Muscles of mastication
-
Upload
indian-dental-academy -
Category
Health & Medicine
-
view
1.402 -
download
4
Transcript of Muscles of mastication

Muscles of Mastication
1) Introduction
2) Development
3) Types

Introduction:
Muscle:
Tissue of characterized by the aggregation of cells whose primary role is to produce
contraction, causing and allowing movements of parts and organs of the body.
It may also be defined as a band of contractile fibrous tissues, which produces
movements in an animal body.
Muscle cells, which make up the bundles, are long and narrow and one called as
FIBRES. A muscle fibre can be several cm in length and 0.1 mm in diameter the cell
membrane of the muscle fibre is called as SARCOLEMANA.
Mastication:
Rhythmic opposition and separation of jaws with the involvement of teeth lips,
cheeks, tongue for chewing of food in order to prepare it for swallowing and digestion.
In simple words it is the process of chewing. Mastication is the first mechanical
process to which entry in to alimentary tract. The main purpose of mastication is to
reduce the size of food particles to a size that is convenient for swallowing (Bolus
formation) with the help of saliva. The muscles concerned with mandibular movement
during mastication and speech are four primary muscles.
1) MASSETER
2) TEMPORALIS
3) MEDIAL PTERYGOIN

4) LATERAL PTERYGOIN
And some of the suprahyoid group of muscles being used as secondary or
supplementary muscles they are
1) Digastric
2) Mylohyoid
3) Geniohyoid
Hence the four primary muscles, which act upon mandible, are traditionally approved
as muscles of mastication.
The muscles of mastication are primarily responsible for ELEVATING,
PROTRUDING, RETRUDING OR CAUSING MANDIBLE TO MOVE LATERALLY.
Muscles of mastication are powerful muscles have evolved through ages and got
adapted to the requirement placed before it.
A strong layer of fascia, derived from the deep cervical fascia and named the
PAROTID FASCIA, covers the masseter and is firmly connected with it. It is attached to
the lower border of the zygomatic arch and invests the parotid gland.

Development:
The muscles of mastication are developed from the embryonic MESODERM of
different pharyngeal arches and are supplied of the nerve of respective arches.
1) I ARCH OR MANDIBULAR ARCH
Masseter
Temporalis
Medial pterygoid
Lateral pterygoid
Mylohyoid
Anterior belly of digastric
Supplied by mandibular nerve
2) II ARCH
Posterior belly of digastrics
Supplied by facial nerve
Origin:
Origin of a muscle is the end is the end of the muscle that is attached to the least
movable structure.
Insertion:
Insertion of the muscle it the other end of the muscle that is attached to the more
movable structure.
Action:

Action is the work that is accomplished when the muscle fibres contract.
Generally during action, insertion moves towards the origin.
Types:
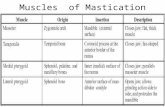
I) MASSETER
The masseter muscle is probably the most powerful of the muscles of
mastication.
It is a Quadrilateral muscle and has three layers.
i) Superficial layer
ii) Middle layer
iii) Deep layer
*Superficial layer: superficial layer of masseter is largest
Origin: It arises by a thick aponeurosis from the zygomatic process of maxilla and
anterior 2/3rd of the lower border of zygomatic arch.
* It s fibres passes downward and backwards at an angle of 45 and
Insertion: Inserted into the angle and lower half of the lateral surface of the ramous of
the mandible.
* Middle layer:
Origin: It arises from the deep surface of the anterior 2/3rd of the zygomatic arch and
lower border of the posterior 1/3rd of the zymatic arch and passes vertically down wards.
Insertion: is inserted into the middle of the ramus of the mandibles.

Deep layer
Origin: Arises from the deep surface of the zygomatic arch and its fibres pass vertical
downward and
Insertion: is inserted into the upper part of the ramus of the mandible and into the
coronoid process.
The middle and deep layers of the masseter together constitute the DEEP PART.
*3 layers are separated posterio-inferiorly by an artery and nerve.
On the account of its proximity to the skin, the masseter can be palpated when it
is thrown into contraction vigorously, as in clenching the teeth.
Relations
Superficial to the muscle
Are the integument, platysma, risonius, zygomaticus major and the parotid gland;
the parotid duct, branches of facial nerve and the transverse facial cross the muscle.
Deep surface
Medially: Overlies the insertion of templralis muscle and the ramus of the mandible,
a mass of fat separates it is front buccinator and the buccal nerve.
The massetric nerve and artery reach the deep surface of the muscle by passing
through the dorsal part of the mandibular inclsure.
Posterior margin:
Is overlapped by the parotid gland.

