Philhealth circ61_2012
Transcript of Philhealth circ61_2012
-
7/28/2019 Philhealth circ61_2012
1/7
Re pub lic of the Philippine sP^t- "@ ,,>'?PHILIPPINE HEALTH INSURANCE CORPORATION** v "
Citystate Centre, 709 Shaw Boulevard, Pasig CityHealthline 441-7444 www.philhealth.eov.ph
PHILHEALTH CIRCULARNo. D(jI , s. 2012c^T O :A L L I N D IV I D U A L L Y P A Y I N G M E M B E R S , A C C R E D I TE D
HEALTH CARE PROVIDERS, ACCREDITED COLLECTINGAGENTS, PHILHEALTH OFFICES AND ALL CONCERNED
SU BJEC T : N ew Provisions on the Issuance of the Individual Policy
I.RATIONALEThe Individual Policy Contract (IPC ) is a legal docum ent executed by and betweenPhilHealth and an Individually Paying M ember (IPM ) as evidence of m embership andcoverage in the National Health Insurance Program (NH IP). It is intended to guide andencourage m emb ers lo sustain act ive part icipat ion in the N HIP and gu arantee theentitlement to benefits thereby providing continuous financial risk protection in health carecosts within a specified validity period enunciated under PhilHealth Circular No. 20 s. 2012.In order to ensure utm ost customer satisfaction, the IPC gu arantees more flexible terms inaccessing health care benefits and shall serve as the primary docum ent for IPMs and theirdependen ts to avail of benefits.Effective January 1, 2013, IPC issuance shall form part of the regular registration procedureamong individual mem bers under the Individually Paying Program (IPP).
I I .EXCLUSIONActive IPM s covered by the Group P olicy Contract sealed between PhilHealth and theOrganized G roup under the iGroup Program shall not be required to sign IPC. Coverageunder the iGroup shall be separate and distinct from that covered under the IPC.
III.SUPPLEMENTAL IMPLEMENTING GUIDELINESStarting Janua ry 1, 2013, all IPM s shall be issued an enhan ced IPC w hich includeadditional amendatory conditions:
LC -_F{PI!i? P"')r:- '"@ ': 'rr ':
-
7/28/2019 Philhealth circ61_2012
2/7
A. IPC VALIDITYAn option to apply for a minimum of twelve (12) months IPC validity, twenty-four (24) or a maximum of thirty-six (36) months with fiscal year application;
a.A 3-yea r IPC validity shall be required to qualify a me m ber to avail ofCase Type Z Benefits;
b.Entitlemen t to Case Ty pe Z benefits also requires a minimum of one (1)year advance premium payment.
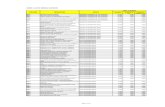
To acquire an IPC, an IPM shall be required the following minimum prem iumcontribution according to num ber of years contracted and shall be locked in tothe current premium rate if fully paid upon signing of the IPC :
a. An IPM who w ould opt for monthly mode of paym ent will still berequired to pay the initial 25% p remium contribution for a 1 year IPC.Succeeding payments may then be made mon thly.
b. An IPM cannot change the originally set mode of paym ent within thevalidity of the IPC
B. DEADLINE OF PREMIUM REMITTANCE AND MODE OF PAYMENT1. Premium contributions may be p aid or remitted according to any of the
following mode:
j CERTiFsii.i
IPCValidity
1year2years3years
Option1AdvanceFullPayment
PremiumcontributionshallbelockedinandcomputedbasedonthecurrentrateuponsigningoftheIPC.IPMshallnotbechargedwithunderpaymentifanypremiumincreaseisimplementedwithinavalidityperiod.
