PARA PNEUMONIC EFFUSION
-
Upload
aslam-calicut -
Category
Health & Medicine
-
view
2.714 -
download
2
description
Transcript of PARA PNEUMONIC EFFUSION

PARA PNEUMONIC EFFUSION
Dr MUHAMMED ASLAM
PG RESPIRATORY MEDICINE

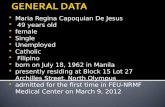
• A parapneumonic effusion is a type of pleural effusion that arises as a result of a pneumonia, lung abscess, or bronchiectasis

CLASSIFICATION
• Uncomplicated (UPPE)• Complicated (CPPE)• Empyema thoracis

Uncomplicated parapneumonic effusions• Exudative, predominantly neutrophilic effusions reflecting
increasing passage of interstitial fluid as a result of inflammation associated with pneumonia.
• cloudy or even clear, without any organisms noted on Gram stain or culture.
• They resolve with appropriate antibiotic treatment of the pneumonia.

Complicated Parapneumonic effusions• Bacterial invasion into the pleural space • Increased number of neutrophils, decreased glucose
levels, pleural fluid acidosis, and an elevated lactic dehydrogenase (LDH)
• Often are sterile. • Classified as complicated because it requires drainage
for resolution.

Empyema thoracis
• Frank pus accumulates in the pleural space

Etiology
• Bacterial, viral,Atypical • Aerobic gram-positive –S pneumoniae
Staphylococcus aureus , streptococcus milleri
• Aerobic gram-negative Klebsiella,Pseudomonas, E coli, and Haemophilus
• Anaerobic -Bacteroides and Peptostreptococcus • Patients with pneumonia due to Legionella species

Pathophysiology
3 stages• Exudative• Fibrinopurulent• Organization stages.

Exudative stage
• The pleural fluid originates in the interstitial spaces of the lung and in the capillaries of the visceral pleura because of increased permeability.
• Sterile pleural fluid • Low WBC count and LDH level• Glucose and pH levels are normal• Resolve with antibiotic therapy, and chest tube insertion
is not required.• 2-5 days from the onset of pneumonia.

Fibrinopurulent stage
• Bacterial invasion of the pleural space • Accumulation of neutrophils, bacteria, and cellular
debris. • A tendency toward loculation and septation • pleural fluid pH (< 7.20) and glucose levels are lower (<
60 mg/dL), and the LDH level increases.• Bacteriological stains or cultures of the pleural fluid can
be positive for microorganisms. • 5-10 days after pneumonia onset.

Organization stage
• Fibroblasts grow into the exudates from both the visceral and parietal pleural surfaces and forms inelastic membrane called pleural peel.
• Pleural fluid is thick.• In an untreated patient, pleural fluid may drain
spontaneously through the chest wall (empyema necessitatis).
• Take 2-3 weeks to develop.


Risk factors for Empyema thoracis
• Age -children and elderly persons• Debilitation• Bronchiectasis• Rheumatoid arthritis• Alcoholism• Diabetes • Gastroesophageal reflux disease • Intravenous drug abuse

Clinical manifestations
• Depend on aerobic or anaerobic infection. • Aerobic infections are more acute in onset • Anaerobic infections can be indolent

Aerobic
• Patients present with an acute febrile illness with chest pain, cough with sputum production, and dyspnoea.
• A complicated parapneumonic effusion is suggested by the presence of a fever lasting more than 48 hours after the initiation of antibiotic therapy.

Anaerobic bacterial infection
• Usually subacute illness.• Most have symptoms for more than 7 days• a/i Poor oral hygiene,alcoholism, and factors predispose
to recurrent aspiration.

ON EXAMINATION
• Febrile with Tachypnea and tachycardia• Decreased tactile fremitus and VR• Dullness to percussion• Decreased or absent breath sounds• Tracheal shift possible with large effusions• In areas in which pneumonia and lung consolidation are
adjacent and more extensive than pleural fluid-crackles ,bronchial breath sounds ,egophony.

INVESTIGATIONS
• BLOOD-leukocytosis may be present (>12,000/µL• Sputum for Gram stain &culture. • ***

Chest radiography
• PA , Lateral and Decubitus view
***

Chest radiograph of a 63-year-old woman withleft lower lobe pneumonitis

The patient developed a large leftsidedpleural effusion despite 5 days of oral antibiotic therapy

Ultrasonography
• Localize fluid for a thoracentesis• Distinguish loculated pleural fluid from an infiltrate.

