Neonatal examination
-
Upload
mohamed-abass -
Category
Health & Medicine
-
view
422 -
download
2
Transcript of Neonatal examination
THE FIRST 24 HOURS:
The newborn infant should
undergo a complete physical
examination within 24 h of birth.
It is easier to listen to the heart
and lungs first when the infant is
quiet.
Warming the stethoscope..3
Appearance:
Signs such as cyanosis, nasal flaring,
intercostal retractions, and grunting suggest
pulmonary disease.
Meconium staining of the umbilical cord, nails,
and skin suggest fetal distress and the
possibility of MAS. The level of spontaneous
activity, passive muscle tone, quality of the cry,
and apnea are useful screening signs to
evaluate the state of the nervous system. 4
1-VITAL SIGNS:
Temprature: axillary method is prefered (36.0-37
°C).
Heart rate :(normal rate, 120 to 160 beats/ min
when awake, 70-80 beats/min when asleep).
Respiratory rate: ( normal rate is 40 to 60 cycle
per min) should be assessed within a whole
minute.
Blood pressure: (often reserved for sick infants).5
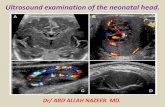
GESTATIONAL AGE :
prenatally by the following techniques:
date of last menstrual period.
date of first reported fetal activity (quickening usually
occurs at 16-18 weeks).
first reported heart sounds (10-12 weeks by Doppler
ultrasound examination).
ultrasound examination (very accurate if obtained
before 20 weeks' gestation).7
Postnatally is determined by an assessment of various physical signs
and neuromuscular characteristics that vary according to fetal age
and maturity.
A. Rapid delivery room assessment. :creases in the sole of the
foot, size of the breast nodule, nature of the scalp hair, cartilaginous
development of the ear lobe, and scrotal rugae and testicular descent
in males.
B. New Ballard Score. The Ballard maturational score has been
expanded and updated to include extremely premature infants. It has
been renamed the New Ballard Score (NBS). The score now spans
from 10 (correlating with 20 weeks' gestation) to 50 (correlating with
44 weeks' gestation). It is best performed at <12 h of age if the infant
is <26 weeks' gestation. If the infant is >26 weeks' gestation, there is
no optimal age of examination up to 96 h.
The examination is accurate whether the infant is sick or well to
within 2 weeks of gestational age. 8
NEW BELLARD SCORE
Physical criteria , including
increasing firmness of the pinna of
the ear; increasing size of the breast
tissue; decreasing fine, immature
lanugo hair over the back; and
decreasing opacity of the skin.
Neurologic criteria including
increasing flexion of the legs, hips,
and arms; increasing tone of the
flexor muscles of the neck; and
decreasing laxity of the joints.
These signs are determined during
the first day of life and are assigned
scores.9
Classification. Infants are classified as
preterm (<37 weeks), term (37-
41weeks), or post term (>42 weeks).
10
SMALL FOR GESTATIONAL AGE
Defined as 2 standard deviations
below the mean weight for
gestational age or below the
10th percentile.
Seen in infants of mothers who
have hypertension or
preeclampsia or who smoke.
also been associated with
TORCH infections,
chromosomal abnormalities,
and other congenital
malformations.11
LARGE FOR GESTATIONAL AGE
Defined as 2 standard
deviations above the mean
weight for gestational age
or above the 90th
percentile.
Seen in infants of diabetic
mothers, infants with
Beckwith's
syndrome,familial and
infants with hydrops fetalis.. 14
III-GENERAL APPEARANCE
Observe the infant and record the general
appearance (eg, activity, skin color, and
obvious congenital abnormalities).
15
1. Plethora (deep,
rosy red color).
Plethora is more
common in infants with
polycythemia but can
be seen in an
overoxygenated or
overheated infant. It is
best to obtain a central
hematocrit on any
plethoric infant.
IV. SKINA-COLOR:
16
2. Jaundice
With jaundice, bilirubin
levels are usually >5
mg/dL.