Anterior margin:
Projects over the buccinator and is crossed below by the facial vein.
Nerve supply:
MASSETRIC NERVE, a branch of anterior division of mandibular nerve (which is
the 3rd part of V cranial nerve- trigeminal nerve).
Blood supply:
Maxillary artery, which is a branch of external carotid artery.
Actions:
Elevates the mandible to close the mouth and to occlude the teeth in mastication.
Its activity in the resting position is minimal.
It has a small effect in side-to-side movement, protraction and retraction.
Although anatomically, there are 2 components of muscles that can be readily
distinguished but in functional terms, this muscle is divided into 4 components namely.
Deep anterior
Deep posterior
Superficial anterior
Superficial posterior

2) TEMPORALIS
Temporal facial covers the temporalis. It is strong fibrous investment covered,
laterally, by the auriculars anteriorly and epicranial opoveurosis and orbicularies oculi
superiorly.
Superficial temporal vessels and auriculo-tempotal nerve ascends over it.
Above, it is a single layer, attached to the whole of the superior temporal line;
below it has two layers one attached to the lateral and the other to the medial margin of
the upper border of zygomatic arch.
A small amount of fat.
Zygomatic branch of the superficial temporal artery and
Zygomatic temporal branch of maxillary nerve.
Deep surface of the fascia affords attachment to the superficial fibers of the
temporalis.
Temporalis: is a fan shaped muscle. It has a very wide origin from the entire temnporal
fossa and fascia covering the muscle.
It is a Bipennate muscle
ORIGIN:
Arises from the whole of the temporal fossa concept the part formed by the
zygomatic bone) and from the deep coverage and descend into a tendon which passes
through the gap between the zygomatic arch and the side of the skull, and;

INSERTION: Inserted to the medial surface, apex, anterior and posterior border of the
coronoid process of the mandible and the anterior border of the ramus of the mandible
nearly as far as possible to the last molar.
RELATIONS:
Superficial to the muscle are
Skin
Temporal fascia
Superficial temporal vessels
Auriculo temporal nerve
Temporal branches of ficial nerve
Zygomatico temporal nerve,
The galea aponeurotica
The zygomatic arch
Masseter
DEEP SURFACE
Temporal fossa
Lateral pterygoid
Superficial head of medial pterygoid
Small pant of buccinator
Maxillary artery and its deep temporal branches
Deep temporal nerves

Buccal vessels and nerves
ANTERIOR BORDER
Anterior border is separated from the zygomatic bone by a mass of fat.
POSTERIOR BORDER
Massetric nerves and arteries
BLOOD SUPPLY
Deep temporal part of maxillary artery
NERVE SUPPLY
Temporalis is supplied by the deep temporal branches of the anterior trunk of
mandibular nerve.
ACTIONS
Temporalis elevates the mandible and so closer the mouth and approximates the
teeth this movements requires both the upward pull of anterior fibres and the backwards
pull of the posterior border, b’coz the head of the mandible rests on the articular
eminence when mouth is open.
The posterior fibres draw the mandible backward after it has been protuded.
It also contributes to side to side grinding movements.

Owing to the strength of the temporal fascia, the muscle is not easy to palpate,
but its contraction is easy to feel. Its upper limit can be made out along the inferior
temporal bone, when the teeth are formerly clenched
3) MEDIAL PTERYGOID
Is a thock QUADRILATERAL MUSCLE. It has two heads.
A small superficial head.
A larger deep head
ORIGIN
SUPERFICIAL HEAD
Originates from maxillary tuberosity just behind the third molar and
From the lateral surfaces of the pyramidal process of the palatine bone.
DEEP HEAD (LARGE)
Originates fro the medial surface of the LATERAL PTERYGOID PLATE and
The grooved surface of the PYRAMIOAL PROCESS OF THE PALATINE BONE.
Its fibres runs downward, laterally and backward and are attached, by a strong
tendinous lamina.
INSERTEO
Inserted into the posterior inferior part of the medial surfaces of the ramus and
angle of the mandible, as high as mandibular foramen and nearly as far forward as the
mylohyoid groove.

