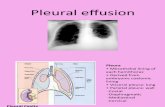
Pleural effusion
-
Upload
aaron-mascarenhas -
Category
Documents
-
view
5.374 -
download
1
Transcript of Pleural effusion

• 65 years old Male, smoker came with left-sided chest pain and increasing difficulty breathing since 2 weeks. He reports having fever and decreased appetite. He recalls being treated for tuberculosis when he was a child. He has a clear chest x-ray taken 15 years ago.
• On examination pallor present, trachea shifted to the right, chest expansion decreased on left side, dullness in the mammary, infra axillary areas, absent breath sounds in the same area.

• Pleural Effusion on the left side, secondary to TB with anemia

Clinical FeaturesSymptoms• Chest pain (pleurisy)• Breathlessness• Symptoms associated with the actual cause of
pleural effusion– Pnemonia– Renal disorder, Cardiac and liver disease– TB– Risk for thromboembolism– Exposure to asbestos (occupation)

Signs• Trachea shifted to opposite side• Bulge ?• Chest movements decreased• Stony dullness• Absent breath sounds. Above effusion,
crackles may be present.• Decreased vocal resonance and fremitus on
same side• Traubes space percussion and tidal percussion

ETIOPATHOGENESIS OF PLEURAL EFFUSION

Normal Physiology
• Normally pleural space contains a thin layer of fluid.
• Fluid enters the pleural space from the capillaries in the parietal pleural and is removed by the lymphatics in the parietal pleura.
• Fluid can also enter the pleural space from the interstitial spaces of the lung via the visceral pleura or from the peritoneal cavity through the diaphragm.

PATHOGENESIS
• Pleural fluid accumulates whenFormation increasesAbsorption decreases
• Pleural effusion can beTransudative Exudative

• Transudative effusion occurs commonly due to systemic factors which either increase the hydrostatic pressure or decrease the plasma oncotic pressure.
• Exudative effusion occurs due to local pathology in the lung or the pleura.

AETIOLOGY
• Transudative pleural effusion– Congestive cardiac failure– Cirrhosis– Pulmonary embolism– Nephrotic syndrome– Peritoneal dialysis– Myxoedema

Exudative Pleural Effusion
• Neoplastic diseases– Metastatic diseases– Mesothelioma
• Infectious diseases– Pneumonia – Tuberculosis
• Gastrointestinal diseases– Pancreatic disease– Esophageal perforation– Intraabdominal abscess– Diaphragmatic hernia

Exudative Pleural Effusion
• Collagen vascular diseases– Rheumatoid arthritis– SLE– Drug-induced lupus– Immunoblastic lymphadenopathy– Sjogrens syndrome– Wegener’s granulomatosis– Churg-strauss syndrome
• Asbestos exposure• Sarcoidosis• Uremia• Meigs’ syndrome

Investigations
Aaron John Mascarenhas080201022

Radiological examination
Types of Pleural Effusion on X-ray:1. Free fluid in the pleural space
a. Lamellar effusionb. Subpulmonary effusionc. Fissural effusion
2. Loculated effusion3. Massive pleural effusion

Free fluid
1. First appears in the posterior CP angle (100-200ml fluid): Lateral film
2. Meniscus sign: – Dense homogenous opacity– Well defined concave upper edge– Higher laterally than medially– Obscures the diaphragmatic shadow

Atypical distribution of fluid
• Lamellar effusions:– Shallow collections between lung surface and visceral
pleural– Represent interstial pulmonary fluid
• When large they form subpulmonary effusion– Contour of diaphragm altered, apex shifted– Blunting of CP angles and tracking into fissures– Left: distance between gastric bubble and lung base– Postural shifts in fluid

Loculated effusion
1. No change by gravitational methods2. ?Extrapleural opacity, ?Peripheral lung lesion
Fissural effusion:3. Lenticular, round or oval shadow4. “Thickened” fissure5. ‘Pseudo’ or ‘ Vanishing’ tumors?

Also look for?
1. Positioning?2. Breast shadows?3. Rib: Erosions, #4. Trachea: Shift, Paratracheal shadows5. Cardiac shadow6. Lung fields: Cavity, “cotton wool” infiltrates, Cannon
ball mets7. Hilum: Lymphadenopathy8. Air-fluid level9. Pleura: Masses, thickening.