This condition is abnormal
in infants <24 h old and
may signify Rh
incompatibility, sepsis, and
TORCH infections.
After 24 h, ABO
incompatibility or
physiologic causes.17
3-Pallor
Pallor may be
secondary to
anemia, birth
asphyxia, shock, or
patent ductus
arteriosus (Ductal
pallor).
18
4-CYANOSISDesaturation of 5 g of hemoglobin usually necessary for one to note a bluish
color
Central cyanosis (bluish skin, including the tongue and lips). Central cyanosis
is caused by low oxygen saturation in the blood. It may be associated with
congenital heart or lung disease.
Acrocyanosis (bluish hands and feet only). normal, cold stress. decreased
peripheral perfusion secondary to hypovolemia.
19
associated with a prolonged
and difficult delivery and may
result in early jaundice.
Petechiae (pinpoint
hemorrhages). If they are
widespread and progressive
do coagulation profile.
5-ECCHYMOSES
20
B-HARLEQUIN COLORATIONclear line of demarcation
between an area of redness
and an area of normal
coloration).
The cause is usually
unknown.
The coloration can be benign
and transient (lasting usually
<20 min) or can be indicative
of shunting of blood
(persistent pulmonary
hypertension or coarctation
of the aorta).21
C- MOTTLING
(lacy red pattern) may be seen
in healthy infants and in those
with cold stress, hypovolemia,
or sepsis.
Persistent mottling, referred to
as cutis marmorata, is found
in infants with Down syndrome,
trisomy 13, or trisomy 18.
22
D-VERNIX CASEOSA
greasy white
substance that covers
the skin until the 38th
week of gestation. Its
purpose is to provide a
moisture barrier. It is
completely normal.
23
E-COLLODION INFANT
Congenital ichtyosis
skin resembles
parchment, and there
can be some
restriction in growth of
the nose and ears.
24
F-RASHES
1. MILIA:
Whitish, tiny, sebaceous retention
cysts are usually on the chin,
nose, forehead, and cheeks.
No erythema is seen.
These benign cysts disappear
within a few weeks after birth.
These are seen in approximately
33% of infants.25
2-ERYTHEMA TOXICUM
Numerous small areas of
red skin with a yellow
white papule in the
centre.
Appear 48hr after birth
last for 7-10 days.
Common in full term.26
3-ACNE NEONATORUMSeen over the cheeks,
chin, and forehead and
consist of comedones
and papules.
Benign and requires no
therapy; however, severe
cases may require
treatment with mild
keratolytic agents.
27
4-NEONATAL PUSTULAR MELANOSIS
Three stages of lesions, which
may appear over the entire
body:
• Pustules.
• Ruptured vesicopustules with
scaling/typical halo
appearance.
• Hyperpigmented macules.
This benign, self-limiting
condition requires no specific
therapy. 28
6-CANDIDA ALBICANS RASH
Common seen in napkin area so
called Napkin Dermatitis
Erythematous plaques with sharply
demarcated edges. Satellite bodies
are also seen.
Gram's stain of a smear or 10%
potassium hydroxide preparation of
the lesion reveals budding yeast
spores
Treated with nystatin cream applied
to the rash 4 times daily for 7-10
days. 30
G-NEVI
1- MACULAR HEMANGIOMA ("STORK BITES")(ANGEL KISS)
True vascular nevus normally seen
on the occipital area, eyelids, and
glabella.
The lesions disappear
spontaneously within the first year
of life.31
2-PORT-WINE STAIN (NEVUS FLAMMEUS)
Seen at birth, does not
blanch with pressure,
and does not disappear
with time.
SturgeWeber syndrome
(port-wine stain over
the forehead and upper
lip, glaucoma, and
contralateral jacksonian
seizures). 32
3-CAVERNOUS HEMANGIOMA
large, red, cyst-like, firm, ill-
defined mass and may be
found anywhere on the body.
The majority of these lesions
regress with age, but some
require corticosteroid therapy or
surgical resection.
