Mediastinal Malignant Lymphoma*€¦ · lymphoma. S ome reported series of malignant mediastinal...
Transcript of Mediastinal Malignant Lymphoma*€¦ · lymphoma. S ome reported series of malignant mediastinal...

Mediastinal Malignant Lymphoma*
lonuthan A. uan Heerden, M.B., Ch.B., Edgar G. Harrison, Jr., M.D., Philip E. Bematz, M.D., F.C.C.P., and Joseph M. Kiely, M.D.
Ninety-seven cases of mdipant lymphoma, clinically presenting in tbe mediadomu, were dhgmd by examination of smgical pathologic specimens, These specimens were aaalyzed in the light of newer concepts regarding lymphoma, hch~dhg current Elanrrification and clinical staging of these tamor& The influences of clinkal and histopatbo1ogic features and therapentic mod& tiea were assessed in regard to prognosis. FWy-seven patients bad Hodgkin's disease and 613 percent of these patients survived five years, whereas 40 patients had lymphosareomas and only 15 percent of these patients sorvived five year& Generally, matme lympbocylic predominance of lympbonum md nodnlarity, particPtarly in lympbosarcoma, were histopatbologic features that were assodated with increased survival. Nodular sclerosis was noted in 35 of the patients and mixed cellular@ in 19, and these patients had favorable snrvival rates. Thirteen of the 15 patients with lymphoma of stage I survived five year& Five of the six patients with thymic HodgWs disease treated by surgical excision and roentgen therapy survived five years or more. Radical surgery has a distinct place in the therapy of selected patients with medinstinal lymphoma.
ome reported series of malignant mediastinal S tumors do not include malignant lymphoma (such as lymphosarcoma, lymphoblastoma, reticu- lum cell sarcoma, and Hodgkin's disease) because of the often-held belief that these tumors are usual- ly part of a systemic process.14
The medical literature of the last 30 years or more is filled with codicting statements in regard to malignant lymphoma. Controversy exists as to histologic classification and nomenclature, clinical staging, treatment, and eventual prognosis. Dog- matic statements exemphfy the diverse opinions of many authorities.
"An almost unparalleled profusion of terms has been provoked by the unique diversity of the clini-
'Ma o Clinic and Mayo Foundation: Section of Surgical patiology (Dr. Harrison), of Surgery (Dr. Bernatz), and of 'Medicine (Dr. Kiely). Mayo Graduate School of Medi- cine (University of Minnesota), Rochester: Resident in Surgery (Dr. van Heerden). Presented at the 35th Annual Meeting, American College of Chest Physicians, Chicago, October 29-November 2, 1969.
cal and morphologic features of Hodglun's di~ease."~ Easson5 has said that a general attitude of
pessimism, based on the idea that Hodgkin's disease is incurable, exists and that "This attitude encour- ages the pernicious policy of pessimism, pills and procrastination."
Hall and Olson6 in 1956 stated: "The physician who manages a patient with a malignant lymphoma is faced with the problem of whether the histologic diagnosis made by the pathologist has any signifi- cance other than to establish the diagnosis of a malignant lymphoma."
Despite this confusion and former general atti- tude of pessimism, the field of malignant lymphoma is today one of dynamic change. Great strides are being in all facets of this disease, especial- ly in the clarification of histopathologic features and clinical staging as these relate to prognosis, and in the critical evaluation of newer forms of treat- ment.
This study of mediastinal lymphoma was thus stimulated, and undertaken, with five aims in mind:
Downloaded From: http://journal.publications.chestnet.org/pdfaccess.ashx?url=/data/journals/chest/21496/ on 06/26/2017

MEDl ASTINAL MALIGNANT LYMPHOMA
1. To present the clinicopathologic features of malignant lymphoma clinically presenting in the mediastinum and diagnosed in surgical pathology at the Mayo Clinic during a leyear period (1950 through 1961 ) .
2. To utilize a classification of malignant lym- phoma based on newer concepts regarding their histopathologic features.
3. To evaluate the influence of clinical staging on prognosis.
4. To evaluate the influence of histopathologic features on prognosis.
5. To assess the influence of treatment on prog- nosis and to determine, if possible, whether resec- tion is a useful mode of therapy in certain selected patients.
Age and Sex: In our experience malignant lymphoma is a disease particularly of the second, third, and fourth decades of life, with a slight female preponderance. In our study, there were 1.3 times more females than males: 55 females (average age 36.1 years) and 42 males (average age 37.2 years), with an overall average age of 36.9 years (average with lymphosarcoma was 38 years, while average with Hodgkin's disease was 35.4 years). The youngest patient in our series was a 5-year-old boy, and the oldest was a 79- year-old man.
The age and sex distribution of the patients with lymph- oma of various cell types is shown in Table 1. In the mediastinum, the mixed type of Hodgkin's disease ("granu- loma") is a disease of young females, as evidenced by the male-to-female ratio of about 1:2.4; in the nodular sclerosis type, the ratio was 1:1.4 in our 35 cases (Table 1). The only other noticeable (but not statistically significant) sex difference was found in the group with immature lympho- cytic (lymphoblastic) lesions and the group with mature lymphocytic lesions in which males predominate in a ratio of about 2:l (Table 1).
Clinical Presentation: The mode of presentation was diverse although all patients had mediastinal involvement noted as part of their initial manifestation of lymphoma; the presenting symptoms and signs are listed in Table 2. Twenty-six patients (26.8 percent) were entirely asympto- matic. In 13 of these, the mediastid mass was d i m 4 on routine roentgenographic examination of the chest, and
Table 1-Age and Sex Distribution of 97 Patients With Malignant Mediastinal Lymphoma According to
Histopathologic Type
Age Range, Lesion Males Females Yr
Lymphosarcoma Mature lymphocytic 4 1 9 to 61 Immature lymphocytic 13 6 5 to 79 Mixed 6 4 32 to 61 Reticulum cell 2 4 2Oto49
Hodgkin's disease Lymphocytic predominance 1 2 14to40 Mixed cellularity 5 14 9 to69 Nodular sclerosis 10 25 16 to 58
CHEST, VOL. 57, NO. 6, JUNE 1970
Table %Presenting Symptom and Signs in 97 Cases of Mediasfid Lymphoma
Sign or Symptom No.
