Presentation on mi
-
Upload
laxmirani -
Category
Health & Medicine
-
view
590 -
download
0
description
Transcript of Presentation on mi

Acute Myocardial Ischemia

•CASE PRESENTATION
•ACUTE MYOCARDIAL INFARCTION
• Definition• Etiology• Pathophysiology • Clinical features• Diagnosis• Management• Complication• Nursing care

Case :
55 yr/M alcoholic and smoker
Presented with: pain in Left side of chest since 5 am radiating to lt. shoulder and back

O/E GCS fairP-76BP 130/84
S/E : WNL
Inv: Hb- 12.9 TLC-6700BLOOD SUGAR Random 146 Urine normalUrea-25Creatinine -0.9
CKMB 28 Trop T - negative
ECG:Chest x ray: WNL
Pt was prescribed tab. Pantocid and syp DigeneAnd was send for TMT from ECHS empanelled hospital

At around 5 pm the same evening he came back with
severe chest pain following TMT2 episodes of vomitingexcessive sweatingand TMT positive for provocation
Pt was admitted to ICU and was investigated:pulse : 97BP: 110/72mm hgresp:26
Chest : B/L basal crepts +CVSCNS WNLP/A

Inv: Trop T : positiveCKMB : 98 ---- 110 next morningSGOT : 140SGPT: 72
ECG: Q waves in lead 2, 3, aVf, V1- V2

Inj LMWH : 1 mg / kg SC BD
Inj NTG infusion : 5 mcg/ min till pain free
Atorvastatin : 40 mg stat and OD
Clopidogrel : 75 mg BD
Ecosprin 1 stat and OD
Beta blocker: Metaprolol : 12.5 mg BD
Thrombolysed using Streptokinase
Management

DIAGNOSIS:
ANT, INF wall MI

DEFINITION:-
is the rapid development of myocardial necrosis by a critical imbalance between oxygen supply and demand to the myocardium
Myocardial Infarction ,
Commonly known as HEART ATTACK

Classification
• Acute coronary syndromes include ST-elevation MI (STEMI) Non ST-elevation MI ( NSTEMI) Unstable Angina

Classification
• Anatomic or morphologic Transmural= Full thickness Non-transmural= Partial thickness
• ECG Q wave MI Non Q wave MI Does not distinguish transmural from a non-
transmural MI as determined by pathology

Risk Factors
• Smoking• Family history• Hypertension• Diabetes mellitus• Elevated triglycerides and cholesterol levels• Obesity• Sedentary lifestyle• Aging• Stress• Men more than women (but women are increasing)

Causes
• Athrosclerosis (90%)• Constriction or spasm of the coronary artery• Coronary artery embolus• Coronary artery thrombus

Pathophysiology
• 90% - coronary artery thrombosis• 10% - vasospasm• Irreversible cell death occurs within 20-40
minutes of cessation of blood flow• Wavefront of cellular death proceeds from
endocardium to epicardium

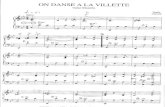
FIGURE 25-1 Determinants of myocardial oxygen supply and demand.

Pathophysiology
• Wavefront produces zones– Zone of necrosis– Zone of injury– Zone of ischemia
• Amount of damage/necrosis depends on duration of occlusion, which artery is blocked, degree of collateral blood flow

Zones of Ischemia Injury and Infarction with Transmural and Subendocardial Infarction

Clinical Presentation
• Chest pain• Associated signs/symptoms• Physical examination

Clinical PresentationChest pain
• Approximately 80% experience chest pain• Pain is similar to angina, but usually more
severe, lasting greater than 30 minutes, not relieved by NTG or rest

Rough diagram of pain zones
(Dark red = most typical (light red = other possible area) area)

Clinical PresentationAssociated Symptoms/Signs
• Nausea/Vomiting – irritation to diaphragm/vagal stimulation
• Profound weakness, cold perspiration, sense of doom
• Dizziness• Palpitations• Dyspnea

Physical Examination
• Anxious, restless• Skin may be cool, clammy, pale• HR – Tachy or Brady• Pulse changes – Decreased quality,
irregularities• Blood pressure – Elevated or Lowered• Heart sounds – S3, S4, Systolic murmur,
pericardial friction rub• Signs of LV dysfunction – congestion,
peripheral hypoperfusion

