MPPRC: SLE
-
Upload
api-3722051 -
Category
Documents
-
view
514 -
download
1
Transcript of MPPRC: SLE

Case 20Systemic Lupus Erythematosus
February 12, 2008Group C10

History of Present Illness

Patient Data
• H.H., 19 y.o., Filipino female, single, Roman Catholic, a student from San Pedro, Laguna
• Source: patient and her mother• Reliability: 80%• Date of Admission: Jan 17, 2008• Date of Interview: Jan 25, 2008

Chief Complaint: Dyspnea
HPI:Two years prior to admission
• Headache- more prominent on the right– Self-medicated: mefenamic acid
offered relief
• Joint and muscle pains
• Generalized weakness– Persisted and progressed that patient
needed help in order to ambulate

HPI:51 weeks prior toadmission
• Anorexia• Skin sores in the anterior thorax• Wounds on her breast around the
areolar region• Recurrence of headache• Persistence of joint and muscle
pains and generalized weakness• Prompted consultation at Medical
City– Tested for visual problems = (-)– Asked to consult psychiatrist =did not
comply

HPI:50 weeks prior toadmission
• Continuous fever = 400C– Persisted for a week
• Bluish discoloration of fingers
• Prompted another consultation at Medical City
• During consultation, suddenly experienced difficulty of breathing
• Rushed to the ER then moved to the ICU because of pulmonary edema

HPI:48 weeks prior toadmission
• Diagnosed with systemic lupus erythematosus (SLE) with class V lupus nephritis
• Treated with hydrocortisone (unrecalled dosage)
• Discharged with medications: prednisone
• She was not compliant due to side-effects of treatment: weight gain and acne development
46 weeks prior to
admission

HPI:• Started to develop oral sores and
ulcers over most of her buccal cavity• Prompted consultation and confined
for five days at Medical City• Was given unrecalled medications
and was discharged when sores were healed
10 months prior
to admission

HPI:• Bilateral knee pain• Could not stand alone• Confined at Medical City for fifteen
days• Treated with hydrocortisone and
methyprednisolone (Solu-medrol) – unrecalled dosage
• Soon experienced weakness and hair fall (alopecia)
• Reduced dosage of the drugs improved her condition
• Prescribed with prednisone, vitamins (for anemia), and calcium
• Not compliant with prednisone intake due to side-effects
7 months prior
to admission

HPI:• Abnormally enlarging abdomen• Self-medicated with previously
prescribed steroids but to no avail
• Consulted at USTH OPD• Prescribed with prednisone and
hydroxychloroquine (Plaquenil)– Abdominal flattened
• Returned to OPD for lab results• Diagnosed with UTI• Prescribed ciprofloxacin and
azathioprine (Imuran) – unrecalled dosages
1 month prior
to admission
8 days prior
to admission
7 days prior
to admission

HPI:• Abdomen started to enlarge again• Accompanied by swelling of hands
and feet• Progressed rapidly• Also experienced vomiting
• Difficulty of breathing even at rest• Rushed to USTH emergency room
and was admitted
3 days prior
to admission
2 hours prior
to admission

Medical History

Obstetric and Gynecological History
• G0P0• Menarche at 12 y.o.• Irregular menstrual flow (1-2 months with no
period)• Menstrual periods last 5 days• Consumes 2-3 pads a day• LMP: December 2007 (unrecalled date)

Past Medical History
• Bronchopneumonia: 3 months old
• Dislocated left knee while dancing
1988
2001

Past Medical History
• SLE with lupus nephritis class V
• Blood transfusion (1 bag packed RBC)
2006
Feb 2006

Past Medical History• Has skin allergies with no identified trigger/agent –
takes Celestamine
• No history of surgery
• Current medications: prednisone as treatment of SLE
• Immunizations: given DPT, BCG, OPV; no hepatitis vaccines, MMR or influenza

Family History
• No family history of gout or arthritis, allergy, cancer or stroke
• Mother: (+) anemia
• Father: (+) hypertension, (+) heart disease
• Grandmother, mother’s side: (+) DM

Personal and Social History
• Non-smoker, non-alcoholic, no illicit drug use
• Fond of eating fried food, usually pork or chicken and rarely eats vegetables

Personal and Social History
• Household chores are the only form of exercise
• Lives in Laguna with her parents and 2 younger sisters which are all healthy

Personal and Social History
• Piggeries around the house and a nearby river, but is not polluted
• SLE has greatly affected her teenage lifestyle
• Common concerns such as weight gain and acne development has made her non-compliant to steroid therapy

Review of Systems• General: Has anorexia and weakness of the whole body. No
significant weight changes. No fever, sweats, insomnia.
• Skin: Has erythematous, flat rash over the malar eminences. No color change in the other parts of the body
• HEENT: – Head: No history of head injury. – Eyes: No visual dysfunction or lacrimation. No itchiness,
pain or recent changes in vision. – Ears: Hearing good. No tinnitus, vertigo, infections. – Nose, sinuses: No hay fever, sinus trouble. – Throat: No soreness or tonsilitis.

