Mortality at 120 days after prostatic biopsy: A population-based study of 22,175 men
-
Upload
andrea-gallina -
Category
Documents
-
view
212 -
download
0
Transcript of Mortality at 120 days after prostatic biopsy: A population-based study of 22,175 men

Mortality at 120 days after prostatic biopsy: A population-based
study of 22,175 men
Andrea Gallina1,2, Nazareno Suardi1,2, Francesco Montorsi2, Umberto Capitanio1,2, Claudio Jeldres1, Fred Saad1,Markus Graefen3, Shahrokh F. Shariat4, Hugues Widmer1, Philippe Arjane1, Francois P�eloquin1,Paul Perrotte
1and Pierre I. Karakiewicz
1*
1Cancer Prognostics and Health Outcomes Unit, University of Montreal, Montreal, Quebec, Canada2Department of Urology, Vita-Salute University, Milan, Italy3Martini Clinic-Prostate Cancer Center, University of Hamburg, Hamburg, Germany4Department of Urology, University of Texas Southwestern Medical Center, Dallas, TX
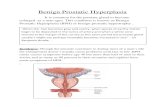
Trans-rectal ultrasound guided biopsy of the prostate representsthe diagnostic standard for prostate cancer, but its mortality ratehas never been examined. We performed a population-based studyof 120-day mortality after prostate biopsy in 22,175 patients, whounderwent prostate biopsy between 1989 and 2000. The controlgroup consisted of 1,778 men aged 65–85 years (median 69.5), whodid not undergo a biopsy. Univariable and multivariable logisticregression analyses were performed in 11,087 of 22,175 (50%)men subjected to prostate biopsy, to identify predictors of 120-daymortality. Variables were age at biopsy, baseline Charlson comor-bidity index and cumulative number of biopsy procedures. Weexternally validated the model’s predictors in the remaining 50%of men. Overall 120-day mortality after biopsy was 1.3% versus0.3% (p < 0.001) in the control group. Of men aged ≤60 years,0.2% died within 120 days versus 2.5% aged 76–80. Zero Charlsoncomorbidity score yielded 0.7% mortality versus 2.2%, if 3–4.First ever biopsy procedures carried a higher mortality risk thansubsequent procedures (1.4 vs. 0.8 vs. 0.6%). In the multivariablemodel, first ever biopsy, increasing age and comorbidity predictedhigher mortality. Overall, the model’s variables were 79% accu-rate in predicting the probability of 120-day mortality after bi-opsy. In conclusion, our data suggest that prostate biopsy mightpredispose to higher mortality rate. The certainty of this associa-tion remains to be proven.' 2008 Wiley-Liss, Inc.
Key words: prostate cancer; diagnosis; prostate biopsy; mortality;nomogram
Prostate cancer (PCa) is one of the most common male malig-nancies in the United States.1 Trans-rectal ultrasound (TRUS)guided biopsy of the prostate represents the cornerstone diagnosticprocedure in patients at risk for PCa. The indications for perform-ing a TRUS biopsy have substantially broadened over the past 2decades.2 An increasing number of men without digital rectalexamination (DRE) abnormalities and with increasingly lowerprostate specific antigen (PSA) blood levels are subjected toTRUS biopsy and may result in higher absolute number of compli-cations.3–8 Infectious complications are most common and mayresult in septic shock or other life-threatening conditions. Instan-ces of severe hemorrhage,9,10 osteitis pubis,11 abscess forma-tion,12–14 endocarditis,15,16 multi-drug resistant infections,17 sepsisor septic shock have been reported.12,18 These complications arerare but nonetheless can result in biopsy related mortality. To thebest of our knowledge, except for isolated case reports, no previ-ous large-scale analysis addressed the rate of mortality afterTRUS prostate biopsy. To address this void, we performed a popu-lation-based study of 120-day mortality after TRUS biopsy in22,175 men subjected to TRUS-guided prostate biopsy. Moreover,we tested whether patients at a negligible risk of 120-day mortalitycan be accurately identified.
Material and methods
The Quebec Health Plan represents the exclusive insurer in theProvince of Quebec and its database allows ascertainment of allhealth services covered by the Plan. These include prostate biopsy.
Moreover, the Health Plan relies on ICD-9 diagnostic codes andtheir respective dates allow defining individual Charlson comor-bidity index scores.19,20 Finally, the Health Plan provides crudesurvival data for all enrollees.
