullTransient behavioral abnormalities such as poor feeding irritability or excessive crying or sleepiness (typically in an alternating pattern) may be observed bullTypically resolves in 24h
Moderately severe hypoxic-ischemic encephalopathyThe infant is lethargic with significant hypotonia and diminished deep tendon reflexesThe grasping Moro and sucking reflexes may be sluggish or absentThe infant may experience occasional periods of apneaSeizures typically occur early within the first 24 hours after birthFull recovery within 1-2 weeks is possible and is associated with a better long-term outcome
Severe hypoxic-ischemic encephalopathySeizures can be delayed and severe and may be initially resistant to conventional treatments The seizures are usually generalized and their frequency may increase during the 24-48 hours after onset correlating with the phase of reperfusion injury As the injury progresses seizures subside and the electroencephalogram becomes isoelectric or shows a burst suppression pattern At that time wakefulness may deteriorate further and the fontanelle may bulge suggesting increasing cerebral edema
Other symptoms include the following Stupor or coma is typical the infant may not respond to any physical stimulus except the most noxiousBreathing may be irregular and the infant often requires ventilatory support Generalized hypotonia and depressed deep tendon reflexes are common Neonatal reflexes (eg sucking swallowing grasping Moro) are absent Disturbances of ocular motion such as a skewed deviation of the eyes nystagmus bobbing and loss of dolls eye (ie conjugate) movements may be revealed by cranial nerve examination Pupils may be dilated fixed or poorly reactive to lightIrregularities of heart rate and blood pressure are common during the period of reperfusion injury as is death from cardiorespiratory failure An initial period of well-being or mild hypoxic-ischemic encephalopathy may be followed by sudden deterioration suggesting ongoing brain cell dysfunction injury and death during this period seizure intensity may increase
Imaging of neonatal hypoxic-ischemic encephalopathy
Ultrasonography is the first-line imaging technique for the evaluation of the newborn brain These past few years have seen an increasing role of MRI in the investigation of HIE because of greater sensitivity and specificity Electro-encephalogram(EEG)Computed Tomography(CT)MRI MRS and DWI
MRI sequencesT1 WI T2 WI++ FLAIR are not very useful to detect lesion in young infant less than 24 months due to brain maturation IR T1-weighted Has been very helpful in the last two decades before generalization of high fields MRI as it gives excellent images of brain anatomy and maturation It also shows accurately the differentiation between myelinated and unmyelinated WM Three-dimensional GE T1 weighted sequence (3DT1) bullallow 1 mm contiguous slices which can be reconstructed in any anatomic plane T2 to detect hemorrhagic lesions DWI It is now recommended that DWI should be performed between 2 days and 8 days of life Multiple studies have shown DWI are more sensitive in the detection of HIE lesions than conventional MRI especially for early diagnosis
MRI ProtocolSagittal and axial T1 WI Axial and coronal T2 WI Axial T2 3D T1 FLAIR (older child) DWI MRSLactate peak bulldue to anaerobic glycolysis bullfound within 24 h of life Subsequently a reduction in N-acetyl aspartate (NAA) is evident due to neuronal loss
Advanced technique Perfusion
Arterial Spin-Labeled (ASL) Perfusion bullRecent advances in novel research imaging modalitybullallows noninvasive evaluation of CBF (cerebral blood flow) using electromagnetically labeled arterial blood water as an endogenous contrast agent bullDemonstrates low CBF in neonates who have suffered HIE and in infants and children after stroke
Imaging RecommendationCranial sonography (US) bullFirst between 7 and 14 days bullRepeat before discharge from the hospital MRI DWI MRS bullWhen US is abnormal MRI precise lesion extension and aide in prognosticating bull Defining injury in VLBW neonates with normal US
PrognosisPoor outcome if bullIVH plus PVL bullPVL with volume loss widespread infarction or seizures bullPVL with enlarged cysts
It is necessary to bullknow the normal cerebral appearance before interpret pathological aspect bulldistinguish hypoxic-ischemic brain damage from normal myelination Brain compositionChanges in brain composition Changes in cellular density increase in complex lipids content due to the evolving process of myelination decrease in water content mostly in the WM
Shortening of T1 Shortening of T2
Imaging PatternThe imaging patterns of HIE can be classified into 3 types Lesions predominantly located in the PVWM Lesions predominantly located in the basal ganglia or thalamus Multicystic encephalomalcia The pattern of injury is postulated to depend on bull The type of hypoxiandashischaemia (acute and profound or prolonged and partial) bullThe gestational age (term or pre-term)
HIE in preterm infantRisk FactorsPregnancy Gestational ageweight previous preterm birth spontaneous preterm labor Intrapartum Abruption pre-eclampsia premature rupture of membranes chorioamnionitis group B Strep Peri amp postnatal factors Respiratory distress sepsis anemia apnea bradycardia cardiac arrest
General Features++ PVL +- associated to Germinal matrix and IVH PV hemorrhagic infarction Cerebellar infarction Definition bullPVL is the HIE driven periventricular white matter (PVWM) necrosis seen in very low birth weight premies (lt1500g) EpidemiologybullBirth weight lt 1500 g 45 incidence of PVL (higher if associated with IVH) bullGestational age lt 33 weeks 38 incidence of PVL bullgt 50 of patients with PVL or grade III IVH develop cerebral palsy
Cranial ultrasound coronal view day 1 showing severe echogenicity in the white matter MRI (T2SE (TR 6284TE 120) and ADC) performed on day 3 showing increased signal intensity in the white matter on T2SE and low signal intensity in the deep white matter on the ADC map with sparing of the anterior periventricular white matter and asymmetrical distribution in the parieto-occipital white matter The child died and was subsequently diagnosed to have molybdenum cofactor deficiency
Cranial sonography in 5-day old term with HIE with increase in echogenicity of white matter consistent with edemaCD ultrasound shows reversal of diastolic flow reflecting increased vascular resistance secondary to edema
PVL in a preterm infant (a) Coronal head US image obtained in the 1st week of life shows increased echogenicity in the periventricular white matter (arrows) (b) Follow-up US image obtained 2 months later shows development of cystic changes in these regions and dilatation of the adjacent lateral ventricles findings that are consistent with PVL
CT images show decrease In basal ganglia density related to Cytotoxic edemaSubtle loss of the normally sharp Transition from grey matter to White matter at the corticomedullary Junction Cerebral edema seen with effacementof the cortical sulci and the sylvian Fissures
PVL in a preterm neonate Axial T1-weighted (a) and T2-weighted (b) MR images obtained on day 4 of life demonstrate T1 hypointensity and T2 hyperintensity in the periventricular whitematter Note the punctate foci of high signal intensity on the T1-weighted image (arrows in a) These foci should be distinguished from foci of hemorrhage whichwould demonstrate greater T2 shortening on the corresponding T2-weighted image
28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

Risk FactorsMany different risk factors play a role in causing a neonatal stroke Some maternal disorders that may contribute to neonatal strokes include autoimmune disorders coagulation disorders prenatal cocaine exposure infection congenital heart disease diabetes and trauma Placental disorders that increase the risk of stroke include placental thrombosis placental abruption placental infection and chorioamnionitis Other disorders that may increase the risk of a neonatal stroke are blood homocysteine and lipid disorders such as polycythemia disseminated intravascular coagulopathy prothrombinmutation lipoprotein (a) deficiency Factor VIII deficiency and Factor V Leiden mutation Infectious disorders such as central nervous system (CNS) infection or systemic infection may also contributeMany infants who suffer a neonatal stroke also follow an uncomplicated pregnancy and delivery without identifiable risk factors which exemplifies the necessity for further research on this subject
Perinatal arterial ischemic stroke (PAIS) has an estimated incidence
of 1 in 2300 live births Most often PAIS presents with convulsions Initial assessment is performed with (Doppler) ultrasound and amplitude-integrated electroencephalography (aEEG) Magnetic resonance imaging (MRI) is used to confirm PAIS Although neonatal MRI enables prediction of motor outcome in PAIS patients by localizing the stroke area according to the posterior limb of the internal capsule or by visualizing pre-Wallerian degeneration it remains difficult to determine the viability of brain tissue after stroke In adults it has been shown that
arterial spin labeling (ASL) perfusion MRI a noninvasive technique is
valuable for the assessment of acute stroke Perfusion deficits and perfusionndashdiffusion mismatches as visualized on the ASL images have been proven to correspond with dynamic susceptibility contrast-enhanced images Furthermore a relation between perfusion in the affected hemisphere and outcome has been shown Although noninvasive ASL perfusion imaging seems to be a promising tool in the neonatal population experience is still limited and only one study has described the use of ASL MRI in the evaluation of PAIS ASL MRI could demonstrate areas of hypo- and hyperperfusion in patients with PAIS However ASL has not yet been used to assess changes in perfusion (abnormalities) over time in neonates with stroke In addition regional cerebral oxygenation (rScO2) was monitored compared with reported rScO2 values in neonates (63thinspplusmnthinsp12 and analyzed as a function of the perfusion signal as visualized on the ASL MR images
Radiographic features
CTdiffuse edema with effacement of the CSF-containing spacesdecreased cortical gray matter attenuation with loss of normal gray-white differentiationdecreased bilateral basal ganglia attenuationreversal sign reversal of the normal CT attenuation of grey and white matter demonstrated within the first 24 hours in a small number of these patients
it has been proposed that this finding is due to the distention of deep medullary veins secondary to partial obstruction of venous outflow from the elevated intracranial pressure caused by diffuse edemathe end result is that the cerebral white matter is of higher attenuation than the cortical gray matter
white cerebellum sign has been described in at least one study as a component of the reversal sign and in which there is diffuse edema and hypoattenuation of the cerebral hemispheres with sparing of the cerebellum and brainstem resulting in apparent high attenuation of the cerebellum and brainstem relative to the cerebral hemisphereslinear hyperdensity outlining the cortex as well as linear cortical enhancement (later and less evident signs) correspond to cortical laminar necrosis
MRIDiffusion-weighted MR imaging is the earliest imaging modality to become positive usually within the first few hours after a hypoxic-ischemic event due to early cytotoxic edema During the first 24 hours there may be restricted diffusion in the cerebellar hemispheres basal ganglia or cerebral cortex (in particular the perirolandic and occipital cortices) The thalami brainstem or hippocampi may also be involved Diffusion-weighted imaging abnormalities usually pseudo-normalize by the end of the 1st week As in younger patients conventional T1 and T2 weighted images are often normal or demonstrate only very subtle abnormalities In the early subacute period (24 hoursndash2 weeks) conventional T2 weighted images typically become positive and demonstrate increased signal intensity and swelling of the injured gray matter structures T1 hyperintensities signaling cortical laminar necrosis become evident after two weeks This hyperintense signal does not represent hemorrhage its believed to be caused by the accumulation of denatured proteins in dying cells This hyperintensity can be seen also within a few days on FLAIR
Acute Ischemic Stroke NECT and Axial DWI-diffusion
CT of a 7 day old with history of perinatal asphyxia shows diffuse low attenuating supratentorial brain parenchyma with relatively hyperdense Cerebellum - CT Reversal sign of Global hypoxia
CT scan show bilateral hypodensity involving the basal ganglia and the thalami Axial T1WI show hyperintensity of the basal gangliaAxial T2WI shows corresponding hypointensity DWI reveals hyperintensity at the basal ganglia hippocampi and occipital lobes consistent with restricted diffusion of acute ischemic injury
CT without and with iv contrast Axial T2 with bilateral thalamic infarct
Global hypoxic-ischemic brain injury
Hypoxic-ischemic brain injury
Images show the temporal evolution of a right-sided main branch MCA territory infarction (patient 1) on T1-weighted images (top row) and T2-weighted images (bottom row) obtained on days 2 5 12 42 and 75 post-delivery
Graph shows DWIs of a patient with an infarction within the PCA territory showing severe HSI on day 3 (A) and mild-to-moderate HSI on day 10 (B)
MRI Diffusion show bilateral fronto parietal and parieto occipital cortical restricted diffusion Similar restricted diffusion in caudate nuclei Area of involvement corresponds to cortical as well as internal border zone infarcts Imaging wise Bilateral border infarcts
A Axial T2-weighted fast spin-echo image (3200851) with an echo train length of 8 obtained at 13 hours of life shows no abnormality B Trace LSDI image (15206251) with a b max of 750 secondsmm2 obtained at 13 hours of life shows no abnormality C Corresponding ADC map D Axial T2-weighted fast spin-echo image obtained at 5 days of life shows very subtle hyperintensity in the posterior putamen bilaterally (arrows) E Trace LSDI image obtained at 5 days of life shows decreased diffusion in corresponding areas (arrows) F Corresponding ADC map G T1-weighted axial spin-echo image (600202) obtained at 6 weeks of life shows hyperintensity within the posterior putamen and ventrolateral thalamus bilaterally (arrows)
The neonatal mean diffusion-weighted image (mDWI) shows an ischemic area in the middle cerebral artery territory which resulted in a cyst observed at 3 and 24 mo The neonatal Z map shows normal Z values in all regions At 3 mo low Z values representing abnormal fractional anisotropy (FA) values were observed in the affected corticospinal tract which corresponded with the subsequent development of unilateral motor deficits The Z map at 24 mo was essentially identical Interestingly FA values in the fornix continued to decrease from the time of the neonatal scan to 24 mo suggesting delayed degeneration in this tract
Restricted diffusion signal in the DCST Left middle cerebral artery infarction (A) results in DWI signal changes throughout the DCST PLIC and cerebral peduncle involvement are evident on coronal (B) and sagittal images (C) Signal in the basis pontis and medullary pyramids can be seen on left (D) but not right (E) parasagittal sections
Neonate with left middle cerebral artery stroke and chronic hemiparesis DWI signal is appreciated throughout the DCST including PLIC (A) peduncle (B C) pons (D E) and pontomedullary junction (F)
Axial diffusion weighted images from a neonate (A) with a modified pediatric ASPECTS of eight (involvement of left internal capsule insula M3 M5 M6 P1 P2 and thalamus) and a child (B) with a modified pediatric ASPECTS of 10 (involvement of left caudate lentiform internal capsule insula and middle cerebral artery territories M1ndashM6)
(A) Axial diffusion-weighted image showing hyperintensity in the territory of left middle cerebral artery (B) MR angiography demonstrates loss of flow distal to the left middle cerebral artery bifurcation
A B
Perinatal asphyxia more appropriately known as hypoxic-
ischemic encephalopathy (HIE) is characterized by clinical and laboratory evidence of acute or subacute brain injury due to asphyxia The primary causes of this condition are systemic hypoxemia andor reduced cerebral blood flow (CBF) Birth asphyxia causes 840000 or 23 of all neonatal deaths worldwideHIE- Acute brain injury that occur before during or after birth
Signs and symptomsMild hypoxic-ischemic encephalopathybullMuscle tone may be slightly increased and deep tendon reflexes may be brisk during the first few daysbullTransient behavioral abnormalities such as poor feeding irritability or excessive crying or sleepiness (typically in an alternating pattern) may be observed bullTypically resolves in 24h
Moderately severe hypoxic-ischemic encephalopathyThe infant is lethargic with significant hypotonia and diminished deep tendon reflexesThe grasping Moro and sucking reflexes may be sluggish or absentThe infant may experience occasional periods of apneaSeizures typically occur early within the first 24 hours after birthFull recovery within 1-2 weeks is possible and is associated with a better long-term outcome
Severe hypoxic-ischemic encephalopathySeizures can be delayed and severe and may be initially resistant to conventional treatments The seizures are usually generalized and their frequency may increase during the 24-48 hours after onset correlating with the phase of reperfusion injury As the injury progresses seizures subside and the electroencephalogram becomes isoelectric or shows a burst suppression pattern At that time wakefulness may deteriorate further and the fontanelle may bulge suggesting increasing cerebral edema
Other symptoms include the following Stupor or coma is typical the infant may not respond to any physical stimulus except the most noxiousBreathing may be irregular and the infant often requires ventilatory support Generalized hypotonia and depressed deep tendon reflexes are common Neonatal reflexes (eg sucking swallowing grasping Moro) are absent Disturbances of ocular motion such as a skewed deviation of the eyes nystagmus bobbing and loss of dolls eye (ie conjugate) movements may be revealed by cranial nerve examination Pupils may be dilated fixed or poorly reactive to lightIrregularities of heart rate and blood pressure are common during the period of reperfusion injury as is death from cardiorespiratory failure An initial period of well-being or mild hypoxic-ischemic encephalopathy may be followed by sudden deterioration suggesting ongoing brain cell dysfunction injury and death during this period seizure intensity may increase
Imaging of neonatal hypoxic-ischemic encephalopathy
Ultrasonography is the first-line imaging technique for the evaluation of the newborn brain These past few years have seen an increasing role of MRI in the investigation of HIE because of greater sensitivity and specificity Electro-encephalogram(EEG)Computed Tomography(CT)MRI MRS and DWI
MRI sequencesT1 WI T2 WI++ FLAIR are not very useful to detect lesion in young infant less than 24 months due to brain maturation IR T1-weighted Has been very helpful in the last two decades before generalization of high fields MRI as it gives excellent images of brain anatomy and maturation It also shows accurately the differentiation between myelinated and unmyelinated WM Three-dimensional GE T1 weighted sequence (3DT1) bullallow 1 mm contiguous slices which can be reconstructed in any anatomic plane T2 to detect hemorrhagic lesions DWI It is now recommended that DWI should be performed between 2 days and 8 days of life Multiple studies have shown DWI are more sensitive in the detection of HIE lesions than conventional MRI especially for early diagnosis
MRI ProtocolSagittal and axial T1 WI Axial and coronal T2 WI Axial T2 3D T1 FLAIR (older child) DWI MRSLactate peak bulldue to anaerobic glycolysis bullfound within 24 h of life Subsequently a reduction in N-acetyl aspartate (NAA) is evident due to neuronal loss
Advanced technique Perfusion
Arterial Spin-Labeled (ASL) Perfusion bullRecent advances in novel research imaging modalitybullallows noninvasive evaluation of CBF (cerebral blood flow) using electromagnetically labeled arterial blood water as an endogenous contrast agent bullDemonstrates low CBF in neonates who have suffered HIE and in infants and children after stroke
Imaging RecommendationCranial sonography (US) bullFirst between 7 and 14 days bullRepeat before discharge from the hospital MRI DWI MRS bullWhen US is abnormal MRI precise lesion extension and aide in prognosticating bull Defining injury in VLBW neonates with normal US
PrognosisPoor outcome if bullIVH plus PVL bullPVL with volume loss widespread infarction or seizures bullPVL with enlarged cysts
It is necessary to bullknow the normal cerebral appearance before interpret pathological aspect bulldistinguish hypoxic-ischemic brain damage from normal myelination Brain compositionChanges in brain composition Changes in cellular density increase in complex lipids content due to the evolving process of myelination decrease in water content mostly in the WM
Shortening of T1 Shortening of T2
Imaging PatternThe imaging patterns of HIE can be classified into 3 types Lesions predominantly located in the PVWM Lesions predominantly located in the basal ganglia or thalamus Multicystic encephalomalcia The pattern of injury is postulated to depend on bull The type of hypoxiandashischaemia (acute and profound or prolonged and partial) bullThe gestational age (term or pre-term)
HIE in preterm infantRisk FactorsPregnancy Gestational ageweight previous preterm birth spontaneous preterm labor Intrapartum Abruption pre-eclampsia premature rupture of membranes chorioamnionitis group B Strep Peri amp postnatal factors Respiratory distress sepsis anemia apnea bradycardia cardiac arrest
General Features++ PVL +- associated to Germinal matrix and IVH PV hemorrhagic infarction Cerebellar infarction Definition bullPVL is the HIE driven periventricular white matter (PVWM) necrosis seen in very low birth weight premies (lt1500g) EpidemiologybullBirth weight lt 1500 g 45 incidence of PVL (higher if associated with IVH) bullGestational age lt 33 weeks 38 incidence of PVL bullgt 50 of patients with PVL or grade III IVH develop cerebral palsy
Cranial ultrasound coronal view day 1 showing severe echogenicity in the white matter MRI (T2SE (TR 6284TE 120) and ADC) performed on day 3 showing increased signal intensity in the white matter on T2SE and low signal intensity in the deep white matter on the ADC map with sparing of the anterior periventricular white matter and asymmetrical distribution in the parieto-occipital white matter The child died and was subsequently diagnosed to have molybdenum cofactor deficiency
Cranial sonography in 5-day old term with HIE with increase in echogenicity of white matter consistent with edemaCD ultrasound shows reversal of diastolic flow reflecting increased vascular resistance secondary to edema
PVL in a preterm infant (a) Coronal head US image obtained in the 1st week of life shows increased echogenicity in the periventricular white matter (arrows) (b) Follow-up US image obtained 2 months later shows development of cystic changes in these regions and dilatation of the adjacent lateral ventricles findings that are consistent with PVL
CT images show decrease In basal ganglia density related to Cytotoxic edemaSubtle loss of the normally sharp Transition from grey matter to White matter at the corticomedullary Junction Cerebral edema seen with effacementof the cortical sulci and the sylvian Fissures
PVL in a preterm neonate Axial T1-weighted (a) and T2-weighted (b) MR images obtained on day 4 of life demonstrate T1 hypointensity and T2 hyperintensity in the periventricular whitematter Note the punctate foci of high signal intensity on the T1-weighted image (arrows in a) These foci should be distinguished from foci of hemorrhage whichwould demonstrate greater T2 shortening on the corresponding T2-weighted image
28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

Perinatal arterial ischemic stroke (PAIS) has an estimated incidence
of 1 in 2300 live births Most often PAIS presents with convulsions Initial assessment is performed with (Doppler) ultrasound and amplitude-integrated electroencephalography (aEEG) Magnetic resonance imaging (MRI) is used to confirm PAIS Although neonatal MRI enables prediction of motor outcome in PAIS patients by localizing the stroke area according to the posterior limb of the internal capsule or by visualizing pre-Wallerian degeneration it remains difficult to determine the viability of brain tissue after stroke In adults it has been shown that
arterial spin labeling (ASL) perfusion MRI a noninvasive technique is
valuable for the assessment of acute stroke Perfusion deficits and perfusionndashdiffusion mismatches as visualized on the ASL images have been proven to correspond with dynamic susceptibility contrast-enhanced images Furthermore a relation between perfusion in the affected hemisphere and outcome has been shown Although noninvasive ASL perfusion imaging seems to be a promising tool in the neonatal population experience is still limited and only one study has described the use of ASL MRI in the evaluation of PAIS ASL MRI could demonstrate areas of hypo- and hyperperfusion in patients with PAIS However ASL has not yet been used to assess changes in perfusion (abnormalities) over time in neonates with stroke In addition regional cerebral oxygenation (rScO2) was monitored compared with reported rScO2 values in neonates (63thinspplusmnthinsp12 and analyzed as a function of the perfusion signal as visualized on the ASL MR images
Radiographic features
CTdiffuse edema with effacement of the CSF-containing spacesdecreased cortical gray matter attenuation with loss of normal gray-white differentiationdecreased bilateral basal ganglia attenuationreversal sign reversal of the normal CT attenuation of grey and white matter demonstrated within the first 24 hours in a small number of these patients
it has been proposed that this finding is due to the distention of deep medullary veins secondary to partial obstruction of venous outflow from the elevated intracranial pressure caused by diffuse edemathe end result is that the cerebral white matter is of higher attenuation than the cortical gray matter
white cerebellum sign has been described in at least one study as a component of the reversal sign and in which there is diffuse edema and hypoattenuation of the cerebral hemispheres with sparing of the cerebellum and brainstem resulting in apparent high attenuation of the cerebellum and brainstem relative to the cerebral hemisphereslinear hyperdensity outlining the cortex as well as linear cortical enhancement (later and less evident signs) correspond to cortical laminar necrosis
MRIDiffusion-weighted MR imaging is the earliest imaging modality to become positive usually within the first few hours after a hypoxic-ischemic event due to early cytotoxic edema During the first 24 hours there may be restricted diffusion in the cerebellar hemispheres basal ganglia or cerebral cortex (in particular the perirolandic and occipital cortices) The thalami brainstem or hippocampi may also be involved Diffusion-weighted imaging abnormalities usually pseudo-normalize by the end of the 1st week As in younger patients conventional T1 and T2 weighted images are often normal or demonstrate only very subtle abnormalities In the early subacute period (24 hoursndash2 weeks) conventional T2 weighted images typically become positive and demonstrate increased signal intensity and swelling of the injured gray matter structures T1 hyperintensities signaling cortical laminar necrosis become evident after two weeks This hyperintense signal does not represent hemorrhage its believed to be caused by the accumulation of denatured proteins in dying cells This hyperintensity can be seen also within a few days on FLAIR
Acute Ischemic Stroke NECT and Axial DWI-diffusion
CT of a 7 day old with history of perinatal asphyxia shows diffuse low attenuating supratentorial brain parenchyma with relatively hyperdense Cerebellum - CT Reversal sign of Global hypoxia
CT scan show bilateral hypodensity involving the basal ganglia and the thalami Axial T1WI show hyperintensity of the basal gangliaAxial T2WI shows corresponding hypointensity DWI reveals hyperintensity at the basal ganglia hippocampi and occipital lobes consistent with restricted diffusion of acute ischemic injury
CT without and with iv contrast Axial T2 with bilateral thalamic infarct
Global hypoxic-ischemic brain injury
Hypoxic-ischemic brain injury
Images show the temporal evolution of a right-sided main branch MCA territory infarction (patient 1) on T1-weighted images (top row) and T2-weighted images (bottom row) obtained on days 2 5 12 42 and 75 post-delivery
Graph shows DWIs of a patient with an infarction within the PCA territory showing severe HSI on day 3 (A) and mild-to-moderate HSI on day 10 (B)
MRI Diffusion show bilateral fronto parietal and parieto occipital cortical restricted diffusion Similar restricted diffusion in caudate nuclei Area of involvement corresponds to cortical as well as internal border zone infarcts Imaging wise Bilateral border infarcts
A Axial T2-weighted fast spin-echo image (3200851) with an echo train length of 8 obtained at 13 hours of life shows no abnormality B Trace LSDI image (15206251) with a b max of 750 secondsmm2 obtained at 13 hours of life shows no abnormality C Corresponding ADC map D Axial T2-weighted fast spin-echo image obtained at 5 days of life shows very subtle hyperintensity in the posterior putamen bilaterally (arrows) E Trace LSDI image obtained at 5 days of life shows decreased diffusion in corresponding areas (arrows) F Corresponding ADC map G T1-weighted axial spin-echo image (600202) obtained at 6 weeks of life shows hyperintensity within the posterior putamen and ventrolateral thalamus bilaterally (arrows)
The neonatal mean diffusion-weighted image (mDWI) shows an ischemic area in the middle cerebral artery territory which resulted in a cyst observed at 3 and 24 mo The neonatal Z map shows normal Z values in all regions At 3 mo low Z values representing abnormal fractional anisotropy (FA) values were observed in the affected corticospinal tract which corresponded with the subsequent development of unilateral motor deficits The Z map at 24 mo was essentially identical Interestingly FA values in the fornix continued to decrease from the time of the neonatal scan to 24 mo suggesting delayed degeneration in this tract
Restricted diffusion signal in the DCST Left middle cerebral artery infarction (A) results in DWI signal changes throughout the DCST PLIC and cerebral peduncle involvement are evident on coronal (B) and sagittal images (C) Signal in the basis pontis and medullary pyramids can be seen on left (D) but not right (E) parasagittal sections
Neonate with left middle cerebral artery stroke and chronic hemiparesis DWI signal is appreciated throughout the DCST including PLIC (A) peduncle (B C) pons (D E) and pontomedullary junction (F)
Axial diffusion weighted images from a neonate (A) with a modified pediatric ASPECTS of eight (involvement of left internal capsule insula M3 M5 M6 P1 P2 and thalamus) and a child (B) with a modified pediatric ASPECTS of 10 (involvement of left caudate lentiform internal capsule insula and middle cerebral artery territories M1ndashM6)
(A) Axial diffusion-weighted image showing hyperintensity in the territory of left middle cerebral artery (B) MR angiography demonstrates loss of flow distal to the left middle cerebral artery bifurcation
A B
Perinatal asphyxia more appropriately known as hypoxic-
ischemic encephalopathy (HIE) is characterized by clinical and laboratory evidence of acute or subacute brain injury due to asphyxia The primary causes of this condition are systemic hypoxemia andor reduced cerebral blood flow (CBF) Birth asphyxia causes 840000 or 23 of all neonatal deaths worldwideHIE- Acute brain injury that occur before during or after birth
Signs and symptomsMild hypoxic-ischemic encephalopathybullMuscle tone may be slightly increased and deep tendon reflexes may be brisk during the first few daysbullTransient behavioral abnormalities such as poor feeding irritability or excessive crying or sleepiness (typically in an alternating pattern) may be observed bullTypically resolves in 24h
Moderately severe hypoxic-ischemic encephalopathyThe infant is lethargic with significant hypotonia and diminished deep tendon reflexesThe grasping Moro and sucking reflexes may be sluggish or absentThe infant may experience occasional periods of apneaSeizures typically occur early within the first 24 hours after birthFull recovery within 1-2 weeks is possible and is associated with a better long-term outcome
Severe hypoxic-ischemic encephalopathySeizures can be delayed and severe and may be initially resistant to conventional treatments The seizures are usually generalized and their frequency may increase during the 24-48 hours after onset correlating with the phase of reperfusion injury As the injury progresses seizures subside and the electroencephalogram becomes isoelectric or shows a burst suppression pattern At that time wakefulness may deteriorate further and the fontanelle may bulge suggesting increasing cerebral edema
Other symptoms include the following Stupor or coma is typical the infant may not respond to any physical stimulus except the most noxiousBreathing may be irregular and the infant often requires ventilatory support Generalized hypotonia and depressed deep tendon reflexes are common Neonatal reflexes (eg sucking swallowing grasping Moro) are absent Disturbances of ocular motion such as a skewed deviation of the eyes nystagmus bobbing and loss of dolls eye (ie conjugate) movements may be revealed by cranial nerve examination Pupils may be dilated fixed or poorly reactive to lightIrregularities of heart rate and blood pressure are common during the period of reperfusion injury as is death from cardiorespiratory failure An initial period of well-being or mild hypoxic-ischemic encephalopathy may be followed by sudden deterioration suggesting ongoing brain cell dysfunction injury and death during this period seizure intensity may increase
Imaging of neonatal hypoxic-ischemic encephalopathy
Ultrasonography is the first-line imaging technique for the evaluation of the newborn brain These past few years have seen an increasing role of MRI in the investigation of HIE because of greater sensitivity and specificity Electro-encephalogram(EEG)Computed Tomography(CT)MRI MRS and DWI
MRI sequencesT1 WI T2 WI++ FLAIR are not very useful to detect lesion in young infant less than 24 months due to brain maturation IR T1-weighted Has been very helpful in the last two decades before generalization of high fields MRI as it gives excellent images of brain anatomy and maturation It also shows accurately the differentiation between myelinated and unmyelinated WM Three-dimensional GE T1 weighted sequence (3DT1) bullallow 1 mm contiguous slices which can be reconstructed in any anatomic plane T2 to detect hemorrhagic lesions DWI It is now recommended that DWI should be performed between 2 days and 8 days of life Multiple studies have shown DWI are more sensitive in the detection of HIE lesions than conventional MRI especially for early diagnosis
MRI ProtocolSagittal and axial T1 WI Axial and coronal T2 WI Axial T2 3D T1 FLAIR (older child) DWI MRSLactate peak bulldue to anaerobic glycolysis bullfound within 24 h of life Subsequently a reduction in N-acetyl aspartate (NAA) is evident due to neuronal loss
Advanced technique Perfusion
Arterial Spin-Labeled (ASL) Perfusion bullRecent advances in novel research imaging modalitybullallows noninvasive evaluation of CBF (cerebral blood flow) using electromagnetically labeled arterial blood water as an endogenous contrast agent bullDemonstrates low CBF in neonates who have suffered HIE and in infants and children after stroke
Imaging RecommendationCranial sonography (US) bullFirst between 7 and 14 days bullRepeat before discharge from the hospital MRI DWI MRS bullWhen US is abnormal MRI precise lesion extension and aide in prognosticating bull Defining injury in VLBW neonates with normal US
PrognosisPoor outcome if bullIVH plus PVL bullPVL with volume loss widespread infarction or seizures bullPVL with enlarged cysts
It is necessary to bullknow the normal cerebral appearance before interpret pathological aspect bulldistinguish hypoxic-ischemic brain damage from normal myelination Brain compositionChanges in brain composition Changes in cellular density increase in complex lipids content due to the evolving process of myelination decrease in water content mostly in the WM
Shortening of T1 Shortening of T2
Imaging PatternThe imaging patterns of HIE can be classified into 3 types Lesions predominantly located in the PVWM Lesions predominantly located in the basal ganglia or thalamus Multicystic encephalomalcia The pattern of injury is postulated to depend on bull The type of hypoxiandashischaemia (acute and profound or prolonged and partial) bullThe gestational age (term or pre-term)
HIE in preterm infantRisk FactorsPregnancy Gestational ageweight previous preterm birth spontaneous preterm labor Intrapartum Abruption pre-eclampsia premature rupture of membranes chorioamnionitis group B Strep Peri amp postnatal factors Respiratory distress sepsis anemia apnea bradycardia cardiac arrest
General Features++ PVL +- associated to Germinal matrix and IVH PV hemorrhagic infarction Cerebellar infarction Definition bullPVL is the HIE driven periventricular white matter (PVWM) necrosis seen in very low birth weight premies (lt1500g) EpidemiologybullBirth weight lt 1500 g 45 incidence of PVL (higher if associated with IVH) bullGestational age lt 33 weeks 38 incidence of PVL bullgt 50 of patients with PVL or grade III IVH develop cerebral palsy
Cranial ultrasound coronal view day 1 showing severe echogenicity in the white matter MRI (T2SE (TR 6284TE 120) and ADC) performed on day 3 showing increased signal intensity in the white matter on T2SE and low signal intensity in the deep white matter on the ADC map with sparing of the anterior periventricular white matter and asymmetrical distribution in the parieto-occipital white matter The child died and was subsequently diagnosed to have molybdenum cofactor deficiency
Cranial sonography in 5-day old term with HIE with increase in echogenicity of white matter consistent with edemaCD ultrasound shows reversal of diastolic flow reflecting increased vascular resistance secondary to edema
PVL in a preterm infant (a) Coronal head US image obtained in the 1st week of life shows increased echogenicity in the periventricular white matter (arrows) (b) Follow-up US image obtained 2 months later shows development of cystic changes in these regions and dilatation of the adjacent lateral ventricles findings that are consistent with PVL
CT images show decrease In basal ganglia density related to Cytotoxic edemaSubtle loss of the normally sharp Transition from grey matter to White matter at the corticomedullary Junction Cerebral edema seen with effacementof the cortical sulci and the sylvian Fissures
PVL in a preterm neonate Axial T1-weighted (a) and T2-weighted (b) MR images obtained on day 4 of life demonstrate T1 hypointensity and T2 hyperintensity in the periventricular whitematter Note the punctate foci of high signal intensity on the T1-weighted image (arrows in a) These foci should be distinguished from foci of hemorrhage whichwould demonstrate greater T2 shortening on the corresponding T2-weighted image
28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

