MAR-MAY 2006 TEInsight Mar-May06.pdfnovel, low-cost intra-vitreal therapy regime for CMV Retinitis...
Transcript of MAR-MAY 2006 TEInsight Mar-May06.pdfnovel, low-cost intra-vitreal therapy regime for CMV Retinitis...

Marking yet another first in the region, surgeons in TEI @ TanTock Seng Hospital and National University Hospital havesuccessfully performed more than eighty vitreo-retinal
surgeries in the past few months utilising a new minimally invasive,sutureless technique.
The new method has benefited almost all TEI patients with retinalconditions requiring vitrectomy (used to surgically treat blinding retinalconditions such as diabetic vitreous haemorrhage, retinal detachment,macular holes, epiretinal membranes, infection, trauma, etc), withoutthe pain and discomfort from conventional surgery. An additionalbonus is shorter surgical duration, as well as reduced recovery timefor the patient.
At the core of this new technique is a more refined 23 gauge setof specialised tools. The current standard technique for vitrectomyrequires the use of sutures and larger 20 gauge instruments.
Dr Lee Jong Jian, a vitreo-retinal consultant trained in the UnitedStates and United Kingdom, introduced this technique from NewYork, the only centre in US to pioneer this surgery in the West. Thistechnique was invented by the renowned Professor C Eckardt fromGermany. TEI’s vitreo-retinal team has endorsed this new technique,after finding it to be highly efficient and beneficial to our patients.
TEInsightMICA (P) 188/02/2006D E L I V E R I N G T H E F I N E S T Q U A L I T Y E Y E C A R E
Macular Holes
3 6SuturelessSquintSurgery
Myopia7 4 Floaters: What you
should know
7 Optometrists’ Column8 Quiz
P O S T E R
Sutureless Vitreo-Retinal Surgery A First for Asia
M A R - M A Y 2 0 0 6
A publication of
IN THE SPOTLIGHT Vitreo-Retina and Paediatric Ophthalmology
INS
IDE
Barely there…a close up of the self-sealing scleral wound created by the23G vitrectomy trocar-cannula system
Dr Lee Jong Jian performing 23G sutureless vitrectomy on a patient withtraumatic complex retinal detachment.
Continued next page
TEInsight is sponsored by

2 T
EIn
sig
ht
MA
R-M
AY
06
Dear Readers,
We hope TEInsight #3 finds you ingood health.
We are making the rounds of all thesubspecialties, and having coveredRefractive Surgery & Oculoplastics (Issue 1),followed by Neuro-ophthalmology &Glaucoma (Issue 2), we now arrive atVitreo-Retina and PaediatricOphthalmology.
The link between the lead articlescontributed by our two subspecialty teamsthis time is uncanny – both highlight thedawn or maturation of sutureless surgeryin their respective fields.
More than mere coincidence, thesetechniques represent our drive to developand adopt innovative, more rapid andpainless surgery for our patients, withoutany compromise on quality of outcome orpatient safety. It would have been radicalto even consider not “closing up” forsquint surgery or a vitrectomy up to acouple of years ago, but it now seems thatthese methods have strong potential tobecome the status quo in the near future.
Elsewhere in this issue: ouroptometrists contribute a useful checklistfor their peers who may be confrontedwith a child who “can’t see”; the hypethat surrounds “treatment” for myopia isinspected in the cold light of day; andfinally, some good news, in the form ofbetter-than-previously-assumed results formacular hole surgery.
May you find TEInsight #3 a good read.Cataracts and Diabetic Eye Disease arewaiting in the wings. Until then, I wish youthe best of luck and health.
Dr Wong Hon Tym
TEInsight Editorial TeamDr Wong Hon Tym (Chief Editor)
Mr Christopher Koh (Secretariat)
Dr Gangadhara Sundar
Dr Christopher Khng
Dr Ronald Chung
A/Prof Goh Lee Gan (Advisor)
Editor’sMessage
The method utilises the trocar-cannula system where the entry site(sclerostomy) is first prepared by a slanting surgical blade to create a shelvingwound through the conjunctiva and sclera. The cannula is then introduced intothe wound via a trocar. Retinal surgery can then be performed by gainingaccess through the sclerostomies. After its completion, the cannula is simply
withdrawn, with the wound self-sealing suturelessly. As operatingtime is markedly reduced, theoperative risks and costs for patientsare also reduced. With faster visualrecovery, patients can return to theirwork or routine activities with fewerclinic follow-ups. Depending on thecondition, this may be as early as 2weeks, compared to the usual 4 to 6weeks of medical leave issued forthe conventional vitrectomy.