Review of Systems• Neck: Has stiff neck. No lumps, goiter, pain. No swollen
glands
• Breasts: No lumps, pain, discharge
• Respiratory: Has dyspnea. Cough productive of sputum that is difficult to expectorate. Has back pains. No orthopnea
• Cardiovascular: Hypertensive with highest recorded BP 150/110. Has edema in the upper and lower extremities. No chest pain and palpitations. No PND, syncope

Review of Systems• Gastrointestinal: Distended abdomen. No nausea, vomiting,
indigestion. Has regular bowel movements. No abdominal pain.
• Urinary: Has oliguria and flank pains. No other urinary problems
• Genital: No straining, genital lesions or urethral discharge
• Musculoskeletal: Has generalized edema and some limitations in movement of hands and feet. Has generalized weakness.

Review of Systems
• Endocrine: No neck surgery, irradiation, polydypsia or polyphagia.
• Hematologic: Anemic. No bleeding problems.
• Neurologic: No fainting, seizures, motor or sensory loss. Memory good.
• Nails: No clubbing

General Survey• Conscious, coherent,
ambulatory and in cardiorespiratory distress
• BP -140/80 mmHg PR 140, regular
RR 40 Temp 38.2°C
General Survey• Conscious, coherent,
oriented as to time, place and person, not in cardio-respiratory distress
• BP – 140/90 mmHgPR 96, regular,RR 24, regular pattern of breathing Temp 36.2 C
• Height- 5’6’’ Weight- 65 kg
PHYSICAL EXAMINATIONPHYSICAL EXAMINATIONON ADMISSION ON ACTUAL EXAMINATION

General Survey
• Warm, moist skin, no active dermatoses
General Survey
• Skin is shiny, stretched due to edema
• erythematous flat rash over malar eminences
• non-erythematous macular lesions less than 1cm in the anterior thorax near the neck
PHYSICAL EXAMINATIONPHYSICAL EXAMINATIONON ADMISSION ON ACTUAL EXAMINATION

Malar Rash
Source: http://www.emedicine.com/med/images/329097-332244-5270.jpg

HEENT• Pale palpebral conjuctiva,
anicteric sclera
• No ear and nasal discharge
• Moist buccal mucosa, (+) oral ulcers
• No palpable cervical lymphadenopathies, no neck masses
HEENT• Pale palpebral conjuctiva,
anicteric sclera
• No ear and nasal dischage
• Moist buccal mucosa, (+) oral ulcers
• No palpable cervical lymphadenopathies, no neck masses
PHYSICAL EXAMINATIONPHYSICAL EXAMINATIONON ADMISSION ON ACTUAL EXAMINATION

Respiratory
• Symmetrical chest expansion
• no retractions
• decreased tactile and vocal fremiti
• decreased breath sounds on the left T6-T7 down
• (+) crackles on left lung field
Respiratory
• Symmetrical chest expansion
• no retractions• Resonant• decreased tactile and vocal
fremiti in the left posterior lower lung region
• fine rales heard
PHYSICAL EXAMINATIONPHYSICAL EXAMINATIONON ADMISSION ON ACTUAL EXAMINATION

Cardiovascular• Adynamic precordium, apex
beat 5th LICS MCL (apex: S1>S2; base: S2>S1), no murmurs
Cardiovascular• JVP 3.0cm above the sternal
angle at 300 • CAP has rapid upstroke
gradual downstroke• Adynamic precordium, apex
beat at the 5th LICS, MCL. • Apex: Loud S1 followed by
soft S2; base: Soft S1 followed by loud S2, splits at inspiration , no murmurs, no heaves, thrills, or lifts.
PHYSICAL EXAMINATIONPHYSICAL EXAMINATIONON ADMISSION ON ACTUAL EXAMINATION

Abdominal• Flabby abdomen
• normoactive bowel sounds
Abdominal• Abdomen is distended and
shiny with silvery white striae• normoactive bowel sounds, no
bruits
• (+) dullness over abdominal region
• could not assess liver dullness
PHYSICAL EXAMINATIONPHYSICAL EXAMINATIONON ADMISSION ON ACTUAL EXAMINATION

Abdominal
• soft, direct tenderness on LUQ
• (+) bulging flanks, (+) fluid wave
Extremities• Pulses full and equal, (+)
edema, (-) cyanosis
Abdominal• no abnormal masses• no tenderness upon palpation• no costovertebral angle
tenderness• (+) shifting dullness, (+) fluid
wave
Extremities• (+) edema
PHYSICAL EXAMINATIONPHYSICAL EXAMINATIONON ADMISSION ON ACTUAL EXAMINATION