Kasabach-Merritt syndrome:
(thrombocytopenia associated
with a rapidly expanding
hemangioma) should be
considered. 33
4-STRAWBERRY HEMANGIOMA
Flat, bright red, sharply
demarcated lesions
that are most
commonly found on
the face.
Spontaneous
regression usually
occurs (70%
disappearance by 7
years of age).34
5-MONGOLIAN SPOT
Dark blue or purple
bruise-like macular spots
usually located over the
sacrum.
Usually present in 90% of
blacks and Asians, and
disappear by 4 years of
age.
They are the most
common birthmark. 35
V. HEAD
Note the general shape of the head.
Inspect for any bruises secondary to forceps or
fetal monitor leads.
Transillumination can be done for severe
hydrocephalus.
Check for microcephaly or macrocephaly36
A. ANTERIOR AND POSTERIOR FONTANELLES
Anterior fontanelle usually closes at 9-12 months and the posterior
fontanelle at 2-4 months.
A large anterior fontanelle is seen with hypothyroidism
,osteogenesis imperfecta, hypophosphatasia, and chromosomal
abnormalities and in those who are small for gestational age.
A bulging fontanelle may be associated with increased
intracranial pressure, meningitis, or hydrocephalus.
Depressed (sunken) fontanelles are seen dehydration.
A small anterior fontanelle may be associated with
hyperthyroidism, microcephaly, or craniosynostosis. 37
B-SKULL MOLDING
Temporary asymmetry of the
skull resulting from the birth
process.
Most often seen with
prolonged labor and vaginal
deliveries, it can be seen in
cesarean deliveries if the
mother had a prolonged
course of labor before delivery.
A normal head shape is
usually regained within 1 week.38
C. CAPUT SUCCEDANEUM
Diffuse edematous
swelling of the soft
tissues of the scalp that
may extend across the
suture lines.
It is secondary to the
pressure of the uterus or
vaginal wall.
It resolves within several
days39
D. CEPHALHEMATOMASubperiosteal hemorrhage that
never extends across the suture
line. It can be secondary to a
traumatic delivery or forceps
delivery.
X-ray films or(CT) scans of the
head should be obtained if an
underlying skull fracture is
suspected (<5% of all
cephalhematomas). Hematocrit
and bilirubin levels should be
monitored in these patients.
Most cephalhematomas resolve in
2-3 weeks. Aspiration of the
hematoma is rarely necessary
40
E. SUBGALEAL HEMATOMA
Bleeding below the
epicranial aponeurosis.
It can cross over the
suture line and into the
neck or ear.
It may be necessary to
replace blood volume
lost and correct
coagulopathy if present 41
F. INCREASED INTRACRANIAL PRESSURE
• Bulging anterior fontanelle
• Separated sutures
• Paralysis of upward gaze
(setting-sun sign)
• Prominent veins of the scalp
• Increasing macrocephaly
Secondary to hydrocephalus,
hypoxic- ischemic brain injury,
intracranial hemorrhage, or
subdural hematoma. 42
G. CRANIOSYNOSTOSISPremature closure of one or
more sutures of the skull. It
should be considered in any
infant with an asymmetric
skull.
On palpation of the skull, a
bony ridge over the suture line
may be felt, and inability to
freely move the cranial bones
may occur.
X-ray studies of the head
should be performed, and
surgical consultation may be
necessary.
43
H. CRANIOTABES
softening of the skull
that usually occurs
around the suture lines
and disappears within
days to a few weeks
after birth.
It may be secondary to
a calcium deficiency,
and osteogenesis
imperfecta and syphilis.44
VI. NECK
Rooting reflex causes the infant to turn the head
and allows easier examination of the neck.
Palpate the sternocleidomastoid for a hematoma
and the thyroid for enlargement, and check for
thyroglossal duct cysts.
A short neck is seen in Turner's, Noonan's, and
Klippel-Feil syndromes.
45
VII. FACELook for obvious abnormalities, general shape of the nose,
mouth, and chin.hypertelorism (eyes widely separated) or
low-set ears.
