Management of symptoms in end stage liver disease. · Chronic hepatitis B infection Non-alcoholic...
Transcript of Management of symptoms in end stage liver disease. · Chronic hepatitis B infection Non-alcoholic...

Management of symptoms in end stage liver disease.
January 2018

Grace Ting, Kate Rugen
Literature Review
Sue Howarth, Jenny Hill Audit Results
Andrew Khodabukus People’s Voice
Andrew Khodabukus
Proposed Standards & Guidelines
Dr Paul Richardson and Dr Lynn Owens
Invited Local Experts

GDG Membership Andrew Khodabukus Consultant in Palliative Medicine
Royal Liverpool University Hospital
Sarah Fradsham Consultant in Palliative Medicine
Marie Curie Hospice Liverpool
Grace Ting Specialist Registrar in Palliative Medicine
Royal Liverpool University Hospital
Katherine Rugen Specialty doctor in Palliative Medicine
Woodlands Hospice
Susan Howarth Clinical Nurse Specialist in Palliative Care
University Hospital Aintree
Jenny Hill Clinical Nurse Specialist in Palliative Care
University Hospital Aintree
Diane Foster Advanced Nurse Practitioner in HPB
University Hospital Aintree
Joanna Henry Lead medical admissions pharmacist (specialist pharmacist in digestive diseases) University Hospital Aintree
Expert reviewers
Dr Paul Richardson
Dr Lynn Owens
Consultant Gastroenterologist Royal Liverpool University Hospital Nurse Consultant in HPB
Royal Liverpool University Hospital

Introduction

Introduction • New standards and guidelines.
• Raised as a topic from Clinical Practice Summaries Taskgroup. – Supportive and palliative care for this patient group.
– Management of symptoms in the dying phase.
• Selected 3 common conditions at end of life – Hepatic encephalopathy
– Management of life threatening haemorrhage
– Management multi-morbidity and multiorgan failure

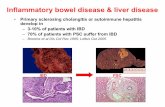
Causes of end stage liver disease
Alcohol-related liver disease Hepatitis C infection
Chronic hepatitis B infection Non-alcoholic fatty liver disease
Hepatocellular carcinoma Primary sclerosing cholangitis
Haemachromatosis Primary biliary cirrhosis
Autoimmune hepatitis Wilson disease
Alpha-1 antitrypsin deficiency Infection

Hepatic encephalopathy
West Haven Criteria for hepatic encephalopathy
GRADE CRITERIA
I Minimal lack of awareness, euphoria or anxiety, shortened attention span, impairment of addition or subtraction, altered sleep rhythm
II Lethargy or apathy, disorientation for time, obvious personality change, inappropriate behaviour, dyspraxia, asterixis.
III Somnolence to semistupor, responsive to stimuli, confused, gross disorientation, bizarre behaviours.
IV Coma (unresponsive to verbal or noxious stimuli)

Concomitant multi-organ failure
• Challenges when patients have concomitant renal and liver dysfunction
– Choice of medications
– Level of interventions in treatment

Statistics
• 5th ‘big killer’ in England & Wales after heart, cancer, stroke and respiratory disease.
• In 2014, the number of deaths from liver disease in England rose to 11,597.
• 25% increase in liver deaths between 2001 – 2009.
• 90% of people who die from liver disease are under 70 years old.
• More than 1:10 deaths of people in their 40s are from liver disease

National End of Life Care Intelligence Network

National End of Life Care Intelligence Network

Challenges in end of life care for people with liver disease
• Over 70% people with liver disease die in hospital.
• Younger patients, often from either isolated or ethnically diverse subcultures.
• Stigma : Difficult to access care, difficult for families in bereavement
• Guilt
• Complicated course of advanced liver disease – sometimes patients can be very sick and near death, but eventually make a recovery.

Literature Review

Questions for the literature review
1. In adult patients with end stage liver disease receiving palliative care, what are the best treatments for common symptoms seen at the end of life e.g. pain, breathlessness, agitation, nausea & vomiting and respiratory secretions?
2. In adult patients with end stage liver disease receiving palliative care, what are the recommended treatments for hepatic encephalopathy, prevention and management of massive haemorrhage and hepatorenal syndrome?

