NS 335 – Special Populations Unit 2 Seminar – GI Tract, Liver, Gallbladder, and Pancreas.
-
Upload
ira-norman -
Category
Documents
-
view
217 -
download
1
Transcript of NS 335 – Special Populations Unit 2 Seminar – GI Tract, Liver, Gallbladder, and Pancreas.

NS 335 – Special PopulationsNS 335 – Special Populations
Unit 2 Seminar – GI Tract, Liver, Gallbladder, and Pancreas

The GI SystemThe GI System
The gastrointestinal (GI) tract extends from the mouth to the anus.
All disturbances related to food intake, digestion, absorption, and elimination affect the GI tract and usually require special diets.

Mirror the Human ConditionMirror the Human Condition
Psychological factors play a role when we consider disorders of the GI tract.
The digestive system is said to “Mirror the Human Condition”
Stress factors such as anxiety, fear, work pressure, grief, emotional makeup, and coping patterns have a great deal to do with how foods are tolerated.
Physiological factors can also be related with intolerances (such and an enzyme deficiency) which will eliminated foods that can be eaten

Let’s Play a Game!!Let’s Play a Game!!
What type of DisorderAm I??

How To PlayHow To Play I will give you a word scrambled with a brief
description of the disorder it is
“Buzz in” by typing a # into the chat box.
Wait until I call on you to type in your response.
The first person to correctly identify the type of assessment wins that question

If you’re ready, let’s get started!
Remember to “buzz in” by typing in a # into the chat

Name the DisorderName the Disorder
reutfacdr ajw-Has high nutritional needs-May have to be wired which causes problems eating-Diet needs of high calorie, high protein, vitamins,
and minerals is needed to promote healing-Liquid must pass through a straw without causing it
to move

Diet for a Fractured JawDiet for a Fractured Jaw
Breakfast: Strained Juice, Hot Blended Drink, Coffee, Beverage of Choice
Lunch: Fruit Drink, Hot Blended Drink, Coffee, Beverage of Choice
Dinner: Fruit Eggnog, Hot Blended Drink, Beverage of Choice
Table 17-1 of Text

Name the DisorderName the Disorder
dlatne ierasc-A lot of this problem comes from dietary in nature-Lack of Calcium, Phosphorus, Fluorine, and Vitamins
A, D, and C affect tooth and gum formation and development
-Can occur with infants with milk, juice, or sweetened drinks left in a bottle against an infant’s gums during sleep.

Name the DisorderName the Disorder
fectl pilA congenital defect of newbornsCan be corrected with a series of
surgeries after the infant reaches a weight safe enough to withstand a surgical procedure

Cleft Lip / Cleft PalateCleft Lip / Cleft Palate
These infants have high nutritional requirements to prepare for surgery and rapid growth

pticpe uecrl Most common of the problems affecting the upper
GI tract Causative factors include:1) Increased acidity and secretion of gastric juices2) Decreased secretion of mucous linings and buffers3) Prolonged use of nonsteroidal anti-inflammatory
drugs (NSAIDs) such as aspirin, ibuprofen, and others.
4) Helico pylori (H. pylori) infection.
Name the DisorderName the Disorder

Peptic UlcerPeptic Ulcer
Treatment goals: relieve pain, heal erosion, prevent complications, prevent recurrences
Drug therapies are used Diet Therapy:1) Follow regular diet with guidelines based on the
individual2) 3 meals daily without snacks, especially at bedtime3) Moderate meal size4) No need to eliminate a food unless it causes
discomfort5) No fiber restriction

Peptic Ulcer ContinuedPeptic Ulcer Continued
6) Determine individual tolerances (seasonings, alcohol, coffee adjustments)
7) General recommendations to avoid aspirin, quit smoking, try antidepressant medications, initial diet modification

Name that DisorderName that Disorder
taiahl irnaeh-This results when the stomach partially protrudes
above the diaphragm because of the weakening of the diaphragm opening

Hiatal HerniaHiatal Hernia
Usually treated with antacids and a low-fat diet
6 small meals a day are recommended and fluids are taken between meals
Foods that irritate esophageal mucosa are eliminated

Gastric Surgery for Ulcer Gastric Surgery for Ulcer DiseaseDisease
Perforation and hemorrhage are two major complications of ulcer disease for which surgery are indicated.
Dumping syndrome

Dumping SyndromeDumping Syndrome
Food reaches the jejunum 10 to 15 minutes after eating
With part of the stomach removed, the food is not digested properly and instead of being delivered slowly, it is “dumped” quickly into the small intestine

Dumping SyndromeDumping Syndrome
Foods prohibited: Breads with nuts, jams, or dried fruits made with bran, presweetened cereals, highly seasoned or smoked meats, if not tolerated-milk, alcohol, carbonated beverages; creamed or gas forming vegetables, fruits canned with sugar syrup, sweetened dried fruits, pickles, peppers, chili powder, nuts, olives, candy, milk gravy

QUESTIONS??

