National Perinatal Depression Initiative: North …/media/Files/Hospitals...At the extreme end,...
Transcript of National Perinatal Depression Initiative: North …/media/Files/Hospitals...At the extreme end,...

i
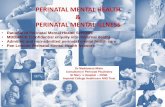
National Perinatal Depression Initiative:
North Metropolitan Integrated Service Model
Progress Evaluation WA Perinatal Mental Health Unit Women’s Health Clinical Care Unit
July 2012

ii
Citation The citation below should be used when referencing this work: WA Perinatal Mental Health Unit, Women’s Health Clinical Care Unit, Women and Newborn Health Service (2012). National Perinatal Depression Initiative: North Metropolitan Integrated Service Model Progress Evaluation. Perth, WA: Department of Health. © Department of Health, State of Western Australia (2012). Copyright to this material produced by the Western Australian Department of Health belongs to the State of Western Australia, under the provisions of the Copyright Act 1968 (C’wth Australia). Apart from any fair dealing for personal, academic, research or non-commercial use, no part may be reproduced without written permission of the WA Perinatal Mental Health Unit, Women and Newborn Health Service, Western Australian Department of Health. The WA Department of Health is under no obligation to grant this permission. Please acknowledge the WA Department of Health when reproducing or quoting material from this source. Important Disclaimer
All information and content in this Material is provided in good faith by the WA Department of Health, and is based on sources believed to be reliable and accurate at the time of development. The State of Western Australia, the WA Department of Health and their respective officers, employees and agents, do not accept legal liability or responsibility for the Material, or any consequences arising from its use. For further information contact: Miriam Maclean, Research Officer
WA Perinatal Mental Health Unit
Women’s Health CCU
15 Loretto Street, Subiaco, WA 6008
Phone: (08) 9340 1795
Fax: (08) 9340 1782
Email: [email protected]

iii
Glossary
AMH Adult Mental Health (in full - North Metropolitan Adult Mental Health
Program)
ATAPS Access to Allied Psychological Services
CACH Child and Adolescent Community Health
CAMI clinic Childbirth and Mental Illness clinic (King Edward Memorial Hospital)
CHN Child health nurse
CNS Clinical nurse specialist
CL Consultation Liaison, now Department of Psychological Medicine (King
Edward Memorial Hospital)
DOHA Department of Health and Aging
EPDS Edinburgh Postnatal Depression Scale
FTE Full time equivalent
GP General practitioner
KEMH King Edward Memorial Hospital
MBU Mother Baby Unit (located at King Edward Memorial Hospital)
MOU Memorandum of Understanding
NPDI National Perinatal Depression Initiative
OPH Osborne Park Hospital
PD Professional development
PND Postnatal depression1
WA Western Australia
WACHS WA Country Health Service
WAPMHU WA Perinatal Mental Health Unit
VC Video-conferencing
1 PND is widely used to refer to postnatal depression, however with increasing use of the term ‘perinatal mental health’, PND is sometimes used to refer to perinatal depression. Where comments are quoted from other sources, they may be referring to either Postnatal or Perinatal depression.

iv
Executive Summary
This report outlines the mid-point progress evaluation of a new perinatal depression service
model developed in Western Australia (WA). The North Metropolitan Integrated Service Model
(‘the service model’) is funded by the Department of Health and Ageing under the National
Perinatal Depression Initiative (NPDI) and has been developed to improve the patient/client
journey, reduce the service barriers and encourage better communication pathways between
service providers. WA Perinatal Mental Health Unit (WAPMHU) has entered into collaborative
arrangements with North Metropolitan Adult Mental Health Program (AMH), Child and
Adolescent Community Health (CACH), and Mother Baby Unit / Consultation Liaison Service
(MBU/CL) Women and Newborn Health Service to establish the service model.
Funding was initially provided for three 0.8 full time equivalent (FTE) Clinical Nurse
Specialist (CNS) positions to work collaboratively in providing a comprehensive service for
women in the North Metropolitan Area who are at risk of, or experiencing, mild, moderate or
severe depression in the perinatal period. By December 2009, all positions were filled and
located in:
• Child and Adolescent Community Health (CACH), North
• Adult Mental Health (AMH), Osborne Adult Community Mental Health Service
• King Edward Memorial Hospital (KEMH), Mother Baby Unit (MBU) and Psychological
Medicine Consultation Liaison Service (CL).
The purpose of the evaluation is to assess the processes and activities of service
implementation, and progress towards the service model’s expected outcomes:
1. Build and Sustain Relationships - with and between maternity and mental health
services, and other services involved in the care of women with perinatal depression.
2. Clinical Service - inclusive of individual and therapeutic group work as needed within
the local catchment area.
3. Collegial Support - which involves providing perinatal mental health support, information
and advice to colleagues.
In addition, the memorandum of understanding (MOU) for each position outlines a series of
expected outputs related to quantifying service activities. These are provided in the initial 3-
month scoping and planning report provided by each CNS, and subsequent 6-monthly
progress reports. Data is drawn from the first three six-monthly reports to August 2011. In
addition to quantitative service data, qualitative information from stakeholders is essential to
assess qualitative outcomes such as the strengthening of relationships. A total of 36
participants were interviewed.
There is a large amount of flexibility in the development of each CNS role, within the
framework provided by the MOU. Each of the positions sits within a different agency, and

v
targets a different level of depression risk or severity. The CNSs were expected to develop
their roles in response to the needs and context of their catchment area. Consequently, the
three positions have developed quite differently, and part of the evaluation process is to outline
how each has evolved and is being implemented.
Overall, there has been good progress towards all three expected outcomes and many
achievements over the first 21 months of operation. Key findings from this evaluation include:
• Within the area of Relationship Building the service model has facilitated a number of
notable improvements to referral and communication systems through which the
services interact, has established a Perinatal Mental Health Working Group in
Ellenbrook that brings together stakeholders from a range of services to address
perinatal mental health needs, and a range of collaborative projects have been
undertaken, including training and professional development.
• Clinical Service has included over 400 new referrals to the CNS’s, 947 patient related
occasions of service or follow-up visits, and approximately 180 individual assessments.
• Activities in the area of Collegial Relationships have included the provision of
professional development related to perinatal mental health to approximately 400 health
and social services professionals. Informal collegial support such as advice and
debriefing has also been provided.
• Stakeholder feedback is generally very positive, and describes outcomes including:
o Reduced waiting times and increased support for women with perinatal depression
o Increased support for health professionals leading to higher levels of comfort and
skill in working with mothers with perinatal depression
o Improved knowledge of referral pathways
o Increased networking and collaboration related to perinatal depression and
increased focus on perinatal depression by services.
• Various challenges have been identified, including:
o Overcoming various obstacles to implementing a jointly facilitated perinatal support
group between the AMH and CACH CNS requires continued effort
o The client catchment restrictions for the different positions can limit referral pathways
and connections between the positions
o Although feedback on relationship building has primarily been positive, there are still
areas to strengthen and further consolidate
o The broad scope of work and time constraints have required ongoing decision-
making and prioritisation in order to maintain a manageable workload and avoid the
CNSs being ‘spread too thin’ to be effective.

vi
Recommendations:
1. Continue funding of the service model, with furt her evaluation prior to June 2013 .
Based on the findings from this evaluation, good progress has been made towards the
expected outcomes and provision of outputs.
2. Address barriers to establishing co-facilitated group/s run by the AMH and CACH
CNSs. Joint activities such as co-facilitated groups provide an excellent opportunity for
bringing together the different areas of expertise in mental health and child health, and
developing a greater shared understanding. Ongoing solutions will increase the
feasibility of further collaborative activities.
3. Further strengthen the links between the three s ervices, through activities such
as joint strategic planning . It will be necessary to include the CNSs as well as all
operational and strategic managers, for a shared vision, role clarity and forward
planning.
4. Explore higher turnover rates in AMH CNS positio ns and develop strategies to
facilitate retention .
5. Explore ways to strengthen relationships between mainstream mental health and
perinatal services. Conduct perinatal mental health education sessions that enable
shared learning between mental health, midwives and child health nurses. Increase
awareness among mainstream mental health professionals of the potential negative
outcomes of perinatal mental health problems for women, infants and families (including
mortality and infant mental health issues).
6. Continue to build communication and address area s of conflict that arise when
bringing together diverse cross-disciplinary, cross -agency and cross-sectoral
groups. Improve communication between mental health and midwifery staff in the form
of referral feedback summaries. Improve consultation with non-government
stakeholders regarding forward planning for state-wide perinatal mental health services.
7. Plan the future scope and positioning of roles w ithin the service model, including
expansion scenarios and infrastructure needs such a s co-location.
8. Use the information from this evaluation and str ategic planning in developing a
business case for continuing the model beyond June 2013.

vii
Contents 1 Introduction ....................................... ............................................................................1
1.1 Literature Review..................................................................................................2 1.2 The National Perinatal Depression Initiative North Metropolitan Perinatal Service Model .............................................................................................................................3 1.3 Development of the three positions ......................................................................5
2 Evaluation Framework ............................... ...................................................................7 2.1 Expected Outcomes .............................................................................................8 2.2 Key Performance Indicators/Outputs....................................................................8 2.3 Stakeholder Interviews .........................................................................................9 2.4 Additional Data Sources .....................................................................................10 2.5 Data Preparation and Analysis ...........................................................................10
3 Findings ........................................... ............................................................................11 4 Service Model Approach ............................. ...............................................................11 5 Expected Outcomes.................................. ..................................................................12
5.1 Building and Sustaining Relationships................................................................12 5.2 Qualitative themes relating to ongoing relationship building and collaborations.22 5.3 Clinical Service ...................................................................................................29 5.4 Collegial Relationships .......................................................................................34 5.5 Service Issues and Staff Perspectives ...............................................................37
6 Discussion and Recommendations..................... ......................................................46 6.1 Relationship Building ..........................................................................................46 6.2 Clinical Service ...................................................................................................48 6.3 Collegial Relationships .......................................................................................48 6.4 Summary ............................................................................................................49 6.5 Recommendations..............................................................................................50
References......................................... .....................................................................................51 Appendices......................................... ....................................................................................53

1
1 Introduction This report outlines the mid-point progress evaluation of the North Metropolitan Service
Model (‘the service model’) funded by the Department of Health and Ageing under the National
Perinatal Depression Initiative (NPDI). It is the first of two reports, with a final evaluation report
to be published in 2013.
Depression affects approximately 10-15% of women in the year following birth and is
almost as common during pregnancy (beyondblue, 2011; Segre, O'Hara, Arndt, & Stuart,
2007). At the extreme end, mental illness is one of the leading causes of maternal mortality in
the perinatal period (Austin, Kildea, & Sullivan, 2007). For the majority of women with perinatal
depression and related disorders, the effects are less dramatic, but still have a pervasive
impact on the wellbeing and functioning of the woman and her family. Maternal depression is
associated with a range of adverse developmental outcomes for children (Barker, Jaffee, Uher,
& Maughan, 2011; Lewis, Rice, Harold, Collishaw, & Thapar, 2011).
The Australian Government has committed significant funds over five years (2008/2009 to
2012/2013) for States and Territories to improve prevention and early detection of
antenatal/postnatal depression and provide better support and treatment for expectant and
new mothers experiencing depression.
One of the key activity areas to be addressed in the National Partnership Agreement is
“Follow-up, treatment, care and support for women assessed as being at risk of, or
experiencing, perinatal depression - mild, moderate and severe” such as:
• Focussed psychological treatment
• Counselling services
• Fostering better networks of support groups for new mothers
• Community-based care and support
• Acute inpatient care
Under this key activity area, WA Perinatal Mental Health Unit (WAPMHU), North
Metropolitan Adult Mental Health Program (AMH), Child and Adolescent Community Health
(CACH), and Mother Baby Unit / Psychological Medicine Consultation Liaison Service2
(MBU/CL) Women and Newborn Health Service have entered into a collaborative service
model to improve the patient/client journey, reduce the service barriers and encourage better
communication pathways between service providers.
2 Now known as the Department of Psychological Medicine

- 2 -
1.1 Literature Review Various bodies of research and theory support the importance of developing strong links
and effective communication between different organisations or parts within an organisation.
Organisational research has highlighted the ‘silo mentality’ where units within an organisation
or disciplines within a healthcare setting work separately, without communication or
integration, which can impede overall performance and effective service provision (Gillespie,
Chaboyer, Longbottom, & Wallis, 2010). Health researchers drawing on ‘systems-thinking’
approaches have advocated the importance of “a network-centric approach that encourages
relationship-building among and between individuals and organizations across traditional
disciplines and fields in order to achieve relevant goals and objectives” (Leischow et al., 2008)
p. 196). Effective communication and collaboration is recognised as an important goal in
strengthening service provision.
Perinatal mental health is a particularly challenging area for collaborative and integrated
services as patient needs fall across disciplines and timeframes (Myors, Schmied, Johnson, &
Cleary, 2011). Although perinatal mental health can be an area of specialty in itself, in many
healthcare systems it tends to fall between two areas of practice – with some services
addressing general maternal and child health issues and other services addressing general
mental health. Early intervention requires midwives, nurses and general practitioners (GPs)
who are usually the first point of contact for women during the perinatal period, to effectively
screen, identify risk and make one or more appropriate referrals based on the potentially
complex needs of the patient/client. When considered in more detail, this ideal response relies
on the health professional having knowledge and information regarding the “bewildering” range
of perinatal mental health problems with different levels of severity and associated care
pathways, which in turn requires appropriate training and support (Hayes, 2010). Early
intervention also relies on the availability and response of secondary or tertiary mental health
services following referral.
Research suggests that the health care services for women, children and families are often
inconsistent and fragmented. There is a need for increased collaboration and partnerships to
provide a more integrated perinatal service delivery (Schmied et al., 2010). Barnett (2011) has
highlighted the need for integrated models of perinatal care, despite the acknowledged
difficulty of achieving this goal. A recent review by Myors and colleagues (2011) examined
research on professionals’ views and experiences of working in collaborative perinatal models
of care. The process of ‘making it happen’ was the overarching theme identified by the review.
Within this, eight elements were identified as important in this process. The elements were
funding and resources for collaboration; shared vision, aims and goals; pathways and