Option2MinimumPremiumRequirement
2 5 % o fan n u a lpremium5 0 %o f an n u a lpremium1yearfullpayment
EffectofOption2tosucceedingcontributionsincaseofpremiumincreasewithinavalidityperiodPremiumcontributionshallbeadjustedbasedoncurrentapplicablerateuponpaymentorremittance
-
7/28/2019 Philhealth circ61_2012
3/7
a.Monthly - one (1) month premium contribution which shall be paid onor before the last working day o f the month prior to the applicable
month;b.Quarterly - twen ty-five percent (25% ) of the annual prem ium
contribution which shall be paid on or before the last working day ofthe month prior to the applicable three-month period;
c.Semi-annual @ fifty percent (50%) of the annual premium contributionwhich shall be paid on or before the last working day of the m onth
prior to the applicable six-month period;d.Annual - one hundred percent (100% ) of the annual premium
contribution which shall be paid on or before the last working day ofthe month prior to the applicable twelve-month period;
2. A ll premium contributions shall have prospective application. Exceptions tothis rule are:
1. IPMs who shifted from a different paying mem bership category in order toavoid gaps in entitlement to benefits and premium remittance. Thus, IPPpremium payment for the current period may be accepted provided thatthe member is a shifter with previous active contribution immediately prior
to applicable period.Example: Emploved to IPP
JAN 2013FEB 2013IPC Validity (1 year/semi-annual moae;
EmployedIPMFeb 2013 - January 20141.Require 50% advance premium
PremiumAccept IPPcomputed at Php 1,800 annualPaidpremiumpremium rate for CY 2013 OR PhP
900.00 to cover Feb - July 2013;2.Remaining 50% should be paid on
or before the last working day ofJuly 2013 to cover August 2013 to
January 2014.3.Any increase in CY 2014 shall be
effective upon renewal of the IPC.
2. Acceptance of retroactive paymen ts for overdue prem ium/s w ith interestcharges.
:.rRT!."?cfjJn-vJ.'s copy
-
7/28/2019 Philhealth circ61_2012
4/7
c. GRACE PERIODGrace period shall be allowed for delayed remittance once w itnm a twelvemonth period. Succeeding delay/s in premium remittance w ithin a twelvemonth validity period shall be subject to corresponding interest charge/s thatmay be imposed by the Corporation as penalty;Grace period may van/ according the elected m ode of paym ent;
Mode ofPaymentAnnualSemi-annualQuarterly
Grace period Interest charge forPaym ent made afterthe Grace Period
30 days (renewal)15 days10 days5 days
Subject to applicableinterest rates and
penalties
D. PAYMENT OF OVERDUE PREMIUMS1.Interest charges shall be applicable to the validity period w ith unpaid or
incorrect premium contribution.2.Paym ent of overdue premium /s plus charges, // applicable, may be allowed
within 60 days from date of discharge from hospital confinement to allow theprocessing of benefit claim/s;
Example: IPM w ith 1 year IPC/quarterly mode of payment
4.
RemarksPayment on the 4r" qtr w ill require:
-2"" Qtr plus interest charge-3r" Qtr plus interest charge, and-4lh Qtr contribution w ithout interest charge if m ade
within the 10 days grace period; or-4m Qtr contribution plus interest charge if paid
Benefit claim m ay be processed if payment for the junpaid period 0 " Q tr), with interest charges, were jmade before the end of the 60 days prescribed period :(in this case, before Nov 15) to file a benefit claim
No benefit claim wilh retroactive pay men t/s shall be processed unlessarrearage s are paid in full .
Filing of claim s for those covered by premium arrearages paid shall be theresponsibility of the member and shall be submitted to the nearest PhilHealth
CEIm w ^
RUE
-
7/28/2019 Philhealth circ61_2012
5/7
Local Health Insurance Office. The LH IO shall assist the IPM on theprocedures; involved in direct filing.
5.The PhilHe alth Official Receipt shall reflect paym ents made for prem iumarrears and interest charges.
6.The Fund M anagement Sector shall guide the PRO Fund M anagementSections on proper recording of advance payments as premium collection for
applicable year/s.
E. IPC RENEW ALRenew al is the process of applying for a subsequent IPC covering a new validity period orthe process of ex tending the go od status of a co ntract prior to its expiration to effectcontinuity or resump tion of benefit entitlemen t. IPC ren ew al for purposes of this Circularmay also apply to an expired and /or terminated IPC.
1.The IPM shall request for the renew al of his/her an IPC within the quarterprior to its expiration to avoid gaps in benefits availment. Regular IPCapplication procedure shall apply.
