NEW OPPORTUNITIES IN CHRONIC CARE MANAGEMENT … · multiple chronic conditions under CPT code...
Transcript of NEW OPPORTUNITIES IN CHRONIC CARE MANAGEMENT … · multiple chronic conditions under CPT code...

A white paper brought to you by
Copyright 2017 Symphony CareNavigate, LLC - All Rights Reserved. SymphonyCare™ and Navigate™ are trademarks of Symphony CareNavigate, LLC
NEW OPPORTUNITIES IN CHRONIC CARE MANAGEMENT
What 2017 CMS Changes Mean for Providers Navi

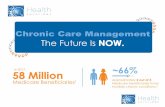
While the movement toward a fee-for-value model in healthcare is old news, exciting new developments in chronic care management (CCM) are beginning to take shape wherein healthcare providers can get reimbursed in more traditional ways for performing tasks associated with improved outcomes and overall, long-term cost reductions.
Center for Medicare & Medicaid (CMS) established CPT®* code 99490 in 2015 to pay for up to 20 minutes each month to manage the care for patients with multiple chronic conditions. As of November of 2016, CMS reports that about 513,000 unique Medicare beneficiaries received any such services under the new CCM code. This constitutes a small fraction of the estimated tens of millions of eligible Medicare patients.
In 2017, CMS has made the opportunity far more enticing for providers to increase value-based payments through CCM services by expanding the group of reimbursable services under new CCM-based codes, as well by relaxing some of the requirements for such reimbursement. As a result, providers have plenty of opportunities to benefit from expansion of valuable CCM services through their staff or through competent partners.
* - CPT codes, descriptions and other data only are copyright 2016 American Medical Association. All Rights Reserved. Applicable FARS/HHSAR apply. CPT only copyright 2016 American Medical Association. All rights reserved. CPT is a registered trademark of the American Medical Association. Applicable FARS\HHSAR Restrictions Apply to Government Use. Fee schedules, relative value units, conversion factors and/or related components are not assigned by the AMA, are not part of CPT, and the AMA is not recommending their use. The AMA does not directly or indirectly practice medicine or dispense medical services. The AMA assumes no liability for data contained or not contained herein.

NEW OPPORTUNITIES IN CHRONIC CARE MANAGEMENT
3
BACKGROUNDIn January of 2015, the Centers for Medicare & Medicaid Services (CMS) started a program to reimburse healthcare providers for delivering non-face-to-face care to patients with multiple chronic conditions under CPT code 99490. As of November of 2016, only 513,000 Medicare beneficiaries have had a chronic care management (CCM), which could be as low as 1% of all beneficiaries eligible for such services¹.
Healthcare providers should recognize the opportunity set forth by CMS for CCM services deemed important for the management of Medicare patients with multiple chronic diseases. The secular trends begin to paint the picture. Pew Research population projections indicate that more than 10,000 Baby Boomers will turn 65 every day until 2029, and by 2030 when the last of Baby Boomers cross the Medicare age threshold, over 18% of the US population will be over 65². According to MEPS survey data in 2010, over 80% of all patients over 65 years old suffer from multiple chronic conditions, and this percentage is likely to get worse before it gets better³.
The CCM opportunity continues to brighten by evolving CMS programs to pay providers monthly reimbursements tied to delivering key servies to chronically ill patients in order to improve health outcomes and reduce avoidable healthcare costs. When the program began in 2015, the CCM-centric reimbursements were limited to CPT 99490, which at the time averaged roughly a $41 per patient per month reimbursement for 20 minutes of non-face-to-face chronic care management. However, 2017 changes also incorporate additional reimbursements for what is considered “complex CCM” and additional time spent on such cases. These changes, in addition to some relaxed requirements regarding care planning and care plan access, make CCM programs far more enticing and realizable for providers.
1 “Physician Groups Split on Chronic Care Pay in Medicare Rule,” by Andis Robeznieks, HFMA, Nov. 7, 20162 “Baby Boomers Retire,” by Russell Heimlich, Pew Research Center, Dec. 29, 20103 “Multiple Chronic Conditions Chartbook: 2010 MEPS Data,” AHRQ, 2010
80%Percentage of Americans 65 or older with multiple chronic conditions

