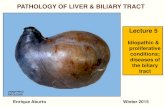
NEOPLASMS OF EXTRA HEPATIC BILE DUCTS · NEOPLASMS OF THE EXTRA HEPATIC BILE DUCTS By ANDREW M....
Transcript of NEOPLASMS OF EXTRA HEPATIC BILE DUCTS · NEOPLASMS OF THE EXTRA HEPATIC BILE DUCTS By ANDREW M....

june 1951 DESMOND: Neoplasms of the Extra Hepatic Bile Ducts 277
brother nor father with son nor mother withdaughter, nor would neighbour break bread withneighbour. There was no kindness among us, butmisery and -unhappiness. In the streets unkind-ness one to another; at home anguish, seeingchildren crying for bread and others dying'(' Chronicle of Novgorod,' A.D. I230). In theIrish famine in the middle of the last centuryDonovan described a father engaging in a life anddeath struggle with his son for the sake of apotato. Loss of all the normal standards of mor-ality under the impact of undernutrition has beendescribed again and again in history, and there isno reason to suppose it would be any different today.The population of the world is increasing at an
alarming rate. India and China are on the vergeof starvation today, and countries such as England,with a population greater than the land canpossibly support, may be called upon at any timethrough war or even through the operation of thenormal laws of economics to face a period of under-nutrition and perhaps worse. Mankind has theknowledge and ability to prevent all this, but willhe do it ? Those horsemen of the Apocalypse aregrim figures and they are galloping round theworld just as furiously today as they were at theend of the Isth century. They have lived longerthan the saints and we can only hope that as theysweep on they will not be allowed to ravage anddestroy as they would like to do.
NEOPLASMS OF THE EXTRA HEPATICBILE DUCTS
By ANDREW M. DESMOND, F.R.C.S.Consultant Surgeon, St. James's Hospital, Balham
The object of this communication is to drawattention to certain neoplasms occurring in theextra-hepatic biliary duct system, and it is basedon a small series of cases treated with varyingresults. The anatomical region involved is shownin Fig. i, to which is appended the relative fre-quency of occurrence at each site as notpd byRolleston and McNee (1929). Neoplasms of thegall bladder itself are not discussed, neither arethose tumours referred to as carcinomata of theampulla of Vater, although there is good evidenceto suggest that many of these cancers have theirorigin in the lower end of the common bile duct.The neoplasms under discussion are frequentlyvery small and localized, and may not be recognizedduring a laparotomy for obstructive jaundice unlessthe surgeon is aware of their occurrence.
Anatomical ConsiderationsThe hepatic ducts issue from the liver and unite
to forn the common hepatic duct often only a fewmillimetres from the liver substance, so thatneoplasms arising from them involve the liver at an'arly stage and early become inoperable.
The common hepatic duct usually has a separateexistence for 2 to 3 cm. before being joined by thecystic duct to form the common bile duct, so thatit is possible that a small neoplasm could be ex-cised with restoration of duct continuity. It willbe seen (Fig. i) that the greatest proportion oftumours arise at the junction of the cystic andcommon hepatic ducts and would require at leasta cholecystectomy and partial choledochotomy.The common bile duct is approximately 7 cm.
long and consists of an easily accessible supra-duodenal portion and a retroduodenal part, whichmay or may not be embedded in the substance ofthe pancreatic head. Tumours of the supra-duodenal portion could be treated by local ex-cision, but removal of a retroduodenal one wouldprobably necessitate a wedge pancreatectomy orpreferably a radical pancreatico-duodenectomy.The lymphatics of the bile ducts drain into the
hepatic glands related to the stem of the hepaticartery and extending into the porta hepatis. Thecystic duct lymphatics drain into the cystic glandnear the neck of the gall bladder, though thisgland may also drain the other biliary channels as
by copyright. on N
ovember 25, 2020 by guest. P
rotectedhttp://pm
j.bmj.com
/P
ostgrad Med J: first published as 10.1136/pgm
j.27.308.277 on 1 June 1951. Dow
nloaded from

POSTGRADUATE MEDICAL JOURNAL
illustrated in Case 6. Efferents from all theseglands pass to the coeliac group.