Radiographic features
CTdiffuse edema with effacement of the CSF-containing spacesdecreased cortical gray matter attenuation with loss of normal gray-white differentiationdecreased bilateral basal ganglia attenuationreversal sign reversal of the normal CT attenuation of grey and white matter demonstrated within the first 24 hours in a small number of these patients
it has been proposed that this finding is due to the distention of deep medullary veins secondary to partial obstruction of venous outflow from the elevated intracranial pressure caused by diffuse edemathe end result is that the cerebral white matter is of higher attenuation than the cortical gray matter
white cerebellum sign has been described in at least one study as a component of the reversal sign and in which there is diffuse edema and hypoattenuation of the cerebral hemispheres with sparing of the cerebellum and brainstem resulting in apparent high attenuation of the cerebellum and brainstem relative to the cerebral hemisphereslinear hyperdensity outlining the cortex as well as linear cortical enhancement (later and less evident signs) correspond to cortical laminar necrosis
MRIDiffusion-weighted MR imaging is the earliest imaging modality to become positive usually within the first few hours after a hypoxic-ischemic event due to early cytotoxic edema During the first 24 hours there may be restricted diffusion in the cerebellar hemispheres basal ganglia or cerebral cortex (in particular the perirolandic and occipital cortices) The thalami brainstem or hippocampi may also be involved Diffusion-weighted imaging abnormalities usually pseudo-normalize by the end of the 1st week As in younger patients conventional T1 and T2 weighted images are often normal or demonstrate only very subtle abnormalities In the early subacute period (24 hoursndash2 weeks) conventional T2 weighted images typically become positive and demonstrate increased signal intensity and swelling of the injured gray matter structures T1 hyperintensities signaling cortical laminar necrosis become evident after two weeks This hyperintense signal does not represent hemorrhage its believed to be caused by the accumulation of denatured proteins in dying cells This hyperintensity can be seen also within a few days on FLAIR
Acute Ischemic Stroke NECT and Axial DWI-diffusion
CT of a 7 day old with history of perinatal asphyxia shows diffuse low attenuating supratentorial brain parenchyma with relatively hyperdense Cerebellum - CT Reversal sign of Global hypoxia
CT scan show bilateral hypodensity involving the basal ganglia and the thalami Axial T1WI show hyperintensity of the basal gangliaAxial T2WI shows corresponding hypointensity DWI reveals hyperintensity at the basal ganglia hippocampi and occipital lobes consistent with restricted diffusion of acute ischemic injury
CT without and with iv contrast Axial T2 with bilateral thalamic infarct
Global hypoxic-ischemic brain injury
Hypoxic-ischemic brain injury
Images show the temporal evolution of a right-sided main branch MCA territory infarction (patient 1) on T1-weighted images (top row) and T2-weighted images (bottom row) obtained on days 2 5 12 42 and 75 post-delivery
Graph shows DWIs of a patient with an infarction within the PCA territory showing severe HSI on day 3 (A) and mild-to-moderate HSI on day 10 (B)
MRI Diffusion show bilateral fronto parietal and parieto occipital cortical restricted diffusion Similar restricted diffusion in caudate nuclei Area of involvement corresponds to cortical as well as internal border zone infarcts Imaging wise Bilateral border infarcts
A Axial T2-weighted fast spin-echo image (3200851) with an echo train length of 8 obtained at 13 hours of life shows no abnormality B Trace LSDI image (15206251) with a b max of 750 secondsmm2 obtained at 13 hours of life shows no abnormality C Corresponding ADC map D Axial T2-weighted fast spin-echo image obtained at 5 days of life shows very subtle hyperintensity in the posterior putamen bilaterally (arrows) E Trace LSDI image obtained at 5 days of life shows decreased diffusion in corresponding areas (arrows) F Corresponding ADC map G T1-weighted axial spin-echo image (600202) obtained at 6 weeks of life shows hyperintensity within the posterior putamen and ventrolateral thalamus bilaterally (arrows)
The neonatal mean diffusion-weighted image (mDWI) shows an ischemic area in the middle cerebral artery territory which resulted in a cyst observed at 3 and 24 mo The neonatal Z map shows normal Z values in all regions At 3 mo low Z values representing abnormal fractional anisotropy (FA) values were observed in the affected corticospinal tract which corresponded with the subsequent development of unilateral motor deficits The Z map at 24 mo was essentially identical Interestingly FA values in the fornix continued to decrease from the time of the neonatal scan to 24 mo suggesting delayed degeneration in this tract
Restricted diffusion signal in the DCST Left middle cerebral artery infarction (A) results in DWI signal changes throughout the DCST PLIC and cerebral peduncle involvement are evident on coronal (B) and sagittal images (C) Signal in the basis pontis and medullary pyramids can be seen on left (D) but not right (E) parasagittal sections
Neonate with left middle cerebral artery stroke and chronic hemiparesis DWI signal is appreciated throughout the DCST including PLIC (A) peduncle (B C) pons (D E) and pontomedullary junction (F)
Axial diffusion weighted images from a neonate (A) with a modified pediatric ASPECTS of eight (involvement of left internal capsule insula M3 M5 M6 P1 P2 and thalamus) and a child (B) with a modified pediatric ASPECTS of 10 (involvement of left caudate lentiform internal capsule insula and middle cerebral artery territories M1ndashM6)
(A) Axial diffusion-weighted image showing hyperintensity in the territory of left middle cerebral artery (B) MR angiography demonstrates loss of flow distal to the left middle cerebral artery bifurcation
A B
Perinatal asphyxia more appropriately known as hypoxic-
ischemic encephalopathy (HIE) is characterized by clinical and laboratory evidence of acute or subacute brain injury due to asphyxia The primary causes of this condition are systemic hypoxemia andor reduced cerebral blood flow (CBF) Birth asphyxia causes 840000 or 23 of all neonatal deaths worldwideHIE- Acute brain injury that occur before during or after birth
Signs and symptomsMild hypoxic-ischemic encephalopathybullMuscle tone may be slightly increased and deep tendon reflexes may be brisk during the first few daysbullTransient behavioral abnormalities such as poor feeding irritability or excessive crying or sleepiness (typically in an alternating pattern) may be observed bullTypically resolves in 24h
Moderately severe hypoxic-ischemic encephalopathyThe infant is lethargic with significant hypotonia and diminished deep tendon reflexesThe grasping Moro and sucking reflexes may be sluggish or absentThe infant may experience occasional periods of apneaSeizures typically occur early within the first 24 hours after birthFull recovery within 1-2 weeks is possible and is associated with a better long-term outcome
Severe hypoxic-ischemic encephalopathySeizures can be delayed and severe and may be initially resistant to conventional treatments The seizures are usually generalized and their frequency may increase during the 24-48 hours after onset correlating with the phase of reperfusion injury As the injury progresses seizures subside and the electroencephalogram becomes isoelectric or shows a burst suppression pattern At that time wakefulness may deteriorate further and the fontanelle may bulge suggesting increasing cerebral edema
Other symptoms include the following Stupor or coma is typical the infant may not respond to any physical stimulus except the most noxiousBreathing may be irregular and the infant often requires ventilatory support Generalized hypotonia and depressed deep tendon reflexes are common Neonatal reflexes (eg sucking swallowing grasping Moro) are absent Disturbances of ocular motion such as a skewed deviation of the eyes nystagmus bobbing and loss of dolls eye (ie conjugate) movements may be revealed by cranial nerve examination Pupils may be dilated fixed or poorly reactive to lightIrregularities of heart rate and blood pressure are common during the period of reperfusion injury as is death from cardiorespiratory failure An initial period of well-being or mild hypoxic-ischemic encephalopathy may be followed by sudden deterioration suggesting ongoing brain cell dysfunction injury and death during this period seizure intensity may increase
Imaging of neonatal hypoxic-ischemic encephalopathy
Ultrasonography is the first-line imaging technique for the evaluation of the newborn brain These past few years have seen an increasing role of MRI in the investigation of HIE because of greater sensitivity and specificity Electro-encephalogram(EEG)Computed Tomography(CT)MRI MRS and DWI
MRI sequencesT1 WI T2 WI++ FLAIR are not very useful to detect lesion in young infant less than 24 months due to brain maturation IR T1-weighted Has been very helpful in the last two decades before generalization of high fields MRI as it gives excellent images of brain anatomy and maturation It also shows accurately the differentiation between myelinated and unmyelinated WM Three-dimensional GE T1 weighted sequence (3DT1) bullallow 1 mm contiguous slices which can be reconstructed in any anatomic plane T2 to detect hemorrhagic lesions DWI It is now recommended that DWI should be performed between 2 days and 8 days of life Multiple studies have shown DWI are more sensitive in the detection of HIE lesions than conventional MRI especially for early diagnosis
MRI ProtocolSagittal and axial T1 WI Axial and coronal T2 WI Axial T2 3D T1 FLAIR (older child) DWI MRSLactate peak bulldue to anaerobic glycolysis bullfound within 24 h of life Subsequently a reduction in N-acetyl aspartate (NAA) is evident due to neuronal loss
Advanced technique Perfusion
Arterial Spin-Labeled (ASL) Perfusion bullRecent advances in novel research imaging modalitybullallows noninvasive evaluation of CBF (cerebral blood flow) using electromagnetically labeled arterial blood water as an endogenous contrast agent bullDemonstrates low CBF in neonates who have suffered HIE and in infants and children after stroke
Imaging RecommendationCranial sonography (US) bullFirst between 7 and 14 days bullRepeat before discharge from the hospital MRI DWI MRS bullWhen US is abnormal MRI precise lesion extension and aide in prognosticating bull Defining injury in VLBW neonates with normal US
PrognosisPoor outcome if bullIVH plus PVL bullPVL with volume loss widespread infarction or seizures bullPVL with enlarged cysts
It is necessary to bullknow the normal cerebral appearance before interpret pathological aspect bulldistinguish hypoxic-ischemic brain damage from normal myelination Brain compositionChanges in brain composition Changes in cellular density increase in complex lipids content due to the evolving process of myelination decrease in water content mostly in the WM
Shortening of T1 Shortening of T2
Imaging PatternThe imaging patterns of HIE can be classified into 3 types Lesions predominantly located in the PVWM Lesions predominantly located in the basal ganglia or thalamus Multicystic encephalomalcia The pattern of injury is postulated to depend on bull The type of hypoxiandashischaemia (acute and profound or prolonged and partial) bullThe gestational age (term or pre-term)
HIE in preterm infantRisk FactorsPregnancy Gestational ageweight previous preterm birth spontaneous preterm labor Intrapartum Abruption pre-eclampsia premature rupture of membranes chorioamnionitis group B Strep Peri amp postnatal factors Respiratory distress sepsis anemia apnea bradycardia cardiac arrest
General Features++ PVL +- associated to Germinal matrix and IVH PV hemorrhagic infarction Cerebellar infarction Definition bullPVL is the HIE driven periventricular white matter (PVWM) necrosis seen in very low birth weight premies (lt1500g) EpidemiologybullBirth weight lt 1500 g 45 incidence of PVL (higher if associated with IVH) bullGestational age lt 33 weeks 38 incidence of PVL bullgt 50 of patients with PVL or grade III IVH develop cerebral palsy
Cranial ultrasound coronal view day 1 showing severe echogenicity in the white matter MRI (T2SE (TR 6284TE 120) and ADC) performed on day 3 showing increased signal intensity in the white matter on T2SE and low signal intensity in the deep white matter on the ADC map with sparing of the anterior periventricular white matter and asymmetrical distribution in the parieto-occipital white matter The child died and was subsequently diagnosed to have molybdenum cofactor deficiency
Cranial sonography in 5-day old term with HIE with increase in echogenicity of white matter consistent with edemaCD ultrasound shows reversal of diastolic flow reflecting increased vascular resistance secondary to edema
PVL in a preterm infant (a) Coronal head US image obtained in the 1st week of life shows increased echogenicity in the periventricular white matter (arrows) (b) Follow-up US image obtained 2 months later shows development of cystic changes in these regions and dilatation of the adjacent lateral ventricles findings that are consistent with PVL
CT images show decrease In basal ganglia density related to Cytotoxic edemaSubtle loss of the normally sharp Transition from grey matter to White matter at the corticomedullary Junction Cerebral edema seen with effacementof the cortical sulci and the sylvian Fissures
PVL in a preterm neonate Axial T1-weighted (a) and T2-weighted (b) MR images obtained on day 4 of life demonstrate T1 hypointensity and T2 hyperintensity in the periventricular whitematter Note the punctate foci of high signal intensity on the T1-weighted image (arrows in a) These foci should be distinguished from foci of hemorrhage whichwould demonstrate greater T2 shortening on the corresponding T2-weighted image
28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

MRIDiffusion-weighted MR imaging is the earliest imaging modality to become positive usually within the first few hours after a hypoxic-ischemic event due to early cytotoxic edema During the first 24 hours there may be restricted diffusion in the cerebellar hemispheres basal ganglia or cerebral cortex (in particular the perirolandic and occipital cortices) The thalami brainstem or hippocampi may also be involved Diffusion-weighted imaging abnormalities usually pseudo-normalize by the end of the 1st week As in younger patients conventional T1 and T2 weighted images are often normal or demonstrate only very subtle abnormalities In the early subacute period (24 hoursndash2 weeks) conventional T2 weighted images typically become positive and demonstrate increased signal intensity and swelling of the injured gray matter structures T1 hyperintensities signaling cortical laminar necrosis become evident after two weeks This hyperintense signal does not represent hemorrhage its believed to be caused by the accumulation of denatured proteins in dying cells This hyperintensity can be seen also within a few days on FLAIR
Acute Ischemic Stroke NECT and Axial DWI-diffusion
CT of a 7 day old with history of perinatal asphyxia shows diffuse low attenuating supratentorial brain parenchyma with relatively hyperdense Cerebellum - CT Reversal sign of Global hypoxia
CT scan show bilateral hypodensity involving the basal ganglia and the thalami Axial T1WI show hyperintensity of the basal gangliaAxial T2WI shows corresponding hypointensity DWI reveals hyperintensity at the basal ganglia hippocampi and occipital lobes consistent with restricted diffusion of acute ischemic injury
CT without and with iv contrast Axial T2 with bilateral thalamic infarct
Global hypoxic-ischemic brain injury
Hypoxic-ischemic brain injury
Images show the temporal evolution of a right-sided main branch MCA territory infarction (patient 1) on T1-weighted images (top row) and T2-weighted images (bottom row) obtained on days 2 5 12 42 and 75 post-delivery
Graph shows DWIs of a patient with an infarction within the PCA territory showing severe HSI on day 3 (A) and mild-to-moderate HSI on day 10 (B)
MRI Diffusion show bilateral fronto parietal and parieto occipital cortical restricted diffusion Similar restricted diffusion in caudate nuclei Area of involvement corresponds to cortical as well as internal border zone infarcts Imaging wise Bilateral border infarcts
A Axial T2-weighted fast spin-echo image (3200851) with an echo train length of 8 obtained at 13 hours of life shows no abnormality B Trace LSDI image (15206251) with a b max of 750 secondsmm2 obtained at 13 hours of life shows no abnormality C Corresponding ADC map D Axial T2-weighted fast spin-echo image obtained at 5 days of life shows very subtle hyperintensity in the posterior putamen bilaterally (arrows) E Trace LSDI image obtained at 5 days of life shows decreased diffusion in corresponding areas (arrows) F Corresponding ADC map G T1-weighted axial spin-echo image (600202) obtained at 6 weeks of life shows hyperintensity within the posterior putamen and ventrolateral thalamus bilaterally (arrows)
The neonatal mean diffusion-weighted image (mDWI) shows an ischemic area in the middle cerebral artery territory which resulted in a cyst observed at 3 and 24 mo The neonatal Z map shows normal Z values in all regions At 3 mo low Z values representing abnormal fractional anisotropy (FA) values were observed in the affected corticospinal tract which corresponded with the subsequent development of unilateral motor deficits The Z map at 24 mo was essentially identical Interestingly FA values in the fornix continued to decrease from the time of the neonatal scan to 24 mo suggesting delayed degeneration in this tract
Restricted diffusion signal in the DCST Left middle cerebral artery infarction (A) results in DWI signal changes throughout the DCST PLIC and cerebral peduncle involvement are evident on coronal (B) and sagittal images (C) Signal in the basis pontis and medullary pyramids can be seen on left (D) but not right (E) parasagittal sections
Neonate with left middle cerebral artery stroke and chronic hemiparesis DWI signal is appreciated throughout the DCST including PLIC (A) peduncle (B C) pons (D E) and pontomedullary junction (F)
Axial diffusion weighted images from a neonate (A) with a modified pediatric ASPECTS of eight (involvement of left internal capsule insula M3 M5 M6 P1 P2 and thalamus) and a child (B) with a modified pediatric ASPECTS of 10 (involvement of left caudate lentiform internal capsule insula and middle cerebral artery territories M1ndashM6)
(A) Axial diffusion-weighted image showing hyperintensity in the territory of left middle cerebral artery (B) MR angiography demonstrates loss of flow distal to the left middle cerebral artery bifurcation
A B
Perinatal asphyxia more appropriately known as hypoxic-
ischemic encephalopathy (HIE) is characterized by clinical and laboratory evidence of acute or subacute brain injury due to asphyxia The primary causes of this condition are systemic hypoxemia andor reduced cerebral blood flow (CBF) Birth asphyxia causes 840000 or 23 of all neonatal deaths worldwideHIE- Acute brain injury that occur before during or after birth
Signs and symptomsMild hypoxic-ischemic encephalopathybullMuscle tone may be slightly increased and deep tendon reflexes may be brisk during the first few daysbullTransient behavioral abnormalities such as poor feeding irritability or excessive crying or sleepiness (typically in an alternating pattern) may be observed bullTypically resolves in 24h
Moderately severe hypoxic-ischemic encephalopathyThe infant is lethargic with significant hypotonia and diminished deep tendon reflexesThe grasping Moro and sucking reflexes may be sluggish or absentThe infant may experience occasional periods of apneaSeizures typically occur early within the first 24 hours after birthFull recovery within 1-2 weeks is possible and is associated with a better long-term outcome
Severe hypoxic-ischemic encephalopathySeizures can be delayed and severe and may be initially resistant to conventional treatments The seizures are usually generalized and their frequency may increase during the 24-48 hours after onset correlating with the phase of reperfusion injury As the injury progresses seizures subside and the electroencephalogram becomes isoelectric or shows a burst suppression pattern At that time wakefulness may deteriorate further and the fontanelle may bulge suggesting increasing cerebral edema
Other symptoms include the following Stupor or coma is typical the infant may not respond to any physical stimulus except the most noxiousBreathing may be irregular and the infant often requires ventilatory support Generalized hypotonia and depressed deep tendon reflexes are common Neonatal reflexes (eg sucking swallowing grasping Moro) are absent Disturbances of ocular motion such as a skewed deviation of the eyes nystagmus bobbing and loss of dolls eye (ie conjugate) movements may be revealed by cranial nerve examination Pupils may be dilated fixed or poorly reactive to lightIrregularities of heart rate and blood pressure are common during the period of reperfusion injury as is death from cardiorespiratory failure An initial period of well-being or mild hypoxic-ischemic encephalopathy may be followed by sudden deterioration suggesting ongoing brain cell dysfunction injury and death during this period seizure intensity may increase
Imaging of neonatal hypoxic-ischemic encephalopathy
Ultrasonography is the first-line imaging technique for the evaluation of the newborn brain These past few years have seen an increasing role of MRI in the investigation of HIE because of greater sensitivity and specificity Electro-encephalogram(EEG)Computed Tomography(CT)MRI MRS and DWI
MRI sequencesT1 WI T2 WI++ FLAIR are not very useful to detect lesion in young infant less than 24 months due to brain maturation IR T1-weighted Has been very helpful in the last two decades before generalization of high fields MRI as it gives excellent images of brain anatomy and maturation It also shows accurately the differentiation between myelinated and unmyelinated WM Three-dimensional GE T1 weighted sequence (3DT1) bullallow 1 mm contiguous slices which can be reconstructed in any anatomic plane T2 to detect hemorrhagic lesions DWI It is now recommended that DWI should be performed between 2 days and 8 days of life Multiple studies have shown DWI are more sensitive in the detection of HIE lesions than conventional MRI especially for early diagnosis
MRI ProtocolSagittal and axial T1 WI Axial and coronal T2 WI Axial T2 3D T1 FLAIR (older child) DWI MRSLactate peak bulldue to anaerobic glycolysis bullfound within 24 h of life Subsequently a reduction in N-acetyl aspartate (NAA) is evident due to neuronal loss
Advanced technique Perfusion
Arterial Spin-Labeled (ASL) Perfusion bullRecent advances in novel research imaging modalitybullallows noninvasive evaluation of CBF (cerebral blood flow) using electromagnetically labeled arterial blood water as an endogenous contrast agent bullDemonstrates low CBF in neonates who have suffered HIE and in infants and children after stroke
Imaging RecommendationCranial sonography (US) bullFirst between 7 and 14 days bullRepeat before discharge from the hospital MRI DWI MRS bullWhen US is abnormal MRI precise lesion extension and aide in prognosticating bull Defining injury in VLBW neonates with normal US
PrognosisPoor outcome if bullIVH plus PVL bullPVL with volume loss widespread infarction or seizures bullPVL with enlarged cysts
It is necessary to bullknow the normal cerebral appearance before interpret pathological aspect bulldistinguish hypoxic-ischemic brain damage from normal myelination Brain compositionChanges in brain composition Changes in cellular density increase in complex lipids content due to the evolving process of myelination decrease in water content mostly in the WM
Shortening of T1 Shortening of T2
Imaging PatternThe imaging patterns of HIE can be classified into 3 types Lesions predominantly located in the PVWM Lesions predominantly located in the basal ganglia or thalamus Multicystic encephalomalcia The pattern of injury is postulated to depend on bull The type of hypoxiandashischaemia (acute and profound or prolonged and partial) bullThe gestational age (term or pre-term)
HIE in preterm infantRisk FactorsPregnancy Gestational ageweight previous preterm birth spontaneous preterm labor Intrapartum Abruption pre-eclampsia premature rupture of membranes chorioamnionitis group B Strep Peri amp postnatal factors Respiratory distress sepsis anemia apnea bradycardia cardiac arrest
General Features++ PVL +- associated to Germinal matrix and IVH PV hemorrhagic infarction Cerebellar infarction Definition bullPVL is the HIE driven periventricular white matter (PVWM) necrosis seen in very low birth weight premies (lt1500g) EpidemiologybullBirth weight lt 1500 g 45 incidence of PVL (higher if associated with IVH) bullGestational age lt 33 weeks 38 incidence of PVL bullgt 50 of patients with PVL or grade III IVH develop cerebral palsy
Cranial ultrasound coronal view day 1 showing severe echogenicity in the white matter MRI (T2SE (TR 6284TE 120) and ADC) performed on day 3 showing increased signal intensity in the white matter on T2SE and low signal intensity in the deep white matter on the ADC map with sparing of the anterior periventricular white matter and asymmetrical distribution in the parieto-occipital white matter The child died and was subsequently diagnosed to have molybdenum cofactor deficiency
Cranial sonography in 5-day old term with HIE with increase in echogenicity of white matter consistent with edemaCD ultrasound shows reversal of diastolic flow reflecting increased vascular resistance secondary to edema
PVL in a preterm infant (a) Coronal head US image obtained in the 1st week of life shows increased echogenicity in the periventricular white matter (arrows) (b) Follow-up US image obtained 2 months later shows development of cystic changes in these regions and dilatation of the adjacent lateral ventricles findings that are consistent with PVL
CT images show decrease In basal ganglia density related to Cytotoxic edemaSubtle loss of the normally sharp Transition from grey matter to White matter at the corticomedullary Junction Cerebral edema seen with effacementof the cortical sulci and the sylvian Fissures
PVL in a preterm neonate Axial T1-weighted (a) and T2-weighted (b) MR images obtained on day 4 of life demonstrate T1 hypointensity and T2 hyperintensity in the periventricular whitematter Note the punctate foci of high signal intensity on the T1-weighted image (arrows in a) These foci should be distinguished from foci of hemorrhage whichwould demonstrate greater T2 shortening on the corresponding T2-weighted image
28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

Acute Ischemic Stroke NECT and Axial DWI-diffusion
CT of a 7 day old with history of perinatal asphyxia shows diffuse low attenuating supratentorial brain parenchyma with relatively hyperdense Cerebellum - CT Reversal sign of Global hypoxia
CT scan show bilateral hypodensity involving the basal ganglia and the thalami Axial T1WI show hyperintensity of the basal gangliaAxial T2WI shows corresponding hypointensity DWI reveals hyperintensity at the basal ganglia hippocampi and occipital lobes consistent with restricted diffusion of acute ischemic injury
CT without and with iv contrast Axial T2 with bilateral thalamic infarct
Global hypoxic-ischemic brain injury
Hypoxic-ischemic brain injury
Images show the temporal evolution of a right-sided main branch MCA territory infarction (patient 1) on T1-weighted images (top row) and T2-weighted images (bottom row) obtained on days 2 5 12 42 and 75 post-delivery
Graph shows DWIs of a patient with an infarction within the PCA territory showing severe HSI on day 3 (A) and mild-to-moderate HSI on day 10 (B)
MRI Diffusion show bilateral fronto parietal and parieto occipital cortical restricted diffusion Similar restricted diffusion in caudate nuclei Area of involvement corresponds to cortical as well as internal border zone infarcts Imaging wise Bilateral border infarcts
A Axial T2-weighted fast spin-echo image (3200851) with an echo train length of 8 obtained at 13 hours of life shows no abnormality B Trace LSDI image (15206251) with a b max of 750 secondsmm2 obtained at 13 hours of life shows no abnormality C Corresponding ADC map D Axial T2-weighted fast spin-echo image obtained at 5 days of life shows very subtle hyperintensity in the posterior putamen bilaterally (arrows) E Trace LSDI image obtained at 5 days of life shows decreased diffusion in corresponding areas (arrows) F Corresponding ADC map G T1-weighted axial spin-echo image (600202) obtained at 6 weeks of life shows hyperintensity within the posterior putamen and ventrolateral thalamus bilaterally (arrows)
The neonatal mean diffusion-weighted image (mDWI) shows an ischemic area in the middle cerebral artery territory which resulted in a cyst observed at 3 and 24 mo The neonatal Z map shows normal Z values in all regions At 3 mo low Z values representing abnormal fractional anisotropy (FA) values were observed in the affected corticospinal tract which corresponded with the subsequent development of unilateral motor deficits The Z map at 24 mo was essentially identical Interestingly FA values in the fornix continued to decrease from the time of the neonatal scan to 24 mo suggesting delayed degeneration in this tract
Restricted diffusion signal in the DCST Left middle cerebral artery infarction (A) results in DWI signal changes throughout the DCST PLIC and cerebral peduncle involvement are evident on coronal (B) and sagittal images (C) Signal in the basis pontis and medullary pyramids can be seen on left (D) but not right (E) parasagittal sections
Neonate with left middle cerebral artery stroke and chronic hemiparesis DWI signal is appreciated throughout the DCST including PLIC (A) peduncle (B C) pons (D E) and pontomedullary junction (F)
Axial diffusion weighted images from a neonate (A) with a modified pediatric ASPECTS of eight (involvement of left internal capsule insula M3 M5 M6 P1 P2 and thalamus) and a child (B) with a modified pediatric ASPECTS of 10 (involvement of left caudate lentiform internal capsule insula and middle cerebral artery territories M1ndashM6)
(A) Axial diffusion-weighted image showing hyperintensity in the territory of left middle cerebral artery (B) MR angiography demonstrates loss of flow distal to the left middle cerebral artery bifurcation
A B
Perinatal asphyxia more appropriately known as hypoxic-
ischemic encephalopathy (HIE) is characterized by clinical and laboratory evidence of acute or subacute brain injury due to asphyxia The primary causes of this condition are systemic hypoxemia andor reduced cerebral blood flow (CBF) Birth asphyxia causes 840000 or 23 of all neonatal deaths worldwideHIE- Acute brain injury that occur before during or after birth
Signs and symptomsMild hypoxic-ischemic encephalopathybullMuscle tone may be slightly increased and deep tendon reflexes may be brisk during the first few daysbullTransient behavioral abnormalities such as poor feeding irritability or excessive crying or sleepiness (typically in an alternating pattern) may be observed bullTypically resolves in 24h
Moderately severe hypoxic-ischemic encephalopathyThe infant is lethargic with significant hypotonia and diminished deep tendon reflexesThe grasping Moro and sucking reflexes may be sluggish or absentThe infant may experience occasional periods of apneaSeizures typically occur early within the first 24 hours after birthFull recovery within 1-2 weeks is possible and is associated with a better long-term outcome
Severe hypoxic-ischemic encephalopathySeizures can be delayed and severe and may be initially resistant to conventional treatments The seizures are usually generalized and their frequency may increase during the 24-48 hours after onset correlating with the phase of reperfusion injury As the injury progresses seizures subside and the electroencephalogram becomes isoelectric or shows a burst suppression pattern At that time wakefulness may deteriorate further and the fontanelle may bulge suggesting increasing cerebral edema
Other symptoms include the following Stupor or coma is typical the infant may not respond to any physical stimulus except the most noxiousBreathing may be irregular and the infant often requires ventilatory support Generalized hypotonia and depressed deep tendon reflexes are common Neonatal reflexes (eg sucking swallowing grasping Moro) are absent Disturbances of ocular motion such as a skewed deviation of the eyes nystagmus bobbing and loss of dolls eye (ie conjugate) movements may be revealed by cranial nerve examination Pupils may be dilated fixed or poorly reactive to lightIrregularities of heart rate and blood pressure are common during the period of reperfusion injury as is death from cardiorespiratory failure An initial period of well-being or mild hypoxic-ischemic encephalopathy may be followed by sudden deterioration suggesting ongoing brain cell dysfunction injury and death during this period seizure intensity may increase
Imaging of neonatal hypoxic-ischemic encephalopathy
Ultrasonography is the first-line imaging technique for the evaluation of the newborn brain These past few years have seen an increasing role of MRI in the investigation of HIE because of greater sensitivity and specificity Electro-encephalogram(EEG)Computed Tomography(CT)MRI MRS and DWI
MRI sequencesT1 WI T2 WI++ FLAIR are not very useful to detect lesion in young infant less than 24 months due to brain maturation IR T1-weighted Has been very helpful in the last two decades before generalization of high fields MRI as it gives excellent images of brain anatomy and maturation It also shows accurately the differentiation between myelinated and unmyelinated WM Three-dimensional GE T1 weighted sequence (3DT1) bullallow 1 mm contiguous slices which can be reconstructed in any anatomic plane T2 to detect hemorrhagic lesions DWI It is now recommended that DWI should be performed between 2 days and 8 days of life Multiple studies have shown DWI are more sensitive in the detection of HIE lesions than conventional MRI especially for early diagnosis
MRI ProtocolSagittal and axial T1 WI Axial and coronal T2 WI Axial T2 3D T1 FLAIR (older child) DWI MRSLactate peak bulldue to anaerobic glycolysis bullfound within 24 h of life Subsequently a reduction in N-acetyl aspartate (NAA) is evident due to neuronal loss
Advanced technique Perfusion
Arterial Spin-Labeled (ASL) Perfusion bullRecent advances in novel research imaging modalitybullallows noninvasive evaluation of CBF (cerebral blood flow) using electromagnetically labeled arterial blood water as an endogenous contrast agent bullDemonstrates low CBF in neonates who have suffered HIE and in infants and children after stroke
Imaging RecommendationCranial sonography (US) bullFirst between 7 and 14 days bullRepeat before discharge from the hospital MRI DWI MRS bullWhen US is abnormal MRI precise lesion extension and aide in prognosticating bull Defining injury in VLBW neonates with normal US
PrognosisPoor outcome if bullIVH plus PVL bullPVL with volume loss widespread infarction or seizures bullPVL with enlarged cysts
It is necessary to bullknow the normal cerebral appearance before interpret pathological aspect bulldistinguish hypoxic-ischemic brain damage from normal myelination Brain compositionChanges in brain composition Changes in cellular density increase in complex lipids content due to the evolving process of myelination decrease in water content mostly in the WM
Shortening of T1 Shortening of T2
Imaging PatternThe imaging patterns of HIE can be classified into 3 types Lesions predominantly located in the PVWM Lesions predominantly located in the basal ganglia or thalamus Multicystic encephalomalcia The pattern of injury is postulated to depend on bull The type of hypoxiandashischaemia (acute and profound or prolonged and partial) bullThe gestational age (term or pre-term)
HIE in preterm infantRisk FactorsPregnancy Gestational ageweight previous preterm birth spontaneous preterm labor Intrapartum Abruption pre-eclampsia premature rupture of membranes chorioamnionitis group B Strep Peri amp postnatal factors Respiratory distress sepsis anemia apnea bradycardia cardiac arrest
General Features++ PVL +- associated to Germinal matrix and IVH PV hemorrhagic infarction Cerebellar infarction Definition bullPVL is the HIE driven periventricular white matter (PVWM) necrosis seen in very low birth weight premies (lt1500g) EpidemiologybullBirth weight lt 1500 g 45 incidence of PVL (higher if associated with IVH) bullGestational age lt 33 weeks 38 incidence of PVL bullgt 50 of patients with PVL or grade III IVH develop cerebral palsy
Cranial ultrasound coronal view day 1 showing severe echogenicity in the white matter MRI (T2SE (TR 6284TE 120) and ADC) performed on day 3 showing increased signal intensity in the white matter on T2SE and low signal intensity in the deep white matter on the ADC map with sparing of the anterior periventricular white matter and asymmetrical distribution in the parieto-occipital white matter The child died and was subsequently diagnosed to have molybdenum cofactor deficiency
Cranial sonography in 5-day old term with HIE with increase in echogenicity of white matter consistent with edemaCD ultrasound shows reversal of diastolic flow reflecting increased vascular resistance secondary to edema
PVL in a preterm infant (a) Coronal head US image obtained in the 1st week of life shows increased echogenicity in the periventricular white matter (arrows) (b) Follow-up US image obtained 2 months later shows development of cystic changes in these regions and dilatation of the adjacent lateral ventricles findings that are consistent with PVL
CT images show decrease In basal ganglia density related to Cytotoxic edemaSubtle loss of the normally sharp Transition from grey matter to White matter at the corticomedullary Junction Cerebral edema seen with effacementof the cortical sulci and the sylvian Fissures
PVL in a preterm neonate Axial T1-weighted (a) and T2-weighted (b) MR images obtained on day 4 of life demonstrate T1 hypointensity and T2 hyperintensity in the periventricular whitematter Note the punctate foci of high signal intensity on the T1-weighted image (arrows in a) These foci should be distinguished from foci of hemorrhage whichwould demonstrate greater T2 shortening on the corresponding T2-weighted image
28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

