Pleural Effusion-Individual CP
Transcript of Pleural Effusion-Individual CP

1
Capitol University
Corrales Extension, Cagayan de Oro City
College of Nursing
PLEURAL EFFUSION
SUBMITTED TO:
MR. RICK WILSON BUNAO, RN MN
(Clinical Instructor)
SUBMITTED BY:
KRISTINE MAE U. SUGAROL
RLE 7 GROUP 21
January 19, 2010

2
TABLE OF CONTENTS
I. Introduction………………………………………………..…………….…3
A. General objective…………………………………………………6B. Specific objectives………………………………………………..6C. Scope and limitations……………………………………………6
II. Assessment
A. Patient demographic data………………………………………7B. Assessment tool…………………………………………………8C. Laboratory results……………………………………………….13
III. Anatomy and physiology…………………………………………….…17
IV. Pathophysiology
A. Narrative form…………………………………………………….24B. Schematic Diagram………………………………………………26
V. Medical management
A. Nursing Care Plan……………………………………………….28B. Drug study………………………………………………..………34
VI. Health Teaching ……………….…………………………..……………37
VII. Learning Experience ……………………………………….…….…...38
VIII. Discharge Planning….…………………………………….….………39
IX. Doctor’s Order …………………….……………………………………41
X. References ……………………….………………………………...……42
I. INTRODUCTION

3
Approximately 1 million pleural effusions are diagnosed in the United
States each year. The clinical importance of pleural effusions ranges from incidental
manifestations of cardiopulmonary diseases to symptomatic inflammatory or malignant
diseases (as shown in the image below) requiring urgent evaluation and treatment.
Pleural effusion is excess fluid that accumulates in the pleural cavity, the
fluid-filled space that surrounds the lungs. Excessive amounts of such fluid can impair
breathing by limiting the expansion of the lungs during inhalation.
Pleural fluid normally seeps continually into the pleural space from the
capillaries lining the parietal pleura and is reabsorbed by the visceral pleural capillaries
and lymphatic system. Any condition that interferes with either secretion or drainage of
this fluid leads to pleural effusion.
Causes of pleural effusion can be grouped into four major categories:
Increased systemic hydrostatic pressure (e.g., heart failure)
Reduced capillary oncotic pressure (e.g., liver or renal failure)
Increased capillary permeability (e.g., infections or trauma)
Impaired lymphatic function (e.g., lymphatic obstruction caused by tumor)
Anteroposterior upright chest radiograph shows a massive left-sided pleural effusion with contralateral mediastinal shift.

4
A pleural effusion is an abnormal collection of
fluid in the pleural space resulting from excess fluid
production or decreased absorption. It is the most
common manifestation of pleural disease. The pleural
space is bordered by the parietal and visceral pleurae.
The parietal pleura covers the inner surface of the
thoracic cavity, including the mediastinum, diaphragm,
and ribs. The visceral pleura envelops all lung
surfaces, including the interlobar fissures. The right
and left pleural spaces are separated by the
mediastinum.
The pleural space plays an important role in
respiration by coupling the movement of the chest wall
with that of the lungs in two ways. First, a relative
vacuum in the space keeps the visceral and parietal
pleurae in close proximity. Second, the small volume
of pleural fluid, which has been calculated at 0.13
mL/kg of body weight under normal circumstances, serves as a lubricant to facilitate
movement of the pleural surfaces against each other in the course of respirations. This
small volume of fluid is maintained through the balance of hydrostatic and oncotic
pressure and lymphatic drainage, a disturbance of which may lead to pathology.
Clinical manifestations depend on the amount of fluid present and the
severity of lung compression. If the effusion is small (i.e., 250ml), its presence may be
discovered only on a chest radiograph. With larger effusions, lung expansion may be
restricted, and the client may experience dyspnea, primarily on exertion, and a dry,
nonproductive cough caused by bronchial irritation or mediastinal shift. Tactile fremitus
may be decreased or absent, and percussion notes dull or flat.
Dyspnea is the most common symptom associated with pleural effusion
and is related more to distortion of the diaphragm and chest wall during respiration
than to hypoxemia. In many patients, drainage of pleural fluid alleviates symptoms
despite limited improvement in gas exchange.
Underlying intrinsic lung or heart disease, obstructing endobronchial
lesions or diaphragmatic paralysis can also cause dyspnea, especially after coronary
artery bypass surgery. Drainage of pleural fluid may partially relieve symptoms but also
may allow the underlying disease to be recognized on repeat chest radiographs.

5
Less common symptoms of pleural effusions include mild, nonproductive
cough or chest pain. Other symptoms may suggest the etiology of the pleural effusion.
More severe cough or production of purulent or bloody sputum suggests an underlying
pneumonia or endobronchial lesion. Constant chest wall pain may reflect chest wall
invasion by bronchogenic carcinoma or malignant mesothelioma. Pleuritic chest pain
suggests either pulmonary embolism or an inflammatory pleural process. Systemic
toxicity evidenced by fever, weight loss, and inanition suggests empyema.
Thoracentesis is used to remove excess pleural fluid. The removed fluid is
analyzed to determine whether it is transudate or exudate. Transudates are
substances that have passed through a membrane or tissue surface. They occur
primarily in conditions in which there are protein loss and low protein content (e.g.,
hypoalbuminemia, criihosis, nephrosis) or increased hydrostatic pressure (e.g., heart
failure). Exudates are substances that have escaped from blood vessels. They contain
an accumulation of cells, have a high specific gravity and a high lactate dehydrogenase
(LDH) level, and occur in response to malignancies, infections or inflammatory
processes. Exudates occur when there is an increase in capillary permeability.
Differentiating between transudates and exudates helps establish a specific diagnosis.
Diagnosis may also require analysis of the fluid for white and red blood cells, malignant
cells, bacteria, glucose content, pH, and LDH.
Pleural fluid may be (1) hemorrhagic (or bloody), such as when a tumor is
present or after trauma or pulmonary embolus with infarction; (2) chylous (or thick and
white), such as after lymphatic obstruction or trauma to the thoracic duct; or (3) rich in
cholesterol, such as in chronic, recurrent effusions caused by tuberculosis or
rheumatoid arthritis. If there is a high in WBC count and the pleural fluid is purulent, the
effusion is called emphysema. Emphysema of any volume requires drainage and
treatment of the infection.
If the pus is not drained, it may become thick and almost solidified or
loculated (containing cavities), a condition called fibrothorax.
After the thoracentesis, closed-chest drainage with suction is used to re-
expand the lung rapidly and fill the pleural space. If the fibrous material has restricted
the lung for some time, the lung may not re-expand effectively and further intervention
(usually thoracoplasty) may be needed.

