Majority or Authority in a return dec Controlling Charity ... · Norfolk & Suffolk NHS Foundation...
Transcript of Majority or Authority in a return dec Controlling Charity ... · Norfolk & Suffolk NHS Foundation...
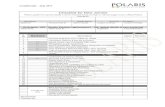
Norfolk & Suffolk NHS Foundation Trust Board of Directors – Declarations of Interest (version – 10Nov 2014)
Board of Director I:\Trust Secretariat\Board of Directors - Public\Public BoD 2014\07. 18 Dec 2014\Att A - BoD Decs of interest - Updated 10Nov2014.doc Page 1 of 6
NAME
Directorships of Private
Companies, sole trader or
PLCs
Ownership or Part Ownership of
Companies likely, or seeking, to do
business with the NHS
Majority or Controlling
Shareholdings in Organisations likely,
or seeking, to do business with the
NHS
Position of Authority in a
Charity or Voluntary Body in the Field of Health
Care, Social Services or
Housing
Material Connection with a Voluntary or
Other Body Contracting for
Services with the NHS
Declarations by Immediate
Family Members
Date of return dec
BALL, Hadrian
None None None None Secondary Care Specialist Advisor
Leicester City Clinical Commissioning Group
Wife is CEO for Norwich MIND
11.02.14
BRIERLEY, John
None None None Hon. Treasurer, Trustee and Director Norwich & Central Norfolk MIND
Hon. Treasurer, Trustee and Director Norwich & Central Norfolk MIND
None 11.02.14
BROOKS, Roz None None None None None Sister (C.E. Watson) Offender Health Commissioner at Area Team.
Husband (Dr R Brooks) undertakes S.12 work within Norfolk.
27.10.14
Norfolk & Suffolk NHS Foundation Trust Board of Directors – Declarations of Interest (version – 10Nov 2014)
Board of Director I:\Trust Secretariat\Board of Directors - Public\Public BoD 2014\07. 18 Dec 2014\Att A - BoD Decs of interest - Updated 10Nov2014.doc Page 2 of 6
NAME
Directorships of Private
Companies, sole trader or
PLCs
Ownership or Part Ownership of
Companies likely, or seeking, to do
business with the NHS
Majority or Controlling
Shareholdings in Organisations likely,
or seeking, to do business with the
NHS
Position of Authority in a
Charity or Voluntary Body in the Field of Health
Care, Social Services or
Housing
Material Connection with a Voluntary or
Other Body Contracting for
Services with the NHS
Declarations by Immediate
Family Members
Date of return dec
CREELMAN, Graham
Graham Creelman Associates Ltd
New Writing Partnership Ltd
None None Occasional consultancy work with University of East Anglia
Pro-Chancellor of Norwich University of the Arts and Visiting Professor of Media Until June 2014 Sheriff of Norwich (non-political appointment representing the interests of the City.)
Wife is MD of a television programme company which conceivably could bid for a commission to make a health-related film or video
19.02.14
HOWLETT (formerly FLEMING), Leigh
None None None None None Husband is a non-voting Director of South Essex Partnership University FT
21.03.14
Norfolk & Suffolk NHS Foundation Trust Board of Directors – Declarations of Interest (version – 10Nov 2014)
Board of Director I:\Trust Secretariat\Board of Directors - Public\Public BoD 2014\07. 18 Dec 2014\Att A - BoD Decs of interest - Updated 10Nov2014.doc Page 3 of 6
NAME
Directorships of Private
Companies, sole trader or
PLCs
Ownership or Part Ownership of
Companies likely, or seeking, to do
business with the NHS
Majority or Controlling
Shareholdings in Organisations likely,
or seeking, to do business with the
NHS
Position of Authority in a
Charity or Voluntary Body in the Field of Health
Care, Social Services or
Housing
Material Connection with a Voluntary or
Other Body Contracting for
Services with the NHS
Declarations by Immediate
Family Members
Date of return dec
HOPKINS, Andrew
None None None None
Member of Supervisory Board of the East of England Collaborative Procurement Hub (an NHS organization providing procurement services to the NHS in the East)
Partner is a partner for N A Wilson & Associates who provide management consultancy work to the NHS.
11.02.14
JEFFERYS, Peter
None None None None None None 20.02.14
MARSHALL-ROBB, Jane
Director of Changing Perspectives Ltd
None None None None None 11.02.14
NEWCOMB, Tim
None None None None None None 15.09.14
PAGE, Gary None None None Chair Hoffman Foundation for Autism
None Partner is a counsellor for Suffolk MIND
28.10.14
Norfolk & Suffolk NHS Foundation Trust Board of Directors – Declarations of Interest (version – 10Nov 2014)
Board of Director I:\Trust Secretariat\Board of Directors - Public\Public BoD 2014\07. 18 Dec 2014\Att A - BoD Decs of interest - Updated 10Nov2014.doc Page 4 of 6
NAME
Directorships of Private
Companies, sole trader or
PLCs
Ownership or Part Ownership of
Companies likely, or seeking, to do
business with the NHS
Majority or Controlling
Shareholdings in Organisations likely,
or seeking, to do business with the
NHS
Position of Authority in a
Charity or Voluntary Body in the Field of Health
Care, Social Services or
Housing
Material Connection with a Voluntary or
Other Body Contracting for
Services with the NHS
Declarations by Immediate
Family Members
Date of return dec
PARROTT, Brian
Brian Parrott Ltd
None
None None Co-chair, Association of Directors of Adult Social Services (ADASS) Associates Network Independent Chair, Safeguarding Adults Boards, London Boroughs of Richmond and Tower Hamlets
Wife is a Director of Brian Parrott Ltd
13.10.14
SAUNDERS, Marion
Non-executive director of UIA Insurance Ltd.
None None None Consultancy with Reconstruct Training
None 18.09.14
SAYER Jane
None None None None None None 17.02.14
Norfolk & Suffolk NHS Foundation Trust Board of Directors – Declarations of Interest (version – 10Nov 2014)
Board of Director I:\Trust Secretariat\Board of Directors - Public\Public BoD 2014\07. 18 Dec 2014\Att A - BoD Decs of interest - Updated 10Nov2014.doc Page 5 of 6
NAME
Directorships of Private
Companies, sole trader or
PLCs
Ownership or Part Ownership of
Companies likely, or seeking, to do
business with the NHS
Majority or Controlling
Shareholdings in Organisations likely,
or seeking, to do business with the
NHS
Position of Authority in a
Charity or Voluntary Body in the Field of Health
Care, Social Services or
Housing
Material Connection with a Voluntary or
Other Body Contracting for
Services with the NHS
Declarations by Immediate
Family Members
Date of return dec
SCOTT Michael
Director of Barrowby Management Solutions – currently dormant, has not traded for 3yrs
None None None None None 24.06.14
SMITH, Stuart
Partner in Stuart Smith Partners LLP
None None None None None 10.02.14
SMITH, Stuart Additional note (05.09.14): Max Heron a partner in SSPLLP has been engaged by Provide, the Central Essex Community Services NHS Trust, to carry out a property strategy. This work started in February 2014 and is expected to conclude within the next month. The work has been carried out through a different legal entity, Ardeola Ltd, in which Stuart Smith holds no interest. Max Heron has recently been working with several public sector organisations across health, education and local government. In particular, he is working with the East of England Local Government Association (EELGA) who are driving forward the Government's One Public Estate initiative. As part of this, Stuart Smith understands that a lead has now been appointed to look at the public estate across Norfolk and Suffolk.
SOLOMKA, Bohdan
None None None None None None 03.11.14
Norfolk & Suffolk NHS Foundation Trust Board of Directors – Declarations of Interest (version – 10Nov 2014)
Board of Director I:\Trust Secretariat\Board of Directors - Public\Public BoD 2014\07. 18 Dec 2014\Att A - BoD Decs of interest - Updated 10Nov2014.doc Page 6 of 6
NAME
Directorships of Private
Companies, sole trader or
PLCs
Ownership or Part Ownership of
Companies likely, or seeking, to do
business with the NHS
Majority or Controlling
Shareholdings in Organisations likely,
or seeking, to do business with the
NHS
Position of Authority in a
Charity or Voluntary Body in the Field of Health
Care, Social Services or
Housing
Material Connection with a Voluntary or
Other Body Contracting for
Services with the NHS
Declarations by Immediate
Family Members
Date of return dec
STOTT, Adrian Trustee – Mental Health Foundation
Board lay member of the Faculty of Public Health
Son 3-month work (10/13-1/14) for Suffolk Community Healthcare (Serco)
Son 3-month work (10/13 – 1/14) for Suffolk Community Healthcare (Serco)
17.02.14
WHITE, Debbie
None None None None None None 10.02.14
Updated 19.02.14 – February 2014 updates made Updated 24.06.14 – Cynthia Conquest removed, Michael Scott added. Updated 15.09.14 – Barry Capon removed, Kathy Chapman removed. Updated 15.09.14 – Stuart Smith additional information added regarding public estates management, following email 05.09.14 Updated 15.09.14 – Tim Newcomb and Marion Saunders added. Updated 27.10.14 - Roz Brooks added. Updated 27.10.14 – Gary Page updated entry Updated 03.11.14 - Bohdan Solomka added
Board of Directors Public, 23rd
October 2014, unconfirmed minutes
Version 0.1
Author: Lucy Want
Department: Corporate
Page 1 of 11 Date produced: 23rd
October 2014 Retention period: 30 years
B
Unconfirmed
Minutes of the Board of Directors – Public Session
held on Thursday 23rd October 2014 at the Kirkley Centre, 154 London Road South, Lowestoft, Suffolk, NR33 0AZ
Present:
Hadrian Ball: Medical Director
John Brierley: Non-Executive Director
Roz Brooks: Interim Director of Operations (Suffolk) (left 15:16)
Andrew Hopkins: Director of Finance
Peter Jefferys: Non-Executive Director
Jane Marshall-Robb: Director of Workforce & OD
Tim Newcomb: Non-Executive Director
Gary Page: Trust Chair (Chair)
Brian Parrott: Non-Executive Director
Marion Saunders: Non-Executive Director
Jane Sayer: Director of Nursing, Quality & Patient Safety
Michael Scott: Chief Executive
Stuart Smith: Non-Executive Director
Adrian Stott: Non-Executive Director (arrived 09:48)
Debbie White: Director of Operations (Norfolk & Waveney) (left 15:16)
In attendance:
Robert Nesbitt: Trust Secretary
Lucy Want: Committee & Meetings Secretary (minutes)
There were five governors, four members of staff and two representatives from the CQC in attendance.
Meeting commenced at: 09:36
There was a break: 11:46 – 12:09 and 13:12 – 13:42
Certain items were taken out of order, but for clarity the minutes reflect the agenda order.
14.136 Chair’s welcome, notification of any urgent business and apologies for absence
Date: 18 December 2014 B
Item: 14.168
Board of Directors Public, 23rd
October 2014, unconfirmed minutes
Version 0.1
Author: Lucy Want
Department: Corporate
Page 2 of 11 Date produced: 23rd
October 2014 Retention period: 30 years
The Chair welcomed those present and clarified that as this was a Board meeting held in public, questions were welcomed from the audience although precedence would be given to the Board members. Apologies for absence had been received from Leigh Howlett.
One item of urgent business had been notified to the Chair; the reappointment of hospital managers.
14.137 Standing Item: Declarations of Interest
It was noted that Brian Parrott had submitted a revised schedule. There were no further declarations of interest.
14.138 To approve the minutes of the previous public meeting held on 28th August 2014
The minutes of the meeting held on 28th August 2014 were approved with no amendments. It was confirmed that the Matters Arising had been dealt with at the September 2014 meeting.
Brian Parrott drew attention to minute 14.108 where it was stated that the Trust’s learning disability service and strategy would be taken to the October 2014 public Board meeting. Gary Page confirmed it would be taken in public and will be added to the agenda for the next public meeting.
Action 14.138
The LD service strategy to be put on agenda to come to the next available public Board meeting (December 2014 or January 2015) (Robert Nesbitt)
14.139 To receive the minutes of the Annual General Meeting, held on 19th September 2014
The minutes were reviewed and the following amendments agreed:
Jane Millar to be added to list of attendees
Apologies to be noted for Pat Southgate.
The minutes will be formally agreed at the 2015 Annual General Meeting.
14.140 Chair’s Report
Gary Page advised that he had attended a meeting with the Suffolk Youth Council which is now up and running. The relocation of the Trust’s Youth Services premises in Suffolk has been announced although the Youth Council had not been consulted on the decision. Paul Cathmoir and Mark Kittle will be meeting with the Youth Council to ensure they have the opportunity to comment on the plans.
The Board noted the report.
14.141 CEO’s report
Michael Scott highlighted the key points of his report as follows:
Board of Directors Public, 23rd
October 2014, unconfirmed minutes
Version 0.1
Author: Lucy Want
Department: Corporate
Page 3 of 11 Date produced: 23rd
October 2014 Retention period: 30 years
The stakeholder event and interviews for the Director of Operations for Suffolk are scheduled for 3rd and 4th November 2014. There are 5 candidates attending and a successful appointment is expected.
The CCG has been supportive in terms of the changes in Great Yarmouth & Waveney (GY&W) and NSFT’s relationship with them has been strengthened as a result of the process. The Joint Health Overview and Scrutiny Committee are also in support of the changes.
Staff at Carlton Court are not comfortable with the decision made and this was flagged as a risk for the BoD to monitor. Michael Scott assured the Board of his confidence that the situation is being well managed. The need for staff to have clarity on the process and timescales was emphasised and Debbie White advised that the HR processes will be carried out quickly. Redundancies are not expected although it is possible that roles will change.
Prof Michael West has agreed to speak to the Senior Management Forum on the topic of good HR practice across the NHS. The date for this is yet to be confirmed.
The Suffolk Users Forum event went well and covered subjects such as the value of listening to the voice of service users and detecting early signs of mental illness. ‘Mental wealth’ was the focus of the day.
14.142 Items for approval
i. Patient Safety and Quality Report (Dr Jane Sayer) incorporating “Min 14.48iv: update on Triangle of Care compliance”
Brian Parrott drew attention to the reference to 17 recorded medication administration errors. Jane Sayer advised that these were individual issues and did not indicate a trend. This is also monitored by the Service Governance Committee (SGC) and it was noted that the threshold for reporting errors is very low.
The number of serious incidents (SIs) remains at a consistent level and John Brierley requested that a moving average be provided to help identify any trends in the volume of incidents. The increase in Trust liaison services means that more service users with a higher risk profile are being seen, leading to an increase in SIs. Analysis shows no connection between community deaths and the timing of their last contact with services. The Board received assurance that the SGC focus on individual localities and take any issues back through the locality governance mechanisms.
Stuart Smith questioned the action being taken to reduce the number of physical assaults. Jane Sayer said that the provision of PMA training is being reviewed to ensure the focus is on de-escalation, and preventing patients reaching the point where an assault is made. East Suffolk are leading on rolling out safe wards where a number of interventions are used to reduce the likelihood of patients becoming distressed and violent; this is being rolled out gradually to other areas. It was noted that some events will always be unprovoked and unpredictable. Staffing levels were discussed and Jane Sayer advised that staffing is a concern in the Norvic Clinic and more training is being rolled out where required.
Hadrian Ball noted that there has been an increase in complaints over the last two years. Peter Jefferys agreed and advised that other Trusts are experiencing
Board of Directors Public, 23rd
October 2014, unconfirmed minutes
Version 0.1
Author: Lucy Want
Department: Corporate
Page 4 of 11 Date produced: 23rd
October 2014 Retention period: 30 years
similar increases, as are the Ombudsman. Since the Hard Truths report all complaints are centrally registered and therefore the change in reporting process may have contributed to the increase. The Board acknowledged the improvements made by the Complaints Team which has resulted in a higher quality in complaint responses.
Jane Sayer outlined the structure of the Friends and Family Test. The results reported only account for 6 days worth of data and therefore it was clarified that these are only illustrative at this stage. Three questions are currently included although it is possible to add questions and categorise these by themes to address any specific concerns that may arise.
The Triangle of Care update makes reference to two dedicated Carers Leads in the Central Norfolk Community Teams. Peter Jefferys questioned the funding arrangements as it is felt these roles would be beneficial in the majority of services. Jane Sayer advised that Central Norfolk had agreed the investment and at this stage funding in other areas has not been identified. Excellent work has taken place in other areas without a dedicated post and therefore other possibilities, such as integrating the responsibilities into another role, are being considered. John Brierley stressed the need to allocate dedicated time for staff if extra responsibilities are to be built into existing roles.
Guenever Pachent, Lead Governor, was in attendance and requested that the improvement plans resulting from the Community Service User Survey be published. Jane Sayer advised that the plans would be shared with governors and NEDs once they had been finalised by each locality. The SGC will be monitoring progress against the plans. Hadrian Ball commented that the improvement plans should address the reduction in service users who feel they have been involved in medication decisions. It was noted that the sample size had been nationally mandated and that a larger sample would be beneficial for the 2015 survey.
The Board discussed section 4.1 relating to national reporting of incidents. Staff are actively encouraged to report any potential risks to patient safety and these are collated weekly. This is monitored by the SGC.
Safe staffing was discussed, particularly in relation to Foxhall. A full time team leader has been appointed and recruitment plans are in place. Vacancies are currently being covered by support work staff. Work is ongoing with team managers to ensure shifts are covered sensibly through efficient rostering.
Brian Parrott voiced concerns regarding Chilton Houses following the recent MHA visit from the CQC. An action plan is due by the end of week commencing 20th October 2014. Marion Saunders requested assurance that the action plans are effective as several issues had been raised in previous inspections. The Board agreed that management need to be clear that not responding to action plans is unacceptable. Issues regarding ligature points were discussed; there could be a business case to invest more capital and resolve the issues, rather than having additional staff to mitigate the safety risks to individual patients. The older nature of some sites mean it is difficult to meet the increasingly stringent standards.
Assurance was given to the Board that the Trust is preparing for any consequences of the Ebola outbreak and alerts are being forwarded to Locality Managers as appropriate.
Board of Directors Public, 23rd
October 2014, unconfirmed minutes
Version 0.1
Author: Lucy Want
Department: Corporate
Page 5 of 11 Date produced: 23rd
October 2014 Retention period: 30 years
Action 14.142i
a. The SI report to include a moving average and explanatory narrative for November 2014 BoD (Jane Sayer)
b. The SI report to be broken down by locality and showing ratio of incidents to caseload / activity measures for November 2014 BoD (Jane Sayer)
c. Service improvement plans (in relation to the SU community survey) for each locality will be monitored by the Service Governance Committee for it’s December 2014 meeting and will be published once available (Jane Sayer)
ii. Board Assurance Framework (BAF)
Robert Nesbitt introduced the report by saying that a reformat of the BAF is now required to ensure the narrative flow on each theme is clear. The Board approved the reformatting of the BAF for the next meeting.
The following updates were received:
1.0 Staffing
Work has been done to look at safe caseloads and it was agreed that the BAF would be updated for the November 2014 BoD meeting. Gary Page questioned whether the risk had been reduced as indicated in section 1.4; the Executive Team will consider this in their next meeting.
The need to retain staff was emphasised and Jane Marshall-Robb confirmed that work is on-going to review exit interviews, agree recruitment incentives and identify other retention mechanisms. This will be reflected in the BAF report for the November 2014 BoD meeting.
2.0 System Confidence
Stuart Smith stated that the confidence level had been reviewed by the Finance & Performance Committee. It had been agreed this should remain as ‘amber’ due to the challenges in increasing new business and achieving 100% of CQUIN targets.
3.0 Quality
Peter Jefferys advised that there has been changes in root cause analysis reports and the SGC will follow this through to track improvements. The Board discussed the increase in demand which has led to more out of area placements, the level of demand linked to the IAPT contract and the impact seen as a result of the S75 changes.
4.0 Public relations
It was agreed that the Executive Team would review the confidence level to determine whether this could be moved to ‘amber’.
5.0 Staff morale
Jane Marshall-Robb advised that a staff engagement initiative has been launched within the Trust and it is hoped this will positively impact sickness
Board of Directors Public, 23rd
October 2014, unconfirmed minutes
Version 0.1
Author: Lucy Want
Department: Corporate
Page 6 of 11 Date produced: 23rd
October 2014 Retention period: 30 years
levels. It was noted that the last sentence of section 5.1 should reflect the decrease from last month’s 12 month high.
6.0 Maintaining and growing business
Adrian Stott advised that there has been no progress in developing a bid list or increasing the resource in the Bid Team. This was discussed further under item 14.144iv.
Michael Scott provided an update on the corporate restructure; the design phase is active and communications will be issued to staff by the end of November 2014.
7.0 Maintaining CoSRR of 3 from 2014/15 onwards
The confidence level was clarified as ‘red’. The risk was discussed further under item 14.142iii.
8.0 ICT weaknesses
The Investment Committee had agreed to keep the confidence level at ‘amber / green’ until more progress has been made.
Action 14.142ii
a. BAF format to be updated to provide a clearer narrative flow. November 2014 Bod (Robert Nesbitt)
b. Under S1, Staffing:
(1) a narrative on recording and monitoring process for safe caseloads to be included for November 2014 BoD (Debbie White for N&W, Roz Brooks for Suffolk);
(2) The Executive Team will review Datix risks 1116 and 1133 which relate to staffing issues to check whether the ratings reflect the current position. Datix and BAF to then be updated to reflect outcome of review for November 2014 BoD (Robert Nesbitt)
(3) Under mitigation, additional narrative will be added to highlight actions being taken on retention of staff. November 2014 BoD (Jane Marshall-Robb)
c. Under S4, Public Relations the Executive Team will consider whether the confidence mitigation level can move to ‘amber’ from ‘amber/red’. November 2014 BoD (Robert Nesbitt)
iii. Finance Report M06
Andrew Hopkins highlighted the main issues and actions. A recorded deficit of £330k results in a year to date deficit of £1.72m. In spite of this the continuity of service risk rating (COSRR) of 3 has been maintained. Some balance sheet provision has been released which has reduced the deficit position. Overspends on staffing, out of area placements and the non-achievement of CIP savings continue to be the three key issues. It is felt that the COSRR rating of 3 is likely to reduce to 2 in quarter 3.
£2.2m is being spent per month on temporary staffing. This is linked to safe staffing and the change in patients now seen on the wards. Approximately 35% of current spending on nursing staff is due to special observations and
Board of Directors Public, 23rd
October 2014, unconfirmed minutes
Version 0.1
Author: Lucy Want
Department: Corporate
Page 7 of 11 Date produced: 23rd
October 2014 Retention period: 30 years
therefore this is an area of focus. Work is in progress to look at rostering and to ensure the interpretation of safe staffing is consistent across all wards.
£1.25m of the CIP shortfall is due to two acute units being open in GY&W when it had been planned that only one would still be used.
Out of area placements remain higher than planned and the long term approach should focus on receiving adequate resourcing from the CCGs; although it is yet to be determined whether this would be in additional beds or community resources. Hadrian Ball reported that the External Placements Panel is aware of increasing numbers of clinically supported requests for out of area specialist placements.
The cash position was discussed and Andrew Hopkins confirmed there is an increase in cash availability due to a lower level of spend than planned. Additionally some long term debts have been collected. The receipt of the sale of St Clements is included in the plans for the 2015/16 financial year.
Brian Parrott raised questions around the impact of delayed transfers of care. Michael Scott agreed that work could be done around reducing length of stays. However, additional beds are required to reduce caseload levels within the community teams. This will enable community staff to focus on a more intensive initial support within the community, reducing the need for admissions. Tim Newcomb highlighted that the issue should not be addressed in isolation but needs to be part of the wider assessment of demand and how the Trust’s operating model should function.
Item 14.144iii was taken at this time and Stuart Smith provided the following update:
“NSFT financial position and outlook
The Trust is experiencing unprecedented demand for its services and feeling the resulting pressure, particularly in areas such as our adult community services. I would like to place on record my view that NSFT as a mental health service provider is under funded and has already endured several years of reducing funding. In the spirit of 'parity of esteem' I hope our Commissioners will recognise this, however we are where we are!
So what do we do given our deteriorating financial situation evidenced by the fact that we have moved from a Trust in Surplus to a Trust that is month on month in deficit and whose Reserves will have run out by the end of the financial year.
The Trust has implemented a Financial Recovery Plan but early signs are that despite assigning high quality leadership to this important task that this situation is not going to be turned around quickly. Particularly given our desire to ensure that the quality of our services are not compromised. The principle drivers of this deficit are well understood and include:
a) OOA placement costs which are in part a reflection of the enormous demand for services placed on our Trust compounded by the difficulty in placing service users that are ready for discharge, our Adult community teams are the bellows that have had to absorb much of this pressure and this in turn given high caseloads has led to more inpatient admissions and OOA placements.
Board of Directors Public, 23rd
October 2014, unconfirmed minutes
Version 0.1
Author: Lucy Want
Department: Corporate
Page 8 of 11 Date produced: 23rd
October 2014 Retention period: 30 years
b) High temporary staffing costs and turnover which despite strenuous recruitment activity we are still struggling to bring back to more acceptable levels whilst also increasingly focusing more on retention.
c) CIP undershoot in 2 respects, this year struggling to achieve much more than £3m against a target of £14.7m but of course this is a consequence of being unable to find substantial recurrent savings in previous years, this is also a signal that there is very little in the way of straight forward further cost savings to be found.
d) I also suspect that due to block contracts and other complexities we are providing services that are beneficial to our Service Users but not fully funded.
Given this gloomy backdrop in my opinion it will take significant extra funding OR a paradigm shift to put us back into surplus AND quite possibly both.
So what do we do in the meantime:
a) energetically pursue the Financial Recovery Plan and recognise the importance of the CIP steering group led by Cynthia Conquest
b) as a matter of urgency release the time to put high quality resource into developing an Operating Model that is sustainable going forward and it is this respect that I think we will require something of a paradigm shift, both to do the analytical, design and shaping work in the first place and probably even more difficult implementing effectively.”
The Board discussed the forecast position and it was agreed that more information regarding the COSRR trajectory and CIP scenario planning would be prepared for the November 2014 BoD meeting.
Action 14.142iii
a. The forecast report to include the COSRR trajectory for the November 2014 BoD meeting (Andrew Hopkins)
b. The Finance Report to include upside, base and downside cases for November 2014 BoD meeting (Andrew Hopkins).
iv. Business Performance Report M06
Andrew Hopkins reported that all Monitor and governance targets were green. Data completeness remains an issue. Waiting times have improved and were confirmed to be back on target.
Duncan Double questioned the impact of staff caseloads and referrals on Monitor ratings. Michael Scott advised that there is no direct feed into Monitor governance ratings although it was noted there could be a potential link if crisis resolution gatekeeping targets were not being met.
v. Monitor Compliance Framework declaration
The Board agreed to sign the governance declaration.
Andrew Hopkins recommended that the Board not sign the finance declaration as it is unlikely the Trust will maintain a COSRR rating of 3 over the next 12 months. In this case a narrative would need to be provided outlining the recovery plan. The Board approved the response and it was
Board of Directors Public, 23rd
October 2014, unconfirmed minutes
Version 0.1
Author: Lucy Want
Department: Corporate
Page 9 of 11 Date produced: 23rd
October 2014 Retention period: 30 years
agreed that the narrative would be provided by Michael Scott, Andrew Hopkins and Gary Page.
Action 14.142v
Following the decision to report ‘no’ on COSRR 3 forecast (appendix 1 (4)) a narrative report is to be agreed by Michael Scott, Andrew Hopkins and Gary Page setting out the recovery plan for submission at the end of October 2014. This is then to be circulated to the BoD (Andrew Hopkins)
vi. Updated election rules in Constituation to allow for e-voting
Robert Nesbitt advised that Bevan Brittan have integrated the electronic voting rules into the Trust’s Constitution. Members will still receive a paper ballot paper although electronic voting will also now be available. The benefits to introducing e-voting include more voting options for members, a potential increase in response levels and financial savings in postage due to fewer paper forms being returned.
The Board approved the Constitution.
14.143 Items for debate
i. Quality Account Report including update on equality objectives (Sue Barrett) incorporating “Min 14.100iii – Executive leads to be identified for each element”
Jane Sayer introduced the report outlining that significant progress has been made in achieving the quality priorities. Planning for the 2015 priorities is now required. Gary Page suggested that the process needs to be made more meaningful to patients and staff and the BoD needs to become more involved. It was noted that information captured during the strategic planning activity would be relevant to this.
The equality objectives were discussed by the Board and they expressed their thanks to Ravi Seenan for his hard work. Peter Jefferys suggested that a bank of equality and diversity questions be developed for inclusion in recruitment interviews.
Action 14.143i
a. Thanks to be passed to Ravi Seenan for his hard work in making progress on the EDS objectives (Robert Nesbitt)
b. To develop a suite of model equality questions that can be used as part of values-based selection interviews, using a co-production approach by end of February 2015 to be reported via OD&WFC (Robert Nesbitt)
c. Future EDS quality reports to be stand-alone, rather than part of the Quality Account report (Robert Nesbitt).
ii. Annual suicide and self-harm report, including National Confidential Inquiry into Suicide and Homicide (Dr Hadrian Ball), incorporating update on the Risk Assessment Audit (Dr Peter Jefferys)
Hadrian Ball explained that as a Trust we routinely audit and report suicides and deaths from undetermined injuries. The report covered the 12 months ending
Board of Directors Public, 23rd
October 2014, unconfirmed minutes
Version 0.1
Author: Lucy Want
Department: Corporate
Page 10 of 11 Date produced: 23rd
October 2014 Retention period: 30 years
31st March 2013. It was noted that 1.1 in Attachment Li should refer to ‘31 March 2013’. Further more detailed analysis of the results and key actions is required.
Hadrian Ball ran through the slides of the presentation, emphasising that caution must be used when drawing conclusions from any one set of figures. The Trust’s reported figures do fluctuate over time and are consistent with the national picture. The National Confidential Inquiry are recommending that deaths of service users within 3 days of discharge should be considered to be a ‘never event’; an event that should never happen and would show evidence of a service failure. If it is decided the Trust will adopt this approach it will come back to the BoD for approval.
Peter Jefferys advised that an assessment of 20 community incidents has taken place and outlined the outcomes of the review. Risk assessments were noted as a strength although the actions taken following the assessments could be improved.