PHYSICAL EXAMINATIONPHYSICAL EXAMINATION
PULSE CAROTID BRACHIAL RADIAL FEMORAL POPLITEAL DOR PEDIS POST TIBIAL
RIGHT ++ ++ ++ ++ ++ ++ ++
LEFT ++ ++ ++ ++ ++ ++ ++
Central and Peripheral Pulses(0)=absent (+)=decreased(++)=normal (+++)=hyperactive (Br)=bruit

Musculoskeletal• Temporomandibular joint: no skin changes, abnormal
contours or deformities; no swelling or tenderness, good movement
Upper extremities• Shoulder joint: no skin changes and deformities, symmetrical,
no swelling and tenderness, no limitation in motion• Elbow joint: no skin changes and deformities, no tenderness
and thickening, slight limitation in motion due to edema, right elbow has an IV so could not be moved
PHYSICAL EXAMINATIONPHYSICAL EXAMINATIONON ACTUAL EXAMINATION

Upper extremities• Forearm, wrist and hand: edematous, bulky hands; no
redness, nodules, no metacarpophalangeal tenderness; no interphalangeal tenderness; right hand unable to make a fist and has limited extension and flexion; left hand has limited extension and slightly limited flexion.
• Neck: Sternomastoid muscles are symmetrical, has no deformities nor abnormal postures; Trapezius muscles are tender; Cervical spinous processes and muscles between the scapulae are non-tender; No limitation in movement of the neck joint
PHYSICAL EXAMINATIONPHYSICAL EXAMINATIONON ACTUAL EXAMINATION

Musculoskeletal• Back: no skin changes, abnormal contours and deformity; no
swelling and tenderness of cervical, thoracic and lumbar spinous processes; no abnormal postures or lateral curvatures; no limitation in movement
Lower Extremities• Hip joint: no skin changes, abnormal contours and deformity;
no swelling and tenderness; no limitation in movement
PHYSICAL EXAMINATIONPHYSICAL EXAMINATIONON ACTUAL EXAMINATION

Lower Extremities• Knee joint: no skin changes, abnormal contours and
deformity; no muscle atrophies and thickening; slight swelling due to edema and no tenderness in the patellar region; no limitation in movement, no instabilities; (-) bulge sign, (-) balloon sign
• Ankle and foot joints: edematous feet, (+) pitting edema = 3-4+, no abnormal contours and deformity; no muscle atrophies and thickening; no metatarsophalangeal tenderness; no interphalangeal joint swelling and tenderness; slight limitation in movement
PHYSICAL EXAMINATIONPHYSICAL EXAMINATIONON ACTUAL EXAMINATION

Neurologic• Alert , awake. Can follow simple
commands.• Pupils 2-3mm ERTL, EOMs full
and equal.• V1V2V3 intact, can smile, clench
teeth, raise eyebrows, tongue midline, can shrug shoulders
• DTR: normoreflexive on knee and ankle jerk
• MMT: All major muscle groups of bilateral UE/LE are 4/5
Neurologic• Conscious ,GCS 15
• Coherent, oriented to time, place and person; good registration, good attention, calculation and recall, good sense of language and constructional ability, good memory
• CN I – XII are all intact
• No muscle atrophy, good muscle bulk and tone, MMT 3/5 in the upper extremities while 4/5 in the lower extremities
PHYSICAL EXAMINATIONPHYSICAL EXAMINATIONON ADMISSION ON ACTUAL EXAMINATION

Neurologic• ROM: No limitations on
range of motion• (-) nuchal rigidity, (-)
Kernig’s sign, (-) Brudzinski’s sign, (-) Babinski
Neurologic• Can do FTNT and
alternating pronation and supination
• Balance and equilibrium was not assessed
• No sensory deficits• Reflexes was not assessed
due to edema• (-) Babinski• Good neck mobility, (-)
Brudzinski’s sign, (-) Kernig’s sign
PHYSICAL EXAMINATIONPHYSICAL EXAMINATIONON ADMISSION ON ACTUAL EXAMINATION

SALIENT FEATURESObjective Findings
PERTINENT POSITIVES
• Female, 19 years old (reproductive age)
• Oral sores and ulcers• Skin sores on anterior thorax
and breast
• Erythematous flat rash over malar eminences
• Anasarca
PERTINENT NEGATIVES
• No chest pain and palpitations
• Normal JVP, CAP and adynamic precordium
• No musculoskeletal deformities

