Molecular and Cellular Endocrinology · called mitochondrial endocrinology (Wrutniak-Cabello et...
Transcript of Molecular and Cellular Endocrinology · called mitochondrial endocrinology (Wrutniak-Cabello et...

Editorial
Mitochondrial endocrinology – Mitochondria as key to hormones and metabolism
Mitochondria are puzzling organelles, which provided excitinginsights into cellular function as recently reviewed by one of its pio-neers (Schatz, 2013). But still many of their features in (patho)phys-iologic conditions and in disease states are not fully understood.Despite their critical role for all animal organisms, their impact onseveral endocrine and metabolic functions is of specific importance.Not do they only host several metabolic pathways, including the tri-carboxylic (Krebs) cycle and b-oxidation, mitochondria are also thekey to lipid, cholesterol and hormone biosynthesis as well as main-tain the cytosolic free calcium concentration. Free cytosolic calciumin turn serves as cellular signal in divergent pathways, such as hor-monal signaling (Stark and Roden, 2007). On the other hand, certainhormones exert their central endocrine action directly or indirectlyvia affecting mitochondrial function in various tissues and diver-gent cell-types.
The growing interest of current research in this field stimulatedus to compile contributions to hot topics addressing aspects of so-called mitochondrial endocrinology (Wrutniak-Cabello et al.,2002). First, studies of humans with genetically confirmed mito-chondrial abnormalities, commonly called mitochondrial diseases,can serve as nature’s proof of the importance of mitochondria alsofor endocrine function, which is not limited to the pancreatic ß cellby causing mitochondrial diabetes. These inborn diseases mighttherefore help to better understand abnormal mitochondrial func-tion in humans. Reviewing hormone synthesis, with a focus on ste-roid hormones and vitamin D, and hormone action, particularlydescribing the role of thyroid hormones for mitochondrial biogene-sis, is followed by a summary on the complex role of mitochondriafor sex hormone synthesis but also steroid-independent effects onmammalian reproduction. Second, seminal studies in the field ofmetabolism stimulated mitochondrial endocrinology over the lastdecade by shedding more light on regulation of energy homeostasisor precisely the balance between energy intake and expenditure foralterations associated with ageing, obesity and diabetes mellitus. Arelevant proportion of these new insights resulted from the devel-opment of novel invasive and noninvasive technologies allowingassessing various aspects of mitochondria, also in humans (Szendr-oedi et al., 2011). The findings range from age-dependent altera-tions over dynamic changes in mitochondrial function in skeletalmuscle and liver to the chameleon-like behavior of adipose tissueto adapt heat production and subtle regulation of ß-cell function.
While the present selection cannot be comprehensive, it wasdesigned to briefly summarize hot topics in mitochondrial endocri-nology as of 2013. I would like to thank all the contributors fortheir excellent cooperation, the team of Mol Cell Endocrinol fortheir support and my Assistant Mrs. Beate Stodieck for her helpwith this task.
References
Schatz, G., 2013. Getting mitochondria to center stage. Biochem. Biophys. Res.Commun. 434, 407–410.
Stark, R., Roden, M., 2007. ESCI Award 2006. Mitochondrial function and endocrinediseases. Eur. J. Clin. Invest. 37, 236–248.
Wrutniak-Cabello, C., Casas, F., Grandemange, S., Seyer, P., Busson, M., Carazo, A.,Cabello, G., 2002. Study of thyroid hormone action on mitochondria opens up anew field of research: mitochondrial endocrinology. Curr. Opin. Endocrinol.Diab. 9, 387–392.
Szendroedi, J., Phielix, E., Roden, M., 2011. The role of mitochondria in insulinresistance and type 2 diabetes mellitus. Nat. Rev. Endocrinol. 8, 92–103.
Michael RodenInstitute for Clinical Diabetology,
German Diabetes Center,Leibniz Center for Diabetes Research, Düsseldorf, Germany
Unic. Clinics of Endocrinology and Diabetology,Heinrich-Heine University, Düsseldorf, Germany
E-mail address: [email protected]
Available online 20 June 2013
0303-7207/$ - see front matter ! 2013 Elsevier Ireland Ltd. All rights reserved.http://dx.doi.org/10.1016/j.mce.2013.06.017
Molecular and Cellular Endocrinology 379 (2013) 1–1
Contents lists available at SciVerse ScienceDirect
Molecular and Cellular Endocrinology
journal homepage: www.elsevier .com/locate /mce

Review
Endocrine disorders in mitochondrial disease q
Andrew M. Schaefer a,⇑, Mark Walker b, Douglass M. Turnbull a, Robert W. Taylor a,⇑a Wellcome Trust Centre for Mitochondrial Research, Institute for Ageing and Health, Newcastle University, Newcastle upon Tyne, UKb Institute of Cellular Medicine, Newcastle University, Newcastle upon Tyne, UK
a r t i c l e i n f o
Article history:Available online 13 June 2013
Keywords:Mitochondrial diseaseEndocrinemtDNADiabetesm.3243A > G
a b s t r a c t
Endocrine dysfunction in mitochondrial disease is commonplace, but predominantly restricted to diseaseof the endocrine pancreas resulting in diabetes mellitus. Other endocrine manifestations occur, but arerelatively rare by comparison. In mitochondrial disease, neuromuscular symptoms often dominate theclinical phenotype, but it is of paramount importance to appreciate the multi-system nature of the dis-ease, of which endocrine dysfunction may be a part. The numerous phenotypes attributable to pathogenicmutations in both the mitochondrial (mtDNA) and nuclear DNA creates a complex and heterogeneouscatalogue of disease which can be difficult to navigate for novices and experts alike. In this article we pro-vide an overview of the endocrine disorders associated with mitochondrial disease, the way in which theunderlying mitochondrial disorder influences the clinical presentation, and how these factors influencesubsequent management.
! 2013 The Authors. Published by Elsevier Ireland Ltd. All rights reserved.
Contents
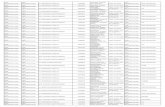
1. Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 32. Mitochondrial biochemistry and genetics. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 33. Investigation of mitochondrial disease . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 34. Diabetes mellitus . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 45. Mitochondrial diabetes . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4
5.1. Pattern recognition . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 45.2. Age-at-onset . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 55.3. Insulin requirements . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 55.4. Body Mass Index (BMI) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 55.5. End organ disease . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 55.6. Pancreatic pathology . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 65.7. Diabetes management. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6
6. Hypoparathyroidism . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 67. Hypothalamo-pituitary axis. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 78. Growth hormone deficiency . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 79. Hypogonadism . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7
10. Hypothyroidism . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 711. Hypoadrenalism . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 712. SIADH . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 713. Adipose tissue as an endocrine organ. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 714. Autoimmune endocrinopathy . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 815. Conclusion . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8
Acknowledgments . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8References . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8
0303-7207/$ - see front matter ! 2013 The Authors. Published by Elsevier Ireland Ltd. All rights reserved.http://dx.doi.org/10.1016/j.mce.2013.06.004
q This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial-No Derivative Works License, which permits non-commercial use, distribution, and reproduction in any medium, provided the original author and source are credited.⇑ Corresponding authors. Address: Wellcome Trust Centre for Mitochondrial Research, Institute for Ageing and Health, The Medical School, Newcastle University,
Framlington Place, Newcastle upon Tyne NE2 4HH, UK. Tel.: +44 1912223685.E-mail addresses: [email protected] (A.M. Schaefer), [email protected] (R.W. Taylor).
Molecular and Cellular Endocrinology 379 (2013) 2–11
Contents lists available at ScienceDirect
Molecular and Cellular Endocrinology
journal homepage: www.elsevier .com/locate /mce

1. Introduction
The term mitochondrial disease refers to a heterogeneous groupof multi-system disorders characterised by mitochondrial respira-tory chain deficiency in which neurological involvement is oftenprominent (McFarland et al., 2010; Ylikallio and Suomalainen,2012). Numerous distinct genotypes give rise to varied and over-lapping phenotypes. Endocrine dysfunction is a frequent feature,predominantly due to the prevalence of diabetes mellitus associ-ated with the m.3243A > G mutation, the most common hetero-plasmic mtDNA mutation associated with human disease(Schaefer et al., 2008). Other forms of endocrine disease are de-scribed less frequently, occurring in numerous mitochondrial dis-orders due to either mutations within mtDNA or associated withnuclear-driven disorders of mtDNA maintenance. For many muta-tions, reports of endocrine disease are so rare as to challenge thehypothesis that they are mediated by defects of oxidative phos-phorylation at all, and merely represent the background preva-lence of endocrine disease in a well studied population. There isa danger that associations based on single case reports (sometimesdating back 20 years and beyond) are repeatedly cited in reviewssuch as this, perpetuating an unproven connection with mitochon-drial disease. Analysis of large patient cohorts are likely to be key,and while this dilemma may not be readily resolved for rare muta-tions, it should be feasible to answer the question in more preva-lent disorders. As ever, further studies are needed in this area.
This review summarises the range of endocrine involvement inmitochondrial disease and the genotypes and phenotypes in whichthese occur. We offer insights from a specialist mitochondrial clinicas to the use of pattern recognition and pedigree analysis in thediagnosis and subsequent management of these complex patientsand their families.
2. Mitochondrial biochemistry and genetics
Mitochondria are essential organelles, present in all nucleatedmammalian cells, whose main role is to produce ATP by the pro-cess of oxidative phosphorylation (OXPHOS). The OXPHOS machin-ery is made up of !90 different polypeptides, organised into fivetransmembrane complexes. The oxidation of foodstuffs generateselectrons which are shuttled to oxygen along the first four respira-tory chain complexes whilst protons are pumped across the innermitochondrial membrane from the matrix to the intermembranespace forming an electrochemical gradient which is harnessed byATP synthase, to phosphorylate ADP to form ATP. Mitochondrialfunction and biosynthesis is under the dual genetic control of boththe mitochondrial genome – encoding just 13 proteins and 37 geneproducts in total and the nuclear genome, which encodes for some1400–1500 mitochondrial proteins. Whilst mutations within eitherDNA molecule can cause a respiratory chain defect, the unique ge-netic rules which govern the behaviour of the mitochondrial gen-ome provide some insight into the phenotypic heterogeneitywhich particularly characterise mtDNA disorders.
Several recent reviews have detailed the importance of mtDNAmutations in human disease (Greaves et al., 2012; Schon et al.,2012). The mitochondrial genome is a highly-organised, 16.6 kbcircular genome whose complete sequence was published over30 years ago (Anderson et al., 1981), prompting the discovery ofthe first pathogenic mutations in 1988 involving either mtDNArearrangements or deletions (Holt et al., 1988) or point mutations(Wallace et al., 1988). Strictly inherited through the maternal line-age, it is present within cells in multiple copies, reflecting the de-mand for OXPHOS-derived energy of that particular tissue. Whenall mtDNA molecules within a cell are identical, a situation knownas homoplasmy prevails. The presence of two or more
mitochondrial genotypes, as typified in many pathogenic mtDNAmutations, results in a situation known as heteroplasmy in whichthe ratio of wild-type to mutated mtDNA determines the onset ofclinical symptoms. A minimum critical proportion of mutatedmtDNA molecules are required before biochemical deficiency man-ifests as a clinical phenotype, with this threshold level varying fordifferent mutations and tissues. Functional consequences are mostcommonly seen in post-mitotic tissues with high energy require-ments (e.g. muscle, brain, and heart) but almost any tissue canbe involved, including the endocrine organs. Individual mtDNAmutations often dictate the pattern of involvement, with somemore strongly associated with endocrine disease than others.
The exact prevalence of mtDNA disease has proven difficult todefine but estimates from our cohort in the North East of Englandsuggest that mtDNA mutations of all types cause a point preva-lence of disease in adults of 9.2/100,000 population, with a further16.5/100,000 at risk of developing disease due to carrier status atany one time (Schaefer et al., 2008). Birth prevalence studies havereported mutation frequencies of 0.14% for some common mtDNAmutations such as the m.3243A > G mutation (Elliott et al., 2008),although most individuals will not manifest clinical disease asthe majority of mutations are present at subthreshold levels.
Several other factors are important in understanding the behav-iour of pathogenic, heteroplasmic mtDNA mutations in relation toclinical disease. During mitotic cell division, mitochondria are ran-domly segregated to daughter cells and as such the proportion ofmutated mtDNA can shift in the presence of heteroplasmy. Theobservation of a rapid segregation in mammalian heteroplasmicmtDNA genotypes between generations is evidence for the exis-tence of a mtDNA developmental genetic bottleneck; this involvesa marked reduction in mtDNA copy number in the germline fol-lowed by the replication of a subgroup of mtDNA molecules duringoogenesis although the precise mechanism remains to be fullydetermined (Cao et al., 2007; Cree et al., 2008; Wai et al., 2008).
In addition to primary mtDNA mutations, mutations in nucleargenes involved in mtDNA replication or repair (often termedmtDNA maintenance) can give rise to secondary qualitative orquantitative mtDNA abnormalities. Mutations in nuclear genesimplicated in many other mitochondrial processes including struc-tural respiratory chain components, mitochondrial nucleotide sal-vage and synthesis and mitochondrial translation are increasinglybeing described with the advent of next-generation screeningand mito-exome sequencing (Ylikallio and Suomalainen, 2012;Calvo et al., 2012) highlighting that mitochondrial disease maybe inherited as Mendelian traits, with autosomal dominant (ad-),autosomal recessive (ar-), and even X-linked forms.
3. Investigation of mitochondrial disease
The complex interplay between mtDNA heteroplasmy and phe-notypic expression, and the potential contribution from both nu-clear and mitochondrial genomes, makes mitochondrial diseaseone of the most difficult inherited disorders to diagnose. The lackof curative treatments for these conditions places greater emphasison accurate genetic advice and counselling, which should beundertaken by a specialist with experience in this area.
Our own algorithms for the laboratory investigation of mito-chondrial disease have been published extensively (Taylor et al.,2004; Tuppen et al., 2010; McFarland et al., 2010) and rely oninformation from the clinical phenotype and functional data (his-tochemistry and biochemistry) to guide genetic studies of bothmtDNA and nuclear genes. Some common mtDNA mutations canbe reliably detected and screened in blood, but there is a potentialfor false-negative results in some mutations. This possibilityshould be highlighted in the case of the m.3243A > G mutation,
A.M. Schaefer et al. / Molecular and Cellular Endocrinology 379 (2013) 2–11 3

particularly as it is the most frequently requested analysis for pre-sumed mitochondrial disease and is associated with numerous clin-ical syndromes including mitochondrial encephalomyopathy, lacticacidosis and stroke-like episodes (MELAS), maternally-inheriteddiabetes and deafness (MIDD), and, less commonly, myoclonic epi-lepsy with ragged red fibres (MERRF). Levels of this mutation withinleucocytes have been shown to decrease by!1.4% per year (Rahmanet al., 2001) and we have several patients within our own cohort inwhom the m.3243A > G mutation would not have been detectedfrom blood alone. The risk of false negative results may be decreasedby screening alternative mtDNA sources including urinary epithelialcells (McDonnell et al., 2004; Blackwood et al., 2010). For somemutations, notably m.3243A > G, the level in this tissue correlateswell with clinical severity (Whittaker et al., 2009). Muscle biopsy re-mains the gold standard, yet in a minority of patients a complete bio-chemical analysis of muscle tissue can be normal, whilst thedemonstration of histological and histochemical hallmarks of mito-chondrial disease still require additional genetic testing. A prag-matic strategy for genetic testing is often best derived from liaisonwith a specialist mitochondrial centre. Pattern recognition is keyand specific phenotypes may raise an otherwise rare mutation tothe forefront of the process (e.g. Alper syndrome due to reces-sively-inherited POLG gene mutations). Pathogenic mtDNA muta-tions and mtDNA rearrangements are now relatively easy toexclude where a muscle biopsy has already been performed, andin many cases should be screened in both adults and children priorto nuclear genetic testing, a process which may require investigatingnumerous candidate genes. This once laborious process is being rev-olutionised by the next-generation sequencing revolution leading tothe identification of many new mitochondrial disease genes over thelast 2–3 years.
4. Diabetes mellitus
Diabetes mellitus is well recognised within mitochondrial phe-notypes and is the most common endocrine manifestation of dis-ease. This is mainly because of its association with the MIDDphenotype which is common in patients carrying them.3243A > G MTTL1 mutation (van den Ouweland et al., 1992;Whittaker et al., 2007). Diabetes is also a common condition inits own right, estimated to affect 4.45% of the UK population. It isnot surprising, therefore, that it is common for mitochondrial dia-betes to be misdiagnosed, even in the presence of other featuresthat may provide clues as to the underlying genetic disease. Theimportance of pattern recognition in diagnosis is discussed subse-quently, but for the m.3243A > G mutation, the cardinal featuresare of maternal inheritance and pre-senile sensorineural hearingloss. Prevalence of the m.3243A > G mutation in unselected dia-betic populations varies between 0% and 2.8% from the larger stud-ies (Vionnet et al., 1993; Katagiri et al., 1994; Otabe et al., 1994;t’Hart et al., 1994; Kishimoto et al., 1995; Odawara et al., 1995;Uchigata et al., 1996; Abad et al., 1997; Saker et al., 1997; Tsukudaet al., 1997; Holmes-Walker et al., 1998; Lehto et al., 1999; Matsu-ura et al., 1999; Malecki et al., 2001; Ohkubo et al., 2001; Suzukiet al., 2003; Maassen et al., 2004; Murphy et al., 2008). Deafness,neuromuscular disease, end stage renal disease, and a maternalfamily history all increase the likelihood of mitochondrial disease(t’Hart et al., 1994; Majamaa et al., 1997; Newkirk et al., 1997;Smith et al., 1999; Ng et al, 2000; Iwasaki et al., 2001; Klemmet al., 2001; Suzuki et al., 2003; Murphy et al., 2008). There are sev-eral other mtDNA mutations recognised to consistently express aphenotype which includes diabetes. These include them.14709T > C mutation (Hanna et al., 1995; Vialettes et al., 1997;Choo-Kang et al., 2002) which has been reported to be homoplas-mic in some patients (McFarland et al., 2004) and may cause up to13% of mitochondrial diabetes in the North East of England (Whit-
taker et al., 2007). The m.8296A > G MTTK gene mutation was iden-tified in 0.9% unrelated Japanese patients with diabetes, and 2.3%with diabetes and deafness (Kameoka et al., 1998). Them.14577T > C MTND6 mutation, associated with isolated complexI deficiency, was found in 0.79% unrelated Japanese patients withdiabetes (Tawata et al., 2000).
Other mtDNA point mutations have been described but appearmuch rarer. The m.12258T > C MTTS2 gene mutation has beenassociated with diabetes (Lynn et al., 1998) but in other mater-nally-related kindreds, diabetes has been notably absent (Man-sergh et al., 1999). The m.3271T > C MTTL1 mutation has beenassociated with the MIDD, MELAS and MERRF phenotypes (Gotoet al., 1991; Suzuki et al., 1996; Tsukuda et al., 1997), whilst them.3264T > C MTTL1 mutation was observed with MIDD, the pro-band having chronic progressive external ophthalmoplegia (CPEO)and cervical lipomata in addition (Suzuki et al., 1997).
In a number of mtDNA mutations, diabetes is not consideredpart of the established phenotype, despite rare reports. This groupincludes the m.8344A > G mutation causing myoclonic epilepsyand ragged-red fibres (MERRF) (Austin et al., 1998; Whittakeret al., 2007), the m.8993T > C mutation which is associated withthe maternally-inherited Leigh syndrome (MILS) phenotype (Naga-shima et al., 1999) and mtDNA mutations causing Leber hereditaryoptic atrophy (LHON) (Newman et al., 1991; Du Bois and Feldon,1992; Pilz et al., 1994; Cole and Dutton, 2000).
Single, large-scale mtDNA deletions have been reported tocause diabetes in 11% (6 of 55 patients) of well-defined, clinical co-horts of patients with CPEO and Kearns Sayre Syndrome (KSS)(Whittaker et al., 2007). An earlier paper reviewing existing casereports of KSS reported the prevalence of diabetes to be 13% (29of 226) but not all cases had genetic confirmation of a deletedmitochondrial genome (Harvey and Barnett, 1992). A single reportdocuments a child who presented with insulin dependent diabetesmellitus (IDDM) and adrenal insufficiency prior to the develop-ment of ophthalmoplegia and a diagnosis of KSS (Mohri et al.,1998). Rarely, mtDNA deletions have been reported to cause IDDMin Pearson’s Syndrome, but on the whole pancreatic failure is usu-ally exocrine (Superti-Furga et al., 1993; Williams et al., 2012).Other mtDNA rearrangements, notably maternally-transmittedduplications of the mitochondrial genome, have been reported inassociation with diabetes (Rötig et al., 1992; Ballinger et al., 1994).
The recognised spectrum of disease due to mutations withinnuclear maintenance genes is still expanding, but diabetes hasbeen reported in 11% of adult CPEO phenotypes with ar-POLGmutations (Horvath et al., 2006). In adult-onset PEO due to RRM2Bmutations, only 4.5% (1 of 22 in this cohort) had diabetes (Pit-ceathly et al., 2012). Late-onset type-2 diabetes is rare (3 of 83)in OPA1 pedigrees (Yu-Wai-Man et al., 2010) and is not a featureof ar-PEO1 (Twinkle) gene mutations (Lönnqvist et al., 2009).
There are other documented mutations associated with diabetes,most of which are sufficiently rare as an individual entity as to notwarrant lengthy discussion in this review. The role of the 16,189 var-iant in causing diabetes remains unclear (Poulton et al., 2002; Daset al., 2007) but the numerous reports of pathogenic mtDNA muta-tions associated with a diabetic phenotype does highlight that theendocrine pancreas is particularly susceptible to mitochondrial dys-function. Combined with involvement of other tissues this is a usefulpointer towards mitochondrial disease as a diagnosis.
5. Mitochondrial diabetes
5.1. Pattern recognition
Faced with the fact that mitochondrial diabetes is relativelyscarce in the general diabetes clinic, it is helpful to have a
4 A.M. Schaefer et al. / Molecular and Cellular Endocrinology 379 (2013) 2–11

structured approach to help decide which patients should be con-sidered for mtDNA mutation screening.
The text book description of the short, deaf patient with diabe-tes is in reality a rare occurrence and probably represents the tip ofthe iceberg in terms of mitochondrial diabetes. Historically thesedescriptions referred to patients with severe disease due to eitherm.3243A > G or KSS. These ‘textbook’ patients are usually youngerand with low Body Mass Index (BMI) as well as height. This prob-ably reflects more extensive multisystem involvement with higherlevels of heteroplasmy in most tissues, and rarely will the diabeticclinic be the first medical encounter for these patients. The same istrue of recessive forms of mitochondrial disease, where clear mul-tisystem disease is likely to have raised the question of mitochon-drial disease already.
There are differences between mitochondrial diabetes and type-2 diabetes, and these will be discussed in the subsequent para-graphs. Within the real world however, of busy clinics filled withcommon disorders, a physician who diagnoses mitochondrial dia-betes without additional clues should consider themselves partic-ularly astute. A maternal family history or sensorineural deafnessshould raise suspicion. While deafness in old age or a family his-tory of type-2 diabetes is not uncommon, pre-senile sensorineuraldeafness is unusual, and especially so if combined with diabetesand a maternal history of either disorder, and/or other conditionssuch as cardiomyopathy, epilepsy, ptosis or unusual soundingstrokes. Each additional feature adds weight to the growing suspi-cion of a mitochondrial disorder. Asymptomatic individuals andapparently ‘skipped’ generations within a pedigree should not les-sen the suspicion as this is a common observation in mtDNA muta-tions due to carriers with low levels of heteroplasmy. In ourmitochondrial cohort in the North East of England, 82/138 (59%)individuals within m.3243A > G pedigrees showed no signs of dis-ease at the time of assessment, despite being at risk by virtue ofmaternal inheritance patterns; 82% of relatives opting for predic-tive testing subsequently test positive (Schaefer et al., 2008). Thisfrequency remains constant whether testing 1st, 2nd or 3rd degreerelatives. 30% of these patients go on to develop typical featuresassociated with the m.3243A > G mutation over the next 5 years(Schaefer et al., 2008) and this figure continues to rise with subse-quent follow up (Schaefer and colleagues, unpublished data).
There is conflicting evidence regarding the predictive value of amaternal family history alone (Ng et al., 2000; Choo-Kang et al.,2002). As pure diabetic phenotypes are extremely rare in mtDNAdisease, it is probably true that a family history of diabetes aloneis unlikely to suggest mitochondrial disease (Choo-Kang et al.,2002). The detail of the pedigree analysis is all important, however,as often enquiry is restricted to the scope of the clinic being at-tended, whether diabetic or neurological; and important associa-tions may be easily overlooked. Most mitochondrial patients inthe diabetic clinic will have a more subtle presentation, but deaf-ness is usually present when diabetes is diagnosed (Suzuki et al.,1994; Guillausseau et al., 2001; Uimonen et al., 2001). An audio-gram can confirm its presence if it has not been formally assessed.A variable number of additional features (such as ptosis, proximalmyopathy, cerebellar ataxia, axonal sensorimotor neuropathy, gas-trointestinal dysmotility and pigmentary retinopathy) are com-monly present, but are often subtle and may be missed if notlooked for specifically. Regular ophthalmologic assessments in dia-betic patients afford an opportunity to identify pigmentary retin-opathies, but the pick-up rate is increased if the ophthalmologistis aware of the clinical suspicion.
5.2. Age-at-onset
Mitochondrial diabetes usually presents insidiously, much liketype-2 diabetes. When due to the m.3243A > G mutation it can
present at virtually any age, but typically develops in mid-life withan average age-at-onset of 37 or 38 years (Guillausseau et al.,2004; Whittaker et al., 2007). Only rarely does the diabetes presentin childhood (Guillausseau et al., 2004).
5.3. Insulin requirements
Mitochondrial diabetes is felt to occur as a result of insulin defi-ciency (Reardon et al., 1992; Oka et al., 1993; Kadowaki et al.,1993; Kadowaki et al., 1994; Katagiri et al., 1994; Walker et al.,1995a) rather than insulin resistance (Walker et al., 1995b; Velhoet al., 1996), but in some patients both mechanisms may play apart (Szendroedi et al., 2009). Approximately 20% of cases of mito-chondrial diabetes may present acutely, with 8% suffering fromketoacidosis (Guillausseau et al., 2001; Guillausseau et al., 2004;Maassen et al., 2004), but only 13% of diabetic patients carryingthe m.3243A > G mutation require insulin at diagnosis (Whittakeret al., 2007). Of the remaining 87% of patients, mitochondrial dia-betes develops insidiously but usually progresses rapidly to insulinrequirement, another observation unusual in type-2 diabetes;45.2% of such patients made this transition (Whittaker et al.,2007). Average transition rates to insulin requirement range be-tween 2 and 4.2 years (Guillausseau et al., 2001; Guillausseauet al., 2004; Maassen et al., 2004; Whittaker et al., 2007). Those pa-tients assessed by Whittaker and colleagues were under stringentreview in a specialist mitochondrial clinic, and early diagnosis ofdiabetes through screening programmes may explain the longertransition times as compared to other studies.
5.4. Body Mass Index (BMI)
One of the clues that appears consistent in mitochondrial diabe-tes is the tendency for patients to have a lower than average BMI(Guillausseau et al., 2004; Whittaker et al., 2007), an unusualobservation in typical type-2 diabetes. Lower BMI tends to corre-late with earlier onset of diabetes, earlier insulin requirements,and higher HbA1C measurements (Guillausseau et al., 2004). Thisprobably reflects a higher overall disease burden as lower BMItends to be associated with an earlier onset of disease and a moresevere phenotype in general (Schaefer and colleagues, unpublisheddata).
5.5. End organ disease
Although neuropathy and renal disease can occur indepen-dently of diabetes in the m.3243A > G mutation, each complicationhas been reported to be significantly more prevalent in those pa-tients with diabetes. In addition, patients with diabetic retinopathyor renal impairment demonstrated higher HbA1C levels than thosewho did not (Whittaker et al., 2007). This suggests that poor gly-caemic control plays a major role in their pathogenesis. The riskof neuropathy and renal disease in the same diabeticm.3243A > G cohort was reported to be higher than in other formsof either type-1 or type-2 diabetes, which implies that pre-existentmitochondrial dysfunction within these end organs predisposes tothe microvascular complications of diabetes (Whittaker et al.,2007). Prevalence rates for these complications exceed those re-ported in the United Kingdom Prospective Diabetes Study intype-2 diabetes or the DCCT in type-1 diabetes (The Diabetes Con-trol and Complications Trial Research Group, 1993; Adler et al.,2003). Interestingly, several studies have reported lower rates ofdiabetic retinopathy in MIDD (Holmes-Walker et al., 1998; Massinet al., 1999; Smith et al., 1999; Latvala et al., 2002) than would nor-mally be expected in type-1 or type-2 diabetes (Misra et al., 2009;Thomas et al., 2012). The same appears true of cataracts. This hasbeen proposed to be due to reduced glucose metabolism by the
A.M. Schaefer et al. / Molecular and Cellular Endocrinology 379 (2013) 2–11 5

polyol pathway (Holmes-Walker et al., 1998). Abnormal glucosetolerance also appears to increase the clinical expression of the pig-mentary retinopathy typically seen in patients with them.3243A > G mutation. 15 of 23 patients from MIDD kindredshad evidence of a pigmentary retinopathy, 13 of which had evi-dence of glucose intolerance (Holmes-Walker et al., 1998).
m.3243A > G heteroplasmy levels from muscle-derived mtDNAdid not correlate with the age of onset of diabetes, whilst hetero-plasmy levels from blood or muscle did not correlate with the timetaken to progress to insulin requirement, or the risk of diabeticcomplications; an inverse correlation between age of diabetic on-set and heteroplasmy level in blood derived mtDNA was reported(Whittaker et al., 2007), but the true significance of this was diffi-cult to predict as heteroplasmy levels in blood are known to de-crease year by year in patients carrying the m.3243A > Gmutation due to replicative disadvantage (Rahman et al., 2001). Asubsequent multicentre study found that correcting for age ne-gated the significance of a similar finding in their cohort, but didnote a correlation between age-adjusted blood heteroplasmy levelsand both HbA1C, levels and low BMI (Laloi-Michelin et al., 2009).
5.6. Pancreatic pathology
Mitochondrial dysfunction within the metabolically active pan-creatic B-cells is presumed to account for reduced function andultimately loss of B-cell mass (Kobayashi et al., 1997; Lynn et al.,2003). It has been difficult to demonstrate apoptosis (Kobayashiet al., 1997) which is the presumed explanation for the surprisinglylow levels of heteroplasmy found in remaining B-cell tissue at au-topsy (Togashi et al., 2000; Lynn et al., 2003). HLA polymorphismsassociated with type-1 susceptibility have not been found in mito-chondrial diabetes (van Essen et al., 2000). Our own m.3243A > Gcohort do not, in general, carry islet cell or GAD antibodies (unpub-lished data) but these have been found in a minority of patients byother groups (Oka et al., 1993; Murphy et al., 2008). These casesmay represent coincidental autoimmune type-1 diabetes but ithas also been hypothesised that antibodies might be produced indirect response to pancreatic B-cell destruction as a result of mito-chondrial mechanisms (Oka et al., 1993). Acute or chronic pancre-atitis is rarely described (Kishnani et al., 1996; Schleiffer et al.,2000; Verny et al., 2008; Ishiyama et al., 2012).
5.7. Diabetes management
The majority of patients present with non-insulin dependentdiabetes. A sulphonylurea is the first agent of choice. Care mustbe taken because some patients appear to be particularly sensitiveto sulphonylurea induced hypoglycaemia. For this reason, we fa-vour sulphonylureas with a short half-life, and always start withthe very lowest dose and titrate up. Metformin is best avoided be-cause of the risk of exacerbating lactic acidosis. Having said this,we have used metformin in patients with accompanying obesityand have not experienced any clinical problems. The emergenceof newer agents such as DDP4 inhibitors and GLP-1 analogues offeralternative therapeutic opportunities, and we are using them assecond line treatment in preference to metformin depending uponthe clinical indications. As detailed above, a minority of patients re-quire insulin from the time of diagnosis, and those with initial non-insulin dependent diabetes often progress rapidly to insulin ther-apy. We tailor the insulin regimen to patient’s individual lifestyleand daily needs.
As described above, progression to end stage renal failure andkidney transplantation is a recognised outcome. This opens upthe possibility of pancreas transplantation, either as a simulta-neous kidney and pancreas procedure or as a pancreas after kidneytransplant. A key attraction is that there is no on-going
autoimmune process in mitochondrial diabetes (unlike patientswith type 1 diabetes undergoing transplantation), and so the trans-planted organs in theory should last longer.
While discussing management it is worth clarifying the role ofstatins in mitochondrial diabetes. Statins are often recommendedfor diabetic patients to help lessen the risks of atherosclerotic com-plications. Understandably, use of a drug with the potential to in-duce a myositis often causes concern in relation to pre-existingmitochondrial myopathy. In the majority of cases we do not be-lieve the risks outweigh the benefits, but do advise caution. Asmany patients with mitochondrial disease often have a mildly ele-vated creatine kinase (CK < 1000IU) at baseline, we recommenddocumentation of pre-treatment CK levels with repeat CK mea-surements while on statin therapy and advise to report new myal-gia or weakness.
It is evident that mitochondrial diabetes is complicated. Thedisease pattern with a high risk of rapid progression to insulinand the high prevalence of complications means that patients needaccess to a specialist diabetes service offering regular review. Thesituation is further complicated by the multisystem nature of mito-chondrial disease. As a consequence, we have just recently estab-lished a combined mitochondrial/diabetes clinic run jointly bythe neurologists and diabetologists that provides an integrated,one-stop service for patients with mitochondrial diabetes. We havealso developed Best Practice Guidelines for mitochondrial diabeteswhich are available online (http://www.newcastle-mitochon-dria.com/service/patient-care-guidelines/).
6. Hypoparathyroidism
Hypoparathyroidism is best described in KSS which occurs as aresult of a sporadic, single large-scale mtDNA rearrangement.Although reports are relatively rare, they seem consistent (Quadeet al., 1992; Isotani et al., 1996; Katsanos et al., 2001; Cassandriniet al., 2006; Wilichowski et al., 1997). In each case children havemultisystem disease, often with renal disease or other endocrinop-athies in addition to the classic KSS phenotype. There does not ap-pear to be an autoimmune basis to the hypoparathyroidoism(Isotani et al., 1996). Autopsy studies suggest absent or atrophichypoparathyroid glands (Horwitz and Roessmann, 1978; Bordarieret al., 1990). Although some patients with basal ganglia calcifica-tion on CT have been found to have hypoparathyroidism (Seigelet al., 1979; Cassandrini et al., 2006) the majority have no abnor-malities of calcium homeostasis. The genetic basis of KSS was firstconfirmed in 1988 (Holt et al., 1988) and reports of hypoparathy-roidism (and other endocrinopathies) in KSS prior to that periodare unsupported by genetic studies ((Horwitz and Roessmann,1978; Seigel et al., 1979; Dewhurst et al., 1986). It is possible thatsome of these cases may have harboured mtDNA point mutations(e.g. m.3243A > G) or multiple mtDNA deletions of a nuclear cause.Harvey and Barnett’s (1992) review found 14 of 226 patients withKSS and CPEO to have hypoparathyroidism, but the relevant mes-sage from this study is probably more pertinent to endocrine dis-ease associated with the phenotype than the genotype, as not allcases had been genetically confirmed (Harvey and Barnett, 1992).Hypoparathyroidism has been described in patients with ar-RRM2Bmutations, for example, and historically would have been includedin this group on the basis of the clinical features (Pitceathly et al.,2012).
In our experience, hypoparathyroidism is extremely rare inadult forms of mitochondrial disease. The paucity of case reportsin the literature suggests likewise (Tanaka et al., 2000). It seemsmost likely to occur in very severely affected patients who presentin childhood with multisystem disease. This may suggest that clin-ically significant levels of heteroplasmy within the parathyroid
6 A.M. Schaefer et al. / Molecular and Cellular Endocrinology 379 (2013) 2–11

glands, or alternatively the heteroplasmic threshold for dysfunc-tion of the parathyroid glands, is only reached in cases where veryhigh levels of heteroplasmy are present in most tissues.
7. Hypothalamo-pituitary axis
The most consistent descriptions of endocrine dysfunctiondue to impairment of the hypothalamopituitary axis appear tobe in severe mitochondrial phenotypes presenting in childhood.MELAS and KSS appear the most common phenotypes. The endo-crine disorder may precede the neurological features and lacticacidosis is often the clue to a mitochondrial cause. Short statureis usually present and more classical phenotypic expressiondevelops later if the patient survives. Reports in adults are muchrarer.
8. Growth hormone deficiency
Growth hormone (GH) deficiency has been described in KSS,both before and after genetic testing became available (Harveyand Barnett, 1992; Quade et al., 1992; Mohri et al., 1998; Berioand Piazzi, 2000; Cassandrini et al., 2006; Berio and Piazzi, 2007).It has also been reported in MELAS due to the m.3243A > G muta-tion in children (Yorifuji et al., 1996; Robeck et al., 1996; Balestriand Grosso, 2000; Matsuzaki et al., 2002) and in very rare adultcases with the MELAS (Ishii et al., 1991) and MIDD phenotypes(Joko et al., 1997). GH deficiency is often declared to be the causeof short stature in the mitochondrial myopathies, but the causesare more likely to be complex and multi-factorial for most patients(Wolny et al., 2009). Publication bias is probably to blame for thelack of reports documenting short stature and normal GH, butthese probably form the majority of cases.
9. Hypogonadism
Mutations in the POLG gene have been associated with primarytesticular failure (Filosto et al., 2003), primary ovarian failure (Luo-ma et al., 2004; Hakonen et al., 2005), and ovarian dysgenesis (Bek-heirnia et al., 2012). ar-PEO1 mutations are reported to causefemale hypergonadotrophic hypogonadism by teen age (Lönnqvistet al., 2009). Hypogonadism has been reported in association withmtDNA depletion due to ar-RRM2B mutations whilst cases of bothhypergonadotropic and hypogonadotropic hypogonadism havebeen described in reports of mitochondrial neurogastrointestinalencephalopathy (MNGIE) (Carod-Artal et al., 2007; Kalkan et al.,2012). It has been suggested from review of the early literaturethat up to 20% of patients with KSS develop gonadal dysfunction,either before or after puberty (Harvey and Barnett, 1992; Quadeet al., 1992). Both sexes were affected equally. It is possible how-ever that some of the patients diagnosed on clinical and histologi-cal grounds alone may have carried other mtDNA mutations or ARforms of disease rather than single deletions of the mtDNA. Genet-ically-confirmed case reports exist but are rare (Barrientos et al.,1997). Low levels of follicle stimulating hormone (FSH) and lutein-izing hormaone (LH) have both been reported in MELAS (Ishii et al.,1991; Robeck et al., 1996; Ohkoshi et al., 1998; Balestri and Grosso,2000) but are also rare. In both KSS and MELAS it is possible thathypogonadism is underdiagnosed where other forms of multisys-tem disease dominate the clinical picture.
10. Hypothyroidism
Thyroid disease is not a recognised complication of mitochon-drial disease. Observations from our own mitochondrial cohort
are that it occurs in similar frequency to the background popula-tion, and is often associated with thyroid antibodies as might beexpected. Reports in KSS are rare and usually associated with auto-immunity (Berio and Piazzi, 2006; Sanaker et al., 2007); only rarereports exist for patients with the m.3243A > G mutation (Balestriand Grosso, 2000; Lau et al., 2007). Hypothyroidism was docu-mented in 2/18 adult RRM2B patients, but antibody status wasnot reported (Pitceathly et al., 2012).
11. Hypoadrenalism
This is rarely described in mitochondrial disease but impor-tantly has been reported in children prior to the development oftypical features of KSS. Patients are often neurologically normalat presentation but have short stature and may exhibit a lactic aci-dosis. Adrenocorticotropic hormone (ACTH) is elevated but anti-bodies negative (Nicolino et al., 1997; Boles et al., 1998). Wehave recently identified an adult harbouring a single, large-scalemtDNA deletion and a mild KSS phenotype who developed non-autoimmune adrenal insufficiency at 51 years of age (personalobservation).
12. SIADH
The syndrome of inappropriate anti-diuretic hormone secretion(SIADH) is probably under recognised as an endocrine disorder inmitochondrial disease. Hyponatraemia may also occur as a resultof unrecognised renal disease, adrenal insufficiency, or gastrointes-tinal losses related to pseudoileus, while in other cases the causemay not be identified (Kubota et al., 2005; Gurrieri et al., 2001).In our experience, hyponatraemia is relatively common in patientscarrying the m.3243A > G mutation, but not always due to SIADH.When this occurs it is usually transient and associated with stroke-like episodes and more specifically ongoing seizure activity (Patelet al., 2007). In this respect SIADH can sometimes be an indicationof active cerebral dysfunction. MELAS patients appear prone toSIADH, or exacerbation of pre-existing SIADH, with certain anti-convulsants such as carbamazepine. In most cases this is not severeenough to prevent the use of clinically useful drugs in the acutesetting, but may affect subsequent treatment choices.
13. Adipose tissue as an endocrine organ
There has been very little work looking at adipose tissue func-tion in mitochondrial diabetes. A recent study compared adiposetissue and liver fat metabolism between patients with them.3243A > G mutation and healthy control subjects. They foundthat patients with the mutation showed evidence of adipose tissueinsulin resistance and a tendency to increased liver fat. However,as there were no diabetes controls, it was not clear to what extentthe metabolic changes reflect the diabetic state rather than specificchanges related to the mitochondrial disease (Lindroos et al.,2011). Further work is needed to determine whether there are adi-pose tissue abnormalities that are specific to mitochondrialdisease.
One such scenario occurs in Ekbom’s Syndrome. Originally de-scribed as ‘hereditary ataxia, photomyoclonus, skeletal deformitiesand lipoma’ (Ekbom, 1975), it was subsequently confirmed to oc-cur as a result of the m.8344A > G MTTK mutation associated withthe MERRF phenotype (Träff et al., 1995). Many MERRF patients de-velop unusual lipomata around the neck and shoulder region cor-responding to the distribution of brown fat tissue; these lesionsmay be painful, restrict movement, and account for major aesthetic
A.M. Schaefer et al. / Molecular and Cellular Endocrinology 379 (2013) 2–11 7

and psychological morbidity, although the mechanisms underlyingthis phenomenon are currently undetermined.
14. Autoimmune endocrinopathy
Autoimmune endocrine disease has been reported in severalforms of mitochondrial disease. Despite this, overall there is a lackof firm evidence to suggest autoimmune disorders are any moreprevalent in mitochondrial cohorts than in the general population.Most cases of MIDD do not have anti-GAD or islet cell antibodiesbut these have been reported in small numbers (Oka et al., 1993;Murphy et al., 2008) and more frequently in some cohorts (Kobay-ashi et al., 1996). It has been hypothesised that mitochondrial dys-function may play some role in the development of autoimmunitybut this remains unproven. In diabetes, pancreatic B-cell destruc-tion has been proposed as the catalyst for antibody production(Oka et al., 1993).
Autoimmune hypothyroidism is described rarely in patientswith KSS, one such report also having Addison’s disease with adre-nal antibodies (Berio and Piazzi, 2006; Sanaker et al., 2007).
Autoimmune polyglandular syndrome type II has been reportedonce in a mild KSS/CPEO phenotype. The endocrine features wereAddison’s disease, IDDM, autoimmune thyroiditis and primaryovarian failure. Interestingly this patient carried both a 2,532-bpdeletion of her mtDNA, consistent with KSS, but also a heteroplas-mic m.3243A > G mutation which was also present in her mother’smtDNA. Whether mitochondrial disease played a role in this is un-clear (Ohno et al., 1996).
15. Conclusion
Endocrine dysfunction in mitochondrial disease is common,but predominantly due to the prevalence of the m.3243A > Gmutation and its association with diabetes mellitus. OthermtDNA mutations reliably expressing a diabetic phenotype arerare, and other forms of endocrine dysfunction are unusual whenconsidering the mitochondrial diseases as a whole. Pattern rec-ognition and detailed pedigee analysis are key when evaluatingthe likelihood of a mitochondrial disorder, and the presence ofendocrine disease may contribute to the diagnostic process.Furthermore, appreciation of the endocrine organs at risk in aspecified genotype/phenotype allows an appropriate level ofscreening to be initiated as part of the patient’s multidisciplinarycare strategy. KSS patients are at risk of hypoparathyroidism, andpatients with advanced multi-system disease presenting in child-hood, whether due to mtDNA mutations or nuclear mtDNAmaintenance genes, appear at risk of hypothalamopituitary dys-function. Most patients with mitochondrial disease, but mostnotably those carrying the m.3243A > G mutation, should haveaccess to annual screening for diabetes. The tendency to multi-system disease in these complex families can make managementdifficult, even in asymptomatic carriers. For this reason we rec-ommend referral to a specialist mitochondrial centre for diseasespecific advice and management plans.
Acknowledgments
D.M.T. and R.W.T. are supported by a Strategic Award from theWellcome Trust (096919/Z/11/Z). A.M.S., D.M.T. and R.W.T.acknowledge the support of the UK NHS Specialist Commissionerswhich funds the ‘‘Rare Mitochondrial Disorders of Adults and Chil-dren’’ Clinical and Diagnostic Service in Newcastle upon Tyne.
References
Abad, M.M., Cotter, P.D., Fodor, F.H., Larson, S., Ginsberg-Fellner, F., Desnick, R.J.,et al., 1997. Screening for the mitochondrial DNA A3243G mutation in childrenwith insulin-dependent diabetes mellitus. Metabolism 46, 445–449.
Adler, A.I., Stevens, R.J., Manley, S.E., Bilous, R.W., Cull, C.A., Holman, R.R., 2003.Development and progression of nephropathy in Type 2 diabetes: the UnitedKingdom Prospective Diabetes Study (UKPDS 64). Kidney Int. 63, 225–232.
Anderson, S., Bankier, A.T., Barrell, B.G., de Bruijn, M.H., Coulson, A.R., Drouin, J.,et al., 1981. Sequence and organization of the human mitochondrial genome.Nature 290, 457–465.
Austin, S., Vriesendorp, F., Thandroyen, F., Hecht, J., Jones, O., Johns, D., 1998.Expanding the phenotype of the 8344 transfer RNA lysine mitochondrial DNAmutation. Neurology 51, 1447–1450.
Balestri, P., Grosso, S., 2000. Endocrine disorders in two sisters affected by MELASsyndrome. J. Child Neurol. 15, 755–758.
Ballinger, S.W., Shoffner, J.M., Gebhart, S., Koontz, D.A., Wallace, D.C., 1994.Mitochondrial diabetes revisited. Nat. Genet. 7, 458–459.
Barrientos, A., Casademont, J., Genis, D., Cardellach, F., Fernández-Real, J.M., Grau,J.M., et al., 1997. Sporadic heteroplasmic single 5.5 kb mitochondrial DNAdeletion associated with cerebellar ataxia, hypogonadotropic hypogonadism,choroidal dystrophy, and mitochondrial respiratory chain complex I deficiency.Hum. Mutat. 10, 212–216.
Bekheirnia, M.R., Zhang, W., Eble, T., Willis, A., Shaibani, A., Wong, L.J., et al., 2012.POLG mutation in a patient with cataracts, early-onset distal muscle weaknessand atrophy, ovarian dysgenesis and 3-methylglutaconic aciduria. Gene 499,209–212.
Berio, A., Piazzi, A., 2000. Kearns–Sayre syndrome with GH deficiency. Pediatr. Med.Chir. 22, 43–46.
Berio, A., Piazzi, A., 2006. A case of Kearns–Sayre sindrome with autoimmunethyroiditis and complete atrio-ventricular block. Min. Cardioangiol. 54, 387–391.
Berio, A., Piazzi, A., 2007. Facial anomalies in a patient with cytochrome-oxidasedeficiency and subsequent Kearns–Sayre sindrome with growth hormonedeficiency. Min. Med. 98, 81–85.
Blackwood, J.K., Whittaker, R.G., Blakely, E.L., Alston, C.L., Turnbull, D.M., Taylor,R.W., 2010. The investigation and diagnosis of pathogenic mitochondrial DNAmutations in human urothelial cells. Biochem. Biophys. Res. Commun. 393,740–745.
Boles, R.G., Roe, T., Senadheera, D., Mahnovski, V., Wong, L.J.C., 1998. MitochondrialDNA deletion with Kearns Sayre syndrome in a child with Addison disease. Eur.J. Ped. 157, 643–647.
Bordarier, C., Duyckaerts, C., Robain, O., Ponsot, G., Laplane, D., 1990. Kearns–Sayresyndrome: two clinico-pathological cases. Neuropediatrics 21, 106–109.
Calvo, S.E., Compton, A.G., Hershman, S.G., Lim, S.C., Lieber, D.S., Tucker, E.J.,Laskowski, A., 2012. Molecular diagnosis of infantile mitochondrial disease withtargeted next-generation sequencing. Sci. Transl. Med. 25, 118ra10.
Cao, L., Shitara, H., Horii, T., Nagao, Y., Imai, H., Abe, K., et al., 2007. Themitochondrial bottleneck occurs without reduction of mtDNA content infemale mouse germ cells. Nat. Genet. 39, 386–390.
Carod-Artal, F.J., Herrero, M.D., Lara, M.C., López-Gallardo, E., Ruiz-Pesini, E., Martí,R., et al., 2007. Cognitive dysfunction and hypogonadotrophic hypogonadism ina Brazilian patient with mitochondrial neurogastrointestinalencephalomyopathy and a novel ECGF1 mutation. Eur. J. Neurol. 14, 581–585.
Cassandrini, D., Savasta, S., Bozzola, M., Tessa, A., Pedemonte, M., Assereto, S., et al.,2006. Mitochondrial DNA deletion in a child with mitochondrialencephalomyopathy, growth hormone deficiency, and hypoparathyroidism. J.Child Neurol. 21, 983–985.
Choo-Kang, A., Lynn, S., Taylor, G., Daly, M.E., Sihota, S.S., Wardell, T.M., et al., 2002.Defining the importance of mitochondrial gene defects in maternally inheriteddiabetes by sequencing the entire mitochondrial genome. Diabetes 51, 2317–2320.
Cole, A., Dutton, G.N., 2000. Leber’s hereditary optic neuropathy and maturity onsetdiabetes mellitus: is there a metabolic association? Br. J. Ophthalmol. 84, 439–440.
Cree, L.M., Samuels, D.C., de Sousa Lopes, S.C., Rajasimha, H.K., Wonnapinij, P.,Mann, J.R., et al., 2008. A reduction of mitochondrial DNA molecules duringembryogenesis explains the rapid segregation of genotypes. Nat. Genet. 40,249–254.
Das, S., Bennett, A.J., Sovio, U., Ruokonen, A., Martikainen, H., Pouta, A., et al., 2007.Detailed analysis of variation at and around mitochondrial position 16189 in alarge Finnish cohort reveals no significant associations with early growth ormetabolic phenotypes at age 31 years. J. Clin. Endocrinol. Metab. 92, 3219–3223.
Dewhurst, A.G., Hall, D., Schwartz, M.S., McKeran, R.O., 1986. Kearns–Sayresyndrome, hypoparathyroidism, and basal ganglia calcification. J. Neurol.Neurosurg. Psych. 49, 1323–1324.
Du Bois, L.G., Feldon, S.E., 1992. Evidence for a metabolic trigger for Leber’shereditary optic neuropathy. J. Clin. Neuro-Ophthalmol. 12, 15–16.
Ekbom, K., 1975. Hereditary ataxia, photomyoclonus, skeletal deformities andlipoma. Acta Neurol. Scand. 51, 393–404.
Elliott, H.R., Samuels, D.C., Eden, J.A., Relton, C.L., Chinnery, P.F., 2008. Pathogenicmitochondrial DNA mutations are common in the general population. Am. J.Hum. Genet. 83, 254–260.
8 A.M. Schaefer et al. / Molecular and Cellular Endocrinology 379 (2013) 2–11

Filosto, M., Mancuso, M., Nishigaki, Y., Pancrudo, J., Harati, Y., Gooch, C., et al., 2003.Clinical and genetic heterogeneity in progressive external ophthalmoplegia dueto mutations in polymerase gamma. Arch. Neurol. 60, 1279–1284.
Goto, Y., Nonaka, I., Horai, S., 1991. A new mtDNA mutation associated withmitochondrial myopathy, encephalopathy, lactic acidosis and stroke-likeepisodes (MELAS). Biochim. Biophys. Acta 1097, 238–240.
Greaves, L.C., Reeve, A.K., Taylor, R.W., Turnbull, D.M., 2012. Mitochondrial DNA anddisease. J. Pathol. 226, 274–286.
Guillausseau, P.J., Massin, P., Dubois-Laforge, D., Timsit, J., Virally, M., Gin, H., et al.,2001. Maternally inherited diabetes and deafness: a multicenter study. Ann. Int.Med. 134, 721–728.
Guillausseau, P.J., Dubois-Laforge, D., Massin, P., Laloi-Michelin, M., Bellanne-Chantelot, C., Gin, H., et al., 2004. Heterogeneity of diabetes phenotype inpatients with 3243-bp mutation of mitochondrial DNA (maternally inheriteddiabetes and deafness or MIDD). Diabet. Metab. 30, 181–186.
Gurrieri, C., Kivela, J.E., Bojanic, K., Gavrilova, R.H., Flick, R.P., Sprung, J., et al., 2001.Anesthetic considerations in mitochondrial encephalomyopathy, lactic acidosis,and stroke-like episodes syndrome: a case series. Can. J. Anaesth. 58, 751–763.
Hakonen, A.H., Heiskanen, S., Juvonen, V., Lappalainen, I., Luoma, P.T., Rantamaki,M., et al., 2005. Mitochondrial DNA polymerase W748S mutation: a commoncause of autosomal recessive ataxia with ancient European origin. Am. J. Hum.Genet. 77, 430–441.
Hanna, M.G., Nelson, I., Sweeney, M.G., Cooper, J.M., Watkins, P.J., Morgan-Hughes,J.A., et al., 1995. Congenital encephalomyopathy and adult-onset myopathy anddiabetes mellitus: different phenotypic associations of a new heteroplasmicmtDNA tRNA glutamic acid mutation. Am. J. Hum. Genet. 56, 1026–1033.
Harvey, J.N., Barnett, D., 1992. Endocrine dysfunction in Kearns–Sayre syndrome.Clin. Endocrinol. 37, 97–103.
Holmes-Walker, D., Mitchell, P., Boyages, S., 1998. Does mitochondrial genomemutation in subjects with maternally inherited diabetes and deafness decreaseseverity of diabetic retinopathy. Diabet. Med. 15, 946–952.
Holt, I.J., Harding, A.E., Morgan-Hughes, J.A., 1988. Deletions of musclemitochondrial DNA in patients with mitochondrial myopathies. Nature 331,717–719.
Horvath, R., Hudson, G., Ferrari, G., Fütterer, N., Ahola, S., Lamantea, E., et al., 2006.Phenotypic spectrum associated with mutations of the mitochondrialpolymerase c gene. Brain 129, 1674–1684.
Horwitz, S.J., Roessmann, U., 1978. Kearns Sayre syndrome withhypoparathyroidism. Ann. Neurol. 3, 513–518.
Ishii, A., Watanabe, S., Ohkoshi, N., Mizusawa, H., Kanazawa, I., 1991. Mitochondrialencephalomyopathy, lactic acidosis and stroke-like episodes (MELAS)associated with hypothalamo-pituitary hypofunction: a case report. Clin.Neurol. 31, 179–183.
Ishiyama, A., Komaki, H., Saito, T., Saito, Y., Nakagawa, E., Sugai, K., et al., 2012.Unusual exocrine complication of pancreatitis in mitochondrial disease. BrainDev., pii:S0387-7604(12)00273-2.
Isotani, H., Fukumoto, Y., Kawamura, H., Furukawa, K., Ohsawa, N., Goto, Y.I., et al.,1996. Hypoparathyroidism and insulin-dependent diabetes mellitus in apatient with Kearns–Sayre syndrome harbouring a mitochondrial DNAdeletion. Clin. Endocrin. 45, 637–641.
Iwasaki, N., Babazono, T., Tsuchiya, K., Tomonaga, O., Suzuki, A., Togashi, M., et al.,2001. Prevalence of A-to-G mutation at nucleotide 3243 of the mitochondrialtRNALeu(UUR) gene in Japanese patients with diabetes mellitus and end-stagerenal disease. J. Hum. Genet. 46, 330–334.
Joko, T., Iwashige, K., Hashimoto, T., Ono, Y., Kobayashi, K., Sekiguchi, N., et al., 1997.A case of mitochondrial encephalomyopathy, lactic acidosis and stroke-likeepisodes associated with diabetes mellitus and hypothalamo-pituitarydysfunction. Endocr. J. 44, 805–809.
Kadowaki, H., Tobe, K., Mori, Y., Sakura, H., Sakuta, R., Nonaka, I., et al., 1993.Mitochondrial gene mutation and insulin-deficient type of diabetes mellitus.Lancet 341, 893–894.
Kadowaki, T., Kadowaki, H., Mori, Y., Tobe, K., Sakuta, R., Suzuki, Y., et al., 1994. Asubtype of diabetes mellitus associated with a mutation of mitochondrial DNA.N. Eng. J. Med. 330, 962–968.
Kalkan, I.H., Tayfur, O., Oztas!, E., Beyazit, Y., Yildiz, H., Tunç, B., 2012. A novel findingin MNGIE (Mitochondrial Neurogastrointestinal Encephalomyopathy):hypergonadotropic hypogonadism. Hormones (Athens) 11, 377–379.
Kameoka, K., Isotani, H., Tanaka, K., Kitaoka, H., Ohsawa, N., 1998. Impaired insulinsecretion in Japanese diabetic subjects with an A-to-G mutation at nuceotide8296 of the mitochondrial DNA in tRNALys. Diabet. Care 21, 2034–2035.
Katagiri, H., Asano, T., Ishihara, H., Inukai, K., Anai, M., Yamanouchi, T., et al., 1994.Mitochondrial diabetes mellitus: prevalence and clinical characterization ofdiabetes due to mitochondrial tRNALeu(UUR) gene mutation in Japanese patients.Diabetologia 37, 504–510.
Katsanos, K.H., Elisaf, M., Bairaktari, E., Tsianos, E.V., 2001. Severe hypomagnesemiaand hypoparathyroidism in Kearns–Sayre syndrome. Am. J. Nephrol. 21, 150–153.
Kishimoto, M., Hashiramoto, M., Araki, S., Ishida, Y., Kazumi, T., Kand, E., et al., 1995.Diabetes mellitus carrying a mutation in the mitochondrial tRNA Leu(UUR) gene.Diabetologia 38, 193–200.
Kishnani, P.S., Van Hove, J.L.K., Shoffner, J.S., Kaufman, A., Bossen, E.H., Kahler, S.G.,1996. Acute pancreatitis in an infant with lactic acidosis and a mutation atnucleotide 3243 in the mitochondrial DNA tRNALeu(UUR) gene. Eur. J. Pediatr.155, 898–903.
Klemm, T., Neumann, S., Trulzsch, B., Pistrosch, F., Hanefeld, M., Paschke, R., 2001.Search for mitochondrial DNA mutation at position 3243 in German patientswith a positive family history of maternal diabetes mellitus. Exp. Clin.Endocrinol. Diabet. 109, 283–287.
Kobayashi, T., Oka, Y., Katagiri, H., Falorni, A., Kasuga, A., Takei, I., et al., 1996.Association between HLA and islet cell antibodies in diabetic patients with amitochondrial DNA mutation at base pair 3243. Diabetologia 39, 1196–1200.
Kobayashi, T., Nakanishi, K., Nakase, H., Kajio, H., Okubo, M., Murase, T., et al., 1997.In situ characterization of islets in diabetes with a mitochondrial DNA mutationat nucleotide position 3243. Diabetes 46, 1567–1572.
Kubota, H., Tanabe, Y., Takanashi, J.I., Kohno, Y., 2005. Episodic hyponatremia inmitochondrial encephalomyopathy, lactic acidosis, and strokelike episodes(MELAS). J. Child Neurol. 20, 116–119.
Laloi-Michelin, M., Meas, T., Ambonville, C., Bellanné-Chantelot, C., Beaufils, S.,Massin, P., et al., 2009. Mitochondrial Diabetes French Study Group. The clinicalvariability of maternally inherited diabetes and deafness is associated with thedegree of heteroplasmy in blood leukocytes. J. Clin. Endocrinol. Metab. 94,3025–3030.
Latvala, T., Mustonen, E., Uusitalo, R., Majamaa, K., 2002. Pigmentary retinopathy inpatients with the MELAS mutation 3243A > G in mitochondrial DNA. Arch. Clin.Exp. Ophthalmol. 240, 795–801.
Lau, K.K., Yang, S.P., Haddad, M.N., Butani, L., Makker, S.P., 2007. Mitochondrialencephalopathy with lactic acidosis and stroke-like episodes syndrome withhypothyroidism and focal segmental glomerulosclerosis in a paediatric patient.Int. J. Urol. Nephrol. 39, 941–946.
Lehto, M., Wipemo, C., Ivarsson, S., Lindgren, C., Lipsanen-Nyman, M., Weng, J., et al.,1999. High frequency of mutations in MODY and mitochondrial genes inScandinavian patients with familial early-onset diabetes. Diabetologia 42,1131–1137.
Lindroos, B., Suuronen, R., Miettinen, S., 2011. The potential of adipose stem cells inregenerative medicine. Stem Cell Rev. 7, 269–291.
Lönnqvist, T., Paetau, A., Valanne, L., Pihko, H., 2009. Recessive twinkle mutationscause severe epileptic encephalopathy. Brain 132, 1553–1562.
Luoma, P., Melberg, A., Rinne, J.O., Kaukonen, J.A., Nupponen, N.N., Chalmers, R.M.,et al., 2004. Parkinsonism, premature menopause, and mitochondrial DNApolymerase gamma mutations: clinical and molecular genetic study. Lancet364, 875–882.
Lynn, S., Wardell, T., Johnson, M.A., Chinnery, P.F., Daly, M.E., Walker, M., et al., 1998.Mitochondrial diabetes: investigation and identification of a novel mutation.Diabetes 47, 1800–1802.
Lynn, S., Borthwick, G.M., Charnley, R.M., Walker, M., Turnbull, D.M., 2003.Heteroplasmic ratio of the A3243G mitochondrial DNA mutation in singlepancreatic beta cells. Diabetologia 46, 296–299.
Maassen, J., t’Hart, L., van Essen, E., Heine, R., Nijpels, G., Jahangir Tafrechi, R., et al.,2004. Mitochondrial diabetes: molecular mechanisms and clinical presentation.Diabetes 53, S103–S109.
Majamaa, K., Turkka, J., Karppa, M., Winqvist, S., Hassinen, I.E., 1997. The commonMELAS mutation A3243G in mitochondrial DNA among young patients with anoccipital brain infarct. Neurology 49, 1331–1334.
Malecki, M.T., Klupa, T., Wanic, K., Frey, J., Cyganek, K., Sieradzki, J., 2001. Search formitochondrial A3243G tRNA(Leu) mutation in Polish patients with Type 2diabetes mellitus. Med. Sci. Monit. 7, 246–250.
Mansergh, F.C., Millington-Ward, S., Kennan, A., Kiang, A.-S., Humphries, M., Farrar,G.J., et al., 1999. Retinitis pigmentosa and progressive sensorineural hearing losscaused by a C12258A mutation in the mitochondrial MTTS2 gene. Am. J. Hum.Genet. 64, 971–985.
Massin, P., Virally-Monod, M., Vialettes, B., Paques, M., Gin, H., Porokhov, B., et al.,1999. Prevalence of macular pattern dystrophy in maternally inherited diabetesand deafness. GEDIAM group. Ophthalmology 106, 1821–1827.
Matsuura, N., Suzuki, S., Yokota, Y., Kazahari, K., Kazahari, M., Toyota, T., et al., 1999.The prevalence of mitochondrial gene mutations in childhood diabetes in Japan.J. Pediatr. Endocrinol. Metab. 12, 27–30.
Matsuzaki, M., Izumi, T., Shishikura, K., Suzuki, H., Hirayama, Y., 2002.Hypothalamic growth hormone deficiency and supplementary GH therapy intwo patients with mitochondrial myopathy, encephalopathy, lactic acidosis andstroke-like episodes. Neuropediatrics 33, 271–273.
McDonnell, M.T., Blakely, E.L., Schaefer, A.M., McFarland, R., Turnbull, D.M., Taylor,R.W., 2004. Non-invasive diagnosis of the 3243A > G mitochondrial DNAmutation using urinary epithelial cells. Eur. J. Hum. Genet. 12, 778–781.
McFarland, R., Schaefer, A.M., Gardner, J.L., Lynn, S., Hayes, C.M., Barron, M.J., et al.,2004. Familial myopathy: new insights into the T14709C mitochondrial tRNAmutation. Ann. Neurol. 55, 478–484.
McFarland, R., Taylor, R.W., Turnbull, D.M., 2010. A neurological perspective onmitochondrial disease. Lancet Neurol. 9, 829–840.
Misra, A., Bachmann, M.O., Greenwood, R.H., Jenkins, C., Shaw, A., Barakat, O., et al.,2009. Trends in yield and effects of screening intervals during 17 years of a largeUK community-based diabetic retinopathy screening programme. Diabet. Med.26, 1040–1047.
Mohri, I., Taniike, M., Fujimura, H., Matsuoka, T., Inui, K., Nagai, T., et al., 1998. A caseof Kearns–Sayre syndrome showing a constant proportion of deletedmitochondrial DNA in blood cells during 6 years of follow-up. J. Neurol. Sci.158, 106–109.
Murphy, R., Turnbull, D.M., Walker, M., Hattersley, A.T., 2008. Clinical features,diagnosis and management of maternally inherited diabetes and deafness
A.M. Schaefer et al. / Molecular and Cellular Endocrinology 379 (2013) 2–11 9

(MIDD) associated with the 3243A > G mitochondrial point mutation. Diabet.Med. 25, 383–399.
Nagashima, T., Mori, M., Katayama, K., Nunomura, M., Nishihara, H., Hiraga, H., et al.,1999. Adult Leigh syndrome with mitochondrial DNA mutation at 8993. ActaNeuropathol. 97, 416–422.
Newkirk, J.E., Taylor, R.W., Howell, N., Bindoff, L.A., Chinnery, P.F., Alberti, K.G., et al.,1997. Maternally inherited diabetes and deafness: prevalence in a hospitaldiabetic population. Diabet. Med. 14, 457–460.
Newman, N.J., Lott, M.T., Wallace, D.C., 1991. The clinical characteristics ofpedigrees of Leber’s hereditary optic neuropathy with the 11778 mutation.Am. J. Ophthalmol. 111, 750–762.
Ng, M., Yeung, V., Chow, C., Li, J., Smith, P., Mijovic, C., et al., 2000. MitochondrialDNA A3243G mutation in patients with early or late-onset Type 2 diabetesmellitus in Hong Kong Chinese. Clin. Endocrinol. 52, 557–564.
Nicolino, M., Ferlin, T., Forest, M., Godinot, C., Carrier, H., David, M., et al., 1997.Identification of a large-scale mitochondrial deoxyribonucleic acid deletion inendocrinopathies and deafness: report of two unrelated cases with diabetesmellitus and adrenal insufficiency, respectively. J. Clin Endocrin. Metab. 82,3063–3067.
Odawara, M., Sasaki, K., Yamashita, K., 1995. Prevalence and clinicalcharacterisation of Japanese diabetes mellitus with an A to G mutation atnucleotide 3243 of the mitochondrial tRNALeu(UUR) gene. J. Clin. Endocrinol.Metab. 80, 1290–1294.
Ohkoshi, N., Ishii, A., Shiraiwa, N., Shoji, S.I., Yoshizawa, K., 1998. Dysfunction of thehypothalamic-pituitary system in mitochondrial encephalomyopathies. J. Med.29, 13–29.
Ohkubo, K., Yamano, A., Nagashima, M., Mori, Y., Anzai, K., Akehi, Y., et al., 2001.Mitochondrial gene mutations in the tRNALeu(UUR) region and diabetes:prevalence and clinical phenotypes in Japan. Clin. Chem. 47, 1641–1648.
Ohno, K., Yamamoto, M., Engel, A.G., Harper, C.M., Roberts, L.R., Tan, G.H., 1996.MELAS- and Kearns–Sayre-type co-mutation [corrected] with myopathy andautoimmune polyendocrinopathy. Ann. Neurol. 39, 761–766.
Oka, Y., Katagiri, H., Yazaki, Y., Murase, T., Kobayashi, T., 1993. Mitochondrial genemutation in islet-cell-antibody-positive patients who were initially non-insulindependent diabetics. Lancet 342, 527–528.
Otabe, S., Sakura, H., Shimokawa, K., Mori, Y., Kadowaki, H., Yasuda, K., et al., 1994.The high prevalence of diabetic patients with a mutation in the mitochondrialgene in Japan. J. Clin. Endocrinol. Metab. 79, 768–771.
Patel, I.B., Sidani, M., Zoorob, R., 2007. Mitochondrial encephalopathy, lactic acidosisand stroke-like syndrome (MELAS): a case report, presentation, andmanagement. Southern Med. J. 100, 70–72.
Pilz, D., Quarrell, O.W., Jones, E.W., 1994. Mitochondrial mutation commonlyassociated with Leber’s hereditary optic neuropathy observed in a patient withWolfram syndrome (DIDMOAD). J. Med. Genet. 31, 328–330.
Pitceathly, R.D., Smith, C., Fratter, C., Alston, C.L., He, L., Craig, K., et al., 2012. Adultswith RRM2B-related mitochondrial disease have distinct clinical and molecularcharacteristics. Brain 135, 3392–3403.
Poulton, J., Luan, J., Macaulay, V., Hennings, S., Mitchell, J., Wareham, N.J., 2002. Type2 diabetes is associated with a common mitochondrial variant: evidence from apopulation-based case-control study. Hum. Mol. Genet. 11, 1581–1583.
Quade, A., Zierz, S., Klingmüller, D., 1992. Endocrine abnormalities in mitochondrialmyopathy with external ophthalmoplegia. Clin. Invest. 70, 396–402.
Rahman, S., Poulton, J., Marchington, D., Suomalainen, A., 2001. Decrease of 3243A ? G mtDNA mutation from blood in MELAS syndrome: a longitudinal study.Am. J. Hum. Genet. 68, 238–240.
Reardon, W., Ross, R., Sweeney, M., Luxon, L., Pembrey, M., Harding, A., et al., 1992.Diabetes mellitus associated with a pathogenic point mutation in mitochondrialDNA. Lancet 340, 1376–1379.
Robeck, S., Stefan, H., Engelhardt, A., Neundörfer, B., 1996. Follow-up studies anddisorders of endocrinologic function in MELAS syndrome. Nervenarzt 67, 465–470.
Rötig, A., Bessis, J.L., Romero, N., Cormier, V., Saudubray, J.M., Narcy, P., et al., 1992.Maternally inherited duplication of the mitochondrial genome in a syndrome ofproximal tubulopathy, diabetes mellitus, and cerebellar ataxia. Am. J. Hum.Genet. 50, 364–370.
Saker, P., Hattersley, A., Barrow, B., Hammersley, M., Horton, V., Gillmer, M., et al.,1997. UKPDS 21: low prevalence of the mitochondrial transfer RNA gene(tRNALeu(UUR)) mutation at position 3243 bp in UK Caucasian Type 2 diabeticpatients. Diabet. Med. 14, 42–45.
Sanaker, P.S., Husebye, E.S., Fondenes, O., Bindoff, L.A., 2007. Clinical evolution ofKearns–Sayre syndrome with polyendocrinopathy and respiratory failure. ActaNeurol. Scand. 115, 64–67.
Schaefer, A.M., McFarland, R., Blakely, E.L., He, L., Whittaker, R.G., Taylor, R.W., et al.,2008. Prevalence of mitochondrial DNA disease in adults. Ann. Neurol. 63, 35–39.
Schleiffer, T., t’Hart, L.M., Schurfeld, C., Kraatz, K., Riemann, J.F., 2000. Maternallyinherited diabetes and deafness (MIDD): unusual occult exocrine pancreaticmanifestation in an affected German family. Exp. Clin. Endocrinol. Diabet. 108,81–85.
Schon, E.A., DiMauro, S., Hirano, M., 2012. Human mitochondrial DNA: roles ofinherited and somatic mutations. Nat. Rev. Genet. 13, 878–890.
Seigel, R.S., Seeger, J.F., Gabrielsen, T.O., Allen, R.J., 1979. Computerised tomographyin oculocraniosomatic disease (Kearns–Sayre syndrome). Radiology 130, 159–164.
Smith, P., Bain, S., Good, P., Hattersley, A., Barnett, A., Gibson, J., et al., 1999.Pigmentary retinal dystrophy and the syndrome of maternally inheriteddiabetes and deafness caused by the mitochondrial DNA 3243 tRNA Leu A toG mutation. Opthalmology 106, 1101–1108.
Superti-Furga, A., Schoenle, E., Tuchschmid, P., Caduff, R., Sabato, V., DeMattia, D.,et al., 1993. Pearson bone marrow-pancreas syndrome with insulin-dependentdiabetes, progressive renal tubulopathy, organic aciduria and elevated fetalhaemoglobin caused by deletion and duplication of mitochondrial DNA. Eur. J.Pediatr. 152, 44–50.
Suzuki, S., Hinokio, Y., Hirai, S., Onoda, M., Matsumoto, M., Ohtomo, M., et al., 1994.Pancreatic beta-cell defect associated with mitochondrial point mutation of thetRNALeu(UUR) gene: a study in seven families with mitochondrialencephalomyopathy, lactic acidosis and stroke-like episodes (MELAS).Diabetologia 37, 818–825.
Suzuki, Y., Tsukuda, K., Atsumi, Y., Goto, Y., Hosokawa, K., Asahina, T., et al., 1996.Clinical picture of a case of diabetes with mitochondrial tRNA mutation atposition 3271. Diabet. Care 19, 1304–1305.
Suzuki, Y., Suzuki, S., Hinokio, Y., Chiba, M., Atsumi, Y., Hosokawa, K., et al., 1997.Diabetes associated with a novel 3264 mitochondrial tRNALeu(UUR) mutation.Diabet. Care 20, 1138–1140.
Suzuki, Y., Taniyama, M., Muramatsu, T., Ohta, S., Murata, C., Atsumi, Y., et al., 2003.Mitochondrial tRNALeu(UUR) mutation at position 3243 and symptomaticpolyneuropathy in Type 2 diabetes. Diabet. Care 26, 1315–1316.
Szendroedi, J., Schmid, A.I., Meyerspeer, M., Cervin, C., Kacerovsky, M., Smekal, G.,et al., 2009. Impaired mitochondrial function and insulin resistance of skeletalmuscle in mitochondrial diabetes. Diabet. Care 32, 677–679.
Tanaka, K., Takaday, Y., Matsunaka, T., Yuyama, S., Fujino, S., Maguchi, M., et al.,2000. Diabetes mellitus, deafness, muscle weakness and hypocalcemia in apatient with an A3243G mutation of the mitochondrial DNA. Int. Med. 39, 249–252.
Tawata, M., Hayashi, J., Isobe, K., Ohkubo, E., Ohtaka, M., Chen, J., et al., 2000. A newmitochondrial DNA mutation at 14577 T/C is probably a major pathogenicfactor for maternally inherited Type 2 diabetes. Diabetes 49, 1269–1272.
Taylor, R.W., Schaefer, A.M., Barron, M.J., McFarland, R., Turnbull, D.M., 2004. Thediagnosis of mitochondrial muscle disease. Neuromuscul. Disord. 14, 237–245.
t’Hart, L.M., Lemkes, H.H., Heine, R.J., Stolk, R.P., Feskens, E.J., Jansen, J.J., et al., 1994.Prevalence of maternally inherited diabetes and deafness in diabeticpopulations in The Netherlands. Diabetologia 37, 1169–1170.
The Diabetes Control and Complications Trial Research Group, 1993. The effect ofintensive treatment of diabetes on the development and progression of long-term complications in insulin dependent diabetes mellitus. N. Engl. J. Med. 329,977–986.
Thomas, R.L., Dunstan, F., Luzio, S.D., Roy Chowdury, S., Hale, S.L., North, R.V., et al.,2012. Incidence of diabetic retinopathy in people with Type 2 diabetes mellitusattending the diabetic retinopathy screening service for Wales: retrospectiveanalysis. BMJ 344, e874.
Togashi, M., Yanada, H., Iwasaki, N., et al., 2000. Selective loss of pancreatic B-cellsin a diabetic patient with a mitochondrial 3243 mutation. J. Jpn. Diabet. Soc. 43,455–458.
Träff, J., Holme, E., Ekbom, K., Nilsson, B.Y., 1995. Ekbom’s syndrome ofphotomyoclonus, cerebellar ataxia and cervical lipoma is associated with thetRNALys A8344G mutation in mitochondrial DNA. Acta Neurol. Scand. 92, 394–397.
Tsukuda, K., Suzuki, Y., Kameoka, K., Osawa, N., Goto, Y.-I., Katagiri, H., et al., 1997.Screening of patients with maternally transmitted diabetes for mitochondrialgene mutations in the tRNALeu(UUR) region. Diabet. Med. 14, 1032–1037.
Tuppen, H.A., Blakely, E.L., Turnbull, D.M., Taylor, R.W., 2010. Mitochondrial DNAmutations and human disease. Biochim. Biophys. Acta 1797, 113–128.
Uchigata, M., Mizota, M., Yangisawa, Y., Nakagawa, Y., Otani, T., Ikegami, H., et al.,1996. Large-scale study of an A-to-G transition at position 3243 of themitochondrial gene and IDDM in Japanese patients. Diabetologia 39, 245–246.
Uimonen, S., Moilanen, J.S., Sorri, M., Hassinen, I.E., Majamaa, K., 2001. Hearingimpairment in patients with 3243A > G mtDNA mutation: phenotype and rateof progression. Hum. Genet. 108, 284–289.
van den Ouweland, J., Lemkes, H., Ruitenbeek, W., Sandkujl, L., de Vijlder, M.,Struyvenberg, P., et al., 1992. Mutation in mitochondrial tRNALeu(UUR) gene in alarge pedigree with maternally transmitted Type 2 diabetes and deafness. Nat.Genet. 1, 368–371.
van Essen, E., Roep, B., t’Hart, L., Jansen, J., van den Ouweland, J., Lemkes, H., et al.,2000. HLA-DQ polymorphism and degree of heteroplasmy of the A3243Gmitochondrial DNA mutation in maternally inherited diabetes and deafness.Diabet. Med. 17, 841–847.
Velho, G., Byrne, M.M., Clement, K., Sturis, J., Pueyo, M.E., Blanche, H., et al., 1996.Clinical phenotypes, insulin secretion, and insulin sensitivity in kindreds withmaternally inherited diabetes and deafness due to mitochondrial tRNALeu(UUR)
gene mutation. Diabetes 45, 478–487.Verny, C., Amati-Bonneau, P., Letournel, F., Person, B., Dib, N., Malinge, M.C., et al.,
2008. Mitochondrial DNA A3243G mutation involved in familial diabetes,chronic intestinal pseudo-obstruction and recurrent pancreatitis. Diabet.Metab. 34, 620–626.
Vialettes, B., Paquis-Fluckinger, V., Pelissier, J.-F., Bendahan, D., Narbonne, H.,Silvestre-Aillaud, P., et al., 1997. Phenotypic expression of diabetes secondary toa T14709C mutation of mitochondrial DNA. Comparison with MIDD syndrome(A3243G mutation): a case report. Diabet. Care 20, 1731–1737.
10 A.M. Schaefer et al. / Molecular and Cellular Endocrinology 379 (2013) 2–11