6
A. GENERAL OBJECTIVE
At the end of this case presentation, I will be able to improve knowledge in
various concepts related to my patient’s condition, and skills in careful assessment and
rendering of nursing interventions involved in the management of the client’s case; and
develop positive attitudes as I accomplish my case study using concepts that I have
acquired from our RLE, theory classes and previous related subjects in the BSN
curriculum.
B. SPECIFIC OBJECTIVES
1. Perform a thorough assessment and careful gathering of data that are clinically
significant and will be utilized as reliable cues for our care plans.
2. Further completion of data that will supplement our assessment.
3. Trace and familiarize the pathophysiology of our patient’s disease process.
4. Design individualized nursing care plans based on nursing diagnoses that are
suitable and feasible to carry out.
5. Carry out nursing interventions that are effective, reality based, time-bounded,
achievable and beneficial for our client.
6. Develop a sense of positive thinking in coming up with the case study.
C. SCOPE AND LIMITATION
The study focuses on the assessment, anatomy, and pathophysiology and
its diagram, nursing care plans, discharge plan, prognosis, recommendation and
conclusion revolving around the diagnosis of the patient which is Pleural Effusion
probably secondary to pneumonia.
This study is limited only to the available records found on the patient’s
chart and the information being provided for by the family members present at the
patient’s room during the time of assessment. Other factors that will also be considered

7
as limitations to this study would include the short-duration of time given for ICU
rotation.
II. ASSESSMENT
A. PATIENT DEMOGRAPHIC PROFILE
Patient Demographic Profile
Name of patient: Panugaling, Jonathan Castro
Age: 27 years old
Birthday: July 2, 1982
Sex: Male
Address: Purok 3-C Baloy, Tablon, Cagayan de Oro City, Misamis Oriental
Civil status: Single
Height: NA
Weight: NA
Language spoken: Visayan
Educational Attainment: Elementary Graduate
Religion: Roman Catholic
Nationality: Filipino
Name of Father: Felipe Panugaling
Name of Mother: Saturnina Monte Castro
Occupation: barber
Income: P1700/month
Chief complaint: cough and fever
Name of Hospital: Northern Mindanao Medical Center
Date of Admission: January 7, 2010 (11:00pm)
Name of Attending Physician: Dr. Sarmiento

8
Admitting Diagnosis:
Pleural Effusion probably secondary to Pneumonia
B. ASSESSMENT TOOL
VITAL SIGNS:
Temperature: 36.7°c
Pulse Rate: 64 BPM
Respiratory Rate: 24 CPM
Blood Pressure: 120/190 mmHg
Weight: NA
Height: NA
GENERAL DATA:
A case of 27 y.o., male, single, Roman Catholic from Tablon, Cagayan de
Oro City, admitted for the 1st time due to cough
Source of information:
Patient: 90% reliability
HISTORY OF PRESENT ILLNESS:
5 days PTA, noted to have cough, productive of whitish phlegm
associated with fever, on and off, low to moderate grade and back pains on the left.
Consult done at the Family Medicine OPD. Work up done with CXR which revealed
pleural effusion L. Patient refused in our institution for further evaluation and
management. Hence this admission,
( + ) occasional SOB ( + ) easy fatigue ability
( - ) chest pain
PAST MEDICAL HISTORY:
Previous admission due to vehicular accident 2007 Head injury sutured
( - ) operation
Non asthmatic

9
Non diabetic
Non hypertensive
( - ) food/drug allergy
( - ) illness
FAMILY HISTORY:
( + ) HPN (paternal)
PERSONAL / SOCIAL HISTORY:
Non smoker but occasional alcoholic beverage drinks
Single, barber
FUNCTION HEALTH PATTERNS
ACTIVITY-EXERCISE PATTERN
Pt.X pericordial area is flat; PMI is best heard at 5th ICS midclavicular line with
apical rate of 142bpm. Her peripheral pulse is symmetrical, palpable, and regular & her
capillary refill is 2sec. No pacemaker attached & hemodynamic monitoring but Chest
Thoracostomy Tube (CTT) is attached at the left mid-axillary line of the patient’s body.
Has O2 inhalation attached to patient’s nose upon assessment.
Pt. X is in irregular breathing pattern of 33cpm upon assessment. The lung
expansion is asymmetrical, with diminished or delayed expansion on the side of effusion
which is at the left.
Pt. X ADL is in total dependence and mobility status is limited because of fear of
injury to the site of the CTT. Pt. X back & extremities has no deformities but ROM is
also limited. The spine is in the midline.

10
NUTRITION & METABOLIC PATTERN
Prior to admission pt. X has no special diet. Does not have any supplement
rather than Ferrous sulfate.
Pt. X mouth & mucosa are pinkish; tongue is in the midline. Uvula is in the
midline & pinkish, tonsils are not inflamed. The trachea is in the midline with non-
palpable thyroids & minimal ROM on bed.
Pt. X skin general color is pallor, rough, firm, warm to touch. Patient has an
ongoing IVF of PNSS 940cc regulated at 30gtts/min. Patient has also a surgical wound
(suture) in the left mid-axillary line where Chest Thoracostomy Tube is attached with
drainage of 590 level in bloody color.
ELIMINATION PATTERN
During admission pt. X defecates 1 time with yellow, slightly firm stool at medium
amount. Last bowel movement on January 13, 2010; and the day of assessment was
January 14, 2010. No incontinence & any method use to manage bowel movement
noted.
The abdomen is symmetrical but flat and normoactive without any abnormal
findings upon palpation. Pt. X usually urinates 1-2 times a day, appeared in yellow color
and has no problem in urinating. Patient also sweats minimally during afternoon but no
noted excessive perspiration.
SLEEP-REST PATTERN
Pt. X sleeps 7-8 hours at night. There were no histories of sleep disturbances of
the patient. Pt. X is always at the bed and easily drops to sleep.
COGNITIVE-PERCEPTION PATTERN

11
Pt. X is conscious and calm upon assessment and disoriented to time. The head
is normocephalic with symmetrical facial movements & sunken fontanels. Hair is dry
with dandruff seen in the scalp. Pt. X eyelids are asymmetrical, with pink conjunctiva.
No lesions in the cornea & lens & anecteric sclera. Pupils are at equal size with 4mm in
diameter.
Pt. X external pinnae of ears is normoset with cerumen discharge & intact
tympanic membrane. The nasal septum is in the midline with pinkish mucosa & both
patent.
SELF-PERCEPTION & SELF CONCEPT PATTERN
Pt. X feels fine about himself but I observed that he is not. Pt. X is depressed
about himself for being sick and hospitalized.
ROLE-RELATIONSHIP PATTERN
Pt. X lives with his mother, father and younger siblings. When it comes to the
feelings of his family members regarding her illness, pt. X mother felt so sad about her
son’s condition but she tries to understand the nature of the problem and accepts the
fact about the condition of her son. The mother also verbalized that her son needs
support about his present condition.
DAY 1: PHYSICAL ASSESSMENT (Jan. 14, 2010)
SKIN - General color is pallor, rough, firm, and warm to touch.
NAILS
- His nails were pallor but it is firm and convex-shape.
HAIR - Her hair is dry and black, with dandruff.
HEAD - Normocephalic head and facial movements are symmetrical in size- Sunken fontanels.
EYES - He has no edema. Both eyes are coordinated with parallel alignment.- Anicteric sclera and conjunctiva and no abnormal tears noted.
EARS - Normal voice tones audible.

