Most orbital roof fractures can be treated conservatively ......commonly associated facial fracture...
Transcript of Most orbital roof fractures can be treated conservatively ......commonly associated facial fracture...

Oakstone Publishing, LLC • 2700 Corporate Drive • Suite 100 • Birmingham, AL 35242 205-991-5188 • 1-800-633-4743 • www.practicalreviews.com • [email protected]
What Is the Appropriate Treatment for Orbital Roof Fracture?
Traumatic Orbital Roof Fractures: Interdisciplinary Evaluation and Management.
Cossman JP, Morrison CS, et al:
Plast Reconstr Surg 2014; 133 (March): 335e-343e
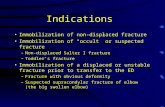
Most orbital roof fractures can be treated conservatively, but require a multidisciplinary approach including facial trauma team, neurosurgery, and ophthalmology for safe and comprehensive care.
Background: The orbital roof is formed by the frontal bone and the lesser wing of the sphenoid bone and constitutes the lateral aspects of the anterior skull base. Although less common than other facial fractures, orbital roof fractures pose significant potential for associated ophthalmologic and neurologic injury and justifies careful evaluation and interdisciplinary management. Objective: To review the authors' experience with management of orbital roof fractures, including associated injuries, indications for surgery, and results of operative and nonoperative management. Methods: The authors reviewed 60 consecutive patients at a Level I trauma center with orbital roof fractures from 2009 to 2011. Patient demographics, mechanism of injury, associated injuries, treatment, outcomes, and complications were analyzed. Results: The average age was 38.1 years, and the male-to-female ratio was 4:1. Fall was the most common mechanism of injury (33%) followed by assault (25%). Associated craniofacial fractures were common (87%) as were ophthalmologic injuries (47%) and traumatic brain injury with intracranial hemorrhage (65%). The most commonly associated facial fracture was an ipsilateral zygomaticomaxillary complex fracture (40%), and the least common were mandible fractures (3%). An isolated orbital roof fracture was uncommon and occurred in only 8 patients (13%). Pneumocephalus was noted in 19 patients (32%), suggesting dural laceration. Although all operative fractures had pneumocephalus, the majority of patients with pneuomocephalus were managed conservatively. Six patients (10%) underwent operative repair of the orbital roof fracture, all of whom had a dural laceration and cerebrospinal fluid leak. A split calvarial bone graft was used in 5 patients and absorbable mesh in 1 pediatric patient. Most patients (90%) had minimal displacement and no clinically evident cerebrospinal fluid leak (CSF) and were treated with observation without complications. Conclusions: Orbital roof fractures are an uncommon but potentially morbid consequence of high-energy craniofacial trauma. Most can be safely observed; however, an interdisciplinary approach is crucial to providing comprehensive care. Reviewer's Comments: Indications for emergent intervention for an orbital roof fracture are largely related to visual and neurologic compromise. Nonemergent surgical indications include CSF leak or significant bony displacement concerning for orbital volume changes. If significant bony comminution precludes anatomical reduction and fixation, a split calvarial bone graft, titanium mesh, or prosthetic can be used to reconstruct the orbital roof. (Reviewer-Tang Ho, MD). © 2014, Oakstone Publishing, LLC
Keywords: Orbital Roof Fracture, Facial Fracture, Management
Print Tag: Refer to original journal article

Oakstone Publishing, LLC • 2700 Corporate Drive • Suite 100 • Birmingham, AL 35242 205-991-5188 • 1-800-633-4743 • www.practicalreviews.com • [email protected]
It Is Safe to Perform Nasal Reconstruction in Children
Corrective Nasal Surgery in the Younger Patient.
Adil E, Goyal N, Fedok FG:
JAMA Facial Plast Surg 2014; 16 (February 6): 176-182
Nasal reconstructive surgery can be prudently performed on properly selected pediatric patients.
Background: Physicians have been cautioned not to perform surgery on the pediatric nose because of the potential damage to the nasal growth centers. Nasal and midface growth continues until age 14 to 17 years, and it has been shown that the nasal septum continues to grow until 36 years of age. Objectives: To review the authors' experience with reconstructive nasal surgery in pediatric patients and to describe the clinical parameters for managing pediatric patients with nasal anatomical deformity or functional impairment. Methods: A retrospective review was performed for all male patients younger than 16 years and female patients younger than 14 years who underwent septoplasty or nasal reconstruction at a tertiary referral center between 1996 and 2012. A total of 54 pediatric patients were included in the study, including 39 males (72%) and 15 females (28%). The mean age was 12.2 years, ranging from 5.6 to 15.3 years. The mean follow-up period was approximately 21 months. Results: The most common surgery indications were posttraumatic deformities (n=36; 67%) and severe airway obstruction (n=48; 89%). Significant septal deviation, defined as obstructing at least 70% of the airway, was noted in 43 patients (80%). Six patients (11%) had evidence of saddle nose deformity on evaluation. Septoplasty alone was performed in 9 patients (17%), while 32 patients (59%) underwent septoplasty in combination with other procedures. An open approach was used in 19 patients (35%), and 8 patients (15%) underwent tip work to help address vestibular stenosis. Auricular cartilage was used for grafting in 7 patients (13%), septal cartilage in 10 patients (19%), and rib cartilage in 5 patients (9%). Staged procedures were performed in 5 patients with no revisions, while nasal growth appeared to continue as anticipated for all patients. Conclusions: Pediatric patients with nasal obstruction and deformity can safely undergo nasal reconstructive surgery. Special considerations include preserving normal structures and judicious use of grafts. Reviewer's Comments: Obstructive nasal septal deformity can lead to chronic mouth breathing, which has been shown to affect craniofacial development. Uncorrected septal deformities can also continue to worsen and have an impact on the frequency of sinusitis and otitis media. Furthermore, trans-septal surgery for brain tumors in pediatric patients has not had reports of craniofacial deformity following the procedure. (Reviewer-Tang Ho, MD). © 2014, Oakstone Publishing, LLC
Keywords: Pediatric Nasal Reconstruction, Septoplasty, Pediatric Patients
Print Tag: Refer to original journal article

