Pentavalent Antimonials Combined with Other Therapeutic...
Transcript of Pentavalent Antimonials Combined with Other Therapeutic...

Review ArticlePentavalent Antimonials Combined with OtherTherapeutic Alternatives for the Treatment of Cutaneous andMucocutaneous Leishmaniasis: A Systematic Review
Taisa Rocha Navasconi Berbert,1 Tatiane França Perles de Mello,2
Priscila Wolf Nassif,1 Camila Alves Mota,1 Aline Verzignassi Silveira,3
Giovana Chiqueto Duarte,4 Izabel Galhardo Demarchi ,5
SandraMara Alessi Aristides,5 Maria Valdrinez Campana Lonardoni ,5
Jorge Juarez Vieira Teixeira,5 and Tha-s Gomes Verziganassi Silveira 5
1Graduate Program in Health Sciences, State University Maringa, Avenida Colombo, 5790 Jardim Universitario, 87020-900,Maringa, PR, Brazil
2Graduate Program in Bioscience and Physiopathology, State University Maringa, Avenida Colombo, 5790 Jardim Universitario,87020-900Maringa, PR, Brazil
3Medical Residency, Santa Casa de Sao Paulo, R. Dr. Cesario Mota Junior, 112 Vila Buarque,01221-900 Sao Paulo, SP, Brazil
4Undergraduation Course in Medicine, State University Maringa, Avenida Colombo, 5790 Jardim Universitario,87020-900Maringa, PR, Brazil
5Department of Clinical Analysis and Biomedicine, State University Maringa, Avenida Colombo, 5790 Jardim Universitario,87020-900Maringa, PR, Brazil
Correspondence should be addressed toThaıs Gomes Verziganassi Silveira; [email protected]
Received 31 August 2018; Revised 19 November 2018; Accepted 5 December 2018; Published 24 December 2018
Academic Editor: Markus Stucker
Copyright © 2018 Taisa Rocha Navasconi Berbert et al. This is an open access article distributed under the Creative CommonsAttribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work isproperly cited.
The first choice drugs for the treatment of cutaneous and mucocutaneous leishmaniasis are pentavalent antimonials, sodiumstibogluconate, or meglumine antimoniate.However, the treatment with these drugs is expensive, can cause serious adverse effects,and is not always effective. The combination of two drugs by different routes or the combination of an alternative therapy withsystemic therapy can increase the efficacy and decrease the collateral effects caused by the reference drugs. In this systematic reviewwe investigated publications that described a combination of nonconventional treatment for cutaneous and mucocutaneous withpentavalent antimonials. A literature review was performed in the databases Web of Knowledge and PubMed in the period from01st of December 2004 to 01st of June 2017, according to Prisma statement.Only clinical trials involving the treatment for cutaneousor mucocutaneous leishmaniasis, in English, and with available abstract were added. Other types of publications, such as reviews,case reports, comments to the editor, letters, interviews, guidelines, and errata, were excluded. Sixteen articles were selected andthe pentavalent antimonials were administered in combination with pentoxifylline, granulocyte macrophage colony-stimulatingfactor, imiquimod, intralesional sodium stibogluconate, ketoconazole, silver-containing polyester dressing, lyophilized LEISH-F1protein, cryotherapy, topical honey, and omeprazole. In general, the combined therapy resulted in high rates of clinical cure andwhen relapse or recurrence was reported, it was higher in the groups treated with pentavalent antimonials alone. The majorityof the articles included in this review showed that cure rate ranged from 70 to 100% in patients treated with the combinations.Serious adverse effects were not observed in patients treated with drugs combination.The combination of other drugs or treatmentmodalities with pentavalent antimonials has proved to be effective for cutaneous and mucocutaneous leishmaniasis and for mostseemed to be safe. However, new randomized, controlled, and multicentric clinical trials with more robust samples should beperformed, especially the combination with immunomodulators.
HindawiDermatology Research and PracticeVolume 2018, Article ID 9014726, 21 pageshttps://doi.org/10.1155/2018/9014726

2 Dermatology Research and Practice
1. Introduction
Leishmaniasis is an important zoonosis around the world,being reported that about 20,000 to 30,000 deaths occurannually as a consequence of the disease [1]. The mostfrequent form is cutaneous leishmaniasis (CL), which ispresent in several countries, mainly in the Americas, theMediterranean basin, the Middle East, and Central Asia. Anannual occurrence of 0.6 to 1.0 million new cases is estimated[2] and around 399 million of people are at risk of infectionin 11 high-burden countries [1].
The pentavalent antimonials, sodium stibogluconate ormeglumine antimoniate, are drugs commonly used to treatcutaneous and mucocutaneous leishmaniasis. However, thetreatment with these drugs is expensive and can cause seriousadverse effects, such as cardiac toxicity and elevation inthe levels of hepatic enzymes [3–5], and, sometimes, it isineffective or presents low cure rates [6, 7]. AmphotericinB, pentamidine, fluconazole, and miltefosine can be used assecond choice drugs, but they also exhibit toxicity. Moreover,the efficacy of the treatment also depends on the Leishmaniaspecies involved in the infection, since some species are moreresistant to some drugs [6].
Local therapies, such as cryotherapy, CO2laser, ther-
motherapy, and photodynamic therapy, are alternatives toconventional drugs, since they are less toxic to the patientand the main adverse effects are restricted to the site ofapplication [8–13]. However, the exclusive use of local therapyis controversial, since some New World species can lead tomucosal leishmaniasis after primarily cutaneous lesions [3].
The combination of two drugs or the combination of alocal therapy with systemic therapy can be an alternative toincrease the efficacy of local therapy and may decrease thecollateral effects caused by the reference drugs. Some studieshave evaluated the efficacy of this type of combination [14–17], being necessary prospective and multicenter studies forsafer evidence. Our central question was evaluated if thecombination of an alternative therapy with meglumine anti-moniate presents more efficiency that only meglumine anti-moniate in the treatment of cutaneous and mucocutaneousleishmaniasis. In this sense, we investigated published articlesthat used the combination of an alternative therapy withpentavalent antimonials in the treatment of cutaneous andmucocutaneous leishmaniasis through systematic review.
2. Methodology
2.1. Literature Search. A literature review was performed inthe databases Web of Knowledge and PubMed, consideringthe period from 01st December 2004 to 01st June 2017according to Prisma statement [18].The screening of the titlesand abstracts was performed by researchers (TRNB, CAM,PWN, TFPM, GCD and AVS). The MeSH (Medical SubjectHeadings) terms, strategy used for the search on PubMed,were also selected by these researchers based on publicationson the topic at PubMed. Any disagreements were decided byconsensus. The MeSH terms were validated by two experts(JVT and TGVS) and were divided into two groups: Group1 “Antiprotozoal Agents” OR “Combined Modality Therapy”
OR “DrugTherapy, Combination” OR “Treatment Outcome”OR “Amphotericin B” OR “Meglumine” OR “ProtozoanVaccines” OR “Organometallic Compounds” OR “AntimonySodium Gluconate” OR “Antimony” OR “Pentamidine” OR“Anti-Infective Agents” OR “Medication Therapy Manage-ment” OR “Complementary Therapies”; AND Group 2“Leishmaniasis”OR “Leishmania”.The research in theWeb ofKnowledge database was carried out by topic, which ensuresgood sensitivity.
2.2. Inclusion, Exclusion Criteria, and Studies Selection. Arti-cles that describe a combination of therapeutic alternativeswith pentavalent antimonials for cutaneous or mucocuta-neous leishmaniasis were included in this review. Only origi-nal clinical trials, in English and with abstract available, wereadded. Other types of publications (reviews, case reports,comments to the editor, letters, interviews, guidelines, anderrata) were excluded. After the search the papers initiallyselected were analyzed by the researchers of group 1 (TRNB,CAM, PWN, TFPM, GCD, and AVS) and disagreementsabout inclusion or exclusion of articles were decided byconsensus. To increase the search sensitivity, the researchersin group 1 checked all references from the selected publica-tions to retrieve other unidentified publications in the otherphases of the search. The validation of selected articles wasperformed by four independent evaluators of group 2 (TGVS,MVCL, SMAA, and IGD).
2.3. Data Extraction. The structure of the topics to composethe tables was organized by researchers from group 1 with thesupport of two experts (TGVS and JVT): Table 1 (study, areacountry, study design, period of study, age range or mean inyears, gender, clinical forms, patients enrolled, leishmaniasisdiagnosis, and statistics); Table 2 (study, Leishmania species,treatment, patients at the end, percentage of clinically healedpatients or lesions, percentage of therapy failure, and percent-age of relapse or recurrence); Table 3 (treatment, side effectspercentage, and study source); and Table 4 (treatment, dose,route of administration, time efficacy, safety, practice/clinicalimplications, and study source).The tables were completed byresearchers in group 1 and then checked by researchers fromgroup 2.
3. Results
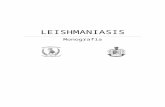
Based on the inclusion criteria defined by consensus, 16articles were selected, being from Iran (6), Peru (4), Brazil(4), Yemen (1), and Afghanistan (1) (see Figure 1). In all,1,302 patients aged between 1 and 87 years were involved inthe studies, with cutaneous or mucocutaneous leishmaniasis,being predominant the cutaneous form of the disease. Themost reported species of Leishmania were L. braziliensis, L.tropica, and L. major (Table 1).
In the selected articles, pentavalent antimonials were ad-ministered in combination with different drugs or treatmentmodalities, which were pentoxifylline; granulocyte macro-phage colony-stimulating factor; imiquimod; intralesionalsodium stibogluconate; ketoconazole; nonsilver-containing

Dermatology Research and Practice 3
Table1:Ba
selin
echaracteristicso
fclin
icaltrialsinclu
dedin
thea
nalysis
ofcombinatio
nsforthe
treatmento
ftegum
entary
leish
maniasis.
Stud
ysource
Area,
Cou
ntry
Stud
ydesign
Period
ofstud
yAge
rang
e,mean(years)
Gen
der
Clin
ical
form
Patie
nts
enrolle
dLe
ishm
aniasisd
iagn
osis
Statistic
s
Alm
eida
etal.,2005
Bahia,Brazil
Open-label
clinicaltrial
NR
14-25,18
Male6
0%Female4
0%Cu
taneou
s5
ClinicalandLabo
ratory
(skintest,
andiso
latio
nin
cultu
re)
No
Arevaloetal.,2007
Lima,Peru
Com
parativ
estudy;
Rand
omized
Con
trolledTrial
8/2005–10/2005
18-87,34.9
Male5
5%Female4
5%Cu
taneou
s20
ClinicalandLabo
ratory
(microscop
y,cultu
re,
and/or
PCR,
and
Mon
tenegroskin
test)
Yes
Brito
etal.,2017
Bahia,Brazil
Rand
omized
-con
trolledtrial
12/2010–
10/2013
18-62
Predom
inance
ofmale
Cutaneou
s162
Clinicalandlabo
ratoria
l(Leishmaniaskin
test,
and/or
histo
patholog
y,cultu
reandPC
R)
Yes
El-Sayed
&Anw
ar,
2010
Sanaa,Yemen
Com
parativ
estudy;
Rand
omized
Con
trolledTrial
6/2006
–6/200
712-50,23.5
Male5
3.3%
Female4
6.7%
Cutaneou
s30
ClinicalandLabo
ratory
(smearfor
amastig
otea
ndtissuec
ulture)
Yes
Farajza
fehetal.,2
015
Iran
Rand
omized
clinical
trial
2011-2012
2-60
,18.52
Male3
4Female3
6NR10
Cutaneou
s80
Labo
ratory
(smear
microscop
y)Yes
Firooz
etal.,2006
Razavi,Iran
Multic
enterS
tudy;
Rand
omized
Con
trolledTrial
8/2004
-/2005
12-60,27.0
Male4
4.5%
Female5
5.5%
Cutaneou
s119
Labo
ratory
(smearo
rcultu
re)
Yes
Khatamietal.,2013
Kashan,Iran
Rand
omized
Con
trolledClinical
Trial
9/200–
4/2010
12-60,28.8
Male4
7%Female5
3%Cu
taneou
s83
Labo
ratory
(smearo
rcultu
re)
Yes
Llanos
Cuentasetal.,
2010
Cusco,Peru
Rand
omized
Con
trolledTrial
8/2004
–6/2005
18-59
Male9
6%Female4
%Mucosal
48Labo
ratory
(microscop
y,PC
Ror
invitro
cultu
re)
Yes
Machado
etal.,2007
Bahia,Brazil
Rand
omized
Con
trolledTrial
NR
18-65
Male8
3%Female17%
Mucosal
23
Labo
ratory
(Intradermal
skin
test,
parasiteisolatio
nby
cultu
re,and
/or
histo
pathological)
Yes
Meymandi
etal.,2
011Ke
rman,Iran
Com
parativ
eStudy;
Rand
omized
Con
trolledTrial
11/2007-8/200
97-60
Male4
6.6%
Female5
3.4%
Cutaneou
s191
Labo
ratory
(smearo
rskin
biop
sy)
Yes
Mira
nda-Ve
raste
guiet
al.,2
005
Lima,Peru
Rand
omized
Con
trolledTrial
2/2001
–8/2002
1-78
Male5
7.5%
Female4
2.5%
Cutaneou
s40
Labo
ratory
(aspira
tion,
smear,biop
sy,culture,
and/or
PCR)
Yes