SALIENT FEATURESSubjective Findings
PERTINENT POSITIVES• Headache• Fever• Joint and muscle pains• Generalized weakness
– Assisted ambulation• Anorexia• Bluish discoloration of fingers• Difficulty of breathing• Bilateral knee pain• Skin allergies • Anemia
PERTINENT NEGATIVES
• No family history of gout or arthritis, allergy, cancer or stroke
• No seizures• No memory loss

14Peripheral neuropathy
15Ocular
20Reynaudsphenomenon
21Gastrointestinal
25Pericarditis
33Myalgia
46Pleuritis
50CNS
50Renal
63Weight loss
81Fatigue
83Fever
85Skin
90Arthritis
100Hematologic
PREVALENCE IN PATIENTS, %
CLINICAL MANIFESTATION
14Peripheral neuropathy
15Ocular
20Reynaudsphenomenon
21Gastrointestinal
25Pericarditis
33Myalgia
46Pleuritis
50CNS
50Renal
63Weight loss
81Fatigue
83Fever
85Skin
90Arthritis
100Hematologic
PREVALENCE IN PATIENTS, %
CLINICAL MANIFESTATION
From Robbins and Cotran Pathologic Basis of Disease 7th ed.

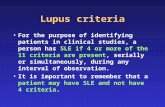
1997 REVISED CRITERIA FOR CLASSIFICATION OF SYSTEMIC LUPUS ERYTHEMATOUS
CRITERION DEFINITION
1. Malar rash Fixed erythema over the malar eminence
2. Discoid rash Erythematous raised patches
3. Photosensitivity Skin rash as a result of exposure to UV light
4. Oral ulcers Oral or nasopharyngeal ulceration
5. Arthritis Nonerosive arthritis
6. Serositis Pleuritis, Pericarditis
7. Renal disorder Persistent proteinuria
8. Neurologic disorder Seizures, Psychosis
9. Hematologic disorder Hemolytic anemia, Leukopenia, Lymphopenia, Thrombocytopenia
10. Immunologic disorder Anti-ds DNA, anti- Sm, and/or antiphospholipid
11. Antinuclear antibody An abnormal titer of antinuclear antibody
Data from Tan EM, et al. The Revised Criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 25:1271, 1982; and Hochberg, MC: Updating the American College of Rheumatology revised criteria for he classification of systemic lupus eryhtematosus. Arthritis Rheum 40: 1735, 1997

1997 REVISED CRITERIA FOR CLASSIFICATION OF SYSTEMIC LUPUS ERYTHEMATOUS
• 11 criteria
• SLE– 4 or more are present– serially or simultaneuosly, during any interval of observation
• Patient– arthritis– oral ulcers– malar rash– renal disorder– hematologic disorder

Definition of Terms
• Rheumatology– rheuma – that which flows as a river or stream– encompasses the autoimmune diseases, arthritis,
and musculoskeletal conditions. While rheumatologists are generally thought to be specialists dedicated to rheumatoid arthritis, lupus and scleroderma, we also care for patients with a wide array of systemic, inflammatory, autoimmune diseases as well as very common musculoskeletal disorders (e.g., osteoarthritis and osteoporosis) and sports-related injuries.
Source: http://en.wikipedia.org/wiki/Rheumatologyhttp://www.rheumatology.org/students/faq.asp (American College of Rheumatology)

Definition of Terms
• Rheumatism– non-specific term used to describe any painful
disorder affecting the loco-motor system including joints, muscles, connective tissues, soft tissues around the joints and bones
– A term used for acute and chronic conditions marked by inflammation, muscle soreness and stiffness, and pain in joints and associated structures
Source: http://en.wikipedia.org/wiki/Rheumatology

Pathophysiology of SLE

Autoimmune Diseases• autoantibodies react against self-antigens
• autoantibodies are not always pathological
• requirements to establish pathologic immunity
– presence of an autoimmune reaction
– evidence that the reaction is not secondary to tissue damage
– absence of another well-defined cause of the disease
From Robbins and Cotran Pathologic Basis of Disease 7th ed.

From Robbins and Cotran Pathologic Basis of Disease 7th ed. p 223
TABLE 6-7 Autoimmune Diseases Organ-Specific Systemic
Hashimoto’s thyroiditis Systemic lupus erythematosus
Autoimmune hemolytic anemia Rheumatoid arthritis
Autoimmune atrophic gastritis of pernicious anemia Sjögren syndrome
Multiple sclerosis Reiter syndrome
Autoimmuse orchitis Inflammatory myopathies
Goodpasture syndrome Systemic sclerosis (scleroderma)
Autoimmune thrombocytopenia Polyarteritis nodosa
Insulin-depedndent diabetes mellitus
Myasthenia gravis
Graves disease
Primary biliary cirrhosis
Autoimmune (chronic active) hepatitis
Ulcerative colitis

Self-tolerance• lack of responsiveness to an individual’s own antigens
• normal individuals: intact
• 2 postulated mechanisms
– Central Tolerance • clonal deletions of self-reactive T and B cell clones occur during their maturation• some may still reach the periphery
– Peripheral Tolerance• anergy - permanent inactivation of lymphocytes • deletion by apoptosis • suppression by regulatory T cells • antigen sequestration
From Robbins and Cotran Pathologic Basis of Disease 7th ed.

