Medical Imaging - Universitetet i oslo · Department of Informatics UUestyoOsoniversity of Oslo...
Transcript of Medical Imaging - Universitetet i oslo · Department of Informatics UUestyoOsoniversity of Oslo...

INF GEO 4310 ImagingINF-GEO 4310 Imaging
Medical Imaging
18.11.201318.11.2013
Fritz AlbregtsenFritz AlbregtsenDepartment of Informatics
University of OsloU e s ty o Os o
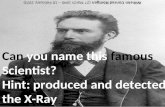
Wilhelm C Röntgen
18.11.2013 INF-GEO 4310 1
Wilhelm C. Röntgen
OverviewOverview Medical imaging coordinate system
1. X-ray medical imagingP j t d X i ia. Projected X-ray imaging
b. Computed tomography (CT) with X-rays
2. Nuclear medical imaginga. SPECTb. PET
3 Magnetic resonance imaging (MRI)3. Magnetic resonance imaging (MRI)
4. (Ultrasound imaging covered in previous lecture)
18.11.2013 INF-GEO 4310 2
( g g p )
Medical imaging coordinatesMedical imaging coordinates• The anatomic coordinate system is used• The anatomic coordinate system is used. • The three axes are referenced to the body.
– superior-inferior (S/I)
– left-right (L/R) • Note: L/R as seen from
the view of the patient !
– anterior-posterior (A/P)
18.11.2013 INF-GEO 4310 3
Medical imaging planesMedical imaging planes
• Axial plane: perpendicular to body long axisperpendicular to body long axis
• Sagittal plane:Sagittal plane: bisects the left from the right.
• Coronal plane: bisects the front from the back.
18.11.2013 INF-GEO 4310 4

Image planes: Examples:Image planes: Examples:• What are the four directions
?in a sagittal imaging plane? – ”Superior” points toward head – ”Inferior” points towards the feetp– ”Anterior” points forward– ”Posterior” points backward
• Three letters indicate the sequence• Three letters indicate the sequence and orientation of the (x,y,z)-axes of the image. – LSA means that
the a is goes from Left to right• the x-axis goes from Left to right, • the y-axis goes from Superior to inferior, • the z-axis goes from Anterior to posterior.
• CT images are LAS, while C-arm images are RPI.• What do you have to do before overlaying them?
18.11.2013 INF-GEO 4310 5
y y g
Invasive / non invasiveInvasive / non-invasiveImaging the inside of the body involves:Imaging the inside of the body involves:
• Invasive techniques:O i i id b d d [ d i id ]– Optics inside body, e.g., endoscope [gr.: endo=inside]
– Cutting into it, i.e., open surgery– Cameras in minimal-invasive surgery
• ”Camera pills” in veins or digestive tract• Non-invasive techniques (Medical imaging):
– Planar projections vs. cross-sectional images– Static images vs. dynamic series of images
18.11.2013 INF-GEO 4310 6
Different physical signalsDifferent physical signals
Non-invasive imaging (Medical imaging): 4 physical processes that generate signalsp y p g g
– Ultrasonic backscattering /reflection of wavesg– X-ray transmission
Gamma ray emission from radioisotopes– Gamma ray emission from radioisotopes– Spin precession in magnetic fields
18.11.2013 INF-GEO 4310 7
Imaging modalitiesImaging modalitiesUltrasound imaging High-frequency Back-scattering orUltrasound imaging g q y
pressure waves reflection imaging
Projection radiography j g p y(X-ray)
IonizingTransmission imaging
Computed tomography Ionizing radiation
Computed tomography (CT, C-arm)
Nuclear imagingNuclear imaging (SPECT, PET)
Emission imaging
Magnetic resonanceMagnetic resonance imaging
(MRI, fMRI)
Nuclear spinprecession
Magnetic resonanceimaging
18.11.2013 INF-GEO 4310 8