Histologically the ducts consist of an outerlayer of fibro-areolar tissue containing some circu-lar muscle fibres, and an inner mucous membraneof'columnar epithelium with lobulated mucousglands.
Pathological ConsiderationsThese tumours may be benign or malignant.
BenignChristopher (1933) collected 4I cases of benign
tumour of the extra-hepatic bile ducts from theliterature; i6 were -papillomata, 15 adenomata,4 lipomata,' 2 fibromata, i neuroma, i granuloma,i melanoma and i carcinoid. He himself reeportdone further adenoma. All the patients weremiddle aged or over and presented with obstruc-tive jaundice. Cattell and Pyrtek (1950) reportedtwo further papillomata which were successfullytreated by transduodenal resection. Below is re-ported a further personal case of papilloma (Case8). There seems to be some evidence that thesebenign tumours are the precursors of the malignantones, and both types may occur in the same patient(Case 6). Cattell and Pyrtek make a most con-vincing case for their belief that in four of theircases a carcinoma in the ampullary region arosefrom an adenoma 'or papilloma.
MalignantIt is perhaps fortunate that the occurrence of
carcinoma in these narrow bile channels results inthe onset of a serious symptom, i.e. jaundice, at anearly stage, so that the patient may submit himselffor treatment before extensive metastases havedeveloped. If, therefore, itfcan be shown thatthese growths are of low malignancy, a local asopposed to a radical resection may suffice with acorresponding lower operative mortality.
Opinion seems to be divided on this point.Dick (1939), reporting I3 cases discovered atautopsy, stated that in i i of these there was no.extension outside the duct wall, nor was there anyevidence of glandular or other metastases. Thetumours were adenocarcinomata with very littleanaplasia, the acini being well formed althoughirregular and with darkly staining nuclei. Mitoseswere unusual and the stroma dense. The tumourswere small (0.4 to 2.0 cm.) and tended to be in-filtrative rather than proliferative. They wereconfined to a small area or extended diffusely overa length of duct 2 cm. or more.A diametrically opposite view is expressed by
Brunschwig (1948) who states that the tumoursare commonly anaplastic and very malignant, theprognosis being uniformly bad. Willis (I948) in
his series of I 5 autopsy cases also found them tobe relatively benign and metastases infrequent.Gordon-Taylor (I942), however, described a casein which he removed a tumour of the lower endof a very dilated bile duct, but the patient diedfrom metastases in one year.
All these views are, of course, correct, for mostcarcinomata exist in relatively benign and malig-nant forms, but the personal experience of any oneclinician of a rare condition of this type will tendto give him a biased opinion. From a review ofthe literature, however, I have formed the im-pression that the majority are of low malignancy.In the present series also this has been true.Unlike carcinomata of the gall bladder, the co-existence of gall stones in these cases appears tobe the exception rather than the rule.
Clinical ManifestationsThe presenting symptom is usually progressive,
painless, obstructive jaundice with pale stools anddark urine. There may be a history of flatulentdyspepsia. In two of our cases colicky pain andchills heralded the onset of the jaundice andcommon bile duct calculus was suspected. Thejaundice in the benign lesions may be less pro-gressive and tend to vary, the reason for this beingwell demonstrated in Fig. 8, which shows 'how thetumour may act as a ball valve.
Apart from jaundice and perhaps some wasting,the only physical sign may be a palpable gallbladder. This will, of course, depend on theposition of the lesion. A tumour above thecystico-hepatic junction is associated with a col-lapsed gall bladder. If at the cystico-hepaticjunction the gall bladder will be distended withmucus, if below this point it will be distended withbile or mucus (' white bile ').