The Health Plan data allowed us to identify all men who under-went a prostate biopsy between 1989 and 2000. Each recordincluded age at biopsy, number of previous biopsy sessions if ap-plicable, vital status at 120 days after prostate biopsy, as well asthe Charlson comorbidity index score.20 None of included patientsreceived definitive treatment for PCa before the end of the120 days interval. The analyses targeted 22,175 evaluable patients.
For comparison purposes, we also used a convenience sampleof 1,778 men aged 65–85 years (mean 71, median 69), who wereunexposed to a biopsy procedure. These men were entered into theHealth Plan records between 1989 and 1995. The follow-up periodof 120 days consisted of the 120-day interval starting on the 1stday of registration with the Health Plan. Since diagnostic codesused in the definition of the Charlson Comorbidity Index areentered prospectively in the Health Plan database, the calculationof the Charlson Comorbidity Index was not possible for the con-trol group and only overall and age-stratified comparisons with thebiopsy-exposed cohort could be made. Since no new enrolleeswere identified in the 86–90 years of age category, mortality com-parisons could not be made for this age stratum.
Statistical analyses
The proportion of deaths from any cause at 120 days was com-pared using the chi-square statistic, between individuals exposedto prostate biopsy and the controls who did not have a biopsy.Subsequent statistical analyses relied of logistic regression mod-els, which targeted overall mortality at 120 days in a 50% randomsample (n 5 11088) from the original cohort of 22,175 patientsexposed to a prostate biopsy. This cohort will be referred to as thedevelopment cohort. Predictors of 120-day mortality consisted ofage at biopsy (coded as cubic spine to allow non-linear effects),Charlson comorbidity index at biopsy and the cumulative numberof biopsy procedures that each individual was exposed to between1989 and 2000, including the last index biopsy procedure. Thesevariables were then used within a multivariable logistic regressionmodel designed to predict the individual probability of 120-daymortality after prostate biopsy. In multivariable models, fast back-
Grant sponsors: University of Montreal Urology Associates, Fonds de laRecherche en Sant�e du Qu�ebec, the University of Montreal Department ofSurgery and the University of Montreal Foundation.*Correspondence to: Cancer Prognostics and Health Outcomes Unit,
University of Montreal Health Center (CHUM), 1058, rue St-Denis, Mon-tr�eal, Qu�ebec, Canada H2X 3J4. Fax:11514-227-5103.E-mail: [email protected] 5 September 2007; Accepted after revision 25 February 2008DOI 10.1002/ijc.23559Published online 9 May 2008 in Wiley InterScience (www.interscience.
wiley.com).
Int. J. Cancer: 123, 647–652 (2008)' 2008 Wiley-Liss, Inc.
Publication of the International Union Against Cancer

ward variable selection relied on Akaike’s information criteria toidentify independent predictors of biopsy mortality.21
To confirm the validity of our model and the significance of itspredictor variables we tested the accuracy of the model (quantifiedwith the area under the receiver operating characteristics curve[AUC]) within the remaining 50% of our population (n 5 11087).The model was then displayed graphically to illustrate the multi-variable effects of the predictors on the probability of 120-daymortality after biopsy. All statistical tests were performed using S-PLUS Professional, version 1 (MathSoft, Seattle, WA). All testswere two-sided with a significance level set at 0.05.
Results
Patient characteristics are shown in Table I. Mean age at biopsywas 69.3 years (median 69). The distribution of patients across5 year intervals was as follows: �60 years 12.1%, 61–65, 18.9%;66–70, 27.0%; 71–75, 21.6%; 76–80, 12.8%; 81–85, 5.8%; 86–90,1.5% and >90, 0.2%. Charlson comorbidity index score was 0 in
40.7%, 1–2 in 40.4%, 3–4 in 14.4%, 5–6 in 3.7% and 7 or more in0.9% of patients. Most (78.8%) underwent 1 prostate biopsy ses-sion. Two or more biopsy procedures were performed in 15.9 and5.3% of patients, respectively. The nomogram development cohortand the external validation cohort failed to demonstrate statisti-cally significant differences in the distribution of known variables,such as age at biopsy, Charlson comorbidity index score, totalnumber of biopsy procedures, year of biopsy and the region of res-idence.
