Placental Pathology in Early-Onset and Late Onset FGR
-
Upload
euffrasia-monica-atikka-sugiarto -
Category
Documents
-
view
238 -
download
0
description
Transcript of Placental Pathology in Early-Onset and Late Onset FGR
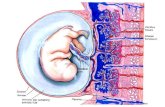
E-Mail [email protected] Review Fetal Diagn Ther 2014;36:117128 DOI: 10.1159/000359969 Placental Pathology in Early-Onset and Late-Onset Fetal Growth Restriction William MifsudNeil J. Sebire Department of Paediatric Histopathology, Great Ormond Street Hospital,London , UK profile. The histological placental findings in FGR are there-fore varied, from morphologically unremarkable through to severeuteroplacentalvasculopathy,withnosinglepatho-logical feature associated with high sensitivity or specificity. Severe early-onset FGR, overlapping with severe early-onset PET, is mainly associated with features of impaired maternal uteroplacental perfusion secondary to defective extravillous trophoblast invasion, and its consequences. Late-onset FGR probably represents a more heterogeneous group with less characteristichistologicalchanges.Futureresearchusing histopathological assessment of aggregated data from mul-tiple studies into larger datasets with centralised pathology review will allow delineation of distinctive clinicopathologi-cal associations and further understanding of pathophysiol-ogy. 2014 S. Karger AG, Basel Introduction There has been increasing interest in defining patterns ofplacentalpathologyassociatedwithintrauterinefetal growthrestriction(FGR),withprogressiveclinicalre-finement of subgroups of fetuses that are small for gesta-tional age (SGA), with and without other features of FGR, Key Words Placental pathology Growth restriction Pre-eclampsia Abstract Several histopathological features are found more frequent-ly in placentas from pregnancies complicated by fetal growth restriction(FGR),includingvillousinfarction,maternalvas-cularchangesandvillousmorphologicalalterations,al-though around one quarter of placentas associated with FGR lackanymorphologicalabnormalityonroutineexamina-tion. Since similar changes may also affect clinically uncom-plicatedpregnancies,thepositivepredictivevalueofsuch findings for pathological FGR in an unselected case remains low.However,thepatternofplacentalpathologiesvaries withclinicalsubgroup.Thecombinationofplacentalbed andparenchymallesionsinFGRwithabnormaluterinear-teryDopplervelocimetryisessentiallyidenticaltopreterm pre-eclampsia(PET),andthereisanassociationbetween FGR with abnormal umbilical artery Doppler findings and le-sions of fetal stem arteries and terminal villous hypovascu-larity. Conversely, placentas from pregnancies complicated by PET or FGR presenting at or near term have a significantly lower frequency of histological abnormalities compared to early-onset disease and absence of a distinctive biochemical Received: January 7, 2014 Accepted after revision: January 23, 2014 Published online: February 21, 2014 Prof. N.J. Sebire Department of Paediatric Histopathology Great Ormond Street Hospital Great Ormond Street, London WC1N 3JH (UK) E-Mail [email protected] 2014 S. Karger AG, Basel10153837/14/03620117$39.50/0 www.karger.com/fdt Downloaded by: 198.143.39.65 - 8/15/2015 11:01:29 AM Mifsud/Sebire Fetal Diagn Ther 2014;36:117128DOI: 10.1159/000359969118suchasabnormalDopplerultrasoundassessmentand maternal serum markers such as placental growth factor and fms-like tyrosine kinase-1. Here, we review the avail-abledataondocumentedhistopathologicalfeaturesof the placenta associated with early versus late-onset FGR, theirsignificance,andtheirrelationshiptofindingsin pre-eclampsia (PET). We also infer possible pathogenetic implicationsofthesefindingsandspeculateonfuture work to better define, understand and manage these con-ditions. General Placental Histopathological Features Associated with FGR There are numerous publications describing a range of morphologicalfeaturesinplacentasfrompregnancies complicated by FGR (or more specifically SGA, since the vast majority of studies, especially early studies, defined the FGR group simply based on a fetal size below a given centile value rather than definitive features of abnormal fetal growth)[1] . Despite this large descriptive literature, no reliable and pathognomonic features for either FGR/SGA or specific aetiologies are documented, but several lesionsaremorecommoncomparedtocontrolsinthe majority of