Radiography is of doubtful value and patho-logical investigations may confirm the obstructivenature of the jaundice, but ate necessary inassessing liver function. The exact diagnosis isthus determined only at laparotomy.At operation the identification of the lesion is of
paramount importance. The duct systems mustbe brought into view and reliance must not beplaced on palpation alone. To facilitate this, acomplete Kocher's mobilization of the duodenummust be carried out. With the assistant gentlyholding the duodenum over to the left, an incisionis made into the peritoneum on the lateral aspectof the duodenum, where apart from a few minuteveins, it is bloodless. The fingers are then passedextraperitoneally behind the duodenum and headof pancreas and a bloodless plane of cleavage can befound between the pancreas and the posteriorabdominal wall, which extends well over to the leftof the duodeno-jejunal flexure. When the
-278 -zone I1951I
by copyright. on N
ovember 25, 2020 by guest. P
rotectedhttp://pm
j.bmj.com
/P
ostgrad Med J: first published as 10.1136/pgm
j.27.308.277 on 1 June 1951. Dow
nloaded from

DE,SNIOND: N(oplasmis of the Extra Hepatic Bile Ducts
duodenum and pancreas have blecii raised foriwardit will be seen that the peritoneum on the lateraland inferior aspects of the third and fourth partsof the duodenum is also bloodless and that whenit is divided the pancreas can be drawn forwardand rotated to the left, bringing into view the wholeretroduodenal portion of the common bile ductand the ampuillary region.
Case ReportsThe first two cases are very briefly described to
demonstrate the hopeless prognosis of carcinomaof the hepatic ducts.
Case I
R.E1., male, aged 65 years. A medical man.April 1949. Complained of flatulent dyspepsia,
anorexia and constipation. During the course ofthe next few weeks he became increasinglyjaundiced.
July 1949. A laparotomy was performed else-where and the communicated findings were asfollows: ' The gall bladder was large but could beemptied easily by pressure. The head of thepancreas was hard but not neoplastic. A diagnosisof chronic pancreatitis was made and cholecyst-duodenostomy performed.' The jaundice failedto clear and in fact deepened.
August 1949. Transferred to St. James'sI lospital.September 1949. Laparotomy. There was a
large carcinoma of the hepatic ducts which ex-tended well into the liver substance at the portahepatis. Choledochotomy was performed and alittle white bile was extruded. Both hepatic ductswere blocked and could not be dilated. Thepatient died ten days later.
Case 2F.G., male, aged 65 years. A cellarman.May I945. Onset of painless progressive
jaundice with dark urine and pale stools. The liverwas enlarged but smooth and the gall bladder wasnot palpable. Pathological investigations con-firmed the obstructive nature of the jaundice.June I945. Laparotomy revealed a collapsed
gall bladder and high in the porta hepatis was amalignant mass extending into the liver substanceand appearing to arise from the common hepaticduct. Choledochotomy was performed but at-tempts to dilate the ducts failed. The abdomenwas closed.He was discharged from hospital but died very
shortly afterwards.
The following two cases were unfit for primaryresection of the growth and cholecyst-gastrostomy
FIG. I.-Diagram of the extrahepatic bile ductsshowing the relative frequency of neoplasmsoccurring within them (Rolleston and McNee,1929).
was performed as a first stage, but both died beforethe second stage could he performed.
Case 3S.C., male, aged 79. A mental defective who
had been in a mental institution for many years-.June I950. Transferred to St. James's Hospital.For ten weeks progressive painless jaundice and
loss of weight.
71),,/I 1951 279
by copyright. on N
ovember 25, 2020 by guest. P
rotectedhttp://pm
j.bmj.com
/P
ostgrad Med J: first published as 10.1136/pgm
j.27.308.277 on 1 June 1951. Dow
nloaded from

POSTGRADUATE MEDICAL JOURNAL
FIG. 2.-Carcinoma just below the cystico-hepatic junction (Case 3).
On examination a feeble mentally defective oldman, deeply jaundiced. Abdomen revealed alarge smooth liver and a palpable gall bladder.Pathological investigations confirmed the obstruc-tive nature of the jaundice and demonstrated poorliver function. After a course of vitamin K andintravenous protein replacement a laparotomy wasperformed under general anaesthesia. The gallbladder was distended with white bile. Therewere no stones. The common hepatic duct wasgrossly dilated. There was a carcinoma of thesupra-pancreatic portion of the common bile ductextending up to the cystico-hepatic junction. Acholecyst-gastrcrtomy was performed.