Mechanism of Autoimmune Disease
• susceptibility genes– influence the preservation of self-tolerance
• environmental factors– infection
• co-stimulators on APCs are indcued loss of anergy• molecular mimicry .
• progression and chronicity is sustained by the continued recruitment of autoreactive T cells that recognize previously cryptic self-antigens
From Robbins and Cotran Pathologic Basis of Disease 7th ed.

Systemic Lupus Erythematosus
• characterized by the presence ANA, anti-dsDNA, and anti-phospholipid Ab
• acute or insidious onset
• chronic, remitting, relapsing, and often febrile illness
• injury to the skin, joints, kidney, serosal membranes
• any other organ in the body may also be affected
• tissue-binding autoantibodies and immune complexes injury
From Robbins and Cotran Pathologic Basis of Disease 7th ed.

Systemic Lupus Erythematosus
• affects 1 in 700 women of child-bearing age
• 90% of patients are of child-bearing age
• 9:1 female to male ratio
• 2:1 female to male ratio for SLE occurring during childhood or after the age of 65
From Robbins and Cotran Pathologic Basis of Disease 7th ed. and Harrison’s Principles of Internal Medicine 16th ed.

Systemic Lupus Erythematosus
• fundamental defect breakdown of mechanisms that maintain self-
tolerance
• Implicated factors – Genetic– Environmental– Hormonal– Primary abnormality in the immune system
From Robbins and Cotran Pathologic Basis of Disease 7th ed. and Harrison’s Principles of Internal Medicine 16th ed.

Genetic Factors• HLA-DQ genes in chromosome 6
– encode MHC class II molecules
– dysfunction production of anti-dsDNA, anti-Sm, and anti-phospholpid antibody
– 1 susceptibility haplotype: 2x risk
– 2 or more susceptibility haplotypes 4x-6x risk
From Robbins and Cotran Pathologic Basis of Disease 7th ed. and Harrison’s Principles of Internal Medicine 16th ed.

Genetic Factors• Complement deficiency (C2, C4, C1q)
– impaired removal of circulating immune complexes
– C4 deficiency • loss of B-cell tolerance
– C1q deficiency• failure of phagocytosis of apoptotic cells• nuclear components of such cells may induce an
immune response• highest genetic risk
From Robbins and Cotran Pathologic Basis of Disease 7th ed. and Harrison’s Principles of Internal Medicine 16th ed.

Environmental Factors
• hydralazine, procainamide, and D-penicillamine lupus-like response
• UV exposure – exacerbations– stimulates keratinocytes to produce IL-1 apoptosis
– apoptotic cells may become antigenic
From Robbins and Cotran Pathologic Basis of Disease 7th ed. and Harrison’s Principles of Internal Medicine 16th ed.

Hormonal Factors
• OC pills, HRT – 2x risk of developing SLE
• Estradiol – bind to receptors on T cells and B cells– increased activation and survival extended
immune response
From Harrison’s Principles of Internal Medicine 16th ed.

Immunologic Factors• hyperreactive and hypersensitive T cells and B cells
• antigen-specific helper T cell-dependent B cell response autoantibody production
• impaired elimination of apoptotic cells and immune complexes
• antigens, autoantibodies, immune complexes persist tissue injury
From Robbins and Cotran Pathologic Basis of Disease 7th ed. and Harrison’s Principles of Internal Medicine 16 th ed.

Autoantibodies
• ANAs can be grouped into:
– Antibodies to DNA
– Antibodies to histones
– Antibodies to nonhistone proteins bound to RNA
– Antibodies to nucleolar antigens
From Harrison’s Principles of Internal Medicine 16th ed.

Autoantibodies
• Other autoantibodies are directed against:
– Red cells
– Platelets
– Lymphocytes
– Proteins complexed to phospholipids
From Harrison’s Principles of Internal Medicine 16th ed.

*Figure 6-30. Taken from Robbins and Cotran Pathologic Basis of Disease 7th ed. p 229

Immune complex-mediated (Type III) Hypersensitivity
• causes majority of the visceral lesions in SLE
• 3 phases
• First phase: Immune complex formation
Taken from Robbins and Cotran Pathologic Basis of Disease 7th ed.