studies, and hence appear associated with the clinical phenotype of FGR/SGA. However, comparison of findingsbetweendifferentstudies,andmoredetailed analysis of the data, is often not straightforward, due to several reasons. There is biological variation in the disease process due to several complex underlying mechanisms resulting in a final common phenotype of FGR, and in-dividual patient responses may differ in response to a giv-en underlying cause. There is variation in placental mor-phology due to the fact that FGR occurs in parallel with many features of growth and development of the fetopla-cental unit, and there may be geographical variation be-tween different areas of the same placenta in relation to samplingadequacy.Inaddition,studiesmayhaveused different sampling protocols, with associated bias and er-rors, and the extent of such regional variations in placen-tal histological changes remains undefined. Studies have used different definitions and thresholds for recognising changes as lesions, many of which are based on subjec-tive assessment by an observer, such that variation in in-terpretationbetweenstudiesisimpossibletocontrol. However, the greatest problem is that the study popula-tions examined are relatively poorly defined and poten-tiallyheterogeneous.Forexample,anyarbitraryfixed proportionofapopulation,suchasthesmallest5%of fetuses, will include a mixture of pathologically growth-restricted fetuses and those who are constitutively small, with many studies defining inclusion based on fetal size rather than growth. However, the progressive refinement ofclinicalsubgroupingforinclusion,throughuseof Dopplerstudiesandplasmabiomarkers,hasfacilitated animprovedunderstandingofFGRpathology,and emerging well-defined subgroups of placental abnormal-ities are now becoming increasingly recognised. Despitethesepotentialdifficultiesininterpretation, therearepatternsofplacentalhistologicalchangesthat are well reported and common to most studies of the pa-thology of FGR. First, it should be noted that, overall, ap-proximatelyonequarterofplacentasassociatedwith FGR/SGA (however defined) lack any morphological ab-normality on routine macroscopic and histological exam-ination[1] . In those cases with lesions present, the most frequentmacroscopicabnormalitythatoccurswithin-creasedfrequencyinFGRplacentasispatchyplacental infarction, being present in around 25% of term FGR ver-sus 10% of controls [214] . This finding illustrates a com-mon theme when interpreting placental findings in FGR, thatthefrequencyofseverallesionsisincreased,but sincesuchlesionsareonlypresentinaminorityofaf-fected cases and are also found in some normal controls, and since non-FGR is far more frequent than FGR in the population, the positive predictive value of such findings for pathological FGR in any given unselected case will be very low. Similarly,severalmicroscopicabnormalitieshave been reported more frequently in FGR placentas, none of which are present in the majority of affected cases in any study, and almost all of which may be encountered in oth-ernon-FGRpregnancies,including [27,925] :villous infarcts (an example from a placenta in a case of FGR is shown infigure 1 a, b), placental abruption/retroplacental haemorrhage,villousmorphologicalabnormalitiessug-gestiveofreduceduteroplacentaland/orfetoplacental flow(hypoxiclesion)suchassyncytiotrophoblast knots,excesscytotrophoblastcells,thickenedtropho-blastic basement membrane, villous fibrosis, hypovascu-lar terminal villi, reduced villous volume, reduced inter-villousspace,andnon-specificinflammatorylesions[villitisofunknownaetiology(VUE)].Inaddition,histologicalfeaturesindicatingdefectiveremodellingof spiral arteries into uteroplacental vessels may be identi-fied, such as inadequate physiological change, fibrinoid necrosisandacuteatherosis(adenseperivascularlym-phocyticinfiltratewithintimalarterialfoamymacro-phages; see fig.2 a, b) [2628] .Downloaded by: 198.143.39.65 - 8/15/2015 11:01:29 AM Placenta in Early and Late FGRFetal Diagn Ther 2014;36:117128DOI: 10.1159/000359969119 Association of Placental Pathologies with Clinical Subgroups The use of well-defined specific clinical subgroups of definite pathological FGR should allow determination of anyspecificpatternsofplacentalabnormalities,and hence,suggestpathophysiologicalpathways.Theintro-ductionofuterineartery(UtA)Dopplerstudiesidenti-fied FGR cases with evidence of maternal