12
- Her ears were symmetrical - There was cerumen noted
NOSE AND SINUSES - There is nasal flaring upon assessment due to SOB- No tender sinuses noted- Gross smell is symmetrical
MOUTH AND THROAT - He has pallor lips, pinkish mucosa - Tongue is in midline with missing teeth- Has pinkish gums
NECK - Trachea is placed midline. Lymph nodes are not palpable.
LUNGS-CHEST WALL - Asymmetric chest expansion, with diminished or delayed expansion on the side
of the effusion- Breaths per minute is 33cpm (abnormal).
Drainage Color: (according to 3-11 shift)
1. Bloody about 320 cc level Jan. 14, 2010
2. Yellowish about 10cc level + 110 water from bottle Jan. 15, 2010
3. Clear yellow about 190 cc level from previous bottle Jan. 16, 2010

13
C. LABORATORY RESULTS:
Hematology Report: Jan. 12, 2010 7:24pm
Test Result Unit Reference Interpretation WBC 5.7 10^3/uL 5.0-10.0 NORMALRBC 4.22 10^6/uL 4.2-5.4 NORMAL
Hemoglobin 11.7 y/dL 12.0-16.0 LOW Hematocrit 35.2 % 37.0-47.0 ANEMIA
MCV 83.4 fL 82.0-98.0 NORMALMCH 27.7 fL 27.0-31.0 NORMAL
MCHC 33.2 g/dL 31.5-35.0 NORMALRDW-CV 12.8 % 12.0-17.0 NORMAL
PDW 9.3 fL 9.0-16.0 NORMALMPV 8.1 fL 8.0-12.0 NORMAL
Differential Count
Lymphocyte (%) 20.8 % 17.4-48.2 NORMALNeutrophil 57.3 % 43.4-76.2 NORMALMonocyte 21.9 % 4.5-10.5 HIGHEosinophil % 1.0-3.0Basophils % 0.0-2.0
Bands/Stabs % 1.0-2.0Platelets 513 10^3/uL 150-400 HIGH
Hematology Result: Jan. 10, 2010 5:11pm
Test Result Unit Reference InterpretationWBC 5.8 10^3/uL 5.0-10.0 NORMALRBC 4.34 10^6/uL 4.2-5.4 NORMAL
Hemoglobin 12.2 y/dL 12.0-16.0 NORMALHematocrit 36.2 % 37.0-47.0 LOW
MCV 83.4 fL 82.0-98.0 NORMALMCH 28.1 fL 27.0-31.0 NORMAL
MCHC 33.7 g/dL 31.5-35.0 NORMALRDW-CV - % 12.0-17.0
PDW - fL 9.0-16.0MPV - fL 8.0-12.0
Differential Count
Lymphocyte (%) 18.3 % 17.4-48.2 NORMAL

14
Neutrophil 21.7 % 43.4-76.2 LOWMonocyte 30.0 % 4.5-10.5 HIGHEosinophil - % 1.0-3.0Basophils - % 0.0-2.0
Bands/Stabs - % 1.0-2.0Platelets 452 10^3/uL 150-400 HIGH
Hematology Result: Jan. 7, 2010 3:33pm
Test Result Unit Reference InterpretationWBC 7.2 10^3/uL 5.0-10.0 NORMALRBC 4.71 10^6/uL 4.2-5.4 NORMAL
Hemoglobin 13.0 y/dL 12.0-16.0 NORMALHematocrit 38.4 % 37.0-47.0 NORMAL
MCV 81.5 fL 82.0-98.0 NORMALMCH 27.6 fL 27.0-31.0 NORMAL
MCHC 33.9 g/dL 31.5-35.0 NORMALRDW-CV 12.6 % 12.0-17.0 NORMAL
PDW 9.9 fL 9.0-16.0 NORMALMPV 8.8 fL 8.0-12.0 NORMAL
Differential Count
Lymphocyte (%) 18.2 % 17.4-48.2 NORMALNeutrophil 56.3 % 43.4-76.2 NORMALMonocyte 24.5 % 4.5-10.5 HIGHEosinophil 0.7 % 1.0-3.0Basophils 0.3 % 0.0-2.0 NORMAL
Bands/Stabs - % 1.0-2.0Platelets 406 10^3/uL 150-400 HIGH
January 10, 2010
Serous Effusions & Synovial Fluid Analysis
Gross Examination:
Volume: 10 mlColor: yellowClarity: hazy
Microscopic Examination:
RBC count: 3697/mm3
WBC count: 1238/mm3
Differential count (%):
Segmenters: 15%Lymphocytes: 85%

15
Mononuclear cells: - Other types: -
Others:Specific gravity: 1.005Rivaltas Test: positiveGlucose: trace
January 7, 2010
BLOOD CHEMISTRY SIGNIFICANCE
Blood sugar (Rbs): 103.2 (60-110) mgs%Blood Urea Nitrogen: (4.6-23.4)Creatinine: 6.75 (0.6-1.2)Electrolyte: 3.93 (3.5-5.3)mmol/LPotassium: 139.55 (135-148)mmol/L
NORMAL-
NORMALNORMALNORMAL
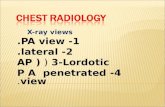
EXAM: CHEST, PA Jan. 7, 2010
Radiographic Report:Chest in PA projections shows homogenous density occupying the lower 2/3 of the left hemithorax eccentric upper border. Heart shadow is slightly deviated to the right. No right parenchymal infiltrate. Right hemidiaphragm and its corresponding sinuses are intact.
Impression:Consider Pneumonia, Left w/ Pleural Effusion.
Suggest: UTS of the left hemithorax to determine the amount of fluid within the pleural activity.
SONOGRAPHIC REPORT: Jan. 7, 2010
There is fluid collection in the left lower hemithorax measuring 11.6cm x 11.9cm x 5.5cm, approximately 395cc. No sepatations, no debris noted within the fluid. At the marked area, skin to parietal pleural is 2.2cm & interpleural distance is 4.7cm.
Impression:

16
Pleural Effusion, left, as described
January 11, 2010
Panugaling, Jonathan C.27/M
NMMC Specimen #: pf 0008Date of Birth: July, 2, 1982 Specimen Date: Jan. 11, 2010Date of Admission: Jan. 7, 2010 Specimen Type: Pleural Fluid
Organism: No GrowthComment: No growth after 72 hours incubation
January 15, 2010MICROBIOLOGY EXAMINATION
Specimen SputumAcid-Fast Stain: First Taking (Negative)

17
III. ANATOMY AND PHYSIOLOGY
Anatomy and Physiology
Anatomy of the lower respiratory tract: Lungs
Lungs
The lungs are paired elastic structures enclosed in the thoracic cage, which is an
airtight chamber with distensible walls. Ventilation requires movement of the walls of the
thoracic cage and of its floor, the diaphragm. The effect of these movements is
alternately to increase and decrease the capacity of the chest. When the capacity of the
chest is increased, air enters through the trachea (inspiration) because of the lowered
pressure within and inflates the lungs. When the chest wall and diaphragm return to
their previous positions (expiration), the lungs recoil and force the air out through the
bronchi and trachea. The inspiratory phase of respiration normally requires energy; the
expiratory phase is normally passive. Inspiration occurs during the first third of the
respiratory cycle, expiration during the latter two thirds.

18
Pleura
The lungs and wall of the thorax are lined with a serous membrane called the
pleura. The visceral pleura cover the lungs; the parietal pleura lines the thorax. The
visceral and parietal pleura and the small amount of pleural fluid between these two
membranes serve to lubricate the thorax and lungs and permit smooth motion of the
lungs within the thoracic cavity with each breath.
Mediastinum
The mediastinum is in the middle of the thorax, between the pleural sacs that
contain the two lungs. It extends from the sternum to the vertebral column and contains
all the thoracic tissue outside the lungs.
Lobes
Each lung is divided into lobes. The left lung consists of an upper and lower lobe,
whereas the right lung has an upper, middle, and lower lobe. Each lobe is further
subdivided into two to five segments separated by fissures, which are extensions of the
pleura.
Bronchi and Bronchioles
These are several divisions of the bronchi within each lobe of the lung. First are
the lobar bronchi (three in the right lung and two in the left lung). Lobar bronchi divide
into segmental bronchi (10 on the right and 8 on the left), which are the structures
identified when choosing the most effective postural drainage position for a given
patient. Segmental bronchi then divide into subsegmental bronchi. These bronchi are
surrounded by connective tissue that contains arteries, lymphatics and nerves. The

19
subsegmental bronchi then branch into bronchioles, which have no cartilage in their
walls. Their patency depends entirely on the elastic recoil of the surrounding smooth
muscle and on the alveolar pressure. The bronchioles contain submucosal glands,
which produce mucus that covers the inside lining of the airways. The bronchi and
bronchioles are lined also with cells that have surfaces covered with cilia. These cilia
create a constant whipping motion that propels mucus and foreign substances away
from the lung toward the larynx. The bronchioles then branch into terminal bronchioles
then become respiratory bronchioles, which are considered to be the transitional
passageways between the conducting airways and the gas exchange airways. Up to
this point, the conducting airways contain about 150 ml of air in the tracheobronchial
tree that does not participate in gas exchange. This is known as physiologic dead
space. The respiratory bronchioles then lead into alveolar ducts and alveolar sacs and
then alveoli. Oxygen and carbon dioxide exchange takes place on the alveoli.
Alveoli
The lung is made up of about 300 million alveoli, which are arranged in clusters
of 15 to 20. These alveoli are so numerous that if their surfaces were united to form one
sheet, it would cover 70 square meters- the size of a tennis court. There are three types
of alveolar cells. Type I alveolar cells are epithelial cells that form the alveolar walls.
Type II alveolar cells are metabolically active. These cells secrete surfactant, a
phospholipid that lines the inner surface and prevents alveolar collapse. Type III
alveolar cell macrophages are large phagocytic cells that ingest foreign matter (eg.
mucus, bacteria) and act as an important defense mechanism).
Function of the Respiratory System
The cells of the body derive the energy they need from the oxidation of
carbohydrates, fats, and proteins. As with any type of combustion, this process requires
oxygen. Certain vital tissues, such as those of the brain and the heart, cannot survive
for long without a continuing supply of oxygen. However, as a result of oxidation in the
body tissues, carbon dioxide is produce and must be remove from the cell to prevent
the build of acid waste products. The respiratory system performs this functions by
facilitating life sustaining processes such oxygen transport, respiration and ventilation,
and gas exchange.
Oxygen transport
Oxygen is supplied to and carbon dioxide is remove from cell by way of
circulating blood cells are enclosed contact with capillaries, and oxygen diffuses from
the capillary through the capillary wall to the interstitial fluid.

20
Respiration
After this, tissue capillary exchanges blood enters systemic veins and travels to
pulmonary circulation. The oxygen diffuses from the alveoli from the blood. Carbon
dioxide diffuses from the blood to alveoli movement of air in and out of the airways
continually replenishes the oxygen and removes the carbon dioxide from the airways in
the lungs this whole process of gas exchange is called respiration.
Ventilation
During inspiration, air flows from the environment into the trachea, bronchi,
bronchioles and alveoli. During expiration, alveolar gas travels the same route in
reverse.
Anatomy of the Pancreas
In humans, the pancreas is a 15-25 cm (6-10 inch) elongated organ in the
abdomen. One of the organs behind the abdominal cavity, it is located posterior to the
stomach and in close association with the duodenum.
It is often described as having three regions: a head, body and tail.
• The pancreatic head abuts the second part of the duodenum.
• The body of the pancreas lies at the level of L2 on the spine.
• The tail of the pancreas extends towards the spleen.
The pancreatic duct (also called the duct of Wirsung) runs the length of the
pancreas and empties into the second part of the duodenum at the ampulla of Vater.
The common bile duct usually joins the pancreatic duct at or near this point. Many
people also have a small accessory duct, the duct of Santorini, which extends from the
main duct more upstream (towards the tail) to the duodenum, joining it more proximal
than the ampulla of Vater.
Arteries and veins
The pancreas is supplied arterially by the Pancreaticoduodenal arteries and the
splenic artery:
• the splenic artery supplies the neck, body, and tail of the pancreas.
• the superior mesenteric artery provides the inferior pancreaticoduodenal artery
• the gastroduodenal artery provides the superior pancreaticoduodenal artery