Diagnostic ECG
• 12 lead ECG over several days shows changes in 75% of patients
• Initially only 24-60% present with changes• Diagnosis may be difficult with previous
infarctions


Diagnosis: ECG
• Zone of Ischemia– T wave inversion– T wave inverts in leads facing ischemic zone and
are upright in leads on opposite side of the heart– Usually symmetrical shape

Diagnosis: ECG
• Zone of Injury– ST segment elevation– ST segment elevation seen in leads facing
injury zone– ST segment depression in opposite leads– Elevation is 1mm or greater in two contiguous
leads– ST elevation in multiple leads is suggestive of
pericarditis

Diagnosis: ECG
• Zone of Infarction – Q waves– Dead tissue does not depolarize– Q wave criteria• >0.03 seconds wide• Depth is at least 25% height of total QRS

Acute MI: ECG Changes

Diagnosis
• Progression of ECG changes in typical Q wave MI– ST segment elevation is usually seen first– T wave inversion occurs within hours and
may be present for months to life–Q wave appears within hours. Usually
permanently

V1
II
Lead
Normal ST SegmentElevation
(minutes to hours)
T Wave Inversion(hours)
Old MIQ WaveDevelopment
(hours to days)
Normal ST SegmentElevation
(minutes to hours)
T Wave Inversion(hours)
Q WaveDevelopment
(hours to days)
Old MI
Evolution of Myocardial Infarction


Region Leads
Inferior wall II , III , aVF
Anterior wall V2 – V5
Lateral wall I , aVL , V6
Posterior wall V1
Rt. Ventricular V1R – V6R

Anatomical Leads
L
I
A
L

Acute Anterior MI

Acute Inferior MI

Acute Posterior MI

Cardiac Biomarkers
• AMI damages cell membranes, releasing chemicals into plasma within 30-60 minutes
• The height and duration of these changes usually correlates with the size of AMI if allowed to run full course

Diagnosis:Cardiac Biomarkers
• Traditional biomarkers
• CK (CPK) – creatinine phosphokinase– Composed of 3 isoenzymes: MB, MM, BB– CK-MB is very sensitive to myocardial injury

Diagnosis:Cardiac Biomarkers
• Traditional biomarkers
• LDH – lactic dehydrogenase– Consists of 5 isoenzymes; LDH 1 being most
reliable for myocardial damage– Increase in LDH 1 occurs after CK elevation

Diagnosis:Cardiac Biomarkers
• Newer biochemical markers• Myoglobin– Found in both heart and skeletal muscles; rises
within 2 hours, not specific to exclude skeletal damage
• Troponin – Structural protein only found in cardiac muscle– Negative if 0 - .6mg/ml; positive if 1.5ng/ml or
greater

Acute MI: Serum Markers
First Detectable
Peak Duration
Troponin I 2-4 hrs 10-24 hrs 5-10 days
Troponin T 2-4 hrs 10-24 hrs 5-14 days
CK-MB 3-4 hrs 10-24 hrs 2-4 days

Acute MI: Serum Markers

Chest X-Ray
• Chest radiography may provide clues to an alternative diagnosis ( aortic dissection or pneumothorax)
• Chest radiography also reveals complications of myocardial infarction such as heart failure

MANAGEMENT:-

Collaborative ManagementGoals of Therapy
• Re-establish supply and demand balance• Limit infarction size• Relieve pain• Prevent/treat complications• Identify and manage risk factors

Initial Management in ED
• Initial evaluation with 12-lead ECG in < 10 minutes• BP, HR monitoring• IV access • Draw blood for serum cardiac markers magnesium,
hematology, lipid profile panel

Acute Therapies
• Recommended in first 10 minutes of AMI (“MONA”)
–Oxygen
–Nitroglycerin
–Aspirin–Morphine

Oxygen
• 4-6 liters per nasal cannula to maintain oxygen saturation >90%

Aspirin
• Action– Inhibits platelet aggregation
• Indication– Routinely recommended at earliest opportunity
for all pts with chest pain suspected to be of ischemic etiology
• Dose– 160-325 mg/day (chewable or rectal)