Michael Scott noted that the Trust only holds data on those patients using their services; these account for approximately 30% of suicide cases in Norfolk and Suffolk. Information from Public Health was requested to ensure we have a full picture of the situation.
Action 14.143ii
a. NSFT’s audit data to be integrated with data from the wider public health field (i.e. those people now known to NSFT) (Hadrian Ball to provide an update to December BoD meeting on timescale)
b. A plan to address the weaknesses found in care, risk and crisis plans to go the SGC which will provide assurance to the BoD on progress – for January 2015 BoD (Debbie White for N&W, Roz Brooks for Suffolk)
14.144 Items for Information
i. Audit & Risk Committee Chair’s report from meeting on 8th October 2014 (John Brierley) including the revised Service Governance Committee ToR for approval (Peter Jefferys)
John Brierley advised that the reviews of the Register of Seals and Register of Gifts and Hospitality had been completed with no actions required.
The revised Terms of Reference (TOR) for the SGC was received. Peter Jefferys outlined the key proposal to increase the membership to involve lead clinicians from the 5 localities. The Board agreed the proposal and expanded this to ensure that both Directors of Operations, or their nominees, are also invited to ensure there is operational involvement. It was agreed that the TOR would be reviewed again in April 2015.
Action 14.144i
a. Membership to include Director of Operations x 2 or their nominees (Jane Sayer)
b. A review of the SGC TOR will take place in April 2015 – to be added to agenda planner (Robert Nesbitt)
ii. Communications Committee Chair’s report from meeting on 14th October 2014
Board of Directors Public, 23rd
October 2014, unconfirmed minutes
Version 0.1
Author: Lucy Want
Department: Corporate
Page 11 of 11 Date produced: 23rd
October 2014 Retention period: 30 years
Michael Scott requested that future reports include the graphical analysis of media covered.
The Board noted the report.
Action 14.144ii
Future reports to include graphical analysis of media coverage (Leigh Howlett)
iii. Finance & Performance Committee Chair’s report from meeting on 21st October 2014
See item 14.142iii.
iv. Investment Committee Chair’s report from meeting on 21st October 2014
It had been agreed this would be covered in the private BoD meeting to follow.
v. OD and Workforce Committee Chair’s report from meeting on 9th October 2014
The Board noted the report.
14.145 Any other urgent business, previously notified to the Chair
i. Reappointment of Hospital Managers
Robert Nesbitt tabled a paper detailing the Hospital Managers. The Board approved their reappointment for a further 12 months.
Gary Page proposed a resolution to move to the private session of the board which was carried.
14.146 Date, time and location of the next meeting
The next public meeting of the Board of Directors will be held on Thursday 18th December 2014 at 10:00 at the Public Library, Sergeants Walk, St Andrews Street North, Bury St Edmunds, Suffolk, IP33 1TZ.
Meeting closed at: 14:09
Chair: ……...…..…………………
Date: ……....…………………………….
Board of Directors – Private October 2014 Chair’s Report
Version 1.0
Author: Gary Page Department: Corporate
Page 1 of 2 Date produced: December 2014 Retention period: 30 years
Report To: Board of Directors - Public
Meeting Date: 18th December 2014
Title of Report: Chairs Report
Action Sought: For Information
Estimated time: 15 minutes
Author: Gary Page, Chair
Director:
Executive Summary:
The report details my most significant meetings and my key observations over the last month.
1.0 Interaction with External Organisations 1.1 I met with Simon Dowse of BDO Healthcare who has experience of working with Monitor
on restructuring FT’s and is bidding on providing advisory work to Trusts evaluating mutualisation as part of the Pathfinder Programme.
1.2 I met Ken Applegate, Chair of Norfolk Community Health and Care Trust 1.3 Michael Scott and I met with the Campaign to Save Mental Health Services on the
subject of support for Carers 1.4 Michael Scott and I met with a group of Norfolk and Suffolk MP’s in London to provide
an update on the challenges facing the Trust 1.5 I met with Suzy Clifford of Survivors of Bereavement by Suicide to follow up on the
successful Lowestoft launch of their third branch in Suffolk 1.6 Together with Michael Scott I am scheduled to meet with John Stammers Chair and
Andy Evans Chief Officer of the Yarmouth and Waveney CCG 1.7 I attended the East of England Mental Health Chairs Meeting 1.8 I was part of the panel deciding on the Norfolk Care Awards 1.9 I met with Alex Stewart and Bill Armstrong of Healthwatch Norfolk 2.0 Interaction with Services and Staff
2.1 I met with Cllr Tony Goldson who has joined the BOG as the Suffolk CC Partner Governor
18 December 2014
C 14.169
Board of Directors – Private October 2014 Chair’s Report
Version 1.0
Author: Gary Page Department: Corporate
Page 2 of 2 Date produced: December 2014 Retention period: 30 years
2.2 I visited the Coastal Integrated Delivery Team at Walker Close, Ipswich and met with staff who particularly wanted to focus on staff wellbeing
2.3 I attended two separate meetings with Suffolk and Norfolk Governors. The meetings were appreciated and will now be held quarterly meeting
2.4 I met with Gary Hazelden regardingThe Military Covenant and NSFT treatment for veterans where good progress is being made
2.5 I met with Dr Zeyer Win, Associate Specialist Older Peoples Services to discuss his participation in the Elisabeth Garrett Anderson programme at the Leadership Academy focussing specifically on staff engagement.
2.6 I visited Kings Lynn and met with Ian Bell manager of Child Family and Young Persons together with some of the Team, Marcus Hayward Locality Manager and A group of managers at the Fermoy Unit. I also visited The Ward and Community Teams in Fermoy and had a meeting with Andy Mack of the Wellbeing Service
2.7 I attended the Hospital Managers Committee meeting which included a briefing on the Monitor Investigation
2.8 I visited the Peddars Centre at Hellesdon and met with staff from the adult Community Team
3.0 Service User and Carers Interaction
3.1 I attended a Recovery College Workshop (Introduction to Recovery) in Bury St Edmunds and saw first head the very positive impact on service Users
3.2 I attended the North Norfolk Service Users Meeting in North Aylsham
3.3 Together with Jane Sayer I met with Anastacia Tohill, Service User
4.0 Key Observations
4.1 Obviously the Monitor investigation has dominated the past few weeks and in discussions with stakeholders there is overwhelming support for the Trust and an acknowledgement that we have a new team at the helm. Whilst staff remain “angry” there is a growing sense of a new approach emerging from the leadership of the Trust.
4.2 I was deeply impressed at seeing the impact of the Recovery Course on a Service User who arrived feeling she had been somewhat armtwisted into attending and left having signed up for a four week course on developing a Wellness Plan . We must stay the course on Imroc!!
Gary Page Chair
December 2014
Board of Directors Chief Executive Report
Version 1.2 Carol Carter
Author: Michael Scott Department: Corporate
Page 1 of 2 Date produced: 5 Dec 2014 Retention period: 30 years
Report To: Board of Directors – Public
Meeting Date: 18 December 2014
Title of Report: CEO Update
Action Sought: For Information
Estimated time: 15 minutes
Author: Michael Scott, Chief Executive
Director: Michael Scott, Chief Executive
Executive Summary: This report provides an update on the main issue, insights, observations and activities undertaken by the Chief Executive for the month.
1.0 Hammerton Court:
1.1 I attended the launch of the Hammerton Court coffee shop which was opened by the Lord Mayor of Norwich; currently the coffee shop is run by NANSA, a local charity as a ‘train and trade’ initiative for Norfolk people with disabilities.
2.0 IAPT Stakeholder Group:
2.1 I met with partners from MIND & Relate to discuss the position of this project.
Confirmation was given that the Primary Care Mental Health Service ITT has been released and is targeted go live September 2015. The Partners element of the contract is approximately £2.3m with an integrated management structure led by NSFT staff. The outcome of the meeting was very positive with a renewed commitment to partnership in this innovative new service.
3.0 Director of Workforce and OD:
3.1 As many of you will be aware, Jane Marshall-Robb tendered her resignation which was accepted. Jane had a short period of ill health and her official resignation came into effect from the 1st December 2014.
3.2 I would also like to take the opportunity in confirming that Leigh Howlett has taken on the role after a reorganisation of her portfolio. This means that the Executive Team is being slimmed down with a consequent cost saving.
4.0 Campaign Meeting:
4.1 The Chair and I met with the campaign again this month to continue our discussions. A number of service users and carers attended the meeting indicating some issues that they had previously experienced with the Trust. We focused on the positive changes we are making in Access and Assessment, links
Date: 18th
December 2014
D Item: 17.170
Board of Directors Chief Executive Report
Version 1.2 Carol Carter
Author: Michael Scott Department: Corporate
Page 2 of 2 Date produced: 5 Dec 2014 Retention period: 30 years
with the MIND crisis line and the new beds on Thurne Ward. Further discussion was held in relation to our support for carers.
5.0 Norvic Service Users Forum:
5.1 I joined the user forum for an evening of discussion and debate.
6.0 Suffolk VASP County meeting:
6.1 I was invited to speak at the Suffolk VASP and heard of their work with the Trust and current concerns.
7.0 Meeting in Westminster:
7.1 The Chair and I met with the Norfolk and Suffolk Members of Parliament for an update on the Trust’s current position, CQC actions and Monitor visit.
8.0 UNISON:
8.1 Sarah Ball and I met with Unison representatives regarding our current position in relation to ‘Annex X’. This is a key part of Agenda for Change relating to workforce change. We reached a positive agreement that we would together involve staff at a much earlier stage to become engaged in service change.
9.0 Recommendation:
9.1 The Board is asked to note the content of this report
Michael Scott Chief Executive
Report To: Board of Directors – Public
Meeting Date: 18th December 2014
Title of Report: Patient Safety and Quality Exception Report November 2014
Action Sought: For Approval
Estimated time: 15 minutes
Author: Jane Sayer, Director of Nursing, Quality and Patient Safety
Director: Jane Sayer, Director of Nursing, Quality and Patient Safety
Executive Summary:
This is an exception report on current quality and patient safety issues. Information is reported on key areas of concern or activity since the last report to the Board in November 2014. The main messages for the Board to note in this report relate to:
Developments in the quality dashboard, enabling more comparisons between services.
NHS Protect feedback on assaults to staff.
Summary feedback from the Quality Governance workshop held on the 2nd December.
1.0 Report contents
1.1 Service user safety indicators, including serious incidents, medication incidents, absconsions and assaults.
1.2 Service user and carer experience indicators including complaints. 1.3 Clinical assurance, including audit and external reports. 1.4 Quality dashboard.
2.0 Service User Safety Indicators 2.1 Serious Incidents
During November there were 16 Serious Incidents reported, which is one more than October. The most reported category was unexpected deaths of which there were ten. One of the incidents involved the death of an inpatient.
Chart 1: Trustwide serious incidents reported, April 2012 – October 2014
Date: 18 December 2014
E Item: 17.171 i.
2.2 Inquests
Inquests since the last report are detailed in Table 1.
Table 1: Summary of Inquests, November 2014
RCA Locality DOD Inquest date Inquest Verdict
453 Gt Yarmouth and Waveney 25.7.14 9.10.14 Accidental death
Suffolk CAMHS 28.7.10 10.11.14 Took her own life
466 Norfolk West 7.8.14 20.11.14 Suicide
322 NRP 26.10.13 27.11.14 Drug related death
434 Gt Yarmouth and Waveney 2.6.14 25.11.14
Died from complications following drug use
355 Norfolk West 22.10.12 6.10.14 Hanged himself. His intention at the time is not known.
446 NRP 26.6.14 14.10.14 Drug related death
2.3 Medication Errors, Absconsions and Assaults
These are now reported in the quality dashboard (Appendix 2). 2.4 Infection Prevention and Control: Seasonal flu vaccination programme
As table 2 below represents, 29% of frontline staff had been vaccinated up to 14th November with more forms arriving to process. Although there is not available an accurate comparison with last year’s figures at this stage, it would appear to be 2 to 3 % lower than 2013.
April May June July Aug Sept Oct Nov Dec Jan Feb March
12 13 14 18 10 14 17 15 17 12 9 11 13 11
13 14 15 7 21 25 8 18 17 9 15 15 8 14
14 15 20 10 25 13 27 16 15 16
0
5
10
15
20
25
30
Nu
mb
er
of
SIs
rep
ort
ed
Comparison of SIs reported from April 2012
12 13
13 14
14 15
The occupational health sessions have been completed. Therefore, there is a reliance on the flu crew to continue to vaccinate local staff. There is obviously a requirement for further encouragement for localities to focus on vaccinating a greater percentage of their clinical staff. Table 2: Flu vaccination progress, November 2014
All staff Frontline Reportable percentage
Non- Frontline
6th October to 14th November 2014
1218
894
29%
274
3.0 Service User and Carer Experience 3.1 Complaints
There were 39 complaints received in November 2014. This is a decrease of 24 from the previous month. There is no known factor at this stage to account for such a dramatic decrease.
Chart 2: Number of Complaints received monthly from April 2013
* to note October figure has been upwardly revised by two to 63 following recording of additional complaints
Of those complaints responded to in November, there continued to be a theme of communication challenges. Whilst not a trend at this stage there have been two complaints in recent months regarding staff talking in front of service users in a different language. Whilst the investigations found there was no harmful intent it highlights the importance of communication being understood by all.
One complaint responded to in this period highlighted the challenges experienced in community services and the impact this has on service users. The complainant had been referred to the Trust and was assessed by the Access and Assessment Team to require intervention by the Adult Community Service. Due to the assessed level of risk being in the low category the service user was placed in the awaiting allocation category. This means they are awaiting allocation of a care coordinator or lead professional but can access support via the team's Duty Worker system. The service user remained in this category for a period of months. The service then reviewed the cases in this category identifying the service user may benefit and receive prompt access to psychological therapy via the Wellbeing Service. The
45
26
71 66
44 50
63
39
0
10
20
30
40
50
60
70
80
April May June July Aug Sept Oct Nov Dec Jan Feb Mar
No o
f com
pla
ints
Period
Chart to show Complaints received from April 2013
13-14
14-15
13-14ave
case was forwarded on. Regrettably the service user was not informed of this review and the proposed change. The Wellbeing Service received the referral and made contact with the service user. Assessment identified that their needs were beyond the provision of the Wellbeing Service and her case was passed back to the Adult Community Service. The Trust apologised for the delays in allocating her case and the absence of continued clear communication. The service user was offered an appointment for a review.
3.2 Service User and Carer Involvement and Engagement Strategy Development Group
Members of this group have expressed that they would like more robust representation from the Board with regard to the development of the new strategy.
This request equates to representation at the monthly development meetings, as well as some very clear objectives from the Board with regard to service user and carer involvement and engagement, .i.e. how would the Board expect to see this happening across the Trust.
The group have developed five priorities/objectives with an action plan; information from the Board will be added to these priorities/actions.
3.3 Triangle of Care
The Carers Leads Advisory Group (CLAG) which monitors the implementation of the ToC across the Trust has requested representation from the Board at meetings. This will not need to be on a monthly basis - but perhaps quarterly.
The group feels very strongly that the ToC represents a real shift in culture and as a Trust we need to be implementing this ethos across our services, thus requiring a visible presence and leadership from the Board so that this way of working is driven across the Trust from the top.
4.0 Clinical Assurance
4.1 Safeguarding
4.1.1 In the same week that the Trust had its full CQC review, the CQC visited Norfolk only (excluding West and South localities) to undertake a review of safeguarding children and looked after child services. We await the report from the NSFT overall review; no information so far available. The Trust like all providers received highlight feedback from the safeguarding and LAC review inspectors on 24th October 2014. The Trust in partnership with other health providers is formulating a composite action plan in response to the initial feedback. This will be updated on receipt of the formal CQC reports; for both inspections.
4.1.2 Recent changes to the statutory guidance in the competencies and requirement of safeguarding training for health professionals will impact on NSFT’s current training strategy and compliance. This will be discussed at the Service Governance committee on the 9th December. It is likely that the Trust’s compliance with training will improve as a result of these changes.
4.1.3 The Trust has appointed Dr Bhadrinath previously a CAMHS Consultant Psychiatrist as the new Named Doctor. He took up post on 11th November 2014 and
will be working two sessions per week. Dr Bhadrinath will be concentrating on safeguarding training for medical staff and medical trainees initially.
4.2 NHS Protect
The data for assaults against NHS staff has recently been published by NHS Protect, and is available at Appendix 2. The data shows that the average number of reported assaults against NHS staff in 2013-2014 per 1000 staff is 201. The figure for NSFT is 314. This difference may be due to a number of factors, including categorisation of assaults, good reporting, or actual higher number of assaults than the national average. Last year’s figure for NSFT was 290 assaults per 1000 staff. In 2012-2013, the Trust took sanctions on 49 occasions. This figure fell to 8 in 2013-14. The figures for sanctions are low this year due to the way NHS Protect has asked for them to be collected; sanctions recorded within the period rather than relating to the sanctions for the assaults declared. This does not mean we are not gaining sanctions just they there will be several relating to this year’s assaults in next year’s submission.
4.3 CQC Full Trust Inspection
There have been no further visits from the CQC to the Trust and we are awaiting the draft report on the 18th December. The action plan identified from the initial feedback letter has been updated at the request of Monitor and this will be sent to Monitor and the CQC by the Monitor deadline of the 15th December.
4.4 Non-Executive Director Visits
Table 3: NED visits reported in November 2014:
Date NED Purpose of Visit Main Findings
2nd July Peter Jefferys
Mock CQC, Rose Ward
Reported to service at time of visit
31st July Peter Jefferys
Mock CQC, Churchill Ward
Reported to service at time of visit
27th August John Brierley
Mock CQC, Fernwood Ward
Concern about implementation of TSS. Positive staff and generally good environment. Staff appear committed and caring.
17th September
Peter Jefferys
Unannounced visit to West Norfolk
Reported to service at time of visit
6th November Peter Jefferys
Unannounced visit to West Norfolk
Excellent cascade and debrief by Locality Manager to SMT. Exciting and imaginative exploration with partners by mental health. Need to ensure reliable diary system for planned appointments maintained by CMHT. Caseload pressure on CMHT continues, aggravated by S75 social worker moves.
4.5 Quality Governance Workshop
As part of the action in response to the Foresight Partnership review, a workshop was held on the 2nd December, facilitated by Sue Rubenstein, Foresight Partnership. Twenty seven Trust staff attended, including Locality Managers, Lead Clinicians, Matrons, Directors, and governance team staff. The purpose of the workshop was to agree common understanding of the purpose of quality governance, establishing the relationship between locality and Trust governance structures, and discussing the support arrangements from the central team to enable localities to work effectively on quality. The workshop produced constructive agreements and ways forward. Some underpinning principles agreed were:
Quality governance is essential for building trust about what we do, and ensuring that we and partners are confident about the safety and effectiveness of our services.
We should learn from success as well as develop awareness of risks, seeking always to improve
We need to build on our openness and transparency and enable everyone to improve quality through the provision of accurate and clear information
The role of locality governance is:
To interpret the Trust strategy into local quality priorities with a focus on outcomes
Provide assurance and build confidence in managing risk and improving quality
To engage service users and carers in the process of improvement
To bring about change in practice, making expectations explicit and embedding learning
Specific actions are to be further agreed in discussion between locality teams and the governance team, but will include:
More focussed information to underpin locality governance meetings
Localities responsible for the dissemination of information, and to consider a variety of ways of doing this, supported by the governance team
Use experiential learning to build change, supported by service users experience.
Agree flexibility on priority setting, so localities can focus on what’s important to them
Allocation of governance practitioners to localities (from January 2015)
Reach clear understanding of roles and responsibilities
Reduce the number of action plans into achievable and SMART goals which can be delivered according to local requirements
From January 2015, localities will contribute to the Service Governance committee, and it is important that regular checks are done to ensure that the governance structure remains robust, and coherent, so reflective time is needed on a regular basis. Feedback will be collated and changes made as required.
5.0 Quality Dashboard (Appendix 2)
The Quality Dashboard is now able to provide data on rates of incidents per community contacts and bed days. This is reported by locality, so service to service
comparisons are available. Some refinement of categorisation is still underway to ensure that services are reported in correct lines.
6.0 Risks / Mitigation in Relation to the Trust Objectives (Implications for Board Assurance Framework)
6.1 Quality and patient safety issues are fundamental to the delivery of Trust objectives, and the Board’s ability to manage the performance of the Trust. Relevant mitigating action is included above, and residual risks are noted.
7.0 Recommendations
7.1 The Board of Directors is asked to note and approve the contents of this report.
Jane Sayer Director of Nursing and Quality 5th December 2014
Background Papers / Information Appendix 1: NHS Protect Appendix 2: Quality Dashboard, November 2014
Report Published 05/12/2014
Quality and Safety Dashboard(graphic version)Q3 (Oct, Nov) 2014-2015 version 2.0
Data Collated and Published by: Informatics Source of Data: Datix Page 1 of 6
Report Published 05/12/2014Risk Management by Region November 2014
0
20
40
60
80
100
120
140
160
180
DSH Assault Restraint STF Abscon. Compl. Med. Pr. Ulcer SI ward SI comm.
Trust
0
10
20
30
40
50
60
70
DSH Assault Restraint STF Abscon. Compl. Med. Pr. Ulcer SI ward SI comm.
Norfolk
0
10
20
30
40
50
60
70
DSH Assault Restraint STF Abscon. Compl. Med. Pr. Ulcer SI ward SI comm.
GT Yarmouth & Waveney
0
10
20
30
40
50
60
70
DSH Assault Restraint STF Abscon. Compl. Med. Pr. Ulcer SI ward SI comm.
Suffolk
0
10
20
30
40
50
60
70
DSH Assault Restraint STF Abscon. Compl. Med. Pr. Ulcer SI ward SI comm.
Secure Services
Commentary: The figures recorded for November show a high level of recorded events regarding restraints. This subject has received a lot of discussion over the past three months at various committees and reporting has been encouraged to identify the areas where focus for support is needed. This will be monitored and reported to the Patient Safety Group, which is identifying where NHSP staff without PMA training are unable to engage in restraint, which puts pressure on permanent staff on the ward. The implementation of the DH positive and practice guidance will closely monitor the number and type of restraints. We are awaiting guidance from NHS England on an agreed definition of restraint, as we are aware that we are high reporters in comparison with other Trusts, having encouraged staff to report any situation where we restrict movement or put hands on a service user to maintain their safety.
Key: DSH - deliberate self harm STF - slips, trips & falls Abscon. - absconsions Compl. - complaints Med. - medication errors (administration and prescription) Pr. Ulcer - pressure ulcers SI ward - serious incidents (ward based patients) SI comm. - serious incidents (community & office)
Data Collated and Published by: Informatics Source of Data: Datix Page 2 of 6
Report Published 05/12/2014Physical Assault by Locality November 2014
GT Yarmouth and Waveney
Norfolk Central
Norfolk West
NRP
Secure Services
Suffolk CountyWide
Suffolk East
Suffolk West
-5
0
5
10
15
20
25
30
35
Inci
den
ts
Physical assault by locality Balloon size is based on community contacts and occupied bed days
0
5
10
15
20
25
30
35
40
45
Dec 13 Jan 14 Feb 14 Mar 14 Apr 14 May 14 Jun 14 Jul 14 Aug 14 Sep 14 Oct 14 Nov 14
0
10
20
30
40
50
60
70
80
Loca
litie
s
Tru
st
Physical assault over 12 months by locality
Trust
GT Yarmouth and Waveney
Norfolk Central
Norfolk West
NRP
Secure Services
Suffolk CountyWide
Suffolk East
Suffolk West
Commentary: The figures shown are for assaults between service user to service user. The increase in West Suffolk occurred on Abbeygate, older persons unit and many incidents occurred around tea time; this has been picked up by the service as an issue to address. Figures for October 2014 were discussed at Patient Safety Group on 13th November. Total for all assaults was 161; (111 service user to staff and 50 service user to service user). Previous 3 months figures were total of 211, 165, 126. No significant changes in trend or significant harm were identified. Of note was that as a result of service user movement, incidents on Reed had increased from 0 in September to 12 in October and Sweetbriar had reduced from 20 in September to 3 in October, due to one patient.
Data Collated and Published by: Informatics Source of Data: Datix Page 3 of 6
Report Published 05/12/2014Absconsions by Locality November 2014
GT Yarmouth and Waveney
Norfolk Central
Norfolk West NRP
Secure Services
Suffolk CountyWide
Suffolk East
Suffolk West
-1
0
1
2
3
4
5
Inci
den
ts
Absconsions by locality
Balloon size is based on community contacts and occupied bed days
0
2
4
6
8
10
Dec 13 Jan 14 Feb 14 Mar 14 Apr 14 May 14 Jun 14 Jul 14 Aug 14 Sep 14 Oct 14 Nov 14
0
2
4
6
8
10
Loca
litie
s
Tru
st
Absconsions over 12 months by locality
Trust
GT Yarmouth and Waveney
Norfolk Central
Norfolk West
NRP
Secure Services
Suffolk CountyWide
Suffolk East
Suffolk West
Commentary: The figures shown in the table are for Mental Health Act sectioned patients only. There has been a significant drop in all areas in November, with Norfolk Central where three clients were on section 17 leave and failed to return and a fourth client went absent from NNUH, all have since returned. Figures for October 2014 were discussed at Patient Safety Group on 13th November. The total including informal patients for the month was 16. Of these, 9 were informal service users and 7 were on MHA section. The previous 3 months figures were total of 15, 10, and 17. No significant changes in trends and no harm had been identified.
Data Collated and Published by: Informatics Source of Data: Datix Page 4 of 6
Report Published 05/12/2014Medication Errors by Locality November 2014
GT Yarmouth and Waveney
Norfolk Central
Norfolk West
NRP
Secure Services
Suffolk CountyWide
Suffolk East
Suffolk West
-2
0
2
4
6
8
10
12
Inci
den
ts
Medication errors by locality Balloon size is based on community contacts and occupied bed days
0
2
4
6
8
10
12
14
16
18
20
Dec 13 Jan 14 Feb 14 Mar 14 Apr 14 May 14 Jun 14 Jul 14 Aug 14 Sep 14 Oct 14 Nov 14
0
5
10
15
20
25
30
35
Loca
litie
s
Tru
st
Medication errors over 12 months by locality
Trust
GT Yarmouth and Waveney
Norfolk Central
Norfolk West
NRP
Secure Services
Suffolk CountyWide
Suffolk East
Suffolk West
Commentary: The figures shown are for administration of medication error, no one site was responsible for the increase in Norfolk Central's reporting and Suffolk East high reporting was identified in May 2014 following an audit of medication charts. Figures for October were discussed at the Drug and Therapeutic Committee on 20th November, where it was highlighted against the National Reporting and Learning System. Whilst we were good at reporting medication events, the Trust reporting was just below the national average for Mental Health Trusts. No significant harm occurred and no one area was identified as a concern.
Data Collated and Published by: Informatics Source of Data: Datix Page 5 of 6
Report Published 05/12/2014Workforce by Region October 2014
3860.04
0%
20%
40%
60%
0
1000
2000
3000
4000
FTE Vacancies Turnover Absence Sick >= 21 d Appraisals Wellbeing
Pe
rfo
rman
ce
FTE
Trust Commentary:
0%
20%
40%
60%
0
500
1000
1500
FTE Vacancies Turnover Absence Sick >= 21 d Appraisals Wellbeing
GT Yarmouth & Waveney 1517.23
0%
20%
40%
60%
0
500
1000
1500
FTE Vacancies Turnover Absence Sick >= 21 d Appraisals Wellbeing
Norfolk
402.11
0%
20%
40%
60%
0
500
1000
1500
FTE Vacancies Turnover Absence Sick >= 21 d Appraisals Wellbeing
Secure Services
1071.09
0%
20%
40%
60%
0
500
1000
1500
FTE Vacancies Turnover Absence Sick >= 21 d Appraisals Wellbeing
Suffolk
Key: FTE - Full time equivalent Vacancies - as % of FTE Turnover - Leavers as % of FTE Absence - days as % of FTE x days (in last 12 months) Sick >= 21 d - spell over 21 days duration as % of episodes Appraisals - Staff appraised in last 12 months as % of FTE Wellbeing - Staff having a wellbeing discussion in last 12 months as % of FTE
Data Collated and Published by: Informatics Source of Data: Datix Page 6 of 6
Tables showing the number of reported physical assaults on NHS staff in 2013/14
National Summary by Sector Type
Sources
(1) NHS Protect Physical Assault Statistics 2013/14(2) Physical assaults at (1) that involved medical factors (see notes below) (3) Physical assaults at (1) that did not involve medical factors(4) NHS Workforce figures 2013 (Medical + Non-Medical) (Published by The Health and
Social Care Information Centre (HSCIC))(5) Assaults per 1,000 staff (calculation based on (4)) (6) Health body declaration of total staff (as at 31st March 2014)(7) Assaults per 1,000 staff (calculation based on (6))(8) Health body declaration of total criminal sanctions applied during the period 1st April 2013 to 31st March 2014
Notes
Sector Total Health Bodies
Total
Assaults
2013/14 (1)
Assaults Involving
Medical Factors
2013/14 (2)
Assaults NOT
Involving
Medical
Factors
2013/14 (3)
NHS Workforce
Total Staff (4)
Assaults per
1,000 Staff
(5)
Declared
Total Staff (6)
Assaults per
1,000 Staff
(7)
Declared
Sanctions (8)
Acute 158 17,900 13,349 4,551 810,838 22 898,736 20 539
Ambulance 10 1,868 508 1,360 37,131 50 41,428 45 384
Mental Health 59 47,184 38,140 9,044 211,622 223 234,860 201 719
Primary Care 37 1,731 1,487 244 72,748 24 87,233 20 7
Special 2 0 0 0 8,801 0 9,300 0 0
Total 266 68,683 53,484 15,199 1,141,140 60 1,271,557 54 1,649
Physical assault statistics (1) are validated by NHS Protect. All other data sets are the responsibility of The Health and Social Care Information Centre (HSCIC)
(4) or the individual health bodies (6) and (8). NHS Workforce figures were published by The Health and Social Care Information Centre (HSCIC) and relate to
September 2013. The health body figures were provided as at 31st March 2014. Both have been listed as there is some variance.Source (2) are the number of physical assaults where the perpetrator did not know what they were doing, or did not know what they were doing was wrong
due to medical illness, mental ill health, severe learning disability or treatment administered. These figures have been calculated by applying the percentage of
total declared assaults identified as involving medical factors, to the validated total assault figure at (1).