- 3 -
guidelines; continuity of care; building relationships and trust; role clarity; training and
education of staff; and support to work in new ways.
It should be noted that collaborative and integrative models of perinatal mental health care
are an emerging area of research: all of the papers identified in the above review were
published since 2004, and half were published since 2008 (Myors, et al., 2011). Consequently,
the research knowledge-base is developing alongside new initiatives such as the NPDI service
model. Lessons learnt through the service model’s development and evaluation will provide
valuable information on implementing integrated perinatal care.
1.2 The National Perinatal Depression Initiative North Metropolitan Perinatal Service Model The aim of the service model is to address some of the gaps in service and bring a greater
collaborative approach to perinatal depression follow-up, treatment, care and support through
better coordination between service providers.
Funding was provided for three 0.8 full time equivalent (FTE) Clinical Nurse Specialist
(CNS) positions to work collaboratively to provide a comprehensive service to women in the
North Metropolitan Area who are at risk of, or experiencing, mild, moderate or severe
depression in the perinatal period. By December 2009, the positions had been filled and were
located in:
• CACH, North
• AMH, Osborne Adult Community Mental Health Service
• King Edward Memorial Hospital (KEMH), MBU and CL.
A further two positions have since commenced in the CACH South Metropolitan region in
2011. Once these positions have become established they will be included in future
evaluations. Bringing together adult mental health, child health and perinatal mental health
CNSs is intended to increase supportive and cooperative relationships between health
professionals in these services, and facilitate the flow of information and referral pathways to
improve service provision. This is seen as a first step in developing a responsive and
coordinated health service. Part of this process is to establish and maintain supportive and
cooperative working relationships between health professionals within the services –
maternity, child health and mental health – as well as non-government agencies and private
health providers such as GPs.
The CNS positions are also intended to cover different levels of severity or risk of
depression: from mild, where services are primarily within the community and child health

- 4 -
areas; to moderate, where out-patient services are often required; to severe, with tertiary
services. Working within these services, they are expected to use and share their expertise to
strengthen agency relationships, undertake clinical activities and provide collegial support to
health professionals (see Figure 1).
Figure 1. The Service Model
Mild/moderate Child Health
0.8FTE
Moderate-severe Mental Health
0.8FTE Severe
MBU / CL 0.4FTE / 0.4FTE
* Building and sustaining relations - local agencies - existing maternity units - child health/mental health/MBU * Clinical services - individuals - groups - service co-ordination * Collegial relationships - professional development - supervision - support
Community Tertiary
Client/patient
Community outreach

- 5 -
1.3 Development of the three positions The three positions were initially filled in October, November and December 2009. The
focus of the CACH CNS position is on prevention, early identification and early intervention for
those considered at risk for mild-moderate perinatal depression. The role has therefore
involved extensive relationship building and information sharing with a wide range of services,
with a focus on community development activities. Numerous organisations can play a
valuable role in early identification or provision of support for women with perinatal depression.
The scope is defined by a geographical catchment area (see Figure 2 on page 6). In 2011 a
second CACH CNS position commenced, covering the South Metropolitan area.
The AMH CNS position targets moderate to severe depression in the perinatal period. This
position sits within the Osborne Adult Community Mental Health Service. The scope is limited
to women birthing at Osborne Park Hospital. The initial contract position was filled from
November 2009 until April 2010. The position was then vacant for approximately 3 months with
the current CNS commencing in August 2010.
The MBU/CL CNS position is located at KEMH. The role is divided between the MBU and
CL, with statewide responsibilities, focussing on severe perinatal depression. The MBU/CL
CNS has been in the position since December 2009.
The memorandum of understanding (MOU) provides a framework for the development of
the CNS roles. Within this framework there is a great deal of flexibility in how each CNS
implements the role. The CNSs were expected to conduct scoping and planning activities, and
to develop their roles in response to the needs and context of their catchment area. The
positions each sit within a different agency and target different levels of depression risk or
severity. Therefore, the positions have developed quite differently, and part of the evaluation
process is to outline how each has evolved and is being implemented. As a new, innovative
service model, it is anticipated that the service will continue to develop over time as CNS’s
respond to emerging needs or opportunities that fit within the goals of the service model.

- 6 -
Figure 2. North Metropolitan Area Health

- 7 -
2 Evaluation Framework
The purpose of the evaluation is to assess progress against the Expected Outcomes, as
measured by reported Outputs or Key Performance Indicators (KPIs), and stakeholder
interview data. Several features of the service model are pertinent in determining the
evaluation approach:
• The Expected Outcomes provide broad parameters and goals, but there is a large
degree of flexibility in how these may be addressed
• The CNSs are each operating within a different setting, with slightly different expected
outcomes and key performance indicators
• The CNSs are expected to be responsive to the needs of their catchment area
• The service model is a new, cutting-edge service that is expected to develop and
change through a process of scoping and planning, trial and error, and continuous
improvement.
As a result, a process evaluation approach (Rossi, Lipton & Freeman, 2004) is used, in
which the activities of the service are explored and described. In addition, stakeholder
feedback is used to assess whether the activities undertaken are resulting in satisfactory
progress towards the expected outcomes of the project. Expected outcomes such as the
building of relationships and provision of collegial support are most suited to qualitative
evaluation, which allows for a deeper understanding of the perceived quality of relationships
and any challenges and conflicts arising. In addition stakeholder interviews provided some
opportunities for assessing the counterfactual (what would have happened if the service model
hadn’t been in place) based on their experiences before and during the implementation of the
service model (Cummings, 2006).
Broadly, the evaluation aims to identify:
• Achievements and progress towards the Expected Outcomes
• Challenges and areas for further development

- 8 -
2.1 Expected Outcomes 1. Build and Sustain Relationships 3 - Build and sustain partnership and collaboration
with local health agencies such as CACH, AMH, GP practices, Women’s Health
Services and other relevant community services. Strengthen linkages to local
maternity units and liaison with tertiary perinatal depression treatment units.
2. Clinical Service - Provide clinical service inclusive of individual and therapeutic
group work as needed within the local catchment area serviced by the Obstetric
Psychiatric Liaison Clinic Osborne Park Hospital (AMH). Provide clinical service
inclusive of individual community based assessments, treatments and follow-up of
perinatal women and their families with moderate to severe depression (MBU/CL).
Provide clinical service in collaboration with respective CNS Mental Health Services
inclusive of individual and therapeutic group work as needed within the local
catchment area.
3. Collegial Support - Provide specialist perinatal mental health support, information
and advice to colleagues (MBU/CL and AMH). Provide support, information and
advice to colleagues, as needed relevant to perinatal depression (CACH).
2.2 Key Performance Indicators/Outputs The Expected Outcomes represent the core goals of the service. Detailed KPIs or Outputs
were agreed between the parties, to achieve the Expected Outcomes (See Appendix B, C and
D). KPIs and Outputs included provision of quantitative information (such as the number of
contact meetings/phone calls, building relationships with maternity, child health and mental
health services) and qualitative information (such as difficulties in developing working
relationships or improvements/successes achieved from the partnership/collaboration). Each
CNS was required to provide a report on the first 3 months of scoping and service
establishment, followed by six-monthly reports relating to the KPIs. Information from these
reports is included in the evaluation, particularly the quantitative information regarding service
activities and background information. At the time of data collection and commencing the
report, progress reports had been provided covering the first 21 months of the service model to
August 2011.
3 The wording of the expected outcomes varied slightly across the three positions to reflect differences in the roles and the strengthening of linkages with the services holding the other CNS positions. An aggregation/summary is included here.

- 9 -
2.3 Stakeholder Interviews A total of 36 participants took part in the interviews during October and November 2011.
Semi-structured interviews were conducted face-to-face or by telephone (see Appendix A for
interview questions). The original list of stakeholders was created by the WAPMHU research
officer in conjunction with the WAPHMU state coordinator and the CNSs, as well as drawing
from the names of services and professionals mentioned in CNSs’ six-monthly reports.
Stakeholders included a wide range of health and social services professionals. Their
involvement in the service model ranged from design and management, implementation,
professional interaction with the service model and/or recipients of service (professionals only
– not patients/health service users).
Sample size requirements in a qualitative study depend on the type of study and
whether the participants and their experiences are homogenous or varied. A common goal is
to achieve ‘saturation’, where interviewing further participants yields little new information.
Recommendations for sampling for interview based studies vary from 6-8 in a homogenous
group, to between 15 and 50 for more diverse groups (Onwuegbuzie & Leech, 2007). As the
experiences of stakeholders might differ depending on catchment and CNS, a minimum of 6-8
participants were required for each CNS catchment, with additional sampling of CACH CNS
stakeholders to reflect the broad range of stakeholders involved in specific activities (such as
child health nurses, and Ellenbrook Perinatal Mental Health Working Group members as well
as representatives from various services).
A sample was selected from the stakeholder list to represent a range of service types (such
as maternity, mental health, and community services), and a wide range of roles. The selection
of stakeholders was not intended to provide a random sample, but instead to gather a wide
range of perspectives of the service model. Selection emphasised, but was not limited to,
those with a larger involvement in the service model. As the aim was to gain a clear picture of
the service model including challenges and areas for improvement, efforts were made to
ensure the sample did not exclude stakeholders on the basis of whether their feedback was
expected to be positive or negative. A small number of participants were able to comment on
the catchment area and activities of more than one CNS.
The three CNSs were interviewed, along with two of their counterparts in the South
Metropolitan area, and the South Coastal Zone. In addition the WAPMHU state coordinator
was interviewed. The state coordinator was responsible for the design, securing of funding,
contract negotiation and strategic management of the service model. Several past and present
line managers responsible for operational management of the CNS roles were also
interviewed.

- 10 -
For the AMH catchment, a further seven participants were interviewed, including
midwifery, antenatal clinic and obstetric/psychiatric liaison service staff at Osborne Park
Hospital, as well as other mental health service providers. Nine additional participants were
interviewed for the MBU/CL component, including staff from the Childbirth and Mental Illness
clinic (CAMI clinic), regional service providers, and staff involved in collaborative activities. For
the CACH North area, additional information was provided by a further 15 participants,
covering a range of government and non-government services, and including several child
health nurses. The larger number of participants reflects the extensive community
development work associated with the CACH role.
2.4 Additional Data Sources In addition, two surveys of child health nurses provide some, though limited, additional
evaluation information. A brief online satisfaction survey was conducted in November 2011,
however there was a relatively small response rate (n=14), from five sections of the North
Metropolitan Area that have received different amounts of input from the service model.
Combined with small number of comments to explain reasons for levels of satisfaction, these
factors suggest that the main information that can be gleaned from the survey is that areas
with greater input from the CNS were more satisfied. A larger survey was undertaken by the
two CACH CNSs and the Riverlands child health nurse in conjunction with the WAPMHU
research officer, which largely focussed on identifying the needs of child health nurses in
relation to the CNS roles. The survey covers a range of topics, including whether participants
have completed Edinburgh Postnatal Depression Scale (EPDS) training and/or would like to
undertake training, and confidence dealing with high scores or the suicidal ideation question
on the EPDS, among many others. A total of 73 participants completed the survey. The survey
is primarily for planning purposes, however a follow-up survey is planned prior to the end of
the funding period, which will allow comparisons between the two time points.
2.5 Data Preparation and Analysis Data drawn from the CNSs’ 6-monthly reports up to August 2011 has been collated and
included where appropriate, particularly in the quantitative description of activities undertaken.
The interview data was entered into Microsoft Excel, and analysed thematically. The themes
tend to fit within the overarching structure of the three expected outcomes, and have been
integrated into the relevant sections of the report along with quotes from the participants.

- 11 -
3 Findings
The service model design is outlined in the following section. The evaluation findings
related to each expected outcome are then discussed, along with broader service and
implementation issues, followed by conclusions and recommendations.
The interviewees provided a wide range of perspectives of the service model. Although the
participants occasionally had conflicting views regarding ideal approaches when organisations
were working together, for the most part there was consistency regarding the activities
undertaken by the CNSs, the achievements of the service model so far, the challenges that
have been overcome and those that remain.
The use of multiple data sources, primarily stakeholder interviews and quantitative activity
reporting data, allows for triangulation, whereby information from one source is validated by
other sources.
4 Service Model Approach The model is intended to strengthen the linkages, information sharing and referral pathways
between maternal, child health and mental health services, as well as community agencies
that support women during the perinatal period. In addition, the model includes provision of
specialist support and information to health professionals relating to perinatal mental health.
This is intended to provide a resource to enable better and more confident care for women
with perinatal depression by health professionals, and facilitate effective referrals. Finally, a
clinical component is included whereby the CNSs can identify a clinical gap and address it by
providing direct assessment, care and support either in groups or one on one. Given the
limited available FTE for the clinical component, it is not expected that the CNSs would fill all
gaps in clinical care for perinatal depression. Instead, specific areas may be targeted, and the
roles are expected to build capacity for improved perinatal depression care and treatment by
supporting and upskilling other health professionals
Positioning CNSs across services that address varying severities of depression risk, and
cover child health, adult mental health and tertiary mental health care in the KEMH position is
intended to facilitate communication and draw on expertise across these areas in order to
provide a more coordinated and comprehensive approach. The three CNS positions were
expected to differ from each other. For example, the mental health nurse (AMH) role was seen
as having a bigger clinical load in follow-up of patients treated by the psychiatrists at the clinic.
Conversely, the child health nurse (CACH) role was expected to have a larger community
development role.

