Peritonitis in Pd Patients
-
Upload
daniel-situngkir -
Category
Documents
-
view
216 -
download
0
Transcript of Peritonitis in Pd Patients
-
8/12/2019 Peritonitis in Pd Patients
1/64
-
8/12/2019 Peritonitis in Pd Patients
2/64
Overview
Peritoneal Dialysis - principles
Anatomy
Physiology
Pathology
Presentations
Management
Key points
www.health.com/
http://www.health.com/http://www.health.com/ -
8/12/2019 Peritonitis in Pd Patients
3/64
Chronic
Kidney
Disease
Diagnosis
End Stage
Kidney
Disease
Diagnosis
DIALYSIS
HAEMODIALYSIS
PERITONEAL DIALYSIS
TRANSPLANTATION
PALLIATIVE CARESTAGE 1 & 2
Proteinuria plus
eGFR 60+
(to determine eGFR
over 60, hand
calculate GFR using
Cockcroft-Gault
formula)
STAGE 3
eGFR 30-59
ml/min
MODERATE
KIDNEY
DAMAGE
Proteinuria
Care plan
STAGE 5
eGFR
-
8/12/2019 Peritonitis in Pd Patients
4/64
Peritoneal Dialysis
A form of renal replacement therapy forpatients with end stage kidney disease
Endeavours to replace some of the functions
of the kidney such as Removing waste products
Removing excess fluid
Correcting acid/base imbalances
Correcting electrolyte imbalances
High maintenance form of therapy requiringmeticulous compliance and effort on part ofpatient
www.agingdiscodiva.com
http://www.agingdiscodiva.com/http://www.agingdiscodiva.com/ -
8/12/2019 Peritonitis in Pd Patients
5/64
IDEAL BODY WEIGHT
IBW
Normotensive (Good BP) 120/70
No signs and symptoms of overload or
dehydration
Set by:
Home Training Staff Royal Perth Hospital
Renal Doctor
Dialysis Staff KSDC
-
8/12/2019 Peritonitis in Pd Patients
6/64
FLUID ASSESSMENT
Blood pressure
Weight
Chest, SaO2, SOB
OedemaAnkles
Back
Facial
JVP Skin tugor
Symptoms
Nausea,vomiting
Diarrhoea
Dizziness
-
8/12/2019 Peritonitis in Pd Patients
7/64
FLUID RESTRICTION
800 1000 mls per day
Weigh patient (will be required daily
SAME SCALES and document
which ones)
In hospital, remove jug
-
8/12/2019 Peritonitis in Pd Patients
8/64
-
8/12/2019 Peritonitis in Pd Patients
9/64
-
8/12/2019 Peritonitis in Pd Patients
10/64
-
8/12/2019 Peritonitis in Pd Patients
11/64
Peritoneal Dialysis
Involves the passage of solutes and water
across a membrane that separates two fluid
containing compartments-blood and dialysate
During dialysis 3 transport processes occursimultaneously
Diffusion
Ultrafiltration
Absorption
http://www.dialyse-45.net/int/info/techniques.htm
-
8/12/2019 Peritonitis in Pd Patients
12/64
Peritoneal Dialysis
2 types
CAPDcontinuous ambulatory peritoneal
dialysis Involves on average 4 dwells per day of 4-8
hours of 22.5L each
APDautomated peritoneal dialysis
Involves 3-10 exchanges overnight of varyingamounts
Usually but not always a daytime dwell
-
8/12/2019 Peritonitis in Pd Patients
13/64
Peritoneal Dialysis
Anatomy
Serosal membrane lining the gut
Thought to be the same as the body surface
areausually 1-2 m2
in adult 2 partsvisceral peritoneum lining the organs
(80% or the peritoneal surface area and theparietal peritoneum lining the walls of theabdominal cavity)
Peritoneal blood flow cant be measured butindirectly estimated to be between 50-100mls/min
-
8/12/2019 Peritonitis in Pd Patients
14/64
Peritoneal Dialysis
-
8/12/2019 Peritonitis in Pd Patients
15/64
Horizontal disposition of the peritoneum in the lower part of the abdomen.