Asymptomatico 26 (26.816) Q u g b 30 Pain 27 Fever 13 Dyspnea 12 Loss of weight 12 Palpable nodes ) 18 Fatigue 6 Pruritus 5 Dysphgia 5 Change in voice 3 Feeling of strangulation 2 Palpitations, hemoptysis, herpes zoster leach
'Mass discovered on routine roentgenogram in 13 patients. t S d e n e or suprasternal region; five patients were s y m p b matic.
13 presented with asymptomatic involvement of adjacent supraclavicular lymph nodes. In the total group, scalene or suprasternal lymph nodes were palpable in 18 (18.6 percent) patients, although positive nodes were found on scalene biopsy in 35 cases.
The recent onset of coughing (30.9 percent) and retroster- nal pain (27.8 percent) were common presentations, while loss of weight, dyspnea, and irregular bouts of unexplained fever were prominent but less frequent. No instance of documented Pel-Ebstein fever was found. Pruritus of gen- eralized distribution was present in five patients, all of whom had Hodgkin's granuloma; in these five patients, pruritus had been a disturbing symptom for periods that varied from five weeks to two years prior to the estab- lishment of the diagnosis of Hodgldn's disease. On the average, symptoms had been present for less than three months prior to definitive diagnosis (ranging from one week to two years).
Retrosternal pain after the ingestion of alcohol12 was present in a 37-year-old woman in ow series. A nodular sclerosing type of Hodgkin's disease of the anterosuperim mediastinum was completely resected, and her retrosternal pain promptly disappeared. However, she died of recurrent intrathoracic disease 18 months later. Loss of weight (10 to 20 Ib) occurred in about a third
of the patients, but the loss did not seem to be related to a decrease in appetite, which often remained hearty.
Thirty of our patients had systemic symptoms, for exam- ple, fever, loss of weight, and pruritus, whereas 67 had symptoms referable only to their mediastinal disease, as cough, feeling of pressure, pain, mild dysphagia, and rarely hoarseness.
One of our patients presented with severe herpes zoster, which had been recurring for 12 months. Her condition was diagnosed as extensive lymphoblastic mediastinal lymphoma, from which she died two months after biopsy. Biche1,la after analysis of 240 cases of malignant lymphoma, reported 11 of associated herpes zoster. He implied that the praence of this condition in a patient with a malignant lymphoma indicated impending involvement of the epidural space by the malignancy.
Two patients in this study underwent bone marrow examination; results of the examinations were normal. Fifty- five patients had peripheral blood smears examined. The most common anomaly was rouleau formation (38.2 per-
Downloaded From: http://journal.publications.chestnet.org/pdfaccess.ashx?url=/data/journals/chest/21496/ on 06/26/2017

VAN HEERDEN ET AL
cent). A hmgbbh level of less dLan 10 gm/100 ml of bbodwasnotsdinonlyfontofour~ta
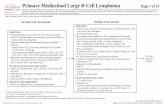
Plafn chert m- wcm the h g l e most im- PortantdialprostlcmeCbodAmnmghnochPracteristicpat- t e r n w a 6 f d a t y p i c a l ~ ~ c e o f a mediartinsl lymphma ia awn in Figum 1A and B; the dspedmanfmn*patiemt3aslUJwninFigurelC.
W e h . v e u t i J i m d a d & o f t h e ~ o f Peten and M i d d h b and that praposed at the "Sym- posium on Hodgkin's Disease Staging in %pbmber, 1068 (Table 3).8.1134 This dadication has a dinical and a ~ c a l p a t b d o g i c b a s i s a n d ~ b a n t y p s r d lymphama- In tbir study, 15 ladom wem stage I, 31 mm stnge 111,
a n d 5 1 ~ e r e ~ I I ~ h ~ n 0 h d s t a g e I I I since we did not include disseminatsd dlsesse in our study.
T b e m a j d ~ d p a ~ h a d ~ i n t h e m t e r c t only one p a t h t m t e d a primary
posteriol n d a s t i d mass, and caused r#rme diag- wetic - mg 2).
The problem of dassifylng mahgnant lymphoma arises
FIGURE I. Antampsterior (A) and lateral (B) views of cheat, depicting large anterior mdiastinal mass. C, Gross sped- ab lymphomatoua maw (~odgldn's nodular s c l d ) resectsd from anterim *urn. Note h e noduhity of cut sur- faoes.
from a lack of general agreement among pathologists re- garding classification and because histologic similadties ba tween categories may make dear-cut diffemdatb in some cases exhmdy diilicult. In this study, we adhered closely to a modi6cation of Rappaport'so and Lukes'll classi- fications (Table a), including the proposals of the Committee on Nomenclature of 1966,14 in Rye, New Yo&. The histo- pathologic types encountered in this study are shown in Figurea 3 through 8. Temnidy, Hodgkin's disease with lymphocytic depletion ("sarcoma") was'* at autopsy in one patient who had had a mixed d u h i t y type in the
Table 3-Clinical Staging of MediruPind Lpphoma
Stage I0 Limited to medhtinum
Stage 11. 1. Limited to two umtiguous anatomic lym- phatic reg&ms (including lymph nodea aad thymus)
2. In mom than two anatomic regians above tbe diaphragm induding lymph nodes, thy- mus, pleura, lung, and pericardium
Stage 111° Involvement below diaphragm or distant in-
'Subgmup A with and sub- B without systemic symp tions.
