May 16, 2008 APRN Regulation: Recent Trends and Implications for Oncology APRN Practice.
-
Upload
sydney-reason -
Category
Documents
-
view
221 -
download
0
Transcript of May 16, 2008 APRN Regulation: Recent Trends and Implications for Oncology APRN Practice.
Julie A Ponto, RN PhD ACNS-BC AOCN®Winona State University
Past President, ONCC Board of Directors
History of APRN Regulation
Nursing Regulation
• The foremost responsibility of nursing regulation is protection of public health, safety and welfare.
• Important because unprepared and incompetent individuals who practice pose risk of harm to the public.
Licensing boards , governed by state regulations and statutes, are the final arbiters of who is recognized to practice in a given state.
State Boards of Nursing• Authorized state entity with legal authority
to regulate nursing• Regulate RN Practice in 50 states, DC and
5 U.S. Territories• Protect the public’s health by overseeing
and ensuring the safe practice of nursing– Establish standards
– Issue licenses
– Monitor licensees’ compliance
– Take action against those who exhibit unsafe practice
State Legislatures enact Nurse Practice Acts:
• Define the authority of the board of nursing
• Define nursing and the boundaries of the scope of practice
• Identify types of licenses
• Identify requirements for licensure
• Protects titles
• Identify grounds for discipline
Boards of nursing develop rules and regulations consistent with the nurse practice act that have the force and effect of law.
“When a RN engages in practice that is determined to be beyond the identified scope of nursing,
legal authorization for that practice must exist in state law.
Any title, even if issued by a certifying body, only carries legal status if that title is recognized or
authorized in statute or regulation.”
NCSBN
Supports the 60 state boards of nursing in the USA and its territories in providing leadership to advance regulatory excellence for public protection. The NCSBN delegate assembly is comprised of representatives from all U.S. Boards of Nursing.
National Council of State Boards of Nursing (NCSBN)
NCSBN• “Trade association” for state boards of
nursing• No regulatory authority• Provides support and direction to state
boards on issues• Develops
Model Nurse Practice Acts Model Rules and Regulations Nursing Compacts Position Statements
1980s
NCSBN Position on Advanced Clinical Practice stated that the preferred method of regulation for the APRN was “designation/recognition” which is the least restrictive form of regulation .
APRNs have
• expanded in numbers and capabilities over the past several decades
• become a highly valued, integral part of the healthcare system.
Between 1986 and 1992• The economic, legislation and
policy changes affecting healthcare in the U.S. regarding cost and access to care increased the interest in alternative approaches to care.
Between 1986 and 1992
• There was increasing recognition of the overlap between medical practice and that of other providers such as NP, CNS, Nurse Midwives and Nurse Anesthetists.
Between 1986 and 1992
• Regulatory authorities were required to foster these overlapping practices in the interest of cost-effective accessible care, while working to protect the public.
1990 - Present
Regulation of APRNs become progressively more structured and developed into licensure, the most restrictive form of regulation.
1990-2000
• State boards began using the results of advanced practice certification examination as one of the requirements for APRN licensure.
• There was collaboration between APRN certifiers and NCSBN to assure certification examinations were acceptable for regulatory purposes.
1990-2000
• To be suitable for regulatory purposes, APRN certification examinations were required to be entry level (test competencies of new graduates) and accredited
• Certifying bodies were required to provide information to state boards regarding the psychometric soundness and legal defensibility of examinations
2002
NCSBN approved Criteria for Evaluating APRN Certification Programs. These criteria included educational requirements for: Education concentration in the specialty 500 hours supervised clinical hours Clinical experience directly related to role
and specialty
2002
NCSBN published Position Paper: Regulation of Advanced Practice Nursing
• APRN – Umbrella term for NP, CNS, NM, NA
• Licensure – Preferred method of regulation
• Education in role/broad specialty must be consistent with certification
• Only broad categories to be recognized – not “subspecialties such as disease entities”
2003-2006
NCSBN drafted APRN Vision Paper to:
• Resolve regulatory concerns such as proliferation of “subspecialties”
• Provide direction to state boards
2006• The NCSBN APRN
Vision Paper elicited a large response from a wide audience of nursing stakeholders.
