Metrics Matter: Use of Operational Metrics to Evaluate a ...€¦ · Metrics Matter: Use of...
Transcript of Metrics Matter: Use of Operational Metrics to Evaluate a ...€¦ · Metrics Matter: Use of...

.
About Northwell Health
The nation’s third-largest non-profit secular healthcare system, Northwell Health delivers world-class clinical
care throughout the New York metropolitan area, pioneering research at the Feinstein Institute for Medical
Research and a visionary approach to medical education, highlighted by the Hofstra Northwell School of
Medicine. The winner of the National Quality Forum’s 2010 National Quality Healthcare Award, Northwell
Health cares for people at every stage of life at 21 hospitals, long-term care facilities and 450 ambulatory
care centers throughout the region. Northwell Health’s owned hospitals and long-term care facilities house
about 6,400 beds, employ more than 10,000 nurses and have affiliations with more than 12,000 physicians. Its
workforce of over 61,000 is the largest on Long Island and the third-largest in New York City. For more
information, go to northwell.edu.
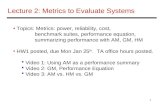
Metrics Matter: Use of Operational Metrics to Evaluate a Growing Inpatient Palliative Consultation
Service
BACKGROUND Data
Results
Conclusion
REFERENCES
• North Shore University Hospital (NSUH) is an 806-bed community teaching hospital with a robust palliative care consultation service.
• Center to Advance Palliative Care (CAPC) have developed strategies to help palliative care programs to best utilize resources for their growth, including defining metrics for palliative care programs to outline strategic data.
• To better understand and improve our services at NSUH we conducted a review of the operational metrics recommended by CAPC
Methods
• A retrospective review was conducted for all initial consultations between January 2015 and March 2016
• Data collected included demographics, top 10 ICD 9 (International Classification of Diseases) diagnoses, referring physician, service/ unit disposition, and length of hospital stay (LOS)
• All data was collected from Electronic Medial Records (EMRs).
• From Dec 2015- March 2016 there were a total of 3077 patients requiring consults
• The most common diagnoses were infection, cerebrovascular disease, malignancy, and heart failure.
• The average days from admission to consult were 2.9, while the average length of stay was 8.6 days
• 42% of patients had a routine discharge, 34% expired during the admission, 8% went to inpatient rehabilitation facilities, 7% to inpatient hospice, and 5% to home hospice
• The palliative care consult service at NSUH serves a vulnerable elderly population. Attention should be given to infections if they are a primary diagnosis on consults called after 15 and 30 days.
• Hematologic malignancies and encounters related to chemotherapy are the primary diagnoses on consults called 45 days after admission. Only 12% of patients were enrolled into hospice care. 66% of patients consulted survived the admission
• Operational metrics have helped with developing educational programs encouraging utilization of palliative care earlier in admissions. This data is also helping in planning projects to compare the impact of palliative care on LOS and ongoing work into helping providers identify hospice-eligible patients and connecting for enrollment.
Nelson J, Bassett R, Boss R, Brassel K, et al: Models for structuring a clinical initiative to enhance palliative care in the intensive care unit: A report from the IPAL-ICU Project
312
67
64
45
40
38
31
30
27
11
5
3
0 50 100 150 200 250 300 350
Sepsis
Stroke
Malignancy
Heart failure
IHC
Aspiration Pneumonitis
Renal Failure
SAH
UTI
No Diagnosis
MI
Resp Failure Top Primary ICD 9 Diagnoses
January 2015-March 2016
Mean Age >65 78% Admit to Consult>15 days 9% Consult to Disch >15 days 12%
Patient Characteristics
40%
35%
8% 6% 5%
Discharge Disposition % (Top 5)
2016
Routine Discharge Expired
Hospice Medical Facility Home Hospice
Inpatient Rehab
[VALUE]
[VALUE]
[VALUE] [VALUE] [PERCENTAG
E]
Discharge Disposition % (Top 5)
2015
Routine Discharge Expired
Inpatient Rehab Hospice Facility
Home Hospice
15.9
13.9 14.4
12.7 13.5
12.4 12.6
15
13.1 12.1
10.8
13.5 12.3 12.4
13.7
12.3
10.1 9.8
8.1 8.1 8 8.9
10.1 9.7
8.3 7.9
10.5
7.9 8.2 9.1
0
2
4
6
8
10
12
14
16
18
Jan-15 Feb-15 Mar-15 Apr-15 May-15 Jun-15 Jul-15 Aug-15 Sep-15 Oct-15 Nov-15 Dec-15 Jan-16 Feb-16 Mar-16
Admission to Discharge
January 2015-March 2016
Average Median
Santiago Lopez MD, Bridget Earle MD, Tara Liberman MD, Maria Carney MD, Marina Kushnirsky BA, Regina Roofeh MPH
Division of Geriatrics and Palliative Care
7.1 6.5
7
5.9 6.7
5.5 4.6
6.1 5.4 5.2
4.2
5.4 5.4 4.7
5.5
8.8
7.4 7.4
6.8 6.8
6.9 8
8.8
7.6 6.9
6.6
8.1
6.9 7.7
8.2
0
2
4
6
8
10
12
14
16
18
Jan-15 Feb-15 Mar-15 Apr-15 May-15 Jun-15 Jul-15 Aug-15 Sep-15 Oct-15 Nov-15 Dec-15 Jan-16 Feb-16 Mar-16
Length of Stay Data
Average Days
Admission to Consult Consult to Discharge