CHEST, VOL. 57, NO. 6, JUNE 1970
Downloaded From: http://journal.publications.chestnet.org/pdfaccess.ashx?url=/data/journals/chest/21496/ on 06/26/2017

MEDl ASTlNAL MALIGNANT LYMPHOMA
I" F~GURE 2. Sites of primary mediastinal lymphoma (97 cases).
mediastinum. The histopathologic distribution of our present series is
shown in Table 5. This table lists the number of cases in which the lesion was predominantly nodular or follicular, as well as the number of cases of Hodgkin's nodular sclerosis. A "stany-sky" appearance, due to histiocytic phagocytosis,la was present in one case only, that of an immature lymphmytic (lymphoblastic) mediastinal lymphoma.
The surgical procedures employed in this series are
Table 4-Histopathologic C l a d j k t h of Malignant Lymphoma
"Lymphosarcoma" types (nodular-"foUi*--or diEuse) 1. Mature lymphocytic 2. Immature lymphocytic (lymphoblastic) 3. Mixed (lymphocytic and reticulum cell) 4. Reticulum cell (histiocytic and stem cell)
Hodnkin's disease - 1. Lpphmytic p r e d o m i n a n d u l a r or ditruse
( paragranuloma" or lympbohistiocytic) 2 Nodular sclerosis 3. Mixed cellularity+Mwe ("granuloma") 4. krm&ocytic deqlm- ("sarcoma," reti&
se fibrosls
CHEST, VOL. 57, NO. 6, JUNE 1970
Table 5-Dietribution of H w t h d o g i c Type8 in 97 Caeer of Malignant Lymphoma of the Medbrtinum
Type No.
lymphocytIc Nodular DifFuse
Immature lymphocytic (kphoblastic") 19 Nodular 4 Diffuse 15
Mixed type (lymphcytic and reticulum dl) 10 Nodular 3 Diffuse 7
Reticulum cell DifhLse
Hodgkin'sdisease Lymphocytic predominanca (diihse) Nodular sclerosis Mixed cellularity (diffuse) Lymphocytic depletion
shown in Table 6. Thoracotomy was performed in 58 pa- tients. Sixteen patients (16.5 percent) had surgical removal of all gross tumor and adjacent lymphoid tissue, and a further 40 patients had biopsy alone. The reasons for in- operability were mainly those imp& by the close confines of the mediastinum and involvement of vital structures.
Involvement of major vascular structures such as the aortic arch and superior vena cava was a commw feature of inoperability. Invasion of the pericardium or thymus, or extension beyond the mediastinum to the lung, was much less of an obstacle to resection. Variations in a surgeon's philosophy about resection of a locally extensive lymphoma in the mediastinum were important factors in tbe considera- tion of resectability of some lesions.
Palliative resections were done in five patients (two with lymphocytic lymphoamma, two with Hodgkin's nodular sclerosis, and one with Hodgkin's disease with lymphocytic predominance). In each of the five patients, involved tissue was knowingly left behind either because of the extent of anatomic involvement or because of the degree of infiltra- tion. A11 five patients survived for more than five years. The role of palliative resections will be discussed when we consider the influence of treatment on prognoeis.
Ancillary treatment to surgery was used in 94 of our 97 patients. By far the most important therapeutic method was radiotherapy to the involved areas (for example, media- stinum and supraclavicular areas) after operation or biopsy.
In this series, if supraclavicular nodes were positive, both the mediastinum and involved side of the neck were ir- radiated, and the adlla on the same side as the affected side of the neck was included in the radiation field.
Table &Surgical Procedures Employed in 97 Casss of Mediaatid L y m p h
Procedure No.
Thoracotomy and biopsy 35 Thoramtomy with curative resedlon 16 (16.5%) Thoramtomy with palliative resection 5 Supradavi& node biopsy 38 Bronchoscopy and biopsy 1 Esophagoscopy and biopsy 1 Tracheostomy 1
Downloaded From: http://journal.publications.chestnet.org/pdfaccess.ashx?url=/data/journals/chest/21496/ on 06/26/2017

FIGURE 4. Malignant hpa-c ) type, reduced from ~60 . )
VAN HEERDEN ET AL
FIGURE 3. Malignant lymphma C'bP-7. A, Ma- lymphocytic type* diffuse. (He- matoxylin and eosin; reduced from XW.) B, Immature Iym- phocrtrc mp-1 typetype, diffuse. (Hematoxyh and e&; x650.)
lymphoma. Immature nodular. (Hematoxylin
lymphocytic and eosin;
FICUR~ 5. Malignant lymphoma. A, Mixed type (lymphocytic and reticulum cell) difhrse. (Hema- toxylin and eosin; reduced from X650.) 8, Reticulum cell type. (Hematoxylin and eusin; re- duced from ~650.)
CHEST, VOL. 57, NO. 6, JUNE 1970
Downloaded From: http://journal.publications.chestnet.org/pdfaccess.ashx?url=/data/journals/chest/21496/ on 06/26/2017

MEDIASTINAL MALIGNANT LYMPHOMA
The use of nitrogem mustard was reserved in most instances for those patients with superior vena c a d ob- struction.
One of our patients has been lost to follow-up. The course of the remaining 96 patients has been evaluated with emphasis on clinical course, as well as the influence of pathologic and therapeutic aspects on prognosis.
When this study was completed, 26 patients were alive and 70 were dead (Table 7). For 54 of these 70 patients, the cause of death was well documented both clinically and by autopsy study (17 patients). It is especially noteworthy that in 29 patients the disease remained intrathoradc and caused death by local extension.