A. Facial nerve injury:
facial asymmetry with crying. The corner of the mouth
droops, and the nasolabial fold is absent in the paralyzed
side. The infant may be unable to close the eye, move the
lip, and drool on the side of the paresis.
If the palsy is secondary to trauma, most symptoms
disappear within the first week of life, but sometimes
resolution may take several months. If the palsy persists,
absence of the nerve should be ruled out. 46
VIII. EARS:
Hairy ears are seen in infants of diabetic mothers.
Gross hearing can be assessed when an infant
blinks in response to loud noises.
Tympanic membranes are dull, gray, opaque, and
immobile in the first 1 to 4 weeks. These findings
should not be confused with otitis media.
47
Seen with many
congenital anomalies
(most commonly
Treacher Collins,
trisomy 9,21 and 18
syndromes).
Low set ear
48
benign, are often seen.
The 2007 Joint Committee
on Infant Hearing
statement lists ear pits as
one of the physical findings
associated with higher risk
for Hearing impairment.
Preauricular skin tags
49
Red reflex with an
ophthalmoscope.
Opacification of the
lens and loss of the
reflex are apparent
with Congenital
cataract.
IX. EYES
50
Normally white,
can have a bluish
tint if the infant is
premature.
If the sclera is deep
blue,
osteogenesis
imperfecta should
be ruled out
Sclera
51
Prader-Willi syndrome
Cystinosis
Pierre Robin syndrome
Rubella
Fetal alcohol syndrome
Mucopolysaccharidoses
SturgeWeber syndrome
Congenital glucoma
52
Rupture of small
conjunctival
capillaries can occur
after a traumatic
delivery.
This condition is seen
in 5% of newborn
infants.
Subconjunctival hemorrhage
54
Aseptic chemical neonatal
conjunctivitis that is induced
by silver nitrate solution,
which is used for prophylaxis
of infectious conjunctivitis.
Septic neonatal
conjunctivitis, with
Chlamydia being the most
common infectious agent.
Conjunctivitis
55
X. NOSE
Choanal atresia is suspected, verify the patency of the
nostrils with gentle passage of a nasogastric tube.
Infants are obligate nose breathers; therefore, if they
have bilateral choanal atresia, they will have severe
respiratory distress.
Nasal flaring is indicative of respiratory distress.
Sniffling and discharge are typical of congenital
syphilis.
Sneezing can be a response to bright light or drug
withdrawal.56
B. EPSTEIN'S PEARLS
Keratin-containing
cysts, which are
normal, are located on
the hard and soft
palates
Resolve
spontaneously.
58
C. MUCOCELE
Secondary to trauma
to the salivary gland
ducts.
It is usually benign
and subsides
spontaneously.
59
D. NATAL TEETH lower incisors X-ray films
are needed
1. Predeciduous teeth.
They are usually loose, and
the roots are absent or
poorly formed. Removal is
necessary to avoid
aspiration.
2. True deciduous teeth.
These teeth are true teeth
that erupt early. They should
not be extracted. 60
E. MACROGLOSSIA
Enlargement of the tongue can
be congenital or acquired.
Localized macroglossia is
usually secondary to congenital
hemangiomas.
Macroglossia can be seen in
Beckwith's syndrome
(macroglossia, gigantism,
omphalocele, and severe
hypoglycemia), congenital
hypothyrodism and Pompe's
disease. 61
F-THRUSH
Infection resulting from C.
albicans.
Whitish patches appear
on the tongue, gingiva, or
buccal mucosa.
Thrush is easily treated
with nystatin suspension
(0.1-1.0 mL) applied to
each side of the mouth, 3-
4 times per day for 7 days.62
XII. CHESTA. Observation. First, note whether the chest is symmetric.
An asymmetric chest may signify a tension pneumothorax.
Tachypnea, sternal and intercostal retractions, and grunting on
expiration indicate respiratory distress.