Oakstone Publishing, LLC • 2700 Corporate Drive • Suite 100 • Birmingham, AL 35242 205-991-5188 • 1-800-633-4743 • www.practicalreviews.com • [email protected]
No Significant Difference in Voice Outcome With Regard to Treatment Modality
Are Patient-Reported Voice Outcomes Better After Surgery or After Radiation for Treatment of T1 Glottic Carcinoma?
Misono S, Merati AL:
Laryngoscope 2011; 121 (March): 461-462
There is no demonstrated difference in voice outcomes in patients with T1 glottic cancer treated with surgery or radiation therapy.
Background: Patients with glottic cancer need to take into account various factors such as effectiveness of treatment, quality of life, survival statistics, and preservation of organs with respect to voice. Endoscopic surgery and radiation therapy are the two primary treatment modalities for treating glottic carcinoma. Objective: To evaluate surgical resection versus radiation therapy as the best treatment for voice preservation in patients with glottic cancer. Methods: A systematic literature review was performed that included studies analyzing 2 treatment methods, radiation and endoscopic resection, to evaluate self-reported voice outcomes in post-treatment glottic cancer patients. Self-reported voice measurements used the Voice Handicap Index (VHI). Studies were assessed for their level of evidence, number of participants, and outcomes. Results: Several studies were identified as levels 3 and 4 evidence. Overall, the studies demonstrated that no significant voice outcome differences were reported with radiation and endoscopic surgery. In a 2006 meta-analysis of 6 studies totaling 299 T1 glottic cancer patients, 208 patients were treated with radiation therapy and 91 with endoscopic resection; no significant difference in voice outcomes was found. Similar results were reported in a 2008 study of 39 patients, with 23 patients undergoing endoscopic resection and 16 who received radiation with a mean follow-up of 4 years. Conclusions: The available evidence indicates voice reported outcomes as measured by the VHI have no significant difference in patients with T1 glottic cancer undergoing radiation therapy compared to endoscopic resection. Reviewer's Comments: The question of surgery versus radiation for laryngeal cancer has been asked many times and in different ways. Researchers and physicians are still trying to sift through the available evidence to figure out which approach works best for which patients. This study asks a clinically important question and attempts to answer it with the available, limited, amount of evidence. This review is clinically useful in that it examines different treatment plans to determine what is the best course for voice preservation. Both radiation and endoscopic resection have similar self-reported voice outcomes, so voice preservation should not be a factor when determining the treatment modality for glottic cancer patients. (Although this article was published >1 year ago, the results and issues that arise from this manuscript are still relevant for otolaryngologists. We will continue to keep the readers abreast of newer findings as they arise.) (Reviewer-Josef Shargorodsky, MD, MPH). © 2014, Oakstone Publishing, LLC
Keywords: T1 Glottic Cancer, Voice, Surgery, Radiation, Outcomes
Print Tag: Refer to original journal article

Oakstone Publishing, LLC • 2700 Corporate Drive • Suite 100 • Birmingham, AL 35242 205-991-5188 • 1-800-633-4743 • www.practicalreviews.com • [email protected]
Complicated Ranula Cases May Require a Cervical Approach
When Do Ranulas Require a Cervical Approach?
Lesperance MM:
Laryngoscope 2013; 123 (August): 1826-1827
Many plunging ranulas can be evacuated via an intraoral incision.
Background: Ranulas are cystic structures arising from the sublingual glands. The etiology is believed to be obstruction of the sublingual gland ducts. Some ranulas can be removed via transoral surgical approaches, while others require a cervical approach. Objective: To evaluate the indications for doing a cervical approach for ranula excision. Methods: A systematic literature review was performed that included studies analyzing outcomes from cervical approaches for ranula excision. Studies were assessed for their level of evidence, number of participants, and outcomes. Results: Five studies were identified. Of those, 4 studies were level 4, and 1 study was a comprehensive review article of case series and case reports. Overall, the studies demonstrated that plunging ranulas may be removed via an intraoral incision. Revision cases or large pseudocysts, however, require a cervical incision. Also, excision of the sublingual gland should be performed for most ranula and can be done via an intraoral incision. Conclusions: The authors of this study propose that the evidence indicates that many plunging ranulas can be evacuated via an intraoral incision, but the more complex cases require a cervical approach. They also assert that the sublingual gland should be removed in most ranula cases. Reviewer's Comments: This study asks a clinically important question and attempts to answer it with the available, limited, amount of evidence. In this case, the evidence is very limited, as all studies are of level 4 evidence. The authors do a nice job with what is available, and come up with some useful conclusions. They find that even some plunging ranulas are amenable to an intraoral incision for evacuation of their contents. However, there are many cases that are more complicated and require a cervical approach. This review is clinically useful in that it shows that the evidence points to the need to remove the sublingual gland for most ranulas, but this, along with the evacuation of the ranula, can often be performed intraorally. (Reviewer-Josef Shargorodsky, MD, MPH). © 2014, Oakstone Publishing, LLC
Keywords: Ranulas, Sublingual Glands, Surgery, Cervical Approach
Print Tag: Refer to original journal article