CT of a 7 day old with history of perinatal asphyxia shows diffuse low attenuating supratentorial brain parenchyma with relatively hyperdense Cerebellum - CT Reversal sign of Global hypoxia
CT scan show bilateral hypodensity involving the basal ganglia and the thalami Axial T1WI show hyperintensity of the basal gangliaAxial T2WI shows corresponding hypointensity DWI reveals hyperintensity at the basal ganglia hippocampi and occipital lobes consistent with restricted diffusion of acute ischemic injury
CT without and with iv contrast Axial T2 with bilateral thalamic infarct
Global hypoxic-ischemic brain injury
Hypoxic-ischemic brain injury
Images show the temporal evolution of a right-sided main branch MCA territory infarction (patient 1) on T1-weighted images (top row) and T2-weighted images (bottom row) obtained on days 2 5 12 42 and 75 post-delivery
Graph shows DWIs of a patient with an infarction within the PCA territory showing severe HSI on day 3 (A) and mild-to-moderate HSI on day 10 (B)
MRI Diffusion show bilateral fronto parietal and parieto occipital cortical restricted diffusion Similar restricted diffusion in caudate nuclei Area of involvement corresponds to cortical as well as internal border zone infarcts Imaging wise Bilateral border infarcts
A Axial T2-weighted fast spin-echo image (3200851) with an echo train length of 8 obtained at 13 hours of life shows no abnormality B Trace LSDI image (15206251) with a b max of 750 secondsmm2 obtained at 13 hours of life shows no abnormality C Corresponding ADC map D Axial T2-weighted fast spin-echo image obtained at 5 days of life shows very subtle hyperintensity in the posterior putamen bilaterally (arrows) E Trace LSDI image obtained at 5 days of life shows decreased diffusion in corresponding areas (arrows) F Corresponding ADC map G T1-weighted axial spin-echo image (600202) obtained at 6 weeks of life shows hyperintensity within the posterior putamen and ventrolateral thalamus bilaterally (arrows)
The neonatal mean diffusion-weighted image (mDWI) shows an ischemic area in the middle cerebral artery territory which resulted in a cyst observed at 3 and 24 mo The neonatal Z map shows normal Z values in all regions At 3 mo low Z values representing abnormal fractional anisotropy (FA) values were observed in the affected corticospinal tract which corresponded with the subsequent development of unilateral motor deficits The Z map at 24 mo was essentially identical Interestingly FA values in the fornix continued to decrease from the time of the neonatal scan to 24 mo suggesting delayed degeneration in this tract
Restricted diffusion signal in the DCST Left middle cerebral artery infarction (A) results in DWI signal changes throughout the DCST PLIC and cerebral peduncle involvement are evident on coronal (B) and sagittal images (C) Signal in the basis pontis and medullary pyramids can be seen on left (D) but not right (E) parasagittal sections
Neonate with left middle cerebral artery stroke and chronic hemiparesis DWI signal is appreciated throughout the DCST including PLIC (A) peduncle (B C) pons (D E) and pontomedullary junction (F)
Axial diffusion weighted images from a neonate (A) with a modified pediatric ASPECTS of eight (involvement of left internal capsule insula M3 M5 M6 P1 P2 and thalamus) and a child (B) with a modified pediatric ASPECTS of 10 (involvement of left caudate lentiform internal capsule insula and middle cerebral artery territories M1ndashM6)
(A) Axial diffusion-weighted image showing hyperintensity in the territory of left middle cerebral artery (B) MR angiography demonstrates loss of flow distal to the left middle cerebral artery bifurcation
A B
Perinatal asphyxia more appropriately known as hypoxic-
ischemic encephalopathy (HIE) is characterized by clinical and laboratory evidence of acute or subacute brain injury due to asphyxia The primary causes of this condition are systemic hypoxemia andor reduced cerebral blood flow (CBF) Birth asphyxia causes 840000 or 23 of all neonatal deaths worldwideHIE- Acute brain injury that occur before during or after birth
Signs and symptomsMild hypoxic-ischemic encephalopathybullMuscle tone may be slightly increased and deep tendon reflexes may be brisk during the first few daysbullTransient behavioral abnormalities such as poor feeding irritability or excessive crying or sleepiness (typically in an alternating pattern) may be observed bullTypically resolves in 24h
Moderately severe hypoxic-ischemic encephalopathyThe infant is lethargic with significant hypotonia and diminished deep tendon reflexesThe grasping Moro and sucking reflexes may be sluggish or absentThe infant may experience occasional periods of apneaSeizures typically occur early within the first 24 hours after birthFull recovery within 1-2 weeks is possible and is associated with a better long-term outcome
Severe hypoxic-ischemic encephalopathySeizures can be delayed and severe and may be initially resistant to conventional treatments The seizures are usually generalized and their frequency may increase during the 24-48 hours after onset correlating with the phase of reperfusion injury As the injury progresses seizures subside and the electroencephalogram becomes isoelectric or shows a burst suppression pattern At that time wakefulness may deteriorate further and the fontanelle may bulge suggesting increasing cerebral edema
Other symptoms include the following Stupor or coma is typical the infant may not respond to any physical stimulus except the most noxiousBreathing may be irregular and the infant often requires ventilatory support Generalized hypotonia and depressed deep tendon reflexes are common Neonatal reflexes (eg sucking swallowing grasping Moro) are absent Disturbances of ocular motion such as a skewed deviation of the eyes nystagmus bobbing and loss of dolls eye (ie conjugate) movements may be revealed by cranial nerve examination Pupils may be dilated fixed or poorly reactive to lightIrregularities of heart rate and blood pressure are common during the period of reperfusion injury as is death from cardiorespiratory failure An initial period of well-being or mild hypoxic-ischemic encephalopathy may be followed by sudden deterioration suggesting ongoing brain cell dysfunction injury and death during this period seizure intensity may increase
Imaging of neonatal hypoxic-ischemic encephalopathy
Ultrasonography is the first-line imaging technique for the evaluation of the newborn brain These past few years have seen an increasing role of MRI in the investigation of HIE because of greater sensitivity and specificity Electro-encephalogram(EEG)Computed Tomography(CT)MRI MRS and DWI
MRI sequencesT1 WI T2 WI++ FLAIR are not very useful to detect lesion in young infant less than 24 months due to brain maturation IR T1-weighted Has been very helpful in the last two decades before generalization of high fields MRI as it gives excellent images of brain anatomy and maturation It also shows accurately the differentiation between myelinated and unmyelinated WM Three-dimensional GE T1 weighted sequence (3DT1) bullallow 1 mm contiguous slices which can be reconstructed in any anatomic plane T2 to detect hemorrhagic lesions DWI It is now recommended that DWI should be performed between 2 days and 8 days of life Multiple studies have shown DWI are more sensitive in the detection of HIE lesions than conventional MRI especially for early diagnosis
MRI ProtocolSagittal and axial T1 WI Axial and coronal T2 WI Axial T2 3D T1 FLAIR (older child) DWI MRSLactate peak bulldue to anaerobic glycolysis bullfound within 24 h of life Subsequently a reduction in N-acetyl aspartate (NAA) is evident due to neuronal loss
Advanced technique Perfusion
Arterial Spin-Labeled (ASL) Perfusion bullRecent advances in novel research imaging modalitybullallows noninvasive evaluation of CBF (cerebral blood flow) using electromagnetically labeled arterial blood water as an endogenous contrast agent bullDemonstrates low CBF in neonates who have suffered HIE and in infants and children after stroke
Imaging RecommendationCranial sonography (US) bullFirst between 7 and 14 days bullRepeat before discharge from the hospital MRI DWI MRS bullWhen US is abnormal MRI precise lesion extension and aide in prognosticating bull Defining injury in VLBW neonates with normal US
PrognosisPoor outcome if bullIVH plus PVL bullPVL with volume loss widespread infarction or seizures bullPVL with enlarged cysts
It is necessary to bullknow the normal cerebral appearance before interpret pathological aspect bulldistinguish hypoxic-ischemic brain damage from normal myelination Brain compositionChanges in brain composition Changes in cellular density increase in complex lipids content due to the evolving process of myelination decrease in water content mostly in the WM
Shortening of T1 Shortening of T2
Imaging PatternThe imaging patterns of HIE can be classified into 3 types Lesions predominantly located in the PVWM Lesions predominantly located in the basal ganglia or thalamus Multicystic encephalomalcia The pattern of injury is postulated to depend on bull The type of hypoxiandashischaemia (acute and profound or prolonged and partial) bullThe gestational age (term or pre-term)
HIE in preterm infantRisk FactorsPregnancy Gestational ageweight previous preterm birth spontaneous preterm labor Intrapartum Abruption pre-eclampsia premature rupture of membranes chorioamnionitis group B Strep Peri amp postnatal factors Respiratory distress sepsis anemia apnea bradycardia cardiac arrest
General Features++ PVL +- associated to Germinal matrix and IVH PV hemorrhagic infarction Cerebellar infarction Definition bullPVL is the HIE driven periventricular white matter (PVWM) necrosis seen in very low birth weight premies (lt1500g) EpidemiologybullBirth weight lt 1500 g 45 incidence of PVL (higher if associated with IVH) bullGestational age lt 33 weeks 38 incidence of PVL bullgt 50 of patients with PVL or grade III IVH develop cerebral palsy
Cranial ultrasound coronal view day 1 showing severe echogenicity in the white matter MRI (T2SE (TR 6284TE 120) and ADC) performed on day 3 showing increased signal intensity in the white matter on T2SE and low signal intensity in the deep white matter on the ADC map with sparing of the anterior periventricular white matter and asymmetrical distribution in the parieto-occipital white matter The child died and was subsequently diagnosed to have molybdenum cofactor deficiency
Cranial sonography in 5-day old term with HIE with increase in echogenicity of white matter consistent with edemaCD ultrasound shows reversal of diastolic flow reflecting increased vascular resistance secondary to edema
PVL in a preterm infant (a) Coronal head US image obtained in the 1st week of life shows increased echogenicity in the periventricular white matter (arrows) (b) Follow-up US image obtained 2 months later shows development of cystic changes in these regions and dilatation of the adjacent lateral ventricles findings that are consistent with PVL
CT images show decrease In basal ganglia density related to Cytotoxic edemaSubtle loss of the normally sharp Transition from grey matter to White matter at the corticomedullary Junction Cerebral edema seen with effacementof the cortical sulci and the sylvian Fissures
PVL in a preterm neonate Axial T1-weighted (a) and T2-weighted (b) MR images obtained on day 4 of life demonstrate T1 hypointensity and T2 hyperintensity in the periventricular whitematter Note the punctate foci of high signal intensity on the T1-weighted image (arrows in a) These foci should be distinguished from foci of hemorrhage whichwould demonstrate greater T2 shortening on the corresponding T2-weighted image
28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

CT scan show bilateral hypodensity involving the basal ganglia and the thalami Axial T1WI show hyperintensity of the basal gangliaAxial T2WI shows corresponding hypointensity DWI reveals hyperintensity at the basal ganglia hippocampi and occipital lobes consistent with restricted diffusion of acute ischemic injury
CT without and with iv contrast Axial T2 with bilateral thalamic infarct
Global hypoxic-ischemic brain injury
Hypoxic-ischemic brain injury
Images show the temporal evolution of a right-sided main branch MCA territory infarction (patient 1) on T1-weighted images (top row) and T2-weighted images (bottom row) obtained on days 2 5 12 42 and 75 post-delivery
Graph shows DWIs of a patient with an infarction within the PCA territory showing severe HSI on day 3 (A) and mild-to-moderate HSI on day 10 (B)
MRI Diffusion show bilateral fronto parietal and parieto occipital cortical restricted diffusion Similar restricted diffusion in caudate nuclei Area of involvement corresponds to cortical as well as internal border zone infarcts Imaging wise Bilateral border infarcts
A Axial T2-weighted fast spin-echo image (3200851) with an echo train length of 8 obtained at 13 hours of life shows no abnormality B Trace LSDI image (15206251) with a b max of 750 secondsmm2 obtained at 13 hours of life shows no abnormality C Corresponding ADC map D Axial T2-weighted fast spin-echo image obtained at 5 days of life shows very subtle hyperintensity in the posterior putamen bilaterally (arrows) E Trace LSDI image obtained at 5 days of life shows decreased diffusion in corresponding areas (arrows) F Corresponding ADC map G T1-weighted axial spin-echo image (600202) obtained at 6 weeks of life shows hyperintensity within the posterior putamen and ventrolateral thalamus bilaterally (arrows)
The neonatal mean diffusion-weighted image (mDWI) shows an ischemic area in the middle cerebral artery territory which resulted in a cyst observed at 3 and 24 mo The neonatal Z map shows normal Z values in all regions At 3 mo low Z values representing abnormal fractional anisotropy (FA) values were observed in the affected corticospinal tract which corresponded with the subsequent development of unilateral motor deficits The Z map at 24 mo was essentially identical Interestingly FA values in the fornix continued to decrease from the time of the neonatal scan to 24 mo suggesting delayed degeneration in this tract
Restricted diffusion signal in the DCST Left middle cerebral artery infarction (A) results in DWI signal changes throughout the DCST PLIC and cerebral peduncle involvement are evident on coronal (B) and sagittal images (C) Signal in the basis pontis and medullary pyramids can be seen on left (D) but not right (E) parasagittal sections
Neonate with left middle cerebral artery stroke and chronic hemiparesis DWI signal is appreciated throughout the DCST including PLIC (A) peduncle (B C) pons (D E) and pontomedullary junction (F)
Axial diffusion weighted images from a neonate (A) with a modified pediatric ASPECTS of eight (involvement of left internal capsule insula M3 M5 M6 P1 P2 and thalamus) and a child (B) with a modified pediatric ASPECTS of 10 (involvement of left caudate lentiform internal capsule insula and middle cerebral artery territories M1ndashM6)
(A) Axial diffusion-weighted image showing hyperintensity in the territory of left middle cerebral artery (B) MR angiography demonstrates loss of flow distal to the left middle cerebral artery bifurcation
A B
Perinatal asphyxia more appropriately known as hypoxic-
ischemic encephalopathy (HIE) is characterized by clinical and laboratory evidence of acute or subacute brain injury due to asphyxia The primary causes of this condition are systemic hypoxemia andor reduced cerebral blood flow (CBF) Birth asphyxia causes 840000 or 23 of all neonatal deaths worldwideHIE- Acute brain injury that occur before during or after birth
Signs and symptomsMild hypoxic-ischemic encephalopathybullMuscle tone may be slightly increased and deep tendon reflexes may be brisk during the first few daysbullTransient behavioral abnormalities such as poor feeding irritability or excessive crying or sleepiness (typically in an alternating pattern) may be observed bullTypically resolves in 24h
Moderately severe hypoxic-ischemic encephalopathyThe infant is lethargic with significant hypotonia and diminished deep tendon reflexesThe grasping Moro and sucking reflexes may be sluggish or absentThe infant may experience occasional periods of apneaSeizures typically occur early within the first 24 hours after birthFull recovery within 1-2 weeks is possible and is associated with a better long-term outcome
Severe hypoxic-ischemic encephalopathySeizures can be delayed and severe and may be initially resistant to conventional treatments The seizures are usually generalized and their frequency may increase during the 24-48 hours after onset correlating with the phase of reperfusion injury As the injury progresses seizures subside and the electroencephalogram becomes isoelectric or shows a burst suppression pattern At that time wakefulness may deteriorate further and the fontanelle may bulge suggesting increasing cerebral edema
Other symptoms include the following Stupor or coma is typical the infant may not respond to any physical stimulus except the most noxiousBreathing may be irregular and the infant often requires ventilatory support Generalized hypotonia and depressed deep tendon reflexes are common Neonatal reflexes (eg sucking swallowing grasping Moro) are absent Disturbances of ocular motion such as a skewed deviation of the eyes nystagmus bobbing and loss of dolls eye (ie conjugate) movements may be revealed by cranial nerve examination Pupils may be dilated fixed or poorly reactive to lightIrregularities of heart rate and blood pressure are common during the period of reperfusion injury as is death from cardiorespiratory failure An initial period of well-being or mild hypoxic-ischemic encephalopathy may be followed by sudden deterioration suggesting ongoing brain cell dysfunction injury and death during this period seizure intensity may increase
Imaging of neonatal hypoxic-ischemic encephalopathy
Ultrasonography is the first-line imaging technique for the evaluation of the newborn brain These past few years have seen an increasing role of MRI in the investigation of HIE because of greater sensitivity and specificity Electro-encephalogram(EEG)Computed Tomography(CT)MRI MRS and DWI
MRI sequencesT1 WI T2 WI++ FLAIR are not very useful to detect lesion in young infant less than 24 months due to brain maturation IR T1-weighted Has been very helpful in the last two decades before generalization of high fields MRI as it gives excellent images of brain anatomy and maturation It also shows accurately the differentiation between myelinated and unmyelinated WM Three-dimensional GE T1 weighted sequence (3DT1) bullallow 1 mm contiguous slices which can be reconstructed in any anatomic plane T2 to detect hemorrhagic lesions DWI It is now recommended that DWI should be performed between 2 days and 8 days of life Multiple studies have shown DWI are more sensitive in the detection of HIE lesions than conventional MRI especially for early diagnosis
MRI ProtocolSagittal and axial T1 WI Axial and coronal T2 WI Axial T2 3D T1 FLAIR (older child) DWI MRSLactate peak bulldue to anaerobic glycolysis bullfound within 24 h of life Subsequently a reduction in N-acetyl aspartate (NAA) is evident due to neuronal loss
Advanced technique Perfusion
Arterial Spin-Labeled (ASL) Perfusion bullRecent advances in novel research imaging modalitybullallows noninvasive evaluation of CBF (cerebral blood flow) using electromagnetically labeled arterial blood water as an endogenous contrast agent bullDemonstrates low CBF in neonates who have suffered HIE and in infants and children after stroke
Imaging RecommendationCranial sonography (US) bullFirst between 7 and 14 days bullRepeat before discharge from the hospital MRI DWI MRS bullWhen US is abnormal MRI precise lesion extension and aide in prognosticating bull Defining injury in VLBW neonates with normal US
PrognosisPoor outcome if bullIVH plus PVL bullPVL with volume loss widespread infarction or seizures bullPVL with enlarged cysts
It is necessary to bullknow the normal cerebral appearance before interpret pathological aspect bulldistinguish hypoxic-ischemic brain damage from normal myelination Brain compositionChanges in brain composition Changes in cellular density increase in complex lipids content due to the evolving process of myelination decrease in water content mostly in the WM
Shortening of T1 Shortening of T2
Imaging PatternThe imaging patterns of HIE can be classified into 3 types Lesions predominantly located in the PVWM Lesions predominantly located in the basal ganglia or thalamus Multicystic encephalomalcia The pattern of injury is postulated to depend on bull The type of hypoxiandashischaemia (acute and profound or prolonged and partial) bullThe gestational age (term or pre-term)
HIE in preterm infantRisk FactorsPregnancy Gestational ageweight previous preterm birth spontaneous preterm labor Intrapartum Abruption pre-eclampsia premature rupture of membranes chorioamnionitis group B Strep Peri amp postnatal factors Respiratory distress sepsis anemia apnea bradycardia cardiac arrest
General Features++ PVL +- associated to Germinal matrix and IVH PV hemorrhagic infarction Cerebellar infarction Definition bullPVL is the HIE driven periventricular white matter (PVWM) necrosis seen in very low birth weight premies (lt1500g) EpidemiologybullBirth weight lt 1500 g 45 incidence of PVL (higher if associated with IVH) bullGestational age lt 33 weeks 38 incidence of PVL bullgt 50 of patients with PVL or grade III IVH develop cerebral palsy
Cranial ultrasound coronal view day 1 showing severe echogenicity in the white matter MRI (T2SE (TR 6284TE 120) and ADC) performed on day 3 showing increased signal intensity in the white matter on T2SE and low signal intensity in the deep white matter on the ADC map with sparing of the anterior periventricular white matter and asymmetrical distribution in the parieto-occipital white matter The child died and was subsequently diagnosed to have molybdenum cofactor deficiency
Cranial sonography in 5-day old term with HIE with increase in echogenicity of white matter consistent with edemaCD ultrasound shows reversal of diastolic flow reflecting increased vascular resistance secondary to edema
PVL in a preterm infant (a) Coronal head US image obtained in the 1st week of life shows increased echogenicity in the periventricular white matter (arrows) (b) Follow-up US image obtained 2 months later shows development of cystic changes in these regions and dilatation of the adjacent lateral ventricles findings that are consistent with PVL
CT images show decrease In basal ganglia density related to Cytotoxic edemaSubtle loss of the normally sharp Transition from grey matter to White matter at the corticomedullary Junction Cerebral edema seen with effacementof the cortical sulci and the sylvian Fissures
PVL in a preterm neonate Axial T1-weighted (a) and T2-weighted (b) MR images obtained on day 4 of life demonstrate T1 hypointensity and T2 hyperintensity in the periventricular whitematter Note the punctate foci of high signal intensity on the T1-weighted image (arrows in a) These foci should be distinguished from foci of hemorrhage whichwould demonstrate greater T2 shortening on the corresponding T2-weighted image
28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

CT without and with iv contrast Axial T2 with bilateral thalamic infarct
Global hypoxic-ischemic brain injury
Hypoxic-ischemic brain injury
Images show the temporal evolution of a right-sided main branch MCA territory infarction (patient 1) on T1-weighted images (top row) and T2-weighted images (bottom row) obtained on days 2 5 12 42 and 75 post-delivery
Graph shows DWIs of a patient with an infarction within the PCA territory showing severe HSI on day 3 (A) and mild-to-moderate HSI on day 10 (B)
MRI Diffusion show bilateral fronto parietal and parieto occipital cortical restricted diffusion Similar restricted diffusion in caudate nuclei Area of involvement corresponds to cortical as well as internal border zone infarcts Imaging wise Bilateral border infarcts
A Axial T2-weighted fast spin-echo image (3200851) with an echo train length of 8 obtained at 13 hours of life shows no abnormality B Trace LSDI image (15206251) with a b max of 750 secondsmm2 obtained at 13 hours of life shows no abnormality C Corresponding ADC map D Axial T2-weighted fast spin-echo image obtained at 5 days of life shows very subtle hyperintensity in the posterior putamen bilaterally (arrows) E Trace LSDI image obtained at 5 days of life shows decreased diffusion in corresponding areas (arrows) F Corresponding ADC map G T1-weighted axial spin-echo image (600202) obtained at 6 weeks of life shows hyperintensity within the posterior putamen and ventrolateral thalamus bilaterally (arrows)
The neonatal mean diffusion-weighted image (mDWI) shows an ischemic area in the middle cerebral artery territory which resulted in a cyst observed at 3 and 24 mo The neonatal Z map shows normal Z values in all regions At 3 mo low Z values representing abnormal fractional anisotropy (FA) values were observed in the affected corticospinal tract which corresponded with the subsequent development of unilateral motor deficits The Z map at 24 mo was essentially identical Interestingly FA values in the fornix continued to decrease from the time of the neonatal scan to 24 mo suggesting delayed degeneration in this tract
Restricted diffusion signal in the DCST Left middle cerebral artery infarction (A) results in DWI signal changes throughout the DCST PLIC and cerebral peduncle involvement are evident on coronal (B) and sagittal images (C) Signal in the basis pontis and medullary pyramids can be seen on left (D) but not right (E) parasagittal sections
Neonate with left middle cerebral artery stroke and chronic hemiparesis DWI signal is appreciated throughout the DCST including PLIC (A) peduncle (B C) pons (D E) and pontomedullary junction (F)
Axial diffusion weighted images from a neonate (A) with a modified pediatric ASPECTS of eight (involvement of left internal capsule insula M3 M5 M6 P1 P2 and thalamus) and a child (B) with a modified pediatric ASPECTS of 10 (involvement of left caudate lentiform internal capsule insula and middle cerebral artery territories M1ndashM6)
(A) Axial diffusion-weighted image showing hyperintensity in the territory of left middle cerebral artery (B) MR angiography demonstrates loss of flow distal to the left middle cerebral artery bifurcation
A B
Perinatal asphyxia more appropriately known as hypoxic-
ischemic encephalopathy (HIE) is characterized by clinical and laboratory evidence of acute or subacute brain injury due to asphyxia The primary causes of this condition are systemic hypoxemia andor reduced cerebral blood flow (CBF) Birth asphyxia causes 840000 or 23 of all neonatal deaths worldwideHIE- Acute brain injury that occur before during or after birth
Signs and symptomsMild hypoxic-ischemic encephalopathybullMuscle tone may be slightly increased and deep tendon reflexes may be brisk during the first few daysbullTransient behavioral abnormalities such as poor feeding irritability or excessive crying or sleepiness (typically in an alternating pattern) may be observed bullTypically resolves in 24h
Moderately severe hypoxic-ischemic encephalopathyThe infant is lethargic with significant hypotonia and diminished deep tendon reflexesThe grasping Moro and sucking reflexes may be sluggish or absentThe infant may experience occasional periods of apneaSeizures typically occur early within the first 24 hours after birthFull recovery within 1-2 weeks is possible and is associated with a better long-term outcome
Severe hypoxic-ischemic encephalopathySeizures can be delayed and severe and may be initially resistant to conventional treatments The seizures are usually generalized and their frequency may increase during the 24-48 hours after onset correlating with the phase of reperfusion injury As the injury progresses seizures subside and the electroencephalogram becomes isoelectric or shows a burst suppression pattern At that time wakefulness may deteriorate further and the fontanelle may bulge suggesting increasing cerebral edema
Other symptoms include the following Stupor or coma is typical the infant may not respond to any physical stimulus except the most noxiousBreathing may be irregular and the infant often requires ventilatory support Generalized hypotonia and depressed deep tendon reflexes are common Neonatal reflexes (eg sucking swallowing grasping Moro) are absent Disturbances of ocular motion such as a skewed deviation of the eyes nystagmus bobbing and loss of dolls eye (ie conjugate) movements may be revealed by cranial nerve examination Pupils may be dilated fixed or poorly reactive to lightIrregularities of heart rate and blood pressure are common during the period of reperfusion injury as is death from cardiorespiratory failure An initial period of well-being or mild hypoxic-ischemic encephalopathy may be followed by sudden deterioration suggesting ongoing brain cell dysfunction injury and death during this period seizure intensity may increase
Imaging of neonatal hypoxic-ischemic encephalopathy
Ultrasonography is the first-line imaging technique for the evaluation of the newborn brain These past few years have seen an increasing role of MRI in the investigation of HIE because of greater sensitivity and specificity Electro-encephalogram(EEG)Computed Tomography(CT)MRI MRS and DWI
MRI sequencesT1 WI T2 WI++ FLAIR are not very useful to detect lesion in young infant less than 24 months due to brain maturation IR T1-weighted Has been very helpful in the last two decades before generalization of high fields MRI as it gives excellent images of brain anatomy and maturation It also shows accurately the differentiation between myelinated and unmyelinated WM Three-dimensional GE T1 weighted sequence (3DT1) bullallow 1 mm contiguous slices which can be reconstructed in any anatomic plane T2 to detect hemorrhagic lesions DWI It is now recommended that DWI should be performed between 2 days and 8 days of life Multiple studies have shown DWI are more sensitive in the detection of HIE lesions than conventional MRI especially for early diagnosis
MRI ProtocolSagittal and axial T1 WI Axial and coronal T2 WI Axial T2 3D T1 FLAIR (older child) DWI MRSLactate peak bulldue to anaerobic glycolysis bullfound within 24 h of life Subsequently a reduction in N-acetyl aspartate (NAA) is evident due to neuronal loss
Advanced technique Perfusion
Arterial Spin-Labeled (ASL) Perfusion bullRecent advances in novel research imaging modalitybullallows noninvasive evaluation of CBF (cerebral blood flow) using electromagnetically labeled arterial blood water as an endogenous contrast agent bullDemonstrates low CBF in neonates who have suffered HIE and in infants and children after stroke
Imaging RecommendationCranial sonography (US) bullFirst between 7 and 14 days bullRepeat before discharge from the hospital MRI DWI MRS bullWhen US is abnormal MRI precise lesion extension and aide in prognosticating bull Defining injury in VLBW neonates with normal US
PrognosisPoor outcome if bullIVH plus PVL bullPVL with volume loss widespread infarction or seizures bullPVL with enlarged cysts
It is necessary to bullknow the normal cerebral appearance before interpret pathological aspect bulldistinguish hypoxic-ischemic brain damage from normal myelination Brain compositionChanges in brain composition Changes in cellular density increase in complex lipids content due to the evolving process of myelination decrease in water content mostly in the WM
Shortening of T1 Shortening of T2
Imaging PatternThe imaging patterns of HIE can be classified into 3 types Lesions predominantly located in the PVWM Lesions predominantly located in the basal ganglia or thalamus Multicystic encephalomalcia The pattern of injury is postulated to depend on bull The type of hypoxiandashischaemia (acute and profound or prolonged and partial) bullThe gestational age (term or pre-term)
HIE in preterm infantRisk FactorsPregnancy Gestational ageweight previous preterm birth spontaneous preterm labor Intrapartum Abruption pre-eclampsia premature rupture of membranes chorioamnionitis group B Strep Peri amp postnatal factors Respiratory distress sepsis anemia apnea bradycardia cardiac arrest
General Features++ PVL +- associated to Germinal matrix and IVH PV hemorrhagic infarction Cerebellar infarction Definition bullPVL is the HIE driven periventricular white matter (PVWM) necrosis seen in very low birth weight premies (lt1500g) EpidemiologybullBirth weight lt 1500 g 45 incidence of PVL (higher if associated with IVH) bullGestational age lt 33 weeks 38 incidence of PVL bullgt 50 of patients with PVL or grade III IVH develop cerebral palsy
Cranial ultrasound coronal view day 1 showing severe echogenicity in the white matter MRI (T2SE (TR 6284TE 120) and ADC) performed on day 3 showing increased signal intensity in the white matter on T2SE and low signal intensity in the deep white matter on the ADC map with sparing of the anterior periventricular white matter and asymmetrical distribution in the parieto-occipital white matter The child died and was subsequently diagnosed to have molybdenum cofactor deficiency
Cranial sonography in 5-day old term with HIE with increase in echogenicity of white matter consistent with edemaCD ultrasound shows reversal of diastolic flow reflecting increased vascular resistance secondary to edema
PVL in a preterm infant (a) Coronal head US image obtained in the 1st week of life shows increased echogenicity in the periventricular white matter (arrows) (b) Follow-up US image obtained 2 months later shows development of cystic changes in these regions and dilatation of the adjacent lateral ventricles findings that are consistent with PVL
CT images show decrease In basal ganglia density related to Cytotoxic edemaSubtle loss of the normally sharp Transition from grey matter to White matter at the corticomedullary Junction Cerebral edema seen with effacementof the cortical sulci and the sylvian Fissures
PVL in a preterm neonate Axial T1-weighted (a) and T2-weighted (b) MR images obtained on day 4 of life demonstrate T1 hypointensity and T2 hyperintensity in the periventricular whitematter Note the punctate foci of high signal intensity on the T1-weighted image (arrows in a) These foci should be distinguished from foci of hemorrhage whichwould demonstrate greater T2 shortening on the corresponding T2-weighted image
28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