21
Venous drainage is via the pancreaticoduodenal veins which end up in the portal
vein. The splenic vein passes posterior to the pancreas but is said to not drain the
pancreas itself. The portal vein is formed by the union of the superior mesenteric vein
and splenic vein posterior to the neck of the pancreas. In some people (some books say
40% of people), the inferior mesenteric vein also joins with the splenic vein behind the
pancreas (in others it simply joins with the superior mesenteric vein instead).
Nerves
The pancreas is innervated by the pancreatic plexus; a subdivision of the celiac
plexus that accompanies pancreatic arteries.
Physiology of the Pancreas
Under a microscope, when properly stained, it is easy to distinguish two different
tissue types in the pancreas. These regions correspond to the main pancreatic
functions:
Appearance Region Function
light staining circles (islets of Langerhans)
endocrine pancreas
secretes hormones that regulate blood glucose levels
Darker surrounding tissue exocrine pancreas
produces enzymes that break down digestible foods
Endocrine
There are four main types of cells in the islets of Langerhans. They are relatively
difficult to distinguish using standard staining techniques, but they can be classified by
their secretion:
Name of cells
Endocrine product
% of islet cells
Representative function
beta cells Insulin and Amylin 50-80% lower blood sugar
alpha cells Glucagon 15-20% raise blood sugar
delta cells Somatostatin 3-10% inhibit endocrine pancreas
PP cells Pancreatic polypeptide 1% inhibit exocrine pancreas

22
The islets are a compact collection of endocrine cells arranged in clusters and
cords and are crisscrossed by a dense network of capillaries. The capillaries of the
islets are lined by layers of endocrine cells in direct contact with vessels, and most
endocrine cells are in direct contact with blood vessels, by either cytoplasmic processes
or by direct apposition. According to the volume The Body, by Alan E. Nourse, in the
Time-Life Science Library Series, the islets are "busily manufacturing their hormone and
generally disregarding the pancreatic cells all around them, as though they were located
in some completely different part of the body.
Anatomy of the Heart
Position
The heart is a hallow organ positioned left of the center in the chest cavity within
the pericardial cavity. The base of the heart is located superiorly in and the apex is
directed downward and leftward and formed by the lateral tip of the left ventricle
Physiology of the Heart
The essential function of the heart is to pump blood to various parts of the body.
The mammalian heart has four chambers: right and left atria and right and left
ventricles. The two atria act as collecting reservoirs for blood returning to the heart while
the two ventricles act as pumps to eject the blood to the body. As in any pumping
system, the heart comes complete with valves to prevent the back flow of blood.
Deoxygenated blood returns to the heart via the major veins (superior and inferior vena
cava), enters the right atrium, passes into the right ventricle, and from there is ejected to
the pulmonary artery on the way to the lungs. Oxygenated blood returning from the
lungs enters the left atrium via the pulmonary veins, passes into the left ventricle, and is
then ejected to the aorta. In the frontal view of the heart shown below, the right atrium is
in blue, the left atrium in yellow, the right ventricle in purple, and the left ventricle in red.
The chambers are semi-transparent so that the valves, drawn in white, can be seen.
The large valve in the foreground is the tricuspid valve that prevents backflow
from the right ventricle to the right atrium. The small round valve you see near the top is
the pulmonary valve, where the pulmonary artery comes out of the right ventricle.
The inner edge of the tricuspid and the mitral valves end in filamentous
connective tissue (chordae tendineae). These are attached to small columns of muscle
(papillary muscles) arising out of the inner surface of the ventricles. As the pressure
builds in the ventricles, the valves snap shut, and the papillary muscles prevent the
valves from blowing into the atrium and opening.

23
Pumping Action of the Heart
The pumping action starts with the simultaneous contraction of the two atria. This
contraction serves to give an added push to get the blood into the ventricles at the end
of the slow-filling portion of the pumping cycle called "diastole." Shortly after that, the
ventricles contract, marking the beginning of "systole." The aortic and pulmonary valves
open and blood is forcibly ejected from the ventricles, while the mitral and tricuspid
valves close to prevent backflow. At the same time, the atria start to fill with blood again.
After a while, the ventricles relax, the aortic and pulmonary valves close, and the mitral
and tricuspid valves open and the ventricles start to fill with blood again, marking the
end of systole and the beginning of diastole. It should be noted that even though equal
volumes are ejected from the right and the left heart, the left ventricle generates a much
higher pressure than does the right ventricle.
Electrical Activity of the Heart
When vertebrate muscles are excited, an electrical signal (called an "action
potential") is produced and spreads to the rest of the muscle cell, causing an increase in
the level of calcium ions inside the cell. The calcium ions bind and interact with
molecules associated with the cell's contractile machinery, the end result being a
mechanical contraction. Even though the heart is a specialized muscle, this
fundamental principle still applies.
One thing that distinguishes the heart from other muscles is that the heart muscle
is a "syncytium," meaning a meshwork of muscle cells interconnected by contiguous
cytoplasmic bridges. Thus, an electrical excitation occurring in one cell can spread to
neighboring cells. Another defining characteristic is the presence of pacemaker cells.
These are specialized muscle cells that can generate action potentials rhythmically.
Under normal circumstances, a wave of electrical excitation originates in the
pacemaker cells in the sinoatrial (S-A) node, located on top of the right atrium.
Specialized muscle fibers transmit this excitation throughout the atria and initiate a
coordinated contraction of the atrial walls. Meanwhile, some of these fibers excite a
group of cells located at the border of the left atrium and ventricle known as the
atrioventricular (A-V) node. The A-V node is responsible for spreading the excitation
throughout the two ventricles and causing a coordinated ventricular contraction.

24
IV. PATHOPHYSIOLOGY
A. NARRATIVE FORM
Microorganisms that produce pneumonia can end up in air sacs in several ways.
In some cases, people inhale microorganisms (which are present in tiny droplets) when
they are near someone already infected. Spread in hospitals and nursing homes often
occurs this way. More common among older people, however, is the presence of
bacteria in their throat (colonization). These bacteria may remain there harmlessly or
suddenly cause pneumonia if mucus or food is inhaled into the airway (aspiration)
instead of passed into the esophagus. When aspiration occurs, the food or mucus can
make its way into the lungs, carrying the bacteria from the throat along for the ride.
Rarely, microorganisms from elsewhere in the body reach the lungs by traveling through
the bloodstream. These are usually blood borne microorganisms that enter the
pulmonary circulation and are trapped in the capillary bed, becoming a potential source
of pneumonia.
Pneumonia often affects both ventilation and diffusion. An inflammatory reaction
can occur in the alveoli, producing an exudate that interferes with the diffusion of
oxygen and carbon dioxide. White blood cells, mostly neutrophils, also migrate into the
alveoli and fill the normally air-containing spaces. Areas of the lung are not adequately
ventilated because of secretions and mucosal edema that cause partial occlusion of the
bronchi or alveoli, with a resultant decrease in the alveolar oxygen tension. Because of
hypoventilation, a ventilation-perfusion mismatch occurs in the affected area of the lung.
Venous blood entering the pulmonary circulation passes through the underventilated
area and exits to the left side of the heart poorly oxygenated. The mixture of oxygenated
and unoxygenated blood eventually results in arterial hypoxemia.
Pleural effusion is an indicator of an underlying disease process that may be
pulmonary or nonpulmonary in origin, acute or chronic.
Normal pleural fluid has the following characteristics:
o Clear ultrafiltrate of plasma that originates from the parietal pleura