Oakstone Publishing, LLC • 2700 Corporate Drive • Suite 100 • Birmingham, AL 35242 205-991-5188 • 1-800-633-4743 • www.practicalreviews.com • [email protected]
Surgical Smoke Can Be More Hazardous Than Cigarette Smoke
How Should We Safely Handle Surgical Smoke?
Born H, Ivey C:
Laryngoscope 2014; (March 19): epub ahead of print
Smoke plume exposure from electrocautery puts patients and operating room staff at increased risk for mutagenicity and disease.
Background: Smoke plumes are an aerosolized substance formed from the use of electrocautery and laser surgical devices. Smoke plumes form a potentially harmful byproduct, which may be dangerous to surgeons, surgical staff, and patients in the operating room. Objective: To evaluate a best practice for reducing the risk of surgical smoke exposure in the operating room. Methods: A literature review was performed that included articles analyzing the risk of smoke plumes. Studies were assessed for their level of evidence, number of participants, and outcomes. Results: Multiple studies were identified. The articles included 1 level 1 study, 1 level 2 study and 3 level 5 evidence studies. One study found that electrocautery produced smoke plumes that were 2 times as mutagenic as compared to carbon dioxide laser irradiation. They determined that smoke plume exposure from electrocautery puts patients and operating room staff at increased risk for mutagenicity and disease. A survey-based study of perioperative nurses in the United States found a 2-times increased prevalence in respiratory conditions such as allergies, sinus infections, asthma, and bronchitis. Conclusions: The authors of this study propose that the evidence indicates that smoke plumes pose a significant health risk to the physician and surgical staff. Current recommendations include the use of personal protective equipment (laser masks) and proper ventilation in the operating room. Reviewer's Comments: The authors note that most of the literature provides anecdotal evidence. However, the available research indicates the presence of a health risk of surgical smoke, and awareness of this danger needs to increase. Survey results have shown that <50% of operating staff use proper evacuation techniques. This is an especially worrisome conclusion of this article. In reality, it is very difficult to study whether or not the health effects of any surgical smoke exposure are real. But the concern, at the very least, does seem to be real among the health care workers. Therefore, the authors propose that standardized guidelines should be considered to increase awareness and compliance. (Reviewer-Josef Shargorodsky, MD, MPH). © 2014, Oakstone Publishing, LLC
Keywords: Surgical Smoke, Safety, Inhalants
Print Tag: Refer to original journal article

Oakstone Publishing, LLC • 2700 Corporate Drive • Suite 100 • Birmingham, AL 35242 205-991-5188 • 1-800-633-4743 • www.practicalreviews.com • [email protected]
Delayed Repair of Mandibular Fractures Does Not Increase Complication Rates
Is Fixation of Mandible Fractures Urgent?
Barker DA, Park SS:
Laryngoscope 2011; 121 (May): 906-907
There is no significant difference in complication rates between early and delayed mandibular fracture repair.
Background: Mandible fractures most often occur due to a traumatic event, so patients are likely suffering from other injuries that require medical attention. While extensive research has studied mandible fractures, controversy exists over the urgency of fixation. Objective: To evaluate if immediate mandibular repair is necessary for long-term outcomes of union and occlusion. Methods: A systematic literature review was performed, which included studies analyzing protocol of mandibular treatment and retrospective studies of immediate versus delayed fixation of mandibular fractures. Studies were assessed for their level of evidence, number of participants, and outcomes. Results: Multiple studies were identified. A retrospective study found no difference in the rate of infection between early and delayed groups, although a significantly greater rate of technical complications was found in the delayed group. A literature review of studies found no significant difference in complication rates between the early and delay group for mandibular repair. Conclusions: The authors propose that evidence does not indicate urgent repair is warranted for better long-term outcomes in patients with mandibular fractures. However, delays can have technical complications such as weakness in the marginal mandibular nerve, exposure of the plate, neuropathic pain, and malocclusion. Reviewer's Comments: The authors analyzed a substantial amount of evidence to lead to their conclusions. Overall, this study provides a useful literature summary and demonstrates that for patients with mandibular fractures, waiting up to 5 days post-injury has not been shown to affect the outcomes of bony union and occlusion. Their conclusions, however, are mostly intuitive. Due to severity of injuries, delay in treatment is often unavoidable. (Although this article was published >1 year ago, the results and issues that arise from this manuscript are still relevant for otolaryngologists. We will continue to keep the readers abreast of newer findings as they arise.) (Reviewer-Josef Shargorodsky, MD, MPH). © 2014, Oakstone Publishing, LLC
Keywords: Mandible Fracture, Fixation, Union, Occlusion
Print Tag: Refer to original journal article