2.Non-com pliance to the payment terms of the IPC or any form ofmisrepresentation shall cause the suspension or termination of the contract.However, renewal pre-conditions shall be made available for members
subject to Ihe approval of PhilHealth.3.Renew al far a suspended or terminated IPC m ay be requested by the
member subject to compliance with specific requirements, such as:a.Full premium payment covering the unpaid period up to the end
validity of the contract with interest charges, as applicable;b.Completion of ihe suspension period, if applicable.
c.Any other documentary p re-requisites that the Corporation m ayimpose as it may deem fit and necessary to effect renewal of the contract.
4.Premium requirement for the payment of the unpaid period shall be based onthe applicable rate for the missed period.
F. BENEFITS ENTITLEMENT1. Ent i tlemen t to avai l of benef i ts shal l be based on the 3 /6 m inimum
requirement regardless of type of illness.a. Exception to this rule are Case Type Z illnesses which require
advance full payment of at least one year premium contribution and
bPiJ-rajMA. TCI'ES'Vfl, OiJu'vOIT/ iDa.S:4SJtgle_1CERTiFiED IR'JF CCFV '
-
7/28/2019 Philhealth circ61_2012
6/7
other future benefits specifically requiring more m an j m ontnscontribution after the effective date of this Circu lar;
b.The 9/12 prerequisite for maternity and other procedures enum eratedunder PhilHealth Circular No 36, s. of 200 6 is superseded by this
guarantee;c.Counting of the three months requirement shall be reckoned from the
immediate 6 months prior to confinement.d.Reckoning of the 45 days allowance for benefits entitlement shall be
based on the applicable annual validity period of an IPC.By signing an IPC, the IPM is assured of no disruption of benefits entitlementeven for premium paym ents made du ring or within 60 days after theconfineme nt of a mem ber or qualified dependen t. This supersedes thespecific prohibition of availme nt stated in PhilHealth C ircular No. 25, s. of2010 on the applicability of current premium contribution;
In case of death of the m em ber, the dependen ts may con tinue to avail ofNH IP benefits for the period already paid in advance;The IPC sh all be issued only once in a given validity period. The IPM shallpresent the PhilHealth Official Receipt (PO R) or P hilHealth Agent's Receipt(PAR ) as proof of eligibility to avail of benefits;Depen clenls not yet reflected in the IPC may b e included upon renew al of thecontract. The IPM shall request for an up dated MD R to validate relationshipw ith a dependent in case benefit availment is necessary within a validityDeriod.
IV. COMPLIANCE1.All PhilHealth LH IOs shall ensure effic ient implem entat ion of IPC issuance
processes at the frontlines and properly inform the m embers on the value of the IPC;
2.All accredited collecting agents shall inform m em bers paying in their differentbranches to present their PhilHealth Agent's Receipt (PAR) at the nearest PhilHealthOffice to be able to secure copies of their respective IPC;
3.IPC renewal and p aym ent of appl icable fees shall be don e at the Local H eal thInsurance Offices where the contract shall be issued;
4.Pre-termination of con tract may be allowed for mem bers shifting to a different NHIPmembership type. There shall be no refund of excess premiums. Premiumpaymen ts already remitted in advance shall be adjusted accordingly to cover futureDavments subject to existing policies on advance payments;
~5A~TER~fiA A. p'.MAQIt' j
-!=Tli-i;,0 ThUii COPY j
TERFSAA.p'.MAOlV
;ERTlFiH
-
7/28/2019 Philhealth circ61_2012
7/7
5.An IPM may issue a Special Power ot Attorney ^raj iu anuw cmumci ^iouh iu j,a..his/her IPC. The SPA must be attached to the IPC to verify the authority of theperson signing the contract;
6.Retroactive paym ents shall be accepted only at PhilHealth LH IOs. Paym ents madein accredited collecting agenis shall be applied prospectively.
7.The P hilHealth Official Rec eipt (PO R) shall reflect paym ent/s made for interestcharge/s and applicable period paid for;
8.Local Health Insurance Offices shall require the updated m obile phone num ber andelectronic mail address of IPMs for electronic notification and billing in case of
default in payment;nidm ch=n ho hnnnri tr. fullv r.nmnlv with the terms of the contract.
V. COND UCT O F INFORM ATION A ND tUUUAUU N oivirMi