Fxcm 7. Hodgkin's disease. Nodular sclerosing type. A, Pat- tern due to advanced fibrat& surrounding nodules. (Hema- toxylin and eosin; reduced from ~ 6 0 . ) B, Center of a nodule demonstrating atypical reticu- lum cells and Reed-Sternberg cell in lacmar-like spaces. (Hematoxylin and eosin; re- duced from X440.)
T a b 7-Cawe of Death in 54 Cores of M a n a n t M e d k d d Lynphoma
ProJ3ressiv8nsediastiaal extension
Distant dbemination PulmanarV-
(radiation)
(b-t iv8dty (hemorrhage)
Hospital mortality ( r e s p W r y fan-)
UxUdabBd
. -
Deaths, Hodgkin's mmatws No. DiPeaPe Types
CHEST, VOL. 57, NO. 6, JUNE 1970
Downloaded From: http://journal.publications.chestnet.org/pdfaccess.ashx?url=/data/journals/chest/21496/ on 06/26/2017

VAN HEERDEN ET AL
FIGVRE 8. Hodgkin's dbease with depletion. (Hematoxylin and eosin, reduced from ~400.)
The single operative death in our series was that of a 64-year-old woman who presented with a large superior mediastinal mass and signs of trach- eobronchial obstruction. During bronchoscopy, un- controllable hemorrhage ensued from what at autop sy proved to be an extensive immature lymphocytic (lymphoblastic) lymphoma, which was entirely intrathoracic. Our interest in the lymphoma-to-leukemia rela-
tionship was stimulated by the inclusion in this study of a five-year-old boy who presented with fever of unknown origin of three months' duration. He had an inoperable posterosuperior mediastinal mass at thoracotomy, which was diagnosed on biopsy as an immature lymphocytic (lymphoblastic) lympho- ma. On review, both the peripheral blood smears and bone marrow at that time were normal. He received mediastinal irradiation and was virtually asymptomatic for 12 months, at which time an acute fulminating leukemia developed from which he died 13 months after the initial thoracotomy. Re- view of the peripheral smears and bone mmow at this later time revealed that the process was one of leukosarcoma-cell leukemia1@-l@
One patient, a 43-year-old woman, had under- gone radical curative resection of a primary mixed type of Hodgkin's disease of the mediastinum 12 years before her death. At autopsy, no residual lymphoma could be detected. However, extensive, severe, bilateral pulmonary radiation fibrosis was found which was believed to be the cause of the terminal right-heart failure.
In calculating and evaluating the survival curves of the patients in our series, we have adhered closely to the method of Berkson and Gage.30
The overall five-year survival rate in this series
of 98 patients with mediastinal lymphoma was 39.1 percent; the ten-year survival rate was 17.1 percent. The only ten-year survivors were patients with Hodglcin's disease of the mediastinum. The five-year survival rate of the 57 patients with Hodgkin's disease was 61.3 percent and the ten-year survival rate was 39.8 percent In our five patients with a mature lymphocytic type of lymphosarama, three lived more than five years. In both the immature lymphocytic (lymphoblastic) and the reticulum cell groups (25 patients), the survival rate was very low---only two patients survived mom than t w ~ years. Both of these survivors had immature lymph- ocytic (lymphoblastic) lesions, one showing a nod- ular pattern.
The best prognosis was found in the group of patients with Hodgkin's disease of the mediastbum. Further breakdown of this group revealed that both the five-year and ten-year survival rates of those pa- tients with Hodgkin's disease showing lymphocytic predominance ("paragranulomam) were the same; two of the three patients survived ten years. In the 19 patients with Hodgkin's disease of the mixed type ("granuloma"), the survival rates were 52.6 percent and 26.3 percent, respectively, and in the 34 with Hodgkin's nodular sclerosing type, it was 64.7 percent and 26.5 percent respectively.
Recently, CrossZ1 has suggested that all cases of nodular sclerosing Hodgkin's disease be subdivided into two groups, those of well-diEerentiated lesions and those of poorly differentiated lesions, de-
Table 8-Motphologic CeZl Types and S w d d Data in 96 Cases* of M e d h i h d Lymphoma
Survival, % No. of - . . ,
nwj Cases Syem 10-year Lymphosmma (40 cases)
Mature lymphocytic 5 60.0 0.0 Immature lymphocytic (lymphoblastic) 19 0.0 0.0 Mixed ( l y m p h o c y t i ~ ~ u m c e l l ) 10 30.0 0.0 Reticulum cell (bistiocytic and stem
ell) 6 0.0 0.0 Total 40) 15.0 0.0
Hodgkin's Disease (56 casese) Lymphocytic predominance ("~aralpanuloma") 3 68.6 88.6
Nodular sclemds 34 84.7 28.5 Mixed cdlularity ("granuloma") 19 52.6 W.3 Total 56 81.3 39.8 O v e d total 88 39.1 17.1 *One patient was loet to follow-up. +There were nine nodular ("f&&") lesioae (four patients survived five years) and 31 diffuse l~ions (only one patient survived five years). This d a m is statistically sigdcant (P < 0.01).
CHEST, VOL. 57, NO. 6, JUNE 1970
Downloaded From: http://journal.publications.chestnet.org/pdfaccess.ashx?url=/data/journals/chest/21496/ on 06/26/2017

MEDIASTINAL MALIGNANT LYMPHOMA
Years after surgery or diagnosis
Hodgkin's disease
40
\-,_L mphosarcoma 20 - -x, --.\ -. ..4/24 surviving
I I I I I (tihospital deaths)
FIGURE 0. Graphic depiction of survival according to clinical stage of mediastinal lymphoma. A, upper: Overall series. B, lower: Stage 11,.
pending on the relative number of mature lympho- cytes and the degree of anaplasia of the abnormal reticulum cells found in the follicles. He found a definite difference in survival time associated with these two groups. In evaluating our cases of Hodg- kin's nodular sclerosis, we have not been able to differentiate clearly distinct subgroups; long-term survivors were distributed evenly among these cases. The range in histopathologic composition of these nodules, and presence of early or advanced sclerosis, had little, if any, prognostic signdcance.