Oakstone Publishing, LLC • 2700 Corporate Drive • Suite 100 • Birmingham, AL 35242 205-991-5188 • 1-800-633-4743 • www.practicalreviews.com • [email protected]
Determine Prophylactic Antibiotic Use on Case-by-Case Basis
Are Prophylactic Antibiotics Useful in the Management of Facial Fractures?
Morris LM, Kellman RM:
Laryngoscope 2014; 124 (June): 1282-1284
There is no evidence that the use of prophylactic antibiotics decreases infection rates in patients with facial fractures.
Background: Infected facial fractures require antibiotics as a course of treatment. Type, timing, duration, and efficacy remain controversial for prophylactic antibiotic use for facial fractures. With cases of antibiotic resistance on the rise, risk and benefits for prophylactic use need to be addressed. Objective: To determine a best practice to determine the efficacy of prophylactic antibiotics for facial fractures. Methods: A systematic literature review was performed, which included studies analyzing the efficacy of prophylactic antibiotics for patients with facial fractures. Studies were assessed for their level of evidence, number of participants, and outcomes. Results: Five studies are explored ranging from 1a, 1b, 2b, 2a, 2b levels of evidence. In a 2006 randomized controlled study of 181 patients, no statistical difference was found for patients receiving postoperative prophylactic antibiotics in open mandibular fractures treated with open reduction internal fixation. A 2010 multi-institutional prospective cohort study of 134 patients with zygomatic fractures found a very low postoperative infection rate of 1.5%. They further evaluated timing of antibiotic use in 223 patients with nonmandibular facial fractures and found no significant benefit of prophylactic antibiotic use outside the perioperative period. In 2011, a systematic review of 9 randomized controlled trials and 22 retrospective case studies found that current evidence supporting the use of antibiotics is limited and that with the risk associated, caution needs to be used. Conclusions: No standard protocol for prophylactic antibiotics can be recommended at this time. Reviewer's Comments: The authors analyzed a substantial amount of evidence to lead to their conclusions. They provide a useful literature summary that demonstrates that further research needs to be conducted. While there is limited evidence to evaluate the efficacy of prophylactic antibiotic use in nonmandibular fractures, there is evidence that suggests postoperative use might not be beneficial. With the growing concern over antibiotic resistance, it is important for physicians to determine if antibiotics are warranted as a prophylactic treatment on a case by case basis. (Reviewer-Josef Shargorodsky, MD, MPH). © 2014, Oakstone Publishing, LLC
Keywords: Prophylactic Antibiotics, Antibiotic Resistance, Facial Fractures
Print Tag: Refer to original journal article

Oakstone Publishing, LLC • 2700 Corporate Drive • Suite 100 • Birmingham, AL 35242 205-991-5188 • 1-800-633-4743 • www.practicalreviews.com • [email protected]
Should You Prescribe Topical Amphotericin B to Treat CRS?
Is Topical Amphotericin B Efficacious in the Treatment of Chronic Rhinosinusitis?
Lupa M, Amedee R:
Laryngoscope 2010; 120 (June): 1080-1081
Routine use of amphotericin B does not improve the symptoms associated with chronic rhinosinusitis.
Background: Chronic rhinosinusitis (CRS) is an inflammatory condition affecting paranasal sinuses and lasting >12 weeks. Although this is one of the most common inflammatory illnesses in the United States, treatment approaches vary among the sinus specialists, and treatment with topical antifungal medication remains controversial. Objective: To evaluate the efficacy of topical amphotericin B for the treatment of CRS. Methods: A systematic literature review was performed that included studies analyzing the use of topical amphotericin B solution irrigations to determine effectiveness. CRS patients were given amphotericin B solution and measured by symptom scores, endoscopic finings, and CT scan compared with placebo groups. Studies were assessed for their level of evidence, number of participants, and outcomes. Results: Multiple studies were identified. Of these, there was 1 case series without an internal control (Level 4), and 4 randomized controlled trials were Level 1 evidence. In a 2002 noncontrolled study of 51 patients and a 2005 double-blind randomized study with 30 patients conducted by the same researcher, amphotericin B was found effective for improved endoscopy score and decreased inflammation, as evidenced by CT scan for patients with CRS. A 2006 randomized controlled trial of 116 patients found no statistical evidence that amphotericin B improves CRS, even when nasal lavages pre- and post-treatment were analyzed. Conclusions: The evidence indicates that topical amphotericin B has a very small likelihood of reducing anti-inflammatory responses either directly or indirectly in CRS and has no effect on severity of symptoms. Reviewer's Comments: CRS is a condition that is very difficult to treat. Therefore, physicians have been looking at multiple different approaches to treat this disease. This study asks a clinically important question and attempts to answer it with the available, but limited, amount of evidence. This review is clinically useful in that it looks at a treatment modality that at least at one point, was used fairly commonly for CRS. Topical amphotericin B rinses were commonly used for a brief period of time when there was a strong belief in the link between CRS and fungal infection. The authors note that the evidence from recent, large randomized controlled trials does not support the efficacy of amphotericin B for the treatment of CRS. However, higher concentrations are not discounted. Further studies need to be conducted to prove effectiveness. (Although this article was published >1 year ago, the results and issues that arise from this manuscript are still relevant for otolaryngologists. We will continue to keep the readers abreast of newer findings as they arise.) (Reviewer-Josef Shargorodsky, MD, MPH). © 2014, Oakstone Publishing, LLC
Keywords: Amphotericin B, Chronic Rhinosinusitis, Antifungal Medications
Print Tag: Refer to original journal article