Vionnet, N., Passa, P., Froguel, P., 1993. Prevalence of mitochondrial gene mutationsin families with diabetes mellitus. Lancet 342, 1429–1430.
Wai, T., Teoli, D., Shoubridge, E.A., 2008. The mitochondrial DNA genetic bottleneckresults from replication of a subpopulation of genomes. Nat. Genet. 40, 1484–1488.
Walker, M., Taylor, R.W., Stewart, M., Bindoff, L.A., Shearing, P., Anyaoka, V., et al.,1995a. Insulin and proinsulin secretion in subjects with abnormal glucosetolerance and a mitochondrial tRNALeu(UUR) mutation. Diabet. Care 18, 1507–1509.
Walker, M., Taylor, R.W., Stewart, M., Bindoff, L., Jackson, M., Alberti, K.G., et al.,1995b. Insulin sensitivity and mitochondrial gene mutation. Diabet. Care 18,273–275.
Wallace, D.C., Singh, G., Lott, M.T., Hodge, J.A., Schurr, T.G., Lezza, A.M., et al., 1988.Mitochondrial DNA mutation associated with Leber’s hereditary opticneuropathy. Science 242, 1427–1430.
Whittaker, R.G., Schaefer, A.M., McFarland, R., Taylor, R.W., Walker, M., Turnbull,D.M., 2007. Prevalence and progression of diabetes in mitochondrial disease.Diabetologia 50, 2085–2089.
Whittaker, R.G., Blackwood, J.K., Alston, C., Blakely, E.L., Elson, J.L., McFarland, R.,et al., 2009. Urine heteroplasmy level is the best predictor of clinical outcome inpatients with the m.3243A > G mtDNA mutation. Neurology 72, 568–569.
Wilichowski, E., Grüters, A., Kruse, K., Rating, D., Beetz, R., Korenke, G.C., et al., 1997.Hypoparathyroidism and deafness associated with pleioplasmic large scalerearrangements of the mitochondrial DNA: a clinical and molecular geneticstudy of four children with Kearns-Sayre syndrome. Pediatr. Res. 41, 193–200.
Williams, T.B., Daniels, M., Puthenveetil, G., Chang, R., Wang, R.Y., Abdenur, J.E.,2012. Pearson syndrome: unique endocrine manifestations including neonataldiabetes and adrenal insufficiency. Mol. Genet. Metab. 106, 104–107.
Wolny, S., McFarland, R., Chinnery, P., Cheetham, T., 2009. Abnormal growth inmitochondrial disease. Acta Paediatr. 98, 553–554.
Ylikallio, E., Suomalainen, A., 2012. Mechanisms of mitochondrial diseases. Ann.Med. 44, 41–59.
Yorifuji, T., Kawai, M., Momoi, T., Sasaki, H., Furusho, K., Muroi, J., et al., 1996.Nephropathy and growth hormone deficiency in a patient with mitochondrialtRNALeu(UUR) mutation. J. Med. Genet. 33, 621–622.
Yu-Wai-Man, P., Griffiths, P.G., Gorman, G.S., Lourenco, C.M., Wright, A.F., Auer-Grumbach, M., et al., 2010. Multi-system neurological disease is common inpatients with OPA1 mutations. Brain 133, 771–786.
A.M. Schaefer et al. / Molecular and Cellular Endocrinology 379 (2013) 2–11 11

Mitochondrial function and insulin secretion
Pierre Maechler ⇑
Department of Cell Physiology and Metabolism, Geneva University Medical Centre, 1 rue Michel-Servet, 1211 Geneva 4, Switzerland
a r t i c l e i n f o
Article history:Available online 20 June 2013
Keywords:b-cellPancreatic isletsInsulin secretionMitochondriaDiabetes
a b s t r a c t
In the endocrine fraction of the pancreas, the b-cell rapidly reacts to fluctuations in blood glucose concen-trations by adjusting the rate of insulin secretion. Glucose-sensing coupled to insulin exocytosis dependson transduction of metabolic signals into intracellular messengers recognized by the secretory machin-ery. Mitochondria play a central role in this process by connecting glucose metabolism to insulin release.Mitochondrial activity is primarily regulated by metabolic fluxes, but also by dynamic morphologychanges and free Ca2+ concentrations. Recent advances of mitochondrial Ca2+ homeostasis are discussed;in particular the roles of the newly-identified mitochondrial Ca2+ uniporter MCU and its regulatory part-ner MICU1, as well as the mitochondrial Na+–Ca2+ exchanger. This review describes how mitochondriafunction both as sensors and generators of metabolic signals; such as NADPH, long chain acyl-CoA, glu-tamate. The coupling factors are additive to the Ca2+ signal and participate to the amplifying pathway ofglucose-stimulated insulin secretion.
! 2013 Elsevier Ireland Ltd. All rights reserved.
1. Introduction
1.1. The pancreatic b-cell
Glucose homeostasis depends on optimal regulation of insulinsecretion from the b-cells and the action of insulin on its target tis-sues; in particular muscles, liver, and adipose tissue. The b-cells arelocated in the endocrine fraction of the pancreas, i.e., the islets ofLangerhans. In humans, b-cells constitute about 70% of the isletsof Langerhans, which are spread throughout the pancreas andcompose 1–2% of this organ (Rahier et al., 1983). It means thatamong the 1013–1014 of cells composing our body, the 109 b-cellscontribute to less than 0.01% of this count. In other words, one sin-gle drop of blood contains as much red blood cells as our wholebody contains b-cells. Nevertheless, this minute amount of endo-crine tissue is essential for life since there is no alternative hor-mone to insulin, as dramatically illustrated by patients sufferingfrom type 1 diabetes. The cytoplasm of each b-cell contains about13,000 secretory granules filled with crystallized insulin (Dean,1973). During glucose stimulation only a small proportion of thegranule pool undergoes exocytosis.
1.2. Diabetes and the b-cell
The initial stages of type 1 diabetes, before b-cell destruction,are characterized by defects in the function of b-cells (O’Sullivan-Murphy and Urano, 2012). The large majority of diabetic patients
are classified as type 2 diabetes, or non-insulin dependent diabetesmellitus. The patients display dysregulation of insulin secretion, of-ten combined with insulin resistance of target tissues. The aetiol-ogy of type 2 diabetes is still poorly understood and has beenelucidated in only a limited number of subtypes. Among these,maturity onset diabetes of the young (MODY) and mitochondrialdiabetes have been linked to specific gene mutations and primaryb-cell dysfunction (Froguel et al., 1993; Byrne et al., 1996; Clocquetet al., 2000; Maassen et al., 2004). The impact of such mutations onthe b-cell highlights the importance of the mitochondria in thecontrol of insulin secretion. Other endocrine tissues play an impor-tant role in metabolic dysregulation and the reader is referred tothe other articles of this special issue of Molecular and CellularEndocrinology for corresponding information.
1.3. Metabolic activation of the b-cell
Both the secretion and the action of insulin contribute to glu-cose homeostasis. Regulated insulin release requires tight couplingin the b-cell between glucose metabolism and insulin secretory re-sponse. The exocytotic process is closely controlled by signals gen-erated by nutrient metabolism (Fig. 1), as well as byneurotransmitters and circulating hormones (Huypens et al.,2000; Schuit et al., 2001; Rubi and Maechler, 2010). The b-cell rap-idly reacts to fluctuations in the blood glucose concentration byadjusting the rate of insulin secretion. This review describes themolecular basis of metabolism–secretion coupling. In particular,it will be discussed how mitochondria function both as sensorsand generators of metabolic signals.
0303-7207/$ - see front matter ! 2013 Elsevier Ireland Ltd. All rights reserved.http://dx.doi.org/10.1016/j.mce.2013.06.019
⇑ Tel.: +41 22 379 55 54.E-mail address: [email protected]
Molecular and Cellular Endocrinology 379 (2013) 12–18
Contents lists available at SciVerse ScienceDirect
Molecular and Cellular Endocrinology
journal homepage: www.elsevier .com/locate /mce

2. Overview of metabolism–secretion coupling in b-cells
2.1. Pathways upstream of mitochondria
In b-cells, metabolism–secretion coupling refers to both theconsensus model and the contribution of additional coupling fac-tors, i.e., the trigger and amplifying pathways of glucose-stimu-lated insulin secretion (Fig. 1). This process is initiated by thepassive entry of glucose within the b-cell across the plasma mem-brane through GLUT2 and its subsequent phosphorylation by glu-cokinase, thereby promoting glycolysis (Iynedjian, 2009). In thecytosolic compartment, glycolysis extracts reducing equivalentstransmitted to NADH. Maintenance of glycolytic flux requires reox-idation of NADH to NAD+ to avoid arrest of glycolysis.
In most tissues, cytosolic conversion of pyruvate to lactate bythe lactate dehydrogenase ensures NADH oxidation to NAD+, whilein b-cells this task is devoted mainly to mitochondrial NADH shut-tles, transferring glycolysis-derived electrons to mitochondria.
2.2. The mitochondrial NADH shuttle system
The mitochondrial NADH shuttle system is composed of theglycerolphosphate and the malate/aspartate shuttles (MacDonald,1982), with its respective key members the mitochondrial glycerolphosphate dehydrogenase (mGPDH) and the aspartate–glutamatecarrier (AGC). The aspartate–glutamate carrier 1 (AGC1, alsonamed Aralar1) is a Ca2+-sensitive member of the malate/aspartateshuttle (del Arco and Satrustegui, 1998). Overexpression of AGC1increases glucose-induced mitochondrial activation and secretoryresponse, both in insulinoma INS-1E cells and rat islets (Rubiet al., 2004). This is accompanied by enhanced glucose oxidationand reduced lactate production. In insulinoma INS-1E b-cells, themirror experiment consisting in silencing AGC1 reduces glucoseoxidation and the secretory response, although primary rat b-cellsare not sensitive to such a manoeuvre (Casimir et al., 2009). There-fore, aspartate–glutamate carrier capacity appears to set a limit forNADH shuttle function and mitochondrial metabolism, exhibitingcell type-specific dependence. The importance of the NADH shuttle
system illustrates the tight coupling between glycolysis and mito-chondrial activation in b-cells, optimizing transfer of pyruvate intomitochondria through the recently identified mitochondrial pyru-vate carrier (Herzig et al., 2012). Subsequently, catabolism of glu-cose-derived pyruvate induces mitochondrial activation resultingin ATP generation. Although mitochondria, and the Krebs cycle inparticular, also oxidize fatty acids and amino acids, carbohydratesare the most important fuel under physiological conditions for theb-cell.
2.3. Pathways downstream of mitochondria
Export of ATP to the cytosolic compartment promotes the clo-sure of ATP-sensitive K+-channels (KATP-channel) on the plasmamembrane and, as a consequence, depolarization of the cell (Ash-croft, 2006). This leads to Ca2+ influx through voltage-gated Ca2+
channels and a rise in cytosolic Ca2+ concentrations (Fig. 1), whichis the main and necessary signal for exocytosis of insulin (Eliassonet al., 2008). Additional signals are required to sustain the secretionelicited by glucose-induced Ca2+ rise. They participate in the ampli-fying pathway (Maechler et al., 2006), formerly referred to as theKATP-channel independent stimulation of insulin secretion. Effi-cient coupling of glucose recognition to insulin secretion is ensuredby the mitochondrion, an organelle that integrates and generatesmetabolic signals (Maechler et al., 2006). This role is additive tothe generation of ATP necessary for the elevation of cytosolicCa2+. The list of additive factors proposed to amplify the Ca2+ sig-nals comprises cAMP, NADPH, long chain acyl-CoA derivatives, glu-tamate, and superoxides. As opposed to the recognized primaryrole of Ca2+ as a necessary signal, the roles of most of these additivefactors are still under debate.
3. Metabolic activation of mitochondria
3.1. Activation of the Krebs cycle
Pyruvate entry within the mitochondria induces metabolic acti-vation of this organelle. There, pyruvate either loses one carbon to
Fig. 1. Model for coupling of glucose metabolism to insulin secretion in the b-cell. Glucose equilibrates across the plasma membrane and is phosphorylated by glucokinase(GK). Further, glycolysis produces pyruvate, which preferentially enters the mitochondria and is metabolized by the TCA cycle. The TCA cycle generates reducing equivalentstransferred by NADH and FADH2 to the electron transport chain (ETC), leading to hyperpolarization of the mitochondrial membrane (Dwm) and generation of ATP. ATP is thentransferred to the cytosol, raising the ATP/ADP ratio. Subsequently, closure of KATP-channels depolarizes the cell membrane (Dwc). This opens voltage-dependent Ca2+
channels, increasing cytosolic Ca2+ concentration ([Ca2+]c), which triggers insulin exocytosis. The amplifying pathway of metabolism–secretion coupling is contributed byadditive coupling factors.
P. Maechler / Molecular and Cellular Endocrinology 379 (2013) 12–18 13

generate acetyl-CoA or gains one carbon to form oxaloacetate;reactions catalyzed by pyruvate dehydrogenase (PDH) and pyru-vate carboxylase (PC), respectively (Fig. 2). PDH is an importantsite of regulation as, among other effectors, the enzyme is activatedby an elevation of mitochondrial [Ca2+] (Duchen, 1999; Rutteret al., 1996). PDH is also regulated by reversible phosphorylationof its E1a subunit, activity of the PDH kinases inhibiting the en-zyme (Sugden and Holness, 2003). Increasing the expression ofeither the PDH phosphatase or the PDH kinase 3 does not changeglucose-stimulated insulin secretion (Nicholls, 2002). Regardingdown-regulation of PDH kinases, silencing of PDH kinase 1 inINS-1 832/13 cells has been reported to increase the secretory re-sponse to glucose (Krus et al., 2010), whereas knockdown of bothPDH kinase 1 and kinase 3 in INS-1E cells does not affect metabo-lism–secretion coupling (Akhmedov et al., 2012). Therefore, theimportance of the phosphorylation state of PDH for the regulationof b-cell function remains unclear.
Condensation of the 2-carbon acetyl group carried by coen-zyme-A with the 4-carbon oxaloacetate yields citrate, thereby acti-vating the tricarboxylic acid (TCA) cycle (or Krebs cycle). Thepyruvate carboxylase enzyme ensures the provision of carbon skel-eton (i.e., anaplerosis) to the TCA cycle, a key pathway in b-cells(Fransson et al., 2006). The remarkably high anaplerotic activityin b-cells indicates important loss of TCA cycle intermediates(i.e., cataplerosis), which is compensated for by de novo oxaloace-tate synthesis by pyruvate carboxylation. In the control of glu-cose-stimulated insulin secretion, TCA cycle intermediates arerecruited to serve as substrates leading to the formation of mito-chondrion-derived coupling factors (Maechler et al., 2006).
Through its oxidative activity, the TCA cycle extracts reducingequivalents from metabolic intermediates, which are then trans-ported mainly by NADH and, quantitatively less important, byFADH2. In order to maintain input of pyruvate products into theTCA cycle upon glucose stimulation, this reduced redox state re-quires continues reoxidation of mitochondrial NADH to NAD+. Thisis achieved primarily by complex I NADH dehydrogenase on the
electron transport chain. However, as complex I activity is limitedby the inherent thermodynamic constraints of proton gradient for-mation, excess of NADH contributed by the high TCA cycle activitymust be reoxidized by alternative dehydrogenases, i.e., throughcataplerotic reactions.
3.2. Activation of the electron transport chain
TCA cycle activation induces transfer of reducing equivalents tothe electron transport chain resulting in hyperpolarization of themitochondrial membrane, respiration, and generation of ATP(Fig. 2). Electron transport chain activity promotes proton exportfrom the mitochondrial matrix across the inner membrane, estab-lishing a strong mitochondrial membrane potential, which is neg-ative on the inside. The respiratory chain comprises fivecomplexes, the subunits of which are encoded by both the nuclearand mitochondrial genomes (Wallace, 1999). Complex I is theacceptor of electrons from NADH in the inner mitochondrial mem-brane and complex II (succinate dehydrogenase) transfers elec-trons to coenzyme-Q from FADH2, the latter being generatedboth by the oxidative activity of the TCA cycle and the glycerol-phosphate shuttle. Complex V (ATP synthase) promotes ATP for-mation from ADP and inorganic phosphate. The synthesized ATPis translocated to the cytosol in exchange for ADP by the adeninenucleotide translocator (ANT). Thus, the actions of the separatecomplexes of the electron transport chain and the adenine nucleo-tide translocator couple respiration to ATP supply.
3.3. Regulation of mitochondrial activity by Ca2+
Mitochondrial activity can be modulated according to the nat-ure of the nutrients, although glucose is the chief secretagogue ascompared to amino acid catabolism (Newsholme et al., 2005) andfatty acid b-oxidation (Rubi et al., 2002). Additional factors regulat-ing mitochondrial activation include mitochondrial Ca2+ concen-trations ([Ca2+]m) (Duchen, 1999; McCormack et al., 1990),
Fig. 2. In the mitochondria, pyruvate (Pyr) is a substrate both for pyruvate dehydrogenase (PDH) and pyruvate carboxylase (PC), forming respectively acetyl-CoA andoxaloacetate (OA). Condensation acetyl-CoA with OA generates citrate that is either processed by the TCA cycle or exported out of the mitochondrion as a precursor for longchain acyl-CoA (LC-CoA) synthesis. The glycerophosphate and malate/aspartate shuttles, as well as the TCA cycle, generate reducing equivalents in the form of NADH andFADH2, which are transferred to the electron transport chain (ETC). This leads to the hyperpolarization of the mitochondrial membrane (wm) and the synthesis of ATP, thentransported to the cytosol by the adenine nucleotide translocator (ANT). Upon glucose stimulation, glutamate (Glut) is produced from a-ketoglutarate (aKG) by glutamatedehydrogenase (GDH) and exported out of mitochondria through the glutamate carrier (GC1). Ca2+ enters into mitochondria via MCU (regulated by MICU1) and gets out viaNCLX.
14 P. Maechler / Molecular and Cellular Endocrinology 379 (2013) 12–18

mitochondrial protein tyrosine phosphatase (Pagliarini et al.,2005), mitochondrial GTP (Kibbey et al., 2007), and matrix alkalin-ization (Wiederkehr et al., 2009). Among these factors, mitochon-drial Ca2+ regulation has recently been highlighted, thanks to aseries of discoveries related to Ca2+ transport through the mito-chondrial membrane. Elevation of [Ca2+]m enhances mitochondrialoxidative activity (Maechler et al., 1998) and promotes generationof coupling factors for insulin exocytosis (Maechler et al., 1997).Conversely, buffering mitochondrial free Ca2+ limits [Ca2+]m peaksinduced by glucose stimulation in INS-1E b-cells. Such limitationin [Ca2+]m amplitude reduces mitochondrial respiration and ATPgeneration with corresponding effects on insulin secretion (Wie-derkehr et al., 2011).
In the recent years, significant advances in mitochondrial Ca2+
channels have been made. In 2011, the mitochondrial Ca2+ uni-porter (MCU) has been identified as the channel responsible formitochondrial Ca2+ uptake (Baughman et al., 2011; De Stefaniet al., 2011). MCU is part of a complex located in the inner mito-chondrial membrane and its activity is modulated by another re-cently identified protein, the mitochondrial Ca2+ uptake 1(MICU1). MICU1 holds Ca2+ sensing subunits, in other words twocanonical EF hands, which are essential for its activity (Perocchiet al., 2010). If Ca2+ gets in mitochondria, it should also get out atsome point, although the vast majority of mitochondrial Ca2+ isbuffered as chelated ion. Mitochondrial Ca2+ efflux is thought tobe mediated by the Na2+/Ca2+ exchanger (NCLX) identified in2010 (Palty et al., 2010). Therefore, MCU and MICU1 would beimplicated in mitochondrial Ca2+ uptake, whereas NCLX would beresponsible for Ca2+ efflux (Fig. 2).
In pancreatic b-cells, silencing of NCLX extends elevations of[Ca2+]m evoked by cell depolarization and also accelerates the risein ATP/ADP ratio in response to glucose stimulation (Tarasov et al.,2012). Consistently, the rise in [Ca2+]m evoked by glucose is en-hanced in b-cells when NCLX is silenced or expressed in a domi-nant negative form (Nita et al., 2012). These recent data are inagreement with a previous study showing increased mitochondrialmetabolism and enhanced glucose-stimulated insulin secretionwhen the Na2+/Ca2+ exchanger was pharmacologically inhibitedby CGP37157 (Lee et al., 2003). Regarding the role of NCLX inATP production, the inhibitor CGP37157 increases glucose-inducedATP generation, whereas knockdown of NCLX using siRNA does not(Nita et al., 2012), suggesting additional effects of CGP37157.
Ca2+ import into mitochondria is regulated by the recently iden-tified MCU (Baughman et al., 2011; De Stefani et al., 2011) andMICU1 (Perocchi et al., 2010). Silencing of MCU in b-cells impairsthe rise in [Ca2+]m evoked by cell depolarization and reduces theplateau phase of ATP/ADP ratio upon glucose stimulation (Tarasovet al., 2012). Accordingly, knockdown of MCU in mouse b-cellsinhibits glucose-induced exocytosis (Tarasov et al., 2013). Suchmanipulation of [Ca2+]m does not affect mitochondrial membranepotential, either at basal or stimulatory glucose concentrations(Tarasov et al., 2012). Regarding MICU1, its silencing in insulinomacells reduces mitochondrial Ca2+ uptake, ATP levels, and insulinsecretion upon glucose stimulation (Alam et al., 2012). In the samestudy, knockdown of MCU provoked similar inhibitory effects(Alam et al., 2012). Collectively, these recent findings indicate thatboth the channel and its regulatory partner, i.e., MCU and MICU1respectively, are necessary for proper regulation of [Ca2+]m in b-cells and participate to glucose-stimulated insulin secretion.
3.4. Regulation of mitochondrial dynamics
Mitochondrial activation also involves changes in organellemorphology and contacts, in particular with the Ca2+-rich endo-plasmic reticulum (de Brito and Scorrano, 2010). Mitochondriaform dynamic networks, continuously modified by fission and
fusion events under the control of specific mitochondrial mem-brane anchor proteins (Westermann, 2008). Over the last years,mitochondrial fission/fusion state was investigated in insulinsecreting cells. Altering fission by down regulation of fission-pro-moting Fis1 protein impairs respiratory function and glucose-stim-ulated insulin secretion (Twig et al., 2008). Intriguingly, a similarphenotype, i.e., reduced energy metabolism and secretory defects,is caused by the mirror experiment consisting in mitochondrialfragmentation by overexpression of Fis1 (Park et al., 2008). Addingpuzzlement to our comprehension of mitochondrial dynamics in b-cell function, fragmented pattern obtained by dominant-negativeexpression of fusion-promoting Mfn1 protein does not affectmetabolism–secretion coupling (Park et al., 2008). Recently, itwas reported that glucose stimulation of INS-1E cells inducesreversible shortening of mitochondrial tubules (Jhun et al., 2013).Expression of a dominant-negative mutant of fission-promotingDrp1 prevents glucose-induced mitochondria shortening and insu-lin secretion (Jhun et al., 2013). Therefore, mitochondrial fragmen-tation per se seems not to alter insulin secreting cells, at least notin vitro. Regarding Ca2+ homeostasis, mitochondrial fragmentationin mouse b-cells lacking prohibitin-2 is associated with bluntedglucose-induced Ca2+ rise but preserved KCl response; indicatingthat ATP generation rather than Ca2+ channels is defective in thesecells (S. Supale and P. Maechler, unpublished observation). In vivo,transgenic mice with b-cell-specific ablation of fusion-promotingOpa1 are hyperglycaemic. Islets from these mice exhibit disman-tled mitochondrial architecture, reduced ATP generation and insu-lin release (Zhang et al., 2011). Additionally, b-cell proliferation isreduced in b-cell-specific Opa1-deficient mice (Zhang et al., 2011).
4. Mitochondria as the source of additional coupling factors forinsulin exocytosis
4.1. Mitochondria as a source of coupling factors
Glucose metabolism induces the triggering and the amplifyingpathways, in other words the necessary Ca2+ rise and generationof additional coupling factors, respectively (Henquin, 2000). Theamplifying pathway can be experimentally uncovered when glu-cose stimulation occurs whilst cytosolic Ca2+ is clamped at permis-sive levels (Gembal et al., 1992). This suggests the existence ofmetabolic coupling factors, generated by glucose, participating tothe amplifying pathway. Mitochondria have been identified as asource of additional coupling factors for insulin exocytosis. For in-stance, the demonstration has been done using permeabilizedinsulin-secreting cells clamped with permissive Ca2+ concentra-tions and stimulated with mitochondrial substrates (Maechleret al., 1997).
4.2. Mitochondria as a source of nucleotides serving as coupling factors
ATP is undoubtedly the primary metabolic factor produced bymitochondria during glucose-stimulated insulin secretion. ATPcloses the KATP-channel leading to the obligatory Ca2+ elevationpromoting insulin exocytosis (Miki et al., 1999). Moreover, ATP isimplicated in secretory granule movement (Yu et al., 2000; Varadiet al., 2002), priming of the granules prior to exocytosis (Eliassonet al., 1997), and in the process of insulin exocytosis per se (Vallaret al., 1987; Rorsman et al., 2000).
The purine nucleoside GTP is also implicated to some extent inthe process of metabolism–secretion coupling. In the cytosol, GTPis mainly generated through the action of nucleoside diphosphatekinase from ATP-dependent phosphorylation of GDP. Glucose stim-ulation raises GTP levels (Detimary et al., 1996), promoting insulinexocytosis via the activity of GTPases (Vallar et al., 1987). In
P. Maechler / Molecular and Cellular Endocrinology 379 (2013) 12–18 15

mitochondria, GTP acts as a positive regulator of the TCA cycle(Kibbey et al., 2007).
NADH and its phosphorylated form NADPH are responsible fortransfer of reducing equivalents in biochemical pathways. NADPHis mostly found in the cytosolic compartment, whilst NADH is par-ticularly abundant in mitochondria. Glucose stimulation modifiesthe redox state of these pyridine nucleotides, raising theNAD(P)H/NAD(P)+ ratio (Capito et al., 1984), first in the cytosoland then in mitochondria (Patterson et al., 2000). Consistent withthe model of metabolism–secretion coupling, increase in NAD(P)Hprecedes the elevation in cytosolic Ca2+ concentrations (Pralonget al., 1990). Beside the rapid changes in NAD(P)H/NAD(P)+ ratio,the total pool of NADPH is elevated upon glucose stimulationthrough the phosphorylating activity of NAD-kinase (Gray et al.,2012).
Cytosolic NADPH is generated by glucose metabolism via thepentose phosphate shunt (Verspohl et al., 1979), although in b-cells mitochondrial shuttles appear to play an important role inthis process (Farfari et al., 2000). The export of citrate out of themitochondria might serve as a signal of fuel abundance, participat-ing in metabolism–secretion coupling (Farfari et al., 2000). Once inthe cytosolic compartment, citrate metabolism contributes to theformation of NADPH and malonyl-CoA, both candidate moleculeson the list of metabolic coupling factors.
NADPH has been proposed as a coupling factor in glucose-stim-ulated insulin secretion, originally by using toadfish islets (Watkinset al., 1968) indicating a direct effect of NADPH on the release ofinsulin (Watkins, 1972) secondary to the uptake of NADPH bygranules (Watkins and Moore, 1977). Subsequently, the role ofNADPH as a coupling factor has been substantiated by experimentsshowing direct stimulation of insulin exocytosis upon intracellularaddition of NADPH (Ivarsson et al., 2005). It has also been reportedthat the NADPH/NADP+ ratio mediates a fast-inactivating K+ cur-rent through regulation of Kv2.1 channels (MacDonald et al., 2003).
Finally, the second messenger cAMP robustly potentiates glu-cose-stimulated insulin secretion (Ahren, 2000). Glucose stimula-tion can promote elevation of cAMP (Charles et al., 1975) that isgenerated by adenylyl cyclase at the plasma membrane usingATP. The cAMP levels are negatively modulated by superoxide, aneffect mediated by NADPH oxidases (Li et al., 2012). In particular,the glucose response of islets deficient in NOX2 is characterizedby lower superoxide, higher cAMP levels, and increased insulinsecretion (Li et al., 2012). Among other hormones, glucagon andGLP-1 (glucagon-like peptide 1) increase cAMP concentrations inb-cells (Schuit et al., 2001), resulting in the amplification of thesecretory response to glucose in human islets (Huypens et al.,2000). In addition to its effects on insulin release, GLP-1 might pre-serve b-cell mass, rendering this hormone and biologically activerelated molecules of interest for the treatment of diabetes (Druckerand Nauck, 2006).
4.3. Mitochondria as a source of precursors for fatty acids serving ascoupling factors
The relative contribution of glucose versus lipid products foroxidative catabolism shapes the metabolic profile of mitochondria.The rate-limiting step for transport and oxidation of fatty acids intomitochondria is catalyzed by carnitine palmitoyltransferase (the li-ver isoform LCPTI in the b-cell). Upon glucose stimulation, citratederived from mitochondria reacts with coenzyme-A (CoA) to gen-erate cytosolic acetyl-CoA necessary for the synthesis malonyl-CoA and then long-chain acyl-CoA. The malonyl-CoA thus formedreduces fatty acid oxidation by inhibiting LCPTI. The hypothesisthat malonyl-CoA/long-chain acyl-CoA act as coupling factors inthe secretory response was originally based on the inhibition offatty acid oxidation by malonyl-CoA, which increases the availabil-
ity of lipid signals implicated in exocytosis (Brun et al., 1996). Inthe cytosol, this process promotes the accumulation of long chainacyl-CoAs such as palmitoyl-CoA (Liang and Matschinsky, 1991;Prentki et al., 1992), enhancing Ca2+-evoked insulin exocytosis(Deeney et al., 2000). Accordingly, LCPTI overexpression in INS-1E b-cells increases oxidation of fatty acids, whilst it reduces glu-cose-stimulated insulin secretion (Rubi et al., 2002). To date, theexact role of long chain acyl-CoA derivatives is still debated, sev-eral studies indicating that malonyl-CoA acts as a factor regulatingthe partitioning of fatty acids into effectors in insulin exocytosis(Prentki et al., 2002). Fatty acids derived from triglyceride storesmay also play a permissive role in the secretory response (Frigerioet al., 2010; Peyot et al., 2009).
4.4. Mitochondria as a source of glutamate serving as coupling factor
The observation of direct stimulation of insulin exocytosis bymitochondrial activation in permeabilized b-cells (Maechleret al., 1997) led to the identification of glutamate as a putativeintracellular messenger (Maechler and Wollheim, 1999; Hoyet al., 2002; Maechler et al., 2002). Collectively, work from our lab-oratory and others indicate that permissive levels of glutamate arenecessary for the full development of the secretory response toglucose stimulation. The cytosolic target of glutamate might bethe insulin granule itself, as several studies by different groupshave shown requirement of glutamate uptake by secretory vesiclesfor insulin exocytosis (Maechler and Wollheim, 1999; Hoy et al.,2002; Eto et al., 2003; Gammelsaeter et al., 2011; Storto et al.,2006).
If intracellular glutamate renders insulin granules exocytosis-competent, concentrations of this amino acid should raise in re-sponse to glucose stimulation. Indeed, during glucose stimulationtotal cellular glutamate levels have been shown to increase in hu-man, mouse and rat islets as well as in clonal b-cells (Maechler andWollheim, 1999; Rubi et al., 2001; Brennan et al., 2002; Bertrandet al., 2002; Broca et al., 2003; Carobbio et al., 2004; Lehtihetet al., 2005), When b-cells are forced to express an enzyme thatdecarboxylates intracellular glutamate, the glucose-induced gluta-mate rise is impaired as well as the secretory response (Rubi et al.,2001). The mitochondrial enzyme glutamate dehydrogenase(GDH), encoded by Glud1, plays a key role in glucose-induced glu-tamate generation (Fig. 2). Abrogation of GDH specifically in the b-cells of bGlud1!/! mice reduces the secretory response (Carobbioet al., 2009). Moreover, measurements of carbon fluxes in mouseislets revealed that, upon glucose stimulation, GDH contributesto the net synthesis of glutamate from the TCA cycle intermediatea-ketoglutarate (Vetterli et al., 2012). In b-cells lacking GDH, glu-cose-stimulated insulin secretion is reduced by half, correlatingwith impaired glutamate formation while the Ca2+ rise is preserved(Vetterli et al., 2012). Importantly, the amplifying pathway charac-terizing the full development of the glucose response fails to devel-op in the absence of GDH, as demonstrated in bGlud1!/! islets(Vetterli et al., 2012).
Regarding export of the newly synthesized glutamate out ofmitochondria, the glutamate carrier GC1 seems to play an impor-tant role. Silencing of GC1 reduces glucose-stimulated insulinsecretion, an effect rescued by the provision of exogenous gluta-mate to the b-cell (Casimir et al., 2009). Finally, prevention of glu-tamate release from b-cells results in concomitant elevations ofintracellular glutamate levels and glucose-evoked insulin secretion(Feldmann et al., 2011). Collectively, data indicate that permissivelevels of glutamate are required in the amplifying pathway of theb-cell. Permissive concentrations of glutamate are also importantfor proper function of the malate–aspartate shuttle, an key playerin insulin secreting cells (Rubi et al., 2004; Casimir et al, 2009),as discussed above.
16 P. Maechler / Molecular and Cellular Endocrinology 379 (2013) 12–18

5. Conclusion
In pancreatic b-cells, mitochondrial activity translates glucosemetabolism into signals controlling the rate of insulin exocytosis.Consequently, mitochondrial function can adjust insulin secretionto the actual glycemia. This role is specific for b-cells, since in mostcell types mitochondrial metabolism is triggered by specific needsof the cells, in terms of energy and building blocks. In b-cells, mito-chondrial metabolism is primarily dictated by the glycolytic flux.The concept of metabolism–secretion coupling that characterizesthe b-cell is tightly controlled by on and off signals, most of themrequiring mitochondrial function. Future studies should better de-fine the molecular targets and mechanism of action of couplingfactors controlling insulin secretion.
Acknowledgments
The author’s laboratory benefits from continuous support bythe Swiss National Science Foundation and the State of Geneva.The most precious contribution of present and past members ofthe laboratory is acknowledged.
References
Ahren, B., 2000. Autonomic regulation of islet hormone secretion–implications forhealth and disease. Diabetologia 43, 393–410.
Akhmedov, D., De Marchi, U., Wollheim, C.B., Wiederkehr, A., 2012. Pyruvatedehydrogenase E1alpha phosphorylation is induced by glucose but does notcontrol metabolism–secretion coupling in INS-1E clonal beta-cells. Biochim.Biophys. Acta 1823, 1815–1824.
Alam, M.R., Groschner, L.N., Parichatikanond, W., Kuo, L., Bondarenko, A.I., Rost, R.,Waldeck-Weiermair, M., Malli, R., Graier, W.F., 2012. Mitochondrial Ca2+ uptake1 (MICU1) and mitochondrial Ca2+ uniporter (MCU) contribute to metabolism–secretion coupling in clonal pancreatic beta-cells. J. Biol. Chem. 287, 34445–34454.
Ashcroft, F.M., 2006. K(ATP) channels and insulin secretion: a key role in health anddisease. Biochem. Soc. Trans. 34, 243–246.
Baughman, J.M., Perocchi, F., Girgis, H.S., Plovanich, M., Belcher-Timme, C.A., Sancak,Y., Bao, X.R., Strittmatter, L., Goldberger, O., Bogorad, R.L., Koteliansky, V.,Mootha, V.K., 2011. Integrative genomics identifies MCU as an essentialcomponent of the mitochondrial calcium uniporter. Nature 476, 341–345.
Bertrand, G., Ishiyama, N., Nenquin, M., Ravier, M.A., Henquin, J.C., 2002. Theelevation of glutamate content and the amplification of insulin secretion inglucose-stimulated pancreatic islets are not causally related. J. Biol. Chem. 277,32883–32891.
Brennan, L., Shine, A., Hewage, C., Malthouse, J.P., Brindle, K.M., McClenaghan, N.,Flatt, P.R., Newsholme, P., 2002. A nuclear magnetic resonance-baseddemonstration of substantial oxidative L-alanine metabolism and L-alanine-enhanced glucose metabolism in a clonal pancreatic beta-cell line: metabolismof L-alanine is important to the regulation of insulin secretion. Diabetes 51,1714–1721.
Broca, C., Brennan, L., Petit, P., Newsholme, P., Maechler, P., 2003. Mitochondria-derived glutamate at the interplay between branched-chain amino acid andglucose-induced insulin secretion. FEBS Lett. 545, 167–172.
Brun, T., Roche, E., Assimacopoulos-Jeannet, F., Corkey, B.E., Kim, K.H., Prentki, M.,1996. Evidence for an anaplerotic/malonyl-CoA pathway in pancreatic beta-cellnutrient signaling. Diabetes 45, 190–198.
Byrne, M.M., Sturis, J., Menzel, S., Yamagata, K., Fajans, S.S., Dronsfield, M.J., Bain,S.C., Hattersley, A.T., Velho, G., Froguel, P., Bell, G.I., Polonsky, K.S., 1996. Alteredinsulin secretory responses to glucose in diabetic and nondiabetic subjects withmutations in the diabetes susceptibility gene MODY3 on chromosome 12.Diabetes 45, 1503–1510.
Capito, K., Hedeskov, C.J., Landt, J., Thams, P., 1984. Pancreatic islet metabolism andredox state during stimulation of insulin secretion with glucose and fructose.Acta Diabetol. Lat. 21, 365–374.
Carobbio, S., Ishihara, H., Fernandez-Pascual, S., Bartley, C., Martin-Del-Rio, R.,Maechler, P., 2004. Insulin secretion profiles are modified by overexpression ofglutamate dehydrogenase in pancreatic islets. Diabetologia 47, 266–276.
Carobbio, S., Frigerio, F., Rubi, B., Vetterli, L., Bloksgaard, M., Gjinovci, A.,Pournourmohammadi, S., Herrera, P.L., Reith, W., Mandrup, S., Maechler, P.,2009. Deletion of glutamate dehydrogenase in beta-cells abolishes part of theinsulin secretory response not required for glucose homeostasis. J. Biol. Chem.284, 921–929.
Casimir, M., Rubi, B., Frigerio, F., Chaffard, G., Maechler, P., 2009. Silencing of themitochondrial NADH shuttle component aspartate–glutamate carrier AGC1/Aralar1 in INS-1E cells and rat islets. Biochem. J. 424, 459–466.
Casimir, M., Lasorsa, F.M., Rubi, B., Caille, D., Palmieri, F., Meda, P., Maechler, P.,2009. Mitochondrial glutamate carrier GC1 as a newly identified player in the
control of glucose-stimulated insulin secretion. J. Biol. Chem. 284, 25004–25014.
Charles, M.A., Lawecki, J., Pictet, R., Grodsky, G.M., 1975. Insulin secretion.Interrelationships of glucose, cyclic adenosine 3:5-monophosphate, andcalcium. J. Biol. Chem. 250, 6134–6140.
Clocquet, A.R., Egan, J.M., Stoffers, D.A., Muller, D.C., Wideman, L., Chin, G.A., Clarke,W.L., Hanks, J.B., Habener, J.F., Elahi, D., 2000. Impaired insulin secretion andincreased insulin sensitivity in familial maturity-onset diabetes of the young 4(insulin promoter factor 1 gene). Diabetes 49, 1856–1864.
de Brito, O.M., Scorrano, L., 2010. An intimate liaison: spatial organization of theendoplasmic reticulum-mitochondria relationship. EMBO J. 29, 2715–2723.
De Stefani, D., Raffaello, A., Teardo, E., Szabo, I., Rizzuto, R., 2011. A forty-kilodaltonprotein of the inner membrane is the mitochondrial calcium uniporter. Nature476, 336–340.
Dean, P.M., 1973. Ultrastructural morphometry of the pancreatic-cell. Diabetologia9, 115–119.
Deeney, J.T., Gromada, J., Hoy, M., Olsen, H.L., Rhodes, C.J., Prentki, M., Berggren, P.O.,Corkey, B.E., 2000. Acute stimulation with long chain acyl-CoA enhancesexocytosis in insulin-secreting cells (HIT T-15 and NMRI beta-cells). J. Biol.Chem. 275, 9363–9368.
del Arco, A., Satrustegui, J., 1998. Molecular cloning of Aralar, a new member of themitochondrial carrier superfamily that binds calcium and is present in humanmuscle and brain. J. Biol. Chem. 273, 23327–23334.
Detimary, P., Van den Berghe, G., Henquin, J.C., 1996. Concentration dependenceand time course of the effects of glucose on adenine and guanine nucleotides inmouse pancreatic islets. J. Biol. Chem. 271, 20559–20565.
Drucker, D.J., Nauck, M.A., 2006. The incretin system: glucagon-like peptide-1receptor agonists and dipeptidyl peptidase-4 inhibitors in type 2 diabetes.Lancet 368, 1696–1705.
Duchen, M.R., 1999. Contributions of mitochondria to animal physiology: fromhomeostatic sensor to calcium signalling and cell death. J. Physiol. 516, 1–17.
Eliasson, L., Renstrom, E., Ding, W.G., Proks, P., Rorsman, P., 1997. Rapid ATP-dependent priming of secretory granules precedes Ca(2+)-induced exocytosis inmouse pancreatic B-cells. J. Physiol. 503, 399–412.
Eliasson, L., Abdulkader, F., Braun, M., Galvanovskis, J., Hoppa, M.B., Rorsman, P.,2008. Novel aspects of the molecular mechanisms controlling insulin secretion.J. Physiol. 586, 3313–3324.
Eto, K., Yamashita, T., Hirose, K., Tsubamoto, Y., Ainscow, E.K., Rutter, G.A., Kimura,S., Noda, M., Iino, M., Kadowaki, T., 2003. Glucose metabolism and glutamateanalog acutely alkalinize pH of insulin secretory vesicles of pancreatic {beta}-cells. Am. J. Physiol. Endocrinol. Metab. 285, E262–E271.
Farfari, S., Schulz, V., Corkey, B., Prentki, M., 2000. Glucose-regulated anaplerosisand cataplerosis in pancreatic beta-cells: possible implication of a pyruvate/citrate shuttle in insulin secretion. Diabetes 49, 718–726.
Feldmann, N., Del Rio, R.M., Gjinovci, A., Tamarit-Rodriguez, J., Wollheim, C.B.,Wiederkehr, A., 2011. Reduction of plasma membrane glutamate transportpotentiates insulin but not glucagon secretion in pancreatic islet cells. Mol. CellEndocrinol. 338, 46–57.
Fransson, U., Rosengren, A.H., Schuit, F.C., Renstrom, E., Mulder, H., 2006.Anaplerosis via pyruvate carboxylase is required for the fuel-induced rise inthe ATP:ADP ratio in rat pancreatic islets. Diabetologia 49, 1578–1586.
Frigerio, F., Brun, T., Bartley, C., Usardi, A., Bosco, D., Ravnskjaer, K., Mandrup, S.,Maechler, P., 2010. Peroxisome proliferator-activated receptor alpha(PPARalpha) protects against oleate-induced INS-1E beta cell dysfunction bypreserving carbohydrate metabolism. Diabetologia 53, 331–340.
Froguel, P., Zouali, H., Vionnet, N., Velho, G., Vaxillaire, M., Sun, F., Lesage, S., Stoffel,M., Takeda, J., Passa, P., 1993. Familial hyperglycemia due to mutations inglucokinase. Definition of a subtype of diabetes mellitus. N. Engl. J. Med. 328,697–702.
Gammelsaeter, R., Coppola, T., Marcaggi, P., Storm-Mathisen, J., Chaudhry, F.A.,Attwell, D., Regazzi, R., Gundersen, V., 2011. A role for glutamate transporters inthe regulation of insulin secretion. PLoS One 6, e22960.
Gembal, M., Gilon, P., Henquin, J.C., 1992. Evidence that glucose can control insulinrelease independently from its action on ATP-sensitive K+ channels in mouse Bcells. J. Clin. Invest. 89, 1288–1295.
Gray, J.P., Alavian, K.N., Jonas, E.A., Heart, E.A., 2012. NAD kinase regulates the size ofthe NADPH pool and insulin secretion in pancreatic beta-cells. Am. J. Physiol.Endocrinol. Metab. 303, E191–E199.
Henquin, J.C., 2000. Triggering and amplifying pathways of regulation of insulinsecretion by glucose. Diabetes 49, 1751–1760.
Herzig, S., Raemy, E., Montessuit, S., Veuthey, J.L., Zamboni, N., Westermann, B.,Kunji, E.R., Martinou, J.C., 2012. Identification and functional expression of themitochondrial pyruvate carrier. Science 337, 93–96.
Hoy, M., Maechler, P., Efanov, A.M., Wollheim, C.B., Berggren, P.O., Gromada, J., 2002.Increase in cellular glutamate levels stimulates exocytosis in pancreatic beta-cells. FEBS Lett. 531, 199–203.
Huypens, P., Ling, Z., Pipeleers, D., Schuit, F., 2000. Glucagon receptors on humanislet cells contribute to glucose competence of insulin release. Diabetologia 43,1012–1019.
Ivarsson, R., Quintens, R., Dejonghe, S., Tsukamoto, K., In ‘t Veld, P., Renstrom, E.,Schuit, F.C., 2005. Redox control of exocytosis: regulatory role of NADPH,thioredoxin, and glutaredoxin. Diabetes 54, 2132–2142.
Iynedjian, P.B., 2009. Molecular physiology of mammalian glucokinase. Cell Mol.Life Sci. 66, 27–42.
Jhun, B.S., Lee, H., Jin, Z.G., Yoon, Y., 2013. Glucose stimulation induces dynamicchange of mitochondrial morphology to promote insulin secretion in theinsulinoma cell line INS-1E. PLoS One 8, e60810.
P. Maechler / Molecular and Cellular Endocrinology 379 (2013) 12–18 17

Kibbey, R.G., Pongratz, R.L., Romanelli, A.J., Wollheim, C.B., Cline, G.W., Shulman,G.I., 2007. Mitochondrial GTP regulates glucose-stimulated insulin secretion.Cell Metab. 5, 253–264.
Krus, U., Kotova, O., Spegel, P., Hallgard, E., Sharoyko, V.V., Vedin, A., Moritz, T.,Sugden, M.C., Koeck, T., Mulder, H., 2010. Pyruvate dehydrogenase kinase 1controls mitochondrial metabolism and insulin secretion in INS-1 832/13 clonalbeta-cells. Biochem. J. 429, 205–213.
Lee, B., Miles, P.D., Vargas, L., Luan, P., Glasco, S., Kushnareva, Y., Kornbrust, E.S.,Grako, K.A., Wollheim, C.B., Maechler, P., Olefsky, J.M., Anderson, C.M., 2003.Inhibition of mitochondrial Na(+)–Ca(2+) exchanger increases mitochondrialmetabolism and potentiates glucose-stimulated insulin secretion in ratpancreatic islets. Diabetes 52, 965–973.
Lehtihet, M., Honkanen, R.E., Sjoholm, A., 2005. Glutamate inhibits proteinphosphatases and promotes insulin exocytosis in pancreatic beta-cells.Biochem. Biophys. Res. Commun. 328, 601–607.
Li, N., Li, B., Brun, T., Deffert-Delbouille, C., Mahiout, Z., Daali, Y., Ma, X.J., Krause,K.H., Maechler, P., 2012. NADPH oxidase NOX2 defines a new antagonistic rolefor reactive oxygen species and cAMP/PKA in the regulation of insulin secretion.Diabetes 61, 2842–2850.
Liang, Y., Matschinsky, F.M., 1991. Content of CoA-esters in perifused rat isletsstimulated by glucose and other fuels. Diabetes 40, 327–333.
Maassen, J.A., LM, T.H., Van Essen, E., Heine, R.J., Nijpels, G., Jahangir Tafrechi, R.S.,Raap, A.K., Janssen, G.M., Lemkes, H.H., 2004. Mitochondrial diabetes: molecularmechanisms and clinical presentation. Diabetes 53 (Suppl. 1), S103–S109.
MacDonald, M.J., 1982. Evidence for the malate aspartate shuttle in pancreaticislets. Arch. Biochem. Biophys. 213, 643–649.
MacDonald, P.E., Salapatek, A.M., Wheeler, M.B., 2003. Temperature and redox statedependence of native Kv2.1 currents in rat pancreatic beta-cells. J. Physiol. 546,647–653.
Maechler, P., Wollheim, C.B., 1999. Mitochondrial glutamate acts as a messenger inglucose-induced insulin exocytosis. Nature 402, 685–689.
Maechler, P., Kennedy, E.D., Pozzan, T., Wollheim, C.B., 1997. Mitochondrialactivation directly triggers the exocytosis of insulin in permeabilizedpancreatic beta-cells. EMBO J. 16, 3833–3841.
Maechler, P., Kennedy, E.D., Wang, H., Wollheim, C.B., 1998. Desensitization ofmitochondrial Ca2+ and insulin secretion responses in the beta cell. J. Biol.Chem. 273, 20770–20778.
Maechler, P., Gjinovci, A., Wollheim, C.B., 2002. Implication of glutamate in thekinetics of insulin secretion in rat and mouse perfused pancreas. Diabetes 51(S1), S99–S102.
Maechler, P., Carobbio, S., Rubi, B., 2006. In beta-cells, mitochondria integrate andgenerate metabolic signals controlling insulin secretion. Int. J. Biochem. Cell.Biol. 38, 696–709.
McCormack, J.G., Halestrap, A.P., Denton, R.M., 1990. Role of calcium ions inregulation of mammalian intramitochondrial metabolism. Physiol. Rev. 70,391–425.
Miki, T., Nagashima, K., Seino, S., 1999. The structure and function of the ATP-sensitive K+ channel in insulin-secreting pancreatic beta-cells. J. Mol.Endocrinol. 22, 113–123.
Newsholme, P., Brennan, L., Rubi, B., Maechler, P., 2005. New insights into aminoacid metabolism, beta-cell function and diabetes. Clin. Sci. (London) 108, 185–194.
Nicholls, D.G., 2002. Mitochondrial function and dysfunction in the cell: itsrelevance to aging and aging-related disease. Int. J. Biochem. Cell. Biol. 34,1372–1381.
Nita, I.I., Hershfinkel, M., Fishman, D., Ozeri, E., Rutter, G.A., Sensi, S.L., Khananshvili,D., Lewis, E.C., Sekler, I., 2012. The mitochondrial Na+/Ca2+ exchangerupregulates glucose dependent Ca2+ signalling linked to insulin secretion.PLoS One 7, e46649.
O’Sullivan-Murphy, B., Urano, F., 2012. ER stress as a trigger for beta-celldysfunction and autoimmunity in type 1 diabetes. Diabetes 61, 780–781.
Pagliarini, D.J., Wiley, S.E., Kimple, M.E., Dixon, J.R., Kelly, P., Worby, C.A., Casey, P.J.,Dixon, J.E., 2005. Involvement of a mitochondrial phosphatase in the regulationof ATP production and insulin secretion in pancreatic beta cells. Mol. Cell. 19,197–207.
Palty, R., Silverman, W.F., Hershfinkel, M., Caporale, T., Sensi, S.L., Parnis, J., Nolte, C.,Fishman, D., Shoshan-Barmatz, V., Herrmann, S., Khananshvili, D., Sekler, I.,2010. NCLX is an essential component of mitochondrial Na+/Ca2+ exchange.Proc. Natl. Acad. Sci. USA 107, 436–441.
Park, K.S., Wiederkehr, A., Kirkpatrick, C., Mattenberger, Y., Martinou, J.C., Marchetti,P., Demaurex, N., Wollheim, C.B., 2008. Selective actions of mitochondrialfission/fusion genes on metabolism–secretion coupling in insulin-releasingcells. J. Biol. Chem. 283, 33347–33356.
Patterson, G.H., Knobel, S.M., Arkhammar, P., Thastrup, O., Piston, D.W., 2000.Separation of the glucose-stimulated cytoplasmic and mitochondrial NAD(P)Hresponses in pancreatic islet beta cells. Proc. Natl. Acad. Sci. USA 97, 5203–5207.
Perocchi, F., Gohil, V.M., Girgis, H.S., Bao, X.R., McCombs, J.E., Palmer, A.E., Mootha,V.K., 2010. MICU1 encodes a mitochondrial EF hand protein required for Ca(2+)uptake. Nature 467, 291–296.
Peyot, M.L., Guay, C., Latour, M.G., Lamontagne, J., Lussier, R., Pineda, M., Ruderman,N.B., Haemmerle, G., Zechner, R., Joly, E., Madiraju, S.R., Poitout, V., Prentki, M.,2009. Adipose triglyceride lipase is implicated in fuel- and non-fuel-stimulatedinsulin secretion. J. Biol. Chem. 284, 16848–16859.
Pralong, W.F., Bartley, C., Wollheim, C.B., 1990. Single islet beta-cell stimulation bynutrients: relationship between pyridine nucleotides, cytosolic Ca2+ andsecretion. EMBO J. 9, 53–60.
Prentki, M., Vischer, S., Glennon, M.C., Regazzi, R., Deeney, J.T., Corkey, B.E., 1992.Malonyl-CoA and long chain acyl-CoA esters as metabolic coupling factors innutrient-induced insulin secretion. J. Biol. Chem. 267, 5802–5810.
Prentki, M., Joly, E., El-Assaad, W., Roduit, R., 2002. Malonyl-CoA signaling, lipidpartitioning, and glucolipotoxicity: role in beta-cell adaptation and failure inthe etiology of diabetes. Diabetes 51 (Suppl. 3), S405–S413.
Rahier, J., Goebbels, R.M., Henquin, J.C., 1983. Cellular composition of the humandiabetic pancreas. Diabetologia 24, 366–371.
Rorsman, P., Eliasson, L., Renstrom, E., Gromada, J., Barg, S., Gopel, S., 2000. The cellphysiology of biphasic insulin secretion. News Physiol. Sci. 15, 72–77.
Rubi, B., Maechler, P., 2010. Minireview: new roles for peripheral dopamine onmetabolic control and tumor growth: let’s seek the balance. Endocrinology 151,5570–5581.
Rubi, B., Ishihara, H., Hegardt, F.G., Wollheim, C.B., Maechler, P., 2001. GAD65-mediated glutamate decarboxylation reduces glucose-stimulated insulinsecretion in pancreatic beta cells. J. Biol. Chem. 276, 36391–36396.
Rubi, B., Antinozzi, P.A., Herrero, L., Ishihara, H., Asins, G., Serra, D., Wollheim, C.B.,Maechler, P., Hegardt, F.G., 2002. Adenovirus-mediated overexpression of livercarnitine palmitoyltransferase I in INS1E cells: effects on cell metabolism andinsulin secretion. Biochem. J. 364, 219–226.
Rubi, B., del Arco, A., Bartley, C., Satrustegui, J., Maechler, P., 2004. The malate–aspartate NADH shuttle member Aralar1 determines glucose metabolic fate,mitochondrial activity, and insulin secretion in beta cells. J. Biol. Chem. 279,55659–55666.
Rutter, G.A., Burnett, P., Rizzuto, R., Brini, M., Murgia, M., Pozzan, T., Tavare, J.M.,Denton, R.M., 1996. Subcellular imaging of intramitochondrial Ca2+ withrecombinant targeted aequorin: significance for the regulation of pyruvatedehydrogenase activity. Proc. Natl. Acad. Sci. USA 93, 5489–5494.
Schuit, F.C., Huypens, P., Heimberg, H., Pipeleers, D.G., 2001. Glucose sensing inpancreatic beta-cells: a model for the study of other glucose-regulated cells ingut, pancreas, and hypothalamus. Diabetes 50, 1–11.
Storto, M., Capobianco, L., Battaglia, G., Molinaro, G., Gradini, R., Riozzi, B., DiMambro, A., Mitchell, K.J., Bruno, V., Vairetti, M.P., Rutter, G.A., Nicoletti, F.,2006. Insulin secretion is controlled by mGlu5 metabotropic glutamatereceptors. Mol. Pharmacol. 69, 1234–1241.
Sugden, M.C., Holness, M.J., 2003. Recent advances in mechanisms regulatingglucose oxidation at the level of the pyruvate dehydrogenase complex by PDKs.Am. J. Physiol. Endocrinol. Metab. 284, E855–E862.
Tarasov, A.I., Semplici, F., Ravier, M.A., Bellomo, E.A., Pullen, T.J., Gilon, P., Sekler, I.,Rizzuto, R., Rutter, G.A., 2012. The mitochondrial Ca2+ uniporter MCU isessential for glucose-induced ATP increases in pancreatic beta-cells. PLoS One 7,e39722.
Tarasov, A.I., Semplici, F., Li, D., Rizzuto, R., Ravier, M.A., Gilon, P., Rutter, G.A., 2013.Frequency-dependent mitochondrial Ca2+ accumulation regulates ATPsynthesis in pancreatic b cells. Pflugers Arch 465, 543–554.
Twig, G., Elorza, A., Molina, A.J., Mohamed, H., Wikstrom, J.D., Walzer, G., Stiles, L.,Haigh, S.E., Katz, S., Las, G., Alroy, J., Wu, M., Py, B.F., Yuan, J., Deeney, J.T., Corkey,B.E., Shirihai, O.S., 2008. Fission and selective fusion govern mitochondrialsegregation and elimination by autophagy. EMBO J. 27, 433–446.
Vallar, L., Biden, T.J., Wollheim, C.B., 1987. Guanine nucleotides induce Ca2+-independent insulin secretion from permeabilized RINm5F cells. J. Biol. Chem.262, 5049–5056.
Varadi, A., Ainscow, E.K., Allan, V.J., Rutter, G.A., 2002. Involvement of conventionalkinesin in glucose-stimulated secretory granule movements and exocytosis inclonal pancreatic beta-cells. J. Cell. Sci. 115, 4177–4189.
Verspohl, E.J., Handel, M., Ammon, H.P., 1979. Pentosephosphate shunt activity ofrat pancreatic islets: its dependence on glucose concentration. Endocrinology105, 1269–1274.
Vetterli, L., Carobbio, S., Pournourmohammadi, S., Martin-Del-Rio, R., Skytt, D.M.,Waagepetersen, H.S., Tamarit-Rodriguez, J., Maechler, P., 2012. Delineation ofglutamate pathways and secretory responses in pancreatic islets with beta-cellspecific abrogation of the glutamate dehydrogenase. Mol. Biol. Cell. 23, 3851–3862.
Wallace, D.C., 1999. Mitochondrial diseases in man and mouse. Science 283, 1482–1488.
Watkins, D.T., 1972. Pyridine nucleotide stimulation of insulin release from isolatedtoadfish insulin secretion granules. Endocrinology 90, 272–276.
Watkins, D.T., Moore, M., 1977. Uptake of NADPH by islet secretion granulemembranes. Endocrinology 100, 1461–1467.
Watkins, D., Cooperstein, S.J., Dixit, P.K., Lazarow, A., 1968. Insulin secretion fromtoadfish islet tissue stimulated by pyridine nucleotides. Science 162, 283–284.
Westermann, B., 2008. Molecular machinery of mitochondrial fusion and fission. J.Biol. Chem. 283, 13501–13505.
Wiederkehr, A., Park, K.S., Dupont, O., Demaurex, N., Pozzan, T., Cline, G.W.,Wollheim, C.B., 2009. Matrix alkalinization: a novel mitochondrial signal forsustained pancreatic beta-cell activation. EMBO J. 28, 417–428.
Wiederkehr, A., Szanda, G., Akhmedov, D., Mataki, C., Heizmann, C.W., Schoonjans,K., Pozzan, T., Spat, A., Wollheim, C.B., 2011. Mitochondrial matrix calcium is anactivating signal for hormone secretion. Cell Metab. 13, 601–611.
Yu, W., Niwa, T., Fukasawa, T., Hidaka, H., Senda, T., Sasaki, Y., Niki, I., 2000.Synergism of protein kinase A, protein kinase C, and myosin light-chain kinasein the secretory cascade of the pancreatic beta-cell. Diabetes 49, 945–952.
Zhang, Z., Wakabayashi, N., Wakabayashi, J., Tamura, Y., Song, W.J., Sereda, S., Clerc,P., Polster, B.M., Aja, S.M., Pletnikov, M.V., Kensler, T.W., Shirihai, O.S., Iijima, M.,Hussain, M.A., Sesaki, H., 2011. The dynamin-related GTPase Opa1 is requiredfor glucose-stimulated ATP production in pancreatic beta cells. Mol. Biol. Cell22, 2235–2245.
18 P. Maechler / Molecular and Cellular Endocrinology 379 (2013) 12–18

Mitochondrial and skeletal muscle health with advancing age
Adam R. Konopka, K. Sreekumaran Nair ⇑
Endocrine Research Unit, Mayo Clinic College of Medicine, Rochester, Minnesota, United States
a r t i c l e i n f o
Article history:Available online 16 May 2013
Keywords:AgingSarcopeniaMitochondriaProtein metabolism
a b s t r a c t
With increasing age there is a temporal relationship between the decline of mitochondrial and skeletalmuscle volume, quality and function (i.e., health). Reduced mitochondrial mRNA expression, proteinabundance, and protein synthesis rates appear to promote the decline of mitochondrial protein qualityand function. Decreased mitochondrial function is suspected to impede energy demanding processessuch as skeletal muscle protein turnover, which is critical for maintaining protein quality and thus skel-etal muscle health with advancing age. The focus of this review was to discuss promising human phys-iological systems underpinning the decline of mitochondrial and skeletal muscle health with advancingage while highlighting therapeutic strategies such as aerobic exercise and caloric restriction for combat-ing age-related functional impairments.
! 2013 Published by Elsevier Ireland Ltd.
1. Introduction
Reports of skeletal muscle atrophy that accompany advancingage (i.e., sarcopenia) and the associated reductions in skeletal mus-cle function and quality have been observed for several decades(Critchley, 1931; Rosenberg, 1989, 1997). Recently, panels of lead-ing scientists and physicians associated with large-scale epidemio-logical studies have created specific, objective criteria based onlean tissue mass and functional capacity to improve the diagnosisand treatment of sarcopenia (Delmonico et al., 2007; Fielding et al.,2011; Goodpaster et al., 2006; Morley et al., 2011; Newman et al.,2003). Human aging starts after the third decade and the progres-sion of skeletal muscle atrophy with age is a slow process (!1% peryear), but accelerates as humans approach 80 years of age (Baum-gartner et al., 1998). With expansion in human lifespan, the ele-vated rate of muscle loss becomes more problematic sinceskeletal muscle is critical for functionality and substrate metabo-lism. When the substrate reservoir deteriorates with age, the asso-ciated cardiometabolic disease states (i.e. insulin resistance,diabetes, cardiovascular disease, obesity) become more prevalent(Atlantis et al., 2009). Many studies have observed reduced skeletalmuscle mass and infiltration of adipose tissue depots within or be-tween skeletal muscle groups that are associated with reducedmuscle function, insulin resistance and obesity (Delmonico et al.,2009; Goodpaster et al., 2005, 2000). A key link between a reduc-tion in skeletal muscle health and prevalence of metabolic disor-ders with advancing age may be related to impaired
mitochondrial function. A reduction in mitochondrial abundanceand function with age has been observed across various species(c elegans, drosphilla, mice, humans) and tissues (skin, nerve,brain, skeletal muscle). Moreover, perturbations in skeletal musclemitochondrial energetics have been correlated with reduced aero-bic capacity (Short et al., 2005a), walking capacity (Coen et al.,2012) and skeletal muscle function (Safdar et al., 2010) in olderadults. The mechanisms of age-related changes in skeletal muscleare multifactorial but the purpose of this review is to highlightthe apparent temporal and functional connection between the de-cline of mitochondrial and skeletal muscle health (Fig. 1).
2. Reduced mitochondrial content and function with age
Electron microscopic assessment of skeletal muscle biopsy sam-ples revealed lower mitochondrial volume density in older adults(Conley et al., 2000). A decline in mitochondrial content, as repre-sented by mitochondrial DNA copy number, has also been demon-strated in rodents (Barazzoni et al., 2000) and humans (Short et al.,2005a). These findings, coupled with investigations that observedreduced levels of mitochondrial protein synthesis (Rooyackerset al., 1996) and expression of proteins encoded by both mitochon-drial and nuclear DNA (Lanza et al., 2008; Short et al., 2005a), areexpected to alter mitochondrial function. Semi-quantitative analy-ses, such as immunoblotting or maximal enzyme activity, supportthe notion that aging skeletal muscle contains less abundance ofenzymes in oxidative metabolism (i.e. Krebs Cycle, beta-oxidation)and/or proteins involved in the electron transport chain (ETC) (Coo-per et al., 1992; Ghosh et al., 2011; Lanza et al., 2008; Rooyackerset al., 1996; Tonkonogi et al., 2003; Trounce et al., 1989). Collec-tively, reductions in mitochondrial proteins and volume may limit
0303-7207/$ - see front matter ! 2013 Published by Elsevier Ireland Ltd.http://dx.doi.org/10.1016/j.mce.2013.05.008
⇑ Corresponding author. Address: Mayo Clinic, 200 First St. SW, Joseph 5-194,Rochester, MN, United States. Tel.: +1 507 255 2415; fax: +1 507 255 4828.
E-mail address: [email protected] (K. Sreekumaran Nair).
Molecular and Cellular Endocrinology 379 (2013) 19–29
Contents lists available at SciVerse ScienceDirect
Molecular and Cellular Endocrinology
journal homepage: www.elsevier .com/locate /mce