Thus, area is often rugged, due to tendinous fascicule in this attachment.
This is just opposite the masseter insertion on the lateral side.
RELATIONS
SUPERFICIALLY CLATERALLY
Lateral pterygoid
Spheno mandibular ligament
Maxillary artery
Inferior alveolar nerves and vassels
Lingual nerve
Process of parotid gland
DEEP SURFACE (MEDIALLY)
Tensor vili palatini
Styloglossus
Stylopharyugeus
Arealar tissue
NERVE SUPPLY
Branch of the main trunk of the mandibular nerve.
BLOOD SUPPLY
Pterygoid branch of 2nd part of maxillary artery

ACTIONS
Elevates of the mandible.
With lateral pterygoid these muscles helps ion protruding the mandible.
With opsilateral lateral pterygoid muscle, it helps in rotating the opposite condyles
along a vertical axix and helps in apposite side movements of the jaw.
4) LATERAL PTERYGOID
It is a short, thick muscle with two parts or heads.
Upper head (small)
Lower head (larger)
ORIGIN
UPPER HEAD –SMALL
Infra temporal surface and
Infra temporal crest of greater wing of the sphenoid bone
LOWER HEAD LARGE
Lateral surface of lateral pterygoid plate (opposite to the origin of the medial
pterygoid)
Its fibres pass horizontally backward and laterally and converge for insertion.
INSERTION

Some fibres from the superior head penetrate the capsule of TMJ and insert into the
anterior border of the articular disc of the joint.
The remainder fibres from this origin and the fibres from the inferior origin insert into
the neck of the condyle i.e. PTERYGOID FOVEA on the anterior surface of the neck
of mandible.
RELATIONS
SUPERFICIAL SURFACE (LATERALLY)
Ramus of the mandible
Maxillary artery
Tendond of the temporalis and
Masseter
DEEP SURFACE (MEDIALLY)
Upper part of the medial pterygoid
Spheno mandibular ligament
Middle meningeal artery and
Mandibular nerve
UPPER BORDER (SUPERIORLY)
Temporal and massetric branches of mandibular nerve
LOWER BORDER (INFERIORLY)

Lingual inferior alveolar nerves
The buccal nerve and the maxillary artery past between the parts of the muscle.
NERVE SUPPLY
The lateral pterygoid is supplied by a branch of anterior division of the
mandibular nerve.
BLOOD SUPPLY
Pterygoid branch of 2nd part of maxillary artery
ACTIONS
1) The lateral pterygoid assists in opening the mouth by pulling forward the condylar
process of the mandible and the articular disc, while the head of the mandible rotates on
the articular disc.
In the reverse movement of closure the backward gliding of the articular disc and
condyle of the mandible is controlled by the slow elongation of the lateral pterygoid,
while the masseter and temporalis restore the jaw to the occlusal position.
2) When the medial and lateral pterygoid of the two sides act together, they protude the
mandible so that the lower incisor project in front of the upper.
3) Acting with the medial pterygoid of the same side, the lateral pterygoid advances the
condyle of that side so that jaw rotates about a vertical axis through the opposite
condyle.

Different actions to the two parts of the lateral pterygoid muscle have been
described, the upper (superior) head mug, being involved in chewing and lower head in
protusion.
SECONDARY MUSCLES TAKING PART IN THE MASTICATION
The 4 primary muscles of mastication are in turn supported or supplemented by
few secondary muscles known as SUPRAHYOID GROUP of muscles they are
DIGASTRIC
MYLOHYOID
GENIOHYOID
STYLOHYOID is other suprahyoid muscle, which does not take part in mastication.
5) DIGASTRIC
It has two bellies united by an inter-mediate rounded tendon.
The anterior belly and
The posterior belly
It lies below the body of the mandible and extends, in an angled form, from the
mastoid process of the chin.
ORIGIN
ANTERIOR BELLY

Is attached to the digastric fossa on the base of the mandible close to the
medium plane.
POSTERIOR BELLY
Longer than the anterior and is attached in the mastoid notch of the temporal
bone.
The fibres of posterior belly pass downwards and forward, and, fibres of anterior
belly pass downwards and backwards. The two bellies meet in an intermediate tendon,
which perforates the stylohyoid.
INSERTION
The intermediate tendon in turn is help by a fibrous pulley attached to hyoid
bone.
NERVE SUPPLY
Anterior belly by mandibular nerve
Posterior belly by facila nerve
RELATIONS
SUPRAFICIALLY
Mastoid process with sternomastoid
Stylohyoid
Parotid gland