25
o pH 7.60-7.64
o Protein content less than 2% (1-2 g/dL)
o Fewer than 1000 WBCs per cubic millimeter
o Glucose content similar to that of plasma
o Lactate dehydrogenase (LDH) less than 50% of plasma
o Sodium, potassium, and calcium concentration similar to that of the
interstitial fluid
The following mechanisms play a role in the formation of pleural effusion:
o Altered permeability of the pleural membranes (eg, inflammation,
malignancy, pulmonary embolus)
o Reduction in intravascular oncotic pressure (e.g., hypoalbuminemia,
cirrhosis)
o Increased capillary permeability or vascular disruption (e.g., trauma,
malignancy, inflammation, infection, pulmonary infarction, drug
hypersensitivity, uremia, pancreatitis)
o Increased capillary hydrostatic pressure in the systemic and/or pulmonary
circulation (eg, congestive heart failure, superior vena cava syndrome)
o Reduction of pressure in the pleural space, preventing full lung expansion
(eg, extensive atelectasis, mesothelioma)
o Decreased lymphatic drainage or complete blockage, including thoracic
duct obstruction or rupture (eg, malignancy, trauma)
o Increased peritoneal fluid, with migration across the diaphragm via the
lymphatics or structural defect (eg, cirrhosis, peritoneal dialysis)
o Movement of fluid from pulmonary edema across the visceral pleura
o Persistent increase in pleural fluid oncotic pressure from an existing
pleural effusion, causing further fluid accumulation
The net result of effusion formation is a flattening or inversion of the diaphragm,
mechanical dissociation of the visceral and parietal pleura, and a restrictive ventilatory
defect.

Inflammation
Precipitating factor:>prolonged back rest>aspiration>inhaled microorganism (Bacteria)
Predisposing factor:>stress>exposure to polluted air>depressed cough reflex
Inhaled in the alveolus
Inhalation of causative agents (CA):Streptococcus pneumoniae
Reproduction of CA in the lungs
Activation of first line of defenseS/sx: cough, mucus production
Partial occlusion of bronchus alveoli
26
B. SCHEMATIC DIAGRAM

Increased capillary permeability or vascular disruption
Exudates
Pleural Effusion
Complication:AtelectasisInfection
hypoxemia
SIGNS AND SYMPTOMS:Dyspnea
chest paindecreased tactile fremitus
diminished or absent breath soundspleural friction rub during both inspiration and expiration
dry nonproductive coughshortness of breath
Treated Not treated
Prevents serious Complications
Metastasis of Complications
Recovery Danger to health (serious)
27

28
NURSING CARE PLAN
NURSING DIAGNOSIS
Ineffective Breathing Pattern related to difficulty of breathing secondary to pneumonia
ASSESSMENT DATA (SUBJECTIVE AND OJECTIVE CUES)
Subjective Cue:
“Maglisod ko ug ginhawa usahay, murag dili ko kaginhawa”, as verbalized by the patient.
Objective Cue:
- Nonproductive cough noted
- Dyspnea on exertion
- Pursed-lip breathing
- Nasal flaring
- Chest pain, scale of 6/10
GOALS AND OBJECTIVE
Short Term Goal:
After 1 hour of Nursing Intervention, the patient will:
- Deep breathing exercises
- Use of relaxation techniques
- Verbalize understanding of technique in doing deep breathing exercise
- maintain adequate ventilation and oxygenation
- maintain a patent airway
Long Term Goal:
After 4-5 days of Nursing Care, the patient will be able to establish a normal/effective respiratory pattern.

29
NURSING INTERVENTION
Independent:
Instruct the patient to do deep breathing exercises
R> to assist the patient in “taking control” of the situation/inspiration
Assist for discomfort and place patient in a high back position
R> This would limit/restrict respiratory effort.
Monitor pulse oximetry as indicated.
R> To verify maintenance of O2 saturation
Dependent:
Medicate with analgesics as appropriate to promote deeper respiration and cough.
R> Tramadol 50mg IVTT q8h is given
Collaborative:
Assist with Chest Thoracentesis Tube insertion as indicated
R> To drain fluid in the pleural space.
EVALUATION
Short Term Goal = Goals met
The patient was able to participate and perform deep breathing exercises and verbalizes understanding about the relaxation techniques when the patient has dyspnea.
Long Term Goals = Goals not met
The goal in not yet met since the patient still has pneumonia and needs for further evaluation.

30
NURSING DIAGNOSIS
Acute Pain related to inflammatory process of the Pleural Effusion due to infectious
process from pneumonia.
ASSESSMENT DATA (SUBJECTIVE AND OJECTIVE CUES)
Subjective Cue:
“Sakit akong dughan duol sa bangag didto sa nay tubo”, as verbalized by the patient.
Objective Cue:
- Chest pain, scale of 6/10
- Guarding behavior noted
- Positioning to avoid injury near CTT observed
- Reduced interaction to people observed
- Flaccid muscle tone of the left arm near CTT noted
- Localized pain identified by the patient
GOALS AND OBJECTIVE
Short Term Goal:
After 8 hours of Nursing Intervention, the patient will:
- Report relief of pain or controlled
- report reduced levels of concern to attached tubing
Long Term Goal:
After 3-4 days of Nursing Care, the patient will experience controlled pain regarding the draining of the pleural fluid.
NURSING INTERVENTION
Independent:
Assess the client’s description of pain
R> Pain is a subjective experience & cannot be felt by others but can be objective when assessed in scale of 0-10
Observe non verbal cues/pain behaviors
R> To determine the congruency of pain reactions to client’s verbalization of pain.