4 Dermatology Research and Practice
Table1:Con
tinued.
Stud
ysource
Area,
Cou
ntry
Stud
ydesign
Period
ofstud
yAge
rang
e,mean(years)
Gen
der
Clin
ical
form
Patie
nts
enrolle
dLe
ishm
aniasisd
iagn
osis
Statistic
s
Mira
nda-Ve
raste
guiet
al.,2
009
Limaa
ndCu
sco,Peru
Com
parativ
eStudy;
Rand
omized
Con
trolledTrial
12/200
5-6/2006
4-52
Male7
7.5%
Female2
2.5%
Cutaneou
s80
Labo
ratory
(smear
microscop
y,cultu
reor
PCR)
Yes
Nascimento
etal.,
2010
Minas
Gerais,
Brazil
Rand
omized
Con
trolledTrial
10/200
4–10/200
618-59,26.4
Male6
3.6%
Female3
6.4%
Cutaneou
s44
Labo
ratory
(microscop
yidentifi
catio
nin
biop
sied
tissue)
Yes
Nilforou
shzadehet
al.,2
007
Isfahan,Iran
Rand
omized
Con
trolledTrial
NR
7-70
Male6
7.7%
Female3
2.3%
Cutaneou
s90
Labo
ratory
(smear
microscop
y)Yes
Nilforou
shzadehet
al.,2
008
Tehran,Iran
Com
parativ
eStudy;
Rand
omized
Con
trolledTrial
NR
7-70
Male7
1.0%
Female2
9.0%
Cutaneou
s124
Labo
ratory
(smear
microscop
y)Yes
VanTh
ieletal.,2010
Northern
Afghanista
n,ClinicalTrial
6/2005-11/2
005
NR
Dutch
Troo
psCu
taneou
s163
Labo
ratory
(smear
microscop
y,cultu
re,and
PCR)
Yes
NR,
notreported;PC
R,po
lymerasec
hain
reactio
n.

Dermatology Research and Practice 5
Table2:Clinic,therapeutic,and
epidem
iologicalcharacteristicso
fclin
icaltrialsinclu
dedin
thes
tudy.
Stud
ysource
Leish
man
iaspecies
Treatm
ent
Patie
ntsa
tthee
ndPrevious
treatm
ent
Clin
icallyhe
aled
Therap
yfailed
Relapseo
rRe
curren
ce
Alm
eida
etal.,2005
L.braziliensis
G1(MA+GM-C
SF)
5Yes
100%
(before120
days
AS)
Follo
w-up:12
mon
thsA
H0%
(12mon
thsA
H)
0%(12mon
thsA
H)
Arevaloetal.,2007
Leish
man
iaspp.
G1(IM
)6
No
0%Fo
llow-up:3mon
thsA
S67%(20days
AS)
33%(3
mon
thsA
S)
G2(M
A)
7No
57%(3
mon
thsA
S)Fo
llow-up:3mon
thsA
S43%(3
mon
thsA
S)0%
(3mon
thsA
S)
G3(M
A+IM
)7
No
100%
(3mon
thsA
S)Fo
llow-up:3mon
thsA
S0%
(3mon
thsA
S)0%
(3mon
thsA
S)
Brito
etal.,2017
L.braziliensis
(62%
ofcases)
G1(MA+PE
)82
NR
45%(6
mon
thsA
E)55%(6
mon
thsA
E)NR
G2(M
A+placebo)
8243%(6
mon
thsA
E)57%(6
mon
thsA
E)NR
El-Sayed
&Anw
ar,2010
NR
G1(ilSSG)
10(12lesio
ns)
No
50%/58.3%
(12we
eksA
S;patie
nts/lesio
ns)
Follo
w-up:6mon
thsA
E
50%/41.7
%(12we
eksA
S;patie
nts/lesio
ns)
NR
G2(il
SSG+im
SSG)
10(15lesio
ns)
No
90%/93.3%
(12we
eksA
S;patie
nts/lesio
ns)
Follo
w-up:6mon
thsA
E
10%/6.7%(12we
eksA
S;patie
nts/lesio
ns)
NR
G3(il
SSG+KE
)10
(13lesio
ns)
No
90%/92.3%
(12we
eksA
S;patie
nts/lesio
ns)
Follo
w-up:6mon
thsA
E
10%/7.7%
(12we
eksA
S;patie
nts/lesio
ns)
NR
Farajza
dehetal.,2
015
NR
G1(Terbinafine
+cryotherapy)
40No(w
ithin
thep
ast9
0days)
37.5%complete(28
days
AS)
10partialcure#
15(28days
AS)
NR
G2(M
A+
cryotherapy)
40No
52.5%(21d
aysA
S)7partialcure#
12(21d
aysA
S)NR
Firooz
etal.,2006∗∗
L.tro
pica
G1(MA+IM
)42
No
18.6%(4
weeksA
S)44
.1%(8
weeksA
S)50.8%(20we
eksA
S)Fo
llow-up:16
weeksA
E
49.2%(20we
eksA
S)3.1%
(16we
eksA
S)
G2(M
A+placebo)
47No
30.0%(4
weeksA
S)48.3%(8
weeksA
S)53.3%(20we
eksA
S)Fo
llow-up:16
weeksA
E
46.7%(20we
eksA
S)8.1%
(16we
eksA
S)
Khatamietal.,2013
L.major
G1(ilMA)
23(40
lesio
ns)
No
12.5%(6
weeksA
S)lesio
ns40
.0%(10we
eksA
S)lesio
nsFo
llow-up:5mon
thsA
E
65.0%(6
weeksA
S)42.5%(10we
eksA
S)0%
(5mon
thsA
E)
G2(il
MA+
non-silverP
D)
21(46
lesio
ns)
No
6.5%
(6we
eksA
S)lesio
ns42.2%(10we
eksA
S)lesio
nsFo
llow-up:5mon
thsA
E
80.4%(6
weeksA
S)55.6%(10we
eksA
S)0%
(5mon
thsA
E)
G3(il
MA+silver
PD)
29(55
lesio
ns)
No
12.7(6
weeksA
S)lesio
ns36.4(10we
eksA
S)lesio
nsFo
llow-up:5mon
thsA
E
74.6%(6
weeksA
S)49.1%
(10we
eksA
S)3.4%
(5mon
thsA
E)

6 Dermatology Research and Practice
Table2:Con
tinued.
Stud
ysource
Leish
man
iaspecies
Treatm
ent
Patie
ntsa
tthee
ndPrevious
treatm
ent
Clin
icallyhe
aled
Therap
yfailed
Relapseo
rRe
curren
ce
Llanos
Cuentasetal.,2010
L.braziliensis
G1(SSG+placebo)
12No(w
ithin
thep
ast3
0days);
22.0%had
received
previously
50%(84days
AS)
100%
(336
days
AS)
Follo
w-up:336days
AS
25%(168
days
AS)
0%(336
days
AS)
8%(336
days
AS)
G2(SSG
+(LEISH
-F1
+MPL
-SE))
LEISH-F1
5𝜇g=11
59%(84days
AS)
94%(336
days
AS)
Follo
w-up:336days
AS
13%(168
days
AS)
6%(336
days
AS)
0%(336
days
AS)
LEISH-F1
10𝜇g=12
LEISH-F1
20𝜇g=11
Machado
etal.,2007
L.braziliensis
G1(MA+placebo)
12No∗
41.6%(90days
AS)
Follo
w-up:150days
AS
42%(150
days
AS)
0%(2
yearsA
E
G2(M
A+PE
)11
No∗
82%(90days
AS)
Follo
w-up:150days
AS
0%(150
days
AS)
0%(2
yearsA
E)
Meymandi
etal.,2
011
L.tro
pica
G1(C02laser)
80No
56.8%(2
weeksA
S)67.6%(6
weeksA
S)44
.4%(12we
eksA
S)93.7%(89/95
lesio
ns)
Follo
w-up:16
weeksA
S
NR
NR
G2(il
MA+
cryotherapy)
80No
15.8%(2
week
AS)
57.5%(6
week
AS)
38.2%(12we
ekAS)
78%(74/95)lesions)
Follo
w-up:16
weeksA
S
NR
NR
Mira
nda-Ve
raste
guietal.,
2005
L.peruvian
aL.braziliensis
G1(MA+IM
)18
(35lesions)
Yes
6%(20days
AE)
50%(1mon
thAE)
61%(2
mon
thsA
E)72%(3
mon
thsA
E)72%(6
mon
thsA
E)72%(12mon
thsA
E)Fo
llow-up:12
mon
thsA
E
27.8%(12mon
thsA
E)NR
G2(M
A+Ve
hicle)
20(40
lesio
ns)
Yes
5%(20days
AE)
15%(1mon
thAE)
25%(2
mon
thsA
E)35%(3
mon
thsA
E)50%(6
mon
thsA
E)75%(12mon
thsA
E)Fo
llow-up:12
mon
thsA
E
25%(12mon
thsA
E)NR

Dermatology Research and Practice 7Ta
ble2:Con
tinued.
Stud
ysource
Leish
man
iaspecies
Treatm
ent
Patie
ntsa
tthee
ndPrevious
treatm
ent
Clin
icallyhe
aled
Therap
yfailed
Relapseo
rRe
curren
ce
Mira
nda-Ve
raste
guietal.,
2009
L.peruvian
aL.
guyanensis
L.braziliensis
G1(SSG+vehicle
cream)
36No
17.5%
(20days
AS)
33%(1mon
thAS)
30%(2
mon
thsA
S)60
%(3
mon
thsA
S)63%(6
mon
thsA
S)58%
(9mon
thsA
S)53%(12mon
thsA
S)Fo
llow-up:12
mon
thsA
S
41.7%(12mon
thsA
S)NR
G2(SSG
+IM
)39
No
5%(20days
AS)
43%(1mon
thAS)
60%(2
mon
thsA
S)78%(3
mon
thsA
S)75%(6
mon
thsA
S)75%(9
mon
thsA
S)75%(12mon
thsA
S)Fo
llow-up:12
mon
thsA
S
23.1%
(12mon
thsA
S)NR
Nascimento
etal.,2010
Leish
man
iaspp.
G1(MA+(LEISH
-F1
+MPL
-SE))
LEISH-F1
5𝜇g=9
No
80%(84days
AS)
Follo
w-up:336days
AS
24%(84days
AS)
4%(84days
AS)
LEISH-F1
10𝜇g=8
LEISH-F1
20𝜇g=8
G2(M
A+M
PL-SE)
8No
50%(84days
AS)
Follo
w-up:336days
AS
50%(84days
AS)
NR
G3(M
A+S
aline)
8No
38%(84days
AS)
Follo
w-up:336days
AS
62%(84days
AS)
38%(84days
AS)
Nilforou
shzadehetal.,2
007
Leish
man
iaspp.
G1(ilMA+topical
honey)
33No
51.1%
(6we
eksA
S)Fo
llow-up:4mon
thsA
S48.9%
(6we
eksA
S)NR
G2(il
MA)
35No
71.1%
(6we
eksA
S)Fo
llow-up:4mon
thsA
S28.9%
(6we
eksA
S)NR
Nilforou
shzadehetal.,2
008
L.tro
pica
L.major
G1(MA60
mg/kg/day
+placebo)
43No
93%(12we
eksA
S)Fo
llow-up:12
weeksA
S7%
(12we
eksA
S)NR
G2(M
A30
mg/kg/day
+OM)
36No
89%
(12we
eksA
S)Fo
llow-up:12
weeksA
S11%
(12we
eksA
S)NR
G3(M
A30
mg/kg/day
+placebo)
45No
80%(12we
eksA
S)Fo
llow-up:12
weeksA
S20%(12we
eksA
S)NR
VanTh
ieletal.,2010
L.major
G1(ilSSG)
118No
55.1%
(6mon
thsA
E)Fo
llow-up:6mon
thsA
E20.3%(6
mon
thsA
E)15.3%(6
mon
thsA
E)
G2(il
SSG+
cryotherapy)
45No
66.7%(6
mon
thsA
E)Fo
llow-up:6mon
thsA
E13.3%(6
mon
thsA
E)11.1%
(6mon
thsA
E)
NR,
notreported;G1,Group
1;G2,Group
2;G3,Group
3.MA,m
eglumineantim
oniate;P
E,pentoxify
lline;G
M-C
SF,g
ranu
locyte
macroph
agecolony-stim
ulatingfactor;IM,imiquimod
;ilS
SG,intralesio
nals
odium
stibo
glucon
ate;
imSSG,intramuscularsodium
stibo
glucon
ate;KE,ketoconazole;ilM
A(in
tralesionalm
egluminea
ntim
oniate);no
n-silverP
D,non
-silvercontaining
polyesterd
ressing;silverP
D,silvercontaining
polyesterd
ressing;SSG,sod
ium
stibo
glucon
ate;
LEISH-F1,lyop
hilized
LEISH-F1p
rotein;M
PL-SE,
adjuvant;O
M,omeprazole.
AS:aft
erthes
tartof
treatment,AE:
after
thee
ndof
treatment,andAH:afte
rthe
healingof
thelesion.
∗Noprevious
treatmento
fmucosalleish
maniasis.Som
epatientsh
adprevious
cutaneou
sleishmaniasis,but
therea
reno
references
toprevious
treatmento
rnot.
∗∗Clinicalcure
rate,therapy
failu
re,and
relapseo
rrecurrencegivenby
Firooz
etal.,2006
,based
ontheinitia
lnum
bero
fpatientsa
llocatedin
each
grou
p.# Partia
lcureF
arajzadeh:decrease
inindu
ratio
nsiz
ebetwe
en25
and75%.