- 12 -
As a new, innovative service model, scoping and development of the roles is an important
task especially in the early stages. Each of the CNSs is required to undertake scoping and
planning in the first three months, to gain an understanding of the operation of relevant
services within their catchment, and identify gaps and areas to target. It is anticipated that as
the CNSs’ knowledge of the services, community and needs within their catchment area
grows, or in response to local changes and new opportunities, the roles will continue to evolve
and develop within the framework provided by the MOUs.
5 Expected Outcomes The following sections outline significant activities undertaken towards each of the three
expected outcomes, and feedback on the results of these activities. Information regarding the
activities undertaken is drawn from the 6 monthly reports, interviews with the CNSs, and
stakeholder interviews. Assessment of the outcomes of these activities is primarily drawn from
stakeholder interviews.
5.1 Building and Sustaining Relationships Expected Outcome 1 is building and sustaining relationships with other agencies, including
maternity, child health and mental health. The aim is for the CNS to not only strengthen their
own links with these agencies, but also to undertake initiatives that strengthen the links
between agencies in order to provide better care pathways.
Overall, there have been some important improvements in building and developing
relationships. While some of these relationship changes are less tangible, significant activities
identified in the evaluation include:
• Scoping and consultation with services
• Ongoing relationship building and collaborative activities
• Improved referral systems between:
o Osborne Park Hospital antenatal clinic and social work staff to
obstetric/psychiatric liaison service
o KEMH CAMI clinic incoming referrals and coordination at birth
o MBU to child health nurses at discharge
o Child health nurses to psychologists via Access to Allied Psychological Services
(ATAPS) referrals
o Other improved knowledge or availability of referral options.
These are individually discussed below, in more detail.

- 13 -
5.1.1 Scoping and consultation with services
The CNSs have undertaken extensive scoping and consultation with relevant services.
During the early months of the service model, activities included:
• All North Metropolitan Area Health Service maternity hospitals in the well as Community
Midwifery WA were contacted and information sought about identification and
management of perinatal depression. Information was provided to support one hospital
that did not yet have a formalised process in place to plan perinatal depression
screening and management.
• Meetings were held with all NMAHS Adult Mental Health Clinic duty officers (except
Morley/Swan) to share information and document processes related to perinatal
depression.
• Meetings were held with consumer groups such as From the Heart WA and the
Consumer Participation Committee (CL) and opportunities for consumer participation
explored.
• Meetings have been held with a wide range of other relevant services to provide
information about the role of the CNS, and gain more information about the services
available, systems in place, and current gaps.
• Examination of Department of Health data on child health nurse contacts related to
perinatal depression demonstrated areas with higher levels of contact, including Stirling.
This was used to select initial areas of more targeted activity.
The scoping and consultation activities highlighted a number of opportunities for
improvements in referral systems, and potential collaborations.
5.1.2 Ongoing relationship building and collaborati ve activities
The CACH CNS position in particular has undertaken extensive network and relationship
building activities related to community development. She has met with representatives from
over 30 organisations. Initial contacts often involve sharing information about the CNS role,
and the service’s activities and procedures relating to perinatal mental health. Many of these
relationship building activities have involved regular contact, and led to a range of service
improvements and collaborative projects.
For example, the Ellenbrook area was identified as presenting significant risk factors for
perinatal depression, and high presentations of women with perinatal depression. The
Ellenbrook Early Years project officer at the City of Swan organised funding to provide
perinatal depression service delivery in the area. The CACH CNS has been involved in
identifying and bringing together stakeholders with an interest in collaborating towards

- 14 -
sustainable solutions, thereby forming a stakeholder committee, known as the Ellenbrook
Perinatal Mental Health Working Group. The working group has brought together significant
expertise and a focus on advocating to meet the needs of families experiencing depression
during the perinatal period.
The CACH CNS also attends a steering committee for collaborative perinatal depression
support groups, initiated by the Joondalup Women’s Healthworks. Together with a From the
Heart WA peer support worker, the CNS co-facilitated a pilot support group “Making Sense of
Motherhood” targeting women diagnosed with PND as an adjunct to treatment. Funding has
been obtained to provide further groups. The CNS is also involved in collaborative activities in
other areas including Balcatta and Warwick. As the AMH CNS works at a hospital located
within the CACH CNS’s catchment area, the two CNS’s do some joint relationships building
activities with local services.
A focus of the MBU/CL CNS’s role has been the provision of training, consultation and
support to WA Country Health Service (WACHS) staff. The CNS has collaborated with a senior
project officer at WACHS to provide monthly presentations on perinatal mental health topics
via video conferencing. From February 2010 to August 2011, 17 presentations were
conducted, with an average of 14 attendees per session (a total of 230 attendances were
recorded for the 18 month period).
The MBU/CL CNS also collaborated with several staff from Women and Newborn Health
Service and mental health services to undertake the Perinatal Mental Health Roadshow in
2011, funded by the Mental Health Commission. Education and training on screening for
perinatal depression had previously been completed by many frontline staff, with the aim of
improving identification of perinatal depression and other mental health issues. Increased
identification of mental health needs should be followed by appropriate referral pathways and
service provision. Regional staff in some areas had identified several gaps in second tier
service provision, highlighting a need for further perinatal mental health awareness and
training and the identification of referral pathways. A one-day workshop was provided in
locations across the Kimberley (Broome, Fitzroy, Derby, Kununurra, and Halls Creek), the
Pilbara (Karratha and Port Hedland) and in the South West (Manjimup, Busselton and Collie).
Although as a professional development activity the roadshow contributes to collegial support,
it has also been an important relationship building activity through partnerships with providers
from other services and the face-to-face contact with staff from WACHS, along with the
relationship building opportunities for regional staff. The CNS describes the networking
process that occurred during roadshow activities:

- 15 -
“It was fed back to us that one of the best things was the exercise on resources –
everyone on a board – they found it really useful for networks. Many are transient – staff
who began 1-2 months ago, lots of them were swapping phone numbers”.
The CNSs have met with staff from a number of maternity and mental health services since
the scoping stage, to establish relationships with additional services, build on existing
relationships, and provide consultation and advice to new staff and services involved in mental
health consultation liaison roles in maternity hospitals, antenatal support groups and other
relevant services.
Part of the vision of the service model is for collaborative activities among the CNSs, in
keeping with previous successful co-facilitation by a child health nurse and mental health
nurse working in the area of perinatal mental health. Such collaborations are intended to draw
on the expertise of both areas of practice, as well as developing stronger links between the
agencies. The CNSs have been actively planning and preparing to run joint groups, particularly
between the AMH and CACH CNSs. However, there have been many obstacles to
implementing such joint projects, including:
• Issues around who or which service should take responsibility for managing clients
needing further support (holding the risk), and maintaining the records of participants.
This has implications such as whether group attendees would be entered on the
PSOLIS mental health database, which is considered a potential deterrent to
participation.
• Differing practice boundaries of CACH and AMH, for example an antenatal depression
support group does not typically fall within the scope of CACH, although its protective
value for the postnatal period can be argued.
• Finding a suitable venue with crèche facilities and related budgetary issues. The use of
a potential venue identified by the CNSs within the mental health service was not
supported as it was considered that this venue may adversely affect the group as a
result of stigma still surrounding mental illness.
Plans and preparations are continuing, and it is hoped that collaborative groups will commence
in 2012.
Finally, for the two CNSs based within a hospital setting (AMH and MBU/CL), another
important aspect of relationship building is improving the links between the maternity and
psychiatric services on the campus. Streamlining referral processes has been a valuable
outcome from this. The CACH CNS has also been involved in improving referral processes by

- 16 -
child health nurses to mental health services, and communication between the MBU and child
health nurses when patients are discharged. Each of these is discussed in more detail in the
following sections.
5.1.3 Improved Referral Systems
Effective referral systems are necessary to ensure that women are referred to appropriate
services to meet their needs, and that health professionals have the information necessary to
provide a responsive and appropriate service. Effective referral systems can reduce the risk
that clients fall between the cracks and do not receive the support or treatment they need.
There is also a reduction in wasted time by patients and health professionals when the
appropriate referral destination is identified at an early stage. Streamlining referral processes
can sometimes reduce waiting times, providing a quicker response. Ensuring health
professionals are aware of the referral options available allows them to provide more confident
and effective support.
Women with or at risk of perinatal depression will often first come into contact with
antenatal clinic staff, GPs, or child health nurses, and these professionals have a vital role to
play in the early identification of risk, and in responding with appropriate support and referrals.
There may be a need for not only mental health care, but also assistance with developing
secure attachment relationships and good parenting skills. Depression can adversely impact
on these areas. In addition, women with social risk factors such as isolation or low income are
at increased risk for perinatal depression, so referrals to appropriate community services,
social workers, or support groups can also be beneficial. The stronger the links between these
different services for perinatal women, the more likely it is that staff will be able to identify
needs and refer appropriately. In addition, for women with more severe depressive disorders,
tertiary care may be required. Again, strong links between tertiary services and other services
that women interact with during the perinatal period can create a smoother journey through the
healthcare system for women and their families. A number of improvements to referral
systems have been implemented by the CNSs in collaboration with service staff.
5.1.4 Osborne Park Hospital
The position of AMH CNS was designed partly in response to an identified need for
multidisciplinary support to streamline and improve referral processes at Osborne Park
Hospital. The previous referral process from the from the antenatal clinic to the
Obstetric/Psychiatric Liaison Service was described as follows:
• Assessed by the social worker in the antenatal clinic.
• Faxed to the duty officer at Osborne Clinic.

- 17 -
o Booked by the duty officer to see the doctor (thus a client would be booked with
a psychiatrist without a mental health assessment).
o Or further assessed by the duty officer.
• Initial assessment by the psychiatrist.
A central impact of the AMH CNS role has been the facilitation of a more streamlined
referral process from the antenatal clinic to either 1) social work for social issues, or 2) to the
CNS for a mental health assessment which leads to a psychiatry appointment where
appropriate with follow-up care as needed while waiting to be seen be the psychiatrist. Social
work and the CNS refer to each other where appropriate. Systems and protocols have been
established to document, clarify and support the referral process. The CNS is mostly based in
the mental health clinic, with one day a week spent in the antenatal clinic. Although being
spread across two locations can create some inconveniences, staff in both clinics appreciated
having regular contact which increased opportunities for communication.
The reported advantages of the new referral system, and having the CNS available to
provide assessments and follow-up for women with depression include:
• Women go through a much more streamlined process, with fewer layers of assessment
before attending the appropriate type of professional (e.g. social worker, psychiatrist,
CNS or external agencies).
• Mental health assessments prior to referral to the obstetric/psychiatric liaison service
are undertaken by the CNS.
• The social workers have a reduced role in the assessment of women with or at risk of
mental health issues, allowing them to concentrate on the wide array of other needs
women may have and that are within the social workers’ scope of expertise.
• The number of women referred to the psychiatrists is reduced as women who do not
require psychiatric care are diverted at an earlier stage to more appropriate care. This
reduces the amount of triaging the psychiatrists are required to do, allowing them to
spend more time on treatment.
• Women not requiring psychiatric care are also likely to benefit from having a more
suitable referral.

- 18 -
Staff indicate that this has enabled them and the service overall to provide a quicker and
more appropriate response to women with perinatal depression. Improvements include
reduced waiting time, interim support from the CNS if needed while waiting for an appointment
with a psychiatrist, fewer assessments that are extraneous or not within the area of
professional expertise of the staff member, and better treatment and care. Comments by
health professionals affected by the new referral system were positive, and included:
“It’s much better for the clients. The position has streamlined it for clients - before they'd
be referred to me, and I'd refer to the clinic, and then the duty manager would triage
them and they’d be given an appointment with the psychiatrist, and can sit in limbo
waiting weeks for an appointment. This way one person deals with the clients, they get
a better service, and quicker” “Overall - fantastic to have the position here, takes a huge
pressure off social work to do assessment we're not really qualified for, streamlined
service for the clients, she can visit, call, picks them up once a weeks so it’s quicker,
she talks to the doctors. If position was based here it would be even better”.
“It’s a very good model…I work at two services, one has it and one doesn’t, and I see
the difference…It’s had a big impact on the program – I would advocate for one CNS in
every community mental health service”.
“From what we can see, we think its improving patients’ journey, more continuity”.
“Really happy with service”.
“Working very well - great to have it on board.” “Women have increased access to
mental health care for depression.”
There have been some challenges in implementing the changes. Staff comments suggest
that these have primarily been the ‘teething difficulties’ associated with any new service and
are being resolved as they arise. Rotation or turnover of staff means that ongoing education
about the referral protocol is required. Several challenges that may require further exploration
are:
• Expectations regarding communication or feedback to midwifery and social work
antenatal clinic staff following referrals differed.

- 19 -
• Being located in a clinical setting, some comments suggested there may be a lack of
understanding by other staff of the non-clinical components of the CNS role. There may
be a need for further education around non-clinical parts of the role.
• Working within the scope of funding (i.e. focussing on depression) is sometimes
perceived by others as a lack of responsiveness to clients presenting with other mental
illnesses.
Initially the CNS focussed on the referrals from the antenatal clinic. The next step is the
development of similar protocols for referrals from the maternity ward. A participant
suggested increasing the CNS presence at the maternity ward would be useful:
“Maybe she could come up once a week to the ward and make herself more visible”.
5.1.5 KEMH Childbirth and Mental Illness Clinic ( CAMI)
The MBU/CL CNS role is divided equally between the MBU, which provides inpatient care
for mothers with severe mental illnesses in the postnatal period, and the CAMI clinic, which
provides comprehensive antenatal care from a multidisciplinary team for women with serious
mental illness. The MBU accepts referrals state-wide, and the CNS role has primarily been
used to increase the support and education available for rural and regional health
professionals. The CAMI clinic sessions form the clinical component of the MBU/CL CNS’s
role.
As well as providing direct treatment and care to women at the CAMI clinic, the MBU/CL
CNS has worked with the clinical midwife to improve incoming referral processes. As a result,
when a new patient arrives at the clinic, staff have greater knowledge of who she is and her
history, allowing them to provide better care from the beginning. In addition, a staff member
described the valuable role the CNS has played in coordinating care at the time of birth for a
small number of very ill women:
“The admission is for obstetric care, but there are severe mental health issues – [the
CNS] coordinates the gap with the hospital. Things like that reduce trauma for the
woman. Psych nurses will ‘special’4, and there’s a need for really good, clear
communication. [The CNS’s] familiar face and liaising can bridge the gaps.” “Her broad
knowledge and scope is fantastic for coordination - bringing together the psychiatric and
obstetric, which work very differently”. 4 Provide special care involving increased allocation of nursing time to a single patient.