If we exclude the group of patients with Hodg- kin's disease and evaluate the 40 patients with lymphosarcoma in regard to the influence of nodu- larity (follicular formation) on prognosis, we find that four of the nine patients with nodular lesions survived five years and that only one of 31 patients with diffuse lesions survived five years, indicating the more favorable prognosis when the lymphosar- coma is nodular (Table 8).
The important influence of the clinical stage of the disease on prognosis has been stressed. The survival curves of the three stages are depicted in Figure 9. Ow study revealed five-year survival rates of 86.6 percent, 54.8 percent, and 19.6 percent, respectively, for all patients with mediastinal lymph- oma of stages I, 111, and 112. In the lymphosarcoma
group, there were only two patients with stage I disease, and both survived more than five years, while only three of nine with stage 111 and one of 29 with stage IIz had such survival. However, five- year survival in Hodgkin's disease was better at more advanced stages of involvement, including 11 of 13 patients with stage I disease, 14 of 22 with stage 111 lesions, and nine of 22 with stage 112 lesions.
Considering the presence of systemic symptoms (pruritus, pyrexia, loss of weight) separately, we found that 26 patients had such symptoms. Sixteen of these patients had Hodgkin's disease, and eight survived five years; of the remaining ten patients with lymphosarcoma, none survived five years. In the other 70 patients, symptoms (if they were present) were related only to the mediastinal dis- ease and its local effects (pain, pressure, and dyspnea). Forty of these patients had Hodgkin's disease, of whom 26 survived five years; of the 30 patients with lymphosarcoma, only six survived five years. Thus, the presence of systemic symptoms would seem to have a deleterious effect on progno- sis, but more so in the group with lymphosarcoma in comparison to Hodgkin's disease.
The five-year survival rate in the overall group for females was 49.1 percent, in contrast to 31.7 percent for males. There was no significant differ- ence in the survival rates by sex in Hodgkin's disease, the five-year survival rate of 41 females being 63 percent in comparison to 53 percent for 15 males. In the lymphosarcoma group, five of 25 males and one of 15 females survived five years; the difference is not statistically significant.
In evaluating the influence of age on five-year survival, we arbitrarily divided our series of patients into three age groups. In group 1, 0 to 15 years of age, there were eight patients and two survived five years; both of these survivors had Hodgkin's disease. Of the remaining six patients who died, five had lymphosarcoma and one had Hodgkin's disease. In group 2, 15 to 50 years of age, there were 68 patients; 34 survived five years. Survivors included four of 22 patients with lymphosarcoma and 30 of the 46 patients with Hodgkin's disease. In group 3, more than 50 years of age, there were 20 patients and four survived five years (two of 12 patients with lymphosarcoma and two of eight with Hodgkin's disease). Lyrnphosarcoma was as- sociated with an unfavorable prognosis at any age level and particularly in the age group 0 to 15 years in which there were no survivors. However, the prognosis in Hodgkin's disease was much more
CHEST, VOL. 57, NO. 6, JUNE 1970
Downloaded From: http://journal.publications.chestnet.org/pdfaccess.ashx?url=/data/journals/chest/21496/ on 06/26/2017

526 VAN HEERDEN ET AL
favorable in the younger age groups, while in the age p u p more than 50 years old it was associated with a poor prognosis.
Sixteen of our patients underwent radical cura- tive-type resection of their mediastinal lymphoma, after which roentgen therapy was given (Table 9). Of these patients, one had Hodgkin's disease with mixed cellularity ("granuloma"), 13 had Hodgkin's nodular sclerosis, one had mixed-cell lymphosar- coma (lymphocytic and reticulum cell), and one had a reticulum cell lymphosarcoma. Thirteen of the 16 survived five years whereas seven of the 16 d v e d ten years. In only one patient (nodular sclerosis) of the six patients who died, the disease became disseminated, whereas in the remaining five patients, the disease remained within the thorax.
In six patients in this series, the thymus was involved by mediastinal lymphoma of the Hodgkin's nodular sclerosis type. It was apparently invaded secondarily in four patients, while in two, the lymphoma appeared to be primarily thymic in origin. The latter patients were women in their early forties. In both women, total surgical extirpa- tion was possible by thymectomy, after which radio- therapy was given. One of these patients died four years later of extensive mediastinal recurrence, whereas the second patient was alive and well 15 years 9 months later. Five of the six patients survived five years.
Although lymphoma is often a multicentric pro- cess, the disease may be confined to the media- stinum and cause death from the local infiltration
or compression of intrathoracic structures. When noted on the routine chest roentgenogram of an asymptomatic patient, the lesion often is localized in the mediastinum and ame~able to aggressive treatment.
It is noteworthy that of the 54 patients in whom the cause of death was ascertained, only 17 died of disseminated disease, and 13 of these deaths were of patients in the lymphosarcoma group. In 29, the disease remained within the thorax and death was due to respiratory failure as a result of tracheobronchial compression and parenchymatous lung involvement, or cardiac tamponade as a result of compression, or direct infiltration of the pericar- d im. Hodgkin's disease particularly extends more often to adjacent regions, whereas lymphosarcoma more often tends toward disseminated disease. This has special significance for the surgeon contemplat- ing the management of mediastinal lymphoma.
Clinical presentation of mediastinal lymphoma is seldom delayed-this is due to the close anatomic confines of the mediastinum and the early effects of an expanding lesion. Although not used in this study, arteriography as a diagnostic tool and retro- peritoneal lymphangiography as an aid to more accurate staging should be mentioned.