1 X ray medical imaging1. X-ray medical imaging
• Radiography:using ionizing electromagnetic radiation to image objectsg g g g j
• Radiotherapy:i i i i l t ti di ti t diusing ionizing electromagnetic radiation to cure a disease
(thus not an imaging modality)
• Ionizing radiation is also used in order to – destroy microorganisms, bacteria, viruses, or insects in food– modify plant behaviour – expose materials to achieve a technical goal.
18.11.2013 INF-GEO 4310 9
The startThe start• Radiography started in 1895: discovery of X rays• Radiography started in 1895: discovery of X-rays
by Wilhelm Conrad Röntgen (1845-1923).
Fi t bli h d i t i X i f A• First published picture using X-rays is of Anna Berthe Röntgen’s hand in the paper "Über eine neue Art von Strahlen” - 28.12.1895.
• Awarded the first Nobel Prize in Physics (1901) ”In recognition of the extraordinary services he g yhas rendered by the discovery of the remarkable rays subsequently named after him".
• X-rays were put to diagnostic use very early, before dangers of ionizing radiation were known.
18.11.2013 INF-GEO 4310 10
Energetic electrons creating X raysEnergetic electrons creating X-rays• Characteristic radiation:Characteristic radiation:
– Energetic electron collides with and ejects K-shell electronand ejects K shell electron
– K-shell ”hole” is filled by electron from L-, M-, or N-shell
– Produces characteristic spectral lines.• Bremsstrahlung: (braking /decelerating radiation)Bremsstrahlung: (braking /decelerating radiation)
– Energetic electron interacts with nucleus of atom– Deceleration causes loss of energy– Deceleration causes loss of energy– Continous spectrum,
peaking at anode-to-cathode potential18.11.2013 INF-GEO 4310 11
peaking at anode to cathode potential
Conventional X ray sourceConventional X-ray source.• Electrostatic lens to focus beam
onto a small spot on the anode
HV supplyOil-cooled
copper anodeHeated cathodeonto a small spot on the anode
• Anode designed to dissipate heat from focused electrons:
copper anode cathodeTungsten target
– Mechanically spun to increase the area heated by the beam.
– Cooled by circulating coolant. Focussed
electron beamX-ray Thin
window
• Anode angled to allow escape of some of the X-ray photons which are emitted essentially
beam
perpendicular to the direction of the electron current.
• Anode is usually made of tungstenAnode is usually made of tungsten (W) or molybdenum (Mo).
• Window designed for escape of generated X-ray photons
18.11.2013 INF-GEO 4310 12
generated X-ray photons.

Image contrastImage contrast• Image contrast caused by varying
absorption in object.
• Absorption depends on atomic b Znumber Z
– Metals distinguished from tissues– Bones distinguished by high Ca-contentg y g
• Absorption grows with Z2 due to dependence of binding energy of inner electronsof inner electrons
• Absorption depends on projected mass densitymass density – Lungs and air passages form good contrast
images because of density difference.– Higher water content (e g pneumonia) easily detected
18.11.2013 INF-GEO 4310 13
Higher water content (e.g., pneumonia) easily detected
Projected X ray transmission imagesProjected X-ray transmission images• Expose object to X-rays, capture "shadow".
• Produces 2-D projection of 3-D object.• ”Shadow" may be converted to light using
a fluorescent screena fluorescent screen.
• Image is then captured on eitherphotographic film– photographic film
– phosphor screen to be "read" by laser (CR)– matrix of detectors (digital radiography).
• Projection radiography uses X-rays in different amounts and strengths depending on what body part is being imaged:– Hard tissues (bone) require a relatively high energy photon source– Hard tissues (bone) require a relatively high energy photon source.
– Soft tissues seen with same machine as for hard tissues, but a "softer" or less-penetrating X-ray beam is used.
18.11.2013 INF-GEO 4310 14
X ray detectorsX-ray detectors• Ordinary photographic film
– Very inefficient, only 1-2% of radiation stopped– Requires unnecessarily large X-ray dose to patient
• Intensifying screens on both sides of filmIntensifying screens on both sides of film– Phosphor transforms x-ray photons into light photons– Two types of luminescence
• Fluorescence: emission within 10-8 s of excitation
• Phosphorescence: emission delayed and extended
– Conversion efficiency: 5 - 20%Conversion efficiency: 5 20%
• X-ray image intensifiers (XRIIs) – Input window of aluminium or titanium– X-ray photons absorbed by phosphor– Channeled toward photocathode– Continous development ...
18.11.2013 INF-GEO 4310 15
MammographyMammography • An X-ray examination used in diagnostic screening for
breast cancer.
• Used by radiologist or surgeon before biopsy (removal of ti l f i ti ) l t (tissue sample for examination) or lumpectomy (surgery to remove e.g. a tumor).
• Radiation used for mammography tends to have a lower• Radiation used for mammography tends to have a lower photon energy than that used for bone & harder tissues.
• Globally breast cancer is the most lethal form of cancer• Globally, breast cancer is the most lethal form of cancer for women (106 cases/yr).
• US and Canada has highest incidence rate (100 perUS and Canada has highest incidence rate (100 per 100.000), but low mortality rate (19 per 100.000).
• Norway: incidence rate 75 per 100.000, mortality 16.18.11.2013 INF-GEO 4310 16
Norway: incidence rate 75 per 100.000, mortality 16.