- 20 -
As patients attending the CAMI clinic are often identified as being at high risk of relapse during
the postnatal period, a guideline has been developed in close collaboration between CL and
the MBU outlining the process for CAMI clinic patients referred to the MBU in the immediate
postpartum period.
5.1.6 KEMH MBU contact child health nurses at disch arge
Child health nurses have a schedule of standard visit times, including checks at 6-8 weeks,
3-4 months and 8 months after the birth. Additional or opportunistic visits are sometimes made
where a contact has been missed, EPDS screening indicates increased risk of depression, or
extra support is otherwise indicated. Consultation with the child health nurses found that they
were often unaware until the next routine visit that the woman, their client, had been admitted
and discharged from the MBU. The lack of information resulted in child health nurses feeling
ill-equipped to provide optimal support. A new procedure has been established where the child
health nurse is contacted upon the woman’s admission and at discharge from the unit. In some
cases, joint home visits are arranged, where there is mutual agreement by the patient, MBU,
and the child health nurse.
5.1.7 Child health nurses referral to psychologists via ATAPS referrals
The Access to Allied Psychological Services (ATAPS) program enables GPs to refer
patients to allied health professionals for up to 12 sessions of individual or group psychological
services by allied health professionals. During the scoping and consultation activities of the
NPDI service model, it became apparent that one of the areas where referral improvements
could be made was following the identification of depression risk through routine screening by
child health nurses. The child health nurse would refer to a GP, who in turn would provide a
referral to a psychologist or other appropriate provider. Waiting for a GP’s appointment could
lengthen the time before the woman saw an allied health professional to receive focussed
psychological strategies under the ATAPS program, and in some cases the expected referral
may not occur.
The CACH CNS has worked with the Perth North Metro Medicare Local (formerly Osborne
GP Network) to enable child health nurses working within the North Coastal Zone to refer
directly into the ATAPS program, with a GP appointment arranged concurrently. The Perth
Primary Care Network is developing similar pathways for referral into the ATAPS program by
child health nurses. The implementation of this referral system under both organisations will

- 21 -
provide more streamlined access to perinatal psychological services for women identified as at
risk of depression by child health nurses.
The CNS has also played a valuable role in informing child health nurses of changes in
referral pathways such as the ATAPS program.
[What, if anything, are the best things about the service model so far? What achievements
has it had?] “The collaborative work with organisations within the community. Not just the child
health nurses. Initially there was no clinical component, so the networking – ‘who's providing
what?’ ‘how can I support the non-government organisations?’ that’s been huge – [the CNS is]
fantastic in building those. And the outcomes – e.g. working with GP networks, there have
been good results with ATAPS, it’s a really valuable addition for nurses”.
“I hadn't used the GP mental health plan, so learning how to use it has given me more
options”.
5.1.8 Other improved knowledge or availability of r eferral options
In addition to these formal referral system improvements, the three CNS positions have
been active in providing information to health professionals about referral options for perinatal
mental health. This occurs during one on one collegial support, as well as group sessions such
as the in-service sessions provided to child health nurses by the CACH CNS, and the
videoconferencing sessions and roadshow activities the MBU/CL CNS provides to rural and
regional health professionals. Further information is provided in the Collegial Relationships
section of this report. A common theme was increased knowledge and accessing of the
referral options available, including clarifying any misconceptions. A few examples are shown
below:
“There’s the extra option of referral to [CACH CNS’s] service, or if I’m unsure where to
refer to, she can advise.”
“When we first started we did a session on MBU referral pathways. It turned out that
some people hadn't been referring as they thought the MBU didn't take women with
psychosis”.
“[Improvements in our regional service include] “Linking in with the preconception clinic
[CAMI clinic initiative that provides preconception counselling for women with serious
mental illnesses related to genetic risks and medication decision making].

- 22 -
One mental health service indicated they get more referrals since the CNS position
commenced.
“We get more referrals from Osborne Park than we used to because of the specialist
PMH nurse, and she knows about us”.
As these referrals follow an assessment, this comment suggests that more of the women who
would benefit from mental health services are being referred.
5.2 Qualitative themes relating to ongoing relati onship building and collaborations
A number of themes related to ongoing relationship building and collaborative activities
were identified from the stakeholder interviews. They all related to different aspects and
outcomes of bringing people together and creating ‘bridges’ between services, including:
1. Communication and networks
2. Systems improvements
3. Collaborative projects
4. Gaps, challenges and opportunities
Theme 1, communication and networks included descriptions of a range of activities
such as steering committees and working groups, videoconferencing and training sessions,
and spending time with people resulting in increased contact, discussion and understanding by
providers from a range of services. In some cases the CNS acted as a bridge between two or
more services within one hospital, in others they created forums of multiple organisations to
share knowledge and work together to achieve goals.
For instance, the CNSs have been involved in improving links between the maternity
services and psychiatric services in the hospitals where they work:
“Misunderstandings come up. [CNS] helps fill the gap, and clear up
misunderstandings”.
They have also helped staff in these settings have a greater understanding of the other
systems their patients are interacting with, such as mental health and child health and
community services:
“[CNS] helps me and the midwife know the process of psychiatric system which is quite
different”.
“A recent development is the involvement of [CNS]. A huge help - her child health
expertise. Services are so patchy, with narrow inclusion criteria, it’s really helpful to

- 23 -
have her consult with us about what’s available. And to discuss child health and mental
health issues, which interact”.
The CNSs also encourage hospital staff to involve relevant services and encourage
communication and collaboration, for example:
[What impact has the service model had on networks, collaborations and partnerships
between agencies providing services to women in the perinatal period?] “Linking in with
From the Heart and those services. Awareness of country clinicians, of more agencies”.
Beyond the services they work within, the CNSs have been involved in bringing together a
range of services. Comments about the meetings, steering committees/working groups and
videoconferencing activities reflect the networking value of such activities:
“[CACH and MBU/CL CNSs] organise a meeting for people working in perinatal mental
health.” [How could the service model be improved over the next 12-18 months?] “My
ideal - continue liaison meetings that [CACH and MBU/CL CNSs] have set up – to get
together, find out what other people are doing, swap info e.g. on how to run a PND
group, referral pathways. Coffee morning format is good”.
“I’ve seen in the Ellenbrook area, an increased linking and focus on perinatal mental
health”.
[Describing steering committee/working group] “Kept in the loop of what services are
available, where to refer clients, how I can be of assistance”.
“A lot of regions are coming together and sharing experiences and stories. A forum for
both education and networking - who in each region is dealing with perinatal mental
health”.
The committee provided a forum where professionals could problem-solve and share
information about their services. For example, one interviewee mentioned an unfortunate
situation, that was tabled at a committee meeting, where services had not worked together
effectively to meet the needs of a family and many gaps in support had occurred. “The steering
committee discussed it - this really helped, let people know what other people were doing”. By
gaining a better understanding of what each of service offers and how they operate, services
can aim to reduce gaps in the support available to clients.
In some situations, the relationship building goes beyond the individuals involved, and
takes steps towards building broader understanding and communication between whole
services or even agencies:

- 24 -
“There’s been a huge impact - a greater understanding for MBU staff of role of child
health nurses and improved communication out to child health nurses from the MBU.
And it’s given Adult Mental Health more focus on baby. It has really opened up
communication between different agencies”.
Nevertheless, as discussed in the ‘Gaps, challenges and tensions’ theme there is still great
scope to build stronger inter-agency relationships between AMH, Women and Newborn Health
Service and CACH and facilitate easier collaboration between agencies
Theme 2, Systems improvements primarily include the referral systems improvements
that have been detailed above. In addition, there have been improvements in the recording of
data, which will provide increased information quality. For example:
“EPDS scoring. [CACH CNS] ran reports and found some areas were not recording well.
She has dedicated time and focus to EPDS scoring, making nurses more aware.”
Theme 3, collaborative projects relates to the actions and outcomes that have resulted
from bringing people together and building relationships. As outlined throughout the report, the
CNSs regularly work collaboratively with other agencies or health professionals. Some of the
interviewees described involvement in collaborative training, clinical projects, or systems
improvements, and generally indicated that these experiences had been positive and
successful. More detail is provided in the relevant sections of the report, but examples include
activities in Ellenbrook. Several participants outlined the objectives met by the working group
so far, and suggested there has been an increase in focus on perinatal mental health.
“Since the working group developed, a number of stakeholders have been committed to
improving perinatal mental health services.”
Specific activities by group members were also outlined, including obtaining funding and
implementing several perinatal service projects.
Increased communication about perinatal mental health can lead to an increase in focus
and service activities on this topic, as described by one service provider:
[“Has the service model impacted on knowledge of perinatal mental health?”] “Definitely
increased in our program. For example we're doing mental health week activities, with
some of the info from [CNS]. The profile and information has increased, and giving the
same information in different ways helps reach more people”.
Relationships with GP Networks have facilitated the improvements to ATAPS referral
systems, and provided a potential solution to barriers faced by the CACH and AMH CNSs in
implementing co-facilitated perinatal wellbeing groups.

- 25 -
There have been many successes and achievements in relationship building over the first
21 months of the service model. Nevertheless, various challenges and gaps were identified.
Also, in bringing together groups of people to work together, it is almost inevitable that some
conflict will occur. Participants were asked about any challenges or shortcomings of the
service model, along with suggestions for ways to improve it.
The final theme is Theme 4, Gaps, challenges and opportunities , which provide potential
avenues for further improvements. Within this theme, the subthemes were:
• Catchments Differ
• Scope of Practice Differs
• Perceived Priorities Differ
• Information Sharing
• Community Capacity Building Challenges
Catchments Differ
The first set of challenges relate to bringing together maternity and child health services
with mental health services. Differences in clientele, systems, expectations and perceived
attitudes create various challenges in working together in a streamlined and collaborative way.
The CNSs and their managers identified a significant difficulty in the form of multiple barriers to
implementing joint projects between the AMH and CACH CNSs. This has been a source of
considerable frustration for the staff involved:
“There have been a lot of roadblocks. Getting the PND groups running has been a massive
fight. It’s in our MOUs but there are so many problems – who holds the notes, the risk, who
runs it, how, etc etc. Also there’s no funding or plan for the resources needed”.
“We are MOU’d to do a PND group. We both brought clinical skills – that was the expertise
we brought to the position. The biggest frustration is the thing we’re best at and employed to
do is the last thing we were able to do”.
Nonetheless, the CNSs remain committed and positive about the joint groups. Ongoing
efforts are being made to overcome these obstacles and progress is occurring.
Communication at various levels between the agencies will continue to facilitate progress.
A related issue is the catchments of each of the CNSs. For example the catchment of the
AMH CNS is constrained to Osborne Park Hospital clients, whereas the CACH CNS works in a
much larger North Metropolitan geographical area that contains multiple hospitals. The
MBU/CL CNS’s clinical work is primarily within the CAMI clinic, which provides antenatal
services.

- 26 -
These catchments have limited the ability for patients to be referred between the three
CNS’s depending on their level of depression risk/severity, as was envisioned in the planning
of the model.
“Boundary issues have been difficult – [AMH CNS] the Osborne Park clients, while [CACH
CNS’s boundaries are] geographic.”
Scope of Practice Differs
The different focuses of specific agencies can create challenges in collaboration and
relationships, for instance whether the CACH CNS can work with antenatal women. Similarly,
the AMH mandate is to provide mental health services to adults, however some participants
working in child health feel this can lead AMH or mental health services in general to “forget
the baby”. Because the mother and baby are so closely linked during the perinatal period, too
narrow a focus may limit the effectiveness of interventions directed at either party. Several
participants mentioned they found it easier to engage with some organisations and professions
than others:
“A lot of not-for-profits that are already focussed on PND are very helpful. Need mental
health/clinical/medical/GP services to help - its harder to get them involved.”
“Population health, child health nurses, midwives & GPs easier to reach than Mental
Health”.
“I feel more engagement with population health”.
However, the differences make it even more vital that strong relationships are built between
the agencies focussing on adults or infants in order to comprehensively meet the mental health
needs of women and their families in the perinatal period.
Perceived Priorities Differ
Another issue perceived to affect willingness of different organisations to work together on
perinatal mental health issues is the level of priority placed on perinatal mental health. Three
participants expressed concerns that some mental health services may not appreciate the
importance of treating perinatal depression:
“PMH is seen as a 'soft end disorder' - they [psychiatrists at the service I work at] don't
understand the risks”. “Probably hasn't improved access to our service - old fashioned
psychiatrists don't let them through the door.”
“Perinatal mental health is seen as ‘not mental health’”
“It’s bigger than [CNS], getting mental health to realise that depression is important,
women die”.

- 27 -
Several comments suggest that there is goodwill towards strengthening these relationships.
For example one participant involved in establishing the videoconferencing training sessions
for rural and remote practitioners said:
“Currently the VC training is mainly used by non-mental health staff. [MBU/CL CNS] is
going to contact mental health and find out what they want, why aren't they accessing it
more - they're our target group. If it’s mainly population health and child health
accessing it, why not mental health? Could be timing etc.” and “When one on one at
discharge mental health is great, but not accessing it”.
One participant from a mental health service spoke very positively about the relationship
building activities of the CNSs, and indicated having staff with time dedicated to this task is
valuable:
“It’s good to have the liaison with other perinatal mental health services, colleagues you can
consult with. Prior to this position, [name] used to get around, but I haven't seen anyone for
a few years”.
Another participant said “Building relationships is a challenge, it takes time, but working
well”.
Information Sharing
As well as the broad interagency and interdisciplinary relationships described above, there
have been challenges when bringing services together. For example, the issue of information
sharing between antenatal clinic staff and mental health services was discussed by several
participants:
“There’s a problem around sharing of info. After the referral to [the CNS] you don't know
what’s happening with it - not the psych assessment, but whether they've been seen or
have an appointment or the case is closed. Talked to [CNS] about it but don't know how
it will be resolved. If [CNS] sees a client here, the notes go in file, but if she goes on a
home visit they don't end up back here. Privacy is an issue, we would need to agree on
a common policy”.
“Midwives and doctors don't know the outcome for the patient e.g. if they have an
appointment, if they're ok etc.”
“Its confidential mental health information. As long as the midwife knows the client has
links, that’s enough”.