Other (n=1)
CINALH (n= 165)
EMBASE
(n= 794) Cochrane (n= 2)
Medline (n=538)
Total after duplicates removed
(n= 897) Exclusions of abstracts and titles
(n=854)
Articles selected for full text review (n=43)
Exclusions full text (n=30) Study did not answer PICO 5 Poor quality study 11
Case studies 4
Study did not meet inclusion criteria 7 Unable to obtain article 3
Studies included in the updated review (n= 13)
Total (n= 1500)
Other
NICE evidence
UpToDate
Hand search (reference lists)
Exclusions
Under 18 years old
Non-English language articles
Case reports, editorials, letters

Literature Review
Evidence: Bass et al (2010) [Level 1-], Sharma et al (2013) [Level 1-], Mittal et al (2017) [Level 1-],
Gluud et al (2016) [Level 1+++]
• Little robust evidence found for managing symptoms of patients with end stage liver disease at end of life.
• Hepatic encephalopathy [Level 1++] – Lactulose reduces recurrence of HE and improves symptoms
– Rifaximin reduces recurrence of HE and improves symptoms
• No literature about management of life threatening haemorrhage in end stage liver disease receiving palliative care
• Hepatorenal syndrome – Terlipressin, Noradrenaline
– Level 1 evidence to suggest this can improve Hepatorenal syndrome – not generalisable to our population

Patient and public representative

Patient and Public Involvement
• People’s Voice 6th June 2017
– keen that NAFLD be included
– focused guideline – not too broad
– ?exclude cancer as different trajectory/management
– focus on end of life care and medications
• British Liver Trust forum
– Open opportunity to participate (8,800 followers)
– No replies received

Patient and Public Involvement
• Literature search - impact of advanced liver disease on the experience of people and those important to them

Patient and Public Involvement Key Themes
Physical • Pain comparable with advanced cancer and
more than advanced heart and lung failure • Fatigue and sleep disturbance • More concerned with pruritus and muscle
cramps than major life threatening bleeds • Impact of illness on sexuality e.g erectile
dysfunction and reduced libido

Patient and Public Involvement Key Themes
Psychological • Best predictor of quality of life • High prevalence of depression • Hepatic encephalopathy impacted significantly
on psychological wellbeing • The life course of living with advanced liver
disease is dynamic and understanding illness, trajectory, plans and prognosis positively impacted on coping

Patient and Public Involvement Key Themes
Social and Demographic • A relatively young patient population compared with other
major diseases. • Age was found to be significantly correlated with worsening
quality of life in patients with cirrhosis and experienced more acutely among the younger participants e.g: – employment, – family life and – adjustment to a diagnosis of a life-limiting illness,
compared with older patients who maybe beyond the most active phase of their lives.

Patient and Public Involvement Key Themes
Social and Demographic • In addition, male participants cited paid employment and
sexual function as their main issues in relation to their illness • Female respondents highlighted their home life and social
life as primary concerns

Proposed New Standards and Guidelines

Overview
• Section 1 : Introduction
• Section 2 : Scope and purpose
• Section 3 : Methods
• Section 4 : Guideline recommendations
– 4.1 Prognostic indicators
– 4.2 Advance care planning
– 4.3 Scenarios in advanced liver disease
– 4.4 Management of symptoms in advanced liver disease
• Section 5 : Standards

Section 4.1 Prognostic Indicators
• Child-Pugh Scores
• MELD
• May guide Advance Care Planning discussion and prompt referral to SPCT services

MELD • Reflects the function of kidney, liver and extrinsic
coagulation pathway (Na, Bil, INR, Creat)
• Complex equation therefore suggest using online calculators.
MELD SCORE 3-MONTH MORTALITY
<9 1.9%
10 - 19 6.0%
20 - 29 19.6%
30 – 39 52.6%
≥ 40 71.3%

Child-Pugh Classification
• More commonly used currently.
• Variables : serum albumin & bilirubin, ascites, encephalopathy, prothrombin time.
CLASS SCORE 1-YEAR SURVIVAL
A 5 – 6 100%
B 7 – 9 80%
C 10 – 15 45%

Definitions
• Advanced Liver Disease
– People with (MELD 30+ or Child Pugh C)
• Severe Hepatic Impairment
– Consider a dose reduction for medicines if one or more of the following are present • prothrombin time >130% of normal
• bilirubin >100micromol/L
• severe cirrhosis +/- encephalopathy
• ascites

Section 4.2 Advance Care Planning
• Advance care planning should be offered for patients with advanced liver disease plus one or more scenarios:
– diuretic resistant ascites,
– hepatic encephalopathy,
– hepatorenal syndrome,
– spontaneous bacterial peritonitis or
– recurrent variceal bleeds