Post-operatively the patient progressed well fora few days, but suppression of urine supervenedand he died on the tenth day. The findings atautopsy are shown in Fig. 2. There was no
evidence of glandular or other metastases. Themicroscopic section showed a well-differentiatedadenocarcinoma of the bile duct extending out-wards to, but not involving, the head of thepancreas.
Case 4D.R., male, aged 86. A mental defective who
had been in an institution for many years.June I950. Transferred to St. James's Hospital.April 1950. He had a sudden attack of ab-
dominal pain, vomiting and chills. He had be-come progressively weaker since this time and forfour weeks had become progressively morejaundiced with pale stools and dark urine. He hadno further attacks of pain but had lost weight.On examination. A feeble old man with severe
chronic bronchitis and emphysema. He was
2.80 fine 1951
by copyright. on N
ovember 25, 2020 by guest. P
rotectedhttp://pm
j.bmj.com
/P
ostgrad Med J: first published as 10.1136/pgm
j.27.308.277 on 1 June 1951. Dow
nloaded from

28IDE!SMOND: Neoplasms of the Extra Hlepatic Bile Ducts
FIG. 3.-Artist's impression of specimen from Case 4 showing growth in supra-duodenal portion of common bile duct.
deeply jaundiced. The abdomen was somewhatdistended and there was some free fluid. The liverwas palpable but the gall bladder could not befelt. Investigations confirmed the obstructive
nature of the jaundice and demonstrated poorliver function.
After a course of vitamin K and intravenousprotein replacement a laparotomy was carried out
YI11C' I1951I
by copyright. on N
ovember 25, 2020 by guest. P
rotectedhttp://pm
j.bmj.com
/P
ostgrad Med J: first published as 10.1136/pgm
j.27.308.277 on 1 June 1951. Dow
nloaded from

POSTGRADUATE Mi\ElIDICAL JOURNAL
Fic;. I.-JExcised portion of common bile duct(X 2l,1) containing at carcinom-a from Case 5.
under local anaesthesia. There was soife strawcoloured free fluid in the peritoneal cavity. Thegall bladder was enlarged and tensely distendedwith clear mucus. There were no stones. A hardtumour was felt in the region of the head of thepancreas but the patient's general condition pre-cluded a more extensive search. A cholecyst-gastrostomy was performed and the wound closed.
Following operation he had suppression ofurine and became comatose after 48 hours anddied on the third post-operative day. The findingsat autopsy are shown in Fig. 3. There was noevidence of glandular or other metastases. Themicroscopic section showed a well-differentiatedadenocarcinoma of the bile duct with local in-vasion of the pancreas over a small area.
Case 5A successful local resection of a carcinoma of the
infraduodenal duct.M.K., a female, aged 6o, was admitted in January
i950 with jaundice. For several months she hadcomplained of epigastric discomfort a few minutesafter meals, made worse by fatty foods. There hadbeen some loss of weight. Six weeks previouslyshe had had an attack of shivering and pain in theright subcostal region. For four weeks she hadbecome increasingly jaundiced with pale stools anddark urine.On examination she was deeply jaundiced but
nutrition was good. The abdomen was obese andthe liver palpable and tender, but the gall bladderwas not felt. Pathological investigations confirmedthe obstructive nature of the jaundice and revealednormal liver function.
After a course of vitamin K a laparotomy wasperformed. The gall bladder was enlarged andtensely distended by a mixture of mucus and bile,and contained one stone. The suprapancreatic
FIG. 5. End in side choledocho-jejunostomy withlateral entero-enterostomv.
bile ducts were grossly dilated. The head of thepancreas was palpably normal. The duodenumand pancreatic head were freely mobilized and acarcinoma of the bile duct about 2.5 cm. from theampulla was found. The pancreas was not in-
282 37tunt, 195s I
by copyright. on N
ovember 25, 2020 by guest. P
rotectedhttp://pm
j.bmj.com
/P
ostgrad Med J: first published as 10.1136/pgm
j.27.308.277 on 1 June 1951. Dow
nloaded from

Je'DESMOND: Neoplasms o the Extra Hepatie Bile Ducts I83
*. .t:...*. .. AXi i..: ci .:
i::
..i... .. ..i:
..... : @..: ..