- 28 -
Staff referring clients to the AMH CNS position expressed a preference for more feedback
such as whether the referral has been acted on, or information that may impact on the clients’
care needs within the antenatal clinic. These staff members are of the view that increased
knowledge would improve their ability to provide optimal care for their clients. Conversely,
mental health staff members are reported to generally hold the opinion that the best care of
women involves maintaining privacy regarding mental health assessments and treatment.
Furthermore, the clients’ notes are held in different places depending on where they are seen
(e.g. at the antenatal clinic or on a home visit), so access to these notes by clinic staff varies
accordingly. There may also be different perceptions regarding how much information
antenatal clinic staff members receive. Having a shared understanding of what information
staff currently have, the benefits and disadvantages for the patient from each approach to
information sharing, and the basic legal/ethical frameworks each profession or service is
making decisions within may be a useful first step in resolving this issue.
Community Capacity Building Challenges
The formation of the Ellenbrook Perinatal Mental Health Working Group and other
stakeholder groups have not been without challenges. In particular, although bringing together
a range of stakeholders from different sectors provides a breadth of expertise and
perspectives, it also brings together diverse expectations, priorities, and ways of working. At
times there has been conflict within the group regarding the best approach to meeting service
needs, and the pace of progress. In part this reflects the different organisational cultures: for
example, government agencies tend to require more extensive planning and scoping stages
and documentation as part of ensuring best practice, whereas the community sector tends to
lean towards providing services at the earliest opportunity. Despite the challenges, the working
group has largely maintained its membership, increased focus on perinatal mental health,
encouraged the strengthening of relationships between agencies with a perinatal mental health
focus, undertaken strategic planning activities, and provided one 10 week postnatal
depression group with crèche facilities.
Two respondents expressed some dissatisfaction with not being fully included in networks,
collaborations and decision-making, however this went beyond the current project to the
broader perinatal mental health area.
A common theme was challenges related to time and the broad scope of the role, however
this goes across all three expected outcomes so is discussed separately later in the report.
Other suggestions and gaps were more varied, including referral information, and strategies to
continue integrating non-government organisations.

- 29 -
“Would help to have a flow chart with names and contact details for referrals.”
“CNS may have sent one out and I just missed it, but it would be good to have a list of
criteria for referral to her service - who she is looking for, anyone that’s not appropriate -
to make sure I'm making appropriate referrals.”
“Interesting that AMH CNS position is quite close to the city. Would prefer satellites”.
“Don't have a sense of a plan - that would be useful. If there is one I don't know of it. Let
people know. And how people including non-government sector can fit in with that. But
first stage has been getting direction”.
“Continue working together. Using what’s existing, education for non-government on
screening and referral”.
5.2.1 Summary of Relationship Building Expected Out come
Overall, the service model has achieved a great deal in building relationships with, and
between, different organisations serving women during the perinatal period. Achievements
have included bringing together a range of stakeholders with a focus on perinatal mental
health, improving referral systems for women with or at risk of depression, increasing
practitioners’ knowledge of the other health systems their clients interact with (e.g. mental
health or child health), and extensive education and training activities. A central challenge is
overcoming barriers to the implementation of joint projects between the AMH and CACH
CNSs, although progress towards this goal is being made through ongoing efforts. Other
challenges include continuing to build and strengthen relationships between services and
agencies with different systems, organisational cultures, expectations and agendas. Again, the
effort and goodwill of many people is creating progress towards stronger relationships.
5.3 Clinical Service The second expected outcome is clinical service. Each of the three CNS positions includes
a clinical component, provided to individuals or groups. For the hospital-based positions (AMH
and MBU/CL), there is a relatively clear-cut clinical role. For the AMH CNS, this involves
assessment and follow-up of women identified by the maternity services as at risk of or
experiencing depression. For the MBU/CL CNS, clinical service provision at the CAMI clinic
was built into the role. In addition, the MBU/CL CNS co-facilitates an antenatal support group
for women with or at risk of depression. A staff member from the Department of Psychological
Medicine (formerly known as CL) is the other co-facilitator. The MBU/CL CNS also undertakes
some clinical activities within the KEMH MBU, mainly follow-up of former CAMI clinic patients

- 30 -
who attend the MBU after giving birth. A KEMH perinatal psychiatric also been established via
videoconferencing in collaboration with WACHS for women in regional or remote areas.
The CACH CNS position is not affiliated with a specific clinical service. Nevertheless, the
CACH CNS has identified several areas where she can provide valuable clinical support or
services. This has included several joint home visits, and referrals from child health nurses. In
addition the CACH CNS co-facilitated a postnatal support group and provided individual
clinical service to participants. She has also established a collaborative clinical service with the
Osborne Obstetric Psychiatric Liaison Clinic, with clients identified as at mild-moderate risk of
perinatal depression are referred to the CACH CNS.
5.3.1 Occasions of Service and Postnatal Depression and/or Women’s
Perinatal Support Groups
Individual occasions of service have been recorded by each of the CNSs. It should be
noted that the location, duration or type of service provided is likely to differ across the roles,
so direct comparisons may not be appropriate. Occasions of service provided by the AMH
CNS are presented in Table 1. All have been provided on an individual basis.
Individual Occasions Of Service
Month New
Referrals
Individual
assessments
Patient related
occasions of
service
Occasions of
service for
fathers/
partners/
carers
Individual
follow-
up/monitoring
visits
Sep 10 – Feb 11 42 32 12 7 144
Mar 11 – Aug 11 59 45 16 3 137
Table 1. AMH CNS Occasions of Individual Clinical S ervice
Table 2 shows the occasions of service provided by the MBU/CL CNS. This includes patients
seen individually, in the antenatal group, and via video-conferencing consultations.

- 31 -
Individual Occasions Of Service
Period New
Referrals
Individual
assessments
Patient related
occasions of
service
Occasions of
service for
fathers/
partners/
carers
Home visits
Feb 10 – Aug 10 111 56 258 6 3
Sep 10 – Feb 11 121 44 219 6 3
Mar 11 – Aug 11 56 nr 128 nr nr
Table 2. MBU/CL CNS Occasions of Individual Clinica l Service
*nr = not recorded
The CACH CNS has provided 43 occasions of service on an individual basis to 17 women.
She has also co-facilitated an 11 week postnatal support group with 6 participants, and
provided perinatal depression awareness raising sessions to approximately 50-60 attendees of
Ngala supported playgroups and foster carers.
5.3.2 Challenges and Plans for Clinical Service Pro vision
Each of the CNSs has faced different challenges in developing, maintaining or managing
their clinical role. The CACH CNS plans to expand her clinical role, having concentrated more
on stakeholder relationships and community development in the first year of the service model.
As described in the previous section, preparations have been made for the CACH and AMH
CNSs to jointly run perinatal support groups, however a number of obstacles have delayed
implementation.
The AMH CNS has initially focussed primarily developing the referral pathway from the
antenatal clinic to the obstetric/psychiatric liaison service. Her plans include more involvement
with the maternity ward to consolidate a similar process and protocol for referrals from the
ward, as well as increased focus on community activities.
The MBU/CL CNS has found that some of her regional activities, especially the travel
required for the perinatal mental health roadshow have impacted on her clinical role at the
CAMI clinic. As a result of having been away, she was unavailable to undertake CAMI clinic
activities for a period of time. She is also considering activities related to “how we work with
fathers/partners”.

- 32 -
5.3.3 Stakeholder perspectives
The interviews yielded three themes, relating to improved clinical service provision, time
constraints, and suggestions for new service activities. Stakeholder feedback indicates that the
CNSs’ activities are improving the clinical service provision for clients:
“I’ve referred one client to [CACH CNS’s] home visiting service. It was really good, the client
was hard to find a good fit for - anxiety, past mental health issues, family issues as well as
sleep and settling – [CACH CNS] was great. It was beyond what I could provide, and even
what [name] could [provide] in the enhanced home visiting. A great fit for the client. So all
very positive”.
“[AMH CNS] has a clinical component, so patients can be supported. There was a gap
before - if they were referred to community mental health they often weren't picked up –
they were seen as not severe”.
“[AMH CNS’s] in-home visits are fantastic for clients e.g. if they're waiting on a
psychiatrist appointment”.
“Hope it continues. Its great to have it, provides expertise to our clients”.
The main shortcomings or gaps identified by stakeholders regarding the clinical services
provided by the CNSs were related to time constraints . Although interviewees were pleased
with the service provided, additional time would allow increased accessibility and increased
face-to-face service provision such as home visits:
“Main limitation – there’s a limited amount of time - reporting and admin requirements
impact on time. Face-to-face would be better but time constraints.”
“Psychiatrists would like to have her doing home visits, but one can take up an
afternoon.”
“Also it would be great to have the position available through all clinic times. She’s
getting busier and busier, harder to get hold of.”
“Not having been there consistently can make it difficult - she sometimes misses the
established communications with patients.”
“A challenge for [MBU/CL CNS] to keep all the balls in the air. More time with our
service would be nice. But that would be at the detriment of the MBU.”
“Would be good if all areas could have the groups and one on one support”.

- 33 -
There were also suggestions for new service activities , including an increase in services
for fathers during the perinatal period:
“Statistics show one in three with PND is a dad. They need to be included more both as
a support for female partners and for the men”. “In the Health dept no-one seems to be
charged with looking after men/fathers.”
“Engagement for dads - lacking at the moment. Biggest gap. And I’d like to see more
rotation of staff through services - would be great if they could all spend time at the
MBU. Clinical supervision on complex patients.”
One participant suggested a general change in antenatal education to better prepare clients
for the role of parenting:
“There’s scope to improve antenatal education, as the focus tends to be on the birth,
perhaps a little bit on parenting – but it needs to cover how to psychologically deal with
parenting”.
Finally, the issue of being focussed on depression alone was raised by some participants.
The CNSs had to make it very clear early on that the funding of their positions requires this
focus, as the mental health services they work with generally have a broader focus and this
caused some conflict. Although this seems to be generally accepted, some participants
expressed the view that expanding the service to other women with mental health issues
would be valuable, for example suggesting:
“Broader-based access to patients - being depression only misses out a significant
percentage of the population”.
5.3.4 Summary of Clinical Service Expected Outcome
Over 400 women have been referred to the CNSs, and 947 patient related occasions of
service or follow-up visits were provided. Approximately 180 individual assessments were
conducted by the CNSs. Although patient feedback does not form part of the evaluation,
stakeholder feedback suggests that this service model is providing valuable clinical services
resulting in a better overall package of care for women experiencing or at risk of depression.
Without an in-built clinical role, the CACH CNS has had to identify suitable opportunities for
a clinical caseload, and first address the significant community development portion of the role,
so this area of clinical service has been slower to develop. In addition, the CACH and AMH
CNS have faced a number of obstacles in implementing jointly facilitated antenatal or postnatal
groups, but continue to work towards achieving this aim. The most common challenge
identified by stakeholder comments is time, with various clinic staff expressing a wish for

- 34 -
increased hours by the CNSs, and suggestions of further service activities that could be
provided if time allowed.
5.4 Collegial Relationships The collegial relationships component of the service model includes the provision of advice,
support and information to health professionals to assist them in providing optimal care to
women with perinatal depression5. The CNSs record the number and description of
professional development session, perinatal depression education and training, and individual
consultations. Health professionals with less experience in perinatal mental health benefit from
the specialist knowledge of the CNSs, while those with extensive experience are able to share
ideas and work collaboratively with the CNSs to achieve common goals.
Several of the activities described above – such as the perinatal mental health roadshow
and consultations with other services – constitute collegial support as well as improving
referral pathways and strengthening relationships with other agencies. In addition the CNSs
frequently provide training and information sessions to professionals working with perinatal
women.
The CNSs collaborate on some of these training and information sessions. For example,
the AMH CNS and CACH CNS have co-facilitated professional development (PD) sessions for
the AMH staff (20 participants), and child health nurses in the Stirling region (11 participants).
The MBU/CL CNS has co-facilitated three professional development sessions with the CACH
CNS and two with the AMH CNS, including presentations to the Rockingham/Kwinana Mental
Health Service (6 participants) and Mirrabooka Mental Health service (8 participants).
Further to these joint PD sessions, the CACH CNS has provided a further 20 sessions, and
the AMH CNS a further 3 sessions. Eight of the PD sessions were conducted for child health
nurses by the CACH CNS between March and August 2010, for which attendance numbers
were not recorded. The PD sessions from September 2010 – August 2011 were attended by
over 132 health professionals, including 42 Aboriginal health workers state-wide, child health
nurses in the Stirling and Joondalup regions, midwives at Peel Hospital, midwives and social
workers at Osborne Park Hospital and the 4 newly appointed NPDI CNSs from regional WA.
Collaborations have included PD sessions facilitated with mental health professionals from
Infant Child Adolescent and Youth Mental Health Service, KEMH Department of Psychological
Medicine, or with health professionals working in Aboriginal maternal health.
5 Although there is some overlap, the collegial relationships component focuses on the provision of support, advice, information and professional development to individual practitioners (whether provided one on one or in groups), whereas the relationship building component of the role focuses more on broader stakeholder relationships, for example strengthening links between services or agencies.