At 120 days, 279 of 22175 men died, which resulted in an over-all mortality rate of 1.3% versus 6 of 1778 men (0.3%, p < 0.001)in the control group. The mortality rate in individuals aged85 years of age or less was 1.1% in the cohort of men exposed toprostate biopsy versus 0.3% in the control group (p 5 0.0018).Age-specific mortality was respectively 0.2, 0.2, 0.8 and 0.8%, forage categories 65–70, 71–75, 76–80 and 81–85 years. Figure 1agraphically displays age-specific overall mortality rate at 120 daysafter prostate biopsy in the entre cohort of 22,175 men versus thecontrol group of 1,778 men (data not shown for men older than85). Despite a difference in the recorded mortality rate between
TABLE I – DESCRIPTIVE CHARACTERISTICS OF PATIENTS INCLUDED IN THE ANALYSES (n 5 22175) AND OF THE CONTROL POPULATION (n 5 1778)
Overall Nomogram development External validation p-value Control population
Number of patients 22,175 11,088 11,087 1,778Age (years) 0.8
Mean (Median) 69.3 (69) 69.3 (69) 69.3 (69) 71.1 (69.5)Range 36–101 36–101 41–97 65–85
1.0�60 2,693 (12.1) 1,345 (12.1) 1,348 (12.2) –61–65 4,184 (18.9) 2,091 (18.9) 2,093 (18.9) –66–70 5,987 (27.0) 3,013 (27.2) 2,974 (26.8) 967 (54.4)71–75 4,795 (21.6) 2,377 (21.4) 2,418 (21.8) 431 (24.2)76–80 2,838 (12.8) 1,429 (12.9) 1,409 (12.7) 250 (14.1)81–85 1,294 (5.8) 648 (5.8) 646 (5.8) 130 (7.3)86–90 333 (1.5) 160 (1.4) 173 (1.6) –>90 51 (0.2) 25 (0.2) 26 (0.2) –
Charlson comorbidity index score 1.00 9,020 (40.7) 4,510 (40.7) 4,510 (40.7) –1–2 8,949 (40.4) 4,475 (40.4) 4,474 (40.4) –3–4 3,183 (14.4) 1,591 (14.3) 1,592 (14.4) –5–6 822 (3.7) 411 (3.7) 411 (3.7) –7 or more 201 (0.9) 101 (0.9) 100 (0.9) –
Number of biopsy session 0.41 17,471 (78.8) 8,693 (78.4) 8,778 (79.2) –2 3,531 (15.9) 1,797 (16.2) 1,734 (15.6) –3 or more 1,173 (5.3) 598 (5.4) 575 (5.2) –
Year or biopsy 0.91989–90 1,608 (7.3) 802 (7.2) 806 (7.3) 636 (35.8)1991 1,047 (4.7) 546 (4.9) 501 (4.5) 302 (17.0)1992 1,689 (7.6) 852 (7.7) 837 (7.5) 230 (12.9)1993 2,303 (10.4) 1,160 (10.5) 1,143 (10.3) 214 (12.0)1994 2,351 (10.6) 1,167 (10.5) 1,184 (10.7) 184 (10.3)1995 1,947 (8.8) 980 (8.8) 967 (8.7) 212 (11.9)1996 1,910 (86) 947 (8.5) 963 (8.7) –1997 2,180 (9.8) 1,065 (9.6) 1,115 (10.1) –1998 2,218 (10.0) 1,103 (9.9) 1,115 (10.1) –1999 2,618 (11.8) 1,324 (11.9) 1,294 (11.7) –2000 2,304 (10.4) 1,142 (10.3) 1,162 (10.5) –
Region of residence 0.6Montreal 5,632 (25.4) 2,797 (25.2) 2,835 (25.6) –Bas Saint Laurent 845 (3.8) 441 (4.0) 404 (3.6) –Saguenay-Lac Saint Jean 721 (3.3) 360 (3.2) 361 (3.3) –Quebec City 1,959 (8.8) 984 (8.9) 975 (8.8) –Mauricie et Centre du Quebec 1,775 (8.0) 884 (8.0) 891 (8.0) –Estrie 1,078 (4.9) 539 (4.9) 539 (4.9) –Chaudiere-Appalches 1,386 (6.3) 701 (6.3) 685 (6.2) –Laval 1,079 (4.9) 556 (5.0) 523 (4.7) –Lanaudiere 921 (4.2) 440 (4.0) 481 (4.3) –Laurentides 1,474 (6.6) 755 (6.8) 719 (6.5) –Monteregie 3,611 (16.3) 1,821 (16.4) 1,790 (16.1) –Others 1,694 (7.6) 810 (7.3) 884 (8.0) –
Mortality at 120 days 279 (1.3) 144 (1.3) 135 (1.2) 0.6 6 (0.3)
Values in paranthesis indicates percentages.