www.theodora.com/anatomy/the_abdomen.html
http://www.theodora.com/anatomy/the_abdomen.htmlhttp://www.theodora.com/anatomy/the_abdomen.html -
8/12/2019 Peritonitis in Pd Patients
16/64
Peritoneal Dialysis
Visceral peritoneum blood supply is from the
superior mesenteric with venous drainage
from the portal system
Parietal peritoneum blood supply is from thelumbar, intercostal and epigastric arteries
while the venous drainage is via the IVC
Main lymphatic drainage is via stomata in the
diaphragmatic peritoneum which drain into
the right lymphatic duct
-
8/12/2019 Peritonitis in Pd Patients
17/64
Three pore model
Peritoneal capillary is the critical barrier toperitoneal transport
Movement of solute and water movement
across the capillary is mediated by pores ofthree different sizes
Large pores 20-40 nmprotein transport
Small pores 4-6nmsmall solutes eg urea,
creatinine, sodium, potassium, water Ultrapores (aquaporins)
-
8/12/2019 Peritonitis in Pd Patients
18/64
Three pore model of peritoneal
transport
Kidney International
ISSN: 0085-2538EISSN: 1523-1755
2009 International Society of Nephrology
http://www.isn-online.org/http://www.isn-online.org/ -
8/12/2019 Peritonitis in Pd Patients
19/64
Peritoneal Transport - Diffusion
Diffusionuraemic solutes and potassiumdiffuse from peritoneal capillary blood into thedialysate. Glucose, lactate, bicarbonate andcalcium diffuse in the opposite direction.
Diffusion depends on concentration gradient(maximal at the start), effective peritonealsurface area, intrinsic peritoneal membraneresistance, molecular weight of the solute (egsmall molecules like urea, diffuse morerapidly than larger molecules such ascreatinine)
-
8/12/2019 Peritonitis in Pd Patients
20/64
Diffusion
www.indiana.edu/.../lecture/lecnotes/diff.html
http://www.indiana.edu/.../lecture/lecnotes/diff.htmlhttp://www.indiana.edu/.../lecture/lecnotes/diff.html -
8/12/2019 Peritonitis in Pd Patients
21/64
Peritoneal Transport - Ultrafiltration
Occurs as a consequence of the osmotic gradient between thehypertonic dialysate and the relatively hypotonic peritonealcapillary blood
Driven by high concentration of glucose in dialysate
Depends on;
concentration gradient of the osmotic agent (glucose) peritoneal surface area
hydraulic conductance of the peritoneal membrane
reflection coefficient for the osmotic agent (how effectivelythe osmotic agent diffuses out of the dialysate into theperitoneal capillaries (0-1 is normalthe lower the value the
faster the osmotic gradient is lost. Gluc is 0.3 as opposed toicodextrin which is close to 1)).