ATP production for energy demanding processes such as myocellu-lar remodeling to maintain protein quality.
Advancements of in vitro and ex vivo measures of mitochondrialenergetics have detected diminished capacity for basal (Petersenet al., 2003) and maximal (Conley et al., 2000; Kent-Braun andNg, 2000; Short et al., 2005a) mitochondrial ATP synthesis in olderadults. When expressing the rate of mitochondrial ATP synthesisrelative to mitochondrial content there remains a deficit in olderadults suggesting that there is not only a reduction in mitochon-drial protein content but also mitochondrial protein quality. Thesefindings appear to be related to physical activity, as sedentary indi-viduals had lower in vivo mitochondrial function compared to ac-tive individuals (Kent-Braun and Ng, 2000; Larsen et al., 2012). Itis important to acknowledge that in aging human skeletal muscle,findings of mitochondrial dysfunction are highly equivocal and thedisparity between studies is not well discussed. In Table 1 we pro-vide potential confounding variables related to the characteristicsof research participants (column A) as well as the use of variousmeasurements of mitochondrial abundance or function (columnB). Key differences exist when interpreting data since each mea-surement in Table 1 assesses different constituents of mitochon-drial abundance or function and each method presents keystrengths and weaknesses as has been reviewed in detail previ-ously (Lanza and Nair, 2010; Perry et al., 2013). One differencecould be comparisons between content or maximal activities of en-zymes in the mitochondrial matrix (e.g., citrate synthase, bHAD)which are completely encoded by nuclear DNA vs. proteins in-volved in oxidative phosphorylation (e.g., cytochrome c oxidase,NADH) that are encoded by both nuclear and mitochondrial gen-omes. Although analysis of maximal mitochondrial energeticsin vivo (i.e., 31P-MRS) and ex vivo (i.e., high-resolution respirome-try) are highly correlated (Lanza et al., 2011), subtle discrepanciesstill exist between different approaches for measuring mitochon-drial function in vivo (basal vs. maximally stimulated) and ex vivo(ATP production vs. oxygen respiration; permeabilized fibers vs.isolated mitochondria). Also, sampling of human muscle tissuefrom various muscle groups consisting of different recruitment
patterns and fiber type composition can create conflicting resultsbetween studies. These variables need to be recognized and ad-dressed to properly assess the true age-related phenotype. Glob-ally, when investigations utilize large sample sizes and rigorouscontrol to avoid many of the confounding variables there appearsto be an age-related decline in mitochondrial protein content,quality and function in the quadriceps femoris muscles. These dataprovide well-founded evidence for perturbations in mitochondrialhealth and connections to impaired functional capacity during sed-entary aging.
Aerobic training is an effective exercise prescription to stimu-late markers of oxidative capacity as established in the 1960s (Hol-loszy, 1967), when it was revealed that aerobic exercise ofsufficient intensity increased mitochondrial enzyme activity in ani-mal models. Numerous other investigations have confirmed theseresults, however, few studies in humans have directly investigatedif age influences exercise induced mitochondrial adaptations afterthe same exercise training program. From the few available stud-ies, it appears that mitochondrial molecular regulation and proteincontent are increased after 12–16 weeks of exercise training, inde-pendent of age, suggesting older individuals (<80 y) adapt favor-ably to exercise training (Ghosh et al., 2011; Short et al., 2003).However, the influence of various exercise training programs (i.e.,aerobic vs. resistance vs. concurrent training) on mitochondrialand skeletal muscle function (ex vivo or in vivo) has yet to be deter-mined and warrants investigation. Collectively, these data suggestthat exercise can improve or prevent the loss of mitochondrialhealth during sedentary aging (Fig. 2).
3. Molecular Regulation of Aging Mitochondria
The mitochondria consist of proteins encoded from both mito-chondrial (mtDNA) and nuclear DNA (nDNA). Although mtDNAcontains just 27 genes that encode 13 proteins (all within the elec-tron transport chain), 2 ribosomal and 22 translational RNA, properorganelle biogenesis and function require input from both gen-
Sedentary Aging
Mitochondrial: Volume Quality
Function
Skeletal Muscle:Volume Quality
Function
Functional Capacity
Morbidity
Healthcare Costs
?
Fig. 1. Reduced mitochondrial and skeletal volume, quality and function with sedentary aging. Sedentary aging is associated with the decline of mitochondrial and skeletalmuscle volume, quality and function. The casual link between the loss of mitochondrial homeostasis and sarcopenia is unknown, however, both appear with advancing ageand are associated with the loss of functional capacity and corresponding increases in comorbidities and annual healthcare costs. Exercise and physical activity are effectiveprescriptions to attenuate the negative consequences of sedentary aging illustrated in Fig. 1.
20 A.R. Konopka, K. Sreekumaran Nair / Molecular and Cellular Endocrinology 379 (2013) 19–29

omes. Several transcription factors and molecular regulators havebeen highlighted in orchestrating mitochondrial biogenesis andsubstrate metabolism. The exploration of the molecular regulationof mitochondria has received much attention to gain insight intothe etiology of aging mitochondria and associated disease condi-tions. The family of sirtuins, NAMPT, PGC-1a, NRF 1, NRF 2, TFAMas well as metabolite sensors such as AMPK, CAMK and calciumflux play an integral role in maintaining mitochondrial homeosta-sis as illustrated in Fig. 2.
3.1. Sirtuins
The Sirtuin family (SIRT 1–7) is an NAD-dependent histone/pro-tein deacetylase that interacts with transcription factors and cofac-tors influencing many metabolic pathways (for review see(Guarente, 2011; Gurd, 2011; Westphal et al., 2007; White andSchenk, 2012)). SIRT1 is the most well described Sirtuin due tothe favorable impact on targets associated with cellular growth,chromatin remodeling, substrate metabolism and mitochondrialbiogenesis. Specifically, the capability of SIRT1 to deacetylatePGC-1a, relaying signal transduction for mitochondrial biogenesis,improved substrate utilization and insulin action is particularlyrelevant in improving the aging phenotype. In addition, SIRT3,which is localized to the mitochondria, is associated with mito-chondrial efficiency and ROS production. SIRT3 knockout animalsdemonstrate hyperacetylation interfering with proper mRNA tran-scription, elevated levels of ROS and concomitant reduction in ATPsynthesis much like many aging models (Ahn et al., 2008; Kimet al., 2010). These data are substantiated from mechanistic studiesdisplaying the ability of SIRT3 to deacetylate and activate MnSODand glutathione-scavenging pathway enzymes to protect fromreactive oxygen species (ROS) during SIRT3 overexpression andcaloric restriction (Someya et al., 2010). Elevated ROS emissionsfrom the mitochondria have been implicated in the progressionof mitochondrial dysfunction and development of insulin resis-tance (Fisher-Wellman and Neufer, 2012). Therefore, SIRT 1 and3 may play a role in mitochondrial health, insulin action and func-tional capacity with advancing age.
Sedentary older adults contain less SIRT3 content, however, itappears those who perform vigorous endurance exercise are capa-
ble of maintaining SIRT3 compared to there younger counterparts(Lanza et al., 2008). Indeed, SIRT3 abundance and activity increaseafter contractile activity and may be a potential mechanism for im-proved ATP synthesis, ROS production and insulin action (Gurdet al., 2012). Exploring the upstream regulation of the sirtuin fam-ily is essential to fully appreciate how various interventions (i.e.,exercise, caloric restriction, medications) mediate the intracellularsignaling pathways associated with mitochondrial biogenesis andprotein quality.
3.2. Peroxisome proliferator-activated receptor-c coactivator (PGC)-1a
In aging human skeletal muscle, there have been observationsof either reduced or unaltered levels of PGC-1a (Lanza et al.,2008; Ling et al., 2004). Since PGC-1a is considered the master reg-ulator of mitochondrial biogenesis, lower levels may partially re-duce downstream transcription factors as well as mitochondrialcontent and function. This hypothesis is supported by a diminishedcapacity to stimulate mitochondrial biogenesis or maintain mito-chondrial content during active-aging in animals with geneticallyaltered PGC-1a (Leick et al., 2010). Additionally, animals withoverexpressed PGC-1a demonstrate mitochondrial biogenesis andreversal of many age-related diseases including sarcopenia (Wenz,2011; Wenz et al., 2009). Acute and chronic aerobic exercise in-crease PGC-1a mRNA expression similarly in young and old indi-viduals (Cobley et al., 2012; Short et al., 2003). Older people whohave maintained a high level of aerobic exercise for several yearshad greater protein expression of PGC-1a than sedentary youngpeople yet failed to achieve similar levels as younger people whoalso maintained high levels of aerobic training (Lanza et al.,2008) suggesting that exercise can mitigate some age-relatedlosses but cannot fully protect the molecular regulation of mito-chondrial biogenesis. Skeletal muscle biopsy samples obtainedfrom a unique group of adults over 80 y of age revealed that thosewho engaged in vigorous life-long endurance exercise have greaterPGC-1a mRNA expression compared to their healthy counterpartswho performed normal activities of daily living (Trappe et al.,2012). Although PGC-1a is not obligatory for exercise inducedmitochondrial biogenesis (Leick et al., 2008) it still appears to be
Table 1Divergent subject characteristics and analytical techniques may contribute to discrepancies regarding aging mitochondrial health.
A. Subject characteristics References B. Analytical techniques References
Age Bua et al. (2006), Chabi et al. (2005) Maximal enzyme activity Barrientos et al. (1996), Coggan et al. (1992), Holloszy (1967),Holloszy and Coyle (1984), Zucchini et al. (1995)
Sample size Chretien et al. (1998), Short et al.(2005a)
Protein abundance Lanza et al. (2008)
Mobility or orthopediclimitations
Boffoli et al. (1994), Joseph et al.(2012), Lezza et al. (1994), Safdar et al.(2010)
mtDNA copy number andmutations
Aiken et al. (2002), Short et al. (2005a)
Exercise/physical activityhistory
Barrientos et al. (1996), Lanza et al.(2008), Proctor et al. (1995)
mRNA expression Short et al. (2003), Wright et al. (2007)
Sarcopenia/frailty Moore et al. (2010), Waters et al.(2009)
Electron microscopy Conley et al. (2000), Hoppeler et al. (1985), Howald et al. (1985)
Adiposity Karakelides et al. (2010) In vivo function (31P-MRS) Amara et al. (2007), Conley et al. (2007), Kent-Braun and Ng(2000), Lanza et al. (2011), Lanza and Nair (2010), Petersen et al.(2003)
Comorbidities (i.e., insulinresistance, COPD, etc.)
Barreiro et al. (2009), Ghosh et al.(2011), Petersen et al. (2003)
Ex vivo function Lanza et al. (2011), Lanza and Nair (2010), Picard et al.(2010,2011), Rasmussen et al. (2003a,b)
Diet and medications Fisher-Wellman and Neufer (2012),Lanza et al. (2012), Robinson et al.(2009)
Skeletal muscle investigated Amara et al. (2007), Houmard et al. (1998), Larsen et al. (2012)
The study of aging mitochondria presents inconsistent findings potentially associated with (A) variability in subject characteristics and (B) different analytical techniques toassess mitochondrial abundance or function within skeletal muscle. To examine the true age-related decline in mitochondrial health, descriptive characteristics listed in (A)need to be comprehensively discussed as these variables may each independently affect mitochondrial health. Moreover, the different analytical techniques listed in (B) areall highly utilized but each approach studies different components of the mitochondria (i.e., citrate synthase enzyme activity vs. ex vivo ATP production in isolatedmitochondria) and therefore may contribute the equivocal findings between studies. Collectively, both subject characteristics and analytical techniques need to be consideredwhen interpreting data describing the aging mitochondrial phenotype. References provided utilize or discuss the associated subject characteristic or analytical technique.
A.R. Konopka, K. Sreekumaran Nair / Molecular and Cellular Endocrinology 379 (2013) 19–29 21

a valuable component in the effects of exercise on skeletal muscleand metabolic health with advancing age. Interestingly, an isoformof PGC-1a (PGC-1a4) has been comprehensively demonstrated tobe involved in skeletal muscle hypertrophy in vitro and in vivo(Ruas et al., 2012). PGC-1a4 appears to be the primary isoformassociated with skeletal muscle growth through the stimulationof IGF-1 and suppression of myostatin, MuRF-1 and Atrogin-1mRNA expression. Interestingly, previous studies have demon-
strated that aerobic (Konopka et al., 2010) and resistance (Kimet al., 2005; Roth et al., 2003; Ryan et al., 2011; Williamsonet al., 2010) exercise training reduced catabolic mRNA expression(i.e., FOXO3a, MuRF-1, Atrogin-1 and/or myostatin) with concomi-tant skeletal muscle hypertrophy. These adaptations could be asso-ciated with elevated levels of PGC-1a4 as recently revealed butfurther examination is needed. Elevated PGC-1a isoforms withexercise training in sedentary humans occurs concomitantly with
AMPNAD
Aerobic Exercise Training
PGC-1α
Mitochondrial Transcription Mitochondrial Dynamics
NRF-1 TFAM nDNA mtDNA
TranscriptionOXPHOS mRNA
Transcription2 rRNAs
13 OXPHOS mRNA
Mitochondrial Content & Function
Mitochondrial Protein Breakdown
Fusion
Fission
FIS1 MFN
Mitochondrial Protein Synthesis
Metabolites
Protein SynthesisnDNA
DRP1 1 & 2
I IIIII
IV
O2 H2O
Intermembrane space
Inner membrane
Matrix
H+ H+ H+
V
H+
ADP+Pi ATPNADH NAD+
PhagophoreFission Autophagosome Bulk Protein Breakdown
Nucleus
mtDNA
Protein Synthesis
Mitochondrion
LON
Targeted Protein Breakdown
Fig. 2. Mitochondrial adaptations to aerobic exercise training. With contractile activity, elevated levels of metabolic byproducts (i.e., NAD, AMP, Ca++, ROS, etc.) provide astimulus for increased molecular regulators of mitochondrial transcription, replication and dynamics (i.e., NAMPT, SIRT-1, PGC-1a, NRF-1, -2, TFAM, MFN-1, -2, FIS1, DRP1).Collectively, these alterations promote the increase in mitochondrial protein turnover allowing for the degradation of damaged proteins and de novo synthesis of newfunctional proteins. Overall, the elevated rate of mitochondrial protein turnover suggests an improvement in the quality of mitochondrial proteins for enhanced ATPproduction and lower reactive oxygen species (ROS) emission. Enhanced mitochondrial function may augment myocellular remodeling, skeletal muscle anabolism andfunctional capacity in older adults.
22 A.R. Konopka, K. Sreekumaran Nair / Molecular and Cellular Endocrinology 379 (2013) 19–29

increased mitochondrial protein content, mixed muscle proteinsynthesis, skeletal muscle hypertrophy and aerobic capacity (Har-ber et al., 2009b, 2012; Ruas et al., 2012; Short et al., 2004, 2003).Collectively, these investigations highlight the advantages of PGC-1a in promoting a healthy aging, skeletal muscle phenotype.
3.3. Mitochondrial transcription factor A (TFAM) and Nuclearrespiratory factor (NRF)-1 and -2
Recent research has revealed that PGC-1a relocates to both themitochondrial and nuclear compartments after a physiologicalstimulus, such as aerobic exercise, to coordinate mitochondrialbiogenesis from both nuclear and mitochondrial genomes (Safdaret al., 2011). Most reports describe PGC-1a by directly acting onNRF-1 and -2 within the nucleus to stimulate increased levels ofmitochondrial transcription factor A (TFAM) followed by importinto the mitochondria. However, it appears that PGC-1a can alsoact independently on NRF-1 and TFAM by binding to the NRF-1promoter region within the nucleus as well as being complexedwith TFAM and the mtDNA D-loop region within the mitochondrialmatrix to transcriptionally coordinate nuclear- and mitochondrial-encoded proteins. These studies established an updated paradigminto the mechanisms of how PGC-1a orchestrates mitochondrialbiogenesis through key transcriptional regulators NRF-1 and TFAM.
In addition to binding to mtDNA for transcriptional induction ofmitochondrial biogenesis, TFAM also has a strong affinity formtDNA to stabilize and package the genome into a nucleoid struc-ture (for detailed review see (Campbell et al., 2012)). StabilizingmtDNA appears to be a protective mechanism to prevent damageand/or loss of mtDNA copy number as observed in aging skeletalmuscle (Short et al., 2005a). However, in aging brain tissue, TFAMwas elevated with a concomitant reduction in mtDNA most likelydue to impaired binding of TFAM to mtDNA regions (Picca et al.,2012). Mitochondrial protein turnover via Lon protease, discussedin the next section, is thought to regulate the TFAM:mtDNA ratio toenhance stability and transcription (Matsushima et al., 2010).Exercise is known to increase TFAM and mtDNA number highlight-ing the potential for improved TFAM-mtDNA binding with chronicexercise. The regulation of transcription, translation and mitochon-drial biogenesis is still not completely understood and further re-search is warranted.
4. Skeletal muscle and mitochondrial protein turnover
In addition to transcriptional regulation, the accretion of newproteins and degradation of older proteins may have a large impacton mitochondrial morphology and function. It is important to notethat changes in mitochondrial protein turnover may not always bereflected by expression of mitochondrial proteins. For example,when the rates of de novo synthesized proteins are elevated whilebeing matched by the breakdown of older irreversibly modifiedproteins, no apparent changes in protein abundance can be de-tected. More importantly, elevated protein turnover (i.e., thereplacement of modified and presumably dysfunctional proteinsby de novo synthesized proteins) may be a strategic mechanismto maintain mitochondrial protein quality and function (Fig. 3).This notion is supported by a study demonstrating that lifelong cal-orie restricted mice maintained mitochondrial function with agebut did not increase mitochondrial abundance (Lanza et al.,2012). Instead of mitochondrial proliferation, calorie restrictedmice improved mitochondrial protein quality compared to theirad libitum fed counterparts. These concepts strongly emphasizethe need to measure mitochondrial protein synthesis and break-down as a process to increase or maintain mitochondrial functionwith age.
4.1. Mitochondrial protein synthesis
Infusion of stable isotope tracer into young and older adultsdemonstrated decreased rates of in vivo mitochondrial protein syn-thesis rate in skeletal muscle of older adults and is accompaniedwith diminished mitochondrial enzyme activity (Rooyackerset al., 1996). These data provide a feasible connection betweenthe decreased ability to replace mitochondrial proteins in agingskeletal muscle leading to mitochondrial enzymatic dysfunction.Furthermore, mitochondrial protein synthesis rates are initially re-duced during middle age, which may be a precursor to the progres-sive loss of mitochondrial protein abundance and function witholder age. Other investigations have confirmed the deficit in mito-chondrial protein synthesis rate in older adults (Guillet et al., 2004)while advancements of innovative methodology has allowed forthe analysis of individual mitochondrial protein synthesis ratesto elucidate specific proteins that may participate in the etiologyof aging mitochondrial dysfunction (Jaleel et al., 2008; Lanzaet al., 2012).
While increased mitochondrial content is an established adap-tation of aerobic exercise, the impact of exercise on mitochondrialprotein turnover is not well characterized. One group has demon-strated that acute and chronic aerobic exercise increases mito-chondrial protein synthesis rates in younger individuals(Wilkinson et al., 2008). However, the effects of exercise on agingmitochondrial protein turnover have not yet been examined. Dueto the clear associations with mitochondrial biogenesis and func-tion, studies are needed to comprehensively elucidate the impactof exercise training on overcoming diminished mitochondrial pro-tein synthesis in aging humans.
4.2. Mitochondrial protein degradation
Due to difficulties of properly assessing protein degradation inhuman skeletal muscle, the literature is equivocal and largely un-known. However, global assessments indicate whole-body proteindegradation is reduced in older adults (Balagopal et al., 1997; Hen-derson et al., 2009). These data, in conjunction with lower rates ofmixed muscle (Short et al., 2004), myosin heavy chain (Balagopalet al., 1997) and mitochondrial protein synthesis (Rooyackerset al., 1996), suggest that a low protein turnover in older adultsmay allow for a reduction in protein quality by accumulation ofmodified proteins in organelles (i.e., mitochondria) and tissues(i.e., skeletal muscle) creating further dysfunction with age(Fig. 3). It is important to note that different skeletal muscle sub-fractions (Balagopal et al., 1997; Rooyackers et al., 1996; Shortet al., 2004; Trappe et al., 2004), fiber types (Dickinson et al.,2010), and individual proteins (Jaleel et al., 2008) have diverserates of protein turnover and warrant further examination as acomponent of the age-related loss of mitochondrial and skeletalmuscle health. Currently, methods to determine skeletal muscleand mitochondrial protein degradation are not well developed.These key limitations highlight the need for advancement of noveltechniques to properly assess protein degradation and propel ourunderstanding of human skeletal muscle biology.
4.2.1. Mitochondrial dynamicsOne particular area of interest regarding mitochondrial turn-
over is the collaboration of mitochondrial fusion, fission andautophagy (i.e. mitochondrial dynamics) to regulate organellemorphology. Mitochondrial fusion is the combination of outermitochondrial membrane and subsequent mixing of intramito-chondrial components to dilute any damaged mitochondrial DNAor proteins. Additionally, mitofusion proteins also assist in moldingthe inner mitochondrial membrane cristae, making the collectivepurpose of mitofusion to prevent the dissipation of mitochondrial
A.R. Konopka, K. Sreekumaran Nair / Molecular and Cellular Endocrinology 379 (2013) 19–29 23

membrane potential and thus ATP synthesis. Investigations utiliz-ing animal knockout models of mitofusion proteins have demon-strated diminished mitochondrial function and biogenesis as wellas muscle atrophy (Chen et al., 2010).
Conversely, when fusion is no longer possible due to the loss ofmitochondrial membrane integrity, fission is responsible for thefragmentation and excision of any altered or damaged mitochon-drial components that are subsequently degraded by mitochon-drial specific autophagy (i.e. mitophagy) (Seo et al., 2010).Mitochondrial dynamics are essential to maintain normal mito-chondrial metabolism, morphology and homeostasis in highly oxi-dative tissues such as skeletal muscle (Masiero et al., 2009).Therefore, from recent research revealing that select mitofusionand mitofission markers (i.e., mRNA) are reduced in aging humanskeletal muscle (Crane et al., 2010), we can infer that mitochon-drial turnover is compromised which could partially mediateage-related mitochondrial dysfunction and impaired skeletal mus-cle health. Interestingly, markers of mitochondrial dynamics areelevated with acute exercise in young individuals (Cartoni et al.,2005; Slivka et al., 2012) suggesting that exercise can increasemitochondrial turnover, which may lead to favorable mitochon-drial functional improvements.
4.2.2. Proteolytic pathwaysThe autophagy-lysosome and ubiquitin–proteasome (UPP)
pathways are two major systems that mediate protein degradationand maintain cellular homeostasis. Autophagy appears to be asso-ciated with more bulk protein degradation of large areas and/ororganelles, such as mitochondria, that are encapsulated by thephagophore, fused with the lysosome and subsequently brokendown to amino acids (Fig. 2). Conversely, the UPP is responsiblefor marking select proteins that are damaged or misfolded withan ubiquitin tail for degradation via the proteasome. Recent re-search suggests that the UPP may interact with autophagy byassisting the regulation of mitochondrial dynamics and disposalof damaged mitochondrial proteins. Additionally, evidence indi-cates the role of UPP in regulating cellular homeostasis may be dis-tinct in various skeletal muscle organelles or sub-fractions (i.e.sarcoplasmic, myofibrillar, mitochondrial).
One mitochondrial quality control mechanism is the ATP-stim-ulated Lon protease located in the mitochondrial matrix (Fig. 2).Lon protease is believed to be an integral factor in the degradationof oxidatively damaged mitochondrial proteins (Bota and Davies,
2002). In aging models, Lon protease is reduced and thereforehypothesized to play a role in the development of mitochondrialdysfunction in older tissues (Bota et al., 2002; Lee et al., 1999). An-other mitochondrial quality control pathway is autophagy, as evi-denced by the maintenance of mitochondrial function in the liverof older transgenic mice compared to wild type mice (Zhang andCuervo, 2008). Similarly, overexpression of autophagy proteins inhuman umbilical vein endothelial cells appears to remove dam-aged mitochondrial proteins when challenged with reactive oxy-gen species in vitro (Mai et al., 2012). Data in human skeletalmuscle are limited but recent studies have observed no measur-able differences between young and older individuals at the mRNAlevel for markers of UPP or autophagy (Fry et al., 2012a). It is inter-esting to note that mRNA of UPP was elevated and/or autophagyreduced in humans undergoing accelerated atrophy (i.e. >80 y old(Raue et al., 2007; Williamson et al., 2010), para- (Fry et al.,2012b) and hemiplegia (von Walden et al., 2012)). Developmentof dynamic assays to measure protein degradation specific to themitochondrial and myofibrillar proteins are needed to provide a di-rect functional connection to protein metabolism and age.
Acute aerobic exercise appears to increase mRNA expression ofproteolytic pathways within mixed muscle homogenates (Harberet al., 2009a, 2010; Louis et al., 2007; Pasiakos et al., 2010). Thesedata suggest that the molecular induction of protein degradation iselevated by acute exercise, most likely providing amino acids for denovo synthesis (Balagopal et al., 2001) and myocellular remodelingthat leads to improved contractile function after chronic exercise(Harber et al., 2004, 2009b, 2012; Trappe et al., 2001) Interestingly,exercise training programs that improve skeletal muscle size andfunction in adults (<80 y) observed reductions in proteolytic mark-ers (Konopka et al., 2010; Williamson et al., 2010), most likelyshifting protein balance in favor of skeletal muscle protein accre-tion. Collectively, these data reveal the differences between tran-sient alterations and chronic adaptations in proteolyticmachinery while highlighting the need for additional investiga-tions examining protein turnover to substantiate the link to myo-cellular and mitochondrial function after acute and chronicexercise.
5. Insufficient antioxidant capacity and oxidative damage
Reactive oxygen species (ROS) are molecules containing one ormore unpaired electrons mainly produced from complex I and III in
Aging
Protein Quality
Exercise Training
Protein Synthesis
Protein Degradation
Amino Acids
New Proteins
Old Proteins
Protein Turnover
Fig. 3. Effect of aging and exercise on protein damage and quality. With aging, excess reactive oxygen species (ROS) are produced from mitochondria with a concomitantreduction of protein degradation and synthesis (i.e., protein turnover). The combination of elevated ROS and reduced protein turnover can lead to the accumulation of damageto proteins resulting in reduced protein quality and function. We hypothesis that exercise training can attenuate age-related production of ROS and stimulate proteinturnover, in turn, degrading oxidatively damaged proteins and replacing with newly synthesized, functional proteins.
24 A.R. Konopka, K. Sreekumaran Nair / Molecular and Cellular Endocrinology 379 (2013) 19–29

the ETC. These byproducts are normally detoxified by antioxidants(e.g. MnSOD, CuZnSOD, catalase) but when they are generated inexcess of antioxidant capacity they can irreversibly modify (i.e.damage) lipids, proteins, and DNA. Due to inconsistent findingson the antioxidant capacity in older adults (Ghosh et al., 2011;Gianni et al., 2004; Leeuwenburgh et al., 1994; Pansarasa et al.,2000) there is a strong need to determine antioxidant capacity atthe systemic, skeletal muscle and mitochondrial compartmentsto fully identify where these defense mechanisms fail and wheredevelopment of therapies should be focused to ameliorate oxidantdamage and cellular dysfunction with age.
Damage to mtDNA is suspected to occur easily due to the prox-imity near the ETC and lack of protection by histones. The com-bined effects of reduced protein turnover and excess ROSemission create an environment conducive in aging skeletal mus-cle for the accumulation of oxidatively damaged mtDNA and con-tractile proteins (Fig. 3). Accrual of mtDNA damage may then allowproduction of dysfunctional proteins within the ETC, further exag-gerating ROS emission and oxidative damage. This scenario is con-sidered the mitochondrial theory of aging first hypothesized by(Harman, 1972). However, it is important to note that the appear-ance of mtDNA deletion/mutations in human skeletal muscle is rel-atively small, with data indicating that mtDNA deletions may reachlevels of physiological significance only in adults greater than 80 yold (Bua et al., 2006; Chabi et al., 2005; Kopsidas et al., 1998; Kov-alenko et al., 1997) although many age-related changes includingsarcopenia begin much earlier. When mtDNA deletions are presentin single muscle fibers they appear red and ragged, leading to fiberatrophy and eventually fiber loss (Bua et al., 2006). Moreover,mtDNA deletions and fiber atrophy are more prevalent in fastMHC II fibers, which is consistent with age-related loss of fast fibercomposition and contractile properties. The pattern of mtDNAdeletion mutations, fiber atrophy and fiber loss provides a clearrelationship between mitochondria and skeletal muscle atrophy.
Data from mitochondrial bioenergetics supports the role of al-tered mitochondrial membrane potential in mediating excess lev-els of oxidant production (Fisher-Wellman and Neufer, 2012).The concept is based on redox biology of mitochondria where overnutrition (i.e. increased supply) and/or reduced physical activity(i.e. reduced demand) appears to create a buildup of protons thuscreating a high membrane potential that could cause a cessationof electron flow through the ETC. The disruption in electron flowis thought to increase oxidant production by acting as a releasevalve to dissipate the elevated membrane potential. Any mecha-nism to allow protons to flow back to the mitochondrial matrix(ATP synthesis or uncoupling) will also help relieve membrane po-tential and therefore oxidant production. This notion is supportedby findings that lifelong caloric restriction attenuates H2O2 emis-sion by eliminating excess energy intake (i.e. supply) and mitigatesthe accumulation of post-translational modifications, especiallyoxidation and deamidation, while concomitantly maintainingmitochondrial energetics with age (Lanza et al., 2012). These noveldata are available due to recent advancements where proteomequality can be assessed by the evaluation of post-translationalmodifications using tandem mass spectrometry. Not only can thisinnovative approach comprehensively detect global protein modi-fications, it can also determine which amino acid residues are mostcommonly modified. Implementing proteome analysis of post-translational modifications may provide a platform to developand test innovative strategies to reduce the accumulation of mod-ified and functionally impaired proteins.
In addition to caloric restriction, physical activity levels play astrong role in modulating skeletal muscle quality as sedentary old-er individuals have a noticeable decline in antioxidant capacitywith concomitant oxidative damage compared to age-matched ac-tive individuals (Safdar et al., 2010). Oxidative modifications can
affect action potential propagation, ETC complexes, calcium trans-port/regulation, and myosin and actin interaction; collectivelyreducing skeletal muscle function in rodent models (Fulle et al.,2004; Rossi et al., 2008). In a unique model of muscle dysfunction,individuals with chronic obstructive pulmonary disease were char-acterized with increased oxidative damage that was negativelycorrelated with aerobic capacity and isometric skeletal muscleforce production (Barreiro et al., 2009). These data are supportedin older adults as elevated oxidative damage has been correlatedwith diminished functional capacity (Howard et al., 2007; Sembaet al., 2007a) and increased risk of mortality (Semba et al.,2007b). Therefore, there are implications that excess ROS may bean underlying characteristic in the progression of muscle atrophyby introducing oxidative damage that can negatively affect thefunctional capabilities of older adults.
6. A role for epigenetic regulation of mitochondrial andcontractile proteins
The age-related decline in transcription (i.e., mRNA expression)and translation (i.e., protein synthesis) are apparent in the loss ofmitochondrial and contractile protein quality. The underlyingmechanisms for reduced transcription include epigenetics, whichhave a responsibility in shaping the aging phenotype in responseto environmental influences like physical activity and diet. Com-mon epigenetic mechanisms are modifications to DNA and/or his-tones (i.e., acetylation, methylation). Changes in the methylationand acetylation status can modify chromatin structure, which inturn alters the binding capability of transcription factors to createmRNA (Fig. 4). Epigenomic research has large implications inimproving our understanding of the aging mitochondrial and con-tractile dysfunction but is currently at its nascent stages.
It appears with older age there is an increase in DNA methyla-tion of promoter regions for genes involved in oxidative phosphor-ylation and the level of DNA methylation is inversely correlatedwith gene expression (Ling et al., 2007; Ronn et al., 2008). Thesedata suggest that altered methylation could be involved in reducedmitochondrial mRNA expression and protein synthesis observed inolder adults. More expansive investigation is necessary to deter-mine key promoter regions that may be differentially methylated.Furthermore, alterations in mitochondrial function may providefeedback to influence the epigenetic regulation of the mitochon-drial and nuclear genome.
In addition to mitochondrial regulation, epigenetic alterationsalso appear to influence key skeletal muscle contractile proteins.The balance between histone acetylation and deacetylationchanges in concordance with shifts in myosin heavy chain compo-sition during unloading (Pandorf et al., 2009). This is of particularinterest when exploring the mechanisms mediating changes inMHC composition of aging skeletal muscle that occurs with con-comitant reductions in size and contractile performance of fast,MHC IIa fibers (Lexell et al., 1983; Trappe et al., 2003). Fast myosinlight chain isoforms, thought to influence contractile function,were found to be negatively correlated with promoter methylation(Donoghue et al., 1991) suggesting that methylation may inhibitfast fiber performance as observed in older adults.
Currently, exercise seems to be one of the most impactful stim-uli that alters skeletal muscle physiology (i.e., MHC and mitochon-drial protein abundance and function (Balagopal et al., 1997;Coggan et al., 1992; Ghosh et al., 2011; Harber et al., 2009b,2012; Konopka et al., 2011; Short et al., 2005b, 2003)) and servesas a countermeasure to many negative consequences of sedentaryaging. However, the effects of exercise and age on epigenetic regu-lation of mRNA expression and skeletal muscle adaptations are rel-atively unknown. Acute aerobic exercise can induce histone
A.R. Konopka, K. Sreekumaran Nair / Molecular and Cellular Endocrinology 379 (2013) 19–29 25

modifications that may mediate chromatin remodeling and disas-sociations with transcription factors implicated in substratemetabolism (McGee et al., 2009; McGee and Hargreaves, 2004).Moreover, acute and chronic contractile activity increased SIRT1deacylate activity within the nucleus which is most likely relatedto increased PGC-1a mRNA (Gurd, 2011; Gurd et al., 2011). An elo-quent study (Barres et al., 2012) recently revealed that acute aero-bic exercise of sufficient intensity can alter global and promoterspecific methylation leading to changes in mRNA expression re-lated to mitochondrial and substrate regulation in young adults.More investigations like Barres et al., are needed to clearly deter-mine the influence of age and chronic exercise on the epigeneticregulation of global and specific promoter regions related to mito-chondrial (e.g., PGC-1a, SIRT1, TFAM) and contractile proteins (e.g.MHC, MLC, actin, troponin) (Fig. 4). Discovering the epigeneticmodulation of skeletal muscle has vast potential to facilitate thedevelopment of novel therapies to improve protein quality withage.
6.1. Perspectives on aging skeletal muscle and mitochondrial health
The common loss of mitochondrial and skeletal muscle volume,function and quality is an attractive relationship to help explainthe comorbidities associated with aging. More research is neededto confirm that the loss of mitochondria health undermines sarco-penia, especially due to the variability within human studies. Someinconsistency seems to be related to different physical activity andlifestyle choices between subjects. This variability may partially beexplained by the implementation of epigenetic research to gaincomprehensive insight into the molecular regulation of aging insedentary and physically active individuals. Exercise training andphysical activity remain effective strategies to attenuate the devel-opment of mitochondrial and skeletal muscle dysfunction butmany questions remain unanswered. Moreover, the role of chroniccaloric restriction requires controlled studies that balance the po-tential adverse effects due to loss of lean mass and energy balancevs. beneficial effects associated with reduced oxidative damage to
proteins and DNA. In many aging populations, adherence or abilityto participate in exercise is limited due to orthopedic or diseaselimitations (i.e. heart failure, chronic obstructive pulmonary dis-ease) which warrants exploration of other therapies (i.e., caloricrestriction, diet composition, non-traditional exercise, etc.) to helpprevent the negative health consequences and elevated healthcarecosts related to sedentary aging.
Acknowledgment
The authors are grateful for the skillful and diligent assistanceof Katherine Klaus, Dawn Morse, Jill Schimke, Maureen Bigelow,Daniel Jakaitis, Roberta Soderberg, Beth Will, Deborah Sheldonand Melissa Aakre. This research was supported by National Insti-tutes of Health grants UL1-RR-024150-01 and AG09531, R01-DK41973 (KSN) and T32 DK007352 (ARK). Additional supportwas provided by Mayo Foundation and the Murdock-Dole Profes-sorship (KSN).
References
Ahn, B.H., Kim, H.S., Song, S., Lee, I.H., Liu, J., Vassilopoulos, A., Deng, C.X., Finkel, T.,2008. A role for the mitochondrial deacetylase Sirt3 in regulating energyhomeostasis. Proc. Natl. Acad. Sci. USA 105, 14447–14452.
Aiken, J., Bua, E., Cao, Z., Lopez, M., Wanagat, J., McKenzie, D., McKiernan, S., 2002.Mitochondrial DNA deletion mutations and sarcopenia. Ann. NY. Acad. Sci. 959,412–423.
Amara, C.E., Shankland, E.G., Jubrias, S.A., Marcinek, D.J., Kushmerick, M.J., Conley,K.E., 2007. Mild mitochondrial uncoupling impacts cellular aging in humanmuscles in vivo. Proc. Natl. Acad. Sci. USA 104, 1057–1062.
Atlantis, E., Martin, S.A., Haren, M.T., Taylor, A.W., Wittert, G.A., 2009. Inverseassociations between muscle mass, strength, and the metabolic syndrome.Metabolism 58, 1013–1022.
Balagopal, P., Rooyackers, O.E., Adey, D.B., Ades, P.A., Nair, K.S., 1997. Effects of agingon in vivo synthesis of skeletal muscle myosin heavy-chain and sarcoplasmicprotein in humans. Am. J. Physiol. 273, E790–800.
Balagopal, P., Schimke, J.C., Ades, P., Adey, D., Nair, K.S., 2001. Age effect ontranscript levels and synthesis rate of muscle MHC and response to resistanceexercise. Am. J. Physiol. Endocrinol. Metab. 280, E203–8.
Barazzoni, R., Short, K.R., Nair, K.S., 2000. Effects of aging on mitochondrial DNAcopy number and cytochrome c oxidase gene expression in rat skeletal muscle,liver, and heart. J. Biol. Chem. 275, 3343–3347.
Condensed Chromatin During Sedentary Aging
Open ChromatinInduced by Exercise
Mediated by DNMT/HAT/HMTs
&HDACs/HDMs
Mitochondrial Proteins Contractile Proteins
PGC-1α, SIRT1, TFAM MHC, MLC, Actin, Troponin
Fig. 4. Epigenetic regulation of mitochondrial and contractile proteins. Epigenetic control of mitochondrial and contractile proteins may improve our knowledge on thedevelopment of the aging phenotype. During sedentary aging, chromatin is condensed by altered levels of acetylation and/or methylation that prevent binding oftranscription factors. With exercise, modifications of histones (indirect modification) and/or DNA (direct modification) may allow an open chromatin structure wheretranscription factors can bind to DNA promoter regions for mRNA transcription to occur. The shifts between condensed chromatin during sedentary aging and openchromatin with exercise are partially mediated by DNA and histone modifying enzymes: DNA methyl transfereases (DNMT), histone acetyl transferases (HATs), histonemethyl transferases (HMTs), histone deacetylases (HDACs) and histone demethylases (HDMs). The schematic was adopted from (Zwetsloot et al., 2009) and altered to reflectour perspective on epigenetic control of mitochondrial and contractile protein quality.
26 A.R. Konopka, K. Sreekumaran Nair / Molecular and Cellular Endocrinology 379 (2013) 19–29

Barreiro, E., Rabinovich, R., Marin-Corral, J., Barbera, J.A., Gea, J., Roca, J., 2009.Chronic endurance exercise induces quadriceps nitrosative stress in patientswith severe COPD. Thorax 64, 13–19.
Barres, R., Yan, J., Egan, B., Treebak, J.T., Rasmussen, M., Fritz, T., Caidahl, K., Krook,A., O’Gorman, D.J., Zierath, J.R., 2012. Acute exercise remodels promotermethylation in human skeletal muscle. Cell Metab. 15, 405–411.
Barrientos, A., Casademont, J., Rotig, A., Miro, O., Urbano-Marquez, A., Rustin, P.,Cardellach, F., 1996. Absence of relationship between the level of electrontransport chain activities and aging in human skeletal muscle. Biochem.Biophys. Res. Commun. 229, 536–539.
Baumgartner, R.N., Koehler, K.M., Gallagher, D., Romero, L., Heymsfield, S.B., Ross,R.R., Garry, P.J., Lindeman, R.D., 1998. Epidemiology of sarcopenia among theelderly in New Mexico. Am. J. Epidemiol. 147, 755–763.
Boffoli, D., Scacco, S.C., Vergari, R., Solarino, G., Santacroce, G., Papa, S., 1994. Declinewith age of the respiratory chain activity in human skeletal muscle. Biochim.Biophys. Acta. 1226, 73–82.
Bota, D.A., Davies, K.J., 2002. Lon protease preferentially degrades oxidizedmitochondrial aconitase by an ATP-stimulated mechanism. Nat. Cell Biol. 4,674–680.
Bota, D.A., Van Remmen, H., Davies, K.J., 2002. Modulation of Lon protease activityand aconitase turnover during aging and oxidative stress. FEBS Lett. 532, 103–106.
Bua, E., Johnson, J., Herbst, A., Delong, B., McKenzie, D., Salamat, S., Aiken, J.M., 2006.Mitochondrial DNA-deletion mutations accumulate intracellularly todetrimental levels in aged human skeletal muscle fibers. Am. J. Hum. Genet.79, 469–480.
Campbell, C.T., Kolesar, J.E., Kaufman, B.A., 2012. Mitochondrial transcription factorA regulates mitochondrial transcription initiation, DNA packaging, and genomecopy number. Biochim. Biophys. Acta 1819, 921–929.
Cartoni, R., Leger, B., Hock, M.B., Praz, M., Crettenand, A., Pich, S., Ziltener, J.L., Luthi,F., Deriaz, O., Zorzano, A., Gobelet, C., Kralli, A., Russell, A.P., 2005. Mitofusins 1/2and ERRalpha expression are increased in human skeletal muscle after physicalexercise. J. Physiol. 567, 349–358.
Chabi, B., Mousson de Camaret, B., Chevrollier, A., Boisgard, S., Stepien, G., 2005.Random mtDNA deletions and functional consequence in aged human skeletalmuscle. Biochem. Biophys. Res. Commun. 332, 542–549.
Chen, H., Vermulst, M., Wang, Y.E., Chomyn, A., Prolla, T.A., McCaffery, J.M., Chan,D.C., 2010. Mitochondrial fusion is required for mtDNA stability in skeletalmuscle and tolerance of mtDNA mutations. Cell 141, 280–289.
Chretien, D., Gallego, J., Barrientos, A., Casademont, J., Cardellach, F., Munnich, A.,Rotig, A., Rustin, P., 1998. Biochemical parameters for the diagnosis ofmitochondrial respiratory chain deficiency in humans, and their lack of age-related changes. Biochem. J. 329 (Pt 2), 249–254.
Cobley, J.N., Bartlett, J.D., Kayani, A., Murray, S.W., Louhelainen, J., Donovan, T.,Waldron, S., Gregson, W., Burniston, J.G., Morton, J.P., Close, G.L., 2012. PGC-1alpha transcriptional response and mitochondrial adaptation to acute exerciseis maintained in skeletal muscle of sedentary elderly males. Biogerontology 13,621–631.
Coen, P.M., Jubrias, S.A., Distefano, G., Amati, F., Mackey, D.C., Glynn, N.W., Manini,T.M., Wohlgemuth, S.E., Leeuwenburgh, C., Cummings, S.R., Newman, A.B.,Ferrucci, L., Toledo, F.G., Shankland, E., Conley, K.E., Goodpaster, B.H., 2012.Skeletal muscle mitochondrial energetics are associated with maximal aerobiccapacity and walking speed in older adults. J. Gerontol. A. Biol. Sci. Med. Sci..
Coggan, A.R., Spina, R.J., King, D.S., Rogers, M.A., Brown, M., Nemeth, P.M., Holloszy,J.O., 1992. Skeletal muscle adaptations to endurance training in 60- to 70-yr-oldmen and women. J. Appl. Physiol. 72, 1780–1786.
Conley, K.E., Jubrias, S.A., Esselman, P.C., 2000. Oxidative capacity and ageing inhuman muscle. J. Physiol. 526 (Pt 1), 203–210.
Conley, K.E., Jubrias, S.A., Amara, C.E., Marcinek, D.J., 2007. Mitochondrialdysfunction: impact on exercise performance and cellular aging. Exerc. Sport.Sci. Rev. 35, 43–49.
Cooper, J.M., Mann, V.M., Schapira, A.H., 1992. Analyses of mitochondrialrespiratory chain function and mitochondrial DNA deletion in human skeletalmuscle: effect of ageing. J. Neurol. Sci. 113, 91–98.
Crane, J.D., Devries, M.C., Safdar, A., Hamadeh, M.J., Tarnopolsky, M.A., 2010. Theeffect of aging on human skeletal muscle mitochondrial and intramyocellularlipid ultrastructure. J. Gerontol. A. Biol. Sci. Med. Sci. 65, 119–128.
Critchley, M., 1931. The neurology of old age. Lancet 1, 1221–1231.Delmonico, M.J., Harris, T.B., Lee, J.S., Visser, M., Nevitt, M., Kritchevsky, S.B.,
Tylavsky, F.A., Newman, A.B., 2007. Alternative definitions of sarcopenia, lowerextremity performance, and functional impairment with aging in older men andwomen. J. Am. Geriatr. Soc. 55, 769–774.
Delmonico, M.J., Harris, T.B., Visser, M., Park, S.W., Conroy, M.B., Velasquez-Mieyer,P., Boudreau, R., Manini, T.M., Nevitt, M., Newman, A.B., Goodpaster, B.H., 2009.Longitudinal study of muscle strength, quality, and adipose tissue infiltration.Am. J. Clin. Nutr. 90, 1579–1585.
Dickinson, J.M., Lee, J.D., Sullivan, B.E., Harber, M.P., Trappe, S.W., Trappe, T.A., 2010.A new method to study in vivo protein synthesis in slow- and fast-twitchmuscle fibers and initial measurements in humans. J. Appl. Physiol. 108, 1410–1416.
Donoghue, M.J., Alvarez, J.D., Merlie, J.P., Sanes, J.R., 1991. Fiber type- and position-dependent expression of a myosin light chain-CAT transgene detected with anovel histochemical stain for CAT. J. Cell Biol. 115, 423–434.
Fielding, R.A., Vellas, B., Evans, W.J., Bhasin, S., Morley, J.E., Newman, A.B., Abellanvan Kan, G., Andrieu, S., Bauer, J., Breuille, D., Cederholm, T., Chandler, J., DeMeynard, C., Donini, L., Harris, T., Kannt, A., Keime Guibert, F., Onder, G.,
Papanicolaou, D., Rolland, Y., Rooks, D., Sieber, C., Souhami, E., Verlaan, S.,Zamboni, M., 2011. Sarcopenia: an undiagnosed condition in older adults.Current consensus definition: prevalence, etiology, and consequences.International working group on sarcopenia. J. Am. Med. Dir. Assoc. 12, 249–256.
Fisher-Wellman, K.H., Neufer, P.D., 2012. Linking mitochondrial bioenergetics toinsulin resistance via redox biology. Trends Endocrinol. Metab. 23, 142–153.
Fry, C.S., Drummond, M.J., Glynn, E.L., Dickinson, J.M., Gundermann, D.M.,Timmerman, K.L., Walker, D.K., Volpi, E., Rasmussen, B.B., 2012a. SkeletalMuscle Autophagy and Protein Breakdown Following Resistance Exercise areSimilar in Younger and Older Adults. J. Gerontol. A Biol. Sci. Med. Sci..
Fry, C.S., Drummond, M.J., Lujan, H.L., Dicarlo, S.E., Rasmussen, B.B., 2012b.Paraplegia increases skeletal muscle autophagy. Muscle Nerve 46, 793–798.
Fulle, S., Protasi, F., Di Tano, G., Pietrangelo, T., Beltramin, A., Boncompagni, S.,Vecchiet, L., Fano, G., 2004. The contribution of reactive oxygen species tosarcopenia and muscle ageing. Exp. Gerontol. 39, 17–24.
Ghosh, S., Lertwattanarak, R., Lefort, N., Molina-Carrion, M., Joya-Galeana, J., Bowen,B.P., Garduno-Garcia Jde, J., Abdul-Ghani, M., Richardson, A., DeFronzo, R.A.,Mandarino, L., Van Remmen, H., Musi, N., 2011. Reduction in reactive oxygenspecies production by mitochondria from elderly subjects with normal andimpaired glucose tolerance. Diabetes 60, 2051–2060.
Gianni, P., Jan, K.J., Douglas, M.J., Stuart, P.M., Tarnopolsky, M.A., 2004. Oxidativestress and the mitochondrial theory of aging in human skeletal muscle. Exp.Gerontol. 39, 1391–1400.
Goodpaster, B.H., Thaete, F.L., Kelley, D.E., 2000. Thigh adipose tissue distribution isassociated with insulin resistance in obesity and in type 2 diabetes mellitus.Am. J. Clin. Nutr. 71, 885–892.
Goodpaster, B.H., Krishnaswami, S., Harris, T.B., Katsiaras, A., Kritchevsky, S.B.,Simonsick, E.M., Nevitt, M., Holvoet, P., Newman, A.B., 2005. Obesity, regionalbody fat distribution, and the metabolic syndrome in older men and women.Arch. Int. Med. 165, 777–783.
Goodpaster, B.H., Park, S.W., Harris, T.B., Kritchevsky, S.B., Nevitt, M., Schwartz, A.V.,Simonsick, E.M., Tylavsky, F.A., Visser, M., Newman, A.B., 2006. The loss ofskeletal muscle strength, mass, and quality in older adults: the health, agingand body composition study. J. Gerontol. A. Biol. Sci. Med. Sci. 61, 1059–1064.
Guarente, L., 2011. Franklin H. Epstein Lecture: sirtuins, aging, and medicine. NEngl. J. Med. 364, 2235–2244.
Guillet, C., Prod’homme, M., Balage, M., Gachon, P., Giraudet, C., Morin, L., Grizard, J.,Boirie, Y., 2004. Impaired anabolic response of muscle protein synthesis isassociated with S6K1 dysregulation in elderly humans. FASEB J. 18, 1586–1587.
Gurd, B.J., 2011. Deacetylation of PGC-1alpha by SIRT1: importance for skeletalmuscle function and exercise-induced mitochondrial biogenesis. Appl. Physiol.Nutr. Metab. 36, 589–597.
Gurd, B.J., Yoshida, Y., McFarlan, J.T., Holloway, G.P., Moyes, C.D., Heigenhauser, G.J.,Spriet, L., Bonen, A., 2011. Nuclear SIRT1 activity, but not protein content,regulates mitochondrial biogenesis in rat and human skeletal muscle. Am. J.Physiol. Regul. Integr. Compos. Physiol. 301, R67–75.
Gurd, B.J., Holloway, G.P., Yoshida, Y., Bonen, A., 2012. In mammalian muscle, SIRT3is present in mitochondria and not in the nucleus; and SIRT3 is upregulated bychronic muscle contraction in an adenosine monophosphate-activated proteinkinase-independent manner. Metabolism 61, 733–741.
Harber, M.P., Gallagher, P.M., Creer, A.R., Minchev, K.M., Trappe, S.W., 2004. Singlemuscle fiber contractile properties during a competitive season in male runners.Am. J. Physiol. Regul. Integr. Comp. Physiol. 287, R1124–31.
Harber, M.P., Crane, J.D., Dickinson, J.M., Jemiolo, B., Raue, U., Trappe, T.A., Trappe,S.W., 2009a. Protein synthesis and the expression of growth-related genes arealtered by running in human vastus lateralis and soleus muscles. Am. J. Physiol.Regul. Integr. Comp. Physiol. 296, R708–14.
Harber, M.P., Konopka, A.R., Douglass, M.D., Minchev, K., Kaminsky, L.A., Trappe,T.A., Trappe, S., 2009b. Aerobic exercise training improves whole muscle andsingle myofiber size and function in older women. Am. J. Physiol. Regul. Integr.Comp. Physiol. 297, R1452–9.
Harber, M.P., Konopka, A.R., Jemiolo, B., Trappe, S.W., Trappe, T.A., Reidy, P.T., 2010.Muscle protein synthesis and gene expression during recovery from aerobicexercise in the fasted and fed states. Am. J. Physiol. Regul. Integr. Comp. Physiol.299, R1254–62.
Harber, M.P., Konopka, A.R., Undem, M.K., Hinkley, J.M., Minchev, K., Kaminsky, L.A.,Trappe, T.A., Trappe, S., 2012. Aerobic exercise training induces skeletal musclehypertrophy and age-dependent adaptations in myofiber function in young andolder men. J. Appl. Physiol. 113, 1495–1504.
Harman, D., 1972. The biologic clock: the mitochondria? J. Am. Geriatr. Soc. 20,145–147.
Henderson, G.C., Dhatariya, K., Ford, G.C., Klaus, K.A., Basu, R., Rizza, R.A., Jensen,M.D., Khosla, S., O’Brien, P., Nair, K.S., 2009. Higher muscle protein synthesis inwomen than men across the lifespan, and failure of androgen administration toamend age-related decrements. FASEB J. 23, 631–641.
Holloszy, J.O., 1967. Biochemical adaptations in muscle. Effects of exercise onmitochondrial oxygen uptake and respiratory enzyme activity in skeletalmuscle. J. Biol. Chem. 242, 2278–2282.
Holloszy, J.O., Coyle, E.F., 1984. Adaptations of skeletal muscle to enduranceexercise and their metabolic consequences. J. Appl. Physiol. 56, 831–838.
Hoppeler, H., Howald, H., Conley, K., Lindstedt, S.L., Claassen, H., Vock, P., Weibel,E.R., 1985. Endurance training in humans: aerobic capacity and structure ofskeletal muscle. J. Appl. Physiol. 59, 320–327.
Houmard, J.A., Weidner, M.L., Gavigan, K.E., Tyndall, G.L., Hickey, M.S., Alshami, A.,1998. Fiber type and citrate synthase activity in the human gastrocnemius andvastus lateralis with aging. J. Appl. Physiol. 85, 1337–1341.
A.R. Konopka, K. Sreekumaran Nair / Molecular and Cellular Endocrinology 379 (2013) 19–29 27

Howald, H., Hoppeler, H., Claassen, H., Mathieu, O., Straub, R., 1985. Influences ofendurance training on the ultrastructural composition of the different musclefiber types in humans. Pflug. Arch 403, 369–376.
Howard, C., Ferrucci, L., Sun, K., Fried, L.P., Walston, J., Varadhan, R., Guralnik, J.M.,Semba, R.D., 2007. Oxidative protein damage is associated with poor gripstrength among older women living in the community. J. Appl. Physiol. 103, 17–20.
Jaleel, A., Short, K.R., Asmann, Y.W., Klaus, K.A., Morse, D.M., Ford, G.C., Nair, K.S.,2008. In vivo measurement of synthesis rate of individual skeletal musclemitochondrial proteins. Am. J. Physiol. Endocrinol. Metab. 295, E1255–68.
Joseph, A.M., Adhihetty, P.J., Buford, T.W., Wohlgemuth, S.E., Lees, H.A., Nguyen,L.M., Aranda, J.M., Sandesara, B.D., Pahor, M., Manini, T.M., Marzetti, E.,Leeuwenburgh, C., 2012. The impact of aging on mitochondrial function andbiogenesis pathways in skeletal muscle of sedentary high- and low-functioningelderly individuals. Aging Cell..
Karakelides, H., Irving, B.A., Short, K.R., O’Brien, P., Nair, K.S., 2010. Age, obesity, andsex effects on insulin sensitivity and skeletal muscle mitochondrial function.Diabetes 59, 89–97.
Kent-Braun, J.A., Ng, A.V., 2000. Skeletal muscle oxidative capacity in young andolder women and men. J. Appl. Physiol. 89, 1072–1078.
Kim, J.S., Cross, J.M., Bamman, M.M., 2005. Impact of resistance loading onmyostatin expression and cell cycle regulation in young and older men andwomen. Am. J. Physiol. Endocrinol. Metab. 288, E1110–9.
Kim, H.S., Patel, K., Muldoon-Jacobs, K., Bisht, K.S., Aykin-Burns, N., Pennington, J.D.,van der Meer, R., Nguyen, P., Savage, J., Owens, K.M., Vassilopoulos, A., Ozden,O., Park, S.H., Singh, K.K., Abdulkadir, S.A., Spitz, D.R., Deng, C.X., Gius, D., 2010.SIRT3 is a mitochondria-localized tumor suppressor required for maintenanceof mitochondrial integrity and metabolism during stress. Cancer Cell 17, 41–52.
Konopka, A.R., Douglass, M.D., Kaminsky, L.A., Jemiolo, B., Trappe, T.A., Trappe, S.,Harber, M.P., 2010. Molecular adaptations to aerobic exercise training inskeletal muscle of older women. J. Gerontol. A Biol. Sci. Med. Sci. 65, 1201–1207.
Konopka, A.R., Trappe, T.A., Jemiolo, B., Trappe, S.W., Harber, M.P., 2011. Myosinheavy chain plasticity in aging skeletal muscle with aerobic exercise training. J.Gerontol. A Biol. Sci. Med. Sci. 66, 835–841.
Kopsidas, G., Kovalenko, S.A., Kelso, J.M., Linnane, A.W., 1998. An age-associatedcorrelation between cellular bioenergy decline and mtDNA rearrangements inhuman skeletal muscle. Mutat. Res. 421, 27–36.
Kovalenko, S.A., Kopsidas, G., Kelso, J.M., Linnane, A.W., 1997. Deltoid humanmuscle mtDNA is extensively rearranged in old age subjects. Biochem. Biophys.Res. Commun. 232, 147–152.
Lanza, I.R., Nair, K.S., 2010. Mitochondrial metabolic function assessed in vivo andin vitro. Curr. Opin. Clin. Nutr. Metab. Care 13, 511–517.
Lanza, I.R., Short, D.K., Short, K.R., Raghavakaimal, S., Basu, R., Joyner, M.J.,McConnell, J.P., Nair, K.S., 2008. Endurance exercise as a countermeasure foraging. Diabetes 57, 2933–2942.
Lanza, I.R., Bhagra, S., Nair, K.S., Port, J.D., 2011. Measurement of human skeletalmuscle oxidative capacity by 31P-MR spectroscopy: a cross-validation within vitro measurements. J. Magn. Reson Imag. 34, 1143–1150.
Lanza, I.R., Zabielski, P., Klaus, K.A., Morse, D.M., Heppelmann, C.J., Bergen 3rd, H.R.,Dasari, S., Walrand, S., Short, K.R., Johnson, M.L., Robinson, M.M., Schimke, J.M.,Jakaitis, D.R., Asmann, Y.W., Sun, Z., Nair, K.S., 2012. Chronic caloric restrictionpreserves mitochondrial function in senescence without increasingmitochondrial biogenesis. Cell Metab. 16, 777–788.
Larsen, R.G., Callahan, D.M., Foulis, S.A., Kent-Braun, J.A., 2012. Age-related changesin oxidative capacity differ between locomotory muscles and are associatedwith physical activity behavior. Appl. Physiol. Nutr. Metab. 37, 88–99.
Lee, C.K., Klopp, R.G., Weindruch, R., Prolla, T.A., 1999. Gene expression profile ofaging and its retardation by caloric restriction. Science 285, 1390–1393.
Leeuwenburgh, C., Fiebig, R., Chandwaney, R., Ji, L.L., 1994. Aging and exercisetraining in skeletal muscle: responses of glutathione and antioxidant enzymesystems. Am. J. Physiol. 267, R439–45.
Leick, L., Wojtaszewski, J.F., Johansen, S.T., Kiilerich, K., Comes, G., Hellsten, Y.,Hidalgo, J., Pilegaard, H., 2008. PGC-1alpha is not mandatory for exercise- andtraining-induced adaptive gene responses in mouse skeletal muscle. Am. J.Physiol. Endocrinol. Metab. 294, E463–74.
Leick, L., Lyngby, S.S., Wojtaszewski, J.F., Pilegaard, H., 2010. PGC-1alpha is requiredfor training-induced prevention of age-associated decline in mitochondrialenzymes in mouse skeletal muscle. Exp. Gerontol. 45, 336–342.
Lexell, J., Henriksson-Larsen, K., Winblad, B., Sjostrom, M., 1983. Distribution ofdifferent fiber types in human skeletal muscles: effects of aging studied inwhole muscle cross sections. Muscle Nerve 6, 588–595.
Lezza, A.M., Boffoli, D., Scacco, S., Cantatore, P., Gadaleta, M.N., 1994. Correlationbetween mitochondrial DNA 4977-bp deletion and respiratory chain enzymeactivities in aging human skeletal muscles. Biochem. Biophys. Res. Commun.205, 772–779.
Ling, C., Poulsen, P., Carlsson, E., Ridderstrale, M., Almgren, P., Wojtaszewski, J.,Beck-Nielsen, H., Groop, L., Vaag, A., 2004. Multiple environmental and geneticfactors influence skeletal muscle PGC-1alpha and PGC-1beta gene expression intwins. J. Clin. Invest. 114, 1518–1526.
Ling, C., Poulsen, P., Simonsson, S., Ronn, T., Holmkvist, J., Almgren, P., Hagert, P.,Nilsson, E., Mabey, A.G., Nilsson, P., Vaag, A., Groop, L., 2007. Genetic andepigenetic factors are associated with expression of respiratory chaincomponent NDUFB6 in human skeletal muscle. J. Clin. Invest. 117, 3427–3435.
Louis, E., Raue, U., Yang, Y., Jemiolo, B., Trappe, S., 2007. Time course of proteolytic,cytokine, and myostatin gene expression after acute exercise in human skeletalmuscle. J. Appl. Physiol. 103, 1744–1751.
Mai, S., Muster, B., Bereiter-Hahn, J., Jendrach, M., 2012. Autophagy proteins LC3B,ATG5 and ATG12 participate in quality control after mitochondrial damage andinfluence lifespan. Autophagy 8, 47–62.
Masiero, E., Agatea, L., Mammucari, C., Blaauw, B., Loro, E., Komatsu, M., Metzger, D.,Reggiani, C., Schiaffino, S., Sandri, M., 2009. Autophagy is required to maintainmuscle mass. Cell Metab. 10, 507–515.
Matsushima, Y., Goto, Y., Kaguni, L.S., 2010. Mitochondrial Lon protease regulatesmitochondrial DNA copy number and transcription by selective degradation ofmitochondrial transcription factor A (TFAM). Proc. Natl. Acad. Sci. USA 107,18410–18415.
McGee, S.L., Hargreaves, M., 2004. Exercise and myocyte enhancer factor 2regulation in human skeletal muscle. Diabetes 53, 1208–1214.
McGee, S.L., Fairlie, E., Garnham, A.P., Hargreaves, M., 2009. Exercise-inducedhistone modifications in human skeletal muscle. J. Physiol. 587, 5951–5958.
Moore, A.Z., Biggs, M.L., Matteini, A., O’Connor, A., McGuire, S., Beamer, B.A., Fallin,M.D., Fried, L.P., Walston, J., Chakravarti, A., Arking, D.E., 2010. Polymorphismsin the mitochondrial DNA control region and frailty in older adults. PLoS One 5,e11069.
Morley, J.E., Abbatecola, A.M., Argiles, J.M., Baracos, V., Bauer, J., Bhasin, S.,Cederholm, T., Coats, A.J., Cummings, S.R., Evans, W.J., Fearon, K., Ferrucci, L.,Fielding, R.A., Guralnik, J.M., Harris, T.B., Inui, A., Kalantar-Zadeh, K., Kirwan,B.A., Mantovani, G., Muscaritoli, M., Newman, A.B., Rossi-Fanelli, F., Rosano,G.M., Roubenoff, R., Schambelan, M., Sokol, G.H., Storer, T.W., Vellas, B., vonHaehling, S., Yeh, S.S., Anker, S.D., 2011. Sarcopenia with limited mobility: aninternational consensus. J. Am. Med. Dir. Assoc. 12, 403–409.
Newman, A.B., Kupelian, V., Visser, M., Simonsick, E., Goodpaster, B., Nevitt, M.,Kritchevsky, S.B., Tylavsky, F.A., Rubin, S.M., Harris, T.B., 2003. Sarcopenia:alternative definitions and associations with lower extremity function. J. Am.Geriatr. Soc. 51, 1602–1609.
Pandorf, C.E., Haddad, F., Wright, C., Bodell, P.W., Baldwin, K.M., 2009. Differentialepigenetic modifications of histones at the myosin heavy chain genes in fast andslow skeletal muscle fibers and in response to muscle unloading. Am. J. Physiol.Cell Physiol. 297, C6–16.
Pansarasa, O., Castagna, L., Colombi, B., Vecchiet, J., Felzani, G., Marzatico, F., 2000.Age and sex differences in human skeletal muscle: role of reactive oxygenspecies. Free Radical Res. 33, 287–293.
Pasiakos, S.M., McClung, H.L., McClung, J.P., Urso, M.L., Pikosky, M.A., Cloutier, G.J.,Fielding, R.A., Young, A.J., 2010. Molecular responses to moderate enduranceexercise in skeletal muscle. Int. J. Sport Nutr. Exerc. Metab. 20, 282–290.
Perry, C.G., Kane, D.A., Lanza, I.R., Neufer, P.D., 2013. Methods for assessingmitochondrial function in diabetes. Diabetes 62, 1041–1053.
Petersen, K.F., Befroy, D., Dufour, S., Dziura, J., Ariyan, C., Rothman, D.L., DiPietro, L.,Cline, G.W., Shulman, G.I., 2003. Mitochondrial dysfunction in the elderly:possible role in insulin resistance. Science 300, 1140–1142.
Picard, M., Ritchie, D., Wright, K.J., Romestaing, C., Thomas, M.M., Rowan, S.L.,Taivassalo, T., Hepple, R.T., 2010. Mitochondrial functional impairment withaging is exaggerated in isolated mitochondria compared to permeabilizedmyofibers. Aging Cell 9, 1032–1046.
Picard, M., Taivassalo, T., Ritchie, D., Wright, K.J., Thomas, M.M., Romestaing, C.,Hepple, R.T., 2011. Mitochondrial structure and function are disrupted bystandard isolation methods. PLoS One 6, e18317.
Picca, A., Fracasso, F., Pesce, V., Cantatore, P., Joseph, A.M., Leeuwenburgh, C.,Gadaleta, M.N., Lezza, A.M., 2012. Age- and calorie restriction-related changesin rat brain mitochondrial DNA and TFAM binding. Age (Dordr)..
Proctor, D.N., Sinning, W.E., Walro, J.M., Sieck, G.C., Lemon, P.W., 1995. Oxidativecapacity of human muscle fiber types: effects of age and training status. J. Appl.Physiol. 78, 2033–2038.
Rasmussen, U.F., Krustrup, P., Kjaer, M., Rasmussen, H.N., 2003a. Experimentalevidence against the mitochondrial theory of aging. A study of isolated humanskeletal muscle mitochondria. Exp. Gerontol. 38, 877–886.
Rasmussen, U.F., Krustrup, P., Kjaer, M., Rasmussen, H.N., 2003b. Human skeletalmuscle mitochondrial metabolism in youth and senescence. no signs offunctional changes in ATP formation and mitochondrial oxidative capacity.Pflug. Arch 446, 270–278.
Raue, U., Slivka, D., Jemiolo, B., Hollon, C., Trappe, S., 2007. Proteolytic geneexpression differs at rest and after resistance exercise between young and oldwomen. J. Gerontol. A Biol. Sci. Med. Sci. 62, 1407–1412.
Robinson, M.M., Hamilton, K.L., Miller, B.F., 2009. The interactions of somecommonly consumed drugs with mitochondrial adaptations to exercise. J.Appl. Physiol. 107, 8–16.
Ronn, T., Poulsen, P., Hansson, O., Holmkvist, J., Almgren, P., Nilsson, P., Tuomi, T.,Isomaa, B., Groop, L., Vaag, A., Ling, C., 2008. Age influences DNA methylationand gene expression of COX7A1 in human skeletal muscle. Diabetologia 51,1159–1168.
Rooyackers, O.E., Adey, D.B., Ades, P.A., Nair, K.S., 1996. Effect of age on in vivo ratesof mitochondrial protein synthesis in human skeletal muscle. Proc. Natl. Acad.Sci. USA 93, 15364–15369.
Rosenberg, I., 1989. Summary comments: epidemiological and methodologicalproblems in determinig nutritional status of older persons. Am. J. Clin. Nutr. 50,1231–1233.
Rosenberg, I.H., 1997. Sarcopenia: origins and clinical relevance. J. Nutr. 127, 990S–991S.
Rossi, P., Marzani, B., Giardina, S., Negro, M., Marzatico, F., 2008. Human skeletalmuscle aging and the oxidative system: cellular events. Curr. Aging Sci. 1, 182–191.
28 A.R. Konopka, K. Sreekumaran Nair / Molecular and Cellular Endocrinology 379 (2013) 19–29

Roth, S.M., Martel, G.F., Ferrell, R.E., Metter, E.J., Hurley, B.F., Rogers, M.A., 2003.Myostatin gene expression is reduced in humans with heavy-resistancestrength training: a brief communication. Exp. Biol. Med. (Maywood) 228,706–709.
Ruas, J.L., White, J.P., Rao, R.R., Kleiner, S., Brannan, K.T., Harrison, B.C., Greene, N.P.,Wu, J., Estall, J.L., Irving, B.A., Lanza, I.R., Rasbach, K.A., Okutsu, M., Nair, K.S., Yan,Z., Leinwand, L.A., Spiegelman, B.M., 2012. A PGC-1alpha isoform induced byresistance training regulates skeletal muscle hypertrophy. Cell 151, 1319–1331.
Ryan, A.S., Ivey, F.M., Prior, S., Li, G., Hafer-Macko, C., 2011. Skeletal musclehypertrophy and muscle myostatin reduction after resistive training in strokesurvivors. Stroke 42, 416–420.
Safdar, A., Hamadeh, M.J., Kaczor, J.J., Raha, S., Debeer, J., Tarnopolsky, M.A., 2010.Aberrant mitochondrial homeostasis in the skeletal muscle of sedentary olderadults. PLoS One 5, e10778.
Safdar, A., Little, J.P., Stokl, A.J., Hettinga, B.P., Akhtar, M., Tarnopolsky, M.A., 2011.Exercise increases mitochondrial PGC-1alpha content and promotes nuclear-mitochondrial cross-talk to coordinate mitochondrial biogenesis. J. Biol. Chem.286, 10605–10617.
Semba, R.D., Ferrucci, L., Sun, K., Walston, J., Varadhan, R., Guralnik, J.M., Fried, L.P.,2007a. Oxidative stress and severe walking disability among older women. Am.J. Med. 120, 1084–1089.
Semba, R.D., Ferrucci, L., Sun, K., Walston, J., Varadhan, R., Guralnik, J.M., Fried, L.P.,2007b. Oxidative stress is associated with greater mortality in older womenliving in the community. J. Am. Geriatr. Soc. 55, 1421–1425.
Seo, A.Y., Joseph, A.M., Dutta, D., Hwang, J.C., Aris, J.P., Leeuwenburgh, C., 2010. Newinsights into the role of mitochondria in aging: mitochondrial dynamics andmore. J. Cell Sci. 123, 2533–2542.
Short, K.R., Vittone, J.L., Bigelow, M.L., Proctor, D.N., Rizza, R.A., Coenen-Schimke,J.M., Nair, K.S., 2003. Impact of aerobic exercise training on age-related changesin insulin sensitivity and muscle oxidative capacity. Diabetes 52, 1888–1896.
Short, K.R., Vittone, J.L., Bigelow, M.L., Proctor, D.N., Nair, K.S., 2004. Age and aerobicexercise training effects on whole body and muscle protein metabolism. Am. J.Physiol. Endocrinol. Metab. 286, E92–101.
Short, K.R., Bigelow, M.L., Kahl, J., Singh, R., Coenen-Schimke, J., Raghavakaimal, S.,Nair, K.S., 2005a. Decline in skeletal muscle mitochondrial function with agingin humans. Proc. Natl. Acad. Sci. USA 102, 5618–5623.
Short, K.R., Vittone, J.L., Bigelow, M.L., Proctor, D.N., Coenen-Schimke, J.M., Rys, P.,Nair, K.S., 2005b. Changes in myosin heavy chain mRNA and protein expressionin human skeletal muscle with age and endurance exercise training. J. Appl.Physiol. 99, 95–102.
Slivka, D.R., Dumke, C.L., Tucker, T.J., Cuddy, J.S., Ruby, B., 2012. Human mRNAresponse to exercise and temperature. Int. J. Sports Med. 33, 94–100.
Someya, S., Yu, W., Hallows, W.C., Xu, J., Vann, J.M., Leeuwenburgh, C., Tanokura, M.,Denu, J.M., Prolla, T.A., 2010. Sirt3 mediates reduction of oxidative damage andprevention of age-related hearing loss under caloric restriction. Cell 143, 802–812.
Tonkonogi, M., Fernstrom, M., Walsh, B., Ji, L.L., Rooyackers, O., Hammarqvist, F.,Wernerman, J., Sahlin, K., 2003. Reduced oxidative power but unchangedantioxidative capacity in skeletal muscle from aged humans. Pflug. Arch 446,261–269.
Trappe, S., Godard, M., Gallagher, P., Carroll, C., Rowden, G., Porter, D., 2001.Resistance training improves single muscle fiber contractile function in olderwomen. Am. J. Physiol. Cell. Physiol. 281, C398–406.
Trappe, S., Gallagher, P., Harber, M., Carrithers, J., Fluckey, J., Trappe, T., 2003. Singlemuscle fibre contractile properties in young and old men and women. J. Physiol552, 47–58.
Trappe, T., Williams, R., Carrithers, J., Raue, U., Esmarck, B., Kjaer, M., Hickner, R.,2004. Influence of age and resistance exercise on human skeletal muscleproteolysis: a microdialysis approach. J. Physiol. 554, 803–813.
Trappe, S., Hayes, E., Galpin, A.J., Kaminsky, L.A., Jemiolo, B., Fink, W.J., Trappe, T.A.,Jansson, A., Gustafsson, T., Tesch, P.A., 2012. New records in aerobic poweramong octogenarian lifelong endurance athletes. J. Appl. Physiol..
Trounce, I., Byrne, E., Marzuki, S., 1989. Decline in skeletal muscle mitochondrialrespiratory chain function: possible factor in ageing. Lancet 1, 637–639.
von Walden, F., Jakobsson, F., Edstrom, L., Nader, G.A., 2012. Altered autophagy geneexpression and persistent atrophy suggest impaired remodeling in chronichemiplegic human skeletal muscle. Muscle Nerve 46, 785–792.
Waters, D.L., Mullins, P.G., Qualls, C.R., Raj, D.S., Gasparovic, C., Baumgartner, R.N.,2009. Mitochondrial function in physically active elders with sarcopenia. Mech.Ageing Dev. 130, 315–319.
Wenz, T., 2011. Mitochondria and PGC-1alpha in aging and age-associated diseases.J. Aging Res. 2011, 810619.
Wenz, T., Rossi, S.G., Rotundo, R.L., Spiegelman, B.M., Moraes, C.T., 2009. Increasedmuscle PGC-1alpha expression protects from sarcopenia and metabolic diseaseduring aging. Proc. Natl. Acad. Sci. USA 106, 20405–20410.
Westphal, C.H., Dipp, M.A., Guarente, L., 2007. A therapeutic role for sirtuins indiseases of aging? Trends Biochem. Sci. 32, 555–560.
White, A.T., Schenk, S., 2012. NAD(+)/NADH and skeletal muscle mitochondrialadaptations to exercise. Am. J. Physiol. Endocrinol. Metab. 303, E308–21.
Wilkinson, S.B., Phillips, S.M., Atherton, P.J., Patel, R., Yarasheski, K.E., Tarnopolsky,M.A., Rennie, M.J., 2008. Differential effects of resistance and enduranceexercise in the fed state on signalling molecule phosphorylation and proteinsynthesis in human muscle. J. Physiol. 586, 3701–3717.
Williamson, D.L., Raue, U., Slivka, D.R., Trappe, S., 2010. Resistance exercise, skeletalmuscle FOXO3A, and 85-year-old women. J. Gerontol. A Biol. Sci. Med. Sci. 65,335–343.
Wright, D.C., Han, D.H., Garcia-Roves, P.M., Geiger, P.C., Jones, T.E., Holloszy, J.O.,2007. Exercise-induced mitochondrial biogenesis begins before the increase inmuscle PGC-1alpha expression. J. Biol. Chem. 282, 194–199.
Zhang, C., Cuervo, A.M., 2008. Restoration of chaperone-mediated autophagy inaging liver improves cellular maintenance and hepatic function. Nat. Med. 14,959–965.
Zucchini, C., Pugnaloni, A., Pallotti, F., Solmi, R., Crimi, M., Castaldini, C., Biagini, G.,Lenaz, G., 1995. Human skeletal muscle mitochondria in aging: lack ofdetectable morphological and enzymic defects. Biochem. Mol. Biol. Int. 37,607–616.
Zwetsloot, K.A., Laye, M.J., Booth, F.W., 2009. Novel epigenetic regulation of skeletalmuscle myosin heavy chain genes. Focus on ‘‘Differential epigeneticmodifications of histones at the myosin heavy chain genes in fast and slowskeletal muscle fibers and in response to muscle unloading’’. Am. J. Physiol. CellPhysiol. 297, C1–3.
A.R. Konopka, K. Sreekumaran Nair / Molecular and Cellular Endocrinology 379 (2013) 19–29 29