Angiography and thoracic arteriography may be utilized to differentiate vascular from nonvascular lesions of the mediastinurn22 Generally, lymphan- giography does not aid in the diagnosis, but it is the most accurate method for assessment of iliac and retroperitoneal lymph nodes. The resulting staging of the disease is meaningful in tenns of treatment
Table 9-Summary of Treatment by Radical Resection and Andlury Radiotherapy in 16 Caw8 of Mediastina2 Lymphoma
Case Lesion stage Result Cause of Death
Lymphosarcoma 1 Nodular mixed I Alive, 9 yr 3 mo 2 Reticulum cell 112 Dead, 8 mo Mediastid extension
Hodgkin's Disease Mixed type Nodular sclerosis Nodular sclerosis Nodular sclerosis Nodular sclerosis Nodular sclerosis Nodular sclerosis Nodular sclerosis Nodular sclerosis Nodular sclerosis Nodular s d m i s Nodular sclerosis Nodular sclerosis Nodular sclerosis
I Alive, 8 yr 6 rno I Alive, 14 yr 11 mo I Alive, 10 yr3mo
=1 Dead 4 yr Mediastid extension 112 Dead, 11 yr 11 mo Radiation pulmonary fibrosis I Alive, 15 yr 9 mo I Dead, 1 yr 3 mo Visceral extension I Alive, 7 yr 8 mo
112 Alive,Qyr2mo 1 Alive, 10 yr
112 Alive,Qyr2mo I D e a d , l l ~ r Mediastinal extension
IT, Alive, 13 yr 2 mo 11% Dead,5yr6mo Mediastid extension
CHEST, VOL. 57, NO. 6, JUNE 1970
Downloaded From: http://journal.publications.chestnet.org/pdfaccess.ashx?url=/data/journals/chest/21496/ on 06/26/2017

MEDIASTINAL MALIGNANT LYMPHOMA
and prognosis. We currently recommend lymphan- giography in all patients with lymphoma unless general dissemination has occurred.
Prognosis: Various factors apparently d u e n c e the prognosis for patients with malignant lympho- ma. Peters2s stated that the most important aspects in the control of Hodgkin's disease were (1) early diagnosis and a more optimistic prognosis when the disease is localized; (2) proper classification of the lesion; (3) early institution of treatment; and (4) moderately intensive radiation treatment when the disease is not disseminated. Regarding malig- nant lymphoma in general one must consider (1) morphologic type (cellular composition and nodu- larity, if present); (2) clinical stage of the disease; (3) initial anatomic location; (4) age and sex of the patient; (5) mode of treatment and patient response; (6) host resistance to lymphoma and infections; and (7) continued exposure to possible inciting agent^?^
Clinical Features: The presence of constitutional symptoms (fever, loss of weight) has an adverse effect on the course of the disease. The male patient has reduced chances for survival. This difference may be related to an increased frequency of Hodgkin's disease in the female in this series, and in particular the increased frequency of the nodular sclerosing type with its more favorable outlook. In addition, Peters and co-workerss have stated that females are more likely to have localized disease. Survival of patients at the two extremes, less than 15 years old and more than 50 years old, was poor, being two of eight and four of 20, respectively, in comparison to the survival of 34 of 68 in the age group 15 through 50 years. The poor survival rate in the pediatric age group is due to the high incidence of the immature lymphocytic (lymphoblastic) type of lymphoma. In the 20 patients in this series who were 50 years old or older, ten (50 percent) had immature lymphocytic (lymphoblastic) types of lymphoma.
Staging: We agree with Peters and co-workerss who stated: ". . .the extent of the disease prior to treatment so far is the most dependable single influence in predicting the course of the disease." As was indicated in this study, the poorer prognosis in stage I1 lymphosarcoma compared to stage I1 Hodgkin's disease may be, in part, related to earlier and noncontiguous spread of the former, in addition to variations in the other multiple prognostic factors previously mentioned.
Histopathologic Features: Histopathologic cell type is an important prognostic factor. The signifi- cance of a mature lymphocytic component has been
stressed in both lymphosarcoma and Hodgkin's disease.4*s825*26 In our study, best results were found in the group of patients with Hodgkin's disease (61.3 percent five-year survival rate). With- in this group, the most favorable outcome appeared to be in the three cases of Hodgkin's disease with lymphocytic predominance ("paragranuloma"). In Hodgkin's disease the five-year survival rates in those with mixed type ("granuloma") and Hodgkin's nodular sclerosis were 52.6 percent in 19 patients and 64.7 percent in 34 patients respectively. The favorable prognosis in the nodular sclerosing group may be related to the high proportion of females in this category, and is in keeping with that found in the literature. Lymphocytic depletion ("sarco- ma"), which has a grave prognosis, is rarely encountered as primary mediastinal malignant lym- phoma. Caution must be exercised in the diagnosis of lymphocytic depletion because advanced nodular sclerosis, which commonly presents in the media- stinum, may simulate lymphocytic depletion, partic- ularly on a small biopsy specimen.27 Also, some daculty may be encountered in recognizing the very early stage of nodular sclerosis before there are well-established collagenous bands separating the nodules. In fact, in our initial review of these slides, only 16 were noted to be well-developed histopathologic examples of nodular sclerosis. How- ever, on a second review of all available biopsy sections in cases of Hodgkin's disease, an additional 18 slides were classified as showing nodular sclerosis when attention was paid to early evidence of nodu- larity with collections of atypical histiocytes or lacunar Reed-Stemberg cells. Also, small foci of necrosis were not considered conclusive evidence against the diagnosis of nodular sclerosing Hodg- kin's disease. As indicated by Keller and as~miates,2~ pathologists may disagree in the subclassification of some cases of Hodgkin's disease because of the histopathologic subtleties that influence the inter- pretation. In their 176 cases of Hodgkin's disease, complete initial agreement in subclassification was reached in 67 percent. However, two of the three observers eventually agreed in 92 percent.