Immune complex-mediated (Type III) Hypersensitivity
• Second phase: Immune complex deposition
– Determinants if deposition will lead to a disease state
• size of complex: intermediate or small
• Intact mononuclear phagocyte system
– Favored sites:• renal glomeruli• joints• skin• heart• serosal surfaces• small blood vessels
Taken from Robbins and Cotran Pathologic Basis of Disease 7th ed.

Immune complex-mediated (Type III) Hypersensitivity
• Third phase: Inflammation – from the activation of the
complement cascade
– neutrophil and macrophage activation
– platelet aggregation and Hageman factor activation
– microthrombi formation• Vasculitis• Glomerulonephritis• Arthritis
Taken from Robbins and Cotran Pathologic Basis of Disease 7th ed.

Joints• involvement is frequent• typical lesion: nonerosive synovitis with little
deformity – distinguishes this arthritis from that seen in rheumatoid
disease
• acute phases of arthritis in SLE– exudation of neutrophils and fibrin into the synovium – perivascular mononuclear cell infiltrate in the subsynovial
tissue
From Robbins and Cotran Pathologic Basis of Disease 7th ed.

Disorders of Joints
• Localize the complaint• ARTICULAR vs NONARTICULAR
• Determine pathologic process• INFLAMMATORY vs NONINFLAMMATORY
• Determine extent of involvement• MONOARTICULAR, POLYARTICULAR, FOCAL,
WIDESPREAD
• Determine chronology• ACUTE vs CHRONIC
From Harrison’s Principles of Internal Medicine 16th ed.

Articular vs NonarticularSynovium, synovial fluid, articular cartilage, intraarticular ligaments, joint capsule, juxtaarticular bone
Tendons, bursae, muscle, fascia, bone, nerve, skin
Deep or diffuse pain Focal tenderness on areas distinct from articular structures
Limited ROM on active and passive movement
Limited ROM only upon active movement
swelling
Crepitus, instability, deformity Seldom demonstrate crepitus, instability or deformity
From Harrison’s Principles of Internal Medicine 16th ed.

Inflammatory vs noninflammatory
• Infectious; crystal induced (gout); Immune related (RA or SLE); Reactive (rheumatic fever), or idiopathic
• One or all four cardinal signs of inflammation (erythema, warmth, swelling, pain)
• Related to trauma, ineffective repair (osteoarthritis), neoplasm, pain amplification
• Pain without swelling/warmth
• Absence of systemic features
• Minimal/absent morning stiffness
From Harrison’s Principles of Internal Medicine 16th ed.

• Onset – abrupt or indolent• Evolution
– Chronic, migratory, intermittent, additive
• Duration– Acute, chronic (>6 weeks)
*Chronic arthrides often include noninflammatory and immunologic disorders
• Involved articulations– Mono-, oligo- or polyarticular– Focal or diffused
From Harrison’s Principles of Internal Medicine 16th ed.

• In SLE musculoskeletal complaints may be associated with systemic features such as fever, rash, or weakness
From Harrison’s Principles of Internal Medicine 16th ed.

From Harrison’s Principles of Internal Medicine 16th ed.

Dyspnea
• “abnormally uncomfortable awareness of breathing”
• stimulation of receptors in the lungs, airways, respiratory muscles, or chest wall
• excessive or abnormal activation of the respiratory centers in the brainstem
From Harrison’s Principles of Internal Medicine 16th ed.

Pulmonary Manifestations in SLE
• most common pulmonary manifestations: pleuritis and pleural effusion – 50% of patients
• alveolar injury – edema or hemorrhage
• chronic interstitial lung disease
From Robbins and Cotran Pathologic Basis of Disease 7th ed. and Harrison’s Principles of Internal Medicine 16th ed.

Pleural Effusion
• excess quantity of fluid in the pleural space
• pleural fluid formation exceeds pleural fluid absorption
From Harrison’s Principles of Internal Medicine 16th ed.

Alveolar Hemorrhage
• abrupt onset with cough, fever, and dyspnea
• hemoptysis – may be absent at the time of presentation in 1/3 of the cases
• patient: no fever and no hemoptysis
From Harrison’s Principles of Internal Medicine 16th ed.

Interstitial Lung Disease
• involves lung parenchyma – alveoli, alveolar epithelium, capillary endothelium, perivascular and lymphatic tissue
• inflammation and fibrosis (in SLE) or granuomatous reaction in intersititial or vascular areas
From Harrison’s Principles of Internal Medicine 16th ed.