True / False positives / negativesTrue / False positives / negativesE g testing for cancer• True positive (TP):
Patient has cancer and test result is positive. TPTN
E.g., testing for cancerNo cancer | Cancer
• True negative (TN):A healthy patient
and a negative test result.
• False positive (FP):Healthy patient that gets a positive test result.
• False negative (FN):Cancer patient that gets a negative test result.
FN FP
• Good to have: TP & TN• Bad to have: FP (but this will probably be detected)• Worst to have: FN (may go un detected)18.11.2013 INF-GEO 4310 17
• Worst to have: FN (may go un-detected)
Sensitivity and specificitySensitivity and specificity• Sensitivity:• Sensitivity:
the portion of the data set that tested positive out of all the positive patients tested:
• Sensitivity = TP/(TP+FN) TPTN• Sensitivity = TP/(TP+FN)• The probability that the test is positive
given that the patient is sick.
• Higher sensitivity means that• Higher sensitivity means that fewer decease cases go undetected.
• Specificity:th ti f th d t t th t t t d tithe portion of the data set that tested negative out of all the negative patients tested:
• Specificity = TN/(TN+FP)Th b bilit th t t t i ti
FN FP
• The probability that a test is negative given that the patient is not sick.
• Higher specificity means that fewer healthy patients are labeled as sick
18.11.2013 INF-GEO 4310 18
fewer healthy patients are labeled as sick.
ROC curvesROC-curves• Plot of sensitivity vs (1-specificity)
for a binary classifier, as parameters vary.
• An equivalent presentation is to plot – true positive rate vs false positive rate.
• Best possible method would give a point in upper p g p ppleft corner of plane– 100% sensitivity and specificity represents
the perfect classification.p
• Result equivalent to random guessing would lie on the diagonal.
• Sensitivity and specificity are not affected by the prior probabilities of the classes.
18.11.2013 INF-GEO 4310 19
Positive and negative prediction valuesPositive and negative prediction values• Positive prediction value (PPV)
TPTN
– The probability that a patient is sick, given that the result of the test was positive:
• PPV = TP/(TP+FP)• Negative prediction value (NPV)• Negative prediction value (NPV)
– The probability that a patient is not sick, given that the test result was negative:• NPV= TN/(TN+FN)( )
• Assume a classifier with sensitivity = specificity = 0.99, and unequal class probabilities (PN =TN+FP=0.9, PP = TP+FN=0.1)
FN FP
=> 92% probability of a positive result being correct (PPV = 0.92), 0.1% probability of a negative result being wrong (NPV = 0.999)
• For sensitivity = specificity = 0 9 and (PN = 0 9 PP = 0 1)For sensitivity specificity 0.9, and (PN 0.9, PP 0.1) – there is only a 50% probability of a positive result being correct,
but still just a 1.2% chance of a negative result being wrong.
18.11.2013 INF-GEO 4310 20

FluoroscopyFluoroscopy• A technique that provides real-time images. q p g• x-ray source – patient - fluorescent - recorder. • X-ray image intensifier (XRII)
– Cesium iodide phosphorus deposited directly on XRII photocathode.
– Output image approximately 105 times brighter than input image.Output image approximately 10 times brighter than input image. • flux gain (amplification of photon number) ≈ 100• minification gain (from large input onto small output screen) ≈ 100
quantum noise (small number of photons) limiting image quality– quantum noise (small number of photons) limiting image quality.• Flat-panel detectors
– increased sensitivity to X-rays, reducing patient radiation dose. y y , g p– Improved temporal resolution, reducing motion blurring. – Improved contrast ratio over image intensifiers.
Spatial resolution is approximately equal18.11.2013 INF-GEO 4310 21
– Spatial resolution is approximately equal.
C armC-arm• A portable fluoroscopy machine that p py
can move around the surgery table and make digital images for the surgeon.
• A limited number of projections is often used to reconstruct a 2-D ”slice”
through the 3-D volume.
• High density objects (e g a needle)High density objects (e.g. a needle) or density gradients may create disturbing fan-shaped artifacts.
• These may be removed later.
18.11.2013 INF-GEO 4310 22
Using passive contrast agentsUsing passive contrast agents• Enhanced images may be made usingEnhanced images may be made using
a substance which is opaque to X-rays• Normally part of a double contrast technique,Normally part of a double contrast technique,
using positive and negative contrast. • Positive radiographic contrast agents: os t e ad og ap c co t ast age ts
– Iodine (Z=53) can be injected into bloodstream– Barium (Z=56) ( )
• Negative radiographic contrast agents: – air and carbon dioxide (CO2). ( 2)– CO2 is easily absorbed and causes less spasm. – CO2 can be injected into the blood, air must not!
18.11.2013 INF-GEO 4310 23
AngiographyAngiography • Blood has the same X-ray density as surrounding tissue.y y g• An iodine-based contrast is injected into the bloodstream
and imaged as it travels around.• Angiography is used to find
– Aneurysms (abnormal swellings of artery or vein), – Leaks– Leaks, – Thromboses (blood-clots that may cause obstruction of vessel), etc
• The X-ray images may be – Still images, displayed on a fluoroscope or film. – Video sequences (25-30 frames per second)
Retinal angiography is also commonly performed to• Retinal angiography is also commonly performed to identify vessel narrowing in patients with e.g. diabetic retinopathy and macular degeneration.
18.11.2013 INF-GEO 4310 24
p y g