ConstipationConstipation
Involves many variables with its treatment
A regular, high fiber balanced diet and adequate fluid intake is recommended

DiarrheaDiarrhea
Can be serious if prolonged
Treatment involves eliminating the underlying cause, using antidiarrheal drugs as needed and appropriate diet therapy

Diverticular DiseaseDiverticular Disease
DiverticulosisVs.
Diverticulitis

IBDIBD
Inflammatory Bowel Disease - a term used for ulcerative colitis and Chron’s disease

Ulcerative ColitisUlcerative Colitis
Characterized by widespread ulceration and inflammation of the colon, fever, chronic bloody diarrhea, edema, and anemia.
Diet therapy includes: Regular, high fiber diet supplemented with formula feeding as
tolerated High Protein diet: 120-150 grams daily High Calorie: 3000 calories daily High vitamins/minerals, especially vitamins C, B Complex, and
K Moderate fat as tolerated Dairy products usually eliminated to avoid secondary lactose
intolerance or lactose free products used IV fluids in addition to oral feedings TPN is most effective if the bowel has been shortened or the
disease is extensive.

Chron’s DiseaseChron’s Disease
Present in industrial areas and the 50-60 year old age group.
It has onset characterized by tenderness, pain, diarrhea, and cramping in the right lower quadrants of the bowel. There is less blood in the stool than in ulcerative colitis, but more mucous secretions by the bowel.
Widespread problems of malabsorption of fat, protein, carbohydrates, vitamins, minerals, and subsequent weight loss.

Chron’s DiseaseChron’s Disease
Treatment: Drug Therapy: Several types of medications are used to
control inflammation or reduce symptoms caused by ulcerative colitis.
Anti-inflammatory -These drugs are often the first step in the treatment of ulcerative colitis. Most ulcerative colitis patients have mild to moderate cases, which are treated with medications containing mesalamine.
Immune system suppressors-Immunosuppressives (drugs that suppress the immune system) treat ulcerative colitis by blocking inflammation.
Surgery

Diet Therapy for Diseases of the
Liver

HepatitisHepatitis
Viral hepatitis- inflammation of the liver
Diet Therapy:Protein: 1.2-1.5 gm/kg BW per dayNo CHO restriction, but may need to
monitor Glu levels resulting from liver dysfunction

Hepatitis Diet Therapy Hepatitis Diet Therapy ContinuedContinued
Fat: 30% of calories Energy: 25-35 kcals/kg BW Multivitamin used Fluids and Sodium Restriction if edema or
ascites present. If adequate nutrition cannot be maintained
by oral feedings, enteral or TPN are appropriate.

CirrhosisCirrhosis
Cirrhosis is the final stage of certain liver injuries including alcoholism, untreated hepatitis, biliary obstruction, Vitamin A overdose, and drug and poison ingestion.

Diet Therapy for CirrhosisDiet Therapy for Cirrhosis
Protein: If hepatic coma is not indicated, protein remains at 75-100g daily. If the patient shows signs of impending coma, protein intake should be reduced to lessen the chance of coma.
Sodium: Edema or ascites is counteracted by a 500-1000 mg sodium diet daily. Fluid restriction may be limited.
Texture- Esophageal varices, if present, are managed by semisolid or liquid diets to avoid potential rupture and hemorrhage. TF not recommended. Coffee, tea, pepper, chili powder, and other irritating seasonings should be avoided.

Hepatic EncephalopathyHepatic Encephalopathy
Diet therapy includes:Protein intake limited to 0 to 50g protein daily, depending on blood ammonia level.Calories: 1500-2000 calories daily mainly from carbohydrate and fatVitamins – Given IVFluid- Output is balanced by equal intakeTPN or enteral nutrition are standard forms of diet therapy

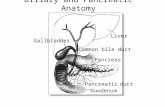
The GallbladderThe Gallbladder
Cholecystitis
Cholelithiasis

Diet Therapy for Gallbladder Diet Therapy for Gallbladder DiseaseDisease
Dietary fat is reduced to diminish gallbladder contraction, which is responsible for pain and associated symptoms. Reduced to 40-50g/day.
Protein comprises 10-12% of total daily calories.
Calories reduced if weight loss indicated. These modifications are generally used
before surgery/cholecystectomy.

Diet Therapy for Acute Diet Therapy for Acute PancreatitisPancreatitis
1)Initial measures are lifesaving-IV and TPN feedings, replacement of fluid and electrolytes, blood transfusions, and drugs for pain and inhibiting gastric secretions. Nothing given by mouth.
2)As healing progresses, the first oral diet usually consists of clear liquid with amino acids, predigested fats, and other commercial preparations added gradually. The patient progresses to a bland diet, given in 6 small meals. No stimulants: coffee, caffeine, tea, colas, alcohol are allowed.

Diet Therapy for Chronic Diet Therapy for Chronic PancreatitisPancreatitis
Diet therapy for chronic pancreatitis usually consists of a bland diet of soft or regular consistency in small meals at frequent intervals (6 feedings) and contains no stimulant foods. Pancreatic enzymes are given usually with food. Alcohol is strictly forbidden.
1) Low fat diet2) Vitamin and Mineral supplementation may be
necessary3) Tube feedings or TPN may be necessary

QUESTIONS??