Section 4.2 Advance Care Planning
• Other triggers include:
– more than 2 hospital admissions a year,
– ongoing alcohol use,
– not suitable for liver transplantation
– a WHO performance status of 3 or 4

Section 4.3 Scenarios in advanced liver disease
1. Pain
2. Hepatic encephalopathy
3. Fatigue
4. Social functioning including sexuality
5. Pruritus
6. Depression
7. Major Haemorrhage
8. Concomitant renal failure
9. Ascites
10.Continued alcohol use

Section 4.3.2 Hepatic Encephalopathy
• Hepatic encephalopathy prevention and management
1. Lactulose 10 to 30 mls qds
2. Phosphate enemas
3. Rifaximin 550mg bd
Aim to maintain 2 - 3 soft stools a day

Pain
WHO Ladder 1 and 2

Medicinal Management of Pain in Advanced Liver Disease [Level 3, Grade D]
Medicine Dose Comments
No adjustments needed
Nefopam 30-90mg PO TDS Non-opioid analgesic. Excreted in faeces. Limited evidence.
Dose or frequency adjustment needed
Paracetamol 0.5-1mg PRN up to 2g in 24 hours. Avoid in severe alcoholic hepatitis or acute liver injury.
Tramadol Reduce dose in hepatic impairment by halving the dose e.g reduce dose frequency to q12h, Tramadol 50mg BD. Avoid in decompensated cirrhosis.Prolonged-release tablets not recommended in severe hepatic dysfunction.
Hepatically metabolized to active metabolite by CYP3A4, 2D6 and glucuronidation.
Avoid use unless individual factors arise preventing use of medicines above
Nonsteroidal anti-inflammatory drugs (NSAIDS)
Avoid in advanced chronic liver disease or cirrhosis.
Associated with increased risk of variceal haemorrhage, impaired renal function and development of diuretic-resistant ascites.
Codeine Avoid in severe hepatic dysfunction. Decreased effectiveness in patients with advanced chronic liver disease/cirrhosis.
Source: Summary of Product Characteristics, electronic Medicines Compendium (eMC) and Palliative
Care Formulary, UptoDate®

Pain
WHO Ladder 3

Medicinal Management of Pain in Advanced Liver Disease [Level 3, Grade D]
Medicine Dose Comments
Dose or frequency adjustment needed
Morphine Start at 2mg PO 4-6 hourly and assess response. Use with caution in patients with advanced chronic liver disease or cirrhosis. Avoid in cirrhosis with concomitant renal failure.
Metabolised in liver. Increased oral bioavailability in advanced chronic liver disease or cirrhosis due to reduced first pass hepatic metabolism. Excreted by kidneys.
Tapentadol IR Start at 50mg 6 hourly to 8 hourly and assess response.
In moderate liver disease use low doses and prolonged dosing intervals. No data in severe liver disease.
Fentanyl Start at 50–200microgram, and subsequently 50microgram SC 1 hourly PRN. In advanced age or multi-morbidity use lower dose of 12.5micrograms to 25microgram SC 1 hourly PRN
Starting doses for CSCI of 100 to 300 micrograms over 24 hours – can be diluted in WFI or 0.9% saline
Metabolised in liver but due to large volume of distribution effect of severe liver impairment often limited. One study showed unchanged pharmacodynamics in patients with cirrhosis, although they had preserved synthetic liver function.
Source: Summary of Product Characteristics, electronic Medicines Compendium (eMC) and Palliative
Care Formulary, UptoDate® Bosilkovska et al

Medicinal Management of Pain in Advanced Liver Disease [Level 3, Grade D]
Medicine Dose Comments
Dose or frequency adjustment needed
Buprenorphine Use if opioid requirements in stable pain are the equivalent of 12mg to 36 mg of daily oral morphine equivalence
Use with caution in patients with advanced chronic liver disease or cirrhosis.
Partially metabolised in liver. Limited data
Source: Summary of Product Characteristics, electronic Medicines Compendium (eMC) and Palliative
Care Formulary, UptoDate® Bosilkovska et al