Oakstone Publishing, LLC • 2700 Corporate Drive • Suite 100 • Birmingham, AL 35242 205-991-5188 • 1-800-633-4743 • www.practicalreviews.com • [email protected]
Is There a Benefit of Transcanalicular Stenting in Endoscopic DCR Cases?
Is Postoperative Stenting Necessary in Endoscopic Dacryocystorhinostomy?
Liang J, Lane A:
Laryngoscope 2013; 123 (November): 2589-2590
Placement of transcanalicular stents does not improve the success rates of endoscopic dacryocystorhinostomy.
Background: Dacryocystorhinostomy (DCR) is commonly performed for the treatment of epiphora from nasolacrimal duct obstruction and can be performed via an external or transnasal endoscopic approach. Transcanalicular stents are often placed at the time of surgery to maintain DCR ostium patency. The importance of the stents, however, is a topic of controversy. Objective: To evaluate whether current evidence supports the placement of stents during endoscopic DCR. Methods: A systematic literature review was performed, which included studies analyzing the outcomes of studies evaluating the effectiveness of transcanalicular stents placed during DCR surgery. Studies were assessed for their level of evidence, number of participants, and outcomes. Results: Three studies were identified, all of which were randomized controlled trials (evidence level 1). Overall, the studies demonstrated that there was no benefit for placing the stents in terms of the success rates of DCR patency. Moreover, the stents may increase the rate of associated complications, such as granulation at the ostium site. Conclusions: The current literature indicates that there is no significant benefit of transcanalicular stents for improving DCR patency in endoscopic DCR cases. Reviewer's Comments: This study asks a clinically important question and attempts to answer it with the available evidence. The authors are able to make a confident conclusion due to the strength of the available evidence. They benefit from having 3 separate randomized controlled studies to draw from. The article is very thoughtful and provides a comprehensive discussion of the topic of whether or not transcanalicular stents are necessary in endoscopic DCR cases. Even though the evidence does not indicate an advantage to using the stents in routine cases, the authors also delve deeper into the topic and suggest that the data do not apply to all cases. For example, revision endoscopic DCR or endoscopic DCR in patients with concurrent rhinosinusitis may warrant stent placement to maintain ostium patency. This review is clinically useful in that it provides guidance backed by strong clinical evidence for surgeons deciding whether or not to place stents during endoscopic DCRs. (Reviewer-Josef Shargorodsky, MD, MPH). © 2014, Oakstone Publishing, LLC
Keywords: Stenting, Dacryocystorhinostomy
Print Tag: Refer to original journal article

Oakstone Publishing, LLC • 2700 Corporate Drive • Suite 100 • Birmingham, AL 35242 205-991-5188 • 1-800-633-4743 • www.practicalreviews.com • [email protected]
Surveillance Recommendations for Inverted Papilloma
What Are the Surveillance Recommendations Following Resection of Sinonasal Inverted Papilloma?
Suh JD, Chiu AG:
Laryngoscope 2014; (March 1): epub ahead of print
Patients whose sites of inverted papilloma are not visible with routine endoscopy should have regular surveillance imaging studies, with MRI as the preferred modality.
Background: Sinonasal inverted papillomas (IPs) are benign tumors of the nose and paranasal sinuses. IPs account for a small percentage of nasal tumors. Due to their high recurrence rate and potential for malignant transformation, surveillance of patients post-resection is crucial. The treatment plan for IP is surgery with endoscopic techniques when feasible. Currently, there are no established guidelines for monitoring patients following IP resection. Objective: To evaluate and determine the appropriate recommendations for surveillance of IP patients post-resection. Methods: A systematic literature review was performed to determine the most effective method of surveillance for IP patients post-resection. Studies were assessed for their level of evidence, number of participants, and outcomes. Results: Specific case studies and systematic reviews were identified. The case studies were level IV and systematic reviews were level III evidence. Overall, the studies demonstrated that the highest risk of IP recurrence is within the first 2 years, although later recurrences can occur. One study found that 73% of the American Society of Head and Neck Surgeons agree with offering monthly follow-up in the first year after surgery, 2- to 3-month follow-up in the second year, and 4- to 6-month follow-up in 3 to 5 years after surgery. They also maintained that the primary method for IP surveillance should be the same as nasal endoscopy, and if the original tumor site is not visible, then annual or biannual imaging studies using MRI as the preferred modality for tumor evaluation should be done. Conclusions: The authors propose that the evidence indicates the importance of establishing surveillance guidelines for patients with IP and suggest that surveillance of IP should be based on those used for head and neck squamous cell carcinoma. Reviewer's Comments: The authors propose a very reasonable perspective on surveillance following IP removal. The article brings up a clinically important question and attempts to answer it with the available, but limited, amount of evidence. This review is clinically useful in that it depicts the necessity of establishing surveillance criteria for IP patients post-resection. Currently, there are no formal established methods for monitoring IP patients after surgery. However, due to the high recurrence rate and risk for malignant transformation, surveillance is important. So a standardized way, such as often used with cancer patients, would go a long way in setting a consistent standard of care for these patients. (Reviewer-Josef Shargorodsky, MD, MPH). © 2014, Oakstone Publishing, LLC
Keywords: Surveillance, Sinonasal Inverted Papilloma, Resection
Print Tag: Refer to original journal article