This new method closely mirrorsan earlier incarnation: a 25 gaugesystem introduced 2 years ago,similarly sutureless, yet limited in itsscope, as it was an extremelydelicate set that was unsuitable forthe more complex retinal conditions.The 23 gauge instruments are morestable and robust enough fordemanding surgery. The benefitsmay be further augmented with a“hands-free” chandelier light source,
another new innovation to enhance visibility and facilitate bimanual surgery inthe more challenging cases. Dr Lee foresees that eventually most retinalsurgeries will be performed in this fashion. Surgical outcomes with 23 gaugevitrectomy have been very encouraging, with no significant complicationsreported at TEI.
By Dr Lee Jong Jian,
TEI@TTSH
Continued from page 1 Sutureless Vitreo-Retinal Surgery
This picture was taken on thefirst post-operative dayfollowing combined phaco-vitrectomy
As operating time is
markedly reduced, the
operative risks and
costs for patients are
also reduced. With
faster visual recovery,
patients can return to
their work or routine
activities with fewer
clinic follow-ups.
In our quest to constantly improve ourselves, we would appreciate your frank feedback on any partof this newsletter, be it on the format or content. Please email your comments to [email protected] mail to Ms Izyani Ayik, The Eye Institute, National Healthcare Group, 6 Commonwealth Lane,Level 6, GMTI Building, Singapore 149547. Please indicate if you would grant us the permission topublish your letter. If you would like to receive our upcoming quarterly e-newsletter, please sendan e-mail with your name to [email protected] with the subject heading ‘TEInsight Subscribe’.

contrast, results from other established international centres suggestthat their patients presented with less severe grades of the disease,with proportional pre- and post-operative visual acuities.
With respect to surgical outcome, for macular holes withoutretinal detachment, our rate of anatomical closure was anencouraging 84%, with 72% demonstrating improvement in visualacuity. The most important predictors of surgical success werepresenting visual acuity, duration of disease and adherence to post-operative posturing.
The most common complication related to this procedure(secondary to the use of intraocular tamponade) was thedevelopment of cataracts and need for subsequent extraction in15% of patients.
The 15 years following the initial description of macular holesurgery have indeed resulted in an explosion of techniques andtamponade options for this once “untreatable” medical condition.The result is a gratifying improvement in anatomical and functionaloutcomes for our patients.
By Dr Shawn Goh, TEI Registrar
Optical Coherence Tomogram images of a macular hole,acquired pre- and post-operatively, clearly showinganatomical closure of the lesion. In this case, the patient’sacuity also improved from 6/36 to 6/6.
Surgical Success with Macular Holes
3 T
EIn
sig
ht
MA
R-M
AY
06
V I T R E O - R E T I N A
SPOTLIGHT ON
TEI’s Vitreo-Retina Team
The perception of age-related macular holes has evolved. Whatwas once thought to be a rare, untreatable medical disease isnow largely regarded as a surprisingly common and repairable
surgical disorder.
Vitreous surgery for macular holes was initially reported in1989, and since then there has been a dramatic shift inmanagement, as clinicians have become more aware of thefrequency of the disease and its successful treatment, augmentedby new technologies like optical coherence tomogram, which allowdirect imaging and intuitive visualization of macula pathology. (Seefigure)
The vitreous is an important factor in the development ofmacular holes. Surgery relieves all tangential traction to the edgesof the lesion by removing cortical vitreous and fine epiretinalmembranes surrounding the hole. Following vitrectomy, retinaltamponade is usually provided by a long-acting gas bubble,followed by strict posturing for a minimum of 1 week. Inexceptional circumstances, silicone oil is used when compliance withposturing may be an issue, or if early air travel is required. Heavysilicone oil, which is denser than water, has been used more recentlyfor patients who are unable to tolerate face-down posturing. Theuse of adjunctive therapies in macular hole closure is as yetunsubstantiated.