Massive Pleural effusion
1. White out lung(WOL) + Contralateral Mediastinal shift
D/D:2. Collapse (WOL + Ipsilateral Mediastinal Shift)3. Consolidation (WOL + Central trachea)

Ultrasonography
• Detects even 5ml of fluid in excess on normal• Differentiation of pleural thickening from
loculated pleural effusion• Associated abnormalities

Pleural aspiration and Analysis
Transudative or Exudative?LIGHT’S CRITERIA:1. Pleural fluid protein/Serum Protein >0.52. Pleural fluid LDH/Serum LDH >0.63. Pleural fluid LDH > 2/3rd the upper limit of
serum LDH


Tuberculous effusion
1. “Amber” coloured to sero-sanguineous2. >10%eosinophils; <5%: Mesothelial cells3. Centrifuged deposits:– AFB +ve: <10% immunocompetent host– Culture +ve: 25%
4. ADA elevated (>40U/L)5. Others: LDH, Soluble IL-2 receptors, IFN-γ6. Detection of Mycobacteria DNA by PCR7. Nucleic acid amplification assays8. Pleural biopsy: Non-caseating granulomas > 80%

MANAGEMENT OF PLEURAL EFFUSION
MEDICAL MANAGEMNTTreatment of underlying causeTherapeutic aspiration is necessary in order to
relieve dyspnoeaPrecautions:
Removing more than 1L in one episode in inadvisable Can result in re-expansion pulmonary oedemaShould never be aspirated to dryness before the exact
etiology is determined

THORACOCENTESIS
INDICATIONSDiagnostictherapeutic
POSITIONSitting position, leaning forward over a support
SITE Below the scapula, posteriorly through the seventh
intercostal space

PROCEDUREInformed consentClean the are with povidine
iodineLocal anesthesiaInsert the needle and flexible
catheter over the needleAspirate pleural fluid

COMPLICATIONSIatrogenic pneumothoraxInfectionDry tap or bloody tapRe-expansion pulmonary oedemaPain and respiratory distress

Surgical Managementof Pleural Effusion

Effusion due to Heart Failure• Most common cause of pleural effusion• a diagnostic thoracentesis is done if:
– the effusions are not bilateral and comparable in size– the patient is febrile– the patient has pleuritic chest pain to verify that the effusion is
transudative• Otherwise the patient's heart failure is treated• If the effusion persists despite therapy, a diagnostic thoracentesis should
be done• A pleural fluid N-terminal pro-brain natriuretic peptide (NT-proBNP)
>1500 pg/mL is diagnostic of an effusion secondary to congestive heart failure

Parapneumonic Effusions• most common cause of exudative pleural effusion (bacterial
pneumonias, lung abscess, bronchiectasis)• The presence of free pleural fluid can be demonstrated with a lateral
decubitus radiograph, CT of the chest, or ultrasound• If the free fluid separates the lung from the chest wall by >10 mm, a
therapeutic thoracentesis should be performed• A procedure more invasive than thoracentesis is needed if the
following factors are present:– Loculated pleural fluid– Pleural fluid pH <7.20– Pleural fluid glucose <3.3 mmol/L (<60 mg/dL)– Positive Gram stain or culture of the pleural fluid– Presence of gross pus in the pleural space

Parapneumonic Effusion• If the fluid recurs after the initial therapeutic thoracentesis and if
any of these characteristics are present - a repeat thoracentesis
• If the fluid cannot be completely removed with the therapeutic thoracentesis,– insert a chest tube and instill a fibrinolytic agent (e.g., tissue
plasminogen activator, 10 mg)– perform a thoracoscopy with the breakdown of adhesions– Decortication (if these measures are ineffective)

Malignant Pleural Effusions• 2nd most common type of exudative pleural effusion (lung carcinoma,
breast carcinoma, & lymphoma)• Diagnosis: cytology of the pleural fluid• If cytology is negative, thoracoscopy is done if malignancy is suspected• Pleural abrasion should be performed to effect a pleurodesis • Pleural abrasion: a scourer is used to scrape off the surface of parietal pleura• An alternative to thoracoscopy : CT- or ultrasound-guided needle biopsy of
pleural thickening or nodules• Patients with a malignant pleural effusion are treated symptomatically • Dyspnea if present and is relieved with a therapeutic thoracentesis, one of
the following procedures should be considered: – insertion of a small indwelling catheter or – tube thoracostomy with the instillation of a sclerosing agent such as
doxycycline, 500 mg

Chylothorax• Occurs when thoracic duct is disrupted and chyle
accumulates in the pleural space. • Thoracentesis shows milky fluid, and biochemical
analysis reveals a triglyceride level that exceeds 1.2 mmol/L (110 mg/dL)
• Treatment: insertion of a chest tube plus the administration of octreotide
• If these measures fail, a pleuroperitoneal shunt should be placed
• An alternative treatment is ligation of the thoracic duct

Hemothorax
• Diagnostic thoracentesis shows bloody pleural fluid,• Hematocrit :if >1/2 of that in the peripheral blood, the
patient is considered to have a hemothorax• Treatment: tube thoracostomy ( helps quantify
bleeding) • If the bleeding emanates from a laceration of the
pleura, apposition of the two pleural surfaces is likely to stop the bleeding.
• If the pleural hemorrhage exceeds 200 mL/h, perform thoracoscopy or thoracotomy