Diagnostic Procedures

Laboratory Diagnosis
• Laboratory tests serve to:– To establish or rule out the diagnosis– To follow the course of disease, particularly to
suggest that a flare is occurring or organ damage is developing
– To identify adverse effects of therapies
Harrison’s Principles of Internal Medicine 16th edition

Laboratory Diagnosis
• Tests for autoantibodies– SLE is characterized by a heterogeneous and
polyclonal antibody response, and the usual case of SLE has an average of three different circulating antibodies present simultaneously
– Diagnostically, the most important autoantibodies to detect are ANA (anti-nuclear antibodies) since the test is positive in >95% of patients, usually at the onset of symptoms
Harrison’s Principles of Internal Medicine 16th editionClinical Diagnosis and Management by Laboratory Methods 20 th edition by John Bernard Henry

Laboratory Diagnosis
• ANA– Diffuse staining pattern
on indirect immunofluorescence
• The whole nucleus is evenly stained
• Most strongly associated with SLE

Laboratory Diagnosis
• Tests for autoantibodies– High-titer IgG antibodies to double-stranded DNA
(dsDNA) (but not to single-stranded DNA) are specific for SLE
• Titer of anti-dsDNA correlates with disease activity, particularly of nephritis or vasculitis
• ELISA, IF and Farr assay
Harrison’s Principles of Internal Medicine 16th edition

Laboratory Diagnosis
• Anti-dsDNA– Immunofluorescent
reaction of sera with the dsDNA in the flagellate Crithidia lucilliae

Laboratory Diagnosis
• Tests for autoantibodies– Antibodies to Sm are also specific for SLE and
assist in diagnosis• Present only in about 30% of patients with SLE• Thus (+) test – SLE; (-) test does not rule out SLE• Do not usually correlate with disease activity and
clinical manifestations
Harrison’s Principles of Internal Medicine 16th edition

Laboratory Diagnosis
• Tests for autoantibodies– aPL (anti-phospholipid) antibodies are not specific
for SLE but their presence fulfils one of the classification criterion and they identify patients at increased risk for venous or arterial clotting, thrombocytopenia and fetal loss
• ELISA, phospholipid-based prothrombin time (dilute Russell venom viper test)
Harrison’s Principles of Internal Medicine 16th edition

Laboratory Diagnosis
Harrison’s Principles of Internal Medicine 16th edition

Laboratory Diagnosis
Harrison’s Principles of Internal Medicine 16th edition

Laboratory Diagnosis
• Standard tests for diagnosis– CBC
• Hemolytic anemia • Leukopenia (<4,000/μL)• Lymphopenia (<1500/μL)
– Platelet count• Thrombocytopenia (<100,000/μL)
– Urinalysis• Proteinuria (>0.5 g/d or ≥+3), or cellular casts
Harrison’s Principles of Internal Medicine 16th edition

Laboratory Diagnosis
Harrison’s Principles of Internal Medicine 16th edition

Laboratory Diagnosis
• Tests for following disease course - indicate the status of organ involvement known to be present during SLE flares– Hemoglobin– Platelet count– Urinalysis– BUN, creatinine or albumin
Harrison’s Principles of Internal Medicine 16th edition

Radiology
• Pleural effusion– Most common thoracic
manifestation– Frequently bilateral– Blunting of costo-
phrenic and cardio-phrenic angles
– Lateral upward sloping of a meniscus-shaped contour
Fraser and Pare’s Diagnosis of Diseases of the Chest 4 th edition

Radiology• Acute lupus pneumonitis
– Increased opacity and poorly defined markings in the mid and lower portions of the chest - (R) x-ray film
Fraser and Pare’s Diagnosis of Diseases of the Chest 4 th edition

Radiology• Pulmonary fibrosis
– Irregular linear opacities in the lower lung zones
Fraser and Pare’s Diagnosis of Diseases of the Chest 4 th edition

Radiology• Joint manifestations
– Metacarpophalangeal subluxations without erosions
Radiology of Bone Diseases 4th edition by Greenfield

Therapeutic Goals
• To control acute and severe flares• To suppress/ alleviate the symptoms• To prevent and treat complications

Treatment

Therapeutic Goals
• To control acute and severe flares• To suppress/ alleviate the symptoms• To prevent and treat complications

Treatment
Pharmacologic

• Indications:• life-threatening manifestations of SLE, such as
glomerulonephritis, CNS involvement, thrombocytopenia, and hemolytic anemia
• debilitating manifestations of SLE (fatigue, rash) that are unresponsive to conservative therapy
Washington Manual of Therapeutics 31st Edition
GLUCOCORTICOIDS

GLUCOCORTICOIDS
• Prednisolone• Methylprednisolone
MOA: inhibits COX-2 and phospholipase A2 which is responsible for the breakdown of cell membrane phospholipids into arachidonic acid
Goodman and Gillman Pharmacological Basis of Therapeutics 11th Edition

• Nonsteroidal Anti-inflammatory Drugs (NSAIDS)– Used for its’ analgesic and antiinflammatory
effects– compete in a reversible manner with arachidonic
acid substrate at the active site of COX-1 and COX-2 decreasing prostaglandin synthesis
– Indomethacin, Ibuprofen , Ketorolac , Mefenamic acid, Naproxen, Diclofenac
Goodman and Gillman Pharmacological Basis of Therapeutics 11th Edition