A 2-year audit of macular hole surgeries performed in TEI @TTSH has yielded significant information. It revealed that of the 40cases operated upon between 2001 and 2002, 40% of our patientswere in the 6th and 7th decades of their lives (average age of 63).Most patients present within 5 months of onset of symptoms withthe complaint of reduced visual acuity in over 90% of patients.Generally speaking, Singaporean patients present fairly late withpoor visual acuity (65% had acuity of 6/120 to hand motions). In
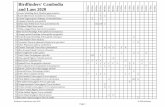
TEI’s VR Team is proudly distinguished by a cache of firsts: the use of scanning laser ophthalmoscopy to dynamically image lesions inage-related macular degeneration; sutureless 23G vitrectomy; the use of intra-vitreal steroids in the treatment of refractory macularoedema; and the use of low-cost intravitreal Ganciclovir therapy for infectious retinitis in AIDS patients.
Dr Billy Tan
Dr Tan is the Head of the SurgicalRetina Service in TEI. He isfellowship-trained from the RoyalEye and Ear Infirmary, MelbourneAustralia and is one of thepioneering vitreo-retinal surgeonsin Singapore. He divides his timebetween his private practice andas Visiting Consultant to TEI @TTSH. He is a strong proponent ofsutureless 23 and 25Gvitrectomies, and is widelyregarded by his peers to be one ofthe very best in conventional 20Gvitrectomy.
A/Prof Lim Tock Han
A/Prof Lim is the Director, TEI andHead of Department,Ophthalmology TTSH. He isfellowship trained in OcularInflammation from Jules Stein EyeInstitute, USA and Vitreo-Retinafrom the Mayo Graduate School ofMedicine, USA. He pioneered thenovel, low-cost intra-vitrealtherapy regime for CMV Retinitis inSingaporean AIDS patients, as wellas introduced High-SpeedIndocyanine Green Angiography inSingapore, which hasrevolutionized the treatment ofAge-Related MacularDegeneration.
A/Prof Au Eong Kah Guan
Adjunct A/Prof Au Eong is theDeputy Director (Research) TEI, andthe Head of Ophthalmology andVisual Sciences, AlexandraHospital. He holds concurrentappointments in the Yong Loo LinSchool of Medicine at the NationalUniversity of Singapore and theSingapore Eye Research Institute.His fellowship was in diseases andsurgery of the vitreous and retinafrom the Manchester Royal EyeHospital, England, and the WilmerEye Institute, Johns HopkinsHospital, Maryland USA. He wasinstrumental in the development ofrevolutionary surgical techniquesincluding sutureless 25Gvitrectomy and was the firstsurgeon to perform maculartranslocation surgery for maculardegeneration in Southeast Asia.
Dr Caroline Chee
Dr Chee is the Head of the MedicalRetina Service in TEI, as well as theHead of Training TEI @ NUH. Sheis the Vitreo-Retinal Consultant inTEI @ NUH, and is immenselyexperienced in medical retinapathology. She is a pioneeringVitreo-Retinal surgeon inSingapore and is fellowship trainedwith Professor Alan Bird inMoorfields, London in diseases ofmedical and surgical retina.
Dr Zaw Minn Din
Dr Zaw is Consultant to the VRservice in TEI @ TTSH. He hasextensive experience and trainingin the United Kingdom where hisarea of interest extends to themedical and surgical managementof vascular diseases of the retina.He is active in local andinternational communityophthalmology with theintroduction of an island-wideweb-based diabetic retinopathyscreening programme which islinked to the NHGP diabeticscreening service.
Dr Lee Jong Jian
Dr Lee is the most recent additionto the VR service in TEI @ TTSH. In2005, he returned fromsubspecialty training in theManchester Royal Eye Hospital UK,as well as the Edward S. HarknessEye Institute, Columbia Universityand Manhattan Eye, Ear andThroat Hospital in New York.On his return, he has pioneerednovel surgical techniques in Asiaincluding the sutureless 23Gvitrectomy system, chandelierillumination system and bimanualsurgical techniques in managingcomplicated retinal surgeries.