- 35 -
In addition, the MBU/CL CNS and management staff from the MBU and CAMI clinic have
undertaken a range of activities aimed at ensuring health professionals can access the
expertise of these services. The MBU/CL CNS has presented variations of “An Overview of
Perinatal Mental Health, the Childbirth and Mental Illness Clinic and the Mother Baby Unit6” to
1077 Community Mental Health Services staff during her first 6 months in the role. Over the
next 12 months the CNS presented to a range of health professionals (143), including Best
Beginnings staff, KEMH midwifery students, Armadale hospital midwives, a psychiatrist and 4
psychiatric registrars at Joondalup Mental Health Unit, paediatric staff at Princess Margaret
Hospital, Alma Street Mental Health Service, and to rural and remote midwives via Telehealth.
The combined training activities represent a significant amount of education about perinatal
mental health, and expansion of the number and range of health professionals aware of the
CNSs’ role and the services available.
The formal collegial support outlined above also provides an opportunity for health
professionals to meet the CNSs and learn about what they offer. This provides a foundation
from which health professionals are more likely to contact the CNSs informally for support and
advice regarding perinatal depression. The MBU/CL also provides clinical supervision to staff
from the Indigenous Perinatal Mental Health Service in Carnarvon. Frontline staff who have
accessed informal collegial support from the CNSs indicated it has been valuable and
improved confidence in working with women with mental health issues:
“I called on [CNS] for support when I had a mum that I wasn't sure how to manage - she
was great”. “I'm becoming more comfortable dealing with mums in the community with
mental health illnesses”. “Yes, the collegial support has been really good. Knowing how
to deal with situations”.
“And supports for staff are fantastic. She comes and updates on mental health and
infant health, debriefs…” “Really helpful, the updates are great. I’ve learnt a lot about
what services are there - I moved from [another area] six or nine months ago, so it’s
been really good – [CNS] knows lots of programs, like the Raphael Centre attachment
one. And keeps us updated on things like PND awareness week and resources for
that”. [What is the best thing about the service model?] “Having someone to debrief with
- knowing that’s available. Some of us have more experience with mental health than
others”.
6 Sometimes the presentation focuses on either the CAMI clinic or the MBU 7 As a result of the way the data has been recorded, the joint sessions have not been excluded from the MBU/CL counts, whereas they have been removed for the other CNS positions

- 36 -
“I get a lot out of it, mostly about clients but also professional development, self-care.
Both [the videoconferencing session and other collegial support provided] are very
good. Its really useful for a remote service like ours”.
Other comments in response to the question “Has the service model impacted on the
availability of collegial support for health professionals related to perinatal mental health?” are
listed below. The majority indicated there was an increase in support as a result of the service
model. Some health professionals already have established collegial support and referral
networks, and many years of experience in the area, which may reduce their need for some of
the types of support offered through the service model. However, it takes time for most new
health professionals to reach this stage, and many experienced professionals also value the
perinatal mental health specific information and support provided.
“Yes, I think so. A lot of regions are coming together and sharing experiences and
stories. A forum for both education and networking – knowing who in each region is
dealing with perinatal mental health.”
“Certainly has been. For example a few times when [psychiatrist] hasn't been there but
[CNS] has. She’s been very supportive - a great resource of knowledge. And support.
She’ll say 'that was a bit traumatic - are you feeling ok?'.”
“Yes, suppose - getting to know what’s going on, reasonably”.
“Yes, still room to improve, but has got better over the six years I've been in this job”.
“I'd say so, there’s more support”.
“The new PMHPA8 - get newsletter and they seem to be quite active out this way. The
support is limited to within the committee”.
“Already fine”.
“Definitely, very happy to call [CNS] etc”
“Do consult/phone [CNS]. Getting harder to get hold of as she gets busier. Ward info on
how to get hold of her is unclear. Clinic staff are very in touch with her”.
“[CNS has] been really useful, we’ve collaborated on a couple of patients in the CAMI
clinic”.
8 The Perinatal Mental Health Professionals Association has been active for many years, however this comment may indicate an increase in networking/knowledge of perinatal mental health organisations and resources.

- 37 -
“Absolutely - in the North I’ve had anecdotal feedback the staff feel very comfortable
contacting [CNS]. Provides nurses with support in managing situation and referrals”.
“Serious mental illness wasn't my area – I feel supported talking about it if I go to [CNS].
She adds validity and expertise”.
“Got to be. Though I'm not in clinical service”.
The comments from stakeholders generally fall within one theme of more support , with sub-
themes of more informed, more confident with patients and less need (i.e. some participants
indicated their existing supports were sufficient, or they had less need for support than a
clinician).
5.5 Service Issues and Staff Perspectives Where analysis of the interview data from stakeholders outside the service showed themes
repeated across the different outcomes, they are considered to be reflective of broader service
issues. In addition, interviews were conducted with the three North Metropolitan CNS positions
included in this evaluation, and with two of their counterparts in the South Metropolitan area
and the South Coastal Zone9. These interviews were conducted to gain background
information about service activities described earlier, and also to identify aspects of the service
model, the processes undertaken, or the resources available that act as facilitators or barriers
to envisaged or ideal implementation of the service model. Key topics included scope and
clarity, where the positions ‘fit’, supports and resources and extending the service.
5.5.1 Scope and Clarity
One of the central features of the CNS positions is their broad scope, covering relationship
building or community development, clinical work as well as the provision of collegial support.
This is one of the strengths of the model, as when it works effectively, the CNSs are able to
target multiple levels (individual clients, health providers and health systems) and work
towards more integrated service provision for women in the perinatal period. By having a
relatively large catchment area, the CNS’s are able to develop broader networks and share
their expertise and support to a wider group. Except where a particular component has been
planned by managers in advance, the CNSs are also given considerable freedom to choose
how to develop the service and which activities or approaches to take as long as they are
9 The two additional CNS’s were included for several reasons. Firstly, final evaluation reporting is likely to integrate findings from across the metropolitan area. Secondly, a broader pool of participants increases the identification of common issues rather than individual issues. Thirdly, relationship building is expected to occur across the five CNSs. However, issues are only included here that are relevant to the service model within the North Metropolitan Area – issues completely unique to the South Metropolitan area are not included in this report.

- 38 -
within the framework provided by the MOU. CNSs can therefore develop the service
responsively to the gaps, needs and setting in which they work.
These features are among the strengths of the model, yet they also create numerous
challenges. The first of these relates to role clarity. Setting up a new service, with such a broad
framework creates a very open-ended role for the CNSs. Role clarity is the degree to which
expectations about procedures, goals and performance criteria are clear and sufficient role
information is available, and research has shown it to be associated with higher job
satisfaction (Whittaker & Mckinney, 2009). Issues relating to role clarity and ambiguity came
up repeatedly in the interviews10 as one of the challenges, as the comments below illustrate.
“This [the expected outcomes in the MOU] was a good framework at the beginning. I felt
a little bit like I was given nine dot points on a piece of paper and told ‘go figure it out’. I
was used to the clinical side, and had an interest in perinatal mental health, good
networking skills and good networks. But I realised they weren’t enough. The framework
was a useful structure… I find it really interesting. But what WAPMHU wants, what [my
organisation] wants, what other organisations want, what the community needs… it can
be huge. Deciding on scope is important”.
With so many choices regarding the service activities, the CNSs naturally tend to compare
their activities to those of the other CNSs in order to establish a performance benchmark, as
illustrated in the comments below. Given the anticipated differences in the roles, this may not
be the ideal way of establishing expectations.
“There’s lovely supportive management, but I don’t know if I’m on the right track, how to
compare with [another CNS’s] efforts etc.”
“The different areas are doing completely different things. At least once a week I think
“Am I doing the right thing here? Should I be doing what [another CNS’s] doing? Or
should it be what the doctors want?”
Although some degree of ambiguity is likely to be inherent in the roles, particularly when
they are newly established and the CNSs are simultaneously within the role, identifying the
needs of the role and designing the role, it may be useful to take steps to reduce role
ambiguity. Setting performance management goals and evaluating achievements is written
into the job descriptions. In addition, an orientation program has been initiated for new NPDI
CNS positions, including the WACHS positions that commenced in 2011. Nonetheless, there
10 Note that due to the smaller number of CNS participants and to protect confidentiality, multiple comments may be shown for each participant (whereas other stakeholder comments are grouped into a paragraph if they are by one participant on one topic). However, to be reported, the theme must be common across two or more CNSs.

- 39 -
appears to be scope for further role clarification. This may involve individual or group
processes that facilitate a plan-implement-evaluate cycle taking into account the specifics of
the role as well as where it fits into the broader service model and the home agency, or
increased input from managers regarding how the strategic plan can be operationalised. The
evaluation may provide an opportunity for reflection, discussion and further clarification of
roles. Several comments from the CNSs indicated that increased communication between
managers of the service model could be valuable. Over time, there seems to be some
reduction in role ambiguity, and a greater ability to enjoy the freedom of the role, however it
would be preferable to facilitate a quicker attainment of this clarity.
A second challenge related to the scope of the role is being ‘spread thin’. Many comments
from the other stakeholders, as well as the CNSs, related to issues of how broad or narrow
their focus should be, and the balancing of time allocated to the three different expected
outcomes. Challenges created by time constraints were a common theme among (non-CNS)
stakeholder comments, along with suggestions of how additional time could be used if it were
available:
“Not enough time - greater expansion of the role into postnatal follow-up”.
“The CNSs cover a large area, but in practice have to focus on a section of it.”
“The geographical area [CACH CNS] is expected to cover is unrealistic. It is too big for
one person to take on the North role.”
“Big geographic area to cover. Can spend all the time networking and not get to do
anything i.e. clinical. Ellenbrook’s been a lot of work.”
“Employment of more staff or perhaps the nurse being allocated to specific areas that
show a great need for perinatal mental health support or can demonstrate they are
willing to work in a more coordinated way.”
“A challenge for [CNS] to keep all the balls in the air. More time with our service would
be nice. But that would be at the detriment of the MBU.”
“Increase FTE. [CNS] needs to maintain collaborative relationships. If you don't work on
those they fall off. As she develops the clinical role, keep in mind those others are still
important.”
“Would be good if all areas could have the groups and one on one support”.

- 40 -
“Being less thinly spread. Would give her time to consolidate. It comes down to
opportunity cost. But it might be better to consolidate a few things than spreading
across so many”.
“Psychiatrists would like to have her doing home visits, but one can take up an
afternoon.”
“Main limitation – there’s a limited amount of time - reporting and admin requirements
impact on time. Face-to-face would be better but time constraints.”
“Also it would be great to have the position available through all clinic times. She’s
getting busier and busier, harder to get hold of.”
“Maybe she could come up once a week to ward and make herself more visible”.
“Generalise to other obstetric services and community mental health services.”
“More funding in Armadale. No NPDI money here”
As the CACH CNS has a large geographic catchment area, the CNS and managers agreed
at an early stage to select areas to focus on for specific activities, rather than trying to provide
all services uniformly across the entire North Metropolitan Area. The CNS identified several
areas to focus on based on analysis of EPDS screening data and other needs analysis.
Although this has been a necessary and effective strategy to contain and focus the role, it
does leave some areas with less coverage. Two comments from the stakeholder interviews
and online child health nurse survey suggest there is scope for more input in the Oceanic
region.
Not surprisingly, with so many potential geographic and service areas to develop, another
common challenge the CNSs identified is the sense their time is sometimes spread across too
many tasks to be optimally effective. This issue was raised by several of the CNSs, and
different approaches were suggested as to how to manage this issue:
“Would set up a program like this but limit to one hospital, or one area – get rid of being
spread so thin”.
“MOU needs to not be so broad. It needs to be narrowed down. You’re doing a lot of
things in the role, but are you doing them well? Might do one [expected outcome] to a
better quality.”

- 41 -
“It’s fantastic that there have been initiatives, but as a practitioner it’s frustrating, you
don’t have the time to do it well, which is less rewarding. There’s a huge sense of
responsibility”
“When setting up a new position – and it’s my first time in one – there’s difficulties
inherent in that. Difficulties in the scope of the position. I feel like have to keep cutting
down to what can realistically be done”.
“Got to be careful not to try and be everything to everyone – focus our energies and do
it well”.
Sometimes the time spent achieving one expected outcome impacts on the time available
to address the other expected outcomes. For example, in undertaking the Perinatal Mental
Health Roadshow, the MBU/CL CNS was away from her clinical role in Perth for longer than
she would have liked. Time was the main difficulty identified by participants in relation to her
clinical role at the CAMI clinic.
“Not having been there consistently can make it difficult - she sometimes misses the
established communications with patients. She's there about 3 times out of 4, but
because you may not see the woman for another 10 weeks that can impact.”
The MBU/CL CNS plans to focus more on the clinical role next year. To do so may impact
on the amount of regional relationship building activities she can undertake over this period.
Some stakeholders would prefer her to increase rather than decrease visits to regional areas:
“Can't rely on VC all the time. Would be good for [MBU/CL CNS] and others to get out
to these places for more face-to-face education, be in with the people”.
Similarly, the CACH CNS has plans to increase her clinical role in the coming year, which is
likely to require a reduction in time spent on building relationships. She has approached the
role in stages, focussing more on the relationship building and community development
initially, then increasing clinical activities. Yet another stakeholder pointed out the risk of losing
ground in the relationships that have been developed if insufficient time is available:
“Needs to maintain collaborative relationships. If you don't work on those they fall off. As
she develops the clinical role, keep in mind those others are still important.”
The balancing of the three components is likely to require ongoing management by the
CNSs. At the time of reporting, approximately 18 months of funding for the service model
remain. Each of the CNSs discussed plans for the coming 12-18 months, such as ideas for
new initiatives, progress on existing plans, consolidation of established components and areas

- 42 -
they may need to pull back from. It may be timely to consider the balance between starting
new activities and consolidation of established activities.
5.5.2 Where the Positions ‘Fit’
Another issue affecting the development of the service model is establishing where each
position ‘fits’ within the service model, and within the context of the organisation, specific work
settings and the broader range of services with which the CNS interacts.
Of particular importance to implementing the service model as planned is how the CNS
positions fit together. The service model diagram (Figure 1 on page 4) emphasises the links
between the positions and bringing together the different expertise of the CNSs. As outlined
previously, the different catchments of the three positions have limited the capacity for referrals
between the three CNSs, and various barriers to establishing joint groups have delayed their
implementation. These factors appear to have limited the degree to which the three positions
have a sense of being connected and are able to work jointly. For example:
“The position doesn’t really link... There’s a different catchment group – [MBU/CL CNS’s]
only birth at KEMH11…[AMH CNS’s] are only women that birth at Os Park, so there can’t be
any crossover with [MBU/CL CNS’s] catchment, so the diagram doesn’t really fit where the
three are linked in.”
Relationships between the CNSs are positive, described for example as “friendly”;
“good to relate to clinically”; “[CNS] and I contact each other, work closely”, and as providing
“collegial support, sharing the load a bit”. Furthermore, the CACH CNS and AMH CNS have
integrated some of their activities, for example the establishment of a clinical role where
women at Osborne Park Hospital identified as at mild-moderate risk of depression are referred
to the CACH CNS, and the inclusion of the AMH CNS into relationship building activities
commenced by the CACH CNS. There is also regular contact through monthly meetings
between all the NPDI funded CNS positions, supplemented by more frequent contact as
needed. Yet there appears to be scope to further strengthen linkages between these positions
in line with the strategic intent of the service model.
There were also a number of challenges in where the positions ‘fit’ within the service where
they are located. As the service model was conceptualised, and then specific placement of
positions negotiated with suitable collaborating agencies, there have been some issues in
aligning the two frameworks and philosophies within which each CNS works (the framework of
the service model, and the framework of the service within which they are located). For
11 Although the MBU/CL CNS’s role includes a statewide component as part of the MBU responsibilities, the clinical role at the CAMI clinic is confined to KEMH patients.