Digital subtraction angiographyDigital subtraction angiography• Angiography images: made while injecting contrast medium
into the bloodstreaminto the bloodstream. – Image includes all overlying structures besides the blood vessels. – Useful for determining anatomical position of blood vessels.
To remove distracting structures and a mask image of the same• To remove distracting structures and, a mask image of the same area is acquired before contrast medium is administered.
• An image intensifier (fluoroscopy) is used, producing images at a rate of 1 - 6 frames per second subtracting all subsequent imagesrate of 1 - 6 frames per second, subtracting all subsequent images from the original 'mask' image in real time.
• Hence the term 'digital subtraction angiography' (DSA)'digital subtraction angiography' (DSA).
• DSA is being used less and less. • It is being taken over by CT Angiography• It is being taken over by CT Angiography,
which is less invasive and stressful .
18.11.2013 INF-GEO 4310 25
Reconstruction from projectionsReconstruction from projections• A 3-D object distribution can be mapped j pp
as a series of 2-D projections.• With a sufficient number of projections the mapping
b i t d d th 3 D di t ib tiprocess can be inverted and the 3-D distribution reconstructed from the projections.
• If the projection axes lie in a plane the reconstructionIf the projection axes lie in a plane, the reconstruction may be carried out one slice at a time.
• Then the inversion is simpler and may be done using a Fourier method.
• To avoid a large matrix, a ML method is used and the solution is found by iterationand the solution is found by iteration.
• The mathematical foundation was made by Johann Radon in 1917.
18.11.2013 INF-GEO 4310 26
y
CT historyCT history• CT (Computed Tomography) is an imaging technique ( p g p y) g g q
described by Cormack in 1963.
• First clinical implementation made by Hounsfield in 1972First clinical implementation made by Hounsfield in 1972.
• 1971 prototype made 160 parallel readings in 180 angles, with each scan taking five minuteswith each scan taking five minutes.
• Image reconstruction from these scans took 2.5 hours
• Hounsfield and Cormac shared the 1979 Nobel Prize.
• CT is also called CAT (Computed Axial Tomography) as it gives axial sections of the body.
18.11.2013 INF-GEO 4310 27
Reconstruction radiographyReconstruction radiography• CT uses X-raysCT uses X rays.• Instead of a 3-D cone beam,
they are collimated to travelthey are collimated to travelin a 2-D ”fan-beam”.A 2 D j ti f ti f th b d i• A 2-D projection of a cross section of the body is detected by a large number of detectors.
• Repeated for many orientations as the X-ray tube and the detectors rotate around the patient.
• An image of the cross-section is then computed from the projections.
18.11.2013 INF-GEO 4310 28
p j