IMPORTANT - care should be taken when comparing assault figures as there are many factors which may influence a health body's published figures including:
a) population served b) geographical setting (i.e. rural/urban), c) level of provision of mental health, learning disability and elderly care services, d) changes in
service provision, e) health body amalgamations and splits f) embedding of reporting culture.
Page 1 of 12© NHS Protect
November 2014
NHS Protect
Tables showing the number of reported physical assaults on NHS staff in 2013/14, broken down by health body
National Listing by Health Body
Sources
(1) NHS Protect Physical Assault Statistics 2013/14(2) Physical assaults at (1) that involved medical factors (see notes below) (3) Physical assaults at (1) that did not involve medical factors(4) NHS Workforce figures 2013 (Medical + Non-Medical) (Published by The Health and Social Care Information Centre (HSCIC))(5) Assaults per 1,000 staff (calculation based on (4)) (6) Health body declaration of total staff (as at 31st March 2014)(7) Assaults per 1,000 staff (calculation based on (6))(8) Health body declaration of total criminal sanctions applied during the period 1st April 2013 to 31st March 2014
Notes
Name of Health Body
Type
Total
Assaults
(1)
Assaults
Involving
Medical
Factors (2)
Assaults NOT
Involving
Medical Factors
(3)
NHS
Workforce
Total Staff
(4)
Assaults
per 1,000
Staff (5)
Declared
Total Staff
(6)
Assaults
per 1,000
Staff (7)
Declared
Sanctions
(8)
National Total 68,683 53,484 15,199 1,141,140 60 1,271,557 54 1,649
2gether NHS Foundation Trust MEN 648 169 479 1,946 333 2,320 279 27
5 Boroughs Partnership NHS Foundation Trust MEN 948 844 104 3,388 280 3,696 256 13
Aintree University Hospital NHS Foundation Trust ACU 125 94 31 4,622 27 4,572 27 0
Airedale NHS Foundation Trust ACU 49 48 1 2,630 19 2,600 19 1
Alder Hey Childrens NHS Foundation Trust ACU 66 59 7 2,819 23 2,400 28 0
Anglian Community Enterprise CIC PCC 16 11 5 1,091 15 1,267 13 0
Ashford and St Peter's Hospitals NHS Foundation Trust ACU 48 47 1 3,361 14 3,355 14 0
Avon and Wiltshire Mental Health Partnership NHS Trust MEN 887 546 341 3,899 227 4,422 201 16
Barking, Havering and Redbridge University Hospitals NHS Trust ACU 159 144 15 5,752 28 6,604 24 5
Barnet and Chase Farm Hospitals NHS Trust ACU 68 41 27 4,255 16 4,962 14 1
Barnet, Enfield and Haringey Mental Health NHS Trust MEN 476 293 183 2,692 177 2,836 168 2
Barnsley Hospital NHS Foundation Trust ACU 106 88 18 2,852 37 3,288 32 9
Barts Health NHS Trust ACU 142 83 59 13,978 10 21,043 7 13
Basildon and Thurrock University Hospitals NHS Foundation Trust ACU 99 86 13 4,514 22 5,767 17 0
Bedford Hospital NHS Trust ACU 22 22 0 2,448 9 2,500 9 0
Berkshire Healthcare NHS Foundation Trust MEN 797 737 60 4,136 193 4,510 177 2
Birmingham and Solihull Mental Health NHS Foundation Trust MEN 1,190 213 977 4,103 290 4,737 251 4
Birmingham Children's Hospital NHS Foundation Trust ACU 53 51 2 3,355 16 3,481 15 2
Birmingham Community Healthcare NHS Trust PCC 287 282 5 5,017 57 5,843 49 1
Birmingham Women's NHS Foundation Trust ACU 2 0 2 1,624 1 1,456 1 0
Black Country Partnership NHS Foundation Trust MEN 339 264 75 1,973 172 2,472 137 0
Blackpool Teaching Hospitals NHS Foundation Trust ACU 142 134 8 6,446 22 5,625 25 4
Bolton NHS Foundation Trust ACU 81 78 3 5,301 15 5,170 16 2
Bradford District Care Trust MEN 921 272 649 2,861 322 2,989 308 0
Bradford Teaching Hospitals NHS Foundation Trust ACU 165 161 4 5,603 29 6,420 26 2
Bridgewater Community Healthcare NHS Trust PCC 15 13 2 3,316 5 3,569 4 0
Brighton and Sussex University Hospitals NHS Trust ACU 103 52 51 7,133 14 7,100 15 2
Bristol Community Health CIC PCC 15 13 2 1,107 14 1,167 13 0
Bromley Healthcare CIC PCC 33 33 0 750 44 989 33 0
Buckinghamshire Healthcare NHS Trust ACU 80 33 47 5,623 14 6,165 13 0
Burton Hospitals NHS Foundation Trust ACU 54 36 18 3,098 17 3,670 15 0
Calderdale and Huddersfield NHS Foundation Trust ACU 129 16 113 5,916 22 6,685 19 1
Calderstones Partnership NHS Foundation Trust MEN 1,195 1,195 0 1,635 731 1,088 1,098 44
Cambridge University Hospitals NHS Foundation Trust ACU 158 146 12 8,435 19 7,800 20 10
Cambridgeshire and Peterborough NHS Foundation Trust MEN 451 44 407 2,331 193 2,363 191 0
Cambridgeshire Community Services NHS Trust PCC 9 6 3 3,672 2 3,517 3 0
Camden and Islington NHS Foundation Trust MEN 221 12 209 1,872 118 1,448 153 17
Care Plus Group CIC PCC 3 3 0 792 4 866 3 0
Central and North West London NHS Foundation Trust MEN 1,259 1,229 30 6,354 198 7,393 170 12
Central Essex Community Services CIC PCC 14 13 1 1,153 12 1,200 12 0
Central London Community Healthcare NHS Trust PCC 42 23 19 3,023 14 3,480 12 1
Central Manchester University Hospitals NHS Foundation Trust ACU 480 309 171 12,486 38 13,739 35 28
Chelsea and Westminster Hospital NHS Foundation Trust ACU 110 98 12 3,293 33 3,476 32 2
Cheshire and Wirral Partnership NHS Foundation Trust MEN 605 605 0 3,370 180 3,500 173 2
Chesterfield Royal Hospital NHS Foundation Trust ACU 113 105 8 3,632 31 4,225 27 5
City Health Care Partnership CIC PCC 12 4 8 1,303 9 2,007 6 1
City Hospitals Sunderland NHS Foundation Trust ACU 126 111 15 4,982 25 4,927 26 4
Colchester Hospital University NHS Foundation Trust ACU 128 125 3 4,248 30 4,380 29 1
Cornwall Partnership NHS Foundation Trust MEN 581 558 23 1,719 338 1,914 304 2
Countess of Chester Hospital NHS Foundation Trust ACU 118 106 12 3,755 31 4,457 26 12
County Durham and Darlington NHS Foundation Trust ACU 233 152 81 8,009 29 8,840 26 4
Coventry and Warwickshire Partnership NHS Trust MEN 2,540 2,539 1 4,034 630 4,916 517 1
Croydon Health Services NHS Trust ACU 41 29 12 3,485 12 3,500 12 2
Cumbria Partnership NHS Foundation Trust MEN 383 371 12 3,716 103 5,103 75 4
Dartford and Gravesham NHS Trust ACU 135 104 31 2,491 54 2,911 46 0
Derby Hospitals NHS Foundation Trust ACU 203 158 45 7,647 27 12,172 17 0
Derbyshire Community Health Services NHS Trust PCC 244 208 36 4,341 56 4,947 49 0
Derbyshire Healthcare NHS Foundation Trust MEN 246 233 13 2,421 102 2,423 102 13
Devon Partnership NHS Trust MEN 594 589 5 2,216 268 2,366 251 0
Doncaster and Bassetlaw Hospitals NHS Foundation Trust ACU 204 138 66 6,367 32 6,512 31 0
Dorset County Hospital NHS Foundation Trust ACU 49 48 1 2,502 20 3,258 15 0
Dorset Healthcare University NHS Foundation Trust MEN 746 242 504 5,226 143 6,154 121 1
Dudley and Walsall Mental Health Partnership NHS Trust MEN 344 344 0 1,109 310 1,213 284 2
Ealing Hospital NHS Trust ACU 84 67 17 3,426 25 4,441 19 3
East and North Hertfordshire NHS Trust ACU 131 131 0 5,485 24 5,595 23 0
East Cheshire NHS Trust ACU 70 70 0 3,554 20 3,500 20 0
East Coast Community Healthcare CIC PCC 4 3 1 922 4 1,030 4 0
East Kent Hospitals University NHS Foundation Trust ACU 128 90 38 7,498 17 6,617 19 4
East Lancashire Hospitals NHS Trust ACU 223 133 90 7,553 30 7,330 30 14
East London NHS Foundation Trust MEN 1,153 1,153 0 3,629 318 4,255 271 27
East Midlands Ambulance Service NHS Trust AMB 115 18 97 2,821 41 3,800 30 91
Physical assault statistics (1) are validated by NHS Protect. All other data sets are the responsibility of The Health and Social Care Information Centre (HSCIC) (4) or the individual health bodies (6) and (8). NHS
Workforce figures were published by The Health and Social Care Information Centre (HSCIC) and relate to September 2013. The health body figures were provided as at 31st March 2014. Both have been listed
as there is some variance.
Source (2) are the number of physical assaults where the perpetrator did not know what they were doing, or did not know what they were doing was wrong due to medical illness, mental ill health, severe
learning disability or treatment administered. These figures have been calculated by applying the percentage of total declared assaults identified as involving medical factors, to the validated total assault figure
at (1).
IMPORTANT - care should be taken when comparing assault figures as there are many factors which may influence a health body's published figures including: a) population served b) geographical setting
(i.e. rural/urban), c) level of provision of mental health, learning disability and elderly care services, d) changes in service provision, e) health body amalgamations and splits f) embedding of reporting culture.
Page 2 of 12© NHS Protect
November 2014
NHS Protect
Tables showing the number of reported physical assaults on NHS staff in 2013/14, broken down by health body
National Listing by Health Body
Name of Health Body
Type
Total
Assaults
(1)
Assaults
Involving
Medical
Factors (2)
Assaults NOT
Involving
Medical Factors
(3)
NHS
Workforce
Total Staff
(4)
Assaults
per 1,000
Staff (5)
Declared
Total Staff
(6)
Assaults
per 1,000
Staff (7)
Declared
Sanctions
(8)
East Of England Ambulance Service NHS Trust AMB 188 53 135 4,080 46 4,112 46 33
East Sussex Healthcare NHS Trust ACU 123 68 55 6,934 18 7,471 16 0
Epsom and St Helier University Hospitals NHS Trust ACU 78 29 49 4,454 18 4,514 17 0
First Community Health and Care CIC PCC 5 5 0 - - 450 11 0
Frimley Park Hospital NHS Foundation Trust ACU 128 103 25 4,386 29 5,612 23 4
Gateshead Health NHS Foundation Trust ACU 161 157 4 3,664 44 3,799 42 1
George Eliot Hospital NHS Trust ACU 44 5 39 2,115 21 2,000 22 4
Gloucestershire Care Services NHS Trust PCC 65 47 18 2,628 25 2,956 22 0
Gloucestershire Hospitals NHS Foundation Trust ACU 109 94 15 7,564 14 7,252 15 2
Great Ormond Street Hospital for Children NHS Foundation Trust ACU 1 1 0 3,762 0 4,500 0 0
Great Western Hospitals NHS Foundation Trust ACU 85 19 66 5,149 17 6,162 14 0
Greater Manchester West Mental Health NHS Foundation Trust MEN 686 683 3 2,823 243 3,595 191 0
Guy’s and St Thomas NHS Foundation Trust ACU 178 89 89 12,536 14 17,366 10 65
Hampshire Hospitals NHS Foundation Trust ACU 36 36 0 5,467 7 5,571 6 1
Harrogate and District NHS Foundation Trust ACU 72 62 10 3,411 21 3,826 19 0
Heart of England NHS Foundation Trust ACU 248 226 22 10,228 24 10,388 24 0
Heatherwood and Wexham Park Hospitals NHS Foundation Trust ACU 41 41 0 3,750 11 4,014 10 0
Hertfordshire Community NHS Trust PCC 28 24 4 2,894 10 3,188 9 0
Hertfordshire Partnership University NHS Foundation Trust MEN 1,034 1,034 0 2,553 405 2,653 390 0
Hinchingbrooke Health Care NHS Trust ACU 28 14 14 1,562 18 1,896 15 0
Homerton University Hospital NHS Foundation Trust ACU 38 30 8 3,526 11 3,390 11 7
Hounslow and Richmond Community Healthcare NHS Trust PCC 7 5 2 968 7 1,020 7 0
Hull and East Yorkshire Hospitals NHS Trust ACU 251 221 30 7,621 33 8,500 30 18
Humber NHS Foundation Trust MEN 157 157 0 2,756 57 3,286 48 0
Imperial College Healthcare NHS Trust ACU 140 52 88 9,144 15 10,507 13 0
Ipswich Hospital NHS Trust ACU 104 99 5 3,745 28 4,100 25 0
Isle of Wight NHS Trust MEN 108 104 4 3,032 36 3,523 31 4
James Paget University Hospitals NHS Foundation Trust ACU 88 87 1 2,991 29 3,574 25 0
Kent and Medway NHS and Social Care Partnership Trust MEN 1,133 486 647 3,075 368 3,918 289 0
Kent Community Health NHS Trust PCC 63 52 11 5,433 12 5,487 11 0
Kettering General Hospital NHS Foundation Trust ACU 88 76 12 3,522 25 3,725 24 0
King's College Hospital NHS Foundation Trust ACU 226 99 127 8,113 28 11,358 20 9
Kingston Hospital NHS Foundation Trust ACU 67 50 17 2,705 25 3,448 19 0
Lancashire Care NHS Foundation Trust MEN 1,446 1,040 406 6,641 218 8,392 172 50
Lancashire Teaching Hospitals NHS Foundation Trust ACU 143 132 11 7,041 20 8,833 16 3
Leeds and York Partnership NHS Foundation Trust MEN 1,275 1,232 43 3,301 386 3,864 330 14
Leeds Community Healthcare NHS Trust PCC 24 20 4 2,972 8 3,500 7 0
Leeds Teaching Hospitals NHS Trust ACU 217 176 41 14,773 15 15,000 14 13
Leicestershire Partnership NHS Trust MEN 723 677 46 5,322 136 5,393 134 0
Lewisham and Greenwich NHS Trust ACU 131 111 20 3,065 43 7,540 17 1
Lincolnshire Community Health Services NHS Trust PCC 27 24 3 2,377 11 2,572 10 0
Lincolnshire Partnership NHS Foundation Trust MEN 563 527 36 1,980 284 2,160 261 3
Liverpool Community Health NHS Trust PCC 29 23 6 2,946 10 2,908 10 0
Liverpool Heart and Chest NHS Foundation Trust ACU 13 13 0 1,469 9 1,200 11 0
Liverpool Women's NHS Foundation Trust ACU 0 0 0 1,396 0 1,400 0 0
Locala Community Partnerships CIC PCC 7 4 3 1,168 6 1,193 6 0
London Ambulance Service NHS Trust AMB 414 105 309 4,511 92 4,933 84 33
Luton and Dunstable University Hospital NHS Foundation Trust ACU 67 50 17 3,635 18 6,000 11 0
Maidstone and Tunbridge Wells NHS Trust ACU 97 89 8 5,704 17 6,375 15 0
Manchester Mental Health and Social Care Trust MEN 206 174 32 1,738 119 1,704 121 3
Medway Community Healthcare CIC PCC 45 43 2 1,279 35 1,339 34 0
Medway NHS Foundation Trust ACU 116 46 70 4,007 29 3,855 30 0
Mersey Care NHS Trust MEN 841 348 493 3,757 224 4,216 199 106
Mid Cheshire Hospitals NHS Foundation Trust ACU 69 46 23 3,435 20 3,550 19 25
Mid Essex Hospital Services NHS Trust ACU 66 40 26 4,068 16 4,850 14 2
Mid Staffordshire NHS Foundation Trust ACU 135 94 41 2,845 47 2,827 48 0
Mid Yorkshire Hospitals NHS Trust ACU 118 87 31 7,927 15 8,110 15 0
Milton Keynes Hospital NHS Foundation Trust ACU 56 47 9 2,922 19 3,644 15 8
Moorfields Eye Hospital NHS Foundation Trust ACU 1 0 1 1,769 1 1,875 1 1
NAViGO Health and Social Care CIC MEN 50 45 5 485 103 660 76 0
NHS Blood and Transplant SpHa 0 0 0 5,733 0 5,500 0 0
NHS Business Services Authority SpHa 0 0 0 3,068 0 3,800 0 0
Norfolk and Norwich University Hospitals NHS Foundation Trust ACU 206 193 13 6,911 30 8,022 26 5
Norfolk and Suffolk NHS Foundation Trust MEN 1,220 944 276 3,948 309 3,888 314 8
Norfolk Community Health and Care NHS Trust PCC 83 70 13 2,627 32 2,980 28 0
North Bristol NHS Trust ACU 170 166 4 8,821 19 9,000 19 0
North Cumbria University Hospitals NHS Trust ACU 95 88 7 3,903 24 3,975 24 0
North East Ambulance Service NHS Trust AMB 73 26 47 2,290 32 2,397 30 30
North East London NHS Foundation Trust MEN 200 200 0 5,439 37 6,000 33 0
North Essex Partnership University NHS Foundation Trust MEN 375 248 127 1,994 188 2,087 180 8
North Middlesex University Hospital NHS Trust ACU 12 9 3 2,384 5 2,640 5 0
North Somerset Community Partnership CIC PCC 2 2 0 618 3 644 3 0
North Staffordshire Combined Healthcare NHS Trust MEN 398 381 17 1,439 277 1,591 250 7
North Tees and Hartlepool NHS Foundation Trust ACU 123 111 12 5,412 23 5,308 23 1
North West Ambulance Service NHS Trust AMB 377 178 199 4,798 79 5,178 73 79
North West London Hospitals NHS Trust ACU 130 114 16 4,754 27 4,500 29 3
Northampton General Hospital NHS Trust ACU 208 205 3 4,687 44 4,400 47 3
Northamptonshire Healthcare NHS Foundation Trust MEN 736 707 29 3,483 211 4,274 172 8
Northern Devon Healthcare NHS Trust ACU 133 126 7 4,354 31 4,362 30 1
Northern Lincolnshire and Goole NHS Foundation Trust ACU 107 66 41 5,864 18 8,449 13 0
Northumberland, Tyne and Wear NHS Foundation Trust MEN 3,335 3,225 110 6,020 554 6,464 516 25
Northumbria Healthcare NHS Foundation Trust ACU 282 224 58 8,402 34 9,126 31 0
Nottingham CityCare Partnership CIC PCC 5 4 1 1,311 4 1,734 3 1
Nottingham University Hospitals NHS Trust ACU 284 222 62 13,319 21 14,470 20 7
Nottinghamshire Healthcare NHS Trust MEN 1,363 1,224 139 8,830 154 8,848 154 48
Oxford Health NHS Foundation Trust MEN 690 679 11 5,666 122 6,250 110 0
Oxford University Hospitals NHS Trust ACU 170 154 16 10,470 16 11,598 15 3
Oxleas NHS Foundation Trust MEN 474 0 474 3,197 148 3,471 137 0
Papworth Hospital NHS Foundation Trust ACU 28 28 0 1,799 16 2,082 13 0
Peninsular Community Health CIC PCC 89 84 5 2,075 43 2,015 44 0
Pennine Acute Hospitals NHS Trust ACU 209 162 47 9,233 23 9,308 22 29
Pennine Care NHS Foundation Trust MEN 615 584 31 5,920 104 7,033 87 6
Peterborough and Stamford Hospitals NHS Foundation Trust ACU 88 67 21 3,751 23 4,652 19 0
Plymouth Community Healthcare CIC PCC 173 173 0 2,179 79 2,129 81 2
Plymouth Hospitals NHS Trust ACU 176 47 129 6,249 28 6,000 29 0
Page 3 of 12© NHS Protect
November 2014
NHS Protect
Tables showing the number of reported physical assaults on NHS staff in 2013/14, broken down by health body
National Listing by Health Body
Name of Health Body
Type
Total
Assaults
(1)
Assaults
Involving
Medical
Factors (2)
Assaults NOT
Involving
Medical Factors
(3)
NHS
Workforce
Total Staff
(4)
Assaults
per 1,000
Staff (5)
Declared
Total Staff
(6)
Assaults
per 1,000
Staff (7)
Declared
Sanctions
(8)
Poole Hospital NHS Foundation Trust ACU 90 56 34 3,576 25 4,350 21 0
Portsmouth Hospitals NHS Trust ACU 88 80 8 6,174 14 6,319 14 0
Queen Victoria Hospital NHS Foundation Trust ACU 5 2 3 939 5 1,192 4 0
Rotherham, Doncaster and South Humber NHS Foundation Trust MEN 1,070 1,062 8 3,797 282 3,800 282 9
Royal Berkshire NHS Foundation Trust ACU 188 75 113 5,218 36 4,200 45 1
Royal Brompton and Harefield NHS Foundation Trust ACU 2 2 0 3,223 1 2,500 1 0
Royal Cornwall Hospitals NHS Trust ACU 142 137 5 5,498 26 6,500 22 3
Royal Devon and Exeter NHS Foundation Trust ACU 119 38 81 6,198 19 7,081 17 1
Royal Free London NHS Foundation Trust ACU 38 13 25 5,003 8 6,695 6 0
Royal Liverpool and Broadgreen University Hospitals NHS Trust ACU 141 113 28 5,935 24 5,766 24 9
Royal National Hospital for Rheumatic Diseases NHS Foundation Trust ACU 0 0 0 274 0 349 0 0
Royal National Orthopaedic Hospital NHS Trust ACU 10 9 1 1,375 7 2,517 4 0
Royal Surrey County Hospital NHS Foundation Trust ACU 69 62 7 3,614 19 3,544 19 0
Royal United Hospital Bath NHS Trust ACU 127 83 44 4,098 31 5,195 24 4
Salford Royal NHS Foundation Trust ACU 227 217 10 6,548 35 6,341 36 2
Salisbury NHS Foundation Trust ACU 82 80 2 3,266 25 3,952 21 2
Sandwell and West Birmingham Hospitals NHS Trust ACU 176 129 47 7,379 24 11,129 16 0
Seqol PCC 117 39 78 - - 876 134 0
Sheffield Children’s NHS Foundation Trust ACU 164 162 2 2,795 59 2,989 55 0
Sheffield Health and Social Care NHS Foundation Trust MEN 1,143 804 339 2,738 417 3,180 359 0
Sheffield Teaching Hospitals NHS Foundation Trust ACU 230 208 22 14,792 16 15,923 14 3
Sherwood Forest Hospitals NHS Foundation Trust ACU 140 40 100 4,368 32 4,136 34 0
Shrewsbury and Telford Hospital NHS Trust ACU 271 245 26 5,431 50 6,391 42 9
Shropshire Community Health NHS Trust PCC 20 20 0 1,636 12 1,745 11 0
Solent NHS Trust MEN 134 125 9 3,848 35 4,079 33 0
Somerset Partnership NHS Foundation Trust MEN 541 349 192 3,780 143 4,454 121 54
South Central Ambulance Service NHS Foundation Trust AMB 132 24 108 2,823 47 3,116 42 21
South Devon Healthcare NHS Foundation Trust ACU 55 36 19 4,144 13 4,681 12 1
South East Coast Ambulance Service NHS Foundation Trust AMB 113 22 91 3,409 33 3,661 31 9
South Essex Partnership University NHS Foundation Trust MEN 494 429 65 5,985 83 7,063 70 5
South London and Maudsley NHS Foundation Trust MEN 1,192 477 715 4,627 258 4,358 274 28
South Staffordshire and Shropshire Healthcare NHS Foundation Trust MEN 942 910 32 3,453 273 3,452 273 8
South Tees Hospitals NHS Foundation Trust ACU 188 161 27 8,975 21 9,151 21 4
South Tyneside NHS Foundation Trust ACU 94 88 6 4,483 21 4,996 19 4
South Warwickshire NHS Foundation Trust ACU 95 51 44 4,123 23 4,206 23 1
South West London and St George's Mental Health NHS Trust MEN 387 387 0 2,113 183 2,963 131 17
South West Yorkshire Partnership NHS Foundation Trust) MEN 706 193 513 4,827 146 5,161 137 0
South Western Ambulance Service NHS Foundation Trust AMB 139 14 125 4,156 33 5,166 27 38
Southend University Hospital NHS Foundation Trust ACU 62 47 15 4,738 13 4,524 14 0
Southern Health NHS Foundation Trust MEN 2,731 2,618 113 7,719 354 8,996 304 0
Southport and Ormskirk Hospital NHS Trust ACU 61 59 2 3,515 17 3,613 17 0
St George's Healthcare NHS Trust ACU 78 34 44 7,849 10 7,950 10 3
St Helens and Knowsley Hospitals NHS Trust ACU 73 35 38 4,649 16 5,618 13 0
Staffordshire and Stoke On Trent Partnership NHS Trust PCC 45 40 5 4,823 9 6,401 7 0
Stockport NHS Foundation Trust ACU 187 168 19 5,907 32 5,851 32 4
Suffolk Community Healthcare PCC 5 4 1 - - 1,007 5 0
Surrey and Borders Partnership NHS Foundation Trust MEN 392 392 0 2,651 148 2,400 163 4
Surrey and Sussex Healthcare NHS Trust ACU 100 99 1 3,565 28 3,631 28 0
Sussex Community NHS Trust PCC 87 83 4 4,343 20 4,982 17 0
Sussex Partnership NHS Foundation Trust MEN 596 587 9 4,149 144 4,500 132 12
Tameside Hospital NHS Foundation Trust ACU 96 79 17 2,473 39 2,500 38 8
Taunton and Somerset NHS Foundation Trust ACU 108 73 35 4,084 26 4,745 23 3
Tavistock and Portman NHS Foundation Trust MEN 82 82 0 538 152 572 143 0
Tees, Esk and Wear Valleys NHS Foundation Trust MEN 1,548 1,501 47 6,100 254 7,178 216 0
The Christie NHS Foundation Trust ACU 3 3 0 2,480 1 2,500 1 0
The Clatterbridge Cancer Centre NHS Foundation Trust ACU 5 5 0 920 5 931 5 0
The Dudley Group NHS Foundation Trust ACU 128 57 71 4,689 27 5,597 23 3
The Hillingdon Hospitals NHS Foundation Trust ACU 48 29 19 2,856 17 3,305 15 7
The Newcastle Upon Tyne Hospitals NHS Foundation Trust ACU 201 161 40 13,418 15 13,336 15 4
The Princess Alexandra Hospital NHS Trust ACU 47 43 4 2,947 16 2,706 17 2
The Queen Elizabeth Hospital King's Lynn NHS Foundation Trust ACU 105 103 2 2,900 36 3,416 31 0
The Robert Jones and Agnes Hunt Orthopaedic and District Hospital NHS Trust ACU 24 21 3 1,280 19 1,482 16 0
The Rotherham NHS Foundation Trust ACU 76 7 69 4,216 18 4,403 17 0
The Royal Bournemouth and Christchurch Hospitals NHS Foundation Trust ACU 146 73 73 4,209 35 5,037 29 1
The Royal Marsden NHS Foundation Trust ACU 12 10 2 3,798 3 3,500 3 0
The Royal Orthopaedic Hospital NHS Foundation Trust ACU 4 4 0 915 4 941 4 0
The Royal Wolverhampton Hospitals NHS Trust ACU 67 58 9 6,827 10 7,500 9 0
The Walton Centre NHS Foundation Trust ACU 44 40 4 1,193 37 1,200 37 0
The Whittington Hospital NHS Trust ACU 64 24 40 4,063 16 4,088 16 3
Torbay & Southern Devon Health and Care NHS Trust PCC 50 49 1 2,034 25 2,454 20 1
United Lincolnshire Hospitals NHS Trust ACU 171 137 34 7,324 23 7,500 23 5
University College London Hospitals NHS Foundation Trust ACU 122 46 76 7,838 16 8,750 14 11
University Hospital of North Staffordshire NHS Trust ACU 131 42 89 7,216 18 9,227 14 0
University Hospital of South Manchester NHS Foundation Trust ACU 95 90 5 5,915 16 5,100 19 0
University Hospital Southampton NHS Foundation Trust ACU 206 96 110 8,814 23 10,177 20 8
University Hospitals Birmingham NHS Foundation Trust ACU 72 39 33 8,255 9 8,624 8 10
University Hospitals Bristol NHS Foundation Trust ACU 318 264 54 8,098 39 9,610 33 35
University Hospitals Coventry and Warwickshire NHS Trust ACU 156 136 20 6,868 23 7,781 20 5
University Hospitals of Leicester NHS Trust ACU 165 59 106 11,361 15 13,074 13 0
University Hospitals of Morecambe Bay NHS Foundation Trust ACU 156 64 92 4,920 32 5,693 27 1
Virgin Care - Integrated Children's Services PCC 27 26 1 - - 1,100 25 0
Virgin Care - Surrey Community Health PCC 16 16 0 - - 2,532 6 0
Walsall Healthcare NHS Trust ACU 134 106 28 4,143 32 4,994 27 0
Warrington and Halton Hospitals NHS Foundation Trust ACU 168 114 54 3,949 43 3,987 42 7
West Hertfordshire Hospitals NHS Trust ACU 149 145 4 4,121 36 4,343 34 0
West London Mental Health NHS Trust MEN 818 818 0 3,270 250 3,185 257 103
West Middlesex University Hospital NHS Trust ACU 71 68 3 1,833 39 1,800 39 3
West Midlands Ambulance Service NHS Foundation Trust AMB 207 57 150 3,813 54 4,386 47 25
West Suffolk NHS Foundation Trust ACU 83 78 5 3,052 27 3,976 21 0
Western Sussex Hospitals NHS Foundation Trust ACU 118 83 35 6,506 18 8,071 15 2
Weston Area Health NHS Trust ACU 90 84 6 1,767 51 2,000 45 0
Wirral Community NHS Trust PCC 2 2 0 1,332 2 1,380 1 0
Wirral University Teaching Hospital NHS Foundation Trust ACU 173 115 58 5,868 29 5,500 31 3
Worcestershire Acute Hospitals NHS Trust ACU 120 58 62 5,811 21 6,067 20 0
Worcestershire Health and Care NHS Trust MEN 256 255 1 3,998 64 4,131 62 0
Page 4 of 12© NHS Protect
November 2014
NHS Protect
Tables showing the number of reported physical assaults on NHS staff in 2013/14, broken down by health body
National Listing by Health Body
Name of Health Body
Type
Total
Assaults
(1)
Assaults
Involving
Medical
Factors (2)
Assaults NOT
Involving
Medical Factors
(3)
NHS
Workforce
Total Staff
(4)
Assaults
per 1,000
Staff (5)
Declared
Total Staff
(6)
Assaults
per 1,000
Staff (7)
Declared
Sanctions
(8)
Wrightington, Wigan and Leigh NHS Foundation Trust ACU 141 117 24 4,715 30 4,848 29 20