Hydrostatic pressure gradientcap press around 20mmversus intraperitoneal pressure around 7mm Hg whichfavours ultrafiltration
-
8/12/2019 Peritonitis in Pd Patients
22/64
Ultrafiltration
http://www.dialysistips.com/principles.html
-
8/12/2019 Peritonitis in Pd Patients
23/64
Peritoneal TransportUltrafiltration 2
Depends on; Oncotic pressure gradient which acts to keep fluid in
blood, opposing ultrafiltration (low inhypoalbuminaemic patients so ultrafiltration tends tobe high)
Sievingoccurs when solute moves along with wateracross a semipermeable membrane by convection butsome of the solute is held backsieved. The soluteconcentration in the ultrafiltrate that has passed
through the membrane is lower than the sourcesolution. Different solutes sieve differently rangingfrom 0 (complete sieving) to 1 (no sieving)
Other osmotic agents such as icodextrin with a largereflection coefficient so ultrafiltration is sustained
-
8/12/2019 Peritonitis in Pd Patients
24/64
Ultrafiltration
http://www.advancedrenaleducation.com/PeritonealDialysis/Ultrafiltration/HowtoAchieveAdequatePDUF/tabid/229/Default.aspx
-
8/12/2019 Peritonitis in Pd Patients
25/64
Peritoneal TransportFluid
Absorption
Occurs via the lymphatics at constant rate
Typical values for peritoneal fluid absorption
are 1-2 mls/minute
Affected by intraperitoneal hydrostaticpressure
Effectiveness of lymphatics
http://www.fmc-ag.com/gb_2006/en/05/glossar.html
-
8/12/2019 Peritonitis in Pd Patients
26/64
Peritonitis
Peritoneal Dialysis is a great form of renal
replacement therapy
Peritonitis is a significant complication
Incidence peritonitis episodes varies from 1/9patient-months to 1/53 patient-months
(Grunberg 2005; Kawaguchi 1999)
Our figures pending but are likely to be on
the lower end of the scale
http://mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD005284/bibliography.htmlhttp://mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD005284/bibliography.htmlhttp://mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD005284/bibliography.htmlhttp://mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD005284/bibliography.html -
8/12/2019 Peritonitis in Pd Patients
27/64
Peritonitis in PD pts
Risk Factors
Diabetes
Non caucasian
Obesity Temperate climate
Depression
Possibly the peritoneal dialysis
modality but not proven(Huang 2001; Oo 2005).
http://www.diabetesandrelatedhealthissues
.com/
http://mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD005284/bibliography.htmlhttp://mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD005284/bibliography.htmlhttp://mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD005284/bibliography.htmlhttp://mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD005284/bibliography.html -
8/12/2019 Peritonitis in Pd Patients
28/64
Peritonitis in PD pts
Significant morbidity
Some mortality - It is estimated that PD-
associated peritonitis results in death in 6%
of affected patients (Troidle 2006).
gymsoap.com
http://mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD005284/bibliography.htmlhttp://mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD005284/bibliography.html -
8/12/2019 Peritonitis in Pd Patients
29/64
Peritonitis in PD pts
Catheter removal may become necessary ifpt is not responding to antibiotics or ifinfection is fungal. May be temporary orpermanent
Ultrafiltration failure can occur both acutelydue to increases in capillary permeability(Ates 2000; Smit 2004) and in the longerterm resulting in technique failure (Coles2000; Davies 1996).
http://mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD005284/bibliography.htmlhttp://mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD005284/bibliography.htmlhttp://mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD005284/bibliography.htmlhttp://mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD005284/bibliography.htmlhttp://mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD005284/bibliography.htmlhttp://images.google.com.au/imgres?imgurl=http://www.walkeravenue.com/Health/Kidneys/images_kidneys/Patient_on_peritoneal_Dialysis..png&imgrefurl=http://www.walkeravenue.com/Health/Kidneys/preesrd_education.htm&usg=__pzDOUt8Ria3NEyTSXmUuPHDpAys=&h=270&w=240&sz=16&hl=en&start=2&um=1&tbnid=j2paqOfYjG2_dM:&tbnh=113&tbnw=100&prev=/images%253Fq%253Dperitoneal%252Bdialysis%252Bcatheter%2526hl%253Den%2526sa%253DX%2526um%253D1http://mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD005284/bibliography.htmlhttp://mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD005284/bibliography.htmlhttp://mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD005284/bibliography.htmlhttp://mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD005284/bibliography.htmlhttp://mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD005284/bibliography.html -
8/12/2019 Peritonitis in Pd Patients
30/64
Pathogenesis
1. Potential routes of infection
Intraluminalimproper technique; access tobacteria via the catheter lumen
Periluminalbacteria present on skin surfaceenter the peritoneal cavity via the cathetertract
Transmuralbacteria of intestinal originmigrate through the bowel wall
Haematogenousperitoneum seeded via theblood stream
Transvaginal - ??