Tomographic reconstructionTomographic reconstruction• Data series collected as integrals
at position r across a projection at angle θat position r, across a projection at angle θ.
• Repeated for various angles.
T t l tt ti i i b li i t lryx
dsyxrp
sincos
),(),(
• Total attenuation is given by line integral:
• This is Radon transform of the 2-D object. dxdyryxyxrp )sincos(),(),(
• Projection-slice theorem:– Using infinite number of projections,
we could perfectly reconstruct original object.
• Inverse Radon transform give us μ(x,y)• Unstable with respect to noisy data. • A stabilized and discretized version is usedA stabilized and discretized version is used,
– “filtered back projection algorithm”.
18.11.2013 INF-GEO 4310 29
Three CT modalitiesThree CT modalities• A single-slit CT is the simplest modality.g p y
– Gives a single axial-plane image– In axial ”step and shoot”, the table is moved between each slice.
I h li l CT th X t b d th d t t t t• In helical CT, the X-ray tube and the detectors rotate, while the patient is moved along an axis through the center of rotation.– Rapidly acquires 3-D data– Slightly lower z-axis resolution than ”step and shoot”.
M tilt d t t ±30° l ti t th i f t ti– May tilt detector ±30° relative to the axis of rotation.• In multislice CT, several rows of detectors gather a cone of
X-ray data, giving a 2-D projection of the 3-D patient.X ray data, giving a 2 D projection of the 3 D patient.– With 1-3 revolutions per second, near real-time 3-D imaging is
possible, with translation speeds up to 20 cm per second.
18.11.2013 INF-GEO 4310 30
CT advantagesCT advantages• CT eliminates superimposition of p p
structures outside ROI.• Small differences in physical
d it b di ti i h ddensity can be distinguished.• CT data can be viewed as images
– in an axial plane– in an axial plane – In a coronal plane – In a sagittal plane – (multiplanar reformatted imaging).
• CT angiography avoids invasive insertion of an arterial catheter and guide-wirecatheter and guide-wire
• CT colonography is as useful as a barium enema X-ray for detection of tumors, but may use lower radiation dose.
18.11.2013 INF-GEO 4310 31
y
CT disadvantagesCT disadvantages• CT is a moderate to high radiation diagnostic technique.
– Improved radiation efficiency => lower doses– Higher-resolution imaging => higher doses
M l t h i hi h d– More complex scan techniques => higher doses.
• Increased availabilityIncreased availability + increasing number of conditions
= large rise in popularity.
• CT constituted 21% of 4.3 million radiologic examinations in Norway in 2008 (dental X-ray not included).y ( y )
• Contributed 80% of total collective medical X-ray dose.• Overall rise in total amount of medical radiation used,
despite reductions in other areas18.11.2013 INF-GEO 4310 32
despite reductions in other areas.

Contrast agent disadvantagesContrast agent disadvantages• A certain level of risk associated with contrast agents. • Some patients may experience severe allergic reactions.• Contrast agent may also induce kidney damage.
If normal kidney function contrast nephropathy risk negligible– If normal kidney function, contrast nephropathy risk negligible – Risk is increased with patients who have
• preexisting renal insufficiency (kidney failure)pree isting diabetes• preexisting diabetes
• reduced intravascular volume.
For moderate kidney failure use MRI instead of CT– For moderate kidney failure, use MRI instead of CT. – Dialysis patients do not require special precautions
• little function remaining• further damage not relevant• further damage not relevant• dialysis will remove contrast agent.
18.11.2013 INF-GEO 4310 33
3 D rendering3-D rendering• Surface renderingg
– Threshold value chosen by operator (e.g. corresponds to bone). – A threshold level is set, using edge detection algorithms.
From this a 3 dimensional model can be displayed– From this, a 3-dimensional model can be displayed. – different thresholds and colors may represent
• bone, muscle, and cartilage (Norw. “brusk”). – interior structure of each element is not visible in this mode– will only display surface closest to viewer.
• Volume rendering– transparency and colors are utilized
• bones could be displayed as semi-transparent• one part of the image does not conceal another.
18.11.2013 INF-GEO 4310 34
Rendering exampleRendering example• Slices of a cranial CTSlices of a cranial CT
scan (extreme right). • Blood vessels are brightBlood vessels are bright
due to injection of contrast agent.
• Surface rendering shows high density bones.
• Segmentation removes the bone, and previously concealed vessels can now be demonstrated.
18.11.2013 INF-GEO 4310 35
2 Nuclear medical imaging2. Nuclear medical imagingWe need to generate contrast by local activityWe need to generate contrast by local activity.1.We inject a radioisotope carried by a molecule
which is absorbed differentially according towhich is absorbed differentially according to local metabolic rate.
2.Most of the radiation from the decay should yescape the body without attenuation or scatter.
3.Half-life of decay should match duration of dprocedure.
• SPECT involves high patient dose, gives poor spatial resolution but exceptional contrastspatial resolution, but exceptional contrast.
• PET solves most of SPECTs shortcomings, but procedure is more complex and expensive.
18.11.2013 INF-GEO 4310 36
procedure is more complex and expensive.