• NCSBN APRN Advisory Committee met with the APRN Consensus Work Group and agreed to begin a joint dialogue, working together toward a future model for APRN regulation.
2006
• The APRN Consensus Work Group and the NCSBN APRN Advisory Committee publish the Consensus Model for APRN Regulation: Licensure, Accreditation, Certification and Education
2008
The Present
Both APRN requirements and approaches to APRN regulation continued to vary widely from state to state.
Interstate Compact
• Offer states the mechanisms for mutually recognizing licenses/authority to practice
• RN/LPN/VN Compact– Enacted in 2000
– Currently includes 22 states
APRN Interstate Compact
• Model language adopted 2002
• Only states that have adopted RN/LVN/PN may participate
• Utah, Iowa and Texas have passed ARPN Compact into law
• No rule writing has begun
• No date for implementation
Carlton G. Brown, PhD APRN AOCN®Georgetown University
President, ONCC Bard of Directors
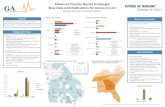
Data on Oncology APRNs and Educational Programs
ONCC Survey of Oncology APRNs
April 2008
• E-mail invitation to participate sent to 3734 ONS members who list NP or CNS as their primary position
• Response rate = 1248 (33%)
• Demographics of respondents indicate they are representative of the ONS members who are APRNs
Graduate Programs in Oncology Nursing
• 23 Programs– 14 NP
– 12 CNS
– 1 Blended
• Most Linked to Broader Specialty– Adult
– Medical-Surgical
– Acute Care
• Number of oncology-specific courses offered ranges from 2-10
Transcript ReviewAOCNP® Candidates
2005-2007Specialty Focus
Family 33%
Adult 30%
Oncology 21% *
Acute Care 8%
Gerontology 2%
Other 6%* Includes oncology combined with others such as adult
or acute care
Transcript ReviewAOCNS® Candidates
2005-2007Specialty Focus
Oncology 31%*
Adult 17%
Medical –Surgical 9%
Administration 8%
Education 7%
Community 6%
Family 5%
Other 12%
None 5%
* Includes oncology combined with others such as adult or acute care
Oncology (AOCN®) 38%Oncology (AOCNS®) 27%Adult/Medical-Surgical CNS 21%
12-15% of CNSs who hold AOCNS® or AOCN® also hold another CNS certification
Survey Data
Certifications HeldCNS
Adult Primary Care NP 36%Family NP 33%Oncology (AOCNP®) 21%Oncology (AOCN®) 17%Adult Acute Care NP 10%Gerontological NP 4%
60-65% of NP who hold AOCNP® or AOCN® also hold another NP certification
Survey Data
Certifications HeldNP
State Board Regulation
Credentialed by State Board of Nursing
CNS 52% NP 97% Blended 87%
Title Protection
CNS 29% NP 34% Blended 46%
State Board Regulation
Expanded Scope of Practice
APRN License
CNS 35% NP 87% Blended 81%
Prescriptive Authority
CNS 13% NP 91% Blended 73%
State Board RegulationCertification Used by CNS
Oncology (AOCN®) 16%
Adult or Medical Surgical CNS 10%
Oncology (AOCNS®) 7%
Pediatric CNS 1%
Other 6%
State Board RegulationCertification Used by NP
Adult (Primary and/or Acute) NP 38%
Family NP 27%
Oncology (AOCNP®) 5%
Oncology (AOCN®) 4%
Women’s Health NP 2%
Pediatric NP 1%
Gerontological NP 2%
Other 3%
State Board RegulationCertification Used by Blended Role
AOCN® 27%
Adult NP 26%
Family NP 10%
Adult or Medical-Surgical CNS 10%
AOCNS® 5%
AOCNP® 4%
Cyndi Miller Murphy, RN MSN CAEExecutive Director
Oncology Nursing Certification Corporation
Consensus Model for APRN Regulation: Licensure,
Accreditation, Certification and Education
Currently there is no uniform model of APRN regulation across states. Each state independently determines:
• APRN legal scope of practice• Roles that are recognized• Criteria for entry into advanced practice• Certification examinations accepted for
entry-level competence assessment
Issue
This lack of uniformity has created a significant barrier for APRNs to move from state to state and has limited access to care for patients.