uterine malper-fusion, with placental bed biopsies in these cases demon-stratingdefectivespiralarteryremodelling,including inadequate physiological change and fibrinoid necrosis/atherosis[27,29].Ferrazzietal. [30]studiedplacentas from women with FGR and reported that extensive hy-a b Fig. 1. Placental infarct, secondary to maternal vascular underper-fusion. At low magnification ( a ), the infarct can be seen as an area with severe reduction of the intervillous space and aggregation of villi.Intheareasurroundingtheinfarcttheintervillousspaceis increased and there are several very small villi. At higher magnifi-cation ( b ), villous aggregation can be better appreciated, and the syncytiotrophoblasticshowvariousstagesofdegeneration,with pyknosis, karyorrhexis and replacement by fibrin-like eosinophil-ic amorphous (hyaline) material. a b Fig. 2. Lesions of acute atherosis at low ( a ) and high (b ) magnifica-tion.Thearterialwallsareirregular,necroticandreplacedwith fibrin-like eosinophilic material. In later stages, there are greater numbersoflipid-ladenmacrophages(lipophages)andthereisa perivascularmononuclearinflammatoryinfiltrate.Theselesions occur in vessels with inadequate extravillous trophoblast invasion. Color version available onlineColor version available onlineDownloaded by: 198.143.39.65 - 8/15/2015 11:01:29 AM Mifsud/Sebire Fetal Diagn Ther 2014;36:117128DOI: 10.1159/000359969120poxicvillousdamage(morethan30%ofterminalvilli withoneormoreofthefollowing:syncytiotrophoblast knotting, excess cytotrophoblast cells, thickened tropho-blastic basement membrane, villous fibrosis, hypovascu-larity),non-peripheralinfarctsinvolvingmorethan5% ofplacentalparenchyma,andplacentalabruptionwere found only in those FGR cases with abnormal UtA velo-cimetry, regardless of the presence or absence of pregnan-cy-inducedhypertension(PIH).UtAvelocimetryis therefore a marker for defective remodelling of spiral ar-teries with consequent placental malperfusion and asso-ciated impaired fetal growth. Abnormal UtA Doppler Is Associated with a Common Set of Placental Ischaemic Lesions in FGR and Preterm PET Thecombinationofplacentalbedandparenchymal lesions described in FGR with abnormal UtA velocimetry isessentiallyidenticaltolesionsdescribedinpreterm PET, particularly when subsets of preterm PET and pre-term FGR are compared[12, 15, 26, 2837]. Indeed, ab-normally raised UtA resistance is associated with defec-tive trophoblast migration on placental bed biopsies in-dependentofthepresenceorabsenceoftheclinical syndrome of PIH [38] . Whilst placental findings in preterm PET and FGR are therefore similar, defining the extent of similarity and its dependenceonabnormalUtADopplerwouldbebest achieved by a quantitative meta-analysis, but this is dif-ficultduetothereasonsdescribedintheIntroduction. Nevertheless, two studies [12, 35] were performed by the same group on the same study population (delivering be-tween 22 and 32 weeks gestation); including 48 cases with FGR(1 vessel not reported 10.0Chronic maternal vasculitis: 1 vessel only not reported 20.0Absence of spiral artery physiological changes not reported 30.0Fibrinoid necrosis and/or atherosis of spiral arteries: multiple arteries 10.424.0 Fibrinoid necrosis and/or atherosis of spiral arteries: 1 artery only 12.5Villous fibrosis: severe* 27.1 82.0Villous fibrosis: mild 39.6 not reportedVillous hypovascularity: severe* 25.0 72.0Villous hypovascularity: mild 39.6 not reportedVillous infarction: multiple 37.5 45.0Villous infarction: single 20.8 24.0 (focal)Villous infarct location: peripheral 10% 10.4 11.0Villous infarct location: central 90% 29.2 36.0Villous infarct location: peripheral & central 16.7 18.0Syncytiotrophoblast knotting: severely increased 39.0 40.0Syncytiotrophoblast knotting: mildly increased 43.8 not reportedProliferation of cytotrophoblast cells: severe 36.9 42.0Proliferation of cytotrophoblast cells: mild 27.1 not reportedAbruption: frank 10.4 12.0Abruption: consistent with 31.3 37.0Perivillous fibrin deposition: severely increased 45.8 43.0Perivillous fibrin deposition: mildly increased 41.7 not reportedFetal vascular thrombosis not reported 4.0Haemorrhagic endovasculitis not reported 12.0Avascular terminal villi: multifocal 18.8 20.0Avascular terminal villi: focal 29.2 25.0Nucleated erythrocytes: numerous 17.576.0Nucleated erythrocytes: present, not numerous 56.3* Parameters with a significant difference