648 GALLINA ET AL.

the 2 groups, across all age ranges, the confidence intervals aroundthe survival estimates of biopsy exposed and biopsy unexposedmen overlap. Figure 1b illustrates the difference in the rate of mor-tality in controls relative to men exposed to prostate biopsy, afterrestricting the biopsy population to those men without any comor-bidity, according to the Charlson index. Figures 1c–1f respectivelyillustrate the mortality rates according to the time interval after bi-opsy, the Charlson comorbidity index score, the number of biopsy
session and the year of biopsy during the study period in the popu-lation of 22,175 men.
For example, the mortality in patients younger than 60 years oldwas 0.2 versus 2.5% for men aged 76–80 years (Table II). Simi-larly, the mortality in patients without comorbidities was 0.7 vs.2.2% in patients with 3–4 comorbidities. Finally, the mortality inpatients subjected to 3 or more biopsy procedure was 0.6% versus1.4% in patients subjected to only 1 biopsy procedure. During the
FIGURE 1 – Mortality at 120 days after prostate biopsy according to age category (Panel 1a). Mortality at 120 days after prostate biopsyaccording to age category in men with no comorbidities (Panel 1b). Mortality at 30, 60, 90 and 120 days after biopsy (Panel 1c). Mortality at120 days after prostate biopsy according to Charlson comorbidity index score (Panel 1d), number of biopsy session (Panel 1e) and year of biopsy(Panel 1f). Panels 1a–1c also show the mortality rate in the control population. [Color figure can be viewed in the online issue, which is availableat www.interscience.wiley.com.]
TABLE II – MORTALITY AT 120 DAYS AFTER BIOPSY, ACCORDING TO AGE, COMORBIDITY,NUMBER OF BIOPSY SESSION AND YEAR OF BIOPSY
Biopsy population Control population
n (%) 95% confidence intervals n (%) 95% confidence intervals
Total 279 (1.3) 1.11–1.41 6 (0.3) 0.12–0.73Age
�60 5 (0.2) 0.06–0.43 – –61–65 12 (0.3) 0.15–0.50 – –66–70 37 (0.6) 0.44–0.85 2 (0.21) 0.03–0.7571–75 60 (1.3) 0.96–1.61 1 (0.23) 0.01–1.2976–80 72 (2.5) 1.99–3.18 2 (0.8) 0.09–2.8681–85 57 (4.4) 3.35–5.67 1 (7.7) 0.02–4.2186–90 25 (7.5) 4.92–10.88 – –>90 11 (21.6) 11.29–35.32 – –
Charlson comorbidity index score0 65 (0.7) 0.5–0.9 – –1–2 107 (1.2) 0.9–1.4 – –3–4 69 (2.2) 1.7–2.7 – –5–6 26 (3.2) 2.1–4.6 – –71 12 (6.0) 3.1–10.2 – –
Number of biopsy session1 242 (1.4) 1.2–1.5 – –2 30 (0.8) 0.5–1.2 – –31 7 (0.6) 3.1–10.2 – –
Year of biopsy1989–90 28 (1.7) 1.1–2.5 – –1991 18 (1.7) 1.0–2.7 – –1992 32 (1.9) 1.3–2.6 – –1993 31 (1.3) 0.9–1.9 – –1994 30 (1.3) 0.8–1.8 – –1995 17 (0.9) 0.5–1.4 – –1996 27 (1.4) 0.9–2.0 – –1997 24 (1.1) 0.7–1.6 – –1998 27 (1.2) 0.8–1.7 – –1999 28 (1.1) 0.7–1.5 – –2000 17 (0.7) 0.4–1.2 – –
Data for controls are only stratified according to age.
649MORTALITY AFTER PROSTATE BIOPSY

study period, a decreasing albeit non-significant (p 5 0.1) trend in120-day mortality rate was recorded.
Table III shows univariable and multivariable logistic regres-sion models addressing to the mortality at 120 days after prostatebiopsy in the nomogram development cohort. In univariable anal-yses, age (p < 0.001), Charlson comorbidity index score (p <0.001) and the total number of biopsy procedures (p 5 0.02) werehighly statistically significant, whereas the year of biopsy (p 50.1) and the region of origin (p 5 0.6) failed to reach statisticalsignificance. In multivariable analyses, age, Charlson comorbidityindex score and the total number of biopsy procedures representedindependent predictors of 120-day mortality (all p � 0.03), werenot removed from the final multivariate model and were includedin the nomogram.