(a) Pre-Operative (b) Post-Operative
Visiting Consultants:Dr Ang Beng ChongTEI @ NUH
Dr Yap Eng YiatTEI @ TTSH
Dr Ronald YeohTEI @ NUH

I see black spots flying around in front of my eyes – what are they?The black spots you see are called floaters. They can look like dots, spider webs, circles, lines or insects. Some peopleeven think they look like Chinese words.
Where do these floaters come from?Although they look like they are floating in front of you, floaters are actually inside your eyeball. They are due toparticles in the vitreous gel, which is a “jelly ball” that fills your eye. Vitreous is usually transparent and clear, untilageing or degeneration sets in – that is when the particles and floaters appear. Vitreous degeneration is the mostcommon cause of floaters, and it is harmless.
Public Education Material with compliments ofTEInsightM A R - M A Y 2 0 0 6
I find my floaters very annoying.Is there any treatment? You don’t need treatment for floaters caused by vitreousdegeneration, because they tend to fade out of view. Eyedrops won’t help, and eye doctors do not perform eyesurgery for floaters, as the benefits really don’t justify therisks. Thankfully, with time, almost all people get used totheir floaters, and learn how to ignore them.
So are all floaters harmless?No. Sometimes they may be caused by eye conditions thatneed urgent treatment. For example, floaters could signifyretinal holes or retinal detachments. This tends tohappen in people with high myopia (i.e. very shortsighted), or in people who’ve suffered an injury to the eye.If you are diabetic, floaters may signify bleeding insidethe eyeball. Less commonly, floaters could also signifyinfection deep inside the eye.
You should see an eye doctor immediately if:
1. The floaters appear suddenly, and you’ve neverhad them before.“New” floaters may signify the onset of an eyeproblem such as a retinal hole.
2. There are a large number of floaters.In general, one or a few floaters are no cause foralarm. But if you have a large number, you shouldseek medical attention without delay. A largenumber of floaters could mean a bleed inside theeye.
3. The floaters are accompanied by flashes of light.Flashes look like electric sparks or lightning bolts, andmean that there is a “pulling” force on your retinathat may result in a retinal tear.
4. If you have diabetes. Diabetics may developbleeding in the eyeball, giving rise to floaters.
5. You are highly short-sighted (myopic) or havejust had an eye injury. High myopia and traumaare associated with retinal holes and detachments, aswell as bleeding.
6. You feel that your vision is blurred. Blurred visioncould signify serious eye problems such as infections,bleeding, or retinal detachments.
7. You feel that something is blocking your visionat the sides, like someone has drawn a curtainacross part of your vision. This ominous symptomcould mean that you have a retinal detachment andit needs urgent treatment.
In general, floaters aresafe if:
1. You’ve had them for along time.
2. You’ve always hadroughly the samenumber of floaters.
These floaters are usuallythe consequence ofageing of the eye.
WHEN TO WORRY WHEN TORELAX
WHAT YOU SHOULD KNOWFLOATERS
Photograph courtesy of Dr Mandeep Singh, TEI @ NUH
P UL L O
UT F
OR Y
OU
R
C L I NI C
NO
T I CE B
OA
R D
The information on this poster will help you recognize which type of floaters need urgent attention, and which are theones you need not worry about.
But always remember, when in doubt, it’s safer to get your eyes checked as soon as you can.

6 T
EIn
sig
ht
MA
R-M
AY
06
P A E D I A T R I C O P H T H A L M O L O G Y
Sutureless Squint SurgeryImproved Comfort & Cosmesis
SPOTLIGHT ON
TEI’s Paediatric Ophthalmology Team
Strabismus surgery, performed to correctsquints (ocular misalignment), can beachieved by weakening, tightening or
modifying the function of the extraocularmuscles. The most common strabismussurgery done in Singapore is to correctexotropia (divergent squint, Fig 1). For this,bilateral lateral rectus recession isperformed, wherein the insertion of eachlateral rectus is re-positioned moreposteriorly and further away from thelimbus, so as to weaken it.