.. .:::.: :.:
t-- --- a -
E El--l-!
:, .-i :;- -:
.;: ::.. , , - . ....: i:,:: ;.. ... : : : .::
.. :}:
j. .: ..
.. ...; ::.. ..
FIG. 6.-End to end choledocho-jejunostomy with entero-anastomosisen Roux.
volved and there were no metastases. 'T'he bileduct was easily freed from both duodenum andpancreas, some brisk haemorrhage being con-trolled by suture. A portion of the bile ductabout 2.5 cm. long containing the growth was re-sected (Fig. 4). The distal duct was ligated andan end-in-side choledocho-jejunostomy was per-formed over a tube. A wide lateral anastomosisbetween the two jejunal loops was made (Fig. S),and the operation completed by performing acholecystostomy and removing the gall stone.Rutherford-Morrison's pouch was drained througha stab wound.
Convalescence was uneventful and the patientwas discharged one month later. Microscopicsection showed a well-differentiated adenocar-cinoma confined to the bile duct.
In April an X-ray showed that the tube hadpassed although the patient had no knowledge ofthis. At the follow-up in January I95I she waswell and had put on weight, and there was noevidence of recurrence.
In Case 6 a primary resection was performedbut the patient developed suppression of urine anddied.
C.T., aged 68, a medical man, was admitted inAugust 1950 with painless jaundice.He was transferred from another hospital with a
vague history of nausea and anorexia for a fewweeks followed by the gradual development ofjaundice. 'There had been considerable weightloss. 'I'he stools were pale and the urine dark.On examination he was thin and jaundiced. His
mental state was peculiar, with an intense cancero-phobia, and he constantly threatened to take hisown life. 'lThe gall bladder was easily palpable.I'atlhological investigations confirmiied the obstruc-
GAiLL SLAOOER --O
.....T. L. N.D
FiG. 7.-Resected specimen from Case 6.
by copyright. on N
ovember 25, 2020 by guest. P
rotectedhttp://pm
j.bmj.com
/P
ostgrad Med J: first published as 10.1136/pgm
j.27.308.277 on 1 June 1951. Dow
nloaded from

41OSTGRADUATrE MEIDICAL JOURNALJ
FIG. 8.-Artist's impression of resected specimen from Case 8.
tive nature of the jaundice and revealed poor liverfunction. Barium meal was essentially normal.
After a course of vitamin K and high proteinand carbohydrate diet a laparotomy was performed.The gall bladder was enlarged and tensely dis-tended with a mixture of bile and mucus. A masswas felt in the region of the lower end of the bile
duct and the duodenum and pancreas were freelymobilized, revealing a carcinoma of the lower endof the common bile duct. The cystic gland wasenlarged and hard. The gall bladder, cystic gland,cystic duct and lower part of the common hepaticduct were mobilized and removed with the wholecommon bile duct and a wedge of pancreas ob-
284 YaIDI 1 951I
by copyright. on N
ovember 25, 2020 by guest. P
rotectedhttp://pm
j.bmj.com
/P
ostgrad Med J: first published as 10.1136/pgm
j.27.308.277 on 1 June 1951. Dow
nloaded from

DESMOND: Neoplasms of the Extra Hepatic Bile Ducts
viously involved by growth. Brisk pancreatichaemorrhage was controlled by suture. Anend-to-end choledocho-jejunostomy was made andthe proximal jejunum anastomosed end-in-side tothe distal (Roux) (Fig. 6).The resected specimen is shown in Fig. 7.
The microscopic section showed a well-differ-entiated adenocarcinoma of the common bile duct.There was a dense fibrous stroma. The carcinomahad spread beyond the confines of the duct wallto involve the head of the pancreas over a smallarea. In Hartmann's pouch was a benign papil-loma. The cystic gland contained secondarydeposits.
Following operation the patient developed com-plete suppression of urine and in spite of alltreatment died on the fourth day. Autopsy re-vealed no evidence of metastases.The prognosis in these cases is difficult to
assess as there are very few reports in the literatureof successful resections followed up for a longperiod. The following case throws some light onthis problem as she died from recurrence fot ryears after local resection. The growth was moreextensive and a pancreatico-duodenectomy mighthave resulted in a happier outcome. The longsurvival, however, does illustrate the relativelybenign nature of some of the growths.