The role of weight loss and exercise in correcting skeletal musclemitochondrial abnormalities in obesity, diabetes and aging
Frederico G.S. Toledo, Bret H. Goodpaster ⇑
Division of Endocrinology and Metabolism, Department of Medicine, School of Medicine, University of Pittsburgh, Pittsburgh, PA, United States
a r t i c l e i n f o
Article history:Available online 20 June 2013
Keywords:MitochondriaWeight lossExercisePhysical activitySkeletal muscleObesity
a b s t r a c t
Mitochondria within skeletal muscle have been implicated in insulin resistance of obesity and type 2 dia-betes mellitus as well as impaired muscle function with normal aging. Evaluating the potential of inter-ventions to improve mitochondria is clearly relevant to the prevention or treatment of metabolic diseasesand age-related dysfunction. This review provides an overview and critical evaluation of the effects ofweight loss and exercise interventions on skeletal muscle mitochondria, along with implications for insu-lin resistance, obesity, type 2 diabetes and aging. The available literature strongly suggests that the lowermitochondrial capacity associated with obesity, type 2 diabetes and aging is not an irreversible lesion.However, weight loss does not appear to affect this response, even when the weight loss is extreme. Incontrast, increasing physical activity improves mitochondrial content and perhaps the function of indi-vidual mitochondrion. Despite the consistent effect of exercise to improve mitochondrial capacity, stud-ies mechanistically linking mitochondria to insulin resistance, reductions in intramyocellular lipid orimprovement in muscle function remain inconclusive. In summary, studies of diet and exercise traininghave advanced our understanding of the link between mitochondrial oxidative capacity and insulin resis-tance in obesity, type 2 diabetes and aging. Nevertheless, additional inquiry is necessary to establish thesignificance and clinical relevance of those perturbations, which could lead to targeted therapies for amyriad of conditions and diseases involving mitochondria.
! 2013 Elsevier Ireland Ltd. All rights reserved.
1. Introduction
Mitochondria within skeletal muscle (SkM) provide energy re-quired for contraction, and by extension, mobility and the abilityto perform physical work. To support this primary role of skeletalmuscle, mitochondria are also critical to other essential myocellu-lar functions, including storage and utilization of fuel, primarilyglucose and fatty acids, as well as cell signaling and modulatingoxidative stress. Therefore, it is not surprising that mitochondriawithin skeletal muscle have been implicated in aging as well asinsulin resistance (IR) of obesity and type 2 diabetes mellitus(T2DM). Targeting mitochondria with interventions to prevent,attenuate, or treat aging, age-related diseases and metabolic dis-eases and dysfunction could then have important public healthimplications. The primary purpose of this review is to provide anobjective overview and critical evaluation of studies examiningthe effects of weight loss and exercise interventions on skeletalmuscle mitochondria, along with implications for deranged energymetabolism, most notably IR, obesity, T2DM and aging.
2. A potential role for mitochondria in the pathophysiology ofskeletal muscle insulin resistance
Despite a great deal of progress that has been made in unravel-ing the mechanisms behind the etiology of IR, its pathophysiologyremains far from clear. This is due in part to the recognized multi-plicity of factors that contribute to the development of IR. No singledisturbance exclusively explains the pathophysiology of this con-dition. For instance, both genetic and a number of acquired factors(e.g., obesity, sedentary lifestyle, and neurohormonal influences)work in concert to modulate insulin sensitivity in organs such asliver and muscle, which are responsible for partitioning glucoseand maintaining normal plasma glucose homeostasis. Therefore,several players participate in the pathophysiology of IR. In the pastdecade, mitochondria have emerged as an additional player in IRassociated with obesity, T2DM, and perhaps aging.
Although mitochondria have been reported as abnormal or‘‘dysfunctional’’ in insulin-resistant states and aging, their exactrole in glucose homeostasis and fuel metabolism is not completelyunderstood. Nevertheless, in the context of IR of obesity, T2DM andaging, there have been great advances in our understanding of howmitochondria react to weight loss and to physical activity. These
0303-7207/$ - see front matter ! 2013 Elsevier Ireland Ltd. All rights reserved.http://dx.doi.org/10.1016/j.mce.2013.06.018
⇑ Corresponding author. Address: University of Pittsburgh, 3459 Fifth Avenue,MUH N810, Pittsburgh, PA 15213, United States. Tel.: +1 412 692 2848; fax: +1 412692 2165.
E-mail address: [email protected] (B.H. Goodpaster).
Molecular and Cellular Endocrinology 379 (2013) 30–34
Contents lists available at SciVerse ScienceDirect
Molecular and Cellular Endocrinology
journal homepage: www.elsevier .com/locate /mce

advances have shed light on the relationship between mitochon-dria and fuel metabolism.
The objective of this review is to give the reader an overview ofwhat has been learned from human studies that have investigatedhow skeletal muscle mitochondria adapt and react to changes inmetabolism induced by diet and exercise in the context of glucosemetabolism. This review will focus predominantly on human SkMstudies for two reasons: (a) Reports of abnormal mitochondrialcapacity in SkM have direct relevance to human disease; and (b)While the association between mitochondria and obesity-inducedIR has been replicated numerous times in humans, animal datahas been less consistent and probably reflective of interspecies dif-ferences between animals and humans.
2.1. Terminology
Terms such as ‘‘mitochondrial dysfunction’’ (Petersen et al.,2003; Petersen et al., 2004) and ‘‘mitochondrial impairments’’ (Kel-ley et al., 2002) have been commonly employed in the obesity, dia-betes, and physiology of aging literature. However, this reviewfavors avoiding those terminologies, because they are potentiallyconfusing for a couple of reasons. First, ‘‘dysfunction’’ impliespathology in SkM, but it is far from established whether alteredmitochondria reflect a physiological adaptation, pathological mal-adaptation, or primarily a pathological phenomenon. Second, thereis a multiplicity of mitochondrial functions in cell biology. Mito-chondrial function can be measured in terms of ATP generation,substrate oxidation, intracellular calcium buffering, induction ofapoptosis, to name a few. Therefore, the term mitochondrial ‘‘func-tion’’ can be imprecise unless clearly defined. In this review, mito-chondrial function specifically refers to the function of fueloxidation. Furthermore and equally important, the total mitochon-drial oxidative capacity of a cell depends on not only its total mito-chondrial content, but also on the functional capacity of eachmitochondrion (i.e. ‘‘intrinsic mitochondrial function’’). Whenreferring to mitochondrial ‘‘function’’ or ‘‘dysfunction’’, it may notbe always obvious whether it refers to either a deficit in total oxi-dative capacity, or to the intrinsic function of each mitochondrion.Since the total oxidative capacity of a cell depends on both contentand function of mitochondria, we prefer to employ the term mito-chondrial capacity, as adopted in previous studies (Toledo et al.,2006; Toledo et al., 2007; Toledo et al., 2008), to denote the globalintegrated components of content and function, which is a morerelevant parameter for cell metabolism. Thus, whenever appropri-ate, mitochondrial function per individual mitochondrion or mito-chondrial content will be specified. It should also be noted that theterm ‘mitochondrial capacity’ reflects the maximal cellular capacityfor oxidation in SkM. Therefore, the term distinctively does not ap-ply to situations where measurements occur in sub-maximal con-ditions of metabolic demand (e.g. muscle at rest); in thoseinstances mitochondrial activity for a given condition, rather thanmaximal capacity, is being quantified.
2.2. Are mitochondria abnormal in insulin-resistant skeletal muscle?
At a cellular level, a common feature of IR is the presence of in-creased lipid accumulation in insulin-responsive tissues such as li-ver and SkM. This ectopic fat accumulation helps explain whyobesity and lipodystrophy are associated with IR: when adiposetissue capacity to store lipids is sub-optimal, lipid is ectopicallystored in SkM and liver, but this ectopic fat disrupts substrate uti-lization in these tissues, leading to IR. While excess intramyocellu-lar lipid (IMCL) has been clearly associated with IR, and excess lipidsupply to muscle certainly plays a role in conditions of energy ex-cess, high-fat diet and obesity, the underlying cellular mechanismsfor inappropriate accumulation of lipids during physiological con-
ditions are much less clear. Since lipids are oxidized in mitochon-dria, one such factor could theoretically be the overallmitochondrial capacity of SkM. It has been theorized that if defi-cient, a reduced mitochondrial capacity might predispose to lipidaccumulation and thus aggravate IR (Lowell and Shulman, 2005).
Since the pioneering studies by Randle and colleagues in the1960s (Randle et al., 1963) supporting a model of fuel competitionand IR, there have been numerous investigations into the role offuel selection in the etiology of muscle IR (for a review see Kelleyand Mandarino, 2000). Many of these earlier studies revealedimpairments in fatty acid oxidation, lower mitochondrial enzymeactivities and lower expression of genes related to oxidative capac-ity within skeletal muscle in obesity and T2DM (Hulver et al., 2003;Kelley et al., 1999; Kim et al., 2000; McGarry, 1995; Simoneauet al., 1999; Mootha et al., 2003; Patti et al., 2003).
3. Effects of weight loss and exercise training on mitochondrialoxidative capacity in insulin-resistant obesity
While a lower mitochondrial oxidative capacity observed ininsulin-resistant subjects has been consistently demonstrated, itspathophysiological significance remains unsettled. To date, it isnot clear whether it represents a pathological defect or a physio-logical adaptation. Favoring the notion that it represents a patho-logical state, the term ‘‘mitochondrial dysfunction’’ has beenproposed (Petersen et al., 2003; Kelley et al., 2002). In support ofthis hypothesis, signs of mitochondrial abnormalities were re-ported in lean healthy subjects with a parental history of type 2diabetes, raising the possibility of an inheritable etiology (Petersenet al., 2004). However, others have proposed that the lower oxida-tive capacity in IR is not necessarily a form of mitochondrialpathology and may represent a consequence of the insulin-resis-tant state or stress induced by nutrient overload (Stump et al.,2003; Anderson et al., 2009). While it remains unclear whetherthe reduction in oxidative capacity represents either a defect oran adaptation, the extent to which it is either reversible or anenduring defect has now been well characterized by interventionalstudies that are discussed in this review. Examining how mito-chondria respond to weight loss, exercise training, and insulin sen-sitizers has broadened our understanding of mitochondrial biologyin IR.
One of the earliest studies to suggest that significant mitochon-drial plasticity is preserved in the obese/insulin-resistant stateshowed that overall oxidative capacity in SkM can be improvedby lifestyle modifications typically recommended for obesity(Menshikova et al., 2005). In a 16-week lifestyle modification pro-gram consisting of reduced calorie intake and weekly moderate-intensity aerobic training, obese non-diabetic volunteers experi-enced a 9.7% weight loss and significant improvements in whole-body aerobic capacity, insulin sensitivity and whole-body fat oxi-dation. In parallel with these changes, total NADH oxidase and suc-cinate oxidase activities were increased after the intervention,denoting improved electron-transport chain oxidative capacityand remodeling of mitochondrial oxidative capacity. However,mtDNA content was not significantly increased in response to theintervention, suggesting impaired biogenesis with intact functionalremodeling of mitochondria. In line with the notion of subnormalbiogenesis, citrate synthase (a surrogate marker of mitochondrialcontent) was unchanged in half of the participants in that study.Similarly, citrate synthase was also unchanged in the CALERIEstudy, in which overweight volunteers underwent either caloricrestriction or caloric restriction with exercise. In both instances,citrate synthase activity did not increase (Civitarese et al., 2007).
The uncertainty surrounding the effect of those interventionson mitochondrial content expansion may be in part attributable
F.G.S. Toledo, B.H. Goodpaster / Molecular and Cellular Endocrinology 379 (2013) 30–34 31

to methodological reasons. The tight cytoskeleton apparatus ofSkM represents a technical challenge for isolation of mitochondriaand pure mitochondrial preparations without contaminants arenot easy to obtain. Furthermore, mitochondria can be functionallyharmed during isolation methods resulting in potentially mislead-ing results (Picard et al., 2010; Picard et al., 2011), For instance,mtDNA has been shown to be a poor marker of mitochondrial con-tent (Larsen et al., 2012). Finally, at least in some instances citratesynthase can be regulated by exercise in a manner disconnected tomitochondrial content (Tonkonogi et al., 1997). The first unequiv-ocal demonstration that mitochondrial content expands in re-sponse to lifestyle modifications in obesity/IR was made possibleby studies employing transmission electron microscopy withquantitative stereologic analysis (Toledo et al., 2006). The advan-tage of that approach is that mitochondrial content is measuredin situ, therefore overcoming the issues of preparation purity, func-tional damage, and modulation of enzyme activity independent ofenzyme content. Using that approach, it was found that SkM mito-chondrial content increased on average by 42% after weight lossand exercise training (Toledo et al., 2006). Mitochondrial morphol-ogy was also affected, noted by a 19% increase in mitochondrialsize. In that study, both mitochondrial content and size stronglycorrelated with the degree of change in insulin sensitivity(r = 0.72 and r = 0.68, respectively). While not necessarily suggest-ing causality, it reinforced the notion of a tight link between mito-chondria and IR. However, as will be discussed later in this review,the link between mitochondria and insulin resistance can some-times be dissociated.
3.1. Intervention effects in T2DM
In the spectrum of obesity and IR, the most severe impairmentsin mitochondrial content seem to occur in T2DM (Chomentowskiet al., 2011). Subjects with T2DM also display the greatest degreesof derangements in insulin sensitivity in SkM and the greatestIMCL lipid accumulation. They also have hyperglycemia, whichmight conceivably be another insult to mitochondria. But as dem-onstrated by interventional studies, even subjects with T2DM re-tain a substantial capacity for increasing mitochondrialbiogenesis in response to simple lifestyle modifications. In a studyinvolving subjects with T2DM, a 4-month intervention consistingof diet to achieve weight loss and daily exercise training resultedin robust improvements in SkM mitochondrial oxidative capacity(Toledo et al., 2007). Mitochondrial content measured by quantita-tive TEM, citrate synthase, and the activity of NADH oxidase wereall increased by the intervention. While many factors unrelated tomitochondria are responsible for improvements in blood glucoselevels in diabetic subjects after that type of intervention, that studyalso reported a relationship between changes in SkM mitochondriaand hyperglycemia as measured by HbA1c. In line with this obser-vation, Fritz et al. reported that skeletal muscle adaptations of in-creased oxidative gene expression induced by low-intensityexercise are a correlate of systemic metabolic improvements intype 2 diabetes, including insulin sensitivity (Fritz et al., 2006).While causality is difficult to establish with those types of observa-tions, those studies reveal a still poorly-understood relationshipbetween mitochondria in SkM and systemic metabolism.
The aforementioned studies have collectively demonstratedthat in IR mitochondria are not irreversibly impaired, and that atleast partial amelioration of this abnormality can be achieved bylifestyle modifications that are typically recommended to adultswith IR. However, it is also important to consider that both dietarycaloric restriction and exercise are stimuli for a negative caloricbalance and that while weight loss may reduce IMCL lipid content,chronic exercise increases it (Dube et al., 2008; Goodpaster et al.,2001; Pruchnic et al., 2004). Therefore, it is important to consider
whether weight loss and exercise training have independent ef-fects upon mitochondrial plasticity.
3.2. Separate effects of weight loss and exercise on mitochondria
In normal healthy SkM, exercise training is a potent stimulus formitochondrial biogenesis. Therefore, it stands to reason that exer-cise training may be the key factor necessary for stimulating mito-chondrial biogenesis in IR. On the other hand, the distinctpossibility that mitochondrial dysfunction may be secondary to ex-cess lipid accumulation in SkM has also been proposed and thusweight loss per se might also conceivably influence mitochondrialdysfunction. In a study that compared the relative contribution ofexercise training versus that of weight loss, overweight and obesesubjects with insulin resistance were randomized to either diet-in-duced weight loss, or diet-induced weight loss combined withexercise training (Toledo et al., 2008). Both groups experiencedcomparable degrees of total body weight loss, fat mass loss, andcomparable improvements in SkM insulin sensitivity. However,only the group that combined training with caloric restrictionexperienced an improvement in mitochondrial content and respi-ratory chain enzymatic activity, demonstrating that exercise train-ing, not weight loss, is the key factor responsible for mitochondrialplasticity. Subsequent studies have confirmed that exercise train-ing can increase SkM mitochondrial content in insulin-resistantsubjects with and without T2DM (Meex et al., 2010; Phielixet al., 2010).
Although it has now been well established that exercise train-ing per se improves mitochondrial content in IR, it is less clearwhether intrinsic mitochondrial function improves too. In studiesfrom our group, exercise training for 16–20 weeks resulted in en-hanced electron transport chain activity that exceeded changes inmitochondrial mtDNA content and citrate synthase activity, sug-gesting that training results in improvements in total oxidativecapacity that exceed that expected from an increase in mitochon-drial content alone (Toledo et al., 2007; Menshikova et al., 2005;Toledo et al., 2008). However, at least one study concluded thatintrinsic function per mitochondrion does not improve with train-ing: subjects with T2DM and BMI-matched control individualsenrolled in a 12-week exercise program and mitochondrial func-tion was assessed by high-resolution respirometry in permeabili-zed muscle fibers (Phielix et al., 2010). When mitochondrialrespiratory rates were adjusted for mtDNA content, no improve-ments in mitochondrial function after exercise training were ob-served. However, compared to earlier studies (Toledo et al.,2006; Toledo et al., 2007; Menshikova et al., 2005; Toledo et al.,2008), this study had a relative shorter duration of training(12 weeks versus 16–20 weeks), a lower exercise training dose,and included a combination of aerobic and resistance exercise.It is likely that a certain threshold of duration of aerobic training,exercise frequency and intensity, or a combination of these, mustbe achieved in order to enhance intrinsic mitochondrial function,and may explain differences in the training response among stud-ies. Therefore, a conservative interpretation of the current studiespublished so far is that intrinsic mitochondrial function does notalways improve, but may do so in certain circumstances depend-ing on the type and duration of training, and the frequency andintensity of exercise bouts. Clearly, more research is needed inthis field in order to establish what the minimum exercise train-ing prescription should be in order to achieve enhancement ofintrinsic mitochondrial function.
The effects of weight loss in improving obesity-related insulinresistance are well established, but less is known about the impactof weight loss on SkM mitochondria. This relatively paucity of datais not surprising since mitochondrial abnormalities in obesity/IRhave only been appreciated relatively recently. The majority of
32 F.G.S. Toledo, B.H. Goodpaster / Molecular and Cellular Endocrinology 379 (2013) 30–34

studies published so far show that weight loss by dietary caloricrestriction does not reverse the lower mitochondrial capacity ob-served in IR, including in response to degrees of weight lossdeemed clinically significant for glucose and lipid metabolism. Inan older study, Kern et al. suggested an increase in succinate dehy-drogenase (SDH) activity in SkM of obese women who had under-gone moderate weight loss (Kern et al., 1999). However, it is notentirely clear if the SDH activity increased in response to concom-itant changes in physical activity since the study did not control forphysical activity and no objective metric of aerobic capacity wasreported. Simoneau et al. studied muscle biopsy samples from ob-ese volunteers who experienced significant weight loss (14–16% ofbaseline weight) and observed no improvements in enzymaticmarkers of mitochondria, namely citrate synthase and CPT-I, sug-gesting no effect on mitochondria (Simoneau et al., 1999). Cyto-chrome oxidase and beta-hydroxyacyl CoA dehydrogenaseactivities decreased significantly in women, but not in men, leavingsome doubt about the uniformity of mitochondrial response toweight loss.
We have conducted a more comprehensive assessment of theimpact of weight loss per se on both mitochondrial content andfunction in the insulin resistant state associated with obesity (To-ledo et al., 2008). Non-diabetic insulin resistant obese subjects lost10.8% of their initial weight with moderate caloric restriction,which was associated with a nearly 30% improvement in insulinsensitivity. Subjects were instructed not to change their levels ofphysical activity and, accordingly, maximal aerobic capacity didnot change. Despite marked weight loss and improved insulin sen-sitivity, mitochondrial content did not change as assessed by quan-titative TEM. Other markers of mitochondrial content, such asmtDNA copy number and cardiolipin content (a marker of inner-mitochondrial membrane mass), were not changed either. NADH-oxidase was also unaffected, indicating no changes in mitochon-drial function. The lack of changes in mitochondrial content andfunction occurred in spite of a robust decrease in IR in SkM. Theseobservations suggest that the lower oxidative capacity in obesity/IR cannot be explained solely as consequence of IR. This observa-tion is relevant because experimental evidence suggests that acuteinsulin signaling in SkM lowers mitochondrial oxidative capacity(Asmann et al., 2006).
Another important finding from this study was that mitochon-drial oxidative capacity did not change in spite of a reduction inIMCL content, and therefore suggests that the lower oxidativecapacity in obesity/IR is unlikely to be a consequence of excess li-pid accumulation per se. Alternatively, the same result could beinterpreted as an indication that perhaps greater degrees of caloricrestriction are necessary for mitochondrial recovery. This does not,however, seem to the case. In a study by Berggren and colleagues,mitochondrial fatty acid oxidation was measured by incubation ofskeletal muscle homogenates with [1-14C]palmitate and measuring14CO2 production (Berggren et al., 2008). Mitochondrial fatty acidoxidation in obese women who had marked weight loss (about50 kg) was similar to that of extremely obese subjects. Moreover,SkM fatty acid oxidation did not change in extremely obese womenafter 1 year of weight loss (mean 55 kg lost). There were also nochanges in mRNA content for PDK4, CPT I, and PGC-1a, suggestingthat the transcriptional program for mitochondrial biogenesis isnot activated by weight loss. Therefore, even significantly profoundweight loss does not seem to result in amelioration of mitochon-drial oxidative capacity. In fact, some studies suggest that oxidativepathways may even be reduced by weight loss. After biliopancreat-ic diversion surgery for morbid obesity, weight loss reduced theexpression of peroxisome proliferator-activated receptor-a(!46.7%), carnitine palmitoyltransferase-1B (!43.1%), acyl-CoAoxidase 1 (!37.8%), and acetyl-CoA carboxylase B (!48.7%) (Fabriset al., 2004).
4. Effects of weight loss and exercise on mitochondria in aging
Regardless of whether or not mitochondria are mechanisticallylinked with IR, there is little argument that mitochondria likelyplay an important role in altered energy metabolism with aging.The effects of exercise to increase mitochondria content and capac-ity in older humans are also generally very consistent (Pruchnicet al., 2004; Jubrias et al., 2001; Menshikova et al., 2006; Orlanderand Aniansson, 1980; Rimbert et al., 2004; Short et al., 2003;Waters et al., 2003). However, the separate effect of weight lossand exercise on mitochondria content and performance in olderhumans is not known. Indeed, there is some evidence to suggestthat aging is associated with a blunted response to interventionsknown to increase mitochondria (Reznick et al., 2007).
A decline in mitochondria content and/or function often paral-lels the loss of muscle mass and function with age. Only until re-cently, however, have studies been conducted – in cell systemsand animal models – to provide mechanistic evidence linkingmitochondria with muscle growth/atrophy signaling, autophagyand sarcopenia (Masiero et al., 2009; Romanello et al., 2010; Wenzet al., 2009). A conundrum for older obese men and women is thattraditional diet-induced weight loss programs can result in notonly loss of adipose tissue but also a significant loss of muscle(Chomentowski et al., 2009). How this potentially translates intofurther decrements in muscle function is not clear.
The CALERIE study reported that energy restriction-inducedweight loss increased expression of oxidative phosphorylationgenes in SkM (Civitarese et al., 2007), although the related enzymeactivities were unchanged. Moreover, the average age of their sub-jects was <60 years old (39–41). Subjects in the CALERIE studywere not obese, and thus not representative of the typical obeseinsulin-resistant phenotype in which a lower mitochondrial oxida-tive capacity has been mostly reported. We have reported in a ran-domized trial that diet-induced weight loss fails to increasemarkers of mitochondrial oxidative capacity in overweight to ob-ese older men and women (Dube et al., 2011). This was in contrastto an improvement in mitochondrial enzyme activity in those whocompleted an exercise-training program without significantweight loss. Although further evidence is clearly needed to deter-mine the effects of weight loss on mitochondria in the elderly,the limited evidence is consistent with that observed for middle-aged men adults. Based on the high prevalence of older adultsattempting to lose weight with dieting, it is imperative to provideadditional objective evidence concerning the pros and cons ofweight loss in this population.
5. Conclusions
In summary, the lower mitochondrial capacity associated withobesity and T2DM is not an irreversible lesion: substantial plastic-ity of mitochondrial biogenesis is retained in the insulin resistantstate. However, weight loss does not appear to significantly affectthis response, even when the weight loss is extreme. In contrast,increasing physical activity improves mitochondrial content andperhaps oxidative function of individual mitochondrion as well.These biological responses are not triggered by amelioration ofthe insulin-resistant state or a reduction in IMCL content, but likelya reflection of a concerted biological response to chronic contrac-tile activity induced by exercise.
Studies of diet and exercise training have advanced our under-standing of the link between perturbations in mitochondrial oxida-tive capacity and the insulin resistant state seen in obesity, T2DM,and aging. Nevertheless, a complete picture of the role of mito-chondria in T2DM and aging remains a work in progress. Morestudies are necessary to establish the relative impact and
F.G.S. Toledo, B.H. Goodpaster / Molecular and Cellular Endocrinology 379 (2013) 30–34 33

significance of those mitochondrial perturbations, which couldlead to targeted therapies for these conditions.
References
Anderson, E.J., Lustig, M.E., Boyle, K.E., Woodlief, T.L., Kane, D.A., Lin, C.T., Price 3rd,J.W., Kang, L., Rabinovitch, P.S., Szeto, H.H., Houmard, J.A., Cortright, R.N.,Wasserman, D.H., Neufer, P.D., 2009. Mitochondrial H2O2 emission and cellularredox state link excess fat intake to insulin resistance in both rodents andhumans. J. Clin. Invest. 119, 573–581.
Asmann, Y.W., Stump, C.S., Short, K.R., Coenen-Schimke, J.M., Guo, Z., Bigelow, M.L.,Nair, K.S., 2006. Skeletal muscle mitochondrial functions, mitochondrial DNAcopy numbers, and gene transcript profiles in type 2 diabetic and nondiabeticsubjects at equal levels of low or high insulin and euglycemia. Diabetes 55,3309–3319.
Berggren, J.R., Boyle, K.E., Chapman, W.H., Houmard, J.A., 2008. Skeletal muscle lipidoxidation and obesity: influence of weight loss and exercise. Am. J. Physiol.Endocrinol. Metab. 294, E726–E732.
Chomentowski, P., Dube, J.J., Amati, F., Stefanovic-Racic, M., Zhu, S., Toledo, F.G.S.,Goodpaster, B.H., 2009. Moderate exercise attenuates the loss of skeletal musclemass that occurs with intentional caloric restriction-induced weight loss in older,overweight to obese adults. J. Gerontol. Ser. A – Biol. Sci. Med. Sci. 64, 575–580.
Chomentowski, P., Coen, P.M., Radikova, Z., Goodpaster, B.H., Toledo, F.G., 2011.Skeletal muscle mitochondria in insulin resistance: differences inintermyofibrillar versus subsarcolemmal subpopulations and relationship tometabolic flexibility. J. Clin. Endocrinol. Metab. 96, 494–503.
Civitarese, A.E., Carling, S., Heilbronn, L.K., Hulver, M.H., Ukropcova, B., Deutsch,W.A., Smith, S.R., Ravussin, E., Team, C.P., 2007. Calorie restriction increasesmuscle mitochondrial biogenesis in healthy humans. PLoS Med. 4, e76.
Dube, J.J., Amati, F., Stefanovic-Racic, M., Toledo, F.G.S., Sauers, S.E., Goodpaster, B.H.,2008. Exercise-induced alterations in intramyocellular lipids and insulinresistance: the athlete’s paradox revisited. Am. J. Physiol. Endocrinol. Metab.294, E882.
Dube, J.J., Amati, F., Toledo, F.G., Stefanovic-Racic, M., Rossi, A., Coen, P., Goodpaster,B.H., 2011. Effects of weight loss and exercise on insulin resistance, andintramyocellular triacylglycerol, diacylglycerol and ceramide. Diabetologia 54,1147–1156.
Fabris, R., Mingrone, G., Milan, G., Manco, M., Granzotto, M., Pozza, A.D., Scarda, A.,Serra, R., Greco, A.V., Federspil, G., Vettor, R., 2004. Further lowering of musclelipid oxidative capacity in obese subjects after biliopancreatic diversion. J. Clin.Endocrinol. Metab. 89, 1753–1759.
Fritz, T., Kramer, D.K., Karlsson, H.K., Galuska, D., Engfeldt, P., Zierath, J.R., Krook, A.,2006. Low-intensity exercise increases skeletal muscle protein expression ofPPARdelta and UCP3 in type 2 diabetic patients. Diabetes Metab. Res. Rev. 22,492–498.
Goodpaster, B.H., He, J., Watkins, S., Kelley, D.E., 2001. Skeletal muscle lipid contentand insulin resistance: evidence for a paradox in endurance-trained athletes. J.Clin. Endocrinol. Metab. 86, 5755–5761.
Hulver, M.W., Berggren, J.R., Cortright, R.N., Dudek, R.W., Thompson, R.P., Pories,W.J., MacDonald, K.G., Cline, G.W., Shulman, G.I., Dohm, G.L., Houmard, J.A.,2003. Skeletal muscle lipid metabolism with obesity. Am. J. Physiol. Endocrinol.Metab. 284, E741.
Jubrias, S.A., Esselman, P.C., Price, L.B., Cress, M.E., Conley, K.E., 2001. Large energeticadaptations of elderly muscle to resistance and endurance training. J. Appl.Physiol. 90, 1663–1670.
Kelley, D.E., Mandarino, L.J., 2000. Fuel selection in human skeletal muscle in insulinresistance: a reexamination. Diabetes 49, 677–683.
Kelley, D.E., Goodpaster, B., Wing, R.R., Simoneau, J.A., 1999. Skeletal muscle fattyacid metabolism in association with insulin resistance, obesity, and weight loss.Am. J. Physiol. 277, E1130.
Kelley, D., He, J., Menshikova, E., Ritov, V., 2002. Dysfunction of mitochondria inhuman skeletal muscle in type 2 diabetes mellitus. Diabetes 51, 2944–2950.
Kern, P.A., Simsolo, R.B., Fournier, M., 1999. Effect of weight loss on muscle fibertype, fiber size capillarity, and succinate dehydrogenase activity in humans. J.Clin. Endocrinol. Metab. 84, 4185–4190.
Kim, J.Y., Hickner, R.C., Cortright, R.L., Dohm, G.L., Houmard, J.A., 2000. Lipidoxidation is reduced in obese human skeletal muscle. Am. J. Physiol. Endocrinol.Metab. 279, E1039.
Larsen, S., Nielsen, J., Hansen, C.N., Nielsen, L.B., Wibrand, F., Stride, N., Schroder,H.D., Boushel, R., Helge, J.W., Dela, F., Hey-Mogensen, M., 2012. Biomarkers ofmitochondrial content in skeletal muscle of healthy young human subjects. J.Physiol. 590, 3349–3360.
Lowell, B.B., Shulman, G.I., 2005. Mitochondrial dysfunction and type 2 diabetes.Science 307, 384–387.
Masiero, E., Agatea, L., Mammucari, C., Blaauw, B., Loro, E., Komatsu, M., Metzger, D.,Reggiani, C., Schiaffino, S., Sandri, M., 2009. Autophagy is required to maintainmuscle mass. Cell Metab. 10, 507–515.
McGarry, J.D., 1995. The mitochondrial carnitine palmitoyl transerase system: itsbroadening role in fuel homeostasis and new insights into its molecularfeatures. Biochem. Soc. Trans. 23, 321–324.
Meex, R.C., Schrauwen-Hinderling, V.B., Moonen-Kornips, E., Schaart, G., Mensink,M., Phielix, E., van de Weijer, T., Sels, J.P., Schrauwen, P., Hesselink, M.K., 2010.Restoration of muscle mitochondrial function and metabolic flexibility in type 2diabetes by exercise training is paralleled by increased myocellular fat storageand improved insulin sensitivity. Diabetes 59, 572–579.
Menshikova, E.V., Ritov, V.B., Toledo, F.G., Ferrell, R.E., Goodpaster, B.H., Kelley, D.E.,2005. Effects of weight loss and physical activity on skeletal musclemitochondrial function in obesity. Am. J. Physiol. Endocrinol. Metab. 288, E818.
Menshikova, E.V., Ritov, V.B., Fairfull, L., Ferrell, R.E., Kelley, D.E., Goodpaster, B.H.,2006. Effects of exercise on mitochondrial content and function in aging humanskeletal muscle. J. Gerontol. Ser. A – Biol. Sci. Med. Sci. 61, 534–540.
Mootha, V.K., Lindgren, C.M., Eriksson, K.F., Subramanian, A., Sihag, S., Lehar, J.,Puigserver, P., Carlsson, E., Ridderstrale, M., Laurila, E., Houstis, N., Daly, M.J.,Patterson, N., Mesirov, J.P., Golub, T.R., Tamayo, P., Spiegelman, B., Lander, E.S.,Hirschhorn, J.N., Altshuler, D., Groop, L.C., 2003. PGC-1alpha-responsive genesinvolved in oxidative phosphorylation are coordinately downregulated inhuman diabetes. Nat. Genet. 34, 267–273.
Orlander, J., Aniansson, A., 1980. Effect of physical training on skeletal muscle metabolismand ultrastructure in 70 to 75-year-old men. Acta Physiol. Scand. 109, 149–154.
Patti, M.E., Butte, A.J., Crunkhorn, S., Cusi, K., Berria, R., Kashyap, S., Miyazaki, Y., Kohane, I.,Costello, M., Saccone, R., Landaker, E.J., Goldfine, A.B., Mun, E., DeFronzo, R., Finlayson,J., Kahn, C.R., Mandarino, L.J., 2003. Coordinated reduction of genes of oxidativemetabolism in humans with insulin resistance and diabetes: potential role of PGC1and NRF1. Proc. Nat. Acad. Sci. USA 100, 8466–8471.
Petersen, K.F., Befroy, D., Dufour, S., Dziura, J., Ariyan, C., Rothman, D.L., DiPietro,L., Cline, G.W., Shulman, G.I., 2003. Mitochondrial dysfunction in the elderly:possible role in insulin resistance. Science 300, 1140–1142.
Petersen, K.F., Dufour, S., Befroy, D., Garcia, R., Shulman, G.I., 2004. Impairedmitochondrial activity in the insulin-resistant offspring of patients with type 2diabetes. N. Engl. J. Med. 350, 664–671.
Phielix, E., Meex, R., Moonen-Kornips, E., Hesselink, M.K., Schrauwen, P., 2010.Exercise training increases mitochondrial content and ex vivo mitochondrialfunction similarly in patients with type 2 diabetes and in control individuals.Diabetologia 53, 1714–1721.
Picard, M., Ritchie, D., Wright, K.J., Romestaing, C., Thomas, M.M., Rowan, S.L.,Taivassalo, T., Hepple, R.T., 2010. Mitochondrial functional impairment withaging is exaggerated in isolated mitochondria compared to permeabilizedmyofibers. Aging Cell 9, 1032–1046.
Picard, M., Taivassalo, T., Ritchie, D., Wright, K.J., Thomas, M.M., Romestaing, C.,Hepple, R.T., 2011. Mitochondrial structure and function are disrupted bystandard isolation methods. PLoS ONE 6, e18317.
Pruchnic, R., Katsiaras, A., He, J., Kelley, D.E., Winters, C., Goodpaster, B.H., 2004.Exercise training increases intramyocellular lipid and oxidative capacity inolder adults. Am. J. Physiol. Endocrinol. Metab. 287, E857–E862.
Randle, P.J., Garland, P.B., Hales, C.N., Newsholme, E.A., 1963. The glucose fatty acidcycle: its role in insulin sensitivity and the metabolic didturbances of diabetesmellitus. Lancet 1, 785–789.
Reznick, R.M., Zong, H., Li, J., Morino, K., Moore, I.K., Yu, H.J., Liu, Z.X., Dong, J.,Mustard, K.J., Hawley, S.A., Befroy, D., Pypaert, M., Hardie, D.G., Young, L.H.,Shulman, G.I., 2007. Aging-associated reductions in AMP-activated proteinkinase activity and mitochondrial biogenesis. Cell Metab. 5, 151–156.
Rimbert, V., Boirie, Y., Bedu, M., Hocquette, J.-F., Ritz, P., Morio, B., 2004. Muscle fatoxidative capacity is not impaired by age but by physical inactivity: associationwith insulin sensitivity. FASEB J. 18, 737–739.
Romanello, V., Guadagnin, E., Gomes, L., Roder, I., Sandri, C., Petersen, Y., Milan, G.,Masiero, E., Del Piccolo, P., Foretz, M., Scorrano, L., Rudolf, R., Sandri, M., 2010.Mitochondrial fission and remodelling contributes to muscle atrophy. EMBO J.29, 1774–1785.
Short, K.R., Vittone, J.L., Bigelow, M.L., Proctor, D.N., Rizza, R.A., Coenen-Schimke,J.M., Nair, K.S., 2003. Impact of aerobic exercise training on age-related changesin insulin sensitivity and muscle oxidative capacity. Diabetes 52, 1888–1896.
Simoneau, J.A., Veerkamp, J.H., Turcotte, L.P., Kelley, D.E., 1999. Markers of capacityto utilize fatty acids in human skeletal muscle: relation to insulin resistance andobesity and effects of weight loss. FASEB J. 13, 2051–2060.
Stump, C.S., Short, K.R., Bigelow, M.L., Schimke, J.M., Nair, K.S., 2003. Effect of insulinon human skeletal muscle mitochondrial ATP production, protein synthesis,and mRNA transcripts. Proc. Natl. Acad. Sci. USA 100, 7996–8001.
Toledo, F.G., Watkins, S., Kelley, D.E., 2006. Changes induced by physical activity andweight loss in the morphology of intermyofibrillar mitochondria in obese menand women. J. Clin. Endocrinol. Metab. 91, 3224–3227.
Toledo, F.G., Menshikova, E.V., Ritov, V.B., Azuma, K., Radikova, Z., DeLany, J., Kelley,D.E., 2007. Effects of physical activity and weight loss on skeletal musclemitochondria and relationship with glucose control in type 2 diabetes. Diabetes56, 2142–2147.
Toledo, F.G., Menshikova, E.V., Azuma, K., Radikova, Z., Kelley, C.A., Ritov, V.B.,Kelley, D.E., 2008. Mitochondrial capacity in skeletal muscle is not stimulatedby weight loss despite increases in insulin action and decreases inintramyocellular lipid content. Diabetes 57, 987–994.
Toledo, F.G.S., Menshikova, E.V., Azuma, K., Radikova, Z., Kelley, C.A., Ritov, V.B.,Kelley, D.E., 2008. Mitochondrial capacity in skeletal muscle is not stimulatedby weight loss despite increases in insulin action and decreases inintramyocellular lipid content. Diabetes 57, 987–994.
Tonkonogi, M., Harris, B., Sahlin, K., 1997. Increased activity of citrate synthase inhuman skeletal muscle after a single bout of prolonged exercise. Acta Physiol.Scand. 161, 435–436.
Waters, D.L., Brooks, W.M., Qualls, C.R., Baumgartner, R.N., 2003. Skeletal musclemitochondrial function and lean body mass in healthy exercising elderly. Mech.Ageing Dev. 124, 301–309.
Wenz, T., Rossi, S.G., Rotundo, R.L., Spiegelman, B.M., Moraes, C.T., 2009.Increased muscle PGC-1alpha expression protects from sarcopenia andmetabolic disease during aging. Proc. Natl. Acad. Sci. USA 106, 20405–20410.
34 F.G.S. Toledo, B.H. Goodpaster / Molecular and Cellular Endocrinology 379 (2013) 30–34

Review
Hepatic energy metabolism in human diabetes mellitus, obesityand non-alcoholic fatty liver disease
Chrysi Koliaki a, Michael Roden a,b,⇑a Institute for Clinical Diabetology, German Diabetes Center, Leibniz Center for Diabetes Research, Heinrich Heine University, Düsseldorf, Germanyb Division of Endocrinology and Diabetology and Metabolic Diseases, University Clinics Düsseldorf, Düsseldorf, Germany
a r t i c l e i n f o
Article history:Available online 12 June 2013
Keywords:MitochondrionSteatosisNon-alcoholic steatohepatitis (NASH)Lipotoxicity
a b s t r a c t
Alterations of hepatic mitochondrial function have been observed in states of insulin resistance and non-alcoholic fatty liver disease (NAFLD). Patients with overt type 2 diabetes mellitus (T2DM) can exhibitreduction in hepatic adenosine triphosphate (ATP) synthesis and impaired repletion of their hepaticATP stores upon ATP depletion by fructose. Obesity and NAFLD may also associate with impaired ATPrecovery after ATP-depleting challenges and augmented oxidative stress in the liver. On the other hand,patients with obesity or NAFLD can present with upregulated hepatic anaplerotic and oxidative fluxes,including b-oxidation and tricarboxylic cycle activity. The present review focuses on the methods anddata on hepatic energy metabolism in various states of human insulin resistance. We propose that theliver can adapt to increased lipid exposition by greater lipid storing and oxidative capacity, resulting inincreased oxidative stress, which in turn could deteriorate hepatic mitochondrial function in chronicinsulin resistance and NAFLD.
! 2013 Elsevier Ireland Ltd. All rights reserved.
Contents
1. Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 352. Literature search. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 363. Assessment of hepatic energy metabolism. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 36
3.1. In vitro methods . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 363.2. In vivo methods. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 363.3. Ex vivo methods . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 37
4. The physiological role of liver energy metabolism and mitochondrial function . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 375. Liver mitochondrial function in healthy humans . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 386. Liver mitochondrial function in T2DM . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 397. Liver mitochondrial function in obesity and steatosis . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 398. Liver mitochondrial function in advanced NAFLD . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 409. Conclusions. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 40
Acknowledgements . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 41References . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 41
1. Introduction
Non-alcoholic fatty liver disease (NAFLD) comprises a broadspectrum of chronic liver diseases, ranging from uncomplicated
hepatic steatosis to non-alcoholic steatohepatitis (NASH), fibrosis,and finally liver cirrhosis and hepatocellular carcinoma (Angulo,2002; Smith and Adams, 2011). Hepatic steatosis is defined asintrahepatic fat content above 5.5% (Browning et al., 2004; Roden,2006) and represents a clinical finding typically coexisting withobesity, while NASH and other forms of advanced NAFLD are char-acterized by histological signs of inflammation and fibrosis (Roden,2006; Smith and Adams, 2011). As liver biopsies are not routinelyperformed, only rough estimates of the prevalence of NAFLD are
0303-7207/$ - see front matter ! 2013 Elsevier Ireland Ltd. All rights reserved.http://dx.doi.org/10.1016/j.mce.2013.06.002
⇑ Corresponding author. Address: Institute for Clinical Diabetology, GermanDiabetes Center, Leibniz Center for Diabetes Research, Heinrich Heine University,Auf’m Hennekamp 65, 40225 Düsseldorf, Germany. Tel.: +49 211 3382 201.
E-mail addresses: [email protected] (C. Koliaki), [email protected] (M. Roden).
Molecular and Cellular Endocrinology 379 (2013) 35–42
Contents lists available at SciVerse ScienceDirect
Molecular and Cellular Endocrinology
journal homepage: www.elsevier .com/locate /mce

available, which range from 3% to 30%, with NASH being present inapproximately one third of all cases (Clark, 2006; Smith andAdams, 2011). Even higher estimates are suggested for insulinresistant cohorts such as patients with type 2 diabetes mellitus(T2DM) or severe obesity, suggesting that these entities and NAFLDshare common pathogenic mechanisms (Roden, 2006). NAFLD re-sults from the dynamic interplay of increased lipid influx into theliver, increased de novo hepatic lipogenesis and defective lipid uti-lization, which will stimulate hepatic lipid accumulation. Chronicdietary overload with fructose and saturated fatty acids, will alsoenhance accumulation of lipid metabolites along with oxidativeand endoplasmic reticulum stress and release of cytokines, andthereby foster NAFLD progression (Krebs and Roden, 2004; Roden,2006; Smith and Adams, 2011).
Insulin resistance is tightly associated with ectopic fat accumu-lation in peripheral tissues, including skeletal muscle and liver asthe most important sites (Roden, 2005; Szendroedi and Roden,2009). For skeletal muscle, increased intramyocellular fat content,specifically increased lipid availability, promotes insulin resistancethrough several mechanisms including diacylglycerol (DAG) acti-vation of novel protein kinase C (PKC) isoforms, leading to im-paired insulin-stimulated glucose transport and muscle glycogensynthesis (Roden, 2004). Insulin resistant humans such as patientswith T2DM and first-degree relatives of T2DM patients, may fur-ther show impaired mitochondrial function in muscle, character-ized by lower flux through adenosine triphosphate (ATP)synthase under basal and insulin-stimulated conditions (Petersenet al., 2005; Szendroedi et al., 2007). These abnormalities havebeen mainly attributed to decreased mitochondrial content ratherthan to an inherent impairment of mitochondrial functionality(Boushel et al., 2007; Morino et al., 2005). Whether impaired mito-chondrial function is causally associated with insulin resistanceand how intramyocellular lipids modulate mitochondrial substrateoxidation remains a matter of debate, because recent data supporta dissociation of muscle mitochondrial function from insulin sensi-tivity (Asmann et al., 2006; Boushel et al., 2007; De Feyter et al.,2008; Holloszy, 2009).
Elevated hepatocellular lipid content can promote hepatic insu-lin resistance in the setting of NAFLD, through mechanisms similarto those involved in lipid-induced muscle insulin resistance, suchas hepatic accumulation of DAG and DAG-induced activation ofPKCe (Jornayvaz and Shulman, 2012; Kumashiro et al., 2011; Sam-uel et al., 2004). Although alterations in mitochondrial functioncould contribute to hepatic insulin resistance and NAFLD, the exactnature of this relationship remains a hot topic of metabolic re-search. Recent data from both humans and animal models showedeither decreased, unchanged or even increased hepatic mitochon-drial function and oxidative phosphorylation capacity in insulinresistant states such as T2DM, obesity and NAFLD (Lockman andNyirenda, 2010; Vial et al., 2010). It cannot be precluded that tis-sue-specific differences exist in the association between mitochon-drial function and insulin resistance or intracellular lipid content,but this requires confirmation by adequately controlled humanstudies, examining both liver and muscle mitochondrial functionin these metabolic states.
The present review aims to provide a concise update of theavailable data on hepatic energy metabolism in several phenotypesof insulin resistance (T2DM, obesity, NAFLD), and analyzes patho-genetic concepts possibly underlying alterations of energy homeo-stasis in human liver.
2. Literature search
The PubMed electronic database was searched repeatedly overthree months for all types of articles published in English languageuntil January 2013, using the following search terms: ‘‘hepatic en-
ergy metabolism and insulin resistance’’, ‘‘hepatic energy metabo-lism and NAFLD’’, ‘‘hepatic energy metabolism and T2DM’’,‘‘hepatic energy metabolism and obesity’’, ‘‘hepatic energy metab-olism and liver steatosis’’, ‘‘hepatic mitochondrial function andinsulin resistance’’, ‘‘hepatic mitochondrial function and NAFLD’’.Full-text articles and reference lists of selected review papers werecritically reviewed. Our literature search strategy was restricted tostudies in humans, but a limited number of mechanistic studiesusing animal models of insulin resistance and NAFLD were also re-viewed and are briefly discussed herein.
3. Assessment of hepatic energy metabolism
Liver mitochondrial function can be evaluated directly or indi-rectly by in vitro, in vivo and ex vivo techniques.
3.1. In vitro methods
The in vitro methods include measurements of mitochondrialmass and functionality in biopsy-derived liver samples. They com-prise mitochondrial membrane potential and proton leak kinetics,assessment of mitochondrial content by ultrastructural observa-tions, citrate synthase activity and ratio of mitochondrial relativeto nuclear DNA, polarographic determination of oxygen consump-tion rates, enzyme activities of mitochondrial respiratory com-plexes I–V, markers of oxidative stress such as mitochondrialproduction of superoxide anion and lipid peroxidation products,and anti-oxidant capacity such as superoxide dismutase specificactivity and reduced to oxidized glutathione ratio (Bouderbaet al., 2012; García-Ruiz et al., 1995; Pérez-Carreras et al., 2003;Raffaella et al., 2008; Vendemiale et al., 2001; Vial et al., 2011).
3.2. In vivo methods
Most studies assessed hepatic energy metabolism in vivo byusing non-invasive, phosphorous magnetic resonance spectros-copy (31P MRS) techniques to quantify ATP concentrations or syn-thesis in human liver (Bourdel-Marchasson et al., 1996; Chmelíket al., 2008; Cortez-Pinto et al., 1999; Nair et al., 2003; Schmidet al., 2008; Sharma et al., 2009; Szendroedi et al., 2009). 31P-MRS allows for quantification of hepatic phosphorous metabolitessuch as gamma nucleotide triphosphate (c-NTP), alpha NTP (a-NTP), beta NTP (b-NTP), inorganic phosphate (Pi), phosphomono-esters and phosphodiesters. Fig. 1 depicts a typical liver 31P MRSspectrum of one healthy subject with all the peaks correspondingto hepatocellular phosphorous metabolites that are resolved withthis technique. This technique can now be also applied on clinicalscanners (Laufs et al., 2013). High resolution three dimensional(3D) magnetic spectroscopy imaging is the most recent develop-ment providing absolute concentrations of phosphorus com-pounds, corrected for hepatocellular fat content, as well as theirregional distribution within the liver (Chmelík et al., 2008). 31PMRS can also allow for assessing hepatic ATP synthesis, yieldinga direct estimate of the unidirectional flux through ATP synthase(Schmid et al., 2008). Intravenous fructose challenge with monitor-ing of the degree of ATP depletion and the extent of ATP recoveryyields a measure of the flexibility of hepatic energy homeostasis(Abdelmalek et al., 2012). Fructose induces transient decrease ofhepatic ATP as a result of its rapid phosphorylation by fructokinaseafter entering hepatocytes. Since hepatic fructose metabolism alsocauses a rapid intracellular uric acid elevation, serum uric acid con-centrations have been proposed as a surrogate marker of hepaticATP repletion upon ATP-depleting challenges (Abdelmalek et al.,2012). Another non-invasive molecular imaging tool is positronemission tomography (PET) combined with intravenous adminis-
36 C. Koliaki, M. Roden / Molecular and Cellular Endocrinology 379 (2013) 35–42

tration of lipid radiotracers such as 18-fluoro-6-thia-heptadeca-noic acid and 11C-palmitate, which enables the quantification ofhepatic fatty acid uptake, oxidation and esterification (Iozzoet al., 2010; Viljanen et al., 2009). Additional in vivo methods in-clude stable isotope tracer techniques, such as the oral administra-tion of [U-13C]propionate and deuterated water (2H2O), and theintravenous infusion of [3,4-13C2]glucose, [1,2-13C2]b-hydroxybu-tyrate, [3,4-13C2]acetoacetate and [13C4]palmitate, which help pro-file hepatic glucose and mitochondrial metabolism and assessvarious systemic and hepatic pathways including lipolysis, gluco-neogenesis, tricarboxylic acid cycle function (TCA), non-oxidativepathways replenishing TCA cycle intermediates (anaplerosis) andketogenesis (Sunny et al., 2011). Stable isotopes, such as 13C-octa-noate, 13C-methionine and 13C-ketoisocaproate, have been also ap-plied in non-invasive carbon-labeled breath tests, to assess hepaticmitochondrial b-oxidation and the severity of NAFLD, by measur-ing the cumulative percentage of isotope exhalation or the 13CO2
enrichment in exhaled air (Banasch et al., 2011; Miele et al.,2003; Portincasa et al., 2006). Finally, plasma concentrations of3-hydroxybutyrate have been used as a simple and less informa-tive, but organ-specific biochemical surrogate marker of hepatic li-pid oxidation (Kotronen et al., 2009).
3.3. Ex vivo methods
High resolution respirometry by oxygraphs has been frequentlyapplied to skeletal muscle, but could also be performed in liver tis-sue and isolated mitochondria. This method will provide usefulinformation on coupled and uncoupled maximal respiratory capac-ity of liver tissue or hepatic mitochondria after addition of variousmitochondrial substrates such as octanoyl-coenzyme A, malate,pyruvate, glutamate, succinate. To our knowledge, there are nopublished data with this technique in humans so far, but prelimin-ary data in mice are promising and lay the ground for applyinghigh resolution respirometry to quantify human liver mitochon-drial function in several disease states (Benard et al., 2006; Kozlovet al., 2006; Kuznetsov et al., 2002).
4. The physiological role of liver energy metabolism andmitochondrial function
The human liver plays a critical role in regulating glucose andlipid metabolism and whole-body energy homeostasis. Liver main-
tains blood glucose within a narrow concentration range, by itsability to store glucose as glycogen and produce glucose aftereither glycogen breakdown (glycogenolysis) or de novo glucoseproduction from gluconeogenic precursors (gluconeogenesis) (Ro-den and Bernroider, 2003). In healthy humans, hepatic glycogenol-ysis and gluconeogenesis are stimulated in the fasted state andimmediately inhibited in the postprandial state as a result of rapidinsulin action (Tappy, 1995). On the contrary, patients with T2DMexhibit reduced postprandial hepatic glycogen synthesis and in-creased hepatic glucose output in both fasting and postprandialconditions, mainly driven by enhanced hepatic gluconeogenesis(Krssak et al., 2004). The rise in the portal glucagon:insulin ratioand the increased hepatic free fatty acid oxidation are held mainlyresponsible for enhanced gluconeogenesis in T2DM (Roden andBernroider, 2003).
Liver mitochondria represent the major orchestrator of hepato-cellular energy metabolism, since they are the site of fatty acid oxi-dation and ATP synthesis (Pessayre et al., 2002). Three differentsources contribute to the hepatic levels of free fatty acids: de novolipogenesis within hepatocytes from acetyl-CoA, uptake of circulat-ing plasma free fatty acids released by adipose tissue with lipolysisand hydrolysis of intestinal chylomicrons (McGarry and Foster,1980). Hepatic free fatty acids can either enter mitochondria to un-dergo b-oxidation or be esterified into triglycerides. Hepatic tri-glycerides in turn either accumulate within hepatocytes ascytoplasmic lipid droplets, or are secreted as very low density lipo-protein (VLDL) particles into blood circulation (Lavoie and Gauthi-er, 2006; McGarry and Foster, 1980; Nguyen et al., 2008; Pessayreet al., 2001). The entry of long-chain free fatty acids into hepaticmitochondria is regulated by carnitine palmitoyl-transferase typeI (CPT-I), which is located in the outer mitochondrial membraneand sensitive to inhibition by malonyl-CoA, the first substrate ofhepatic de novo lipogenesis (Pessayre et al., 2001). Successive cy-cles of b-oxidation split hepatic free fatty acids into subunits ofacetyl-CoA, which are either completely degraded to carbon diox-ide in the TCA (or Krebs) cycle, or condensed to ketone bodies(ketogenesis), which are then secreted by hepatic cells into circula-tion (Lavoie and Gauthier, 2006). Fatty acid oxidation in hepaticmitochondria is associated with the reduction of oxidized coen-zymes, which are in turn re-oxidized by the mitochondrial respira-tory chain (Pessayre et al., 2002, 2001). During their re-oxidation,they transfer their electrons to the polypeptide complexes of themitochondrial respiratory chain. The electron transfer along therespiratory chain is coupled with an export of protons from
Fig. 1. Liver 31P MRS spectrum of a representative healthy person obtained with the 3-Tesla whole-body magnetic resonance spectrometer (Philips Achieva, Best, TheNetherlands) at the German Diabetes Center, Düsseldorf, Germany. The eleven peaks correspond to the phosphorous metabolites of liver cells. Upper right panel: transversalimage with a voxel of interest (VOI) placement, using a 14 cm linear polarized surface coil, positioned over the lateral aspect of liver. ppm: parts per million; NTP:triphosphate nucleoside; NADPH: nicotinamide adenine dinucleotide phosphate; UDPG: uridine diphosphoglucose; PEP: phosphoenol-pyruvate; GPC: glycerol phospho-choline; GPE: glycerol phosphoethanolamine; Pi: inorganic phosphate; PC: phosphocholine; PE: phosphoethanolamine Phosphomonoesters (PME) include PE and PC,phosphodiesters (PDE) include GPE and GPC.
C. Koliaki, M. Roden / Molecular and Cellular Endocrinology 379 (2013) 35–42 37

mitochondrial matrix to intermembrane space, creating a largeelectrochemical gradient across the inner mitochondrial mem-brane, which acts as an energy reservoir. When energy is needed,protons can re-enter matrix through ATP synthase (complex V),causing the conversion of adenosine diphosphate (ADP) into ATP.The adenine dinucleotide translocator proteins can then exportmitochondrial ATP in exchange for cytosolic ADP, and the cytoplas-mic ATP can be used to power all hepatocellular energy-requiringmetabolic processes (Pessayre et al., 2002, 2001).
5. Liver mitochondrial function in healthy humans
Despite the limited data on the normal range of mitochondrialfunction in human liver, some information can be derived fromclinical studies, which have compared direct or indirect measuresof hepatic mitochondrial function between insulin resistant andinsulin sensitive humans. Table 1 summarizes the key data of thesestudies, while Fig. 2 depicts in a graphical way the percentage dif-ferences of liver mitochondrial function between healthy humansand several insulin resistant phenotypes.
Employing 31P MRS to assess liver ATP turnover revealed thatyoung healthy humans display hepatic concentrations of c-ATP
Table 1Studies in humans on hepatic energy metabolism under conditions of type 2 diabetes mellitus (T2DM), insulin resistance and non-alcoholic fatty liver disease (NAFLD).
Reference Cohort Methods Results
Szendroedi et al. (2009) 9 T2DM in vivo 31P-MRS ;cATP and Pi contents9 matcheda controls in T2DM9 young lean controls
Schmid et al. (2011) 9 T2DM in vivo 31P MRS ;flux through ATP synthase8 matcheda controls in T2DM
Abdelmalek et al. (2012) 25 obese T2DM in vivo 31P MRS ;ATP recoverywith high or low fructoseconsumption
fructose challenge in high fructose consumers
Nair et al. (2003) 7 overweight in vivo 31P MRS ;ATP content7 obese fructose challenge in overweight and obese5 lean controls unchanged ATP recovery
Viljanen et al. (2009) 34 healthy obese 18-fluoro-6-thia- ;hepatic fatty acid uptakeheptadecanoic acid PETimaging
after VLCD for 6 weeks
Iozzo et al. (2010) 8 obese 11C-palmitate PET imaging "hepatic fatty acid oxidation7 lean controls in obese
Kotronen et al. (2009) 29 NAFLD plasma levels of no differences in hepatic lipid oxidation29 controls 3-OHB
Sharma et al. (2009) 20 obese + NAFLD in vivo 31P MRS "PME/Pi and PME/cATP ratios20 non-obese + NAFLD in obese + NAFLD20 non-obese -NAFLD
Sunny et al. (2011) 8 high HCL in vivo stable isotope tracers "TCA cycle, anaplerosis, lipolysis and gluconeogenesis8 low HCL in high HCL
Cortez-Pinto et al. (1999) 8 NASH in vivo 31P MRS ;ATP recovery7 controls fructose challenge in NASH
Sanyal et al. (2001) 6-10 NASH in vitro hepatic "ß-oxidation and ox. stress6 steatosis lipid peroxidation in NASH and steatosis6 controls serum b-OHB mitochondrial defects in NASH
Miele et al. (2003) 10 NASH 13C-octanoate breath test "hepatic mitochondrial20 controls ß-oxidation in NASH
Pérez-Carreras et al.(2003)
43 NASH in vitro ETC ;activity of ETC CI-V correlation with insulin resistance andinflammation
16 controls enzyme activity
Serviddio et al. (2008b) 10 NASH in vitro proton leak, "UCP-2, proton leak and oxidative stress8 controls UCP-2 expression,
ROS production,ATP content
ATP: adenosine triphosphate; ß-OHB: ß-hydroxybutyrate; 3-OHB: 3-hydroxybutyrate; CI-V: complexes I–V; ETC: electron transport chain; HCL: hepatocellular lipids; 31PMRS: phosphorous magnetic resonance spectroscopy; NAFLD: non-alcoholic fatty liver disease; NASH: non-alcoholic steatohepatitis; PET: positron emission tomography; Pi:inorganic phosphate; PME: phosphomonoesters; ROS: reactive oxygen species; TCA: tricarboxylic acid cycle; T2DM: type 2 diabetes mellitus; UCP-2: uncoupling protein 2;VLCD: very low calorie diet.
A Matched for age and body mass index.
Fig. 2. Hypothetical changes in hepatic energy metabolism in states of obesity,steatosis, non-alcoholic steatohepatitis (NASH) and type 2 diabetes mellitus(T2DM). Different features of hepatic energy metabolism such as ATP, b-oxidationand respiratory complex activities were obtained from studies including healthycontrol groups. The respective percent changes are compared to the data of therespective healthy control group, which were set as 100%. Data are derived from thefollowing references: Cortez-Pinto et al. (1999); Iozzo et al. (2010); Miele et al.(2003); Pérez-Carreras et al. (2003); Schmid et al. (2011); Sunny et al. (2011);Szendroedi et al. (2009).
38 C. Koliaki, M. Roden / Molecular and Cellular Endocrinology 379 (2013) 35–42

ranging from 2.0 to 2.6 mmol/l and hepatic Pi levels ranging from1.2 to 1.7 mmol/l (Szendroedi et al., 2009). Elderly non-diabetic,but slightly insulin resistant humans, display absolute c-ATP levelsin the range of 1.9–3.1 mmol/l, Pi concentrations in the range of 1–1.9 mmol/l and flux through ATP synthase in the range of 15–41 mmol/l/min (Schmid et al., 2011; Szendroedi et al., 2009). Com-bining 31P MRS with an ATP-depleting fructose challenge identifiedthat in healthy subjects, hepatic b-ATP levels fall by 50% to theirnadir at 12 min, and recover fully at 60 min after fructose adminis-tration (Cortez-Pinto et al., 1999).
Furthermore, enzyme activities of mitochondrial respiratorychain proteins have been measured in biopsy-derived liver speci-mens obtained from healthy humans. Relative to citrate synthaseactivity, complex I activity was found to range between 30 and43 nmol/min/mg protein, complex II activity between 28 and46 nmol/min/mg protein, complex III activity between 38 and60 nmol/min/mg protein, complex IV activity between 24 and46 nmol/min/mg protein, and complex V activity between 99 and167 nmol/min/mg protein (Pérez-Carreras et al., 2003). In the samestudy, citrate synthase specific activity, reflecting mitochondrialprotein mass, was found to range between 112 and 168 nmol/min/mg protein in healthy controls.
Measuring biochemical surrogates of hepatic lipid oxidation re-vealed that fasting b-hydroxybutyrate levels range between 81 and99 lmol/l and are suppressed by 50% under conditions of hyperin-sulinemia in healthy humans (Sanyal et al., 2001). Furthermore, ithas been shown that hepatic fatty acid oxidation accounts for 40%of liver fat uptake and fatty acid esterification for 60%, as assessedwith 11C-palmitate kinetics and PET imaging in healthy humans(Iozzo et al., 2010).
Of note, the rates of ATP synthesis in human liver are approxi-mately 50% lower than those in isolated perfused rat liver, indicat-ing species-specific differences in hepatic energy metabolismunder normal conditions (Schmid et al., 2008).
6. Liver mitochondrial function in T2DM
Only recently, two studies reported that patients with T2DMhave lower hepatic ATP turnover measured by 31P MRS, when com-pared with age- and BMI-matched non-diabetic subjects (Schmidet al., 2011; Szendroedi et al., 2009) and young lean controls(Szendroedi et al., 2009) (Table 1). In detail, the absolute hepaticconcentrations of c-ATP and Pi were 23–26% and 28–31% lowerin T2DM (Szendroedi et al., 2009) (Fig. 2). Furthermore, c-ATPand Pi absolute concentrations were negatively correlated withinsulin-mediated endogenous glucose production (r = !0.67,p = 0.01), even after adjusting for hepatocellular fat content, butthey were not significantly associated with peripheral insulin sen-sitivity (M-value) (Szendroedi et al., 2009). Endogenous glucoseproduction was the only significant independent predictor of c-ATP levels, explaining 57% of variance of hepatic ATP concentra-tions (Szendroedi et al., 2009). A similar group of T2DM patientsfeatured a 42% reduction in the hepatic flux through ATP synthase,which was mainly driven by decreased hepatic Pi levels (Schmidet al., 2011). In this study, flux through ATP synthase was positivelycorrelated with both peripheral and hepatic insulin sensitivity(r = 0.66–0.72, p < 0.05), independently of hepatic lipid content,and was negatively correlated with waist circumference and BMI(r = !0.52 to !0.81, p " 0:001). Although the cohort of T2DM pa-tients displayed adequate glycemic control under oral glucose low-ering treatment, hepatic flux through ATP synthase correlatednegatively with measures of short- and long-term glycemic controlsuch as fasting glucose and glycosylated hemoglobin. This indi-cates that even minor degree of hyperglycemia for long time peri-
ods might impair hepatic mitochondrial function (Schmid et al.,2011).
Likewise, high dietary fructose consumption (>15 g per day) canseverely deplete hepatic ATP stores and impair ATP re-synthesisafter intravenous fructose challenge in obese patients with T2DM(Abdelmalek et al., 2012) (Table 1). This was particularly true forpatients with serum uric acid concentrations of 5.5 mg/dl or more.This study suggests that high dietary fructose intake could contrib-ute to the worsening of abnormal hepatic energy homeostasis inT2DM patients, and may further predispose them to the develop-ment and/or progression of NAFLD (Abdelmalek et al., 2010; Ouy-ang et al., 2008).
Studies in animal models of T2DM such as the diabetes-pronePsammomys obesus model, are in the same direction with the clin-ical studies, showing an impaired hepatic energy metabolism in ratliver tissue after a hypercaloric diabetogenic diet (Bouderba et al.,2012). In this rat model, liver mitochondrial function was assessedwith respirometry in isolated mitochondria and respiratory com-plex enzyme activities, and was found to be significantly declinedin diabetic animals.
In conclusion, patients with T2DM display lower hepatic energymetabolism compared to both young and elderly non-diabetic hu-mans, which is expressed as reduced hepatic flux through ATP syn-thase and reduced hepatic ATP and Pi concentrations. Of note,parameters of hepatic mitochondrial metabolism other than hepa-tic ATP homeostasis have not yet been evaluated in T2DM patients.
7. Liver mitochondrial function in obesity and steatosis
Similar to T2DM, some studies found that overweight and obesehumans have lower hepatic ATP levels compared to normal-weighthumans (Table 1). Hepatic ATP content related inversely to BMI notonly in the obese, but also in normal-weight subjects (Cortez-Pintoet al., 1999; Nair et al., 2003). However, obese persons can featureimpaired (Cortez-Pinto et al., 1999) or normal (Nair et al., 2003)repletion of hepatic ATP upon fructose challenging. Of note, livermitochondria of rats with high fat diet-induced obesity and insulinresistance exhibit an elevated rate of b-oxidation and TCA cycleactivity, which is however combined with an impaired respiratorycapacity and greater oxidative stress (Raffaella et al., 2008; Satapatiet al., 2012).
Hepatic fatty acid oxidation measured by 11C-palmitate com-bined with PET imaging is 50% higher (Fig. 2), while fatty acid up-take and esterification are not different in obese compared to leanpersons (Iozzo et al., 2010). Another PET study found that a verylow calorie diet decreases by 26% hepatic fatty acid uptake andameliorates hepatic insulin resistance in healthy obese persons(Viljanen et al., 2009), without however providing any data aboutother aspects of hepatic mitochondrial metabolism such as mito-chondrial respiration or fat oxidation.
A very frequent comorbidity of obesity is liver steatosis, since60–90% of persons with steatosis (based on liver biopsies) are over-weight or obese (Choudhury and Sanyal, 2004). Considering thatthere are only limited data for obese humans, the few studies con-ducted in steatotic humans complement those in obese, and shedmore light into the association of obesity with liver mitochondrialfunction. From plasma 3-hydroxybutyrate concentrations, hepaticlipid oxidation was rated similar in overweight patients with stea-tosis and healthy humans, under both basal and insulin-stimulatedconditions (Kotronen et al., 2009) (Table 1). However, significantdifferences not only in fat oxidation, but also in other aspects of he-patic mitochondrial function were observed in another studyemploying non-invasive in vivo tracer techniques. Sunny et al. re-ported that persons with steatosis, as defined by liver fat contentof more than 6%, have two-fold greater hepatic mitochondrial oxi-
C. Koliaki, M. Roden / Molecular and Cellular Endocrinology 379 (2013) 35–42 39

dative metabolism than those with liver fat content less than 6%(Sunny et al., 2011). Both groups had similar age and comparabledegree of obesity, elevation of liver enzymes and whole-body insu-lin resistance, whereas hepatic insulin resistance was more pro-nounced in those with steatosis. In detail, subjects with steatosisexhibited 100% higher TCA cycle flux, 50% higher rates of lipolysisand anaplerosis, and 25% higher rates of gluconeogenesis com-pared to those without steatosis (Table 1 and Fig. 2). Of note, hepa-tic fat content correlated positively with measures of bothoxidative and non-oxidative mitochondrial metabolism. Thesefindings support the concept that mitochondrial pathways couldbe upregulated in steatosis as an adaptive mechanism in responseto chronic fat overload. Recent animal studies are in absoluteaccordance with this contention, by showing elevated TCA cyclefunction and mitochondrial b-oxidation in states of diet-inducedhepatic insulin resistance and liver steatosis (Satapati et al., 2012).
Taken together, all the above data in humans with obesity andsteatosis illustrate the importance of the homeostasis of hepaticfatty acid handling. Any increase in hepatic fatty acid uptake wouldbe balanced by an up-regulation of b-oxidation, which – in the set-ting of chronic lipid overloading – would stimulate ATP productionand generation of ROS. This would in turn lead to increased triglyc-eride synthesis and export as VLDL, as well as to hepatic oxidativestress with promotion of NAFLD and ultimately impairment ofmitochondrial functionality.
8. Liver mitochondrial function in advanced NAFLD
Advanced NAFLD typically associates with insulin resistanceand unfavorable hepatic adaptations of hepatocellular energyhomeostasis, which render the liver more vulnerable to oxidativeinjury and cell death, and are reflected by ultrastructural mito-chondrial defects (Sanyal et al., 2001). It has been suggested thatimpaired mitochondrial respiratory capacity plays a key role inthe pathogenesis of advanced NAFLD, particularly in the progres-sion to NASH and cirrhosis (Begriche et al., 2006; Serviddio et al.,2011, 2008a). Studies in humans have failed to support a conceptof generalized defects in mitochondrial b-oxidation in biopsy-pro-ven NAFLD (Sanyal et al., 2001). In contrast, patients with NAFLDand insulin resistance show greater liver mitochondrial b-oxida-tion, while those with drug-induced NAFLD have diminished mito-chondrial oxidation (Fromenty et al., 2004; Miele et al., 2003). Anaugmented hepatic b-oxidation and oxidative stress seem thus toaccompany peripheral insulin resistance as the most prominentcharacteristics of advanced NAFLD (Sanyal et al., 2001).
NASH is recognized as the most common subtype of advancedNAFLD (Clark, 2006). In a pilotic study in eight patients withbiopsy-proven NASH, it was found that the ability of these patientsto regenerate their hepatic ATP reserve after a transient ATP deple-tion induced by fructose ingestion was reduced by 30% comparedto age- and sex-matched controls (Cortez-Pinto et al., 1999)(Fig. 2). Of note, in human NASH, functional mitochondrial abnor-malities are furthermore combined with a number of structural de-fects such as loss of mitochondrial cristae and paracrystallineinclusions, and presence of linear crystalline inclusions in swollenmitochondria (Sanyal et al., 2001). Furthermore, it has been shownthat patients with NASH have a severely defective hepatic mito-chondrial respiratory chain, and this dysfunction correlates posi-tively with inflammation and peripheral insulin resistance(Pérez-Carreras et al., 2003). More specifically, patients with NASHwere found to exhibit significantly decreased activity of all respira-tory chain complexes compared to control subjects (42.4–70.6%reduction for complexes I–V), and increased availability of hepaticfree fatty acids, expressed as an increased ratio of long-chainacylcarnitine esters relative to free carnitine (Pérez-Carreras
et al., 2003) (Table 1 and Fig. 2). It has been also reported that pa-tients with NASH display an increased proton leak across the elec-tron transport chain due to a 2-fold increased hepatic expression ofuncoupling protein 2 (UCP-2) (Serviddio et al., 2008b) (Table 1).The upregulation of UCP-2 in human NASH induces an uncouplingbetween oxidative phosphorylation and ATP production, reducesthe redox pressure on mitochondrial respiratory chain, and actsas a potential protective mechanism against further liver damage.UCP-2-dependent mitochondrial uncoupling can be perceived as aprotective mechanism to halt damage progression but compro-mises on the other hand the liver capacity to respond to acutehigh-energy demands, such as ischaemia–reperfusion injury. Addi-tional abnormalities of hepatic energy metabolism that have beenreported in human and animal NASH (rat models of high fat,methionine and choline-deficient diet) include increased ROS pro-duction, abnormal cellular and mitochondrial redox homeostasis,oxidative stress-mediated depletions of mitochondrial DNA encod-ing some of the polypeptide components of mitochondrial respira-tory chain and increased rate of b-oxidation (Miele et al., 2003;Morris et al., 2011; Serviddio et al., 2008a; Romestaing et al.,2008) (Table 1).
The underlying pathophysiology of perturbed hepatic energymetabolism in NASH can be described by a vicious circle, involvingfree fatty acids, lipid peroxidation products and inflammatorymarkers (Fromenty et al., 2004; Pessayre, 2007; Pessayre et al.,2002, 2001). This ominous cascade begins with a mild respiratorydysfunction induced by lipid oversupply in hepatocytes. In addi-tion, the increased availability of hepatic free fatty acids resultsin an increased import of free fatty acids into hepatic mitochondriaand an elevated rate of mitochondrial fatty acid b-oxidation (Mieleet al., 2003). Due to the increased rate of b-oxidation, an imbalanceoccurs between a high electron input and a restricted electron out-flow, leading to accumulation of electrons within respiratory com-plexes I and III and a subsequent reaction of these electrons withoxygen to form ROS. ROS can promote lipid peroxidation and lipidperoxidation products can in turn alter mitochondrial DNA andcause severe oxidative damage to critical mitochondrial proteinssuch as cytochrome c oxidase and adenine nucleotide translocatorproteins, resulting in impaired electron flow along the respiratorychain and establishing a vicious circle between impaired respira-tory chain capacity, ROS formation, lipid peroxidation and mito-chondrial damage (Fromenty et al., 2004; Pessayre, 2007;Pessayre et al., 2002, 2001). ROS and lipid peroxidation productscan also promote hepatic inflammation, fibrosis and cell death,leading to the characteristic necroinflammatory and fibrotic alter-ations of hepatic tissue observed in advanced stages of NAFLD. Dueto excessive ROS production, the anti-oxidant defense systems ofmitochondria (enzymes and vitamins) are rapidly consumed, andthis depletion of anti-oxidant capacity hampers the inactivationof ROS and may further augment ROS-mediated damage.
9. Conclusions
The liver is a central player in the physiological regulation ofwhole-body energy homeostasis as well as the pathogenesis ofthe epidemiologically relevant endocrine disorders obesity anddiabetes. Patients with long-standing T2DM can have lower hepa-tic ATP synthesis during fasting and after fructose administration.In advanced NAFLD, abnormal hepatic mitochondrial functionand morphology may occur, possibly due to local lipotoxic, inflam-matory and oxidative stress pathways. On the other hand, non-dia-betic obese humans can show normal or even greater hepaticmitochondrial function than lean humans. Such increases in b-oxi-dation, ketogenesis and anaplerotic fluxes can be interpreted as aresponse to lipid oversupply and may correlate with steatosis.
40 C. Koliaki, M. Roden / Molecular and Cellular Endocrinology 379 (2013) 35–42

Thus, we propose that hepatic energy metabolism transitionallyadapts to chronic lipid overload in states of obesity and steatosisby upregulated oxidative capacity, which can be followed by pro-gressive decline in liver mitochondrial function during prolongedchronic insulin resistance, associated with T2DM and NASH(Fig. 2).
Of note, these conclusions are based on a limited number ofsmall-scale human studies. More clinical studies combiningin vivo and ex vivo state-of-the art methods are needed to addresshepatic energy metabolism in well-phenotyped and matched co-horts. Such an approach could help to identify novel markers ofthe deterioration of hepatic energy metabolism and predictors ofprogression of NAFLD in obesity and diabetes mellitus.
Acknowledgements
C.K. is on leave of absence from the Endocrine Unit and DiabetesResearch Center of Attikon University Hospital, Athens UniversityMedical School, Greece, and was supported by the National Foun-dation of State Scholarships of Greece (IKY). The work of M.R. isor has been supported in part by the European Foundation forthe Study of Diabetes, German Research Foundation, Schmutzler-Stiftung, Skröder-Stiftung, and the German Center for Diabetes Re-search (DZD e.V.).
References
Abdelmalek, M.F., Suzuki, A., Guy, C., Unalp-Arida, A., Colvin, R., Johnson, R.J., Diehl,A.M., 2010. Increased fructose consumption is associated with fibrosis severityin patients with nonalcoholic fatty liver disease. Hepatology 51, 1961–1971.
Abdelmalek, M.F., Lazo, M., Horska, A., Bonekamp, S., Lipkin, E.W.,Balasubramanyam, A., Bantle, J.P., Johnson, R.J., Diehl, A.M., Clark, J.M., 2012.Higher dietary fructose is associated with impaired hepatic adenosinetriphosphate homeostasis in obese individuals with type 2 diabetes.Hepatology 56, 952–960.
Angulo, P., 2002. Nonalcoholic fatty liver disease. N. Engl. J. Med. 346, 1221–1231.Asmann, Y.W., Stump, C.S., Short, K.R., Coenen-Schimke, J.M., Guo, Z., Bigelow, M.L.,
Nair, K.S., 2006. Skeletal muscle mitochondrial functions, mitochondrial DNAcopy numbers, and gene transcript profiles in type 2 diabetic and nondiabeticsubjects at equal levels of low or high insulin and euglycemia. Diabetes 55,3309–3319.
Banasch, M., Ellrichmann, M., Tannapfel, A., Schmidt, W.E., Goetze, O., 2011. Thenon-invasive (13)C-methionine breath test detects hepatic mitochondrialdysfunction as a marker of disease activity in non-alcoholic steatohepatitis.Eur. J. Med. Res. 16, 258–264.
Begriche, K., Igoudjil, A., Pessayre, D., Fromenty, B., 2006. Mitochondrial dysfunctionin NASH: causes, consequences and possible means to prevent it.Mitochondrion 6, 1–28.
Benard, G., Faustin, B., Passerieux, E., Galinier, A., Rocher, C., Bellance, N., Delage, J.P.,Casteilla, L., Letellier, T., Rossignol, R., 2006. Physiological diversity ofmitochondrial oxidative phosphorylation. Am. J. Physiol. Cell Physiol. 291,C1172–C1182.
Bouderba, S., Sanz, M.N., Sánchez-Martín, C., El-Mir, M.Y., Villanueva, G.R., Detaille,D., Koceïr, E.A., 2012. Hepatic mitochondrial alterations and increased oxidativestress in nutritional diabetes-prone Psammomys obesus model. Exp. DiabetesRes. 2012, 430176.
Bourdel-Marchasson, I., Biran, M., Thiaudière, E., Delalande, C., Decamps, A.,Manciet, G., Canioni, P., 1996. 31P magnetic resonance spectroscopy of humanliver in elderly patients: changes according to nutritional status andinflammatory state. Metabolism 45, 1059–1061.
Boushel, R., Gnaiger, E., Schjerling, P., Skovbro, M., Kraunsøe, R., Dela, F., 2007.Patients with type 2 diabetes have normal mitochondrial function in skeletalmuscle. Diabetologia 50, 790–796.
Browning, J.D., Szczepaniak, L.S., Dobbins, R., Nuremberg, P., Horton, J.D., Cohen, J.C.,Grundy, S.M., Hobbs, H.H., 2004. Prevalence of hepatic steatosis in an urbanpopulation in the United States: impact of ethnicity. Hepatology 40, 1387–1395.
Chmelík, M., Schmid, A.I., Gruber, S., Szendroedi, J., Krssák, M., Trattnig, S., Moser, E.,Roden, M., 2008. Three-dimensional high-resolution magnetic resonancespectroscopic imaging for absolute quantification of 31P metabolites in humanliver. Magn. Reson. Med. 60, 796–802.
Choudhury, J., Sanyal, A.J., 2004. Clinical aspects of fatty liver disease. Sem. Liver Dis.24, 349–362.
Clark, J.M., 2006. The epidemiology of nonalcoholic fatty liver disease in adults. J.Clin. Gastroenterol 40 (Suppl 1), S5-10.
Cortez-Pinto, H., Chatham, J., Chacko, V.P., Arnold, C., Rashid, A., Diehl, A.M., 1999.Alterations in liver ATP homeostasis in human nonalcoholic steatohepatitis: apilot study. JAMA 282, 1659–1664.
De Feyter, H.M., van den Broek, N.M., Praet, S.F., Nicolay, K., van Loon, L.J., Prompers,J.J., 2008. Early or advanced stage type 2 diabetes is not accompanied by in vivoskeletal muscle mitochondrial dysfunction. Eur. J. Endocrinol. 158, 643–653.
Fromenty, B., Robin, M.A., Igoudjil, A., Mansouri, A., Pessayre, D., 2004. The ins andouts of mitochondrial dysfunction in NASH. Diabetes Metab. 30, 121–138.
García-Ruiz, C., Colell, A., Morales, A., Kaplowitz, N., Fernández-Checa, J.C., 1995.Role of oxidative stress generated from the mitochondrial electron transportchain and mitochondrial glutathione status in loss of mitochondrial functionand activation of transcription factor nuclear factor-kappa B: studies withisolated mitochondria and rat hepatocytes. Mol. Pharmacol. 48, 825–834.
Holloszy, J.O., 2009. Skeletal muscle ‘‘mitochondrial deficiency’’ does not mediateinsulin resistance. Am. J. Clin. Nutr. 89, 463S–466S.
Iozzo, P., Bucci, M., Roivainen, A., Någren, K., Järvisalo, MJ., Kiss, J., Guiducci, L.,Fielding, B., Naum, AG., Borra, R., Virtanen, K., Savunen, T., Salvadori, PA.,Ferrannini, E., Knuuti, J., Nuutila, P., 2010. Fatty acid metabolism in the liver,measured by positron emission tomography, is increased in obese individuals.Gastroenterology 139, 846–856.
Jornayvaz, F.R., Shulman, G.I., 2012. Diacylglycerol activation of protein kinase Ceand hepatic insulin resistance. Cell Metab. 15, 574–584.
Kotronen, A., Seppälä-Lindroos, A., Vehkavaara, S., Bergholm, R., Frayn, K.N.,Fielding, B.A., Yki-Järvinen, H., 2009. Liver fat and lipid oxidation in humans.Liver Int. 29, 1439–1446.
Kozlov, A.V., Staniek, K., Haindl, S., Piskernik, C., Ohlinger, W., Gille, L., Nohl, H.,Bahrami, S., Redl, H., 2006. Different effects of endotoxic shock on therespiratory function of liver and heart mitochondria in rats. Am. J. Physiol.Gastrointest. Liver Physiol. 290, G543–G549.
Krebs, M., Roden, M., 2004. Nutrient-induced insulin resistance in human skeletalmuscle. Curr. Med. Chem. 11, 901–908.
Krssak, M., Brehm, A., Bernroider, E., Anderwald, C., Nowotny, P., Dalla Man, C.,Cobelli, C., Cline, G.W., Shulman, G.I., Waldhäusl, W., Roden, M., 2004.Alterations in postprandial hepatic glycogen metabolism in type 2 diabetes.Diabetes 53, 3048–3056.
Kumashiro, N., Erion, D.M., Zhang, D., Kahn, M., Beddow, S.A., Chu, X., Still, C.D.,Gerhard, G.S., Han, X., Dziura, J., Petersen, K.F., Samuel, V.T., Shulman, G.I., 2011.Cellular mechanism of insulin resistance in nonalcoholic fatty liver disease.Proc. Nat. Acad Sci. USA 108, 16381–16385.
Kuznetsov, A.V., Strobl, D., Ruttmann, E., Königsrainer, A., Margreiter, R., Gnaiger, E.,2002. Evaluation of mitochondrial respiratory function in small biopsies of liver.Anal. Biochem. 305, 186–194.
Laufs, A., Livingstone, R., Nowotny, B., Nowotny, P., Wickrath, F., Giani, G., Bunke, J.,Roden, M., Hwang, J.H., 2013. Quantitative liver 31P MR spectroscopy at 3T on aclinical scanner. Magn. Res. Med. (in press).
Lavoie, J.M., Gauthier, M.S., 2006. Regulation of fat metabolism in the liver: link tonon-alcoholic hepatic steatosis and impact of physical exercise. Cell Mol. LifeSci. 63, 1393–1409.
Lockman, K.A., Nyirenda, M.J., 2010. Interrelationships between hepatic fat andinsulin resistance in non-alcoholic fatty liver disease. Curr. Diabetes Rev. 6,341–347.
McGarry, J.D., Foster, D.W., 1980. Regulation of hepatic fatty acid oxidation andketone body production. Annu. Rev. Biochem. 49, 395–420.
Miele, L., Grieco, A., Armuzzi, A., Candelli, M., Forgione, A., Gasbarrini, A., Gasbarrini,G., 2003. Hepatic mitochondrial beta-oxidation in patients with nonalcoholicsteatohepatitis assessed by 13C-octanoate breath test. Am. J. Gastroenterol. 98,2335–2336.
Morino, K., Petersen, K.F., Dufour, S., Befroy, D., Frattini, J., Shatzkes, N., Neschen, S.,White, M.F., Bilz, S., Sono, S., Pypaert, M., Shulman, G.I., 2005. Reducedmitochondrial density and increased IRS-1 serine phosphorylation in muscleof insulin-resistant offspring of type 2 diabetic parents. J. Clin. Invest. 115,3587–3593.
Morris, E.M., Rector, R.S., Thyfault, J.P., Ibdah, J.A., 2011. Mitochondria and redoxsignaling in steatohepatitis. Antioxid Redox Signal 15, 485–504.
Nair, S., P Chacko, V., Arnold, C., Diehl, A.M., 2003. Hepatic ATP reserve andefficiency of replenishing: comparison between obese and nonobese normalindividuals. Am. J. Gastroenterol 98, 466–470.
Nguyen, P., Leray, V., Diez, M., Serisier, S., Le Bloc’h, J., Siliart, B., Dumon, H., 2008.Liver lipid metabolism. J. Anim Physiol. Anim Nutr. (Berl.) 92, 272–283.
Ouyang, X., Cirillo, P., Sautin, Y., McCall, S., Bruchette, J.L., Diehl, A.M., Johnson, R.J.,Abdelmalek, M.F., 2008. Fructose consumption as a risk factor for non-alcoholicfatty liver disease. J. Hepatol. 48, 993–999.
Pérez-Carreras, M., Del Hoyo, P., Martín, M.A., Rubio, J.C., Martín, A., Castellano, G.,Colina, F., Arenas, J., Solis-Herruzo, J.A., 2003. Defective hepatic mitochondrialrespiratory chain in patients with nonalcoholic steatohepatitis. Hepatology 38,999–1007.
Pessayre, D., 2007. Role of mitochondria in non-alcoholic fatty liver disease. J.Gastroenterol. Hepatol. 1, 20–27.
Pessayre, D., Berson, A., Fromenty, B., Mansouri, A., 2001. Mitochondria insteatohepatitis. Semin. Liver Dis. 21, 57–69.
Pessayre, D., Mansouri, A., Fromenty, B., 2002. Nonalcoholic steatosis andsteatohepatitis. V. Mitochondrial dysfunction in steatohepatitis. Am. J.Physiol. Gastrointest Liver Physiol. 282, 193–199.
Petersen, K.F., Dufour, S., Shulman, G.I., 2005. Decreased insulin-stimulated ATPsynthesis and phosphate transport in muscle of insulin-resistant offspring oftype 2 diabetic parents. PLoS Med. 2, e233.
Portincasa, P., Grattagliano, I., Lauterburg, B.H., Palmieri, V.O., Palasciano, G.,Stellaard, F., 2006. Liver breath tests non-invasively predict higher stages ofnon-alcoholic steatohepatitis. Clin. Sci. (Lond.). 111, 135–143.
C. Koliaki, M. Roden / Molecular and Cellular Endocrinology 379 (2013) 35–42 41