http://images.google.com.au/imgres?imgurl=http://www.medionics.com/cather01.jpg&imgrefurl=http://www.medionics.com/catheter.htm&usg=__Ae0nif5kpqg2YbaKTBdYZYjlmOE=&h=480&w=400&sz=29&hl=en&start=5&um=1&tbnid=_nJt38SkW3INeM:&tbnh=129&tbnw=108&prev=/images%253Fq%253Dperitoneal%252Bdialysis%252Bcatheter%2526hl%253Den%2526sa%253DX%2526um%253D1 -
8/12/2019 Peritonitis in Pd Patients
31/64
Pathogenesis
2. Bacteria laden plaquethe intraperitoneal portionof the catheter is covered with a bacteria ladenplaque - ? Role in pathogenesis of peritonitis
3. Host defencesperitoneal leucocytes critical in
combating bacteria that have entered theperitoneum. Affected by
A. dialysis solution and phhypertonic solutioninhibits activity
B. Calcium levelslow calcium in dialysate inhibits
activity Peritoneal IgG levelslow levels inhibit activity
HIVlittle known effect
-
8/12/2019 Peritonitis in Pd Patients
32/64
Aetiology
Staph aureus
Coag neg staph (S.Epidermidis)
E coli
Pseudomonas
Sternotropomonas
Candida
Atypical TB
http://images.google.com.au/imgres?imgurl=http://asymptotia.com/wp-images/2008/08/e_coli.jpg&imgrefurl=http://asymptotia.com/category/science/biology/&usg=__RRTS6QDOvMvQ6Bid0HmnJTI7I88=&h=599&w=600&sz=67&hl=en&start=3&um=1&tbnid=dIOpq8M9nmCBdM:&tbnh=135&tbnw=135&prev=/images%253Fq%253De%252Bcoli%2526hl%253Den%2526um%253D1http://swampie.files.wordpress.com/2008/02/staphylococcus-aureus.jpg -
8/12/2019 Peritonitis in Pd Patients
33/64
Diagnosis
2 of the following 3 conditions
Symptoms and signs of peritoneal
inflammation (pain, tenderness, guarding,
rebound) Cloudy peritoneal fluid with increased white
cell count (specifically neutrophils)
Demonstration of bacteria on gram stain or
culture
-
8/12/2019 Peritonitis in Pd Patients
34/64
Diagnosissymptoms and signs
Abdo pain most common but in a PD pt
suspect peritonitis if general malaise,
nausea, vomiting or diarrhoea
Dont be blinded by the PD These pts get other pathology
EG. Strangulated hernia, withdrawal from
steroids (if they stop taking meds suddenly
and they happen to be on steroids), rupturedviscus, ulcers, perforations etc
EXAMINE THE PATIENT
http://images.google.com.au/imgres?imgurl=http://www.pain-free.eu/userdata/Image/pain_free/Abdominal%252520pain_3811288.jpg&imgrefurl=http://www.pain-free.eu/Abdominal%252520Pain&usg=__p1msd23yoqHs-4Tb3I-IWj4jLP0=&h=512&w=384&sz=118&hl=en&start=2&um=1&tbnid=Bt9s55cQzugywM:&tbnh=131&tbnw=98&prev=/images%253Fq%253Dabdo%252Bpain%2526hl%253Den%2526um%253D1 -
8/12/2019 Peritonitis in Pd Patients
35/64
Diagnosissymptoms and signs
PercentageSymptoms
Abdo pain 95
Nausea and vomiting 30
Fever 30
Chills 20
Constipation or diarrhoea 15
Signs
Cloudy peritoneal fluid 99
Abdo tenderness 80
Rebound tenderness 10-50Increased temperature 33
Blood leucocytosis 25
CRP 100 but can be delayed
Daugirdas JT et al 2007 p 419
-
8/12/2019 Peritonitis in Pd Patients
36/64
-
8/12/2019 Peritonitis in Pd Patients
37/64
Peritoneal fluid culture
Send the whole bag
Label it (preferable with textalabel can sweat off)
Let the lab know it is coming
Ask for urgent gram stain and cell count and ask this
to be telephoned to you. Be aware that the gramstain may be negative in 50% of cases of subsequentculture proven peritonitis
Also ask for M/C/S and fungal cultures
Follow up the culture Do a full septic workup each timeincluding blood
cultures