Medicinal Management of Pain in Advanced Liver Disease [Level 3, Grade D]
Medicine Dose Comments
Avoid use unless individual factors arise preventing use of medicines above
Oxycodone Start at 1mg PO 8 hourly and assess response. Use with caution at reduced doses and prolonged dosing intervals.
Metabolised in liver. Excreted by kidneys. Variable onset and analgesic efficacy in hepatic insufficiency. 50% greater peak plasma concentrations in mild-moderate hepatic impairment
Hydromorphone Increase dosing intervals in severe liver impairment i.e 1.3mg PO 8 hourly and assess response. Avoid in severe liver dysfunction with concomitant renal failure.
Metabolised in liver. Limited data. Use cautiously under Specialist Palliative Care guidance.
Alfentanil Dose should be reduced and dosing frequency extended. Fentanyl is preferred to alfentanil.
Effects prolonged and enhanced in moderate and severe hepatic failure.
Source: Summary of Product Characteristics, electronic Medicines Compendium (eMC) and Palliative
Care Formulary, UptoDate® Bosilkovska et al

Pain
Specialist Palliative Care Initiated Medicines

Medicinal Management of Pain in Advanced Liver Disease [Level 3, Grade D]
Medicine Dose Comments
Dose or frequency adjustment needed
Methadone (for analgesia)
Reduce starting dose e.g by at least 50% and titrate according to response.
Use with caution for pain. Metabolised in liver but accumulates in tissues. Use cautiously under Specialist Palliative Care guidance. In use for opioid substitution in substance misuse, usual dose may need to be adjusted.
Ketamine
(for analgesia) Dose reductions to be considered. Metabolised in the liver. Prolonged
duration of action may occur in cirrhosis or other types of liver impairment. May cause abnormal liver function tests. Use cautiously under Specialist Palliative Care guidance.
Source: Summary of Product Characteristics, electronic Medicines Compendium (eMC) and Palliative
Care Formulary, UptoDate®

Breathlessness

Medicinal Management of Breathlessness in Advanced Liver Disease [Level 3, Grade D]
Medicine Dose Comments
Dose or frequency adjustment needed
Morphine Start at 2mg PO 4-6 hourly and assess response. Use with caution in patients with advanced chronic liver disease or cirrhosis. Avoid in cirrhosis with concomitant renal failure.
Metabolised in liver. Increased oral bioavailability in advanced chronic liver disease or cirrhosis due to reduced first pass hepatic metabolism. Excreted by kidneys.
Fentanyl Start at 50–200microgram, and subsequently 50microgram SC 1 hourly PRN. In advanced age or multi-morbidity use lower dose of 12.5micrograms to 25microgram SC 1 hourly PRN
Starting doses for CSCI of 100 to 300 micrograms over 24 hours – can be diluted in WFI or 0.9% saline
Metabolised in liver but due to large volume of distribution effect of severe liver impairment often limited. One study showed unchanged pharmacodynamics in patients with cirrhosis, although they had preserved synthetic liver function.
Source: Summary of Product Characteristics, electronic Medicines Compendium (eMC) and Palliative
Care Formulary, UptoDate® Bosilkovska et al

Medicinal Management of Breathlessness in Advanced Liver Disease [Level 3, Grade D]
Medicine Dose Comments
Dose or frequency adjustment needed
Lorazepam 500 micrograms to 1mg PO/SL q4hrly PRN up to 4mg in 24 hours
Conflicting evidence. PCF consider to be generally pharmacologically safe in severe liver impairment but manufacturers recommend its use is limited in severe hepatic impairment because of risk of precipitating hepatic encephalopathy.
Midazolam Begin at 1mg to 2.5mg SC q2hrly PRN and individually titrate
Use cautiously
30–60% of the dose is metabolized through the liver. 60%-80% of dose is renally excreted.
Source: Summary of Product Characteristics, electronic Medicines Compendium (eMC) and Palliative
Care Formulary, UptoDate® Bosilkovska et al

Medicinal Management of Breathlessness in Advanced Liver Disease [Level 3, Grade D]
Medicine Dose Comments
Avoid use unless individual factors arise preventing use of medicines above
Oxycodone Start at 1mg PO 8 hourly and assess response. Use with caution at reduced doses and prolonged dosing intervals.
Metabolised in liver. Excreted by kidneys. Variable onset and analgesic efficacy in hepatic insufficiency. 50% greater peak plasma concentrations in mild-moderate hepatic impairment
Hydromorphone Increase dosing intervals in severe liver impairment i.e 1.3mg PO 8 hourly and assess response. Avoid in severe liver dysfunction with concomitant renal failure.
Metabolised in liver. Limited data. Use cautiously under Specialist Palliative Care guidance.
Alfentanil Dose should be reduced and dosing frequency extended. Fentanyl is preferred to alfentanil.
Effects prolonged and enhanced in moderate and severe hepatic failure.
Source: Summary of Product Characteristics, electronic Medicines Compendium (eMC) and Palliative
Care Formulary, UptoDate® Bosilkovska et al