Case 7A.L., a female, aged 56, was admitted in July
1941 with painless progressive jaundice of twoweeks' duration, with pale stools and dark urine.The gall bladder was palpable. Pathological in-vestigations confirmed the obstructive nature ofthe jaundice and revealed good liver function.
After a preliminary course of vitamin K alaparotomy was performed. The gall bladder wasenlarged and tensely distended with clear bile.There was a small mass in the head of the pan-creas. A first stage cholecyst-gastrostomy wasperformed.The jaundice cleared up and one month later
the abdomen was re-opened. Mobilization of theduodenum and pancreatic head revealed a car-cinoma of the lower end of the bile duct involvingthe head of the pancreas and the duodenal wall.A wedge of tissue consisting of a portion of pan-creas, the common bile duct, a section of theduodenal wall and one hepatic lymphatic glandwas removed. The duodenum was sutured andthe proximal end of the bile duct ligated. Post-operatively a pancreatic fistula developed, whichdrained for five weeks and then healed.
Microscopic section showed a well-differentiatedadenocarcinoma of the bile duct involving pan-creas and duodenum. Resection appeared to be
well clear of the growth. 'The gland containedmetastases.The patient remained well until February I945
when she began to lose weight. She then de-veloped gross steatorrhoea and osteoporosis, anddied in June 1945. At post-mortem there was arecurrent growth in the pancreatic head andmetastases in the liver and kidneys.The last case is the report of a successful
pancreatic resection for a papilloma of the ampullaof VTater.
Case 8W.A., a male, aged 6i, an estate agent, was
admitted in July 1950 with a history of four weeksflatulent dyspepsia, increasing jaundice, palestools and dark urine.
Examination showed a deeply jaundiced man.The gall bladder was palpable. Pathological in-vestigations confirmed the obstructive nature ofthe jaundice and revealed good liver function.After a preliminary course of vitamin K a laparo-tomy was performed. It was noticed on themorning of the day of operation that the jaundicewas beginning to fade.The gall bladder and common bile duct were
not dilated. A hard, small tumour was felt in theregion of the ampulla of Vater and was consideredto be an early carcinoma. A pancreatico-duo-denectomy was performed, the duodeno-jejunalflexure not being removed. An end-in-sidecholedocho-jejunostomy over a tube and a gastro-jejunostomy were made. A safety valve chole-cystostomy was performed. The pancreatic stumpwas oversewn and embedded. The wound wasclosed with drainage; bile drained for I2 days butthe fistula then closed. He then developed apancreatic fistula which was treated by continuoussuction, and eventually closed in about four weeks.The patient was discharged well after two monthsin hospital and returned to work one month later.He has remained well and his nutrition remainsgood with pancreatin; although the stools arebulky and fatty, there is no diarrhoea.An artist's impression of the resected speci-
men is shown in Fig. 8.The papilloma was i cm. long and its distal
part 3 mm. diameter. Its long stalk and somelaxity of the mucous membrane to which it wasattached suggest that attempts were being madeto extrude it.The microscopic section showed a simple
papilloma of the bile duct and there was noepithelial hyperplasia. Serial sections failed toshow the structure of the stalk or base.One must admit that a radical operation-was
unnecessary in this case. The correct procedureshould have been to open the duodenum and in-
_7une I195 I 285by copyright.
on Novem
ber 25, 2020 by guest. Protected
http://pmj.bm
j.com/
Postgrad M
ed J: first published as 10.1136/pgmj.27.308.277 on 1 June 1951. D
ownloaded from

286 POSTGRADUATE MEDICAL JOURNAL J/lne I951
spect the ampulla when a local diatlieriiiy CxcisioIiof the polyp could have been carried out as advisedly Cattell (Cattell and Pyrtek, I950).
CommentaryI feel that the brief reports of these eight cases
offer their own lessons, but would like to sum-marize shortly my own opinions.