http://images.google.com.au/imgres?imgurl=http://www.diabetesmonitor.com/images/dialys.gif&imgrefurl=http://www.diabetesmonitor.com/b120.htm&usg=__H_l97wjRow--D2Rm8Ait6oCqJXM=&h=274&w=252&sz=12&hl=en&start=65&um=1&tbnid=0bp7SVgbuiBJyM:&tbnh=113&tbnw=104&prev=/images%253Fq%253Dperitoneal%252Bdialysis%252Bbag%2526ndsp%253D18%2526hl%253Den%2526sa%253DN%2526start%253D54%2526um%253D1 -
8/12/2019 Peritonitis in Pd Patients
38/64
Peritonitis
Common things occur commonly and
peritonitis is unfortunately common in our
population of PD patients
BUT Dont lose sight of the bigger picture and
these patients can suffer from any other
pathologyalways keep an open mind
http://www.youthwithanopenmind.com/images/openmind_print_logo.gif -
8/12/2019 Peritonitis in Pd Patients
39/64
Peritonitis Management
Broad spectrum coverage
Vancomycin (2.5g if more than 60kg / 2 g if 60kg orless)
Gentamicin (200mg if more than 60kg / 140mg if 60kg
or less) IP is better than IV (confirmed on large Cochrane
review April 2009)
Await culture. If gram positive, then repeat the vancdose in 1 week. If gram negative then usually
ceftriaxone 1g intraperitoneally daily for 14 days Things to note; if pseudomonas tube is very often lost.
May need to consider adding a second antibiotic suchas daily ciprofloxacin
PERITONITIS MANAGEMENT
-
8/12/2019 Peritonitis in Pd Patients
40/64
Initial symptoms may include;
diarrhoea, vomiting, nausea,
abdominal pain, mental confusion or feeling unwell
COLLECT DRAINED BAG
*Seeadditional resources (pink section) for drainage instructions* Send entirebag for urgent MC&S (including WCC differential) and Fungal elements. ****
Must cc KRSS ****
Intraperitoneal (IP) Antibiotics (see Procedures)Give BOTH
Gentamycin 160mgs if 60kgs or less
(gramve organisms) 200mg if > 60kgs
AND
Vancomycin - 2gms if 60kgs or less
(gram +ve organisms) 2.5grams if > 60kgs
Give both in a 2L 2.3%bag
Dwell in the abdomen for minimum 6 hours(Consult microbiologist if Vanc or Gent allergy)
must be able to read newspaper print through the
bag
LOOK FOR OTHER CAUSES
Call PD Coordinator or
Renal GP
ATTENTION:Vanc and Gent provide some coverage while
awaiting sensitivities.****Further antibiotics WILL be required ****
If Staph/gram +ve, give IP Vancomicin again on Day 7
If gram negative, refer to sensitivities, but
usually 14 days of IP Ceftriaxone1gmYOU MUSTfollow up the MC & S 48 hours after initial IP treatment.
A WCC > 100 confirms peritonitis.If the patient is not improving within 24 hrs, or any other concerns, contact PD coordinator
CLEAR BAG CLOUDY BAG
-
8/12/2019 Peritonitis in Pd Patients
41/64
Peritonitis Mx
CAPD/APD
Drain abdomen and send bag off with path
request as above
Change the transfer set completely followingusual aseptic techniques
Load 2.3% 2 litre dialysate bag (use 1.5% bag
if patient hypotensive) with Vancomycin and
Gentamicin as per above guideline Infuse bag into peritoneum
6 hour dwell
-
8/12/2019 Peritonitis in Pd Patients
42/64
Peritonitisfungal infection
If fungal organisms are seen on gram stain,
or cultured, it is unlikely you will be able to
save the tube
Once the tube is colonized, the only cure isremoval of tube, peritoneal rest (pt on
Haemodialysis for a few months) and then
start from scratch
-
8/12/2019 Peritonitis in Pd Patients
43/64
Peritonitis
If you think that the patient has peritonitis but youthink they have life threatening sepsis eghypotension, tachycardia, fever (or no fever as maynot be able to mount an immune response), alteredconscious state etc, your patient is likely to require IV
broad spectrum antibiotics. Ring the microbiologiston call. Dont wait to get IP regime in. That can go inwhile you are making calls and obtaining results.