Oakstone Publishing, LLC • 2700 Corporate Drive • Suite 100 • Birmingham, AL 35242 205-991-5188 • 1-800-633-4743 • www.practicalreviews.com • [email protected]
LEMG Useful for Evaluation of Laryngeal Paralysis/Paresis
Is Laryngeal Electromyography Useful in the Diagnosis and Management of Vocal Fold Paresis/Paralysis?
Meyer TK, Hillel AD:
Laryngoscope 2011; 121 (February): 234-235
Laryngeal electromyography can help differentiate vocal fold immobility from neural disruption from that caused by a structural abnormality.
Background: Vocal fold impairment is a challenging disorder that can potentially be debilitating. The accurate and precise assessment of vocal fold mobility may be difficult. Laryngeal electromyography (LEMG) is an electrodiagnostic study to help determine the exact motor activity of the vocal folds. Objective: To evaluate whether LEMG is a useful diagnostic modality for patients with suspected vocal fold mobility impairment. Methods: A systematic literature review was performed, which included studies analyzing the usefulness of LEMG. Studies were assessed for their level of evidence, number of participants, and outcomes. Results: Five studies were identified. Of those, 3 studies were level 4 evidence, and 2 studies were literature reviews. Overall, the studies demonstrated that LEMG is a useful diagnostic tool, especially in differentiating structural immobility from neural disruption as the cause of impaired vocal fold mobility. The study can also determine the side of the dysfunction in cases that are subtle. Conclusions: The authors propose that the evidence indicates that the LEMG is a very useful clinical tool. The clinicians can use the LEMG to diagnose the etiology of the vocal fold immobility, confirm the side of the dysfunction, and determine the severity, with the goal of being able to better tailor the appropriate management for these patients. Reviewer's Comments: This study asks a clinically important question and attempts to answer it with the available, limited, amount of evidence. The amount of data is, in fact, very limited, with no prospective or randomized studies available. The authors, nonetheless, do a good job in analyzing the available literature and coming up with useful conclusions. Overall, they determine that the LEMG is a very useful study. Given that certain aspects of vocal fold mobility cannot be assessed with just endoscopy, the additional information attained from an LEMG can help provide the correct diagnosis for these patients. This review is clinically useful in that it validates his important diagnostic tool for vocal fold mobility assessment, which may ultimately improve these patients' management. (Although this article was published >1 year ago, the results and issues that arise from this manuscript are still relevant for otolaryngologists. We will continue to keep the readers abreast of newer findings as they arise.) (Reviewer-Josef Shargorodsky, MD, MPH). © 2014, Oakstone Publishing, LLC
Keywords: Laryngeal Electromyography, Vocal Fold Paresis/Paralysis
Print Tag: Refer to original journal article

Oakstone Publishing, LLC • 2700 Corporate Drive • Suite 100 • Birmingham, AL 35242 205-991-5188 • 1-800-633-4743 • www.practicalreviews.com • [email protected]
Treating Patulous Eustachian Tube With Hydroxyapatite Injection
Endoscopic Hydroxyapatite Augmentation for Patulous Eustachian Tube.
Vaezeafshar R, Turner JH, et al:
Laryngoscope 2014; 124 (January): 62-66
Patulous eustachian tube augmentation with hydroxyapatite may be a safe and effective treatment option.
Background: Patulous eustachian tube (PET) is a bothersome condition, presenting with autophony, aural fullness, and tinnitus. While several treatment approaches have been documented, none have been consistently effective. Objective: To evaluate the safety and efficacy of hydroxyapatite injections for treatment of PET. Methods: The authors performed a retrospective case series of 14 patients, all with at least 2 of the major PET symptoms on history and with diagnosis confirmed by tympanic membrane hypermobility with nasal breathing on otoscopy who were undergoing endoscopic hydroxyapatite injection for PET. The injection was performed under general anesthesia, injecting hydroxyapatite at 3, 9, and 12 o'clock positions along the torus tubarius. Postoperative outcomes were assessed using a standardized PET scoring system. Results: Fourteen patients were treated (5 unilateral and 9 bilateral). For voice autophony, 59% of patients noted complete or significant postoperative improvement as did 63% of patients with ear fullness. There were no intraoperative or postoperative complications. In patients with documented improvement, there was recurrence of symptoms for the duration of the follow-up period. Conclusions: Endoscopic injection of hydroxyapatite is a feasible surgical procedure for patients with PET. It is a promising, minimally invasive, and reversible option for treating PET. Reviewer's Comments: PET is difficult to treat due to its anatomic location and the associated physiology, with a very limited number of treatment options. This study takes a creative approach for a minimally invasive surgical solution to the difficult problem. Hydroxyapatite injections are reversible, providing an extra level of safety in case the treatment does not work. In this thoughtful and clinically relevant study, the authors describe a very simple and reproducible method of safely injecting a temporary filler to decrease the patulous nature of the eustachian tube orifice. They demonstrate a good safety profile, as there were no complications in their patient cohort. The effectiveness is comparable with the more invasive procedures that have been tried to address this problem. Overall, it is an interesting study, with a proposed surgical approach that deserves further consideration. (Reviewer-Josef Shargorodsky, MD, MPH). © 2014, Oakstone Publishing, LLC
Keywords: Patulous Eustachian Tube, Hydroxyapatite, Augmentation
Print Tag: Refer to original journal article