8 Dermatology Research and Practice
Table 3: Description of adverse effects of combinations for the treatment of tegumentary leishmaniasis.
Treatment Side effects Study source
MA + IM
Localized pruritus, erythema and edema (77%); arthralgia, myalgia, flu-likesymptoms (86%); and elevated liver enzyme levels (64%). Arevalo et al., 2007
Moderate pruritus and burning sensation (7.1%). Firooz et al., 2006
Edema (35%); itching (10%); burning (15%); pain (5%); erythema (55%). Miranda-Verastegui et al.,2005
MA + PE
Nausea (27.3%); arthralgias (9.1%); dizziness, abdominal pain, and diarrhea(9.1%). Machado et al., 2007
Vomiting (2.4%); Diarrhea (1.2%); Nausea (8.6%); Headache (11%); Asthenia(3.7%); Anorexia (3.7%); Epigastralgia (3.7%); Pain (2.4%); Dizziness (2.4%);Fever (7.4%); Arthralgia (8.6%); Myalgia (13.5%)
Brito et al., 2017
MA + cryotherapy No adverse effects were observed Farajzadeh et al., 2015
MA + (LEISH-F1 +MPL-SE)
Local: induration (44.4 – 77.8%); erythema (11.1 – 100%); tenderness(33.3-44.4%).Systemic: headache (0-22.2%); pyrexia (0-22.2%).MA-related AEs (22.2 – 88.9%).
Nascimento et al., 2010
MA + GM-CSF No adverse effects were observed Almeida et al., 2005MA + OM NR Nilforoushzadeh et al., 2008il MA + silver PD Itching and burning (35.3%); edema (33.3%). Khatami et al., 2013il MA + topical honey Dermatitis to honey (3%). Nilforoushzadeh et al., 2007
il MA + cryotherapy Hyper pigmentation+trivial scar (18.7%); atrophic scar (7.5%); hypopigmentation+trivial scar (18.8%). Meymandi et al., 2011
SSG + (LEISH-F1 +MPL-SE)
Local: induration (41.7 – 75.0%); erythema (50.0 – 100.0%); tenderness (66.7 –91.7%).Systemic: anorexia (0 – 8.3%); fatigue (0 – 8.3%); malaise (25.0%); myalgia (0– 8.3%); headache (33.3 – 50.0%).SSG-related (100%).
Llanos Cuentas et al., 2010
SSG + IM Swelling (30%); itching (25%); pain (12.5%); erythema (32.5%). Miranda-Verastegui et al.,2009
il SSG + im SSG im SSG: Pain at the injection site (100%).il SSG: Pain and swelling at the intralesional injection site (100%). El-Sayed & Anwar, 2010
il SSG + KE KE: No.il SSG: Pain and swelling at the intralesional injection site (100%). El-Sayed & Anwar, 2010
il SSG + cryotherapy Secondary infection (31%); lymphatic involvement (48.8%); pain at theinjection site VanThiel et al., 2010
NR, not reported; G1, Group 1; G2, Group 2; G3, Group 3. MA, meglumine antimoniate; PE, pentoxifylline; GM-CSF, granulocyte macrophage colony-stimulating factor; IM, imiquimod; il SSG, intralesional sodium stibugluconate; im SSG, intramuscular sodium stibugluconate; KE, ketoconazole; il MA(intralesional meglumine antimoniate); non-silver PD, non-silver containing polyester dressing; silver PD, silver containing polyester dressing; SSG, sodiumstibugluconate; LEISH-F1, lyophilized LEISH-F1 protein; MPL-SE, adjuvant; OM, omeprazole; AEs, adverse events.
polyester dressing; silver-containing polyester dressing;lyophilized LEISH-F1 protein; cryotherapy, topical honey,and omeprazole.
Among the patients involved in the studies, 92.0%(1199/1302) ended the treatment, of which 48.0% (575/1199)underwent a combination treatment (antimonial pentavalentplus other treatment) and the remaining 52.0% (624/1199)were treated only with pentavalent antimonials or other treat-ment modalities (Table 2). Most of them had not undergoneprevious treatments.
The combination of drugs revealed high rates of clinicalcure among the groups treated with drug combination.Two papers reported a cure rate of 100% in these groups(Almeida et al. 2005 [19]; Arevalo et al. 2007 [20]), while8 authors reported 70-94% cure in the groups treated with
combinations (El-Sayed and Anwar 2010 [21]; Llanos Cuentaset al. 2010 [22]; Machado et al. 2007 [15]; Meymand et al. 2011[10]; Miranda-Verastegui et al. 2005 [23]; Miranda-Verasteguiet al. 2009 [24]; Nascimento et al. 2010 [25]; Nilforoushzadehet al. 2008 [26]). The other authors reported cure rates below70% and ranged from 36.4% to 66.7%. The lowest curerate was (36.4%) in the combination of IL-MA+ silver PD(Khatami et al. 2013 [27]) (Table 2).
Among the combinations, those with 100% of curerate were meglumine antimoniate (MA) plus granulocytemacrophage colony-stimulating factor (GM-CSF) (Almeidaet al. 2010) and meglumine antimoniate plus imiquimod(Arevalo et al. 2007). The other combinations that resultedin 70-94% of cure were the combinations of sodium sti-bogluconate (SSG) plus LEISH-F1 + MPL-SE (94%) (Llanos

Dermatology Research and Practice 9
Table4:Con
clusio
non
combinatio
ntre
atmentasa
newtre
atmento
ftegum
entary
leish
maniasis
inthes
ystematicreview
.
Treatm
ent
Dose
Routeo
fAdm
inistration/Time
Time
Efficacy
Safety
Practic
e/clinical
implications
Stud
ysource
MA+IM
IM:L
esion≤3c
m:1
dose
of7.5
%cream.
Lesio
n>3cm
:2do
seso
f7.5
%cream.
Each
dose
=125mg.
IM:top
ical-d
aily
20days
Efficaciou
sAc
ceptableris
kwith
specialized
mon
itorin
gInvestigatio
nal
Arevaloetal.,2
007
MA:20mg/kg/day.
MA:IV-d
aily
IM:5%cream.
IM:top
ical-3
times
perd
ayIM
:28days
Likely
efficaciou
sAc
ceptableris
kwith
specialized
mon
itorin
gInvestigatio
nal
Firooz
etal.,2006
MA:20m
gSb5+/kg/day.
MA:IM
daily
MA:14days
IM:5%cream.
IM:Top
ical-d
aily.
IM:20days.
Efficaciou
sAc
ceptableris
kwith
out
specialized
mon
itorin
gClinicallyuseful
Mira
nda-
Veraste
gui
etal.,2005
MA:20m
g/kg/day.
MA:IM
daily
inchild
ren,
andIV
infusio
nin
older
subjects.
MA:20days.
MA+PE
MA:20m
g5+/kg/day
MA:daily
MA:30days
Efficaciou
sAc
ceptableris
kwith
specialized
mon
itorin
gClinicallyuseful
Machado
etal.,2
007
PE:400
mg
PE:oral–
3tim
esdaily
PE:30days
MA:20m
gsbv/K
g/day
MA:IV-
daily
MA:20days
Not
efficaciou
sAc
ceptableris
kwith
specialized
mon
itorin
gNot
useful
Brito
etal.,2017
PE:400
mPE
:oral-3tim
esdaily
PE:20days
MA+
cryotherapy
Cryotherapy:fre
ezetim
e(10-25
s)
Cryotherapy:on
thelesion
until
1-2mm
ofsurrou
ndingno
rmaltissue
appeared
frozen
Everytwowe
eks
Likely
efficaciou
sAc
ceptableris
kwith
out
specialized
mon
itorin
gPo
ssiblyuseful
Farajza
dehetal.,
2015
MA:15mg/kg/day
Intram
uscular
Everydayfor3
weeks
MA+
(LEISH
-F1+
MPL
-SE)
LEISH-F1:5,10
or20𝜇g+
25𝜇gMPL
-SE.
LEISH-F1:SU
B–3tim
es.
LEISH-F1:Onday0,28
and56.
Likely
efficaciou
sAc
ceptableris
kwith
specialized
mon
itorin
gPo
ssiblyuseful
Nascimento
etal.,
2010
MA:10mg/
Sb5+kg/day.
MA:IV–10-daysc
ycles
follo
wedby
11days
ofrest.
MA:Th
efirst10-days
cycleo
nDay
0.Ad
ditio
nalcycleso
ndays
21,42,and63
MA+GM-C
SFGM-C
SF:1-2
mL(10
𝜇g/mL).
GM-C
SF:top
ical–3tim
esperw
eek.
GM-C
SF:3
weeks
Efficaciou
sAc
ceptableris
kwith
out
specialized
mon
itorin
gInvestigatio
nal
Alm
eida
etal.,2005
MA:20mgSb5+/kg/day.
MA:IV–daily.
MA:20days