Global hypoxic-ischemic brain injury
Hypoxic-ischemic brain injury
Images show the temporal evolution of a right-sided main branch MCA territory infarction (patient 1) on T1-weighted images (top row) and T2-weighted images (bottom row) obtained on days 2 5 12 42 and 75 post-delivery
Graph shows DWIs of a patient with an infarction within the PCA territory showing severe HSI on day 3 (A) and mild-to-moderate HSI on day 10 (B)
MRI Diffusion show bilateral fronto parietal and parieto occipital cortical restricted diffusion Similar restricted diffusion in caudate nuclei Area of involvement corresponds to cortical as well as internal border zone infarcts Imaging wise Bilateral border infarcts
A Axial T2-weighted fast spin-echo image (3200851) with an echo train length of 8 obtained at 13 hours of life shows no abnormality B Trace LSDI image (15206251) with a b max of 750 secondsmm2 obtained at 13 hours of life shows no abnormality C Corresponding ADC map D Axial T2-weighted fast spin-echo image obtained at 5 days of life shows very subtle hyperintensity in the posterior putamen bilaterally (arrows) E Trace LSDI image obtained at 5 days of life shows decreased diffusion in corresponding areas (arrows) F Corresponding ADC map G T1-weighted axial spin-echo image (600202) obtained at 6 weeks of life shows hyperintensity within the posterior putamen and ventrolateral thalamus bilaterally (arrows)
The neonatal mean diffusion-weighted image (mDWI) shows an ischemic area in the middle cerebral artery territory which resulted in a cyst observed at 3 and 24 mo The neonatal Z map shows normal Z values in all regions At 3 mo low Z values representing abnormal fractional anisotropy (FA) values were observed in the affected corticospinal tract which corresponded with the subsequent development of unilateral motor deficits The Z map at 24 mo was essentially identical Interestingly FA values in the fornix continued to decrease from the time of the neonatal scan to 24 mo suggesting delayed degeneration in this tract
Restricted diffusion signal in the DCST Left middle cerebral artery infarction (A) results in DWI signal changes throughout the DCST PLIC and cerebral peduncle involvement are evident on coronal (B) and sagittal images (C) Signal in the basis pontis and medullary pyramids can be seen on left (D) but not right (E) parasagittal sections
Neonate with left middle cerebral artery stroke and chronic hemiparesis DWI signal is appreciated throughout the DCST including PLIC (A) peduncle (B C) pons (D E) and pontomedullary junction (F)
Axial diffusion weighted images from a neonate (A) with a modified pediatric ASPECTS of eight (involvement of left internal capsule insula M3 M5 M6 P1 P2 and thalamus) and a child (B) with a modified pediatric ASPECTS of 10 (involvement of left caudate lentiform internal capsule insula and middle cerebral artery territories M1ndashM6)
(A) Axial diffusion-weighted image showing hyperintensity in the territory of left middle cerebral artery (B) MR angiography demonstrates loss of flow distal to the left middle cerebral artery bifurcation
A B
Perinatal asphyxia more appropriately known as hypoxic-
ischemic encephalopathy (HIE) is characterized by clinical and laboratory evidence of acute or subacute brain injury due to asphyxia The primary causes of this condition are systemic hypoxemia andor reduced cerebral blood flow (CBF) Birth asphyxia causes 840000 or 23 of all neonatal deaths worldwideHIE- Acute brain injury that occur before during or after birth
Signs and symptomsMild hypoxic-ischemic encephalopathybullMuscle tone may be slightly increased and deep tendon reflexes may be brisk during the first few daysbullTransient behavioral abnormalities such as poor feeding irritability or excessive crying or sleepiness (typically in an alternating pattern) may be observed bullTypically resolves in 24h
Moderately severe hypoxic-ischemic encephalopathyThe infant is lethargic with significant hypotonia and diminished deep tendon reflexesThe grasping Moro and sucking reflexes may be sluggish or absentThe infant may experience occasional periods of apneaSeizures typically occur early within the first 24 hours after birthFull recovery within 1-2 weeks is possible and is associated with a better long-term outcome
Severe hypoxic-ischemic encephalopathySeizures can be delayed and severe and may be initially resistant to conventional treatments The seizures are usually generalized and their frequency may increase during the 24-48 hours after onset correlating with the phase of reperfusion injury As the injury progresses seizures subside and the electroencephalogram becomes isoelectric or shows a burst suppression pattern At that time wakefulness may deteriorate further and the fontanelle may bulge suggesting increasing cerebral edema
Other symptoms include the following Stupor or coma is typical the infant may not respond to any physical stimulus except the most noxiousBreathing may be irregular and the infant often requires ventilatory support Generalized hypotonia and depressed deep tendon reflexes are common Neonatal reflexes (eg sucking swallowing grasping Moro) are absent Disturbances of ocular motion such as a skewed deviation of the eyes nystagmus bobbing and loss of dolls eye (ie conjugate) movements may be revealed by cranial nerve examination Pupils may be dilated fixed or poorly reactive to lightIrregularities of heart rate and blood pressure are common during the period of reperfusion injury as is death from cardiorespiratory failure An initial period of well-being or mild hypoxic-ischemic encephalopathy may be followed by sudden deterioration suggesting ongoing brain cell dysfunction injury and death during this period seizure intensity may increase
Imaging of neonatal hypoxic-ischemic encephalopathy
Ultrasonography is the first-line imaging technique for the evaluation of the newborn brain These past few years have seen an increasing role of MRI in the investigation of HIE because of greater sensitivity and specificity Electro-encephalogram(EEG)Computed Tomography(CT)MRI MRS and DWI
MRI sequencesT1 WI T2 WI++ FLAIR are not very useful to detect lesion in young infant less than 24 months due to brain maturation IR T1-weighted Has been very helpful in the last two decades before generalization of high fields MRI as it gives excellent images of brain anatomy and maturation It also shows accurately the differentiation between myelinated and unmyelinated WM Three-dimensional GE T1 weighted sequence (3DT1) bullallow 1 mm contiguous slices which can be reconstructed in any anatomic plane T2 to detect hemorrhagic lesions DWI It is now recommended that DWI should be performed between 2 days and 8 days of life Multiple studies have shown DWI are more sensitive in the detection of HIE lesions than conventional MRI especially for early diagnosis
MRI ProtocolSagittal and axial T1 WI Axial and coronal T2 WI Axial T2 3D T1 FLAIR (older child) DWI MRSLactate peak bulldue to anaerobic glycolysis bullfound within 24 h of life Subsequently a reduction in N-acetyl aspartate (NAA) is evident due to neuronal loss
Advanced technique Perfusion
Arterial Spin-Labeled (ASL) Perfusion bullRecent advances in novel research imaging modalitybullallows noninvasive evaluation of CBF (cerebral blood flow) using electromagnetically labeled arterial blood water as an endogenous contrast agent bullDemonstrates low CBF in neonates who have suffered HIE and in infants and children after stroke
Imaging RecommendationCranial sonography (US) bullFirst between 7 and 14 days bullRepeat before discharge from the hospital MRI DWI MRS bullWhen US is abnormal MRI precise lesion extension and aide in prognosticating bull Defining injury in VLBW neonates with normal US
PrognosisPoor outcome if bullIVH plus PVL bullPVL with volume loss widespread infarction or seizures bullPVL with enlarged cysts
It is necessary to bullknow the normal cerebral appearance before interpret pathological aspect bulldistinguish hypoxic-ischemic brain damage from normal myelination Brain compositionChanges in brain composition Changes in cellular density increase in complex lipids content due to the evolving process of myelination decrease in water content mostly in the WM
Shortening of T1 Shortening of T2
Imaging PatternThe imaging patterns of HIE can be classified into 3 types Lesions predominantly located in the PVWM Lesions predominantly located in the basal ganglia or thalamus Multicystic encephalomalcia The pattern of injury is postulated to depend on bull The type of hypoxiandashischaemia (acute and profound or prolonged and partial) bullThe gestational age (term or pre-term)
HIE in preterm infantRisk FactorsPregnancy Gestational ageweight previous preterm birth spontaneous preterm labor Intrapartum Abruption pre-eclampsia premature rupture of membranes chorioamnionitis group B Strep Peri amp postnatal factors Respiratory distress sepsis anemia apnea bradycardia cardiac arrest
General Features++ PVL +- associated to Germinal matrix and IVH PV hemorrhagic infarction Cerebellar infarction Definition bullPVL is the HIE driven periventricular white matter (PVWM) necrosis seen in very low birth weight premies (lt1500g) EpidemiologybullBirth weight lt 1500 g 45 incidence of PVL (higher if associated with IVH) bullGestational age lt 33 weeks 38 incidence of PVL bullgt 50 of patients with PVL or grade III IVH develop cerebral palsy
Cranial ultrasound coronal view day 1 showing severe echogenicity in the white matter MRI (T2SE (TR 6284TE 120) and ADC) performed on day 3 showing increased signal intensity in the white matter on T2SE and low signal intensity in the deep white matter on the ADC map with sparing of the anterior periventricular white matter and asymmetrical distribution in the parieto-occipital white matter The child died and was subsequently diagnosed to have molybdenum cofactor deficiency
Cranial sonography in 5-day old term with HIE with increase in echogenicity of white matter consistent with edemaCD ultrasound shows reversal of diastolic flow reflecting increased vascular resistance secondary to edema
PVL in a preterm infant (a) Coronal head US image obtained in the 1st week of life shows increased echogenicity in the periventricular white matter (arrows) (b) Follow-up US image obtained 2 months later shows development of cystic changes in these regions and dilatation of the adjacent lateral ventricles findings that are consistent with PVL
CT images show decrease In basal ganglia density related to Cytotoxic edemaSubtle loss of the normally sharp Transition from grey matter to White matter at the corticomedullary Junction Cerebral edema seen with effacementof the cortical sulci and the sylvian Fissures
PVL in a preterm neonate Axial T1-weighted (a) and T2-weighted (b) MR images obtained on day 4 of life demonstrate T1 hypointensity and T2 hyperintensity in the periventricular whitematter Note the punctate foci of high signal intensity on the T1-weighted image (arrows in a) These foci should be distinguished from foci of hemorrhage whichwould demonstrate greater T2 shortening on the corresponding T2-weighted image
28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

Hypoxic-ischemic brain injury
Images show the temporal evolution of a right-sided main branch MCA territory infarction (patient 1) on T1-weighted images (top row) and T2-weighted images (bottom row) obtained on days 2 5 12 42 and 75 post-delivery
Graph shows DWIs of a patient with an infarction within the PCA territory showing severe HSI on day 3 (A) and mild-to-moderate HSI on day 10 (B)
MRI Diffusion show bilateral fronto parietal and parieto occipital cortical restricted diffusion Similar restricted diffusion in caudate nuclei Area of involvement corresponds to cortical as well as internal border zone infarcts Imaging wise Bilateral border infarcts
A Axial T2-weighted fast spin-echo image (3200851) with an echo train length of 8 obtained at 13 hours of life shows no abnormality B Trace LSDI image (15206251) with a b max of 750 secondsmm2 obtained at 13 hours of life shows no abnormality C Corresponding ADC map D Axial T2-weighted fast spin-echo image obtained at 5 days of life shows very subtle hyperintensity in the posterior putamen bilaterally (arrows) E Trace LSDI image obtained at 5 days of life shows decreased diffusion in corresponding areas (arrows) F Corresponding ADC map G T1-weighted axial spin-echo image (600202) obtained at 6 weeks of life shows hyperintensity within the posterior putamen and ventrolateral thalamus bilaterally (arrows)
The neonatal mean diffusion-weighted image (mDWI) shows an ischemic area in the middle cerebral artery territory which resulted in a cyst observed at 3 and 24 mo The neonatal Z map shows normal Z values in all regions At 3 mo low Z values representing abnormal fractional anisotropy (FA) values were observed in the affected corticospinal tract which corresponded with the subsequent development of unilateral motor deficits The Z map at 24 mo was essentially identical Interestingly FA values in the fornix continued to decrease from the time of the neonatal scan to 24 mo suggesting delayed degeneration in this tract
Restricted diffusion signal in the DCST Left middle cerebral artery infarction (A) results in DWI signal changes throughout the DCST PLIC and cerebral peduncle involvement are evident on coronal (B) and sagittal images (C) Signal in the basis pontis and medullary pyramids can be seen on left (D) but not right (E) parasagittal sections
Neonate with left middle cerebral artery stroke and chronic hemiparesis DWI signal is appreciated throughout the DCST including PLIC (A) peduncle (B C) pons (D E) and pontomedullary junction (F)
Axial diffusion weighted images from a neonate (A) with a modified pediatric ASPECTS of eight (involvement of left internal capsule insula M3 M5 M6 P1 P2 and thalamus) and a child (B) with a modified pediatric ASPECTS of 10 (involvement of left caudate lentiform internal capsule insula and middle cerebral artery territories M1ndashM6)
(A) Axial diffusion-weighted image showing hyperintensity in the territory of left middle cerebral artery (B) MR angiography demonstrates loss of flow distal to the left middle cerebral artery bifurcation
A B
Perinatal asphyxia more appropriately known as hypoxic-
ischemic encephalopathy (HIE) is characterized by clinical and laboratory evidence of acute or subacute brain injury due to asphyxia The primary causes of this condition are systemic hypoxemia andor reduced cerebral blood flow (CBF) Birth asphyxia causes 840000 or 23 of all neonatal deaths worldwideHIE- Acute brain injury that occur before during or after birth
Signs and symptomsMild hypoxic-ischemic encephalopathybullMuscle tone may be slightly increased and deep tendon reflexes may be brisk during the first few daysbullTransient behavioral abnormalities such as poor feeding irritability or excessive crying or sleepiness (typically in an alternating pattern) may be observed bullTypically resolves in 24h
Moderately severe hypoxic-ischemic encephalopathyThe infant is lethargic with significant hypotonia and diminished deep tendon reflexesThe grasping Moro and sucking reflexes may be sluggish or absentThe infant may experience occasional periods of apneaSeizures typically occur early within the first 24 hours after birthFull recovery within 1-2 weeks is possible and is associated with a better long-term outcome
Severe hypoxic-ischemic encephalopathySeizures can be delayed and severe and may be initially resistant to conventional treatments The seizures are usually generalized and their frequency may increase during the 24-48 hours after onset correlating with the phase of reperfusion injury As the injury progresses seizures subside and the electroencephalogram becomes isoelectric or shows a burst suppression pattern At that time wakefulness may deteriorate further and the fontanelle may bulge suggesting increasing cerebral edema
Other symptoms include the following Stupor or coma is typical the infant may not respond to any physical stimulus except the most noxiousBreathing may be irregular and the infant often requires ventilatory support Generalized hypotonia and depressed deep tendon reflexes are common Neonatal reflexes (eg sucking swallowing grasping Moro) are absent Disturbances of ocular motion such as a skewed deviation of the eyes nystagmus bobbing and loss of dolls eye (ie conjugate) movements may be revealed by cranial nerve examination Pupils may be dilated fixed or poorly reactive to lightIrregularities of heart rate and blood pressure are common during the period of reperfusion injury as is death from cardiorespiratory failure An initial period of well-being or mild hypoxic-ischemic encephalopathy may be followed by sudden deterioration suggesting ongoing brain cell dysfunction injury and death during this period seizure intensity may increase
Imaging of neonatal hypoxic-ischemic encephalopathy
Ultrasonography is the first-line imaging technique for the evaluation of the newborn brain These past few years have seen an increasing role of MRI in the investigation of HIE because of greater sensitivity and specificity Electro-encephalogram(EEG)Computed Tomography(CT)MRI MRS and DWI
MRI sequencesT1 WI T2 WI++ FLAIR are not very useful to detect lesion in young infant less than 24 months due to brain maturation IR T1-weighted Has been very helpful in the last two decades before generalization of high fields MRI as it gives excellent images of brain anatomy and maturation It also shows accurately the differentiation between myelinated and unmyelinated WM Three-dimensional GE T1 weighted sequence (3DT1) bullallow 1 mm contiguous slices which can be reconstructed in any anatomic plane T2 to detect hemorrhagic lesions DWI It is now recommended that DWI should be performed between 2 days and 8 days of life Multiple studies have shown DWI are more sensitive in the detection of HIE lesions than conventional MRI especially for early diagnosis
MRI ProtocolSagittal and axial T1 WI Axial and coronal T2 WI Axial T2 3D T1 FLAIR (older child) DWI MRSLactate peak bulldue to anaerobic glycolysis bullfound within 24 h of life Subsequently a reduction in N-acetyl aspartate (NAA) is evident due to neuronal loss
Advanced technique Perfusion
Arterial Spin-Labeled (ASL) Perfusion bullRecent advances in novel research imaging modalitybullallows noninvasive evaluation of CBF (cerebral blood flow) using electromagnetically labeled arterial blood water as an endogenous contrast agent bullDemonstrates low CBF in neonates who have suffered HIE and in infants and children after stroke
Imaging RecommendationCranial sonography (US) bullFirst between 7 and 14 days bullRepeat before discharge from the hospital MRI DWI MRS bullWhen US is abnormal MRI precise lesion extension and aide in prognosticating bull Defining injury in VLBW neonates with normal US
PrognosisPoor outcome if bullIVH plus PVL bullPVL with volume loss widespread infarction or seizures bullPVL with enlarged cysts
It is necessary to bullknow the normal cerebral appearance before interpret pathological aspect bulldistinguish hypoxic-ischemic brain damage from normal myelination Brain compositionChanges in brain composition Changes in cellular density increase in complex lipids content due to the evolving process of myelination decrease in water content mostly in the WM
Shortening of T1 Shortening of T2
Imaging PatternThe imaging patterns of HIE can be classified into 3 types Lesions predominantly located in the PVWM Lesions predominantly located in the basal ganglia or thalamus Multicystic encephalomalcia The pattern of injury is postulated to depend on bull The type of hypoxiandashischaemia (acute and profound or prolonged and partial) bullThe gestational age (term or pre-term)
HIE in preterm infantRisk FactorsPregnancy Gestational ageweight previous preterm birth spontaneous preterm labor Intrapartum Abruption pre-eclampsia premature rupture of membranes chorioamnionitis group B Strep Peri amp postnatal factors Respiratory distress sepsis anemia apnea bradycardia cardiac arrest
General Features++ PVL +- associated to Germinal matrix and IVH PV hemorrhagic infarction Cerebellar infarction Definition bullPVL is the HIE driven periventricular white matter (PVWM) necrosis seen in very low birth weight premies (lt1500g) EpidemiologybullBirth weight lt 1500 g 45 incidence of PVL (higher if associated with IVH) bullGestational age lt 33 weeks 38 incidence of PVL bullgt 50 of patients with PVL or grade III IVH develop cerebral palsy
Cranial ultrasound coronal view day 1 showing severe echogenicity in the white matter MRI (T2SE (TR 6284TE 120) and ADC) performed on day 3 showing increased signal intensity in the white matter on T2SE and low signal intensity in the deep white matter on the ADC map with sparing of the anterior periventricular white matter and asymmetrical distribution in the parieto-occipital white matter The child died and was subsequently diagnosed to have molybdenum cofactor deficiency
Cranial sonography in 5-day old term with HIE with increase in echogenicity of white matter consistent with edemaCD ultrasound shows reversal of diastolic flow reflecting increased vascular resistance secondary to edema
PVL in a preterm infant (a) Coronal head US image obtained in the 1st week of life shows increased echogenicity in the periventricular white matter (arrows) (b) Follow-up US image obtained 2 months later shows development of cystic changes in these regions and dilatation of the adjacent lateral ventricles findings that are consistent with PVL
CT images show decrease In basal ganglia density related to Cytotoxic edemaSubtle loss of the normally sharp Transition from grey matter to White matter at the corticomedullary Junction Cerebral edema seen with effacementof the cortical sulci and the sylvian Fissures
PVL in a preterm neonate Axial T1-weighted (a) and T2-weighted (b) MR images obtained on day 4 of life demonstrate T1 hypointensity and T2 hyperintensity in the periventricular whitematter Note the punctate foci of high signal intensity on the T1-weighted image (arrows in a) These foci should be distinguished from foci of hemorrhage whichwould demonstrate greater T2 shortening on the corresponding T2-weighted image
28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

Images show the temporal evolution of a right-sided main branch MCA territory infarction (patient 1) on T1-weighted images (top row) and T2-weighted images (bottom row) obtained on days 2 5 12 42 and 75 post-delivery
Graph shows DWIs of a patient with an infarction within the PCA territory showing severe HSI on day 3 (A) and mild-to-moderate HSI on day 10 (B)
MRI Diffusion show bilateral fronto parietal and parieto occipital cortical restricted diffusion Similar restricted diffusion in caudate nuclei Area of involvement corresponds to cortical as well as internal border zone infarcts Imaging wise Bilateral border infarcts
A Axial T2-weighted fast spin-echo image (3200851) with an echo train length of 8 obtained at 13 hours of life shows no abnormality B Trace LSDI image (15206251) with a b max of 750 secondsmm2 obtained at 13 hours of life shows no abnormality C Corresponding ADC map D Axial T2-weighted fast spin-echo image obtained at 5 days of life shows very subtle hyperintensity in the posterior putamen bilaterally (arrows) E Trace LSDI image obtained at 5 days of life shows decreased diffusion in corresponding areas (arrows) F Corresponding ADC map G T1-weighted axial spin-echo image (600202) obtained at 6 weeks of life shows hyperintensity within the posterior putamen and ventrolateral thalamus bilaterally (arrows)
The neonatal mean diffusion-weighted image (mDWI) shows an ischemic area in the middle cerebral artery territory which resulted in a cyst observed at 3 and 24 mo The neonatal Z map shows normal Z values in all regions At 3 mo low Z values representing abnormal fractional anisotropy (FA) values were observed in the affected corticospinal tract which corresponded with the subsequent development of unilateral motor deficits The Z map at 24 mo was essentially identical Interestingly FA values in the fornix continued to decrease from the time of the neonatal scan to 24 mo suggesting delayed degeneration in this tract
Restricted diffusion signal in the DCST Left middle cerebral artery infarction (A) results in DWI signal changes throughout the DCST PLIC and cerebral peduncle involvement are evident on coronal (B) and sagittal images (C) Signal in the basis pontis and medullary pyramids can be seen on left (D) but not right (E) parasagittal sections
Neonate with left middle cerebral artery stroke and chronic hemiparesis DWI signal is appreciated throughout the DCST including PLIC (A) peduncle (B C) pons (D E) and pontomedullary junction (F)
Axial diffusion weighted images from a neonate (A) with a modified pediatric ASPECTS of eight (involvement of left internal capsule insula M3 M5 M6 P1 P2 and thalamus) and a child (B) with a modified pediatric ASPECTS of 10 (involvement of left caudate lentiform internal capsule insula and middle cerebral artery territories M1ndashM6)
(A) Axial diffusion-weighted image showing hyperintensity in the territory of left middle cerebral artery (B) MR angiography demonstrates loss of flow distal to the left middle cerebral artery bifurcation
A B
Perinatal asphyxia more appropriately known as hypoxic-
ischemic encephalopathy (HIE) is characterized by clinical and laboratory evidence of acute or subacute brain injury due to asphyxia The primary causes of this condition are systemic hypoxemia andor reduced cerebral blood flow (CBF) Birth asphyxia causes 840000 or 23 of all neonatal deaths worldwideHIE- Acute brain injury that occur before during or after birth
Signs and symptomsMild hypoxic-ischemic encephalopathybullMuscle tone may be slightly increased and deep tendon reflexes may be brisk during the first few daysbullTransient behavioral abnormalities such as poor feeding irritability or excessive crying or sleepiness (typically in an alternating pattern) may be observed bullTypically resolves in 24h
Moderately severe hypoxic-ischemic encephalopathyThe infant is lethargic with significant hypotonia and diminished deep tendon reflexesThe grasping Moro and sucking reflexes may be sluggish or absentThe infant may experience occasional periods of apneaSeizures typically occur early within the first 24 hours after birthFull recovery within 1-2 weeks is possible and is associated with a better long-term outcome
Severe hypoxic-ischemic encephalopathySeizures can be delayed and severe and may be initially resistant to conventional treatments The seizures are usually generalized and their frequency may increase during the 24-48 hours after onset correlating with the phase of reperfusion injury As the injury progresses seizures subside and the electroencephalogram becomes isoelectric or shows a burst suppression pattern At that time wakefulness may deteriorate further and the fontanelle may bulge suggesting increasing cerebral edema
Other symptoms include the following Stupor or coma is typical the infant may not respond to any physical stimulus except the most noxiousBreathing may be irregular and the infant often requires ventilatory support Generalized hypotonia and depressed deep tendon reflexes are common Neonatal reflexes (eg sucking swallowing grasping Moro) are absent Disturbances of ocular motion such as a skewed deviation of the eyes nystagmus bobbing and loss of dolls eye (ie conjugate) movements may be revealed by cranial nerve examination Pupils may be dilated fixed or poorly reactive to lightIrregularities of heart rate and blood pressure are common during the period of reperfusion injury as is death from cardiorespiratory failure An initial period of well-being or mild hypoxic-ischemic encephalopathy may be followed by sudden deterioration suggesting ongoing brain cell dysfunction injury and death during this period seizure intensity may increase
Imaging of neonatal hypoxic-ischemic encephalopathy
Ultrasonography is the first-line imaging technique for the evaluation of the newborn brain These past few years have seen an increasing role of MRI in the investigation of HIE because of greater sensitivity and specificity Electro-encephalogram(EEG)Computed Tomography(CT)MRI MRS and DWI
MRI sequencesT1 WI T2 WI++ FLAIR are not very useful to detect lesion in young infant less than 24 months due to brain maturation IR T1-weighted Has been very helpful in the last two decades before generalization of high fields MRI as it gives excellent images of brain anatomy and maturation It also shows accurately the differentiation between myelinated and unmyelinated WM Three-dimensional GE T1 weighted sequence (3DT1) bullallow 1 mm contiguous slices which can be reconstructed in any anatomic plane T2 to detect hemorrhagic lesions DWI It is now recommended that DWI should be performed between 2 days and 8 days of life Multiple studies have shown DWI are more sensitive in the detection of HIE lesions than conventional MRI especially for early diagnosis
MRI ProtocolSagittal and axial T1 WI Axial and coronal T2 WI Axial T2 3D T1 FLAIR (older child) DWI MRSLactate peak bulldue to anaerobic glycolysis bullfound within 24 h of life Subsequently a reduction in N-acetyl aspartate (NAA) is evident due to neuronal loss
Advanced technique Perfusion
Arterial Spin-Labeled (ASL) Perfusion bullRecent advances in novel research imaging modalitybullallows noninvasive evaluation of CBF (cerebral blood flow) using electromagnetically labeled arterial blood water as an endogenous contrast agent bullDemonstrates low CBF in neonates who have suffered HIE and in infants and children after stroke
Imaging RecommendationCranial sonography (US) bullFirst between 7 and 14 days bullRepeat before discharge from the hospital MRI DWI MRS bullWhen US is abnormal MRI precise lesion extension and aide in prognosticating bull Defining injury in VLBW neonates with normal US
PrognosisPoor outcome if bullIVH plus PVL bullPVL with volume loss widespread infarction or seizures bullPVL with enlarged cysts
It is necessary to bullknow the normal cerebral appearance before interpret pathological aspect bulldistinguish hypoxic-ischemic brain damage from normal myelination Brain compositionChanges in brain composition Changes in cellular density increase in complex lipids content due to the evolving process of myelination decrease in water content mostly in the WM
Shortening of T1 Shortening of T2
Imaging PatternThe imaging patterns of HIE can be classified into 3 types Lesions predominantly located in the PVWM Lesions predominantly located in the basal ganglia or thalamus Multicystic encephalomalcia The pattern of injury is postulated to depend on bull The type of hypoxiandashischaemia (acute and profound or prolonged and partial) bullThe gestational age (term or pre-term)
HIE in preterm infantRisk FactorsPregnancy Gestational ageweight previous preterm birth spontaneous preterm labor Intrapartum Abruption pre-eclampsia premature rupture of membranes chorioamnionitis group B Strep Peri amp postnatal factors Respiratory distress sepsis anemia apnea bradycardia cardiac arrest
General Features++ PVL +- associated to Germinal matrix and IVH PV hemorrhagic infarction Cerebellar infarction Definition bullPVL is the HIE driven periventricular white matter (PVWM) necrosis seen in very low birth weight premies (lt1500g) EpidemiologybullBirth weight lt 1500 g 45 incidence of PVL (higher if associated with IVH) bullGestational age lt 33 weeks 38 incidence of PVL bullgt 50 of patients with PVL or grade III IVH develop cerebral palsy
Cranial ultrasound coronal view day 1 showing severe echogenicity in the white matter MRI (T2SE (TR 6284TE 120) and ADC) performed on day 3 showing increased signal intensity in the white matter on T2SE and low signal intensity in the deep white matter on the ADC map with sparing of the anterior periventricular white matter and asymmetrical distribution in the parieto-occipital white matter The child died and was subsequently diagnosed to have molybdenum cofactor deficiency
Cranial sonography in 5-day old term with HIE with increase in echogenicity of white matter consistent with edemaCD ultrasound shows reversal of diastolic flow reflecting increased vascular resistance secondary to edema
PVL in a preterm infant (a) Coronal head US image obtained in the 1st week of life shows increased echogenicity in the periventricular white matter (arrows) (b) Follow-up US image obtained 2 months later shows development of cystic changes in these regions and dilatation of the adjacent lateral ventricles findings that are consistent with PVL
CT images show decrease In basal ganglia density related to Cytotoxic edemaSubtle loss of the normally sharp Transition from grey matter to White matter at the corticomedullary Junction Cerebral edema seen with effacementof the cortical sulci and the sylvian Fissures
PVL in a preterm neonate Axial T1-weighted (a) and T2-weighted (b) MR images obtained on day 4 of life demonstrate T1 hypointensity and T2 hyperintensity in the periventricular whitematter Note the punctate foci of high signal intensity on the T1-weighted image (arrows in a) These foci should be distinguished from foci of hemorrhage whichwould demonstrate greater T2 shortening on the corresponding T2-weighted image
28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