Single photon emission computed tomography (SPECT)Single photon emission computed tomography (SPECT)
• Mostly used for study of blood-flow y y(Injection, ingestion or inhalation of radiopharmaceutical)
• Image obtained by gamma camera is a 2-D view of 3-D distribution of a radionuclide.
• SPECT imaging is performed by using a gamma cameraSPECT imaging is performed by using a gamma camera to acquire multiple 2-D images.
T hi t ti i ld• Tomographic reconstruction yields 3-D dataset.
• From this dataset we may show thin slices along any chosen axis
i il t MRI CT PET18.11.2013 INF-GEO 4310 37
– similar to MRI, CT, PET.
Choice of radioactive isotopeChoice of radioactive isotope • Radiation from decay should escape body
– eliminates alpha radiation• Minimal scatter, to make good images
– eliminates beta radiationeliminates beta radiation• Energy deposition should be minimal
– eliminates gamma emission below 70 keV
• Half-life to match duration of procedure.• Short half-life to minimize radiation dose.
=> radioactive isotope with – gamma half-life ≈ 103 s, energy ≈ 105 eV.
=> 99Tc produced by β decay of 99Mo=> 99Tc, produced by β-decay of 99Mo, produced in nutron-induced fission of 235U or produced by neutron absorption by 98Mo.
18.11.2013 INF-GEO 4310 38
p y p y
SPECT camerasSPECT cameras• SPECT images are collected by rotating pinhole g y g p
gamma camera around the patient.
• Projections are acquired at defined points during the• Projections are acquired at defined points during the rotation, typically every 3-6 degrees.
»
• A full 360 degree rotation gives optimal reconstruction.– 15 – 20 seconds per projection. – Total scan time of 15-20 minutes– Total scan time of 15-20 minutes.
• Multi-headed gamma cameras give faster acquisition.– Dual-head camera give 2 projections simultaneously– Triple-head cameras with 120 degree spacing are also used.
18.11.2013 INF-GEO 4310 39
SPECT reconstructionSPECT reconstruction• Images have low resolution (64x64 or 128x128 pixels).g ( p )• Pixel sizes ranging from 3-6 mm.
• Reconstructed images compared to planar images:• Reconstructed images compared to planar images:– lower resolution, increased noise, reconstruction artifacts.
U di t ib ti f lid l tif t• Uneven distribution of nuclids may also cause artifacts. – extensive streaking of the images.
• Attenuation gives underestimation of activity with depth. – Modern SPECT equipment integrated with X-ray CT scanner.
• CT images are attenuation map of tissues• CT images are attenuation map of tissues• Incorporated into the SPECT reconstruction to correct for attenuation.
– Co-registered CT images provide anatomical information.
18.11.2013 INF-GEO 4310 40

Positron emission tomography (PET)Positron emission tomography (PET)• A sugar (fluorodeoxyglucose, FDG) suga ( uo odeo yg ucose, G)
containing radioactive 18F is injected.
• During decay, isotope emits positron.• Positron annihilates with an electron.
• This produces a pair of gamma photons moving in exactly opposite directionsmoving in exactly opposite directions.
• Gamma photons are detected by scanning device.
• Only simultaneous pair of photons d f i t ti
18.11.2013 INF-GEO 4310 41are used for image reconstruction.
PET examplesPET examplesMaximum intensity projection of typical full body 18F FDG
PET scan of human brainyp y
18.11.2013 INF-GEO 4310 42
Orthogonal PET slicesOrthogonal PET slices
18.11.2013 INF-GEO 4310 43
Shift in PET application areasShift in PET application areas
Main PET Application Areas
t d
Main PET Application Areas
i th 90 todayin the 90s
Cardiology: disorders of the heart and blood vesselsOnclology: Tumors (cancer)Neurology: the nervous system
18.11.2013 INF-GEO 4310 44
eu o ogy e e ous sys e