In a case of obstructive jaundice in which thereis some doubt as to the cause at laparotomy:
i. When the gall bladder is collapsed a carefuldissection in the porta hepatis may reveal a growth.UTsually little can be done but f would suggest thatby opening the duct below and dilating the malig-nant stricture, palliation may be achieved withtemporary clearance of the jaundice.
2. When the gall bladder is distended theduodenum and head of pancreas should be freelymobilized and the bile duct brought under directvision. If there is a growth and it is absolutelyconfined to the bile duct a local resection isadvised. If it appears to have spread outside theconfines of the duct and involved the pancreatichead, a pancreatico-duodenectomy should beperformed.
3. Where a lesion of the ampulla is suspectedand there is the slightest doubt as to its nature,a transduodenal inspection should be made aftermobilizing the duodenum. If doubt still exists,and facilities for frozen sections are available, adiathermy excision should be performed and the
treatiueoit -,ill bc depend(lent on the patlhologicalrepor..
Having performed a resection of one sort oranother, the bile duct should be anastomosed tothe jejunum, and this is much easier to performover a soft rubber tube. The portion of jejunumshould always be defunctioned (Figs. 5 and 6) toobviate the danger of ascending cholangitis. Ihave found that ligation of the proximal end of theduct and usage of the gall bladder to re-establishbiliary continuity is unsatisfactory, the dangerbeing that the bile duct will slough and thepatient succumb to a biliary peritonitis.The decision to perform a one- or two-stage
operation depends upon the age and general con-dition of the patient. A one-stage operation ispreferable but when the liver function is demon-strably poor a two-stage procedure is necessary.We have found that the most useful liver functiontests are serum protein, thymol turbidity andalkaline phosphatase estimations.
fn conclusion I would like to say that althoughthese are relatively rare tumours they are ascommon as carcinoma of the gall bladder and ascarcinoma of the pancreas (Willis, 1948). Theiridentification may often mean the saving of lifeby a relatively simple surgical procedure.
I am grateful to Mr. Norman C. Tanner forgiving me access to his notes, and to Mrs. Maceand Miss Mason of the photographic departmentof St. James's Hospital.
BIBLIOGRAPHYBRUNSCHWIG, A. ( 948), 7.A.M.A., 136, 28.CATTELL, R. B., and PYRTEK, L. J. (1950), S,,r. Gin. &
Obst., 90, 2 I.CHRISTOPHER, F. (1933), Siurg. Gvni. Le Obst., 56, 202.I)IC K, J. C. (io.19), Brit..7. ,'Sllkg., 26, 757.
GORDON-TAYLOR, G. (1942), Brit. Med..7., ii, ii9.ROLLESTON, and McNEE (1929), 'Diseases of Liver, Gall
Bladder and B3ile Ducts,' MacMillan, London.WVILLIS, R. A. (1948), 'Pathology of Tumours,' Btitterworth,
I ondon.
ATOM BOMBS AND RADIATION INJURIES *
By SURGEON COMMANDER G. D. WEDD, R.N., SURGEON COMMANDER D. A. HOVENDEN, R.N., andINSTRUCTOR LIEUTENANT A. J. ALABASTER, R.N.
J?oyal Naziy Medical School, Al? erstoke
The story of Hiroshima and Nagasaki is nowancient history. It is well known that the twoatomic bombs killed about ioo,ooo people and in-jured as many more, besides producing untoldmaterial damage. Of those who were killed about
* Part of this article has been taken from ' SomeMedical Aspects of Atomic Warfare,' G. D. Wedd,Public Healthi, June 1950.
8o per cent. died from burning or from mechanicalinjuries due to blast damage, which are the normalaccompaniments of any explosion. There re-mained a smaller number, variously estimated atfrom IO to 20 per cent., who were uninjured ortrivially injured at the time, but who died days orweeks later from the effects of radioactivity.
Radioactivity then is a relatively minor cause of
by copyright. on N
ovember 25, 2020 by guest. P
rotectedhttp://pm
j.bmj.com
/P
ostgrad Med J: first published as 10.1136/pgm
j.27.308.277 on 1 June 1951. Dow
nloaded from