Nausea and Vomiting

Medicinal Management of Nausea and Vomiting in Advanced Liver Disease [Level 3, Grade D]
Medicine Dose Comments
Dose or frequency adjustment needed
Metoclopramide Start with 10mg q12h PO PRN
If oral route unavailable, start with 10mg SC PRN or 15mg/24h in CSCI. Monitor carefully and cautiously increase dose as needed.
Metabolised in the liver. Eliminated by kidneys. Both hepatic & renal impairment result in higher plasma levels and prolonged halflife. Recommended to halve usual starting dose.
Ondansetron Maximum dose of 8mg PO/SC/IV in 24 hours. Metabolised in liver. Reduced clearance in severe liver dysfunction with prolonged serum half life.
Haloperidol Start with 250 to 500 micrograms q2 hrly PO PRN
If oral route unavailable start with 250 to 500 micrograms q2 hrly SC PRN NB SC route is twice as potent. Further doses may be administered and adjusted according to the individual’s response
Use cautiously. Limited data. Extensive liver metabolism, it is recommended to halve the initial dose.
Source: Summary of Product Characteristics, electronic Medicines Compendium (eMC) and Palliative
Care Formulary, UptoDate®

Medicinal Management of Nausea and Vomiting in Advanced Liver Disease [Level 3, Grade D]
Medicine Dose Comments
Dose or frequency adjustment needed
Levomepromazine Start at 2.5mg SC q1hrly PRN and individually titrate.
Use cautiously. Limited data. Eliminated via urine and faeces
Avoid use unless individual factors arise preventing use of medicines above
Cyclizine Avoid in severe liver disease. Increased risk of sedation in severe liver disease.
Domperidone Avoid in severe liver impairment. Metabolised in liver.
Source: Summary of Product Characteristics, electronic Medicines Compendium (eMC) and Palliative
Care Formulary, UptoDate®

Delirium

Medicinal Management of Delirium in Advanced Liver Disease [Level 3, Grade D]
Medicine Dose Comments
Dose or frequency adjustment needed
Lorazepam 500 micrograms to 1mg PO/SL q4hrly PRN up to 4mg in 24 hours
Conflicting evidence. PCF consider to be generally pharmacologically safe in severe liver impairment but manufacturers recommend its use is limited in severe hepatic impairment because of risk of precipitating hepatic encephalopathy.
Haloperidol Begin with 250 to 500 micrograms q2 hrly PO PRN
If oral route unavailable begin with 250 to 500 micrograms q2 hrly SC PRN NB SC route is twice as potent. Further doses may be administered and adjusted according to the individual’s response
Use cautiously. Limited data. Extensive liver metabolism, it is recommended to halve the initial dose.
Olanzapine Begin with 2.5mg PO nocte. Further doses may be administered and adjusted according to the individual’s response
Use cautiously. Limited data. Extensive liver metabolism. Excreted through urine and faeces. Manufacturer recommends discontinuation if hepatitis occurs Source: Summary of Product Characteristics, electronic Medicines Compendium (eMC) and Palliative
Care Formulary, UptoDate®

Terminal Agitation

Medicinal Management of Terminal Agitation[Level 3, Grade D]
Medicine Dose Comments
Dose or frequency adjustment needed
Midazolam First line. Begin at 1mg to 2.5mg SC q2hrly PRN and individually titrate
Use cautiously
30–60% of the dose is metabolized through the liver. 60%-80% of dose is renally excreted.
Levomepromazine Second line. Begin at 12.5mg to 25mg SC q1hrly PRN and individually titrate
Use cautiously. Limited data. Eliminated via urine and faeces
Phenobarbital Third line. Begin at 100 mg IM q1hrly PRN, increasing to 200mg if dose not effective after 30 minutes
Use cautiously under Specialist Palliative Care guidance. Limited data. Highly protein-bound, there is a danger of toxicity if the dose is not adjusted if the patient is hypo-albuminaemic or is jaundiced
Source: Summary of Product Characteristics, electronic Medicines Compendium (eMC) and Palliative
Care Formulary, UptoDate®