B. Breath sounds. A good place to listen is in the right and left
axillae.
Absent or unequal sounds may indicate pneumothorax or
atelectasis.
Absent breath sounds with the presence of bowel sounds indicates
a diaphragmatic hernia.
C. Pectus excavatum: sternum is altered in shape. Usually, this
condition is of no clinical concern. 64
D. Breasts in a newborn:
1 cm in diameter in term male and female infants.
They may be abnormally enlarged (3-4 cm)
secondary to the effects of maternal estrogens. This
effect, which lasts <1 week, is of no clinical concern.
A usually white discharge, commonly referred to as
may be present, Never squeeze it.
Supernumerary nipples are extra nipples and occur
as a normal variant.65
XIII. HEARTThe position of the heart in infants is more midline than in older
children.
The first heart sound is normal, whereas the second heart sound
may not be split in the first day of life. Decreased splitting of the
second heart sound is noted in PPHN, TGA, and pulmonary atresia.
Heart murmurs in newborns are common in the delivery room and
during the first day of life. Most of these murmurs are transient and
are due to closure of the ductus arteriosus, peripheral pulmonary
artery stenosis, or a small VSD.
Pulses should be palpated in the upper and lower extremities (over
the brachial and femoral arteries).
Blood pressure in the upper and lower extremities should be
measured in all patients with a murmur or heart failure. An upper to
lower extremity gradient of more than 10 to 20 mm Hg suggests
coarctation of the aorta.
66
XIV. ABDOMEN
A. Observation. Obvious
defects may include an
omphalocele, in which the
intestines are covered by
peritoneum and the
umbilicus is centrally
located
67
Gastroschisis
Intestine are not
covered by
peritoneum (the
defect is usually
to the right of the
umbilicus).
68
B. Auscultation: Listen for bowel sounds.
C. Palpation: Check the abdomen for distention, tenderness,
or masses.
The liver can be palpated 1-2 cm below the costal margin and
the spleen tip at the costal margin.
Hepatomegaly can be seen with congestive heart failure,
hepatitis, or sepsis.
Splenomegaly is found with cytomegalovirus (CMV) or rubella
infections or sepsis.
The kidneys (especially on the right) can often be palpated.
Kidney size may be increased with polycystic disease, renal
vein thrombosis, or hydronephrosis. Abdominal masses are
more commonly related to the urinary tract. 70
XV. UMBILICUSPresence of only two vessels (one artery and one vein)
could indicate renal or genetic problems (most commonly
trisomy 18).
If there is a single umbilical artery, there is an increased
prevalence of congenital anomalies and intrauterine growth
retardation and a higher rate of perinatal mortality.
If the umbilicus is abnormal, ultrasonography of the
abdomen is recommended. In addition, inspect for any
discharge, redness, or edema around the base of the cord
that may signify a patent urachus or omphalitis.
The cord should be translucent; a greenish-yellow color
suggests meconium staining, usually secondary to fetal
distress. 71
XVI. GENITALIAAny infant with ambiguous genitalia should not undergo gender
assignment until a formal endocrinology evaluation has been
performed.
A male with any question of a penile abnormality should not be
circumcised until he is evaluated by a urologist or a pediatric
surgeon.
A. Male. Check for dorsal hood, hypospadias, epispadias, and
chordee. Normal penile length at birth is >2 cm. Determine the site
of the meatus. Verify that the testicles are in the scrotum and
examine for groin hernias. Undescended testicles are more
common in premature infants. Hydroceles are common and
usually disappear by 1 year of age. Observe the color of the
scrotum. A bluish color may suggest testicular torsion and requires
immediate urologic/surgical consultation. Infants will have well-
developed scrotal rugae at term. A smooth scrotum suggests
prematurity.
72
B. Female:
Examine the labia and clitoris. A mucosal tag
is commonly attached to the wall of the
vagina.
Discharge from the vagina is common and is
often blood tinged secondary to maternal
estrogen withdrawal.