Raffaella, C., Francesca, B., Italia, F., Marina, P., Giovanna, L., Susanna, I., 2008.Alterations in hepatic mitochondrial compartment in a model of obesity andinsulin resistance. Obesity 16, 958–964.
Roden, M., 2004. How free fatty acids inhibit glucose utilization in human skeletalmuscle. News Physiol. Sci. 19, 92–96.
Roden, M., 2005. Muscle triglycerides and mitochondrial function: possiblemechanisms for the development of type 2 diabetes. Int. J. Obes. (Lond.) 29,111–115.
Roden, M., 2006. Mechanisms of Disease: hepatic steatosis in type 2 diabetes–pathogenesis and clinical relevance. Nat. Clin. Pract. Endocrinol. Metab. 2, 335–448.
Roden, M., Bernroider, E., 2003. Hepatic glucose metabolism in humans–its role inhealth and disease. Best Pract. Res. Clin. Endocrinol. Metab. 17, 365–383.
Romestaing, C., Piquet, M.A., Letexier, D., Rey, B., Mourier, A., Servais, S., Belouze, M.,Rouleau, V., Dautresme, M., Ollivier, I., Favier, R., Rigoulet, M., Duchamp, C.,Sibille, B., 2008. Mitochondrial adaptations to steatohepatitis induced by amethionine- and choline-deficient diet. Am. J. Physiol. Endocrinol. Metab. 294,110–119.
Samuel, V.T., Liu, Z.X., Qu, X., Elder, B.D., Bilz, S., Befroy, D., Romanelli, A.J., Shulman,G.I., 2004. Mechanism of hepatic insulin resistance in non-alcoholic fatty liverdisease. J. Biol. Chem. 279, 32345–32353.
Sanyal, A.J., Campbell-Sargent, C., Mirshahi, F., Rizzo, W.B., Contos, M.J., Sterling,R.K., Luketic, V.A., Shiffman, M.L., Clore, J.N., 2001. Nonalcoholic steatohepatitis:association of insulin resistance and mitochondrial abnormalities.Gastroenterology 120, 1183–1192.
Satapati, S., Sunny, N.E., Kucejova, B., Fu, X., He, T.T., Méndez-Lucas, A., Shelton, J.M.,Perales, J.C., Browning, J.D., Burgess, S.C., 2012. Elevated TCA cycle function inthe pathology of diet-induced hepatic insulin resistance and fatty liver. J. Lipid.Res. 53, 1080–1092.
Schmid, A.I., Chmelík, M., Szendroedi, J., Krssák, M., Brehm, A., Moser, E., Roden, M.,2008. Quantitative ATP synthesis in human liver measured by localized 31Pspectroscopy using the magnetization transfer experiment. NMR Biomed. 21,437–443.
Schmid, A.I., Szendroedi, J., Chmelik, M., Krssák, M., Moser, E., Roden, M., 2011. LiverATP synthesis is lower and relates to insulin sensitivity in patients with type 2diabetes. Diabetes Care. 34, 448–453.
Serviddio, G., Sastre, J., Bellanti, F., Viña, J., Vendemiale, G., Altomare, E., 2008a.Mitochondrial involvement in non-alcoholic steatohepatitis. Mol. Aspects Med.29, 22–35.
Serviddio, G., Bellanti, F., Tamborra, R., Rollo, T., Capitanio, N., Romano, A.D., Sastre,J., Vendemiale, G., Altomare, E., 2008b. Uncoupling protein-2 (UCP2) induces
mitochondrial proton leak and increases susceptibility of non-alcoholicsteatohepatitis (NASH) liver to ischaemia-reperfusion injury. Gut 57, 957–965.
Serviddio, G., Bellanti, F., Vendemiale, G., Altomare, E., 2011. Mitochondrialdysfunction in nonalcoholic steatohepatitis. Expert Rev. Gastroenterol.Hepatol. 5, 233–244.
Sharma, R., Sinha, S., Danishad, K.A., Vikram, N.K., Gupta, A., Ahuja, V., Jagannathan,N.R., Pandey, R.M., Misra, A., 2009. Investigation of hepatic gluconeogenesispathway in non-diabetic Asian Indians with non-alcoholic fatty liver diseaseusing in vivo ((31)P) phosphorus magnetic resonance spectroscopy.Atherosclerosis 203, 291–297.
Smith, B.W., Adams, L.A., 2011. Non-alcoholic fatty liver disease. Crit. Rev. Clin. Lab.Sci. 48, 97–113.
Sunny, N.E., Parks, E.J., Browning, J.D., Burgess, S.C., 2011. Excessive hepaticmitochondrial TCA cycle and gluconeogenesis in humans with nonalcoholicfatty liver disease. Cell Metab. 14, 804–810.
Szendroedi, J., Roden, M., 2009. Ectopic lipids and organ function. Curr. Opin.Lipidol. 20, 50–56.
Szendroedi, J., Schmid, A.I., Chmelik, M., Toth, C., Brehm, A., Krssak, M., Nowotny, P.,Wolzt, M., Waldhausl, W., Roden, M., 2007. Muscle mitochondrial ATP synthesisand glucose transport/phosphorylation in type 2 diabetes. PLoS Med. 4, 154.
Szendroedi, J., Chmelik, M., Schmid, A.I., Nowotny, P., Brehm, A., Krssak, M., Moser,E., Roden, M., 2009. Abnormal hepatic energy homeostasis in type 2 diabetes.Hepatology 50, 1079–1086.
Tappy, L., 1995. Regulation of hepatic glucose production in healthy subjects andpatients with non-insulin-dependent diabetes mellitus. Diabetes Metab. 21,233–240.
Vendemiale, G., Grattagliano, I., Caraceni, P., Caraccio, G., Domenicali, M., Dall’Agata,M., Trevisani, F., Guerrieri, F., Bernardi, M., Altomare, E., 2001. Mitochondrialoxidative injury and energy metabolism alteration in rat fatty liver: effect of thenutritional status. Hepatology 33, 808–815.
Vial, G., Dubouchaud, H., Leverve, X.M., 2010. Liver mitochondria and insulinresistance. Acta Biochim. Pol. 57, 389–392.
Vial, G., Dubouchaud, H., Couturier, K., Cottet-Rousselle, C., Taleux, N., Athias, A.,Galinier, A., Casteilla, L., Leverve, X.M., 2011. Effects of a high-fat diet on energymetabolism and ROS production in rat liver. J. Hepatol. 54, 348–356.
Viljanen, A.P., Iozzo, P., Borra, R., Kankaanpää, M., Karmi, A., Lautamäki, R., Järvisalo,M., Parkkola, R., Rönnemaa, T., Guiducci, L., Lehtimäki, T., Raitakari, O.T., Mari,A., Nuutila, P., 2009. Effect of weight loss on liver free fatty acid uptake andhepatic insulin resistance. J. Clin. Endocrinol. Metab. 94, 50–55.
42 C. Koliaki, M. Roden / Molecular and Cellular Endocrinology 379 (2013) 35–42

Energy dissipation in brown adipose tissue: From mice to men
Maarten J. Vosselman, Wouter D. van Marken Lichtenbelt, Patrick Schrauwen ⇑
Department of Human Biology, NUTRIM School for Nutrition, Toxicology and Metabolism, Maastricht University Medical Center+, Maastricht, The Netherlands
a r t i c l e i n f o
Article history:Available online 28 April 2013
Keywords:Brown adipose tissueBeige adipocytesUCP-1ThermogenesisMitochondriaObesity
a b s t r a c t
In rodents, brown adipose tissue (BAT) is a metabolic organ that produces heat in response to cold anddietary intake through mitochondrial uncoupling. For long time, BAT was considered to be solely impor-tant in small mammals and infants, however recent studies have shown that BAT is also functional inadult humans. Interestingly, the presence and/or functionality of this thermogenic tissue is diminishedin obese people, suggesting a link between human BAT and body weight regulation. In the last years, evi-dence has also emerged for the existence of adipocytes that may have an intermediate thermogenic phe-notype between white and brown adipocytes, so called brite or beige adipocytes. Together, these findingshave resulted in a renewed interested in (human) brown adipose tissue and pathways to increase theactivity and recruitment of these thermogenic cells. Stimulating BAT hypertrophy and hyperplasia inhumans could be a potential strategy to target obesity. Here we will review suggested pathways leadingto BAT activation in humans, and discuss novel putative BAT activators in rodents into humanperspective.
! 2013 Elsevier Ireland Ltd. All rights reserved.
1. Introduction
Brown adipose tissue (BAT) is a crucial organ in facultativethermogenesis (acute response) and has a great plasticity to re-spond to long-term changes (e.g. cold acclimation), known asadaptive thermogenesis. In addition to its important role in main-taining thermal homeostasis, BAT is likely to be involved in en-ergy homeostasis as well, since ablation of the essential proteinfor heat production in BAT, uncoupling protein-1 (UCP-1), leadsto an obese phenotype in mice housed at a thermoneutral tem-perature (Feldmann et al., 2009). Furthermore, it has been shownin mice that BAT is involved in plasma triglyceride clearance (Bar-telt et al., 2011) and glucose homeostasis (Guerra et al., 2001;Gunawardana and Piston, 2012). This implies the important roleof BAT in rodents to combat obesity and its related metabolic dis-eases, such as diabetes and cardiovascular disease. Interestingly,prospective studies have now demonstrated BAT to be presentand functional in most (prevalence varying from 40% to 100%)young lean human adults by exposing them to cold (Cypesset al., 2012; Orava et al., 2011; Ouellet et al., 2012; Vijgenet al., 2011; Vosselman et al., 2012; Yoneshiro et al., 2012,
2011). Importantly, an inverse relationship has been shown be-tween adiposity and BAT activity, indicating a relationship be-tween BAT and obesity (Cypess et al., 2009; Saito et al., 2009;van Marken Lichtenbelt et al., 2009; Vijgen et al., 2011). In addi-tion, there is evidence that BAT contributes to nonshivering ther-mogenesis (Orava et al., 2011; Ouellet et al., 2012; Vijgen et al.,2011; Yoneshiro et al., 2011), although this relationship has notalways been found (van Marken Lichtenbelt et al., 2009; Vossel-man et al., 2012). It has been estimated that fully activated BATin humans can contribute to 5% of the basal metabolic rate (vanMarken Lichtenbelt and Schrauwen, 2011). This means that stim-ulation of BAT can have an impact on long-term energy balanceand thus body weight, however only when other factors (e.g. foodintake) remain stable (Christiansen and Garby, 2002). Maybemore important, stimulation of BAT could be supportive in bodyweight maintenance. Therefore, finding strategies to increaseBAT activity and recruitment in humans could be important tocombat obesity and its related chronic metabolic diseases. Cur-rently, much effort is being put in finding ways to increase BATthermogenesis and the recruitment of brown adipocytes in ro-dents. The recent discovery of the so-called brown-in-white(brite) or beige adipocytes has further increased the interest inBAT. Increased ‘‘browning’’ of WAT could be an attractive wayto induce weight loss. It is therefore important to find strategiesto increase the thermogenic machinery of BAT and brown-like tis-sues in humans. This review will provide an overview of the mostpromising pathways to increase BAT activity and recruitment inhumans.
0303-7207/$ - see front matter ! 2013 Elsevier Ireland Ltd. All rights reserved.http://dx.doi.org/10.1016/j.mce.2013.04.017
⇑ Corresponding author. Address: Department of Human Biology, NUTRIM Schoolfor Nutrition, Toxicology and Metabolism, Maastricht University Medical Center,P.O. Box 616, 6200 MD Maastricht, The Netherlands. Tel.: +31 (0) 43 3881502; fax:+31 (0) 43 3670976.
E-mail addresses: [email protected] (M.J. Vosselman),[email protected] (W.D. van Marken Lichtenbelt),[email protected] (P. Schrauwen).
Molecular and Cellular Endocrinology 379 (2013) 43–50
Contents lists available at SciVerse ScienceDirect
Molecular and Cellular Endocrinology
journal homepage: www.elsevier .com/locate /mce

2. Brown, beige and white adipose tissue
2.1. Brown versus white adipose tissue
In rodents, brown adipose tissue is clearly distinguishable fromwhite adipose tissue, since it is richly innervated by the sympa-thetic nervous system (SNS), is highly vascularized, and containsbrown adipocytes with several small lipid vacuoles and many largemitochondria (Frontini and Cinti, 2010). Unique for the brown adi-pocyte is the protein UCP-1 located in the inner mitochondrialmembrane, which allows protons in the intermembrane space tore-enter the mitochondrial matrix without generating ATP, ulti-mately resulting in heat production.
White and brown adipose tissue in mice can be found in distinc-tive or classical (i.e. pure white or pure brown) depots (Fig. 1A). Allthese depots have been characterized by genetic markers, and havea distinct genetic profile that probably determines its function(Waldén et al., 2012). Note that these adipose tissue depots some-times are also viewed as one organ, known as the adipose organ(Cinti, 2001).
The largest BAT depot found in mice, iBAT, is predominantlyfound in human neonates and infants, and then gradually disap-pears after childhood (Heaton, 1972) and is rarely seen in humanadults (Fig. 1B). In adult humans, BAT ([18F]FDG-uptake) is oftenfound in the neck, the mediastinum (para-aortic), and above thekidney (suprarenal), which is comparable to some BAT depots(cBAT, mBAT, prBAT) in mice. Furthermore, BAT in humans is lo-cated along the spinal cord, in the axillary and abdominal region
(suprarenal and perihepatic), and sometimes in areas such as theabdominal wall and acromial–clavicular area. The most prominentand most reported BAT depot in humans is supraclavicular BAT,which has not been found as a distinct depot in mice.
2.2. Brown like cells in white adipose tissue
In addition to classical BAT, a distinct type of adipocytes hasbeen found within WAT depots, the so-called brite (Petrovicet al., 2010) or beige adipocytes (Wu et al., 2012). However, thisis still under dispute as white fat cells may differentiate into brownfat cells (Cinti, 2002). At present, no consensus on the terminologyof these brown-like white adipocytes has been reached, and is ur-gently awaited. However, for sake of clarity we will refer to thesecells as beige adipocytes in the remainder of this review. Thesebeige adipocytes can appear within WAT depots after long-termadrenergic stimulation and cold exposure, and especially appearin the inguinal depot. In the basal state, these beige cells resemblethe unilocular white adipocytes, whereas upon stimulation thesecells obtain a more brown like phenotype. Furthermore, these cellsdo not express the myogenic markers nor the brown adipocytespecific markers Zic1, Lhx8, Meox2, and PRDM16 (Petrovic et al.,2010), but express specific markers as well (e.g. Hoxc9) (Waldénet al., 2012). Interestingly, Wu et al. (2012) were able to isolatebrown-like cells from the subcutaneous (inguinal) adipose depotand found a distinct pool of progenitors giving rise to these so-called beige cell lines. Linkage of the expressed genes after micro-array analysis in these cell lines revealed that beige adipocytes are
A
C
B
D
S
Fig. 1. Overview of brown adipose tissue and beige adipose depots in rodents and humans. (A) Image of a mouse demonstrating classical BAT depots and WAT depots that aresusceptible to browning (beige depots). (B) The upper part shows a PET image of a lean human adult demonstrating 18F-FDG-uptake in BAT locations during cold exposureand the lower image a transversal PET/CT fusion slice, which demonstrates a rare example of interscapular BAT in a lean human adult. (C) Overview of depot specific markersfor both BAT and beige depots in mice. (D) Overview of depot specific markers determined in human BAT based on marker found in beige depots from mice. BAT = Brownadipose tissue, WAT = White adipose tissue. !Measured in children (Sharp et al., 2012), !!Measured in human adults (Wu et al., 2012).
44 M.J. Vosselman et al. / Molecular and Cellular Endocrinology 379 (2013) 43–50

identical, but not similar, to classical brown adipocytes. Thesebeige adipocytes were characterized by unique genetic markers,such as CD137, Tmem26, and Tbx1, and did not contain uniqueBAT markers such as Ebf3, Eva1 and Fbxo31 (Fig. 1C). Furthermore,they found that unstimulated beige cells resemble white adipo-cytes since they have similar low expression of the brown adipo-cyte markers UCP-1, Cidea, and Cox7a1. However, upon cAMPstimulation absolute levels of UCP-1 mRNA and respiratory capac-ity were comparable to classical brown adipocytes. In coherencewith this, Petrovic et al. (2010) showed beige cell recruitment inthe inguinal depot, and that even the purest WAT depot (epidydi-mal) contains preadicpocytes that can be induced to functionalbeige adipocytes. Again, a low basal UCP-1 expression was foundduring baseline conditions, however, after rosiglitazone (PPARcactivator) treatment beige cells increased UCP-1 expression anddemonstrated many features of the classical brown adipocytes.Moreover, oxygen consumption increased after treating these cellswith norepinephrine. In conclusion, it is clear that beige adipocytesare molecular and developmentally different from classical brownadipocytes, however, after stimulation these cells show compara-ble thermogenic potential.
2.3. Type of brown adipocytes in humans
Do humans have brown, beige or both types of adipocytes?Studies measuring BAT via FDG-PET/CT cannot determine the typeof BAT, as it merely measures glucose uptake. However, biopsiesfrom the supraclavicular region (Virtanen et al., 2009) and the peri-thyroid region (Zingaretti et al., 2009) have already demonstrated amixture of both white and brown adipocytes, and showed thatbrown adipocytes occur as islands within WAT. The clearly browncolored depots as found in mice, have not (yet) been found in hu-mans. Interestingly, a recent study has examined several adiposedepots in 13 post-mortem children (aged between 3 days and18 years) and also found the brown like cells dispersed withinWAT (Sharp et al., 2012). These brown adipocyte islands were lo-cated in the subcutaneous supraclavicular areas, posterior medias-tinum, retroperitoneal, intraabdominal, and mesenteric depots.
In the study by Wu et al. (2012), human adipose tissue biopsies(both WAT and BAT) from the supraclavicular area were analyzedfor gene expression. Interestingly, we found increased mRNAexpression of the genes that were characteristic for beige cells(CD137, Tmem26, Tbx1) and not classical murine BAT (Ebf3,Eva1, Fbxo31) (Fig. 1D). In addition, we also performed immuno-histochemistry to identify the beige marker proteins (CD137 andTmem26), and found positive staining for both proteins in theUCP-1 positive cells. Thus, human BAT from the supraclaviculararea in adults has beige characteristics. In the study by Sharpet al. (2012), total RNA was isolated from the BAT depots frompost-mortem children, and interestingly, all BAT depots expressedbeige-cell selective genes and no classical brown fat-selectivegenes (Fig. 1D). They found that these BAT depots correlated wellwith the expression of brown fat genes such as PGC1a andPRDM16, and with beige-cell genes (e.g. Cited1), however not withclassical BAT genes (e.g. Zic1) (Sharp et al., 2012). These findingsthus indicate that human BAT may be composed of mainly beigeadipocytes.
3. BAT physiology
Crucial in activating BAT thermogenesis is the sympathetic ner-vous system (SNS). Furthermore, the thermogenic capacity of BATis dependent on the thyroid hormone axis as well. After sympa-thetic stimulation, norepinephrine (NE) is released at the nerveendings activating the adrenergic receptors on the brown adipo-
cytes. This leads to increased cAMP levels activating protein kinaseA (PKA), which has both acute and chronic effects on BAT. Theacute response of PKA is to increase lipolysis leading to increasedcytosolic FFA levels. These FFA’s are essential for mitochondrial en-ergy dissipation, as they are both used as substrates and to activateUCP-1 in the inner mitochondrial membrane. This acute effect in-creases UCP-1 activity within seconds. On the other hand, pro-longed stimulation of BAT for hours and days will result inincreased amounts of UCP-1 protein, mitochondrial biogenesis,and both hyperplasia and hypertrophy of BAT (Lowell and Spiegel-man, 2000). The thyroid hormone works synergistic with NE and isrequired to generate the full thermogenic response (Silva, 2006).Crucial is the enzyme type II iodothyronine deiodinase (D2, whichcan transform the inactive prohormone thyroxine (T4) into the bio-active hormone triiodothyronine (T3).
In contrast to the extensive knowledge in rodents, the regula-tion and activation of human BAT is still fairly unknown. However,both the SNS and the thyroid axis are thought to be crucial in acti-vation of BAT in humans too. For instance, patients with pheochro-mocytoma, who have elevated plasma catecholamine levels due toa catecholamine-secreting tumor in de adrenal gland, had highrates of [18F]FDG-uptake in BAT in the basal state (Hadi et al.,2007; Joshi and Lele, 2012; Kuji et al., 2008; Yamaga et al., 2008),which disappeared after resection of the tumor (Hadi et al.,2007; Yamaga et al., 2008). Thus, high systemic levels of NE canactivate human BAT, indicating a role for the adrenergic part ofthe SNS. In support, inhibition of b-adrenergic receptors with pro-pranolol diminished [18F]FDG-uptake in the supraclavicular BATduring room temperature (Parysow et al., 2007; Soderlund et al.,2007). In 2009, anatomical evidence for the SNS involvement inBAT was found, as BAT biopsies from the perithyroid (Zingarettiet al., 2009) and supraclavicular region (Virtanen et al., 2009) dem-onstrated sympathetic innervation and mRNA expression of the b3-adrenergic receptor respectively. Finally, disruption of the sympa-thetic fibers completely abolished [18F]FDG-uptake in BAT in a pa-tient with the Horner Syndrome (deficiency of sympatheticactivity) (Lebron et al., 2010). With respect to the thyroid hormoneaxis, it is known from patients that thyroid hormone replacementhas significant effects on resting energy expenditure (al-Adsaniet al., 1997). It has also been shown that elevated levels of thyroidhormones are able to increase mitochondrial uncoupling in skele-tal muscle (Lebon, 2001; Mitchell et al., 2010). Although these re-sults may suggest that thyroid hormone also plays a role inactivation of BAT, evidence for such a role in humans has so farnot been demonstrated.
4. Known BAT activators in humans
Since the discovery of functional BAT in adult humans, somestudies have examined possible routes to activate BAT in humans,which will be discussed here.
4.1. Cold exposure and acclimatization
Currently, the strategy for which most evidence has been gath-ered to activate BAT in humans is cold exposure. In our cold expo-sure experiments we applied a personalized cooling protocol inwhich we decreased ambient temperature until shivering occurred(16–17 "C) and then increased temperature slightly again. At thesemild cold temperatures, cold-induced thermogenesis levels inyoung lean male adults were observed between 5% and 30% (vanMarken Lichtenbelt et al., 2009; Vosselman et al., 2012). Brownadipose tissue was present in all individuals, however the activitylevel of BAT did not correlate to cold-induced thermogenesis. Otherstudies did find a relationship between BAT presence and/or activ-
M.J. Vosselman et al. / Molecular and Cellular Endocrinology 379 (2013) 43–50 45

ity and cold-induced thermogenesis (Orava et al., 2011; Ouelletet al., 2012; Vijgen et al., 2012, 2011; Yoneshiro et al., 2011). Coldexposure likely increased BAT activity via the SNS as shown by in-creased plasma NE levels during cold exposure (Orava et al., 2011;Vosselman et al., 2012).
It is well known from animal studies that long-term cold expo-sure leads to BAT recruitment in both BAT and WAT depots (Younget al., 1984). A cold acclimation study in humans in 1961 demon-strated that long-term cold exposure was effective to increasecold-induced thermogenesis in man, with a decrease in shivering,indicating a potential role for BAT (Davis, 1961). Preliminary re-sults from our lab confirm this adaptive response to cold acclima-tion as both cold-induced (non-shivering) thermogenesis and BATactivity increase (unpublished results).
4.2. Isoprenaline and ephedrine
Rodent studies have clearly demonstrated that BAT can be acti-vated (acute) and recruited (chronic) upon adrenergic receptoragonist treatment. Recently, three studies measured the effect ofadrenergic stimulation on BAT activity in human adults. We mea-sured BAT activity in lean human adults during infusion of the non-selective b-adrenergic agonist isoprenaline, and compared this tocold exposure (Vosselman et al., 2012). Isoprenaline infusion in-creased energy expenditure with 20% comparable to levels duringcold exposure (17%). Surprisingly, nine out of ten subjects showedno BAT activity during isoprenaline infusion, whereas cold expo-sure increased BAT activity in all subjects. Cypess et al. (2012)studied the effects of ephedrine (1 mg/kg), which is a sympathom-imetic drug activating b-adrenergic receptors directly and indi-rectly by enhancing NE release from the sympathetic terminals,on BAT activity and compared this with cold exposure and placebo.In coherence with our results (Vosselman et al., 2012), ephedrinedid not result in BAT activity measured by FDG-PET/CT measure-ments, whereas cold exposure activated BAT in all subjects (Cypesset al., 2012). However, a recent study using higher dosages ofephedrine (2.5 mg/kg) did find increased BAT activity in six outof nine lean human adults, however not in obese subjects (Careyet al., 2013). This is the first study that showed that pharmacolog-ical treatment of BAT in humans is possible. The activity level ofBAT was still 4-fold lower than observed during cold exposure.The explanation for the lack of effect of systemic adrenergic stim-ulation on BAT activation is likely that the concentrations of NEreached at the brown adipocyte cell surface during central stimu-lation (e.g. cold exposure) are higher than systemically reachedby the sympathomimetics used in these studies. Thus, pharmaco-logical stimulation of BAT is possible, however high dosages are re-quired. A major burden of very high levels of sympathomimeticdrugs is the cardiovascular load induced by adrenergic agonists.All three studies observed increased blood pressure and heart ratelevels, with the highest increase in systolic blood pressure(45 mmHg) measured in the study by Carey et al. (2013).
4.3. Capsinoids
Another route to activate BAT via the SNS is via ingestion of cer-tain food components. One such component are the capsinoids(non-pungent capsaicin analogs), the active compound found inchili pepper, which is known to increase BAT activity in rodents(Kawabata et al., 2009), and RMR in humans (Whiting et al.,2012), although this has not been consistenly shown (among oth-ers: Galgani and Ravussin, 2010). A recent study showed that cap-sinoids could be effective in activating BAT in humans (Yoneshiroet al., 2012), without inducing unwanted side-effects. Althoughthey did not directly measure the effect of capsinoid intake onBAT activity, they found that subjects with BAT (based on cold
PET-CT) showed a higher increase in energy expenditure upon cap-sinoid intake compared to subjects without BAT. The proposedmechanism is that capsinoids activate the transient receptor po-tential channel 1 (TRPV1) located in the upper digestive tract lead-ing to increased sympathetic nerve activity to BAT, asdemonstrated in interscapular BAT in rats (Ono et al., 2011). Directevidence for the effect of capsinoids on BAT in humans is needed todraw definite conclusions. Furthermore, whether long-termadministration of these bioactive compounds can induce weightloss via BAT remains to be studied.
4.4. Insulin
Another way to induce glucose uptake in BAT is via insulin(Orava et al., 2011). In this study, insulin infusion (hyperinsuline-mic euglycemia) was compared with cold exposure on BAT glucoseuptake and perfusion. They showed that insulin increased[18F]FDG-uptake in BAT to similar levels as in skeletal muscle,and much higher than in WAT. This was most likely due to the highexpression of GLUT4 in BAT compared to WAT. However, the in-creased [18F]FDG-uptake in BAT was not accompanied by increasedperfusion, suggesting that glucose is solely transported in BATwithout concomitant thermogenesis taking place. Since insulinleads to high glucose uptake in BAT, it would be interesting to mea-sure whether BAT is involved in glucose uptake, and possibly ther-mogenesis, in the postprandial state as well. It is known fromrodent studies that single meals can activate BAT, which could bedue to insulin release (Cannon and Nedergaard, 2004).
5. Novel putative BAT activators
Next to the known activators of BAT as described above, novelfindings in mainly rodent studies hint towards other potentiallyimportant activators of BAT. The focus of this paragraph will beon the hormones irisin (released by muscle) and the natriureticpeptides (released by heart). We have chosen for these hormonesas they are released under physiological conditions (exercise andcardiac stress), and because there is already indirect evidence ofthese activators in humans. For information on the other potentialBAT activators we would like to refer to other reviews (Whittle,2012; Whittle and Vidal-Puig, 2012).
5.1. Exercise and brown adipose tissue: irisin
Exercise is well known for its beneficial effects on systemicmetabolism. In the past decades, several animal studies haveinvestigated whether exercise has beneficial effects on BAT activityand recruitment. It was hypothesized that exercise could affectBAT function via the SNS, as exercise is known to increase generalSNS activity (Wickler et al., 1987). However, most studies did notfind any stimulatory effect of exercise on BAT activity (Scarpaceet al., 1994; Segawa et al., 1998; Shibata and Nagasaka, 1987;Wickler et al., 1987), except for studies using swimming exerciseprotocols (Hirata, 1982a,b; Oh-ishi et al., 1996), which probably in-duced BAT activity to compensate for the heat loss to the water.
However, recent studies in rodents did observe stimulating ef-fects of exercise on brown and beige adipocytes (Boström et al.,2012; Seebacher and Glanville, 2010; Slocum et al., 2012; Xuet al., 2011). A study in rats demonstrated that a low level of exer-cise training is beneficial for the metabolic response upon coldexposure in classical BAT (Seebacher and Glanville, 2010). It wasshown that exercise in combination with cold exposure led to anincrease in UCP-1 expression in BAT, whereas cold exposure(12 "C) alone did not, suggesting that physical activity is requiredfor an optimal heat producing BAT machinery. Xu et al. (2011)
46 M.J. Vosselman et al. / Molecular and Cellular Endocrinology 379 (2013) 43–50

found that exercise in mice led to increased recruitment of adipo-genic progenitor cells in interscapular BAT and increased UCP-1expression ("twofold). Interestingly, in addition to these stimulat-ing effects of exercise on classical BAT, they found an increasedexpression of the thermogenic gene program in epidydimal (vis-ceral) adipose tissue, including increased UCP-1 levels ("twofold).Another study showed the occurrence of beige cells within the ret-roperitoneal depot (visceral) of rats already after 1 week of exer-cise (De Matteis et al., 2012). Quantification of UCP-1 positiveadipocytes within the retriperitoneal WAT showed a 8-fold in-crease in the number of brown cells in the exercise group versuscontrols.
Interestingly, a recent study demonstrated that endurance exer-cise predominantly results in browning of subcutaneous WAT(Boström et al., 2012). In this study, Boström et al. found that miceoverexpressing the transcriptional coactivator PGC1-a showed in-creased browning in inguinal WAT. Since exercise also increasesPGC1-a, they examined the effect of endurance exercise on mark-ers of browning and observed similar effects. In further studies,they identified a new hormone called irisin, which is released byskeletal muscle after proteolysis of the membrane protein FNDC5.Boström et al. found that the irisin precursor FNDC5 inducedbrowning in primary subcutaneous white adipocytes demon-strated by increased UCP1 mRNA (7–500-fold) and the upregula-tion of thermogenic genes (Ucp1, Elovl3, Cox7a1 and Otop1).Adenoviral-mediated overexpression of FNDC5 in mouse liver re-sulted in plasma irisin levels to be increased 3–4-fold, which in-creased UCP1 mRNA 13-fold in subcutaneous WAT. Furthermore,the same technique was used in C557BL/6 mice, which are proneto diet-induced obesity and diabetes, and increased irisin levelsleading to improved glucose tolerance, decreased fasting insulin,increased oxygen consumption and reduced body weight. Togetherthese results demonstrate the possible beneficial effects of endur-ance exercise on the recruitment of beige cells within subcutane-ous white adipose tissue, and moreover, the potential of irisin toinduce a more healthy metabolic phenotype.
Are these stimulating effects of exercise on the recruitment ofbeige cells translatable to humans? Importantly, the authorsshowed that irisin in mice and humans are 100% identical and thatplasma irisin levels were increased twofold after 10 weeks ofendurance training in human subjects (Boström et al., 2012). Inter-estingly, a study in patients with heart failure demonstrated in-creased FNDC5 expression in skeletal muscle in the patient groupwith a better aerobic performance (Lecker et al., 2012). Conversely,a recent study by Timmons et al. (2012) demonstrated that thestimulating effect of exercise on FNDC5 is limited. They analyzedFNDC5 induction by means of gene expression arrays in musclebiopsies from "200 subjects from different exercise programs(both endurance and resistance straining) from earlier publishedstudies. They found that endurance exercise (6 weeks of endurancecycling) in young adults as well as resistance training in 20–80 year old men did not increase FNDC5 mRNA. However, onlyhighly active elderly subjects did show increased (30%) FNDC5compared to sedentary controls. The authors therefore concludethat the stimulatory effect of exercise on irisin production is lim-ited and that irisin probably has little contribution to the overallbroad benefits of exercise on metabolic status.
Another recent paper on irisin presented data from cross-sec-tional and interventional studies on the physiological role of irisinin humans looking at correlations with anthropometric, metabolic,and hormonal parameters (Huh et al., 2012). The presence ofFNDC5 in human tissues, in skeletal muscle but also in the pericar-dium, intracranial artery, and rectum (cardiac and smooth mus-cles) was confirmed and muscle mass was found to be theprimary predictor of circulating irisin in humans. However no sup-port for a beneficial role for irisin in metabolic regulation in a cross
sectional study of 117 middle-aged women (BMI range 20–47.7 kg/m2) was found. Interestingly, acute anaerobic exercise (sprint exer-cise) in young healthy subjects increased irisin levels, whereaschronic exercise of 8 weeks (three times sprint exercise per week)did not. It is important to note that this study solely looked atanaerobic exercise; it is known that aerobic exercise increasesPGC1a to a greater extent than anaerobic exercise (Handschinand Spiegelman, 2008), and this (aerobic) type of exercise wouldthus be more effective in irisin production.
These first human studies question the potential beneficial ef-fects of irisin on metabolic status. However, prospective studiesthat measure the direct effects of exercise on browning are re-quired, and prospective studies should focus on aerobic exerciseprotocols. In addition to the physiological release of irisin by exer-cise, the therapeutic use of irisin in human clinical trials should beinvestigated.
5.2. Natriuretic peptides and brown adipose tissue
A recent study showed that the cardiac natriuretic peptides(NPs) are capable of browning white adipocytes from mice and hu-mans (Bordicchia et al., 2012). The cardiac peptides, atrial NP (ANP)and the ventricular form (BNP), are predominantly known for theirrole in the homeostatic control of blood pressure, by promotingvasodilatation, natriuresis and diuresis, and inhibiting renin andaldosterone release (Levin et al., 1998). Later, these hormones werealso found to regulate lipolysis as demonstrated both in vitro asin vivo (Sengenès et al., 2000). Natriuretic peptides mediate theselipolytic effects predominantly via the NP receptor A (NPRA),whereas the clearance receptor (NPRC) removes the peptides fromthe circulation. Binding of the NPs to the guanylyl cyclase receptorNPRA leads to increased cellular cGMP, which stimulates lipolysisby acting on HSL (Sengenès et al., 2000). These lipolytic effects ofthe NPs were only observed in human WAT, and were thought tobe primate specific due to the high expression of clearance recep-tors and a low expression of ‘‘biologically active’’ receptors in otherspecies (Sengenès et al., 2002).
This was confirmed in the study by Bordicchia et al. (2012), inwhich primary adipocyte cultures from wildtype mice showed nolipolytic response upon ANP infusion. However, in NPRC knockoutmice they did find increased lipolysis in these adipocytes, indicat-ing the inhibitory effects of this clearance receptor. Interestingly,these knockout mice had reduced adipose tissue mass and a morebrownish adipose tissue phenotype. In support, brown adipocytemarker genes, such as PRDM16, were elevated in both BAT andWAT (inguinal and epididymal). These results indicated the brown-ing effects on WAT via the NPs. It was then shown that exposingmice to cold (4" for 6 h) significantly increased plasma BNP levels,and ANP and BNP mRNA expression in the heart. Furthermore, BNPinfusion in mice increased UCP-1 and PGC-1a mRNA expression inboth WAT and BAT (Bordicchia et al., 2012). Altogether, these datademonstrate that the NPs have the capacity to enhance BAT activ-ity and recruitment in mice in vitro and in vivo.
Do these NPs exert similar effects in humans? AdministeringANP systemically and via a microdialysis probe increased lipolysisin healthy men (Birkenfeld et al., 2005). One functional role for thelipolytic effects of NPs could be substrate supply of fatty acids tothe heart and muscle during aerobic exercise (Moro et al., 2006).In addition, it is thought that the NPs are important regulators inpostprandial fatty acid oxidation in humans (Birkenfeld et al.,2008). Interestingly, it is known in humans that low NP levelsare associated with hypertension, obesity, insulin resistance anddiabetes (Khan et al., 2011; Magnusson et al., 2012). Furthermore,weight loss in obese subjects by lifestyle intervention (Chainani-Wu et al., 2010) and bariatric surgery (Changchien et al., 2011;Chen-Tournoux et al., 2010; St Peter et al., 2006) showed that
M.J. Vosselman et al. / Molecular and Cellular Endocrinology 379 (2013) 43–50 47

BNP levels are increased after weight loss. Interestingly patientswith heart failure who suffer from severe weight loss (cachexia)have increased levels of both forms of NPs (de Lemos et al.,2003; Tikkanen et al., 1985), and elevated energy expenditure lev-els, and it could be suggested that elevated NP levels increasebrown adipocyte recruitment and activity leading to elevated EE.Birkenfeld et al. (2005, 2008) showed that ANP infusion increasedpostprandial energy expenditure, however energy expenditure inthe fasted state was not affected. The dosage (25 ng/kg/min) ofANP used by Birkenfeld et al. (2008) increased plasma ANP concen-trations fourfold (approximately 300 pg/mL), which is lower thanfound in heart failure patients (>500 pg/mL). This relative low dosealready affected lipid mobilization and postprandial thermogenesis(and possibly BAT) without causing any adverse effects. Currently,therapeutic use of NPs (carperitide and nesiritide) in patients withacute heart failure and acutely decompensated heart failure is onlypossible by means of infusion and not orally (Saito, 2010).
The potential effect of NPs on browning in humans has beendemonstrated in the study of Bordicchia et al., where they testedwhether NPs could induce a thermogenic gene program in differ-entiated human multipotent adipose-derived stem (hMADS) cellsand subcutaneous adipocytes. Interestingly, both ANP and BNPactivated PGC-1a and UCP-1 expression, induced mitochondrialbiogenesis, and increased uncoupled and total respiration. Thesefindings imply the potential role of the NPs in increasing acutethermogenesis and brown adipocyte recruitment in humans. Theydemonstrated that the mechanism of action of the NP’s share acommon downstream target with the adrenergic pathway, namelyp38 MAPK. Activation of the p38 MAPK pathway ultimately leadsto increased transcription of UCP-1 and PGC-1a (Bordicchia et al.,2012). Moreover, it was shown that ANP treatment of hMADS ledto a similar increase in UCP-1, PGC-1a, and cytochrome c proteinlevels as shown during b-adrenergic treatment. The authors alsofound that both the adrenergic and NP’s signaling pathways workadditive at very low (physiological) concentrations. The activationpathway of the NPs could therefore play a prominent role in addi-tion to the well-known adrenergic pathway in inducing both short-term as long-term effects on BAT. Currently, this is the only directevidence of browning effects via NPs in humans and future studiesare warranted.
6. Conclusions and perspectives
The current global obesity problem is affecting more than 1.4billion adults of 20 years and older, and strikingly, more than 40million children under the age of five were overweight in 2010(WHO). Obesity goes along with increased risk on developing dis-eases such as type 2 diabetes and cardiovascular diseases. Findingstrategies to induce weight loss are therefore necessary. Currently,brown adipose tissue is regarded as a potential tissue to tackleobesity due to its great capacity to increase energy expenditureand thereby stimulating weight loss. The rediscovery of functionalBAT in humans has resulted in an explosion of BAT studies, espe-cially in rodents, to find potential molecules that could lead toBAT hypertrophy and hyperplasia. It is now clear that a third typeof adipocyte exists, the beige adipocyte, which can be recruitedwithin WAT after cold acclimation and long-term adrenergicreceptor stimulation. This distinct type of adipocyte has shownto arise from a different lineage as the other two types, althoughfunctionally and metabolically seen it is similar to the brown adi-pocyte. Current evidence shows that human BAT is likely com-posed of mainly beige adipocytes.
Prospective studies in humans are scarce, mostly because of thedifficulties associated with the technique to measure BAT activity(PET-CT). Nevertheless, current studies have shown that cold expo-
sure is the most effective in stimulating BAT in humans. Adjustingambient temperature in public buildings to the lower range of ourthermoneutral zone could therefore be a sensible and physiologicalway to increase thermogenesis by increasing the thermogenic po-tential of BAT. Adrenergic agonists (isoprenaline and ephedrine)have not shown to be effective in BAT activation as high dosagesare required. This indicates that pharmacological activation ofBAT via the adrenergic part of the SNS is difficult. Furthermore, amajor drawback of adrenergic agonists and sympathomimetics isthe associated cardiovascular stress. Sympathetic activation viacapsinoids could be a way to increase energy expenditure and pos-sibly weight loss (with low risks of adverse events), and the indi-rect evidence of BAT being a mediator is promising. Insulin hasbeen shown to induce glucose uptake in BAT to higher levels thanWAT, and comparable to skeletal muscle. However, since perfusionof BAT was absent, it remains unclear whether actual thermogen-esis takes place after insulin stimulation.
Interestingly, studies in rodents have shown additionalpathways to activate BAT and recruit beige adipocytes. Two ofthem – irisin and NPs – have recently attracted much attention,but definitive answers in humans are so far lacking. Therefore,the coming years are crucial in finding and testing novel activatorsof BAT in human clinical trials, but most of all to test the hypoth-esis that activation of BAT may indeed be of importance in thetreatment of human obesity. Furthermore, future studies shouldalso reveal if continuous activation of mitochondrial uncouplingin BAT could lead to hyperthermia, as has previously been shownto occur when dinitrophenol was used in humans to obtain weightloss.
Acknowledgements
We would like to thank Boudewijn Brans for his helpful sugges-tions and Anouk van der Lans for providing the PET-CT image.
References
al-Adsani, H., Hoffer, L., Silva, J., 1997. Resting energy expenditure is sensitive tosmall dose changes in patients on chronic thyroid hormone replacement. J. Clin.Endocrinol. Metab. 82, 1118–1125.
Bartelt, A., Bruns, O.T., Reimer, R., Hohenberg, H., Ittrich, H., Peldschus, K., Kaul, M.G.,Tromsdorf, U.I., Weller, H., Waurisch, C., Eychmüller, A., Gordts, P.L., Rinninger,F., Bruegelmann, K., Freund, B., Nielsen, P., Merkel, M., Heeren, J., 2011. Brownadipose tissue activity controls triglyceride clearance. Nat. Med. 17, 200–205.
Birkenfeld, A., Boschmann, M., Moro, C., Adams, F., Heusser, K., Franke, G., Berlan, M.,Luft, F., Lafontan, M., Jordan, J., 2005. Lipid mobilization with physiological atrialnatriuretic peptide concentrations in humans. J. Clin. Endocrinol. Metab. 90,3622–3628.
Birkenfeld, A., Budziarek, P., Boschmann, M., Moro, C., Adams, F., Franke, G., Berlan,M., Marques, M., Sweep, F., Luft, F., Lafontan, M., Jordan, J., 2008. Atrialnatriuretic peptide induces postprandial lipid oxidation in humans. Diabetes 57,3199–3204.
Bordicchia, M., Liu, D., Amri, E.-Z., Ailhaud, G., Dessì-Fulgheri, P., Zhang, C.,Takahashi, N., Sarzani, R., Collins, S., 2012. Cardiac natriuretic peptides act viap38 MAPK to induce the brown fat thermogenic program in mouse and humanadipocytes. J. Clin. Invest. 122, 1022–1036.
Boström, P., Wu, J., Jedrychowski, M., Korde, A., Ye, L., Lo, J., Rasbach, K., Boström, E.,Choi, J., Long, J., Kajimura, S., Zingaretti, M.C., Vind, B.F., Tu, H., Cinti, S., Højlund,K., Gygi, S.P., Spiegelman, B.M., 2012. A PGC1-a-dependent myokine that drivesbrown-fat-like development of white fat and thermogenesis. Nature 481, 463–468.
Cannon, B., Nedergaard, J., 2004. Brown adipose tissue: function and physiologicalsignificance. Physiol. Rev. 84, 277–359.
Carey, A.L., Formosa, M.F., Van Every, B., Bertovic, D., Eikelis, N., Labert, G.W., Kalff,V., Duffy, S.J., Cherk, M.H., Kingwell, B.A., 2013. Ephedrine activates brownadipose tissue in lean but not obese humans. Diabetologia 56, 147–155.
Chainani-Wu, N., Weidner, G., Purnell, D., Frenda, S., Merritt-Worden, T., Kemp, C.,Kersh, E., Ornish, D., 2010. Relation of B-type natriuretic peptide levels to bodymass index after comprehensive lifestyle changes. Am. J. Cardiol. 105, 1570–1576.
Changchien, E., Ahmed, S., Betti, F., Higa, J., Kiely, K., Hernandez-Boussard, T.,Morton, J., 2011. B-type natriuretic peptide increases after gastric bypasssurgery and correlates with weight loss. Surg. Endosc. 25, 2338–2343.
Chen-Tournoux, A., Khan, A., Baggish, A., Castro, V., Semigran, M., McCabe, E.,Moukarbel, G., Reingold, J., Durrani, S., Lewis, G., Newton-Cheh, C., Scherrer-
48 M.J. Vosselman et al. / Molecular and Cellular Endocrinology 379 (2013) 43–50

Crosbie, Kaplan, L.M., Wang, T.J., 2010. Effect of weight loss after weight losssurgery on plasma N-terminal pro-B-type natriuretic peptide levels. Am. J.Cardiol. 106, 1450–1455.
Christiansen, E., Garby, L., 2002. Prediction of body weight changes caused bychanges in energy balance. Eur. J. Clin. Invest. 32, 826–830.
Cinti, S., 2001. The adipose organ: morphological perspectives of adipose tissues.Proc. Nutr. Soc. 60, 319–328.
Cinti, S., 2002. Adipocyte differentiation and transdifferentiation: Plasticity of theadipose organ. J. Endicrinol. Invest. 25, 823–825.
Cypess, A.M., Lehman, S., Williams, G., Tal, I., Rodman, D., Goldfine, A.B., Kuo, F.C.,Palmer, E.L., Tseng, Y.H., Doria, A., Kolodny, G.M., Kahn, C.R., 2009. Identificationand importance of brown adipose tissue in adult humans. N. Engl. J. Med. 360,1509–1517.
Cypess, A.M., Chen, Y.C., Sze, C., Wang, K., English, J., Chan, O., Holman, A.R., Tal, I.,Palmer, M.R., Kolodny, G.M., Kahn, C.R., 2012. Cold but not sympathomimeticsactivates human brown adipose tissue in vivo. Proc. Natl. Acad. Sci. USA 109,10001–10005.
Davis, T., 1961. Chamber cold acclimatization in man. J. Appl. Physiol. 16, 1011–1015.
de Lemos, J., McGuire, D., Drazner, M., 2003. B-type natriuretic peptide incardiovascular disease. Lancet 362, 316–322.
De Matteis, R., Lucertini, F., Guescini, M., Polidori, E., Zeppa, S., Stocchi, V., Cinti, S.,Cuppini, R., 2012. Exercise as a new physiological stimulus for brown adiposetissue activity. Nutr. Metab. Cardiovac. Dis. (Epub ahead of print).
Feldmann, H.M., Golozoubova, V., Cannon, B., Nedergaard, J., 2009. UCP1 ablationinduces obesity and abolishes diet-induced thermogenesis in mice exempt fromthermal stress by living at thermoneutrality. Cell Metab. 9, 203–209.
Frontini, A., Cinti, S., 2010. Distribution and development of brown adipocytes in themurine and human adipose organ. Cell Metab. 11, 253–256.
Galgani, J., Ravussin, E., 2010. Effect of dihydrocapsiate on testing metabolic rate inhumans. Am. J. Clin. Nutr. 92, 1089–1093.
Guerra, C., Navarro, P., Valverde, A., Arribas, M., Brüning, J., Kozak, L., Kahn, C.,Benito, M., 2001. Brown adipose tissue-specific insulin receptor knockoutshows diabetic phenotype without insulin resistance. J. Clin. Invest. 108, 1205–1213.
Gunawardana, S.C., Piston, D.W., 2012. Reversal of type 1 diabetes in mice by brownadipose tissue transplant. Diabetes 61, 674–682.
Hadi, M., Chen, C., Whatley, M., Pacak, K., Carrasquillo, J., 2007. Brown fat imagingwith (18)F-6-fluorodopamine PET/CT, (18)F-FDG PET/CT, and (123)I-MIBGSPECT: a study of patients being evaluated for pheochromocytoma. J. Nucl.Med. 48, 1077–1083.
Handschin, C., Spiegelman, B., 2008. The role of exercise and PGC1alpha ininflammation and chronic disease. Nature 454, 463–469.
Heaton, J., 1972. The distribution of brown adipose tissue in the human. J. Anat. 112,35–39.
Hirata, K., 1982a. Blood flow to brown adipose tissue and norepinephrine-inducedcalorigenesis in physically trained rats. Jpn. J. Physiol. 32, 279–291.
Hirata, K., 1982b. Enhanced calorigenesis in brown adipose tissue in physicallytrained rats. Jpn. J. Physiol. 32, 647–653.
Huh, J., Panagiotou, G., Mougios, V., Brinkoetter, M., Vamvini, M., Schneider, B.,Mantzoros, C., 2012. FNDC5 and irisin in humans: I. Predictors of circulatingconcentrations in serum and plasma and II. mRNA expression and circulatingconcentrations in response to weight loss and exercise. Metabolism 61, 1725–1738.
Joshi, P., Lele, V., 2012. Unexpected visitor on FDG PET/CT-Brown Adipose Tissue(BAT) in mesentery in a case of retroperitoneal extra-adrenalpheochromocytoma: is the BAT activation secondary to catecholamine-secreting pheochromocytoma? Clin. Nucl. Med. 37, 20.
Kawabata, F., Inoue, N., Masamoto, Y., Matsumura, S., Kimura, W., Kadowaki, M.,Higashi, T., Tominaga, M., Inoue, K., Fushiki, T., 2009. Non-pungent capsaicinanalogs (capsinoids) increase metabolic rate and enhance thermogenesis viagastrointestinal TRPV1 in mice. Biosci. Biotechnol. Biochem. 73, 2690–2697.
Khan, A., Cheng, S., Magnusson, M., Larson, M., Newton-Cheh, C., McCabe, E.,Coviello, A., Florez, J., Fox, C., Levy, D., Robins, S.J., Arora, P., Bhasin, S., Lam, C.S.,Vasan, R.S., Melander, O., Wang, T.J., 2011. Cardiac natriuretic peptides, obesity,and insulin resistance: evidence from two community-based studies. J. Clin.Endocrinol. Metab. 96, 3242–3249.
Kuji, I., Imabayashi, E., Minagawa, A., Matsuda, H., Miyauchi, T., 2008. Brownadipose tissue demonstrating intense FDG uptake in a patient with mediastinalpheochromocytoma. Ann. Nucl. Med. 22, 231–235.
Lebon, V., 2001. Effect of triiodothyronine on mitochondrial energy coupling inhuman skeletal muscle. J. Clin. Invest. 108.
Lebron, L., Chou, A., Carrasquillo, J., 2010. Interesting image. Unilateral F-18 FDGuptake in the neck, in patients with sympathetic denervation. Clin. Nucl. Med.35, 899–901.
Lecker, S., Zavin, A., Cao, P., Arena, R., Allsup, K., Daniels, K., Joseph, J., Schulze, P.,Forman, D., 2012. Expression of the irisin precursor FNDC5 in skeletal musclecorrelates with aerobic exercise performance in patients with heart failure. Circ.Heart. Fail. 5, 812–818.
Levin, E., Gardner, D., Samson, W., 1998. Natriuretic peptides. N. Engl. J. Med. 339,321–328.
Lowell, B.B., Spiegelman, B.M., 2000. Towards a molecular understanding ofadaptive thermogenesis. Nature 404, 652–660.
Magnusson, M., Jujic, A., Hedblad, B., Engström, G., Persson, M., Struck, J.,Morgenthaler, N., Nilsson, P., Newton-Cheh, C., Wang, T., Melander, O., 2012.Low plasma level of atrial natriuretic peptide predicts development of diabetes:
the prospective Malmo Diet and Cancer study. J. Clin. Endocrinol. Metab. 97,638–645.
Mitchell, C., Savage, D., Dufour, S., Schoenmakers, N., Murgatroyd, P., Befroy, D.,Halsall, D., Northcott, S., Raymond-Barker, P., Curran, S., Henning, E., Keogh, J.,Owen, P., Lazarus, J., Rothman, D.L., Farooqi, I.S., Shulman, G.I., Chatterjee, K.,Petersen, K.F., 2010. Resistance to thyroid hormone is associated with raisedenergy expenditure, muscle mitochondrial uncoupling, and hyperphagia. J. Clin.Invest. 120, 1345–1354.
Moro, C., Polak, J., Hejnova, J., Klimcakova, E., Crampes, F., Stich, V., Lafontan, M.,Berlan, M., 2006. Atrial natriuretic peptide stimulates lipid mobilization duringrepeated bouts of endurance exercise. Am. J. Physiol. Endocrinol. Met. 290,E864–869.
Oh-ishi, S., Kizaki, T., Toshinai, K., Haga, S., Fukuda, K., Nagata, N., Ohno, H., 1996.Swimming training improves brown-adipose-tissue activity in young and oldmice. Mech. Ageing Dev. 89, 67–78.
Ono, K., Tsukamoto-Yasui, M., Hara-Kimura, Y., Inoue, N., Nogusa, Y., Okabe, Y.,Nagashima, K., Kato, F., 2011. Intragastric administration of capsiate, a transientreceptor potential channel agonist, triggers thermogenic sympatheticresponses. J. Appl. Physiol. 110, 789–798.
Orava, J., Nuutila, P., Lidell, M., Oikonen, V., Noponen, T., Viljanen, T., Scheinin, M.,Taittonen, M., Niemi, T., Enerbäck, S., Virtanen, K.A., 2011. Different metabolicresponses of human brown adipose tissue to activation by cold and insulin. CellMetab. 14, 272–279.
Ouellet, V., Labbé, S., Blondin, D., Phoenix, S., Guérin, B., Haman, F., Turcotte, E.,Richard, D., Carpentier, A., 2012. Brown adipose tissue oxidative metabolismcontributes to energy expenditure during acute cold exposure in humans. J.Clin. Invest. 122, 545–552.
Parysow, O., Mollerach, A.M., Jager, V., Racioppi, S., San Roman, J., Gerbaudo, V.H.,2007. Low-dose oral propranolol could reduce brown adipose tissue F-18 FDGuptake in patients undergoing PET scans. Clin. Nucl. Med. 32, 351–357.
Petrovic, N., Walden, T., Shabalina, I., Timmons, J., Cannon, B., Nedergaard, J., 2010.Chronic peroxisome proliferator-activated receptor gamma (PPARgamma)activation of epididymally derived white adipocyte cultures reveals apopulation of thermogenically competent, UCP1-containing adipocytesmolecularly distinct from classic brown adipocytes. J. Biol. Chem. 285, 7153–7164.
Saito, Y., 2010. Roles of atrial natriuretic peptide and its therapeutic use. J. Cardiol.56, 262–270.
Saito, M., Okamatsu-Ogura, Y., Matsushita, M., Watanabe, K., Yoneshiro, T., Nio-Kobayashi, J., Iwanaga, T., Miyagawa, M., Kameya, T., Nakada, K., Kawai, Y.,Tsujisaki, M., 2009. High incidence of metabolically active brown adipose tissuein healthy adult humans: effects of cold exposure and adiposity. Diabetes 58,1526–1531.
Scarpace, P., Yenice, S., Tümer, N., 1994. Influence of exercise training and age onuncoupling protein mRNA expression in brown adipose tissue. Pharmacol.Biochem. Behav. 49, 1057–1105.
Seebacher, F., Glanville, E., 2010. Low levels of physical activity increase metabolicresponsiveness to cold in a rat (Rattus fuscipes). PLoS ONE 5, e13022.
Segawa, M., Oh-Ishi, S., Kizaki, T., Ookawara, T., Sakurai, T., Izawa, T., Nagasawa, J.,Kawada, T., Fushiki, T., Ohno, H., 1998. Effect of running training on brownadipose tissue activity in rats: a reevaluation. Res. Commun. Mol. Pathol.Pharmacol. 100, 77–82.
Sengenès, C., Berlan, M., De Glisezinski, I., Lafontan, M., Galitzky, J., 2000. Natriureticpeptides: a new lipolytic pathway in human adipocytes. FASEB J. 14, 1345–1351.
Sengenès, C., Zakaroff-Girard, A., Moulin, A., Berlan, M., Bouloumié, A., Lafontan, M.,Galitzky, J., 2002. Natriuretic peptide-dependent lipolysis in fat cells is aprimate specificity. Am. J. Physiol. Regul. Integr. Comp. Physiol. 283, R257–265.
Sharp, L., Shinoda, K., Ohno, H., Scheel, D., Tomoda, E., Ruiz, L., Hu, H., Wang, L.,Pavlova, Z., Gilsanz, V., Kajimura, S., 2012. Human BAT possesses molecularsignatures that resemble beige/brite cells. PLoS ONE 7, e49452.
Shibata, H., Nagasaka, T., 1987. The effect of forced running on heat production inbrown adipose tissue in rats. Physiol. Behav. 39, 377–380.
Silva, J., 2006. Thermogenic mechanisms and their hormonal regulation. Physiol.Rev. 86, 435–464.
Slocum, N., Durrant, J., Bailey, D., Yoon, L., Jordan, H., Barton, J., Brown, R., Clifton, L.,Milliken, T., Harrington, W., Kimbrough, C., Faber, C.A., Cariello, N., Elangbam,C.S., 2012. Responses of brown adipose tissue to diet-induced obesity, exercise,dietary restriction and ephedrine treatment. Exp. Toxicol. Pathol. (Epub aheadof print).
Soderlund, V., Larsson, S.A., Jacobsson, H., 2007. Reduction of FDG uptake in brownadipose tissue in clinical patients by a single dose of propranolol. Eur. J. Nucl.Med. Mol. Imaging 34, 1018–1022.
St Peter, J., Hartley, G., Murakami, M., Apple, F., 2006. B-type natriuretic peptide(BNP) and N-terminal pro-BNP in obese patients without heart failure:relationship to body mass index and gastric bypass surgery. Clin. Chem. 52,680–685.
Tikkanen, I., Fyhrquist, F., Metsärinne, K., Leidenius, R., 1985. Plasma atrialnatriuretic peptide in cardiac disease and during infusion in healthyvolunteers. Lancet 2, 66–69.
Timmons, J.A., Baar, K., Davidsen, P.K., Atherton, P.J., 2012. Is irisin a human exercisegene? Nature 480, E9–10.
van Marken Lichtenbelt, W., Schrauwen, P., 2011. Implications of nonshiveringthermogenesis for energy balance regulation in humans. Am. J. Physiol. Regul.Integr. Comp. Physiol. 301, 96.
M.J. Vosselman et al. / Molecular and Cellular Endocrinology 379 (2013) 43–50 49

van Marken Lichtenbelt, W.D., Vanhommerig, J.W., Smulders, N.M., Drossaerts, J.M.,Kemerink, G.J., Bouvy, N.D., Schrauwen, P., Teule, G.J., 2009. Cold-activatedbrown adipose tissue in healthy men. N. Engl. J. Med. 360, 1500–1508.
Vijgen, G.H., Bouvy, N.D., Teule, G.J., Brans, B., Schrauwen, P., van MarkenLichtenbelt, W.D., 2011. Brown adipose tissue in morbidly obese subjects.PLoS ONE 6, e17247.
Vijgen, G., Bouvy, N., Teule, G.J., Brans, B., Hoeks, J., Schrauwen, P., van MarkenLichtenbelt, W., 2012. Increase in brown adipose tissue activity after weight lossin morbidly obese subjects. J. Clin. Endocrinol. Metab. 97, E1229–1233.
Virtanen, K.A., Lidell, M.E., Orava, J., Heglind, M., Westergren, R., Niemi, T., Taittonen,M., Laine, J., Savisto, N.J., Enerback, S., Nuutila, P., 2009. Functional brownadipose tissue in healthy adults. N. Engl. J. Med. 360, 1518–1525.
Vosselman, M.J., van der Lans, A.A., Brans, B., Wierts, R., van Baak, M.A., Schrauwen,P., Lichtenbelt, W.D., 2012. Systemic b-adrenergic stimulation of thermogenesisis not accompanied by brown adipose tissue activity in humans. Diabetes 61,3106–3113.
Waldén, T., Hansen, I., Timmons, J., Cannon, B., Nedergaard, J., 2012. Recruited vs.nonrecruited molecular signatures of brown, ‘‘brite’’, and white adipose tissues.Am. J. Physiol. Endocrinol. Metab. 302, E19–31.
Whiting, S., Derbyshire, E., Tiwari, B., 2012. Capsaicinoids and capsinoids. Apotential role for weight management? A systematic review of the evidence.Appetite 59, 341–348.
Whittle, A.J., 2012. Searching for ways to switch on brown fat: are we gettingwarmer? J. Mol. Endocrinol. 49, 79–87.
Whittle, A.J., Vidal-Puig, A., 2012. NPs – heart hormones that regulate brown fat? J.Clin. Invest. 122, 804–807.
Wickler, S., Stern, J., Glick, Z., Horwitz, B., 1987. Thermogenic capacity and brown fatin rats exercise-trained by running. Metabolism 36, 76–81.
Wu, J., Boström, P., Sparks, L., Ye, L., Choi, J., Giang, A.-H., Khandekar, M., Virtanen, K.,Nuutila, P., Schaart, G., Huang, K., Tu, H., van Marken Lichtenbelt, W.D., Hoeks, J.,Enerbäck, S., Schrauwen, P., Spiegelman, B.M., 2012. Beige adipocytes are adistinct type of thermogenic fat cell in mouse and human. Cell 150, 366–376.
Xu, X., Ying, Z., Cai, M., Xu, Z., Li, Y., Jiang, S., Tzan, K., Wang, A., Parthasarathy, S., He,G., Rajagopalan, S., Sun, Q., 2011. Exercise ameliorates high-fat diet-inducedmetabolic and vascular dysfunction, and increases adipocyte progenitor cellpopulation in brown adipose tissue. Am. J. Physiol. Regul. Integr. Comp. Physiol.300, R1115–R1125.
Yamaga, L., Thom, A., Wagner, J., Baroni, R., Hidal, J., Funari, M., 2008. The effect ofcatecholamines on the glucose uptake in brown adipose tissue demonstrated by(18)F-FDG PET/CT in a patient with adrenal pheochromocytoma. Eur. J. Nucl.Med. Mol. Imaging 35, 446–447.
Yoneshiro, T., Aita, S., Matsushita, M., Kameya, T., Nakada, K., Kawai, Y., Saito, M.,2011. Brown adipose tissue, whole-body energy expenditure, andthermogenesis in healthy adult men. Obesity (Silver Spring) 19, 13–16.
Yoneshiro, T., Aita, S., Kawai, Y., Iwanaga, T., Saito, M., 2012. Nonpungent capsaicinanalogs (capsinoids) increase energy expenditure through the activation ofbrown adipose tissue in humans. Am. J. Clin. Nutr. 95, 845–850.
Young, P., Arch, J., Ashwell, M., 1984. Brown adipose tissue in the parametrial fatpad of the mouse. FEBS Lett. 167, 10–14.
Zingaretti, M.C., Crosta, F., Vitali, A., Guerrieri, M., Frontini, A., Cannon, B.,Nedergaard, J., Cinti, S., 2009. The presence of UCP1 demonstrates thatmetabolically active adipose tissue in the neck of adult humans trulyrepresents brown adipose tissue. FASEB J. 23, 3113–3120.
50 M.J. Vosselman et al. / Molecular and Cellular Endocrinology 379 (2013) 43–50

Review
Thyroid hormones and mitochondria: With a brief look at derivativesand analogues
Federica Cioffi a,1, Rosalba Senese b,1, Antonia Lanni b,⇑, Fernando Goglia a,⇑a Dipartimento di Scienze e Tecnologie, Università degli Studi del Sannio, Via Port’Arsa 11, 82100 Benevento, Italyb Dipartimento di Scienze e Tecnologie Ambientali, Biologiche e Farmaceutiche, Seconda Università di Napoli, Via Vivaldi 43, 81100 Caserta, Italy
a r t i c l e i n f o
Article history:Available online 13 June 2013
Keywords:MitochondrionThyroid hormoneIodothyronineThyroid hormone analogue
a b s t r a c t
Thyroid hormones (TH) have a multiplicity of effects. Early in life, they mainly affect development and differ-entiation, while later on they have particularly important influences over metabolic processes in almost all tis-sues. It is now quite widely accepted that thyroid hormones have two types of effects on mitochondria. Thefirst is a rapid stimulation of respiration, which is evident within minutes/hours after hormone treatment,and it is probable that extranuclear/non-genomic mechanisms underlie this effect. The second response occursone to several days after hormone treatment, and leads to mitochondrial biogenesis and to a change in mito-chondrial mass. The hormone signal for the second response involves both T3-responsive nuclear genes and adirect action of T3 at mitochondrial binding sites. T3, by binding to a specific mitochondrial receptor andaffecting the transcription apparatus, may thus act in a coordinated manner with the T3 nuclear pathwayto regulate mitochondrial biogenesis and turnover. Transcription factors, coactivators, corepressors, signalingpathways and, perhaps, all play roles in these mechanisms. This review article focuses chiefly on TH, but alsolooks briefly at some analogues and derivatives (on which the data is still somewhat patchy). We summarizedata obtained recently and in the past to try to obtain an updated picture of the current research position con-cerning the metabolic effects of TH, with particular emphasis on those exerted via mitochondria.
! 2013 Elsevier Ireland Ltd. All rights reserved.
Contents
1. Thyroid hormones and iodothyronines: the general picture . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 522. Actions of thyroid hormones . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 52
2.1. Overview of nuclear pathways . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 522.2. Overview of non-nuclear pathways . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 52
3. Mitochondria . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 533.1. Mitochondrial plasticity . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 54
4. Thyroid hormones and mitochondria . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 554.1. Direct way . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 554.2. Indirect ways . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 55
5. Thyroid hormones and mitochondrial energetics. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 565.1. Uncoupling mechanism . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 565.2. Other mechanisms . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 56
6. Thyroid hormone derivatives and analogues . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 576.1. Derivatives . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 576.2. Analogues. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 57
7. Conclusions. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 587.1. Perspectives . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 58References . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 59
0303-7207/$ - see front matter ! 2013 Elsevier Ireland Ltd. All rights reserved.http://dx.doi.org/10.1016/j.mce.2013.06.006
⇑ Corresponding authors. Tel.: +39 0823 274542; fax: +39 0823 274545 (A.Lanni), tel.: +39 0823 274571; fax: +39 0824 23013 (F. Goglia).
E-mail addresses: [email protected] (A. Lanni), [email protected](F. Goglia).
1 These authors contributed equally to the manuscript.
Molecular and Cellular Endocrinology 379 (2013) 51–61
Contents lists available at SciVerse ScienceDirect
Molecular and Cellular Endocrinology
journal homepage: www.elsevier .com/locate /mce