Oakstone Publishing, LLC • 2700 Corporate Drive • Suite 100 • Birmingham, AL 35242 205-991-5188 • 1-800-633-4743 • www.practicalreviews.com • [email protected]
EMLP Is Effective Surgical Approach for Refractory Frontal Sinusitis
Long-Term Outcomes for the Endoscopic Modified Lothrop/Draf III Procedure: A 10-Year Review.
Naidoo Y, Bassiouni A, et al:
Laryngoscope 2014; 124 (January): 43-49
The endoscopic modified Lothrop procedure provides good long-term relief for patients with refractory frontal sinusitis.
Background: Recalcitrant frontal sinusitis provides a significant surgical challenge for otolaryngologists. Prior research has documented the short-term effectiveness of the endoscopic modified Lothrop procedure (EMLP), but long-term outcomes have not been confirmed for this patient group. Objective: To evaluate the long-term outcomes for the EMLP for patients with frontal sinusitis recalcitrant to prior medical and conventional surgical treatment. Design/Participants: Retrospective review of patients, conducted over a 10-year period, undergoing EMLP for recalcitrant frontal sinusitis. Methods: Patients were included if they had persistent frontal sinusitis despite at least a 2-month course of maximal medical therapy, including systemic steroids, topical steroids, saline irrigations, and culture directed antibiotics. All of the patients also had prior standard endoscopic sinus surgery. Data collected included demographic factors, allergy status, symptom questionnaires, postoperative endoscopic and symptom-based evaluation, and measured dimension of the frontal sinus ostium. The surgery consisted of complete removal of ethmoid partitions and superior septectomy with frontal sinus drillout. Results: A total of 229 patients were identified for the study, with a mean follow-up of 45 months. All patients reported postoperative symptomatic improvement. Forty-seven percent of patients reported being completely asymptomatic after surgery, while only 8% had persistent severe symptoms. The frontal sinus patency rate was 97%. Twelve patients required revision EMLP for persistent symptoms and narrowing of the frontal sinus ostium. Conclusions: According to the authors, this is the largest series of EMLP patients, and the results illustrate effective long term disease control in the vast majority of patients undergoing the operation. A small percentage of patients continue to have further symptomatic inflammation, and further research is needed to determine the underlying reason for these treatment failures. Reviewer's Comments: This excellent review of a single surgeon's results over a 10-year period clearly demonstrates the effectiveness of the treatment approach in his patient population. It does a good job identifying the proper patient population for the procedure, and selects multiple relevant outcome measures for review. The biggest weakness of the article is that it is a single-institution, single-surgeon patient population. Although this may bias the results and reduce the reproducibility, it also adds consistency to the treatment approach that may not be possible with multiple centers. The article also does a good job explaining treatment failures. Clearly, further research is needed to identify reasons for why patients fail their initial sinus surgery and medical therapy and why a small percentage even fail the extended approach described in this article. (Reviewer-Josef Shargorodsky, MD, MPH). © 2014, Oakstone Publishing, LLC
Keywords: Frontal Sinus, Sinusitis, Modified Lothrop, Outcomes Research
Print Tag: Refer to original journal article

Oakstone Publishing, LLC • 2700 Corporate Drive • Suite 100 • Birmingham, AL 35242 205-991-5188 • 1-800-633-4743 • www.practicalreviews.com • [email protected]
When Should Imaging Be Obtained for Suspected CRS?
Primary Care and Upfront Computed Tomography Scanning in the Diagnosis of Chronic Rhinosinusitis: A Cost-Based
Decision Analysis.
Leung RM, Chandra RK, et al:
Laryngoscope 2014; 124 (January): 12-18
Obtaining a sinus CT prior to an otolaryngology referral by a primary care physician is cost-effective.
Background: Current guidelines recommend a combination of persistent subjective symptoms and an objective positive finding on either a CT scan or endoscopy to diagnose chronic rhinosinusitis (CRS). The recommended limitation of CT scanning leads many patients to be treated empirically and referred to otolaryngologists prior to either confirming or ruling out the diagnosis. An earlier use of CT scanning may decrease the health care costs for these patients. Objective: To assess the cost-effectiveness of obtaining a CT scan prior to medical treatment or an otolaryngology referral to provide an evidence-based guide for the primary practitioner. Methods: A cost-effectiveness analysis was performed evaluating 2 management algorithms: (1) for the primary care physician (PCP) to obtain sinus CT imaging based on reported symptoms prior to medical treatment or an otolaryngology referral; or (2) treating the patient based on clinical suspicion according to their reported symptoms, with either upfront medical management or an otolaryngology referral, with the CT only being obtained in cases that require the imaging for surgical planning. Within each algorithm, a scenario was created where the PCP either treats the patient medically for suspected CRS or refers to an otolaryngologist. These 2 different scenarios were simulated in a model of cost-based decision analysis based on probabilities and Medicare costs reported in the existing literature. Results: The first scenario, where the PCP treats the patient medically demonstrated a cost savings of obtaining a CT upfront of >$503.10 per patient. The second scenario, where the PCP refers the patient demonstrated a cost savings of $326.04 when the CT was ordered upfront. Conclusions: Obtaining the sinus CT upfront by the PCP is cost-effective as compared with either initial medical management or otolaryngology referral. This approach can potentially save the U.S. health care system over $3 billion per year. Reviewer's Comments: This study is well thought out and, if true, the recommendations can provide substantial cost savings to the health care system. However, as the authors note, predicting PCP comfort with diagnosing and treating CRS is difficult. Given that this study is based on models that attempt to do just that, the conclusions must be approached with caution. Patients who present with facial pain are much more likely to have migraine variants than actual CRS, but often push on their physicians to provide treatment for their "sinusitis," leading to misdiagnosis and inappropriate treatment. While this study notes this difficulty, in reality, this phenomenon provides inconsistencies in patient encounters that cannot be assessed in the models used in this study. Nonetheless, the study does point out the need for further cost-effectiveness analyses of when imaging should be obtained for patients with suspected CRS. (Reviewer-Josef Shargorodsky, MD, MPH). © 2014, Oakstone Publishing, LLC
Keywords: Chronic Sinusitis, Primary Care, Endoscopy, Imaging, Diagnosis
Print Tag: Refer to original journal article