Oncology: Lung caseOncology: Lung case55-year-old female. Diagnosed with
stage III Lung Non-Small Cell
• Traditionally, lung masses evaluated with X-rays, CT.
stage III Lung Non Small Cell Carcinoma (NSSC).
y• More recently, MR.• To determine malignancy: g y
biopsy and thoracotomies have been performed.
• Now, PET can determine malignancy simply and non invasivelynon-invasively. PET Findings: Increased uptake of
FDG in several lung nodules indicates recurrent tumor. Abnormal uptake in
18.11.2013 INF-GEO 4310 45
ecu e u o b o a up a ethe cervical lymph nodes also evident.
PET benefitsPET benefits• Principal benefit of PET/FDG is its• Principal benefit of PET/FDG is its
sensitivity in imaging metabolic activity. • Spatial information
– better than SPECT, worse than CT or MRI.,• PET images may be fused with CT X-ray
th ti t– on the patient – at the same time– in the same machine.=>functional + anatomical image
18.11.2013 INF-GEO 4310 46
>functional + anatomical image
PET limitationsPET limitations• PET scanning uses short half-life isotopes
– 11C (~20 min), 13N (~10 min), 15O (~2 min), and 18F (~110 min).
• Timing limitations restrict clinical PET to tracers withTiming limitations restrict clinical PET to tracers with – 18F, which can be transported some distance
• Frequent recalibration of remaining dose of 18F needed.
• Ethical limitations to injecting radioactive material– short-lived radionuclides minimize radiation doseshort lived radionuclides minimize radiation dose– in cancer therapy, risk from lack of knowledge may be
much greater than the risk from the test radiation.
• Isotopes must be produced in a cyclotron (=>high costs).
18.11.2013 INF-GEO 4310 47
3 Magnetic resonance imaging3. Magnetic resonance imaging• Non invasive method based on nuclear magnetic resonance• Non-invasive method based on nuclear magnetic resonance.
• Images pathological or other physiological alterations
• First utilized in physical and chemical spectroscopy.
• 1971: MRI first demonstrated on test tube samples.1971: MRI first demonstrated on test tube samples.
• 1973: First image published.
• 1977: First image of human published.
• 1987: Magnetic resonance angiography demonstrated.
• 1992 Functional MRI (fMRI) developed.
18.11.2013 INF-GEO 4310 48

MRI basicsMRI basics• Nuclei of hydrogen atoms (protons) align• Nuclei of hydrogen atoms (protons) align
either parallel or antiparallel to the magnetic field.
• Tissue is then briefly exposed to RF pulsesin a plane perpendicular to the magnetic field.
• Puts nuclei in non-aligned high-energy state.
• As protons return to alignment, they precess.
Precession generates an RF signal• Precession generates an RF signal– RF signal can be picked up by a antenna.
18.11.2013 INF-GEO 4310 49
Image formationImage formation• To image different parts of object, orthogonal B-gradients are used. • Gradients in principal axes (x, y, z) are common
– But MRI allows completely flexible orientations.
“Slice selection“ in 3D• “Slice selection“ in 3D– RF pulse + B gradient reduce spatial encoding to 2D. – Spatial encoding can then be done in 2D
or in 3D without slice selection– or in 3D without slice selection.
• Stronger gradients permits faster imaging or higher resolution– faster imaging, or higher resolution
• Faster switching of gradients permits– faster scanningfaster scanning– limited by safety concerns over nerve stimulation.
• Typical resolution is about 1 mm³
18.11.2013 INF-GEO 4310 50
yp
The T processThe T1 process• At equilibrium:
– Magnetization vector of the proton lies along direction of the applied magnetic field Bocalled the equilibrium magnetization Mo. Z t f ti ti M l M– Z component of magnetization MZ equals Mo.
– MZ : longitudinal magnetization. – No transverse magnetization MX or MYX Y
• Time constant (T1) : describes how MZ returns to equilibrium: “spin lattice relaxation time”spin lattice relaxation time
Mz = Mo ( 1 - e-t/T1 )
• T1 : time to reduce the difference between the longitudinal magnetization (MZ) and its equilibrium value by a factor of e.
18.11.2013 INF-GEO 4310 51
The T processThe T2 process• T2 : describes the return to equilibrium of the 2
transverse magnetization, MXY“spin-spin relaxation time”
tMXY =MXYo e-t/T2
Spin spin relaxation time T is time to reduce– Spin-spin relaxation time, T2, is time to reduce transverse magnetization by a factor e.
• T2 and T1 processes occur simultaneously• T2 and T1 processes occur simultaneously
• Always: T2 ≤ T1y 2 1– Mz → Mo as t → ∞ , with time constant = T1– MXY → 0 as t → ∞ , with time constant = T2
18.11.2013 INF-GEO 4310 52