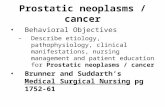
Figure 2a shows the graphical representation of the effect of thepredictor variables on the rate of mortality at 120 days after bi-opsy. The model’s overall predictive accuracy was confirmed inthe independent cohort of 11,087 patients, where the model dem-onstrated 79.3% accuracy (AUC p < 0.001). Moreover, the testingof our model’s performance characteristics confirmed excellentcalibration, which was evidenced by virtually perfect correlationbetween predicted probabilities and observed rates of 120-daymortality (Fig. 2b).
Discussion
PCa is one of the most common non-cutaneous male malignan-cies in North America.1 TRUS guided prostate biopsy is the diag-nostic gold standard for men at risk of PCa. Despite its overallproven safety profile, prostate biopsy has been associated with
life-threatening complications.9–18 However, we are unaware oflarge scale, population-based studies that reported short-term mor-tality rates after biopsy. On the basis of this limitation, we decidedto address 120-day mortality in a large population-based adminis-trative database. We hypothesized that prostate biopsy may berelated to non-negligible rate of 120-day mortality and we testedour hypothesis in a cohort of 22,175 men subjected to a prostatebiopsy. We used a convenience sample of 1,778 men unexposedto prostate biopsy to assess 120-day mortality in a control group.
Our analyses demonstrated a 1.3% overall mortality rate at 120-days after biopsy vs. 0.3% in the control group. The mortality rateaccording to 5-year age strata from 66–85 years ranged from 0.6to 4.4% in the cohort of 22,175 biopsied patients versus from 0.2to 0.8% in the control group of 1,778 men. This differencebetween controls and biopsy-exposed individuals persisted, whenwe restricted the analysis to men without any comorbiditiesaccording to the Charlson index and to 85 years of age or younger.
In the univariable logistic regression analyses predicting 120-days mortality in the development cohort of 11,088 men, age,Charlson comorbidity and the total number of biopsy procedurewere statically significant predictors (Table II). In the multivari-able logistic regression models, age, Charlson comorbidity indexscore and the total number of biopsy procedures represented inde-pendent predictors. We confirmed the accuracy of this model inthe remaining 50% of the population, where the model achieved79.3% accuracy (AUC p < 0.001).
All diagnostic procedures are associated with complications. In-fectious complications represent the main adverse outcomes ofprostate biopsy. Severe infections and septic shock have beenreported in several publications.12,15,17,18 The mortality of septic
TABLE III – UNIVARIABLE AND MULTIVARIABLE LOGISTIC REGRESSION ANALYSES PREDICTING MORTALITY AT 120 DAYSAFTER PROSTATE BIOPSY IN THE NOMOGRAM DEVELOPMENT COHORT (n 5 11,088)
PredictorsUnivariable logistic regression Multivariable logistic regression
OR 95% CI p-value OR 95% CI p-value
Age at biopsy – – <0.001 – – <0.001Age 1.06 0.87–1.29 0.5 1.06 0.87–1.28 0.6Age 1.23 0.78–1.91 0.4 1.21 0.77–1.88 0.4Age 0.52 0.47–7.70 0.4 0.55 0.13–2.20 0.4
Charlson comorbidity index score – – <0.001 – – <0.0011–2 vs. 0 1.77 1.15–2.74 0.01 1.43 0.92–2.23 0.13–4 vs. 0 3.33 2.07–5.37 <0.001 2.20 1.35–3.57 0.0025–6 vs. 0 4.57 2.38–8.78 <0.001 2.65 1.36–5.17 0.00471 vs. 0 8.84 3.61–21.64 <0.001 4.52 1.80–11.32 0.001
Cumulative number of prostate biopsy procedures – – 0.02 – – 0.032 vs. 1 0.49 0.28–0.87 0.015 0.55 0.31–0.96 0.023 or more vs. 1 0.45 0.17–1.23 0.1 0.22 0.05–0.89 0.2
Year of biopsy – – 0.11991 vs. 1989–90 1.36 0.62–3.01 0.41992 vs. 1989–90 1.38 0.68–2.82 0.41993 vs. 1989–90 0.90 0.44–1.87 0.81994 vs. 1989–90 0.90 0.43–1.86 0.81995 vs. 1989–90 0.50 0.21–1.21 0.1 – – –1996 vs. 1989–90 0.65 0.28–1.49 0.31997 vs. 1989–90 0.69 0.31–1.52 0.41998 vs. 1989–90 0.84 0.40–1.77 0.61999 vs. 1989–90 0.56 0.25–1.22 0.12000 vs. 1989–90 0.48 0.21–1.13 0.1
Region of residence – – 0.2Bas Saint Laurent vs. Montreal 1.08 0.48–2.43 0.8Saguenay – Lac Saint Jean vs. Montreal 1.33 0.59–2.99 0.5Quebec City vs. Montreal 1.32 0.76–2.29 0.3Mauricie – Center du Quebec vs. Montreal 0.85 0.43–1.66 0.6Estrie vs. Montreal 0.38 0.12–1.22 0.1Chaudiere – Appalache vs. Montreal 1.37 0.74–2.53 0.3 – – –Laval vs. Montreal 0.61 0.24–1.55 0.3Lanaudiere vs. Montreal 1.09 0.48–2.44 0.8Laurentides vs. Montreal 0.72 0.34–1.54 0.4Monteregie vs. Montreal 0.56 0.31–1.01 0.055Others vs. Montreal 0.59 0.26–1.31 0.2
OR, Odds ratio; CI, confidence interval.