between preterm FGR and preterm PET groups, with respective percentages in bold. Percentages are italicised if significantly different from control population used in original study. In the preterm symmetrical FGR study [12], the control population was preterm placentas from pregnan-cies without FGR (340 cases). In the preterm PET study [35], the control population (353 cases) was a combina-tion of spontaneous premature rupture of membranes (192 cases) and premature labour with intact membranes (161 cases).Downloaded by: 198.143.39.65 - 8/15/2015 11:01:29 AM Mifsud/Sebire Fetal Diagn Ther 2014;36:117128DOI: 10.1159/000359969122esasconsequencesofsuchaprimaryabnormality,and several other lines of evidence suggest that this is errone-ous. Changes in the stem villous arteries are strongly sug-gestive of a response to chronic vasoconstriction [45] , and develop in parallel with a progressive UA Doppler abnor-mality[45, 55] , and similar downstream changes in termi-nalvilliarepresentintheterritoryofanupstreamfetal vesselwithocclusivethrombus [56,57] .Importantly,in most cases there is also defective uteroplacental perfusion withassociatedUtADopplerstudiesprecedingtheUA Doppler changes[46, 47] . Furthermore, experimental ev-idence in sheep demonstrates a rapid increase in UA re-sistance upon reducing maternal placental perfusion[58, 59]andthereisexperimentalevidenceofrapidandre-versiblefetalvasoconstrictioninthehumanplacentain response to hypoxia[60] , in an analogous manner to the lung,involvinginhibitionofpotassiumchannels [61] . Similartothepulmonarycirculation,hypoxia-induced andK +channel-mediateddepolarisationofvascular smooth muscle cells activates voltage-gated L-type gated Ca 2+ channels, which provides cytosolic Ca 2+ for activat-ing the contractile apparatus [62] . Such hypoxic vasocon-strictionallowsautoregulationtooptimisefetomaternal flow matching, but when widespread results in increased globalflowresistance.However,experimentaldemon-strations of possible fetal hypoxic vasoconstriction in the placentahavebeenmadewithoxygentensionsthatare higher than those in the placenta in vivo[6062] , and to thebestofourknowledge,nostudieshavereportedthe effect of hypoxia at levels approximating those in the pla-centa, on preparations including the entire fetal subchori-onicvasculature.Therehavebeenreportsstudyingpla-cental levels of hypoxia on isolated chorionic plate arteries and veins with diameters of 268 13 m (arteries) and 266 19 m (veins) at 2% oxygen [63, 64] , showing increased chorionic vein vasodilatation in response to nitric oxide, but no convincing hypoxic chorionic artery vasoconstric-tion.However,theisolatedvesselsusedinthesestudies were too large to represent stem villus vessels, whose di-ameter is typically in the range of 10100 m in both nor-mal and FGR pregnancies[54] . Regulation of stem venous tonemayalsooccurtomaintainwaterbalance [45,6567] . To adequately test these hypotheses, one would need an experimental system that can maintain placental coty-ledons at physiological levels of oxygenation and also tru-ly representative levels of hypoxia, while allowing for in-dependentvariationofintervillousperfusionpressure and for measurement of vascular tone across all the differ-entvesseltypes(arterial,venous,differentcalibres).To date, such a system has not been reported. More recently, the similarity of the changes in the stem villus arteries between severe FGR and preterm PET was further demonstrated by the discovery that in both clini-cal situations the smooth muscle cells in the stem villus arteriesshowmarkedlyreducedexpressionofcystathi-one-lyase, responsible for synthesis of the potent vasodi-lator hydrogen sulphide (H 2 S). Its reduced expression in the fetal villous resistance vessels supports the view that there is vasoconstriction in the fetal stem villi in associa-tion with abnormal umbilical Doppler profile [68] . Inter-estingly,cystathione-lyaseisnotonlydownregulatedin cases with abnormal UA Doppler profile, but shows in-creased expression in PET with normal UA Doppler find-ings compared to non-PET controls, although expression in both groups appeared heterogeneous by Western blot-ting. In addition, the PET cases with normal UA Doppler findingswerepretermcases(deliveredat29.51.5 weeks), while the control cases were delivered at term (39 0.6 weeks) [68] . Other Placental Histological Lesions Associatedwith FGR In addition to the