NEW OPPORTUNITIES IN CHRONIC CARE MANAGEMENT
4
OPPORTUNITY: CPT 99490In January of 2015, CMS rolled out its CCM program aimed at paying providers for care management activities that are known to achieve better health outcomes and avoid unnecessary healthcare expenditures. The linchpin in this program was CPT code 99490, which paid providers roughly $41 per patient per month for 20 or more minutes of non-face-to-face chronic care mangement to Medicare patients with multiple chronic conditions.
REMAINING CHALLENGESWhile some providers did indeed take advantage of CPT code 99490 to bill for nearly $93 million⁴ in reimbursable CCM services, this accounts for only 1% of the eligible Medicare beneficiaries. Through 2016, several barriers remained that prevented most providers from taking advantage of this opportunity to improve health outcomes and boost quality scores. As shown in the table below, several barriers prevent the smooth, efficient roll-out of a CCM program.
4 “Physician Groups Split on Chronic Care Pay in Medicare Rule,” by Andis Robeznieks, HFMA, Nov. 7, 2016
Economics
Compliance
Awareness
A one-size-fits-all approach contained under a single CPT code, paying on average (and no more than) $41 per month for even highly complex cases, is economically unfeasible for many providers
Many providers are concerned about meeting all of the original 2015 requirements regarding technology, access, billing, and workflow
Many providers are unaware of the details surrounding the original CCM provisions, to speak nothing of the evolving nature of these requirements

NEW OPPORTUNITIES IN CHRONIC CARE MANAGEMENT
5
NEW OPPORTUNITIES IN 2017 AND BEYONDThe new year has brought the easing of the CCM billing rules and expanded payment codes for CCM services. These new CMS policies not only open up new reimbursement opportunities, and thus making CCM programs economically viable, but they also ease compliance concerns that left many providers still relcutant to engage in ambitious initiatives out of fear that they could still fall short. As a result, healthcare providers should strongly consider implementing a robust CCM program to take adavntage of the more favorable politicies. In the following sections we will explore some of those changes in greater detail, as well as highlight some key next steps for providers in taking full advantage of these opportunities.
Recent CMS changes address the often-daunting requirements place on providers, which have hindered the widespresad adoption of productive CCM programs. The table below summarizes some of the important changes in rules for 2017 that simplify the CCM process for healthcare providers, making such a program far more feasible, and potentially expanding the reach of existing programs.
Simplified CCM Processes
2016 Rules
Consent Form with patient’s signature required for provider to bill for CCM services
24/7 access to the care plan within the practice and immediately available electronically outside the practice
Face-to-face initiating visit must be conducted by the billing physician prior to enrollment
Continuity of care document must be formatted according to certified EHR requirements
No such formatting required of the clinical summaries for continuity of care
NO face-to-face visit required unless a new patient or a patient has not seen in past 12 months
Care plan delivery must be timely but can be made via fax both within and without the practice
NO Consent Form required, instead only verbal agreement recorded within the medical record
2017 Rules