To gain access to the muscle, the eyesurgeon first needs to make an incision inthe conjunctiva. Traditionally, this is done atthe limbus, resulting in a fairly large woundwhich invariably requires suture closure.
The newer approach is to make theincision in the fornix (deeper in the eye nearthe eyelids). This very elegant technique wasdeveloped by the late Marshall Parks, one ofthe icons of paediatric ophthalmology.When properly placed, this incision can beself-closed by gently massaging theconjunctiva up into the fornix, sidesteppingthe need for suture closure. TEI @ Tan TockSeng Hospital is so far the first and onlyhospital in Southeast Asia to offer thissutureless approach.
The fornix incision is somewhat difficultto learn, but when mastered, provides anexcellent approach to the extraocularmuscles. Unlike the limbal approach, thewound is tucked away under the lid, andpatients are very comfortablepostoperatively. This advantage is extremely
crucial in children who, because of theirthicker conjunctiva and Tenon’s capsule, aremore uncomfortable in the first weekfollowing a limbal incision. This is worsenedby the exposed knots required to close thelimbal wound.
In contrast, the sutureless fornixapproach permits excellent eye movementand opening postoperatively. It avoidscomplications related to the limbalconjunctiva such as dellen formation, peri-limbal scarring and distortion. Cosmesis isexcellent. There is less bleeding and lessoperative time involved. The fornixapproach also facilitates re-operation,especially when the first operation involvedlimbal surgery, because the incision is nowbehind the muscle insertion, which thus
avoids any anterior scar. Unlike the limbalapproach which gives access to only onemuscle, the fornix approach gives access totwo or more muscles with a single incision.Regional anaesthesia is recommended forthis technique.
However, this approach is not suitablefor all patients. Elderly patients with friableconjunctiva and patients with extensiveconjunctival scarring (thus requiringconjunctival recession) are not appropriatecandidates.
At the end of the surgery, the fornixincision is inspected. If there is prolapse ofTenon’s capsule, or if the wound has beeninadvertently stretched, closure with suturesthen becomes necessary. However, withproper techniques and instrumentation, themajority of fornix incisions are self-closingand left sutureless.
By Dr Leo Seo Wei
Dr Leo Seo WeiConsultant
Dr Leo, whose main interests are strabismus surgery (adult & paediatric) and refractive errors, recentlycompleted 2 intensive fellowships in paediatric ophthalmology and strabismus in the USA. The first was anAmerican Association of Pediatric Ophthalmology & Strabismus-accredited clinical fellowship at theUniversity of Michigan and W.K. Kellogg Eye Center, Ann Arbor, under the tutelage of Prof Monte DelMonte and Prof Steven Archer. This was followed by a shorter stint with the renowned Dr Kenneth Wrightin Los Angeles. She has since published numerous peer-reviewed articles and presented at internationalconferences. The mother of two young children, Dr Leo has also set her sights on nurturing the growth ofher subspeciality in the region.
Dr Gangadhara Sundar Consultant
Dr Gangadhara, profiled in the first issue of TEInsight, also has a special interest in paediatric oculoplastics.
Dr Lim Su Ann Consultant
Dr Lim was similarly profiled in the previous issue of TEInsight, and has a special interest in paediatricneuro-ophthalmology & adult strabismus, particularly those of neurologic origin.
Dr Sonal FarzavandiTEI @ NUH
Visiting Consultant:Dr Khoo Boo KianTEI @ TTSH
Figure 1 Right exotropiaNote the ‘malposition’ of the corneal reflex, which hasbeen displaced nasally due to the divergence of that eye
Figure 4The operated eye immediately post-op. Only mild chemosisis seen, with no haemorrhage, exposed sutures or knots
Figure 2 The fornix approachThe scissors are positioned at the site of incision. Theforceps show where the limbal incision would have beenperformed
Figure 3Isolating the lateral rectus via the fornix incision

Singapore’s myopia prevalence rate ranksamong the highest in the world. Fourstudies carried out here showed
escalating numbers with age: 8.6% inkindergarten children, 24.9% in 10 year-oldChinese children, 63.0% in universityfreshman, and 82.0% in medical students.Alarmingly, our children are also becomingmyopic at an earlier age.