Antibiotics must be given within 1 hour ofpresentationit is an emergency.
I usually ring SCGH as they maintain a 24 hourconsultant micro roster 93463333 but remember allour patients who require transfer must go to RoyalPerth Hospital as they are under the RPH consultant
-
8/12/2019 Peritonitis in Pd Patients
44/64
Peritonitis
Patients can have dual pathology
Eg it is not uncommon for patients to have
peritonitis, delay treatment, splint their
abdomen and get pneumonia. This needs tobe treated as per the normal guidelines for
pneumonia
http://images.google.com.au/imgres?imgurl=http://www.med-ed.virginia.edu/courses/rad/cxr/web%252520images/rul-pneumonia-pa.jpg&imgrefurl=http://www.med-ed.virginia.edu/courses/rad/cxr/pathology3chest.html&usg=__BmCnP3nxpkWKlbnd5ognWKNQVQg=&h=450&w=400&sz=19&hl=en&start=2&um=1&tbnid=VQ6GGqACl7HlpM:&tbnh=127&tbnw=113&prev=/images%253Fq%253Dpneumonia%2526hl%253Den%2526um%253D1 -
8/12/2019 Peritonitis in Pd Patients
45/64
Peritonitis
Additives to bags
Vancomycin, aminoglycosides andcephalosporins are safe to mix in the samebag
Aminoglycosides are incompatible withpenicillins
Vancomycin is stable for 28 days in dialysate(normal room temp)
Cefazolin is stable for 8 days
Gentamicin is stable for 14 days
Heparin added decreases duration of stability
-
8/12/2019 Peritonitis in Pd Patients
46/64
Peritonitis
Often get formation of fibrin clots which
increases risk of catheter block
May need to add 500units of heparin to 1 or 2
bags a day until fibrin clots decrease Constipation is commonyou may need to
stop the calcium based phosphate binders
temporarily but better off using aperients
early and preventing the need to alter routinemeds
http://images.google.com.au/imgres?imgurl=http://tell.fll.purdue.edu/JapanProj/FLClipart/Medical/constipation.gif&imgrefurl=http://tell.fll.purdue.edu/JapanProj/FLClipart/Medical.html&usg=__AvCBbR8wMo-cqxSEMPJ5YJZCHTA=&h=1355&w=1782&sz=35&hl=en&start=6&um=1&tbnid=BFROXmxKGYw-zM:&tbnh=114&tbnw=150&prev=/images%253Fq%253Dconstipation%2526hl%253Den%2526um%253D1 -
8/12/2019 Peritonitis in Pd Patients
47/64
Peritonitis
Fluid regimes
Depends whether patient is overloaded orunderloaded
Can usually continue normal regime but tailor to
patient If BP low, use 1.5% bags x 4 a day
If BP high use 2.3% bags, minimum of 4 a day
Aim for BP 120/
APD pts can continue on APD or if needed canconvert temporarily to CAPDin Broome withresources this should not be necessary
-
8/12/2019 Peritonitis in Pd Patients
48/64
Peritonitis
Can get changes in the permeability of the peritoneal
membrane
Permeability to water, glucose and proteins is
increased
Rapid glucose absorption from the dialysis solutionreduces amount of ultrafiltration and can result in fluid
overload
May need high glucose concentration dialysate with
shorter dwells Hyperglycaemia is common
Protein loss is increased in peritonitis so patients will
need high protein supplements
-
8/12/2019 Peritonitis in Pd Patients
49/64
Peritonitis
Dont forget secondary causes of peritonitis
Perforated gastric or duodenal ulcer
Pancreatitis
Appendicitis Diverticulitis
PID
Talk to the surgeon if you are not sure
-
8/12/2019 Peritonitis in Pd Patients
50/64
Peritonitis
You dont necessarily have to admit the
patient
Admission dictated by symptoms and distress
and often social circumstances up here
blogs.southshorenow.ca/louise/cms.ich.ucl.ac.uk/website/imagebank/images