Graph shows DWIs of a patient with an infarction within the PCA territory showing severe HSI on day 3 (A) and mild-to-moderate HSI on day 10 (B)
MRI Diffusion show bilateral fronto parietal and parieto occipital cortical restricted diffusion Similar restricted diffusion in caudate nuclei Area of involvement corresponds to cortical as well as internal border zone infarcts Imaging wise Bilateral border infarcts
A Axial T2-weighted fast spin-echo image (3200851) with an echo train length of 8 obtained at 13 hours of life shows no abnormality B Trace LSDI image (15206251) with a b max of 750 secondsmm2 obtained at 13 hours of life shows no abnormality C Corresponding ADC map D Axial T2-weighted fast spin-echo image obtained at 5 days of life shows very subtle hyperintensity in the posterior putamen bilaterally (arrows) E Trace LSDI image obtained at 5 days of life shows decreased diffusion in corresponding areas (arrows) F Corresponding ADC map G T1-weighted axial spin-echo image (600202) obtained at 6 weeks of life shows hyperintensity within the posterior putamen and ventrolateral thalamus bilaterally (arrows)
The neonatal mean diffusion-weighted image (mDWI) shows an ischemic area in the middle cerebral artery territory which resulted in a cyst observed at 3 and 24 mo The neonatal Z map shows normal Z values in all regions At 3 mo low Z values representing abnormal fractional anisotropy (FA) values were observed in the affected corticospinal tract which corresponded with the subsequent development of unilateral motor deficits The Z map at 24 mo was essentially identical Interestingly FA values in the fornix continued to decrease from the time of the neonatal scan to 24 mo suggesting delayed degeneration in this tract
Restricted diffusion signal in the DCST Left middle cerebral artery infarction (A) results in DWI signal changes throughout the DCST PLIC and cerebral peduncle involvement are evident on coronal (B) and sagittal images (C) Signal in the basis pontis and medullary pyramids can be seen on left (D) but not right (E) parasagittal sections
Neonate with left middle cerebral artery stroke and chronic hemiparesis DWI signal is appreciated throughout the DCST including PLIC (A) peduncle (B C) pons (D E) and pontomedullary junction (F)
Axial diffusion weighted images from a neonate (A) with a modified pediatric ASPECTS of eight (involvement of left internal capsule insula M3 M5 M6 P1 P2 and thalamus) and a child (B) with a modified pediatric ASPECTS of 10 (involvement of left caudate lentiform internal capsule insula and middle cerebral artery territories M1ndashM6)
(A) Axial diffusion-weighted image showing hyperintensity in the territory of left middle cerebral artery (B) MR angiography demonstrates loss of flow distal to the left middle cerebral artery bifurcation
A B
Perinatal asphyxia more appropriately known as hypoxic-
ischemic encephalopathy (HIE) is characterized by clinical and laboratory evidence of acute or subacute brain injury due to asphyxia The primary causes of this condition are systemic hypoxemia andor reduced cerebral blood flow (CBF) Birth asphyxia causes 840000 or 23 of all neonatal deaths worldwideHIE- Acute brain injury that occur before during or after birth
Signs and symptomsMild hypoxic-ischemic encephalopathybullMuscle tone may be slightly increased and deep tendon reflexes may be brisk during the first few daysbullTransient behavioral abnormalities such as poor feeding irritability or excessive crying or sleepiness (typically in an alternating pattern) may be observed bullTypically resolves in 24h
Moderately severe hypoxic-ischemic encephalopathyThe infant is lethargic with significant hypotonia and diminished deep tendon reflexesThe grasping Moro and sucking reflexes may be sluggish or absentThe infant may experience occasional periods of apneaSeizures typically occur early within the first 24 hours after birthFull recovery within 1-2 weeks is possible and is associated with a better long-term outcome
Severe hypoxic-ischemic encephalopathySeizures can be delayed and severe and may be initially resistant to conventional treatments The seizures are usually generalized and their frequency may increase during the 24-48 hours after onset correlating with the phase of reperfusion injury As the injury progresses seizures subside and the electroencephalogram becomes isoelectric or shows a burst suppression pattern At that time wakefulness may deteriorate further and the fontanelle may bulge suggesting increasing cerebral edema
Other symptoms include the following Stupor or coma is typical the infant may not respond to any physical stimulus except the most noxiousBreathing may be irregular and the infant often requires ventilatory support Generalized hypotonia and depressed deep tendon reflexes are common Neonatal reflexes (eg sucking swallowing grasping Moro) are absent Disturbances of ocular motion such as a skewed deviation of the eyes nystagmus bobbing and loss of dolls eye (ie conjugate) movements may be revealed by cranial nerve examination Pupils may be dilated fixed or poorly reactive to lightIrregularities of heart rate and blood pressure are common during the period of reperfusion injury as is death from cardiorespiratory failure An initial period of well-being or mild hypoxic-ischemic encephalopathy may be followed by sudden deterioration suggesting ongoing brain cell dysfunction injury and death during this period seizure intensity may increase
Imaging of neonatal hypoxic-ischemic encephalopathy
Ultrasonography is the first-line imaging technique for the evaluation of the newborn brain These past few years have seen an increasing role of MRI in the investigation of HIE because of greater sensitivity and specificity Electro-encephalogram(EEG)Computed Tomography(CT)MRI MRS and DWI
MRI sequencesT1 WI T2 WI++ FLAIR are not very useful to detect lesion in young infant less than 24 months due to brain maturation IR T1-weighted Has been very helpful in the last two decades before generalization of high fields MRI as it gives excellent images of brain anatomy and maturation It also shows accurately the differentiation between myelinated and unmyelinated WM Three-dimensional GE T1 weighted sequence (3DT1) bullallow 1 mm contiguous slices which can be reconstructed in any anatomic plane T2 to detect hemorrhagic lesions DWI It is now recommended that DWI should be performed between 2 days and 8 days of life Multiple studies have shown DWI are more sensitive in the detection of HIE lesions than conventional MRI especially for early diagnosis
MRI ProtocolSagittal and axial T1 WI Axial and coronal T2 WI Axial T2 3D T1 FLAIR (older child) DWI MRSLactate peak bulldue to anaerobic glycolysis bullfound within 24 h of life Subsequently a reduction in N-acetyl aspartate (NAA) is evident due to neuronal loss
Advanced technique Perfusion
Arterial Spin-Labeled (ASL) Perfusion bullRecent advances in novel research imaging modalitybullallows noninvasive evaluation of CBF (cerebral blood flow) using electromagnetically labeled arterial blood water as an endogenous contrast agent bullDemonstrates low CBF in neonates who have suffered HIE and in infants and children after stroke
Imaging RecommendationCranial sonography (US) bullFirst between 7 and 14 days bullRepeat before discharge from the hospital MRI DWI MRS bullWhen US is abnormal MRI precise lesion extension and aide in prognosticating bull Defining injury in VLBW neonates with normal US
PrognosisPoor outcome if bullIVH plus PVL bullPVL with volume loss widespread infarction or seizures bullPVL with enlarged cysts
It is necessary to bullknow the normal cerebral appearance before interpret pathological aspect bulldistinguish hypoxic-ischemic brain damage from normal myelination Brain compositionChanges in brain composition Changes in cellular density increase in complex lipids content due to the evolving process of myelination decrease in water content mostly in the WM
Shortening of T1 Shortening of T2
Imaging PatternThe imaging patterns of HIE can be classified into 3 types Lesions predominantly located in the PVWM Lesions predominantly located in the basal ganglia or thalamus Multicystic encephalomalcia The pattern of injury is postulated to depend on bull The type of hypoxiandashischaemia (acute and profound or prolonged and partial) bullThe gestational age (term or pre-term)
HIE in preterm infantRisk FactorsPregnancy Gestational ageweight previous preterm birth spontaneous preterm labor Intrapartum Abruption pre-eclampsia premature rupture of membranes chorioamnionitis group B Strep Peri amp postnatal factors Respiratory distress sepsis anemia apnea bradycardia cardiac arrest
General Features++ PVL +- associated to Germinal matrix and IVH PV hemorrhagic infarction Cerebellar infarction Definition bullPVL is the HIE driven periventricular white matter (PVWM) necrosis seen in very low birth weight premies (lt1500g) EpidemiologybullBirth weight lt 1500 g 45 incidence of PVL (higher if associated with IVH) bullGestational age lt 33 weeks 38 incidence of PVL bullgt 50 of patients with PVL or grade III IVH develop cerebral palsy
Cranial ultrasound coronal view day 1 showing severe echogenicity in the white matter MRI (T2SE (TR 6284TE 120) and ADC) performed on day 3 showing increased signal intensity in the white matter on T2SE and low signal intensity in the deep white matter on the ADC map with sparing of the anterior periventricular white matter and asymmetrical distribution in the parieto-occipital white matter The child died and was subsequently diagnosed to have molybdenum cofactor deficiency
Cranial sonography in 5-day old term with HIE with increase in echogenicity of white matter consistent with edemaCD ultrasound shows reversal of diastolic flow reflecting increased vascular resistance secondary to edema
PVL in a preterm infant (a) Coronal head US image obtained in the 1st week of life shows increased echogenicity in the periventricular white matter (arrows) (b) Follow-up US image obtained 2 months later shows development of cystic changes in these regions and dilatation of the adjacent lateral ventricles findings that are consistent with PVL
CT images show decrease In basal ganglia density related to Cytotoxic edemaSubtle loss of the normally sharp Transition from grey matter to White matter at the corticomedullary Junction Cerebral edema seen with effacementof the cortical sulci and the sylvian Fissures
PVL in a preterm neonate Axial T1-weighted (a) and T2-weighted (b) MR images obtained on day 4 of life demonstrate T1 hypointensity and T2 hyperintensity in the periventricular whitematter Note the punctate foci of high signal intensity on the T1-weighted image (arrows in a) These foci should be distinguished from foci of hemorrhage whichwould demonstrate greater T2 shortening on the corresponding T2-weighted image
28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

MRI Diffusion show bilateral fronto parietal and parieto occipital cortical restricted diffusion Similar restricted diffusion in caudate nuclei Area of involvement corresponds to cortical as well as internal border zone infarcts Imaging wise Bilateral border infarcts
A Axial T2-weighted fast spin-echo image (3200851) with an echo train length of 8 obtained at 13 hours of life shows no abnormality B Trace LSDI image (15206251) with a b max of 750 secondsmm2 obtained at 13 hours of life shows no abnormality C Corresponding ADC map D Axial T2-weighted fast spin-echo image obtained at 5 days of life shows very subtle hyperintensity in the posterior putamen bilaterally (arrows) E Trace LSDI image obtained at 5 days of life shows decreased diffusion in corresponding areas (arrows) F Corresponding ADC map G T1-weighted axial spin-echo image (600202) obtained at 6 weeks of life shows hyperintensity within the posterior putamen and ventrolateral thalamus bilaterally (arrows)
The neonatal mean diffusion-weighted image (mDWI) shows an ischemic area in the middle cerebral artery territory which resulted in a cyst observed at 3 and 24 mo The neonatal Z map shows normal Z values in all regions At 3 mo low Z values representing abnormal fractional anisotropy (FA) values were observed in the affected corticospinal tract which corresponded with the subsequent development of unilateral motor deficits The Z map at 24 mo was essentially identical Interestingly FA values in the fornix continued to decrease from the time of the neonatal scan to 24 mo suggesting delayed degeneration in this tract
Restricted diffusion signal in the DCST Left middle cerebral artery infarction (A) results in DWI signal changes throughout the DCST PLIC and cerebral peduncle involvement are evident on coronal (B) and sagittal images (C) Signal in the basis pontis and medullary pyramids can be seen on left (D) but not right (E) parasagittal sections
Neonate with left middle cerebral artery stroke and chronic hemiparesis DWI signal is appreciated throughout the DCST including PLIC (A) peduncle (B C) pons (D E) and pontomedullary junction (F)
Axial diffusion weighted images from a neonate (A) with a modified pediatric ASPECTS of eight (involvement of left internal capsule insula M3 M5 M6 P1 P2 and thalamus) and a child (B) with a modified pediatric ASPECTS of 10 (involvement of left caudate lentiform internal capsule insula and middle cerebral artery territories M1ndashM6)
(A) Axial diffusion-weighted image showing hyperintensity in the territory of left middle cerebral artery (B) MR angiography demonstrates loss of flow distal to the left middle cerebral artery bifurcation
A B
Perinatal asphyxia more appropriately known as hypoxic-
ischemic encephalopathy (HIE) is characterized by clinical and laboratory evidence of acute or subacute brain injury due to asphyxia The primary causes of this condition are systemic hypoxemia andor reduced cerebral blood flow (CBF) Birth asphyxia causes 840000 or 23 of all neonatal deaths worldwideHIE- Acute brain injury that occur before during or after birth
Signs and symptomsMild hypoxic-ischemic encephalopathybullMuscle tone may be slightly increased and deep tendon reflexes may be brisk during the first few daysbullTransient behavioral abnormalities such as poor feeding irritability or excessive crying or sleepiness (typically in an alternating pattern) may be observed bullTypically resolves in 24h
Moderately severe hypoxic-ischemic encephalopathyThe infant is lethargic with significant hypotonia and diminished deep tendon reflexesThe grasping Moro and sucking reflexes may be sluggish or absentThe infant may experience occasional periods of apneaSeizures typically occur early within the first 24 hours after birthFull recovery within 1-2 weeks is possible and is associated with a better long-term outcome
Severe hypoxic-ischemic encephalopathySeizures can be delayed and severe and may be initially resistant to conventional treatments The seizures are usually generalized and their frequency may increase during the 24-48 hours after onset correlating with the phase of reperfusion injury As the injury progresses seizures subside and the electroencephalogram becomes isoelectric or shows a burst suppression pattern At that time wakefulness may deteriorate further and the fontanelle may bulge suggesting increasing cerebral edema
Other symptoms include the following Stupor or coma is typical the infant may not respond to any physical stimulus except the most noxiousBreathing may be irregular and the infant often requires ventilatory support Generalized hypotonia and depressed deep tendon reflexes are common Neonatal reflexes (eg sucking swallowing grasping Moro) are absent Disturbances of ocular motion such as a skewed deviation of the eyes nystagmus bobbing and loss of dolls eye (ie conjugate) movements may be revealed by cranial nerve examination Pupils may be dilated fixed or poorly reactive to lightIrregularities of heart rate and blood pressure are common during the period of reperfusion injury as is death from cardiorespiratory failure An initial period of well-being or mild hypoxic-ischemic encephalopathy may be followed by sudden deterioration suggesting ongoing brain cell dysfunction injury and death during this period seizure intensity may increase
Imaging of neonatal hypoxic-ischemic encephalopathy
Ultrasonography is the first-line imaging technique for the evaluation of the newborn brain These past few years have seen an increasing role of MRI in the investigation of HIE because of greater sensitivity and specificity Electro-encephalogram(EEG)Computed Tomography(CT)MRI MRS and DWI
MRI sequencesT1 WI T2 WI++ FLAIR are not very useful to detect lesion in young infant less than 24 months due to brain maturation IR T1-weighted Has been very helpful in the last two decades before generalization of high fields MRI as it gives excellent images of brain anatomy and maturation It also shows accurately the differentiation between myelinated and unmyelinated WM Three-dimensional GE T1 weighted sequence (3DT1) bullallow 1 mm contiguous slices which can be reconstructed in any anatomic plane T2 to detect hemorrhagic lesions DWI It is now recommended that DWI should be performed between 2 days and 8 days of life Multiple studies have shown DWI are more sensitive in the detection of HIE lesions than conventional MRI especially for early diagnosis
MRI ProtocolSagittal and axial T1 WI Axial and coronal T2 WI Axial T2 3D T1 FLAIR (older child) DWI MRSLactate peak bulldue to anaerobic glycolysis bullfound within 24 h of life Subsequently a reduction in N-acetyl aspartate (NAA) is evident due to neuronal loss
Advanced technique Perfusion
Arterial Spin-Labeled (ASL) Perfusion bullRecent advances in novel research imaging modalitybullallows noninvasive evaluation of CBF (cerebral blood flow) using electromagnetically labeled arterial blood water as an endogenous contrast agent bullDemonstrates low CBF in neonates who have suffered HIE and in infants and children after stroke
Imaging RecommendationCranial sonography (US) bullFirst between 7 and 14 days bullRepeat before discharge from the hospital MRI DWI MRS bullWhen US is abnormal MRI precise lesion extension and aide in prognosticating bull Defining injury in VLBW neonates with normal US
PrognosisPoor outcome if bullIVH plus PVL bullPVL with volume loss widespread infarction or seizures bullPVL with enlarged cysts
It is necessary to bullknow the normal cerebral appearance before interpret pathological aspect bulldistinguish hypoxic-ischemic brain damage from normal myelination Brain compositionChanges in brain composition Changes in cellular density increase in complex lipids content due to the evolving process of myelination decrease in water content mostly in the WM
Shortening of T1 Shortening of T2
Imaging PatternThe imaging patterns of HIE can be classified into 3 types Lesions predominantly located in the PVWM Lesions predominantly located in the basal ganglia or thalamus Multicystic encephalomalcia The pattern of injury is postulated to depend on bull The type of hypoxiandashischaemia (acute and profound or prolonged and partial) bullThe gestational age (term or pre-term)
HIE in preterm infantRisk FactorsPregnancy Gestational ageweight previous preterm birth spontaneous preterm labor Intrapartum Abruption pre-eclampsia premature rupture of membranes chorioamnionitis group B Strep Peri amp postnatal factors Respiratory distress sepsis anemia apnea bradycardia cardiac arrest
General Features++ PVL +- associated to Germinal matrix and IVH PV hemorrhagic infarction Cerebellar infarction Definition bullPVL is the HIE driven periventricular white matter (PVWM) necrosis seen in very low birth weight premies (lt1500g) EpidemiologybullBirth weight lt 1500 g 45 incidence of PVL (higher if associated with IVH) bullGestational age lt 33 weeks 38 incidence of PVL bullgt 50 of patients with PVL or grade III IVH develop cerebral palsy
Cranial ultrasound coronal view day 1 showing severe echogenicity in the white matter MRI (T2SE (TR 6284TE 120) and ADC) performed on day 3 showing increased signal intensity in the white matter on T2SE and low signal intensity in the deep white matter on the ADC map with sparing of the anterior periventricular white matter and asymmetrical distribution in the parieto-occipital white matter The child died and was subsequently diagnosed to have molybdenum cofactor deficiency
Cranial sonography in 5-day old term with HIE with increase in echogenicity of white matter consistent with edemaCD ultrasound shows reversal of diastolic flow reflecting increased vascular resistance secondary to edema
PVL in a preterm infant (a) Coronal head US image obtained in the 1st week of life shows increased echogenicity in the periventricular white matter (arrows) (b) Follow-up US image obtained 2 months later shows development of cystic changes in these regions and dilatation of the adjacent lateral ventricles findings that are consistent with PVL
CT images show decrease In basal ganglia density related to Cytotoxic edemaSubtle loss of the normally sharp Transition from grey matter to White matter at the corticomedullary Junction Cerebral edema seen with effacementof the cortical sulci and the sylvian Fissures
PVL in a preterm neonate Axial T1-weighted (a) and T2-weighted (b) MR images obtained on day 4 of life demonstrate T1 hypointensity and T2 hyperintensity in the periventricular whitematter Note the punctate foci of high signal intensity on the T1-weighted image (arrows in a) These foci should be distinguished from foci of hemorrhage whichwould demonstrate greater T2 shortening on the corresponding T2-weighted image
28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

A Axial T2-weighted fast spin-echo image (3200851) with an echo train length of 8 obtained at 13 hours of life shows no abnormality B Trace LSDI image (15206251) with a b max of 750 secondsmm2 obtained at 13 hours of life shows no abnormality C Corresponding ADC map D Axial T2-weighted fast spin-echo image obtained at 5 days of life shows very subtle hyperintensity in the posterior putamen bilaterally (arrows) E Trace LSDI image obtained at 5 days of life shows decreased diffusion in corresponding areas (arrows) F Corresponding ADC map G T1-weighted axial spin-echo image (600202) obtained at 6 weeks of life shows hyperintensity within the posterior putamen and ventrolateral thalamus bilaterally (arrows)
The neonatal mean diffusion-weighted image (mDWI) shows an ischemic area in the middle cerebral artery territory which resulted in a cyst observed at 3 and 24 mo The neonatal Z map shows normal Z values in all regions At 3 mo low Z values representing abnormal fractional anisotropy (FA) values were observed in the affected corticospinal tract which corresponded with the subsequent development of unilateral motor deficits The Z map at 24 mo was essentially identical Interestingly FA values in the fornix continued to decrease from the time of the neonatal scan to 24 mo suggesting delayed degeneration in this tract
Restricted diffusion signal in the DCST Left middle cerebral artery infarction (A) results in DWI signal changes throughout the DCST PLIC and cerebral peduncle involvement are evident on coronal (B) and sagittal images (C) Signal in the basis pontis and medullary pyramids can be seen on left (D) but not right (E) parasagittal sections
Neonate with left middle cerebral artery stroke and chronic hemiparesis DWI signal is appreciated throughout the DCST including PLIC (A) peduncle (B C) pons (D E) and pontomedullary junction (F)
Axial diffusion weighted images from a neonate (A) with a modified pediatric ASPECTS of eight (involvement of left internal capsule insula M3 M5 M6 P1 P2 and thalamus) and a child (B) with a modified pediatric ASPECTS of 10 (involvement of left caudate lentiform internal capsule insula and middle cerebral artery territories M1ndashM6)
(A) Axial diffusion-weighted image showing hyperintensity in the territory of left middle cerebral artery (B) MR angiography demonstrates loss of flow distal to the left middle cerebral artery bifurcation
A B
Perinatal asphyxia more appropriately known as hypoxic-
ischemic encephalopathy (HIE) is characterized by clinical and laboratory evidence of acute or subacute brain injury due to asphyxia The primary causes of this condition are systemic hypoxemia andor reduced cerebral blood flow (CBF) Birth asphyxia causes 840000 or 23 of all neonatal deaths worldwideHIE- Acute brain injury that occur before during or after birth
Signs and symptomsMild hypoxic-ischemic encephalopathybullMuscle tone may be slightly increased and deep tendon reflexes may be brisk during the first few daysbullTransient behavioral abnormalities such as poor feeding irritability or excessive crying or sleepiness (typically in an alternating pattern) may be observed bullTypically resolves in 24h
Moderately severe hypoxic-ischemic encephalopathyThe infant is lethargic with significant hypotonia and diminished deep tendon reflexesThe grasping Moro and sucking reflexes may be sluggish or absentThe infant may experience occasional periods of apneaSeizures typically occur early within the first 24 hours after birthFull recovery within 1-2 weeks is possible and is associated with a better long-term outcome
Severe hypoxic-ischemic encephalopathySeizures can be delayed and severe and may be initially resistant to conventional treatments The seizures are usually generalized and their frequency may increase during the 24-48 hours after onset correlating with the phase of reperfusion injury As the injury progresses seizures subside and the electroencephalogram becomes isoelectric or shows a burst suppression pattern At that time wakefulness may deteriorate further and the fontanelle may bulge suggesting increasing cerebral edema
Other symptoms include the following Stupor or coma is typical the infant may not respond to any physical stimulus except the most noxiousBreathing may be irregular and the infant often requires ventilatory support Generalized hypotonia and depressed deep tendon reflexes are common Neonatal reflexes (eg sucking swallowing grasping Moro) are absent Disturbances of ocular motion such as a skewed deviation of the eyes nystagmus bobbing and loss of dolls eye (ie conjugate) movements may be revealed by cranial nerve examination Pupils may be dilated fixed or poorly reactive to lightIrregularities of heart rate and blood pressure are common during the period of reperfusion injury as is death from cardiorespiratory failure An initial period of well-being or mild hypoxic-ischemic encephalopathy may be followed by sudden deterioration suggesting ongoing brain cell dysfunction injury and death during this period seizure intensity may increase
Imaging of neonatal hypoxic-ischemic encephalopathy
Ultrasonography is the first-line imaging technique for the evaluation of the newborn brain These past few years have seen an increasing role of MRI in the investigation of HIE because of greater sensitivity and specificity Electro-encephalogram(EEG)Computed Tomography(CT)MRI MRS and DWI
MRI sequencesT1 WI T2 WI++ FLAIR are not very useful to detect lesion in young infant less than 24 months due to brain maturation IR T1-weighted Has been very helpful in the last two decades before generalization of high fields MRI as it gives excellent images of brain anatomy and maturation It also shows accurately the differentiation between myelinated and unmyelinated WM Three-dimensional GE T1 weighted sequence (3DT1) bullallow 1 mm contiguous slices which can be reconstructed in any anatomic plane T2 to detect hemorrhagic lesions DWI It is now recommended that DWI should be performed between 2 days and 8 days of life Multiple studies have shown DWI are more sensitive in the detection of HIE lesions than conventional MRI especially for early diagnosis
MRI ProtocolSagittal and axial T1 WI Axial and coronal T2 WI Axial T2 3D T1 FLAIR (older child) DWI MRSLactate peak bulldue to anaerobic glycolysis bullfound within 24 h of life Subsequently a reduction in N-acetyl aspartate (NAA) is evident due to neuronal loss
Advanced technique Perfusion
Arterial Spin-Labeled (ASL) Perfusion bullRecent advances in novel research imaging modalitybullallows noninvasive evaluation of CBF (cerebral blood flow) using electromagnetically labeled arterial blood water as an endogenous contrast agent bullDemonstrates low CBF in neonates who have suffered HIE and in infants and children after stroke
Imaging RecommendationCranial sonography (US) bullFirst between 7 and 14 days bullRepeat before discharge from the hospital MRI DWI MRS bullWhen US is abnormal MRI precise lesion extension and aide in prognosticating bull Defining injury in VLBW neonates with normal US
PrognosisPoor outcome if bullIVH plus PVL bullPVL with volume loss widespread infarction or seizures bullPVL with enlarged cysts
It is necessary to bullknow the normal cerebral appearance before interpret pathological aspect bulldistinguish hypoxic-ischemic brain damage from normal myelination Brain compositionChanges in brain composition Changes in cellular density increase in complex lipids content due to the evolving process of myelination decrease in water content mostly in the WM
Shortening of T1 Shortening of T2
Imaging PatternThe imaging patterns of HIE can be classified into 3 types Lesions predominantly located in the PVWM Lesions predominantly located in the basal ganglia or thalamus Multicystic encephalomalcia The pattern of injury is postulated to depend on bull The type of hypoxiandashischaemia (acute and profound or prolonged and partial) bullThe gestational age (term or pre-term)
HIE in preterm infantRisk FactorsPregnancy Gestational ageweight previous preterm birth spontaneous preterm labor Intrapartum Abruption pre-eclampsia premature rupture of membranes chorioamnionitis group B Strep Peri amp postnatal factors Respiratory distress sepsis anemia apnea bradycardia cardiac arrest
General Features++ PVL +- associated to Germinal matrix and IVH PV hemorrhagic infarction Cerebellar infarction Definition bullPVL is the HIE driven periventricular white matter (PVWM) necrosis seen in very low birth weight premies (lt1500g) EpidemiologybullBirth weight lt 1500 g 45 incidence of PVL (higher if associated with IVH) bullGestational age lt 33 weeks 38 incidence of PVL bullgt 50 of patients with PVL or grade III IVH develop cerebral palsy
Cranial ultrasound coronal view day 1 showing severe echogenicity in the white matter MRI (T2SE (TR 6284TE 120) and ADC) performed on day 3 showing increased signal intensity in the white matter on T2SE and low signal intensity in the deep white matter on the ADC map with sparing of the anterior periventricular white matter and asymmetrical distribution in the parieto-occipital white matter The child died and was subsequently diagnosed to have molybdenum cofactor deficiency
Cranial sonography in 5-day old term with HIE with increase in echogenicity of white matter consistent with edemaCD ultrasound shows reversal of diastolic flow reflecting increased vascular resistance secondary to edema
PVL in a preterm infant (a) Coronal head US image obtained in the 1st week of life shows increased echogenicity in the periventricular white matter (arrows) (b) Follow-up US image obtained 2 months later shows development of cystic changes in these regions and dilatation of the adjacent lateral ventricles findings that are consistent with PVL
CT images show decrease In basal ganglia density related to Cytotoxic edemaSubtle loss of the normally sharp Transition from grey matter to White matter at the corticomedullary Junction Cerebral edema seen with effacementof the cortical sulci and the sylvian Fissures
PVL in a preterm neonate Axial T1-weighted (a) and T2-weighted (b) MR images obtained on day 4 of life demonstrate T1 hypointensity and T2 hyperintensity in the periventricular whitematter Note the punctate foci of high signal intensity on the T1-weighted image (arrows in a) These foci should be distinguished from foci of hemorrhage whichwould demonstrate greater T2 shortening on the corresponding T2-weighted image
28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