If the labia are fused and the clitoris is
enlarged, adrenal hyperplasia should be
suspected. 73
XVII. Lymph nodes:
Palpable lymph nodes, usually in the inguinal and cervical
areas, are found in ~33% of normal neonates.
XVIII. Anus and rectum:
Check for patency of the anus to rule out imperforate
anus.
Check the position of the anus.
Meconium should pass within 48 h of birth.
74
XIX. EXTREMITIES
A. Syndactyly abnormal
fusion of the digits, most
commonly involves the
second and third toes.
A strong family history
exists.
Surgery is performed
when the neonates are
older.75
B. Polydactyly is extra digits on
the hands or the feet. This
condition is associated with a
strong family history. An x-ray film
should done
If there are no bony structures, a
suture can be tied around the digit
until it falls off.
If bony structures are present,
surgical removal is necessary.
Axial extra digits are associated
with heart anomalies 76
C. Simian crease. A
single transverse
palmar crease is most
commonly seen in
Down syndrome but is
occasionally a normal
variant.
77
D- Talipes
equinovarus(clubfoot)
is more common in
males.
If this problem can be
corrected with gentle
force, it will resolve
spontaneously. If not,
orthopedic treatment and
follow-up are necessary.78
XX. Trunk and spine.
Check for any gross defects
of the spine.
Any abnormal pigmentation
or hairy tufts over the lower
back should increase the
suspicion that an underlying
vertebral abnormality exists.
A sacral or pilonidal dimple
may indicate a small
meningocele or other
anomaly.80
XXI. HIPS
Congenital hip dislocation occurs in
~1 in 800 live births. More common
in white females, unilateral left hip.
Two clinical signs of dislocation are
asymmetry of the skinfolds on the
dorsal surface and shortening of
the affected leg.
Evaluate for congenital hip
dislocation by using the Ortolani
and Barlow maneuvers.
81
2. Hypertonia:
Increased resistance is
apparent when the
arms and legs are
extended.
Hyperextension of the
back and tightly
clenched fists are often
seen. 83
B. Reflexes. The following
reflexes are normal for a
newborn infant.
1. Rooting reflex. Stroke the
lip and the corner of the cheek
with a finger and the infant will
turn in that direction and open
the mouth.
84
3. Grasp reflex.
Place a finger in the
palm of the infant's
hand and the infant
will grasp the finger.
86
4. Neck-righting
reflex. Turn the
infant's head to the
right or left and
movement of the
contralateral shoulder
should be obtained in
the same direction.
87
5. Moro reflex
Support the infant behind the
upper back with one hand, and
then drop the infant back 1 cm or
more to but not on the
mattress. This should cause
abduction of both arms and
extension of the fingers.
Asymmetry may signify a
fractured clavicle, hemiparesis,
or brachial plexus injury.
88
C. Cranial nerves. Note the presence of gross
nystagmus, the reaction of the pupils, and the
ability of the infant to follow moving objects with his
or her eyes.
D. Movement. Check for spontaneous movement
of the limbs, trunk, face, and neck.
A fine tremor is usually normal. Clonic movements
are not normal and may be seen with seizures.
90
E. Peripheral nerves
1. Erb-Duchenne
paralysis involves
injury to C5,6.
This condition can be
associated with
diaphragm paralysis.
91
2. Klumpke's
paralysis involves C7,8
T1. The hand is flaccid
with little or no control.
If the sympathetic fibers
of the first thoracic root
are injured, ipsilateral
ptosis and miosis can
occur.
92
F. General signs of neurologic disorders
1. Symptoms of increased intracranial pressure.
2. Hypotonia or hypertonia.
3. Irritability or hyperexcitability.
4. Poor sucking and swallowing reflexes.
5. Shallow, irregular respirations.
6. Apnea.
7. Apathy.
8. Staring.
9. Seizure activity (sucking or chewing of the tongue, blinking of the eyelids, eye rolling, and
hiccups).
10. Absent, depressed, or exaggerated reflexes.
11. Asymmetric reflexes. 93