Oakstone Publishing, LLC • 2700 Corporate Drive • Suite 100 • Birmingham, AL 35242 205-991-5188 • 1-800-633-4743 • www.practicalreviews.com • [email protected]
Prophylactic Antibiotics Not Recommended for Skull Base Fractures
What Is the Efficacy of Prophylactic Antibiotics in Basilar Skull Fractures?
Nellis JC, Kesser BW, Park SS:
Laryngoscope 2014; 124 (January): 8-9
There is no statistically significant evidence for treating patients with skull base fractures with prophylactic antibiotics.
Background: Although there is concern for meningitis in patients with basilar skull fractures with associated cerebrospinal fluid (CSF) leaks, the efficacy of prophylactic antibiotics in preventing meningitis has not been established. Objective: To determine whether or not there is sufficient evidence to recommend prophylactic antibiotics to decrease the risk of meningitis in patients with basilar skull base fractures with associated CSF leaks. Methods: A review was made of the current literature for studies comparing the risks of meningitis in patients with CSF leaks from skull base fractures who received antibiotics versus those who did not. Studies were analyzed based on their quality scores, patient numbers, and outcomes. Results: Four studies were identified. All of the studies showed a trend toward a higher incidence of meningitis in patients who did not receive prophylactic antibiotics, although only 1 study demonstrated a significant difference in the incidence between those who did and did not receive antibiotics (P =0.006). The study that showed a statistically higher incidence of meningitis had a level of evidence of 3a, while the other three studies had evidence levels of 3a, 1b, and 1a. Conclusions: There is large body of evidence demonstrating no significant reduction in meningitis incidence with the use of prophylactic antibiotics in patients with CSF leaks from skull base fractures. Reviewer's Comments: This is an important study that addresses a common and important question in otolaryngology practice. The authors do a good job of objectively evaluating the existing evidence. The findings help guide future medical practice in recommending avoidance of prophylactic antibiotics for patients with CSF leaks from skull base fractures. Although review papers, such as this one, have to rely on the available evidence, which is often conflicting, the studies evaluated in this review are of a high quality (2 out of 4 with an evidence level of 1a or 1b, and combined have almost 2,000 participants. While future larger studies may shed more light on this subject, the studies analyzed in this review allow for a fairly confident conclusion. (Reviewer-Josef Shargorodsky, MD, MPH). © 2014, Oakstone Publishing, LLC
Keywords: Prophylactic Antibiotics, Skull Base Fracture, Meningitis
Print Tag: Refer to original journal article

Oakstone Publishing, LLC • 2700 Corporate Drive • Suite 100 • Birmingham, AL 35242 205-991-5188 • 1-800-633-4743 • www.practicalreviews.com • [email protected]
Adenoidectomy or Adenotonsillectomy for Upper Airway Obstruction?
Is Adenoidectomy Alone Sufficient for the Treatment of Airway Obstruction in Children?
Black AP, Shott SR:
Laryngoscope 2014; 124 (January): 6-7
Adenoidectomy alone is sufficient without tonsillectomy to treat children with upper airway obstruction without significant tonsillar hypertrophy.
Background: Adenoidectomy and adenotonsillectomy are often performed to improve a child's upper airway obstruction. The addition of tonsillectomy, however, more than triples the risk of postoperative bleeding as compared with just adenoidectomy. In children with adenoid hypertrophy without tonsil hypertrophy, both procedures are often performed despite the significant additional morbidity of the tonsillectomy. Objective: To evaluate whether adenoidectomy alone is sufficient for the treatment of upper airway obstruction in children who have adenoid but not tonsil hypertrophy. Methods: A systematic literature review was performed that included studies analyzing outcomes of adenoidectomy alone as compared with adenotonsillectomy for children with upper airway obstruction and adenoid but not tonsil hypertrophy. Studies were assessed for their level of evidence, number of participants, and surgical outcomes. Results: Four studies were identified. Of these, 2 studies were level 3 and 2 were level 4 evidence. Overall, the studies demonstrated that adenoidectomy alone was sufficient for the majority of children examined, with no need for subsequent tonsillectomy. The risk of needing subsequent tonsillectomy ranged from 2% to 29%, and the risk factors for needing tonsillectomy included age <2 years for everyone and <3 years for girls as well as presence of tonsillar hypertrophy. Conclusions: An adenoidectomy alone is sufficient to treat upper airway obstruction in the majority of children with upper airway obstruction with adenoid but not tonsillar hypertrophy. Reviewer's Comments: This study asks a clinically important question and attempts to answer it with the available, but limited, amount of evidence. Adenoid hypertrophy is very common in children, and adenoidectomy is one of the most common pediatric surgical procedures. Adding tonsillectomy to the procedure adds significant risks, the most notable of which is postoperative hemorrhage. And yet, tonsillectomy is commonly performed in conjunction with adenoidectomy to avoid having to put the child through another surgical procedure later on, assuming that many children will ultimately need it. These authors attempted to address that assumption, looking at whether there is enough evidence in the literature to determine if a sizable enough proportion of children undergoing adenoidectomy for airway obstruction ultimately end up requiring a tonsillectomy later on. They found that the evidence is rather limited, but does not appear to demonstrate a significant amount of children requiring subsequent tonsillectomy to warrant performing adenotonsillectomy even in the absence of significant tonsillar hypertrophy. They do, however, identify risk factors for needing future tonsillectomy, including age <2 years old and tonsillar hypertrophy. This review is clinically useful in that it demonstrates that it is reasonable to avoid performing a tonsillectomy unless the surgical candidate fits into one of the above risk factor groups. (Reviewer-Josef Shargorodsky, MD, MPH). © 2014, Oakstone Publishing, LLC
Keywords: Adenoidectomy, Tonsillectomy, Obstruction, Pediatric
Print Tag: Refer to original journal article