The neonatal mean diffusion-weighted image (mDWI) shows an ischemic area in the middle cerebral artery territory which resulted in a cyst observed at 3 and 24 mo The neonatal Z map shows normal Z values in all regions At 3 mo low Z values representing abnormal fractional anisotropy (FA) values were observed in the affected corticospinal tract which corresponded with the subsequent development of unilateral motor deficits The Z map at 24 mo was essentially identical Interestingly FA values in the fornix continued to decrease from the time of the neonatal scan to 24 mo suggesting delayed degeneration in this tract
Restricted diffusion signal in the DCST Left middle cerebral artery infarction (A) results in DWI signal changes throughout the DCST PLIC and cerebral peduncle involvement are evident on coronal (B) and sagittal images (C) Signal in the basis pontis and medullary pyramids can be seen on left (D) but not right (E) parasagittal sections
Neonate with left middle cerebral artery stroke and chronic hemiparesis DWI signal is appreciated throughout the DCST including PLIC (A) peduncle (B C) pons (D E) and pontomedullary junction (F)
Axial diffusion weighted images from a neonate (A) with a modified pediatric ASPECTS of eight (involvement of left internal capsule insula M3 M5 M6 P1 P2 and thalamus) and a child (B) with a modified pediatric ASPECTS of 10 (involvement of left caudate lentiform internal capsule insula and middle cerebral artery territories M1ndashM6)
(A) Axial diffusion-weighted image showing hyperintensity in the territory of left middle cerebral artery (B) MR angiography demonstrates loss of flow distal to the left middle cerebral artery bifurcation
A B
Perinatal asphyxia more appropriately known as hypoxic-
ischemic encephalopathy (HIE) is characterized by clinical and laboratory evidence of acute or subacute brain injury due to asphyxia The primary causes of this condition are systemic hypoxemia andor reduced cerebral blood flow (CBF) Birth asphyxia causes 840000 or 23 of all neonatal deaths worldwideHIE- Acute brain injury that occur before during or after birth
Signs and symptomsMild hypoxic-ischemic encephalopathybullMuscle tone may be slightly increased and deep tendon reflexes may be brisk during the first few daysbullTransient behavioral abnormalities such as poor feeding irritability or excessive crying or sleepiness (typically in an alternating pattern) may be observed bullTypically resolves in 24h
Moderately severe hypoxic-ischemic encephalopathyThe infant is lethargic with significant hypotonia and diminished deep tendon reflexesThe grasping Moro and sucking reflexes may be sluggish or absentThe infant may experience occasional periods of apneaSeizures typically occur early within the first 24 hours after birthFull recovery within 1-2 weeks is possible and is associated with a better long-term outcome
Severe hypoxic-ischemic encephalopathySeizures can be delayed and severe and may be initially resistant to conventional treatments The seizures are usually generalized and their frequency may increase during the 24-48 hours after onset correlating with the phase of reperfusion injury As the injury progresses seizures subside and the electroencephalogram becomes isoelectric or shows a burst suppression pattern At that time wakefulness may deteriorate further and the fontanelle may bulge suggesting increasing cerebral edema
Other symptoms include the following Stupor or coma is typical the infant may not respond to any physical stimulus except the most noxiousBreathing may be irregular and the infant often requires ventilatory support Generalized hypotonia and depressed deep tendon reflexes are common Neonatal reflexes (eg sucking swallowing grasping Moro) are absent Disturbances of ocular motion such as a skewed deviation of the eyes nystagmus bobbing and loss of dolls eye (ie conjugate) movements may be revealed by cranial nerve examination Pupils may be dilated fixed or poorly reactive to lightIrregularities of heart rate and blood pressure are common during the period of reperfusion injury as is death from cardiorespiratory failure An initial period of well-being or mild hypoxic-ischemic encephalopathy may be followed by sudden deterioration suggesting ongoing brain cell dysfunction injury and death during this period seizure intensity may increase
Imaging of neonatal hypoxic-ischemic encephalopathy
Ultrasonography is the first-line imaging technique for the evaluation of the newborn brain These past few years have seen an increasing role of MRI in the investigation of HIE because of greater sensitivity and specificity Electro-encephalogram(EEG)Computed Tomography(CT)MRI MRS and DWI
MRI sequencesT1 WI T2 WI++ FLAIR are not very useful to detect lesion in young infant less than 24 months due to brain maturation IR T1-weighted Has been very helpful in the last two decades before generalization of high fields MRI as it gives excellent images of brain anatomy and maturation It also shows accurately the differentiation between myelinated and unmyelinated WM Three-dimensional GE T1 weighted sequence (3DT1) bullallow 1 mm contiguous slices which can be reconstructed in any anatomic plane T2 to detect hemorrhagic lesions DWI It is now recommended that DWI should be performed between 2 days and 8 days of life Multiple studies have shown DWI are more sensitive in the detection of HIE lesions than conventional MRI especially for early diagnosis
MRI ProtocolSagittal and axial T1 WI Axial and coronal T2 WI Axial T2 3D T1 FLAIR (older child) DWI MRSLactate peak bulldue to anaerobic glycolysis bullfound within 24 h of life Subsequently a reduction in N-acetyl aspartate (NAA) is evident due to neuronal loss
Advanced technique Perfusion
Arterial Spin-Labeled (ASL) Perfusion bullRecent advances in novel research imaging modalitybullallows noninvasive evaluation of CBF (cerebral blood flow) using electromagnetically labeled arterial blood water as an endogenous contrast agent bullDemonstrates low CBF in neonates who have suffered HIE and in infants and children after stroke
Imaging RecommendationCranial sonography (US) bullFirst between 7 and 14 days bullRepeat before discharge from the hospital MRI DWI MRS bullWhen US is abnormal MRI precise lesion extension and aide in prognosticating bull Defining injury in VLBW neonates with normal US
PrognosisPoor outcome if bullIVH plus PVL bullPVL with volume loss widespread infarction or seizures bullPVL with enlarged cysts
It is necessary to bullknow the normal cerebral appearance before interpret pathological aspect bulldistinguish hypoxic-ischemic brain damage from normal myelination Brain compositionChanges in brain composition Changes in cellular density increase in complex lipids content due to the evolving process of myelination decrease in water content mostly in the WM
Shortening of T1 Shortening of T2
Imaging PatternThe imaging patterns of HIE can be classified into 3 types Lesions predominantly located in the PVWM Lesions predominantly located in the basal ganglia or thalamus Multicystic encephalomalcia The pattern of injury is postulated to depend on bull The type of hypoxiandashischaemia (acute and profound or prolonged and partial) bullThe gestational age (term or pre-term)
HIE in preterm infantRisk FactorsPregnancy Gestational ageweight previous preterm birth spontaneous preterm labor Intrapartum Abruption pre-eclampsia premature rupture of membranes chorioamnionitis group B Strep Peri amp postnatal factors Respiratory distress sepsis anemia apnea bradycardia cardiac arrest
General Features++ PVL +- associated to Germinal matrix and IVH PV hemorrhagic infarction Cerebellar infarction Definition bullPVL is the HIE driven periventricular white matter (PVWM) necrosis seen in very low birth weight premies (lt1500g) EpidemiologybullBirth weight lt 1500 g 45 incidence of PVL (higher if associated with IVH) bullGestational age lt 33 weeks 38 incidence of PVL bullgt 50 of patients with PVL or grade III IVH develop cerebral palsy
Cranial ultrasound coronal view day 1 showing severe echogenicity in the white matter MRI (T2SE (TR 6284TE 120) and ADC) performed on day 3 showing increased signal intensity in the white matter on T2SE and low signal intensity in the deep white matter on the ADC map with sparing of the anterior periventricular white matter and asymmetrical distribution in the parieto-occipital white matter The child died and was subsequently diagnosed to have molybdenum cofactor deficiency
Cranial sonography in 5-day old term with HIE with increase in echogenicity of white matter consistent with edemaCD ultrasound shows reversal of diastolic flow reflecting increased vascular resistance secondary to edema
PVL in a preterm infant (a) Coronal head US image obtained in the 1st week of life shows increased echogenicity in the periventricular white matter (arrows) (b) Follow-up US image obtained 2 months later shows development of cystic changes in these regions and dilatation of the adjacent lateral ventricles findings that are consistent with PVL
CT images show decrease In basal ganglia density related to Cytotoxic edemaSubtle loss of the normally sharp Transition from grey matter to White matter at the corticomedullary Junction Cerebral edema seen with effacementof the cortical sulci and the sylvian Fissures
PVL in a preterm neonate Axial T1-weighted (a) and T2-weighted (b) MR images obtained on day 4 of life demonstrate T1 hypointensity and T2 hyperintensity in the periventricular whitematter Note the punctate foci of high signal intensity on the T1-weighted image (arrows in a) These foci should be distinguished from foci of hemorrhage whichwould demonstrate greater T2 shortening on the corresponding T2-weighted image
28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

Restricted diffusion signal in the DCST Left middle cerebral artery infarction (A) results in DWI signal changes throughout the DCST PLIC and cerebral peduncle involvement are evident on coronal (B) and sagittal images (C) Signal in the basis pontis and medullary pyramids can be seen on left (D) but not right (E) parasagittal sections
Neonate with left middle cerebral artery stroke and chronic hemiparesis DWI signal is appreciated throughout the DCST including PLIC (A) peduncle (B C) pons (D E) and pontomedullary junction (F)
Axial diffusion weighted images from a neonate (A) with a modified pediatric ASPECTS of eight (involvement of left internal capsule insula M3 M5 M6 P1 P2 and thalamus) and a child (B) with a modified pediatric ASPECTS of 10 (involvement of left caudate lentiform internal capsule insula and middle cerebral artery territories M1ndashM6)
(A) Axial diffusion-weighted image showing hyperintensity in the territory of left middle cerebral artery (B) MR angiography demonstrates loss of flow distal to the left middle cerebral artery bifurcation
A B
Perinatal asphyxia more appropriately known as hypoxic-
ischemic encephalopathy (HIE) is characterized by clinical and laboratory evidence of acute or subacute brain injury due to asphyxia The primary causes of this condition are systemic hypoxemia andor reduced cerebral blood flow (CBF) Birth asphyxia causes 840000 or 23 of all neonatal deaths worldwideHIE- Acute brain injury that occur before during or after birth
Signs and symptomsMild hypoxic-ischemic encephalopathybullMuscle tone may be slightly increased and deep tendon reflexes may be brisk during the first few daysbullTransient behavioral abnormalities such as poor feeding irritability or excessive crying or sleepiness (typically in an alternating pattern) may be observed bullTypically resolves in 24h
Moderately severe hypoxic-ischemic encephalopathyThe infant is lethargic with significant hypotonia and diminished deep tendon reflexesThe grasping Moro and sucking reflexes may be sluggish or absentThe infant may experience occasional periods of apneaSeizures typically occur early within the first 24 hours after birthFull recovery within 1-2 weeks is possible and is associated with a better long-term outcome
Severe hypoxic-ischemic encephalopathySeizures can be delayed and severe and may be initially resistant to conventional treatments The seizures are usually generalized and their frequency may increase during the 24-48 hours after onset correlating with the phase of reperfusion injury As the injury progresses seizures subside and the electroencephalogram becomes isoelectric or shows a burst suppression pattern At that time wakefulness may deteriorate further and the fontanelle may bulge suggesting increasing cerebral edema
Other symptoms include the following Stupor or coma is typical the infant may not respond to any physical stimulus except the most noxiousBreathing may be irregular and the infant often requires ventilatory support Generalized hypotonia and depressed deep tendon reflexes are common Neonatal reflexes (eg sucking swallowing grasping Moro) are absent Disturbances of ocular motion such as a skewed deviation of the eyes nystagmus bobbing and loss of dolls eye (ie conjugate) movements may be revealed by cranial nerve examination Pupils may be dilated fixed or poorly reactive to lightIrregularities of heart rate and blood pressure are common during the period of reperfusion injury as is death from cardiorespiratory failure An initial period of well-being or mild hypoxic-ischemic encephalopathy may be followed by sudden deterioration suggesting ongoing brain cell dysfunction injury and death during this period seizure intensity may increase
Imaging of neonatal hypoxic-ischemic encephalopathy
Ultrasonography is the first-line imaging technique for the evaluation of the newborn brain These past few years have seen an increasing role of MRI in the investigation of HIE because of greater sensitivity and specificity Electro-encephalogram(EEG)Computed Tomography(CT)MRI MRS and DWI
MRI sequencesT1 WI T2 WI++ FLAIR are not very useful to detect lesion in young infant less than 24 months due to brain maturation IR T1-weighted Has been very helpful in the last two decades before generalization of high fields MRI as it gives excellent images of brain anatomy and maturation It also shows accurately the differentiation between myelinated and unmyelinated WM Three-dimensional GE T1 weighted sequence (3DT1) bullallow 1 mm contiguous slices which can be reconstructed in any anatomic plane T2 to detect hemorrhagic lesions DWI It is now recommended that DWI should be performed between 2 days and 8 days of life Multiple studies have shown DWI are more sensitive in the detection of HIE lesions than conventional MRI especially for early diagnosis
MRI ProtocolSagittal and axial T1 WI Axial and coronal T2 WI Axial T2 3D T1 FLAIR (older child) DWI MRSLactate peak bulldue to anaerobic glycolysis bullfound within 24 h of life Subsequently a reduction in N-acetyl aspartate (NAA) is evident due to neuronal loss
Advanced technique Perfusion
Arterial Spin-Labeled (ASL) Perfusion bullRecent advances in novel research imaging modalitybullallows noninvasive evaluation of CBF (cerebral blood flow) using electromagnetically labeled arterial blood water as an endogenous contrast agent bullDemonstrates low CBF in neonates who have suffered HIE and in infants and children after stroke
Imaging RecommendationCranial sonography (US) bullFirst between 7 and 14 days bullRepeat before discharge from the hospital MRI DWI MRS bullWhen US is abnormal MRI precise lesion extension and aide in prognosticating bull Defining injury in VLBW neonates with normal US
PrognosisPoor outcome if bullIVH plus PVL bullPVL with volume loss widespread infarction or seizures bullPVL with enlarged cysts
It is necessary to bullknow the normal cerebral appearance before interpret pathological aspect bulldistinguish hypoxic-ischemic brain damage from normal myelination Brain compositionChanges in brain composition Changes in cellular density increase in complex lipids content due to the evolving process of myelination decrease in water content mostly in the WM
Shortening of T1 Shortening of T2
Imaging PatternThe imaging patterns of HIE can be classified into 3 types Lesions predominantly located in the PVWM Lesions predominantly located in the basal ganglia or thalamus Multicystic encephalomalcia The pattern of injury is postulated to depend on bull The type of hypoxiandashischaemia (acute and profound or prolonged and partial) bullThe gestational age (term or pre-term)
HIE in preterm infantRisk FactorsPregnancy Gestational ageweight previous preterm birth spontaneous preterm labor Intrapartum Abruption pre-eclampsia premature rupture of membranes chorioamnionitis group B Strep Peri amp postnatal factors Respiratory distress sepsis anemia apnea bradycardia cardiac arrest
General Features++ PVL +- associated to Germinal matrix and IVH PV hemorrhagic infarction Cerebellar infarction Definition bullPVL is the HIE driven periventricular white matter (PVWM) necrosis seen in very low birth weight premies (lt1500g) EpidemiologybullBirth weight lt 1500 g 45 incidence of PVL (higher if associated with IVH) bullGestational age lt 33 weeks 38 incidence of PVL bullgt 50 of patients with PVL or grade III IVH develop cerebral palsy
Cranial ultrasound coronal view day 1 showing severe echogenicity in the white matter MRI (T2SE (TR 6284TE 120) and ADC) performed on day 3 showing increased signal intensity in the white matter on T2SE and low signal intensity in the deep white matter on the ADC map with sparing of the anterior periventricular white matter and asymmetrical distribution in the parieto-occipital white matter The child died and was subsequently diagnosed to have molybdenum cofactor deficiency
Cranial sonography in 5-day old term with HIE with increase in echogenicity of white matter consistent with edemaCD ultrasound shows reversal of diastolic flow reflecting increased vascular resistance secondary to edema
PVL in a preterm infant (a) Coronal head US image obtained in the 1st week of life shows increased echogenicity in the periventricular white matter (arrows) (b) Follow-up US image obtained 2 months later shows development of cystic changes in these regions and dilatation of the adjacent lateral ventricles findings that are consistent with PVL
CT images show decrease In basal ganglia density related to Cytotoxic edemaSubtle loss of the normally sharp Transition from grey matter to White matter at the corticomedullary Junction Cerebral edema seen with effacementof the cortical sulci and the sylvian Fissures
PVL in a preterm neonate Axial T1-weighted (a) and T2-weighted (b) MR images obtained on day 4 of life demonstrate T1 hypointensity and T2 hyperintensity in the periventricular whitematter Note the punctate foci of high signal intensity on the T1-weighted image (arrows in a) These foci should be distinguished from foci of hemorrhage whichwould demonstrate greater T2 shortening on the corresponding T2-weighted image
28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

Neonate with left middle cerebral artery stroke and chronic hemiparesis DWI signal is appreciated throughout the DCST including PLIC (A) peduncle (B C) pons (D E) and pontomedullary junction (F)
Axial diffusion weighted images from a neonate (A) with a modified pediatric ASPECTS of eight (involvement of left internal capsule insula M3 M5 M6 P1 P2 and thalamus) and a child (B) with a modified pediatric ASPECTS of 10 (involvement of left caudate lentiform internal capsule insula and middle cerebral artery territories M1ndashM6)
(A) Axial diffusion-weighted image showing hyperintensity in the territory of left middle cerebral artery (B) MR angiography demonstrates loss of flow distal to the left middle cerebral artery bifurcation
A B
Perinatal asphyxia more appropriately known as hypoxic-
ischemic encephalopathy (HIE) is characterized by clinical and laboratory evidence of acute or subacute brain injury due to asphyxia The primary causes of this condition are systemic hypoxemia andor reduced cerebral blood flow (CBF) Birth asphyxia causes 840000 or 23 of all neonatal deaths worldwideHIE- Acute brain injury that occur before during or after birth
Signs and symptomsMild hypoxic-ischemic encephalopathybullMuscle tone may be slightly increased and deep tendon reflexes may be brisk during the first few daysbullTransient behavioral abnormalities such as poor feeding irritability or excessive crying or sleepiness (typically in an alternating pattern) may be observed bullTypically resolves in 24h
Moderately severe hypoxic-ischemic encephalopathyThe infant is lethargic with significant hypotonia and diminished deep tendon reflexesThe grasping Moro and sucking reflexes may be sluggish or absentThe infant may experience occasional periods of apneaSeizures typically occur early within the first 24 hours after birthFull recovery within 1-2 weeks is possible and is associated with a better long-term outcome
Severe hypoxic-ischemic encephalopathySeizures can be delayed and severe and may be initially resistant to conventional treatments The seizures are usually generalized and their frequency may increase during the 24-48 hours after onset correlating with the phase of reperfusion injury As the injury progresses seizures subside and the electroencephalogram becomes isoelectric or shows a burst suppression pattern At that time wakefulness may deteriorate further and the fontanelle may bulge suggesting increasing cerebral edema
Other symptoms include the following Stupor or coma is typical the infant may not respond to any physical stimulus except the most noxiousBreathing may be irregular and the infant often requires ventilatory support Generalized hypotonia and depressed deep tendon reflexes are common Neonatal reflexes (eg sucking swallowing grasping Moro) are absent Disturbances of ocular motion such as a skewed deviation of the eyes nystagmus bobbing and loss of dolls eye (ie conjugate) movements may be revealed by cranial nerve examination Pupils may be dilated fixed or poorly reactive to lightIrregularities of heart rate and blood pressure are common during the period of reperfusion injury as is death from cardiorespiratory failure An initial period of well-being or mild hypoxic-ischemic encephalopathy may be followed by sudden deterioration suggesting ongoing brain cell dysfunction injury and death during this period seizure intensity may increase
Imaging of neonatal hypoxic-ischemic encephalopathy
Ultrasonography is the first-line imaging technique for the evaluation of the newborn brain These past few years have seen an increasing role of MRI in the investigation of HIE because of greater sensitivity and specificity Electro-encephalogram(EEG)Computed Tomography(CT)MRI MRS and DWI
MRI sequencesT1 WI T2 WI++ FLAIR are not very useful to detect lesion in young infant less than 24 months due to brain maturation IR T1-weighted Has been very helpful in the last two decades before generalization of high fields MRI as it gives excellent images of brain anatomy and maturation It also shows accurately the differentiation between myelinated and unmyelinated WM Three-dimensional GE T1 weighted sequence (3DT1) bullallow 1 mm contiguous slices which can be reconstructed in any anatomic plane T2 to detect hemorrhagic lesions DWI It is now recommended that DWI should be performed between 2 days and 8 days of life Multiple studies have shown DWI are more sensitive in the detection of HIE lesions than conventional MRI especially for early diagnosis
MRI ProtocolSagittal and axial T1 WI Axial and coronal T2 WI Axial T2 3D T1 FLAIR (older child) DWI MRSLactate peak bulldue to anaerobic glycolysis bullfound within 24 h of life Subsequently a reduction in N-acetyl aspartate (NAA) is evident due to neuronal loss
Advanced technique Perfusion
Arterial Spin-Labeled (ASL) Perfusion bullRecent advances in novel research imaging modalitybullallows noninvasive evaluation of CBF (cerebral blood flow) using electromagnetically labeled arterial blood water as an endogenous contrast agent bullDemonstrates low CBF in neonates who have suffered HIE and in infants and children after stroke
Imaging RecommendationCranial sonography (US) bullFirst between 7 and 14 days bullRepeat before discharge from the hospital MRI DWI MRS bullWhen US is abnormal MRI precise lesion extension and aide in prognosticating bull Defining injury in VLBW neonates with normal US
PrognosisPoor outcome if bullIVH plus PVL bullPVL with volume loss widespread infarction or seizures bullPVL with enlarged cysts
It is necessary to bullknow the normal cerebral appearance before interpret pathological aspect bulldistinguish hypoxic-ischemic brain damage from normal myelination Brain compositionChanges in brain composition Changes in cellular density increase in complex lipids content due to the evolving process of myelination decrease in water content mostly in the WM
Shortening of T1 Shortening of T2
Imaging PatternThe imaging patterns of HIE can be classified into 3 types Lesions predominantly located in the PVWM Lesions predominantly located in the basal ganglia or thalamus Multicystic encephalomalcia The pattern of injury is postulated to depend on bull The type of hypoxiandashischaemia (acute and profound or prolonged and partial) bullThe gestational age (term or pre-term)
HIE in preterm infantRisk FactorsPregnancy Gestational ageweight previous preterm birth spontaneous preterm labor Intrapartum Abruption pre-eclampsia premature rupture of membranes chorioamnionitis group B Strep Peri amp postnatal factors Respiratory distress sepsis anemia apnea bradycardia cardiac arrest
General Features++ PVL +- associated to Germinal matrix and IVH PV hemorrhagic infarction Cerebellar infarction Definition bullPVL is the HIE driven periventricular white matter (PVWM) necrosis seen in very low birth weight premies (lt1500g) EpidemiologybullBirth weight lt 1500 g 45 incidence of PVL (higher if associated with IVH) bullGestational age lt 33 weeks 38 incidence of PVL bullgt 50 of patients with PVL or grade III IVH develop cerebral palsy
Cranial ultrasound coronal view day 1 showing severe echogenicity in the white matter MRI (T2SE (TR 6284TE 120) and ADC) performed on day 3 showing increased signal intensity in the white matter on T2SE and low signal intensity in the deep white matter on the ADC map with sparing of the anterior periventricular white matter and asymmetrical distribution in the parieto-occipital white matter The child died and was subsequently diagnosed to have molybdenum cofactor deficiency
Cranial sonography in 5-day old term with HIE with increase in echogenicity of white matter consistent with edemaCD ultrasound shows reversal of diastolic flow reflecting increased vascular resistance secondary to edema
PVL in a preterm infant (a) Coronal head US image obtained in the 1st week of life shows increased echogenicity in the periventricular white matter (arrows) (b) Follow-up US image obtained 2 months later shows development of cystic changes in these regions and dilatation of the adjacent lateral ventricles findings that are consistent with PVL
CT images show decrease In basal ganglia density related to Cytotoxic edemaSubtle loss of the normally sharp Transition from grey matter to White matter at the corticomedullary Junction Cerebral edema seen with effacementof the cortical sulci and the sylvian Fissures
PVL in a preterm neonate Axial T1-weighted (a) and T2-weighted (b) MR images obtained on day 4 of life demonstrate T1 hypointensity and T2 hyperintensity in the periventricular whitematter Note the punctate foci of high signal intensity on the T1-weighted image (arrows in a) These foci should be distinguished from foci of hemorrhage whichwould demonstrate greater T2 shortening on the corresponding T2-weighted image
28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

Axial diffusion weighted images from a neonate (A) with a modified pediatric ASPECTS of eight (involvement of left internal capsule insula M3 M5 M6 P1 P2 and thalamus) and a child (B) with a modified pediatric ASPECTS of 10 (involvement of left caudate lentiform internal capsule insula and middle cerebral artery territories M1ndashM6)
(A) Axial diffusion-weighted image showing hyperintensity in the territory of left middle cerebral artery (B) MR angiography demonstrates loss of flow distal to the left middle cerebral artery bifurcation
A B
Perinatal asphyxia more appropriately known as hypoxic-
ischemic encephalopathy (HIE) is characterized by clinical and laboratory evidence of acute or subacute brain injury due to asphyxia The primary causes of this condition are systemic hypoxemia andor reduced cerebral blood flow (CBF) Birth asphyxia causes 840000 or 23 of all neonatal deaths worldwideHIE- Acute brain injury that occur before during or after birth
Signs and symptomsMild hypoxic-ischemic encephalopathybullMuscle tone may be slightly increased and deep tendon reflexes may be brisk during the first few daysbullTransient behavioral abnormalities such as poor feeding irritability or excessive crying or sleepiness (typically in an alternating pattern) may be observed bullTypically resolves in 24h
Moderately severe hypoxic-ischemic encephalopathyThe infant is lethargic with significant hypotonia and diminished deep tendon reflexesThe grasping Moro and sucking reflexes may be sluggish or absentThe infant may experience occasional periods of apneaSeizures typically occur early within the first 24 hours after birthFull recovery within 1-2 weeks is possible and is associated with a better long-term outcome
Severe hypoxic-ischemic encephalopathySeizures can be delayed and severe and may be initially resistant to conventional treatments The seizures are usually generalized and their frequency may increase during the 24-48 hours after onset correlating with the phase of reperfusion injury As the injury progresses seizures subside and the electroencephalogram becomes isoelectric or shows a burst suppression pattern At that time wakefulness may deteriorate further and the fontanelle may bulge suggesting increasing cerebral edema
Other symptoms include the following Stupor or coma is typical the infant may not respond to any physical stimulus except the most noxiousBreathing may be irregular and the infant often requires ventilatory support Generalized hypotonia and depressed deep tendon reflexes are common Neonatal reflexes (eg sucking swallowing grasping Moro) are absent Disturbances of ocular motion such as a skewed deviation of the eyes nystagmus bobbing and loss of dolls eye (ie conjugate) movements may be revealed by cranial nerve examination Pupils may be dilated fixed or poorly reactive to lightIrregularities of heart rate and blood pressure are common during the period of reperfusion injury as is death from cardiorespiratory failure An initial period of well-being or mild hypoxic-ischemic encephalopathy may be followed by sudden deterioration suggesting ongoing brain cell dysfunction injury and death during this period seizure intensity may increase
Imaging of neonatal hypoxic-ischemic encephalopathy
Ultrasonography is the first-line imaging technique for the evaluation of the newborn brain These past few years have seen an increasing role of MRI in the investigation of HIE because of greater sensitivity and specificity Electro-encephalogram(EEG)Computed Tomography(CT)MRI MRS and DWI
MRI sequencesT1 WI T2 WI++ FLAIR are not very useful to detect lesion in young infant less than 24 months due to brain maturation IR T1-weighted Has been very helpful in the last two decades before generalization of high fields MRI as it gives excellent images of brain anatomy and maturation It also shows accurately the differentiation between myelinated and unmyelinated WM Three-dimensional GE T1 weighted sequence (3DT1) bullallow 1 mm contiguous slices which can be reconstructed in any anatomic plane T2 to detect hemorrhagic lesions DWI It is now recommended that DWI should be performed between 2 days and 8 days of life Multiple studies have shown DWI are more sensitive in the detection of HIE lesions than conventional MRI especially for early diagnosis
MRI ProtocolSagittal and axial T1 WI Axial and coronal T2 WI Axial T2 3D T1 FLAIR (older child) DWI MRSLactate peak bulldue to anaerobic glycolysis bullfound within 24 h of life Subsequently a reduction in N-acetyl aspartate (NAA) is evident due to neuronal loss
Advanced technique Perfusion
Arterial Spin-Labeled (ASL) Perfusion bullRecent advances in novel research imaging modalitybullallows noninvasive evaluation of CBF (cerebral blood flow) using electromagnetically labeled arterial blood water as an endogenous contrast agent bullDemonstrates low CBF in neonates who have suffered HIE and in infants and children after stroke
Imaging RecommendationCranial sonography (US) bullFirst between 7 and 14 days bullRepeat before discharge from the hospital MRI DWI MRS bullWhen US is abnormal MRI precise lesion extension and aide in prognosticating bull Defining injury in VLBW neonates with normal US
PrognosisPoor outcome if bullIVH plus PVL bullPVL with volume loss widespread infarction or seizures bullPVL with enlarged cysts
It is necessary to bullknow the normal cerebral appearance before interpret pathological aspect bulldistinguish hypoxic-ischemic brain damage from normal myelination Brain compositionChanges in brain composition Changes in cellular density increase in complex lipids content due to the evolving process of myelination decrease in water content mostly in the WM
Shortening of T1 Shortening of T2
Imaging PatternThe imaging patterns of HIE can be classified into 3 types Lesions predominantly located in the PVWM Lesions predominantly located in the basal ganglia or thalamus Multicystic encephalomalcia The pattern of injury is postulated to depend on bull The type of hypoxiandashischaemia (acute and profound or prolonged and partial) bullThe gestational age (term or pre-term)
HIE in preterm infantRisk FactorsPregnancy Gestational ageweight previous preterm birth spontaneous preterm labor Intrapartum Abruption pre-eclampsia premature rupture of membranes chorioamnionitis group B Strep Peri amp postnatal factors Respiratory distress sepsis anemia apnea bradycardia cardiac arrest
General Features++ PVL +- associated to Germinal matrix and IVH PV hemorrhagic infarction Cerebellar infarction Definition bullPVL is the HIE driven periventricular white matter (PVWM) necrosis seen in very low birth weight premies (lt1500g) EpidemiologybullBirth weight lt 1500 g 45 incidence of PVL (higher if associated with IVH) bullGestational age lt 33 weeks 38 incidence of PVL bullgt 50 of patients with PVL or grade III IVH develop cerebral palsy
Cranial ultrasound coronal view day 1 showing severe echogenicity in the white matter MRI (T2SE (TR 6284TE 120) and ADC) performed on day 3 showing increased signal intensity in the white matter on T2SE and low signal intensity in the deep white matter on the ADC map with sparing of the anterior periventricular white matter and asymmetrical distribution in the parieto-occipital white matter The child died and was subsequently diagnosed to have molybdenum cofactor deficiency
Cranial sonography in 5-day old term with HIE with increase in echogenicity of white matter consistent with edemaCD ultrasound shows reversal of diastolic flow reflecting increased vascular resistance secondary to edema
PVL in a preterm infant (a) Coronal head US image obtained in the 1st week of life shows increased echogenicity in the periventricular white matter (arrows) (b) Follow-up US image obtained 2 months later shows development of cystic changes in these regions and dilatation of the adjacent lateral ventricles findings that are consistent with PVL
CT images show decrease In basal ganglia density related to Cytotoxic edemaSubtle loss of the normally sharp Transition from grey matter to White matter at the corticomedullary Junction Cerebral edema seen with effacementof the cortical sulci and the sylvian Fissures
PVL in a preterm neonate Axial T1-weighted (a) and T2-weighted (b) MR images obtained on day 4 of life demonstrate T1 hypointensity and T2 hyperintensity in the periventricular whitematter Note the punctate foci of high signal intensity on the T1-weighted image (arrows in a) These foci should be distinguished from foci of hemorrhage whichwould demonstrate greater T2 shortening on the corresponding T2-weighted image
28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