Sub mandibulat lymph nodes
Angle of mandible with medial pteygoid
DEEPLY
Internal and external carotic artery
Lingual, facial and occipital arteries
Internal jugular vein
Vagus, accessory and hypoglossal nerve
SUPERIORLY
Posterior arricular artery
Stylohyoid muscle
INFERIORLY
Occipital artery
ACTIONS
1) The muscle has secondary role in mastication as a depressor muscle adding to
the action of lateral pterygoid muscle when mouth is to be opened against
resistance.
2) Elevation of hyoid bone
6) MYLOHYOID

It is a flat, triangular muscle for lying superior or deep to the anterior belly of
digastric and both right and left muscle together form the floor of the mouth this is
attached to the whole length of the mylohyoid line of the mandible.
ORIGIN
It has 3 fibres- posterior, middle and anterior, which originates from the
mylohyoid line of the mandible.
INSERTION
Posterior fibres pass medially and slightly downwards and are inserted into the
body of the hyoid bone.
Anterior and middle fibres from each side interest in a medium fibrous rouphe
that unites right and left muscles of form floor of the mouth.
Sometimes it is futed with the anterior belly of digastric.
NERVE SUPPLY
Mylohyoid nerve a branch of mandibular nerve branch of inferior also nerve.
ACTION
1) The secondary role of this muscle is evidnent as a depressor seen in action
when mouth is to be opened against resistance.
2) It elevates the floor of mouth to help in deglutition.

RELATIONS
INFERIOR OR SUPERFICIAL SURFACE
Is related to platysma, anterior belly of digastric, superficial part of the sub
mandibular gland, facial and sub mental vassals and mylohyoid nerves and vessels.
SUPERIOR OF INTERNAL SURFACE
I in relation with geniohyoid, part of hyoglossus and styloglossus, hypoglossal
and lingual nerves, sublingual gland, sub mandibular ganglion, sub mandibular duct,
lingual and sublingual vessels,
POSTERIORLY
With mucous membrane of mouth
ORIGIN
Originates from inferior general tubercle on the lingual surface of anterior part of the
mandible.
INSERTION
Fibres run backward and downward and inserted into the anterior surface of body of
the hyoid bone.
NERVE SUPPLY

First cervical spinal nerve through the hypoglossal nerve
ACTION
Geniohyoid elevates the hyoid bone and draws it forward, thus acting as a partial
antagonist to stylohyoid.
When the hyoid bone is fixed, it depresses the mandible.
MUSCLE PROTEINS
CONTRATILE PROTEINS- ACTION (THIN) AND MYOSIN
REGULATORY PROTEINS- TROPONIN TROPMYOSIAS
TROPOMYOPSIN Strand like and covers acting molecular
TROPONIN present along with tropomyosin, has 3 component
1) Troponin C- has affinity for Ca ++.
2) Tropnin – has strong affinity for acting and does not allow it to combine with
myosin.
3) Troponin – combines with tropomyosin
PHYSIOLOGY: NEURO-MUSCULAR OKENSEN- oral surgery TRANSMISSION (NMT)
The function of masticatory system is complex. A highly refined neurologic
control system regulates and co-ordinates the activities of the entire masticatory
system. It consists primary of nerves and muscler, hence the term neuro-muscular
system.

The basic component of neuro-muscular system is the motor unit,, which
consists of muscle fibres that are innervated by one motor neuron each neuron joins the
muscle fibres at the motor end plats which has thick soorcolema. There are folds of end
plate are called as ”SUB NEURAL FOLDS”, which increases the surface area of end
plate region.
Cell membrane of nerve terminal or “PRE-JUNCTIONAL MEMBRANE” and
muscle fibre (end) plated is “POST JUCTIONAL MEMBRANE”. The space b/w the pre
and post junctional membrane is called as “NEURO-MUSCULAR CLEFT”. This cleft
contains choline esterase enzyme (which destroys acetyl choline). Motor nerve terminal
contains abundant mitochondria and vesicles containing Ach (Acetylcholine). Receptors
of Ach are present in post junctional membrane (motor and plate).
SEQUENCE OF EVENTS IN NMT
N-M transmission is chemical
When the neuron is activated, there is a opining up of Ca++ channels; Ca ++ enters
the nerve terminals.
DIAGRAM