1. Thyroid hormones and iodothyronines: the general picture
The thyroid gland produces two main iodothyronines: 3,5,30,50-tetraiodothyronine (thyroxine or T4) and 3,5,30-triiodo-L-thyronine(T3). TH release from the thyroid occurs as part of a feedback mech-anism involving the pituitary–hypothalamic axis. At any giventime, most T4 and T3 in the body is bound to transport proteins,with only a small, ‘‘unbound’’ or ‘‘free’’, fraction being biologicallyactive. The functions of these proteins most probably include: (a)ensuring a constant supply of TH to the cells and tissues by prevent-ing urinary loss, (b) protecting the organism against abrupt changesin thyroid-hormone production and/or degradation, and (c) ulti-mately protecting against iodine deficiency.
All the circulating T4 is secreted by the thyroid gland, whereasmost (about 80%) of the systemic T3 is generated by deiodinationof T4 within peripheral tissues. T3 is further deiodinated to yield3,30-T2 and also, perhaps, 3,5-T2.
Thyroid-hormone deiodination is mediated by three iodothyro-nine deiodinases: type I deiodinase (D1), preferentially expressedin the liver but also present in kidney, thyroid, and pituitary; typeII deiodinase (D2), present in the central nervous system, anteriorpituitary, brown adipose tissue, and placenta; type III deiodinase(D3), present in the central nervous system, placenta, skin, and fe-tal tissue. For further details on deiodinases, the reader is referredto Orozco et al., 2012; Dentice and Salvatore, 2011; Bianco, 2011.
As mentioned above, T4 is synthesized entirely within the thy-roid, while approximately 80% of T3 is formed by peripheral con-version of T4. Uptake of TH into peripheral tissues is mediated byspecific membrane transporter proteins. Several transporter fami-lies have been identified, among which the monocarboxylatetransporter (MCT) family deserves special attention. Fourteenmembers of this family have been recognized so far, but in only6 of them has a ligand-binding site been identified. MCT8 andMCT10 have been identified as specific TH transporters. However,while MCT8 is currently known to be highly specific only for TH(Friesema et al., 2003), MCT10 also has the ability to carry differenttypes of amino acid [e.g., the carrier polypeptide of various organicanion transporters (OATP1C1, OATP1A2, OPTP1A4)]. Among theOATPs, OATP1C1 is the most interesting for the present purposesbecause it displays high specificity and affinity for certain iodothy-ronines (especially for T4 and rT3, although not for T3). Moreover,its preferential localization within the endothelium of brain capil-laries suggests that OATP1C1 is important for the transport of THacross the blood–brain barrier (Mayerl et al., 2012). The physiolog-ical roles performed by the TH transporters have been discussed inrecent reviews (Kinne et al., 2011; Visser et al., 2011) and so willnot be described here any further.
2. Actions of thyroid hormones
TH act via two distinct pathways: (1) nuclear pathways and (2)non-nuclear pathways.
2.1. Overview of nuclear pathways
At the beginning of the 1960s, Tata and coworkers were the firstto show that administration of TH to hypothyroid rats induced anincrease in their basal metabolic rate, while the simultaneousinjection of an inhibitor of transcription (such as actinomycin-D)inhibited this effect (Tata, 1963). These data implicated the nucleusas the locus for the above action. In other experiments, using iso-lated nuclei, they showed that T3 stimulated DNA-dependentRNA-polymerase activity. Later, Samuels et al. and Oppenheimeret al. identified high-affinity nuclear binding sites for TH, suggest-ing that thyroid hormone nuclear receptors (TR) mediated the
effects of T3 (Tata et al., 1962; Tata et al., 1963; Samuels et al.,1974; Oppenheimer et al., 1974; Bassett et al., 2003). In the ensu-ing years, efforts were made to purify the receptors, but the resultsdid not allow detailed investigation of their molecular propertiesuntil the simultaneous cloning of the receptors by Sap et al.(1986) and Weinberger et al. (1986). In mammals, two genes,TRalpha and TRbeta, encode several thyroid-receptor isoforms(TRalpha1, the two splicing variants TRalpha2 and TRalpha3;TRbeta1, TRbeta2, and TRbeta3, respectively). All TRbeta isoformsretain T3-binding activity, whereas only TRalpha1 of the TRalphaisoforms possesses binding activity. The existence of various iso-forms of TRs raises the question as to whether they have distinctor redundant roles. Their tissue-dependent expressions and devel-opmentally regulated differential expression suggest that theymediate specific isoform-dependent actions. In view of theirsubstantial amino-acid homology with respect to steroid hormonereceptors, all TR isoforms are considered to be members of thelarge superfamily of nuclear receptors that also includes the recep-tors for retinoic acid, vitamin D and peroxisomal proliferator acti-vators. These receptors contain multiple functional domains thatinclude, in particular, a DNA-binding domain (DBD) and a car-boxyl-terminal ligand-binding domain (LBD). The DBD domaincontains about 70 amino acids forming two ‘‘zinc fingers’’. Thisregion is highly conserved and interacts with the specific DNA seg-ments known as ‘‘thyroid-hormone response-elements’’ (TREs). T3receptors are transcription factors: they modulate transcriptionmainly by binding TREs. In the absence of T3, the TR has an intrin-sic transcriptional repressor function. In most cases, the TRs act asheterodimers with a 9-cis retinoic acid receptor (RXR), but thereare also multiple TR complexes that bind to TREs (Farach-Carsonand Davis, 2003). In addition to RXR, many other molecules are di-rectly or indirectly functionally associated with TRs (vitamin D3,peroxisome proliferator-activated receptor (PPAR), corepressors,coactivators, etc.). The transcriptional activity of TRs is regulatedat multiple levels: by T3 itself; by the type of TRE located on thepromoters of T3 target genes; by the developmental- andtissue-dependent expressions of TR isoforms; and by a host ofnuclear coregulatory factors (coactivators and corepressors) withT3-dependent activity. Deeper consideration of these mechanismscan be found in some recent reviews (Oetting and Yen, 2007; Yenet al., 2006; Cheng et al., 2010; Flamant and Gauthier, 2012; Tata,2012).
2.2. Overview of non-nuclear pathways
A number of effects mediated by iodothyronines have been de-scribed for which a binding to TRs can be excluded, and it is cur-rently assumed that these effects involve extranuclear bindingsites in several compartments of the cell (including the plasmamembrane, the cytoskeleton, the cytoplasm, and mitochondria:for review, see Cheng et al., 2010). Unlike the nuclear effects, theextranuclear ones: (i) are independent of thyroid hormone nuclearreceptors; (ii) may occur within a short time (seconds to minutes);and (iii) may be mediated by signal-transducing pathways such ascAMP and protein kinases (Bassett et al., 2003; Farach-Carson andDavis, 2003; Saelim et al., 2004; Axelband et al., 2011). Some stud-ies have demonstrated that plasma membrane-initiated actionsbegin at a binding site on integrin aVb3, a heterodimer protein thatinteracts both with extracellular matrix proteins and thyroidhormones (Bergh et al., 2005; Cody et al., 2007). Other molecules– such as stilbene, resveratrol (Lin et al., 2007, 2008), and dihydro-testosterone (Lin et al., 2009a) – also bind to this integrin (Daviset al., 2009). Lin et al. (2009b) demonstrated that the hormone-binding domain comprises two binding sites. One site is solelyfor the binding of T3 and activates the phosphatidylinositol 3-ki-nase (PI3K) pathway, leading to cytoplasm-to-nucleus shuttling
52 F. Cioffi et al. / Molecular and Cellular Endocrinology 379 (2013) 51–61

of TRa1 and to transcription of the hypoxia-inducible factor-1agene. The second site binds both T3 and T4 and appears to triggerPKC, Ras, Raf1, and MEK, resulting in tyrosine phosphorylation,activation, and nuclear translocation of MAPK (Lin et al., 2009a;Lin et al., 2009b; for review, see Cheng et al., 2010). It is known thatTH affect cellular calcium homeostasis, and this effect is probablydue to a nongenomic action. In fact, a recent study on GH3 cellsshowed that both T2 and T3 exert short-term nongenomic effectson intracellular calcium by modulating plasma-membrane andmitochondrial pathways (Del Viscovo et al., 2012). Those authorsshowed that nimodipine largely prevented the [Ca2+]i increaseselicited by T2 and T3, suggesting that these two iodothyroninesshare L-type VDCC as a plasma-membrane target. Clear nonge-nomic actions have been reported that involve AMP-activatedprotein kinase (AMPK) (Irrcher et al., 2008) and Akt/protein kinaseB (Moeller et al., 2005). In skeletal muscle in vivo, T3 stimulatesboth fatty acid and glucose metabolism through rapid activationsof the associated signaling pathways involving AMPK and Akt/pro-tein kinase B (de Lange et al., 2008). (For a short summary of nucle-ar/non-nuclear pathways of TH see Table 1).
3. Mitochondria
The evidence that TH affects metabolic rate dates back a longway. However, despite this and the increasing knowledge of thephysiology and mechanism of action of TH, several aspects of theireffects on metabolic rate (also called calorigenic effects) remain tobe elucidated. The existing evidence and the current debate are fo-cused on two possible mechanisms that might underlie the calor-igenic effects of TH: (a) a mechanism involving their interactionwith nuclear receptors (TR) and (b) a mechanism involving bothTR and/or certain cellular sites such as mitochondria and the cellmembrane. Actually, both pathways may have cellular respirationas their ultimate target. Mitochondria, because of their knownphysiological functions, have been and continue to be the targetof most studies on the calorigenic effects of TH. Mitochondria, infact, provide about the 90% of the cellular energy supply, and theyare also the headquarters for a multitude of biochemical pathwaysrelated to metabolism (for details, see Fig. 1). Indeed, besides ATPsynthesis, mitochondria are the site of other important biochemi-cal events such as oxidation of fatty acids, production of free
Table 1Some information about nuclear and non-nuclear pathways of TH actions.(For references see text).
Nuclear pathways Non-nuclear signaling pathways
Nuclear Thyroid Hormone Receptors (TR): – cAMP-activated protein kinase (AMPK)– TR-a (TR-a1, TR-a2 e TR-a3)– TR- b (TR-b1, TR-b2 e TR-b3)– TRs act as heterodimers [with i.e.: retinoid X receptor (RXR), peroxisome proliferator-activated
receptors (PPARs) and vitamin D3]– Akt/protein kinase B
– Corepressor [silencing mediator of TH and retinoid action (SMRT) and nuclear corepressor(NCoR)]
– Phosphatidylinositol 3-kinase (PI3K)
– Coactivators [p300, steroid receptor coactivator 1 (SRC-1) and Trip230] – PKC, Ras, Raf1, MEK resulting in activation of mitogen-acti-vated protein kinase (MAPK)
Fig. 1. Schematic representation of most of the mitochondrial activities and functions. The respiratory chain transfers electrons from reduced coenzymes [coming from intra(b-oxidation and TCA cycle) – and extra-mitochondrial (glycolysis) oxidative pathways] to O2 and, pumping out H+ from the matrix to the intermembrane space, generates anelectrochemical gradient, DlH+, which provides the driving force for ATP synthesis by FoF1-ATPase. H+ can also enter the matrix by mechanisms not coupled to ATPsynthesis either directly, across the lipid bilayer, or indirectly, by protein-mediated transport (mechanism not represented). Phosphate carrier (PiC), ADP/ATP carrier (ANT),and Uncoupling protein (UCP) are represented individually. Mitochondrial calcium uniporter (MCU). Anion carriers (ACs). Translocator Inner Membrane (TIM), TranslocatorOuter Membrane (TOM), mitochondrial transcription factor A (mtTFA), Apoptosis-inducing factor (AIF). For further details, see text.
F. Cioffi et al. / Molecular and Cellular Endocrinology 379 (2013) 51–61 53

radical, heme synthesis, the metabolism of some amino acids, theformation and export of Fe/S clusters, iron metabolism, and cal-cium homeostasis. Very recently, the inner-membrane mitochon-drial calcium uniporter has been identified as the channelresponsible for ruthenium-red-sensitive mitochondrial Ca2+ uptake(De Stefani et al., 2011). In addition, mitochondria contribute tomany processes central to both cellular function and dysfunction,including calcium signaling, cell growth and differentiation, cell-cycle control, and cell death.
Mitochondria utilize metabolic substrates to generate ATP. SuchATP synthesis, which occurs via ATPase complex, is coupled to oxy-gen consumption via the proton electrochemical gradient existingacross the inner mitochondrial membrane. The inner mitochon-drial membrane might be expected to be proton-proof and themechanism to be tightly coupled, but actually the coupling is notperfect, and the proton flux across the inner membrane that isnot coupled to ATP synthesis (the so-called proton leak) dissipatespart of the gradient as heat.
3.1. Mitochondrial plasticity
Mitochondrial shape and their positioning within cells is crucialand is tightly regulated by processes of fission and fusion, biogen-esis and autophagy, thus ensuring a relatively stable mitochondrialpopulation (Hailey et al., 2010; Osellame et al., 2012.) In addition,mitochondria are known to be involved in apoptosis, and somerecent data show that they are involved in many other cellularpathways, such as the recently highlighted ones that participatein innate immune responses (West et al., 2011). The number ofmitochondria varies according to the function of the cell-typeand to the physiological state of the cell/organism. The mecha-nisms underlying mitochondrial turnover (i.e., biogenesis,
degradation, autophagy) are now quite well elucidated, at leastin some respects. The process of mitochondrial biogenesis requiresthe coordination of mitochondrial and nuclear genomes. In fact, themitochondrial proteome includes about 1500 proteins, most ofwhich are coded by the nuclear genome, with only 13 being codedby the mitochondrial genome. Accordingly, the biogenesis, abun-dance, morphology, and physiological properties of mitochondriaare regulated primarily by the nuclear genome through a seriesof transcription factors that regulate the activity of the mitochon-drial genome and the expressions of mitochondrial proteins (seeFig. 2).
In recent decades, our knowledge regarding the dynamics ofthese organelles has greatly improved. Indeed, the old view of iso-lated mitochondria as static bean-shaped organelles is agonizingand is now replaced by the view of a dynamic and branched net-work moving throughout the cell and undergoing structural transi-tions and changing the shape, morphology, and size. These changesdepend on the cell-type and on the cell’s status (for review, see Lie-sa et al., 2009). In mitochondria, plasticity and function are interre-lated since plasticity may affect the activity of the organelles, whiletheir function/dysfunction may affect their morphology anddynamics (Kuznetsov et al., 2009). These changes are tightly regu-lated by the balance between ‘‘fusion’’ and ‘‘fission’’, and determinethe appearance of the dynamic organelles, their composition, andfinally their activities and functions (Michel et al., 2012). The prin-cipal elements participating in these events are:
For fusion:
– Mitofusin 1 and 2 (MFN1 and MFN2), which are located in theouter mitochondrial membrane and form homo- and hetero-oligomeric complexes between apposing mitochondria (Koshi-ba et al., 2004; Meeusen et al., 2004; Chen et al., 2005; Detmer
Fig. 2. Schematic representation of the TH-dependent nucleus–mitochondrion cross-talk in the regulation of mitochondrial functions (biogenesis, oxygen consumption, andgene expression). Trough active transport or passive diffusion, TH move from outside the plasma membrane into the cytoplasm approaching the extra-nuclear as well as theextra-mitochondrial space. In the cytoplasm, several events can occur, among which deiodination and binding to cytosolic proteins (i.e. cytosolic TH receptors). These canactivate signal transduction pathways involving MAPKs, PKC and PI3-K-AKT/PKB. Genomic action requires thyroid hormone responsive elements (TREs) for the recognition ofgenes for direct transcriptional regulation [a first set of TH target genes (early expression)]. Some of these target genes serve as intermediate factors and regulate a secondseries of TH target genes (late expression). This group of intermediate factors encompasses transcription factors (NRF-1, NRF-2, PPARc) and transcriptional coactivators (PGC-1a, PGC-1b). These can ultimately enter the mitochondrion and regulate a second series of T3 target genes [e.g. mitochondrial transcription factor A (mtTFA)]. For furtherdetails, see text.
54 F. Cioffi et al. / Molecular and Cellular Endocrinology 379 (2013) 51–61

and Chan, 2007). They are mainly involved in the fusion of outermitochondrial membranes (OMM) and the tethering of mito-chondria to the endoplasmic reticulum (ER) (de Brito and Scorr-ano, 2009).
– The dynamin-like GTPase protein OPA1 (optic atrophy type 1),which is located in the intermembrane space (associated withthe inner mitochondrial membrane) and mediates the fusionof the inner membranes (Cipolat et al., 2004; Chen et al., 2005).
For fission:
– Recruitment of Drp1 (a GTPase belonging to the dynamin family)from the cytosol to the OMM. This step is mediated by a mito-chondrial integral outer membrane protein called Fis1 (fissionprotein 1 homolog) (Liesa et al., 2009). Drp1 oligomerization(regulated by post-translational modification) leads finally tofission (for review, see Chang and Blackstone, 2010). Duringthe above mitochondrial processes, there is mitochondrialexchange of such molecules as mtDNA, and proteins, and partsof membranes (for review, see Westermann, 2010 and Oteraand Mihara, 2011). Several external stimuli may affect mito-chondrial plasticity, including thyroid hormones; however, toour knowledge there are few or no data on this issue at present.
4. Thyroid hormones and mitochondria
Modulation of mitochondrial activity by TH may be effected inone of two ways: direct or indirect.
4.1. Direct way
The direct mode requires the presence inside the organelles ofspecific binding sites for the hormone. In contrast, the indirectone does not need these sites to be present but instead may bemediated by signaling pathways located in different parts of thecell. Concerning the first possibility, the presence of binding sitesfor T3 has been reported by several laboratories. High-affinitybinding sites for T3 in the mitochondrial inner membrane werefirst reported in 1975 by Sterling and Milch (1975). The existenceof mitochondrial binding sites for T3 were confirmed by othersin 1981 (Goglia et al., 1981), but despite this and despite several re-ports of rapid effects of T3 on mitochondria, the physiological sig-nificance of these sites and indeed their very existence, and thephysiological significance of the direct effects were controversialat that time. Subsequently, however, the existence of specific mito-chondrial binding sites for T3 received additional confirmationfrom the work of Morel et al. (1996) and Wrutniak et al. (1995).Morel et al. studied the kinetics of the internalization and specificsubcellular binding of T3 in mouse liver, both in vivo and in vitro.They showed, by quantitative electron microscopic autoradiogra-phy, that after the injection of radiolabeled T3, specific bindingwas evident in five cell-compartments (including mitochondria).Surprisingly, specific binding was not evident in the cytosol, whichcontains T3-binding proteins. Wrutniak et al., using a photoaffinitylabeling technique, identified two T3-binding proteins in rat livermitochondrial extracts. One (molecular weight 43 kDa) was lo-cated in the matrix and the other (MW 28 kDa) in the inner mem-brane. These results are in partial agreement with those obtainedby Sterling and Milch (1975) and by us (Goglia et al., 1981). Thesame group (Wrutniak et al., 1995), using antibodies against thetwo binding domains of c-erbA K1, identified two proteins [mito-chondrial matrix T3-binding protein (p43) and inner mitochondrialmembrane T3-binding protein (p28)] whose location and molecu-lar weight were identical to the mitochondrial T3-binding proteinspreviously described. Bigler et al. (1992) had previously demon-strated that truncated c-erbAK1 proteins are synthesized from
the c-erbA mRNA encoding the full-length TR (47 kDa) by meansof an internal AUG codon. Using an expression vector providedby these authors, Wrutniak et al. (1995) overexpressed a truncated43 kDa c-erbAK1 protein in CV1 cells, and then by cyto-immuno-fluorescence experiments demonstrated that this truncated TRKprotein is specifically imported into mitochondria. Interestingly,the same authors have identified five sequences highly related toTRE within the rat mitochondrial genome, and they further showedthat p43 binds to one of these sequences in the D-loop region,which contains the promoters of the mitochondrial genome. Veryrecently, the same group (Carazo et al., 2012) described an atypicalmechanism for the import of p43 into the mitochondrion andidentified the protein sequences involved in its import. Indeed,two alpha helices in the C-terminal part of p43 are actually mito-chondrial import sequences since fusion to a cytosolic proteininduces its mitochondrial translocation. Helix 5 drives the atypicalmitochondrial import process, whereas helices 10/11 induce aclassical import process. The authors further showed that despiteits inability to drive any mitochondrial import, the N-terminal re-gion of p43 also plays a permissive role since in the presence of theC-terminal import sequences, different N-terminal regions deter-mine whether the protein is imported or not imported. These re-sults clearly demonstrate that p43 has the ability to function as aT3-dependent mitochondrial transcription factor. The p43 mito-chondrial T3 receptor may perform an important role in skeletalmuscle since its depletion adversely affects skeletal muscle devel-opment and activity (Pessemesse et al., 2012).
All these data raise the possibility that mitochondrial bindingsites for T3 may play very important physiological roles in regulat-ing the mitochondrial transcription apparatus, thus leading to aregulation of mitochondrial biogenesis by acting in synchrony withthe nuclear genome. This is an attractive possibility for two rea-sons: (a) T3 influences mitochondrial biogenesis and turnover and(b) the mitochondrial biogenesis or turnover needs the coordinatedparticipation of the nuclear and mitochondrial genetic apparatuses.Actually, early results obtained by us and by others – showing thatT3 regulates the mitochondrial population and the mitochondrialnucleic acid level (Gadaleta et al., 1972; Mutvei et al., 1989; Leoet al., 1976; Goglia et al., 1983) – had already suggested just sucha possibility. Apparently confirmatory results were obtained byMartino et al. (1986), who showed a direct action of T3 on mito-chondrial RNA-polymerase in isolated mitochondria, and subse-quently by Enríquez et al. (1999). The latter authors studied theeffect of T3 (both in vivo and in vitro) on ‘‘in organello’’ mtDNA tran-scription and on the ‘‘in organello’’ footprinting patterns in themtDNA regions involved in the regulation of transcription. Their re-sults confirmed a direct influence of T3 on the mitochondrial tran-scription apparatus, and in particular they showed that T3selectively modulates the alternative H-strand transcription initia-tion sites without a previous activation of nuclear genes.
4.2. Indirect ways
On the basis of the data discussed above, it seems reasonable toconclude that TH have at least three different, but probablyinterconnected, mode of action, by which they regulate the expres-sions of target genes contributing to mitochondrial biogenesis. Thefirst relies on a binding of TH to nuclear TR, and for TH to affect nu-clear gene expression by binding to a TRE. The second involves THaffecting mitochondrial transcription directly by binding to amitochondrial TR. In the third, intermediate factors such as the tran-scription factors NRF-1, NRF-2, and PPARc, and the coactivatorsPGC-1alpha and PGC-1beta may be synthesized, and by enteringthe nucleus, regulate other series of TH-target genes. These mecha-nisms may be additionally affected by many nongenomic actions
F. Cioffi et al. / Molecular and Cellular Endocrinology 379 (2013) 51–61 55

such as post-translational modifications, by the local bioavailabilityor by the direct binding of TH to some cellular targets (see Fig. 2).
The above-mentioned coactivators include the PGC-1 family.The first member of this family to be identified was PGC-1alpha(peroxisome proliferator-activated receptor gamma coactivator1alpha). PGC-1alpha is rapidly and strongly induced by TH. Indeed,PGC-1a expression levels and protein levels were increased,respectively, 13-fold (Weitzel and Iwen 2011) and 3-fold (Irrcheret al., 2003; Weitzel et al., 2003; Venditti et al., 2009) 6 h afteradministration of T3 and this action is mediated by a TRE in thepromoter (Wulf et al., 2008). Besides, recently, Thakran et al. haveshown that PGC-1a partecipates in the T3 induction of CPT1a andPDK4 in the liver and, for regulation of hepatic gene expression,PGC-1a was deacetylated probably through the activation of thenuclear deacetylase SIRT1 (Thakran et al., 2013). It has been shownthat PGC-1alpha has profound influences on adaptive thermogen-esis in brown adipose tissue, on hepatic gluconeogenesis, and onmitochondrial biogenesis. In addition, PGC-1alpha coactivates var-ious nuclear receptors and nuclear respiratory factors, includingthe thyroid hormone receptor (Puigserver et al., 1998; Sadanaet al., 2007; Attia et al., 2010). However, PGC-1alpha knock-outmice and knock-down in cell culture have revealed, respectively:few alterations in mitochondrial biogenesis (Ventura-Clapieret al., 2008; Hock and Kralli, 2009) and few defects in TH-mediatedgene-expression patterns (Wulf et al., 2007). It is possible thatother coactivators of the PGC-1 family may play roles. Recently,the presence of PGC-1alpha has been demonstrated in mitochon-dria. This opens interesting perspectives on the possible roles ofthese coactivators, but further studies will be needed to undiscovertheir functions (Aquilano et al., 2010). PGC-1beta, another memberof the PGC-1 family, seems to be closely related to PGC-1alpha butthere are some differences. PGC-1b, on the other hand, activatesmithochondrial biogenesis by binding to different transcriptionfactors (including TR) and its expression has been shown to be rap-idly and strongly induced by TH (Weitzel et al., 2003) suggesting adirect regulation via a TRE. So PGC-1a and PGC-1b are endoge-nously and rapidly regulated by TH in vivo via a TRE. Other activa-tors regulated by TH include coactivator SRC-1, which plays a rolein thermogenesis (Picard et al., 2002). SRC-1 knock-out mice dis-play features of thyroid resistance (Weiss et al., 1999) highlightinga close connection between SRC-1 and TH. These important aspectshave been recently reviewed in an excellent and comprehensivemanner by Weitzel and Iwen (2011). Recently, other studies havehighlight the clinical relevance of TH. Indeed, recent observationand animal models have shaped our understanding of signalingpathways of thyroid hormone and how this insight might be trans-lated into therapeutic strategies, especially for treating hyperlipid-emia and obesity but also to treat cardiac disease, cancer andimprove cognitive function (Brent, 2012). Infact, TR-b mutationshave been identified in a broad range of cancer including hepato-cellular carcinoma, renal cell carcinoma, erythroleukemias andthyroid cancer (Rosen et al., 2011; Chan and Privalsky, 2010). Inaddition, thyroid hormone acting through TR-a regulates adulthyppocampal neurogenesis which is important in learning, mem-ory and moon (Desouza et al., 2005; Kapoor et al., 2010).
5. Thyroid hormones and mitochondrial energetics
It is universally recognized that TH are unique in their ability tostimulate thermogenesis/calorigenesis (the well-known calori-genic effect of TH). Their main action consists in a stimulation ofcellular respiration while at the same time reducing metabolic effi-ciency. However, despite this phenomenon being known since theend of the 19th century (Magnus-Levy, 1895) and being the subject
of a large number of papers, the mechanism by which TH exerttheir effects on energy metabolism is far from firmly established.
5.1. Uncoupling mechanism
One of the most intriguing hypothesis is the uncouplinghypothesis. This proposes that TH stimulates metabolic rate by act-ing at the mitochondrial level to uncouple the electron transportchain from ATP synthesis. This hypothesis predicts a thyroid-dependent stimulation of energy expenditure without a concomi-tant increase in ATP production (decreased P/O ratio). The earlyexperiments supporting such a possibility were those performedby Lardy and Feldott (1951) and by Hess and Martius (1951),who showed that mitochondria prepared from T4-treated ratsexhibited lower P/O ratios than those from untreated euthyroidcontrols. However, in the early 1960s its validity was questioned,principally because uncoupling was observed only with pharmaco-logical doses of TH. Since some effects were observable in vitro (inisolated mitochondria), the theory implied that TH acted directly atthe mitochondrial level. In addition, the results of such in vitrostudies were not always reproducible, and they were widelythought to reflect chemical artifacts. But, this hypothesis has neverbeen dropped, and it continues to this day to be investigated usingnew approaches. Indeed, it received renewed attention when thediscovery was made that uncoupling proteins are present not onlyin brown adipose tissue (where UCP1, by the mechanism of uncou-pling, is able to dissipate energy, so producing heat), but in almostall tissues and cells, and that their expressions are increased by T3(Lanni et al., 1997; Lanni et al., 1999; de Lange et al., 2001; for re-view, see also Lanni et al., 2003 and Cioffi et al., 2009). These find-ings stimulated attempts to show a possible involvement of theseproteins in the calorigenic effect of T3. In particular, UCP2 (ubiqui-tously expressed) and UCP3 (predominantly expressed in skeletalmuscle) have attracted great interest. The realization that UCP3is present in skeletal muscle, a tissue that is metabolically veryactive, led to this protein being viewed as a possible candidatefor the mediator of the effects of thyroid hormones on resting met-abolic rate. This hypothesis has been investigated and the authorsconcluded that UCP3 does indeed have the potential to be a molec-ular determinant of the effects of T3 on resting metabolic rate (deLange et al., 2001). In that study, they showed that when a singleinjection of T3 was given to hypothyroid rats, a maximal stimula-tion of UCP3 expression was evident at 48 h after the injection. Atthis time-point, the resting metabolic rate also reached its maximalvalue and at the mitochondrial level there was a corresponding in-crease in the proton leak. These results received support from thestudy by Flandin et al. (2009). In that study, to test the possibilitythat T3 might act via UCP3, a UCP3-knockout (KO) model was used.This model was found to exhibit a normal phenotype except thatupon T3 administration, the stimulation of oxygen consumptionwas significantly weaker (by 6%) in the UCP3 KO mice than in thewild-type (WT) mice. These results reinforce the idea that UCP3might play a role in the modulation of energy balance by TH. How-ever, the real uncoupling capacity of UCP3 is under debate, and aquestion has been raised as to whether the uncoupling effect ofUCP3 is a primary function or a secondary one (Goglia and Skula-chev, 2003; and for review, see Azzu et al., 2010).
5.2. Other mechanisms
Other mechanisms have been proposed to contribute to theuncoupling effect of T3. For instance, a recent study showed thatthe mitochondrial uncoupling induced by T3 is transduced (in ratsin vivo and in cultured Jurkat cells) by a gating of the mitochondrialpermeability transition pore (PTP). This T3-induced PTP gating wasabrogated in inositol 1,4,5-trisphosphate [IP(3)] receptor1
56 F. Cioffi et al. / Molecular and Cellular Endocrinology 379 (2013) 51–61

[IP(3)R1](!/!) cells, indicating that the endoplasmic reticulumIP(3)R1 may serve as the upstream target for the mitochondrialactivities of T3 (Yehuda-Shnaidman et al., 2010). Other mechanismsthat may play a role in the calorigenic effects of TH include: (i) themaintenance of transmembrane ion gradients through the action ofNa+/K+-ATPase, Ca2+-ATPase, and Ca2+ cycling in muscle and othertissues, as reviewed in a number of articles (Silva, 2006; Lanniet al., 2001; Silvestri et al., 2005) and (ii) regulation of the expres-sions of a selected set of nuclear genes encoding mitochondrial in-ner membrane proteins (Nelson et al., 1995). However, it seemsunlikely to us that a rapid regulation of mitochondrial respirationcould be achieved by synthesizing respiratory components forinsertion into pre-existing membranes. It seems more likely thatin the regulation of cellular respiration by TH, a double mechanismoperates. One would be a short-term mechanism, useful for a rapidresponse to sudden physiological changes in energy requirements.The other would be a long-term mechanism, useful for respondingto prolonged stimuli (days or weeks) such as a long period of coldexposure or a change in diet or developmental stage. Such a long-term mechanism would ultimately produce a new mitochondrialpopulation that is more or less active (depending on the increasedpresence of respiratory components) and/or more or less efficient(depending on the increased presence of some specific components,such as UCPs). The action of TH on calcium homeostasis may alsoplay a role in the modulation of mitochondrial energy transduction.
6. Thyroid hormone derivatives and analogues
6.1. Derivatives
Until a few years ago, it was a common assumption in the liter-ature that T4 was a precursor, and that T3 was the only active iod-othyronine. However, accumulating evidence suggest that otheriodothyronines – such as T4 itself, as well as some metabolites suchas reverse T3 (rT3), 3-iodothyronamine (T1AM), and 3,5-T2 (T2) –may be of biological relevance. This issue requires too much spacefor us to discuss it here in any detail, and since several published re-views have already provided extensive analyses of the availabledata on these molecules, we will only give a few examples.
First, concerning T4 and rT3: Farwell et al. (2006) compared theabilities of iodothyronines to initiate actin polymerization in astro-cytes, and found that T4 and rT3 are each more potent than T3. Inaddition, they found that acute hormone replacement with eitherT4 or rT3 completely restored microfilament organization, whileacute T3 replacement failed to correct this defect (Farwell et al.,2006).
Second, concerning T1AM: thyronamines (TAMs) are a recentlyidentified class of endogenous signaling compounds. With theexception that TAMs do not possess a carboxylate group, theirstructure is identical to that of thyroid hormone and to those ofdeiodinated thyroid hormone derivatives. The iodothyronamines,which are probably generated by the combined action of deiodin-ases and aromatic amino acid decarboxylase, activate a biogenicamine-like G-protein-coupled receptor (GPCR): namely, traceamine receptor 1 (TAR1). T1AM, which is present both in the bloodand in peripheral tissues, seems to have actions opposite to theclassic actions of TH; indeed, when injected into mice, T1AMinduces rapid falls in body temperature and heart rate. Quite re-cently, it has been shown that T(1)AM has significant physiologicaleffects in mammals, such as reversible, dose-dependent negativeinotropic and chronotropic effects on the heart and a cardioprotec-tive effect in perfused rat hearts subjected to ischemia and reper-fusion (Frascarelli et al., 2011). A more exhaustive description ofthe actions and mechanisms of action of T1AM can be found in arecent review by Piehl et al. (2011).
Third, concerning 3,5-diiodothyronine: until quite recently, thisnaturally occurring molecule was considered to be an inactive iod-othyronine, but the discovery of metabolic effects of T2 attractedthe attention of several group of investigators. Early studiesshowed that T2 was able to stimulate mitochondrial activities(Lanni et al., 1992, 1993, 1994; O’Reilly and Murphy, 1992); the ef-fects of T2 seem to be mediated by a direct interaction with mito-chondria. Specific binding sites for T2 (Goglia et al., 1994b) havebeen described in rat liver mitochondria, but the data concerningmitochondrial sites need to be interpreted with some caution be-cause of the limitations inherent in such studies. Indeed, due tothe inner-ring labeling procedure the 3,5-125I-T2 used for the mea-surement of binding parameters had a low specific activity and itwas possible to perform studies only over a narrow range of con-centrations. However, subsequent studies (Lanni et al., 1994; Ar-nold et al., 1998; Goglia et al., 1994a) showed that addition of T2to the COX complex isolated from bovine heart stimulated itsactivity, and suggested that subunit Va of the COX complex mightbe the binding site for T2 (for review, see Goglia, 2005). Effects ofT2 have also been observed at the level of the plasma membrane(Huang et al., 1999; Incerpi et al., 2002). Interestingly, we recentlysucceeded in showing that in rats that had been fed a high-fat diet,administration of T2 stimulated metabolic rate, reduced the serumcholesterol and triglyceride levels, and improved both glucose tol-erance and insulin resistance, effects which involve the well knownSirtuin 1/AMP-activated protein kinase/PGC-1a pathway (Lanniet al., 2005; de Lange et al., 2011; Moreno et al., 2011,). Similar ef-fects have been observed in humans (Antonelli et al., 2011). How-ever, whether or not the function of T2 is physiological remains tobe elucidated.
6.2. Analogues
The metabolic effects of thyroid hormones have long been thefocus of research because of the potential use of these hormonesas drugs to stimulate body-weight loss and lipid metabolism andto treat some disease such as obesity and diabetes (see Aguerand Harper, 2012). However, the simultaneous induction of delete-rious side effects – such as a thyrotoxic state (tachycardia, musclewasting, bone loss), and especially those at the cardiac level –effectively stopped TH being used for these purposes. Recently,however, it has been shown that newly discovered analogues andderivatives may have similar desirable effects without the delete-rious side effects. Indeed, since the middle of the last century mucheffort has been devoted to the development of analogues of thyroidhormones that might improve serum lipid profiles (i.e., plasmacholesterol, lipoprotein, etc.) without having undesirable cardiaceffects. In the past few years, the attention of scientists has beenfocused on the study of agents that are both tissue- and TRb-selec-tive (TRb-receptors are barely expressed in cardiomyocytes), withthe principal aim of addressing such major medical problems asobesity, ectopic fat accumulation, and atherosclerosis. Representa-tive analogues endowed with these characteristics are GC-1 (sobet-irome) and KB2115 (or eprotirome). They have the potential toreduce serum LDL cholesterol, lipoprotein (a), and triglyceride lev-els without harmful effects on heart or muscle in humans (for re-view, see Moreno et al., 2008; Baxter and Webb, 2009; and Cioffiet al., 2010; Berkenstam et al., 2008). At cellular level, GC-1 is ableto stimulate mitochondrial oxidative processes (Venditti et al.,2010). KB2115 also works additively with another cholesterol-low-ering therapy, statins, to produce greater reductions in serum cho-lesterol (Ladenson et al., 2010). However, very recently it has beenshown that thyroid hormone receptor b agonists prevent hepaticsteatosis in fat-fed rats but impair insulin sensitivity (Vatneret al., 2013. This suggest that the development of future TRbagonists must consider the potential adverse effects on insulin
F. Cioffi et al. / Molecular and Cellular Endocrinology 379 (2013) 51–61 57

sensitivity. (The structure of TH and its analogues/derivates areshown in Table 2).
7. Conclusions
The demands of mitochondria and their complex integrationinto cell biology extend far beyond the provision of ATP. This hasprompted a radical change in our perception of mitochondria,and has made these organelles a major target of investigations intomany aspects of cell biology and medicine. The identification ofnovel mechanisms governing mitochondrial biogenesis andreplication, and of the delicately poised signaling pathways coordi-nating the mitochondrial and nuclear genomes, constitute funda-mental steps in in-depth investigations of the role of TH in themodulation of metabolism and of the real involvement of mito-chondria in these actions. TH affect many aspects of mitochondriaactivity (bioenergetics, transcription, calcium homeostasis, etc.),
and thanks to the considerable efforts made by several groups ofinvestigators around the globe, our knowledge of the influence ofiodothyronines has grown and grown.
7.1. Perspectives
In the future, progress in research into TH and mitochondriamay come from investigations using methods such as proteomics.Indeed, mitochondrial proteomics can be a powerful tool in thestudy of the actions of TH since its coverage can extend to mito-chondrial proteins from all mitochondrial metabolic pathways,including the respiratory chain. Indeed, Silvestri et al. (2010) bycombining 2D-E, mass spectrometry, and blue native (BN) PAGE re-cently identified T2-induced mitochondrial proteins that may beresponsible for the beneficial effects of T2 on liver adiposity andmetabolism. In addition, in the future it should be possible to makeprogress into the possible use of TH analogues/derivatives to
Table 2Structure of TH derivates/analogues.
Thyroid hormones
Thyroid Hormones
Derivates/Analogues
58 F. Cioffi et al. / Molecular and Cellular Endocrinology 379 (2013) 51–61

improve certain worldwide diseases that result from the wide-spread adoption of an inappropriate lifestyle (involving inadequateexercise and an unhealthy diet). These include obesity, cardiovas-cular disease, dyslipidemias, insulin-resistance, and type II diabe-tes. Another future research goal may involve modulation of thenetwork subserving signaling for TH and some analogues/deriva-tives as a way of improving adaptation to endocrine and otherenvironmental signals.
References
Aguer, C., Harper, M.E., 2012. Skeletal muscle mitochondrial energetics in obesityand type 2 diabetes mellitus: endocrine aspects. Best Pract. Res. Clin.Endocrinol. Metab. 26 (6), 805–819.
Antonelli, A., Fallahi, P., Ferrari, S.M., Di Domenicantonio, A., Moreno, M., Lanni, A.,Goglia, F., 2011. 3,5-Diiodo-L-thyronine increases resting metabolic rate andreduces body weight without undesirable side effects. J. Biol. Regul. Homeost.Agents 25 (4), 655–660.
Aquilano, K., Vigilanza, P., Baldelli, S., Pagliei, B., Rotilio, G., Ciriolo, M.R., 2010.Peroxisome proliferator-activated receptor gamma co-activator 1alpha (PGC-1alpha) and sirtuin 1 (SIRT1) reside in mitochondria: possible direct function inmitochondrial biogenesis. J. Biol. Chem. B 285 (28), 21590–21599.
Arnold, S., Goglia, F., Kadenbach, B., 1998. 3,5-Diiodothyronine binds to subunit Vaof cytochrome-c oxidase and abolishes the allosteric inhibition of respiration byATP. Eur. J. Biochem. 252 (2), 325–330.
Attia, R.R., Connnaughton, S., Boone, L.R., Wang, F., Elam, M.B., Ness, G.C., Cook, G.A.,Park, E.A., 2010. Regulation of pyruvate dehydrogenase kinase 4 (PDK4) bythyroid hormone: role of the peroxisome proliferator-activated receptorgamma coactivator (PGC-1 alpha). J. Biol. Chem. 285, 2375–2385.
Axelband, F., Dias, J., Ferrão, F.M., Einicker-Lamas, M.J., 2011. Nongenomic signalingpathways triggered by thyroid hormones and their metabolite 3-iodothyronamine on the cardiovascular system. J. Cell. Physiol. 226 (1), 21–28.
Azzu, V., Jastroch, M., Divakaruni, A.S., Brand, M.D., 2010. The regulation andturnover of mitochondrial uncoupling proteins. Biochim. Biophys. Acta 1797(6–7), 785–791.
Bassett, J.H., Harvey, C.B., Williams, G.R., 2003. Mechanisms of thyroid hormonereceptor-specific nuclear and extra nuclear actions. Mol. Cell. Endocrinol. 213(1), 1–11.
Baxter, J.D., Webb, P., 2009. Thyroid hormone mimetics: potential applications inatherosclerosis, obesity and type 2 diabetes. Nat. Rev. Drug Discov. 8, 308–320.
Bergh, J.J., Lin, H.Y., Lansing, L., Mohamed, S.N., Davis, F.B., Mousa, S., Davis, P.J.,2005. Integrin alphaVbeta3 contains a cell surface receptor site for thyroidhormone that is linked to activation of mitogen-activated protein kinase andinduction of angiogenesis. Endocrinology 146 (7), 2864–2871.
Berkenstam, A., Kristensen, J., Mellstro, M.K., Carlsson, B., Malm, J., Rehnmark, S.,Garg, N., Andersson, C.M., Rudling, M., Sjo berg, F., Angelin, B., Baxter, J.D., 2008.The thyroid hormone mimetic compound KB2115 lowers plasma LDLcholesterol and stimulates bile acid synthesis without cardiac effects inhumans. Proc. Natl. Acad. Sci. USA 105, 663–667.
Bianco, A.C., 2011. Minireview: cracking the metabolic code for thyroid hormonesignaling. Endocrinology 152 (9), 3306–3311.
Bigler, J., Hokanson, W., Eisenman, R.N., 1992. Thyroid hormone receptortranscriptional activity is potentially autoregulated by truncated forms of thereceptor. Mol. Cell. Biol. 12 (5), 2406–2417.
Brent, G.A., 2012. Mechanisms of thyroid hormone action. J. Clin. Invest. 122 (9),3035–3043.
Carazo, A., Levin, J., Casas, F., Seyer, P., Grandemange, S., Busson, M., Pessemesse, L.,Wrutniak-Cabello, C., Cabello, G., 2012. Protein sequences involved in themitochondrial import of the 3,5,30-L-triiodothyronine receptor p43. J. Cell.Physiol. 227 (12), 3768–3777.
Chan, I.H., Privalsky, M.L., 2010. A conserved lysine in the thyroid hormonereceptor-alpha1 DNA-binding domain, mutated in hepatocellular carcinoma,serves as a sensor for transcriptional regulation. Mol. Cancer Res. 8 (1), 15–23.
Chang, C.R., Blackstone, C., 2010. Dynamic regulation of mitochondrial fissionthrough modification of the dynamin-related protein Drp1. Ann. N. Y. Acad. Sci.1201, 34–39.
Chen, H., Chomyn, A., Chan, D.C., 2005. Disruption of fusion results in mitochondrialheterogeneity and dysfunction. J. Biol. Chem. 280 (28), 26185–26192.
Cheng, S.Y., Leonard, J.L., Davis, P.J., 2010. Molecular aspects of thyroid hormoneactions. Endocr. Rev. 31 (2), 139–170.
Cioffi, F., Senese, R., de Lange, P., Goglia, F., Lanni, A., Lombardi, A., 2009. Uncouplingproteins: a complex journey to functions discovery. BioFactors 35, 417–428.
Cioffi, F., Lanni, A., Goglia, F., 2010. Thyroid hormones, mitochondrial bioenergeticsand lipid handling. Curr. Opin. Endocrinol. Diabetes Obes. 17 (5), 402–407.
Cipolat, S., de Brito, O.M., Dal, Zilio B., Scorrano, L., 2004. OPA1 requires mitofusin 1to promote mitochondrial fusion. Proc. Natl. Acad. Sci. USA 101 (45), 15927–15932.
Cody, V., Davis, P.J., Davis, F.B., 2007. Molecular modeling of the thyroid hormoneinteractions with alpha v beta 3 integrin. Steroids 72 (2), 165–170.
Davis, P.J., Davis, F.B., Lin, H.Y., Mousa, S.A., Zhou, M., Luidens, M.K., 2009.Translational implications of nongenomic actions of thyroid hormoneinitiated at its integrin receptor. Am. J. Physiol. Endocrinol. Metab. 297 (6),E1238–E1246.
de Brito, O.M., Scorrano, L., 2009. Mitofusin-2 regulates mitochondrial andendoplasmic reticulum morphology and tethering: the role of Ras.Mitochondrion 9 (3), 222–226.
de Lange, P., Lanni, A., Beneduce, L., Moreno, M., Lombardi, A., Silvestri, E., Goglia, F.,2001. Uncoupling protein-3 is a molecular determinant for the regulation ofresting metabolic rate by thyroid hormone. Endocrinology 142, 3414–3420.
de Lange, P., Senese, R., Cioffi, F., Moreno, M., Lombardi, A., Silvestri, E., Goglia, F.,Lanni, A., 2008. Rapid activation by 3,5,30-L-triiodothyronine of adenosine 50-monophosphate-activated protein kinase/acetyl-coenzyme a carboxylase andakt/protein kinase B signaling pathways: relation to changes in fuel metabolismand myosin heavy-chain protein content in rat gastrocnemius muscle in vivo.Endocrinology 149 (12), 6462–6470.
de Lange, P., Cioffi, F., Senese, R., Moreno, M., Lombardi, A., Silvestri, E., De Matteis,R., Lionetti, L., Mollica, M.P., Goglia, F., Lanni, A., 2011. Nonthyrotoxic preventionof diet-induced insulin resistance by 3,5-diiodo-L-thyronine in rats. Diabetes 60(11), 2730–2739.
De Stefani, D., Raffaello, A., Teardo, E., Szabo, I., Rizzuto, R., 2011. A forty-kilodaltonprotein of the inner membrane is the mitochondrial calcium uniporter. Nature476, 336–340.
Del Viscovo, A., Secondo, A., Esposito, A., Goglia, F., Moreno, M., Canzoniero, L.M.,2012. Intracellular and plasma membrane-initiated pathways involved in the[Ca2+]i elevations induced by iodothyronines (T3 and T2) in pituitary GH3 cells.Am. J. Physiol. Endocrinol. Metab. 302 (11), E1419–E1430.
Dentice, M., Salvatore, D., 2011. Deiodinases: the balance of thyroid hormone: localimpact of thyroid hormone inactivation. J. Endocrinol. 209 (3), 273–282.
Desouza, L.A., Ladiwala, U., Daniel, S.M., Agashe, S., Vaidya, R.A., Vaidya, V.A., 2005.Thyroid hormone regulates hippocampal neurogenesis in the adult rat brain.Mol. Cell. Neurosci. 29 (3), 414–426.
Detmer, S.A., Chan, D.C., 2007. Complementation between mouse Mfn1 and Mfn2protects mitochondrial fusion defects caused by CMT2A disease mutations. J.Cell Biol. 176 (4), 405–414.
Enríquez, J.A., Fernández-Silva, P., Garrido-Pérez, N., López-Pérez, M.J., Pérez-Martos, A., Montoya, J., 1999. Direct regulation of mitochondrial RNA synthesisby thyroid hormone. Mol. Cell. Biol. 19 (1), 657–670.
Farach-Carson, M.C., Davis, P.J., 2003. Steroid hormone interactions with targetcells: cross talk between membrane and nuclear pathways. J. Pharmacol. Exp.Ther. 307 (3), 839–845.
Farwell, A.P., Dubord-Tomasetti, S.A., Pietrzykowski, A.Z., Leonard, J.L., 2006.Dynamic nongenomic actions of thyroid hormone in the developing rat brain.Endocrinology 147, 2567–2574.
Flamant, F., Gauthier, K., 2012. Thyroid hormone receptors: the challenge ofelucidating isotype-specific functions and cell-specific response. Biochim.Biophys. Acta June 13.
Flandin, P., Lehr, L., Asensio, C., Giacobino, J.P., Rohner-Jeanrenaud, F., Muzzin, P.,Jimenez, M., 2009. Uncoupling protein-3 as a molecular determinant of theaction of 3,5,30-triiodothyronine on energy metabolism. Endocrine 36 (2), 246–254.
Frascarelli, S., Ghelardoni, S., Chiellini, G., Galli, E., Ronca, F., Scanlan, T.S., Zucchi, R.,2011. Cardioprotective effect of 3-iodothyronamine in perfused rat heartsubjected to ischemia and reperfusion. Cardiovasc. Drugs Ther. 25 (4), 307–313.
Friesema, E.C., Ganguly, S., Abdalla, A., Manning Fox, J.E., Halestrap, A.P., Visser, T.J.,2003. Identification of monocarboxylate transporter 8 as a specific thyroidhormone transporter. J. Biol. Chem. 278 (41), 40128–40135.
Gadaleta, M.N., Barletta, A., Caldarazzo, M., De Leo, T., Saccone, C., 1972.Triiodothyronine action on RNA synthesis in rat-liver mitochondria. Eur. J.Biochem. 30 (2), 376–381.
Goglia, F., 2005. Biological effects of 3,5-diiodothyronine (T2). Biochemistry (Mosc.)70 (2), 164–172.
Goglia, F., Skulachev, V.P., 2003. A function for novel uncoupling proteins:antioxidant defense of mitochondrial matrix by translocating fatty acidperoxides from the inner to the outer membrane leaflet. FASEB J. 17 (12),1585–1591.
Goglia, F., Torresani, J., Bugli, P., Barletta, A., Liverini, G., 1981. In vitro binding oftriiodothyronine to rat liver mitochondria. Pflug. Arch. 390 (2), 120–124.
Goglia, F., Liverini, G., De Leo, T., Barletta, A., 1983. Thyroid state and mitochondrialpopulation during cold exposure. Pflug. Arch. 396 (1), 49–53.
Goglia, F., Lanni, A., Barth, J., Kadenbach, B., 1994a. Interaction of diiodothyronineswith isolated cytochrome c oxidase. FEBS Lett. 346 (2–3), 295–298.
Goglia, F., Lanni, A., Horst, C., Moreno, M., Thoma, R., 1994b. In vitro binding of 3,5-di-iodo-L-thyronine to rat liver mitochondria. J. Mol. Endocrinol. 13 (3), 275–282.
Hailey, D.W., Rambold, A.S., Satpute-Krishnan, P., Mitra, K., Sougrat, R., Kim, P.K.,Lippincott-Schwartz, J., 2010. Mitochondria supply membranes forautophagosome biogenesis during starvation. Cell 141 (4), 656–667.
Hess, B., Martius, C., 1951. The mode of action of thyroxin. Arch. Biochem. Biophys.33 (3), 486–487.
Hock, M.B., Kralli, A., 2009. Transcriptional control of mitochondrial biogenesis andfunction. Annu. Rev. Physiol. 71, 177–203.
Huang, C.J., Geller, H.M., Green, W.L., Craelius, W., 1999. Acute effects of thyroidhormone analogs on sodium currents in neonatal rat myocytes. J. Mol. Cell.Cardiol. 31 (4), 881–893.
Incerpi, S., De Vito, P., Luly, P., Spagnuolo, S., Leoni, S., 2002. Short-term effects ofthyroid hormones and 3,5-diiodothyronine on membrane transport systems inchick embryo hepatocytes. Endocrinology 143 (5), 1660–1668.
Irrcher, I., Adhihetty, P.J., Sheehan, T., Joseph, A.M., Hood, D.A., 2003. PPARgammacoactivator-1alpha expression during thyroid hormone- and contractile
F. Cioffi et al. / Molecular and Cellular Endocrinology 379 (2013) 51–61 59

activity-induced mitochondrial adaptations. Am. J. Physiol. Cell Physiol. 284 (6),C1669–C1677.
Irrcher, I., Walkinshaw, D.R., Sheehan, T.E., Hood, D.A., 2008. Thyroid hormone(T3)rapidly activates p38 and AMPK in skeletal muscle in vivo. J. Appl. Physiol.104, 178–185.
Kapoor, R., van Hogerlinden, M., Wallis, K., Ghosh, H., Nordstrom, K., Vennstrom, B.,Vaidya, V.A., 2010. Unliganded thyroid hormone receptor alpha1 impairs adulthippocampal neurogenesis. FASEB J. 24 (12), 4793–4805.
Kinne, A., Schülein, R., Krause, G., 2011. Primary and secondary thyroid hormonetransporters Thyroid Research 4 (Suppl. 1), S7.
Koshiba, T., Detmer, S.A., Kaiser, J.T., Chen, H., McCaffery, J.M., Chan, D.C., 2004.Structural basis of mitochondrial tethering by mitofusin complexes. Science305 (5685), 858–862.
Kuznetsov, A.V., Hermann, M., Saks, V., Hengster, P., Margreiter, R., 2009. The cell-type specificity of mitochondrial dynamics. Int. J. Biochem. Cell Biol. 41 (10),1928–1939.
Ladenson, P.W., Kristensen, J.D., Ridgway, E.C., Olsson, A.G., Carlsson, B., Klein, I.,Baxter, J.D., Angelin, B., 2010. Use of the thyroid hormone analogue eprotiromein statin-treated dyslipidemia. N. Engl. J. Med. 362 (10), 906–916.
Lanni, A., Moreno, M., Cioffi, M., Goglia, F., 1992. Effect of 3,30-diiodothyronine and3,5-diiodothyronine on rat liver oxidative capacity. Mol. Cell. Endocrinol. 86,143–148.
Lanni, A., Moreno, M., Cioffi, M., Goglia, F., 1993. Effect of 3,30-di-iodothyronine and3,5-di-iodothyronine on rat liver mitochondria. J. Endocrinol. 136, 59–64.
Lanni, A., Moreno, M., Lombardi, A., Goglia, F., 1994. Rapid stimulation in vitro of ratliver cytochrome oxidase activity by 3,5-diiodo-L-thyronine and by 3,30-diiodo-L-thyronine. Mol. Cell. Endocrinol. 99 (1), 89–94.
Lanni, A., De Felice, M., Lombardi, A., Moreno, M., Fleury, C., Ricquier, D., Goglia, F.,1997. Induction of UCP2 mRNA by thyroid hormones in rat heart. FEBS Lett. 418,171–174.
Lanni, A., Beneduce, L., Lombardi, A., Moreno, M., Boss, O., Muzzin, P., Giacobino, J.P.,Goglia, F., 1999. Expression of uncoupling protein-3 and mitochondrial activityin the transition from hypothyroid to hyperthyroid state in rat skeletal muscle.FEBS Lett. 444, 250–254.
Lanni, A., Moreno, M., Lombardi, A., de Lange, P., Goglia, F., 2001. Control of energymetabolism by iodothyronines. J. Endocrinol. Invest. 24 (11), 897–913.
Lanni, A., Moreno, M., Lombardi, A., Goglia, F., 2003. Thyroid hormone anduncoupling proteins. FEBS Lett. 543, 5–10.
Lanni, A., Moreno, M., Lombardi, A., de Lange, P., Silvestri, E., Ragni, M., Farina, P.,Baccari, G.C., Fallahi, P., Antonelli, A., Goglia, F., 2005. 3,5-Diiodo-L-thyroninepowerfully reduces adiposity in rats by increasing the burning of fats. FASEB J.19 (11), 1552–1554.
Lardy, H.A., Feldott, G., 1951. Metabolic effects of thyroxine in vitro. Ann. N. Y. Acad.Sci. 54 (4), 636–648.
Leo, T., Meo, S., Barletta, A., Martino, G., Goglia, F., 1976. Modification of nucleic acidlevels per mitochondrion induced by thyroidectomy or triiodothyronineadministration. Pflug. Arch. 366 (1), 73–77.
Liesa, M., Palacín, M., Zorzano, A., 2009. Mitochondrial dynamics in mammalianhealth and disease. Physiol. Rev. 89 (3), 799–845.
Lin, H.Y., Tang, H.Y., Shih, A., Keating, T., Cao, G., Davis, P.J., Davis, F.B., 2007. Thyroidhormone is a MAPK-dependent growth factor for thyroid cancer cells and isanti-apoptotic. Steroids 72 (2), 180–187.
Lin, H.Y., Tang, H.Y., Keating, T., Wu, Y.H., Shih, A., Hammond, D., Sun, M., Hercbergs,A., Davis, F.B., Davis, P.J., 2008. Resveratrol is pro-apoptotic and thyroidhormone is anti-apoptotic in glioma cells: both actions are integrin and ERKmediated. Carcinogenesis 29, 62–69.
Lin, H.Y., Sun, M., Lin, C., Tang, H.Y., London, D., Shih, A., Davis, F.B., Davis, P.J., 2009a.Androgen induced human breast cancer cell proliferation is mediated bydiscrete mechanisms in estrogen receptor-alpha-positive and -negative breastcancer cells. J. Steroid Biochem. Mol. Biol. 113, 182–188.
Lin, H.Y., Sun, M., Tang, H.Y., Lin, C., Luidens, M.K., Mousa, S.A., Incerpi, S., DrusanoG,L., Davis, F.B., Davis, P.J., 2009b. L-Thyroxine vs. 3,5,3-triiodo-L-thyronine andcell proliferation: activation of mitogen-activated protein kinase andphosphatidylinositol 3-kinase. Am. J. Physiol. Cell Physiol. 296, C980–C991.
Magnus-Levy, A., 1895. Ueber den respiratorishen Gaswechsel unter Einfluss derThyroidea sowie unter verschieden pathologische Zustand. Berliner KlinischeWochenshrift 32, 650–652.
Martino, G., Covello, C., De Giovanni, R., Filippelli, R., Pitrelli, G., 1986. Direct in vitroaction of thyroid hormones on mitochondrial RNA-polymerase. Mol. Biol. Rep.11 (4), 205–211.
Mayerl, S., Visser, T.J., Darras, V.M., Horn, S., Heuer, H., 2012. Endocrinology 153 (3),1528–1537.
Meeusen, S., McCaffery, J.M., Nunnari, J., 2004. Mitochondrial fusion intermediatesrevealed in vitro. Science 305 (5691), 1747–1752.
Michel, S., Wanet, A., De Pauw, A., Rommelaere, G., Arnould, T., Renard, P., 2012.Crosstalk between mitochondrial (dys)function and mitochondrial abundance.J. Cell. Physiol. 227 (6), 2297–2310.
Moeller, L.C., Dumitrescu, A.M., Refetoff, S., 2005. Cytosolic action of thyroidhormone leads to induction of hypoxia-inducible factor-1_ and glycolytic genes.Mol. Endocrinol. 19, 2955–2963.
Morel, G., Ricard-Blum, S., Ardail, D., 1996. Kinetics of internalization andsubcellular binding sites for T3 in mouse liver. Biol. Cell 86 (2–3), 167–174.
Moreno, M., de Lange, P., Lombardi, A., Silvestri, E., Lanni, A., Goglia, F., 2008.Metabolic effects of thyroid hormone derivatives. Thyroid 18 (2), 239–253.
Moreno, M., Silvestri, E., De Matteis, R., de Lange, P., Lombardi, A., Glinni, D., Senese,R., Cioffi, F., Salzano, A.M., Scaloni, A., Lanni, A., Goglia, F., 2011. 3,5-Diiodo-L-
thyronine prevents high-fat-diet-induced insulin resistance in rat skeletalmuscle through metabolic and structural adaptations. FASEB J. 25 (10), 3312–3324.
Mutvei, A., Kuzela, S., Nelson, B.D., 1989. Control of mitochondrial transcription bythyroid hormone. Eur. J. Biochem. 180 (1), 235–240.
Nelson, B.D., Luciakova, K., Li, R., Betina, S., 1995. The role of thyroid hormone andpromoter diversity in the regulation of nuclear encoded mitochondrial proteins.Biochim. Biophys. Acta 271 (1), 85–91.
Oetting, A., Yen, P.M., 2007. New insights into thyroid hormone action. Best Pract.Res. Clin. Endocrinol. Metab. 21 (2), 193–208.
Oppenheimer, J.H., Schwartz, H.L., Surks, M.I., 1974. Tissue differences in theconcentration of triiodothyronine nuclear binding sites in the rat: liver, kidney,pituitary, heart, brain, spleen and testis. Endocrinology 95, 897–903.
O’Reilly, I., Murphy, M.P., 1992. Studies on the rapid stimulation of mitochondrialrespiration by thyroid hormones. Acta Endocrinol. (Copenh.) 127 (6), 542–546.
Orozco, A., Valverde, R.C., Olvera, A., García, G.C., 2012. Iodothyronine deiodinases: afunctional and evolutionary perspective. J. Endocrinol. 215 (2), 207–219.
Osellame, L.D., Blacker, T.S., Duchen, M.R., 2012. Cellular and molecularmechanisms of mitochondrial function. Best Pract. Res. Clin. Endocrinol.Metab. 26 (6), 711–723.
Otera, H., Mihara, K., 2011. Molecular mechanisms and physiologic functions ofmitochondrial dynamics. J. Biochem. 149 (3), 241–251.
Pessemesse, L., Schlernitzauer, A., Sar, C., Levin, J., Grandemange, S., Seyer, P., Favier,F.B., Kaminski, S., Cabello, G., Wrutniak-Cabello, C., Casas, F., 2012. Depletion ofthe p43 mitochondrial T3 receptor in mice affects skeletal muscle developmentand activity. FASEB J. 26 (2), 748–756.
Picard, F., Géhin, M., Annicotte, J., Rocchi, S., Champy, M.F., O’Malley, B.W.,Chambon, P., Auwerx, J., 2002. SRC-1 and TIF2 control energy balancebetween white and brown adipose tissues. Cell 111 (7), 931–941.
Piehl, S., Hoefig, C.S., Scanlan, T.S., Köhrle, J., 2011. Thyronamines past, present, andfuture. Endocr. Rev. 32 (1), 64–80.
Puigserver, P., Wu, Z., Park, C.W., Graves, R., Wright, M., Spiegelman, B.M., 1998. Acold-inducible coactivator of nuclear receptors linked to adaptivethermogenesis. Cell 92, 829–839.
Rosen, M.D., Chan, I.H., Privalsky, M.L., 2011. Mutant thyroid hormone receptors(TRs) isolated from distinct cancer types display distinct target genespecificities: a unique regulatory repertoire associated with two renal clearcell carcinomas. Mol. Endocrinol. 25 (8), 1311–1325.
Sadana, P., Zhang, Y., Song, S., Cook, G.A., Elam, M.B., Park, E.A., 2007. Regulation ofcarnitine palmitoyltransferase I (CPT-I alpha) gene expression by theperoxisome proliferator activated receptor gamma coactivator (PGC-1)isoforms. Mol. Cell. Endocrinol. 267, 6–16.
Saelim, N., John, L.M., Wu, J., Park, J.S., Bai, Y., Camacho, P., Lechleiter, J.D., 2004.Nontranscriptional modulation of intracellular Ca2+ signaling by ligandstimulated thyroid hormone receptor. J. Cell Biol. 167 (5), 915–924.
Samuels, H.H., Tsai, J.S., Casanova, J., 1974. Thyroid hormone action: in vitrodemonstration of putative receptors in isolated nuclei and soluble nuclearextracts. Science 184 (4142), 1188–1191.
Sap, J., Muñoz, A., Damm, K., Goldberg, Y., Ghysdael, J., Leutz, A., Beug, H.,Vennström, B., 1986. The c-erb-A protein is a high-affinity receptor for thyroidhormone. Nature 324 (6098), 635–640.
Silva, J.E., 2006. Thermogenic mechanisms and their hormonal regulation. Physiol.Rev. 86 (2), 435–464.
Silvestri, E., Schiavo, L., Lombardi, A., Goglia, F., 2005. Thyroid hormones asmolecular determinants of thermogenesis. Acta Physiol. Scand. 184, 265–283.
Silvestri, E., Cioffi, F., Glinni, D., Ceccarelli, M., Lombardi, A., de Lange, P., Chambery,A., Severino, V., Lanni, A., Goglia, F., Moreno, M., 2010. Pathways affected by 3,5-diiodo-L-thyronine in liver of high fat-fed rats: evidence from two-dimensionalelectrophoresis, blue-native PAGE, and mass spectrometry. Mol. BioSyst. 6 (11),2256–2271.
Sterling, K., Milch, P.O., 1975. Thyroid hormone binding by a component ofmitochondrial membrane. Proc. Natl. Acad. Sci. USA 72 (8), 3225–3229.
Tata, J.R., 1963. Inhibition of the biological action of thyroid hormones byactinomycin D and puromycin. Nature 197, 1167–1168.
Tata, J.R., 2012. The road to nuclear receptors of thyroid hormone. Biochim. Biophys.Acta March 17.
Tata, J.R., Ernster, L., Lindberg, O., 1962. Control of basal metabolic rate by thyroidhormones and cellular function. Nature 193, 1058–1060.
Tata, J.R., Ernster, L., Lindberg, O., Arrhenius, E., Pedersen, S., Hedman, R., 1963. Theaction of thyroid hormones at the cell level. Biochem. J. 86 (3),408–428.
Thakran, S., Sharma, P., Attia, R.R., Hori, R.T., Deng, X., Elam, M.B., Park, E.A., 2013.Role of sirtuin 1 in the regulation of hepatic gene expression by thyroidhormone. J. Biol. Chem. 288 (2), 807–818.
Vatner, D.F., Weismann, D., Beddow, S.A., Kumashiro, N., Erion, D.M., Liao, X-H.,Grover, G.J., Webb, P., Phillips, K.J., Weiss, R.E., Bogan, J.S., Baxter, J., Shulman,G.I., Varman, T., Samuel, V.T., 2013. Thyroid hormone receptor b agonistsprevent hepatic steatosis in fat-fed rats but impair insulin sensitivity viadiscrete pathways. Am. J. Physiol. Endocrinol. Metab. May 7. http://dx.doi.org/10.1152/ajpendo.00573.20.
Venditti, P., Bari, A., Di Stefano, L., Cardone, A., Della, Ragione.F., D’Esposito, M., DiMeo, S., 2009. Involvement of PGC-1, NRF-1, and NRF-2 in metabolic responseby rat liver to hormonal and environmental signals. Mol. Cell. Endocrinol. 305(1–2), 22–29.
Venditti, P., Chiellini, G., Di Stefano, L., Napolitano, G., Zucchi, R., Columbano, A.,Scanlan, T.S., Di Meo, S., 2010. The TRbeta-selective agonist, GC-1, stimulates
60 F. Cioffi et al. / Molecular and Cellular Endocrinology 379 (2013) 51–61

mitochondrial oxidative processes to a lesser extent than triiodothyronine. J.Endocrinol. 2010 (205), 279–289.
Ventura-Clapier, R., Garnier, A., Veksler, V., 2008. Transcriptional control ofmitochondrial biogenesis: the central role of PGC-1alpha. Cardiovasc. Res. 79(2), 208–217.
Visser, W.E., Friesema, E.C., Visser, T.J., 2011. Minireview: thyroid hormonetransporters: the knowns and the unknowns. Mol. Endocrinol. 25 (1), 1–14.
Weinberger, C., Thompson, C.C., Ong, E.S., Lebo, R., Gruol, D.J., Evans, R.M., 1986. Thec-erb-A gene encodes a thyroid hormone receptor. Nature 324 (6098), 641–646.
Weiss, R.E., Xu, J., Ning, G., Pohlenz, J., O’Malley, B.W., Refetoff, S., 1999. Micedeficient in the steroid receptor co-activator 1 (SRC-1) are resistant to thyroidhormone. EMBO J. 18 (7), 1900–1904.
Weitzel, J.M., Iwen, K.A., 2011. Coordination of mitochondrial biogenesis by thyroidhormone. Mol. Cell. Endocrinol. 342 (1–2), 1–7.
Weitzel, J.M., Iwen, K.A., Seitz, H.J., 2003. Regulation of mitochondrial biogenesis bythyroid hormone. Exp. Physiol. 88 (1), 121–128.
West, A.P., Shadel, G.S., Ghosh, S., 2011. Mitochondria in innate immune responses.Nat. Rev. Immunol. 11 (6), 389–402.
Westermann, B., 2010. Mitochondrial fusion and fission in cell life and death. Nat.Rev. Mol. Cell Biol. 11 (12), 872–884.
Wrutniak, C., Cassar-Malek, I., Marchal, S., Rascle, A., Heusser, S., Keller, J.M.,Fléchon, J., Dauça, M., Samarut, J., Ghysdael, J., Cabello, G., 1995. A 43-kDaprotein related to c-Erb A alpha 1 is located in the mitochondrial matrix of ratliver. J. Biol. Chem. 270 (27), 16347–16354.
Wulf, A., Harneit, A., Weitzel, J.M., 2007. T3-mediated gene expression isindependent of PGC-1alpha. Mol. Cell. Endocrinol. 270 (1–2), 57–63.
Wulf, A., Harneit, A., Kröger, M., Kebenko, M., Wetzel, M.G., Weitzel, J.M., 2008. T3-mediated expression of PGC-1alpha via a far upstream located thyroid hormoneresponse element. Mol. Cell. Endocrinol. 287 (1–2), 90–95.
Yehuda-Shnaidman, E., Kalderon, B., Azazmeh, N., Bar-Tana, J., 2010. Gating of themitochondrial permeability transition pore by thyroid hormone. FASEB J. 24,93–104.
Yen, P.M., Ando, S., Feng, X., Liu, Y., Maruvada, P., Xia, X., 2006. Thyroid hormoneaction at the cellular, genomic and target gene levels. Mol. Cell. Endocrinol. 246(1–2), 121–127.
F. Cioffi et al. / Molecular and Cellular Endocrinology 379 (2013) 51–61 61

Steroid hormone synthesis in mitochondria
Walter L. Miller ⇑
Department of Pediatrics, University of California San Francisco, San Francisco, CA 94143-1346, USADivision of Endocrinology, University of California San Francisco, San Francisco, CA 94143-1346, USA
a r t i c l e i n f o
Article history:Available online 28 April 2013
Keywords:Cholesterol transportCholesterol side chain cleavageOuter mitochondrial membraneSteroidogenesisSteroidogenic acute regulatory proteinVitamin D
a b s t r a c t
Mitochondria are essential sites for steroid hormone biosynthesis. Mitochondria in the steroidogenic cellsof the adrenal, gonad, placenta and brain contain the cholesterol side-chain cleavage enzyme, P450scc,and its two electron-transfer partners, ferredoxin reductase and ferredoxin. This enzyme system convertscholesterol to pregnenolone and determines net steroidogenic capacity, so that it serves as the chronicregulator of steroidogenesis. Several other steroidogenic enzymes, including 3b-hydroxysteroid dehydro-genase, 11b-hydroxylase and aldosterone synthase also reside in mitochondria. Similarly, the mitochon-dria of renal tubular cells contain two key enzymes participating in the activation and degradation ofvitamin D. The access of cholesterol to the mitochondria is regulated by the steroidogenic acute regula-tory protein, StAR, serving as the acute regulator of steroidogenesis. StAR action requires a complexmulti-component molecular machine on the outer mitochondrial membrane (OMM). Components of thismachine include the 18 kDa translocator protein (TSPO), the voltage-dependent anion chanel (VDAC-1),TSPO-associated protein 7 (PAP7, ACBD3), and protein kinase A regulatory subunit 1a (PKAR1A). The pre-cise fashion in which these proteins interact and move cholesterol from the OMM to P450scc, and themeans by which cholesterol is loaded into the OMM, remain unclear. Human deficiency diseases havebeen described for StAR and for all the mitochondrial steroidogenic enzymes, but not for the electrontransfer proteins or for the components of the cholesterol import machine.
! 2013 Elsevier Ireland Ltd. All rights reserved.
1. Introduction
Six classes of steroid hormones, all of which are indispensablefor mammalian life, are made from cholesterol via complex biosyn-
thetic pathways that are initiated by specialized, tissue-specific en-zymes found in mitochondria. These hormones includeglucocorticoids (cortisol, corticosterone) and mineralocorticoids(aldosterone) produced in the adrenal cortex; estrogens (estradiol),progestins (progesterone) and androgens (testosterone, dihydro-testosterone) produced in the gonads; and calciferols (1,25-dihy-droxy vitamin D [1,25OH2D]) produced in the kidney. Thebiosynthesis of the steroid hormones (Miller and Auchus, 2011)and of 1,25OH2D (a sterol) (Feldman et al., 2013) from cholesterolhave been reviewed recently. There are two specialized aspects tothe mitochondria of these steroidogenic tissues – the specializedmechanisms by which cholesterol is delivered to the mitochondriaand the specialized intra-mitochondrial enzymes that paricipate inthe synthesis of hormonal steroids.
2. Delivery of cholesterol to mitochondria
2.1. Sources of cholesterol
The intracellular transport and distribution of cholesterol priorto its delivery to the mitochondria has been reviewed recently(Miller and Bose, 2011). Cholesterol may be produced de novo fromacetate via a complex pathway primarily found in the endoplasmic
0303-7207/$ - see front matter ! 2013 Elsevier Ireland Ltd. All rights reserved.http://dx.doi.org/10.1016/j.mce.2013.04.014
Abbreviations: 1,25(OH)2D, 1,25 dihydroxy vitamin D (calcitriol); 3bHSD, 3b-hydroxysteroid dehydrogenase; ACAT, acyl transferase; ACTH, adrenocorticotropichormone; ANT, adenine nucleotide transporter; ER, endoplasmic reticulum; CRAC,cholesterol recognition amino acid consensus domain; FAD, flavin adenine dinu-cleotide; HDL, high density lipoproteis; HSL, hormone-sensitive neutral lipase;HMGCoA, 3-hydroxy-3-methylglutaryl co-enzyme A; IMM, inner mitochondrialmembrane; IMS, intramembranous space; Km, Michaelis constant; LAL, lysosomalacid lipase; LDL, low-density lipoproteins; LH, luteinizing hormone; MENTAL,MLN64 N-terminal; MENTHO, MLN64 N-terminal domain homologue; MLN64,metastatic lymph node clone 64; NADPH, nicotinamide adenine dinucleotidephosphate; NPC, Niemann Pick type C; OMM, outer mitochondrial membrane;PAP7, TSPO-associated protein 7 (ACBD3); PBR, peripheral benzodiazepine recep-tor; PCP, phosphate carrier protein; PKA, protein kinase A; PKAR1A, protein kinase Aregulatory subunit 1a; PRAX1, TSPO-associated protein 1; PTH, parathyroidhormone; P450scc, mitochondrial cytochrome P450 specific for cholesterol side-chain cleavage; SF1, steroidogenic factor 1; SOAT, sterol O-acetyltransferase; SR-B1,scavenger receptor B1; StAR, steroidogenic acute regulatory protein; START, StAR-related lipid transfer domain; SREBPs, sterol regulatory element binding proteins;TSPO, 18 kDa translocator protein; VDAC1, voltage-dependent anion channel.⇑ Address: Department of Pediatrics, University of California San Francisco, San
Francisco, CA 94143-1346, USA.E-mail address: [email protected]
Molecular and Cellular Endocrinology 379 (2013) 62–73
Contents lists available at SciVerse ScienceDirect
Molecular and Cellular Endocrinology
journal homepage: www.elsevier .com/locate /mce

reticulum (ER) (Porter and Herman, 2011), but most steroidogeniccholesterol is derived from circulating lipoproteins. High densitylipoproteins (HDL) may be taken up via scavenger receptor B1(SR-B1) and low-density lipoproteins (LDL) are taken up by recep-tor-mediated endocytosis via LDL receptors. LDL can suppress therate-limiting enzyme in cholesterol synthesis, 3-hydroxy-3-meth-ylglutaryl co-enzyme A (HMGCoA) reductase. Rodents preferenti-aly use the HDL/SR-B1 pathway to obtain steroidogeniccholesterol, but the principal human source is receptor-mediatedendocytosis of LDL. Nevertheless, patients with congenital abeta-lipoproteinemia have low LDL cholesterol but have normal basalcortisol concentrations, and only mildly impaired cortisol re-sponses to adrenocorticotropic hormone (ACTH) (Illingworthet al., 1982), and those treated with high doses of statins have noimpairment of cortisol secretion (Dobs et al., 2000). Thus endoge-nously produced cholesterol is sufficient in most situations, andthe HDL/SR-B1 system plays a relatively minor role in human ste-roidogenesis. The regulation of cholesterol uptake, intracellulartransport, and utilization is coordinated by a family of basic he-lix-loop-helix transcription factors called the sterol regulatory ele-ment binding proteins (SREBPs). The cell biology of intracellularcholesterol trafficking is summarized in Fig. 1.
2.2. Lipases and the processing of cholesterol esters
After circulating LDL is internalized by receptor-mediated endo-cytosis, the resulting endocytic vesicles fuse with lysosomes,where the LDL proteins are degraded by proteolysis, liberatingthe cholesteryl esters, which are then hydrolyzed to ‘free’ choles-terol by lysosomal acid lipase (LAL). However, cholesterol is nevertruly free, as its solubility is only about 20 lmol per liter, so thatthe term ‘free cholesterol’ refers to cholesterol that is bound to pro-teins or membranes, but lacks a covalently linked group. Free cho-lesterol may be used by the cell or stored in lipid droplets followingre-esterification by acyl-coenzyme-A-cholesterol-acyl-transferase
(ACAT) also known as sterol-O-acetyltransferase (SOAT1). Simi-larly, HDL cholesteryl esters that enter the cell via SR-B1 are actedon by hormone-sensitive neutral lipase (HSL), following which thefree cholesterol may also be used or re-esterified for storage. ACTHand luteinizing hormone (LH) respectively increase intracellularlevels of cAMP in the adrenal and gonad, stimulating HSL andinhibiting ACAT, thus increasing the availability of free cholesterolfor steroid hormone synthesis. ACTH, LH and other factors that in-crease cAMP stimulate the activity of HMGCoA reductase and theuptake of LDL cholesterol. When intracellular cholesterol concen-trations are high, the genes for the LDL receptor, HMGCoA reduc-tase and LAL are repressed while ACAT is induced, therebydecreasing cholesterol uptake, synthesis and de-esterification.Conversely, when intracellular cholesterol concentrations arelow, this process is reversed.
Mutations in the LIPA gene encoding LAL cause Wolman disease,characterized by visceral accumulation of cholesteryl esters andtriglycerides, with secondary adrenal insufficiency; cholesterol es-ter storage disease is a milder, adult variant (Lohse et al., 1999). Af-fected infants quickly develop hepatosplenomegaly, malabsorptivemalnutrition and developmental delay; the diagnosis may be sug-gested by calcification that outlines the adrenal glands, and isestablished by finding deficient lysosomal acid lipase activity inleukocytes, fibroblasts or prenatal amniocytes. Bone marrow trans-plantation may ameliorate the disease, but the mechanism is un-clear. In contrast to LAL, no known human disease is associatedwith HSL deficiency.
2.3. Endosomal processing of cholesterol
The entry and exit of cholesterol from lipid droplets involvesthe NPC proteins, so named because their mutation causes Nie-mann Pick type C (NPC) disease, which is characterized by endo-somal accumulation of LDL-cholesterol and glycosphingolipids.Patients are normal in infancy but develop ataxia, dementia, loss
Fig. 1. Intracellular cholesterol trafficing. Human steroidogenic cells take up circulating low-density lipoproteins (LDLs) by receptor-mediated endocytosis, directing thecholesterol to endosomes; rodent cells utilize cholesterol from high-density lipoproteins (HDLs) via scavenger receptor B1 (SRB1). Cholesterol may also be synthesized fromacetate in the ER. Cholesteryl esters are cleaved by lysosomal acid lipase (LAL); free cholesterol is then bound by NPC1, transferred to NPC2, and exported. The MLN64/MENTHO system resides in the same endosomes as the NPC system, but its role in cholesterol trafficking remains uncertain. Cholesterol may be re-esterified by acyl-CoA:cholesterol transferase (ACAT) and stored in lipid droplets as cholesteryl esters. Free cholesterol may be produced by hormone-sensitive lipase (HSL). Cholesterol can reachthe outer mitochondrial membrane (OMM) by non-vesicular means by utilizing START-domain proteins or other cholesterol transport proteins. Movement of cholesterolfrom the OMM to the inner mitochondrial membrane (IMM) requires a multi-protein complex on the OMM. In the adrenals and gonads, the steroidogenic acute regulatoryprotein, StAR, is responsible for the rapid movement of cholesterol from the OMM to the IMM, where it can be converted to pregnenolone by P450scc. (!WL Miller).
W.L. Miller / Molecular and Cellular Endocrinology 379 (2013) 62–73 63

of speech and spasticity at 2–4 years, and usually die during theirsecond decade (Vanier and Millat, 2003). Cholesterol and other lip-ids accumulate in Purkinje cells and other neurons, and there is ro-bust glial infiltration. The diagnosis is typically made by findingcharacteristic foamy Niemann-Pick cells and ‘sea-blue’ histiocytesin the bone marrow. The NPC1 or NPC2 proteins participate inendosomal/lysosomal cholesterol transport. NPC1 is a 1278 AA gly-coprotein containing 13 transmembrane domains that span theendo-lysosomal membrane (Kwon et al., 2009), and NPC2 is a sol-uble 151 AA glycoprotein found in the lysosomal lumen (Xu et al.,2007). NPC2 binds cholesteryl esters with the cholesterol side-chain buried is in a hydrophobic pocket and the polar 3bOH groupexposed, allowing LAL to cleave cholesteryl esters while they arebound to NPC2. The free cholesterol is then transferred to the N-terminal domain of NPC1 in the lysosomal lumen, which bindscholesterol the 3bOH group buried in the protein and the sidechain partially exposed. Thus, the NPC2 and NPC1 proteins act to-gether to insert cholesterol into the lysosomal membrane with thehydrophobic side-chain going in first.
Two proteins named MLN64 (metastatic lymph node clone 64)and MENTHO (MLN64 N-terminal domain homologue) may alsoparticipate in endosomal cholesterol trafficking. MLN64 is a cho-lesterol-binding protein that co-localizes with NPC1 in late endo-somes (Zhang et al., 2002; Alpy and Tomasetto, 2006). The N-terminal ‘MENTAL’ domain (for MLN64 N-TerminAL) is structurallyrelated to the late-endosomal protein, MENTHO (Alpy et al., 2002),contains 4 transmembrane domains, and targets MLN64 to lateendosomal membranes. The C-terminal domain of MLN64 is calledthe START (StAR-related lipid transfer) domain because it is similarto the lipid-biding domain of the steroidogenic acute regulatoryprotein (StAR) (Alpy et al., 2001; Clark, 2012) (see Section 3). TheMENTAL domains of MENTHO and MLN64 can interact to formhomo- and heterodimers and to bind cholesterol, suggesting a rolein endosomal cholesterol transport. MLN64 lacking the MENTALdomain (N-234 MLN64) has 50–60% of StAR-like activity to stimu-late mitochondrial uptake of cholesterol (Bose et al., 2000). TheSTART domain of MLN64 may interact with cytoplasmic HSP60to stimulate steroidogenesis in placental mitochondria (Olvera-Sanchez et al., 2011). The function of MLN64 remains unclear:knockout of the START domain of MLN64 yielded viable, neurolog-ically intact, fertile mice with normal plasma and hepatic lipids(Kishida et al., 2004), and no human disorders of MLN64 or MEN-THO have been described. Accumulation of cholesterol in NPC1-deficient cells increased MLN64-mediated cholesterol transportto mitochondria and accumulation of cholesterol in the outermitochondiral membrane (OMM), suggesting that cholesteroltransport from endosomes to mitochondria may involve MLN64(Charman et al., 2010).
2.4. Non-vesicular intracytoplasmic cholesterol transport
Intracellular cholesterol transport may may be ‘vesicular’ (med-iated by membrane fusion) or ‘non-vesicular’ (bound to proteins).Because membranes participating in vesicular transport are fluid,the lipid compositions of the mitochondrial membranes may vary.Protein-protein interactions between lipid droplets, mitochondria,and other organelles may facilitate vesicular cholesterol transport.Both vesicular and non-vesicular cholesterol transport occur in ste-roidogenic cells, but non-vesicular transport involving high-affin-ity cholesterol-binding START-domain proteins appears to be theprincipal means of cholesterol transport from lipid droplets tomitochondria (Miller and Bose, 2011). START-domain proteinsare found in fungi, plants and animals; the mammalian START-do-main proteins are termed StarD1-15 (Clark, 2012). The START pro-teins most closely related to StAR (StarD4, D5 and D6), bindcholesterol and are induced by SREBP. StarD4, D5, and D6 lack N-
terminal signal sequences, suggesting they are cytosolic proteins.StarD1 (StAR), StarD3 (MLN64), StarD4 and StarD5 bind cholesterolwith high affinity and specificity, facilitate cholesterol transportthrough an aqueous environment, and appear to play importantroles in cellular cholesterol homeostasis (Rodriguez-Agudo et al.,2008). StAR and StarD6 stimulate the movement of cholesterolfrom the OMM to the inner mitochondrial membrane (IMM), butStarD4 and StarD5 do not (Bose et al., 2008a). StarD4 and/or StarD5may bring cholesterol to the OMM; however, StarD4 knockoutmice have no changes in steroidogenesis and minimal changes inweight and serum lipids, hence an essential function of StarD4 isnot established (Riegelhaupt et al., 2010). While all the mecha-nisms that move cholesterol to the mitochondria have not beendetermined, the current view is that the principal mechanism isby non-vesicular transport via StarD proteins, but that StAR itselfplays a minor role in this step. The OMM of adrenal mitochondriacontains abundant cholesterol, while the IMM contains little cho-lesterol. Whether or not all OMM cholesterol is potentially avail-able for steroidogenesis has been unclear. Early studies identifieda distinct pool of ‘‘steroidogenic’’ OMM cholesterol that was dis-tinct from the structural membrane cholesterol and could be mobi-lized by cAMP (Stevens et al., 1992). Movement of cholesterol fromthe OMM to the IMM is central to the initiation of steroidogenesis,because the cholesterol side-chain cleavage enzyme (P450scc) sys-tem is localized to the IMM. Whether or nor there are two kineti-cally distinct pools of cholesterol in the OMM, and how cholesterolis transferred to the IMM remain under investigation.
3. Entry of cholesterol into steroidogenic mitochondria: actionof the steroidogenic acute regulatory protein, StAR
3.1. Acute and chronic regulation of steroidogenesis
Unlike cells that produce polypeptide hormones, which storelarge amounts of mature hormone available for rapid release, cellsthat produce steroid homones store very little steroid, so that ste-roid secretion requires induction of steroid synthesis. There areseveral distinct mechanisms regulating steroidogenesis. In theadrenal, ACTH promotes steroidogenesis at three levels. First, overthe course of months ACTH promotes adrenal growth via fibroblastgrowth factor, epidermal growth factor, insulin-like growth factor2, and possibly other factors. Second, over the course of days,ACTH, acting via cAMP in the adrenal zona fasciculata and angio-tensin II acting via calcium/calmodulin in the zona reticularis pro-mote transcription of genes for steroidogenic enzymes, especiallythe gene encoding P450scc (CYP11A1) thus increasing the amountsof steroidogenic enzymes. Third, acting on a 15-60 min time scale,ACTH rapidly stimulates both the activation of pre-existing StARand the synthesis of new StAR. ACTH/cAMP stimulates phosphory-lation of StAR at Ser195 almost immediately, doubling its activity(Arakane et al., 1997), and induces StAR transcription within min-utes (Jo et al., 2005; Manna et al., 2009). StAR then interacts with acomplex macromolecular machine on the OMM to increase theflow of cholesterol from the OMM to the IMM where it becomesthe substrate for P450scc. The first two modes of steroid regulationcomprise the chronic steroidogenic response and the action of StARcomprises the acute steroidogenic response.
3.2. The steroidogenic acute regulatory protein, StAR
StAR was discovered in the search for the factor that triggers theacute steroidogenic response. Autoradiographic spots were notedon 2-dimentional gels that appeared within 30 min of stimulatingsteroidogenic tissues (Pon and Orme-Johnson, 1986; Pon et al.,1986; Epstein and Orme-Johnson, 1991; Stocco and Sodeman
64 W.L. Miller / Molecular and Cellular Endocrinology 379 (2013) 62–73