650 GALLINA ET AL.

shock is roughly 50%.22 Therefore, prostate biopsy mortality rateis non-negligible. However, this most feared complication hasnever been reported in large scale studies. In consequence, thereare no validated risk factors for prediction of short-term mortalityafter prostatic biopsy. An explanation for the unavailability ofprostatic biopsy mortality data is related to lack of inclusion ofthis endpoint in the standard institutional urologic databases,where focus is placed on detection rates and on less severe compli-cations. Alternatively, severe septic complications may be treatedat different institution and patients may be lost from urologicalfollow-up, as most will not volunteer for another biopsy session.Therefore, administrative population-based databases represent avalid alternative for capturing these relatively rare events.
Our findings have several crucial clinical implications. PCa is aslowly progressive disease. Bill-Axelsson et al. demonstrated verylow disease specific mortality rates at 10 years, either in thewatchful waiting or in the radical prostatectomy arm, especially inpatients older than 65 years.23–25 Others suggested that treatmentbenefits are not negligible up to 75 years of age.26,27 This impliesdisease detection up to that age. Our data support a more conserv-ative approach to diagnostic prostate biopsy, as advanced age rep-resented the most informative predictor of prostate biopsy mortal-ity at 120 days. For example a 70 years old man, without anycomorbidities who is undergoing the first biopsy has a <1% riskof 120-day mortality. However, the risk increases to 5%, if an 85-year-old without comorbidities is subjected to his first biopsy.Interestingly, the number of biopsy session exerts a protectiveeffect on the recorded rate of mortality. This effect is highly likelyattributable to a selection of men among those exposed to morethan 1 biopsy session.
Taken together, our findings indicate that the 120-day mortalityrate is higher in men exposed to prostate biopsy than in controlsubjects. Our nomogram-based multivariable analysis demon-strates the specific effect of studied variables on the individualrisk of mortality after prostate biopsy. It suggests that the indica-tions for biopsy may warrant a reappraisal. For example, older andless healthy men should be carefully prescreened to weigh therisks and benefits of a biopsy. These men represent the category ofindividuals who benefit the least from the diagnosis of early local-
ized PCa.23,28 Moreover, a more restrictive approach to prostatebiopsy may reduce the cost related to this diagnostic procedure.Indirectly, a more restrictive approach to biopsy may result inlower detection rate of indolent PCa, especially in older individu-als. Conversely, a more restrictive approach will also result in astage shift at diagnosis, whereby some of the older and sicker indi-viduals will be diagnosed with more advanced stages of PCa.These men may require systemic therapies for more locallyadvanced disease, if they do not succumb to old age or comorbidconditions.
