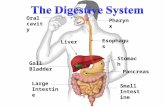
Physiolgoy Lecture 9, GIT 3 (Pancreas and Intestine) (Slides)
-
Upload
ali-hassan-al-qudsi -
Category
Documents
-
view
151 -
download
2
description
Transcript of Physiolgoy Lecture 9, GIT 3 (Pancreas and Intestine) (Slides)

Bile duct from liver
Hormones(insulin,glucagon)
Endocrine portionof pancreas(Islets of Langerhans)
Acinar cells secrete digestive enzymes
Duct cells secrete aqueousNaHCO3 solution
Exocrine portion of panaceas (Acinar and duct cells)
The pancreas contains exocrine and endocrine cells
stomach
Sphincter of Oddi

The pancreas contains exocrine and endocrine cells.• Endocrine cells are isolated islands called islets of
Langerhans. These islets secrete hormones (insulin and glucagon) into blood.
• The exocrine pancreas secretes pancreatic juice consisting of a. digestive enzymes: secreted by the aciner cells b. an aqueous alkaline fluid: secreted by the duct cells . The alkaline
fluid has sodium bicarbonate.****Pancreatic exocrine secretion is regulated by secretin and CCK
hormones that secreted by the small intestine. **Secretin stimulates the secretion of sodium bicarbonate from the
pancreas. ***CCK stimulates (regulates) the secretion of pancreas digestive
enzymes.

Pancreatic digestive enzymes
• The digestive enzymes produced by pancrease are:1. proteolytic enzymes: They are for protein digestion***Trypsinogen, Chymotrypsingen and
procarboxypeptidase.
2. pancreatic amylase: It converts starch to disaccharides.
3. pancreatic lipase: It hydrolyzes (digests) dietary lipids. ## Note: proteolytic enzymes are secreted in inactive forms
and are activated in small intestinal lumen, while lipase and amylase are secreted in active forms.

Activation of pancreatic proteolytic enzymesOccurs in small intestine lumen
• Trypsinogen Trypsin
• Chemotrypsinogen chemotrypsin
• Procarboxypeptidase carboxypeptidase
entrokinase
Entrokinase is produced by duodenal epithelial cells. It coverts trypsinogen into active proteolytic enzyme (trypsin)
**** Once trypsin is formed it acts on trypsiongen to produce trypsin (autocatalytic). It also acts on chemotrypsinogen and procarboxypeptidase to activate them.

Pancreatic digestive enzymes (cont.)
• The active pancreatic digestive enzymes act on different places protein polypeptide chain. The end result of protein digestion by these proteolytic enzymes is small polypeptides and individual amino acids.
• Pancreas produces trypsin inhibitor which stops trypsin (if it is formed accidentally) action within pancreas.
• Pancreatic amylase breaks down polysaccharides into disaccharides
• Pancreatic lipase breaks down triglycerides into monoglycerides and fatty acids.

Factors regulate pancreatic secretion
• Neural – parasympathetic nervous system stimulate pancreatic secretion.
• Hormonal:
a. Secretin- Stimulus for secretin secretion is the acidity of the
chyme reaching the duodenum- Effects of secretin is to increase secretion from
pancratic ducts ( alkaline watery fluid contains large amount of HCO3 ions) to neutralize the acid.
b. Cholycystokinin- Stimulus for CCK secretion is presence of fat (mainly)
and protein in the chyme reaching duodenum.- Effect of CCK is to stimulate acinar cells to produce
digestive enzymes.

Acid induodenallumen
Fat and proteinproducts induodenal lumen
Secretin releasefrom duodenalmucosa
CCK releasefrom duodenalmucosa
(Secretin carriedby blood)
Pancreatic acinarcells
Secretion of aqueousNaHCO3 solution intoduodenal lumen
Secretion ofpancreatic digestiveenzymes intoduodenal lumen
Pancreatic ductcells
Neutralizes Digests(CCK carriedby blood)

The liver carries out numerous functions. One is bile production.
• It carries out the metabolic processing of nutrients.• It detoxifies or degrades body wastes.• It synthesizes most plasma proteins (except
immunoglobulin).• It synthesizes most clotting factors.
• It stores substances such as glycogen and fats.• It activates vitamin D.• It removes bacteria and old RBCs .• It excretes cholesterol and bilirubin.

Heart
AortaInferiorvena cava
Hepatic veinHepatic artery
Liversinusoids
Liver
Hepatic portal vein
Digestivecapillaries
Digestivetract
Arteries todigestive tract
Blood enters the liver from the digestive tract by the hepatic portal system. The portal vein of this system breaks into a capillary network, the liver sinusoids. Blood leaves liver through hepatic vein. Also liver receives arterial blood through hepatic artery.

Branch ofhepatic artery
Branch ofhepatic portal vein
Connectivetissue
Kupffer cell
Bilecanaliculi
Sinusoids
Central vein
Hepatic plateCords of hepatocytes(liver cells)
Bileduct
•The liver lobules are delineated by vascular and bile channels. Hepatocytes continuously secrete bile into bile channels.