Respiratory Tract Secretions

Medicinal Management of Respiratory Tract Secretions /Colic in Advanced Liver Disease [Level 3, Grade D]
Medicine Dose Comments
No adjustments needed
Glycopyrronium 200 micrograms SC q1hrly PRN up to 1200 micrograms in 24 hours
Predominant excretion renal
Hyoscine butylbromide
20 mg SC q1hrly PRN up to 120mg in 24 hours 42 to 61% is excreted renally and 28.3 to 37% faecally
Avoid use unless individual factors arise preventing use of medicines above
Hyoscine hydrobromide
Not recommended in severe liver dysfunction Metabolised in the liver and excreted in urine
Source: Summary of Product Characteristics, electronic Medicines Compendium (eMC) and Palliative
Care Formulary, UptoDate®

Concomitant Severe Liver and Severe Renal Impairment

Pain
Non opioid analgesia
Nefopam 30mg to 90mg PO TDS
Paracetamol up to 2g in 24 hours PO/IV/PR
As Required Opioid Analgesia
Fentanyl 12.5micrograms to 25 micrograms q4hrly SC PRN
If an oral option is desired then begin with oxycodone liquid PO 1mg 8hrly
and titrate to symptoms
1mg of oral oxycodone = 20 micrograms of fentanyl SC
If Continuous Analgesia is needed
Fentanyl from 100 micrograms via CSCI/24hrs

Breathlessness
Supportive Measures
Assurance and explanation, Use of fan or cool air across face, Adequate
positioning of the patient to aid breathing, oxygen if evidence of hypoxia
Opioid
Fentanyl 12.5micrograms to 25
micrograms q4hrly SC PRN
If an oral option is desired then
begin with oxycodone liquid PO
1mg 8hrly and titrate to symptoms
1mg of oral oxycodone = 20
micrograms of fentanyl SC
Benzodiazepine
Prescribe Midazolam 1mg to
2.5mg SC up to 2-4 hourly PRN
for BREATHLESSNESS

Nausea & Vomiting
Supportive Measures
Review potential causes e.g. cough, uncontrolled pain, urinary retention,
constipation.
As Required Medication for Nausea
Haloperidol
Start with 250 to 500 micrograms q2 hrly PO PRN
If oral route unavailable start with 250 to 500 micrograms q2 hrly SC PRN
NB SC route is twice as potent.
Further doses may be administered and adjusted according to the
individual’s response
Levomepromazine
Start at 2.5mg SC q1hrly PRN and individually titrate.

Restlessness & Agitation
Review reversible causes
For example: full bladder and rectum, pain, withdrawal (medication,
nicotine, alcohol), spiritual and psychological needs
Supportive Measures
Explanation and improve environmental factors to promote calm
Midazolam 1mg to2. 5mg SC q1hrly PRN
Seek Specialist Palliative Care advice if doses above 30mg of midazolam may be
needed, higher doses may be used under specialist guidance
If evidence of distressing hallucinations prescribe haloperidol 500 microgram SC up to 2
hourly PRN and monitor for the development of extra pyramidal side effects
Levomepromazine 12.5mg to 25mg SC q1hrly PRN
Seek Specialist Palliative Care advice if doses above 25mg of levomepromazine may be
needed. higher doses may be used under specialist guidance
Under Specialist Palliative Care Guidance
Phenobarbital 100mg IM q1hrly PRN increasing to 200mg if dose not effective after 30
minutes

Supportive Measures
Explanation, Repositioning, Active Surveillance, Consider Suction
PRN – Prescribe “For SECRETIONS”:
Glycopyrronium 100 micrograms SC PRN OR
If PRN medication is used consider CSCI over 24 hours of
Glycopyrronium 600 micrograms to 1200 micrograms
Treat any side effects with frequent mouth care which may include
artificial saliva replacement gels /sprays.
Respiratory Tract Secretions

Standards 1. 100% of people with advanced liver disease (MELD 30+ or
Child Pugh C) should have an individualised management plan for hepatic encephalopathy. [Grade A]
2. 100% of people with advanced liver disease (MELD 30+ or Child Pugh C) should be offered an advance care planning discussion. [Grade D]
3. 100% of people with advanced liver disease (MELD 30+ or Child Pugh C) and an eGFR of less than 30mls/min/1.72m2 should be offered a referral to Specialist Palliative Care Services. [Grade D]

Invited Experts
Dr Richardson / Dr Owens

Discussion