Our findings are not devoid of limitations. Lack of cause-spe-cific mortality data represents the foremost limitation. It may beargued that the overall health status of men in whom a biopsy wasperformed should not be so poor that they succumb to comorbidconditions within 120 days after biopsy. Individuals whose healthstatus is so poor would not be considered for biopsy by any urolo-gist. Therefore, it might be argued that the deaths that occurredwithin 120 days after biopsy were attributable to the prostate bi-opsy. Our control group at least partly validates this observation.However, we do not have cause-specific mortality to ensure thatthe deaths were not related to other causes, in exceptional cases.Unfortunately, a controlled trial of the effect of biopsy on mortal-ity cannot be considered, due to ethical issues. However, onlysuch design would definitively prove the causality effect. In its ab-sence our findings need to be considered as partial proof, or morespecifically as an association without causation. The nature of ourdatabase also prevented adjusting for antibiotic prophylaxis. Dif-ferences in antibiotic regimens may contribute to differences in120-day mortality rates. Moreover, the extent of the biopsy proce-dure also could not be included. However, more extensive biop-sies, such as 12 or more cores schemes, may contribute to smallabsolute but important relative differences in septic complicationrates. These differences may not be interpreted as significant inunderpowered small scale negative studies. Absence of indicationfor biopsy represents another limitation of the current study. Forexample, 20–30% of the patients underwent a biopsy despite beingover 75 years of age. It is conceivable that the indication for bi-opsy was to confirm clinically evident disease prior to initiation ofandrogen deprivation therapy. Such practice is no longer required,
FIGURE 2 – Nomogram predicting 120-day mortality after prostate biopsy (Panel 2a) and its calibration plot (Panel 2b). *Including theplanned biopsy; Nomogram instructions: To obtain nomogram predicted probability of 120-day mortality after prostate biopsy, locate patientvalues at each axis. Draw a vertical line to the ‘‘Point’’ axis to determine how many points are attributed for each variable value. Sum the pointsfor all variables. Locate the sum on the ‘‘Total Points’’ line to be able to assess the individual probability of 120-day mortality after biopsy onthe ‘‘Probability of mortality at 120 days’’ line. Calibration plot: This calibration plot shows the performance of the nomogram in an externalvalidation cohort. Specifically, nomogram predicted probabilities are compared to the observed proportions of 120-day mortality after biopsy.X-axis represents nomogram predicted probability of 120-day mortality after biopsy. Y-axis shows observed proportion of 120-day mortalityafter biopsy. Perfect prediction would correspond to a slope of 1 (diagonal 45� broken line). Solid line indicates nomogram performance in theexternal cohort.
651MORTALITY AFTER PROSTATE BIOPSY

especially when reversible LHRH agonist therapy is delivered.Our data also indicate that the median age at biopsy has decreasedover time (from 71 to 69 years). It might be postulated thatyounger age at biopsy contributed to the decreasing mortality rateover time (from 1.7 to 0.7%). This is particularly encouraginggiven that the absolute numbers of men subjected to biopsyincreased from less than a 1,000 to over 2,000 per year over time.Despite these limitations, our data provide the first population-based assessment of biopsy mortality and indicate that in some,relatively rare instances mortality might be attributable to the bi-opsy procedure. The novelty of our findings requires corroborationin other population-based registries and limits our report to a hy-pothesis generating manuscript
In conclusion, prostate biopsy is associated with higher mortal-ity than that observed in controls unexposed to biopsy. The risk ofdeath at 120-days after biopsy increases with age and Charlsoncomorbidity index. Conversely, increasing number of previous bi-opsy sessions exerts a protective effect. Moreover, the causality ofthis association has not been proven.
Acknowledgements
Dr. Pierre I. Karakiewicz is partially supported by the Univer-sity of Montreal Urology Associates, Fonds de la Recherche enSant�e du Qu�ebec, the University of Montreal Department ofSurgery and the University of Montreal Foundation.
References
1. Jemal A, Siegel R, Ward E, Murray T, Xu J, Thun MJ. Cancer statis-tics, 2007. CA: Cancer J Clin 2007;57:43–66.
2. Smith RA, Cokkinides V, Eyre HJ American Cancer Society guide-lines for the early detection of cancer, 2006. CA: Cancer J Clin 2006;56:11–25 (quiz 49–50).
3. Walz J, Graefen M, Chun FK, Erbersdobler A, Haese A, Steuber T,Schlomm T, Huland H, Karakiewicz PI. High incidence of prostatecancer detected by saturation biopsy after previous negative biopsyseries. Eur Urol 2006;50:498–505.
4. Thompson IM, Pauler DK, Goodman PJ, Tangen CM, Lucia MS,Parnes HL, Minasian LM, Ford LG, Lippman SM, Crawford ED,Crowley JJ, Coltman CA, Jr. Prevalence of prostate cancer amongmen with a prostate-specific antigen level < or 54.0 ng per milliliter.N Engl J Med 2004;350:2239–46.
5. Thompson IM, Ankerst DP, Chi C, Lucia MS, Goodman PJ, CrowleyJJ, Parnes HL, Coltman CA, Jr. Operating characteristics of prostate-specific antigen in men with an initial PSA level of 3.0 ng/ml orlower. JAMA 2005;294:66–70.
6. Nadler RB, Loeb S, Roehl KA, Antenor JA, Eggener S, Catalona WJ.Use of 2.6 ng/ml prostate specific antigen prompt for biopsy in menolder than 60 years. J Urol 2005;174:2154–7 (discussion 7).