- 43 -
example, all of the CNSs working in a mental health setting commented on the challenges of
working in one area of mental health (depression), in a general mental health clinic:
“[At the clinic] there are needs for an ‘other mental illnesses’ nurse, not just perinatal
depression – has had limitations”
“Hard in clinical role – really hard – being only depression. If a woman has a pre-
existing psychosis etc to say I can’t see her – I’m in a mental health clinic! Trying to
incorporate into an existing clinic with its own framework is challenging”.
On occasion this appears to have limited the degree to which a CNS has been welcomed
into the clinic. Working with a narrower range of clients therefore created various difficulties in
working in a mental health clinic. That is not to say that a mental health clinic is not an
appropriate setting for mental health nurses focussing on perinatal depression. However,
ongoing support and education are required to alleviate some of the difficulties involved. At
some stage it may be appropriate to broaden the CNS roles or overall service model to include
other perinatal mental health disorders, however there is already a broad and demanding role
for each of the CNSs within the area of perinatal depression. Increased FTE would be advised
if the roles were to be broadened.
The WAPMHU state coordinator was responsible for strategic direction, with the services
providing operational line management for each position. However, the MBU/CL position line
management was split between MBU and the Department of Psychological medicine. Those
based within a hospital setting tend to divide their time across at least two locations (e.g.
based in a mental health clinic, with some time spent in the antenatal clinic). As is so often the
case with the service model, the ‘bridging’ role of the CNSs helps to create successes, when
the knowledge and relationships built within each area lead to improved systems,
communication, and service provision, yet it also create challenges.
“The operationalising of the role is hardest – and how it’s going to fit into the
organisation you’re being put in – do they know how to support the role? Also having
two directors – I had to work out who to go to for what and they don’t talk that much
about my role”.
These challenges were addressed through consideration of the issues, along with
discussion:
“Share and talk to people about the problem. I’m grateful to have [strategic and
operational managers and other personnel] for questions”.

- 44 -
It is generally recognised that multiple-reporting arrangements can be difficult, so in these
arrangements it is especially important to maintain effective communication and avoid
unnecessary duplication of tasks.
Across the service model, the CNSs indicated that some work settings have understood
and embraced the role more than others. Even in supportive environments there can be a
degree of isolation that comes from being a unique position within a service, particularly a
position that has been developed in a separate context and then placed within a service. The
CNSs have been active in establishing peer support networks among the NPDI positions as
well as similar positions across the state. As the number of positions has grown, the availability
of collegial support from other CNS positions has increased. Having another CNS within the
same agency (CACH or Adult Mental Health) has also helped the CNS’s as they have more
similar roles and systems to work within.
The service model has maintained a reasonable degree of stability in staffing, with the
original incumbents still in place in the CACH positions and the MBU/CL position. There has
been higher turnover within the AMH positions in both the North and South Metropolitan areas.
The South Metropolitan AMH CNS resigned in November 2011. The initial North Metropolitan
AMH contract position was filled from November 2009 until April 2010. After being vacant for
approximately 3 months the position was filled by the current CNS in August 2010. There will
also be a third person in the role for most of 2012, however this is to cover maternity leave.
Higher turnover and shorter lengths of time in the role is likely to impact on the development of
relationships, and other service initiatives. Although some turnover naturally occurs in any
service, it is recommended that the reasons for higher turnover within the AMH CNS positions
are explored, and any contributing factors addressed.
5.5.3 Supports and Resources
The availability of sufficient supports and resources can impact on the implementation of a
service model. The following types of supports and resources were discussed:
• Collegial and supervisory support – is important in providing forums for discussion that
help the CNSs establish a sense of direction in the role, especially in the early stages.
The availability of this varied between positions. Several comments reflected
appreciation that managers were supportive and allowed the CNSs to make decisions
and work creatively in their roles.
• Clinical supervision – some of the CNSs have clinical supervision. Clinical supervision
can provide an important support and facilitate higher quality clinical work, so it would

- 45 -
be useful for all of the CNSs to have clinical supervision arrangements in place. The
MBU/CL CNS currently provides clinical supervision to another service, and has
expressed a willingness to provide similar supervision to newly established positions
where appropriate. The most suitable type of clinical supervisor will depend on the
professional training and type of clinical work undertaken.
• Facilities and budgets – one of the obstacles in establishing the joint support groups to
be run by the AMH and CACH CNS has been finding a venue and budgetary issues
around crèche staff. One suggestion put forward was to provide a budget for running
the groups. Having identified the potential difficulties in jointly run groups, future plans
for joint groups within the North Metropolitan and other NPDI service model areas
should identify strategies to address these obstacles as early as possible, and where
necessary with management support. The provision of resources such as a car appears
to differ between the positions.
• Information and skills – for the most part, the CNSs appear to have sufficient
information and skills to work effectively. One CNS indicated that it would have been
useful to have more information regarding project management and information sharing
specifically in relation to working within the two systems in which she is employed and
positioned.
5.5.4 Extending the service
A number of participants concluded the interview by reiterating the value of the service model
or encouraging the continuation of the service model beyond the current funding period:
“Keep it going. It’s a great service”.
“Think it’s very good. Hope it continues. There’s a very experienced clinician doing it, if
funding is lost the position could be lost after 2013”.
“It’s a really great opportunity for the community to have this service available, and it will
grow and improve over time”.
“It’s been really good for WACHS”.
“Just great to have the resource available & be able to call [CNS]”.
“Great initiative, I hope goes longer than 3 years. It’s definitely of great benefit, helping
to demystify and destigmatise what a lot of our mums go through”.

- 46 -
6 Discussion and Recommendations The process and progress of the NPDI service model within the North Metropolitan Area
has been evaluated, focussing on the three positions that had been established for more than
12 months. The primary sources of data were stakeholder interviews conducted with 36
participants, and the service outputs provided in the CNSs six monthly progress reports.
Additional data was provided by two surveys of child health nurses.
Nearly all of the expected outputs outlined in the MOUs have been provided by the
CNSs. Several areas have been identified to explore for data for the final evaluation report,
including waitlist times for clinical services. Anecdotal evidence suggests that the AMH CNS
role has made a significant difference in reducing the time before women receive treatment or
support for depression; service data may be able to quantify this impact. In addition, if data is
available it may be possible to further measure the impact of initiatives with ATAPS referrals
and within the MBU. In addition, repeating the child health nurse survey to compare perceived
needs and rates of training completion will allow comparisons in the final evaluation. Data
showing EPDS screening levels within the North Metropolitan Area may also be available for
comparisons and inclusion in the final evaluation.
Stakeholder feedback confirms that significant progress has been made towards each of
the three expected outcomes. Notable successes have been achieved in all three outcome
areas.
6.1 Relationship Building The service model has had a number of successes in building the relationships between
maternity/child health services and mental health services. These have included improvements
in the formalised referral and communication systems through which the services interact,
including:
o Osborne Park Hospital antenatal clinic and social work staff referrals to
obstetric/psychiatric liaison service
o KEMH CAMI clinic incoming referrals and coordination at birth
o MBU contact child health nurses at discharge
o Child health nurse direct referrals to psychologists via ATAPS referrals.
The participants expressed the view that these improvements were very valuable in the
provision of a quicker response and better service to meet the needs of women with or at risk
of perinatal depression. Participants also indicated general improvements in knowledge and
availability of referral options.

- 47 -
As well as these formal system improvements, there have also been a range of activities
that bring together different services with a focus on perinatal mental health, collaborative
projects, and increased understanding by practitioners of the other health systems with which
their clients interact.
The themes within the interview data were fairly consistent with those noted in the research
literature. Stakeholder feedback was generally very positive about the relationship building
activities, although a small number expressed some dissatisfaction regarding group processes
or level of consultation. Benefits such as increased confidence, communication with other
professionals, and more efficient use of time and resources are similar to benefits noted in a
recent review (Myors, et al., 2011). This review also noted the importance of developing formal
pathways, which has been one of the notable areas of achievement of the current service
model. At times the process of building collaborative projects and networks is challenging, as
different people and organisations have different ideas and agendas and these can be difficult
to integrate. In addition, the CNS positions are aimed to provide a bridge between a range of
different service types (especially maternity and mental health, but in practice this includes
government services, and large and small non-government organisations, with disciplines
including nursing (child health, mental health, midwifery), general practice, obstetrics,
psychiatry, social work and others. Different types of organisations are likely to have different
cultures and work in different ways, with different systems, procedures, expectations and value
systems regarding to how best address the needs of the community. Again, these challenges
are consistent with those experienced by other organisations developing more integrated and
collaborative services.
Myors, et al., (2011) noted the presence of ‘us and them’ mentalities between mental health
and non-mental health services, and between child and parent focussed services, which can
hinder the development of shared vision, aims and goals and consequently affect
collaboration. Potential differences in values and philosophies need to be appreciated, with
some blending required to create high-level collaboration (Horwath & Morrison, 2007). Cross-
disciplinary, cross-sectoral and cross-agency communication and collaboration is continuing to
develop, but requires ongoing effort at multiple levels. Some agencies and services more
easily align and collaborate as a result of similar client groups, systems and attitudes, however
the agencies that are more different from each other may have the greatest capacity to
improve the overall service for women during the perinatal period by building collaborative
relationships.

- 48 -
Although the CACH and AMH CNSs have been working towards co-facilitated perinatal
support groups, there have been numerous obstacles to achieving this goal. Progress is being
made, and ongoing efforts will be necessary to see plans to fruition.
6.2 Clinical Service The AMH and MBU/CL CNSs each work within a mental health clinic and have an in-built
clinical role. The CACH CNS role is not clinic-based, so suitable opportunities for a clinical
caseload have been slowly developed over time. In total, more than 400 women have been
referred to the CNSs, and 947 patient related occasions of service or follow-up visits were
provided. Approximately 180 individual assessments were conducted by the CNSs.
Stakeholder feedback indicates that the service model is providing valuable clinical services
resulting in a better overall package of care for women experiencing or at risk of depression.
In addition to difficulties in establishing jointly run groups, the main challenge impacting on
clinical service is time. Stakeholders encouraged the expansion of the service to include more
time in each clinic, and more face-to-face time including home visiting. However, they were
generally very satisfied with the clinical services that are being provided.
6.3 Collegial Relationships The service model has provided numerous perinatal mental health professional
development sessions to health professionals. Over 400 separate attendances at PD events
have been recorded during the first 18 months of operation. These sessions have covered a
range of perinatal mental health topics, increasing participants knowledge of perinatal
depression, EPDS screening, the tertiary services based at KEMH that are available state-
wide, and the CNS roles, along with other relevant information.
The PD sessions also provide an opportunity for attendees to get to know the CNSs, and to
become aware of the informal or one on one collegial support available. Service providers
working with women with perinatal depression can contact the CNSs for advice. One pleasing
outcome is that some of the child health nurses interviewed indicated this support had
increased their confidence in working with mothers with mental health issues. Child health
nurses are an important point of contact for new mothers, with scheduled visits providing
support, screening and an opportunity to link the woman in with appropriate services. Although
child health nurses are not generally specialists in mental health, a result of routine EPDS
screening as well as in discussions, they may uncover high levels of distress, suicidal ideation
and other symptoms of perinatal depression or other mental illness. It is therefore important

- 49 -
that the nurse is supported by the CNS to access sufficient information, support and referral
pathways to deal effectively with such situations.
While the primary aim of this collegial support is to facilitate better treatment and care for
women with perinatal depression, collegial support is also valuable for the healthcare
workforce. Research has shown that the emotionally demanding nature of the work places
healthcare providers at high risk of burnout (Awa, Plaumann & Walter, 2010). In Australia and
internationally, burnout is considered as an important factor in the retention of nurses, and
impacts on quality of care (Duffield & O’Brien-Pallas, 2002; (Poghosyan, Aiken, & Sloane,
2009). Resources, including collegial support, are important to enable staff to effectively cope
with the demands of their work, and assist in the prevention of burnout (Demerouti, Bakker,
Nachreiner & Schaufeli, 2001). Thus, in providing collegial support in working with women with
perinatal depression, which interviewees indicated has increased their skills, knowledge and
comfort in assisting this group, there are likely to be positive impacts both on the service
provided to women and the skills and wellbeing of the healthcare providers.
6.4 Summary
The service model has had many achievements in the first 21 months of operation. The
service model has a three-pronged approach, with CNSs focussing on relationship building,
clinical service and collegial support. Targeting services, systems and health professionals,
and the links and networks between them creates a broader reach and impact than could have
been achieved using a more conventional approach focussing on clinical service alone. The
CNSs have provided a significant amount of education and information on perinatal
depression, screening and referral options. Various networks, stakeholder groups and
collaborations have been initiated. Clinical service has been provided to hundreds of women
with or at risk of perinatal depression. Almost all of the expected outputs have been met. The
quantitative and qualitative data show that the service model is making good progress across
all expected outcomes.
There are various challenges that require ongoing effort. In particular, relationship building
is a long-term activity, and collaboration between agencies can require substantial effort to
establish suitable systems and processes and access to facilities. In addition, there are
challenges related to the broad scope of the roles, although planning addresses some of these
issues by determining priorities and implementing strategies to contain the scope of work.