Issue
An invitation to participate in the process was sent to 50 organizations with a stake in advanced practice nursing
Development of APRN Consensus Work Group
2004
32 organizations (including ONS and ONCC) convened in June to initiate a discussion of issues related to APRN definition, specialization, subspecialization, education, certification and licensure.
Development of APRN Consensus Work Group
2004
Based on recommendations generated at the June conference, a smaller work group of designees of 23 organizations with broad representation from APRN certification, licensure, education, accreditation and practice was formed.
Development of APRN Consensus Work Group
2004
Development of APRN Consensus Work Group
2004
The group was charged with developing a statement that addresses the issues delineated during the Conference with the goal of envisioning a future model for APRNs
• Strive for harmony and common understanding in the APRN regulatory community that would continue to promote quality APRN education and practice
• Develop a vision for APRN regulation, including education, certification, licensure
Goals of APRN Consensus Process
• Establish a set of standards that protect the public, improve mobility, and improve access to safe, quality APRN care
• Produce a written statement that reflects consensus on APRN regulatory issues
Goals of APRN Consensus Process
October 2004 – April 2008
• Sixteen days of in-person intensive discussion and multiple conference calls
December 2005
• ANA convened a meeting of the broad stakeholder group
APRN Consensus Work Group
April 2006
• APRN Consensus Work Group met with NCSBN APRN Advisory Panel to discuss the NCSBN Vision Paper and to request feedback from NCSBN on the Consensus Group draft paper
APRN Consensus Work Group
January 2007• Representatives from the APRN
Consensus Work Group met with representatives from the NCSBN APRN Advisory Panel with the goal of assuring that the revised Vision Paper and the final paper from the Consensus Group would not conflict, but rather complement one another.
APRN Joint Dialogue Group
As the two groups continued to meet in joint dialogue, much progress was made regarding areas of agreement and it was determined that one joint paper would be developed which reflects the work of both groups.
APRN Joint Dialogue Group
Sixteen months after the Joint Dialogue Group was formed, the draft paper was released to the boards of the stakeholders groups.
APRN Joint Dialogue Group
• Licensure – granting of authority to practice
• Accreditation – formal review and approval by a recognized agency of education degree programs or certification programs
• Certification – formal recognition of knowledge, skills and experience demonstrated by the achievement of standards identified by the profession
• Education – formal preparation of APRNs in graduate degree – granting or post-graduate certificate programs
APRN Regulatory Model: LACE
• Completed accredited graduate level education program in one of four roles of CRNA, CNM, CNS, CNP
• Passed national certification that measures APRN role and population-based competencies
• Acquired advanced clinical knowledge and skills to provide direct care to patients (Defining factor for all APRNs is that significant component of education and practice focuses on the direct care of individuals)
Definition of APRN
• Practice builds on RN competencies with – Greater depth/breadth of
knowledge
– Greater synthesis of data
– Increased complexity of skills and interventions
– Greater role autonomy
Definition of APRN
• Educationally prepared to assume responsibility/accountability for:– Health promotion/ maintenance– Assessment, diagnosis, management
of patient problems– Use and prescription of
pharmacologic and nonpharmacologic interventions
Definition of APRN
• Clinical experience with sufficient depth and breadth
• Licensed as independent practitioner to practice as APRN in role of CRNA, CNM, CNS or CNP
Definition of APRN
For entry into practice and regulatory purposes APRN education must:
• Be through a formal graduate or post-graduate accredited institution
• Comprehensive, at graduate level
• Prepare graduates to practice as CRNA, CNM, CNS or CNP across at least one population foci (neonatal, pediatric, adult, gender-specific or psych-mental health)
Broad-based APRN Education
For entry into practice and regulatory purposes APRN education must:
Include at least three separate comprehensive graduate-level courses:
• Advanced physiology/pathophysiology
• Advanced health assessment
• Advanced pharmacology
Broad-based APRN Education
May also include preparation in a specialty area of practice, but it must build upon the APRN role and population – focus competencies.