10 Dermatology Research and Practice
Table4:Con
tinued.
Treatm
ent
Dose
Routeo
fAdm
inistration/Time
Time
Efficacy
Safety
Practic
e/clinical
implications
Stud
ysource
MA+OM
MA:30m
g/kg/day
MA:IM-d
aily
MA:3
weeks
Likely
efficaciou
sAc
ceptableris
kwith
specialized
mon
itorin
gClinicallyuseful
Nilforou
shzadehet
al.,2008
OM:40m
gOM:oral-
daily
OM:3
weeks
ilMA+silver
PD
MA:il
MA:Intraderm
allyin
each
onec
entim
eter
square
ofa
lesio
nun
tilblanching
occurred
intralesional,on
cewe
ekly.
42days
Not
efficaciou
sAc
ceptableris
kwith
specialized
mon
itorin
gInvestigatio
nal
Khatamietal.,2013
Silver
PD:onthelesion
Silver
dressin
g:topical–
once
daily
ilMA+topical
honey
MA:il
MA:ileno
ughto
blanch
thelesionand1m
mrim
ofthes
urroun
ding
norm
alskin,oncew
eekly.
Untilcompleteh
ealin
gor
form
axim
um6we
eksNot
efficaciou
sInsufficientevidence
Investigatio
nal
Nilforou
shzadehet
al.,2007
Hon
ey:soakedgauze
Hon
ey:top
ical–twiced
aily
ilMA+
cryotherapy
Cryotherapy:fre
ezetim
e(10-2
5s)
Cryotherapy:on
thelesion
until
2-3m
mhaloform
sarou
nd,w
eekly,before
ILMA.
Untilcompletec
ureo
rforu
pto
12we
eks
Likely
efficaciou
sAc
ceptableris
kwith
out
specialized
mon
itorin
gPo
ssiblyuseful
Meymandi
etal.,
2011
MA:(0.5–
2ml)
MA:intraderm
ally,
all
directions,untilthelesion
hadcompletely
blanched,
weekly.
SSG+
(LEISH
-F1+
MPL
-SE)
LEISH-F
1:5,10
or20𝜇g+
25𝜇gMPL
-SE.
LEISH-F1:SU
B–3tim
es.
LEISH-F1:Onday0,28
and56.
Efficaciou
sAc
ceptableris
kwith
specialized
mon
itorin
gInvestigatio
nal
Llanos
Cuentase
tal.,2010
SSG:20m
g/kg/day
SSG:IV–daily
SSG:day
0to
27
SSG+IM
IM:5%cream.
IM:Top
ical-3
times
per
week.
IM:20days
Efficaciou
sAc
ceptableris
kwith
out
specialized
mon
itorin
gClinicallyuseful
Mira
nda-
Veraste
gui
etal.,2009
SSG:20mg/kg/day
SSG:IV–daily.
SSG:20days
ilSSG+im
SSG
ilSSG(100
mg/mL),the
dose
varie
dbetween0.3-3.0
mL.Maxim
umdo
se20mg/Kg
/day.
il:Infiltrated
inmultip
lesites
until
complete
blanchinganda1-m
mwide
ringof
thes
urroun
ding
norm
alskin.
ilSSGon
days
1,3,5in
ones
essio
n-u
pto
3cycles.
Efficaciou
sAc
ceptableris
kwith
specialized
mon
itorin
gPo
ssiblyuseful
El-Sayed
&Anw
ar,
2010
imSSG(a
partof
thed
ose
20mg/Kg/dayalreadygiven
provided
toIL
SSGin
the
samed
ays).
im:one
injectionon
days
1,3,5-u
pto
3cycles
with
4we
eksinterval.

Dermatology Research and Practice 11
Table4:Con
tinued.
Treatm
ent
Dose
Routeo
fAdm
inistration/Time
Time
Efficacy
Safety
Practic
e/clinical
implications
Stud
ysource
ilSSG+KE
ilSSG(100
mg/mL),the
dose
varie
dbetween0.3-3.0
mL,maxim
umdo
se20mg/Kg
/day.
il:Infiltrated
inmultip
lesites
until
complete
blanchinganda1-m
mwide
ringof
thes
urroun
ding
norm
alskin.
il:on
days
1,3,5in
one
session-u
pto
3cycles.
Efficaciou
sAc
ceptableris
kwith
specialized
mon
itorin
gPo
ssiblyuseful
El-Sayed
&Anw
ar,
2010
KE:200
mg.
KE:3
times
daily.
KE:4
weeks.
ilSSG+
cryotherapy
ilSSG:1-2ml.
ilSSG:intomarginof
each
lesio
n,allaroun
d,un
tilblanchingwith
cryotherapy
precedingthefi
rst
injection.
ilSSG:3
injections
SSG
with
intervalso
f1-3
days.Effi
caciou
sAc
ceptableris
kwith
out
specialized
mon
itorin
gClinicallyuseful
vanTh
ieletal.,2010
Cryotherapy:localw
itha
doub
lefre
eze-thaw
cycle.
20second
sfor
freezing
cyclea
ndthaw
ingtim
ebetweencycles
of45-90
second
s.
Cryotherapy:tre
atment
was
repeated
until
clinicalim
provem
ent
(range
1-163
days).
MA,m
eglumineantim
oniate;P
E,pentoxify
lline;G
M-C
SF,g
ranu
locyte
macroph
agecolony-stim
ulatingfactor;IM,imiquimod
;ilS
SG,intralesio
nals
odium
stibo
glucon
ate;
imSSG,intramuscularsodium
stibo
glucon
ate;KE,
ketoconazole;ilM
A(in
tralesionalm
eglumineantim
oniate);no
nsilver
PD,n
onsilverc
ontainingpo
lyesterd
ressing;silverP
D,silver
containing
polyesterd
ressing;SSG,sod
ium
stibo
glucon
ate;
LEISH-F1,lyop
hilized
LEISH-F1p
rotein;M
PL-SE,
adjuvant;O
M,omeprazole;IV,
intravenou
s;IM
,intramuscular;SU
B,subcutaneously.

12 Dermatology Research and Practice
Articles identified through databasesearching(n= 4,725)
Publications recovered in the referencesof the selected articles
(n = 0)
Records identified a�er applying filters(Abstract; Humans; English; Clinical
(n= 363)Trial)
Records a�er removal of duplicates(n= 311)
Articles assessed in full text for
(n= 90)eligibility
Full text articles included in the
(n=16)systematic review
Full text articles excluded for not
(n= 74)meeting the goals of the study
Excluded articles (n= 221)- Visceral leishmaniasis/Kala-azar (n= 91)
- Did notmeet the goals of the study (n= 90)(n= 20)
(n= 9)- No human subjects
- Case report ( n= 1)
- Related the Leishmania species to the response totreatment (n= 1)
- Review articles (n= 9)-- In vitro studies
Iden
tifica
tion
Scre
enin
gEl
igib
ility
Inclu
sion
Figure 1: Flow diagram of study selection for the systematic review.

Dermatology Research and Practice 13
Cuentas et al. 2010); intralesional sodium stibogluconate plusketoconazole (90%) (El-Sayed and Anwar 2010); meglumineantimoniate plus omeprazole (89%) (Nilforoushzadeh et al.2008); MA and pentoxifylline (82%) (Machado et al. 2007);meglumine antimoniate plus LEISH-F1 + MPL-SE (80%)(Nascimento et al. 2010); intralesional sodium stibogluconateplus cryotherapy (78%) (Meymand et al. 2011); sodiumstibogluconate plus imiquimod (75%) (Miranda-Verasteguiet al., 2009); and meglumine antimoniate plus imiquimod(72%) (Miranda-Verastegui et al. 2005). It is important tonote that most combinations that showed high cure rates(70-100%)were combinations of pentavalent antimonial withsome immunomodulators.
Relapse or recurrence, when reported, was higher in thegroups treated with pentavalent antimonial alone and variedfrom 0 to 38% (Llanos Cuentas et al., 2010; Nascimentoet al., 2010 [22, 25]). For the associated groups, only fourassociations presented relapse or recurrence, and these ratesranged from0 to 11.1% (Firooz et al. 2006;Van-Thiel et al. 2010[28, 29]) (Table 2).
No serious adverse effects were observed in patientstreated with the drugs combination. For the combination ofimiquimod andmeglumine antimoniate, adverse effects werelocally limited, being the most reported pruritus/itching,erythema, and edema. For the combination of imiquimodwith sodium stibogluconate, the same was observed. OnlyMiranda-Verastegui et al. (2005) [23] reported elevated liverenzyme levels.
In relation to granulocyte macrophage-stimulating fac-tor, there were no reports of side effects. With lyophilizedLEISH-F1 protein in association to meglumine antimoniate,the observed side effects were induration, erythema, andtenderness; in combination with sodium stibogluconate, thepresence of induration, erythema, and tenderness sites wasreported, in addition to headache pyrexia and systemicmalaise.The common adverse effects of the use ofmeglumineantimoniate and sodium stibogluconate were also observed.
To the combination of meglumine antimoniate and pen-toxifylline, the common adverse effects, described in twostudies, were nausea, arthralgia, dizziness, pain, and diarrhea.
In the use of intralesional sodium stibogluconate, aloneor in association with other medicinal products, secondaryinfection, pain and swelling at injection site, and lymphaticinvolvement were observed. The pentavalent intralesionalantimonials also showed adverse effects related to the appli-cation site, such as pain, pruritus/itching, and edema.
Intralesional sodium stibogluconate, when associatedwith cryotherapy, resulted in secondary infection and lym-phatic involvement, in addition to the inherent symptomsof intralesional application of stibogluconate already men-tioned. Meglumine antimoniate combined with silver PDpresented only itching, burning, and edema, in contrast towhen combined with topical honey, in which only dermatitis,caused by honey, was reported. Cryotherapy combined withmeglumine antimoniate had only local adverse effects suchas hyperpigmentation plus trivial scar, atrophic scar, andhypopigmentation plus trivial scar (Table 3).
Each of the combinations was classified according totheir efficacy (efficacious/likely efficacious/not efficacious)
and the clinical implications (investigational/clinically use-ful/possibly useful) [30].
In this context, imiquimod associated with meglumineantimoniate (Miranda-Verastegui et al. 2005 [23]) and sti-bogluconate (Miranda-Verastegui et al. 2009 [24]) andcryotherapy-associated stibogluconate (Van-Thiel et al. 2010[29]) were classified as clinically useful and with acceptablerisk without specialized monitoring. Themeglumine antimo-niate associated with pentoxifylline (Machado et al. 2007)were classified as clinically useful and with acceptable riskwith specialized monitoring (Machado et al. 2007 [15]). Onthe other hand the combination of meglumine antimoniateassociated with pentoxifylline performed by Brito et al. 2017[31] to treat cutaneous leishmaniasis caused by Leishmaniabraziliensis was classified as not efficacious and not useful.Meglumine antimoniate associated with omeprazole (Nil-foroushzadeh et al. 2008 [26]) was classified as clinicallyuseful and with acceptable risk with specialized monitoring.
Some combinations have been classified as possibly usefulwith acceptable risks without specialized monitoring, such ascryotherapy combined with meglumine antimoniate (Fara-jzadeh et al. 2015 [32]) and the intralesional meglumineantimoniate with cryotherapy (Meymandi et al. 2011 [10]).The combination LEISH-F1 + MPL-SE plus meglumine anti-moniate (Nascimento et al. 2010 [25]) and sodium stiboglu-conate with ketoconazole (EL-Sayed and Anwar 2010 [21])was classified as possibly useful and with an acceptable riskwith specialized monitoring.
GM-CSF plus meglumine antimoniate (Almeida etal. 2005 [19]) was still classified as investigational andwith acceptable risk without specialized monitoring, whileother combinations were classified as investigational, butwith acceptable risk with specialized monitoring, such as:imiquimod plus meglumine antimoniate (Arevalo et al.,2007 [20]), Leish-F1+ MPLE-SE plus sodium stibogluconate(Llanos Cuentas et al. 2010 [22]), meglumine antimoniatecombined with silver PD (Khatami et al. 2013 [27]), andimiquimod plus meglumine antimoniate (Firooz et al. 2006[28]). The evidence provided by the study with the combi-nation of intralesional meglumine antimoniate and topicalhoney was insufficient to classify this combination in relationto safety (Table 4).
Regarding effectiveness, only three combinations wereclassified as noneffective: intralesional meglumine antimo-niate associated with topical honey performed by Nil-foroushzadeh et al. (2007) [33], intralesional meglumineantimoniate associated with silver PD tested by Khatami et al.(2013) [27], and pentoxifylline plus meglumine antimoniateperformed by Brito et al. (2017).The other combinations wereclassified as “efficacious” or “likely efficacious”.
4. Discussion
In this review, we saw that the majority of the combinationsresulted in an elevated cure rate. Relapse or recurrence,when reported, were higher in the groups treated with theisolated drugs than in the ones treated with the drugs com-bination. These findings indicate that the combinations with