(A) Axial diffusion-weighted image showing hyperintensity in the territory of left middle cerebral artery (B) MR angiography demonstrates loss of flow distal to the left middle cerebral artery bifurcation
A B
Perinatal asphyxia more appropriately known as hypoxic-
ischemic encephalopathy (HIE) is characterized by clinical and laboratory evidence of acute or subacute brain injury due to asphyxia The primary causes of this condition are systemic hypoxemia andor reduced cerebral blood flow (CBF) Birth asphyxia causes 840000 or 23 of all neonatal deaths worldwideHIE- Acute brain injury that occur before during or after birth
Signs and symptomsMild hypoxic-ischemic encephalopathybullMuscle tone may be slightly increased and deep tendon reflexes may be brisk during the first few daysbullTransient behavioral abnormalities such as poor feeding irritability or excessive crying or sleepiness (typically in an alternating pattern) may be observed bullTypically resolves in 24h
Moderately severe hypoxic-ischemic encephalopathyThe infant is lethargic with significant hypotonia and diminished deep tendon reflexesThe grasping Moro and sucking reflexes may be sluggish or absentThe infant may experience occasional periods of apneaSeizures typically occur early within the first 24 hours after birthFull recovery within 1-2 weeks is possible and is associated with a better long-term outcome
Severe hypoxic-ischemic encephalopathySeizures can be delayed and severe and may be initially resistant to conventional treatments The seizures are usually generalized and their frequency may increase during the 24-48 hours after onset correlating with the phase of reperfusion injury As the injury progresses seizures subside and the electroencephalogram becomes isoelectric or shows a burst suppression pattern At that time wakefulness may deteriorate further and the fontanelle may bulge suggesting increasing cerebral edema
Other symptoms include the following Stupor or coma is typical the infant may not respond to any physical stimulus except the most noxiousBreathing may be irregular and the infant often requires ventilatory support Generalized hypotonia and depressed deep tendon reflexes are common Neonatal reflexes (eg sucking swallowing grasping Moro) are absent Disturbances of ocular motion such as a skewed deviation of the eyes nystagmus bobbing and loss of dolls eye (ie conjugate) movements may be revealed by cranial nerve examination Pupils may be dilated fixed or poorly reactive to lightIrregularities of heart rate and blood pressure are common during the period of reperfusion injury as is death from cardiorespiratory failure An initial period of well-being or mild hypoxic-ischemic encephalopathy may be followed by sudden deterioration suggesting ongoing brain cell dysfunction injury and death during this period seizure intensity may increase
Imaging of neonatal hypoxic-ischemic encephalopathy
Ultrasonography is the first-line imaging technique for the evaluation of the newborn brain These past few years have seen an increasing role of MRI in the investigation of HIE because of greater sensitivity and specificity Electro-encephalogram(EEG)Computed Tomography(CT)MRI MRS and DWI
MRI sequencesT1 WI T2 WI++ FLAIR are not very useful to detect lesion in young infant less than 24 months due to brain maturation IR T1-weighted Has been very helpful in the last two decades before generalization of high fields MRI as it gives excellent images of brain anatomy and maturation It also shows accurately the differentiation between myelinated and unmyelinated WM Three-dimensional GE T1 weighted sequence (3DT1) bullallow 1 mm contiguous slices which can be reconstructed in any anatomic plane T2 to detect hemorrhagic lesions DWI It is now recommended that DWI should be performed between 2 days and 8 days of life Multiple studies have shown DWI are more sensitive in the detection of HIE lesions than conventional MRI especially for early diagnosis
MRI ProtocolSagittal and axial T1 WI Axial and coronal T2 WI Axial T2 3D T1 FLAIR (older child) DWI MRSLactate peak bulldue to anaerobic glycolysis bullfound within 24 h of life Subsequently a reduction in N-acetyl aspartate (NAA) is evident due to neuronal loss
Advanced technique Perfusion
Arterial Spin-Labeled (ASL) Perfusion bullRecent advances in novel research imaging modalitybullallows noninvasive evaluation of CBF (cerebral blood flow) using electromagnetically labeled arterial blood water as an endogenous contrast agent bullDemonstrates low CBF in neonates who have suffered HIE and in infants and children after stroke
Imaging RecommendationCranial sonography (US) bullFirst between 7 and 14 days bullRepeat before discharge from the hospital MRI DWI MRS bullWhen US is abnormal MRI precise lesion extension and aide in prognosticating bull Defining injury in VLBW neonates with normal US
PrognosisPoor outcome if bullIVH plus PVL bullPVL with volume loss widespread infarction or seizures bullPVL with enlarged cysts
It is necessary to bullknow the normal cerebral appearance before interpret pathological aspect bulldistinguish hypoxic-ischemic brain damage from normal myelination Brain compositionChanges in brain composition Changes in cellular density increase in complex lipids content due to the evolving process of myelination decrease in water content mostly in the WM
Shortening of T1 Shortening of T2
Imaging PatternThe imaging patterns of HIE can be classified into 3 types Lesions predominantly located in the PVWM Lesions predominantly located in the basal ganglia or thalamus Multicystic encephalomalcia The pattern of injury is postulated to depend on bull The type of hypoxiandashischaemia (acute and profound or prolonged and partial) bullThe gestational age (term or pre-term)
HIE in preterm infantRisk FactorsPregnancy Gestational ageweight previous preterm birth spontaneous preterm labor Intrapartum Abruption pre-eclampsia premature rupture of membranes chorioamnionitis group B Strep Peri amp postnatal factors Respiratory distress sepsis anemia apnea bradycardia cardiac arrest
General Features++ PVL +- associated to Germinal matrix and IVH PV hemorrhagic infarction Cerebellar infarction Definition bullPVL is the HIE driven periventricular white matter (PVWM) necrosis seen in very low birth weight premies (lt1500g) EpidemiologybullBirth weight lt 1500 g 45 incidence of PVL (higher if associated with IVH) bullGestational age lt 33 weeks 38 incidence of PVL bullgt 50 of patients with PVL or grade III IVH develop cerebral palsy
Cranial ultrasound coronal view day 1 showing severe echogenicity in the white matter MRI (T2SE (TR 6284TE 120) and ADC) performed on day 3 showing increased signal intensity in the white matter on T2SE and low signal intensity in the deep white matter on the ADC map with sparing of the anterior periventricular white matter and asymmetrical distribution in the parieto-occipital white matter The child died and was subsequently diagnosed to have molybdenum cofactor deficiency
Cranial sonography in 5-day old term with HIE with increase in echogenicity of white matter consistent with edemaCD ultrasound shows reversal of diastolic flow reflecting increased vascular resistance secondary to edema
PVL in a preterm infant (a) Coronal head US image obtained in the 1st week of life shows increased echogenicity in the periventricular white matter (arrows) (b) Follow-up US image obtained 2 months later shows development of cystic changes in these regions and dilatation of the adjacent lateral ventricles findings that are consistent with PVL
CT images show decrease In basal ganglia density related to Cytotoxic edemaSubtle loss of the normally sharp Transition from grey matter to White matter at the corticomedullary Junction Cerebral edema seen with effacementof the cortical sulci and the sylvian Fissures
PVL in a preterm neonate Axial T1-weighted (a) and T2-weighted (b) MR images obtained on day 4 of life demonstrate T1 hypointensity and T2 hyperintensity in the periventricular whitematter Note the punctate foci of high signal intensity on the T1-weighted image (arrows in a) These foci should be distinguished from foci of hemorrhage whichwould demonstrate greater T2 shortening on the corresponding T2-weighted image
28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

Perinatal asphyxia more appropriately known as hypoxic-
ischemic encephalopathy (HIE) is characterized by clinical and laboratory evidence of acute or subacute brain injury due to asphyxia The primary causes of this condition are systemic hypoxemia andor reduced cerebral blood flow (CBF) Birth asphyxia causes 840000 or 23 of all neonatal deaths worldwideHIE- Acute brain injury that occur before during or after birth
Signs and symptomsMild hypoxic-ischemic encephalopathybullMuscle tone may be slightly increased and deep tendon reflexes may be brisk during the first few daysbullTransient behavioral abnormalities such as poor feeding irritability or excessive crying or sleepiness (typically in an alternating pattern) may be observed bullTypically resolves in 24h
Moderately severe hypoxic-ischemic encephalopathyThe infant is lethargic with significant hypotonia and diminished deep tendon reflexesThe grasping Moro and sucking reflexes may be sluggish or absentThe infant may experience occasional periods of apneaSeizures typically occur early within the first 24 hours after birthFull recovery within 1-2 weeks is possible and is associated with a better long-term outcome
Severe hypoxic-ischemic encephalopathySeizures can be delayed and severe and may be initially resistant to conventional treatments The seizures are usually generalized and their frequency may increase during the 24-48 hours after onset correlating with the phase of reperfusion injury As the injury progresses seizures subside and the electroencephalogram becomes isoelectric or shows a burst suppression pattern At that time wakefulness may deteriorate further and the fontanelle may bulge suggesting increasing cerebral edema
Other symptoms include the following Stupor or coma is typical the infant may not respond to any physical stimulus except the most noxiousBreathing may be irregular and the infant often requires ventilatory support Generalized hypotonia and depressed deep tendon reflexes are common Neonatal reflexes (eg sucking swallowing grasping Moro) are absent Disturbances of ocular motion such as a skewed deviation of the eyes nystagmus bobbing and loss of dolls eye (ie conjugate) movements may be revealed by cranial nerve examination Pupils may be dilated fixed or poorly reactive to lightIrregularities of heart rate and blood pressure are common during the period of reperfusion injury as is death from cardiorespiratory failure An initial period of well-being or mild hypoxic-ischemic encephalopathy may be followed by sudden deterioration suggesting ongoing brain cell dysfunction injury and death during this period seizure intensity may increase
Imaging of neonatal hypoxic-ischemic encephalopathy
Ultrasonography is the first-line imaging technique for the evaluation of the newborn brain These past few years have seen an increasing role of MRI in the investigation of HIE because of greater sensitivity and specificity Electro-encephalogram(EEG)Computed Tomography(CT)MRI MRS and DWI
MRI sequencesT1 WI T2 WI++ FLAIR are not very useful to detect lesion in young infant less than 24 months due to brain maturation IR T1-weighted Has been very helpful in the last two decades before generalization of high fields MRI as it gives excellent images of brain anatomy and maturation It also shows accurately the differentiation between myelinated and unmyelinated WM Three-dimensional GE T1 weighted sequence (3DT1) bullallow 1 mm contiguous slices which can be reconstructed in any anatomic plane T2 to detect hemorrhagic lesions DWI It is now recommended that DWI should be performed between 2 days and 8 days of life Multiple studies have shown DWI are more sensitive in the detection of HIE lesions than conventional MRI especially for early diagnosis
MRI ProtocolSagittal and axial T1 WI Axial and coronal T2 WI Axial T2 3D T1 FLAIR (older child) DWI MRSLactate peak bulldue to anaerobic glycolysis bullfound within 24 h of life Subsequently a reduction in N-acetyl aspartate (NAA) is evident due to neuronal loss
Advanced technique Perfusion
Arterial Spin-Labeled (ASL) Perfusion bullRecent advances in novel research imaging modalitybullallows noninvasive evaluation of CBF (cerebral blood flow) using electromagnetically labeled arterial blood water as an endogenous contrast agent bullDemonstrates low CBF in neonates who have suffered HIE and in infants and children after stroke
Imaging RecommendationCranial sonography (US) bullFirst between 7 and 14 days bullRepeat before discharge from the hospital MRI DWI MRS bullWhen US is abnormal MRI precise lesion extension and aide in prognosticating bull Defining injury in VLBW neonates with normal US
PrognosisPoor outcome if bullIVH plus PVL bullPVL with volume loss widespread infarction or seizures bullPVL with enlarged cysts
It is necessary to bullknow the normal cerebral appearance before interpret pathological aspect bulldistinguish hypoxic-ischemic brain damage from normal myelination Brain compositionChanges in brain composition Changes in cellular density increase in complex lipids content due to the evolving process of myelination decrease in water content mostly in the WM
Shortening of T1 Shortening of T2
Imaging PatternThe imaging patterns of HIE can be classified into 3 types Lesions predominantly located in the PVWM Lesions predominantly located in the basal ganglia or thalamus Multicystic encephalomalcia The pattern of injury is postulated to depend on bull The type of hypoxiandashischaemia (acute and profound or prolonged and partial) bullThe gestational age (term or pre-term)
HIE in preterm infantRisk FactorsPregnancy Gestational ageweight previous preterm birth spontaneous preterm labor Intrapartum Abruption pre-eclampsia premature rupture of membranes chorioamnionitis group B Strep Peri amp postnatal factors Respiratory distress sepsis anemia apnea bradycardia cardiac arrest
General Features++ PVL +- associated to Germinal matrix and IVH PV hemorrhagic infarction Cerebellar infarction Definition bullPVL is the HIE driven periventricular white matter (PVWM) necrosis seen in very low birth weight premies (lt1500g) EpidemiologybullBirth weight lt 1500 g 45 incidence of PVL (higher if associated with IVH) bullGestational age lt 33 weeks 38 incidence of PVL bullgt 50 of patients with PVL or grade III IVH develop cerebral palsy
Cranial ultrasound coronal view day 1 showing severe echogenicity in the white matter MRI (T2SE (TR 6284TE 120) and ADC) performed on day 3 showing increased signal intensity in the white matter on T2SE and low signal intensity in the deep white matter on the ADC map with sparing of the anterior periventricular white matter and asymmetrical distribution in the parieto-occipital white matter The child died and was subsequently diagnosed to have molybdenum cofactor deficiency
Cranial sonography in 5-day old term with HIE with increase in echogenicity of white matter consistent with edemaCD ultrasound shows reversal of diastolic flow reflecting increased vascular resistance secondary to edema
PVL in a preterm infant (a) Coronal head US image obtained in the 1st week of life shows increased echogenicity in the periventricular white matter (arrows) (b) Follow-up US image obtained 2 months later shows development of cystic changes in these regions and dilatation of the adjacent lateral ventricles findings that are consistent with PVL
CT images show decrease In basal ganglia density related to Cytotoxic edemaSubtle loss of the normally sharp Transition from grey matter to White matter at the corticomedullary Junction Cerebral edema seen with effacementof the cortical sulci and the sylvian Fissures
PVL in a preterm neonate Axial T1-weighted (a) and T2-weighted (b) MR images obtained on day 4 of life demonstrate T1 hypointensity and T2 hyperintensity in the periventricular whitematter Note the punctate foci of high signal intensity on the T1-weighted image (arrows in a) These foci should be distinguished from foci of hemorrhage whichwould demonstrate greater T2 shortening on the corresponding T2-weighted image
28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

Moderately severe hypoxic-ischemic encephalopathyThe infant is lethargic with significant hypotonia and diminished deep tendon reflexesThe grasping Moro and sucking reflexes may be sluggish or absentThe infant may experience occasional periods of apneaSeizures typically occur early within the first 24 hours after birthFull recovery within 1-2 weeks is possible and is associated with a better long-term outcome
Severe hypoxic-ischemic encephalopathySeizures can be delayed and severe and may be initially resistant to conventional treatments The seizures are usually generalized and their frequency may increase during the 24-48 hours after onset correlating with the phase of reperfusion injury As the injury progresses seizures subside and the electroencephalogram becomes isoelectric or shows a burst suppression pattern At that time wakefulness may deteriorate further and the fontanelle may bulge suggesting increasing cerebral edema
Other symptoms include the following Stupor or coma is typical the infant may not respond to any physical stimulus except the most noxiousBreathing may be irregular and the infant often requires ventilatory support Generalized hypotonia and depressed deep tendon reflexes are common Neonatal reflexes (eg sucking swallowing grasping Moro) are absent Disturbances of ocular motion such as a skewed deviation of the eyes nystagmus bobbing and loss of dolls eye (ie conjugate) movements may be revealed by cranial nerve examination Pupils may be dilated fixed or poorly reactive to lightIrregularities of heart rate and blood pressure are common during the period of reperfusion injury as is death from cardiorespiratory failure An initial period of well-being or mild hypoxic-ischemic encephalopathy may be followed by sudden deterioration suggesting ongoing brain cell dysfunction injury and death during this period seizure intensity may increase
Imaging of neonatal hypoxic-ischemic encephalopathy
Ultrasonography is the first-line imaging technique for the evaluation of the newborn brain These past few years have seen an increasing role of MRI in the investigation of HIE because of greater sensitivity and specificity Electro-encephalogram(EEG)Computed Tomography(CT)MRI MRS and DWI
MRI sequencesT1 WI T2 WI++ FLAIR are not very useful to detect lesion in young infant less than 24 months due to brain maturation IR T1-weighted Has been very helpful in the last two decades before generalization of high fields MRI as it gives excellent images of brain anatomy and maturation It also shows accurately the differentiation between myelinated and unmyelinated WM Three-dimensional GE T1 weighted sequence (3DT1) bullallow 1 mm contiguous slices which can be reconstructed in any anatomic plane T2 to detect hemorrhagic lesions DWI It is now recommended that DWI should be performed between 2 days and 8 days of life Multiple studies have shown DWI are more sensitive in the detection of HIE lesions than conventional MRI especially for early diagnosis
MRI ProtocolSagittal and axial T1 WI Axial and coronal T2 WI Axial T2 3D T1 FLAIR (older child) DWI MRSLactate peak bulldue to anaerobic glycolysis bullfound within 24 h of life Subsequently a reduction in N-acetyl aspartate (NAA) is evident due to neuronal loss
Advanced technique Perfusion
Arterial Spin-Labeled (ASL) Perfusion bullRecent advances in novel research imaging modalitybullallows noninvasive evaluation of CBF (cerebral blood flow) using electromagnetically labeled arterial blood water as an endogenous contrast agent bullDemonstrates low CBF in neonates who have suffered HIE and in infants and children after stroke
Imaging RecommendationCranial sonography (US) bullFirst between 7 and 14 days bullRepeat before discharge from the hospital MRI DWI MRS bullWhen US is abnormal MRI precise lesion extension and aide in prognosticating bull Defining injury in VLBW neonates with normal US
PrognosisPoor outcome if bullIVH plus PVL bullPVL with volume loss widespread infarction or seizures bullPVL with enlarged cysts
It is necessary to bullknow the normal cerebral appearance before interpret pathological aspect bulldistinguish hypoxic-ischemic brain damage from normal myelination Brain compositionChanges in brain composition Changes in cellular density increase in complex lipids content due to the evolving process of myelination decrease in water content mostly in the WM
Shortening of T1 Shortening of T2
Imaging PatternThe imaging patterns of HIE can be classified into 3 types Lesions predominantly located in the PVWM Lesions predominantly located in the basal ganglia or thalamus Multicystic encephalomalcia The pattern of injury is postulated to depend on bull The type of hypoxiandashischaemia (acute and profound or prolonged and partial) bullThe gestational age (term or pre-term)
HIE in preterm infantRisk FactorsPregnancy Gestational ageweight previous preterm birth spontaneous preterm labor Intrapartum Abruption pre-eclampsia premature rupture of membranes chorioamnionitis group B Strep Peri amp postnatal factors Respiratory distress sepsis anemia apnea bradycardia cardiac arrest
General Features++ PVL +- associated to Germinal matrix and IVH PV hemorrhagic infarction Cerebellar infarction Definition bullPVL is the HIE driven periventricular white matter (PVWM) necrosis seen in very low birth weight premies (lt1500g) EpidemiologybullBirth weight lt 1500 g 45 incidence of PVL (higher if associated with IVH) bullGestational age lt 33 weeks 38 incidence of PVL bullgt 50 of patients with PVL or grade III IVH develop cerebral palsy
Cranial ultrasound coronal view day 1 showing severe echogenicity in the white matter MRI (T2SE (TR 6284TE 120) and ADC) performed on day 3 showing increased signal intensity in the white matter on T2SE and low signal intensity in the deep white matter on the ADC map with sparing of the anterior periventricular white matter and asymmetrical distribution in the parieto-occipital white matter The child died and was subsequently diagnosed to have molybdenum cofactor deficiency
Cranial sonography in 5-day old term with HIE with increase in echogenicity of white matter consistent with edemaCD ultrasound shows reversal of diastolic flow reflecting increased vascular resistance secondary to edema
PVL in a preterm infant (a) Coronal head US image obtained in the 1st week of life shows increased echogenicity in the periventricular white matter (arrows) (b) Follow-up US image obtained 2 months later shows development of cystic changes in these regions and dilatation of the adjacent lateral ventricles findings that are consistent with PVL
CT images show decrease In basal ganglia density related to Cytotoxic edemaSubtle loss of the normally sharp Transition from grey matter to White matter at the corticomedullary Junction Cerebral edema seen with effacementof the cortical sulci and the sylvian Fissures
PVL in a preterm neonate Axial T1-weighted (a) and T2-weighted (b) MR images obtained on day 4 of life demonstrate T1 hypointensity and T2 hyperintensity in the periventricular whitematter Note the punctate foci of high signal intensity on the T1-weighted image (arrows in a) These foci should be distinguished from foci of hemorrhage whichwould demonstrate greater T2 shortening on the corresponding T2-weighted image
28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

Other symptoms include the following Stupor or coma is typical the infant may not respond to any physical stimulus except the most noxiousBreathing may be irregular and the infant often requires ventilatory support Generalized hypotonia and depressed deep tendon reflexes are common Neonatal reflexes (eg sucking swallowing grasping Moro) are absent Disturbances of ocular motion such as a skewed deviation of the eyes nystagmus bobbing and loss of dolls eye (ie conjugate) movements may be revealed by cranial nerve examination Pupils may be dilated fixed or poorly reactive to lightIrregularities of heart rate and blood pressure are common during the period of reperfusion injury as is death from cardiorespiratory failure An initial period of well-being or mild hypoxic-ischemic encephalopathy may be followed by sudden deterioration suggesting ongoing brain cell dysfunction injury and death during this period seizure intensity may increase
Imaging of neonatal hypoxic-ischemic encephalopathy
Ultrasonography is the first-line imaging technique for the evaluation of the newborn brain These past few years have seen an increasing role of MRI in the investigation of HIE because of greater sensitivity and specificity Electro-encephalogram(EEG)Computed Tomography(CT)MRI MRS and DWI
MRI sequencesT1 WI T2 WI++ FLAIR are not very useful to detect lesion in young infant less than 24 months due to brain maturation IR T1-weighted Has been very helpful in the last two decades before generalization of high fields MRI as it gives excellent images of brain anatomy and maturation It also shows accurately the differentiation between myelinated and unmyelinated WM Three-dimensional GE T1 weighted sequence (3DT1) bullallow 1 mm contiguous slices which can be reconstructed in any anatomic plane T2 to detect hemorrhagic lesions DWI It is now recommended that DWI should be performed between 2 days and 8 days of life Multiple studies have shown DWI are more sensitive in the detection of HIE lesions than conventional MRI especially for early diagnosis
MRI ProtocolSagittal and axial T1 WI Axial and coronal T2 WI Axial T2 3D T1 FLAIR (older child) DWI MRSLactate peak bulldue to anaerobic glycolysis bullfound within 24 h of life Subsequently a reduction in N-acetyl aspartate (NAA) is evident due to neuronal loss
Advanced technique Perfusion
Arterial Spin-Labeled (ASL) Perfusion bullRecent advances in novel research imaging modalitybullallows noninvasive evaluation of CBF (cerebral blood flow) using electromagnetically labeled arterial blood water as an endogenous contrast agent bullDemonstrates low CBF in neonates who have suffered HIE and in infants and children after stroke
Imaging RecommendationCranial sonography (US) bullFirst between 7 and 14 days bullRepeat before discharge from the hospital MRI DWI MRS bullWhen US is abnormal MRI precise lesion extension and aide in prognosticating bull Defining injury in VLBW neonates with normal US
PrognosisPoor outcome if bullIVH plus PVL bullPVL with volume loss widespread infarction or seizures bullPVL with enlarged cysts
It is necessary to bullknow the normal cerebral appearance before interpret pathological aspect bulldistinguish hypoxic-ischemic brain damage from normal myelination Brain compositionChanges in brain composition Changes in cellular density increase in complex lipids content due to the evolving process of myelination decrease in water content mostly in the WM
Shortening of T1 Shortening of T2
Imaging PatternThe imaging patterns of HIE can be classified into 3 types Lesions predominantly located in the PVWM Lesions predominantly located in the basal ganglia or thalamus Multicystic encephalomalcia The pattern of injury is postulated to depend on bull The type of hypoxiandashischaemia (acute and profound or prolonged and partial) bullThe gestational age (term or pre-term)
HIE in preterm infantRisk FactorsPregnancy Gestational ageweight previous preterm birth spontaneous preterm labor Intrapartum Abruption pre-eclampsia premature rupture of membranes chorioamnionitis group B Strep Peri amp postnatal factors Respiratory distress sepsis anemia apnea bradycardia cardiac arrest
General Features++ PVL +- associated to Germinal matrix and IVH PV hemorrhagic infarction Cerebellar infarction Definition bullPVL is the HIE driven periventricular white matter (PVWM) necrosis seen in very low birth weight premies (lt1500g) EpidemiologybullBirth weight lt 1500 g 45 incidence of PVL (higher if associated with IVH) bullGestational age lt 33 weeks 38 incidence of PVL bullgt 50 of patients with PVL or grade III IVH develop cerebral palsy
Cranial ultrasound coronal view day 1 showing severe echogenicity in the white matter MRI (T2SE (TR 6284TE 120) and ADC) performed on day 3 showing increased signal intensity in the white matter on T2SE and low signal intensity in the deep white matter on the ADC map with sparing of the anterior periventricular white matter and asymmetrical distribution in the parieto-occipital white matter The child died and was subsequently diagnosed to have molybdenum cofactor deficiency
Cranial sonography in 5-day old term with HIE with increase in echogenicity of white matter consistent with edemaCD ultrasound shows reversal of diastolic flow reflecting increased vascular resistance secondary to edema
PVL in a preterm infant (a) Coronal head US image obtained in the 1st week of life shows increased echogenicity in the periventricular white matter (arrows) (b) Follow-up US image obtained 2 months later shows development of cystic changes in these regions and dilatation of the adjacent lateral ventricles findings that are consistent with PVL
CT images show decrease In basal ganglia density related to Cytotoxic edemaSubtle loss of the normally sharp Transition from grey matter to White matter at the corticomedullary Junction Cerebral edema seen with effacementof the cortical sulci and the sylvian Fissures
PVL in a preterm neonate Axial T1-weighted (a) and T2-weighted (b) MR images obtained on day 4 of life demonstrate T1 hypointensity and T2 hyperintensity in the periventricular whitematter Note the punctate foci of high signal intensity on the T1-weighted image (arrows in a) These foci should be distinguished from foci of hemorrhage whichwould demonstrate greater T2 shortening on the corresponding T2-weighted image
28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

Imaging of neonatal hypoxic-ischemic encephalopathy
Ultrasonography is the first-line imaging technique for the evaluation of the newborn brain These past few years have seen an increasing role of MRI in the investigation of HIE because of greater sensitivity and specificity Electro-encephalogram(EEG)Computed Tomography(CT)MRI MRS and DWI
MRI sequencesT1 WI T2 WI++ FLAIR are not very useful to detect lesion in young infant less than 24 months due to brain maturation IR T1-weighted Has been very helpful in the last two decades before generalization of high fields MRI as it gives excellent images of brain anatomy and maturation It also shows accurately the differentiation between myelinated and unmyelinated WM Three-dimensional GE T1 weighted sequence (3DT1) bullallow 1 mm contiguous slices which can be reconstructed in any anatomic plane T2 to detect hemorrhagic lesions DWI It is now recommended that DWI should be performed between 2 days and 8 days of life Multiple studies have shown DWI are more sensitive in the detection of HIE lesions than conventional MRI especially for early diagnosis
MRI ProtocolSagittal and axial T1 WI Axial and coronal T2 WI Axial T2 3D T1 FLAIR (older child) DWI MRSLactate peak bulldue to anaerobic glycolysis bullfound within 24 h of life Subsequently a reduction in N-acetyl aspartate (NAA) is evident due to neuronal loss
Advanced technique Perfusion
Arterial Spin-Labeled (ASL) Perfusion bullRecent advances in novel research imaging modalitybullallows noninvasive evaluation of CBF (cerebral blood flow) using electromagnetically labeled arterial blood water as an endogenous contrast agent bullDemonstrates low CBF in neonates who have suffered HIE and in infants and children after stroke
Imaging RecommendationCranial sonography (US) bullFirst between 7 and 14 days bullRepeat before discharge from the hospital MRI DWI MRS bullWhen US is abnormal MRI precise lesion extension and aide in prognosticating bull Defining injury in VLBW neonates with normal US
PrognosisPoor outcome if bullIVH plus PVL bullPVL with volume loss widespread infarction or seizures bullPVL with enlarged cysts
It is necessary to bullknow the normal cerebral appearance before interpret pathological aspect bulldistinguish hypoxic-ischemic brain damage from normal myelination Brain compositionChanges in brain composition Changes in cellular density increase in complex lipids content due to the evolving process of myelination decrease in water content mostly in the WM
Shortening of T1 Shortening of T2
Imaging PatternThe imaging patterns of HIE can be classified into 3 types Lesions predominantly located in the PVWM Lesions predominantly located in the basal ganglia or thalamus Multicystic encephalomalcia The pattern of injury is postulated to depend on bull The type of hypoxiandashischaemia (acute and profound or prolonged and partial) bullThe gestational age (term or pre-term)
HIE in preterm infantRisk FactorsPregnancy Gestational ageweight previous preterm birth spontaneous preterm labor Intrapartum Abruption pre-eclampsia premature rupture of membranes chorioamnionitis group B Strep Peri amp postnatal factors Respiratory distress sepsis anemia apnea bradycardia cardiac arrest
General Features++ PVL +- associated to Germinal matrix and IVH PV hemorrhagic infarction Cerebellar infarction Definition bullPVL is the HIE driven periventricular white matter (PVWM) necrosis seen in very low birth weight premies (lt1500g) EpidemiologybullBirth weight lt 1500 g 45 incidence of PVL (higher if associated with IVH) bullGestational age lt 33 weeks 38 incidence of PVL bullgt 50 of patients with PVL or grade III IVH develop cerebral palsy
Cranial ultrasound coronal view day 1 showing severe echogenicity in the white matter MRI (T2SE (TR 6284TE 120) and ADC) performed on day 3 showing increased signal intensity in the white matter on T2SE and low signal intensity in the deep white matter on the ADC map with sparing of the anterior periventricular white matter and asymmetrical distribution in the parieto-occipital white matter The child died and was subsequently diagnosed to have molybdenum cofactor deficiency
Cranial sonography in 5-day old term with HIE with increase in echogenicity of white matter consistent with edemaCD ultrasound shows reversal of diastolic flow reflecting increased vascular resistance secondary to edema
PVL in a preterm infant (a) Coronal head US image obtained in the 1st week of life shows increased echogenicity in the periventricular white matter (arrows) (b) Follow-up US image obtained 2 months later shows development of cystic changes in these regions and dilatation of the adjacent lateral ventricles findings that are consistent with PVL
CT images show decrease In basal ganglia density related to Cytotoxic edemaSubtle loss of the normally sharp Transition from grey matter to White matter at the corticomedullary Junction Cerebral edema seen with effacementof the cortical sulci and the sylvian Fissures
PVL in a preterm neonate Axial T1-weighted (a) and T2-weighted (b) MR images obtained on day 4 of life demonstrate T1 hypointensity and T2 hyperintensity in the periventricular whitematter Note the punctate foci of high signal intensity on the T1-weighted image (arrows in a) These foci should be distinguished from foci of hemorrhage whichwould demonstrate greater T2 shortening on the corresponding T2-weighted image
28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

MRI sequencesT1 WI T2 WI++ FLAIR are not very useful to detect lesion in young infant less than 24 months due to brain maturation IR T1-weighted Has been very helpful in the last two decades before generalization of high fields MRI as it gives excellent images of brain anatomy and maturation It also shows accurately the differentiation between myelinated and unmyelinated WM Three-dimensional GE T1 weighted sequence (3DT1) bullallow 1 mm contiguous slices which can be reconstructed in any anatomic plane T2 to detect hemorrhagic lesions DWI It is now recommended that DWI should be performed between 2 days and 8 days of life Multiple studies have shown DWI are more sensitive in the detection of HIE lesions than conventional MRI especially for early diagnosis
MRI ProtocolSagittal and axial T1 WI Axial and coronal T2 WI Axial T2 3D T1 FLAIR (older child) DWI MRSLactate peak bulldue to anaerobic glycolysis bullfound within 24 h of life Subsequently a reduction in N-acetyl aspartate (NAA) is evident due to neuronal loss
Advanced technique Perfusion
Arterial Spin-Labeled (ASL) Perfusion bullRecent advances in novel research imaging modalitybullallows noninvasive evaluation of CBF (cerebral blood flow) using electromagnetically labeled arterial blood water as an endogenous contrast agent bullDemonstrates low CBF in neonates who have suffered HIE and in infants and children after stroke
Imaging RecommendationCranial sonography (US) bullFirst between 7 and 14 days bullRepeat before discharge from the hospital MRI DWI MRS bullWhen US is abnormal MRI precise lesion extension and aide in prognosticating bull Defining injury in VLBW neonates with normal US
PrognosisPoor outcome if bullIVH plus PVL bullPVL with volume loss widespread infarction or seizures bullPVL with enlarged cysts
It is necessary to bullknow the normal cerebral appearance before interpret pathological aspect bulldistinguish hypoxic-ischemic brain damage from normal myelination Brain compositionChanges in brain composition Changes in cellular density increase in complex lipids content due to the evolving process of myelination decrease in water content mostly in the WM
Shortening of T1 Shortening of T2
Imaging PatternThe imaging patterns of HIE can be classified into 3 types Lesions predominantly located in the PVWM Lesions predominantly located in the basal ganglia or thalamus Multicystic encephalomalcia The pattern of injury is postulated to depend on bull The type of hypoxiandashischaemia (acute and profound or prolonged and partial) bullThe gestational age (term or pre-term)
HIE in preterm infantRisk FactorsPregnancy Gestational ageweight previous preterm birth spontaneous preterm labor Intrapartum Abruption pre-eclampsia premature rupture of membranes chorioamnionitis group B Strep Peri amp postnatal factors Respiratory distress sepsis anemia apnea bradycardia cardiac arrest
General Features++ PVL +- associated to Germinal matrix and IVH PV hemorrhagic infarction Cerebellar infarction Definition bullPVL is the HIE driven periventricular white matter (PVWM) necrosis seen in very low birth weight premies (lt1500g) EpidemiologybullBirth weight lt 1500 g 45 incidence of PVL (higher if associated with IVH) bullGestational age lt 33 weeks 38 incidence of PVL bullgt 50 of patients with PVL or grade III IVH develop cerebral palsy
Cranial ultrasound coronal view day 1 showing severe echogenicity in the white matter MRI (T2SE (TR 6284TE 120) and ADC) performed on day 3 showing increased signal intensity in the white matter on T2SE and low signal intensity in the deep white matter on the ADC map with sparing of the anterior periventricular white matter and asymmetrical distribution in the parieto-occipital white matter The child died and was subsequently diagnosed to have molybdenum cofactor deficiency
Cranial sonography in 5-day old term with HIE with increase in echogenicity of white matter consistent with edemaCD ultrasound shows reversal of diastolic flow reflecting increased vascular resistance secondary to edema
PVL in a preterm infant (a) Coronal head US image obtained in the 1st week of life shows increased echogenicity in the periventricular white matter (arrows) (b) Follow-up US image obtained 2 months later shows development of cystic changes in these regions and dilatation of the adjacent lateral ventricles findings that are consistent with PVL
CT images show decrease In basal ganglia density related to Cytotoxic edemaSubtle loss of the normally sharp Transition from grey matter to White matter at the corticomedullary Junction Cerebral edema seen with effacementof the cortical sulci and the sylvian Fissures
PVL in a preterm neonate Axial T1-weighted (a) and T2-weighted (b) MR images obtained on day 4 of life demonstrate T1 hypointensity and T2 hyperintensity in the periventricular whitematter Note the punctate foci of high signal intensity on the T1-weighted image (arrows in a) These foci should be distinguished from foci of hemorrhage whichwould demonstrate greater T2 shortening on the corresponding T2-weighted image
28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