Recently, Oels and associates16 have emphasized the poor prognostic outlook in patients exhibiting a "starry-sky" (histiocytic phagocytosis) appearance. This appearance, which is the result of severe histimytic phagocytosis, is found predominantly in patients with immature lymphocytic (lymphoblas- tic) lymphomas or reticulum cell lymphomas and is especially striking in Burkitt's tumor. One of our patients with an immature lymphocytic (lymph- oblastic) lymphoma exhibited this feature; death
CHEST, VOL. 57, NO. 6, JUNE 1970
Downloaded From: http://journal.publications.chestnet.org/pdfaccess.ashx?url=/data/journals/chest/21496/ on 06/26/2017

VAN HEERDEN ET AL
occurred three months later. We regard a "stany- sky" appearance as another ancillary clue to prognosis.
It is commonly stated that nodularity is a reliable prognostic sign. We found this to be especially true in our series of patients with lymphosarcoma in which four of nine patients with nodular (follicu- lar) lesions and only one of 31 of those with diguse lesions survived five years. In the group of patients with Hodgkin's disease, nodular formation did not iduence survival as much.
Treatment: The persistent localhtion of lympho- ma in 53 percent of patients, "even unto death," suggests that the surgeon's responsibility for patients with mediastinal lymphoma should go beyond merely providing tissue for diagnosis. The location of these tumors in the anterosuperior mediastinum dictates an anterior sternal-splitting or an antero- lateral thoracotomy to facilitate complete removal.
Radiotherapy still remains the primary mode of treatment in mediastinal lymphoma. It is used routinely, either after biopsy when it is employed as the definitive therapeutic procedure or after radical excision when its use is both supplementary and prophylactic. The radiotherapeutic approach is also becoming more aggressive, with hope that the employment of the so-called "mantle-field" (mediastinum, neck, and both axillae) and in- creased tumor dose will lead to improved long-term survival.
The most striking increase in surival rate was found in the group of 16 patients who underwent complete excision of their mediastinal lesion, with subsequent radiation therapy. Thirteen of the 16 patients in this group survived five years as com- pared to only 32 of the remaining 80 patients with a similar survival. It is important to note that not all of these patients had stage I disease (nine of 16 had stage I disease), so that stage I1 media- stinal disease does not necessarily imply inopera- bility or the impossibility of longterm survival. All of these patients received postoperative radiother- apy, whereas two patients received intravenously administered nitrogen mustard in addition. The selection of these patients, especially the decision to undertake complete resection at exploratory thoracotomy, was left to the discretion of the individual surgeon and was not necessarily the result of definitive evidence indicating that the mediastinum was the sole site of disease. The striking results in the small group of patients who underwent partial or palliative resection should encourage a more aggressive surgical attitude.
Insufficient time has elapsed to allow an adequate
comparison of the "new" radical radiotherapy in mediastinal lymphoma with radical resection plus ancillary radiotherapy. We believe that the latter form of treatment has a distinct place in cases of mediastinal malignant lymphoma.6
We believe that for malignant lymphoma the concept of early localized (unicentric) disease is becoming established and that general pessimism is waning. Accurate diagnostic methods are at our disposal, and with the use of lymphangiography, more precise staging is possible. Distinction between the histopathologic types of malignant lymphoma can be made. A team approach including a clinician, surgeon, surgical pathologist, and radiotherapist can prevent decentralization of therapy and can afford the patient the best chance for long-term survival.
1 BLADES, B.: Mediastinal tumors: report of cases treated at army thoracic surgery centers in the United States, Ann. Surg., 123749, 1946.
2 ELLIS, F.H., JR.: Primary tumors of the mediastinum, J . LouisimM Med. Soc., 112:33, 1960.
3 HWER, G.J., AND ANDRUS, N.D.: The surgery of media- stinal tumors, Amer. J. Surg., n.s. 50:146, 1940.
4 LUKES, R.J., BUTLER, J.J., AND HICKS, E.B.: Natural history of Hodgkin's disease as related to its pathologic picture, Cancer, 19:317, 1966.
5 EASSON, E.C.: Possibilities for the cure of Hodgkin's disease, Cancer, 19345, 1966.
6 HALL, C.A., AND OLSON, K.B.: Prognosis of the malig- nant lymphomas, Ann. Intem. Med., 44687, 1956.
7 AISENBERC, A.C.: Primary management of Hodgkin's disease, New Eng. J . Med., 27893, 1968.
8 PETERS, M.V., ALISON, R.E., AND BUSH, R.S.: Natural history of Hodgkin's disease as related to staging, Cancer, 19:30& 1968.
9 RAPPAPORT, H.: Tumors of the hematopoietic system, A t h of Tumor Pathology, Section I n , Fascicle 8, Washington, D.C., 1966, Armed Forces Institute of Pathology, 442 pp.
10 SMETANA, H.F., AND &HEN, B.M.: Mortality in relation to histologic type in Hodgkin's disease, Blood, 11:211, 1956.
11 Symposium: Obstacles to the control of Hodgkin's dis- ease, Cancer Res., 26:1041, 1966.
12 H o s m , H.A.: Hodgkin's disease, Amer. J. Roentgen., %4:913, 1950.
13 BICHEL, J.: Herpes zoster in Hodgkin's disease, Fdb Clin. Int. (Barc.), 6:304, 1956.
14 LUKE$, R.J., ~ V E R , L.F., HAU, T.C., RAPPAPORT, H., AND RUBEN, P.: Report of the Nomenclature Committee, Cancer Res., 26:1311, 1966.
15 O m , H.C., HARRISON, E.G., JR., AND KIELY, J.M.: Lymphoblastic lymphoma with histiocytic phagocytosis ("starry sky" appearance) in adults: a guide to prog- nosis, Cancer, 21:368, 1968.