Wye Valley NHS Trust ACU 79 78 1 2,795 28 3,847 21 1
Yeovil District Hospital NHS Foundation Trust ACU 77 67 10 1,950 39 2,223 35 0
York Teaching Hospital NHS Foundation Trust ACU 110 59 51 8,376 13 9,100 12 7
Yorkshire Ambulance Service NHS Trust AMB 110 11 99 4,430 25 4,679 24 25
Your Healthcare CIC PCC 16 16 0 618 26 759 21 0
Page 5 of 12© NHS Protect
November 2014
NHS Protect
Tables showing the number of reported physical assaults on NHS staff in 2013/14, broken down by health body
Acute Sector
Sources
(1) NHS Protect Physical Assault Statistics 2013/14(2) Physical assaults at (1) that involved medical factors (see notes below) (3) Physical assaults at (1) that did not involve medical factors(4) NHS Workforce figures 2013 (Medical + Non-Medical) (Published by The Health and Social Care Information Centre (HSCIC))(5) Assaults per 1,000 staff (calculation based on (4)) (6) Health body declaration of total staff (as at 31st March 2014)(7) Assaults per 1,000 staff (calculation based on (6))(8) Health body declaration of total criminal sanctions applied during the period 1st April 2013 to 31st March 2014
Notes
Name of Health Body Total
Assaults
(1)
Assaults
Involving
Medical
Factors (2)
Assaults NOT
Involving
Medical
Factors (3)
NHS
Workforce
Total Staff
(4)
Assaults
per 1,000
Staff (5)
Declared
Total Staff
(6)
Assaults
per 1,000
Staff (7)
Declared
Sanctions
(8)
Sector Total 17,900 13,349 4,551 810,838 898,736 901,236 20 539
Aintree University Hospital NHS Foundation Trust 125 94 31 4,622 27 4,572 27 0
Airedale NHS Foundation Trust 49 48 1 2,630 19 2,600 19 1
Alder Hey Childrens NHS Foundation Trust 66 59 7 2,819 23 2,400 28 0
Ashford and St Peter's Hospitals NHS Foundation Trust 48 47 1 3,361 14 3,355 14 0
Barking, Havering and Redbridge University Hospitals NHS Trust 159 144 15 5,752 28 6,604 24 5
Barnet and Chase Farm Hospitals NHS Trust 68 41 27 4,255 16 4,962 14 1
Barnsley Hospital NHS Foundation Trust 106 88 18 2,852 37 3,288 32 9
Barts Health NHS Trust 142 83 59 13,978 10 21,043 7 13
Basildon and Thurrock University Hospitals NHS Foundation Trust 99 86 13 4,514 22 5,767 17 0
Bedford Hospital NHS Trust 22 22 0 2,448 9 2,500 9 0
Birmingham Children's Hospital NHS Foundation Trust 53 51 2 3,355 16 3,481 15 2
Birmingham Women's NHS Foundation Trust 2 0 2 1,624 1 1,456 1 0
Blackpool Teaching Hospitals NHS Foundation Trust 142 134 8 6,446 22 5,625 25 4
Bolton NHS Foundation Trust 81 78 3 5,301 15 5,170 16 2
Bradford Teaching Hospitals NHS Foundation Trust 165 161 4 5,603 29 6,420 26 2
Brighton and Sussex University Hospitals NHS Trust 103 52 51 7,133 14 7,100 15 2
Buckinghamshire Healthcare NHS Trust 80 33 47 5,623 14 6,165 13 0
Burton Hospitals NHS Foundation Trust 54 36 18 3,098 17 3,670 15 0
Calderdale and Huddersfield NHS Foundation Trust 129 16 113 5,916 22 6,685 19 1
Cambridge University Hospitals NHS Foundation Trust 158 146 12 8,435 19 7,800 20 10
Central Manchester University Hospitals NHS Foundation Trust 480 309 171 12,486 38 13,739 35 28
Chelsea and Westminster Hospital NHS Foundation Trust 110 98 12 3,293 33 3,476 32 2
Chesterfield Royal Hospital NHS Foundation Trust 113 105 8 3,632 31 4,225 27 5
City Hospitals Sunderland NHS Foundation Trust 126 111 15 4,982 25 4,927 26 4
Colchester Hospital University NHS Foundation Trust 128 125 3 4,248 30 4,380 29 1
Countess of Chester Hospital NHS Foundation Trust 118 106 12 3,755 31 4,457 26 12
County Durham and Darlington NHS Foundation Trust 233 152 81 8,009 29 8,840 26 4
Croydon Health Services NHS Trust 41 29 12 3,485 12 3,500 12 2
Dartford and Gravesham NHS Trust 135 104 31 2,491 54 2,911 46 0
Derby Hospitals NHS Foundation Trust 203 158 45 7,647 27 12,172 17 0
Doncaster and Bassetlaw Hospitals NHS Foundation Trust 204 138 66 6,367 32 6,512 31 0
Dorset County Hospital NHS Foundation Trust 49 48 1 2,502 20 3,258 15 0
Ealing Hospital NHS Trust 84 67 17 3,426 25 4,441 19 3
East and North Hertfordshire NHS Trust 131 131 0 5,485 24 5,595 23 0
East Cheshire NHS Trust 70 70 0 3,554 20 3,500 20 0
East Kent Hospitals University NHS Foundation Trust 128 90 38 7,498 17 6,617 19 4
East Lancashire Hospitals NHS Trust 223 133 90 7,553 30 7,330 30 14
East Sussex Healthcare NHS Trust 123 68 55 6,934 18 7,471 16 0
Epsom and St Helier University Hospitals NHS Trust 78 29 49 4,454 18 4,514 17 0
Frimley Park Hospital NHS Foundation Trust 128 103 25 4,386 29 5,612 23 4
Gateshead Health NHS Foundation Trust 161 157 4 3,664 44 3,799 42 1
George Eliot Hospital NHS Trust 44 5 39 2,115 21 2,000 22 4
Gloucestershire Hospitals NHS Foundation Trust 109 94 15 7,564 14 7,252 15 2
Great Ormond Street Hospital for Children NHS Foundation Trust 1 1 0 3,762 0 4,500 0 0
Great Western Hospitals NHS Foundation Trust 85 19 66 5,149 17 6,162 14 0
Guy’s and St Thomas’ NHS Foundation Trust 178 89 89 12,536 14 17,366 10 65
Hampshire Hospitals NHS Foundation Trust 36 36 0 5,467 7 5,571 6 1
Harrogate and District NHS Foundation Trust 72 62 10 3,411 21 3,826 19 0
Heart of England NHS Foundation Trust 248 226 22 10,228 24 10,388 24 0
Heatherwood and Wexham Park Hospitals NHS Foundation Trust 41 41 0 3,750 11 4,014 10 0
Hinchingbrooke Health Care NHS Trust 28 14 14 1,562 18 1,896 15 0
Homerton University Hospital NHS Foundation Trust 38 30 8 3,526 11 3,390 11 7
Hull and East Yorkshire Hospitals NHS Trust 251 221 30 7,621 33 8,500 30 18
Imperial College Healthcare NHS Trust 140 52 88 9,144 15 10,507 13 0
Ipswich Hospital NHS Trust 104 99 5 3,745 28 4,100 25 0
James Paget University Hospitals NHS Foundation Trust 88 87 1 2,991 29 3,574 25 0
Kettering General Hospital NHS Foundation Trust 88 76 12 3,522 25 3,725 24 0
King's College Hospital NHS Foundation Trust 226 99 127 8,113 28 11,358 20 9
Kingston Hospital NHS Foundation Trust 67 50 17 2,705 25 3,448 19 0
Lancashire Teaching Hospitals NHS Foundation Trust 143 132 11 7,041 20 8,833 16 3
Leeds Teaching Hospitals NHS Trust 217 176 41 14,773 15 15,000 14 13
Lewisham and Greenwich NHS Trust 131 111 20 3,065 43 7,540 17 1
IMPORTANT - care should be taken when comparing assault figures as there are many factors which may influence a health body's published figures including: a) population served b)
geographical setting (i.e. rural/urban), c) level of provision of mental health, learning disability and elderly care services, d) changes in service provision, e) health body amalgamations and
splits f) embedding of reporting culture.
Physical assault statistics (1) are validated by NHS Protect. All other data sets are the responsibility of The Health and Social Care Information Centre (HSCIC) (4) or the individual health bodies
(6) and (8). NHS Workforce figures were published by The Health and Social Care Information Centre (HSCIC) and relate to September 2013. The health body figures were provided as at 31st
March 2014. Both have been listed as there is some variance.Source (2) are the number of physical assaults where the perpetrator did not know what they were doing, or did not know what they were doing was wrong due to medical illness, mental ill
health, severe learning disability or treatment administered. These figures have been calculated by applying the percentage of total declared assaults identified as involving medical factors, to
the validated total assault figure at (1).
Page 6 of 12© NHS Protect
November 2014
NHS Protect
Tables showing the number of reported physical assaults on NHS staff in 2013/14, broken down by health body
Acute Sector
Name of Health Body Total
Assaults
(1)
Assaults
Involving
Medical
Factors (2)
Assaults NOT
Involving
Medical
Factors (3)
NHS
Workforce
Total Staff
(4)
Assaults
per 1,000
Staff (5)
Declared
Total Staff
(6)
Assaults
per 1,000
Staff (7)
Declared
Sanctions
(8)
Liverpool Heart and Chest NHS Foundation Trust 13 13 0 1,469 9 1,200 11 0
Liverpool Women's NHS Foundation Trust 0 0 0 1,396 0 1,400 0 0
Luton and Dunstable University Hospital NHS Foundation Trust 67 50 17 3,635 18 6,000 11 0
Maidstone and Tunbridge Wells NHS Trust 97 89 8 5,704 17 6,375 15 0
Medway NHS Foundation Trust 116 46 70 4,007 29 3,855 30 0
Mid Cheshire Hospitals NHS Foundation Trust 69 46 23 3,435 20 3,550 19 25
Mid Essex Hospital Services NHS Trust 66 40 26 4,068 16 4,850 14 2
Mid Staffordshire NHS Foundation Trust 135 94 41 2,845 47 2,827 48 0
Mid Yorkshire Hospitals NHS Trust 118 87 31 7,927 15 8,110 15 0
Milton Keynes Hospital NHS Foundation Trust 56 47 9 2,922 19 3,644 15 8
Moorfields Eye Hospital NHS Foundation Trust 1 0 1 1,769 1 1,875 1 1
Norfolk and Norwich University Hospitals NHS Foundation Trust 206 193 13 6,911 30 8,022 26 5
North Bristol NHS Trust 170 166 4 8,821 19 9,000 19 0
North Cumbria University Hospitals NHS Trust 95 88 7 3,903 24 3,975 24 0
North Middlesex University Hospital NHS Trust 12 9 3 2,384 5 2,640 5 0
North Tees and Hartlepool NHS Foundation Trust 123 111 12 5,412 23 5,308 23 1
North West London Hospitals NHS Trust 130 114 16 4,754 27 4,500 29 3
Northampton General Hospital NHS Trust 208 205 3 4,687 44 4,400 47 3
Northern Devon Healthcare NHS Trust 133 126 7 4,354 31 4,362 30 1
Northern Lincolnshire and Goole NHS Foundation Trust 107 66 41 5,864 18 8,449 13 0
Northumbria Healthcare NHS Foundation Trust 282 224 58 8,402 34 9,126 31 0
Nottingham University Hospitals NHS Trust 284 222 62 13,319 21 14,470 20 7
Oxford University Hospitals NHS Trust 170 154 16 10,470 16 11,598 15 3
Papworth Hospital NHS Foundation Trust 28 28 0 1,799 16 2,082 13 0
Pennine Acute Hospitals NHS Trust 209 162 47 9,233 23 9,308 22 29
Peterborough and Stamford Hospitals NHS Foundation Trust 88 67 21 3,751 23 4,652 19 0
Plymouth Hospitals NHS Trust 176 47 129 6,249 28 6,000 29 0
Poole Hospital NHS Foundation Trust 90 56 34 3,576 25 4,350 21 0
Portsmouth Hospitals NHS Trust 88 80 8 6,174 14 6,319 14 0
Queen Victoria Hospital NHS Foundation Trust 5 2 3 939 5 1,192 4 0
Royal Berkshire NHS Foundation Trust 188 75 113 5,218 36 4,200 45 1
Royal Brompton and Harefield NHS Foundation Trust 2 2 0 3,223 1 2,500 1 0
Royal Cornwall Hospitals NHS Trust 142 137 5 5,498 26 6,500 22 3
Royal Devon and Exeter NHS Foundation Trust 119 38 81 6,198 19 7,081 17 1
Royal Free London NHS Foundation Trust 38 13 25 5,003 8 6,695 6 0
Royal Liverpool and Broadgreen University Hospitals NHS Trust 141 113 28 5,935 24 5,766 24 9
Royal National Hospital for Rheumatic Diseases NHS Foundation Trust 0 0 0 274 0 349 0 0
Royal National Orthopaedic Hospital NHS Trust 10 9 1 1,375 7 2,517 4 0
Royal Surrey County Hospital NHS Foundation Trust 69 62 7 3,614 19 3,544 19 0
Royal United Hospital Bath NHS Trust 127 83 44 4,098 31 5,195 24 4
Salford Royal NHS Foundation Trust 227 217 10 6,548 35 6,341 36 2
Salisbury NHS Foundation Trust 82 80 2 3,266 25 3,952 21 2
Sandwell and West Birmingham Hospitals NHS Trust 176 129 47 7,379 24 11,129 16 0
Sheffield Children’s NHS Foundation Trust 164 162 2 2,795 59 2,989 55 0
Sheffield Teaching Hospitals NHS Foundation Trust 230 208 22 14,792 16 15,923 14 3
Sherwood Forest Hospitals NHS Foundation Trust 140 40 100 4,368 32 4,136 34 0
Shrewsbury and Telford Hospital NHS Trust 271 245 26 5,431 50 6,391 42 9
South Devon Healthcare NHS Foundation Trust 55 36 19 4,144 13 4,681 12 1
South Tees Hospitals NHS Foundation Trust 188 161 27 8,975 21 9,151 21 4
South Tyneside NHS Foundation Trust 94 88 6 4,483 21 4,996 19 4
South Warwickshire NHS Foundation Trust 95 51 44 4,123 23 4,206 23 1
Southend University Hospital NHS Foundation Trust 62 47 15 4,738 13 4,524 14 0
Southport and Ormskirk Hospital NHS Trust 61 59 2 3,515 17 3,613 17 0
St George's Healthcare NHS Trust 78 34 44 7,849 10 7,950 10 3
St Helens and Knowsley Hospitals NHS Trust 73 35 38 4,649 16 5,618 13 0
Stockport NHS Foundation Trust 187 168 19 5,907 32 5,851 32 4
Surrey and Sussex Healthcare NHS Trust 100 99 1 3,565 28 3,631 28 0
Tameside Hospital NHS Foundation Trust 96 79 17 2,473 39 2,500 38 8
Taunton and Somerset NHS Foundation Trust 108 73 35 4,084 26 4,745 23 3
The Christie NHS Foundation Trust 3 3 0 2,480 1 2,500 1 0
The Clatterbridge Cancer Centre NHS Foundation Trust 5 5 0 920 5 931 5 0
The Dudley Group NHS Foundation Trust 128 57 71 4,689 27 5,597 23 3
The Hillingdon Hospitals NHS Foundation Trust 48 29 19 2,856 17 3,305 15 7
The Newcastle Upon Tyne Hospitals NHS Foundation Trust 201 161 40 13,418 15 13,336 15 4
The Princess Alexandra Hospital NHS Trust 47 43 4 2,947 16 2,706 17 2
The Queen Elizabeth Hospital King's Lynn NHS Foundation Trust 105 103 2 2,900 36 3,416 31 0
The Robert Jones and Agnes Hunt Orthopaedic and District Hospital NHS Trust 24 21 3 1,280 19 1,482 16 0
The Rotherham NHS Foundation Trust 76 7 69 4,216 18 4,403 17 0
The Royal Bournemouth and Christchurch Hospitals NHS Foundation Trust 146 73 73 4,209 35 5,037 29 1
The Royal Marsden NHS Foundation Trust 12 10 2 3,798 3 3,500 3 0
The Royal Orthopaedic Hospital NHS Foundation Trust 4 4 0 915 4 941 4 0
The Royal Wolverhampton Hospitals NHS Trust 67 58 9 6,827 10 7,500 9 0
The Walton Centre NHS Foundation Trust 44 40 4 1,193 37 1,200 37 0
The Whittington Hospital NHS Trust 64 24 40 4,063 16 4,088 16 3
United Lincolnshire Hospitals NHS Trust 171 137 34 7,324 23 7,500 23 5
University College London Hospitals NHS Foundation Trust 122 46 76 7,838 16 8,750 14 11
University Hospital of North Staffordshire NHS Trust 131 42 89 7,216 18 9,227 14 0
University Hospital of South Manchester NHS Foundation Trust 95 90 5 5,915 16 5,100 19 0
University Hospital Southampton NHS Foundation Trust 206 96 110 8,814 23 10,177 20 8
University Hospitals Birmingham NHS Foundation Trust 72 39 33 8,255 9 8,624 8 10
University Hospitals Bristol NHS Foundation Trust 318 264 54 8,098 39 9,610 33 35
University Hospitals Coventry and Warwickshire NHS Trust 156 136 20 6,868 23 7,781 20 5
University Hospitals of Leicester NHS Trust 165 59 106 11,361 15 13,074 13 0
University Hospitals of Morecambe Bay NHS Foundation Trust 156 64 92 4,920 32 5,693 27 1
Walsall Healthcare NHS Trust 134 106 28 4,143 32 4,994 27 0
Page 7 of 12© NHS Protect
November 2014
NHS Protect
Tables showing the number of reported physical assaults on NHS staff in 2013/14, broken down by health body
Acute Sector
Name of Health Body Total
Assaults
(1)
Assaults
Involving
Medical
Factors (2)
Assaults NOT
Involving
Medical
Factors (3)
NHS
Workforce
Total Staff
(4)
Assaults
per 1,000
Staff (5)
Declared
Total Staff
(6)
Assaults
per 1,000
Staff (7)
Declared
Sanctions
(8)
Warrington and Halton Hospitals NHS Foundation Trust 168 114 54 3,949 43 3,987 42 7
West Hertfordshire Hospitals NHS Trust 149 145 4 4,121 36 4,343 34 0
West Middlesex University Hospital NHS Trust 71 68 3 1,833 39 1,800 39 3
West Suffolk NHS Foundation Trust 83 78 5 3,052 27 3,976 21 0
Western Sussex Hospitals NHS Foundation Trust 118 83 35 6,506 18 8,071 15 2
Weston Area Health NHS Trust 90 84 6 1,767 51 2,000 45 0
Wirral University Teaching Hospital NHS Foundation Trust 173 115 58 5,868 29 5,500 31 3
Worcestershire Acute Hospitals NHS Trust 120 58 62 5,811 21 6,067 20 0
Wrightington, Wigan and Leigh NHS Foundation Trust 141 117 24 4,715 30 4,848 29 20
Wye Valley NHS Trust 79 78 1 2,795 28 3,847 21 1
Yeovil District Hospital NHS Foundation Trust 77 67 10 1,950 39 2,223 35 0
York Teaching Hospital NHS Foundation Trust 110 59 51 8,376 13 9,100 12 7
Page 8 of 12© NHS Protect
November 2014
NHS Protect
Tables showing the number of reported physical assaults on NHS staff in 2013/14, broken down by health body
Ambulance Sector
Sources
(1) NHS Protect Physical Assault Statistics 2013/14(2) Physical assaults at (1) that involved medical factors (see notes below) (3) Physical assaults at (1) that did not involve medical factors(4) NHS Workforce figures 2013 (Medical + Non-Medical) (Published by The Health and Social Care Information Centre (HSCIC))(5) Assaults per 1,000 staff (calculation based on (4)) (6) Health body declaration of total staff (as at 31st March 2014)(7) Assaults per 1,000 staff (calculation based on (6))(8) Health body declaration of total criminal sanctions applied during the period 1st April 2013 to 31st March 2014
Notes
Name of Health Body Total
Assaults (1)
Assaults
Involving
Medical
Factors (2)
Assaults NOT
Involving Medical
Factors (3)
NHS
Workforce
Total Staff (4)
Assaults per
1,000 Staff
(5)
Declared
Total Staff
(6)
Assaults
per 1,000
Staff (7)
Declared
Sanctions (8)
Sector Total 1,868 508 1,360 37,131 50 41,428 45 384
East Midlands Ambulance Service NHS Trust 115 18 97 2,821 41 3,800 30 91
East Of England Ambulance Service NHS Trust 188 53 135 4,080 46 4,112 46 33
London Ambulance Service NHS Trust 414 105 309 4,511 92 4,933 84 33
North East Ambulance Service NHS Trust 73 26 47 2,290 32 2,397 30 30
North West Ambulance Service NHS Trust 377 178 199 4,798 79 5,178 73 79
South Central Ambulance Service NHS Foundation Trust 132 24 108 2,823 47 3,116 42 21
South East Coast Ambulance Service NHS Foundation Trust 113 22 91 3,409 33 3,661 31 9
South Western Ambulance Service NHS Foundation Trust 139 14 125 4,156 33 5,166 27 38
West Midlands Ambulance Service NHS Foundation Trust 207 57 150 3,813 54 4,386 47 25
Yorkshire Ambulance Service NHS Trust 110 11 99 4,430 25 4,679 24 25
IMPORTANT - care should be taken when comparing assault figures as there are many factors which may influence a health body's published figures including: a) population served b)
geographical setting (i.e. rural/urban), c) level of provision of mental health, learning disability and elderly care services, d) changes in service provision, e) health body amalgamations and
splits f) embedding of reporting culture.
Physical assault statistics (1) are validated by NHS Protect. All other data sets are the responsibility of The Health and Social Care Information Centre (HSCIC) (4) or the individual health
bodies (6) and (8). NHS Workforce figures were published by The Health and Social Care Information Centre (HSCIC) and relate to September 2013. The health body figures were provided as
at 31st March 2014. Both have been listed as there is some variance.Source (2) are the number of physical assaults where the perpetrator did not know what they were doing, or did not know what they were doing was wrong due to medical illness, mental ill
health, severe learning disability or treatment administered. These figures have been calculated by applying the percentage of total declared assaults identified as involving medical factors,
to the validated total assault figure at (1).
Page 9 of 12© NHS Protect
November 2014
NHS Protect
Tables showing the number of reported physical assaults on NHS staff in 2013/14, broken down by health body
Mental Health Sector
Sources
(1) NHS Protect Physical Assault Statistics 2013/14(2) Physical assaults at (1) that involved medical factors (see notes below) (3) Physical assaults at (1) that did not involve medical factors(4) NHS Workforce figures 2012 (Medical + Non-Medical) (Published by The Health and Social Care Information Centre (HSCIC))(5) Assaults per 1,000 staff (calculation based on (4)) (6) Health body declaration of total staff (as at 31st March 2014)(7) Assaults per 1,000 staff (calculation based on (6))(8) Health body declaration of total criminal sanctions applied during the period 1st April 2013 to 31st March 2014
Notes
Name of Health BodyTotal
Assaults (1)
Assaults
Involving
Medical
Factors (2)
Assaults NOT
Involving
Medical Factors
(3)
NHS
Workforce
Total Staff
(4)
Assaults
per 1,000
Staff (5)
Declared
Total Staff
(6)
Assaults
per 1,000
Staff (7)
Declared
Sanctions (8)
Sector Total 47,184 38,140 9,044 211,622 223 234,860 201 719
2gether NHS Foundation Trust 648 169 479 1,946 333 2,320 279 27
5 Boroughs Partnership NHS Foundation Trust 948 844 104 3,388 280 3,696 256 13
Avon and Wiltshire Mental Health Partnership NHS Trust 887 546 341 3,899 227 4,422 201 16
Barnet, Enfield and Haringey Mental Health NHS Trust 476 293 183 2,692 177 2,836 168 2
Berkshire Healthcare NHS Foundation Trust 797 737 60 4,136 193 4,510 177 2
Birmingham and Solihull Mental Health NHS Foundation Trust 1,190 213 977 4,103 290 4,737 251 4
Black Country Partnership NHS Foundation Trust 339 264 75 1,973 172 2,472 137 0
Bradford District Care Trust 921 272 649 2,861 322 2,989 308 0
Calderstones Partnership NHS Foundation Trust 1,195 1,195 0 1,635 731 1,088 1,098 44
Cambridgeshire and Peterborough NHS Foundation Trust 451 44 407 2,331 193 2,363 191 0
Camden and Islington NHS Foundation Trust 221 12 209 1,872 118 1,448 153 17
Central and North West London NHS Foundation Trust 1,259 1,229 30 6,354 198 7,393 170 12
Cheshire and Wirral Partnership NHS Foundation Trust 605 605 0 3,370 180 3,500 173 2
Cornwall Partnership NHS Foundation Trust 581 558 23 1,719 338 1,914 304 2
Coventry and Warwickshire Partnership NHS Trust 2,540 2,539 1 4,034 630 4,916 517 1
Cumbria Partnership NHS Foundation Trust 383 371 12 3,716 103 5,103 75 4
Derbyshire Healthcare NHS Foundation Trust 246 233 13 2,421 102 2,423 102 13
Devon Partnership NHS Trust 594 589 5 2,216 268 2,366 251 0
Dorset Healthcare University NHS Foundation Trust 746 242 504 5,226 143 6,154 121 1
Dudley and Walsall Mental Health Partnership NHS Trust 344 344 0 1,109 310 1,213 284 2
East London NHS Foundation Trust 1,153 1,153 0 3,629 318 4,255 271 27
Greater Manchester West Mental Health NHS Foundation Trust 686 683 3 2,823 243 3,595 191 0
Hertfordshire Partnership University NHS Foundation Trust 1,034 1,034 0 2,553 405 2,653 390 0
Humber NHS Foundation Trust 157 157 0 2,756 57 3,286 48 0
Isle of Wight NHS Trust 108 104 4 3,032 36 3,523 31 4
Kent and Medway NHS and Social Care Partnership Trust 1,133 486 647 3,075 368 3,918 289 0
Lancashire Care NHS Foundation Trust 1,446 1,040 406 6,641 218 8,392 172 50
Leeds and York Partnership NHS Foundation Trust) 1,275 1,232 43 3,301 386 3,864 330 14
Leicestershire Partnership NHS Trust 723 677 46 5,322 136 5,393 134 0
Lincolnshire Partnership NHS Foundation Trust 563 527 36 1,980 284 2,160 261 3
Manchester Mental Health and Social Care Trust 206 174 32 1,738 119 1,704 121 3
Mersey Care NHS Trust 841 348 493 3,757 224 4,216 199 106
NAViGO Health and Social Care CIC 50 45 5 485 103 660 76 0
Norfolk and Suffolk NHS Foundation Trust 1,220 944 276 3,948 309 3,888 314 8
North East London NHS Foundation Trust 200 200 0 5,439 37 6,000 33 0
North Essex Partnership University NHS Foundation Trust 375 248 127 1,994 188 2,087 180 8
North Staffordshire Combined Healthcare NHS Trust 398 381 17 1,439 277 1,591 250 7
Northamptonshire Healthcare NHS Foundation Trust 736 707 29 3,483 211 4,274 172 8
Northumberland, Tyne and Wear NHS Foundation Trust 3,335 3,225 110 6,020 554 6,464 516 25
Nottinghamshire Healthcare NHS Trust 1,363 1,224 139 8,830 154 8,848 154 48
Oxford Health NHS Foundation Trust 690 679 11 5,666 122 6,250 110 0
Oxleas NHS Foundation Trust 474 0 474 3,197 148 3,471 137 0
Pennine Care NHS Foundation Trust 615 584 31 5,920 104 7,033 87 6
Rotherham, Doncaster and South Humber NHS Foundation Trust 1,070 1,062 8 3,797 282 3,800 282 9
Sheffield Health and Social Care NHS Foundation Trust 1,143 804 339 2,738 417 3,180 359 0
Solent NHS Trust 134 125 9 3,848 35 4,079 33 0
Somerset Partnership NHS Foundation Trust 541 349 192 3,780 143 4,454 121 54
South Essex Partnership University NHS Foundation Trust 494 429 65 5,985 83 7,063 70 5
South London and Maudsley NHS Foundation Trust) 1,192 477 715 4,627 258 4,358 274 28
South Staffordshire and Shropshire Healthcare NHS Foundation Trust 942 910 32 3,453 273 3,452 273 8
South West London and St George's Mental Health NHS Trust 387 387 0 2,113 183 2,963 131 17
South West Yorkshire Partnership NHS Foundation Trust 706 193 513 4,827 146 5,161 137 0
Southern Health NHS Foundation Trust 2,731 2,618 113 7,719 354 8,996 304 0
Surrey and Borders Partnership NHS Foundation Trust 392 392 0 2,651 148 2,400 163 4
Sussex Partnership NHS Foundation Trust 596 587 9 4,149 144 4,500 132 12
Tavistock and Portman NHS Foundation Trust 82 82 0 538 152 572 143 0
Tees, Esk and Wear Valleys NHS Foundation Trust 1,548 1,501 47 6,100 254 7,178 216 0
IMPORTANT - care should be taken when comparing assault figures as there are many factors which may influence a health body's published figures including: a) population served b)
geographical setting (i.e. rural/urban), c) level of provision of mental health, learning disability and elderly care services, d) changes in service provision, e) health body amalgamations and
splits f) embedding of reporting culture.