http://blogs.southshorenow.ca/louise/http://cms.ich.ucl.ac.uk/website/imagebank/imageshttp://cms.ich.ucl.ac.uk/website/imagebank/imageshttp://blogs.southshorenow.ca/louise/ -
8/12/2019 Peritonitis in Pd Patients
51/64
Peritonitis - bugs
StaphVancomycin and repeat in 1 week
Patients should have nasal carriage treated withmupirocin bd for 5 days and then once a week of bdfor 5 days once a month
Gram NegsIP Ceftriaxone for 2 weeks andconsider repeating the dose of gentamicin after aweek or adding oral ciprofloxacin to the regime
Pseudomonas difficult to treat
Sternotrophomonasusually requires 2 antibiotics
and usually for 4 weeks Campylobacter not that commonresponds to
gentamicin
-
8/12/2019 Peritonitis in Pd Patients
52/64
-
8/12/2019 Peritonitis in Pd Patients
53/64
Peritonitis
Culture negative disease
If cell count less than 50 x 106unlikely toperitonitis
If higher white cell count, then repeat empirictherapy
Make sure lab is doing cultures for AFBs andfungus
If not improving consider legionella,
campylobacter, ureaplama, mycoplasma,enteroviruses, fungus, histoplasmacapsulatum
-
8/12/2019 Peritonitis in Pd Patients
54/64
Peritonitis
Fungal peritonitis
Predisposing factors
Prior antibiotic use especially if not full treatment
Immunosuppressive therapy HIV
Malnutrition
Low albumin
Diabetes
-
8/12/2019 Peritonitis in Pd Patients
55/64
Peritonitis
Fungal peritonitis
We tend to try and save the tube by giving
antifungals but guidelines recommend prompt
removal of catheter, conversion tohaemodialysis for a few weeks and then start
from scratch
Penetration of antifungals to peritoneum other
than with IP administration, is poor
http://images.google.com.au/imgres?imgurl=http://www.kaiscience.com/thumbimage.php%253Fid%253D79&imgrefurl=http://www.kaiscience.com/ph_79-Soil_fungus_condiophore_and_conidia_Trichoderma_sp._Copyright_Dennis_Kunkel_Microscopy&usg=__e64sTlCXU05-V6zgOTb1b3hMiDQ=&h=353&w=300&sz=25&hl=en&start=2&um=1&tbnid=i5lgwUzM0td0QM:&tbnh=121&tbnw=103&prev=/images%253Fq%253Dfungus%252Bmicroscopy%2526hl%253Den%2526um%253D1 -
8/12/2019 Peritonitis in Pd Patients
56/64
Peritonitis
Refractory disease
Defined as disease that is treated with
appropriate antibiotics for 5 days without
improvement Catheter removal necessary to reduce
morbidity and preserve peritoneum
Increased with gram neg bugs
-
8/12/2019 Peritonitis in Pd Patients
57/64
Peritonitis
Relapsing disease
Peritonitis with the same organism within 4 weeks of stoppingtherapy
Usually Staph epidermidis or a gram negative organism
If pseudomonas or gram negatives, remove the catheter
If staph, may be able to rescue with repeat vancomycin weeklyfor a month or may be able to remove the tube andsimultaneously insert a new tube (as opposed to any otherorganism where a 2 month peritoneal rest is required)
Sometimes can use urokinase to strip the biofilm (bacteria
entrapped in fibrin in the peritoneal membrane) in relapsingdiseaselast resort but worth a go
-
8/12/2019 Peritonitis in Pd Patients
58/64
Peritonitis
20% of episodes temporally associated with
exit site and tunnel infections (Piraino et al
2005)
Treat exit site infections if red and purulent Swab it
Start Flucloxacillin empirically and change or
add ciprofloxacin if gram neg
Exit sites are another whole topic
http://images.google.com.au/imgres?imgurl=http://userweb.port.ac.uk/~norrismj/antimicrobial_agents/images/flucloxacillin.jpg&imgrefurl=http://userweb.port.ac.uk/~norrismj/antimicrobial_agents/Penicillins.html&usg=__NEub6FBelfkHq1UjbvLBqOviCfc=&h=192&w=256&sz=8&hl=en&start=6&um=1&tbnid=2slNyhkigq4NjM:&tbnh=83&tbnw=111&prev=/images%253Fq%253Dflucloxacillin%2526hl%253Den%2526um%253D1 -