14 Dermatology Research and Practice
pentavalent antimonials were more efficacious to preventrelapse or recurrence. Several authors have demonstrated thatthe combination of some drugs with pentavalent antimonialshowed a higher percentage of cure.
4.1. Pentavalent Antimonials. Pentavalent antimonials areconsidered the first line drugs to treat CL, but they havecollateral effects and, in some cases, low cure rate. Accordingto a systematic review by Tuon et al. (2008) [34], meg-lumine antimoniate (MA), in the recommended dose (20mg/kg/day), presents an average cure of 76.5%. However,among the studies evaluated by Tuon et al. (2008) [34] andother studies, meglumine antimoniate (20 mg/kg/day) curerates are quite variable: 40.4% [7, 16], 56.9% [35], 69.4% [7],79% [36], 84% [5], 85% [37], and 100% [38, 39].
For sodium stibogluconate (SSG), the cure rate shown byTuon et al. (2008) [34] was of 75.5% in different dosages, witha maximum dose of 20 mg/kg/day. However, the efficacy forthis pentavalent antimonial is also variable, being reportedrates of 53% [24], 56% [40], 70% [41], and 100% [22, 42].
It is known that the use of systemic meglumine antimo-niate can be lead to serious adverse effects, so the applicationin the lesion site showed to be an efficacious and more securealternative to treat CL. Some authors have demonstrated thatthe intralesional MA is as effective as the systemic MA andhad few adverse effects [43–45]. It is important to note that,unlike in the articles included in this study, Vasconcellos et al.(2014) [46] reported that one patient presented eczema afterthe treatment with intralesional meglumine antimoniate.After use of oral dexchlorpheniramine, eczema and ulcerreceded. Thus, the administration of intralesional MA mustbe carefully conducted, especially due to the possibility ofoccurring hypersensitivity.
For the SSG, the intralesional application has also showngood results [47, 48]. The application twice a week is welltolerated and the lesions healed faster than only once a week[49].
4.2. GranulocyteMacrophageColony-Stimulating Factor (GM-CSF). The granulocyte macrophage colony-stimulating fac-tor (GM-CSF) acts in the recruitment of monocytes andneutrophils. It is produced by a wide range of cellssuch as macrophages, neutrophils, dendritic cells, T cells,eosinophils, fibroblasts and endothelial cells. It is alsobelieved that it promotes the differentiation of the macro-phages to a proinflammatory phenotype [50].
In view of its role in the recruitment of different types ofcells, GM-CSF has been investigated for the CL treatment. Intheir study, Almeida et al. (2005) [19] evaluated the topical useof GM-CSF (10 𝜇g/mL) in combination with the meglumineantimoniate (20 mg/kg/day) and showed that 60% of thepatients were clinically healed 50 days after the treatmentstart, and the remaining 40% were cured 120 days after thebeginning of the treatment. Similar results were found bySantos et al. (2004) [51], when they use this combination.On the other hand, among the patients treated only withmeglumine antimoniate, just 20% were clinically healed at 45days after the start of treatment, and 100%of the patients werecured after 256 days.
In a previous study, Almeida et al. (1999) [52] showedthat clinical cure in patients treated with the combination ofpentavalent antimonial and GM-CSF was faster than in thecontrol group that was treated with pentavalent antimonialalone. Possibly the factor that contributed for the quickcure associated by GM-CSF was the modulation of theimmunologic balance, by inducing differentiation for theTh1 subtype [52–54] and activation of macrophages to killLeishmania [55].
GM-CSF combined with pentavalent antimonial can bean alternative to treat CL, since the risk inherent to thiscombination is acceptable and its use deserves to be greatlyinvestigated.
4.3. Imiquimod. Imiquimod is an immunomodulator thatwas first approved to treat genital and perianal warts and thento treat actinic keratosis.
Imiquimod stimulates the immune system in differentways. It is believed that imiquimod is an agonist of thetool like receptors 7 and 8, so the stimulation of thesereceptors leads to the synthesis of different inflammatorymediators, such as INF-𝛼, TNF-𝛼, interleukins 1, 6, 8, 10 and12, granulocyte colony -stimulating factor and granulocytemacrophage colony-stimulating factor [56–58]. In addition,the use of imiquimod also indirectly contributes to theimmune response acquired, through the induction of Th1type cytokines, such as INF-Υ [58, 59].The induction of INF-Υ an IL-12 production induces toTh1 differentiation and it isimportant in the control of CL.
Imiquimod has been investigated in the treatment of CLand its efficacy is controversial. Arevalo et al. (2007) [20]and Seeberger et al. (2003) [60] showed no efficacy in theuse of imiquimod alone. In combination with pentavalentantimonials, imiquimod can be an adjuvant; moreover, thesuccess in treatment with imiquimod is directly related tothe concentration used. Only at the concentration of 7.5%imiquimod combined with meglumine antimoniate appearsto be more effective than the antimonate alone [20]. Authorsthat administered imiquimod at 5% in combination withmeglumine antimoniate observed that the efficacy was sim-ilar to that of patients treated with meglumine antimoniatealone [23, 28].
However, when Miranda-Verastegui et al. (2009) [24]used imiquimod 5% combined with sodium stibogluconate,the combination was more effective than sodium stiboglu-conate alone.
Meymandi et al. (2011) [61] showed the combinationof intralesional meglumine antimoniate and imiquimod asbeneficial its resulted in a decrease in parasitic load, anincrease in lymphocyte numbers, and a decrease in histiocyteaggregation in the lesion site. In addition, they observed thatimiquimod alone was also ineffective.
Imiquimod appears to be a good adjuvant for pentavalentantimonial when used in the appropriate concentration. Therisk involved in its use is acceptable. More evidence is neededto strengthen its application in clinical practice.
4.4. Silver-Containing Polyester Dressing. The silver-contain-ing polyester dressing (silver PD) is composed of hydropho-bic polyamide netting with silver-coated fibers. Silver PD

Dermatology Research and Practice 15
differs from each other by the way silver is incorporated andhow it is liberated in the lesion. It is known that silver hasantimicrobial activity in solutions, but it does not differentiateat pathogens from the other cells, such as fibroblast andkeratinocytes [62, 63].
Clinical trials using silver PD to treat CL are scarce. Inthis review, only one study used silver PD with this aim. Noefficacy in silver PD was shown, not even combined withintralesional meglumine in the treatment of CL [27]. In thisstudy, silver PD Atrauman Ag� by Hartmann was used.
Asmentioned before, silver can cause the death of humancells [63]. However, according to the manufacturer of theAtrauman Ag�, a higher concentration of silver is needed tolead to the death of human cells and, specifically in the caseof Atrauman Ag�, the release of silver is small. Moreover thisdressing released silver only when in contact with bacteriaand no negative influence of the silver ions was exercised inhuman cells [64]. Since amastigote forms are phagocytosedby macrophages, they remaining and multiplying. The silverreleased by the dressing, for being in small quantities, maynot be able to reach the amastigotes phagocytosed.
There are some inherent characteristics of polyester dress-ing that influence in their activity, such as their capacity in therelease of silver [65]. Besides that, the compounds binding tosilver can contribute to this activity.
The use of silver PD isolated or in combination withpentavalent antimonial needs to be further investigated dueto the scarcity of studies that used silver PD to treat CL andthe several factors that can influence its efficacy.
4.5. LEISH-F1+MPL-SE. LEISH-F1+MPL-SE was the firstcandidate vaccine for entry in clinical trials. It was composedby recombinant fusion protein Leish-111f and an adjuvantin an oil-water emulsion (monophosphoryl lipid A - MPL).MPL is a TLR4 agonist, safely used in other vaccines, such ashepatitis [66].
Authors demonstrated that LEISH-F1+MPL-SE was safe,immunogenic, and effective in inducing the production ofIgG antibodies, INF-Υ, and other cytokines in humans andmice [67–69].
In the two articles included in this review, LEISH-F1+MPL-SE was tested in combination with SSG or meglu-mine antimoniate in the treatment of CL. One of these LlanosCuentas et al. (2010) [22] observed similar clinically curein both groups; however in addition, relapse or recurrencedid not occur in the combination groups. The stimulation ofthe immune response was greater in the LEISH-F1+MPL-SEgroup than in the SSG group, a fact that may have contributedto the absence of recurrences.
Nascimento et al. (2010) [25], on the other hand, observeda greater clinical cure rate (80%) in the group treated with thecombination of LEISH-F1+MPL-SE and meglumine antimo-niate than in the groups treated with meglumine antimoniatealone (38%) or the adjuvant MPL-SE alone (50%).
LEISH-F1+MPL-SE in combination with pentavalentantimonials can be useful to treat CL, mainly because thiscombination appears to decrease recurrences observed with
pentavalent antimony alone. The risks related to its use areacceptable therefore its use should be better explored.
4.6. Topical Honey. Honey was used, many years ago to treatseveral types of lesions, but there is no consensus on itseffectiveness in lesion healing. In relation to CL, there are fewdata on the use of honey for its treatment.
It is well established that honey has an antimicrobialaction, which can act on tissues, contributing to their repair[70], and also on the immune system, having both proinflam-matory and anti-inflammatory action [71].
FDA has already approved some honey-based productswith different clinical indications, but some authors remaincautious regarding its clinical use for lesion healing. Jull etal. (2013) [72], in a review about the use of topical honey inthe treatment of wounds, concluded that honeymay delay thetime of wound healing in some types of wounds, such as CLand deep burns, but it is good for moderate burns. Still, intheir opinion, more clinical studies are needed to guide theuse of honey in clinical practice in other types of wounds thanmoderate burns.
In the same line Saikaly and Khachemoune (2017) [73]concluded in their study that the use of honey seems to bebeneficial to wound healing in some types of lesions and thatnew technologies have contributed to the understanding ofthe action mechanisms of honey. However, more evidence isstill needed to elucidate precisely the results obtainedwith theuse of honey.
The combination of topical honey with IL-MA to treatCL was tested by Nilforoushzadeh et al. (2007) [33] and didnot show efficacy. In this study, gauze soaked in honey wasused, not beingmentioned the type of honey used. It is knownthat there are different types of honey of different constitutionand that, therefore, they may have different properties [71].The choice of dressing must also be taken into consideration,as one should choose the dressing most appropriate for thewound to be treated [70].
There are several factors related to honey that should betaken into account, such as honey type and composition, aswell as the best form of application, and it deserves to bebetter evaluated in order to be combined with pentavalentantimonials in the treatment of CL.
4.7. Omeprazole. Omeprazole is a drug used to treat pepticulcer disease, due to its interference with the stomach pH.Omeprazole acts by inhibiting the human gastric K+, H+-ATPase enzyme, resulting in the disruption of acid secretion[74].
In the intracellular environment, omeprazole accumu-lates in the lysosomes, in the same place that the amastigotesin the macrophages. Jiang et al. (2002) [75] showed thatomeprazole inhibits the K+, H+-ATPase enzyme located onthemembrane surface of Leishmania, and this drug had leish-manicidal activity against Leishmania donovani intracellularamastigotes in a dose-dependent manner.
In their study, Nilforoushzadeh et al. 2008 [26] reportedthat omeprazole (40 mg) plus intramuscular meglumineantimoniate (30 mg/kg/day) showed similar clinical cure