Sonographic study of the pleural space showed marked septation throughout the fluid collection

CT Thorax
• Pleural enhancement can be seen in patients with active inflammation
• “split pleura sign”• Distinguish pleural from parenchymal abnormalities • Determine the precise location and extent• Detect loculations • Find airway and parenchymal abnormalities that may be
relevant to the etiology of the pleural infection.

split pleura sign

Thoracentesis
• When parapneumonic pleural effusion is greater than or equal to 10 mm thick on a lateral decubitus chest radiograph

Pleural fluid
• Appearance -clear yellow liquid to an opaque turbid fluid to grossly purulent thick, viscous, foul-smelling pus(anaerobic infection).
• WBC count• Total protein• LDH• Glucose• pH• Microbiology

Complicated pleural effusion or empyema
• LDH value of greater than 1000 U/L • Glucose level of less than 40 mg/d • pH of less than 7.20.


Staging
Category 1 (parapneumonic effusion)• Minimal free-flowing fluid, smaller than 10 mm on
decubitus films• Culture, Gram stain, and pH unknown• No thoracentesis needed; treatment with antibiotics
alone

Category 2 (uncomplicated parapneumonic effusion)
• Larger than 10 mm fluid and less than half the hemithorax on decubitus films
• Gram stain and culture negative• pH higher than 7.20• Treatment with antibiotics alone

Category 3 (complicated parapneumonic effusion)• Large free-flowing effusion, more than half the
hemithorax• pH lower than 7.20, LDH level greater than 1000 U/L and
glucose level less than 40 mg/dL• Gram stain or culture positive• Treatment with tube thoracostomy and antibiotics• Multiloculated effusions may require multiple tubes• Thrombolytics may help resolution

Category 4 (empyema)
• Large free-flowing effusion, greater than equal to half the hemithorax
• Loculated effusion or effusion with thickened pleura• Gross pus on aspiration• Treatment with tube thoracostomy• Thrombolytics may help resolution• May require decortication

TREATMENT
• selection of an appropriate antibiotic • Assessment of need for drainage of pleural fluid

ANTIBIOTIC SELECTION
• Community-acquired pneumonia : second- or third-generation cephalosporins in addition to a macrolide.
• severe community-acquired pneumonia-initiate treatment with a macrolide plus a third-generation cephalosporin with antipseudomonal activity.
• If aspiration is evident or suspected, oral anaerobes should also be covered.

• In the absence of a positive gram stain, coverage
for Legionella species and Chlamydia pneumoniae should be added
• For nosocomial infections, broader antibiotic coverage
for gram-negative organisms is recommended

Duration of antibiotic therapy
• antibiotics are continued until: • (1) the patient is afebrile and the white blood cell count is
normal; • (2) the tube thoracostomy drainage yields less than 50
ml of fluid daily• (3) the radiograph shows considerable clearing.
• Typically, 3 to 6 weeks of antibiotic therapy is required to• achieve these results.

Pleural space drainage.
• If the diagnostic thoracentesis yields thick pus( empyema thoracis ) definitive pleural drainage is required.
• If the pleural fluid is not thick pus, then results of pleural fluid Gram stain or culture, pleural fluid pH and glucose levels, and the presence or absence of pleural fluid loculations should guide the course of action

Indications for drainage
• Prolonged pneumonia symptoms, co morbid disease• Failure to respond to antibiotic therapy• Presence of anaerobic organisms • Chest radiograph –Effusion involving >50% of the
hemothorax , loculation, and an air-fluid level.

• Aspiration of pus, a putrid odor associated with an anaerobic infection, a positive Gram stain or culture result, pH <7.20, a glucose level <40 mg/dL, and an LDH level >1000 IU/L
• USG-Stranding or septation• CT-marked pleural enhancement, pleural thickening, and
the split pleura sign

Pleural space drainage
• Repeated thoracentesis• Use of a standard chest tube• An image-guided insertion of a small-bore catheter.

Intrapleural thrombolytic agents
• Most effective in the early fibrinolytic stage• streptokinase,streptodornase,urokinase, and tPA
Indications • occluded small-bore catheter,• multiloculated pleural space • as a trial before committing the patient to surgery.

Surgical Care
• Thoracoscopy, • Video-assisted thoracic surgery (VATS), • Standard thoracotomy• Open drainage

Indication
• When Tube thoracostomy has been ineffective in controlling the pleural infection.
• Empyema that has been present for several days to weeks and that has multiple loculations
• Patients with impaired pulmonary function and debilitation can be treated effectively with VATS

Open Thoracotomy
• Recommended for persistent pleural sepsis and failure of less invasive procedures
• When VATS cannot adequately access the pleural space• optimal method for successful debridement and
decortication. • Decortication (i.e., stripping of the visceral pleural peel)
can be performed early to control pleural sepsis and late (3–6 months after the onset of empyema or CPPE) to treat a symptomatic, restrictive ventilatory defect.

Nutrition
• Patients with empyema enter a catabolic state ; hence ,good nutrition is vital

Conclusions
• The outcome of a PPE depends on the point in the clinical course when the patient presents to the physician, co morbidities, and efficient clinical management.
• Early antibiotic therapy prevents the development of a PPE and progression to a CPPE and empyema.

Thank You