Bile
• Bile contains: water, electrolytes, bile salts, bile pigment (bilirubin), lecithin and cholesterol.
• Bile does not contain digestive enzyme, but it (bile salts) helps in digestion and absorption of fats.
• Bile is stored and concentrated in gallbladder. CCK causes contraction of gallbladder and relaxation of sphincter of Oddi (more bile goes to intestine).
• Bile salts are secreted by hepatocytes. After facilitating the digestion and absorption of fat in small intestine, they reabsorbed from terminal ileum to be reused again (entrohepatic circulation of bile salts).

Bile salts Cholesterol
Liver
Common bile duct
Duodenum
Gallbladder
Sphincter of Oddi
Portalcirculation
Terminal ileum
Colon
***Bile ducts from the lobules in the liver converge to form the common bile duct. This duct transports bile from the liver to the duodenum.
***Bile is stored in the gallbladder between meals. After a meal the liver and gallbladder secrete bile into the small intestine for fat digestion
Entrohepatic circulation of bile salts

Bile salts help in fat digestion and absorption.
• The detergent action of bile emulsifies fats. Fat globules are broken into smaller droplets, increasing surface area to facilitate enzymatic attack (pancreatic lipase).
• Pancreatic lipase is attached to a fat droplet and digests .• Bile salts adsorb on the surface of small fat droplets, preventing
the droplets for recoalescing. This also helps enzymatic attack.• Bilirubin is a waste product excreted in the bile. • Its secretion increases by:1. hormonal mechanism: secretin hormone increases secretion of
alkaline watery solution from the bile caniculi.2. neural mechanism: parasympathetic stimulation increases bile
secretion.3. Bile salts themselves stimulate the secretion of further bile.

Negativity chargedH2O-soluble portion(a carboxyl group atthe end of a glycineor taurine chain)
Lipid-soluble portion(derived from cholesterol)
Small lipid (fat)droplet with bilesalt moleculesabsorbed onits surface
A bile salt consists of a lipid-soluble part that dissolves in the fat droplet and a negatively charged, water-soluble part that projects from the surface of the droplet.
the structure of bile salts and their adsorption on the surface of a small fat droplet

Large fat droplet
Through action of bile salts
Lipidemulsion
Formation of a lipid emulsion through the action of bile salts. When a large fat droplet is broken up into smaller fat droplets by intestinal contractions, bile salts adsorb on the surface of the small droplets, creating shells of negatively charged, water-soluble bile salt components that cause the fat droplets to repel each other. This action holds the fat droplets apart and prevents them from recoalescing, increasing the surface area of exposed fat available for digestion by pancreatic lipase.

Hydrophobic core
Hydrophilic shell
All lipid-soluble
Cholesterol
Bile salt
Water-soluble portion
Lipid-soluble portion
Lecithin
Schematic representation of a micelle. Bile constituents (bile salts, lecithin, and cholesterol) aggregate to form micelles that consist of a hydrophilic (water-soluble) shell and a hydrophobic (lipid-soluble) core. Because the outer shell of a micelle is water soluble, the products of fat digestion, which are not water soluble, can be carried through the watery luminal contents to the absorptive surface of the small intestine by dissolving in the micelle’s lipid-soluble core.

Excretion of bilirubin in bile
• Bilirubin is waste product formed from breakdown of old RBC. It does not share in fat digestion. It gives yellow color to bile
• It is excreted by liver cells into bile and finally into intestine.
• Some of bilirubin is absorbed by blood to be excreted in urine (giving urine it’s yellow color.
• Bilirubin in intestine is modified by intestinal enzymes to produce substance that gives stool it’s characteristic brown color

The small intestine is where most digestion and absorption occur.
• Its three segments are the duodenum, jejunum, and ileum.
• The process of segmentation mixes and slowly propels the food.
• Segmentation contractions are initiated by BER cells.
• The circular smooth muscle responsiveness is influenced by the distension of the intestine, gastrin, and extrinsic nerve activity.
• Segmentation mixes chyme with secretions and slowly moves the contents through the tract.
• The migrating motility complex is an internal housekeeper. It sweeps the intestine clean between meals.

Ascendingcolon
Ileocecal valve
Pushesvalve closedand contractssphincter
Cecum
Gastrin
Ileocecal sphincter
Pushes valve openand relaxes sphincter
Ileum
Appendix
Newmeal
***The ileocecal juncture (between the small and large intestine) prevents contamination of the small intestine by colonic bacteria.
*** Ileocecal sphincter: is relaxed by distention of ileum and hormone gastrin
Pressure on the cecal side pushes the valve closed and contracts the sphincter, preventing the bacteria-laden colonic contents from contaminating the nutrient-
rich small intestine.