Contrast enhancementContrast enhancement• T1- & T2-images don’t always show anatomy/pathology. 1 2
• Specific magnetic properties of contrast agents are used– paramagnetic contrast agent most common
• extremely bright on T1-weighted images• high sensitivity for detection of vascular tissues (e.g. tumors) • permits estimation of brain perfusion (e.g. in stroke).
– Super-paramagnetic contrast agents (e.g. iron oxide nanoparticles).
• very dark on T weighted images• very dark on T2-weighted images • used for liver imaging
– normal liver tissue retains agent; scars, tumors do not.
– diamagnetic contrast agents• (Repulsed by external magnetic field)• barium sulfate for use in gastrointestinal tract.
18.11.2013 INF-GEO 4310 53
g
Modes of MRIModes of MRI• Standard MRI
– Including several different pulse sequences(time-series of different RF pulses to manipulate M).
• Eco-planar imaging (EPI)– Each RF excitation is followed by a train of gradients with
diff t ti l didifferent spatial encoding => rapid data collection => less motion artifacts.
MR t i i i• MR spectroscopic imaging– Images other nuclei besides hydrogen (P, Na, F).
• Functional MRI (fMRI)– MR signal of blood is different depending on
oxygenation level.
18.11.2013 INF-GEO 4310 54
yg
MR angiography (MRA)MR angiography (MRA)• MRA used to image vessels to evaluate forMRA used to image vessels to evaluate for
– stenosis - abnormal narrowing – aneurysms - vessel wall dilatations, at risk of rupture.y , p
»
• A variety of techniques – paramagnetic contrast agent
– (Attracted to magnetic external field)
"flow related enhancement"– flow-related enhancement • tissue is excited inferiorly
– signal is gathered in the plane immediately superior to excitation plane
• imaging blood which has recently moved from the excited plane.
18.11.2013 INF-GEO 4310 55
Magnetic resonance spectroscopy (MRS)Magnetic resonance spectroscopy (MRS)
• MRI shows where a tumour is located.• MRS can tell how aggressive (malignant) it is.
• MRS can be tuned to different chemical nuclei. • MRS is used to investigate
– cancer (brain, breast and prostate)– epilepsy, Parkinson‘s and Huntington's.
• 5 mm thick axial MRI brain slice – (tumor at bottom right).
R d b ROI f MRS– Red box: ROI for MRS.
• Proton MRS spectrum from tumour.red peaks correspond to alanine– red peaks correspond to alanine
– generally only seen in meningiomas.
(University of Hull
18.11.2013 INF-GEO 4310 56
Centre for Magnetic Resonance Investigations)

Functional MRI (fMRI)Functional MRI (fMRI)• Changes in brain activity linked to
– Changes in blood flow and blood oxygenation
• Active nerve cells consumeActive nerve cells consume oxygen carried by hemoglobin.
• Hemoglobin is g– diamagnetic when oxygenated
• (Repulsed by external magnetic field)– paramagnetic when deoxygenated
(Att t d t ti t l fi ld)• (Attracted to magnetic external field)
• MR signal of blood depends on level of oxygenation
=> “Blood-oxygen-level dependent (BOLD) contrast”
18.11.2013 INF-GEO 4310 57
Interventional MRIInterventional MRIMRI scanner used to simultaneously guide• MRI scanner used to simultaneously guide minimally-invasive procedure
– strong magnetic radiofrequency field present
i t ti fi ld t d– quasi-static fields generated
Non-magnetic environment, instruments, and tools requiredinstruments, and tools required
• Open magnet gives surgeon better access to patient.
• Often implies lower field magnets (0.2 T)=> Decreased sensitivity.
18.11.2013 INF-GEO 4310 58
Current density imaging (CDI)Current density imaging (CDI)• Used for mapping electric current pathwaysUsed for mapping electric current pathways.
• External current is applied during MRI session.e a cu e s app ed du g sess o
• Electrical currents generate local magnetic fields.g g
• Such magnetic fields affect the phase of the gmagnetic dipoles during an imaging sequence.
• CDI uses phase information from images to reconstruct current densities within the object.
18.11.2013 INF-GEO 4310 59
CT vs MRICT vs. MRICT diff ti t hi h Z ti (b l ifi ti ) f b b d fl h• CT: differentiates high Z tissue (bone, calcifications) from carbon based flesh.
• MRI: best suited for non-calcified tissue.
• CT: may be enhanced by contrast agents containing high Z (iodine, barium).CT: may be enhanced by contrast agents containing high Z (iodine, barium). • MRI: Contrast agents have paramagnetic properties (e.g. gadolinium).
• CT: utilizes only X-ray attenuation to generate image contrast.• MRI: has a variety of properties that may generate image contrast.
• CT: usually is usually more available, faster, much less expensive.• MRI: is generally superior for tumor detection and identificationMRI: is generally superior for tumor detection and identification.
• CT: if repeated, may expose the patient to excessive ionizing radiation.• MRI: best if patient is to undergo examination several times.
18.11.2013 INF-GEO 4310 60





![Röntgen-Fluoreszenz-Analyse als effiziente Inspektions ...€¦ · 1895 durch Wilhelm Conrad Röntgen [1] erweiterte die moderne Wissenschaft ihren Kenntnisstand über das elektromagnetische](https://static.fdocuments.net/doc/165x107/5eaccd50598211434e284157/rntgen-fluoreszenz-analyse-als-effiziente-inspektions-1895-durch-wilhelm-conrad.jpg)