16 Coo=, J.V.: Mediastinal tumor in acute leukemia: a clinical and roentgenologic study, Amer. I . Db. Child., 44:1153, 1932.
17 SCHWAR-IZ, D.L., PIERRE, R.V., SCBEERER, P.P., REED,
CHEST, VOL. 57, NO. 6, JUNE 1970
Downloaded From: http://journal.publications.chestnet.org/pdfaccess.ashx?url=/data/journals/chest/21496/ on 06/26/2017

MEDlASTlNAL MALIGNANT LYMPHOMA
E.C., JR., AND LINMAN, J.W.: Lyrnphosarcoma cell leu- kemia, A m . 1. Med., 38:778, 1965.
18 WEBS- R.: Lymphosarcoma of the thymus: its I&-
tion to acute lymphatic leukaemia, Med. ]. Awt., 1:582, 1961.
19 WISEMAN, B.K.: Lymphopoiesis, lymphatic hyperplasia, and lymphemia: fundamental observations concerning the pathologic physiology and interrelationships of lymphatic leukemia, leukosarcoma and lymphosarcorna, Ann. Intern. Med., 9:1303, 1936.
20 BERKSON, J., AND GAGE, R.P.: Calculation of survival rates for cancer, Proc. Stuff Meet. Mayo Clin., W:270, 1950.
21 CROSS, R.M.: A clinicopathological study of nodular sclerosing Hodgkin's disease, J . Clin. Path., 2 1 3 3 , 1968.
22 K ~ C A I D , O.W., BRANDENBURG, R.O., AND BERNATZ, P.E.: Experiences with angiography as a guide to mediastinal exploration, J.A.M.A., 173:613, 1980.
23 m, M.V.: A study of survivals in Hodgkin's disease treated radiologically, A m . I. Roentgen., 63:299, 1950.
24 HARGRAVE~, M.M., AND HANLON, D.G.: Leukemia and lymphoma: environmental diseases? in Proceedings of the VlIIth International Congress of Hematology, Tokyo, 1961, Pan P d c Press, vol. 1, pp. 516520.
25 J A ~ ~ N , H., JR., AND P w F., JR.: Hodgkin's Dis- euse and Allied Disorders, Oxford University Press, New York, 1947,177 pp.
26 R ~ E N T H A L , S.R.: Sigdcance of tissue lymphocytes in the prognosis of lymphogranulornatosis, Arch. Path., 21:628, 1938.
27- A.R., I(APLAN, H.S., LUKES, R.J., AND b- PAPORT, H.: Correlation of histopathology with other prognostic indicators in Hodgkin's disease, Cancer, 22: 487,1968.
Reprint requests: Section of Publications, Mayo Clinic, Rochester, Minnesota 55901.
EOSINOPHILS AS DIAGNOSTIC SEMAPHORES
Eosinophilic leukocytes play an important role in some aspects of the defense mechanism of the body. Gross discrepancy between relatively mild symptoms or absence of symptoms and definitive x-ray findings of the lung should alert the physician to the possible diagnosis of Loeffler's syndrome so designated after the first report on the subject (Beitr. z. Klin. d. Tuberk., 79:368, 1932). In the majority of cases, fever is absent. The patient may complain of slight cough and expecto- ration. Accidental death of some of these patients brought about pathologic studies which revealed bron- chopneumonia or lobar pneumonia or sites of infiltration varying from tubercle size to 5 cm in diameter. His- tologic examination showed eosinophilic leukocytes, plasma cells, lymphocytes and occasional giant cells surrounded by histiocytes. In addition to alveolar and interstitial exudation, there were periarterial and peri- capillary idammatory changes with eosinophils and plasma cells predominating. The pulmonary involve- ment is of transitory nature. I t disappears in three to eight days. It is considered allergic or immunologic in origin. Its heterogenous etiolo includes the fol- lowing: intestinal parasites (Ascutis ?' umbricoides, Taeniu saginata, Trichurk trichiura, Ameba histolytica, Strongy- loides stercoralis, Necator americanus), Trichinu spiralis, Ancylostoma brdiense, bacterial allergy, pollens and other allergens, sensitization to drugs. Crofton et al (Thorax 7:1, 1952) classified pulmonary eosinophilias:
1) sim le pulmonary eosinophilia (Loeffler's syndrome); f 2) pro onged or recurrent ulmonary eosinophilia; 3) pulmonary eosinophilia w i i asthma; 4) tropical pul- monary eosinophilia; 5) polyarteritis nodosa. In pro- longed pulmonary eosinophilia, the lung lesions vary from miliary nodules to patchy infiltration and massive pneumonic consolidation which ersist from one month to over one year. Patients with %. condition are likely to have moderate or high fever and other toxic svmn-
D , I
toms in addition to cou h and other respiratory com- f laints. The peripheral ocalization of pneumonic in- &bates prompted Carrington et a1 (New Eng ]. Med. (280:787, 1969) to describe them as "photographic negative" or "reversal" of x-ray appearance of pul- monary edema or alveolar proteinosis. Relative to k"'- monary x-ray findings during attacks of bronc 'a1 asthma, there is no consensus concerning characteristic changes and their path01 c substrate. In some in- stances, disseminated, mostly basal nodular shadows are visualize in size from 2 to 6 mm in diameter. They are attributed to atelectasis or infiltrates. It is well to keep in mind that there are instances of presumably severe, localizing antigenic challenges in which there is no eosinophilia in the peripheral blood despite the excessive number of eosinophils at the site of the lung lesion.
Andrew L. Banyai, M.D.
CHEST, VOL. 57, NO. 6, JUNE 1970
Downloaded From: http://journal.publications.chestnet.org/pdfaccess.ashx?url=/data/journals/chest/21496/ on 06/26/2017