Myopia places a substantial burden onsociety and the individual. Severe myopiaincreases the risk of developing blindingconditions such as retinal detachment,myopic macular degeneration, glaucomaand cataract. It is already a major cause ofblindness worldwide, and may become theleading cause in some countries because ofits rapid increase in prevalence. The rate ofprogression is highest in young children,with an average age of stabilization at 16years. Retarding the progression of myopiais thus critical.
Several modalities have emerged toaddress this:
EyedropsAtropine: This is a non-selective muscarinicantagonist, and although it is gainingprominence in myopia retardation therapy,its mechanism of action is still not fullyunderstood. Recent studies have shown thatregular atropine eyedrops may reducemyopia progression by 50% per year andalso halve the proportion of rapidprogressors. However, the long-term effectsof pupil dilation, risk of ultraviolet light-induced cataracts and retinal toxicity are notwell studied. There are also psychologicalside effects and some studies seem to
indicate a ‘rebound’ following cessation.The jury is still out on the optimalconcentration and duration of application.Pirenzepine: This is a more selectivemuscarinic antagonist with fewer adversereactions, is being evaluated in Singapore.Early results are promising but it is notcommercially available as yet.
Under-correctionThis is controversial. Proponents argue thatretinal defocus in deliberately under-corrected eyes may induce a correctivegrowth response towards hyperopia, thusretarding myopia. However, a two-yearrandomized trial in Malaysia showed thatthe under-corrected group had asignificantly higher progression rate. Furtherstudies clearly need to be done. In themeantime, we should not intentionallyunder-correct.
Bifocal and multifocal lensesAs increased retinal defocus is one of thecausative factors for myopia in animals andmyopic humans exhibit “accommodativelag”, it has been postulated that bifocals or
multifocals may reduce accommodativedemand and retinal defocus in myopicchildren. However, the Correction of MyopiaEvaluation Trial (COMET) involving 469American children concluded that whilemultifocal lenses did retard the progressionof myopia by a small amount, this may notwarrant any changes in clinical practice.
Contact lensesContact lenses may increase the quality ofretinal images and flatten the cornea.However, soft contact lenses were found tobe ineffective in a randomized trial in theUS. Complications like infective keratitis andallergic conjunctivitis were reported. Rigidgas-permeable lenses may have increasedoxygen permeability and safety, but a trial inSingapore also failed to show any effect.
Other methodsA plethora of other methods exist: exercisesto relax the eye muscles or “qi gong”,acupuncture, part-time spectacles, hydrogellenses, biofeedback and orthokeratology(contact lenses fitted to flatten the cornea).These have only been evaluated in smalltrials, hence there is no convincing evidenceas yet of their effectiveness.
In conclusion, the research so far doesnot provide sufficient ballast for the routineuse of any particular method. Atropine &pirenzipine nevertheless appear to bepromising at this juncture. While we awaitfurther evidence, atropine can perhaps bejudiciously considered in children at highrisk of developing pathologic myopia inadulthood, following appropriate parentalcounseling.
By Dr Leo Seo Wei
7 T
EIn
sig
ht
MA
R-M
AY
06
M Y O P I A
General pointers
• Remember the goals of examination:(a) identify and correct refractive errors& amblyopia, (b) exclude strabismus (c)exclude pathological conditions likecongenital cataracts, and (d) knowwhen to refer to an ophthalmologist.
• Engage the child: it is impossible toget good measurements from anunhappy or nervous child. Establish afriendly relationship before carrying outany tests, which can be presented asgames.
• A few toys (especially the currentlypopular ones!) to encourage fixationare crucial.
Testing acuity, refraction & mediaclarity
• Match the test technique to thechild’s age: by 3 years, a child shouldbe able to match the letter that you arepointing to on a Snellen chart with theones on a card he/she is holding. By 5years, most can read directly off aSnellen chart.