Health bodies have been categorised under the Mental Health sector where mental health and/or learning disability services constitute a significant proportion of their overall service
provision.
Physical assault statistics (1) are validated by NHS Protect. All other data sets are the responsibility of The Health and Social Care Information Centre (HSCIC) (4) or the individual health
bodies (6) and (8). NHS Workforce figures were published by The Health and Social Care Information Centre (HSCIC) and relate to September 2013. The health body figures were provided
as at 31st March 2014. Both have been listed as there is some variance.Source (2) are the number of physical assaults where the perpetrator did not know what they were doing, or did not know what they were doing was wrong due to medical illness, mental
ill health, severe learning disability or treatment administered. These figures have been calculated by applying the percentage of total declared assaults identified as involving medical
factors, to the validated total assault figure at (1).
Page 10 of 12© NHS Protect
November 2014
NHS Protect
Tables showing the number of reported physical assaults on NHS staff in 2013/14, broken down by health body
Mental Health Sector
Name of Health BodyTotal
Assaults (1)
Assaults
Involving
Medical
Factors (2)
Assaults NOT
Involving
Medical Factors
(3)
NHS
Workforce
Total Staff
(4)
Assaults
per 1,000
Staff (5)
Declared
Total Staff
(6)
Assaults
per 1,000
Staff (7)
Declared
Sanctions (8)
West London Mental Health NHS Trust 818 818 0 3,270 250 3,185 257 103
Worcestershire Health and Care NHS Trust 256 255 1 3,998 64 4,131 62 0
Page 11 of 12© NHS Protect
November 2014
NHS Protect
Tables showing the number of reported physical assaults on NHS staff in 2013/14, broken down by health body
Primary and Community Care Sector
Sources
(1) NHS Protect Physical Assault Statistics 2013/14(2) Physical assaults at (1) that involved medical factors (see notes below) (3) Physical assaults at (1) that did not involve medical factors(4) NHS Workforce figures 2013 (Medical + Non-Medical) (Published by The Health and Social Care Information Centre (HSCIC))(5) Assaults per 1,000 staff (calculation based on (4)) (6) Health body declaration of total staff (as at 31st March 2014)(7) Assaults per 1,000 staff (calculation based on (6))(8) Health body declaration of total criminal sanctions applied during the period 1st April 2013 to 31st March 2014
Notes
Name of Health BodyTotal
Assaults
(1)
Assaults
Involving
Medical
Factors (2)
Assaults NOT
Involving
Medical Factors
(3)
NHS
Workforce
Total Staff
(4)
Assaults
per 1,000
Staff (5)
Declared
Total Staff
(6)
Assaults
per 1,000
Staff (7)
Declared
Sanctions
(8)
Sector Total 1,731 1,487 244 72,748 24 87,233 20 7
Anglian Community Enterprise CIC 16 11 5 1,091 15 1,267 13 0
Birmingham Community Healthcare NHS Trust 287 282 5 5,017 57 5,843 49 1
Bridgewater Community Healthcare NHS Trust 15 13 2 3,316 5 3,569 4 0
Bristol Community Health CIC 15 13 2 1,107 14 1,167 13 0
Bromley Healthcare CIC 33 33 0 750 44 989 33 0
Cambridgeshire Community Services NHS Trust 9 6 3 3,672 2 3,517 3 0
Care Plus Group CIC 3 3 0 792 4 866 3 0
Central Essex Community Services CIC 14 13 1 1,153 12 1,200 12 0
Central London Community Healthcare NHS Trust 42 23 19 3,023 14 3,480 12 1
City Health Care Partnership CIC 12 4 8 1,303 9 2,007 6 1
Derbyshire Community Health Services NHS Trust 244 208 36 4,341 56 4,947 49 0
East Coast Community Healthcare CIC 4 3 1 922 4 1,030 4 0
First Community Health and Care CIC 5 5 0 - - 450 11 0
Gloucestershire Care Services NHS Trust 65 47 18 2,628 25 2,956 22 0
Hertfordshire Community NHS Trust 28 24 4 2,894 10 3,188 9 0
Hounslow and Richmond Community Healthcare NHS Trust 7 5 2 968 7 1,020 7 0
Kent Community Health NHS Trust 63 52 11 5,433 12 5,487 11 0
Leeds Community Healthcare NHS Trust 24 20 4 2,972 8 3,500 7 0
Lincolnshire Community Health Services NHS Trust 27 24 3 2,377 11 2,572 10 0
Liverpool Community Health NHS Trust 29 23 6 2,946 10 2,908 10 0
Locala Community Partnerships CIC 7 4 3 1,168 6 1,193 6 0
Medway Community Healthcare CIC 45 43 2 1,279 35 1,339 34 0
Norfolk Community Health and Care NHS Trust 83 70 13 2,627 32 2,980 28 0
North Somerset Community Partnership CIC 2 2 0 618 3 644 3 0
Nottingham CityCare Partnership CIC 5 4 1 1,311 4 1,734 3 1
Peninsular Community Health CIC 89 84 5 2,075 43 2,015 44 0
Plymouth Community Healthcare CIC 173 173 0 2,179 79 2,129 81 2
Seqol 117 39 78 - - 876 134 0
Shropshire Community Health NHS Trust 20 20 0 1,636 12 1,745 11 0
Staffordshire and Stoke On Trent Partnership NHS Trust 45 40 5 4,823 9 6,401 7 0
Suffolk Community Healthcare 5 4 1 - - 1,007 5 0
Sussex Community NHS Trust 87 83 4 4,343 20 4,982 17 0
Torbay & Southern Devon Health and Care NHS Trust 50 49 1 2,034 25 2,454 20 1
Virgin Care - Integrated Children's Services 27 26 1 - - 1,100 25 0
Virgin Care - Surrey Community Health 16 16 0 - - 2,532 6 0
Wirral Community NHS Trust 2 2 0 1,332 2 1,380 1 0
Your Healthcare CIC 16 16 0 618 26 759 21 0
IMPORTANT - care should be taken when comparing assault figures as there are many factors which may influence a health body's published figures including: a) population
served b) geographical setting (i.e. rural/urban), c) level of provision of mental health, learning disability and elderly care services, d) changes in service provision, e) health body
amalgamations and splits f) embedding of reporting culture.
Physical assault statistics (1) are validated by NHS Protect. All other data sets are the responsibility of The Health and Social Care Information Centre (HSCIC) (4) or the individual
health bodies (6) and (8). NHS Workforce figures were published by The Health and Social Care Information Centre (HSCIC) and relate to September 2013. The health body figures
were provided as at 31st March 2014. Both have been listed as there is some variance.Source (2) are the number of physical assaults where the perpetrator did not know what they were doing, or did not know what they were doing was wrong due to medical illness,
mental ill health, severe learning disability or treatment administered. These figures have been calculated by applying the percentage of total declared assaults identified as
involving medical factors, to the validated total assault figure at (1).
There were no physical assaults reported to NHS England in 2013/14.
Page 12 of 12© NHS Protect
November 2014
Board of Directors – Public 23 April 2014 Hard Truths: Safe Staffing
Version 1.0
Author: Jane Sayer Department: Trust Management
Page 1 of 4 Date produced: Retention period: 30 years
Report To: Board of Directors – Public
Meeting Date: 18th December 2014
Title of Report: Hard Truths – Safe Staffing Update
Action Sought: For Information
Estimated time: 15 minutes
Author: Michele Allott, Deputy Director of Nursing
Director: Jane Sayer, Director of Nursing, Quality and Patient Safety
Executive Summary:
In line with recommendations published within Hard Truths, the Government’s response to the Francis Inquiry published in November 2013, this report sets out to provide updated information to the Board on safe staffing levels within Norfolk and Suffolk Foundation Trust. This paper is presented to the Board to fulfil the ten expectations of Trust Boards and their responsibility for the quality of care provided to patients, and as a key determinant of the quality of care provided, taking full and collective responsibility for nursing, midwifery and care staffing capacity and capability. The review of staffing numbers and establishments within inpatient areas has been based on available evidence in mental health environments while national guidance is awaited.
1.0 Report contents
1.1 Update on expectations of Trust Boards as outlined in the previous report presented to the Board on 24th April 2014, “Hard Truths – Safe Staffing” by Director of Nursing, Dr Jane Sayer.
1.2 Information regarding new developments to support safe staffing and quality care within NSFT.
1.3 Review of staffing levels in Norfolk and Suffolk Foundation Trust (NSFT) within inpatient areas and the process of the review.
1.4 Update on information from national pilots regarding evidence-based tools to determine safe staffing levels nationally.
2.0 Update on expectations of Trust Boards following the publication of Hard
Truths 2.1 From April 2014, and by June 2014 at the latest, NHS Trusts have been required to
publish ward level information on whether they are meeting their staffing requirements. Actual versus planned nursing and midwifery fill rates must be published every month. NSFT, in accordance with this requirement, has reported
Date: 18 December 2014
F Item: 14.171 ii
Board of Directors – Public 23 April 2014 Hard Truths: Safe Staffing
Version 1.0
Author: Jane Sayer Department: Trust Management
Page 2 of 4 Date produced: Retention period: 30 years
these figures daily on each inpatient area and monthly via the national reporting Unify 2 system and to NSFT Board.
2.2 Since reporting began in May 2014, Table 1 below indicates the average fill rates on
a month by month basis within NSFT. Alongside the reported information on Unify 2 the Board also receives a monthly update on all staffing concerns reported via the datix system within NSFT. The percentage rates for fill rates are not unlike those of acute hospitals in Norfolk and Suffolk.
Table 1: Mean staffing, actual against establishment, May 2014 – October 2014
RN % fill against establishment
HCA % fill against establishment
Day shifts May June July August September October
96.8% 102.7% 99.8% 98.6% 99.1% 98.8%
119.5% 117.4% 122.5% 125.1% 119.5% 121.8%
Nightshifts May June July August September October
89.9% 88.8% 92.5% 90.5% 88.8% 86.8%
125.0% 132.0% 134.2% 138.1% 137.9% 140.4%
2.3 A second review of staffing levels has been conducted following the initial review of
staffing levels in preparation for the reporting onto Unify in April 2014. The review has been conducted using the same method and methodologies as the initial review as, to date, there has been no publication of National Institute for Health and Care Excellence accredited tools for Mental Health Services.
2.4 The Board will continue to receive updates every six months on staffing levels, which
allow for the collection of several data points to inform appropriate staffing. 3.0 New developments to support safe staffing and quality care 3.1 As set out in its mandate, Health Education England is committed to introducing
values-based recruitment for all students entering NHS-funded clinical education programmes. To support this, NSFT has begun its own values-based recruitment events for newly qualified staff, with one event in Norfolk during July 2014 and one event in Suffolk in November 2014.
3.2 Alongside these events NSFT has launched a Nursing Academy for newly qualified
nurses to support and develop newly qualified nurses to deliver compassionate care based on best practice. (Appendix 1).
Board of Directors – Public 23 April 2014 Hard Truths: Safe Staffing
Version 1.0
Author: Jane Sayer Department: Trust Management
Page 3 of 4 Date produced: Retention period: 30 years
3.3 A Deputy Director of Nursing Professional Practice has been appointed. The post will have responsibility for ongoing professional standards, training and development, taking the lead on future safe staffing reviews and reporting within NSFT.
3.4 Introduction of e-rostering into NSFT with the rollout commencing on 24th November 2014 to support safe, fair and efficient rostering practice across NSFT.
4.0 Review of staffing levels across inpatient areas 4.1 During October 2014 the Deputy Director of Nursing has met with all clinical team
leaders (CTLs) across inpatient areas to review their current establishments against the figures recommended in April 2014 and their existing budgets.
4.2 The figures agreed by the Deputy Director of Nursing and CTLs took into account the increasing levels of acuity within services and factored in one additional level of observation. The numbers were calculated using a combination of existing basic tools, benchmarking and professional judgement of operational staff. The numbers only include nursing staff and do not take into account other members of MDT or teams.
4.3 A meeting to review these establishments was held in November with Directors of Nursing, Finance and Operations (Norfolk) along with Associate Director of Operations for Suffolk to agree and review suggested establishments, and agree equity across services, ratios of registered to non-registered nurses and align establishments across NSFT.
4.4 Further consultation was sought from locality managers following this review for their
sign up and agreement for recommended establishments. 4.5 Final figures have been submitted to the finance team who have based the agreed
establishments against a shift calculator to come up with the final figures. 5.0 National updates and progress related to evidence-based tools and practice. 5.1 Work continues within the National Mental Health and Learning Disability Forum with
regard to developing an evidence-based tool to calculate the required numbers within Mental Health and LD services to ensure not only safe staffing numbers but reflecting skill mix and MDT working. Pilot sites have been identified to trial an adapted existing evidence-based tool (HURST Tool) to evaluate its effectiveness within Mental Health and LD environments. The implementation of the pilot is expected in Spring 2015. Results of the pilot will be shared with forum members as the pilot progresses.
5.2 The National Quality Board (NQB) has set out the immediate expectations of NHS providers in providing safe staffing levels. Their guide to nursing, midwifery and care staffing capacity and capability brings together tools, resources and examples of good practice as a practical guide to help NHS providers and commissioners. To take this forward in the longer term, NICE has been asked to conduct a comprehensive review of the evidence in this area and produce definitive guidelines on safe staffing to support local decisions at ward and organisational level.
5.3 The overall approach for developing NICE safe staffing guidelines will follow that used in NICE's other guideline development programmes:
Board of Directors – Public 23 April 2014 Hard Truths: Safe Staffing
Version 1.0
Author: Jane Sayer Department: Trust Management
Page 4 of 4 Date produced: Retention period: 30 years
Development of an initial scope that defines the parameters of the work.
An engagement workshop with key stakeholder organisations for each topic area when the timeline permits. This is to inform stakeholders of the process, to confirm the scope of work is appropriate, and to understand the breadth of evidence that might need to be considered.
A comprehensive evidence review and economic analysis for consideration by the Safe Staffing Advisory Committee, who will develop recommendations.
A period of stakeholder consultation on the recommendations before the guideline is published.
Current progress and timings for the publication of NICE guidance related to Mental Health settings is as follows.
5.4 The guidance is currently in the scoping phase within an initial draft consultation
document expected to be produced in July 2015. The expected completed guidance is expected to be published in October 2015.
6.0 Risks / mitigation in relation to the Trust objectives (implications for Board
Assurance Framework)
6.1 Quality and patient safety issues are fundamental to the delivery of Trust objectives, and the Board’s ability to manage the performance of the Trust. Ensuring that the correct numbers of skilled staff are in place to deliver high quality and safe care is a fundamental duty of the Trust’s Board of Directors. Relevant mitigating action is included above, and residual risks are noted.
7.0 Recommendations
7.1 The Board of Directors is asked to note and approve the contents of this report.
Background Papers / Information Appendix 1 – Nursing Academy
Service Governance Committee 09 December 2014 Chairs Report
Version 0.1
Author: Peter Jeffreys Department: Corporate
Page 1 of 4 Date produced: 11 December 2014 Retention period: 30 years
Report To: Board of Directors - Public
Meeting Date: 18 December 2014
Title of Report: Service Governance Committee Chair’s Report – 9 Dec 2014
Action Sought: For Information
Estimated time: 5 minutes
Author: Peter Jefferys: Chair Service Governance Committee
Director: Dr Peter Jefferys: Non-Executive Director
Executive Summary:
Last (8th) Service Governance Committee meeting in 2014 before membership expansion to include lead clinicians.
Monitoring quality and addressing weakness / learning lessons remains major challenge particularly in areas such as risk assessment, clinical supervision, CPA & physical health compliance..
Need for ‘smarter’ analysis of RCA’s & complaints
Need for simplification of polices with distinction from procedures
Daunting challenge for 2015 of engaging localities in quality agenda
Encouraged by commitment shown at Foresight workshop
1.0 Report from Service Governance Committee meeting 9 Dec 2014:
1.1 Theme 1: Safe Services
1.1.1 West Norfolk CCG deaths audit: Provisional action plan of wider NSFT relevance. Needs to link with ‘learning from RCA’s and SI’s’ work.
1.1.2 Unexpected community deaths: Figures over past 19 months reveal a mean increase in non NRP community deaths from Apr 2013 – Oct 2014. NRP deaths show an unchanged mean. Agreed that future RCA recommendations need to be thematically structured and analysed with more objective measures of outcome with concentration on issues of major importance. Governance Team, supported by Medical Director, will progress. It is to be hoped that the number of recommendations can be reduced to avoid the unacceptable figure of 264 ‘outstanding’ recommendations from 89 SI’s (end Oct 14) awaiting evidence of
Date: 18 December 2014
G Item: 14.171 iii
Service Governance Committee 09 December 2014 Chairs Report
Version 0.1
Author: Peter Jeffreys Department: Corporate
Page 2 of 4 Date produced: 11 December 2014 Retention period: 30 years
completion. SGC remains concerned Need for more constructive engagement with locality governance groups to enhance learning.
1.1.3 Suicide Prevention Strategy: Director of Nursing reported on recent initiative in Norfolk jointly with Police, Coroner, Public Health, NSFT, and others to develop improved primary and secondary suicide prevention strategy. Participation by NSFT welcomed. SGC encouraged similar approach to be adopted in Suffolk.
1.1.4 Safeguarding: In order to comply with new national guidance Level 2 Safeguarding training is now redundant and all higher level training must be Level 3. Chair assured by Safeguarding Lead that change can be made within existing resources. SGC endorsed change. Information on medical staff training compliance still being sought.
1.2 Theme 2: Caring & Responsive Services:
1.2.1 Ombudsman Investigations: Agreed that SGC will receive ‘progress reports’ about ongoing investigations to ensure lessons learned early.
1.2.2 Service User Community Survey & Inpatient Surveys: SGC informed that action plans from localities are being sought currently. Will be collated in due course by Governance Team and reported to SGC.
1.3 Theme 3: Effective Services:
1.3.1 Clinical supervision: SGC informed of intention to present firm proposals to support improvement, including policy revision at early SGC meeting in 2015.
1.3.2 Clinical Policy Reviews & endorsement: SGC approved a range of policies following review by the Effectiveness & Policy Board. Comment was made that most NSFT policies are unwieldy because they incorporate lengthy procedures. It was suggested that policies should be short and easily accessible, with procedural addenda as needed. Rationalisation of overlapping policies would also be useful.
1.3.3 New Nice Guidance on Bipolar Disorder (CG185): SGC noted its recent publication and urged that it be publicised and compliance with it urged and audited as soon as practicable.
1.3.4 Clinical audit programme: It was agreed that significant change to the extensive audit programme was required to priorities issues with greatest impact on patient safety and effectiveness of care, linking outcomes to locality performance. Governance Team will review audit programme with this objective in mind.
1.3.5 Completion of CTO 12 by Approved Clinician (MHAct compliance issue): In response to the Mental Health Law Forum SGC formally agreed that a medical practitioner must provide an explanation of the treatment plan before completion of the relevant Certificate of Consent form. It would be good practice for doctor and Approved Clinician (if non-medical) to jointly examine the patient and for this to be formally recorded.
1.4 SGC Terms of Reference, Work Plan & Locality Quality Governance
Service Governance Committee 09 December 2014 Chairs Report
Version 0.1
Author: Peter Jeffreys Department: Corporate
Page 3 of 4 Date produced: 11 December 2014 Retention period: 30 years
1.4.1 SGC noted that approval of the ToR at November Trust Board and agreed to schedule 10 meetings per year with locality representation (Lead Clinicians) to take effect from Jan 2015. It was confirmed that the primary objective of SGC is to provide the Board with assurance on quality rather than to ensure the delivery of a quality service.
1.4.2 Following a successful workshop facilitated by Foresight on Locality Governance the previous work the Governance Team will work closely with localities to review their local governance arrangements and reporting mechanisms with the aim of providing better assurance for SGC.
1.5 Locality issues: West Norfolk focus
1.5.1 The review was attended by Locality Service Manager, Lead Clinician and Older Persons Services Manager, supported by a high quality report which provided extensive evidence on service governance and on aspects of clinical quality, addressing achievements as well as shortcomings. The team was congratulated on their approach to quality and on the evidence of a wide range of constructive partnerships with other services and agencies that have been established. The locality is well aware its shortcomings, e.g. CPA compliance, additional observations, clinical supervision and has appropriate plans to address them.
2.0 Financial implications (including workforce effects)
2.1 None
3.0 Quality implications
3.1 Dealt with in main report above.
4.0 Equality implications
4.1 None
5.0 Risks / mitigation in relation to the Trust objectives
5.1 No new risks to those previously reported to Board. Further mitigation awaited on several issues (e.g. learning from RCA’s and Complaints).
6.0 Recommendations
6.1 The Board is asked to note the work of the Committee.
Dr Peter Jefferys Non-Executive Director 10 Dec 2014
Service Governance Committee 09 December 2014 Chairs Report
Version 0.1
Author: Peter Jeffreys Department: Corporate
Page 4 of 4 Date produced: 11 December 2014 Retention period: 30 years
Background Papers / Information - None
Board of Directors – 18th
December 2014 2014/15 Financial Performance Report M08
Version 1.0
Author: Adrian Brooke Department: Finance
Page 1 of 3 Date produced: 16th
December 2014
Retention period: 30 years
Report To: Board of Directors - Public
Meeting Date: 18th December 2014
Title of Report: 2014/15 Financial Performance Report (for the eight month period ending 30th November 2014)
Action Sought: For Information
Estimated time: 20 minutes
Author: Adrian Brooke – Business Accounting & Reporting Manager
Director: Andrew Hopkins, Finance Director
Executive Summary:
The purpose of this report is to inform the Board of Directors of the Trust’s financial performance for the period 1 April 2014 to 30th November 2014. Key headlines for the month include:
A deficit in the month of £0.72m, increasing the year to date deficit at month eight to £3.01m. As previously reported a number of actions have been agreed to reduce this deficit and so bring down the year end forecast deficit from a predicted £5.3m to £3.7m.
A reported Continuity of Service Risk Rating (COSRR) of 2 for November, which is forecast to continue to the end of the year. This is based on a number of financial recovery actions which will be required to maintain this rating.
Temporary staffing expenditure levels have fallen for the second month running, with November expenditure down to £1.83m (£2.08m October), and whilst this is still significantly above prior year levels, is actually the lowest monthly reported total this financial year.
The cash position of £16.5m is ahead of plan by £4.7m as at the end of November, but this is expected to fall to £10m at year-end, which is below the original plan of £21.4m.
Year to date capital expenditure of £3.09m against an original plan of £6.69m.
Date: 18th
December 2014
H Item: 14.171 iv.
Board of Directors – 18th
December 2014 2014/15 Financial Performance Report M08
Version 1.0
Author: Adrian Brooke Department: Finance
Page 2 of 3 Date produced: 16th
December 2014
Retention period: 30 years
1.0 Financial Position
The attached power-point document details the overall Trust Financial Performance
as at the end of November 2014. A summarised position is also attached to this
paper in Appendix 1.
The Trust report is reporting a year to date deficit of £3.01m which is £3.40m behind
plan. As a result of the financial position, the Trust continues to report a COSRR of
2.
2.0 Recommendation
The Board of Directors is asked to review and note the report.
Andrew Hopkins
Director of Finance 16
th December 2014
Board of Directors – 18th
December 2014 2014/15 Financial Performance Report M08
Version 1.0
Author: Adrian Brooke Department: Finance
Page 3 of 3 Date produced: 16th
December 2014
Retention period: 30 years
Appendix 1
Actual PlanVariance
(adverse)Forecast Plan
Variance
(adverse)
Nov-14 Nov-14 Nov-14 Mar-15 Mar-15 Mar-15
£m YTD YTD YTD FY FY FY
Operating Income 140.3 136.9 3.4 211.1 204.3 6.9
Pay Costs (109.6) (105.5) (4.1) (164.0) (156.3) (7.7)
Drug Costs (2.4) (2.1) (0.3) (3.5) (3.1) (0.4)
Other Costs (23.8) (21.4) (2.4) (36.1) (31.5) (4.5)
EBITDA 4.4 7.9 (3.5) 7.6 13.3 (5.8)
Depreciation (4.1) (4.5) 0.4 (6.3) (6.9) 0.6
Net interest (0.6) (0.7) 0.0 (0.9) (1.0) 0.1
Other (2.7) (2.3) (0.3) (4.0) (3.5) (0.5)
(3.0) 0.4 (3.4) (3.7) 1.9 (5.6)
Exceptionals - - - - - -
Net surplus / (deficit) (3.0) 0.4 (3.4) (3.7) 1.9 (5.6)
EBITDA margin 3.2% 5.8% (2.6%) 3.6% 6.5% (2.9%)
Actual PlanVariance
(adverse)Forecast Plan
Variance
(adverse)
Nov-14 Nov-14 Nov-14 Mar-15 Mar-15 Mar-15
£m YTD YTD YTD FY FY FY
Non-Currrent Assets 135.3 146.0 (10.7) 137.2 142.7 (5.5)
Current Assets 32.4 19.6 12.9 25.4 26.9 (1.5)
Current Liabilities (29.3) (23.4) (5.9) (27.2) (29.2) 2.1
Non-Current Liabilities (22.6) (23.5) 1.0 (20.2) (20.2) -
TOTAL ASSETS EMPLOYED 115.9 118.6 (2.7) 115.2 120.1 (4.9)
Public dividend capital 81.4 80.6 0.8 81.4 80.6 0.8
Retained Earnings (Accumulated Losses) 8.9 12.3 (3.4) 8.3 13.8 (5.6)
Revaluation reserve 25.5 25.7 (0.2) 25.5 25.7 (0.2)
Donated asset reserve - - - - - -
TOTAL FUNDS EMPLOYED 115.9 118.6 (2.7) 115.2 120.1 (4.9)
Actual PlanVariance
(adverse)Forecast Plan
Variance
(adverse)
Nov-14 Nov-14 Nov-14 Mar-15 Mar-15 Mar-15
£m YTD YTD YTD FY FY FY
EBITDA 4.4 7.9 (3.5) 7.6 13.3 (5.8)
Change in working capital (1.5) (2.3) 0.8 (3.3) 3.9 (7.2)
Cashflow from operations 3.0 5.6 (2.6) 4.3 17.3 (13.0)
(2.6) (5.8) 3.2 (7.0) (4.9) (2.1)
Financing and other (3.3) (2.4) (0.9) (6.7) (5.1) (1.6)
Net cash inflow / (outflow) (2.9) (2.6) (0.3) (9.4) 7.3 (16.7)
Closing cash and cash equivalents 16.5 11.8 4.7 10.0 21.4 (11.4)
Net cash inflow / (outflow) from investing
activities
Statement of
Comprehensive Income
(SOCI)
Statement Of Financial
Performance (SOFP)
Statement of Cashflow
(SOCF)
Index Slides 1 - Executive Summary
Slide 2 - Key Highlights
Slide 3 - Finance Dashboard
Slide 4 - Statement of Comprehensive Income (SOCI)
Slides 5 – 7 Income
Slides 8 – 12 Expenditure – Pay & Non Pay
Slide 13 - CIP
Slide 14 - Capital
Slide 15 - Balance Sheet
Slide 16 - Cash flow
Slide 17 - COSRR
Executive Summary
The month of November has shown an improved I&E position to what was forecast in
October with an in month deficit of £0.72m pushing the YTD deficit to £3.01m. This is less
than the £0.9m forecast last month. The YTD variance against original Annual Plan is now
adverse by £3.40m. The revised year-end forecast now stands at £3.7m, revised down
from £5.3m as a result of a number of initiatives which have been identified through the
Financial Recovery Plan..
As a result of the YTD position the Trust reports a COSRR (Continuity of Service Risk Rating) of 2,
which is expected to remain throughout the remainder of the financial year.
There has once again been an increase in the Acute out of area placements in the month
although it is anticipated that this increase will not continue as a result of the opening of the
new Assessment Ward in the last two months of the year and this has been factored into
the overall forecast.
On a more positive note, there was an improvement of £0.2m in November against
previous forecast expectations for the month, which was driven by a reduction in Temporary
staffing expenditure.
Cash held by the Trust remains ahead of plan by £4.7m YTD. Based on current forecast
however, the cash position is expected to end the year £11.4m below the original plan (see
Cash-flow and Finance Dashboard pages).
1
Key Highlights – YTD Position
3
Acute out of area (OOA) placements expenditure once again rose significantly this month
to £0.61m as bed days increased by 349 days against last month. YTD costs now total
£2.33m. Forecast assumptions have been revised to take account of the impact of the
opening of Thurne Ward for which it is expected to see a gradual decrease in the
expenditure over the last 4 months of the year.
Specialist placement expenditure for the month in Norfolk once again remained relatively
static, although there were two new placements into longer term care during the month.
YTD expenditure remains within original plan totalling £1.20m.
Overall temporary pay expenditure dropped for the second month running, this time to
£1.83m (£2.08m October), with improvement driven by a reduction in Agency expenditure,
evidenced across most areas. Total YTD expenditure now stands at £16.87m (this
compares to £10.16m YTD for last financial year and has now surpassed the total level of
expenditure level made in the prior year).
A £0.8m provision for the under achievement of CQUIN targets has been made YTD.
Latest figures from Norfolk suggest that this may improve over the remaining months due
to achievements recently notified as at the end of Q2.
The Capital programme remains behind plan and as a result of current financial position a
revised (lower) schedule has been agreed. As a result YTD depreciation levels are less
than planned.
Cash held by the Trust at the end of November remains higher than planned, at £4.7m.