NEW OPPORTUNITIES IN CHRONIC CARE MANAGEMENT
6
Just as important, if not more so, than the eased administrative and technical requirements are the new CPT codes for complex CCM, which help facilitate more realistic care for complex patients who are at greatest risk for hospitalization. The increased reimbusement will also contribute to more appropriate care management for these patients, as providers now enjoy more adequate incentive to roll out far-reaching CCM programs through existing clinical staff or in partnership with subcontractors. As a conseqeunce, instead of an average non-facility reimbursement of $41 for CCM, providers can now reimburse anywhere from $43 to upwards of $141 in non-facility payments for patients qualifying for CCM services. The table below shows the addition of CPT code 99487 for complex CCM, as well as CPT 99489 for additional time spent on a complex CCM case.
Expanded CPT Code Reimbursement for Complex CCM
CPT Code 2016 Payment
2017 Payment
99490
99487
99489
$41
-
-
$43
$94
$47
CCM
Complex CCM
Complex CCM Add-on
20 minutes or more of clinical staff time in qualifying services
60 minutes of clinical staff time in qualifying
services
Each additional 30 minutes of clinical staff
time
Clinical Staff Time
Providers may wonder what percentage of their populations are eligible for complex CCM services, and CMS helps out with their own definition of CCM-eligible patients:
Multiple (two or more) chronic conditions expected to last at least 12
months, or until the death of the patient
Chronic conditions place the patient at significant risk of death, acute
exacerbation/decompensation, or functional decline
•
•“

NEW OPPORTUNITIES IN CHRONIC CARE MANAGEMENT
7
Establishment or substantial revision of a comprehensive care plan
Moderate or high complexity medical decision making
Reimbursement for Care Plan Development
Coverage for Prolonged Evaluation & Management
While there is no one-size-fits-all percentage of complex CCM-eligible patients across populations, 2010 MEPS data shows that over 80% of patients 65 or older suffer from multiple chronic conditions. Not all of these patients with multiple chronic conditions will be considered complex by the other aspects of the definition, but certainly many of them will. And, importantly, providers are likely already delivering complex CCM to those patients whether they are being reimbursed fairly or not; fortunately, CMS is starting to recognize the extensive work necessary to care for this at-risk population.
CMS has also acknowledged the difficulty in developing care plans for CCM programs without reimbursements tied directly to these activities. As a result, CMS now allows reimbursement to pay providers for care development under a new code named GPPP7. Importantly, this code is billed in addition to any monthly payments for primary services related to CCM and complex CCM, and is reimbursed at a non-facility rate of $63.68. While often tied to an initiating visit for CCM services, this code can also be billed for patients who require extensive face-to-face assessment and care planning from the billling practitioner.
While CMS reimburses providers for clinical staff performing CCM and complex CCM services, this does not include time spent by physicians. Without recognition of evaluation and management (E/M) time spent by physicians, CCM programs can become either ineffective or economically unfeasible. Recognizing this, CMS will now reimburse prolonged E/M services for two CPT codes, which helps take into account the non-face-to-face E/M activities enacted by physicians. The table below describes the CPT codes and their facility and non-facility reimbursements.
CPT 99358 for the first hour of prolonged E/M service before and/or after direct patient care: $113.41
CPT 99359 for each additional 30 minutes of prolonged E/M service before and/or after direct patient care $54.38
•• ”

NEW OPPORTUNITIES IN CHRONIC CARE MANAGEMENT
8
SUMMARY OF NEW 2017 OPPORTUNITIESIn summary, the changes in 2017, brought on by CMS’s recognition of the difficulty in providing proper care to complex patients with multiple chronic conditions, will make a profound impact on the ability of providers to deliver needed care, as shown with an example in the table below.
2016
2017
Making a robust CCM program
far more sustainable$41 per month for
CCM
$141 for 90 minutes of complex CCM
$168 for 90 minutes of E/M
$63.68 for care planning
Eased requirements
•
•
•
•
Use Case for Complex CCM Patient for One YearAs a more tangible example, consider the following scenario, which is also broken down in the longitudinal view on the following page: A complex CCM patient provided 60 minutes of non-face-to-face complex CCM services for eight months of the year*, as well as 60 minutes of E/M quarterly, and an extensive annual care planning session. This scenario, which is highly realistic for a complex CCM patient, and includes no “add-on” time billing, represents over $1,487 in reimbursements from CMS over the course of 12 months, versus the roughly $492 for 12 months of CCM previously allowed under CPT code 99490.
* - Per CMS rules, prolonged E/M services and complex CCM services cannot be billed in the same calendar month