1991); the cDNA was then cloned (Clark et al., 1994; Sugawaraet al., 1995), and the factor was named the steroidogenic acute reg-ulatory protein, StAR (reviewed in Stocco and Clark, 1996). StAR isa 37-kDa protein with an N-terminal mitochondrial targeting se-quence that is cleaved off during mitochondrial import to yield30-kDa intramitochondrial StAR. Co-expression of StAR andP450scc in nonsteroidogenic cells rapidly increases conversion ofcholesterol to pregnenolone, suggesting that StAR triggers theacute steroidogenic response (Stocco and Clark, 1996). The indis-pensible role of StAR was demonstrated by finding that StAR muta-tions cause congenital lipoid adrenal hyperplasia, in which verylittle steroid is made (Lin et al., 1995; Bose et al., 1996). However,some steroidogenesis can take place in the absence of StAR. In vivo,the human placenta synthesizes steroids via mitochondrialP450scc but does not express StAR (Bose et al, 2000). In vitro, cellsexpressing the P450scc enzyme system but not StAR can convertcholesterol to pregnenolone (Harikrishna et al., 1993; Black et al.,1994) at !14% of the maximal StAR-induced rate (Lin et al.,1995; Bose et al., 1996). StAR-independent steroidogenesis mightoccur without a triggering protein, possibly using intracellularhydroxysterols that bypass StAR action; alternatively, another pro-tein, such as the 30 kDa proteolytic cleavage product of MLN64,may exert StAR-like activity to promote mitochondrial cholesterolimport, but the precise mechanism(s) are unclear.
3.3. StAR acts on the outer mitochondrial membrane
The presence of a typical mitochondrial ‘leader’ sequence ini-tially suggested that 37 kDa cytoplasmic StAR is a ‘precursor. andthat the 30 kDa intramitochondrial protein is the ‘mature form’,but these terms do not describe the biology of StAR (Miller, 2007).The crystallographic structure of the START domain of MLN64 (N-216 MLN64), which shares 37% amino acid sequence identity withStAR, suggested that 30-kDa StAR acts in the intramembranousspace (IMS) to shuttle cholesterol from the OMM to the IMM (Tsuj-ishita and Hurley, 2000). This structure shows a globular proteinwith an a/b helix-grip fold and an elongated hydrophobic pocketapproximately 26 Å deep and 10 Å across at its widest diameter.The structure of StAR was then modeled based on MLN64 (Mathieuet al., 2002; Yaworsky et al., 2005) and these models have been con-firmed by crystallography at 3.4 Å resolution (Thorsell et al., 2011).The sterol-binding pocket of StAR accommodates a single moleculeof cholesterol with its 3b-OH group coordinated by the two polarresidues. These structures and the structure of StarD4 (Romanowskiet al., 2002) are characterized by long N- and C-terminal a-helixes,two short a-helixes, and 9 antiparallel b sheets that form a helix-grip fold. However, deletion of StAR’s mitochondrial leader has noeffect on its activity (Arakane et al., 1996), and both the 37 kDaand 30 kDa forms of StAR are equally active in vivo and in vitro (Boseet al., 2002). When StAR was fused to the cytoplasmic C-terminus ofthe OMM protein Tom-20, thus immobilizing StAR an OMM, it wasconstituitively active, but when StAR was immobilized in the IMS oron the matrix side of the IMM, it was wholly inactive. Furthermore,manipulating the speed of StAR’s mitochondrial entry by manipu-lating the leader sequence showed that faster import decreasedactivity whereas slower import increased activity (Bose et al.,2002). Thus, StAR acts exclusively on the OMM and its activity isproportional to how long it remains on the OMM. Thus it is theOMM localization of StAR, and not its cleavage from the 37 kDa formto the 30 kDa form, that determines its activity.
3.4. StAR’s action requires conformational changes and serinephosphorylation
The mechanism by which StAR triggers cholesterol flux fromthe OMM to the IMM involves a multi-protein complex on the
OMM (see below) and requires pH-induced conformationalchanges in StAR that are needed for StAR to accept and dischargecholesterol (Bose et al., 1999; Baker et al., 2005). StAR can transfercholesterol between synthetic, protein-free membranes in vitro,but with non-physiologic stoichiometry (Tuckey et al., 2002), anda biologically inactive StAR mutant (R182L) can also transfer cho-lesterol to membranes in vitro (Baker et al., 2007). Thus choles-terol-binding is necessary but not sufficient for StAR activity.Proteolysis of StAR bound to synthetic membranes that modelOMM lipid composition showed that only the exterior surface ofthe C-terminal a-helix and small segments of the adjacent X-loopswere protected, suggesting that only these domains interact withthe OMM (Yaworsky et al., 2005). Molecular dynamics studiesshow that cholesterol is blocked from reaching the cholesterol-binding pocket of StAR by a set of hydrogen bonds that are dis-rupted when the surface residues of StAR are protonated (as hap-pens when StAR interacts with charged phospholipids on theOMM), thus eliciting a conformational change that permits choles-terol access (Bose et al., 1999; Baker et al., 2005). When the move-ment of the C-helix is prohibited by mutagenesis that createsdisulfide bonds, activity is lost, but reducing these bonds restoresactivity, showing that the immobilized C-helix, and not the muta-genesis, is responsible for the lost activity (Baker et al., 2005). Thusthe activity of StAR on the OMM requires an acid-induced disrup-tion of hydrogen bonds and a consequent conformational changein StAR to permit it to bind and release cholesterol.
The phosphorylation of StAR on Ser 195 approximately doublesStAR’s activity (Arakane et al., 1997). It appars that the protein ki-nase A (PKA) anchor protein AKAP121 recruits the type II PKA reg-ulatory subunit a (PKAR2A) to the OMM, which phosphorylatesStAR, whereas the type I kinase drives StAR transcription (Dysonet al., 2009). A physical interaction between the 37 kDa cytoplas-mic form of StAR and HSL has also been reported (Shen et al.,2003). StAR is recycled, with each molecule moving hundreds ofmolecules of cholesterol into the mitochondria before StAR is im-ported into the mitochondria and is inactivated (Artemenkoet al., 2001).
4. StAR interacts with an OMM protein complex
4.1. The peripheral benzodiazepine receptor or mitochondrialtransporter protein
StAR acts on the OMM via a complex that consists of severalproteins, most of which are now identified, even though it remainsunclear what role each plays in the mitochondrial importation ofcholesterol (Bose et al., 2008b; Rone et al., 2012; Papadopoulosand Miller, 2012). The first of these proteins to be identified isthe peripheral benzodiazepine receptor (PBR) (Lacapere andPapadopoulos, 2003), now also called the mitochondrial trans-porter protein (TSPO) (Papadopoulos et al., 2006). It was initiallyproposed that PBR/TSPO was the ‘acute trigger’ of steroidogenesis,but it is now clear that StAR plays that role, and that PBR/TSPO ispart of the molecular machine on the OMM through which StARacts (Papadopoulos and Miller, 2012). PBR/TSPO is a ubiquitouslyexpressed 18 kDa protein that comprises up to 2% of OMM protein.PBR/TSPO ligands can stimulate cholesterol movement from theOMM to the IMM and stimulate steroidogenesis (Lacapere andPapadopoulos, 2003). Knockdown of the gene encoding PBR/TSPOin Leydig cells disrupts cholesterol transport and steroidogenesis,and transfection of the PBR/TSPO-disrupted cells with the wild-type cDNA rescues steroidogenesis (Papadopoulos et al., 1997).However, knocking out the PBR/TSPO gene in mice caused earlyembryonic lethality, indicating its indispensible role during devel-opment (Lacapere and Papadopoulos, 2003).
W.L. Miller / Molecular and Cellular Endocrinology 379 (2013) 62–73 65

As is typical of proteins associated with the OMM, PBR/TSPOlacks a cannonical mitochondrial targeting sequence; instead, theC-terminal half targets PBR/TSPO to the OMM (Rone et al., 2009).PBR/TSPO appears to have five transmembrane a-helices spanningthe OMM (Joseph-Liauzun et al., 1998; Korkhov et al., 2010), sug-gesting that TSPO functions as a cholesterol channel, consistentwith data indicating that PBR/TSPO acts downstream from StAR(Hauet et al., 2005; Liu et al., 2006). PBR/TSPO and has a cytoplas-mic domain containing a ‘‘cholesterol recognition amino acid con-sensus’’ (CRAC) domain (Li et al., 2001). PBR/TSPO binds cholesterolat the CRAC domain, suggesting that this domain participates intransferring cholesterol from the OMM to the IMM (Jamin et al.,2005). Mutagenesis of the CRAC domain interferes with cholesterolbinding and transfer of cholesterol to the IMM, and blocking thebinding of cholesterol to the CRAC domain prevents steroidogene-sis (Midzak et al., 2011). Targeted deletion of the TSPO gene in animmortalized Leydig cell line blocked cholesterol transport into themitochondria and reduced steroid production; reintroduction ofTSPO into the deficient cell line restored steroidogenic capacity(Li et al., 2001).
4.2. Other components of the OMM protein complex
PBR/TSPO is a component of a 140–200 kDa multi-protein com-plex consisting of PBR/TSPO, the 34-kDa voltage-dependent anionchannel (VDAC1), the 30-kDa the adenine nucleotide transporter(ANT), the 10-kDa diazepam-binding inhibitor (acyl-CoA-bindingdomain 1, ACBD1), the TSPO-associated protein-1 (PRAX-1), andthe PKA regulatory subunit RIa-associated protein 7 (PAP7) (Roneet al., 2012). PAP7, also known as acyl-CoA binding domain-con-taining protein 3 (ACBD3), binds both TSPO and the regulatory sub-unit RIa of PKA (Fan et al., 2010). PBR/TSPO interacts with VDAC onthe OMM, helping to anchor the multi-protein complex to theOMM and assisting with the binding and import of StAR (Liuet al., 2006); VDAC1 also interacts with ANT on the IMM (McEneryet al., 1992). While a functional interaction between StAR and PBR/TSPO is clear (Hauet et al., 2005), a physical interaction has notbeen demonstrated; protein cross-linking experiments indicatethat StAR directly interacts with VDAC1 and with phosphate carrierprotein (PCP), but not with PBR/TSPO (Bose et al., 2008b). VDAC1also appears to interact with PBR/TSPO (Liu et al., 2006; Roneet al., 2009). It is not clear how VDAC-1 participates in cholesterolimport, as VDAC-1 has a ring-like structure with a hydrophilic inte-rior that is well-suited to anion transport, but is unlikely to form achannel for hydrophobic cholesterol (Bayrhuber et al., 2008; Hilleret al., 2008). VDAC is found at contact sites between the OMM andthe IMM (Mannella et al., 1992) where it may complex with hexo-kinase, ANT, creatine kinase and proteins of the Bcl-2 family(Brdiczka et al., 2006).
5. Mutations in StAR – congenital lipoid adrenal hyperplasia(Lipoid CAH)
Lipoid CAH is characterized by absent or very low serum con-centrations of all steroids, high basal ACTH and plasma renin activ-ity, and grossly enlarged adrenals filled with cholesterol andcholesteryl esters (Miller, 1997). Lipoid CAH was initially thoughtto be an enzymatic disorder and was mis-termed ‘20,22-desmolasedeficiency’, but the CYP11A1 gene for P450scc is not mutated inthese patients (Lin et al., 1991), and the placenta (a fetal tissue)continues to produce progesterone in lipoid CAH (Saenger et al.,1995), indicating a lesion upstream from P450scc, such as in a fac-tor involved in mitochondrial cholesterol transport (Lin et al.,1991). Mutations in the gene for PBR/TSPO were sought and ex-cluded (Lin et al., 1993), but mutations were found in StAR (Lin
et al., 1995; Bose et al., 1996), so that lipoid CAH represents theStAR knockout experiment of nature (Miller, 1997).
The pathophysiology of lipoid CAH is explained by the two-hitmodel (Bose et al., 1996). The first hit is lost StAR activity, causingdiminished steroidogenesis and a compensatory rise in ACTH andgonadotropins. These increased tropic hormones stimulate intra-cellular cAMP production, increasing LDL receptors, LDL choles-terol uptake, and de novo synthesis of cholesterol. Intracellularcholesterol then accumulates, causing the second hit: the loss ofremaining steroidogenic capacity due to mitochondrial damagefrom the accumulated cholesterol, cholesteryl esters, and theirauto-oxidation products (Bose et al., 1996) (Fig. 2). The absenceof StAR activity affects fetal testicular Leydig cells early in gesta-tion, preventing synthesis of the testosterone needed for the devel-opment of male external genitalia, hence affected 46,XY fetuses areborn with female external genitalia. However, the testicular Sertolicells function normally and produce anti-Müllerian hormone, sothe phenotypically female 46,XY fetus lacks female internal repro-ductive organs. The fetal adrenal typically produces very littlealdosterone, so that the zona glomerulosa is not tropicly stimu-lated and hence usually remains undamaged until after birth.Hence, newborns with lipoid CAH may not have a salt-wasting cri-sis until several months of life, when chronic stimulation thenleads to cellular damage.
The two-hit model has been confirmed in clinical studies,explaining why affected 46,XX patients feminize at the age of pub-erty (Bose et al., 1997; Fujieda et al., 1997), and also in knockoutmice (Hasegawa et al., 2000). The fetal ovary makes essentiallyno steroids and remains unstimulated and hence undamaged untiladolescence, when it is stimulated by pubertal gonadotropins,yielding small amounts of estrogen produced by StAR-independentsteroidogenesis. However, this low level of steroidogenesis is insuf-ficient to generate progesterone in response to the mid-cycle LHsurge; continued stimulation results in cholesterol accumulationand cellular damage, impairing the later biosynthesis of progester-one, resulting in anovulatory cycles. Gonadotropin stimulationdoes not promote global ovarian steroidogenesis, but only recruitsindividual follicles, hence most follicles remain undamaged andavailable for future cycles. A new follicle is recruited with each suc-cessive cycle, producing estradiol by StAR-independent steroido-genesis, resulting in breast development, so that the patientexperiences general feminization, monthly estrogen withdrawaland cyclic vaginal bleeding.
Lipoid CAH is relatively common in Japan and Korea, where thecarrier frequency is approximately one in 300, and most affectedindividuals carry the mutation Q258X (Bose et al., 1996; Nakaeet al., 1997; Kim et al., 2011). Mutations retaining about 10–25%of normal StAR activity, especially R188C, cause a milder diseasecalled ‘‘non-classic lipoid CAH’’, characterized by adrenal insuffi-ciency several years after infancy, nearly normal masculinizationof 46,XY individuals, and minimally affected mineralocorticoidsecretion (Baker et al., 2006).
6. The cholesterol side chain cleavage enzyme – the prototypicalmitochondrial P450
6.1. Cytochrome P450 enzymes
Once cholesterol reaches the IMM, it may be converted to preg-nenolone to initiate steroidogenesis. Most steroidogenic enzymesare cytochrome P450 enzymes, all of which have approximately500 residues, contain a single heme group and absorb light at450 nm when reduced with carbon monoxide. The human genomecontains 57 CYP genes encoding cytochrome P450 enzymes; thecorresponding proteins may be given the same name without the
66 W.L. Miller / Molecular and Cellular Endocrinology 379 (2013) 62–73

use of italics (thus CYP11A1 encodes the cholesterol side chaincleavage enzyme, P450scc; which may also be termed CYP11A1,without italics). Seven human cytochrome P450 enzymes are tar-geted to the mitochondria, the other 50 are targeted to the ER;the roles of the human P450 enzymes have been reviewed recently(Nebert et al., 2013). P450 enzymes activate molecular oxygen viatheir heme iron using electrons donated by nicotinamide adeninedinucleotide phosphate (NADPH). Mitochondrial (type 1) P450 en-zymes receive electrons from NADPH via an electron transfer chainconsisting of a flavoprotein termed ferredoxin reductase and asmall iron-sulfur protein termed ferredoxin (Miller, 2005)(Fig. 3). The type 2 P450 enzymes in the ER receive electrons viaa single 2-flavin protein termed P450 oxidoreductase (Miller,2005). All P450 enzymes can catalyze multiple chemical reactions,often with very different substrates.
6.2. Steps in steroidogenesis
Six P450 enzymes participate in steroidogenesis, and at leastthree more participate in the processing of vitamin D; five of theseare found in mitochondria. Steroidogenesis is initiated by mito-chondrial P450scc. P450scc cleaves the 20,22 bond of insolublecholesterol to produce soluble pregnenolone, and is the hormon-ally regulated, rate-limiting step in steroidogenesis. It is theexpression of the CYP11A1 gene that renders a cell ‘steroidogenic’.Pregnenolone may then be converted to progesterone by 3b-hydroxysteroid dehydrogenase (3bHSD), which may be found bothin the mitochondria and in the ER (see Section 9). Alternatively,
pregnenolone may exit the mitochondrion and become the sub-strate for P450c17 in the ER, which catalyzes both 17a-hydroxy-lase and 17,20 lyase activities. Pregnenolone appears to exit themitochondrion unaided; no transport protein has been found,and physiologic evidence does not suggest the presence of such atransporter. Following the activities of 3bHSD and P450c17,
Fig. 2. Two-hit model of lipoid CAH. (A) In normal adrenal cells, cholesterol is primarily derived from low-density lipoproteins, and the rate-limiting step in steroidogenesis ismovement of cholesterol from the OMM to the IMM. (B) Early in lipoid CAH, StAR-independent steroidogenesis moves small amounts of cholesterol into mitochondria,yielding sub-normal steroidogenesis; ACTH secretion increases, stimulating further accumulation of cholesteryl esters in lipid droplets. (C) As lipids accumulate, they damagethe cell through physical engorgement and by the action of cholesterol auto-oxidation products; steroidogenic capacity is destroyed, but tropic stimulation continues.Ovarian follicular cells remain unstimulated and undamaged until puberty, when small amounts of estradiol are produced, as in B, causing phenotypic feminization, withinfertility and hypergonadotropic hypogonadism. Modified from (Bose et al., 1996), with permission.
Fig. 3. Organization of mitochondrial P450 enzyme systems. NADPH first donateselectrons to the FAD moiety of ferredoxin reductase (FeRed); ferredoxin reductasethen interacts with ferredoxin (Fedx) by charge-charge attraction, permittingelectron transfer of the Fedx to the Fe2S2 center (ball and stick diagram). Ferredoxinthen dissociates from ferredoxin reductase and diffuses through the mitochrondrialmatrix. The same surface of ferredoxin that received the electrons from ferredoxinreductase then interacts with the redox-partner binding-site of a mitochondrialP450, such as P450scc, and the electrons then travel to the heme ring of the P450.The heme iron then mediates catalysis with substrate bound to the P450. !WLMiller.
W.L. Miller / Molecular and Cellular Endocrinology 379 (2013) 62–73 67

P450c21 catalyzes the 21-hydroxylation of both glucocorticoidsand mineralocorticoids. The final steps in the synthesis of both glu-cocorticoids and mineralocorticoids again takes place in the mito-chondria, where two proteins that share 93% sequence identity,11b-hydroxylase (P450c11b, CYP11B1), and aldosterone synthase(P450c11AS, CYP11B2) reside. P450c11b catalyzes the 11b-hydrox-ylation of 11-deoxycortisol to cortisol, and P450c11AS catalyzesthe 11b-hydroxylation, 18-hydroxylation, and 18-methyl oxidationto convert deoxycorticosterone to aldosterone. Histologic and elec-tron microscopic examination of steroidogenic cells suggests thatdomains of the ER containing the steroidogenic P450 enzymescome close to the OMM during hormonally-induced steroidogene-sis, forming a steroidogenic complex, so that the movement of ste-roidal intermediates from the mitochondrion to the ER involvesvery small distances.
6.3. Chemistry and transcription of P450scc
P450scc catalyzes three reactions: 22-hydroxylation of choles-terol, 20-hydroxylation of 22(R)-hydroxycholesterol, and oxidativescission of the C20-22 bond of 20(R),22(R)-dihydroxycholesterol,yielding pregnenolone and isocaproaldehyde. The binding of cho-lesterol and 22-hydroxylation are rate-limiting, as the efficiencies(kcat/Km) are much higher for the subsequent reactions, and thehigh KD of !3000 nM drives the dissociation of pregnenolone fromP450scc (Miller and Auchus, 2011). Alternatively, soluble hydrox-ysterols such as 22(R)-hydroxycholesterol can enter the mitochon-drion readily, without the action of StAR and its associatedmachinery. Catalysis by P450scc is slow, with a net turnover ofapproximately 6–20 molecules of cholesterol per molecule ofP450scc per second. The crystal structures of bovine (Mast et al.,2011) and human (Strushkevich et al., 2011) P450scc, the latterin complex with ferredoxin, show that the single active site ofP450scc is in contact with the IMM.
Transcription of the CYP11A1 gene determines cellular steroido-genic capacity. This transcription is regulated by hormonally-responsive factors that differ in different types of steroidogeniccells; both the PKA and PKC second messenger systems can induceCYP11A1 transcription via different promoter elements. Adrenaland gonadal transcription of P450scc and other steroidogenic en-zymes requires the action of steroidogenic factor 1 (SF1) (Schim-mer and White, 2010). By contrast, placental expression ofP450scc is constitutive, independent of SF1 and requires membersof the CP2 (graineyhead) family of transcription factors (also knownas LBP proteins) (Huang and Miller, 2000; Henderson et al., 2007)and TreP-132 (Gizard et al., 2002). Thus, long-term cellular stimu-lation over the course of days will increase the content of P450scc,and the level of basal steroid produced, as well as the capacity ofthe cell to mount a steroidogenic response.
7. Electron transfer to P450scc: ferredoxin reductase andferredoxin
7.1. Ferredoxin reductase
Catalysis by P450scc and other mitochondrial P450 enzymes re-quires two electron-transfer intermediates, ferredoxin reductaseand ferredoxin (Miller, 2005). Ferredoxin reductase receives elec-trons from NADPH then forms a 1:1 complex with ferredoxin,which then dissociates and forms an analogous 1:1 complex witha mitochondrial P450 such as P450scc, thus functioning as anindiscriminate, diffusible electron shuttle for all mitochondrialforms of P450 (Fig. 3). The relative abundances of ferredoxin reduc-tase and ferredoxin, as well as the inherent properties of the mito-chondrial P450, determine catalytic activity (Harikrishna et al.,
1993). Genetic disorders of human ferredoxin reductase and ferre-doxin have not been described, and mouse knockouts have notbeen reported. Mutation of the Drosophila ferredoxin reductasehomologue dare causes developmental arrest and degeneration ofthe adult nervous system secondary to disrupted ecdysone produc-tion (Freeman et al., 1999).
The human FDXR gene produces two alternatively spliced ferre-doxin reductase mRNAs differing by 18 bp (Solish et al., 1988), butonly the protein encoded by the more abundant, shorter mRNA isactive (Brandt and Vickery, 1992). Ferredoxin reductase mRNA iswidely expressed, but is far more abundant in steroidogenic tissues(Brentano et al, 1992). Ferredoxin reductase is a 54.5 kDa flavopro-tein affixed to the IMM that consists of two domains, each com-prising a b-sheet core surrounded by a-helices (Ziegler et al.,1999). The NADP(H)-binding domain is compact, whereas the do-main that binds flavin adenine dinucleotide (FAD) is more open;this domain binds the dinucleotide portion of FAD across a Ross-man fold with the redox-active flavin isoalloxazine ring abuttingthe NADP(H) domain. Electron transfer occurs in the cleft formedby these two domains. This cleft is characterized by basic residuesthat interact with acidic residues on ferredoxin.
7.2. Ferredoxin
The human FDX1 gene encodes ferredoxin (Fdx1), a 14 kDa, sol-uble, iron/sulfur (Fe2S2) protein that resides either free in the mito-chondrial matrix or is loosely bound to the inner mitochondrialmembrane (Miller, 2005). There are two human ferredoxins, Fdx1and Fdx2, but only Fdx1 supports steroidogenic mitochondrialP450 enzymes; Fdx2 participates in the synthesis of heme andFe/S cluster proteins (Sheftel et al., 2010). Ferredoxin has a core re-gion containing four cysteine residues that tether the Fe2S2 cluster,and an interaction domain containing a helix with several chargedresidues, producing a negatively charged surface above the Fe2S2
cluster that interacts with the mitochondrial P450 (Muller et al.,1998).
7.3. Mitochondrial P450 fusion proteins
The same surface of ferredoxin interacts with both ferredoxinreductase and the P450; nevertheless, creation of three-componentfusion proteins of the general scheme H2N-P450-FerredoxinReduc-tase-Ferredoxin-COOH (termed F2) increases Vmax. This designwas first tested with P450scc (Harikrishna et al., 1993) and hasbeen confirmed with P450c27 (Dilworth et al., 1996) andP450c11b (Cao et al., 2000). In such fusions, the ferredoxin moietyis at the C-terminus, tethered by a hydrophilic linker that permitsrotational freedom, so that the same surface of the ferredoxin canaccess both the P450 and the ferredoxin reductase. The require-ment for ferredoxin reductase and ferredoxin is not absolute, atleast in vitro. When P450scc is fused to an alternative electron do-nor, microsomal P450 oxidoreductase and targeted of to the mito-chondria, it remains active; by contrast when P450scc, its fusionprotein, or other P450scc constructs are targeted to the ER, theyare inactive even when supplied with the 22(R)-hydroxycholes-terol substrate that bypasses the StAR system (Black et al., 1994).Thus the mitochondrial localiztion is essential for the enzymaticactivity of P450scc.
8. P450scc deficiency syndromes
Three models of defective P450scc function, a spontaneouslyoccurring CYP11A1 deletion in the rabbit (Yang et al., 1993), knock-out of the gene in the mouse (Hu et al., 2002), and rare patientswith P450scc mutations confirm that P450scc is the only enzyme
68 W.L. Miller / Molecular and Cellular Endocrinology 379 (2013) 62–73

that converts cholesterol to pregnenolone. Because progesterone isneeded to suppress uterine contractility and thus prevent sponta-neous abortion, it would appear that P450scc mutations would beincompatible with term gestation; the mouse and rabbit modelsare explained by the persistence of the maternal corpus luteumin these species, providing an alternative source of progesterone.Nevertheless, beginning in 2001 (Tajima et al., 2001) 19 patientshave been described with mutations in CYP11A1 that affectP450scc activity (Tee et al., 2013). Most of these patients havemutations that ablate all P450scc activity; they probably reachedterm gestation because of the maternal corpus luteum remainedfunctional beyond the second trimester, when it normally invo-lutes. These patients may be clinically indistinguishable from thosewith lipoid CAH. The 46,XY genetic males fail to produce testoster-one during fetal life, and are born with female external genitalia,although their internal reproductive structures are male, as theirtestes produced anti-Müllerian hormone. Following birth, thesepatients require steroid hormone replacement therapy and mayhave long-term survival. As with non-classical lipoid CAH, a milder‘‘non-classical’’ form of P450scc deficiency has been describedcaused by missense mutations that retain 10–20% of normal activ-ity (Rubtsov et al., 2009; Sahakitrungruang et al., 2011). No hor-monal test distinguishes lipoid CAH from P450scc deficiency, butthe adrenals are typically grossly enlarged in lipoid CAH but nor-mal-sized in P450scc deficiency, sometimes permitting radiologicdistinction, but the only definitive test to distinguish these disor-ders is DNA sequencing (Gucev et al., 2013).
9. 3b-hydroxysteroid dehydrogenase
The 42 kDa 3b-hydroxysteroid dehydrogenase (3bHSD) is amember of the short-chain dehydrogenase/reductase (SDR) familyof enzymes, which are are b-a-b proteins having up to seven par-allel b-strands that fan across the center of the molecule, formingthe so-called ‘‘Rossman fold’’, which is characteristic of oxida-tion/reduction enzymes that use nicotinamide cofactors (Agarwaland Auchus, 2005; Penning, 1997). 3bHSD converts D5 steroids(pregnenolone, 17OH-pregneneolone, DHEA), having a doublebond in the B ring to D4 steroids, having a double bond in the Aring (Miller and Auchus, 2011). Members of this family of enzymeslack mitochondrial leader peptides and are generally found in thecytosol. However, 3bHSD was first isolated from mitochondria(Thomas et al., 1989). This unexpected cellular localization wasconfirmed by immunogold electron microscopy showing that3bHSD immunoreactivity is found in mitochondria and endoplas-mic reticulum as well as in the cytoplasm of bovine adrenal zonaglomerulosa cells (Cherradi et al., 1997; Pelletier et al., 2001). Itis not clear if this is also true for human 3bHSD, or if this subcellu-lar distribution differs in various types of steroidogenic cells, butthis property could be a novel mechanism for regulating the direc-tion of steroidogenesis. 3bHSD appears to be associated withP450scc on the IMM, and possibly at OMM-IMM contact sites(Cherradi et al., 1995). 3bHSD and 17a-hydroxylase (P450c17)compete for the pregnenolone produced by P450scc. The Michaelisconstant (Km) for P450c17 in the ER is about 0.8 lM (Auchus et al.,1998), whereas the Km of 3bHSD is about 5.2–5.5 lM (Lee et al.,1999), so that an intramitochondrial location of 3bHSD will facili-tate the formation of progesterone rather than 17OH-pregneno-lone. During its mitochondrial entry, 3bHSD associates withseveral mitochondrial translocase proteins to reach the IMM (Paw-lak et al., 2011) and undergoes a pH-dependent conformationalchange in the intramembranous space that facilitates its two enzy-matic activities (Prasad et al., 2012).
There are two 3bHSD genes and several pseudogenes in a genecluster on chromosome 1p13.1. The two encoded 3bHSD enzymes
are 93.5% identical with nearly indistinguishable enzymology, butwith distinct distributions of expression. The type 1 enzyme cata-lyzes 3bHSD activity in placenta, breast, liver, brain and some othertissues, whereas the type 2 enzyme is expressd in the adrenals andgonads. Deficiency of 3bHSD2 causes a rare form of congenitaladrenal hyperplasia (3bHSD deficiency); mutations have not beenfound in 3bHSD1, possibly reflecting the impact of such a mutationon plcental progesterone synthesis.
10. Other steroidogenic mitochondrial P450 enzymes
Adrenocortical mitochondria contain two additional P450 en-zymes: P450c11b (11b-hydroxylase) is found in zona fasciculatacells where it catalyzes the conversion of 11-deoxycortisol to cor-tisol; P450c11AS (aldosterone synthase) is found in zona glomerul-osa cells where it catalyzes the three distinct reactions needed toconvert deoxycorticosterone to aldosterone (White et al., 1994;Fardella and Miller, 1996; Miller and Auchus, 2011). These twoproteins share 93% amino acid sequence identity and are encodedby duplicated genes termed CYP11B1 (producing P450c11b) andCYP11B2 (producing P450c11AS). Like P450scc, both proteins havetypical mitochondrial targeting sequence and are associated withthe IMM. These enzymes must compete with P450scc for reducingequivalents provided via ferredoxin reductase and ferredoxin.Mutations in CYP11B1 cause 11b-hydroxylase deficiency, a rareform of virilizing congenital adrenal hyperplasia in which the over-production of deoxycorticosterone may lead to mineralocorticoidhypertension. Mutations in CYP11B2 cause aldosterone synthasedeficiency. An unusual recombination between the CYP11B1 andCYP11B2 genes can place the CYP11B1 promoter upstream fromthe CYP11B2 gene, thus producing aldosterone synthase in re-sponse to ACTH, causing glucocorticoid suppressiblehyperaldosteronism.
11. Mitochondrial P450 enzymes in vitamin D synthesis
Vitamin D and its metabolites are not steroids in the strictchemical sense, as the B ring of cholesterol is opened (Fig. 4). Nev-ertheless, these sterols are derived from cholesterol, assumeshapes that are very similar to steroids, and bind to a similar,zinc-finger receptor that regulates gene transcription (Feldmanet al., 2013). The final step in the biosynthesis of cholesterol is con-version of 7-dehydrocholesterol to cholesterol. In human skin,ultraviolet radiation at 270–290 nm directly cleaves the 9–10 car-bon–carbon bond of the cholesterol B ring, converting 7-dehydro-cholesterol to cholecalciferol (vitamin D3) (Norman, 1998). Plantsproduce ergocalciferol (vitamin D2), which has essentially the sameproperties as cholecalciferol. Both calciferols are biologically inac-tive pro-hormones that are then activated, and subsequently inac-tivated, by mitochondrial P450 enzymes.
The initial step in the activation of vitamin D is its hepatic 25-hydroxylation to 25(OH)D, which may be catalyzed by several en-zymes. The principal 25-hydroxylase is CYP2R1 (Cheng et al.,2003), and deficiency of this enzyme causes the very rare 25-hydroxylase deficiency syndrome (Cheng et al., 2004; Dong andMiller, 2004). A hepatic mitochondrial P450 (variously termedP450c25 and P450c27) encoded by the CYP27A1 gene also has vita-min D 25-hydroxylase activity, but its mutation causes cerebroten-dinous xanthomatosis without a disorder in calcium metabolism(Cali et al., 1991; Leitersdorf et al., 1993), hence this mitochondrialenzyme is of marginal importance to vitamin D metabolism.
The active, hormonal form of vitamin D, 1,25(OH)2D, is pro-duced by the 1a-hydroxylation of 25(OH)D by the mitochondrial1a-hydroxylase, P450c1a, encoded by the CYP27B1 gene (Fuet al., 1997a,b). 1,25(OH)2D in the circulation derives primarily
W.L. Miller / Molecular and Cellular Endocrinology 379 (2013) 62–73 69

from the kidney, but 1a-hydroxylase activity is also found in kerat-inocytes, macrophages, osteoblasts and placenta. 1a-hydroxylationis the rate-limiting step in the activation of vitamin D, and renalenzyme activity is tightly regulated by parathyroid hormone(PTH), calcium, phosphorus, and 1,25(OH)2D itself. The first humanclone was obtained from human keratinocytes, but multiple stud-ies, including finding mutations in a patient affected with renal 1a-hydroxylase deficiency, proved that the same gene was expressedin kidney (Fu et al., 1997a). Mutations in this gene cause the disor-der variously termed ‘vitamin D-dependent rickets, Type 1’, ‘pseu-do vitamin D-deficient rickets’ and ‘vitamin D 1a-hydroxylasedeficiency’ (Wang et al., 1998; Kim et al., 2007). The single CYP27B1gene for 1a-hydroxylase is only 5 kb long and has an intron/exonorganization that is very similar to that of other mitochondrialP450 enzymes, especially the mitochondrial cholesterol side-chaincleavage enzyme, P450scc (Fu et al., 1997b). Thus, even though themitochondrial P450 enzymes retain only 30–40% amino acid se-quence identity with each other, they all belong to a single evolu-tionary lineage. More than 100 patients with CYP27B1 mutationshave been described (Edouard et al 2011).
1,25(OH)2D may be inactivated by the principal hepatic drug-metabolizing enzyme, microsomal CYP3A4, or by its 24-hydroxyl-ation by vitamin D 24-hydroxylase (P450c24), encoded by theCYP24A1 gene (Feldman et al., 2013). This mitochondrial enzymecan catalyze the 24-hydroxylation of 25(OH)D to 24,25(OH)2Dand of 1,25(OH)2D to 1,24,25(OH)3D, primarily in the kidney andintestine, thus inactivating vitamin D (Ohyama et al., 1991; Chenet al., 1993). The expression of P450c24 is induced by1,25(OH)2D, providing a direct feedback mechanism to autoregu-late circulating levels of 1,25(OH)2D (Xie et al., 2002). The crystalstructure of rat P450c24 has been determined, showing a classiccytochrome P450 fold with an open conformation which wouldsuggest that this enzyme might bind multiple different substrates,nevertheless, like all other mitochondrial P450’s, P450c24 exhibitsa narrow substrate specificity (Annalora et al., 2010). Rare muta-tions in P450c24 result in elevated circulating concentrations of1,25(OH)2D, causing severe neonatal hypercalcemia (Schlingmannet al., 2011; Dauber et al., 2012).
References
Agarwal, A.K., Auchus, R.J., 2005. Cellular redox state regulates hydroxysteroiddehydrogenase activity and intracellular hormone potency. Endocrinology 146,2531–2538.
Alpy, F., Tomasetto, C., 2006. MLN64 and MENTHO, two mediators of endosomalcholesterol transport. Biochem. Soc. Trans. 34, 343–345.
Alpy, F., Stoeckel, M.E., Dierich, A., Escola, J.M., Wendling, C., Chenard, M.P., Vanier,M.T., Gruenberg, J., Tomasetto, C., Rio, M.C., 2001. The steroidogenic acuteregulatory protein homolog MLN64, a late endosomal cholesterol-bindingprotein. J. Biol. Chem. 276, 4261–4269.
Alpy, F., Wendling, C., Rio, M.C., Tomasetto, C., 2002. MENTHO, a MLN64 homologuedevoid of the START domain. J. Biol. Chem. 277, 50780–50787.
Annalora, A.J., Goodin, D.B., Hong, W.X., Zhang, Q., Johnson, E.F., Stout, C.D., 2010.Crystal structure of CYP24A1, a mitochondrial cytochrome P450 involved invitamin D metabolism. J. Mol. Biol. 396, 441–451.
Arakane, F., Sugawara, T., Nishino, H., Liu, Z., Holt, J.A., Pain, D., Stocco, D.M., Miller,W.L., Strauss 3rd., J.F., 1996. Steroidogenic acute regulatory protein (StAR)retains activity in the absence of its mitochondrial import sequence:
implications for the mechanism of StAR action. Proc. Natl. Acad. Sci. USA 93,13731–13736.
Arakane, F., King, S.R., Du, Y., Kallen, C.B., Walsh, L.P., Watari, H., Stocco, D.M.,Strauss 3rd, J.F., 1997. Phosphorylation of steroidogenic acute regulatoryprotein (StAR) modulates its steroidogenic activity. J. Biol. Chem. 272, 32656–32662.
Artemenko, I.P., Zhao, D., Hales, D.B., Hales, K.H., Jefcoate, C.R., 2001. Mitochondrialprocessing of newly synthesized steroidogenic acute regulatory protein(StAR), but not total StAR, mediates cholesterol transfer to cytochromeP450 side chain cleavage enzyme in adrenal cells. J. Biol. Chem. 276, 46583–46596.
Auchus, R.J., Lee, T.C., Miller, W.L., 1998. Cytochrome b5 augments the 17,20 lyaseactivity of human P450c17 without direct electron transfer. J. Biol. Chem. 273,3158–3165.
Baker, B.Y., Yaworsky, D.C., Miller, W.L., 2005. A pH-dependent molten globuletransition is required for activity of the steroidogenic acute regulatory protein,StAR. J. Biol. Chem. 280, 41753–41760.
Baker, B.Y., Lin, L., Kim, C.J., Raza, J., Smith, C.P., Miller, W.L., Achermann, J.C., 2006.Nonclassic congenital lipoid adrenal hyperplasia: a new disorder of thesteroidogenic acute regulatory protein with very late presentation andnormal male genitalia. J. Clin. Endocrinol. Metab. 91, 4781–4785.
Baker, B.Y., Epand, R.F., Epand, R.M., Miller, W.L., 2007. Cholesterol binding does notpredict activity of the steroidogenic acute regulatory protein, StAR. J. Biol.Chem. 282, 10223–10232.
Bayrhuber, M., Meins, T., Habeck, M., Becker, S., Giller, K., Villinger, S., Vonrhein, C.,Griesinger, C., Zweckstetter, M., Zeth, K., 2008. Structure of the human voltage-dependent anion channel. Proc. Natl. Acad. Sci. USA 105, 15370–15375.
Black, S.M., Harikrishna, J.A., Szklarz, G.D., Miller, W.L., 1994. The mitochondrialenvironment is required for activity of the cholesterol side-chain cleavageenzyme, cytochrome P450scc. Proc. Natl. Acad. Sci. USA 91, 7247–7251.
Bose, H.S., Sugawara, T., Strauss 3rd, J.F., Miller, W.L., 1996. The pathophysiologyand genetics of congenital lipoid adrenal hyperplasia. N. Engl. J. Med. 335,1870–1878.
Bose, H.S., Pescovitz, O.H., Miller, W.L., 1997. Spontaneous feminization in a 46XXfemale patient with congenital lipoid adrenal hyperplasia caused by ahomozygous frame-shift mutation in the steroidogenic acute regulatoryprotein. J. Clin. Endocrinol. Metab. 82, 1511–1515.
Bose, H.S., Whittal, R.M., Baldwin, M.A., Miller, W.L., 1999. The active form of thesteroidogenic acute regulatory protein, StAR, appears to be a molten globule.Proc. Natl. Acad. Sci. USA 96, 7250–7255.
Bose, H.S., Whittal, R.M., Huang, M.C., Baldwin, M.A., Miller, W.L., 2000. N-218MLN64, a protein with StAR-like steroidogenic activity, is folded and cleavedsimilarly to StAR. Biochemistry 39, 11722–11731.
Bose, H.S., Lingappa, V.R., Miller, W.L., 2002. Rapid regulation of steroidogenesis bymitochondrial protein import. Nature 417, 87–91.
Bose, H.S., Whittal, R.M., Ran, Y., Bose, M., Baker, B.Y., Miller, W.L., 2008a. StAR-likeactivity and molten globule behavior of StARD6, a male germ-line protein.Biochemistry 47, 2277–2288.
Bose, M., Whittal, R.M., Miller, W.L., Bose, H.S., 2008b. Steroidogenic activity of StARrequires contact with mitochondrial VDAC1 and phosphate carrier protein. J.Biol. Chem. 283, 8837–8845.
Brandt, M.E., Vickery, L.E., 1992. Expression and characterization of humanmitochondrial ferredoxin reductase in Escherichia coli. Arch. Biochem.Biophys. 294, 735–740.
Brdiczka, D.G., Zorov, D.B., Sheu, S.S., 2006. Mitochondrial contact sites: their role inenergy metabolism and apoptosis. Biochim. Biophys. Acta 1762, 148–163.
Brentano, S.T., Black, S.M., Lin, D., Miller, W.L., 1992. CAMP post-transcriptionallydiminishes the abundance of adrenodoxin reductase mRNA. Proc. Natl. Acad.Sci. USA 89, 4099–4103.
Cali, J.J., Hsieh, C.L., Francke, U., Russell, D.W., 1991. Mutations in the bile acidbiosynthetic enzyme sterol 27-hydroxylase underlie cerebrotendinousxanthomatosis. J. Biol. Chem. 266, 7779–7783.
Cao, P., Bulow, H., Dumas, B., Bernhardt, R., 2000. Construction and characterizationof a catalytic fusion protein system: P-45011-adrenodoxin reductase-adrenodoxin. Biochim. Biophys. Acta 1476, 253–264.
Charman, M., Kennedy, B.E., Osborne, N., Karten, B., 2010. MLN64 mediates egress ofcholesterol from endosomes to mitochondria in the absence of functionalNiemann-Pick Type C1 protein. J. Lipid Res. 51, 1023–1034.
Chen, K.S., Prahl, J.M., DeLuca, H.F., 1993. Isolation and expression of human 1,25-dihydroxyvitamin D3 24-hydroxylase cDNA. Proc. Natl. Acad. Sci. USA 90,4543–4547.
Fig. 4. Biosynthesis of vitamin D3. Ultraviolet light at 290–320 nm acts on the skin to cleave the B ring of 7-dehydrocholesterol to yield cholecalciferol (vitamin D3). VitaminD, is converted to 25OHD by several enzymes in the liver, principally CYP2R1. 25OHD is activated by 1a-hydroxylation in the kidney, yielding the active hormone 1,25(OH)2D,which acts by binding to the vitamin D receptor (VDR). Both 25OHD and 1,25(OH)2D may be inactivated by P450c24 to yield 24,25(OH)2D or 1,24,25(OH)3D, respectively.
70 W.L. Miller / Molecular and Cellular Endocrinology 379 (2013) 62–73

Cheng, J.B., Motola, D.L., Mangelsdorf, D.J., Russell, D.W., 2003. De-orphanization ofcytochrome P450 2R1: a microsomal vitamin D 25-hydroxilase. J. Biol. Chem.278, 38084–38093.
Cheng, J.B., Levine, M.A., Bell, N.H., Mangelsdorf, D.J., Russell, D.W., 2004. Geneticevidence that the human CYP2R1 enzyme is a key vitamin D 25-hydroxylase.Proc. Natl. Acad. Sci. USA 101, 7711–7715.
Cherradi, N., Chambaz, E.M., Defaye, G., 1995. Organization of 3b-hydroxysteroiddehydrogenase/isomerase and cytochrome P450scc into a catalytically activemolecular complex in bovine adrenocortical mitochondria. J. Steroid Biochem.Mol. Biol. 55, 507–514.
Cherradi, N., Rossier, M.F., Vallotton, M.B., Timberg, R., Friedberg, I., Orly, J., Wang,X.J., Stocco, D.M., Capponi, A.M., 1997. Submitochondrial distribution of threekey steroidogenic proteins (steroidogenic acute regulatory protein andcytochrome P450scc and 3-hydroxysteroid dehydrogenase isomeraseenzymes) upon stimulation by intracellular calcium in adrenal glomerulosacells. J. Biol. Chem. 272, 7899–7907.
Clark, B.J., 2012. The mammalian START domain protein family in lipid transport inhealth and disease. J. Endocrinol. 212, 257–275.
Clark, B.J., Wells, J., King, S.R., Stocco, D.M., 1994. The purification, cloning andexpression of a novel luteinizing hormone-induced mitochondrial protein inMA-10 cells mouse Leydig tumor cells. Characterization of the steroidogenicacute regulatory protein (StAR). J. Biol. Chem. 269, 28314–28322.
Dauber, A., Nguyen, T.T., Sochett, E., Cole, D.E., Horst, R., Abrams, S.A., Carpenter,T.O., Hirschhorn, J.N., 2012. Genetic defect in CYP24A1, the vitamin D 24-hydroxylase gene, in a patient with severe infantile hypercalcemia. J. Clin.Endocrinol. Metab. 97, E268–E274.
Dilworth, F.J., Black, S.M., Guo, Y.D., Miller, W.L., Jones, G., 1996. Construction of aP450c27 fusion enzyme – a useful tool for analysis of vitamin D3–25-hydroxylase activity. Biochem. J. 320, 267–271.
Dobs, A.S., Schrott, H., Davidson, M.H., Bays, H., Stein, E.A., Kush, D., Wu, M., Mitchel,Y., Illingworth, R.D., 2000. Effects of high-dose simvastatin on adrenal andgonadal steroidogenesis in men with hypercholesterolemia. Metabolism 49,1234–1238.
Dong, Q., Miller, W.L., 2004. Vitamin D 25-hydroxylase deficiency. Mol. Genet.Metab. 83, 197–198.
Dyson, M.T., Kowalewski, M.P., Manna, P.R., Stocco, D.M., 2009. The differentialregulation of steroidogenic acute regulatory protein-mediated steroidogenesisby type I and type II PKA in MA-10 cells. Mol. Cell. Endocrinol. 300, 94–103.
Edouard, T., Alos, N., Chabot, G., Roughley, P., Glorieux, F.H., Rauch, F., 2011. Short-and long-term outcome of patients with pseudo-vitamin D deficiency ricketstreated with calcitriol. J. Clin. Endocrinol. Metab. 96, 82–89.
Epstein, L.F., Orme-Johnson, N.R., 1991. Regulation of steroid hormone biosynthesis.Identification of precursors of a phosphoprotein targeted to the mitochondrionin stimulated rat adrenal cortex cells. J. Biol. Chem. 266, 19739–19745.
Fan, J., Liu, J., Culty, M., Papadopoulos, V., 2010. Acyl-coenzyme A binding domaincontaining 3 (ACBD3; PAP7; GCP60): an emerging signaling molecule. Prog.Lipid Res. 49, 218–234.
Fardella, C.E., Miller, W.L., 1996. Molecular biology of mineralocorticoidmetabolism. Annu. Rev. Nutr. 16, 443–470.
Feldman, D., Malloy, P.J., Miller, W.L., 2013. Genetic disorders of vitamin D synthesisand action. In: Thakker, R.V., Whyte, M.P., Eisman, J.A., Igarashi, T. (Eds.),Genetics of Bone Biology and Skeletal. Academic Press (Elsevier), London, UK,pp. 537–552.
Freeman, M.R., Dobritsa, A., Gaines, P., Segraves, W.A., Carlson, J.R., 1999. The daregene: steroid hormone production, olfactory behavior, and neural degenerationin Drosophila. Development 126, 4591–4602.
Fu, G.K., Lin, D., Zhang, M.Y.H., Bikle, D.D., Shackleton, C.H.L., Miller, W.L., Portale,A.A., 1997a. Cloning of human 25-hydroxyvitamin D 1-hydroxylase andmutations causing vitamin D-dependent rickets type I. Mol. Endocrinol. 11,1961–1970.
Fu, G.K., Portale, A.A., Miller, W.L., 1997b. Complete structure of the human gene forthe vitamin D 1hydroxylase, P450clDNA. Cell Biol. 16, 1499–1507.
Fujieda, K., Tajima, T., Nakae, J., Sageshima, S., Tachibana, K., Suwa, S., Sugawara, T.,Strauss, J.F.I.I.I., 1997. Spontaneous puberty in 46, XX subjects with congenitallipoid adrenal hyperplasia. Ovarian steroidogenesis is spared to some extentdespite inactivating mutations in the steroidogenic acute regulatory protein(StAR) gene. J. Clin. Invest. 99, 1265–1271.
Gizard, F., Lavallee, B., DeWitte, F., Teissier, E., Staels, B., Hum, D.W., 2002. Thetranscriptional regulating protein of 132 kDa (TReP-132) enhances P450sccgene transcription through interaction with steroidogenic factor-1 in humanadrenal cells. J. Biol. Chem. 277, 39144–39155.
Gucev, Z., Tee, M.K., Chitayat, D., Wherrett, D., Miller, W.L., 2013. Distinguishingdeficiencies of StAR and P450scc causing neonatal adrenal failure. J. Pediatr.162, 819–822.
Harikrishna, J.A., Black, S.M., Szklarz, G.D., Miller, W.L., 1993. Construction andfunction of fusion enzymes of the human cytochrome P450scc system. DNA CellBiol. 12, 371–379.
Hasegawa, T., Zhao, L.P., Caron, K.M., Majdic, G., Suzuki, T., Shizawa, S., Sasano, H.,Parker, K.L., 2000. Developmental roles of the steroidogenic acute regulatoryprotein (StAR) as revealed by StAR knockout mice. Mol. Endocrinol. 14, 1462–1471.
Hauet, T., Yao, Z.X., Bose, H.S., Wall, C.T., Han, Z., Li, W., Hales, D.B., Miller, W.L.,Culty, M., Papadopoulos, V., 2005. Peripheral-type benzodiazepine receptor-mediated action of steroidogenic acute regulatory protein on cholesterol entryinto Leydig cell mitochondria. Mol. Endocrinol. 19, 540–554.
Henderson, Y.C., Frederick, M.J., Jayakumar, A., Choi, Y., Wang, M.T., Kang, Y., Evans,R., Spring, P.M., Uesugi, M., Clayman, G.L., 2007. Human LBP-32/MGR is arepressor of the P450scc in human choriocarcinoma cell line JEG-3. Placenta 28,152–160.
Hiller, S., Garces, R.G., Malia, T.J., Orekhov, V.Y., Colombini, M., Wagner, G., 2008.Solution structure of the integral human membrane protein VDAC-1 indetergent micelles. Science 321, 1206–1210.
Hu, M.C., Hsu, N.C., El Hadj, N.B., Pai, C.I., Chu, H.P., Wang, C.K.L., Chung, B.C., 2002.Steroid deficiency syndromes in mice with targeted disruption of Cyp11a1. Mol.Endocrinol. 16, 1943–1950.
Huang, N., Miller, W.L., 2000. Cloning of factors related to HIV-inducible LBPproteins that regulate steroidogenic factor-1-independent human placentaltranscription of the cholesterol side-chain cleavage enzyme, P450scc. J. Biol.Chem. 275, 2852–2858.
Illingworth, D., Kenney, T.A., Orwoll, E.S., 1982. Adrenal function in heterozygousand homozygous hypobetalipoproteinemia. J. Clin. Endocrinol. Metab. 54, 27–33.
Jamin, N., Neumann, J.M., Ostuni, M.A., Vu, T.K., Yao, Z.X., Murail, S., Robert, J.C.,Giatzakis, C., Papadopoulos, V., Lacapere, J.J., 2005. Characterization of thecholesterol recognition amino acid consensus sequence of the peripheral-typebenzodiazepine receptor. Mol. Endocrinol. 19, 588–594.
Jo, Y., King, S.R., Khan, S.A., Stocco, D.M., 2005. Involvement of protein kinase C andcyclic adenosine 30 ,50-monophosphate-dependent kinase in steroidogenic acuteregulatory protein expression and steroid biosynthesis in Leydig cells. Biol.Reprod. 73, 244–255.
Joseph-Liauzun, E., Delmas, P., Shire, D., Ferrara, P., 1998. Topological analysis of theperipheral benzodiazepine receptor in yeast mitochondrial membranessupports a five-transmembrane structure. J. Biol. Chem. 273, 2146–2152.
Kim, C.J., Kaplan, L.E., Perwad, F., Huang, N., Sharma, A., Choi, Y., Miller, W.L., Portale,A.A., 2007. Mutations in the gene for 1-hydroxylase, CYP27B1, in patients withvitamin D 1-hydroxylase deficiency. J. Clin. Endocrinol. Metab. 92, 3177–3182.
Kim, J.M., Choi, J.H., Lee, J.H., Kim, G.H., Lee, B.H., Kim, H.S., Shin, J.H., Shin, C.H., Kim,C.J., Yu, J., Lee, D.Y., Cho, W.K., Suh, B.K., Lee, J.E., Chung, H.R., Yoo, H.W., 2011.High allele frequency of the p.Q258X mutation and identification of a novelmis-splicing mutation in the STAR gene in Korean patients with congenitallipoid adrenal hyperplasia. Eur. J. Endocrinol. 165, 771–778.
Kishida, T., Kostetskii, I., Zhang, Z., Martinez, F., Liu, P., Walkley, S.U., Dwyer, N.K.,Blanchette-Mackie, E.J., Radice, G.L., Strauss 3rd., J.F., 2004. Targeted mutationof the MLN64 START domain causes only modest alterations in cellular sterolmetabolism. J. Biol. Chem. 279, 19276–19285.
Korkhov, V.M., Sachse, C., Short, J.M., Tate, C.G., 2010. Three-dimensional structureof TspO by electron cryomicroscopy of helical crystals. Structure 18, 677–687.
Kwon, H.J., Abi-Mosleh, L., Wang, M.L., Deisenhofer, J., Goldstein, J.L., Brown, M.S.,Infante, R.E., 2009. Structure of N-terminal domain of NPC1 reveals distinctsubdomains for binding and transfer of cholesterol. Cell 137, 1213–1224.
Lacapere, J.J., Papadopoulos, V., 2003. Peripheral-type benzodiazepine receptor:structure and function of a cholesterol-binding protein in steroid and bile acidbiosynthesis. Steroids 68, 569–585.
Lee, T.C., Miller, W.L., Auchus, R.J., 1999. Medroxyprogesterone acetate anddexamethasone are competitive inhibitors of different human steroidogenicenzymes. J. Clin. Endocrinol. Metab. 84, 2104–2110.
Leitersdorf, E., Reshef, A., Meiner, V., Levitzki, R., Schwartz, S.P., Dann, E.J., Berkman,N., Cali, J.J., Klapholz, L., Berginer, V.M., 1993. Frameshift and splice-junctionmutations in the sterol 27-hydroxylase gene cause cerebrotendinousxanthomatosis in Jews or Moroccan origin. J. Clin. Invest. 91, 2488–2496.
Li, H., Yao, Z., Degenhardt, B., Teper, G., Papadopoulos, V., 2001. Cholesterol bindingat the cholesterol recognition/interaction amino acid consensus (CRAC) of theperipheral-type benzodiazepine receptor and inhibition of steroidogenesis byan HIV TAT-CRAC peptide. Proc. Natl. Acad. Sci. USA 98, 1267–1272.
Lin, D., Gitelman, S.E., Saenger, P., Miller, W.L., 1991. Normal genes for thecholesterol side chain cleavage enzyme, P450scc, in congenital lipoid adrenalhyperplasia. J. Clin. Invest. 88, 1955–1962.
Lin, D., Chang, Y.J., Strauss III, J.F., Miller, W.L., 1993. The human peripheralbenzodiazepine receptor gene: cloning and characterization of alternativesplicing in normal tissues and in a patient with congenital lipoid adrenalhyperplasia. Genomics 18, 643–650.
Lin, D., Sugawara, T., Strauss 3rd, J.F., Clark, B.J., Stocco, D.M., Saenger, P., Rogol, A.,Miller, W.L., 1995. Role of steroidogenic acute regulatory protein in adrenal andgonadal steroidogenesis. Science 267, 1828–1831.
Liu, J., Rone, M.B., Papadopoulos, V., 2006. Protein-protein interactions mediatemitochondrial cholesterol transport and steroid biosynthesis. J. Biol. Chem. 281,38879–38893.
Lohse, P., Maas, S., Sewell, A.C., van Diggelen, O.P., Seidel, D., 1999. Molecular defectsunderlying Wolman disease appear to be more heterogeneous than thoseresulting in cholesteryl ester storage disease. J. Lipid Res. 40, 221–228.
Manna, P.R., Dyson, M.T., Stocco, D.M., 2009. Regulation of the steroidogenic acuteregulatory protein gene expression: present and future perspectives. Mol. Hum.Reprod. 15, 321–333.
Mannella, C.A., Forte, M., Colombini, M., 1992. Toward the molecular structure ofthe mitochondrial channel, VDAC. J. Bioenergy Biomembr. 24, 7–19.
Mast, N., Annalora, A.J., Lodowski, D.T., Palczewski, K., Stout, C.D., Pikuleva, I.A.,2011. Structural basis for three-step sequential catalysis by the cholesterol sidechain cleavage enzyme CYP11A1. J. Biol. Chem. 286, 5607–5613.
Mathieu, A.P., Fleury, A., Ducharme, L., Lavigne, P., LeHoux, J.G., 2002. Insights intosteroidogenic acute regulatory protein (StAR)-dependent cholesterol transfer in
W.L. Miller / Molecular and Cellular Endocrinology 379 (2013) 62–73 71

mitochondria: evidence from molecular modeling and structure-basedthermodynamics supporting the existence of partially unfolded states of StAR.J. Mol. Endocrinol. 29, 327–345.
McEnery, M.W., Snowman, A.M., Trifiletti, R.R., Snyder, S.H., 1992. Isolation of themitochondrial benzodiazepine receptor: association with the voltagedependentanion channel and the adenine nucleotide carrier. Proc. Natl. Acad. Sci. USA 89,3170–3174.
Midzak, A., Akula, N., Lecanu, L., Papadopoulos, V., 2011. Novel androstenetriolinteracts with the mitochondrial translocator protein and controlssteroidogenesis. J. Biol. Chem. 286, 9875–9887.
Miller, W.L., 1997. Congenital lipoid adrenal hyperplasia: the human gene knockoutof the steroidogenic acute regulatory protein. J. Mol. Endocrinol. 19, 227–240.
Miller, W.L., 2005. Minireview: regulation of steroidogenesis by electron transfer.Endocrinology 146, 2544–2550.
Miller, W.L., 2007. StAR search–what we know about how the steroidogenic acuteregulatory protein mediates mitochondrial cholesterol import. Mol. Endocrinol.21, 589–601.
Miller, W.L., Auchus, R.J., 2011. The molecular biology, biochemistry, and physiologyof human steroidogenesis and its disorders. Endocr. Rev. 32, 81–151.
Miller, W.L., Bose, H.S., 2011. Early steps in steroidogenesis: intracellular cholesteroltrafficking. J. Lipid Res. 52, 2111–2135.
Muller, A., Muller, J.J., Muller, Y.A., Uhlmann, H., Bernhardt, R., Heinemann, U., 1998.New aspects of electron transfer revealed by the crystal structure of a truncatedbovine adrenodoxin, Adx(4-108). Structure 6, 269–280.
Nakae, J., Tajima, T., Sugawara, T., Arakane, F., Hanaki, K., Hotsubo, T., Igarashi, N.,Igarashi, Y., Ishii, T., Koda, N., Kondo, T., Kohno, H., Nakagawa, Y., Tachibana, K.,Takeshima, Y., Tsubouchi, K., Strauss III, J.F., Fujieda, K., 1997. Analysis of thesteroidogenic acute regulatory protein (StAR) gene in Japanese patients withcongential lipoid adrenal hyperplasia. Hum. Mol. Genet. 6, 571–576.
Nebert, D.W., Wikvall, K., Miller, W.L., 2013. Human cytochromes P450 in healthand disease. Phil. Trans. R. Soc. B 368, 20120431, <http://dx.doi.org/10.1098/rstb.2012.0431>.
Norman, A.W., 1998. Sunlight, season, skin pigmentation, vitamin D, and 25-hydroxyvitamin D: integral components of the vitamin D endocrine system.Am. J. Clin. Nutr. 67, 1108–1110.
Ohyama, Y., Noshiro, M., Okuda, K., 1991. Cloning and expression of cDNA encoding25-hydroxyvitamin D3 24-hydroxylase. FEBS Lett. 278, 195–198.
Olvera-Sanchez, S., Espinosa-Garcia, M.T., Monreal, J., Flores-Herrera, O., Martinez,F., 2011. Mitochondrial heat shock protein participates in placentalsteroidogenesis. Placenta 32, 222–229.
Papadopoulos, V., Miller, W.L., 2012. Role of mitochondria in steroidogenesis. Bestpractice & research. Clin. Endocrinol. Metab. 26, 771–790.
Papadopoulos, V., Amri, H., Li, H., Boujrad, N., Vidic, B., Garnier, M., 1997. Targeteddisruption of the peripheral-type benzodiazepine receptor gene inhibitssteroidogenesis in the R2C Leydig tumor cell line. J. Biol. Chem. 272, 32129–32135.
Papadopoulos, V., Baraldi, M., Guilarte, T.R., Knudsen, T.B., Lacapere, J.J., Lindemann,P., Norenberg, M.D., Nutt, D., Weizman, A., Zhang, M.R., Gavish, M., 2006.Receptor based on its structure and molecular function. Trends Pharmacol. Sci.27, 402–409.
Pawlak, K.J., Prasad, M., Thomas, J.L., Whittal, R.M., Bose, H.S., 2011. Innermitochondrial translocase Tim50 interacts with 3b-hydroxysteroiddehydrogenase type 2 to regulate adrenal and gonadal steroidogenesis. J. Biol.Chem. 286, 39130–39140.
Pelletier, G., Li, S., Luu-The, V., Tremblay, Y., Belanger, A., Labrie, F., 2001.Immunoelectron microscopic localization of three key steroidogenic enzymes(cytochrome P450(scc), 3b-hydroxysteroid dehydrogenase and cytochromeP450(c17)) in rat adrenal cortex and gonads. J. Endocrinol. 171, 373–383.
Penning, T.M., 1997. Molecular endocrinology of hydroxysteroid dehydrogenases.Endocr. Rev. 18, 281–305.
Pon, L.A., Orme-Johnson, N.R., 1986. Acute stimulation of steroidogenesis incorpus luteum and adrenal cortex by peptide hormones. J. Biol. Chem. 261,6594–6599.
Pon, L.A., Hartigan, J.A., Orme-Johnson, N.R., 1986. Acute ACTH regulation of adrenalcorticosteroid biosynthesis: rapid accumulation of a phosphoprotein. J. Biol.Chem. 261, 13309–13316.
Porter, F.D., Herman, G.E., 2011. Malformation syndromes caused by disorders ofcholesterol synthesis. J. Lipid Res. 52, 6–34.
Prasad, M., Thomas, J.L., Whittal, R.M., Bose, H.S., 2012. Mitochondrial 3-hydroxysteroid dehydrogenase enzyme activity requires reversible pH-dependent conformational changes at the intermembrane space. J. Biol. Chem.287, 9534–9546.
Riegelhaupt, J.J., Waase, M.P., Garbarino, J., Cruz, D.E., Breslow, J.L., 2010. Targeteddisruption of steroidogenic acute regulatory protein D4 leads to modest weightreduction and minor alterations in lipid metabolism. J. Lipid Res. 51, 1134–1143.
Rodriguez-Agudo, D., Ren, S., Wong, E., Marques, D., Redford, K., Gil, G., Hylemon,P.B., Pandak, W.M., 2008. Intracellular cholesterol transporter StarD4 binds freecholesterol and increases cholesteryl ester formation. J. Lipid Res. 49, 1409–1419.
Romanowski, M.J., Soccio, R.E., Breslow, J.L., Burley, S.K., 2002. Crystal structure ofthe Mus musculus cholesterol-regulated START protein 4 (StarD4) containing aStAR-related lipid transfer domain. Proc. Natl. Acad. Sci. USA 99, 6949–6954.
Rone, M.B., Liu, J., Blonder, J., Ye, X., Veenstra, T.D., Young, J.C., Papadopoulos, V.,2009. Targeting and insertion of the cholesterol-binding translocator proteininto the outer mitochondrial membrane. Biochemistry 48, 6909–6920.
Rone, M.B., Midzak, A.S., Issop, L., Rammouz, G., Jagannathan, S., Fan, J., Ye, X.,Blonder, J., Veenstra, T., Papadopoulos, V., 2012. Identification of a dynamicmitochondrial protein complex driving cholesterol import, trafficking, andmetabolism to steroid hormones. Mol. Endocrinol. 26, 1868–1882.
Rubtsov, P., Karmanov, M., Sverdlova, P., Spirin, P., Tiulpakov, A., 2009. A novelhomozygous mutation in CYP11A1 gene is associated with late onset adrenalinsufficiency and hypospadias in a 46 XY patient. J. Clin. Endocrinol. Metab. 94,936–939.
Saenger, P., Klonari, Z., Black, S.M., Compagnone, N., Mellon, S.H., Fleischer, A.,Abrams, C.A.L., Shackleton, C.H.L., Miller, W.L., 1995. Prenatal diagnosis ofcongenital lipoid adrenal hyperplasia. J. Clin. Endocrinol. Metab. 80, 200–205.
Sahakitrungruang, T., Tee, M.K., Blackett, P.R., Miller, W.L., 2011. Partial defect in thecholesterol side-chain cleavage enzyme P450scc (CYP11A1) resemblingnonclassic congenital lipoid adrenal hyperplasia. J. Clin. Endocrinol. Metab.96, 792–798.
Schimmer, B.P., White, P.C., 2010. Steroidogenic factor 1: its roles in differentiation,development and disease. Mol. Endocrinol. 24, 1322–1337.
Schlingmann, K.P., Kaufmann, M., Weber, S., Irwin, A., Goos, C., John, U., Misselwitz,J., Klaus, G., Kuwertz-Broking, E., Fehrenbach, H., Wingen, A.M., Guran, T.,Hoenderop, J.G., Bindels, R.J., Prosser, D.E., Jones, G., Konrad, M., 2011. Mutationsin CYP24A1 and idiopathic infantile hypercalcemia. N. Engl. J. Med. 365, 410–421.
Sheftel, A.D., Stehling, O., Pierik, A.J., Elsasser, H.P., Muhlenhoff, U., Webert, H.,Hobler, A., Hannemann, F., Bernhardt, R., Lill, R., 2010. Humans possess twomitochondrial ferredoxins, Fdx1 and Fdx2, with distinct roles insteroidogenesis, heme, and Fe/S cluster biosynthesis. Proc. Natl. Acad. Sci.USA 107, 11775–11780.
Shen, W.J., Patel, S., Natu, V., Hong, R., Wang, J., Azhar, S., Kraemer, F.B., 2003.Interaction of hormone-sensitive lipase with steroidogenic acute regulatoryprotein. J. Biol. Chem. 278, 43870–43876.
Solish, S.B., Picado-Leonard, J., Morel, Y., Kuhn, R.W., Mohandas, T.K., Hanukoglu, I.,Miller, W.L., 1988. Human adrenodoxin reductase: two mRNAs encoded by asingle gene of chromosome 17cen?25 are expressed in steroidogenic tissues.Proc. Natl. Acad. Sci. USA 85, 7104–7108.
Stevens, V.L., Xu, T., Lambeth, J.D., 1992. Cholesterol pools in rat adrenalmitochondria: use of cholesterol oxidase to infer a complex pool structure.Endocrinology 130, 1557–1563.
Stocco, D.M., Clark, B.J., 1996. Regulation of the acute production of steroids insteroidogenic cells. Endocr. Rev. 17, 221–244.
Stocco, D.M., Sodeman, T.C., 1991. The 30 kDa mitochondrial proteins induced byhormone stimulation in MA-10 mouse Leydig tumor cells are processed fromlarger precursors. J. Biol. Chem. 266, 19731–19738.
Strushkevich, N., MacKenzie, F., Cherkesova, T., Grabovec, I., Usanov, S., Park, H.W.,2011. Structural basis for pregnenolone biosynthesis by the mitochondrialmonooxygenase system. Proc. Natl. Acad. Sci. USA 108, 10139–10143.
Sugawara, T., Holt, J.A., Driscoll, D., Strauss III, J.F., Lin, D., Miller, W.L., Patterson, D.,Clancy, K.P., Hart, I.M., Clark, B.J., Stocco, D.M., 1995. Human steroidogenic acuteregulatory protein (StAR): functional activity in COS-1 cells, tissue-specificexpression, and mapping of the structural gene to 8p11.2 and an expressedpseudogene to chromosome 13. Proc. Natl. Acad. Sci. USA 92, 4778–4782.
Tajima, T., Fujieda, K., Kouda, N., Nakae, J., Miller, W.L., 2001. Heterozygousmutation in the cholesterol side chain cleavage enzyme (P450scc) gene in apatient with 46, XY sex reversal and adrenal insufficiency. J. Clin. Endocrinol.Metab. 86, 3820–3825.
Tee, M.K., Abramsohn, M., Loewenthal, N., Harris, M., Siwach, S., Kaplinsky, A.,Markus, B., Birk, O., Sheffield, V.C., Pavari, R., Hershkovitz, E., Miller, W.L., 2013.Varied clinical presentations with mutations in CYP11A1 encoding thecholesterol side chain cleavage enzyme, P450scc. J. Clin. Endocrinol. Metab.98, 713–720.
Thomas, J.L., Myers, R.P., Strickler, R.C., 1989. Human placental 3-hydroxy-5-ene-steroid dehydrogenase and steroid 5 D 4-ene-isomerase: purification frommitochondria and kinetic profiles, biophysical characterization of the purifiedmitochondrial and microsomal enzymes. J. Steroid Biochem. 33, 209–217.
Thorsell, A.G., Lee, W.H., Persson, C., Siponen, M.I., Nilsson, M., Busam, R.D.,Kotenyova, T., Schuler, H., Lethio, L., 2011. Comparative structural analysis oflipid binding START domains. PLoS ONE 6, e19521–e19532.
Tsujishita, Y., Hurley, J.H., 2000. Structure and lipid transport mechanism of a StAR-related domain. Nat. Struct. Biol. 7, 408–414.
Tuckey, R.C., Headlam, M.J., Bose, H.S., Miller, W.L., 2002. Transfer of cholesterolbetween phospholipid vesicles mediated by the steroidogenic acute regulatoryprotein (StAR). J. Biol. Chem. 277, 47123–47128.
Vanier, M.T., Millat, G., 2003. Niemann-Pick disease type C. Clin. Genet. 64, 269–281.
Wang, J.T., Lin, C.J., Burridge, S.M., Fu, G.K., Labuda, M., Portale, A.A., Miller, W.L.,1998. Genetics of vitamin D 1a-hydroxylase deficiency in 17 families. Am. J.Hum. Genet. 63, 1694–1702.
White, P.C., Curnow, K.M., Pascoe, L., 1994. Disorders of steroid 11-hydroxylaseisozymes. Endocr. Rev. 15, 421–438.
Xie, Z.J., Munson, S.J., Huang, N., Portale, A.A., Miller, W.L., Bikle, D.D., 2002. Themechanism of 1,25-dihydroxyvitamin D3 auto-regulation in keratinocytes. J.Biol. Chem. 277, 36987–36990.
Xu, S., Benoff, B., Liou, H.L., Lobel, P., Stock, A.M., 2007. Structural basis of sterolbinding by NPC2, a lysosomal protein deficient in Niemann-Pick type C2disease. J. Biol. Chem. 282, 23525–23531.
Yang, X., Iwamoto, K., Wang, M., Artwohl, J., Mason, J.I., Pang, S., 1993. Inheritedcongenital adrenal hyperplasia in the rabbit is caused by a deletion in the gene
72 W.L. Miller / Molecular and Cellular Endocrinology 379 (2013) 62–73

encoding cytochrome P450 cholesterol side-chain cleavage enzyme.Endocrinology 132, 1977–1982.
Yaworsky, D.C., Baker, B.Y., Bose, H.S., Best, K.B., Jensen, L.B., Bell, J.D., Baldwin, M.A.,Miller, W.L., 2005. PH-dependent interactions of the carboxyl-terminal helix ofsteroidogenic acute regulatory protein with synthetic membranes. J. Biol. Chem.280, 2045–2054.
Zhang, M., Liu, P., Dwyer, N.K., Christenson, L.K., Fujimoto, T., Martinez, F., Comly,M., Hanover, J.A., Blanchette-Mackie, E.J., Strauss 3rd, J.F., 2002. MLN64
mediates mobilization of lysosomal cholesterol to steroidogenicmitochondria. J. Biol. Chem. 277, 33300–33310.
Ziegler, G.A., Vonrhein, C., Hanukoglu, I., Schulz, G.E., 1999. The structure ofadrenodoxin reductase of mitochondrial P450 systems: electron transfer forsteroid biosynthesis. J. Mol. Biol. 289, 981–990.
W.L. Miller / Molecular and Cellular Endocrinology 379 (2013) 62–73 73

Review
Mitochondria and mammalian reproduction
João Ramalho-Santos a,b,⇑, Sandra Amaral a
a CNC – Center for Neuroscience and Cell Biology, University of Coimbra, Portugalb Department of Life Sciences, University of Coimbra, Portugal
a r t i c l e i n f o
Article history:Available online 13 June 2013
Keywords:ReproductionMitochondriaGametogenesisFertilizationSteroidogenesis
a b s t r a c t
Mitochondria are cellular organelles with crucial roles in ATP synthesis, metabolic integration, reactiveoxygen species (ROS) synthesis and management, the regulation of apoptosis (namely via the intrinsicpathway), among many others. Additionally, mitochondria in different organs or cell types may have dis-tinct properties that can decisively influence functional analysis. In terms of the importance of mitochon-dria in mammalian reproduction, and although there are species-specific differences, these aspectsinvolve both energetic considerations for gametogenesis and fertilization, control of apoptosis to ensurethe proper production of viable gametes, and ROS signaling, as well as other emerging aspects. Crucially,mitochondria are the starting point for steroid hormone biosynthesis, given that the conversion ofcholesterol to pregnenolone (a common precursor for all steroid hormones) takes place via the activityof the cytochrome P450 side-chain cleavage enzyme (P450scc) on the inner mitochondrial membrane.Furthermore, mitochondrial activity in reproduction has to be considered in accordance with the verydistinct strategies for gamete production in the male and female. These include distinct gonadmorpho-physiologies, different types of steroids that are more prevalent (testosterone, estrogens,progesterone), and, importantly, the very particular timings of gametogenesis. While spermatogenesisis complete and continuous since puberty, producing a seemingly inexhaustible pool of gametes in a fixedenvironment; oogenesis involves the episodic production of very few gametes in an environment thatchanges cyclically. These aspects have always to be taken into account when considering the roles ofany common element in mammalian reproduction.
! 2013 Elsevier Ireland Ltd. All rights reserved.
Contents
1. Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 752. Mitochondria in gametogenesis and early embryo development . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 76
2.1. Primordial germ cells and gonad specification . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 762.2. Mitochondria in spermatogenesis . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 762.3. Mitochondria in sperm . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 792.4. Mitochondria in oogenesis . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 792.5. Mitochondria in early embryo development . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 79
3. The endocrine role of mitochondria in reproduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 803.1. The mitochondrial step in steroid biosynthesis. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 803.2. Sex-specific steroidogenesis . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 80
4. Conclusions and future perspectives. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 80Acknowledgements . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 81References . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 81
0303-7207/$ - see front matter ! 2013 Elsevier Ireland Ltd. All rights reserved.http://dx.doi.org/10.1016/j.mce.2013.06.005
⇑ Corresponding author. Address: Department of Life Sciences, University of Coimbra, PO Box 3046, 3001-401 Coimbra, Portugal. Tel.: +351 (239) 855 760; fax: +351 (239)855 789.
E-mail address: [email protected] (J. Ramalho-Santos).
Molecular and Cellular Endocrinology 379 (2013) 74–84
Contents lists available at SciVerse ScienceDirect
Molecular and Cellular Endocrinology
journal homepage: www.elsevier .com/locate /mce