typical uteroplacental and fetopla-centalvascularlesionsdescribedabove,severalstudies have reported an excess frequency of VUE in FGR, with widely varying rates ranging from 8 to 90% [5, 11, 13, 16, Fig. 3. Fetal stem arteries (within the large villi) showing narrow-ing of their luminal diameters and thickened walls and associated terminalvillouschangesofhypovascular,small,straightvilli. These changes are associated with abnormal UA Doppler profiles. Color version available onlineDownloaded by: 198.143.39.65 - 8/15/2015 11:01:29 AM Placenta in Early and Late FGRFetal Diagn Ther 2014;36:117128DOI: 10.1159/00035996912319, 6972] . VUE is characterised by patchy villous infil-tration by chronic inflammatory cells, mainly histiocytes and lymphocytes, especially in basal/maternal floor villi, in the absence of an identifiable infective cause. It is pos-tulatedthatVUErepresentsanabnormalmaternofetal immunereaction,withconsequentlyincreasedriskof VUE recurrence[7377] . VUE is approximately twice as common and more diffuse in multigravidity[78] , and it has a higher than expected concordance in twin pregnan-cies [79] .ThepathologicalfeaturesofVUEarewellre-viewedelsewhere [80] ,althoughthereisconsiderable variationamongstexpertpathologistsinrecognising this histological lesion[81] . Nevertheless, there is a con-sistently increased frequency of VUE in FGR, and also in placentas from cases of PIH and PET, with and without associated FGR, despite the majority of cases being asso-ciated with normal pregnancy outcome [82, 83] . The pre-cise mechanism by which patchy inflammation may lead to impaired fetal growth remains undetermined. Pathology Associated with Late-Onset FGR and PET In the context of the subtypes of FGR defined by Dopp-ler abnormalities, and the similarity of placental findings in early-onset FGR and PET, it is interesting to note in-creasing recognition of clinical groups of PET with differ-ent features and outcomes, Doppler findings, biochemi-cal profile and placental abnormalities. PET presenting at term is associated with a lower fre-quency and severity of FGR compared to early-onset PET [84] . This phenomenon could therefore represent either themanifestationofdifferentpathophysiologicalpath-waysleadingtoasimilarmaternalsyndromeinearly- versus late-onset PET, or may represent the same disease process at different stages or rates of evolution. Late-onset PET could therefore be hypothesised to represent a pro-cess leading to maternal endothelial damage which is un-related to impaired early trophoblast invasion, or associ-atedwithrelativelymildimpairmentoftrophoblasticinvasionofthespiralarteries,orwithadefectinuteroplacentalperfusionthatbecomesfunctionallysig-nificantonlylateringestation,orwithsimilarimpair-mentoftrophoblasticinvasiontothatseeninpreterm PET,butwithadelayedorreducedmaternalresponse (althoughthislatterexplanationwouldnotexplainthe lower incidence and severity of FGR with late-onset PET). Without definitive evidence for and against these possi-bilities, it is possible that each may contribute to a propor-tion of PET with late presentation. Pathological Features Multiplestudieshavereportedthatplacentasfrom PETpresentingattermhaveasignificantlylowerfre-quencyofhistologicallesionsassociatedwithimpaired maternal uteroplacental perfusion compared to early-on-set disease. In an early study of 158 PET placentas there was an inverse relationship between gestation at delivery and the frequency of non-peripheral infarcts, villous hy-permaturity and decidual arteriopathy[85] and another studyof37PETplacentasconfirmedasignificantlyre-duced frequency of non-peripheral infarcts in cases pre-senting near term[86] . A large study (with >900 PET cas-es and >7,000 controls) also reported an inverse relation-shipbetweenthefrequencyofplacentallesionsof maternalunderperfusion(villousinfarction,villousag-glutination, increased syncytial knots, increased intervil-lous fibrin, distal villous hypoplasia, persistent vasculari-sationofbasalplatearteries,muralhypertrophyofde-cidualarterioles,acuteatherosis),andgestationalage. Despite this inverse relationship, even in PET delivered at or beyond 37 weeks gestation, the frequency of maternal underperfusion lesions was relatively high at around 30% [87] . In another series of >1,200 PET placentas, a compa-rable figure of 26% was reported[88] ; in this study, the authorsalsoshowedanassociationoflowplacental weight (