7. Elabbady AA, Khedr MM. Extended 12-core prostate biopsyincreases both the detection of prostate cancer and the accuracy ofGleason score. J Urol 2006;49:49–53 (discussion).
8. Punglia RS, D’Amico AV, Catalona WJ, Roehl KA, Kuntz KM.Effect of verification bias on screening for prostate cancer by mea-surement of prostate-specific antigen. N Engl J Med 2003;349:335–42.
9. Saad A, Hanbury DC, McNicholas TA, Boustead GB. Acute peripro-static haematoma following a transrectal ultrasound-guided needle bi-opsy of the prostate. Prostate Cancer Prostatic Dis 2002;5:63–4.
10. Seymour MA, Oesterling JE. Anterior rectal wall hematoma: compli-cation of transrectal ultrasound-guided biopsy of prostate. Urology1992;39:177–81.
11. Teichman JM, Tsang T, McCarthy MP. Osteitis pubis as a complica-tion of transrectal needle biopsy of the prostate. J Urol 1992;148:1260–1.
12. Borer A, Gilad J, Sikuler E, Riesenberg K, Schlaeffer F, Buskila D.Fatal Clostridium sordellii ischio-rectal abscess with septicaemiacomplicating ultrasound-guided transrectal prostate biopsy. J Infect1999;38:128–9.
13. Sohlberg OE, Chetner M, Ploch N, Brawer MK. Prostatic abscess af-ter transrectal ultrasound guided biopsy. J Urol 1991;146:420–2.
14. Fradet V, McCormack M, Perrotte P, Karakiewicz P, Saad F. An epi-dural abscess following transrectal ultrasound-guided biopsies of theprostate. Can J Urol 2005;12:2899–900.
15. Basaran G. Endocarditis prophylaxis for transrectal prostatic biopsy.JAMA 1998;280:1908.
16. Irani J, Roblot F, Becq Giraudon B, Dore B. Acute bacterial endocar-ditis secondary to transrectal ultrasound-guided prostatic biopsy.Scand J Urol Nephrol 2002;36:156–7.
17. Davidson AJ, Webb DR, Lawrentschuk N, Jennens ID, Sutherland M.Multi-resistant Escherichia coli sepsis following transrectal ultra-sound-guided prostate biopsy. Br J Hosp Med (Lond) 2006;67:98–9.
18. Binsaleh S, Al-Assiri M, Aronson S, Steinberg A. Septic shock aftertransrectal ultrasound guided prostate biopsy. Is ciprofloxacin prophy-laxis always protecting? Can J Urol 2004;11:2352–3.
19. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method ofclassifying prognostic comorbidity in longitudinal studies: develop-ment and validation. J Chronic Dis 1987;40:373–83.
20. D’Hoore W, Sicotte C, Tilquin C. Risk adjustment in outcome assess-ment: the Charlson comorbidity index. Methods Inf Med 1993;32:382–7.
21. Hens N, Aerts M, Molenberghs G. Model selection for incompleteand design-based samples. Stat Med 2006;25:2502–20.
22. Wheeler AP, Bernard GR. Treating patients with severe sepsis. TheNew N Engl J Med 1999;340:207–14.
23. Bill-Axelson A, Holmberg L, Ruutu M, Haggman M, Andersson SO,Bratell S, Spangberg A, Busch C, Nordling S, Garmo H, Palmgren J,Adami HO, et al. Radical prostatectomy versus watchful waiting inearly prostate cancer. N Engl J Med 2005;352:1977–84.
24. Stuart ME, Strite SA. Radical prostatectomy versus watchful waiting.N Engl J Med 2005;353:1298–300 (author reply-300).
25. Marantz PR, Hall CB, Derby CA. Radical prostatectomy versuswatchful waiting. N Engl J Med 2005;353:1298–300 (author reply-300).
26. Alibhai SM, Naglie G, Nam R, Trachtenberg J, Krahn MD. Do oldermen benefit from curative therapy of localized prostate cancer? J ClinOncol 2003;21:3318–27.
27. Schwartz KL, Alibhai SM, Tomlinson G, Naglie G, Krahn MD. Con-tinued undertreatment of older men with localized prostate cancer.Urology 2003;62:860–5.
28. Albertsen PC, Hanley JA, Fine J. 20-year outcomes following con-servative management of clinically localized prostate cancer. JAMA2005;293:2095–101.
652 GALLINA ET AL.