16 Dermatology Research and Practice
presented by meglumine antimoniate (60 mg/kg/day), beingit of 89% and 93%, respectively. Moreover, omeprazole(40 mg) plus intramuscular meglumine antimoniate (30mg/kg/day) showed greater clinical cure rate thanmeglumineantimoniate (30 mg/kg/day), being the cure rates of 89% and80%, respectively.
The combination omeprazole plus meglumine antimoni-ate was well tolerated and the authors reported no side effects,thus it may be a clinically useful alternative likely efficaciousfor CL treatment.
4.8. Cryotherapy. Cryotherapy is a therapeutic modality rec-ommended by the World Health Organization (WHO) forthe treatment of CL. According toWHO, it is a recommendedtreatment regimen for Old World CL, combined or not withintralesional antimonial [4].
Above all, some studies showed that the combinationof cryotherapy with intralesional pentavalent antimonial ismore effective than the antimonial alone [11, 76].
The three articles included in this review, conducted byVan-Thiel et al. (2010) [29], Meymandi et al. (2011) [10] andFarajzadeh et al. (2015) [32], presented a lower cure rate forthe combination of cryotherapy and intralesional sodiumstibogluconate or for the combination with meglumine anti-moniate.
Some variables should be taken into consideration for theperformance of cryotherapy, whichmay directly influence theefficacy of the treatment, such as the size of the lesion and thefrequency of the cryotherapy sessions. Papules smaller thanor equal to 1 cm, respondedmore quickly to cryotherapy thanlesions larger than 1 cm. According to Ranawaka et al. (2011)[77], for smaller papules the cure rate was 90.5% and for theones larger than 1 cm, it was 64.28%.
The frequency of sessions also seems to play an importantrole in the effectiveness of cryotherapy. When performedweekly, cure rates were high (equal or greater than 90%),either alone or in combination with pentavalent antimonials[8, 77]. Application at longer time intervals may result inlower cure rates. Soto et al. (2013) [78] performed only twosessions of cryotherapy at intervals greater than 1 week andobtained a low cure rate (20%).
Another important fact to consider before the applicationof cryotherapy is the phototype of skin. In patients withphototype V, for example, depigmentation may occur. It isalso necessary to investigate the tendency of keloid formation[77].
Cryotherapy is a clinically useful alternative and has few,but not serious, adverse effects. It has a high cure rate whenconsidering the size of the lesion and the frequency of thesessions.
4.9. Ketoconazole. Ketoconazole is an antifungal that inter-feres with the biosynthesis of ergosterol, an important cellmembrane constituent, essential for the viability and survivalof fungi and trypanosomatids. The target of Ketoconazoleis the C14𝛼-demethylase and, thus, it interferes with thedimethylation of the sterol and, consequently, inhibits thesynthesis of ergosterol [79].
Oral ketoconazole alone has been tested for the treatmentof CL for several years and has shown different cure rates[80–83]. In this review, we included the study of El-Sayedand Anwar (2010) [21], which tested the combination ofintralesional sodium stibogluconate and oral ketoconazole(600 mg/day). This combination was more effective than theketoconazole and sodium stibogluconate alone.
Saenz et al. (1990) [80], using ketoconazole alone (600mg/day), obtained a cure rate of 73% and Salamanpour et al.(2001) [82] found a cure rate of 89% in the treatment withketoconazole (600 mg/day) alone.
Possibly the species is a determinant factor in the effi-cacy of ketoconazole. WHO recommends ketoconazole (600mg/day) as the treatment regimen for CL in the New World,specifically when the etiologic agent is Leishmania mexicana,although there are reports of its efficacy in other species [4].El-Sayed and Anwar (2010) [21] did not identify the speciesin their study. Saenz et al. (1990) [80] also did not identifyit, but their study was conducted in Panama. Salmanpouret al. (2001) [82] cited that the patients had Old World CL.Ramanathan et al. (2011) [83] demonstrated efficacy in thetreatment of CL by Leishmania panamensis. With respectto ketoconazole resistance, Andrade-Neto et al. (2012) [84]demonstrated that Leishmania amazonensis can up-regulatetheC-14 demethylase in response to ketoconazole, whichmaycontribute to its resistance to this drug.
Oral administration of ketoconazole combined withintralesional sodium stibogluconate for the treatment of CLis shown acceptable risk with specialized monitoring and noserious adverse effects and in administration are reported.
4.10. Pentoxifylline. Pentoxifylline is a derivative of dimethyl-xanthine classified as a vasodilator agent. It exerts effects ondifferent cell types, such as reduction of the expression ofadhesion molecules with ICAM- 1 in keratinocytes and E-selectin in endothelial cells, inhibition of TNF-𝛼 synthesis,IL-1 and IL-6 and antifibrinolytic effects [14, 85].
In particular, pentoxifylline may potentiate the actionof pentavalent antimonials primarily by two mechanisms:increase in the expression of the inducible nitric oxide syn-thase (iNOS) and, consequently, increase in the production ofnitric oxide, and anti-TNF-𝛼 action [86, 87]. Brito et al. (2014)[88] observed that patients treated with pentoxifylline (400mg - 3 times per day) combined withmeglumine antimoniate(20 mg5+/kg/day) had greater TNF-𝛼 suppression than thosetreated withmeglumine antimoniate alone (20mg5+/kg/day),and cure rates were higher in the combined group than in thesecond group.
Machado et al. (2007) [15] demonstrated in theirstudy that the combination of meglumine antimoniate (20mg5+/kg/day) and pentoxifylline (400 mg - 3 times per day)potentiated the effect of the meglumine antimoniate, sincethe combination resulted in 82% of cure in patients withmucosal leishmaniasis, while meglumine antimoniate (20mg5+/kg/day) alone had a cure rate of 41.6%. Sadeghian andNilforoushzadeh (2006) [17], in which this same combinationwas tested to treat cutaneous leishmaniasis (in endemic areaforLeishmaniamajor) and resulted in 81.3% cure versus 51.6%for meglumine antimoniate alone. In contrast, at the same

Dermatology Research and Practice 17
conditions in the cited studies, Brito et al. (2017) [31] reporteda cure rate of 43% for a combination of pentoxifylline andmeglumine antimoniate to treat cutaneous leishmaniasiscaused by Leishmania braziliensis, as divergences in cure ratesmay be related to intrinsic characteristics of each patient topentoxifylline, and the specie of Leishmania.
The anti-TNF-𝛼 action of pentoxifylline makes its useinteresting, mainly in cases of mucosal and/or treatment-refractory leishmaniasis, since this cytokine is the mainresponsible for mucosal damage. There have been reports ofsuccess in the combination of pentoxifylline and meglumineantimoniate in the treatment of treatment-refractory cases[14] and with high production of TNF-𝛼 [89] or recurrentcases [90].
For Lessa et al. (2001) [14], the efficacy of the combinationpentoxifylline and meglumine antimoniate should make itthe second choice in the treatment, since the administrationis oral and has fewer adverse effects than amphotericin B.
The efficacy of pentoxifylline in combination with meg-lumine antimoniate in the treatment of mucocutaneousleishmaniasis, even in cases refractory to conventional and/orrecurrent treatment, added to few and not severe effects,makes this combination a good therapeutic alternative clin-ically useful for treatment of mucocutaneous leishmaniasis.However to treat cutaneous leishmaniasis with this com-bination it is necessary to take into account the speciesinvolved, since in cases caused by Leishmania braziliensis thiscombination showed not efficacious and not useful.
4.11. Clinical Implications. The first choice drugs for thetreatment of cutaneous or mucocutaneous leishmaniasis donot always show the expected result, so the association ofthese conventional drugs with others drugs or modalities oftherapy, such as local therapies have good cure rates, oftenhigher than those of the drugs of choice, and few adverseeffects. Above all, the combination with immunomodulatorsseems to be promising, even with limited numbers studyand patient it was surprisingly effective, revealing higherefficacy and few adverse effects. In the case of combinationwith local application therapies, the diameter of the lesionappears to be an important factor for successful treatment.In addition to efficacy, many combinations are easy toadminister by the patient andwithout the need for specializedmonitoring, what represents an advantage for use in moreisolated communities.
4.12. Strengths and Limitations of the Study. This system-atic review has gone through many steps in its develop-ment. The precision in publications’ search was guaranteedby two databases. Publications’ identification criteria weremonitored and discussed in many steps of the research toguarantee robustness and rigor of the findings. Special carewas also taken for the identification of the MeSH terms,which were decided by many researchers and by consensus,providing good sensitivity and specificity. The publications’findings were organized and detailed in four tables for betterclarity and quality of data. Concerning the limitations, weidentified that only four of the 16 articles included in the
review highlighted the limitations topic (Llanos Cuentas etal. 2010; Khatami et al. 2013; Farajzadeh et al. 2015; Brito etal. 2017). Other limitations were the inclusion of only twodatabases, with publications merely in English comprisingthe period from 12/2004 to 6/2017. The considerable het-erogeneity between the articles included, mainly due to thesignificant variation of both the substances used and theresearch regions, made it impossible to analyze the data moreprecisely, for example through meta-analysis. Despite theselimitations, we believe the results can contribute positively forthe treatment of cutaneous leishmaniasis andmucocutaneousleishmaniasis.
5. Conclusion
The combination of pentavalent antimonial drugs with otherdrugs seems to be a good alternative to conventional treat-ment, since they presented good cure rates, often higher thanthose of the drugs of choice, and few adverse effects. There-fore, this type of combination deserves to be investigated inmore detail by clinical trials and prospective studies withmore robust population sample to reinforce the effectivenessand safety that this alternative treatment provides to thepatient.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Acknowledgments
The authors would like to thank the Conselho Nacionalde Desenvolvimento Cientıfico e Tecnologico and theCoordenacao de Aperfeicoamento de Pessoal de Nıvel Supe-rior for the financial support. A summary version of thiswork, with the same title, was presented orally at the VInternational Congress of the CCS held in Maringa, Brazil,in 2018.Therefore, the authors thank the congress organizingcommittee for this.
References
[1] WHO,Neglected tropical diseases, 2016, http://www.who.int/ne-glected diseases/news/WHO implement epidemiological sur-veillance leishmaniasis/en/.
[2] WHO, Leishmaniasis, 2017, http://www.who.int/mediacentre/factsheets/fs375/en/.
[3] J. Blum, D. N. Lockwood, L. Visser et al., “Local or sys-temic treatment for New World cutaneous leishmaniasis? Re-evaluating the evidence for the risk of mucosal leishmaniasis,”International Health, vol. 4, no. 3, pp. 153–163, 2012.
[4] World Health Organization, Control of the leishmaniases,World Health Organ Tech Rep Ser, 2010, http://apps.who.int/iris/bitstream/10665/44412/1/WHO TRS 949 eng.pdf.
[5] E. M. Andersen, M. Cruz-Saldarriaga, A. Llanos-Cuentas etal., “Comparison of meglumine antimoniate and pentamidinefor Peruvian cutaneous leishmaniasis,”The American Journal ofTropical Medicine and Hygiene, vol. 72, pp. 133–137, 2005.