There is fusion of Ach vesicles with pre-junctional membrane, by EXOCYTOSIS
vesicles enters neuromuscular cleft.
Ach reach the post-junctional membrane and bind with the receptors present there.
As a result of the combination of Ach and receptors, the Na+ and Ca++ permeability
increases, the entry of Na+ and Ca++ causes end plate potential, i.e. there is
depolarization (which causes muscle to contract).
When nerve and plate potential reaches50 Mv, Ap is hired in end plate region.
This Ap (Action potential) enters sarcoplasm via T tobule, Ca++ from terminal cichern
is released into scarcoplasm and
Ca++ combines with troponin C (strand like with covers action)
Tropemyosin is shafted thus uncovering binding sites on action ( thin filaments of
myofibrils)
There is formation of cross bridge between myosin head (thick filament of
myofibrils) and action.

The action filaments are pulled which slides past myosin towards centre of
sarcomene thus the muscle contracts.
The sloding of action filaments even myosin c/a sliding filament theory of walk
along theory (b’coz action filaments walk along myosin filaments).
Energy for sliding of filaments obtained by hydrolysis of ATPO brought about by
myostu ATPO ats enzyme present in myopsin head.
As, the masseter has greater number of motor fibre pre motor neuron, which
corresponds to its move gross function of providing the face necessary during masseter.
MUSCLE FUNCTION
The motor unit can carry only one action i.e. contraction or shortening, the entire
muscle, however has three potential function.
A) ISOTONIC CONTRACTION
When the muscle shortening and moves a load, the contraction isotonic. Hence
the load remains constant and equal to the muscle tension throughout the most of the
period of contraction. It occurs in the masseter, when the mandibular elevated forcing
the teeth through a bolus of food.
B) ISOMETRIC CONTRACTION
When a muscle does not shorter and length remains same (iso- same, metry-
length), but develops tension, the contraction is isometric. Such type of contraction

occurs when muscle attempts to move a load that is greater than the tension developed
in muscles, this occurs in masseter when an object is held between the teeth. eg. Pipe
or pencil.
C) CONTRACTION RELAXATION
When stimulation of the motor unit is discontinued the fibres of motor unit relax
and return to their normal length. This is seen in masseler when the mouth opens to
accept new bolus of food during mastication.
CHEWING CYCLE: consists of 3 phases (APPLIES ORAL PHYSIOLOGY- LEVELLE)
1) An opening phase
2) A closing phase
3) An occlusal phase
During both the opening and beginning of closing phases, the masticatory
muscles under go isotonic contraction or relaxation phases; however, tension builds up
in the elevator muscles. Elevator muscular contraction is strictly isometric only when
the teeth are in contact or when there is a hand unyielding object b/w them.
During the chewing, the change from isotonic to isometric contraction is gradual
and not abrupt. The opening movement appears to be only just suffieicnt to clear the
bolus; tooth contact with bolus occurs soon after beginning of closing phase.

Mastication is characterized not only by a simple straight opening and closing of
the jaw but also RETRUSIVE, PROTRUSIVE and LATERAL JAW movements. Each
chewing cycle lasts approximates 0.8 to 1.0 sec.
During the closing phase, the temporalis muscle on the working side is first to
become active, followed by masseter and temporalis of the balancing side (non-
working). The masseter and medial pterygoid are first to become active during incisive
during both mandibular protension and opening although it is not strictly a mandibular
depressor. The suprahygoid muscles (digastric, mylohygoid, geniohyoid) become
active during jaw opening.
During opening initial phase of isotonic closing from an open position, the
depressor muscles are first activated. The depressor muscles then gradually relax to
allow the mouth to be closed by the passive tension in the elevator muscles and
ligament.
During opening, there is usually a lateral mandibular shift to the working
(junctional) side. The mandible then swings back during closure into the intercuspal the
intercuspal position.
During initial phase of opening or terminal phase of closing, tooth contact glodes
may occur as apposing teeth contact one another. Thus, both condylar head and
mandibular body move during mastication.