Finance Dashboard
4
Feb
Mar
CIP by Gateway
(800)
(600)
(400)
(200)
-
200
400
600
Apr May Jun Jul Aug Sept Oct Nov Dec Jan Feb Mar
Monthly Surplus/Deficit £000's
Plan Forecast (Actual)
4.9
0.61.1
0.0
2.5
5.5
FY CIP £m
Gateway zero
Gateway one
Gateway two
Gateway three
Gateway four
Gateway five
-
2.0
4.0
6.0
8.0
10.0
12.0
Apr May Jun Jul Aug Sept Oct Nov Dec Jan Feb Mar
Capex £m
Plan Forecast (Actual) Min Max
-
5,000
10,000
15,000
20,000
25,000Twelve month cash balances by month
Actual/Forecast£000
Annual Plan£000
Statement Of Comprehensive Income (SOCI)
5
Statement of Comprehensive Income (SOCI)-Year to date Full Year SOCI
Annual Actual Variance to Annual Forecast Variance
Plan Annual Plan Plan
£'000 £'000 £'000 £'000 £'000 £'000
Operating Income (136,928) (140,294) 3,366 (204,251) (211,143) 6,892
Pay Costs 105,522 109,631 (4,110) 156,306 164,035 (7,729)
Drug Costs 2,087 2,400 (313) 3,097 3,499 (401)
Other Costs 21,383 23,820 (2,436) 31,524 36,054 (4,530)
EBITDA 7,936 4,443 (3,493) 13,324 7,556 (5,768)
Depreciation 4,547 4,139 408 6,928 6,283 645
Net interest 2,996 3,315 (319) 4,495 4,974 (479)
Other
Exceptionals
Net surplus / (deficit) 392 (3,011) (3,404) 1,901 (3,701) (5,601)
EBITDA margin 6% 3% 7% 4%
Income – Summary
8
Year to date Income position Full Year Income position
Annual Actual Variance to Annual Forecast Variance
Plan Annual Plan Plan
£'000 £'000 £'000 £'000 £'000 £'000
Block contracts 116,579 116,165 (413) 174,868 176,159 1,292
Clinical Partnerships 8,669 8,338 (331) 11,863 11,621 (243)
Clinical income-Secondary Commissioning 1,481 1,492 11 2,222 2,238 16
Other clinical income 2,692 3,528 836 4,038 5,451 1,414
NHS Mental Health activity Income, Total 129,421 129,523 102 192,991 195,469 2,479
Research and Development 595 1,340 745 892 1,782 890
Education and Training 2,235 2,356 121 3,353 3,535 182
Misc. Other Operating 4,677 7,075 2,398 7,015 10,357 3,342
Other Operating income, Total 7,507 10,770 3,264 11,260 15,674 4,414
Operating Income, Total 136,928 140,294 3,366 204,251 211,143 6,892
Income – Clinical
Block Contracts – (£403k) lower than plan:
• (£365k) under-occupancy provision for CAMHS Tier 4 and Secure Services. This is currently being
challenged with NHS England as a result of lack of demand and will be factored into the position once
agreement is reached.
• (£799k) CQUIN underachievement provision,
• £386k of Additional Observations for Suffolk CCG’s,
• £244k Additional Income for QEH Liaison and
• £131k of other contract variations and budget phasing.
Clinical Partnerships – (£331k) lower than plan:
• (£165k) reduction in the Section 75 NCC and NRP contracts, and
• (£55k) reclassifying of NCA monies to a block contract with Cambridge & Peterborough CCG
• (£138k) re-phasing of NRP innovation monies. The latter will be recovered at the end of the year and
• £27k of other contract movement.
Other Clinical Income - £836k increase to plan: key contributors are:
• £504k agreed contracts over original Annual Plan assumptions
• £332k – Other contract variations including Norfolk Constabulary and System Wide CQUIN
9
Income – Non Clinical income The graph below shows the breakdown of miscellaneous other income against plan.
The deferred/other income variance continues to be due to the conservative assumptions
used when setting the Annual Plan. All of the income achieved is matched with pay and
non pay expenditure.
ICT trading accounts also reflect increased activity against planned assumptions, by
£614k. Whilst the overall YTD performance reflects a surplus of £107k in the accounts,
£80k of this has been due to receipt of prior year income meaning that trading contracts
make only a minimal profit overall against the level of turnover generated in the year.
Within this there is also a loss making contract held with West Suffolk CCG for the
additional work that has been required on the windows 7 upgrade.
Estates trading income is below plan by £333k YTD due to lost contracts. Where this
applies, there are matching pay and non pay favourable variances to plan with no loss to
the Trust overall.
12
Expenditure – Summary Vacancy levels continue to remain high across the Trust, although some progress has been
made with net recruitment this month to a number of clinical and admin roles across the
Trust. November vacancy levels now stand at 451 WTE’s.
The piece of work to understand the cost implications of the safer staffing rotas has just
been completed which has involved all localities and the Directorate of Nursing. The final
costs are being finalised and will be fed into the 2015/16 budget setting exercise which is
underway.
Whilst temporary pay expenditure continues to exceed the funding available from the
vacant roles (see graphical presentation of forecast Pay position overleaf), expenditure
levels for Agency staff dropped off in November by £0.3m. Total temporary pay expenditure
in the month was £1.83m (£2.08m October), pushing up YTD costs to £16.87m.
Once again there has been an increase in bed days and costs for Out of Area Placements
this month although an action plan to reduce these numbers has now been implemented
and so forecast numbers and costs are expected to now reduce through the remainder of
the year
Other non pay expenditure categories remain broadly in line against original plan.
15
Expenditure – Pay Against original plan, Pay costs report an
adverse variance YTD of £4.11m.
Of the variance, total medical related roles
overspend accounts for £1.05m. There
remains an ongoing review of these
personnel and the vacancies they are
covering in order that expenditure is
restricted as much as possible.
Recruitment plans are in place for a
number of roles in the coming months
which will see the level of expenditure
reduce. It is anticipated however that the
forecast overspend in this area will be in
the region of £1.7m.
The chart shows total spend by pay type
with a forecast level of expenditure. As
previously stated, the drop in October is
due to the TUPE of S75 staff.
The forecast position now accounts for the
additional spend relating to the new
Assessment Ward which will open in
February 2015. Discussions are ongoing
with CCG over the funding of this Ward.
The bank and agency ratio (excluding medical
locum agency) improved significantly this
month with increased Bank expenditure and
greatly reduced Agency costs across DCS
localities and ICT, which in turn has had some
success in recruitment of staff this month.
Bank expenditure now accounts for 51%
(42% last month) of the total bank and agency
expenditure level, some of which is funded by
additional CCG funding for special
observations and ICT trading income.
16
Expenditure – Non Pay 1
The YTD adverse position for Drugs has reduced this month, to £0.31m as costs for
November have come in under budget. This overall adverse position is driven by prior year
costs not accounted for last year and the under-achievement of the Drugs CIP that was
originally planned.
Training and Education expenditure dropped off in the month, and as part of the financial
recovery plan agreement has been reached to reduce expenditure level by £0.1m against
plan. Further discussions across the Trust are ongoing in order to assess training needs for
the remainder of the year. Whilst the YTD position for Training & Education currently reflects
an overspend against the original budget, the Assistant Practitioner and Apprenticeships
training costs have been funded by deferred income received from Health Education
England as well as income from Dementia Alliance. Accounting for this, there is an
underlying favourable position against budget.
The Public Dividend Capital (PDC) forecast reflects the known overspend against plan with
an improved forecast position which has been calculated this month, which in turn has been
reflected in November expenditure levels. Current full year cost pressure is calculated at
£0.54m, but further review could see this reduce again in the coming months.
The favourable position reported for depreciation continues to increase due to the Capital
programme being considerably behind the Trust’s original plan. YTD depreciation is now
favourable by £0.41m with an expected out turn of £0.65m based on the new level of capital
expenditure agreed by the Investment Committee.
17
Expenditure – Non Pay 2
(Specialist and OOA Placements)
Total spend on Specialist and Out of Area placements YTD now amounts to £4.26m.
Specialist placement expenditure in Norfolk accounts for £1.20m of this total but as can be
seen in the graph overleaf, expenditure levels have reduced from earlier in the year and
have largely remained static during last four months, although an increase is reported this
month, which in turn is due to two new placements into longer term care, increasing the
number of externally placed patients to 10. Three of these placements have been identified
as very long term and are currently being reviewed to assess their appropriateness.
A significant rise in the number of bed days once again this month, to 1,221 days (October
872, September 322) for Acute out of area (OOA) placements have seen expenditure
levels rise to their highest ever, at £0.61m for the month. There were 39 admissions in total
during the month. As at the end of the month, 35 patients remain in placements, of which
31 are in the Central locality with 4 over in the West. An action plan has now been put in
place to reduce these numbers going forward and this has led to a review of the forecast
position to the year end. This includes the impact of the new Assessment Ward opening in
February 2015. Total YTD costs now total £2.33m with a forecast level of £4.29m being
predicted. As no specific funding for these placements currently exists, it is these costs
which are placing the biggest cost pressure on the Trust finances. As previously reported
the Trust has indicated to CCGs that responsibility and funding of these placements should
be returned to Commissioning organisations in 2015/16.
There were no PICU placements in the month. YTD expenditure therefore remains at
£0.42m. NHS Funded care costs for November remained at expected levels, pushing the
YTD expenditure to £0.31m. 18
CIP
As previously reported there is a shortfall in the expected CIP delivery at year end
compared to original plan, which has been driven by the Trusts failure to meet prior years
CIP targets on a recurrent basis. Non recurrent measures have been used where possible
to meet these targets to some extent.
Gateway 5 now represents the definite delivery of identified savings including only part of
TSS with a redistribution of savings to other gateways to represent actual savings being
delivered.
The CIP steering group is reviewing a number of initiatives identified by the CIP Interim
Project Director to assess the impact of these over the remaining months of this year on
the Trust’s current forecast deficit of £5.3m. The current position is that the likely impact of
these will reduce this position to a £3.7m forecast deficit.
20
Gateway description
Gateway zero
Gateway one
Gateway two
Gateway three
Gateway four
Gateway five Finance validated and signed off on
delivery plan. Budget is fully allocated
or 100% delivery is certain.
No ideas generated
Idea generated and being investigated
Quality impact assessment (QIA)
completed and signed off.
Detailed Plan completed in full. Full
delivery of plan is highly likely.
Detailed Plan signed off in principle
and adoption started. Full delivery is
likely but details not 100% clear.
Capital
23
The capital programme is now at 77% of the revised plan.
The Trust capital expenditure must remain between £5.53m and £7.48m at year end in
order to meet Monitors acceptable range of 85%-115%.
Currently £3.9m of the capital programme is forecast to be spent in the last four months of
the year, this is 60% of the total 2014/15 capital programme. This high percentage of work
in the latter part of the year is due to a number of delays in work programmes, some of
these are on-going issues and as such a risk that the projects will not be undertaken or
completed by year end exists. A full risk analysis of likelihood of spend has recently been
undertaken and has been reported to the Trust’s Investment Committee.
Balance Sheet
At the end of month 8, the Trust held cash of
£16.5m, £4.7m higher than planned. The
variance is predominantly due to the continuing
low level of capital expenditure. .
Net current liabilities continue to be higher
(£5.9m) than planned due to higher than
anticipated accruals and holding higher levels
of provisions being held for possible HMRC
liabilities. This is offset by a lower than forecast
trade and other payable balance. This is due in
part to non-receipt of invoices for services
currently being accrued for.
Non current assets are now £10.7m behind
plan due to the recognition of St Clements as
an asset held for sale, and slippage on capital
projects.
An aged debtor analysis by Quarter is detailed
in the bottom table.
24
Cash flow
The cash balance of £16.5m is £4.7m ahead of the annual plan. This reflects the slippage
in capital expenditure .
The forecast cash position is currently £10.0m at 31st March 2015 against a plan of
£21.41m. The forecast level of revenue expenditure requires that the cash position will
continue to be under high scrutiny for the remainder of the year and going forward.
Additional controls are being introduced on expenditure over £500 to increase the level of
oversight on non-pay expenditure.
25
COSRR forecast
26
COSRR has now been reviewed against the revised forecast for the 2014-15 financial
year and taking into account the reductions already forecast in expenditure in the period.
There is no allowance for any unforeseen additional spend which may arise.
In light of the revised forecast a COSRR of two is now expected for the remainder of the
year.
Board of Directors – Private 18
th December 2014
Business Performance Report
Version 1 0
Author: Tim Walsh Department: Informatics
Page 1 of 6 Date produced: 08th
December 2014
Retention period: 30 years
Report To: Board of Directors – Public
Meeting Date: 18th December 2014
Title of Report: Business Performance Report – M08 2014/15
Action Sought: For Approval
Estimated time: 20 Minutes
Author: Tim Walsh: Business Intelligence Manager
Director: Andrew Hopkins: Director of Finance
Executive Summary:
The Business Performance report shows that the Trust is compliant across all seven of the key performance standards under the Monitor Risk Assessment Framework. This is shown in the monitor targets section. The overall COSRR rating remains at 2.
1.0 Report contents
1.1 The Business Performance Report is submitted to the Board for month 08 2014/15 and contains details of performance against key Monitor Compliance Framework targets and KPIs for Finance, Organisational Delivery, Quality, Safety & Experience and Workforce Development & Effectiveness.
1.2 The Trust remains at an overall COSRR of 2.
2.0 Monitor Targets
2.1 Monitor Performance Summary
Ref Measure Target Quarter 3 to Date (M08)
M01 CPA patients receiving follow up within 7 days of discharge
95% 99% 146 out of 148 discharges
M02 CPA patients having formal review within 12 months
95% 97% 1,968 out of 2,026 reviews
M03 Minimising Delayed Transfers of Care
7.5% 5% 1334 delayed days out of 26,609 bed days
M04 Admissions to inpatient services had access to Crisis Resolution and Home Treatment (CRHT) teams
95% 99% 222 out of 225 admissions gate-kept
Date: 18 December 2014
I Item: 17.171 v
Board of Directors – Private 18
th December 2014
Business Performance Report
Version 1 0
Author: Tim Walsh Department: Informatics
Page 2 of 6 Date produced: 08th
December 2014
Retention period: 30 years
M05 Meeting commitment to serve new psychosis cases by Early Intervention teams
95% 133% 150 new cases against target of 113
M06 Data completeness: Identifiers 97% 99%
220,038 valid entries out of 221,532 possible data fields
M07 Data completeness: Outcomes 50% 82%
8,683 valid records out of 10,536 records
3.0 Performance
3.1 Director of Operations Norfolk and Waveney Summary
The main areas to highlight in Norfolk and Waveney are:
Out of area placements have decreased in November and the locality has started to see a reduction in out of area placements. Addressing the number of out of area placements remains a priority.
Performance in terms of the timeliness of data entry has further improved in Central Norfolk and West Norfolk for November.
DTOC moved below the 7.5% threshold in November reporting at 6.79% in Central Norfolk.
The IAPT service continued to report below the 15% access trajectory.
The locality is continuing to interview and recruit but they do have an issue with recruiting to certain bands which means that teams have to carry vacancies which increases pressure on the service.
3.2 Director of Operations Suffolk Summary
The main areas to highlight in Suffolk are:
DTOCs in Suffolk East remain high at 11% in November although this is a reduction from the previous month.
Performance against the IAPT 15% access target is improving and was achieved in West Suffolk in November.
The number of 18 week waits has decreased in Suffolk after a spike in October.
3.3 Minimising delayed transfers of care (DTOC)
In November the DTOC position for the trust decreased to 5.01%, but still within the 7.5% threshold. Suffolk East continues to report above the threshold at 11.12%. In Central Norfolk the DTOCs were breaching the 7.5% target in October but this has now reduced to 6.79% in November.
DTOCs were still high in East Suffolk and the locality manager reported that the DTOCs in Suffolk will not be improved until a new service model which is currently being finalised is
Board of Directors – Private 18
th December 2014
Business Performance Report
Version 1 0
Author: Tim Walsh Department: Informatics
Page 3 of 6 Date produced: 08th
December 2014
Retention period: 30 years
put in place. The service is continuing to work in conjunction with Social services to look at the delays especially those that are awaiting placements in residential care especially the Learning Disability patients.
3.4 Percentage of qualifying patients with a MHCT cluster (OD07)
In November the trust reported at 98% against a 99% target. In Suffolk East and West a number of data corrections are being made and the position is expected to improve in future reports. Members of the admin team within the IDTs (integrated delivery teams) are sending out cluster quality reports to clinicians. In addition to this the East Suffolk locality are monitoring the referrals coming from AAT into the IDT to ensure they have a cluster and to return to AAT if it is missing.
3.6 Data quality including timely entry (OD09)
The trust performance improved further from October to November from 92% to 94%. Further improvements were seen in the Central Norfolk and West Norfolk localities at 91% and 96% respectively. All localities are working on a trajectory to improve this data quality item and this continues to be raised within the teams for action and is brought to the attention of service managers at the internal performance review meetings.
3.7 Percentage of IAPT patients who have depression and or anxiety disorders who receive psychological therapy
Access rates continue to be below the target trajectory for November reporting at 7.88% against a target of 10%.
Suffolk West achieved their target, Suffolk East missed the target by 0.7%. Norfolk Central missed the target by 3.01%. The locality manager in Suffolk was keen for this good performance to be carried in to quarter 4 which is when commissioners are expecting the access performance target to be achieved.
In Norfolk a redesign of the way the IAPT service processes referrals and throughput to treatment is taking place. In addition to this, the service are recruiting and training administrative staff to process the increased referrals that are coming through to the service. Action plans remain in place across all localities to meet the 15% access rate by the end of quarter 4 2014/15.
3.8 Medium and Low Secure Bed Occupancy Rate The low secure bed occupancy reached 90% in November, an increase of 4% from last month. Medium secure bed occupancy stayed at 79%, this is below the 90% target. The occupancy rate in these units is being monitored by the service and by commissioners.
3.9 Waiting times in completed pathways breaching standard and Number of incomplete pathways waiting over 18 weeks
The number of 18 week waits decreased from 86 to 80 for the trust between October to November. The numbers of 18 week waits increased in Central Norfolk from 14 to 34. The
Board of Directors – Private 18
th December 2014
Business Performance Report
Version 1 0
Author: Tim Walsh Department: Informatics
Page 4 of 6 Date produced: 08th
December 2014
Retention period: 30 years
reason for the breaches is being investigated. In Suffolk East, the number of 18 week waits decreased from 42 in October to 10 in November.
3.10 Patient Safety Thermometer (QU14)
The trust reported at 97% for the patient safety thermometer in November. There were two falls reported in Reed in Central Norfolk. One fall was also reported in Fernwood and one fall was reported in Foxglove, both in Great Yarmouth and Waveney.
3.11 Bed occupancy, out of locality and out of area acute placements
There were 33 out of area placements reported in Norfolk and Great Yarmouth and Waveney as of the end of November. This figure has decreased from the previous month. Assessors remain in place to review the out of area cases in Norfolk specifically with a task to address the out of area cases. Bed occupancy remains high across the adult acute areas and this was reflective of demand in November.
3.12 Access and Assessment
Norfolk
The Access and Assessment information is not currently available at the time of writing.
Suffolk
In Suffolk, the Access and Assessment is not currently available at the time of writing.
3.13 Norfolk Recovery Partnership (NRP) and Suffolk Alcohol Service
The Norfolk Recovery Partnership has completed all of the actions on the Remedial Action Plan and this has now been signed off by commissioners. October was the first month that the new contract report was submitted to NRP commissioners and the new report was positively received.
NDTMS data is showing an improvement in NRP’s performance especially around the areas that the commissioners were expressing concerns. Now that the local performance management framework has been agreed, this should result in more beneficial local data to not only monitor performance against the contract but also inform service delivery.
With regard to the Suffolk Alcohol Service, performance is robust and constant with no areas of concern. The contract finishes on the 31st March 2015.
3.14 Research Performance Indicators
The Key Performance Indicators as set by the National Institute of Health Research (NIHR – DH) are going to be changed for 2014/15 but have not yet been announced nationally. The KPIs are designed to give a reflection of overall research activity and performance for the Trust compared to other Trusts nationally. The Research Manager does not have the new KPIs to report at present.
Board of Directors – Private 18
th December 2014
Business Performance Report
Version 1 0
Author: Tim Walsh Department: Informatics
Page 5 of 6 Date produced: 08th
December 2014
Retention period: 30 years
4.0 Section 75 Partnership
Suffolk
There have been no notable high level developments with regard to the Suffolk Section 75 Partnership. New procedural arrangements have been implemented across all teams and are subject to on-going monitoring with a more detailed review scheduled for spring 2015.
Work is progressing between Informatics leads in Suffolk CC / NSFT and the Lorenzo Programme Team to ensure that new patient electronic recording system has the capacity to report out on the ‘Adult Social Care Outcome’ requirements for contract monitoring and national reporting requirements.
The partnership between Suffolk CC remains strong and remains jointly motivated to work closely together as they move through service developments. The working arrangements continue to be overseen by the Section 75 Partnership Review Group that meets quarterly and has director level presence from both organisations.
5.0 Workforce Development and Effectiveness
5.1 Vacancies
The Trusts current vacancy rate (WD08) is 11.65%. This is a decrease of 0.15% in the month. In real terms at M8 the Trust had an establishment of 3874.48 and 451.21 vacant posts.
Vacancy rates continue to be above 10% in Corporate Services (20.91%), Suffolk Access and Assessment (14.75%) and Suffolk West (17.62%). All other localities are below 10%.
5.2 Turnover
At M8 staff turnover (WD09) within the Trust is currently at 16.57%,a reduction of -1.29% in the month.
Turnover within Central Norfolk (-2.04%, at 19.19%), Corporate (-1.01%, at 20.16%), Great Yarmouth and Waveney (-6.13%, at 12.95%) and West Norfolk (-2.49%, at 22.38%) have all reduced in the month. Turnover within Secure Services (+0.68% at 13%), Suffolk East (+0.30% at 14.03%) and Suffolk West (+0.83% at 19.26%) have marginally increased in the month.
5.3 Temporary Resourcing
The percentage of nursing shifts that NHSP filled increased from 63.72% to 69.01% in the month. During November, agency staff covered a further 21.68% of available nursing shifts. 9.31% of vacant shifts went unallocated.
5.4 Absence
Overall, the Trusts rolling 12 month sickness absence rate (WD01) has decreased in the month form 5.26% in October 2014 to 5.09% in November 2014.
Board of Directors – Private 18
th December 2014
Business Performance Report
Version 1 0
Author: Tim Walsh Department: Informatics
Page 6 of 6 Date produced: 08th
December 2014
Retention period: 30 years
5.5 Workforce development Appraisals completed since April 2014 within the Trust is currently 63.8%.
5.7 Employee Relations
Currently there are 32 active disciplinary cases within the Trust (+ 4 within the month). There are 8 grievance matters on-going within the Trust (no change within the month). Across all localities, there are 3 formal capability matters (no change within the month). There are 137 absence cases being managed (+5 in month).
6.0 Finance
6.1 Not currently available.
7.0 Recommendations
7.1 The Board is requested to consider the Trust’s performance as described within the Business Performance Report.
Tim Walsh Business Intelligence Manager 09
th December 2014
Business Performance ReportNovember 2014 version 2.0
NSFT Informatics
1 BPR November 2014 v2.0/Front
Monitor
Ref Metric Period Value Apr-14 May-14 Jun-14 Jul-14 Aug-14 Sep-14 Oct-14 Nov-14 Dec-14 Jan-15 Feb-15 Mar-15
Actual 100% 98% 98% 100% 100% 99% 99% 99%
Target 95% 95% 95% 95% 95% 95% 95% 95% 95% 95% 95% 95%
Trend
Actual 98% 97% 97% 98% 98% 97% 97% 97%
Target 95% 95% 95% 95% 95% 95% 95% 95% 95% 95% 95% 95%
Trend
Actual 4.05% 4.87% 4.55% 3.58% 5.04% 5.14% 5.59% 5.01%
Target 7.50% 7.50% 7.50% 7.50% 7.50% 7.50% 7.50% 7.50% 7.50% 7.50% 7.50% 7.50%
Trend
Actual 100% 100% 100% 98% 98% 98% 100% 99%
Target 95% 95% 95% 95% 95% 95% 95% 95% 95% 95% 95% 95%
Trend
Actual 79% 89% 133% 140% 125% 131% 135% 133%
Target 95% 95% 95% 95% 95% 95% 95% 95% 95% 95% 95% 95%
Trend
Actual 100% 100% 100% 100% 99% 100% 99% 99%
Target 97% 97% 97% 97% 97% 97% 97% 97% 97% 97% 97% 97%
Trend
Actual 83% 83% 83% 83% 82% 82% 81% 82%
Target 50% 50% 50% 50% 50% 50% 50% 50% 50% 50% 50% 50%
Trend
Actual 6 6 6 6 6 6 6 6
Target 6 6 6 6 6 6 6 6 6 6 6 6
Trend
Performance is neither improving or worsening
Performance is worsening
Performance is improving
M01CPA patients receiving follow up within
7 days of discharge
Month
YTD
M03 Minimising delayed transfers of careMonth
YTD
M02CPA patients having formal review
within 12 months
Month
YTD
M04Admissions to inpatient services had
access to CRHT teams
Month
YTD
M08
Trend is calculated using Actual at Month 7 2014/2015 as compared to
the Actual in the current month
M05
Meeting commitment to serve new
psychosis cases by early intervention
teams
Month
YTD
M06 Data Completeness: IdentifiersMonth
YTD
Self-certification against compliance
regarding access to healthcare for
people with LD
Month
YTD
M07 Data Completeness : OutcomesMonth
YTD
2 BPR November 2014 v2.0/Monitor
Organisational Delivery
Ref Metric Period Value Apr-14 May-14 Jun-14 Jul-14 Aug-14 Sep-14 Oct-14 Nov-14 Dec-14 Jan-15 Feb-15 Mar-15
Actual 98% 97% 97% 98% 98% 97% 97% 97%
Target 95% 95% 95% 95% 95% 95% 95% 95% 95% 95% 95% 95%
Trend
Actual 4.05% 4.87% 4.55% 3.58% 5.04% 5.14% 5.59% 5.01%
Target 7.50% 7.50% 7.50% 7.50% 7.50% 7.50% 7.50% 7.50% 7.50% 7.50% 7.50% 7.50%
Trend
Actual 100% 100% 100% 98% 98% 98% 100% 99%
Target 95% 95% 95% 95% 95% 95% 95% 95% 95% 95% 95% 95%
Trend
Actual 79% 89% 133% 140% 125% 131% 135% 133%
Target 95% 95% 95% 95% 95% 95% 95% 95% 95% 95% 95% 95%
Trend
Actual 100% 100% 100% 100% 99% 100% 99% 99%
Target 97% 97% 97% 97% 97% 97% 97% 97% 97% 97% 97% 97%
Trend
Actual 83% 83% 83% 83% 82% 82% 81% 82%
Target 50% 50% 50% 50% 50% 50% 50% 50% 50% 50% 50% 50%
Trend
Actual 97% 97% 98% 98% 97% 97% 97% 98%
Target 99% 99% 99% 99% 99% 99% 99% 99% 99% 99% 99% 100%
Trend
OD02 Minimising delayed transfers of careMonth
YTD
OD06 Data Completeness: OutcomesMonth
YTD
OD05 Data Completeness: IdentifiersMonth
YTD
% of qualifying patients with a MHCT
cluster
Month
YTD
OD01CPA patients having formal review
within 12 months
Month
YTD
OD04Meeting commitment to new psychosis
cases by EI
Month
YTD
OD03Admissions to inpatient services had
access to CRHT teams
Month
YTD
OD07
3 BPR November 2014 v2.0/Organisational Delivery
Organisational Delivery
Ref Metric Period Value Apr-14 May-14 Jun-14 Jul-14 Aug-14 Sep-14 Oct-14 Nov-14 Dec-14 Jan-15 Feb-15 Mar-15
OD01CPA patients having formal review
within 12 months
Month
YTD
Actual 91% 91% 89% 92% 93% 91% 92% 94%
Target 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% 100%
Trend
Actual 98% 98% 99% 100% 99% 95% 97% 99%
Target 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% 100%
Trend
Actual 0.73% 1.60% 2.63% 3.69% 4.47% 5.44% 6.61% 7.88%
Target 1.25% 2.50% 3.75% 5.00% 6.25% 7.50% 8.75% 10.00% 11.25% 12.50% 13.75% 15.00%
Trend
Actual 51% 50% 53% 50% 46% 49% 44% 45%
Target 40% 40% 40% 40% 40% 40% 40% 40% 40% 40% 40% 40%
Trend
Actual 81% 82% 83% 79% 78% 83% 79% 79%
Target 90% 90% 90% 90% 90% 90% 90% 90% 90% 90% 90% 90%
Trend
Actual 85% 80% 79% 81% 87% 84% 86% 90%
Target 90% 90% 90% 90% 90% 90% 90% 90% 90% 90% 90% 90%
Trend
Actual 15 16 14 15 17 15 16 17
Target 28 28 28 28 28 28 28 28 28 28 28 28
Trend
Trend is calculated using Actual at Month 7 2014/2015 as
compared to the Actual in the current month
OD16Average Length of Stay - Adult Acute
Service
Month
YTD
OD10
OD13
% of IAPT patients who complete
treatment and 'move to recovery during
the month
Month
YTD
OD12
% of IAPT patients who have
depression and/or anxiety disorders
who receive psy therapy
Month
YTD
% of inpatient Finished Consultant
episodes during the period with an
ICD10 code
Month
YTD
OD09
Number of contacts recorded on Trust
systems within 3 working days of event
(Last 30 days)
Month
YTD
OD15Low Secure Bed Occupancy Rate
(including leave)
Month
YTD
OD14Medium Secure Bed Occupancy Rate
(including leave)
Month
YTD
4 BPR November 2014 v2.0/Organisational Delivery
Quality, Safety and Experience
Ref Metric Period Value Apr-14 May-14 Jun-14 Jul-14 Aug-14 Sep-14 Oct-14 Nov-14 Dec-14 Jan-15 Feb-15 Mar-15
Actual 100% 98% 98% 100% 100% 99% 99% 99%
Target 95% 95% 95% 95% 95% 95% 95% 95% 95% 95% 95% 95%
Trend
Actual 67 54 46 64 49 47 86 80
Target 0 0 0 0 0 0 0 0 0 0 0 0
Trend
Actual 92% 75% 91% 77% 83% 89% 95% 96%
Target 80% 80% 80% 80% 80% 80% 80% 80% 80% 80% 80% 80%
Trend
Actual 97% 100% 97% 100% 96% 95% 98% 97%
Target 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% 100%
Trend
Actual 100% 100% 100% 100% 100% 100% 100% 98%
Target 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% 100%
Trend
QU01CPA patients receiving follow up within
7 days of discharge
Month
YTD
QU04Waiting Times - Number of incomplete
pathways waiting > 18 weeks
Month
YTD
Waiting Times - % of CAMHS patients
seen within standard
Month
YTD
QU14Patient Safety Thermometer
(Development KPI)
Month
YTD
QU05
QU17
% of long-term (over 12 months)
inpatients that have received an annual
health check
Month
YTD
5 BPR November 2014 v2.0/Quality, Safety & Experience
Workforce Development and Effectiveness
Ref Metric Period Value Apr-14 May-14 Jun-14 Jul-14 Aug-14 Sep-14 Oct-14 Nov-14 Dec-14 Jan-15 Feb-15 Mar-15
Actual 5.59% 5.62% 5.55% 5.59% 5.41% 5.34% 5.26% 5.09%
Target 4.76% 4.76% 4.76% 4.76% 4.76% 4.76% 4.76% 4.76% 4.76% 4.76% 4.76% 4.76%
Trend
Actual 12.17% 11.38% 11.37% 11.36% 11.68% 11.52% 11.02% 9.78%
Target 20.00% 20.00% 20.00% 20.00% 20.00% 20.00% 20.00% 20.00% 20.00% 20.00% 20.00% 20.00%
Trend
Actual 11.84% 15.51% 11.96% 12.06% 11.50% 11.61% 10.90% 11.06%
Target 6.52% 6.52% 6.52% 6.52% 6.52% 6.52% 6.52% 6.52% 6.52% 6.52% 6.52% 6.52%
Trend
Actual 24.31% 24.13% 24.52% 25.04% 25.60% 26.02% 26.08% 26.38%
Target 16.17% 16.17% 16.17% 16.17% 16.17% 16.17% 16.17% 16.17% 16.17% 16.17% 16.17% 16.17%
Trend
Actual 61.60% 49.30% 46.20% 16.44% 25.72% 58.80% 39.50% 63.79%
Target 100.00% 100.00% 100.00% 100.00% 100.00% 100.00% 100.00% 100.00% 100.00% 100.00% 100.00% 100.00%
Trend
Actual N/A N/A N/A N/A N/A N/A N/A N/A
Target 100.00% 100.00% 100.00% 100.00% 100.00% 100.00% 100.00% 100.00% 100.00% 100.00% 100.00% 100.00%
Trend
Actual 14 11 13 12 12 11 6 7
Target 33 33 33 33 33 33 33 33 33 33 33 33
Trend
Actual 11.84% 11.59% 12.06% 12.38% 11.97% 11.91% 11.80% 11.65%
Target 10.00% 10.00% 10.00% 10.00% 10.00% 10.00% 10.00% 10.00% 10.00% 10.00% 10.00% 10.00%
Trend
WD07
Number of statutory/mandatory training
elements which are below 40%
compliance.