18 Dermatology Research and Practice
[6] I. Kevric, M. A. Cappel, and J. H. Keeling, “New world and oldworld leishmania infections: a practical review,” DermatologicClinics, vol. 33, no. 3, pp. 579–593, 2015.
[7] G. A. S. Romero, M. V. De Farias Guerra, M. G. Paes, and V.De Oliveira Macedo, “Comparison of cutaneous leishmaniasisdue to Leishmania (Viannia) braziliensis and L. (V.) guyanensisin Brazil: therapeutic response to meglumine antimoniate,”TheAmerican Journal of Tropical Medicine and Hygiene, vol. 65, no.5, pp. 456–465, 2001.
[8] E. Negera, E. Gadisa, J. Hussein et al., “Treatment responseof cutaneous leishmaniasis due to Leishmania aethiopica tocryotherapy and generic sodium stibogluconate from patientsin Silti, Ethiopia,” Transactions of the Royal Society of TropicalMedicine and Hygiene, vol. 106, no. 8, pp. 496–503, 2012.
[9] N. Safi, G. D. Davis, M. Nadir, H. Hamid, L. L. Robert, andA. J. Case, “Evaluation of Thermotherapy for the Treatment ofCutaneous Leishmaniasis in Kabul, Afghanistan: A Random-ized Controlled Trial,”MilitaryMedicine, vol. 177, no. 3, pp. 345–351, 2012.
[10] S. Shamsi Meymandi, S. Zandi, H. Aghaie, and A. Hesh-matkhah, “Efficacy of CO
2laser for treatment of anthro-
ponotic cutaneous leishmaniasis, compared with combinationof cryotherapy and intralesional meglumine antimoniate,” Jour-nal of the European Academy of Dermatology and Venereology,vol. 25, no. 5, pp. 587–591, 2011.
[11] A. Asilian, A. Sadeghinia, G. Faghihi, and A. Momeni,“Comparative study of the efficacy of combined cryotherapyand intralesional meglumine antimoniate (Glucantime�) vs.cryotherapy and intralesional meglumine antimoniate (Glu-cantime�) alone for the treatment of cutaneous leishmaniasis,”International Journal of Dermatology, vol. 43, no. 4, pp. 281–283,2004.
[12] A. Asilian and M. Davami, “Comparison between the efficacyof photodynamic therapy and topical paromomycin in thetreatment of Old World cutaneous leishmaniasis: A placebo-controlled, randomized clinical trial,”Clinical and ExperimentalDermatology, vol. 31, no. 5, pp. 634–637, 2006.
[13] R. Reithinger, M. Mohsen, M. Wahid et al., “Efficacy ofThermotherapy to Treat Cutaneous Leishmaniasis Caused byLeishmania tropica in Kabul, Afghanistan: A Randomized,Controlled Trial,” Clinical Infectious Diseases, vol. 40, pp. 1148–1155, 2005.
[14] E. M. Carvalho,H. A. Lessa, F. Lima et al., “Successful treatmentof refractory mucosal leishmaniasis with pentoxifylline plusantimony.,” The American Journal of Tropical Medicine andHygiene, vol. 65, no. 2, pp. 87–89, 2001.
[15] P. R. Machado, H. Lessa, M. Lessa et al., “Oral pentoxifyllinecombined with pentavalent antimony: a randomized trial formucosal leishmaniasis,” Clinical Infectious Diseases, vol. 44, pp.788–793, 2007.
[16] L. Dastgheib, M. Naseri, and Z. Mirashe, “Both combined oralazithromycin plus allopurinol and intramuscular Glucantimeyield low efficacy in the treatment ofOldWorld cutaneous leish-maniasis: A randomized controlled clinical trial,” InternationalJournal of Dermatology, vol. 51, no. 12, pp. 1508–1511, 2012.
[17] G. Sadeghian and M. A. Nilforoushzadeh, “Effect of combina-tion therapy with systemic glucantime and pentoxifylline in thetreatment of cutaneous leishmaniasis,” International Journal ofDermatology, vol. 45, no. 7, pp. 819–821, 2006.
[18] L. Shamseer, D. Moher, M. Clarke et al., “Preferred report-ing items for systematic review and meta-analysis protocols
(prisma-p) 2015: Elaboration and explanation,” British MedicalJournal, vol. 349, Article ID g7647, 2015.
[19] R. P. Almeida, J. Brito, and P. L. Machado, “Successful treatmentof refractory cutaneous leishmaniasis with gm-csf and antimo-nials,” The American Journal of Tropical Medicine and Hygiene,vol. 73, no. 1, pp. 79–81, 2005.
[20] I. Arevalo, G. Tulliano, A. Quispe et al., “Role of imiquimodand parenteral meglumine antimoniate in the initial treatmentof cutaneous leishmaniasis,”Clinical Infectious Diseases, vol. 44,no. 12, pp. 1549–1554, 2007.
[21] M. El-Sayed and A. Anwar, “Intralesional sodium stiboglu-conate alone or its combination with either intramuscularsodium stibogluconate or oral ketoconazole in the treatment oflocalized cutaneous leishmaniasis: A comparative study,” Jour-nal of the European Academy of Dermatology and Venereology,vol. 24, no. 3, pp. 335–340, 2010.
[22] A. Llanos-Cuentas, W. Calderon, M. Cruz et al., “A clinicaltrial to evaluate the safety and immunogenicity of the LEISH-F1+MPL-SE vaccine when used in combination with sodiumstibogluconate for the treatment of mucosal leishmaniasis,”Vaccine, vol. 28, no. 46, pp. 7427–7435, 2010.
[23] C. Miranda-Verastegui, A. Llanos-Cuentas, I. Arevalo, B. J.Ward, and G. Matlashewski, “Randomized, double-blind clin-ical trial of topical imiquimod 5% with parenteral meglumineantimoniate in the treatment of cutaneous leishmaniasis inPeru,”Clinical Infectious Diseases, vol. 40, no. 10, pp. 1395–1403,2005.
[24] C. Miranda-Verastegui,G. Tulliano, T. W. Gyorkos et al., “First-line therapy for human cutaneous leishmaniasis in Peru usingthe TLR7 agonist imiquimod in combination with pentavalentantimony,” PLOS Neglected Tropical Diseases, vol. 3, no. 7, articlee491, 2009.
[25] E. Nascimento, D. F. Fernandes, E. P. Vieira et al., “A clinicaltrial to evaluate the safety and immunogenicity of the LEISH-F1+MPL-SE vaccine when used in combination with meglu-mine antimoniate for the treatment of cutaneous leishmaniasis,”Vaccine, vol. 28, no. 40, pp. 6581–6587, 2010.
[26] M. A. Nilforoushzadeh, F. Jaffary, N. Ansari, A. H. Siadat, Z.Nilforoushan, and A. Firouz, “A comparative study betweenthe efficacy of systemic meglumine antimoniate therapy withstandard or low dose plus oral omeprazole in the treatment ofcutaneous leishmaniasis,” Journal of Vector Borne Diseases, vol.45, no. 4, pp. 287–291, 2008.
[27] A. Khatami, R. Talaee, M. Rahshenas et al., “Dressings Com-bined with Injection of Meglumine Antimoniate in the Treat-ment of Cutaneous Leishmaniasis: A Randomized ControlledClinical Trial,” PLoS ONE, vol. 8, no. 6, 2013.
[28] A. Firooz, A. Khamesipour, M. H. Ghoorchi et al., “Imiquimodin Combination With Meglumine Antimoniate for CutaneousLeishmaniasis,” JAMA Dermatology, vol. 142, no. 12, 2006.
[29] P.-P. Van Thiel, T. Leenstra, H. J. De Vries et al., “Cutaneousleishmaniasis (Leishmania major infection) in Dutch troopsdeployed in Northern Afghanistan: Epidemiology, clinicalaspects, and treatment,” The American Journal of TropicalMedicine and Hygiene, vol. 83, no. 6, pp. 1295–1300, 2010.
[30] P. W. Nassif, T. F. P. De Mello, T. R. Navasconi et al., “Safetyand efficacy of current alternatives in the topical treatment ofcutaneous leishmaniasis: A systematic review,”Parasitology, vol.144, no. 8, pp. 995–1004, 2017.
[31] E. M. de Carvalho, L. H. Guimaraes, P. R. Machado et al.,“Oral Pentoxifylline Associated with Pentavalent Antimony: ARandomized Trial for Cutaneous Leishmaniasis,”The American

Dermatology Research and Practice 19
Journal of TropicalMedicine andHygiene, vol. 96, no. 5, pp. 1155–1159, 2017.
[32] S. Farajzadeh, I. Esfandiarpour, A. A. Haghdoost et al.,“Comparison between combination therapy of oral terbinafineand cryotherapy versus systemic meglumine antimoniate andcryother-apy in cutaneous leishmaniasis: A randomized clinicaltrial,” Iranian Journal of Parasitology, vol. 10, no. 1, pp. 1–8, 2015.
[33] M. A. Nilforoushzadeh, F. Jaffary, S. Moradi, R. Derakhshan,and E. Haftbaradaran, “Effect of topical honey application alongwith intralesional injection of glucantime in the treatment ofcutaneous leishmaniasis,” BMCComplementary andAlternativeMedicine, vol. 7, article 13, 2007.
[34] F. F. Tuon, V. S. Amato, M. E. Graf, A. M. Siqueira, A. C.Nicodemo, andV.A.Neto, “Treatment ofNewWorld cutaneousleishmaniasis - A systematic review with a meta-analysis,”International Journal of Dermatology, vol. 47, no. 2, pp. 109–124,2008.
[35] L. O. Neves, E. Priscilla, N. Gadelha et al., “A randomized clini-cal trial comparing meglumine antimoniate , pentamidine andamphotericin B for the treatment of cutaneous leishmaniasis byLeishmania guyanensis,” Anais Brasileiros de Dermatologia, vol.86, pp. 1092–1101, 2011.
[36] J. Soto, L. Valda-Rodriquez, J. Toledo et al., “Comparison ofgeneric to branded pentavalent antimony for treatment ofnew world cutaneous leishmaniasis,” The American Journal ofTropical Medicine and Hygiene, vol. 71, no. 5, pp. 577–581, 2004.
[37] L. Lopez, M. Robayo, M. Vargas, and ID. Velez, “Thermother-apy. An alternative for the treatment of American cutaneousleishmaniasis,” Trials, vol. 13, pp. 2–7, 2012, http://www.pub-medcentral.nih.gov/articlerender.fcgi?artid=3441257&tool=pmcentrez&rendertype=abstract.
[38] M. E. C. Dorval, E. T. Oshiro, E. Cupollilo, A. C. C. Castro, andT. P. Alves, “Ocorrencia de leishmaniose tegumentar americanano Estado do Mato Grosso do Sul associada a infeccao porLeishmania (Leishmania) amazonensis,” Journal of the BrazilianSociety of Tropical Medicine, vol. 39, no. 1, pp. 43–46, 2006.
[39] V. A. Laguna-Torres, C. A. C. Silva, D. Correia, E. M. Carvalhoet al., “Efficacy of mefloquine in the treatment of skin leishma-niasis in an endemic area of Leishmania (Viannia) braziliensis,”Revista da Sociedade Brasileira de Medicina Tropical, vol. 32,pp. 529–532, 1999, http://www.embase.com/search/results?sub-action=viewrecord&from=export&id=L29526793.
[40] N. E. Aronson, G. W. Wortmann, W. R. Byrne et al., “ARandomized Controlled Trial of Local Heat Therapy VersusIntravenous Sodium Stibogluconate for the Treatment of Cuta-neous Leishmania major Infection,” PLOS Neglected TropicalDiseases, vol. 4, no. 3, p. e628, 2010.
[41] M. Solomon, F. Pavlotzky, A. Barzilai, and E. Schwartz, “Lipo-somal amphotericin B in comparison to sodium stibogluconatefor Leishmania braziliensis cutaneous leishmaniasis in travel-ers,” Journal of the American Academy of Dermatology, vol. 68,no. 2, pp. 284–289, 2013.
[42] G.Wortmann, R. S. Miller, C. Oster, J. Jackson, andN. Aronson,“A Randomized, Double-Blind Study of the Efficacy of a 10-or 20-Day Course of Sodium Stibogluconate for Treatment ofCutaneous Leishmaniasis in United States Military Personnel,”Clinical Infectious Diseases, vol. 35, no. 3, pp. 261–267, 2002.
[43] M. I. F. Pimentel, E. D. C. F. e Vasconcellos, C. D. O. Ribeiroet al., “Intralesional treatment with meglumine antimoniatein three patients with new world cutaneous leishmaniasis andlarge periarticular lesions with comorbidities,” Journal of the
Brazilian Society of Tropical Medicine, vol. 50, no. 2, pp. 269–272, 2017.
[44] R. E. da Silva, A. Toledo Junior, M. C. Senna, A. Rabello, and G.Cota, “Intralesional meglumine antimoniate for the treatmentof localised cutaneous leishmaniasis: a retrospective review of aBrazilian referral centre,”Memorias do Instituto Oswaldo Cruz,vol. 111, pp. 512–515, 2016, http://www.scielo.br/scielo.php?script=sci arttext&pid=S0074-02762016000800512&lng=en&nrm=iso&tlng=en.
[45] E. D. C. Ferreira E Vasconcellos, M. I. Fernandes Pimentel,A. De Oliveira Schubach et al., “Intralesional meglumineantimoniate for treatment of cutaneous leishmaniasis patientswith contraindication to systemic therapy from Rio de Janeiro(2000 to 2006),”The American Journal of Tropical Medicine andHygiene, vol. 87, no. 2, pp. 257–260, 2012.
[46] E. D. C. F. e Vasconcellos, M. I. F. Pimentel, C. M. Valete-Rosalino, M. D. F. Madeira, and A. D. O. Schubach, “Resolutionof cutaneous leishmaniasis after acute eczema due to intrale-sionalmeglumine antimoniate,”Revista do Instituto deMedicinaTropical de Sao Paulo, vol. 56, no. 4, pp. 361-362, 2014.
[47] R. A. Bumb, N. Prasad, K. Khandelwal et al., “Long-termefficacy of single-dose radiofrequency-induced heat therapy vs.intralesional antimonials for cutaneous leishmaniasis in India,”British Journal ofDermatology, vol. 168, no. 5, pp. 1114–1119, 2013.
[48] R. R. Ranawaka and H. S. Weerakoon, “Randomized, double-blind, comparative clinical trial on the efficacy and safetyof intralesional sodium stibogluconate and intralesional 7%hypertonic sodium chloride against cutaneous leishmaniasiscaused by L. donovani,” Journal of Dermatological Treatment,vol. 21, no. 5, pp. 286–293, 2010.
[49] R. A. Bumb, R. D. Mehta, B. C. Ghiya et al., “Efficacy of short-duration (twice weekly) intralesional sodium stibogluconate intreatment of cutaneous leishmaniasis in India,” British Journalof Dermatology, vol. 163, no. 4, pp. 854–858, 2010.
[50] I. Ushach and A. Zlotnik, “Biological role of granulo-cyte macrophage colony-stimulating factor (GM-CSF) andmacrophage colony-stimulating factor (M-CSF) on cells of themyeloid lineage,” Journal of Leukocyte Biology, vol. 100, no. 3,pp. 481–489, 2016.
[51] J. B. Santos, A. R. De Jesus, P. R. Machado et al., “Antimonyplus recombinant human granulocyte-macrophage colony-stimulating factor applied topically in low doses enhances heal-ing of cutaneous leishmaniasis ulcers: A randomized, double-blind, placebo-controlled study,” The Journal of Infectious Dis-eases, vol. 190, no. 10, pp. 1793–1796, 2004.
[52] R. Almeida, A. D’Oliveira Jr., P. Machado et al., “Randomized,double-blind study of stibogluconate plus human granulocytemacrophage colony-stimulating factor versus stibogluconatealone in the treatment of cutaneous leishmaniasis,”The Journalof Infectious Diseases, vol. 180, no. 5, pp. 1735–1737, 1999.
[53] R. Badaro, I. Lobo, M. Nakatani et al., “Successful use of adefined antigen/GM-CSF adjuvant vaccine to treat mucosalLeishmaniasis refractory to antimony: A case report.,” TheBrazilian journal of infectious diseases : an official publicationof the Brazilian Society of Infectious Diseases, vol. 5, no. 4, pp.223–232, 2001.
[54] T. Dohert and R. L. Coffman, “Leishmania antigens pre-sented by GM-CSF-derived macrophages protect susceptiblemice against challenge with Leishmania majo,” The Journal ofImmunology, vol. 150, pp. 5476–5483, 1993.