The working side condyle moves laterally during the opening phase, whereas,
opposing condyle on the balancing side moves medially downwards and forwards. The
working side condyle rapidly assumes its position within its fossa early in the closing
phase, whereas balancing side condyle moves back into its fossa in the latter phase of
closing.
NEURAL MASTICATION RECEPTORS
Each muscle is innervated by -efferent motor neurous that supply extrafusal
muscle fibres whereas -efferent supply intrafusal muscle fibres of muscle spindles.
Sensory receptors in skeletal muscle generally comprise two basic groups i.e.
Free and encapsulated nerve endings.
Free nerve endings are generally bellowed to be primarily some may be sensitive
to non-noxions stimulus eg muscle stretch.
MUSCLE SPINDLES
They comprise stretch sensitive, slowing adopting specialized (intrafusal) muscle
fibres that are contained within a capsule lying parallel to extrafusal muscle fibres. The
spindle generally has a double afferent innervation a) Large 12-20 hm diameter b) small
4-12 hm diameter.
The efferent (motor) supply to the intrafusal fibres is derived from -motor
neurous located with in CNS some muscles eg mandibular elevators (masseter, medial

pterygoid and temporalis) have large number of facial muscles have few. This suggests
that these latter muscles have either alternative meane of proprioceptive control eg. free
nerve endings/ or depend on other stretch sensitive afferents eg receptors in TMJ. The
formes i.e. masseter, temporalis and medial pterygoid muscles contain numerous
spindles which relay information to the brain about muscle length. The spindle afferents
from the masseter, temporalis and medial poterygoid muscles appear unique, in that
cell bodies reside with in CNS i.e. TRIGEMINAL MESENCEPHALIC NUCLEUS.
There is a concept that the muscles spindles may be involved in correcting small
errors between the intended and actual mandibular movements and maintaining a
constant posture against the effects of gravity.
GOLGI TENDON ORGANS
The golgi tendon organs are receptors primary located at muscle-tendon
junctions (or TMJ capsule). They are innervated byit myclinated afferent (8-12 mm
diameter) fibres. There is no evidence of such units with in masticatory muscles or
tension receptors afferents in the irigeminal ganglion.
PERIODONTAL MECHANORECEPTORS
The PDL contains mechanoreceptors that respond to the teeth. They have wide
range of properties.
Some of these are excited by just a few mictons of tooth displacement.
Some are less sensitive that respond only to the much larger forces.

Some exhibit directional sensitivity, with nerve fibres responding maximally to the
forces in one particular direction.
Some are slowly adopting and produce continous discharge when a constant
stimulus or applied.
Some adopt more rapidly.
Some adopt very rapidly and do not respond unless a very rapid stimulus is applied.
The cell bodies of some of these are located in the TRINGEMINAL
(GASSERIAN) ganglion, while others in the irigeminal mescncephalic ganglion.
MUCOUS MEMBRANE RECEPTORS
The types of receptors respond to the pressure in the palate, particularly in the
region distal to central incisors.
JOINT RECEPTORS
Free nerve fibres comprise the predominant receptors in the TMJ capsule. In
addition a few complex receptors have been recorded including RUFFINI, PACINIAN
AND GLOGI RECEPTORS. These last appear to be confined to the lateral aspect of
the joint capsule and lateral ligament and supplied by a branch of aurioculo-temporal
nerve.
These receptors appear to be associated with joint location perception.
SENSORY RECEPTORS

Specific sensory receptors provide specific information to the afferent neunous
and thus back to CNS. Some of these receptors are specific for DISCOMFORT AND
PAIN. These are called as NOCICEPTIVE RECEPTORS OR NOCICEPTORS.
Other receptors provide information regarding the position and movement of the
mandible and associated oral structures. These are called as PROPRIOCEPTORS.
JAW REPLEXES
They are of two types
1) Simplex reflexes-eg-mandibular depression
2) Complex reflexes eg- masticatory activities
JAW CLOSING REFLEX
The simple jaw closing reflex or (Jaw-Jerk) has a 6 ms latency period between
stimulus and movement.
There is stretch induced masseter or tempolis spindle activation, with the
afferents passing to the trigeminal motor nucleus via trigeminal mesenchepalic nucleus.
Efferent then effects appropriate muscle contraction.
Tapping on the chin initiates the jaw jerk reflex. After a brief depression of the
mandible, there is reflex response in the masseter temporalis muscles, following an
8cms latency. If the jaw jerk is repeated with the subject voluntarily biting on a hard
object, ther is marked increase in reflex masseter muscular activity.