Month
YTD
WD08 Vacancy RateMonth
YTD
WD05
% of staff with an appraisal since April
2013Month
YTD
WD06
% of medical staff compliance with
planned 2014/15 appraisal timetable
(Cohort 1)
Month
YTD
WD03% of sickness absence episodes > = 21
days
Month
YTD
WD04% of sickness absence days attributed
to Anxiety/stress/depression/etc.
Month
YTD
WD01 Annualised sickness absence rateMonth
YTD
WD02% of staff with 4 or more absence
episodes (WD2)
Month
YTD
6 BPR November 2014 v2.0/Workforce Development & Eff
Workforce Development and Effectiveness
Ref Metric Period Value Apr-14 May-14 Jun-14 Jul-14 Aug-14 Sep-14 Oct-14 Nov-14 Dec-14 Jan-15 Feb-15 Mar-15
WD01 Annualised sickness absence rateMonth
YTD
Actual 15.65% 17.54% 15.69% 14.25% 17.37% 17.23% 17.86% 16.57%
Target 10.00% 10.00% 10.00% 10.00% 10.00% 10.00% 10.00% 10.00% 10.00% 10.00% 10.00% 10.00%
Trend
Actual 51.34% 49.91% 51.17% 52.27% 50.52% 47.51% 47.88% 47.51%
Target 45.00% 45.00% 45.00% 45.00% 45.00% 45.00% 45.00% 45.00% 45.00% 45.00% 45.00% 45.00%
Trend
Actual
Target
Trend
Actual
Target
Trend
Trend is calculated using Actual at Month 7 2014/2015 as
compared to the Actual in the current month
WD11Staff engagement - mini survey
(Development KPI)
Month
YTD
WD12Staff in post to caseload ratio
(Development KPI)
Month
YTD
WD09 Turnover RateMonth
YTD
WD10 % of resignations which are voluntaryMonth
YTD
7 BPR November 2014 v2.0/Workforce Development & Eff
Financial Management
Ref Metric Period Value Apr-14 May-14 Jun-14 Jul-14 Aug-14 Sep-14 Oct-14 Nov-14 Dec-14 Jan-15 Feb-15 Mar-15Full Year
Outturn
Actual 3 3 3 3 3 3 2 2
Target 3 3 3 2 2 3 3 3 3 3 3 3 3
Trend
Actual 3 3 3 2 2 2 1 1
Target 3 3 3 3 3 3 4 4 3 4 4 3 3
Trend
Actual 3 3 3 3 3 3 3 2
Target 2 2 2 1 1 2 2 2 2 2 2 3 3
Trend
Actual 10.30% 10.12% 19.48% 29.52% 18.47% 7.37% 7.75% 10.79%
Target 5.00% 5.00% 5.00% 5.00% 5.00% 5.00% 5.00% 5.00% 5.00% 5.00% 5.00% 5.00% 5.00%
Trend
Actual 5.10% 4.48% 5.41% 2.55% -0.85% 0.56% -0.27% -0.02%
Target 5.00% 5.00% 5.00% 5.00% 5.00% 5.00% 5.00% 5.00% 5.00% 5.00% 5.00% 5.00% 5.00%
Trend
Actual 2.02% 7.19% 11.32% 14.74% 17.01% 24.50% 30.25% 43.69%
Target 10.96% 22.30% 35.55% 46.25% 56.50% 64.97% 69.86% 75.34% 81.83% 87.21% 92.62% 100.00% 100.00%
Trend
Actual 51.91% 55.11% 55.11% 70.48% 61.62% 65.52% 67.32% 69.23%
Target 79.91% 81.65% 83.40% 85.15% 86.90% 88.65% 90.54% 92.43% 94.33% 96.22% 98.11% 100.00% 100.00%
Trend
FM01 Continuity of Service Risk RatingMonth
YTD
FM02 Capital Service Cover ratingMonth
YTD
FM03 Liquidity ratingMonth
YTD
FM04Debtors > 90 days past due account for
more than 5% of the total debtor base
Month
YTD
FM05
Creditors > 90 days past due account
for more than 5% of the total creditor
balances
Month
YTD
FM06 CAPEX % of plan spentMonth
YTD
FM07CIPs % of planned CYE (R&NR)
savings achieved
Month
YTD
BPR November 2014 v2.0/KPI Financials 14_15
Board of Directors – Public 18Dec2014 Board Assurance Framework
Version 0.1 Author: Robert Nesbitt Department: Corporate
Page 1 of 2 Date produced: 05Dec2014 Retention period: 30 years
Report To: Board of Directors – public
Meeting Date: 18th December 2014
Title of Report: Board Assurance Framework
Action Sought: For Approval
Estimated time: 10 minutes
Author: Robert Nesbitt: Trust Secretary
Executive: Robert Nesbitt: Trust Secretary
Executive Summary:
The outcomes of the 27th November 2014 board discussion have been incorporated into the December 2014 report (see appendix 1). Risks previously owned by the Director for OD and Workforce have been reallocated. The Board considered that all the main risks to the Trust’s objectives had been captured in the BAF and noted that almost all of the board agenda was focussed on actions to reduce these risks to acceptable levels. Whilst the BAF provides a useful tool for the Board to pull these risks and actions together into one place, the detail of the design of the BAF should not form a significant focus for Board time, since this risks diluting from the focus of the Board on ensuring delivery of the changes required. Since the last meeting, Monitor’s decision to launch an investigation in the light of the Trust’s deteriorating financial position (and the implications this may have for the way the Trust is managed) means that Theme 2, System Confidence, moves to a red on mitigation confidence. The Trust Secretary continues to meet with the Trust’s Head of Risk Management each month to cross-check the BAF with the Risk Register. NB: The mitigation RAAG rating is based on Monitor’s Governance Risk Rating system which is set out below. This 4 point scale is used as a guide only for the use of the Board. A Red ‘likely risk of breach’ is the highest level of unmitigated risk but needs to be understood in the context of the additional actions set out in the BAF and elsewhere in board papers. It does not mean that a breach is necessarily imminent but flags the most serious issues. ‘Red’ (the mitigation is so weak that there is likely risk of a breach to the provider license), ‘Red / Amber’ (the mitigation is such that there are material concerns of a breach to the provider license), ‘Amber Green’ (the mitigation leaves limited concerns of a breach). ‘Green’ (the mitigation is so strong as to mean that there are no material concerns of a breach). Scores shown are ‘Consequence x Likelihood’ as recorded on Datix. The executive owner is not always the
Date: 18th
December 2014
J Item: 14.171 vii
Board of Directors – Public 18Dec2014 Board Assurance Framework
Version 0.1 Author: Robert Nesbitt Department: Corporate
Page 2 of 2 Date produced: 05Dec2014 Retention period: 30 years
risk owner on Datix (this is intentional).
1.0 Conclusion
9.1 Board members are to review the BAF themes and consider whether any additional actions are required to provide assurance on management of the risks.
9.2 The Board is also asked to consider whether there are additional significant risks that have come to light but which are not represented in the BAF at present.
Robert Nesbitt Trust Secretary
Appendix 1 – Board Assurance Framework
Board Assurance Framework December 2014
Board of Directors – Public 18Dec 2014 Board Assurance Framework
Version 0.3
Author: Robert Nesbitt Department: Corporate
Page 1 of 10 Date produced: 08Dec2014 Retention period: 30 years
1. Name of risk theme (board committee with oversight)
Staffing (OD and WF Committee)
1.1 Relevant Trust objectives:
Implementation of Hard Truths recommendations so agreed inpatient staffing levels are achieved, maintained and published weekly from June 2014.
To agree recording and monitoring process for safe caseloads levels by October 2014.
Delivery of a Workforce and OD strategy.
1.2 What is the nature of the risk? The risk is that shortage of staff capacity impacts on safety. The key drivers for this risk include mistakes that were made in the modelling for community team establishments as part of the N&W Trust Service Strategy with underestimates of care coordinator numbers and loss of experienced staff who were able to safely manage risk. Teams which have been fragmented or reconstituted can experience a shift in risk tolerance which moves service pressure into Crisis Teams and OOAs. In inpatient areas risks can arise through a shortage of qualified staff on shifts, staff without the right skills (such as Prevention and Management of Aggression (PMA) training) or staff who have not yet built up experience in supporting people with complex needs.
1.3 How is the risk controlled and mitigated? In community services, the risk is mitigated by the FACT model being introduced across all teams, additional support worker resource being provided by MIND to enhance community capacity, admission prevention service being provided by Julian Support/West Norfolk MIND and a Robust duty worker system in place in all community teams. There is a plan to introduce the “Waves” model for service users with a diagnosis of Personality Disorder in Norfolk and Waveney. A bespoke crisis support telephone line for service users to be introduced (operated by MIND) by December 2014. Recording and monitoring safe caseloads: Implementation of a caseload weighting tool is due for completion 31/12/14. A review of the access and assessment function is underway with a plan to deploy those staff into community teams As an immediate mitigation in inpatient areas, where qualified staff are not available shifts are strengthened with unqualified but experienced support workers. See the Safe Staffing report on the Board agenda this month. Managers allocate staff and move people to other areas so as to prioritise risk. The overspend on temporary staffing indicates that patient safety is prioritised. Staff are encouraged to report staffing shortages using Datix, and they do so, which means that action can be taken by managers to mitigate risks. Risk owner for these aspects are Debbie White Directors of Operations N&W and Ian Young as Acting Directors of Operations Suffolk. In the longer term, the Flexible Working Strategy includes specific measures to improve staffing levels. Some
Confidence level in mitigation:
Red/Amber
Board Assurance Framework December 2014
Board of Directors – Public 18Dec 2014 Board Assurance Framework
Version 0.3
Author: Robert Nesbitt Department: Corporate
Page 2 of 10 Date produced: 08Dec2014 Retention period: 30 years
progress has been made in filling vacancies although retention remains a challenge. See also Staff Engagement report on the agenda this month. The risk owner for this aspect is Leigh Howlett
1.4 What additional actions are required? None in addition to those set out above.
1.5 How do these risks show on the Trust’s Risk Register? Who owns these risks? Datix 1116 (vacancy impact on services) = 4x3=12 Leigh Howlett Datix 1141 Inability to deliver corporate services safely due to high level of vacancies 3 x 3 = 9 Leigh Howlett Datix 1133 (difficulty recruiting in West Suffolk). 3x4 =12. Ian Young. Datix 1155 (accessing PMA staff via NHSP) 4x5=20 Ian Young. Datix 1123 3 x 4 = 12 / 1065 3 x 4 = 12 / 1033 3 x 5 = 15 (high caseloads) Owner Debbie White.
1.6 What is the timeline for the mitigation confidence level to reach ‘green’? To address the N&W community capacity shortages contract negotiations with CCGs have flagged the need for additional funding for care coordinators. This will feed into the 2015/16 contracts. Delivery of the Workforce and OD strategy is part of the two year operational plan and five year strategic plan. The business care for e-rostering bas been approved and will be rolled out by year end with a full implementation date of March 2016. However, it is recognised that whilst e-rostering is a foundation for pre effective use of staff, the behavioural aspects that will deliver changes in practice will need to be promoted by managers and clinicians in order to deliver improvements.
Board Assurance Framework December 2014
Board of Directors – Public 18Dec 2014 Board Assurance Framework
Version 0.3
Author: Robert Nesbitt Department: Corporate
Page 3 of 10 Date produced: 08Dec2014 Retention period: 30 years
2. Name of risk theme (board committees with oversight)
System confidence (Finance and Performance Committee / Comms Committee)
2.1 Relevant Trust objectives:
For the 2014/15 financial year: delivery of all operational targets including receiving 100% CQUIN and the avoidance of any operational and financial penalties from commissioners in the final quarter of the year.
Engage with the wider health economy, third and voluntary sector to ensure the Trust is a known and trusted partner evidenced by a 10% increase in new business with external parties by March 2015, evidenced by financial turnover.
We will look for, and exploit, opportunities to work on prevention and anti-stigma by development and delivery of a robust communication plan, evidenced by monthly positive media messages from launch in September 2014.
2.2 What is the nature of the risk? The Monitor investigation has raised the risk of a loss of system confidence in the management of the Trust. If regulatory action follows it could impact on the ability of the Trust to retain and win contracts, and would impact on management capacity. It could also weaken the public’s confidence in the quality of the service which might inhibit people from seeking help who need our support. A critical CQC report based on the inspection visit in October 2014 could weaken patient (and wider) confidence in the Trust. In addition, the loss of some CQUIN income in Q1 and Q2 means that receiving 100% of CQUIN income as set out in the Trust objective above is not achievable which risks undermining confidence in the Trust’s ability to deliver.
2.3 How is the risk controlled and mitigated?
1. Constructive response to the Monitor investigation to assist the Trust’s recovery plans 2. Prioritisation of meeting performance standards and addressing problems quickly. The Business Performance
Report indicates improvements across several areas, but note the cross-reference with financial performance which continues to fall short (see 7. Finance)
3. Positive attempts to reach out to the Campaign so as to find common ground in our joint desire to protect and improve services.
4. When the draft CQC report is received for comment ensure that the report is an accurate representation of Trust services.
5. There has been recognition in local media of the excellent work of our staff through the work of the communications team.
6. Endeavours to improve CQUIN performance for Q3 – 4 so as to maximise income and system confidence in ability of Trust to deliver. This is supported by moving CQUIN to the Trust’s contracting function and a dedicated resource to support delivery.
7. There are plans in place to increase new business (such as peri-natal mental health and eating disorders) although this does not yet amount to 10% (by turnover).
Confidence level in mitigation:
Red
2.4 What additional actions are required? None in addition to those set out above.
2.5 How do these risks show on the Trust’s Risk Register? Who owns these risks? Datix ID 1112(Risk of damage to Trust reputation) 4 x
Board Assurance Framework December 2014
Board of Directors – Public 18Dec 2014 Board Assurance Framework
Version 0.3
Author: Robert Nesbitt Department: Corporate
Page 4 of 10 Date produced: 08Dec2014 Retention period: 30 years
3 = 12 Owner Michael Scott. Datix ID 1144 (Risk of poor CQC report affecting confidence in Trust) 4 x 3 = 12 Owner Jane Sayer.
2.6 What is the timeline for the mitigation confidence level to reach ‘green’? System confidence is closely linked to the other risk themes on the BAF, and so the finance recovery plan which runs over 18 months sets the outer milestone. However, this could be impacted by the CQC inspection report, the first draft of which is expected on 18.12.14 to for accuracy checking.
Board Assurance Framework December 2014
Board of Directors – Public 18Dec 2014 Board Assurance Framework
Version 0.3
Author: Robert Nesbitt Department: Corporate
Page 5 of 10 Date produced: 08Dec2014 Retention period: 30 years
3. Name of risk theme (board committees with oversight)
Quality (Service Governance Committee / Finance and Performance Committee)
3.1 Relevant Trust objectives:
Achieve zero out of area non specialist bed placements by March 2015.
Achieve a positive CQC review in 2014 and effectively addressing any issues that arise as part of this.
3.2 What is the nature of the risk? Risks to quality are made up of several factors including operational performance and clinical and corporate governance. Service pressures may lead to safety risks to patients and, as a result, to very high stress staff levels. Service user and carer experience may be compromised by service delays and mistakes. Caseload pressures partly as a result of the S.75 changes in N&W and partly because of problems with the TSS modelling assumptions have quality implications across the care pathway including bed pressures. SGC has also flagged that slippage on the work on Restrictive Interventions and weak assurance from an IA report on clinical supervision give rise to quality risks. Weaknesses in the board in having a clear line of sight to services may compromise the ability of the board to provide leadership and to prioritise effectively.
3.3 How is the risk controlled and mitigated? 1. Out of area acute capacity placements in N&W remain high (c.30) but have reduced from their high 40s level earlier in the autumn. Planning is underway to open 10 additional beds. 2. Whilst caseloads in many N&W community teams are unsustainably high there is mitigation in that the whole care pathway is being reviewed to balance resources and improve community services capacity. This cross-references to staff recruitment and retention. 3. There is a risk that learning from incidents is not adequately shared so that lessons are not learned. Mitigation: The DoN and MD scrutinise every report, identifying themes and reporting these to the Senior Mgt Forum. Clinical audit reviews how well embedded lessons are. The Service Governance Ctte continues to flag this as a concern. See SGC report. The Board received an update report on Restrictive Interventions in November 2014. 4. There is a S.75 transitional plan to assist in the managing the caseload pressures. See also 1. Staffing. 5. A working group on clinical supervision will report to SGC in January 2015 6. The external board evaluation identified some weaknesses in the board’s leadership on quality. Mitigation: There is a timed action plan that is implementing the evaluation recommendations.
Confidence level in mitigation:
Red/Amber
3.4 What additional actions are required? None in addition to those set out above.
3.5 How do these risks show on the Trust’s Risk Register? Who owns these risks? Datix 1062 (bed management) 4 x 4 = 16 Owner Debbie White. Datix 1145 (risk of not learning from RCAs) 3 x 4 = 12. Jane Sayer. Datix 1163 (well-led) 4 x 4 = 16 Owner Gary Page. Datix 1123 (High demand for community services in West Norfolk) 3 x 4 = 12 Owner Debbie White
Board Assurance Framework December 2014
Board of Directors – Public 18Dec 2014 Board Assurance Framework
Version 0.3
Author: Robert Nesbitt Department: Corporate
Page 6 of 10 Date produced: 08Dec2014 Retention period: 30 years
Datix 1160 (Impact of S.75 changes on caseloads on quality) 3 x 4 = 12 Owner Debbie White
3.6 What is the timeline for the mitigation confidence level to reach ‘green’? This risk area is made up of several inter-connected elements. The CQC and board evaluation action plans provide a substantial part of this detail. Whilst immediate improvements can be made in some areas, it is likely that the rebalancing of the care pathway to substantially reduce OOA placements will take several months, particularly where additional care coordinators are required in Norfolk as this may be contingent on negotiations with commissioners.
Board Assurance Framework December 2014
Board of Directors – Public 18Dec 2014 Board Assurance Framework
Version 0.3
Author: Robert Nesbitt Department: Corporate
Page 7 of 10 Date produced: 08Dec2014 Retention period: 30 years
4. Name of risk theme (board committees with oversight)
Staff morale (OD & WF Committee)
4.1 Relevant Trust objectives:
Delivery of WF & OD strategy
Vacancies recruited to point of offer within 8 weeks by March 2015
Plans to delivery 7 days services by end of financial year.
Roll out of e-rostering by March 2016
4.2 What is the nature of the risk? Low morale impacts on quality of care and staff well-being. It can impact on staff sickness which increases stress for other staff. Low morale can make it more difficult to attract and retain high calibre staff. For operational staff, this cross-references to the service pressures set out in 3 above, and for corporate and support staff, low morale may impact on the support to front line services.
4.3 How is the risk controlled and mitigated? 1. The Trust is rolling out a staff engagement plan, developed in partnership with Staff Side, as part of the OD strategy and with an emphasis on local ownership. 2.Executive team members have set up engagement sessions to hear staff concerns and to answer questions about the rationale for the changes. 3.The staff appraisal system changes will help staff to see where their role contributes to the Trust’s work in supporting service users and will enable better feedback to staff on their performance. 4.The staff FFT includes 3 staff engagement measures which provides a tool to monitor progress. This reports to OD&WFC. 5.A report on staff engagement will be presented at the December 2014 board meeting.
Confidence level in mitigation:
Red
4.4 What additional actions are required? None in addition to those set out above.
4.5 How do these risks show on the Trust’s Risk Register? Who owns these risks? Datix ID 1164 (Staff Morale) 4 x 5 = 20 Owner Leigh Howlett
4.6 What is the timeline for the mitigation confidence level to reach ‘green’? The Friends and Family Test is quarterly. However, the executive team recognise that the challenges in this area are medium to long term issues and so the expectation is that it will take 12 – 18 months for changes now being implemented to feed through into some measurable improvement. Following the trial of a new central lean recruitment process for three months this is now being rolled out and delivery of the recruitment KPIs is anticipated by March 2016. Enhanced management of sickness absence will be introduced over the next quarter and the results should be seen by March 2016. The position on appraisals had not improved and the backlog appeared to be growing. The target for a stable turnover rate of 10% is March 2016.
Board Assurance Framework December 2014
Board of Directors – Public 18Dec 2014 Board Assurance Framework
Version 0.3
Author: Robert Nesbitt Department: Corporate
Page 8 of 10 Date produced: 08Dec2014 Retention period: 30 years
5. Name of risk theme (board committees with oversight)
Maintaining and growing business (Investment Committee)
5.1 Relevant Trust objectives:
By October 2014, delivery of a Commercial Strategy to protect current services and develop new business.
Engage with the wider health economy, third and voluntary sector to ensure the Trust is a known and trusted partner evidenced by a 10% increase in new business with external parties by March 2015, evidenced by financial turnover.
5.2 What is the nature of the risk? Growth increases the ability of the Trust to bear fixed costs / overheads. Loss of income will destabilise the organisation. Loss of key contracts where we are the incumbent could also damage our reputation since they could be interpreted as a loss of commissioner confidence. The development of the Commercial Strategy has been delayed. Developing bids and winning contracts requires an increasingly specialised skill set where demand is variable and where competitors are continually raising the bar. Successful bids require evidence of a track record of delivery which has been variable in recent months. For an organisation of our size it is a challenge to be able to maintain a strong bid capability with the right skills on tap that is also cost-effective during quieter periods. A bid development team need access to specialist service knowledge in the context of clinical managers who are already short of capacity. Formal regulatory action could affect the Trust’s ability to get past PQQ stage for a bid.
5.3 How is the risk controlled and mitigated? 1. Resources to support improved bidding capability have been set aside for 2014/15. In the interim project support and plans are in place for reviewing and securing current / new business.
Confidence level in mitigation:
Red / Amber
5.4 What additional actions are required? The implementation of the corporate restructure so as to provide a stable platform for the Commercial Strategy.
5.5 How do these risks show on the Trust’s Risk Register? Who owns these risks? This is not represented on the risk register given that there is no specific risk at this time related to a bid.
5.6 What is the timeline for the mitigation confidence level to reach ‘green’? The corporate restructure is being designed in September / October and consultation will begin at the end of November 2014. The project plans for reviewing and securing new business as set out in 5.3 have their own timeframes.
Board Assurance Framework December 2014
Board of Directors – Public 18Dec 2014 Board Assurance Framework
Version 0.3
Author: Robert Nesbitt Department: Corporate
Page 9 of 10 Date produced: 08Dec2014 Retention period: 30 years
6. Name of risk theme (board committees with oversight)
Maintaining a CoSRR of 3 in 2014/15 (Finance and Performance Committee)
6.1 Relevant Trust objectives:
Delivery of the 2014/15 financial plan so the Trust achieves a COSRR of 3 as a foundation for 2015/16
Delivery of the 2014/15 CIP and capital programmes
Develop a new strategy for procurement by end of 2014/15 financial year
For the 2014/15 financial year: delivery of all operational targets including receiving 100% CQUIN and the avoidance of any operational and financial penalties from commissioners in the final quarter of the year.
6.2 What is the nature of the risk? Following the Board’s Monitor Declaration in October 2014 that the Trust would be unable to maintain at CoSRR of 3, and the analysis which shows that delivery of CIPS is significantly behind plan, the risk is that our ability to provide a stable financial footing will affect our future ability to provide services. Monitor have announced that they will be carrying out an investigation into this issue. Financial pressures that are due to out of area placements and use of temporary staffing reflect the priority given to patient safety, but are major factors driving the deficit.
6.3 How is the risk controlled and mitigated? 1. Details on the mitigation arrangements are set out in the financial report to the Board. Dedicated resources have been allocated to the financial recovery / CIPs programme including the appointment of Cynthia Conquest (formerly acting Director of Finance).
Confidence level in mitigation:
Red
6.4 What additional actions are required? Reduction in use of temporary staffing including rationalisation of use of locums. Rebalancing of care pathway to reduce use of OOA beds. Generation of new CIPS programmes to fill gaps in current plans. Implementation of the corporate restructure. Maximisation of income through remaining CQUIN targets (notwithstanding that Q1 will not be fully achieved).
6.5 How do these risks show on the Trust’s Risk Register? Who owns these risks? Datix ID 1084 and 1090 CIPS delivery 4x4=16. Andrew Hopkins. Consideration being given to moving this to 4 x 5 = 20
6.6 What is the timeline for the mitigation confidence level to reach ‘green’? The finance report presented at this meeting sets out progress on actions underway to address these issues. The timeline back to a secure CoSRR of 3 is likely to take 18 months.
Board Assurance Framework December 2014
Board of Directors – Public 18Dec 2014 Board Assurance Framework
Version 0.3
Author: Robert Nesbitt Department: Corporate
Page 10 of 10 Date produced: 08Dec2014 Retention period: 30 years
7. Name of risk theme (board committees with oversight)
ICT weaknesses (Investment Committee)
7.1 Relevant Trust objectives:
Delivery of an ICT strategy which supports engagement with service users and carers in a convenient and timely way and makes best use of clinicians time (e.g. reduce travel) by October 2014
7.2 What is the nature of the risk? The risk is that patient safety and business continuity is compromised by weaknesses in ICT infrastructure.
7.3 How is the risk controlled and mitigated? 1. Following a report to the Investment Committee on 5th June 2014 investment has taken place in data backup and ICT infrastructure.
Confidence level in mitigation:
Amber
7.4 What additional actions are required? There will be an independent audit of ICT capability be the end of the calendar year to confirm that risks have been mitigated, but see below (7.6) for Disaster Recovery updated timetable.
7.5 How do these risks show on the Trust’s Risk Register? Who owns these risks? Datix ID 1101 (data back-up) 5 x 3 = 15. Datix ID 1100 (Disaster Recovery) 5 x 3 = 15 (increased from 12), Datix ID 1095 (ICT infrastructure) 4 x 3 = 12. Leigh Howlett.
7.6 What is the timeline for the mitigation confidence level to reach ‘green’? The Data backup capability <checking with Nick Rackham> ICT infrastructure work is due for completion at year end. The Disaster Recovery Capability work has had to be retendered which will delay resolution until mid-2015.
Board of Directors – Private / Public Date Implementation of NICE guidance ‘Smoking cessation in secondary care’
Version 1.0
Author: Sara Fletcher Department: Service Governance
Page 1 of 8 Date produced: 1st Dec 2014 Retention period: 30 years
Report To: Board of Directors – Public
Meeting Date: 18th December 2014
Title of Report: Implementation of NICE guidance ‘Smoking cessation in secondary care’
Action Sought: For Debate
Estimated time: 10 minutes
Author: Sara Fletcher: DIPC, Physical Health Team Leader
Director: Jane Sayer: Director of Nursing, Quality and Patient Safety / Bohdan Solomka, Medical Director
Executive Summary:
There is a requirement for NSFT to consider the recommendations within the NICE guidance for smoking cessation. There is a note on responsibility within the guidance which states: ‘This guidance represents the views of the Institute and was arrived at after careful consideration of the evidence available. Those working in the NHS, local authorities, the wider public, voluntary and community sectors and the private sector should take it into account when carrying out their professional, managerial or voluntary duties. Implementation of this guidance is the responsibility of local commissioners and/or providers. Commissioners and providers are reminded that it is their responsibility to implement the guidance, in their local context, in light of their duties to have due regard to the need to eliminate unlawful discrimination, advance equality of opportunity, and foster good relations. Nothing in this guidance should be interpreted in a way which would be inconsistent with compliance with those duties.’ It is recognised that there is an irrefutable case to support progress towards smoke-free services to improve morbidity and mortality amongst service users. It is apparent that there are significant concerns amongst staff, service users and staffside organisations around the implementation of a total smoking ban across all staff sites. The Board should consider the information in this report and in the background papers in the context of NSFT services and decide on the best option as presented in the recommendations. The aim is to provide a clear outline of the Trust strategy with ongoing Board support to achieve this.