1. Introduction
Mitochondria are usually mentioned primarily in terms of cellu-lar ATP production by oxidative phosphorylation (OXPHOS) via theelectron transport chain (ETC) located in the inner mitochondrialmembrane. ETC activity generates a transmembrane proton gradi-ent (Fig. 1), of which the mitochondrial membrane potential(MMP) is the main component, driving the ATP synthase (Kakkarand Singh, 2007; Newmeyer and Ferguson-Miller, 2003; Scheffler,2001). A few components of this machinery are encoded by residentmitochondrial DNA (mtDNA) a prokaryotic-like genome that isinherited maternally (Jansen and de Boer, 1998; St John et al., 2010).
However, recent mitochondrial research focuses on other top-ics, such as the production of reactive oxygen species (ROS) bythe ETC and their role(s) in both physiological cell signaling andpathological processes (related to oxidative stress); the regulationof the intrinsic apoptosis pathway and intracellular calcium levels;the production of steroid hormones; quality control of cellularmitochondria via autophagy/mitophagy pathways, or the centralposition of mitochondria in integrating several metabolic and sig-naling pathways, epigenetics and the cell cycle (Folmes et al.,2012; Kakkar and Singh, 2007; Nichols and Ferguson, 2002; Nun-nari and Suomalainen, 2012).
Moreover, although previously mitochondria were thought tohave a fixed and individual morphology, it is now known thatchanges in shape (both in terms of cristae structure and matrixtexture), size (regulated by the fission/fusion machinery) andrelationships with other cellular features (the cytoskeleton,the endoplasmic reticulum) can have important functionalconsequences (Bereiter-Hahn and Voth, 1994; Collins et al., 2002;
Rowland and Voeltz, 2012). Indeed, studies of mitochondrial(dys)function related to aging, degenerative and metabolic disor-ders or cancer encompass several of these aspects, from abnormalOXPHOS activity and ROS production, to defective apoptosis andmitophagy/autophagy, to changes in mtDNA and mitochondrialstructure (Amaral et al., 2008b; Amaral and Ramalho-Santos,2009; Cereghetti and Scorrano, 2011; Correia et al., 2012; Dornand Scorrano, 2010; Martinou and Youle, 2011; Nunnari andSuomalainen, 2012; Oettinghaus et al., 2012; Palmeira and Rama-lho-Santos, 2011; Ramalho-Santos and Rodrigues, 2013; Ramalho-Santos et al., 2009; St John et al., 2010). In short, mitochondria areinvolved in many other duties while (also) making ATP.
In this review we will focus specifically on the role of mitochon-dria in gametogenesis, fertilization and early embryo development.It should noted that mitochondrial function is most often studiedin terms of dysfunction induced by pathological conditions or toxicsubstances (pharmacological agents, environmental contaminants,distinct pathologies, etc.), and how these dysfunctions may ulti-mately affect the reproductive system (Aly and Khafagy, 2011;Amaral et al., 2008a, 2009; Banu et al., 2011; Miyamoto et al.,2010; Mota et al., 2011; Svechnikov et al., 2009; Wang et al.,2009, 2010). Using different aspects of mitochondrial function asdamage indicators in several disease models and, conversely, asdiagnostic tools in Assisted Reproductive Technologies (ART), hasincreased in recent years, in terms of functional sperm analysis(Aitken et al., 2012; Dorn and Scorrano, 2010; Gallon et al., 2006;Marchetti et al., 2002; Marchetti et al., 2012; Nakada et al., 2006;Ruiz-Pesini et al., 1998; Sanchez-Partida et al., 2008; Sousa et al.,2011), and oocyte quality assessment (Van Blerkom, 2011; Wangand Sun, 2007).
Fig. 1. Possible roles of mitochondria in reproduction. Mitochondria are double membrane organelles with their own genome (mtDNA). Mitochondrial substrates derivedfrom glycolysis, beta-oxidation of fatty acids and the Krebs cycle (Tricarboxylic acid cycle- TCA) provide energy for ATP production through oxidative phosphorylation(OXPHOS) by the activity of the electron transfer chain (ETC) on the inner mitochondrial membrane, composed of four inner membrane (IMM)-associated enzyme complexes(I–IV), plus cytochrome c (Cytc) and the mobile electron carrier ubiquinone (Q). This electron transfer generates a proton gradient across the inner membrane that drives ATPsynthase (often known as complex V). However, at several sites of the electron transport chain (mainly complexes I and III) electrons can react with oxygen forming ROS. Theenergy dissipation mechanism promoted by UCPs (uncoupling proteins) can reduce ROS formation. Both beta-oxidation of fatty acids and amino acid catabolism provide TCAintermediates. The initial step of steroidogenesis also takes place in mitochondria. The first step involves cholesterol (Chol) transport into the mitochondria facilitated by StARprotein via its interaction with Translocator protein (TSPO) and voltage dependent anion channel (VDAC) that constitute the transduceosome, located on the outermitochondrial membrane (OMM). Once in the mitochondria, cholesterol will be converted to pregnenolone through the action of side chain cleavage cytochrome P450(P450scc) that depends on the Adrenoxin reductase (AdxRed)–adrenoxin (Adx) system to receive electrons from NADPH. Pregnenolone then diffuses to the smoothendoplasmatic reticulum (SER) where it is further metabolized. See text for discussion.
J. Ramalho-Santos, S. Amaral / Molecular and Cellular Endocrinology 379 (2013) 74–84 75

2. Mitochondria in gametogenesis and early embryodevelopment
2.1. Primordial germ cells and gonad specification
Mammalian gametogenesis is commonly defined by importantsex-specific differences, although the starting point is identical.Gonadal tissue derives from the mesoderm, into which primordialgerm cells (PGCs) migrate from outside the developing embryo andare subjected to distinct sex determination signals. PGCs divideseveral times, and establish functional relationships with somaticcells that will have supportive, protective, nutritional, and endocr-inal roles in gamete formation. In the testis these include Sertoliand Leydig cells, while their homologous equivalents in the ovaryare granulosa and theca cells, respectively (Gilbert, 2010; Soder,2007).
While PGCs that colonize the fetal testes ultimately differenti-ate into spermatogonial stem cells, which remain mostly quies-cent, retinoic acid exposure causes ovarian oogonia to commit tomeiosis in utero. Therefore, at puberty the testis still contains stemcells which can both self-renew and enter meiosis to form sperm,allowing for the continuous production of a large number of malegametes. On the other hand, the ovary contains only a finiteamount of committed primary oocytes, which will mature cycli-cally until the gamete pool is exhausted, ultimately resulting inmenopause (Gassei and Schlatt, 2007; Pereda et al., 2006; Soder,2007). This is one of the main reasons why more information isavailable on male gametogenesis. Anatomical differences are alsoevident between gonads: the testis is comprised of an extensiveduct system formed by seminiferous tubules onto which millionsof small mature sperm are constantly released (ultimately matur-ing in the epidydimis); while the ovary consists of a series of follic-ular structures embedded in the ovarian stroma, each containingone large female gamete which will be released upon ovulation,with the oocyte and follicle developing in unison (Gilbert, 2010;Holstein et al., 2003; McLaughlin and McIver, 2009). In terms ofmitochondrial characteristics and metabolic activity there are alsoseveral sex- and stage-specific differences (Table 1).
2.2. Mitochondria in spermatogenesis
Besides providing support and assisting in sperm formation andtransport Sertoli cells form the blood-testis barrier, creating a sep-arate and immuneprivileged site (Meinhardt and Hedger, 2011;Smith and Braun, 2012). Testosterone-secreting Leydig cells arefound in the intertubular tissue surrounding the capillaries andhave a prominent role in spermatogenesis maintenance, the differ-entiation of male sexual organs and secondary sex characteristics(Ge et al., 2008). Testis-specific morphogenetic events in early go-nad differentiation suggest that male gonads have a higher energyrequirement than ovaries, and that these distinct metabolic fea-tures, focused on mitochondrial activity, might even have a rolein sex determination itself (Matoba et al., 2008; Mittwoch, 2004).
Spermatogenesis takes place in the seminiferous tubules and isa highly dynamic and metabolically active biological process dur-ing which haploid spermatozoa are produced through a gradualtransformation of an interdependent population of germ cells.These cells sequentially migrate from the basal compartment to-wards the luminal regions of the tubules, passing the blood-testisbarrier (Holstein et al., 2003). The existence of numerous mito-chondria in male germ cells (Meinhardt et al., 1999), as well asthe presence of several testis-specific mitochondrial protein iso-forms (Hess et al., 1993; Huttemann et al., 2003) highlights theirimportance in testicular metabolism. As a whole testis mitochon-dria have been shown to possess specific bioenergetical and
controlled proton leak characteristics that distinguish them frommitochondria from other organs, consuming less oxygen in orderto generate approximately the same maximum electric potential(Amaral et al., 2008a, 2009; Mota et al., 2009; Rodrigues et al.,2010). This suggests that, unlike what is usually the case, testicularmitochondria should be considered as the primary mitochondrialmodels to test the effect of distinct substances on male gametogen-esis, and not be substituted by other in vitro models, such as com-monly used liver mitochondria (Mota et al., 2011; Tavares et al.,2009).
Although descriptive studies, or those that consider cells out-side of their biological context (isolated from tissue architecture,grown in nutrient-rich media, under normoxia), must be inter-preted with caution, it is well known that different testicular cellshave morphologically different mitochondria. These differencesmay be due to the mitochondrial fusion/fission machinery (Aiharaet al., 2009), and could have functional consequences, as is the casein other systems (Bereiter-Hahn and Voth, 1994; Campello andScorrano, 2010; Collins et al., 2002; De Martino et al., 1979; Homand Sheu, 2009; Mannella, 2006, 2008). In fact both somatic(Sertoli, Leydig) and germline (spermatogonia, spermatocytes,spermatids, sperm) cells have distinct metabolic preferences andactivities, which are translated into distinct mitochondrial contri-butions (Bajpai et al., 1998; De Martino et al., 1979; Grootegoedet al., 1984; Meinhardt et al., 1999; Nakamura et al., 1984;Robinson and Fritz, 1981) (Table 1). Interestingly, putativesubstrate availability does not fully explain the differences encoun-tered in the testis, as spermatogonia on the basal membraneremain mostly glycolytic although they are closer to blood vessels(and therefore oxygen sources), while spermatocytes in the semi-niferous tubules seem to rely more on OXPHOS, despite being far-ther away from the oxygen supply. This seems to be a peculiarityspermatogonia share with other stem cells (Ramalho-Santos andRodrigues, 2013; Ramalho-Santos et al., 2009).
The importance of ATP formed via OXPHOS for spermatogenesisis exemplified by the meiotic arrest found in mice that do not ex-press a testis-specific adenine nucleotide translocase (ANT4),essential for the translocation of ADP and ATP across the innermitochondrial membrane (Brower et al., 2009). The regulation ofapoptosis is also another aspect of mitochondrial function in thetestis, both to ensure a manageable number of germ cells thatcan be supported by existing Sertoli cells (Ramalho-Santos et al.,2009), or as result of different environmental stimuli (Jia et al.,2010; Reyes et al., 2012; Shaha et al., 2010). The former aspect ishighlighted by several experiments involving genetically modifiedmice that lack different components of the intrinsic apoptosispathway. For example, the deletion of pro-apoptotic BCL-2 familyproteins BAX, BAK, as well as the simultaneous deletion of BIMand BIK (possibly due to redundant functions), results in an excessof germ cells, increased mutagenesis and testicular tumorigenesis(Coultas et al., 2005; Katz et al., 2012; Knudson et al., 1995; Russellet al., 2002; Xu et al., 2010), a process somewhat mirrored follow-ing overexpression of the pro-survival BCL-W in the testis (Yanet al., 2003). On the other hand deletion of this protein also resultsin male infertility (Ross et al., 2001; Russell et al., 2001), and thesame is true for BCL-2 (Yamamoto et al., 2001), although in the for-mer this seems due to BAX-induced death of Sertoli cells, while inthe latter germ cells were more affected. Mice devoid of apoptoticprotease-activating factor-1 (Apaf-1), which is usually activated bycytochrome c, are also infertile, in this case due to degeneratedspermatogonia leading to an almost absence of viable sperm inthe seminiferous tubules (Honarpour et al., 2000). Additionally,mice lacking the testis-specific form of cytochrome c have im-paired sperm function (Narisawa et al., 2002).
Pathophysiological processes such as mitochondrial ROSproduction may also have an (usually detrimental) effect on
76 J. Ramalho-Santos, S. Amaral / Molecular and Cellular Endocrinology 379 (2013) 74–84

Table 1Mitochondrial characteristics and energy metabolism throughout mammalian gametogenesis and early embryo development.
Cell type Mitochondria Mitochondria Energy source Metabolic particularitiesMorphology Cellular localization
MaleSpermatogonia Ovoid shaped, lamellar cristae,
electron translucent matrix –Orthodox
Scattered through thecytoplasm
Glycolysis – Existence of the blood-testis barrier and Oxygen gradient in the seminiferoustubules
Primary spermatocyte Orthodox (Leptotene) ? Condensed(Pachytene, Diplotene) (roundshaped, dense matrix, expansion ofthe intracristal spaces)
Around the nucleus(Zygotene, early Pachytene).Small cytoplasmic clusterswith the nuage(intermitochondrialcement; late Pachytene)
Glycolysis – Associations between germ cell mitochondrial morphology and metabolicstatus have been suggested in which condensed mitochondria are more efficient
OXPHOS – Germ cells have some pentose phosphate pathway activity, mainlyspermatocytes
Secondary spermatocyte Condensed No cluster arrangement OXPHOS – There are several testis-specific mitochondrial protein isoforms
Spermatid Condensed (earlySpermatid) ? intermediate (lateSpermatid) (elongated, crescentshaped cristae, matrix lesscondensed)
No cluster arrangement.Start to localize close toplasma membrane
OXPHOS
In late spermatids localizeclose to the flagellum.
Sperm Intermediate Arranged in the midpiece GlycolysisOXPHOSb-oxidation
Female/embryoOogonia Spherical-ovoid shape. Tubulo-
vesicular cristae ? lamellar cristaeTypically clustered in closeassociation with the nuage(intermitochondrialcement)
Glycolysis – Mitochondrial number increases throughout oocyte maturation
Pale matrix – Despite their primitive state, mitochondria are active in OXPHOS and are theprimary source of ATP in the human oocyte and early embryo– The oocyte contains two populations of mitochondria; the more abundantmitochondria have low MMP and the smaller population is highly polarized.Mitochondrial MMP increases as the oocyte progress through meioticmaturation– Changes in mitochondrial distribution during oocyte growth may be aresponse to different energy demands.– Mammalian oocytes have limited ability in using glucose and therefore rely oncumulus cells. These cells convert glucose into readily utilizable substrates thatenter the oocyte and are further metabolized via TCA followed by OXPHOS. Theorigin of these substrates may also be external (i.e. female reproductive tract)– While growing oocytes preferentially metabolize pyruvate over glucose, thesomatic compartment of ovarian follicles is more gycolitic– The pentose phosphate pathway is important for oocyte development.-Triglycerides provide an additional rich energy supply for oocyte maturationthrough beta-oxidation– Mammalian oocytes may also utilize amino acids mainly via cumulus cells.Aminoacids serve as substrates for the synthesis of proteins, nucleotides, GSH,signaling molecules and provide substrates for the TCA cycle– Bioenergetic deficiencies have been associated with failure of oocytematuration and fertilization and embryo demise during pre-implantation stages
(continued on next page)
J.Ramalho-Santos,S.Am
aral/Molecular
andCellular
Endocrinology379
(2013)74–84
77

Table 1 (continued)
Cell type Mitochondria Mitochondria Energy source Metabolic particularitiesMorphology Cellular localization
1ry Oocyte Spherical. Cristae with lamellarpattern (L,Z,P) ? arch like pattern ordisposed parallel to the outermembrane (D)
Random cytoplasmic (L) OXPHOS
Z,P-high dense matrix perinuclear(Z)D-lighter matrix form a crescent shape mass
near nucleus (D), inassociation with otherorganelles(balbiani’svitelline body)
Growing Oocyte Spherical, cristae pattern change andincreasingly dense matrix
Dispersed in cytoplasm OXPHOS
Beta-oxidation
Preovulatory Oocyte(mature)
Round with arched cristae, densematrix
In the ooplasm. Formvoluminous aggregates withsmooth endoplasmicreticulum tubules andvesicles.
OXPHOS
Zygote Round or oval with few cristaeparallel to the outer mitochondrialmembrane. Some dumb-bell shaped.Electrodense matrix.
Concentrated aroundpronuclei
OXPHOS Although early embryos have poorly differentiated mitochondria, they are activeand the main source of ATP. A more complex form is gradually achieved,matching increasing development energetic requirements.
– A subset of high-polarized mitochondria is observed in zygotes and earlyembryos, and this population increases with cleavage state.– A transient increase in the ratio of high to low MMP was observed in 2-cellstage mouse embryos, synchronized with embryonic genome activation(maternal-embryonic transition)
2 cell Round shape with few smallperipheral cristae. Dense matrix
Uniformly dispersed in theblastomeres with atendency towardsperinuclear arrangement
OXPHOS – In human 8-cell embryos an increased ratio of mitochondria with high- to low-MMP correlates with embryo fragmentation
– It has been hypothesized that up regulation of beta-oxidation might result inincreased availability of carbohydrates such as glucose for use in otherpathways. This situation may also aid metabolic regulation and rapid cellproliferation via the Warburg effect
4 cell More elongated with numeroustransverse cristae. Lighter matrix
Dispersed in blastomeres OXPHOS
6-8 cell Most with elongated shape Associated with nuage(intermitochondrialcement)
Glycolysis
Blastocyst – Mitochondria in the trophoblast are more numerous and hyperpolarized.
Trophoblast Orthodox-like OXPHOSMitochondrial cristae transverselyoriented.
Glycolysis
ICM QuiescentMatrix less dense
Information collected from the following sources: Amaral et al. (2013), Amaral et al. (2009), Bajpai et al. (1998), Bentov et al. (2011), Boussouar and Benahmed (2004), Collado-Fernandez et al. (2012), De Martino et al. (1979),Dumollard et al. (2009), Dunning et al. (2010), Hess et al. (1993), Meinhardt et al. (1999), Mota et al. (2009), Motta et al. (2000), Ramalho-Santos et al. (2009), Songsasen et al. (2012), Van Blerkom (2008), Van Blerkom (2009), VanBlerkom (2011), Wilding et al. (2001).
78J.Ram
alho-Santos,S.Amaral/M
olecularand
CellularEndocrinology
379(2013)
74–84

spermatogenesis and sperm quality (Agarwal et al., 2003; Tremel-len, 2008). For example, mice with a mutation in the inner mito-chondrial membrane peptidase 2-like (Immp2l) gene showimpairment in processing of signal peptide sequences from mito-chondrial cytochrome c and glycerol phosphate dehydrogenase 2,and this causes testicular damage and subfertility, possibly dueto excessive ROS production (George et al., 2012).
2.3. Mitochondria in sperm
In the final step of sperm differentiation (spermiogenesis) mostof the cytoplasm (including most mitochondria) is lost in the so-called residual bodies. The remaining 22–75 mitochondria rear-range end to end in the midpiece (Ho and Wey, 2007; Olson andWinfrey, 1990; Otani et al., 1988). The fact that some mitochondriaare evolutionarily retained in a very specialized sperm region sug-gests that these organelles have a role in sperm function. Indeedthe tight arrangement of mitochondria around the sperm midpieceoften is used to exemplify a strategy to concentrate ATP productionfor a specific function, in this case sperm movement. In fact, mito-chondrial parameters (MMP, ETC complex activity) correlate posi-tively with sperm function (Gallon et al., 2006; Marchetti et al.,2002, 2012; Nakada et al., 2006; Ruiz-Pesini et al., 1998; Sousaet al., 2011), mitochondrial inhibition impairs sperm activity(Ruiz-Pesini et al., 2000; St John et al., 2005), and the introductionof a mutant mtDNA with a pathogenic 4696-bp deletion in mice re-sulted in male infertility (Nakada et al., 2006), with comparabledata being reported in human patients (St John et al., 2005). How-ever, this is probably not due to ATP production specifically direc-ted to fuel movement, as other pathways (such as glycolysis) seemmore prevalent in mammalian sperm for this specific purpose(Amaral et al., 2011; Nascimento et al., 2008). The available evi-dence seems to demonstrate that in the few days it can spend inthe female reproductive tract mammalian sperm might be ableto utilize both glycolysis and OXPHOS to produce ATP for differentpurposes. The balance between these (and other) metabolic path-ways may vary between species, according to the substrates avail-able during in the female reproductive tract and the specificfunction to be carried out (Amaral et al., 2013). Finally, the abilityof sperm mitochondria to accumulate calcium has also been sug-gested to have a role in sperm signaling pathways (Publicoveret al., 2008; Publicover et al., 2007).
2.4. Mitochondria in oogenesis
Essentially the same roles are postulated for mitochondria in fe-male gametogenesis, adapted to the circumstances related to cyclicoogenesis/folliculogenesis. Oogenesis involves the production ofvery few gametes with high developmental competence, ratherthan millions of gametes with reduced (individual) potential,and, as in the testis, intrinsic apoptotic pathways involving mito-chondria also seem to play a role in follicle survival and selection(Hunzicker-Dunn and Mayo, 2006). Indeed, recent mouse data sug-gests that the mitochondrial-dependent intrinsic apoptotic path-way is constitutively active in oocytes, and might help eliminatefemale gametes with meiotic defects (Ene et al., 2013). Interest-ingly there also seem to be sex-specific differences, as noted inmice devoid of BCL-2: while males show decreased spermatogen-esis (as discussed above), folliculogenesis was increased and folli-cle apoptosis inhibited (Yamamoto et al., 2001). Female micewithout BAX also had an increased number of ovarian folliclesand extended fertility (Greenfeld et al., 2007; Perez et al., 2007),although this could be due to an indirect effect on PGC migration(Greenfeld et al., 2007). At any rate targeted expression of BCL-2seemed to provide equivalent results (Morita et al., 1999). Usingsimilar strategies other BCL-2 family proteins expressed in the
ovary (BCL-X, BOK) were shown to have no apparent role (Keet al., 2012; Riedlinger et al., 2002).
Mitochondria are the most abundant and prominent organellein the oocyte and early embryo (Motta et al., 2000; Sathananthanand Trounson, 2000) (Table 1). Depending on the species, a mam-malian oocyte contains around 105 to 108 mitochondria (Chenet al., 1995; Jansen and de Boer, 1998), descending from a re-stricted founder population in PGCs. Interestingly, female miceseem to select against mutated mtDNA that cause extensive dam-age and mitochondrial dysfunction, not including these mutationsin ovulated oocytes (Fan et al., 2008). As noted previously, mito-chondria are transmitted exclusively from the maternal gamete(Cummins, 2001; St John et al., 2010). Contradicting a common no-tion, in mammals the entire sperm enters the oocyte at fertilizationhowever sperm mitochondria are diluted or destroyed inside theembryo (Ankel-Simons and Cummins, 1996; Ramalho-Santos,2011). In rare cases where paternal mitochondria are not destroyeda mixture of mtDNA types in the embryo (mtDNA heteroplasmy)might result, and could impair development (St John et al., 2010).During oocyte maturation mitochondria are relocated to differentregions, in response to localized energy demands (Bavister andSquirrell, 2000; Van Blerkom, 2011), and bursts on ATP productionare correlated with mitochondrial redistribution and oocyte matu-ration (Yu et al., 2010).
Mitochondrial function may determine mammalian oocytequality and mitochondrial activity, mtDNA copy number andmtDNA mutations, have been associated with fertilization rates,embryo development and maternal age, and proposed as bioindi-cators for oocyte competence (Wang and Sun, 2007). Additionally,mitochondria-related factors such as ATP, pyruvate dehydrogenasecomplex and ROS are necessary for correct spindle assembly andchromosome alignment in female meiosis (Choi et al., 2007; John-son et al., 2007; Van Blerkom, 2011; Zhang et al., 2006). On theother hand the mitochondrial Immp2l mutation mentioned earlierin the context of spermatogenesis causes female infertility, byaffecting MMP and ROS production (Lu et al., 2008). Finally, oocytemitochondria also contribute in regulating calcium waves, essen-tial for zygote activation (Dumollard et al., 2003; Dumollardet al., 2004).
2.5. Mitochondria in early embryo development
Similarly to what has been described for spermatogenesis,mitochondrial structure and metabolic activity seem to vary in dis-tinct stages of oocyte and embryo development (Biggers et al.,1967; Gott et al., 1990; Harris et al., 2009; Houghton, 2006; Leese,1995; Van Blerkom, 2009; Van Blerkom, 2011; Wycherley et al.,2005) (Table 1). Nevertheless, OXPHOS is clearly important at cer-tain stages of follicular development/meiotic maturation, duringfertilization, and in the first stages on embryo development.
In the final stage of pre-implantation development (i.e. the blas-tocyst stage) there is a clear division of cellular lineages, with asmall cluster of Inner Cell Mass (ICM)/pluriblast cells, surroundedby a thin layer of trophoblast (called trophectoderm after implan-tation) cells. Interestingly, while ICM cells have low MMP and arealmost quiescent in terms of mitochondrial activity, trophoblastcells are highly polarized and very active, producing more ATPand consuming more oxygen, and both aspects seem to be impor-tant for implantation (Houghton, 2006; Leese, 2012; Van Blerkom,2009; Van Blerkom, 2011) (Table 1). Pluripotent embryonic stemcells (ESCs) isolated from the ICM maintain this characteristic,and favor aerobic glycolysis over OXPHOS in terms of ATP produc-tion (Ramalho-Santos et al., 2009; Van Blerkom, 2008; Varum et al.,2009). More importantly, somatic cell reprogramming to pluripo-tency to generate induced pluripotent stem cells (iPSCs) also in-volves a glycolytic shift away from OXPHOS, and concomitant
J. Ramalho-Santos, S. Amaral / Molecular and Cellular Endocrinology 379 (2013) 74–84 79

changes in mitochondrial function and morphology (Armstronget al., 2010; Folmes et al., 2011; Prigione et al., 2010; Varumet al., 2011). As noted above some of these features are also foundin spermatogonial stem cells, suggesting that they may be commonto all cells with differentiation potential and roles in the transmis-sion of information. The reasons for this remain unknown,although it has been suggested (Ramalho-Santos et al., 2009) thatlow mitochondrial activity would also prevent ROS-inducedcell damage, which might be detrimental both to embryodevelopment (ICM cells), and genetic transmission via the germ-line (spermatogonia).
3. The endocrine role of mitochondria in reproduction
3.1. The mitochondrial step in steroid biosynthesis
The initial enzymatic reaction in the biosynthesis of all steroidstakes place in mitochondria, and involves the conversion of choles-terol to pregnenolone (Manna et al., 2009; Stouffer, 2006). Thisreaction is dependent on cytochrome P450 side-chain cleavage(P450scc; or CYP11A1), located on the matrix-facing side of the in-ner mitochondrial membrane (Fig. 1). In turn, P450cc activity isdependent on electron transfer from NADPH mediated by theadrenoxin-adrenoxin reductase system (Miller, 2005). Pregneno-lone is exported from mitochondria (although it can also be furtherprocessed there in some cases) and can be converted to other com-pounds (progesterone, testosterone) by enzymes in the endoplas-mic reticulum/microsomal system (Stocco and McPhaul, 2006).Other crucial factors for the mitochondrial step in steroid biosyn-thesis are the steroidogenic acute regulatory protein (StAR; (Sto-cco, 2001) and the transducesome complex, which includescomponents such as a 18 kDa translocator protein (TPSO), the volt-age dependent anion channel (VDAC-1), TPSO-associated protein 7and protein kinase A subunit 1a (Hauet et al., 2005; Li et al., 2001;Papadopoulos et al., 2007; Papadopoulos and Miller, 2012). Preg-nenolone synthesis requires the processing of cholesterol by an in-ner mitochondrial membrane cytochrome, i.e., it takes place in amembrane devoid of cholesterol (Tuckey et al., 2002), possibly toavoid changes in membrane fluidity/functionality that might occurelsewhere. Although cholesterol sources for steroid biosynthesismay vary, a limiting step is the transport of this lipid from the out-er to the inner mitochondrial membrane, a process catalyzed byStAR, and in which transduceosome also participates, although de-tails regarding the interaction of StAR with this complex need to befurther clarified (Manna et al., 2009).
3.2. Sex-specific steroidogenesis
Male steroidogenesis involves the final production of testoster-one (or of the more potent testosterone-derived androgen dihydro-testosterone), and also of some estrogens. As noted previously thistakes place mostly in Leydig cells (Ge et al., 2008). Although in theovary theca cells are homologous to Leydig cells, steroidogenesis(notably the production of estrogens and progesterone) also occursin granulosa cells, from androgens initially produced in theca cells,and varies (both in quantity and in quality) in conjunction with thefolliculogenesis/ovulation cycle (Bjersing, 1968; Gelety and Magof-fin, 1997). In fact, follicle growth is related to granulosa cell divi-sion, maturation and increased steroidogenic activity, which alsoinfluences/is influenced by oocyte growth and maturation withinthe follicle, due to gap junctions established between the gameteand its supporting cells (Albertini et al., 2001; Gilchrist et al.,2008). Following ovulation the ruptured follicle contains thecacells and granulosa cells that did not accompany the oocyte (sur-rounding it as cumulus cells). The extensive cellular remodeling
that then takes place seems to include these different cell types,resulting in the formation of the corpus luteum, a transient endo-crine gland crucial for the establishment of a viable pregnancy, andthat produces mainly progesterone (Niswender, 2002; Stouffer,2006). The continuous production of the same steroid hormonesby a defined cell type in the male (following the continuous natureof spermatogenesis) is thus contrasted by the cyclic production ofdifferent steroid hormones by changing cell types in the female.
Several signaling pathways can regulate steroid production byactivating/inactivating distinct factors, or changing their expres-sion levels. This may take place under physiological circumstances(puberty in either sex, different stages of the ovarian cycle), or as aresult of a pathological event. Molecular tools devised to specifi-cally target the gonads have provided information focusing mostlydownstream of initial mitochondrial intervention. Thus, ovarianStAR expression is upregulated during the periovulatory periodin parallel with steroid biosynthesis. It is mainly present in the the-ca interna at the beginning of the ovulatory process, increasing inthe granulosa layer when ovulatory follicles begin producing sub-stantial amounts of progesterone, and continues to be prevalent inthe corpus luteum (Richards and Pangas, 2010a, 2010b). Con-versely in Leydig cells StAR and P450scc expression is reduced asa function of aging, and this might therefore compromise the earlysteps of steroidogenesis (Luo et al., 2001). Furthermore, the impor-tance of StAR in this process was confirmed with KO mice, whichshowed undescended testicles, problems with sperm maturation,and premature ovarian failure (Hasegawa et al., 2000). Similar ap-proaches had been employed to study the role of other participantsin this process, such as the importance of VDAC and of the phos-phate transporter in StAR function (Bose et al., 2008).
Additionally, different in vitro models have been used to studythe role of mitochondria in steroidogenesis. For example, in Leydigcell models it has been convincingly shown that synthesis of preg-nenolone from cholesterol via P450scc requires ETC activity, highMMP and the ability to produce ATP (Allen et al., 2006; Haleset al., 2005; Levine et al., 2007; Midzak et al., 2011; Stocco andMcPhaul, 2006). However, these requirements may well vary withthe system used (e.g. primary cells isolated from the testis, versusimmortal Leydig cell lines), an important point that has been high-lighted in a recent study (Midzak et al., 2011). Similar studies havealso been developed in ovarian cells, mainly regarding the effectsof different substances on mitochondrial function and associatedsteroidogenesis, including putative therapeutic agents (Ortegaet al., 2012) and toxicants (Svechnikova et al., 2007). It has alsobeen shown that P450cc induction takes place before steroidogen-esis (Hanukoglu et al., 1990).
Such models should provide novel insights into the role of mito-chondria in reproduction, although they must always accuratelyspecify, and report back to, the particularities of gametogenesisin either sex. It should also be noted that gonad steroidogenesismay link back to other mitochondrial attributes, for example par-ticipating in the regulation apoptosis in both Sertoli cells and ovar-ian follicles (Simoes et al., 2013; Yacobi et al., 2007).
4. Conclusions and future perspectives
Although some reproductive processes are hard to modelin vitro, or monitor in vivo, many studies have highlighted the sev-eral roles played by mitochondria in mammalian reproduction, asstressed by the fact that mitochondrial dysfunction has been linkedto subfertility and infertility at distinct levels, including poor OX-PHOS activity, changes in mtDNA, excessive ROS production, theabnormal triggering of apoptosis, or defects in steroidogenesis.These studies are extremely relevant, both in terms of fertilitymanagement and for reproductive toxicology. However, there are
80 J. Ramalho-Santos, S. Amaral / Molecular and Cellular Endocrinology 379 (2013) 74–84

a few other emerging topics where the study of mitochondrialfunction may also prove useful.
Although the mechanisms involved remain obscure, recent datashowing a putative transgenerational (and sex-specific) influenceof certain conditions (high fat or low protein diets), or even theuse of modified ART, on offspring (Calle et al., 2012; Caroneet al., 2010; Ng et al., 2010) is particularly interesting, and may alsoinvolve changes in mitochondrial function. Indeed, mitochondrialdysfunction in oocytes and cumulus cells cultured under diabeticor insulin-resistance conditions has been recently related to poorfertility, (Ou et al., 2012; Wang et al., 2009, 2010) and infertilityin obese Leptin-deficient (ob/ob) mice has been linked to ovariandysfunction, and notably to higher levels of apoptosis and de-creased steroidogenesis (Serke et al., 2012).
The integration of mitochondrial functions (especially ETC andTCA) in the wider context of cell homeostasis has also been sug-gested (Folmes et al., 2012; Hitchler and Domann, 2009), as it per-tains to signaling and epigenetic status (for example, withmitochondria providing intermediates for epigenetic post-transla-tional modifications). This may provide novel insights into repro-ductive function, where both erasure of imprints in PGCs and there-placing of sex-specific marks upon gonad colonization are wellknown phenomena (Abramowitz and Bartolomei, 2012).
Finally, mitochondrial function in gonads may also be unex-pectedly related to regulatory RNA processing. Recently male(but not female) KO mice for the mitochondria-specific phospholi-pase D, were shown by two independent groups to be infertile dueto meiotic arrest, and this was correlated with fission-fusion de-fects and, interestingly, also with impaired production of piRNAsthat are crucial for proper spermatogenesis (Huang et al., 2011;Watanabe et al., 2011).
Acknowledgements
Given the extent of available literature, and the specific multi-disciplinary nature of this paper, readers have been often referredto review articles. Apologies are due to all authors whose work wasnot directly cited. Alexandra Amaral is thanked for critical readingof the Manuscript and J. Saints is gratefully acknowledged for lin-guistic suggestions. All lab members are thanked for helpful dis-cussions, especially Paula Mota, Ana Sofia Rodrigues and AnaPaula Sousa. Part of the work in the Authors lab was funded byFEDER and COMPETE, via FCT (Fundação para a Ciência e Tecnolo-gia), Portugal in grants PTDC/EBB-EBI/101114/2008, PTDC/EBB-EBI/120634/2010 and PTDC/QUI-BIQ/120652/2010. Sandra Amaralis the recipient of a FCT fellowship (SFRH/BPD/63190/2009) andthe Center for Neuroscience and Cell Biology (CNC) funding is alsosupported by FCT (PEst-C/SAU/LA0001/2011).
References
Abramowitz, L.K., Bartolomei, M.S., 2012. Genomic imprinting: recognition andmarking of imprinted loci. Curr. Opin. Genet. Dev. 22, 72–78.
Agarwal, A., Saleh, R.A., Bedaiwy, M.A., 2003. Role of reactive oxygen species in thepathophysiology of human reproduction. Fertil. Steril. 79, 829–843.
Aihara, T., Nakamura, N., Honda, S., Hirose, S., 2009. A novel potential role forgametogenetin-binding protein 1 (GGNBP1) in mitochondrial morphogenesisduring spermatogenesis in mice. Biol. Reprod. 80, 762–770.
Aitken, R.J., Gibb, Z., Mitchell, L.A., Lambourne, S.R., Connaughton, H.S., De Iuliis,G.N., 2012. Sperm motility is lost in vitro as a consequence of mitochondrial freeradical production and the generation of electrophilic aldehydes but can besignificantly rescued by the presence of nucleophilic thiols. Biol. Reprod. 87,110.
Albertini, D.F., Combelles, C.M., Benecchi, E., Carabatsos, M.J., 2001. Cellular basis forparacrine regulation of ovarian follicle development. Reproduction 121, 647–653.
Allen, J.A., Shankara, T., Janus, P., Buck, S., Diemer, T., Hales, K.H., Hales, D.B., 2006.Energized, polarized, and actively respiring mitochondria are required for acuteLeydig cell steroidogenesis. Endocrinology 147, 3924–3935.
Aly, H.A., Khafagy, R.M., 2011. 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD)-inducedcytotoxicity accompanied by oxidative stress in rat Sertoli cells: Possible role ofmitochondrial fractions of Sertoli cells. Toxicol. Appl. Pharmacol. 252, 273–280.
Amaral, S., Ramalho-Santos, J., 2009. Aging, mitochondria and male reproductivefunction. Curr. Aging Sci. 2, 165–173.
Amaral, S., Mota, P., Rodrigues, A.S., Martins, L., Oliveira, P.J., Ramalho-Santos, J.,2008a. Testicular aging involves mitochondrial dysfunction as well as anincrease in UCP2 levels and proton leak. FEBS Lett. 582, 4191–4196.
Amaral, S., Oliveira, P.J., Ramalho-Santos, J., 2008b. Diabetes and the impairment ofreproductive function: possible role of mitochondria and reactive oxygenspecies. Curr. Diabetes Rev. 4, 46–54.
Amaral, S., Mota, P.C., Lacerda, B., Alves, M., Pereira Mde, L., Oliveira, P.J., Ramalho-Santos, J., 2009. Testicular mitochondrial alterations in untreatedstreptozotocin-induced diabetic rats. Mitochondrion 9, 41–50.
Amaral, A., Paiva, C., Baptista, M., Sousa, A.P., Ramalho-Santos, J., 2011. Exogenousglucose improves long-standing human sperm motility, viability, andmitochondrial function. Fertil. Steril. 96, 848–850.
Amaral, A., Castillo, J., Estanyol, J.M., Ballesca, J.L., Ramalho-Santos, J., Oliva, R., 2013.Human sperm tail proteome suggests new endogenous metabolic pathways.Mol. Cell. Proteomics 12, 330–342.
Ankel-Simons, F., Cummins, J.M., 1996. Misconceptions about mitochondria andmammalian fertilization: implications for theories on human evolution. Proc.Natl. Acad. Sci. USA 93, 13859–13863.
Armstrong, L., Tilgner, K., Saretzki, G., Atkinson, S.P., Stojkovic, M., Moreno, R.,Przyborski, S., Lako, M., 2010. Human induced pluripotent stem cell lines showstress defense mechanisms and mitochondrial regulation similar to those ofhuman embryonic stem cells. Stem Cells 28, 661–673.
Bajpai, M., Gupta, G., Setty, B.S., 1998. Changes in carbohydrate metabolism oftesticular germ cells during meiosis in the rat. Eur. J. Endocrinol. 138, 322–327.
Banu, S.K., Stanley, J.A., Lee, J., Stephen, S.D., Arosh, J.A., Hoyer, P.B., Burghardt, R.C.,2011. Hexavalent chromium-induced apoptosis of granulosa cells involvesselective sub-cellular translocation of Bcl-2 members, ERK1/2 and p53. Toxicol.Appl. Pharmacol. 251, 253–266.
Bavister, B.D., Squirrell, J.M., 2000. Mitochondrial distribution and function inoocytes and early embryos. Hum. Reprod. 15 (Suppl. 2), 189–198.
Bentov, Y., Yavorska, T., Esfandiari, N., Jurisicova, A., Casper, R.F., 2011. Thecontribution of mitochondrial function to reproductive aging. J. Assist. Reprod.Genet. 28, 773–783.
Bereiter-Hahn, J., Voth, M., 1994. Dynamics of mitochondria in living cells: shapechanges, dislocations, fusion, and fission of mitochondria. Microsc. Res. Tech.27, 198–219.
Biggers, J.D., Whittingham, D.G., Donahue, R.P., 1967. The pattern of energymetabolism in the mouse oocyte and zygote. Proc Natl Acad Sci USA 58, 560–567.
Bjersing, L., 1968. On the morphology and endocrine function of granulosa cells inovarian follicles and corpora lutea. Biochemical, histochemical, andultrastructural studies on the porcine ovary with special reference to steroidhormone synthesis (Copenh). Acta Endocrinol. (Suppl. 12), 121–123.
Bose, M., Whittal, R.M., Miller, W.L., Bose, H.S., 2008. Steroidogenic activity of StARrequires contact with mitochondrial VDAC1 and phosphate carrier protein. J.Biol. Chem. 283, 8837–8845.
Boussouar, F., Benahmed, M., 2004. Lactate and energy metabolism in male germcells. Trends Endocrinol. Metab. 15, 345–350.
Brower, J.V., Lim, C.H., Jorgensen, M., Oh, S.P., Terada, N., 2009. Adenine nucleotidetranslocase 4 deficiency leads to early meiotic arrest of murine male germ cells.Reproduction 138, 463–470.
Calle, A., Miranda, A., Fernandez-Gonzalez, R., Pericuesta, E., Laguna, R., Gutierrez-Adan, A., 2012. Male mice produced by in vitro culture have reduced fertilityand transmit organomegaly and glucose intolerance to their male offspring.Biol. Reprod. 87, 34.
Campello, S., Scorrano, L., 2010. Mitochondrial shape changes: orchestrating cellpathophysiology. EMBO Rep. 11, 678–684.
Carone, B.R., Fauquier, L., Habib, N., Shea, J.M., Hart, C.E., Li, R., Bock, C., Li, C., Gu, H.,Zamore, P.D., Meissner, A., Weng, Z., Hofmann, H.A., Friedman, N., Rando, O.J.,2010. Paternally induced transgenerational environmental reprogramming ofmetabolic gene expression in mammals. Cell 143, 1084–1096.
Cereghetti, G.M., Scorrano, L., 2011. Phagocytosis: coupling of mitochondrialuncoupling and engulfment. Curr. Biol. 21, R852–854.
Chen, X., Prosser, R., Simonetti, S., Sadlock, J., Jagiello, G., Schon, E.A., 1995.Rearranged mitochondrial genomes are present in human oocytes. Am. J. Hum.Genet. 57, 239–247.
Choi, W.J., Banerjee, J., Falcone, T., Bena, J., Agarwal, A., Sharma, R.K., 2007. Oxidativestress and tumor necrosis factor-alpha-induced alterations in metaphase IImouse oocyte spindle structure. Fertil. Steril. 88, 1220–1231.
Collado-Fernandez, E., Picton, H.M., Dumollard, R., 2012. Metabolism throughoutfollicle and oocyte development in mammals. Int. J. Dev. Biol. 56, 799–808.
Collins, T.J., Berridge, M.J., Lipp, P., Bootman, M.D., 2002. Mitochondria aremorphologically and functionally heterogeneous within cells. EMBO J. 21,1616–1627.
Correia, S.C., Santos, R.X., Perry, G., Zhu, X., Moreira, P.I., Smith, M.A., 2012.Mitochondrial importance in Alzheimer’s, Huntington’s and Parkinson’sdiseases. Adv. Exp. Med. Biol. 724, 205–221.
Coultas, L., Bouillet, P., Loveland, K.L., Meachem, S., Perlman, H., Adams, J.M.,Strasser, A., 2005. Concomitant loss of proapoptotic BH3-only Bcl-2 antagonistsBik and Bim arrests spermatogenesis. EMBO J. 24, 3963–3973.
Cummins, J.M., 2001. Mitochondria: potential roles in embryogenesis andnucleocytoplasmic transfer. Hum. Reprod. Update 7, 217–228.
J. Ramalho-Santos, S. Amaral / Molecular and Cellular Endocrinology 379 (2013) 74–84 81

De Martino, C., Floridi, A., Marcante, M.L., Malorni, W., Scorza Barcellona, P., Bellocci,M., Silvestrini, B., 1979. Morphological, histochemical and biochemical studieson germ cell mitochondria of normal rats. Cell Tissue Res. 196, 1–22.
Dorn 2nd, G.W., Scorrano, L., 2010. Two close, too close: sarcoplasmic reticulum-mitochondrial crosstalk and cardiomyocyte fate. Circ. Res. 107, 689–699.
Dumollard, R., Hammar, K., Porterfield, M., Smith, P.J., Cibert, C., Rouviere, C., Sardet,C., 2003. Mitochondrial respiration and Ca2+ waves are linked duringfertilization and meiosis completion. Development 130, 683–692.
Dumollard, R., Marangos, P., Fitzharris, G., Swann, K., Duchen, M., Carroll, J., 2004.Sperm-triggered [Ca2+] oscillations and Ca2+ homeostasis in the mouse egg havean absolute requirement for mitochondrial ATP production. Development 131,3057–3067.
Dumollard, R., Carroll, J., Duchen, M.R., Campbell, K., Swann, K., 2009. Mitochondrialfunction and redox state in mammalian embryos. Semin. Cell Dev. Biol. 20, 346–353.
Dunning, K.R., Cashman, K., Russell, D.L., Thompson, J.G., Norman, R.J., Robker, R.L.,2010. Beta-oxidation is essential for mouse oocyte developmental competenceand early embryo development. Biol. Reprod. 83, 909–918.
Ene, A.C., Park, S., Edelmann, W., Taketo, T., 2013. Caspase 9 is constitutivelyactivated in mouse oocytes and plays a key role in oocyte elimination duringmeiotic prophase progression. Dev. Biol..
Fan, W., Waymire, K.G., Narula, N., Li, P., Rocher, C., Coskun, P.E., Vannan, M.A.,Narula, J., Macgregor, G.R., Wallace, D.C., 2008. A mouse model of mitochondrialdisease reveals germline selection against severe mtDNA mutations. Science319, 958–962.
Folmes, C.D., Nelson, T.J., Martinez-Fernandez, A., Arrell, D.K., Lindor, J.Z., Dzeja, P.P.,Ikeda, Y., Perez-Terzic, C., Terzic, A., 2011. Somatic oxidative bioenergeticstransitions into pluripotency-dependent glycolysis to facilitate nuclearreprogramming. Cell Metab. 14, 264–271.
Folmes, C.D., Dzeja, P.P., Nelson, T.J., Terzic, A., 2012. Metabolic plasticity in stemcell homeostasis and differentiation. Cell Stem Cell 11, 596–606.
Gallon, F., Marchetti, C., Jouy, N., Marchetti, P., 2006. The functionality ofmitochondria differentiates human spermatozoa with high and low fertilizingcapability. Fertil. Steril. 86, 1526–1530.
Gassei, K., Schlatt, S., 2007. Testicular morphogenesis: comparison of in vivo andin vitro models to study male gonadal development. Ann. N. Y. Acad. Sci. 1120,152–167.
Ge, R., Chen, G., Hardy, M.P., 2008. The role of the Leydig cell in spermatogenicfunction. Adv. Exp. Med. Biol. 636, 255–269.
Gelety, T.J., Magoffin, D.A., 1997. Ontogeny of steroidogenic enzyme geneexpression in ovarian theca-interstitial cells in the rat: regulation by aparacrine theca-differentiating factor prior to achieving luteinizing hormoneresponsiveness. Biol. Reprod. 56, 938–945.
George, S.K., Jiao, Y., Bishop, C.E., Lu, B., 2012. Oxidative stress is involved in age-dependent spermatogenic damage of Immp2l mutant mice. Free Radic. Biol.Med. 52, 2223–2233.
Gilbert, S., 2010. Developmental Biology, ninth ed.. Sinauer, New York.Gilchrist, R.B., Lane, M., Thompson, J.G., 2008. Oocyte-secreted factors: regulators of
cumulus cell function and oocyte quality. Hum. Reprod. Update 14, 159–177.Gott, A.L., Hardy, K., Winston, R.M., Leese, H.J., 1990. Non-invasive measurement of
pyruvate and glucose uptake and lactate production by single humanpreimplantation embryos. Hum. Reprod. 5, 104–108.
Greenfeld, C.R., Pepling, M.E., Babus, J.K., Furth, P.A., Flaws, J.A., 2007. BAX regulatesfollicular endowment in mice. Reproduction 133, 865–876.
Grootegoed, J.A., Jansen, R., Van der Molen, H.J., 1984. The role of glucose, pyruvateand lactate in ATP production by rat spermatocytes and spermatids. Biochim.Biophys. Acta 767, 248–256.
Hales, D.B., Allen, J.A., Shankara, T., Janus, P., Buck, S., Diemer, T., Hales, K.H., 2005.Mitochondrial function in Leydig cell steroidogenesis. Ann. N. Y. Acad. Sci. 1061,120–134.
Hanukoglu, I., Suh, B.S., Himmelhoch, S., Amsterdam, A., 1990. Induction andmitochondrial localization of cytochrome P450scc system enzymes in normaland transformed ovarian granulosa cells. J. Cell Biol. 111, 1373–1381.
Harris, S.E., Leese, H.J., Gosden, R.G., Picton, H.M., 2009. Pyruvate and oxygenconsumption throughout the growth and development of murine oocytes. Mol.Reprod. Dev. 76, 231–238.
Hasegawa, T., Zhao, L., Caron, K.M., Majdic, G., Suzuki, T., Shizawa, S., Sasano, H.,Parker, K.L., 2000. Developmental roles of the steroidogenic acute regulatoryprotein (StAR) as revealed by StAR knockout mice. Mol. Endocrinol. 14, 1462–1471.
Hauet, T., Yao, Z.X., Bose, H.S., Wall, C.T., Han, Z., Li, W., Hales, D.B., Miller, W.L.,Culty, M., Papadopoulos, V., 2005. Peripheral-type benzodiazepine receptor-mediated action of steroidogenic acute regulatory protein on cholesterol entryinto leydig cell mitochondria. Mol. Endocrinol. 19, 540–554.
Hess, R.A., Miller, L.A., Kirby, J.D., Margoliash, E., Goldberg, E., 1993.Immunoelectron microscopic localization of testicular and somaticcytochromes c in the seminiferous epithelium of the rat. Biol. Reprod. 48,1299–1308.
Hitchler, M.J., Domann, F.E., 2009. Metabolic defects provide a spark for theepigenetic switch in cancer. Free Radic. Biol. Med. 47, 115–127.
Ho, H.C., Wey, S., 2007. Three dimensional rendering of the mitochondrial sheathmorphogenesis during mouse spermiogenesis. Microsc. Res. Tech. 70, 719–723.
Holstein, A.F., Schulze, W., Davidoff, M., 2003. Understanding spermatogenesis is aprerequisite for treatment. Reprod. Biol. Endocrinol. 1, 107.
Hom, J., Sheu, S.S., 2009. Morphological dynamics of mitochondria–a specialemphasis on cardiac muscle cells. J. Mol. Cell. Cardiol. 46, 811–820.
Honarpour, N., Du, C., Richardson, J.A., Hammer, R.E., Wang, X., Herz, J.,2000. Adult Apaf-1-deficient mice exhibit male infertility. Dev. Biol. 218,248–258.
Houghton, F.D., 2006. Energy metabolism of the inner cell mass and trophectodermof the mouse blastocyst. Differentiation 74, 11–18.
Huang, H., Gao, Q., Peng, X., Choi, S.Y., Sarma, K., Ren, H., Morris, A.J., Frohman, M.A.,2011. PiRNA-associated germline nuage formation and spermatogenesis requireMitoPLD profusogenic mitochondrial-surface lipid signaling. Dev. Cell 20, 376–387.
Hunzicker-Dunn, M., Mayo, K., 2006. Gonadotropin signaling in the ovary. In: Neill,J.e. (Ed.), Knobil and Neill’s Physiology of Reproduction, third ed. AcademicPress/Elsevier, St. Louis, MO, USA, pp. 547–592.
Huttemann, M., Jaradat, S., Grossman, L.I., 2003. Cytochrome c oxidase of mammalscontains a testes-specific isoform of subunit VIb – the counterpart to testes-specific cytochrome c? Mol. Reprod. Dev. 66, 8–16.
Jansen, R.P., de Boer, K., 1998. The bottleneck: mitochondrial imperatives inoogenesis and ovarian follicular fate. Mol. Cell. Endocrinol. 145, 81–88.
Jia, Y., Lee, K.W., Swerdloff, R., Hwang, D., Cobb, L.J., Sinha Hikim, A., Lue, Y.H., Cohen,P., Wang, C., 2010. Interaction of insulin-like growth factor-binding protein-3and BAX in mitochondria promotes male germ cell apoptosis. J. Biol. Chem. 285,1726–1732.
Johnson, M.T., Freeman, E.A., Gardner, D.K., Hunt, P.A., 2007. Oxidative metabolismof pyruvate is required for meiotic maturation of murine oocytes in vivo. Biol.Reprod. 77, 2–8.
Kakkar, P., Singh, B.K., 2007. Mitochondria: a hub of redox activities and cellulardistress control. Mol. Cell. Biochem. 305, 235–253.
Katz, S.G., Fisher, J.K., Correll, M., Bronson, R.T., Ligon, K.L., Walensky, L.D., 2012.Brain and testicular tumors in mice with progenitor cells lacking BAX and BAK.Oncogene.
Ke, F., Voss, A., Kerr, J.B., O’Reilly, L.A., Tai, L., Echeverry, N., Bouillet, P., Strasser, A.,Kaufmann, T., 2012. BCL-2 family member BOK is widely expressed but its losshas only minimal impact in mice. Cell Death Differ. 19, 915–925.
Knudson, C.M., Tung, K.S., Tourtellotte, W.G., Brown, G.A., Korsmeyer, S.J., 1995.Bax-deficient mice with lymphoid hyperplasia and male germ cell death.Science 270, 96–99.
Leese, H.J., 1995. Metabolic control during preimplantation mammaliandevelopment. Hum. Reprod. Update 1, 63–72.
Leese, H.J., 2012. Metabolism of the preimplantation embryo: 40 years on.Reproduction 143, 417–427.
Levine, S.L., Han, Z., Liu, J., Farmer, D.R., Papadopoulos, V., 2007. Disruptingmitochondrial function with surfactants inhibits MA-10 Leydig cellsteroidogenesis. Cell Biol. Toxicol. 23, 385–400.
Li, H., Degenhardt, B., Tobin, D., Yao, Z.X., Tasken, K., Papadopoulos, V., 2001.Identification, localization, and function in steroidogenesis of PAP7: aperipheral-type benzodiazepine receptor- and PKA (RIalpha)-associatedprotein. Mol. Endocrinol. 15, 2211–2228.
Lu, B., Poirier, C., Gaspar, T., Gratzke, C., Harrison, W., Busija, D., Matzuk, M.M.,Andersson, K.E., Overbeek, P.A., Bishop, C.E., 2008. A mutation in the innermitochondrial membrane peptidase 2-like gene (Immp2l) affects mitochondrialfunction and impairs fertility in mice. Biol. Reprod. 78, 601–610.
Luo, L., Chen, H., Zirkin, B.R., 2001. Leydig cell aging: steroidogenic acuteregulatory protein (StAR) and cholesterol side-chain cleavage enzyme. J.Androl. 22, 149–156.
Manna, P.R., Dyson, M.T., Stocco, D.M., 2009. Regulation of the steroidogenic acuteregulatory protein gene expression: present and future perspectives. Mol. Hum.Reprod. 15, 321–333.
Mannella, C.A., 2006. The relevance of mitochondrial membrane topology tomitochondrial function. Biochim. Biophys. Acta 1762, 140–147.
Mannella, C.A., 2008. Structural diversity of mitochondria: functional implications.Ann. N. Y. Acad. Sci. 1147, 171–179.
Marchetti, C., Obert, G., Deffosez, A., Formstecher, P., Marchetti, P., 2002. Study ofmitochondrial membrane potential, reactive oxygen species, DNAfragmentation and cell viability by flow cytometry in human sperm. Hum.Reprod. 17, 1257–1265.
Marchetti, P., Ballot, C., Jouy, N., Thomas, P., Marchetti, C., 2012. Influence ofmitochondrial membrane potential of spermatozoa on in vitro fertilisationoutcome. Andrologia 44, 136–141.
Martinou, J.C., Youle, R.J., 2011. Mitochondria in apoptosis: Bcl-2 family membersand mitochondrial dynamics. Dev. Cell 21, 92–101.
Matoba, S., Hiramatsu, R., Kanai-Azuma, M., Tsunekawa, N., Harikae, K., Kawakami,H., Kurohmaru, M., Kanai, Y., 2008. Establishment of testis-specific SOX9activation requires high-glucose metabolism in mouse sex differentiation. Dev.Biol. 324, 76–87.
McLaughlin, E.A., McIver, S.C., 2009. Awakening the oocyte: controlling primordialfollicle development. Reproduction 137, 1–11.
Meinhardt, A., Hedger, M.P., 2011. Immunological, paracrine and endocrine aspectsof testicular immune privilege. Mol. Cell. Endocrinol. 335, 60–68.
Meinhardt, A., Wilhelm, B., Seitz, J., 1999. Expression of mitochondrial markerproteins during spermatogenesis. Hum. Reprod. Update 5, 108–119.
Midzak, A.S., Chen, H., Aon, M.A., Papadopoulos, V., Zirkin, B.R., 2011. ATP synthesis,mitochondrial function, and steroid biosynthesis in rodent primary and tumorLeydig cells. Biol. Reprod. 84, 976–985.
Miller, W.L., 2005. Minireview: regulation of steroidogenesis by electron transfer.Endocrinology 146, 2544–2550.
Mittwoch, U., 2004. The elusive action of sex-determining genes: mitochondria tothe rescue? J. Theor. Biol. 228, 359–365.
82 J. Ramalho-Santos, S. Amaral / Molecular and Cellular Endocrinology 379 (2013) 74–84

Miyamoto, K., Sato, E.F., Kasahara, E., Jikumaru, M., Hiramoto, K., Tabata, H.,Katsuragi, M., Odo, S., Utsumi, K., Inoue, M., 2010. Effect of oxidative stressduring repeated ovulation on the structure and functions of the ovary, oocytes,and their mitochondria. Free Radic. Biol. Med. 49, 674–681.
Morita, Y., Perez, G.I., Maravei, D.V., Tilly, K.I., Tilly, J.L., 1999. Targeted expression ofBcl-2 in mouse oocytes inhibits ovarian follicle atresia and preventsspontaneous and chemotherapy-induced oocyte apoptosis in vitro. Mol.Endocrinol. 13, 841–850.
Mota, P., Amaral, S., Martins, L., de Lourdes Pereira, M., Oliveira, P.J., Ramalho-Santos, J., 2009. Mitochondrial bioenergetics of testicular cells from thedomestic cat (Felis catus)-a model for endangered species. Reprod. Toxicol.27, 111–116.
Mota, P.C., Cordeiro, M., Pereira, S.P., Oliveira, P.J., Moreno, A.J., Ramalho-Santos, J.,2011. Differential effects of p, p’-DDE on testis and liver mitochondria:implications for reproductive toxicology. Reprod. Toxicol. 31, 80–85.
Motta, P.M., Nottola, S.A., Makabe, S., Heyn, R., 2000. Mitochondrial morphology inhuman fetal and adult female germ cells. Hum. Reprod. 15 (Suppl. 2), 129–147.
Nakada, K., Sato, A., Yoshida, K., Morita, T., Tanaka, H., Inoue, S., Yonekawa, H.,Hayashi, J., 2006. Mitochondria-related male infertility. Proc Natl Acad Sci USA103, 15148–15153.
Nakamura, M., Okinaga, S., Arai, K., 1984. Metabolism of pachytene primaryspermatocytes from rat testes: pyruvate maintenance of adenosinetriphosphate level. Biol. Reprod. 30, 1187–1197.
Narisawa, S., Hecht, N.B., Goldberg, E., Boatright, K.M., Reed, J.C., Millan, J.L., 2002.Testis-specific cytochrome c-null mice produce functional sperm but undergoearly testicular atrophy. Mol. Cell. Biol. 22, 5554–5562.
Nascimento, J.M., Shi, L.Z., Tam, J., Chandsawangbhuwana, C., Durrant, B., Botvinick,E.L., Berns, M.W., 2008. Comparison of glycolysis and oxidative phosphorylationas energy sources for mammalian sperm motility, using the combination offluorescence imaging, laser tweezers, and real-time automated tracking andtrapping. J. Cell. Physiol. 217, 745–751.
Newmeyer, D.D., Ferguson-Miller, S., 2003. Mitochondria: releasing power for lifeand unleashing the machineries of death. Cell 112, 481–490.
Ng, S.F., Lin, R.C., Laybutt, D.R., Barres, R., Owens, J.A., Morris, M.J., 2010. Chronichigh-fat diet in fathers programs beta-cell dysfunction in female rat offspring.Nature 467, 963–966.
Nichols, D.G., Ferguson, S.J., 2002. Bioenergetics, third ed. Academic Press,Amsterdam.
Niswender, G.D., 2002. Molecular control of luteal secretion of progesterone.Reproduction 123, 333–339.
Nunnari, J., Suomalainen, A., 2012. Mitochondria: in sickness and in health. Cell 148,1145–1159.
Oettinghaus, B., Licci, M., Scorrano, L., Frank, S., 2012. Less than perfect divorces:dysregulated mitochondrial fission and neurodegeneration. Acta Neuropathol.123, 189–203.
Olson, G.E., Winfrey, V.P., 1990. Mitochondria-cytoskeleton interactions in thesperm midpiece. J. Struct. Biol. 103, 13–22.
Ortega, I., Cress, A.B., Wong, D.H., Villanueva, J.A., Sokalska, A., Moeller, B.C., Stanley,S.D., Duleba, A.J., 2012. Simvastatin reduces steroidogenesis by inhibitingCyp17a1 gene expression in rat ovarian theca-interstitial cells. Biol. Reprod. 86,1–9.
Otani, H., Tanaka, O., Kasai, K., Yoshioka, T., 1988. Development of mitochondrialhelical sheath in the middle piece of the mouse spermatid tail: regulardispositions and synchronized changes. Anat. Rec. 222, 26–33.
Ou, X.H., Li, S., Wang, Z.B., Li, M., Quan, S., Xing, F., Guo, L., Chao, S.B., Chen, Z., Liang,X.W., Hou, Y., Schatten, H., Sun, Q.Y., 2012. Maternal insulin resistance causesoxidative stress and mitochondrial dysfunction in mouse oocytes. Hum. Reprod.27, 2130–2145.
Palmeira, C.M., Ramalho-Santos, J., 2011. Mitochondrial dysfunction in reproductiveand developmental toxicity. In: Gupta, C. (Ed.), Reproductive andDevelopmental Toxicology R. Elsevier, New York, pp. 815–824.
Papadopoulos, V., Miller, W.L., 2012. Role of mitochondria in steroidogenesis. BestPract. Res. Clin. Endocrinol Metab. 26, 771–790.
Papadopoulos, V., Liu, J., Culty, M., 2007. Is there a mitochondrial signaling complexfacilitating cholesterol import? Mol. Cell. Endocrinol. 265–266, 59–64.
Pereda, J., Zorn, T., Soto-Suazo, M., 2006. Migration of human and mouse primordialgerm cells and colonization of the developing ovary: an ultrastructural andcytochemical study. Microsc. Res. Tech. 69, 386–395.
Perez, G.I., Jurisicova, A., Wise, L., Lipina, T., Kanisek, M., Bechard, A., Takai, Y., Hunt,P., Roder, J., Grynpas, M., Tilly, J.L., 2007. Absence of the proapoptotic Baxprotein extends fertility and alleviates age-related health complications infemale mice. Proc. Natl. Acad. Sci. USA 104, 5229–5234.
Prigione, A., Fauler, B., Lurz, R., Lehrach, H., Adjaye, J., 2010. The senescence-relatedmitochondrial/oxidative stress pathway is repressed in human inducedpluripotent stem cells. Stem Cells 28, 721–733.
Publicover, S.J., Harper, C.V., Barratt, C., 2007. [Ca2+]i signalling in sperm–makingthe most of what you’ve got. Nat. Cell Biol. 9, 235–242.
Publicover, S.J., Giojalas, L.C., Teves, M.E., de Oliveira, G.S., Garcia, A.A., Barratt, C.L.,Harper, C.V., 2008. Ca2+ signalling in the control of motility and guidance inmammalian sperm. Front. Biosci. 13, 5623–5637.
Ramalho-Santos, J., 2011. A sperm’s tail: the importance of getting it right. Hum.Reprod. 26, 2590–2591.
Ramalho-Santos, J., Rodrigues., A.S., 2013. From oocytes and pluripotent stem cellsto fully differentiated fates: (Also) a mitochondrial odyssey. In: St. John, J.C.(Ed.), Mitochondrial DNA Mitochondria Disease and Stem Cells. Humana Press/Springer-Verlag, New York, pp. 69–86.
Ramalho-Santos, J., Varum, S., Amaral, S., Mota, P.C., Sousa, A.P., Amaral, A., 2009.Mitochondrial functionality in reproduction: from gonads and gametes toembryos and embryonic stem cells. Hum. Reprod. Update 15, 553–572.
Reyes, J.G., Farias, J.G., Henriquez-Olavarrieta, S., Madrid, E., Parraga, M., Zepeda,A.B., Moreno, R.D., 2012. The hypoxic testicle: physiology and pathophysiology.Oxid. Med. Cell Longev. 2012, 929285.
Richards, J.S., Pangas, S.A., 2010a. New insights into ovarian function. Handb. Exp.Pharmacol., 3–27.
Richards, J.S., Pangas, S.A., 2010b. The ovary: basic biology and clinical implications.J. Clin. Invest. 120, 963–972.
Riedlinger, G., Okagaki, R., Wagner, K.U., Rucker 3rd, E.B., Oka, T., Miyoshi, K.,Flaws, J.A., Hennighausen, L., 2002. Bcl-x is not required for maintenance offollicles and corpus luteum in the postnatal mouse ovary. Biol. Reprod. 66,438–444.
Robinson, R., Fritz, I.B., 1981. Metabolism of glucose by Sertoli cells in culture. Biol.Reprod. 24, 1032–1041.
Rodrigues, A.S., Lacerda, B., Moreno, A.J., Ramalho-Santos, J., 2010. Proton leakmodulation in testicular mitochondria affects reactive oxygen speciesproduction and lipid peroxidation. Cell Biochem. Funct. 28, 224–231.
Ross, A.J., Amy, S.P., Mahar, P.L., Lindsten, T., Knudson, C.M., Thompson, C.B.,Korsmeyer, S.J., MacGregor, G.R., 2001. BCLW mediates survival of postmitoticSertoli cells by regulating BAX activity. Dev. Biol. 239, 295–308.
Rowland, A.A., Voeltz, G.K., 2012. Endoplasmic reticulum-mitochondria contacts:function of the junction. Nat. Rev. Mol. Cell Biol. 13, 607–625.
Ruiz-Pesini, E., Diez, C., Lapena, A.C., Perez-Martos, A., Montoya, J., Alvarez, E.,Arenas, J., Lopez-Perez, M.J., 1998. Correlation of sperm motility withmitochondrial enzymatic activities. Clin. Chem. 44, 1616–1620.
Ruiz-Pesini, E., Lapena, A.C., Diez-Sanchez, C., Perez-Martos, A., Montoya, J., Alvarez,E., Diaz, M., Urries, A., Montoro, L., Lopez-Perez, M.J., Enriquez, J.A., 2000. HumanmtDNA haplogroups associated with high or reduced spermatozoa motility.Am. J. Hum. Genet. 67, 682–696.
Russell, L.D., Warren, J., Debeljuk, L., Richardson, L.L., Mahar, P.L., Waymire, K.G.,Amy, S.P., Ross, A.J., MacGregor, G.R., 2001. Spermatogenesis in Bclw-deficientmice. Biol. Reprod. 65, 318–332.
Russell, L.D., Chiarini-Garcia, H., Korsmeyer, S.J., Knudson, C.M., 2002. Bax-dependent spermatogonia apoptosis is required for testicular developmentand spermatogenesis. Biol. Reprod. 66, 950–958.
Sanchez-Partida, L.G., Simerly, C.R., Ramalho-Santos, J., 2008. Freeze-dried primatesperm retains early reproductive potential after intracytoplasmic sperminjection. Fertil. Steril. 89, 742–745.
Sathananthan, A.H., Trounson, A.O., 2000. Mitochondrial morphology duringpreimplantational human embryogenesis. Hum. Reprod. 15 (Suppl. 2), 148–159.
Scheffler, I.E., 2001. A century of mitochondrial research: achievements andperspectives. Mitochondrion 1, 3–31.
Serke, H., Nowicki, M., Kosacka, J., Schroder, T., Kloting, N., Bluher, M., Kallendrusch,S., Spanel-Borowski, K., 2012. Leptin-deficient (ob/ob) mouse ovaries show fattydegeneration, enhanced apoptosis and decreased expression of steroidogenicacute regulatory enzyme. Int. J. Obes. (Lond.) 36, 1047–1053.
Shaha, C., Tripathi, R., Mishra, D.P., 2010. Male germ cell apoptosis: regulation andbiology. Philos. Trans. Roy. Soc. Lond. B Biol. Sci. 365, 1501–1515.
Simoes, V.L., Alves, M.G., Martins, A.D., Dias, T.R., Rato, L., Socorro, S., Oliveira, P.F.,2013. Regulation of apoptotic signaling pathways by 5alpha-dihydrotestosterone and 17beta-estradiol in immature rat Sertoli cells. J.Steroid Biochem. Mol. Biol. 135, 15–23.
Smith, B.E., Braun, R.E., 2012. Germ cell migration across Sertoli cell tight junctions.Science 338, 798–802.
Soder, O., 2007. Sexual dimorphism of gonadal development. Best Pract. Res. Clin.Endocrinol. Metab. 21, 381–391.
Songsasen, N., Wesselowski, S., Carpenter, J.W., Wildt, D.E., 2012. The ability toachieve meiotic maturation in the dog oocyte is linked to glycolysis andglutamine oxidation. Mol. Reprod. Dev. 79, 186–196.
Sousa, A.P., Amaral, A., Baptista, M., Tavares, R., Caballero Campo, P., CaballeroPeregrin, P., Freitas, A., Paiva, A., Almeida-Santos, T., Ramalho-Santos, J., 2011.Not all sperm are equal: functional mitochondria characterize a subpopulationof human sperm with better fertilization potential. PLoS ONE 6, e18112.
St John, J.C., Jokhi, R.P., Barratt, C.L., 2005. The impact of mitochondrial genetics onmale infertility. Int. J. Androl. 28, 65–73.
St John, J.C., Facucho-Oliveira, J., Jiang, Y., Kelly, R., Salah, R., 2010. MitochondrialDNA transmission, replication and inheritance: a journey from the gametethrough the embryo and into offspring and embryonic stem cells. Hum. Reprod.Update 16, 488–509.
Stocco, D.M., 2001. StAR protein and the regulation of steroid hormonebiosynthesis. Annu. Rev. Physiol. 63, 193–213.
Stocco, D.M., McPhaul, M.J., 2006. Physiology of testicular steroidogenesis. In: Neill,J.e. (Ed.), Knobil and Neill’s Physiology Of Reproduction, third ed. AcademicPress/Elsevier, St. Louis, MO, USA, pp. 977–1016.
Stouffer, R., 2006. Structure, function, and regulation of the corpus luteum. In: Neill,J.e. (Ed.), Knobil and Neill’s Physiology of Reproduction, third ed. AcademicPress/Elsevier, St. Louis, MO, USA, pp. 475–526.
Svechnikov, K., Spatafora, C., Svechnikova, I., Tringali, C., Soder, O., 2009. Effects ofresveratrol analogs on steroidogenesis and mitochondrial function in rat Leydigcells in vitro. J. Appl. Toxicol. 29, 673–680.
Svechnikova, I., Svechnikov, K., Soder, O., 2007. The influence of di-(2-ethylhexyl)phthalate on steroidogenesis by the ovarian granulosa cells of immature femalerats. J. Endocrinol. 194, 603–609.
J. Ramalho-Santos, S. Amaral / Molecular and Cellular Endocrinology 379 (2013) 74–84 83

Tavares, R.S., Martins, F.C., Oliveira, P.J., Ramalho-Santos, J., Peixoto, F.P., 2009.Parabens in male infertility-is there a mitochondrial connection? Reprod.Toxicol. 27, 1–7.
Tremellen, K., 2008. Oxidative stress and male infertility–a clinical perspective.Hum. Reprod. Update 14, 243–258.
Tuckey, R.C., Headlam, M.J., Bose, H.S., Miller, W.L., 2002. Transfer of cholesterolbetween phospholipid vesicles mediated by the steroidogenic acute regulatoryprotein (StAR). J. Biol. Chem. 277, 47123–47128.
Van Blerkom, J., 2008. Mitochondria as regulatory forces in oocytes,preimplantation embryos and stem cells. Reprod. Biomed. Online 16, 553–569.
Van Blerkom, J., 2009. Mitochondria in early mammalian development. Semin. CellDev. Biol. 20, 354–364.
Van Blerkom, J., 2011. Mitochondrial function in the human oocyte and embryo andtheir role in developmental competence. Mitochondrion 11, 797–813.
Varum, S., Momcilovic, O., Castro, C., Ben-Yehudah, A., Ramalho-Santos, J., Navara,C.S., 2009. Enhancement of human embryonic stem cell pluripotency throughinhibition of the mitochondrial respiratory chain. Stem Cell Res. 3, 142–156.
Varum, S., Rodrigues, A.S., Moura, M.B., Momcilovic, O., Easley, C.A.t., Ramalho-Santos, J., Van Houten, B., Schatten, G., 2011. Energy metabolism in humanpluripotent stem cells and their differentiated counterparts. PLoS ONE 6,e20914.
Wang, Q., Sun, Q.Y., 2007. Evaluation of oocyte quality: morphological, cellular andmolecular predictors. Reprod. Fertil. Dev. 19, 1–12.
Wang, Q., Ratchford, A.M., Chi, M.M., Schoeller, E., Frolova, A., Schedl, T., Moley, K.H.,2009. Maternal diabetes causes mitochondrial dysfunction and meiotic defectsin murine oocytes. Mol. Endocrinol. 23, 1603–1612.
Wang, Q., Frolova, A.I., Purcell, S., Adastra, K., Schoeller, E., Chi, M.M., Schedl, T.,Moley, K.H., 2010. Mitochondrial dysfunction and apoptosis in cumulus cells oftype I diabetic mice. PLoS ONE 5, e15901.
Watanabe, T., Chuma, S., Yamamoto, Y., Kuramochi-Miyagawa, S., Totoki, Y., Toyoda,A., Hoki, Y., Fujiyama, A., Shibata, T., Sado, T., Noce, T., Nakano, T., Nakatsuji, N.,
Lin, Sasaki, H., 2011. MITOPLD is a mitochondrial protein essential for nuageformation and piRNA biogenesis in the mouse germline. Dev. Cell 20, 364–375.
Wilding, M., Carotenuto, R., Infante, V., Dale, B., Marino, M., Di Matteo, L.,Campanella, C., 2001. Confocal microscopy analysis of the activity ofmitochondria contained within the ‘mitochondrial cloud’ during oogenesis inXenopus laevis. Zygote 9, 347–352.
Wycherley, G., Kane, M.T., Hynes, A.C., 2005. Oxidative phosphorylation and thetricarboxylic acid cycle are essential for normal development of mouse ovarianfollicles. Hum. Reprod. 20, 2757–2763.
Xu, G., Vogel, K.S., McMahan, C.A., Herbert, D.C., Walter, C.A., 2010. BAX and tumorsuppressor TRP53 are important in regulating mutagenesis in spermatogeniccells in mice. Biol. Reprod. 83, 979–987.
Yacobi, K., Tsafriri, A., Gross, A., 2007. Luteinizing hormone-induced caspaseactivation in rat preovulatory follicles is coupled to mitochondrialsteroidogenesis. Endocrinology 148, 1717–1726.
Yamamoto, C.M., Hikim, A.P., Lue, Y., Portugal, A.M., Guo, T.B., Hsu, S.Y., Salameh,W.A., Wang, C., Hsueh, A.J., Swerdloff, R.S., 2001. Impairment ofspermatogenesis in transgenic mice with selective overexpression of Bcl-2 inthe somatic cells of the testis. J. Androl. 22, 981–991.
Yan, W., Huang, J.X., Lax, A.S., Pelliniemi, L., Salminen, E., Poutanen, M., Toppari, J.,2003. Overexpression of Bcl-W in the testis disrupts spermatogenesis:revelation of a role of BCL-W in male germ cell cycle control. Mol. Endocrinol.17, 1868–1879.
Yu, Y., Dumollard, R., Rossbach, A., Lai, F.A., Swann, K., 2010. Redistribution ofmitochondria leads to bursts of ATP production during spontaneous mouseoocyte maturation. J. Cell. Physiol. 224, 672–680.
Zhang, X., Wu, X.Q., Lu, S., Guo, Y.L., Ma, X., 2006. Deficit of mitochondria-derivedATP during oxidative stress impairs mouse MII oocyte spindles. Cell Res. 16,841–850.
84 J. Ramalho-Santos, S. Amaral / Molecular and Cellular Endocrinology 379 (2013) 74–84