CPT 99358
Prolonged E/M
Care Planning
Complex CCM
Total of roughly $1,487 in annual per-patient reimbursements*in this realistic, if not conservative, scenario for a complex CCM patient
CPT 99490 alone allowed for a maximum $492 annually
GPPP7
CPT 99487 $94 $94 $94 $94 $94 $94 $94 $94
$64
$113 $113 $113 $113
Jan Feb Mar Apr May Jun Jul Aug Sep Oct Nov Dec
NEW OPPORTUNITIES IN CHRONIC CARE MANAGEMENT
9* - Per CMS rules, prolonged E/M services and complex CCM services cannot be billed in the same calendar month
2017

NEW OPPORTUNITIES IN CHRONIC CARE MANAGEMENT
10
NEXT STEPSWhen take as a whole, these changes for 2017 provide a great opportunity for healthcare providers to offer these services, either through their own staff or through a competent subcontractor. Aside from imminent reimbursement opportunities, CCM and complex CCM have been shown to improve health outcomes and reduce overall costs of care. Also, since these valuable services are now reimbursed more fairly under a traditional fee-for-service model, CCM programs serve as a viable bridge toward the future of value-based healthcare models.
Care Plan
Continuity of Care
Medication Management
24/7 Care
Care Transitions
Patient & Provider Access
Comprehensive care plan that includes updated records from patients and their providers
A care team to coordinate care, manage interventions, and schedule appointments
An emphasis on med recon to combat misuse and non-adherence of medication
Access to clinical staff 24 hours a day, seven days a week, for urgent medical needs
Centralized clinical staff that manages transitions from all providers using proper technology
Access to information and communications tools to interact regarding patient care
For an effective program, CMS lays out guidelines and requirements that place an emphasis on care coordination and proper use and access of information through technology systems.
While care management isn’t somethign new for 2017, the fact remains that only roughly 1% of Medicare patients have been reached by these reimbursable services since 2015. While the eased requirements and new reimbursement opportunities will help, providers will need help in executing key workflow, workforce, and technology activities. For this reason, now more than ever it is important for providers to rely on key strategic partners who can help provide key guidance with supportive technology, as well as extend care management services to supplement existing staff.

NEW OPPORTUNITIES IN CHRONIC CARE MANAGEMENT
11
Schedule a Navigate Demo
Visit Us on the Web
Call Us Today
THE SYMPHONYCARE CCM SOLUTIONSymphonyCare offers a complete CCM solution through partnership with healthcare providers, ACOs, and health plans to take on the technology and workflow challenges associated with CCM programs, including:
SEE WHAT SYMPHONYCARE CAN DO FOR YOU
Award-winning⁵ Navigate platform for population health management and patient engagement
http://www.symphonycare.com/contact
http://www.symphonycare.com
(608) 294-4090
Clinical staff and operations management with deep knowledge of care management workflow and winning patient engagement strategies
Full-service CCM options paired with technology, or hybrid approaches to match your goals and needs
Care coordination activities around the clock, seven days a week
Program-level management of population cohorts and ongoing monitoring of CCM requirements for program viability and reimbursement at the claim level
Incentives aligned with your interests by tying our fees directly to reimbursement for CCM and complex CCM activities
•
•
•
••
•
5 Navigate Recognized by Frost & Sullivan in 2016 with the Patient Engagement Enabling Technology Leadership Award











![Skin Inflammation, [Acute, Suppurative, Chronic, Chronic ... · Skin – Inflammation, [Acute, Suppurative, Chronic, Chronic Active, Granulomatous] presence of mononuclear cells (lymphocytes,](https://static.fdocuments.net/doc/165x107/5f0eb0c97e708231d44075f1/skin-inflammation-acute-suppurative-chronic-chronic-skin-a-inflammation.jpg)