Broad-based APRN Education
– Build upon role and population-focused competencies
– Represent a focused area of practice• Specific population subset
• Specific patient needs– Disease states
– Body system
– Developed, recognized, monitored by the profession (not regulatory agencies)
APRN Specialties
• Preparation cannot replace role/population focused education
• Cross over roles and populations
• Title may not be used in lieu of licensing title which include role and population
• Competencies must be assessed separately from role and population competencies
APRN Specialty
New roles or populations that include a unique or significantly differentiated set of competencies from the current roles and populations may evolve over time. To be recognized criteria must be met:
• Education standards, core competencies
• Accredited graduate, post-graduate educational programs
• Certification program that meets accreditation standards
Emergence of APRN Roles and Populations
Specific Criteria for each prong of regulation
Licensure
Accreditation
Certification
Education
Target date: December 31, 2015
Strategies for Implementation
Grandfathering When states adopt new eligibility
requirements for APRNs, currently practicing APRNs will be permitted to continue practicing within the states(s) of their current licensure. If APRN applies for endorsement by another state, they will need to meet new criteria OR criteria in place when they became licensed.
Strategies for Implementation
The ONS and ONCC Boards of Directors have approved the
concepts in the Consensus Model for
APRN Regulation.
Draft of the complete paper
Consensus Model for APRN Regulation: Licensure,
Accreditation, Certification and Education
Can be found on the ONS website at
http://www.ons.org/clinical/professional/QualityCancer/
issues.shtml
Slide show used to present the model to representatives of
stakeholder groups on
April 14, 2008
can be found at:
http://www.aacn.nche.edu/education/apnpresentations.htm
Barbara B. Rogers CRNP MN AOCN® ANP-BCFox Chase Cancer Center
Past chair, ONCC Advanced Practice Test Development Committee
Implications of the New Model for Oncology APRNs
Goals of the Consensus Model
• Standardization in educational programs
• Enhanced mobility of APRNs due to consistency in licensure requirements
• Uniformity in independent APRN practice
• Greater access to APRN care for patients
Challenges for EducationPrograms must ensure: Students attain APRN core, role
and population competenciesInclusion the three “Ps”Graduates are eligible for
certification in the role/population focus
Transcripts specify role/population focus
Challenges for Education
Adult and Family CNS and NP programs will need to incorporate comprehensive gerontology content into adult program curriculums
Oncology- Specific Challenges for Education
Integration of specialty content, along with the core and population content will lengthen didactic and clinical requirements
Graduates not required to have specialty competencies
Oncology -Specific
Opportunities for Education
Specialty competencies do not have to be obtained within the formal graduate program
Development of post-graduate programsDevelopment of comprehensive
continuing education by ONS to provide APRN competencies
Acquired through professional practice
Challenges for Licensure
State boards of nursing will:
License only at the role and population level
Grant licenses for all four roles of CNS, NP, NM, NA
Challenges for Licensure
State boards of nursing will need to:
Revise rules and regulations for APRN licensure
Grandfather all who currently are recognized to practice in a specific role
Opportunities for Licensure
APRN regulation exclusively by boards of nursing
Standardization of criteria for licensure
Implementation of APRN interstate compact
Challenges for Certification
Population-based certifications for CNS will need to be developed for all six population foci
Specialty competencies will be assessed separately from the role and population competencies
Oncology- Specific Challenges for Certification
Need to demonstrate the value of specialty certification
Oncology APRNs must be encouraged to attain and demonstrate specialty competencies
Employers must be encouraged to require certification for specialty practice
Oncology-Specific Opportunities for Certification
Not required for regulatory purposes
Eligibility criteria not dictated by state boards of nursing
Educational criteria, other than that obtained within the graduate program, can be required
Challenges for Oncology APRNs
Those who currently meet regulatory criteria, will be grandfathered within the same state, but may need to meet new criteria in a new state
Challenges for Oncology APRNs
In states where regulation does not currently exist (e.g. for CNS), grandfathering will occur for those in practice, or APRNs will need to meet the new criteria for licensureEducationCertification