31
Instructed to do relaxation techniques, such as focused breathing.
R> To distract attention & reduce tension from pain.
Monitor the skin color/temperature & vital signs.
R> These are usually altered in severe pain.
Dependent:
Administer analgesics, as indicated to maximum dosage, as needed.
R> To maintain acceptable level of pain. Given with Tramadol every 8 hours 50mg via IVTT route.
EVALUATION
Short Term Goal = Goals met
The patient reported relief or controlled pain from pain scale of 6/10 to 4/10 after given with the medication in given intervals. Also used relaxation techniques and followed treatment regimens.
Long Term Goals = Goals not met
The goal is not met as it has to be evaluated yet.

32
NURSING DIAGNOSIS
Risk for Infection related to, damaged tissue integrity due to insertion of CTT.
ASSESSMENT DATA (SUBJECTIVE AND OJECTIVE CUES)
Objective Cue:
- Has attached Chest Thoracostomy Tube on the left mid-axillary line noted
GOALS AND OBJECTIVE
Short Term Goal:
After 8 hours of Nursing Intervention, the patient will:
- Be free of purulent drainage
- Prevent or decrease the risk of infection
- Be placed with a new dressing to the wound
- Provide clean environment for the patient’s safety to infection
Long Term Goal:
After 2-3 days of Nursing Care, the will maintain an infection free environment from harmful pathogens.
NURSING INTERVENTION
Independent:
Note the risk factors of occurrence of infection like skin/tissue wounds
R> to assess causative or contributing factors of infection
Observe for localized signs of infection at insertion site of invasive lines, surgical incision or wound.
R> to determine the portal of entry causing infection
Change surgical wound dressing as indicated using proper technique for changing or disposing the contaminated materials.
R> to reduce the risk for infection
Dependent:
Discuss importance of not taking antibiotic or using left over drugs unless specifically instructed by the health care provider.
R> inappropriate use can lead to drug-resistant strains.

33
EVALUATION
Short Term Goal = Goals met
Providing a clean environment for the patient was given in order to prevent infection from the damaged tissue due to CTT draining of pleural fluid. The surgical dressing was not advised to be replaced since the chest was totally covered or no openings were noted for risk of infection.
Provision of clean clothes was given in order to prevent infection of the CTT site.
Long Term Goals = Goals not met
The goal is not met as it has to be evaluated yet.

34
DRUG STUDY
DRUG ORDERMECHANISM OF
ACTIONINDICATIONS CONTRAINDICATIONS ADVERSE EFFECTS
OF THE DRUG
NURSING RESPONSIBILITIES/
PRECAUTIONS
Generic name:Cefuroxime
Brand name:Ceftin
Classification:Antibiotic
Dosage:750 mg
Route:IVTT
Frequency:q8h
A second – generation cephalosporin that binds to bacterial cell membranes and inhibits cell wall synthesis
Therapeutic Effect: Bactericidal
Treatment of susceptible infections due to group B streptococci, pneumococci, staphylococci, H. Influinzae, E.coli.
History of anaphylactic reaction to penicillins or hypersensitivity to cephalosporins.
Cautions: renal impairment, history of GI disease (especially ulcerative colitis, antibiotic – associated colitis), concurrent use of nephrotoxic medications.
Antibiotic – associated colitis and other supr infections may result from altered bacterial balance.
Question for history of allergies, particularly cephalosporins, penicillins. Assess oral cavity for white patches on mucous membranes, tongue, monitor bowel activity and stool consistency carefully; mild GI effects ,may be tolerable, but increasing severity may indicate onset of antibiotic associated colitis. Monitor I&O, renal function reports for nephrotoxicity. Be alert for superinfection: severe genital/anal pruritus, severe mouth soreness, moderate to severe diarrhea.

35
DRUG ORDERMECHANISM OF
ACTIONINDICATIONS CONTRAINDICATIONS ADVERSE EFFECTS
OF THE DRUG
NURSING RESPONSIBILITIES/
PRECAUTIONS
Generic name:Tramadol hydrochloride
Brand name:Ultram
Classification:Analgesic
Dosage:50mg
Route:IVTT
Frequency:q8h
An analgesic that binds to mu-opioid receptors and inhibits reuptake of norepinephrine and serotonin reduces the intensity of pain stimuli reaching sensory nerve endings.
Therapeutic Effect:Alters the perception of and emotional response to pain.
Management of moderate to moderately severe pain.
Acute alcohol intoxication, concurrent use of centrally acting analgesics, hypnotics, opioids, or psychotropic drugs, hypersensitivity to opioids.
Seizures have been reported in patients receiving tramadol within the recommended dosage range. Overdose results in respiratory depression and seizures. Tramadol may not have prolonged duration of action and cumulative effect in patients with hepatic or renal impairment.
Check the prescribed medication for 3 time on the first encounter, before and after withdrawing the medR> so that the medicine is properly checked according to the doctor’s prescription.
Give first health teaching before giving the patient.R> to make the patient prepare and know what to expect
The med should be given in IVTT route according to the doctorR> Follow the doctor’s order as prescribed to the patient.

36
DRUG ORDERMECHANISM OF
ACTIONINDICATIONS CONTRAINDICATIONS ADVERSE EFFECTS
OF THE DRUG
NURSING RESPONSIBILITIES/
PRECAUTIONS
Generic name:Paracetamol
Brand name:-
Classification: Analgesics and Antipyretics
Dosage:300mg
Route:IVTT
Frequency:PRN
Paracetamol exhibits analgesic action by peripheral blockage of pain impulse generation. It produces antipyresis by inhibiting the hypothalamic heat – regulating center. Its weak anti-inflammatory activity is related to inhibition of prostaglandin synthesis in the CNS.
For treatment of mild to moderate pain and fever.
No known contraindications.
Nausea, allergic reaction, skin rashes, acute renal tubular necrosis.
Potentially Fatal: Very rare, blood dyscrasias (e.g., thrombocytopenia, leukopenia, neutropenia, agranulocytosis); liver damage.
The medication should be given in IVTT.R> this is according to the doctor’s order.
Assess patient for any drug allergy to the medicine.R> to determine if the patient is allergic to drug
Intruct the patient/ give first health teaching before giving the patient.R> to make the patient prepare and know what to expect

37
HEALTH TEACHING
The patient with Pleural Effusion needs to be given attention especially if the
patient has experienced pain in the site if CTT, had dyspnea, chest pain, nonproductive
cough.
The following are some Nursing Management on Pleural Effusion:
Management:
1. Assess for associated problems.
2. Administer medications which may be prescribed for associated problems such
like Tramadol 50mg IVTT for management of pain.
3. Implement a plan of care that is teaching the client to do deep breathing exercise
since the client has shortness of breath.
4. Encourage the patient and the significant others to do counseling.
5. Explain to the significant others the limitation of the patient’s mobility due to
attached chest thoracostomy tube.
6. Explain tests and procedures to the patient, including thoracentesis, and answer
questions he has.
7. Before thoracentesis, tell the patient to expect a stinging sensation from the local
anesthetic and a feeling of pressure when the needle is inserted. Instruct him to tell you
immediately if he feels uncomfortable or has trouble breathing during the procedure.
8. If the patient developed pleural effusion because of pneumonia or influenza, tell him to
seek medical attention promptly whenever he gets a chest cold.
9. Teach the patient the signs and symptoms of respiratory distress. If any of these
develop, tell him to notify his physician.
10. Fully explain the drug regimen, including adverse effects. Emphasize the importance of
completing the prescribed drug regimen.
11. If the patient smokes, urge him to stop.