8/12/2019 Peritonitis in Pd Patients
59/64
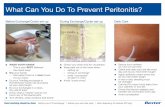
Peritonitis
Prevention
Good technique
Hygiene
Mupirocin Exit site care
Anchor tape
http://images.google.com.au/imgres?imgurl=http://www.homedialysis.org/images/resources/tom/presternal2.jpg&imgrefurl=http://www.homedialysis.org/resources/tom/200507/&usg=__d63G_ug_2drZP4ljNbQ4eVUxMKM=&h=329&w=219&sz=17&hl=en&start=2&um=1&tbnid=uaKvWtG2nO5aoM:&tbnh=119&tbnw=79&prev=/images%253Fq%253Dsite:www.homedialysis.org%252Banchor%252Btape%252Bin%252Bperitoneal%252Bdialysis%2526hl%253Den%2526um%253D1 -
8/12/2019 Peritonitis in Pd Patients
60/64
Cochrane Review 2009
Implications for practiceAt the present time broad spectrum antibiotics should be initiated at thetime a diagnosis of peritonitis is made. When choosing antibiotics theside-effect profile, local drug resistance patterns and previous antibioticuse and infection history in the individual concerned should beconsidered. In cases of recurrent peritonitis dialysis catheters shouldbe removed rather than using intraperitoneal urokinase.
Currently available evidence from RCTs is inadequate in many areas
of clinical practice important in the management of PD-associatedperitonitis. This is a limiting factor in the provision of definitivetreatment guidelines.
-
8/12/2019 Peritonitis in Pd Patients
61/64
Cochrane Review 2009
Implications for researchFurther studies are required to establish the most effective treatment for peritoneal dialysis-associated peritonitis. An essential feature of such studies is inclusion of enough patients toensure adequate power to assess meaningful long and short term outcomes. Short termoutcomes should extend beyond whether cure is achieved without catheter removal, forexample duration of systemic inflammation. Study of long-term outcomes should includepermanent transfer to haemodialysis, development of ultrafiltration failure patient death andlate recurrent episodes of peritonitis beyond four weeks from the original episode.
Specific interventions that would be of value include early versus late catheter removal.Studies designed to study infections due to specific organisms would also be valuable. Anexample is a study of glycopeptide versus cephalosporin therapy in peritonitis due tocoagulase negative Staphylococcal species. The majority of studies have included patientson CAPD rather than APD hence studies designed to test the efficacy of antibiotics in APDare required. This is particularly applicable to studies of intermittent versus continuousdosing when cycler dwell times may well influence pharmacokinetics.Future research should be conducted using standard definitions, with inclusion ofinformation about factors that may influence the response to therapy such as prophylaxis
regimens and dialysis solutions used. Current ISPD guidelines provide a comprehensive listof requirements for future studies that should be referred to when designing studies.
-
8/12/2019 Peritonitis in Pd Patients
62/64
Take home points
Have a high index of suspicion
Use the remote area manual
Always let KRSS know of episode
Copy all results to KRSS
Dont hesitate to ask if you are not sure KRSS team, KRSS GP, Renal GP,
Nephrologist
www.learningradiology.com
-
8/12/2019 Peritonitis in Pd Patients
63/64
-
8/12/2019 Peritonitis in Pd Patients
64/64
Thank you
Questions