• Objective refraction using retinoscopyshould be performed for all children.Simultaneously assess the red reflex.Dark spots, a dull or absent red reflex,or the presence of a white reflex are allimportant indications for referral. Re-confirm with a direct ophthalmoscope ifunsure.
• If you are unable to perform cycloplegicrefraction, always use the foggingmethod for greater accuracy.
• Refer to an ophthalmologist if thechild’s best corrected VA is worse than6/12 (age 3-5) or 6/9 (age 6 and older),or there is two-line difference betweeneyes.
Assessing ocular alignment
• Look out for a head tilt or face turn,which may be secondary to strabismus.Correct any abnormal head posturebefore performing tests to detectsquints.
• Corneal reflections – shine a torchfrom about arm’s length onto the child’sface, and look for centrality of the
corneal reflections. Each millimetre ofdeviation from the centre representsapproximately 7 degrees of deviation inthat eye.
• Cover test- While fixating on a smalltarget, cover one eye to see if the othereye moves to take up fixation.
• Stereopsis testing is a way to assessbinocularity. The Frisby plates are agood example. Poor vision or thepresence of a squint can result inreduced or complete loss of stereovisionin a child.
• Refer to an ophthalmologist if youdetect or suspect a squint.
By Ms Jane Tan
Children rarely complain of visual difficulties, thus the early detection of ocular anomalies in the young is essential to avoid lifelong impairment. Optometrists play a vital role here,but we also know that examining a child can be both daunting and frustrating.
Here is a checklist to run through when confronted with a child who “can’t see”.
VISION SCREENING INCHILDREN OOPTOM’S CORNER
F O R O P T O M E T R I S T S
B Y O P T O M E T R I S T S
Is it possible to retard theprogression of myopia?

EYEQ
W H A T ’ S O N
U p c o m i n g E v e n t s
8 T
EIn
sig
ht
MA
R-M
AY
06
Lt. Col. (Dr) Gerard Nah (2nd from left)at the Refractive Surgery Centre of theNavy Medical Centre San Diego(NMCSD) from 11 - 16 Dec 05. The tripwas hosted by Cpt. Steve SchallhornM.D. (Left) and accompanied by ProfTom Salmon OD, PhD (Centre to right),Lt. Col. Corina Van De Pol OD, PhD andLt. Tyson Bryce OD, PhD.
Drs Yip Chee Chew, Zaw Minn-Din,Shawn Goh, Augustinus Laude and NOGoh Lee Lee travelled to Sagaing,Myanmar 27 Nov – 2 Dec 05 toperform voluntary ophthalmic surgeryat the Sitagu Ayudana Hospital for thelocal population.
During his one-year vitreo-retinalsubspecialty fellowship in Manchester,United Kingdom, Dr Lee Jong Jian(right), furthered his subspecialtytraining and research in surgical andmedical retina in New York with leadingauthority Professor Stanley Chang (left)at the Edward Harkness Eye Institute inColumbia University and ProfessorYannuzzi at the Manhattan Eye, Earand Throat Hospital in CornellUniversity. He has since successfullytransplanted back to Singapore thelatest technique for sutureless vitreo-retinal surgery (cover article).
Invited by the Sumatra OphthalmologyAssociation, Indonesia, Dr ManjunathGupta (right) delivers his talk on‘Current Concepts in Myopia, andPhilosophy of Spectacle Prescription inChildren’ at the Fourth society meet,focusing on Paediatric Ophthalmology.Accompanying him were DrGangadhara Sundar, Consultant (notpictured), and Dr Erlangga Ariadarma(left), Medical Officer.