• Disease Modifying Antirheumatic Drugs (DMARDs)– Drugs that modify the progression of common
rheumatic diseases

DMARDS• Antineoplastic agents
– Methotrexate • For managing arthritis, serositis, cutaneous, and constitutional
symptoms. • Blocks purine synthesis and AICAR, thus increasing anti-
inflammatory adenosine concentration at sites of inflammation. Ameliorates symptoms of inflammation.
– Cyclophosphamide • cross-links DNA, thereby preventing cell replication. • Standard for controlling life threatening active lupus nephritis
– Chlorambucil • Alkylating agent, cross-links DNA, thereby preventing cell
replication.
Basic and Clinical Pharmacology by Katzung 10th Edition

• Immunosuppressants– Indications:
• such life-threatening manifestations of SLE as glomerulonephritis, CNS involvement, thrombocytopenia, and hemolytic anemia
• the inability to reduce corticosteroid dosage or severe corticosteroid side effects
Washington Manual of Therapeutics 31st Edition
DMARDS

– CyclosporineMOA: inhibits IL-2 production by activated T cells
- AzathioprineMOA: suppresses T and B cell functions
– Mycophenil mofetilMOA: inhibits T cell proliferation and interferes
leukocyte adhesion
– CorticosteroidsMOA: inhibits COX-2 and phospholipase A2
DMARDS
Basic and Clinical Pharmacology by Katzung 10th Edition

• Antimalarials– Proposed mechanisms: T cell suppression,
decreases WBC chemotaxis, stabilizes lysosomal enzymes, inhibits DNA and RNA synthesis, and free radical trapping
– reduce dermatitis, arthritis, and fatigue – Chloroquine, Hydroxyhloroquine
DMARDS
Basic and Clinical Pharmacology by Katzung 10th Edition

Prevent Complications
• Sunscreen– Photosensitivity– SPF >30
• Calcium and Vitamin D preparations
Harrison’s Principles Internal Medicine 16th Edition

Treat Complications
Complications Treatment
Hypertension Antihypertensive (B blockers)
Generalized Edema Corticosteroids
UTI Ciprofloxacin
Pulmonary Infiltration Corticosteroids
www.uic.edu/classes/pmpr/pmpr652/final/stevens/sle.html#SLE

• Adequate sleep and avoidance of fatigue • Regular exercise• Education about lupus and self-care • Avoid smoking • Eating a healthy balanced diet• Salt restriction• Developing a support system of family, friends, and health
professionals• For patients with photosensitive rashes use protective
clothing, such as a hat and long sleeves, and avoidance of sun exposure are recommended to prevent flareups

Thank you!

Kidneys
• Nephritis– Immune complex deposition in renal structures:
• Glomeruli• Tubular & peritubular capillary basement membranes
• Thrombosis– Glomeruli– Extraglomerular vasculature
From Harrison’s Principles of Internal Medicine 16th ed.

Thrombosis
• Antiphospholipid antibody– “lupus anticoagulant”
• Hypercoagulable state
From Harrison’s Principles of Internal Medicine 16th ed.

Laboratory Diagnosis
• Staging of lupus nephritis – light microscopy, IF and EM– Class I - minimal mesangial lupus nephritis– Class II - mesangial proliferative lupus nephritis– Class III - focal lupus nephritis– Class IV - diffuse lupus nephritis– Class V - membranous lupus nephritis– Class VI – advanced sclerosing lupus nephritis
eMedicine.com: Nephritis, Lupus by Lawrence Brent MD, updated February 21, 2007

Laboratory Diagnosis
• Class V (membranous lupus nephritis)– Light microscopy
• Diffuse thickening of glomerular basement membrane without inflammatory infiltrate
• Spikes using silver impregnation
Lecture on Pathology of the Kidney by Normando Gonzaga MDInternet Pathology for Medical Education, Florida State University - http://library.med.utah.edu/WebPath/RENAHTML/RENALIDX.html

Laboratory Diagnosis
• Class V (membranous lupus nephritis)– IF
• Granular IgG and C3; diffuse
• “Rosary beads” pattern
Lecture on Pathology of the Kidney by Normando Gonzaga MDInternet Pathology for Medical Education, Florida State University - http://library.med.utah.edu/WebPath/RENAHTML/RENALIDX.html

Laboratory Diagnosis
• Class V (membranous lupus nephritis)– EM
• Subepithelial deposits forming “humps and spikes”
Lecture on Pathology of the Kidney by Normando Gonzaga MDInternet Pathology for Medical Education, Florida State University - http://library.med.utah.edu/WebPath/RENAHTML/RENALIDX.html