There is then followed by SILENT perio-dominant during which the masseter
does not activity, but passes though a period level of activity, but passes through a
period of decreases activity, during which the muscle of totally inactive.
If the teeth are clenched with nothing between them, the jaw jerk is depressed;
although silent period is still present.
There is no reverse jaw jerk i.e. there is no detectable response in either the
elevator or depressor muscle of a relaxed subject if the chin is tapped from under
health.
JAW OPENING REFLEX
It is a response to or facial stimuli and involves two or more synapses and
excitation of the motor neurons that supply the digastric and inferior head of lateral
pterygoid muscles.
The interneurones relaying the sensory afferents from the orofacial region to the
digastric motor neurons are located in the irigeminal spinal tract muscles and adjacent
reticular formation.
Electrical oral stimulation of subject whose elevator and depressor are released
results in now jaw muscle activity. When the elevator muscles are voluntarily
contracted, there is masseteric inhibition, with two periods of inhibition with latencies of
15 and 45 cms.

After stimulation, a slight opening movement occurs presumably reflecting
elevator muscular inhibition. These opening could evoke a stretch reflex in the elevator
muscles.
TOOTH CONTACT REFLEXES
When the upper and lower teeth snapped together, reflex changes occur in the
elevator muscles, similar to those produced by mechanical single tooth stimulation. This
transient activation is followed by a silent period associated activity. There are no
comparable effects on the depressor muscles.
JAW UNLOADING REFLEX
When the jaw is suddenly unloaded, a protective reflex immediately limits further
jaw closing muscular activity. This sudden reduction and complete cessation of elevator
muscle activity is associated with reflex excitement of the jaw depressor muscles.
HORIZONTAL JAW REFLEX
Lateral, protrusive and retrucive reflex mandibular reflexes are important in direly
controlled masticatory mandible movements. Although lateral mandibular movement
reflexes resulting from lateral prerygoid contraction, can be elicited from facile tooth or
oral mucosal stimulation these reflex pathways have bee subjected scant enquiry.
EXAMINATION OF MASTICATORY MUSCLE

To perform the muscle and joint palpation, the patients is first instructed that
contain muscles are going to be pressed in order to help better understand the pain
problem, that the procedure may be uncomfortable at times and the questions about
discriminating pressure from pain and about pain intensity of palpation will be asked.
In epidemiological studies, 0.9 kg for extra oral muscles and 0.45 kg for intra oral
muscles and TMJ. Time for which pressure is to be held is unknown but 3-5 secs
appears to be reasonable.
POINTS TO CONSIDER
1) Muscles are palpated with the patient sitting upright.
2) Operator faces the patient, with weight evenly balanced on both feet and fore
arm parallel to the floor.
3) Patient and operator both are to be relaxed.
4) Patient is told to respond to any pain or discomfort on either or one side when
unilateral pressure is applied.
5) Physiological and psychological factors affect the report of pain on palpation.
There include activation or sensitization of local peripheral nociceptors,
sensitization of second order neurous, and altered processing at the ophthalmic
level and above, which can include perceptual or neunological mechanisms.
Thus evaluation of reported tenderness needs to include consideration of other
factors such as age, vulture, sex, gender, and pain duration and disease states.

EVALUATION OF TEMPORALIS
It is a fan shaped muscles and the posterior fibres above the ear, anterior fibres
in the depression lateral to the eyebrows and the temporally tendon at the superior and
anterior aspect of the coronoid process (metraorally), are palpated.
Thumb is placed anteriorly just behind and above the eye, the second finger on
the middle belly and the third finger on the posterior belly.
Patient is asked to clench firmly, it can also be palpated introlarally into its
insertion is the coronoid process.
EVALUATION OF MASSETER
Ask the patient to do powerful clenching and the superior belly is clearly visible.
Palpate anterior border. The deep belly is palpable with one finger under the zygomatic
arch in front of the ear areas of palpation are
1) Origin
2) Body
3) Insertion
It can also be palpated by Binanual palpation with index finger of one hand placed intra
orally over the muscle and index finger of other hand extra orally over the muscles, and
pressure is applied all over the muscle.
EVALUATION OF LATERAL PTERYGOID

It is not possible to palpate the superior head of the lateral pterygoid directly, but
palpation of lateral poles give indirect information about it.
It is done with equal pressure of the finger on the lateral poles of the condyles as
the patient open and closes the mouth. Palpation of the inferior head is by running the
index finger sliding back, buccally and behind the tuberosity.
EVALUATION OF MEDIAL PTERYGOID
It is palpated by sliding the finger index lingually and by applying pressure the
insertion of the muscles above the corner (angle) the mandible.