MRI ProtocolSagittal and axial T1 WI Axial and coronal T2 WI Axial T2 3D T1 FLAIR (older child) DWI MRSLactate peak bulldue to anaerobic glycolysis bullfound within 24 h of life Subsequently a reduction in N-acetyl aspartate (NAA) is evident due to neuronal loss
Advanced technique Perfusion
Arterial Spin-Labeled (ASL) Perfusion bullRecent advances in novel research imaging modalitybullallows noninvasive evaluation of CBF (cerebral blood flow) using electromagnetically labeled arterial blood water as an endogenous contrast agent bullDemonstrates low CBF in neonates who have suffered HIE and in infants and children after stroke
Imaging RecommendationCranial sonography (US) bullFirst between 7 and 14 days bullRepeat before discharge from the hospital MRI DWI MRS bullWhen US is abnormal MRI precise lesion extension and aide in prognosticating bull Defining injury in VLBW neonates with normal US
PrognosisPoor outcome if bullIVH plus PVL bullPVL with volume loss widespread infarction or seizures bullPVL with enlarged cysts
It is necessary to bullknow the normal cerebral appearance before interpret pathological aspect bulldistinguish hypoxic-ischemic brain damage from normal myelination Brain compositionChanges in brain composition Changes in cellular density increase in complex lipids content due to the evolving process of myelination decrease in water content mostly in the WM
Shortening of T1 Shortening of T2
Imaging PatternThe imaging patterns of HIE can be classified into 3 types Lesions predominantly located in the PVWM Lesions predominantly located in the basal ganglia or thalamus Multicystic encephalomalcia The pattern of injury is postulated to depend on bull The type of hypoxiandashischaemia (acute and profound or prolonged and partial) bullThe gestational age (term or pre-term)
HIE in preterm infantRisk FactorsPregnancy Gestational ageweight previous preterm birth spontaneous preterm labor Intrapartum Abruption pre-eclampsia premature rupture of membranes chorioamnionitis group B Strep Peri amp postnatal factors Respiratory distress sepsis anemia apnea bradycardia cardiac arrest
General Features++ PVL +- associated to Germinal matrix and IVH PV hemorrhagic infarction Cerebellar infarction Definition bullPVL is the HIE driven periventricular white matter (PVWM) necrosis seen in very low birth weight premies (lt1500g) EpidemiologybullBirth weight lt 1500 g 45 incidence of PVL (higher if associated with IVH) bullGestational age lt 33 weeks 38 incidence of PVL bullgt 50 of patients with PVL or grade III IVH develop cerebral palsy
Cranial ultrasound coronal view day 1 showing severe echogenicity in the white matter MRI (T2SE (TR 6284TE 120) and ADC) performed on day 3 showing increased signal intensity in the white matter on T2SE and low signal intensity in the deep white matter on the ADC map with sparing of the anterior periventricular white matter and asymmetrical distribution in the parieto-occipital white matter The child died and was subsequently diagnosed to have molybdenum cofactor deficiency
Cranial sonography in 5-day old term with HIE with increase in echogenicity of white matter consistent with edemaCD ultrasound shows reversal of diastolic flow reflecting increased vascular resistance secondary to edema
PVL in a preterm infant (a) Coronal head US image obtained in the 1st week of life shows increased echogenicity in the periventricular white matter (arrows) (b) Follow-up US image obtained 2 months later shows development of cystic changes in these regions and dilatation of the adjacent lateral ventricles findings that are consistent with PVL
CT images show decrease In basal ganglia density related to Cytotoxic edemaSubtle loss of the normally sharp Transition from grey matter to White matter at the corticomedullary Junction Cerebral edema seen with effacementof the cortical sulci and the sylvian Fissures
PVL in a preterm neonate Axial T1-weighted (a) and T2-weighted (b) MR images obtained on day 4 of life demonstrate T1 hypointensity and T2 hyperintensity in the periventricular whitematter Note the punctate foci of high signal intensity on the T1-weighted image (arrows in a) These foci should be distinguished from foci of hemorrhage whichwould demonstrate greater T2 shortening on the corresponding T2-weighted image
28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

Advanced technique Perfusion
Arterial Spin-Labeled (ASL) Perfusion bullRecent advances in novel research imaging modalitybullallows noninvasive evaluation of CBF (cerebral blood flow) using electromagnetically labeled arterial blood water as an endogenous contrast agent bullDemonstrates low CBF in neonates who have suffered HIE and in infants and children after stroke
Imaging RecommendationCranial sonography (US) bullFirst between 7 and 14 days bullRepeat before discharge from the hospital MRI DWI MRS bullWhen US is abnormal MRI precise lesion extension and aide in prognosticating bull Defining injury in VLBW neonates with normal US
PrognosisPoor outcome if bullIVH plus PVL bullPVL with volume loss widespread infarction or seizures bullPVL with enlarged cysts
It is necessary to bullknow the normal cerebral appearance before interpret pathological aspect bulldistinguish hypoxic-ischemic brain damage from normal myelination Brain compositionChanges in brain composition Changes in cellular density increase in complex lipids content due to the evolving process of myelination decrease in water content mostly in the WM
Shortening of T1 Shortening of T2
Imaging PatternThe imaging patterns of HIE can be classified into 3 types Lesions predominantly located in the PVWM Lesions predominantly located in the basal ganglia or thalamus Multicystic encephalomalcia The pattern of injury is postulated to depend on bull The type of hypoxiandashischaemia (acute and profound or prolonged and partial) bullThe gestational age (term or pre-term)
HIE in preterm infantRisk FactorsPregnancy Gestational ageweight previous preterm birth spontaneous preterm labor Intrapartum Abruption pre-eclampsia premature rupture of membranes chorioamnionitis group B Strep Peri amp postnatal factors Respiratory distress sepsis anemia apnea bradycardia cardiac arrest
General Features++ PVL +- associated to Germinal matrix and IVH PV hemorrhagic infarction Cerebellar infarction Definition bullPVL is the HIE driven periventricular white matter (PVWM) necrosis seen in very low birth weight premies (lt1500g) EpidemiologybullBirth weight lt 1500 g 45 incidence of PVL (higher if associated with IVH) bullGestational age lt 33 weeks 38 incidence of PVL bullgt 50 of patients with PVL or grade III IVH develop cerebral palsy
Cranial ultrasound coronal view day 1 showing severe echogenicity in the white matter MRI (T2SE (TR 6284TE 120) and ADC) performed on day 3 showing increased signal intensity in the white matter on T2SE and low signal intensity in the deep white matter on the ADC map with sparing of the anterior periventricular white matter and asymmetrical distribution in the parieto-occipital white matter The child died and was subsequently diagnosed to have molybdenum cofactor deficiency
Cranial sonography in 5-day old term with HIE with increase in echogenicity of white matter consistent with edemaCD ultrasound shows reversal of diastolic flow reflecting increased vascular resistance secondary to edema
PVL in a preterm infant (a) Coronal head US image obtained in the 1st week of life shows increased echogenicity in the periventricular white matter (arrows) (b) Follow-up US image obtained 2 months later shows development of cystic changes in these regions and dilatation of the adjacent lateral ventricles findings that are consistent with PVL
CT images show decrease In basal ganglia density related to Cytotoxic edemaSubtle loss of the normally sharp Transition from grey matter to White matter at the corticomedullary Junction Cerebral edema seen with effacementof the cortical sulci and the sylvian Fissures
PVL in a preterm neonate Axial T1-weighted (a) and T2-weighted (b) MR images obtained on day 4 of life demonstrate T1 hypointensity and T2 hyperintensity in the periventricular whitematter Note the punctate foci of high signal intensity on the T1-weighted image (arrows in a) These foci should be distinguished from foci of hemorrhage whichwould demonstrate greater T2 shortening on the corresponding T2-weighted image
28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

Imaging RecommendationCranial sonography (US) bullFirst between 7 and 14 days bullRepeat before discharge from the hospital MRI DWI MRS bullWhen US is abnormal MRI precise lesion extension and aide in prognosticating bull Defining injury in VLBW neonates with normal US
PrognosisPoor outcome if bullIVH plus PVL bullPVL with volume loss widespread infarction or seizures bullPVL with enlarged cysts
It is necessary to bullknow the normal cerebral appearance before interpret pathological aspect bulldistinguish hypoxic-ischemic brain damage from normal myelination Brain compositionChanges in brain composition Changes in cellular density increase in complex lipids content due to the evolving process of myelination decrease in water content mostly in the WM
Shortening of T1 Shortening of T2
Imaging PatternThe imaging patterns of HIE can be classified into 3 types Lesions predominantly located in the PVWM Lesions predominantly located in the basal ganglia or thalamus Multicystic encephalomalcia The pattern of injury is postulated to depend on bull The type of hypoxiandashischaemia (acute and profound or prolonged and partial) bullThe gestational age (term or pre-term)
HIE in preterm infantRisk FactorsPregnancy Gestational ageweight previous preterm birth spontaneous preterm labor Intrapartum Abruption pre-eclampsia premature rupture of membranes chorioamnionitis group B Strep Peri amp postnatal factors Respiratory distress sepsis anemia apnea bradycardia cardiac arrest
General Features++ PVL +- associated to Germinal matrix and IVH PV hemorrhagic infarction Cerebellar infarction Definition bullPVL is the HIE driven periventricular white matter (PVWM) necrosis seen in very low birth weight premies (lt1500g) EpidemiologybullBirth weight lt 1500 g 45 incidence of PVL (higher if associated with IVH) bullGestational age lt 33 weeks 38 incidence of PVL bullgt 50 of patients with PVL or grade III IVH develop cerebral palsy
Cranial ultrasound coronal view day 1 showing severe echogenicity in the white matter MRI (T2SE (TR 6284TE 120) and ADC) performed on day 3 showing increased signal intensity in the white matter on T2SE and low signal intensity in the deep white matter on the ADC map with sparing of the anterior periventricular white matter and asymmetrical distribution in the parieto-occipital white matter The child died and was subsequently diagnosed to have molybdenum cofactor deficiency
Cranial sonography in 5-day old term with HIE with increase in echogenicity of white matter consistent with edemaCD ultrasound shows reversal of diastolic flow reflecting increased vascular resistance secondary to edema
PVL in a preterm infant (a) Coronal head US image obtained in the 1st week of life shows increased echogenicity in the periventricular white matter (arrows) (b) Follow-up US image obtained 2 months later shows development of cystic changes in these regions and dilatation of the adjacent lateral ventricles findings that are consistent with PVL
CT images show decrease In basal ganglia density related to Cytotoxic edemaSubtle loss of the normally sharp Transition from grey matter to White matter at the corticomedullary Junction Cerebral edema seen with effacementof the cortical sulci and the sylvian Fissures
PVL in a preterm neonate Axial T1-weighted (a) and T2-weighted (b) MR images obtained on day 4 of life demonstrate T1 hypointensity and T2 hyperintensity in the periventricular whitematter Note the punctate foci of high signal intensity on the T1-weighted image (arrows in a) These foci should be distinguished from foci of hemorrhage whichwould demonstrate greater T2 shortening on the corresponding T2-weighted image
28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

It is necessary to bullknow the normal cerebral appearance before interpret pathological aspect bulldistinguish hypoxic-ischemic brain damage from normal myelination Brain compositionChanges in brain composition Changes in cellular density increase in complex lipids content due to the evolving process of myelination decrease in water content mostly in the WM
Shortening of T1 Shortening of T2
Imaging PatternThe imaging patterns of HIE can be classified into 3 types Lesions predominantly located in the PVWM Lesions predominantly located in the basal ganglia or thalamus Multicystic encephalomalcia The pattern of injury is postulated to depend on bull The type of hypoxiandashischaemia (acute and profound or prolonged and partial) bullThe gestational age (term or pre-term)
HIE in preterm infantRisk FactorsPregnancy Gestational ageweight previous preterm birth spontaneous preterm labor Intrapartum Abruption pre-eclampsia premature rupture of membranes chorioamnionitis group B Strep Peri amp postnatal factors Respiratory distress sepsis anemia apnea bradycardia cardiac arrest
General Features++ PVL +- associated to Germinal matrix and IVH PV hemorrhagic infarction Cerebellar infarction Definition bullPVL is the HIE driven periventricular white matter (PVWM) necrosis seen in very low birth weight premies (lt1500g) EpidemiologybullBirth weight lt 1500 g 45 incidence of PVL (higher if associated with IVH) bullGestational age lt 33 weeks 38 incidence of PVL bullgt 50 of patients with PVL or grade III IVH develop cerebral palsy
Cranial ultrasound coronal view day 1 showing severe echogenicity in the white matter MRI (T2SE (TR 6284TE 120) and ADC) performed on day 3 showing increased signal intensity in the white matter on T2SE and low signal intensity in the deep white matter on the ADC map with sparing of the anterior periventricular white matter and asymmetrical distribution in the parieto-occipital white matter The child died and was subsequently diagnosed to have molybdenum cofactor deficiency
Cranial sonography in 5-day old term with HIE with increase in echogenicity of white matter consistent with edemaCD ultrasound shows reversal of diastolic flow reflecting increased vascular resistance secondary to edema
PVL in a preterm infant (a) Coronal head US image obtained in the 1st week of life shows increased echogenicity in the periventricular white matter (arrows) (b) Follow-up US image obtained 2 months later shows development of cystic changes in these regions and dilatation of the adjacent lateral ventricles findings that are consistent with PVL
CT images show decrease In basal ganglia density related to Cytotoxic edemaSubtle loss of the normally sharp Transition from grey matter to White matter at the corticomedullary Junction Cerebral edema seen with effacementof the cortical sulci and the sylvian Fissures
PVL in a preterm neonate Axial T1-weighted (a) and T2-weighted (b) MR images obtained on day 4 of life demonstrate T1 hypointensity and T2 hyperintensity in the periventricular whitematter Note the punctate foci of high signal intensity on the T1-weighted image (arrows in a) These foci should be distinguished from foci of hemorrhage whichwould demonstrate greater T2 shortening on the corresponding T2-weighted image
28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

Imaging PatternThe imaging patterns of HIE can be classified into 3 types Lesions predominantly located in the PVWM Lesions predominantly located in the basal ganglia or thalamus Multicystic encephalomalcia The pattern of injury is postulated to depend on bull The type of hypoxiandashischaemia (acute and profound or prolonged and partial) bullThe gestational age (term or pre-term)
HIE in preterm infantRisk FactorsPregnancy Gestational ageweight previous preterm birth spontaneous preterm labor Intrapartum Abruption pre-eclampsia premature rupture of membranes chorioamnionitis group B Strep Peri amp postnatal factors Respiratory distress sepsis anemia apnea bradycardia cardiac arrest
General Features++ PVL +- associated to Germinal matrix and IVH PV hemorrhagic infarction Cerebellar infarction Definition bullPVL is the HIE driven periventricular white matter (PVWM) necrosis seen in very low birth weight premies (lt1500g) EpidemiologybullBirth weight lt 1500 g 45 incidence of PVL (higher if associated with IVH) bullGestational age lt 33 weeks 38 incidence of PVL bullgt 50 of patients with PVL or grade III IVH develop cerebral palsy
Cranial ultrasound coronal view day 1 showing severe echogenicity in the white matter MRI (T2SE (TR 6284TE 120) and ADC) performed on day 3 showing increased signal intensity in the white matter on T2SE and low signal intensity in the deep white matter on the ADC map with sparing of the anterior periventricular white matter and asymmetrical distribution in the parieto-occipital white matter The child died and was subsequently diagnosed to have molybdenum cofactor deficiency
Cranial sonography in 5-day old term with HIE with increase in echogenicity of white matter consistent with edemaCD ultrasound shows reversal of diastolic flow reflecting increased vascular resistance secondary to edema
PVL in a preterm infant (a) Coronal head US image obtained in the 1st week of life shows increased echogenicity in the periventricular white matter (arrows) (b) Follow-up US image obtained 2 months later shows development of cystic changes in these regions and dilatation of the adjacent lateral ventricles findings that are consistent with PVL
CT images show decrease In basal ganglia density related to Cytotoxic edemaSubtle loss of the normally sharp Transition from grey matter to White matter at the corticomedullary Junction Cerebral edema seen with effacementof the cortical sulci and the sylvian Fissures
PVL in a preterm neonate Axial T1-weighted (a) and T2-weighted (b) MR images obtained on day 4 of life demonstrate T1 hypointensity and T2 hyperintensity in the periventricular whitematter Note the punctate foci of high signal intensity on the T1-weighted image (arrows in a) These foci should be distinguished from foci of hemorrhage whichwould demonstrate greater T2 shortening on the corresponding T2-weighted image
28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

HIE in preterm infantRisk FactorsPregnancy Gestational ageweight previous preterm birth spontaneous preterm labor Intrapartum Abruption pre-eclampsia premature rupture of membranes chorioamnionitis group B Strep Peri amp postnatal factors Respiratory distress sepsis anemia apnea bradycardia cardiac arrest
General Features++ PVL +- associated to Germinal matrix and IVH PV hemorrhagic infarction Cerebellar infarction Definition bullPVL is the HIE driven periventricular white matter (PVWM) necrosis seen in very low birth weight premies (lt1500g) EpidemiologybullBirth weight lt 1500 g 45 incidence of PVL (higher if associated with IVH) bullGestational age lt 33 weeks 38 incidence of PVL bullgt 50 of patients with PVL or grade III IVH develop cerebral palsy
Cranial ultrasound coronal view day 1 showing severe echogenicity in the white matter MRI (T2SE (TR 6284TE 120) and ADC) performed on day 3 showing increased signal intensity in the white matter on T2SE and low signal intensity in the deep white matter on the ADC map with sparing of the anterior periventricular white matter and asymmetrical distribution in the parieto-occipital white matter The child died and was subsequently diagnosed to have molybdenum cofactor deficiency
Cranial sonography in 5-day old term with HIE with increase in echogenicity of white matter consistent with edemaCD ultrasound shows reversal of diastolic flow reflecting increased vascular resistance secondary to edema
PVL in a preterm infant (a) Coronal head US image obtained in the 1st week of life shows increased echogenicity in the periventricular white matter (arrows) (b) Follow-up US image obtained 2 months later shows development of cystic changes in these regions and dilatation of the adjacent lateral ventricles findings that are consistent with PVL
CT images show decrease In basal ganglia density related to Cytotoxic edemaSubtle loss of the normally sharp Transition from grey matter to White matter at the corticomedullary Junction Cerebral edema seen with effacementof the cortical sulci and the sylvian Fissures
PVL in a preterm neonate Axial T1-weighted (a) and T2-weighted (b) MR images obtained on day 4 of life demonstrate T1 hypointensity and T2 hyperintensity in the periventricular whitematter Note the punctate foci of high signal intensity on the T1-weighted image (arrows in a) These foci should be distinguished from foci of hemorrhage whichwould demonstrate greater T2 shortening on the corresponding T2-weighted image
28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

General Features++ PVL +- associated to Germinal matrix and IVH PV hemorrhagic infarction Cerebellar infarction Definition bullPVL is the HIE driven periventricular white matter (PVWM) necrosis seen in very low birth weight premies (lt1500g) EpidemiologybullBirth weight lt 1500 g 45 incidence of PVL (higher if associated with IVH) bullGestational age lt 33 weeks 38 incidence of PVL bullgt 50 of patients with PVL or grade III IVH develop cerebral palsy
Cranial ultrasound coronal view day 1 showing severe echogenicity in the white matter MRI (T2SE (TR 6284TE 120) and ADC) performed on day 3 showing increased signal intensity in the white matter on T2SE and low signal intensity in the deep white matter on the ADC map with sparing of the anterior periventricular white matter and asymmetrical distribution in the parieto-occipital white matter The child died and was subsequently diagnosed to have molybdenum cofactor deficiency
Cranial sonography in 5-day old term with HIE with increase in echogenicity of white matter consistent with edemaCD ultrasound shows reversal of diastolic flow reflecting increased vascular resistance secondary to edema
PVL in a preterm infant (a) Coronal head US image obtained in the 1st week of life shows increased echogenicity in the periventricular white matter (arrows) (b) Follow-up US image obtained 2 months later shows development of cystic changes in these regions and dilatation of the adjacent lateral ventricles findings that are consistent with PVL
CT images show decrease In basal ganglia density related to Cytotoxic edemaSubtle loss of the normally sharp Transition from grey matter to White matter at the corticomedullary Junction Cerebral edema seen with effacementof the cortical sulci and the sylvian Fissures
PVL in a preterm neonate Axial T1-weighted (a) and T2-weighted (b) MR images obtained on day 4 of life demonstrate T1 hypointensity and T2 hyperintensity in the periventricular whitematter Note the punctate foci of high signal intensity on the T1-weighted image (arrows in a) These foci should be distinguished from foci of hemorrhage whichwould demonstrate greater T2 shortening on the corresponding T2-weighted image
28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

Cranial ultrasound coronal view day 1 showing severe echogenicity in the white matter MRI (T2SE (TR 6284TE 120) and ADC) performed on day 3 showing increased signal intensity in the white matter on T2SE and low signal intensity in the deep white matter on the ADC map with sparing of the anterior periventricular white matter and asymmetrical distribution in the parieto-occipital white matter The child died and was subsequently diagnosed to have molybdenum cofactor deficiency
Cranial sonography in 5-day old term with HIE with increase in echogenicity of white matter consistent with edemaCD ultrasound shows reversal of diastolic flow reflecting increased vascular resistance secondary to edema
PVL in a preterm infant (a) Coronal head US image obtained in the 1st week of life shows increased echogenicity in the periventricular white matter (arrows) (b) Follow-up US image obtained 2 months later shows development of cystic changes in these regions and dilatation of the adjacent lateral ventricles findings that are consistent with PVL
CT images show decrease In basal ganglia density related to Cytotoxic edemaSubtle loss of the normally sharp Transition from grey matter to White matter at the corticomedullary Junction Cerebral edema seen with effacementof the cortical sulci and the sylvian Fissures
PVL in a preterm neonate Axial T1-weighted (a) and T2-weighted (b) MR images obtained on day 4 of life demonstrate T1 hypointensity and T2 hyperintensity in the periventricular whitematter Note the punctate foci of high signal intensity on the T1-weighted image (arrows in a) These foci should be distinguished from foci of hemorrhage whichwould demonstrate greater T2 shortening on the corresponding T2-weighted image
28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

Cranial sonography in 5-day old term with HIE with increase in echogenicity of white matter consistent with edemaCD ultrasound shows reversal of diastolic flow reflecting increased vascular resistance secondary to edema
PVL in a preterm infant (a) Coronal head US image obtained in the 1st week of life shows increased echogenicity in the periventricular white matter (arrows) (b) Follow-up US image obtained 2 months later shows development of cystic changes in these regions and dilatation of the adjacent lateral ventricles findings that are consistent with PVL
CT images show decrease In basal ganglia density related to Cytotoxic edemaSubtle loss of the normally sharp Transition from grey matter to White matter at the corticomedullary Junction Cerebral edema seen with effacementof the cortical sulci and the sylvian Fissures
PVL in a preterm neonate Axial T1-weighted (a) and T2-weighted (b) MR images obtained on day 4 of life demonstrate T1 hypointensity and T2 hyperintensity in the periventricular whitematter Note the punctate foci of high signal intensity on the T1-weighted image (arrows in a) These foci should be distinguished from foci of hemorrhage whichwould demonstrate greater T2 shortening on the corresponding T2-weighted image
28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

PVL in a preterm infant (a) Coronal head US image obtained in the 1st week of life shows increased echogenicity in the periventricular white matter (arrows) (b) Follow-up US image obtained 2 months later shows development of cystic changes in these regions and dilatation of the adjacent lateral ventricles findings that are consistent with PVL
CT images show decrease In basal ganglia density related to Cytotoxic edemaSubtle loss of the normally sharp Transition from grey matter to White matter at the corticomedullary Junction Cerebral edema seen with effacementof the cortical sulci and the sylvian Fissures
PVL in a preterm neonate Axial T1-weighted (a) and T2-weighted (b) MR images obtained on day 4 of life demonstrate T1 hypointensity and T2 hyperintensity in the periventricular whitematter Note the punctate foci of high signal intensity on the T1-weighted image (arrows in a) These foci should be distinguished from foci of hemorrhage whichwould demonstrate greater T2 shortening on the corresponding T2-weighted image
28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

CT images show decrease In basal ganglia density related to Cytotoxic edemaSubtle loss of the normally sharp Transition from grey matter to White matter at the corticomedullary Junction Cerebral edema seen with effacementof the cortical sulci and the sylvian Fissures
PVL in a preterm neonate Axial T1-weighted (a) and T2-weighted (b) MR images obtained on day 4 of life demonstrate T1 hypointensity and T2 hyperintensity in the periventricular whitematter Note the punctate foci of high signal intensity on the T1-weighted image (arrows in a) These foci should be distinguished from foci of hemorrhage whichwould demonstrate greater T2 shortening on the corresponding T2-weighted image
28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

PVL in a preterm neonate Axial T1-weighted (a) and T2-weighted (b) MR images obtained on day 4 of life demonstrate T1 hypointensity and T2 hyperintensity in the periventricular whitematter Note the punctate foci of high signal intensity on the T1-weighted image (arrows in a) These foci should be distinguished from foci of hemorrhage whichwould demonstrate greater T2 shortening on the corresponding T2-weighted image
28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

28-week-old 1100-g infant Initial MR images A (T2-weighted SE [30001201]) and BndashD (T1-weighted SE [400152]) at 38 weeks corrected age show multiple spots of periventricular T1 and T2 shortening (black arrows) with cyst formation (white arrows) and an irregular contour to the ventricular wall Follow-up MR images E and F (T2-weighted SE [30001001]) at 15 months postconceptional age reveal marked irregularity of the ventricular wall white matter loss and periventricular T2 prolongation (arrows) The infant developed a spastic diplegia
28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

28-week-old 1355-g infant Initial MR images A and B (T2-weighted SE [30001201]) and C and D (T1-weighted SE [400152]) at 38 weeks corrected age show large germinal matrix region hemosiderin deposit (arrowhead) with adjacent multiple encephaloclastic cysts (arrows) diffuse hemosiderin deposition along the lateral ventricle ventriculomegaly and absence of periventricular parenchymal signal change Follow-up MR images E and F (T2-weighted SE [30001001]) at 12 months corrected age reveal right periventricular hemosiderin deposition (arrowheads) ventriculomegaly and parenchymal destruction involving the left deep gray matter Also note the periventricular T2 prolongation (arrows) with white matter volume loss The infant developed a spastic diplegia with hemiparesis
HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

HIE in term infant
Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

Severe HII in a 6-yearoldchild (a) Unenhanced CT scanobtained at the level of the basal ganglia after cardiopulmonary arrest that lasted 30 minutes is essentially unremarkable (b) On an unenhanced CT scan obtained just inferior to but contemporaneously with a the cerebellum appears slightly hyperattenuating relative to the rest of the brain This finding is another example of the white cerebellum sign as an early CT indicator of HII (c d) Diffusion-weighted (c) and T2-weighted (d) MR images obtained 4 days later show high signal intensity with corresponding T2 abnormalities in the caudate nuclei (white arrows) lentiform nuclei (black arrows) and occipital lobes ( in c)
CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

CT Scan show Hyperdense thalami Cortical atrophy Ex vacuo dilatation of lateral ventricle with undulating walls suggestive of Gliosis and paucity of periventricular white matter - Periventricular leukomalacia
Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

Full-term infant with acute sentinel event (ruptured uterus) with MRI pattern suggestive of acute near total asphyxia a Inversion recovery sequence (TR 5038TE 30TI 600) does not show a normal signal within the posterior limb of the internal capsule but areas of increased signal intensity within thalami and basal ganglia DWI (bndashd) shows restricted diffusion in the ventrolateral thalami lentiform nuclei cerebral peduncles and in the perirolandic cortex Also note involvement of the hippocampi
Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

Full-term infant with lsquowhite brainrsquo pattern of injury a c T2SE (TR 6284TE 120) shows increased signal intensity in the white matter with loss of cortical ribbon There is relative sparing of the basal ganglia and immediate periventricular white matter DWI (b d) confirms the abnormalities and shows a striking discrepancy in signal intensity with the cerebellum Note high-signal intensity of the mesencephalon (c) on T2SE and symmetrical restricted diffusion in the cerebral peduncles and also in the cerebellum (d)
A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

A 14yo with delayed milestones showing bilateral peri rolandic cortical and occipital cortical Gliosis suggestive of Perinatal Hypoxic Ischemic injury
End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

End-stage PVL in a 9-yearold child who presented with motor and cognitive delay and seizures The patient was born at 32 weeks gestational age Axial fluid-attenuated inversion recovery MR images demonstrate increased signal intensity and a few tiny cysts in the immediate periventricular white matter In b there is enlargement of the atria of the lateral ventricles with a decrease in volume of the adjacent white matter and the walls of the lateral ventricles have a wavy appearance
Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

Color coded white matter directions and FA images The inset indicates the level of horizontal sections displayed in A and B Genu most anterior region of the corpus callosum ALIC anterior limb of the internal capsule PLIC posterior limb of the internal capsule Splenium the most posterior portion of the corpus callosum Isthmus region of the corpus callosum just anterior of the splenium (A) The colors indicate the direction of white matter fibers with blue left-right red anteroposterior and green cranial-caudal (point out from the plane of the page) (B) The intensity corresponds to FA Black corresponds to FA 0 and the higher the FA value the whiter the image
Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

Hypoxic-ischemic encephalopathy From left to right Bilateral basal ganglia hyperintense rounded signal in axial FLAIR T2 images with restricted diffusion hyperintense in DW images and with low ADC values
Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

Delayed leukoencephalopathy after acute carbon monoxide intoxication
Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

Fibre tractography of hypoxic-ischemic leuckoenecephalopathy
Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

Sagittal image of a childwith PVL grade 1
Transverse and sagittal image of a child with PVL grade 2
Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

Sagittal image demonstrating extensive PVL grade 3
Coronal and transverse images demonstrating PVL grade 4
Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

Born at 37 weeks following antenatal diagnosis of fetal supraventricular tachycardia MRI T2SE (TR 6284TE 120) performed on day 3 shows a large left-sided middle cerebral artery infarct of antenatal onset with evidence of Wallerian degeneration and presence of cysts within the area of infarction Diffusion tensor tractography shows loss of fibers with the corticospinal tract of the affected hemisphere
MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

MR spectroscopyBiochemical analysis of the (compromised anaerobic) cerebral tissuesElevated lactate and diminished N-acetyl-aspartate NAA concentrationElevation of choline relative to creatineLactate-choline ratio of 1 indicate a greater than 95 probability of adverse neurodevelopmental outcome
MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

MR spectroscopy of a singlevoxel at 35 msec demonstrate non-specific accumulation of metabolite at 12-13 ppmSpectrum at an echo time of 144 msec shows inversion of the same metabolite which is characteristic for lactate
Thank You

Thank You