38
LEARNING EXPERIENCE
As part of the learning process, there are things that you need to discover
yourself and need to explore in order to fulfill the things that you are curious about. And
I have learned something from this. Although there are hard times and mistakes that we
may encounter, there is only one thing that you can appreciate more which is the
experience. I have learned that through this individual case study, I was able cope
myself in doing the requirement alone without the assistance of anybody, which makes
me feel joyous since this is a tough thing to make a case study. I have learned from this
case the hardship and the joy of fulfilling the requirement and it is a one way step of
developing my skills in doing the case study.
I realized that one should work hard amidst of your limits and accomplish
the things that you are ought to do. Not by just passing a requirement but also learning
from it as part of you dream to become an effective nurse in the future. One must have
focus and not to left the things unappreciated for nurses deals with the lives of many
individuals and thus must be accountable for the patient’s life in alleviating the pain,
restoring the health, etc as possible it may be.
Lastly, as a student nurse, I have learned and kept in mind the most
important thing to do for our patient and that is not to get mistakes in rendering care for
our patient for one slip could end up the life of your patient and that could be your
hardest thing that could happen for you and the patient’s family of losing one’s life in just
a minor mistake. So I guess that I should practice myself to seek for perfection in giving
care to patients and diminish the faulty errors in the clinical area when you are on duty.
At a short period stay at NMMC Medical Ward, I am a student nurses on
action. It is where I put all of what I am in extreme preparation. You should not waste
time doing senseless distractions, rather gain from your opportunities, reading, handling
cases and interactions are just a few that we have mastered. Although change does not
happen overnight, it is a good feeling to know that you have controlled yourself and
leading it to make a difference. As our duty progresses, we have established a great
bond among our group mates. We learn together, we work together and care for each

39
other and that is the beauty in our group. We never fail to be concerned towards each
other as it is just more than a group but a family.
DISCHARGE PLAN
M-MEDICATION
Explain the purpose, dosage, schedule, and route of administration of any prescribed
drugs, as well as side effects to report to the physician or nurse.
Instruct the watcher to refer any abnormalities about the pt. to the nurse or physician to
prevent complications. (The patient is not yet discharged and there were no PO meds
given in the hospital except for IVTT meds).
Outpatient medication therapy is directed at the underlying etiology of the effusion.
A social services professional should be consulted when a patient cannot afford
prescribed medications.
E-EXERCISE
The patient is advised to take rest after discharge in order to prevent injury and to
regain strength. The site of effusion needs proper attention and careful not to be
strained. The patient is not advised to do hard and stressful work yet he can still take
walking exercise that he is capable of doing.
T-TREATMENT
Patient is advised to consult his physician if he cannot afford the treatment. It is best
that the health care provider is aware so that he can make adjustments. Instruct
significant others to monitor patients condition.
H-HEALTH TEACHINGS
Teach the significant others on the simple pathology and physiology of the disease to
help them understand and to clarify misconceptions of the disease. Discuss the possible
causes of the disease, prognosis, and describe the disorder. Demonstrate to significant
others the proper wound care, administration of medicines and how to care for the

40
patient. Explain the effects of the treatment of the patient and what to do when side
effects occur. Aware the patient and significant others the importance of knowing the
Do’s and Don’ts while the effusion is still present. Determine the patient’s expectations
to alleviate fear and anxiety.
OUT-PATIENT CHECK-UP
Follow-up with the patient's primary care physician or a pulmonary specialist within 2-3
days is advisable, especially if thoracentesis is deferred.
If early follow-up seems unlikely, the patient should be given clear instructions to return
to the ED in 2-3 days for reevaluation.
Patient is instructed to have a regular check up in the hospital if there are any signs of
complications of risks and if there is also improvement or progress regarding his case.
DIET
Instruct patient’s family, significant other to follow recommended diet provided by her
dietician if any.
SPIRITUAL
Patient’s family is very religious that is why we always continue to encourage him to
remain that faithful and strong to God. Continue praying and reading the bible and never
forget that during times of difficulties, God carries our burden. It is about putting our trust
in him and never giving up.

41
DOCTOR’S ORDER
January 7, 2010 Thursday11pm
Please admit pt at P1F2 (male charity ward) Secure consent to care DAT Venolysis with PNSS 1L @ 30gtts/min IVFTT PNSS 1L @ 30gtts/min Nursing
1. VS q4h & recordRefer if BP ≥ 130/90 < 90/60mmHg
HR > 100 < 60 beats/minRR > 24 < 12 beats/min
2. I&O q shift3. Refer for signs of respiratory distress
Chest pain, SOB and cyanosis
CXR: Consider, Pneumonia
PA w/ Pleural eff. Diagnostics
1. CBC with pH ct2. URA3. CXR – PA view (attached)
Therapeutics1. Cefuroxime 750mg IVTT q8h ANST2. Paracetamol 300mg IVTT q4h for fever 38.50C
o For thoracenthesis w/ local anesthesiao Refer for unsualities
January 14, 2010 Thursday11:40 am> anemia > CTT drainage monitoring of output > asthmatic > continue meds> SOB > repeat CBC with pH today
> refer> IVF with PNSS 1L @ 30gtts/min x 3
January 15, 2010 Friday11:45am> - SOB > for Sputum AFB 3x> C/L: ECE, CBR > encourage breathing exercise> DTB – murmur > continue present meds> good posture > may D/C O2 inhalation, standby PRN
> IVF w/ PNSS 1L @ 30gtts/min x3 cycle
L

42
> continue CTT bottle draining monitoring
January 16, 2010 Saturday10:00am> - SOB > for Sputum AFB> - chest pain > continue present meds> C/L: ECE, CBR > continue CTT bottle drainage monitoring> DTB, - murmur > refer> good posture, > IVF w/ PNSS 1L @ 30gtts/min x3 cycle - edema
CTT drainagereading
REFERENCE:
www.wisegeek.com
www.wikipedia.com
www.emedicine.medscape.com
Black & Hawks. Medical – Surgical Nursing Clinical Management for Positive
Outcomes. Saunders Elsevier 8th edition.