Date/Time Venue Title Contact Details
For Public25 Mar 06 Alexandra Hospital Public Forum in English and Mandarin: Glaucoma Ms Alice How: 6379 3741, 6379 3540 (fax) 10.00am – 12.00nn [email protected]
15 Apr 06 Alexandra Hospital Public Forum in English, Mandarin, Malay & Tamil: Ms Alice How: 6379 3741, 6379 3540 (fax) 10.00am – 12.00nn Age-related Eye Diseases [email protected]
27 May 06 Alexandra Hospital Public Forum in English and Mandarin: Ms Alice How: 6379 3741, 6379 3540 (fax)10.00am – 12.00nn Diabetic Eye Disease [email protected]
For Ophthalmologists & Trainees10 & 11 Mar 06 National University First Human Cadaver Dissection Course on Ms Valerie Ng: 6772 5318 9.00am – 5.30pm Hospital Orbital Anatomy & Oculoplastic Surgery [email protected]
For GPs29 Apr 06 Tan Tock Seng Practical Approaches to Common Ophthalmic Presentations Mr Eugene Kwek: 6357 7736 1.30pm – 4.00pm Hospital Speakers: Dr Goh Kong Yong, Dr Vernon Yong [email protected]
& Dr Leo Seo Wei Ms Lalitha K: 6357 7648, 6357 7718 (fax)[email protected]
For Doctors, Allied Health & Healthcare Administrators, IT Administrators19 & 20 May 06 Grand Copthorne 3rd National Disease Management Conference www.dmconf.com.sg
Waterfront Hotel
TEI Doctors in the Research JournalsSCB Teoh, J Lim, A Koh, T Lim and E FuAbnormalities on the multifocal electroretingram may precede clinicalsigns of hydroxychloroquine retinotoxicityEYE January 2006,20(1):129-32
Chan DPL, Teoh SCB, Tan CSH, Nah GKM, Rajagopalan R,Prabhakaragupta MK, Chee CKL, Lim ATH, Goh KYNewly Emergent Ophthalmic Complications of Dengue Fever andDengue Hemorrhagic Fever: a Retrospective Observational SeriesEmerg Infect Dis 2006 Feb; 12(2).
Ong WC, Lim TC, Lim J, Gangadhara Sundar,Cervicofacial, retropharyngeal and mediastinal emphysema. Acomplication of orbital fracture.Asian Journal of Surgery 28(4)305-308,
Voon LW, Au Eong KG, Saw SM, Verma D, Laude A.Effect of preoperative counseling on patient fear from the visualexperience during phacoemulsification under topical anesthesia:Multicenter randomized clinical trial.J Cataract Refract Surg. 2005 Oct;31(10):1966-1969.
Wong I, Leo SW, Khoo BK.Loop myopexy for treatment of myopic strabismus fixus.J AAPOS.2005 Dec;9(6):589-91.
Q U I Z TEST YOUR
YOU MAKE THE DIAGNOSIS!
1) The clinical sign is leukocoria or white reflexin the left eye.The normal appearance ofthe pupil of the human eye is black.In flashphotographs the pupil may appear red.Thisis known the red reflex,as seen in thepatient’s right eye,and it is normal.Leukocoria is never normal and requiresevaluation by ophthalmologist.
2) Retinoblastoma,persistent hyperplasticprimary vitreous,cataract,retinopathy of
prematurity,toxocariasis,coloboma ofchoroid,uveitis,Coat’s disease,vitreoushaemorrhage,retinal dysplasia ordetachment
3) The ultrasound confirms the diagnosis ofretinoblastoma which has focal areas ofcalcification within the tumour.Thesecalcifications are seen as highly reflectivefoci within the tumor or vitreous.Whensmall,the tumours are smooth,dome
shaped,and are low to medium in internalreflectivity.As the tumours grow,theybecome more irregular in configuration andmore highly reflective as the amount ofcalcium accumulates.
A N S W E R S
The parents of an 18 month old child notice that his right &left eyes “never look the same” in all his photos.
What is the clinical sign? Which is the abnormal eye?
What are the differential diagnoses?
What does the ultrasound demonstrate?
1
2
3
General Enquiries by E-mail: [email protected]
National University Hospital - Eye ClinicGP Hotline: 6772 2000Clinic Line: 6772 5408Clinic Fax: 6772 5508
Tan Tock Seng Hospital - Eye CentreGP Hotline: 6357 8383Centre Line: 6357 8000Centre Fax: 6357 8675
Alexandra Hospital - Ophthalmology and Visual SciencesGP Hotline: 9369 3912OVS Line: 6379 3500OVS Fax: 6379 6292