MP58-01 MULTI-INSTITUTIONAL VALIDATION OF THE ERUS ROBOTIC SURGERY TRAINING CURRICULUM
Transcript of MP58-01 MULTI-INSTITUTIONAL VALIDATION OF THE ERUS ROBOTIC SURGERY TRAINING CURRICULUM

e658 THE JOURNAL OF UROLOGY� Vol. 191, No. 4S, Supplement, Monday, May 19, 2014
CONCLUSIONS: SRMs under AS grew slowly and had a lowincidence of requiring surgical intervention or progression. Our datashows a low rate of tumor growth especially with complex cystic massesthat exhibit nearly zero net growth. Management of SRMs shouldroutinely include AS as an option in appropriately selected patients.
Source of Funding: None
Prostate Cancer: Localized VI
Moderated Poster
Monday, May 19, 2014 1:00 PM-3:00 PM
MP58-01MULTI-INSTITUTIONAL VALIDATION OF THE ERUS ROBOTICSURGERY TRAINING CURRICULUM
Alessandro Volpe*, Aalst, Belgium; Kamran Ahmed, Prokar Dasgupta,London, United Kingdom; Vincenzo Ficarra, Udine, Italy; Henk Van derPoel, Amsterdam, Netherlands; Alexandre Mottrie, Aalst, Belgium;ERUS board members, Arnhem, Netherlands
INTRODUCTION AND OBJECTIVES: The criteria set for sur-geon’s competence before starting robotic surgery are neither struc-tured nor evidence based. The development of structured and validatedtraining curricula represents one of the current priorities in the roboticurologic field.
METHODS: A 12-weeks structured training program/curriculumwas developed based on a focused group expert panel discussion andused to train 10 fellows from major teaching institutions across Europe.The key components of the curriculum were e-learning, an intensiveweek of structured simulation laboratory training (virtual reality simulatorand dry/wet lab simulation platforms) and modular training in robot-assisted radical prostatectomy (RARP) at each institutions under su-pervision of the mentors. The technical and non- technical skills of thefellows were assessed by the mentors at the end of the program usingpreviously validated GEARS (score 1- 5) and NOTTS (score 1-4)scales. At the end of the training, a full RARP performed by the fellowswas video-recorded and blindly assessed by two independent expertrobotic surgeons using a dedicated assessment scale. The scores ofthe fellows were compared with those of two expert robotic surgeons.The educational impact was evaluated with a dedicated questionnaire.
RESULTS: The fellows had limited previous console exposure(4 mos, IQR 0-6.5). At the end of the training, the fellows received anaverage score >4 (4.1-4.7) from their mentors for all the technical skillsdomains of the GEARS scale, with no negative scores (�2). An averagescore�3.5was also achieved for the 4non-technical skills domains of theNOTTS scale, with no negative scores (�2). Eight fellows were deemedable to perform a RARP alone by their mentors. At the assessment of thevideo-recorded RARP, 6 fellows received a sufficient score by the re-viewers for all steps of the surgical procedure and 8 reached an averageoverall sufficient score. The robotic experts significantly outperformed thefellows for all surgical steps. At the final questionnaire, all fellowsconsidered the program effective in improving their robotic skills andability to perform the surgical steps of RARPwith amean score of 4.7 on aLikert-type scale (1¼strongly disagree to 5¼strongly agree).
CONCLUSIONS: This 12-weeks structured training programwas successful to improve the robotic skills of fellows and their ability toperform the surgical steps of RARP. Further studies are needed todefine the ideal length and schedule of these programs. This pilot studyrepresents a step towards the definition of validated curricula for RARPand other robotic procedures.
Source of Funding: Intuitive Surgical, Inc.
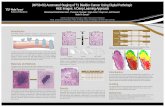
MP58-02OPTICAL BIOPSY OF PROSTATE CANCER THROUGH CONFOCALLASER ENDOMICROSCOPY
Aristeo Lopez*, Kathleen Mach, Daniel Bui, Robert Rouse, Joseph Liao,Stanford, CA
INTRODUCTION AND OBJECTIVES: Standard diagnosis ofprostate cancer relies on random core biopsies and hematoxylin andeosin (H&E) histopathology. Confocal laser endomicroscopy (CLE) isan in vivo optical biopsy technology that enables real time tissue im-aging with micron-scale resolution similar to histopathology. We appliedCLE to fresh, unfixed prostate tissue samples and characterized opticalimaging features of normal, benign and malignant prostate.
METHODS: With IRB approval, patients (n¼13) scheduled forradical prostatectomy were recruited. Fluorescein (10%), as the tissuecontrast agent, was given intravenously prior to prostate removal. Ex vivoprobe-based CLE was performed immediately postoperatively with theCellvizio� system (Mauna Kea Technologies, Paris). Image correlationwithH&Ehistologywasconductedwithassistanceofasurgicalpathologist.
RESULTS: No adverse reactions were observed from IVfluorescein administration. CLE was performed on intact prostates(with and without nerve sparing), tissue slices, and tissue cores.Benign prostatic glands were characterized in tissue slices and coresas irregular, lobular structures highlighted by a rim of fluorescence witha dark lumen. Prostate adenocarcinoma demonstrated crowding ofsmaller glandular structures.
CONCLUSIONS: We report optical biopsy of prostate cancerusing CLE and a first step towards development of an optical imagingatlas of the prostate parenchyma. Pending further development, CLEmay enable true ‘point of care pathology’ and be integrated as part ofprostate cancer management.