Other facts about the small intestine include:
• It does not secrete digestive enzymes. The pancreas secretes enzymes into the tract.
• The small intestine enzymes complete digestion intracellularly. These include the disaccharidases and aminopeptidases.
• A lactose intolerance is due to a deficiency of lactase.• The small intestine has adaptations to maximize absorption. The mucosal
lining has a large surface area due to its circular folds and fingerlike projections called villi. The epithelial cells also have microvilli.
• A villus has a cover of epithelial cells, a connective tissue core, a capillary network, and the terminal lymphatic vessel.
• During absorption molecules produced by digestive enter the capillary or lymphatic vessel.
• The mucosal lining has a rapid turnover. The crypts of Lieberkuhn have stem cells for cell regeneration.

Circular Fold :These folds increase the surface area 3 times
Villi
MicrovilliOr
Brush border
villus
The folds are covered by villi which increase the surface area 10 times
Microvilli increase the surface area 20 times.
Small intestine has huge absorptive surface area (about 200 square meters)

Table 15-6, p. 496

The epithelial cells in the inner lining of the small intestine have a variety of transport mechanisms.
• Energy-dependent sodium transport absorption drives passive water absorption.
• Sodium is pumped from the tract lumen into the interstitial fluid. From their it enters capillaries by diffusion.
• The transport of sodium creates an osmotic pressure. Water follow the sodium as it is absorbed.
• Glucose and galactose are moved by secondary active transport. They are cotransported with sodium.
• Fructose is absorbed by passive facilitated diffusion.• Amino and small peptides are absorbed across intestinal cells
by secondary active transport.

Digested fat is absorbed passively and enters the lymph. It undergoes a series of
transformations for absorption.
• Monoglycerides and free fatty acids are produced by hydrolysis. These water-insoluble products are carried to the inside of water-soluble micelles.
• On the mucosal surface these molecules leave the micelle and passively diffuse through the lipid bilayer of the luminal membrane. They are resynthesized into triglycerides inside the epithelial cells.
• There they form water-soluble chylomicrons which leave the cells by exocytosis.
• They enter the central lacteals, lymphatic vessels.

Fig. 15-23, p. 500
Lipid emulsion
Micelles
Epithelialcell of villus
Lumen
(Exocytosis)
Central lacteal
Aggregate andcoated withlipoprotien
Short ormediumchain Basement
membrane
Capillary
Lumen
Micellesdiffusion
Micelle
Microvillus
Fatty acids,monoglycerides
Passive absorption

Other facts on adsorption include:
• Vitamin adsorption is mainly passive. Water-soluble vitamins are absorbed with water. Fat-soluble vitamins are absorbed in micelles.
• Iron and calcium absorption is regulated. Only a part of ingested iron can be absorbed.
• Some absorbed iron is immediately transported to the blood. Transferrin carries some iron to the bone marrow. Excess iron is stored in the ferritin pool. Unused iron is lost in the feces.
• Most calcium is absorbed by active transport. About two-thirds of ingested calcium is absorbed. The remaining one-thirds is eliminated.
• Most absorbed nutrients immediately pass through the liver for processing. The liver monitors nutrient molecules and controls their concentration in the blood or lymph leaving the liver.
• Extensive absorption by the small intestine keeps pace with secretion. A biochemical balance exists among the stomach, pancreas, and small intestine.
• Diarrhea results in the loss of fluid and electrolytes.

The large intestine is mainly a drying and storage organ.
• It consists of the colon, cecum, appendix, and rectum.
• The colon consists of the cecum, ascending colon, transverse colon, descending colon, and sigmoid colon.
• Most digestion and absorption has been accomplished in the small intestine. The colon receives indigestible food, unabsorbed biliary components, and the remaining fluid.
• The colon extracts water and salt and eliminates the feces.
• Contractions of the haustrae slowly shuffle the colonic contents back and forth. They are initiated by the autonomous rhythmic contractions of the smooth muscle in the wall of the large intestine.
• Mass movements propel colonic contents long distances. They drive the feces into the distal part of the large intestine. Material is stored here until eliminated by defecation.

Table 15-7, p. 501

The feces are eliminated by the defecation reflex .
• Muscle contractions and the relaxation of two sphincter muscles eliminate the feces.
• Constipation occurs when the feces become too dry. There is prolonged distention of the large intestine.
• The large-intestine secretion is entirely protective. It consists of an alkaline mucus solution which protects the intestinal mucosa.
• The colon contains many beneficial bacteria. Their functions include making vitamin K and enhancing intestinal motility.
• Intestinal gases are absorbed or expelled.

There are several important gastrointestinal hormones.
• Gastrin increases the secretion of hydrochloric acid and pepsinogen and enhances gastric motility.
• Secretin inhibits gastric emptying and gastric secretion, stimulate the pancreas to produce sodium bicarbonate, and stimulates the liver to produce bile.
• CCK inhibits gastric motility and secretion, stimulates pancreatic enzymes and signals the gallbladder to secrete bile.
• GIP promotes metabolic processing of nutrients once they are absorbed.