Nitroglycerin
• Actions– Dilate coronary arteries– Venodilator at low doses– Arteriodilator at higher
doses– Decreases pain of
ischemia• Indications– Routine in AMI– Suspected ischemic – Unstable angina– To reduce BP with AMI
• Dose– SL 0.5 mg every 3
min– Initiate IV rate at 5-
10 mcg/min, increasing every 5-10min by 5mcg increments until pain relieved or SBP <100
• Contraindications– With right
ventricular MI– Sinus bradycardia
<50 bpm

Morphine
• Actions– Dilates arteries– Analgesic– Decreases anxiety– Venodilator
• Indications– Continuing pain, not relieved by NTG– Acute pulmonary edema
• Dose– 2-4mg increments every 5-10 minutes until pain
relieved or BP falls• Contraindications– SBP <90– hypovolemia

ACE Inhibitors
• Actions– Reduces preload & afterload– Reduces infarct expansion
• Guidelines for initiation– Give within 12-24 hours– Monitor closely for hypotension– Monitor increase in creatinine level

Beta Blockers• Reduces mortality rates by 20-25% when initiated days to
weeks after AMI• Reduces myocardial demand
– Decreases automaticity. arrhythmias– Decreases HTN– Decreases contractility
• Indications – All patients without
contraindication to B Blockers should be treated within 12 hours of onset of AMI
• Contraindications– Bradycardia or
presence of AV block
– Hypotension– Pulmonary edema– Hx of
bronchospastic disease

Calcium Channel Blockers
• Not recommended as standard first-line therapy
• May be used for significant hypertension or refractory ischemia

Thrombolysis
• Benefit greatest if therapy initiated early • Highly significant reduction in mortality• Benefits patients irrespective of age, gender,
and comorbid conditions• Slightly increased risk of intracerebral
hemorrhage

ThrombolysisCandidates
• Time to therapy 3-6 hours or less• Acute ST-segment elevation• Symptoms consistent with acute MI• Patients without ST-segment elevation should
not receive thrombolytic therapy

Thrombolytic TherapyContraindications
• Active bleeding• Recent major surgery• Stroke within 2 months• Markedly elevated blood pressure• Significant bleeding diathesis

Thrombolytic Agents
• Nonspecific agents deplete coagulation factorsA. StreptokinaseB. Urokinase
C.Anistreplase• Specific agents do not deplete coagulation factors
A. Alteplase (tPA)B. Reteplase

Primary PTCA
• Alternative to thrombolytic therapy if performed in a timely fashion by skilled individuals in high-volume centers
• Reperfusion strategy in patients with risk of bleeding contraindications to thrombolytic therapy

PTCA/Stent
• Clinical Indications– Stable & unstable angina– Evidence of myocardial ischemia upon treadmill
testing– Acute MI


CABG
• Indications– Critical coronary artery obstruction or multiple
ischemic sites– Emergent when hemodynamically unstable as
result of dissecting artery during PTCA

CABG

Complications of MI
Mechanical Electrical
• Acute MR
• RV infarction
• Ventricular septal rupture
• LV thrombus
• Pericarditis
• Brady arrythmias
• Tachy arrythmias

Post MI Prognosis
• Left ventricular ejection fraction• Number of diseased coronary arteries• Presence of spontaneous/inducible ischemia• Presence and extent of ventricular ectopy

Nursing ManagementStart a IV line and blood samples to be taken as per
icu protocol of cardiac patient. Administer oxygen to relieve dyspnea and prevent
arrhythmias.Provide bed rest with semi fowler’s position to
decrease cardiac output.Moniter ECG and hemodynamic procedures.Tablet Aspirin 160-320 mg is given(to chew).
• Asprin alone – reduced mortality 23%
• Asprin with thrombolysis – reduced mortality 42%

Contd.
Nursing Management
Tab sorbitrate 10mg sublingually to be given. Injection morphine 3mg iv can be given ,and .1mg/kg and
total 15mg can be given. NTG drip .5 microgram through infusion pump to be given. Injection streptokinase - 1.5 million units dissolved in
200ml of normal saline over 30-40 minutes. Maintain quiet environment. Anti coagulant as advised. Stool softeners to be given. Anxiety to be relieved.

HEALTH TEACHING ON DISCHARGE
• Patients to take regular medications.• Dietary restrictions—low sodium diet,low
cholesterol,avoidance of caffine.• Risk factors to be explained.• Modifications in life style.• Need to report the following symptoms :-
increased persistent chest pain, dyspnea, weakness, fatigue, persistent palpitation.
• Regular visit to physician as advised.