20 Dermatology Research and Practice
[55] W. Y. Weiser, A. Van Niel, S. C. Clark, David. J. R. et al.,“Recombinant human granulocyte/macrophage colony-stimulating factor activates intracellular killing of Leishmaniadonovani by human monocyte-derived macrophages,” TheJournal of Experimental Medicine, vol. 166, pp. 1436–1446, 1987,http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2189637&tool=pmcentrez& rendertype=abstract.
[56] C. E.Weeks and S. J. Gibson, “Induction of Interferon andOtherCytokines by Imiquimod and Its Hydroxylated Metabolite R-842 in Human Blood Cells In Vitro,” Journal of InterferonResearch, vol. 14, no. 2, pp. 81–85, 1994.
[57] S. J. Gibson, L. M. Imbertson, T. L. Wagner et al., “CellularRequirements for Cytokine Production in Response to theImmunomodulators Imiquimod and S-27609,” Journal of Inter-feron & Cytokine Research, vol. 15, no. 6, pp. 537–545, 1995.
[58] E. Hanna, R. Abadi, andO. Abbas, “Imiquimod in dermatology:an overview,” International Journal of Dermatology, vol. 55, no.8, pp. 831–844, 2016.
[59] A. Weber, C. Zimmermann, A. K. Mausberg, B. C. Kie-seier, H. P. Hartung, and H. H. Hofstetter, “Induction ofpro-inflammatory cytokine production in thymocytes by theimmune response modifiers Imiquimod and Gardiquimod�,”International Immunopharmacology, vol. 17, no. 2, pp. 427–431,2013.
[60] J. Seeberger, S. Daoud, and J. Pammer, “Transient effect oftopical treatment of cutaneous leishmaniasis with imiquimod,”International Journal of Dermatology, vol. 42, no. 7, pp. 576–579,2003.
[61] S. Shamsi Meymandi, A. Javadi, S. Dabiri, M. Shamsi Mey-mandi, and M. Nadji, “Comparative histological and immuno-histochemical changes of dry type cutaneous leishmaniasisafter administration of meglumine antimoniate, imiquimod orcombination therapy,” Archives of Iranian Medicine, vol. 14, no.4, pp. 238–243, 2011.
[62] L. W. Toy and L. Macera, “Evidence-based review of silverdressing use on chronic wounds,” Journal of the AmericanAssociation of Nurse Practitioners, vol. 23, no. 4, pp. 183–192,2011.
[63] V. K. M. Poon and A. Burd, “In vitro cytotoxity of silver:implication for clinical wound care,” Burns, vol. 30, no. 2, pp.140–147, 2004.
[64] Hatmann, Atrauman � Ag – Questions and Answers Con-tent, https://export.catalog.hartmann.info/ph-images/content/img 27085 30.pdf.
[65] R. White, “Efficacy of silver-containing dressings.,” Journal ofWound Care, vol. 15, no. 9, pp. 417-418, 2006.
[66] M. S. Duthie, V. S. Raman, F. M. Piazza, and S. G. Reed,“The development and clinical evaluation of second-generationleishmaniasis vaccines,”Vaccine, vol. 30, no. 2, pp. 134–141, 2012.
[67] J. Chakravarty, S. Kumar, S. Trivedi et al., “A clinical trial toevaluate the safety and immunogenicity of the LEISH-F1+MPL-SE vaccine for use in the prevention of visceral leishmaniasis,”Vaccine, vol. 29, no. 19, pp. 3531–3537, 2011.
[68] I. D. Velez, K. Gilchrist, S. Martınez et al., “Safety and immuno-genicity of a defined vaccine for the prevention of cutaneousleishmaniasis,” Vaccine, vol. 28, no. 2, pp. 329–337, 2009.
[69] R. N. Coler, Y. Goto, L. Bogatzki, V. Raman, and S. G. Reed,“Leish-111f, a recombinant polyprotein vaccine that protectsagainst visceral Leishmaniasis by elicitation of CD4+ T cells,”Infection and Immunity, vol. 75, no. 9, pp. 4648–4654, 2007.
[70] P. Molan, “The evidence and the rationale for the use of honeyas a wound dressing,” Wound Practice & Research, vol. 19, pp.204–220, 2011.
[71] J. Majtan, “Honey: An immunomodulator in wound healing,”Wound Repair and Regeneration, vol. 22, no. 2, pp. 187–192, 2014.
[72] A. B. Jull, N. Walker, and S. Deshpande, “Honey as a topi-cal treatment for wounds,” Cochrane Database of SystematicReviews, vol. 8, no. 4, Article ID CD005083, 2013.
[73] S. K. Saikaly and A. Khachemoune, “Honey and WoundHealing: AnUpdate,”American Journal of Clinical Dermatology,vol. 18, no. 2, pp. 237–251, 2017.
[74] N. J. V. Bell and R. H. Hunt, “Role of gastric acid suppressionin the treatment of gastro-oesophageal reflux disease,”Gut, vol.33, no. 1, pp. 118–124, 1992.
[75] S. Jiang, J. Meadows, S. A. Anderson, and A. J. Mukkada,“Antileishmanial activity of the antiulcer agent omeprazole,”Antimicrobial Agents and Chemotherapy, vol. 46, no. 8, pp.2569–2574, 2002.
[76] A.Asilian, A. Sadeghinia, G. Faghihi,A.Momeni, andA. AminiHarandi, “The efficacy of treatment with intralesional meglu-mine antimoniate alone, compared with that of cryotherapycombined with the meglumine antimoniate or intralesionalsodium stibogluconate, in the treatment of cutaneous leishma-niasis,”Annals of Tropical Medicine and Parasitology, vol. 97, no.5, pp. 493–498, 2003.
[77] R. R. Ranawaka, H. S. Weerakoon, and N. Opathella, “Liquidnitrogen cryotherapy on Leishmania donovani cutaneous leish-maniasis,” Journal of Dermatological Treatment, vol. 22, no. 4,pp. 241–245, 2011.
[78] J. Soto, E. Rojas, M. Guzman et al., “Intralesional antimonyfor single lesions of Bolivian cutaneous Leishmaniasis,” ClinicalInfectious Diseases, vol. 56, no. 9, pp. 1255–1260, 2013.
[79] W. de Souza, J. Cola, and F. Rodrigues, “Sterol BiosynthesisPathway as Target for Anti-trypanosomatid Drugs,” Interdisci-plinary Perspectives on Infectious Diseases, vol. 2009, Article ID642502, 19 pages, 2009.
[80] R. E. Saenz, H. Paz, and J. D. Berman, “Efficacy of ketoconazoleagainst Leishmania braziliensis panamensis cutaneous leishma-niasis,” American Journal of Medicine, vol. 89, no. 2, pp. 147–155,1990.
[81] O. Ozgoztasi and I. Baydar, “A randomized clinical trial oftopical paromomycin versus oral ketoconazole for treatingcutaneous leishmaniasis in Turkey,” International Journal ofDermatology, vol. 36, no. 1, pp. 61–63, 1997.
[82] R. Salmanpour, F.Handjani, andM.K. Nouhpisheh, “Compara-tive study of the efficacy of oral ketoconazole with intra-lesionalmeglumine antimoniate (glucantime) for the treatment ofcutaneous leishmaniasis,” Journal of Dermatological Treatment,vol. 12, no. 3, pp. 159–162, 2001.
[83] R. Ramanathan, K. R. Talaat, D. P. Fedorko, S.Mahanty, andT. E.Nash, “A species-specific approach to the use of non-antimonytreatments for cutaneous leishmaniasis,”The American Journalof Tropical Medicine andHygiene, vol. 84, no. 1, pp. 109–117, 2011.
[84] V. V. Andrade-Neto, H. L. de Matos-Guedes, D. C. D. O.Gomes, M. M. do Canto-Cavalheiro, B. Rossi-Bergmann, andE. C. Torres-Santos, “The stepwise selection for ketoconazoleresistance induces upregulation of C14-demethylase (CYP51)in Leishmania Amazonensis,” Memorias do Instituto OswaldoCruz, vol. 107, no. 3, pp. 416–419, 2012.
[85] O. Zargari, “Pentoxifylline:A drugwith wide spectrumapplica-tions in dermatology,” Dermatology Online Journal, vol. 14, no.11, article no. 2, 2008.

Dermatology Research and Practice 21
[86] K. H. N. Hoebe, N. Gonzalez-Ramon, S. M. Nijmeijer et al.,“Differential effects of pentoxifylline on the hepatic inflamma-tory response in porcine liver cell cultures increase in induciblenitric oxide synthase expression,” Biochemical Pharmacology,vol. 61, no. 9, pp. 1137–1144, 2001.
[87] M. Ahmadi and H. Khalili, “Potential benefits of pentoxifyllineonwoundhealing,”Expert Review of Clinical Pharmacology, vol.9, no. 1, pp. 129–142, 2016.
[88] P. R. Machado, M. Dourado, G. Brito et al., “Clinical andImmunological Outcome in Cutaneous Leishmaniasis PatientsTreated with Pentoxifylline,” The American Journal of TropicalMedicine and Hygiene, vol. 90, no. 4, pp. 617–620, 2014.
[89] A. Bafica, F. Oliveira, L. A. R. Freitas, E. G. Nascimento, andA. Barral, “American Cutaneous Leishmaniasis unresponsive toantimonial drugs: Successful treatment using combination ofN-methilglucamine antimoniate plus pentoxifylline,” Interna-tional Journal of Dermatology, vol. 42, no. 3, pp. 203–207, 2003.
[90] C. M. Gomes, F. D. S. Damasco, O. O. de Morais, C. D. R. dePaula, and R. N. R. Sampaio, “Recurrent cutaneous leishmani-asis,” Anais Brasileiros de Dermatologia, vol. 88, no. 3, pp. 462–464, 2013.

Stem Cells International
Hindawiwww.hindawi.com Volume 2018
Hindawiwww.hindawi.com Volume 2018
MEDIATORSINFLAMMATION
of
EndocrinologyInternational Journal of
Hindawiwww.hindawi.com Volume 2018
Hindawiwww.hindawi.com Volume 2018
Disease Markers
Hindawiwww.hindawi.com Volume 2018
BioMed Research International
OncologyJournal of
Hindawiwww.hindawi.com Volume 2013
Hindawiwww.hindawi.com Volume 2018
Oxidative Medicine and Cellular Longevity
Hindawiwww.hindawi.com Volume 2018
PPAR Research
Hindawi Publishing Corporation http://www.hindawi.com Volume 2013Hindawiwww.hindawi.com
The Scientific World Journal
Volume 2018
Immunology ResearchHindawiwww.hindawi.com Volume 2018
Journal of
ObesityJournal of
Hindawiwww.hindawi.com Volume 2018
Hindawiwww.hindawi.com Volume 2018
Computational and Mathematical Methods in Medicine
Hindawiwww.hindawi.com Volume 2018
Behavioural Neurology
OphthalmologyJournal of
Hindawiwww.hindawi.com Volume 2018
Diabetes ResearchJournal of
Hindawiwww.hindawi.com Volume 2018
Hindawiwww.hindawi.com Volume 2018
Research and TreatmentAIDS
Hindawiwww.hindawi.com Volume 2018
Gastroenterology Research and Practice
Hindawiwww.hindawi.com Volume 2018
Parkinson’s Disease
Evidence-Based Complementary andAlternative Medicine
Volume 2018Hindawiwww.hindawi.com
Submit your manuscripts atwww.hindawi.com