- 50 -
6.5 Recommendations
1. Continue funding of the service model, with furt her evaluation prior to June 2013 .
Based on the findings from this evaluation, good progress has been made towards the
expected outcomes and provision of outputs.
2. Address barriers to establishing co-facilitated group/s run by the AMH and CACH
CNSs. Joint activities such as co-facilitated groups provide an excellent opportunity for
bringing together the different areas of expertise in mental health and child health, and
developing a greater shared understanding. Ongoing solutions will increase the
feasibility of further collaborative activities.
3. Further strengthen the links between the three s ervices, through activities such
as joint strategic planning . It will be necessary to include the CNSs as well as all
operational and strategic managers, for a shared vision, role clarity and forward
planning.
4. Explore higher turnover rates in AMH CNS positio ns and develop strategies to
facilitate retention .
5. Explore ways to strengthen relationships between mainstream mental health and
perinatal services. Conduct perinatal mental health education sessions that enable
shared learning between mental health, midwives and child health nurses. Increase
awareness among mainstream mental health professionals of the potential negative
outcomes of perinatal mental health problems for women, infants and families (including
mortality and infant mental health issues).
6. Continue to build communication and address area s of conflict that arise when
bringing together diverse cross-disciplinary, cross -agency and cross-sectoral
groups. Improve communication between mental health and midwifery staff in the form
of referral feedback summaries. Improve consultation with non-government
stakeholders regarding forward planning for state-wide perinatal mental health services.
7. Plan the future scope and positioning of roles w ithin the service model, including
expansion scenarios and infrastructure needs such a s co-location.
8. Use the information from this evaluation and str ategic planning in developing a
business case for continuing the model beyond June 2013.

- 51 -
References Austin, M.-P., Kildea, S., & Sullivan, E. (2007). Maternal mortality and psychiatric morbidity in
the perinatal period: Challenges and opportunities for prevention in the Australian
setting. The Medical Journal Of Australia, 186(7), 364-367.
Awa, W. L., Plaumann, M., & Walter, U. (2010). Burnout prevention: A review of intervention
programs. Patient Education and Counseling, 78, 184-190.
Barker, E. D., Jaffee, S. R., Uher, R., & Maughan, B. (2011). The contribution of prenatal and
postnatal maternal anxiety and depression to child maladjustment. Depression and
Anxiety, 28(8), 696-702.
Barnett, B. (2011). An integrated model of perinatal care. European Psychiatric Review, 4(2),
4.
beyondblue, (2011), Clinical practice guidelines for depression and related disorders – anxiety,
bipolar disorder and puerperal psychosis – in the perinatal period. A guideline for
primary care health professionals. Melbourne: beyondblue: the national depression
initiative.
Duffield, C., & O'Brien-Pallas, L. (2002). The nursing workforce in Canada and Australia: two
sides of the same coin. Australian Health Review, 25(2), 136-144.
Cummings, R., (2006). ‘What if?’ The counterfactual in program evaluation. Evaluation Journal
of Australasia, 6(2), 6-15.
Demerouti, E., Bakker, A. B., Nachreiner, F., & Schaufeli, W. B. (2001). The job demands-
resources model of burnout. Journal of Applied Psychology, 86(3), 499-512.
Gillespie, B. M., Chaboyer, W., Longbottom, P., & Wallis, M. (2010). The impact of
organisational and individual factors on team communication in surgery: A qualitative
study. International Journal Of Nursing Studies, 47(6), 732-741.
Hayes, B. A. (2010). From ‘postnatal depression’ to ‘perinatal anxiety and depression’: Key
points of the National Perinatal Depression Plan for nurses and midwives in Australian
primary health care settings. Contemporary Nurse: A Journal for the Australian Nursing
Profession, 35(1), 58-67.
Horwath, J., & Morrison, T. (2007). Collaboration, integration and change in children's
services: Critical issues and key ingredients. Child Abuse & Neglect, 31(1), 55-69.
Leischow, S. J., Best, A., Trochim, W. M., Clark, P. I., Gallagher, R. S., Marcus, S. E., et al.
(2008). Systems Thinking to Improve the Public's Health. American Journal Of
Preventive Medicine, 35(2, Supplement), S196-S203.

- 52 -
Lewis, G., Rice, F., Harold, G. T., Collishaw, S., & Thapar, A. (2011). Investigating
environmental links between parent depression and child depressive/anxiety symptoms
using an assisted conception design. Journal Of The American Academy Of Child And
Adolescent Psychiatry, 50(5), 451-459.
Myors, K. A., Schmied, V., Johnson, M., & Cleary, M. (2011). Collaboration and integrated
services for perinatal mental health: an integrative review. Child and Adolescent Mental
Health, (online).
Onwuegbuzie, A., & Leech, N. (2007). A Call for Qualitative Power Analyses. Quality &
Quantity, 41(1), 105-121.
Poghosyan, L., Aiken, L. H., & Sloane, D. M. (2009). Factor structure of the Maslach burnout
inventory: An analysis of data from large scale cross-sectional surveys of nurses from
eight countries. International Journal Of Nursing Studies, 46(7), 894-902.
Rossi, P. H., Lipton, M. W., & Freeman, H. E. (2004). Evaluation: A systematic approach (7th
ed.). Sage:California.
Schmied, V., Mills, A., Kruske, S., Kemp, L., Fowler, C., & Homer, C. (2010). The nature and
impact of collaboration and integrated service delivery for pregnant women, children
and families. Collaboration in universal child and family health services. Journal of
Clinical Nursing, 19(23/24), 3516-3526.
Segre, L. S., O'Hara, M. W., Arndt, S., & Stuart, S. (2007). The prevalence of postpartum
depression: The relative significance of three social status indices. Social Psychiatry
and Psychiatric Epidemiology, 42(4), 316-321.
Whitaker, B., & Mckinney, J. (2009). Role clarity, social skills and the feedback seeking/job
satisfaction link. International Journal of Organisational Behaviour, 14(1), 54-68.

- 53 -
Appendices Appendix A Stakeholder Interview Questionnaire Appendix B Expected Outcomes and Outputs AMH Appendix C Expected Outcomes and Outputs CACH Appendix D Expected Outcomes and Outputs MBU/C

- 54 -
Appendix A Stakeholder Interview Questions We are currently conducting a number of interviews with stakeholders as part of the mid-point evaluation of the National Perinatal Depression Initiative (NPDI) perinatal mental health service model in the North Metropolitan area, especially the more established service areas. This includes the Clinical Nurse Specialist positions in:
• Child and Adolescent Community Health (CACH), North [Name]’s position; • Adult Mental Health [Name]’s position; and • KEMH Mother Baby Unit and Consultation Liaison position [Name]’s position.
The interview will take about half an hour. All feedback you provide will be pooled in with the responses from other participant’s – your comments won’t be attributed to you as an individual and your information will be treated as confidential. There are two aims of evaluation – one is to determine by the end of the 3 year funding period how effective the service model is, and the other is to identify the strengths and weaknesses of the service model so that the information can be used to build on the strengths and address any problems. (Where applicable) Is it ok if I tape this?
1. Firstly, could you tell me a little bit about your role? 2. What contact have you had with the NPDI perinatal service model? 3. Which of the NPDI perinatal positions have you had contact with (prompt if required)? 4. How would you describe the service model?
(prompts as required) a. What does it do? b. How well is it working?
5. What impact has the service model had on networks, collaborations and partnerships
between agencies providing services to women in the perinatal period
a. (prompt if required) What impact has it had on networks, collaborations and partnerships between maternity / health services and mental health services?
6. Has the service model impacted on:
a. Knowledge of perinatal mental health in general? (how?) i. (impact on community knowledge?) ii. (impact on agency knowledge)
b. Knowledge or use of referral pathways? (how?) c. Availability of collegial support for health professionals related to perinatal mental
health? (how?)
7. Have there been any improvements to clinical perinatal mental health services in your area? (tell me about these)
8. What, if anything, are the best things about the service model so far? What achievements has it had?
9. What, if anything, are the difficulties with the service model so far? What challenges or shortcomings have there been?
10. How could it be improved over the next 12-18 months? 11. Is there anything else you would like to add about the NPDI perinatal service model?

- 55 -
Appendix B Expected Outputs AMH
A) Building and sustaining relationships
1. Sustaining partnerships and collaborative relationships with Community Health Services and other relevant agencies – Summary of:
a. Partnerships/collaborations established and with whom b. No. of meetings c. Improvements/successes achieved from the partnership/collaboration d. Difficulties encountered in developing working relationships
2. Strengthen relationship with existing maternity service – Summary of: a. Outline current relationship status with maternity service b. Report on service relationship improvements c. No. of contact meetings related to maternity services d. Report episodes of conflict resolution including outcome and plan to reduce
further conflict 3. Strengthen liaison with tertiary perinatal mental health treatment unit – Summary of:
a. Outline current relationship status with service b. Report on service relationship improvements c. No. of contact meetings d. Development of discharge planning protocols as identified/needed e. Report episodes of conflict resolution including outcome and plan to reduce
further conflict
B). Clinical service
1. Individual occasions of service a. No. of new referrals b. No. of individual assessments c. No of patient related occasions of service d. No. of occasions of service for fathers/partners/carers e. No. of individual follow up/monitoring visits f. Referrals by outcome g. Demographic report
2. Postnatal depression and/or women’s perinatal support groups a. Description of groups e.g. content, co-facilitation arrangements b. No. of postnatal depression groups and/or sessions conducted c. No. of women’s perinatal groups and/or sessions conducted d. No. of participants in each group e. Demographics of participants attending group f. Summary of group evaluations/feedback
C) Collegial relationships
1. No. of professional inservice/training sessions a. Description of sessions b. No of participants c. Type of profession and d. Summary of participant evaluation/feedback
2. No. of individual collegial consultations and type of profession 3. No. of consultations for support groups 4. No of individual and group supervision sessions

- 56 -
Appendix C Expected Outputs CACH A) Building and sustaining relationships
4. Sustaining relationships with other agencies – Summary of: a. Partnerships/collaborations established and with whom b. No of meetings c. Improvements/successes achieved from the partnership/collaboration d. Difficulties encountered in developing working relationships
5. Strengthen relationship with existing maternity services as able – Summary of: a. Outline current relationship status with maternity service b. Report on service relationship improvements c. No. of contact meetings related to maternity service d. Report episodes of conflict resolution including outcome and plan to reduce
further conflict 6. Strengthen liaison with relevant Mental Health Services (Mother Baby Unit and
Consultation Liaison Service, Women and Newborn Health Service, Osborne Obstetric Liaison Clinic, and other child and/or adult community mental health clinics as able, NMAHS in 2009 – 2013, and in stage two, a clinic to be determined in SMAHS in 2011 – 2013) - Summary of:
a. Outline current relationship status with service b. Report on service relationship improvements c. No. of contact meetings specifically related to mental health service d. Report episodes of conflict resolution including outcome and plan to reduce
further conflict
B) Clinical service
1. Postnatal depression and/or women’s perinatal support groups g. Description of groups e.g. content, co-facilitation arrangements h. No. of postnatal depression groups and/or sessions conducted i. No. of women’s perinatal groups and/or sessions conducted j. No. of perinatal depression information sessions with fathers/partners/carers –
individual and group k. No. of participants in each group l. Demographics of participants attending group m. Summary results of group evaluation
2. Individual clinical services n. No. of individual occasions of service o. No. of joint home visits with mental health nurse
C) Collegial relationships – to empower and enhance staff competencies, particularly for
beginning level child health nurses and others as needed.
1. No. of joint home visits in a support role with colleague 2. No. of professional development sessions provided to colleagues with description of
sessions, professional group and no. of participants 3. No. of professional development sessions co-facilitated with mental health
professionals to colleagues with description of sessions, professional group and no. of participants
4. No. of individual collegial consultations with mental health professionals 5. No. of individual consultations/coaching/mentoring sessions with child health nurses 6. No of individual and group clinical supervision sessions with child health nurses

- 57 -
Appendix D Expected Outputs MBU/CL
A) Building and sustaining relationships
1. Sustaining relationships with other agencies – Summary of: a. Partnerships/collaborations established and with whom b. No of meetings c. Improvements/successes achieved from the partnership/collaboration d. Difficulties encountered in developing working relationships
2. Strengthen relationships between MBU, CL and Antenatal Clinic (KEMH) - Summary of: a. Outline current relationship status with maternity service b. Report on service relationship improvements c. No. of contact meetings d. Report episodes of conflict resolution including outcome and plan to reduce further
conflict 3. Strengthen liaison with community perinatal mental health and child health services
statewide - Summary of: a. Outline current relationship status with service e. Report on service relationship improvements f. No. of contact meetings g. In consultation with stakeholders, development of standardised discharge planning
protocols as identified/needed for rural and remote areas. h. Report episodes of conflict resolution including outcome and plan to reduce further
conflict B). Clinical service
1. Individual occasions of service a. No. of new referrals b. No. of individual assessments c. No. of patient related occasions of service d. No. of occasions of service for fathers/partners/carers e. No. of home visits f. No. of cases of depression as a primary diagnosis g. Referrals by age and postcode h. No. of individual psycho-educational sessions
2. Resource and consultation regarding perinatal depression and/or women’s perinatal support groups
a. No. of support groups b. No. of participants c. Description of groups e.g. content, co-facilitation arrangements, resources
distributed d. No. of psycho-educational group sessions e. No of participants
3. Liaise as appropriate with community perinatal mental health and child health services a. Development of a statewide referral template
C) Collegial relationships - Statewide
1. No. of professional development sessions 2. No. of participants

- 58 -
3. Description of sessions, professional group and geographical location 4. No. of individual collegial consultations and type of profession 5. No. of consultations for support groups 6. No. of rural and remote consultations, referrals and networking opportunities 7. No. of health professional training sessions in collaboration with WA Perinatal
Mental Health Education and Training team. 8. No. of peer group supervision sessions