1.0 NICE guidance ‘Smoking cessation in secondary care’ (November 2013)
1.1 This paper considers the recommendations in the NICE public health guidance ‘Smoking cessation in secondary care: acute, maternity and mental health services’ November 2013 and the implications for implementation of these within NSFT services. This guidance
Date: 18 December 2014
K Item: 14.171 viii.
Board of Directors – Private / Public Date Implementation of NICE guidance ‘Smoking cessation in secondary care’
Version 1.0
Author: Sara Fletcher Department: Service Governance
Page 2 of 8 Date produced: 1st Dec 2014 Retention period: 30 years
requires that all premises are smokefree and all staff, patients / service users must abstain from smoking whilst admitted to, or using secondary care services.
1.2 NSFT commissioners have requested that the Trust develop a plan to achieve compliance with this guidance. This is recommendation 16 of the guidance – to commission smokefree secondary care services and to monitor and audit the implementation and impact of the recommendations in the guidance (as outlined in the table 1 below).
1.3 The guidance aims to support smoking cessation, temporary abstinence from smoking and smokefree (the air is free of tobacco smoke) policies in all secondary care settings. It covers drug and alcohol services in secondary care, emergency care, in-patient, residential and long-term care for severe mental illness in hospitals, psychiatric and specialist units and secure hospitals. It includes grounds, vehicles and other settings involved in the delivery of secondary care services.
It recommends:
Strong leadership and management
The availability of an on-site stop smoking service
The availability of pharmacotherapy and intensive behavioural support
Pathways between secondary care, primary care and community services
Appropriately trained staff
Supporting staff to stop or abstain from smoking while at work
No designated smoking areas on trust premises, no staff facilitated smoking breaks
2.0 Key facts:
2.1 Tobacco smoking remains the single greatest cause of preventable illness and premature death in England – most of the reduction in life expectancy among people with serious mental illness is attributable to smoking.
2.2 33% of people with mental health problems and 70% of people in psychiatric units smoke tobacco – recent studies show that these people are just as likely to want to stop smoking as the general population.
2.3 A total ban on smoking complements the duty of care on healthcare staff and the organisation to protect health and promote healthy behaviour.
2.4 The supported environment of an inpatient setting is an ideal opportunity to commence a smoking cessation programme.
2.5 Whilst many NHS secondary care settings have smokefree policies that apply to grounds as well as enclosed areas, there have been problems with compliance and enforcement.
3.0 Background for NSFT
3.1 In March 2010 following a nine month project which included staff training, service user consultation, risk assessment and changes to security arrangements, the
Board of Directors – Private / Public Date Implementation of NICE guidance ‘Smoking cessation in secondary care’
Version 1.0
Author: Sara Fletcher Department: Service Governance
Page 3 of 8 Date produced: 1st Dec 2014 Retention period: 30 years
Norvic clinic and Meadowlands applied a smokefree policy (no smoking anywhere on site or while on escorted leave). In September 2011, the low secure wards at Hellesdon were included.
3.2 There was an escalation of smoking related security breaches and there were legal challenges.
3.3 In March 2012, following assessment of the situation by a working group, smoking was safely reintroduced.
3.4 Recommendations were presented to the Service Governance sub-committee (SGSC) in June 2012:
Remove the current overarching policy
Dedicated smoking areas for service users with info ‘what you can expect when you come into hospital’ to explain the arrangements.
Care pathways for service users that smoke incorporated into wider wellbeing/health promotion strategies.
Support for staff who would wish to give up smoking incorporated into wider HR wellbeing/health promotion strategies (lead by HR).
Consideration given to where staff could smoke to minimise the negative effect that seeing healthcare professionals smoking has on the health promotion work.
Consideration given to how to protect staff from exposure to exhaled smoke.
4.0 Lessons from the past decade of implementation research (Public Health paper 2013):
4.1 There is a longstanding complex relationship between smoking and mental health.
4.2 Achieving smokefree status is a process not an event; success is more likely in striving towards a smokefree goal.
4.3 There is strongly held staff belief that failure to supply patients with tobacco will lead to increased patient aggression, that patients are not interested in quitting and that they are unable to quit. Some staff believe that delivery of care in a smokefree setting will damage the therapeutic relationship with patients.
4.4 Partial smokefree policies have a limited impact on the staff and patient culture of smoking.
4.5 Smoking cessation support during the transition between inpatient and community services is vital.
4.6 There is a need for good levels of appropriately trained staff to provide a range of patient activities and therapeutic interventions.
Board of Directors – Private / Public Date Implementation of NICE guidance ‘Smoking cessation in secondary care’
Version 1.0
Author: Sara Fletcher Department: Service Governance
Page 4 of 8 Date produced: 1st Dec 2014 Retention period: 30 years
5.0 Conclusion
5.1 There is a significant body of evidence demonstrating that a smokefree policy has many positive benefits for the units, staff and patients concerned and that implementation is less burdensome than staff fear.
5.2 The key factors for successful implementation are:
adequate consultation with staff and patients
staff training
clear leadership and management support
adequate resourcing of policy implementation
close follow-up of patients after discharge
consistent implementation practices
dedicated staff resources to provide ongoing mentorship and support to staff
audits of smoking cessation processes that include clearly defined and evidence-based performance indicators
incorporation of nicotine withdrawal management into clinical care
management of ‘high risk’ smokers by smoking cessation specialists
6.0 Financial implications (including workforce effects)
6.1 There will be additional cost to the Trust related to prescribing nicotine replacement therapies.
6.2 There is potential for this to be offset against the reduced cost for some anti-psychotics as lower doses are needed in non-smokers.
7.0 Quality implications
7.1 Clinical staff have a duty of care to protect patients: this is compromised when supporting a known harmful activity such as smoking.
7.2 Larger doses of drugs with known side effects are required in patients who smoke.
7.3 Evidence shows that morbidity and mortality rates are reduced for those who stop smoking.
7.4 Many external areas within in-patient units are monopolised by smokers which may restrict the desire to access outside areas for non-smokers.
8.0 Equality implications
8.1 People with a mental health diagnosis represent a significant proportion of the smoking population. There does not appear to be parity amongst clinical staff on the expectation of these people’s ability to give up compared with the rest of the population.
Board of Directors – Private / Public Date Implementation of NICE guidance ‘Smoking cessation in secondary care’
Version 1.0
Author: Sara Fletcher Department: Service Governance
Page 5 of 8 Date produced: 1st Dec 2014 Retention period: 30 years
9.0 Risks / mitigation in relation to the Trust objectives (implications for Board Assurance Framework)
9.1 The Trust has identified an objective to deliver safe, caring services: compliance with the NICE guidance supports this by improving the longer-term health and wellbeing of mental health service users.
9.2 There is a risk that a poorly supported and poorly resourced strategy will fail.
10.0 Recommendations
10.1 The Board consider the parameters and timescale of an NSFT smoking cessation strategy. Potential options:
a. Full compliance with the NICE guidance: a total smoking ban across all services from admission to discharge with all supporting services available as table 1 within an agreed timeframe.
b. Focus on harm reduction and strengthen the availability of all supporting services as table 1 below with a view to improving the number of patients supported to stop smoking.
c. Use a pilot site to test the feasibility of a total smoking ban prior to implementation of an agreed strategy.
10.2 A working group with wide representation is supported to develop and implement this strategy, once agreed.
Name: Sara Fletcher Title of Author: DIPC, Physical Health Team Leader Date of Paper: 1st December 2014
Background Papers / Information References: NICE public health guidance 48 ‘Smoking cessation in secondary care: acute, maternity and mental health services: November 2013 http://guidance.nice.org.uk/PH48 Achieving Smoke-free mental health Services: Lessons from the past decade of implementation research: International Journal of Environmental Research and Public Health 2013, 10, 4224-4244 Smoking and mental health – Mental Health Network NHS Confederation Briefing document: September 2013 http://www.nhsconfed.org/~/media/Confederation/Files/Publications/Documents/smoking_mentalhealth0913.pdf
Board of Directors – Private / Public Date Implementation of NICE guidance ‘Smoking cessation in secondary care’
Version 1.0
Author: Sara Fletcher Department: Service Governance
Page 6 of 8 Date produced: 1st Dec 2014 Retention period: 30 years
Table 1 - NICE smoking cessation guidance (48) recommendations relevant to Mental Health Trust
Recommendation Current position Comments Proposal to improve current position in relation to harm reduction
1 Provide information (verbal and written) about the smokefree policy prior to appointment or admission
Signs and information on current smoking arrangements available although availability varies across areas.
Would require audit to confirm availability in relation to current policy
Trustwide audit
2 Identify people who smoke and offer help to stop
Part of the physical health assessment on the MDT admission documentation, both community and inpatient. Last audit for compliance in inpatient areas was 2010. Technical Instructors and physical health nurses offer advice and support as part of wellbeing and healthy lifestyle sessions
More staff require brief intervention training to capitalise on this opportunity and progress patient to available options
Make smoking cessation / brief intervention training mandatory – include at induction.
3 Provide intensive behavioural support
Any level 2 smoking cessation trained staff member can offer this support and there is supporting documentation which links with pharmacy. Secure services have good resources.
Feedback from the Trust physical health nurses show minimal referral rate to them from other areas. Low numbers of level 2 trained advisors although there is good access to training courses in both Norfolk and Suffolk.
Requirement for a number of staff to be trained in each area
5 Provide information and advice for carers, family etc. and for visitors
British Heart foundation booklets supplied by physical health team – mainly available in secure
More Trust specific information to be developed
Board of Directors – Private / Public Date Implementation of NICE guidance ‘Smoking cessation in secondary care’
Version 1.0
Author: Sara Fletcher Department: Service Governance
Page 7 of 8 Date produced: 1st Dec 2014 Retention period: 30 years
services.
6 Advise on and provide stop smoking pharmacotherapies
A range of nicotine replacement (NRT) therapies are available as risk assessed by pharmacy. The drug recommended by the Cochrane review as most effective, Varenicline, is only available on a named patient basis.
Varenicline has cautions related to mental health usage but research has not demonstrated this.
Review pharmacotherapy available considering research and clinical effectiveness evidence
7 Adjust drug dosages for people who have stopped smoking
Supported by medical staff and directed by documentation once a decision to stop has been made.
Collect data on outcomes Improve liaison with primary care and community services when discharging patients
9 Put referral systems in place for people who smoke
Systems available to refer to smoking cessation advisor
Not aware of data to quantify uptake or of wider referral to specialist or into the community
Clarify referral pathways for clinicians
10 Provide leadership on stop smoking support
Medical Director is nominated lead within the NSFT policy with clear responsibilities identified for other staff
There are many individuals within the Trust who provide strong leadership in their locality of influence
Identify robust structure though a working group
11 Develop smokefree policies Smoking policy has been updated to include information on e-cigarettes – it remains under review until Trust direction on the NICE guidance has been established
Key priority of a working group
12 Communicate the smokefree policy
Level of application of the current policy has not been established
Key priority of a working group
13 Support staff to stop Identified as an action for HR in Review data to quantify uptake Key priority of a working group
Board of Directors – Private / Public Date Implementation of NICE guidance ‘Smoking cessation in secondary care’
Version 1.0
Author: Sara Fletcher Department: Service Governance
Page 8 of 8 Date produced: 1st Dec 2014 Retention period: 30 years
smoking the SGSC paper (June 2012) – part of employee health and wellbeing strategy
14 Provide stop smoking training for frontline staff
Training is advertised via WFD, e-learning training is available through the national centre for smoking cessation and training (NCSCT)
Review data to quantify uptake Key priority of a working group
15 Ensure local tobacco control strategies include secondary care
Require links to Health and Wellbeing Boards to influence
Board of Directors Improving Staff Morale
Version 3.1 Carol Carter
Author: Michael Scott Department: Corporate
Page 1 of 6 Date produced: 9 Dec 2014 Retention period: 30 years
Report To: Board of Directors – Public
Meeting Date: 18 December 2014
Title of Report: Improving Staff Morale
Action Sought: For Information
Estimated time: 15 minutes
Author: Michael Scott, Chief Executive
Director: Michael Scott, Chief Executive
Executive Summary: This report provides information on the issue of improving staff morale. It outlines the current situation and proposes a 15 point action plan for improvement. Further work is underway to convert this to a time limited implementation plan.
1.0 Introduction
1.1 One of the top priorities for our Trust is the improvement in our staff morale. This is often termed Staff Engagement or Staff Motivation but this report will treat it as a problem of morale. Many actions are already underway and this report adds to these but most importantly brings them together into a coherent framework and action plan.
2.0 The nature of the problem:
2.1 All current guidance makes the connection between staff attitude and patient care. It has become axiomatic that ‘happy staff’ results in’ happy patients’. This forms the corner stone of the Healthy Board, the work of the CQC in its well led domain and it is all founded on the notion of collaborative leadership and the work of Professor Michael West. In short the evidence is that engaged staff produce better patient outcomes and safer trusts. It is not however necessarily so that the converse is true; whilst many metrics of staff engagement are low in our trust we clearly get good feedback on the quality and the safety of our care in many respects. However, there is a continuing commentary on the lack of staff engagement, motivation and morale from external bodies. These can be summarised as follows:
Our staff survey is the second worst of all mental health trusts
Date: 18 December 2014
L Item: 14.172 i
Board of Directors Improving Staff Morale
Version 3.1 Carol Carter
Author: Michael Scott Department: Corporate
Page 2 of 6 Date produced: 9 Dec 2014 Retention period: 30 years
The CQC are likely to be critical of staff morale and its consequent linkage to quality of care.
The Foresight Partnership have commented on a lack on connectivity between the Board and frontline staff.
The family and friends test for staff continues to produce poor results despite its coverage going from 5% to 19% of all staff.
2.2 This problem has been conceived of and addressed in a number of different ways. It has been regarded as a communications problem and we have worked hard to enhance the way we communicate. It has been thought of as a Human Resources problem either within the department or within the HR skills of our managers. It is variously described as a problem of engagement motivation or morale. However, at its heart this paper argues it is a problem of culture and leadership. That is not to deny the contribution of communications and HR but to say that it runs more deeply in the organisation. Cultures are notoriously hard to change and there is no single measure which will address this. This paper therefore proposes a 15 point action plan to ultimately change the culture of the Trust. This must not be seen as “yet another action plan” as we have many of those. Rather it is time to gather actions that are largely in place into an overall and coherent framework. This report describes that together with a case study of good practice.
3.0 15 point action plan
3.1 The following actions are designed in concert to change the culture of the trust. No single one will suffice but it is planned that together they will change ‘the way we do things around here’. There is no priority order implied below; the actions range from fundamental changes of emphasis to relatively small but important issues such as staff recognition and long service awards. However it is believed when played out together they will create a powerful force.
1 Early in the New Year we will be launching a refresh of our values and behaviours framework. External support is currently being sought for this exercise but this external help will simply be in the form of facilitation. Success depends on local managers engaging with all staff to create a bottom up view of how the trust should act and behave. The very act of doing this should create more engagement, however, it will then be the living of these values through a behaviour framework in terms of our day to day behaviour but also in terms of how we recruit, motivate and reward.
Board of Directors Improving Staff Morale
Version 3.1 Carol Carter
Author: Michael Scott Department: Corporate
Page 3 of 6 Date produced: 9 Dec 2014 Retention period: 30 years
2 Following on from this we need a regular programme of Director contact and visits and both at Executive Director and Non-Executive Director level. The non-executives have a locality link system which the executives need to mirror. Plans are being laid to produce a schedule for the year that we are prepared to adhere to. The emphasis will be on going to regular locality based meetings rather than special events which experience shows tend to be poorly attended because of reluctance or work pressures. These visits should always be written up in a ‘you said we did format’ and publicised to demonstrate that not only are we listening and in touch but we are responding and dealing with concerns. In order for this not to by-pass local management we need a clear protocol between Directors and those charged with managing the service locally.
3 External commentators have remarked upon staff’s apparent reluctance or inability to speak up on issues with a consequence that is perceived that the board is not listening or responsive. Several issues are already in train to address this, the first is to clarify the role of all leaders and managers at a local level. Work is reported elsewhere in this meeting which has started that process. We should always seek to use line management as the first route for the expression of concerns, reinforcing this will empower local leaders and enable them to respond to such concerns. We have backed this up already by signing up to the ‘Speak out Safely’ (SOS) campaign; this assures staff that they can indeed speak out safely, however we need to reemphasis this campaign.
4 To augment all of the above there will be a new campaign to “eMail Michael”. This will firstly emphasise staff’s responsibility to work locally with their managers and clinical leaders but will also give the opportunity to openly email myself. It is difficult to estimate the volume this may generate but it may entail short term extra resource to focus on responses. The main value of this will be its very existence and the opportunity to get directly in touch with me, even if its usage is low.
5 The senior management forum is gaining some currency in its role to support all of these initiatives. Already there is a degree of honesty and sharing around our issues and priorities. The first quarterly meeting takes place in December and will have over 100 of our leaders and managers together to discuss our way forward. This is starting to build a leadership and management community and one of the goals for the HR department this year is to create a modular leadership and management development programme to address their needs. This community will also be the foundation of a cascade team briefing system. This is here in embryo in our Trust right now but needs further work and focus to be effective. This will be a key objective for our new Communications Manager.
Board of Directors Improving Staff Morale
Version 3.1 Carol Carter
Author: Michael Scott Department: Corporate
Page 4 of 6 Date produced: 9 Dec 2014 Retention period: 30 years
6 The voice of the board and the Chief Executive is insufficiently strong in communications at the moment; this will change in two ways. Firstly, within days of each board meeting there will be “Gary’s message” this will give a resume of what the board discussed in its most recent meeting. In our Trust update regular newsletter there will also be a regular bulletin from me.
7 We will be drawing from other organisations. As a consequence of Monitors intervention we will be required to “buddy’ with another organisation we have already established a relationship with Birmingham and Solihull mental health trust and reciprocal visits are planned for early in the New Year. I have also made links with Suffolk County Council and their organisational development team who have turned around the culture in their county. We also hope to develop stronger links with Oxleas in South London as described below.
8 I will continue to prioritise my input at the new staff induction. Feedback is generally good on this and is important that new staff get a clear message from me at the beginning. This can impact over 400 new staff every year. A further buddying opportunity exists with Oxleas Trust. Appended to this report is a case study on their approach to staff engagement. This emphasises the role of the Chief Executive and particularly the induction. I am proposing to take his idea and issue postcards at the end of the induction to staff members to post back one month into the job to give feedback on what they’ve found.
9 The same case study emphasis the role of trade unions. We generally have a good relationship here but this has been enhanced by my chairing of the trust partnership meeting. Unions are particularly keen to see an engaging style of change management. To this end we have agreed our approach to Annex X of the Agenda for Change handbook. In essence this means that where we seek to conduct organisational change we will do it and in an engaging and transparent manner. This has been written into our management of change policy and documentation. Further examples of trade union involvement include a letter on staff wellbeing signed off by chair of staff side and myself; chair of staff side being involved in the procurement of support for our values work and many other initiatives
10 The above philosophy has to be put into practice in all of the change and development we are leading. A good example is the proposed changes to Access and Assessment services. We already have very positive feedback on the event to design the new service and there is evidence that it is starting to bring people on board. Typical of the reactions we are getting to these new approaches are indicate by the direct quotes we are getting from staff below:
Board of Directors Improving Staff Morale
Version 3.1 Carol Carter
Author: Michael Scott Department: Corporate
Page 5 of 6 Date produced: 9 Dec 2014 Retention period: 30 years
‘I just wanted to say thank you for your letter. Your transparency and clear honest direction, have given me hope and inspiration for the future of NSFT. Something I haven’t felt for quite a while!’
‘Thank you for the letter and the information – I am somewhat heartened as a result that views and concerns regarding the strategy are being dealt with in a positive and open manner – thank you’
‘I am feeling quite positive’
11 A number of commentators have pointed out that we do not have dedicated change capacity within our organisation. This is being addressed as a part of our corporate restructure within the Directorate of Strategy and resources – our ‘transformation directorate’. Specifically we will also include skills around LEAN and redesign with an explicit philosophy that the people who best know how to improve the process is the front line staff that run it.
12 Our staff health and welfare initiative promotes staff taking a break and looking after their health. We need to make this an integral part of the way we work in every team and site.
13 We have reviewed our long services awards. It is clear that these are not being delivered as well as they might. We have a new proposal which initiates contact with those who have a range of long service contributions and will be arranging for them to be presented with their certificates and vouchers regularly at board meeting lunch time.
In addition we are going to launch regular staff recognition awards to be brought together at year end in an annual awards ceremony
14 At the heart of this all is the recognition that the board needs to demonstrate that it is concerned about the care of our services users and supports staff. Sadly the perceptions of staff have not always been of this image. The culmination of all of these actions is that the board regularly demonstrates its commitment to care and quality. One way into this would be through the values work but we should also re-examine our vision to ensure that it is clinically and quality focused.
15 The basis of all of this will be an organisational philosophy of the inverted organisation. This is described below.
Board of Directors Improving Staff Morale
Version 3.1 Carol Carter
Author: Michael Scott Department: Corporate
Page 6 of 6 Date produced: 9 Dec 2014 Retention period: 30 years
Service users
Our only purpose is to serve our service users and therefore they are at the top of our organisational tree. The people who do that are frontline staff and all the rest of the organisation is conceived as supporting them. This should underpin our entire organisational philosophy and all of our work. Of particular importance here are corporate support departments. They must strike a right balance between enforcing standards and supporting front line staff. It is proposed to achieve this through Service level agreements for each corporate department
4.0 Conclusion and Monitoring:
4.1 Whilst many of the above are tangible actions the results may often be intangible changes in culture. These are sometime difficult to measure beyond anecdote and feel. However, we will use the annual survey and quarterly family and friends as a measure of progress against our objectives.
5.0 Recommendation:
5.1 The Board is asked to note the content of this report
Michael Scott Chief Executive
Frontline Staff
Back Office & Team Leaders
Senior Management
Trust Board & Governors
Chief Executive & Directors
1
IPA Case Study
Employee Engagement at Oxleas NHS Foundation Trust
Oxleas NHS Foundation Trust provides a range of health and social care services to people in south east
London, specialising in community health, mental health and learning disability services. Their
workforce comprises of around 3,500 people, based out of 125 sites across Bromley, Bexley, Greenwich
and Kent.
Senior leaders at the trust have a real focus on employee engagement. Stephen Firn, Chief Executive at
Oxleas explained ‘the longer I’m in the job, the more I understand how important staff engagement is.
It just gets reinforced to you.’ Although most of the research linking engagement to outcomes in the
NHS has focused on acute trusts, they see a clear link between how staff are treated and how they
perform in mental health and learning disability services too.
Employee engagement at the trust has increased significantly in the last decade. Simon Hart, Director
of HR & OD at Oxleas explained that poor performance in the staff survey in 2005 acted as a ‘wake up
call’ for the trust to improve how they engaged with staff. Their efforts have made a significant impact
and Oxleas now has the highest levels of employee engagement among the 57 mental health and
learning disability trusts in the country. Analysis by the Kings Fund has shown that Oxleas has had the
highest level of staff engagement of any NHS organisation over the last four years.
Senior Leadership
The senior leadership team at Oxleas play a significant role in driving employee engagement. Although
engagement is seen as a shared responsibility across all levels, Stephen Firn believes that ‘the
responsibility for setting, maintaining and modelling the cultures sits with the senior leaders.’ Simon Hart
explained how it was important for senior leaders to act as role-models and be seen to live the trust’s
values; ‘you can have as many fancy pictures of your values stuck up on a wall as you want, but unless
it’s lived and believed, it’s meaningless.’
The relative stability at the top of the organisation is seen as an advantage in terms of engaging with
staff. Stephen has been at the trust for 18 years, 12 of those as Chief Executive. The Chairman and
Director of HR & OD and other directors have also been in post of a significant period. This has allowed
them to build up recognition and trust with the workforce.
In order to build the relationship with staff from the very start, Stephen Firn is the first person new
recruits see at their induction. He welcomes staff to the organisation, talks about the trusts values and
his journey from Healthcare Assistant to Chief Executive. Stephen asks that after their first few weeks,
staff tell him what they think about the trust and how things are going. He sees this as important in
getting a fresh perspective on the organisation and making the newcomers feel valued right from the
start.
The board at Oxleas undertake regular visits to services. These were introduced in the wake of the
Francis Report, with its description of a board at Mid Staffs that was distant and out of touch with what
was going on the shop floor. Stephen Firn explained that although the board had regular updates on
2
care quality, finances and HR, ‘you can still read all of those bits of information and not know that in
parts of the organisation, staff might be unhappy.’
Every member of the board – both Directors and NEDs – now undertakes a visit to a service between
each meeting. The emphasis of the visits is on supporting staff rather than fault-finding. The board
members’ aim is to find out what’s going on in the service and how staff are feeling, as well as identifying
and resolving problems. They then feed back to the board to share the knowledge.
As well as being seen as an important tool by board members, employees seemed really to value these
visits. They described how the visits help staff get to know the senior leaders, making them seem more
approachable and breaking down barriers. Employees said it helped them feel they could raise issues
with senior leaders, whatever their role and that it ‘makes people feel that Pinewood [the head office]
is not made up of faceless bureaucrats.’
Employees also explained that the visits help the senior team get to know staff and build their
knowledge about the services they provide. One described how it builds the perception that ‘these
people who are going to be making decisions about staffing and money and all these over-arching
important things, actually understand what it’s like to deal with Mr Bloggs on a rehab ward.’ The visits
are seen as a commitment to the frontline; as one employee saw it, ‘it’s such a small thing to do but it’s
really important.’
The approach of the leadership team is clearly effective. In addition to the positive feedback from the
interviews, the trust far out-performs the average in terms of senior leadership. Compared to the
average for mental health and learning disability trusts, staff at Oxleas are far more likely to recognise
senior managers; they are more positive about communication and involvement in decision-making
making; and they are more likely to say that senior managers are committed to patient care.
Engaging Managers
In addition to the senior leadership, Oxleas seems to perform very well in terms of line management.
The trust comes in the top 20% for mental health and learning disability trusts on support from
immediate managers and scores far higher than the average in terms of having a well-structured
appraisal; something that has been shown to be closely correlated with employee engagement.
The trust has taken action in the last few years to improve the support for managers. This includes a
specific induction for managers and clinical leaders; a development programme; and will in future
include a performance management framework which brings in both hard data and soft data such as
feedback from staff, patients and colleagues. Managers were positive about the support on offer to
them. As one explained, ‘if you don’t get supported as a manager, you can’t support your staff, and your
staff can’t support the patients; it just flows like that. With Oxleas, I find that I get supported.’ Frontline
staff also tended to be very positive about their immediate supervisors, saying that they were
supportive and that supervisions and Personal Development Reviews were carried out effectively.
There was also a strong sense of team working at the trust. This was reflected in the staff survey where
the trust comes in the top 20% nationally. Again, this is something shown in national research to be
closely correlated with high levels of staff engagement.
3
Partnership Working
There is a strong commitment to partnership working with the trade unions at Oxleas. It is seen as
important both to employee engagement and to delivering quality care. Partnership is also underpinned
by a belief that both sides have a shared interest; as Simon Hart explained ‘we’re all part of the same
organisation, we all want Oxleas to be a really good organisation, to offer great care, and to be a good
place to work.’
There is an innovative and effective approach to partnership working at Oxleas. Wendy Lyon, the Chair
of Staff Side is also employed by the trust as Head of Partnership. In the role she acts as an advocate for
all staff, irrespective of union membership, ensuring that their views are heard and considered. Wendy
reports directly to the Chief Executive and has regular access to all Directors.
Wendy and her colleague Yvonne Hayes, who is also a UNITE steward, also run a series of focus groups
in each directorate which give employees the chance to share their views and raise any concerns they
might have anonymously. Simon Hart described how these give the Board ‘an unvarnished,
unadulterated view of what staff are saying. The staff survey is great but it’s just numbers. This is what
staff are really saying and thinking.’ The findings of the focus groups are fed back to Directors who are
expected to act on the issues identified, and report back on progress both to Wendy and their teams.
Wendy in her role as Chair of Staff Side sits on the Executive Director Remuneration Committee, along
with an elected trust governor, increasing the accountability and transparency of the system.
In addition to these structures, partnership working is also supported by the culture at the trust. Both
sides emphasise the importance of communicating regularly and in an open and, honest way. There is
a focus on early engagement with Wendy and Staff Side colleagues being involved in organisational
change before it even starts. The approach is set out in the Partnership Agreement with managers
expected to act in an inclusive way, engaging with the unions and their employees as a whole. The
relationship is based on collaboration with, for example, all HR policies being written together by Staff
Side, HR and management. Although the relationship is positive, as Simon Hart explained ‘it’s not a cosy
relationship by any stretch of the imagination’, as Wendy and her colleagues play an important role in
challenging the senior leadership and she retains her independence and accountability in her role as
Chair of Staff Side.
A further strand to partnership working at Oxleas is the developing relationships between the trust and
the various staff networks. Oxleas has staff networks for BME, LGBT, Disability and Lived Experience of
Mental Health. These provide a further opportunity for consultation and sharing of information as well
as proactively supporting the organisation as a whole. The LGBT network has played a key role in
supporting Oxleas achieving a top 100 place in the Stonewall index of top employers whilst the Disability
and Lived Experience Networks are directly involved in the selection of a new Occupational Health
provider.
The trust leadership really sees value in investing in a partnership relationship. Stephen Firn explained
that in addition to the staff survey, having the relationship with Wendy helps the board really see how
staff are feeling – ‘I don’t see how I could do my job without having that link there.’ The leadership
believe the relationship helps them both make the right decisions, identify and address issues early, and
support engagement. Wendy and her colleagues value the openness of the relationship and the
opportunity to be involved in a meaningful way in decision-making at the trust.
4
Involvement and Innovation
There is a strong sense of employee voice at Oxleas. There have been many changes in the trust over
the past few years and this looks set to continue as the financial challenge grows. There is a strong focus
on involving staff in this process as much as possible, both through Staff Side and directly. This is based
both on a recognition that staff are well-placed to contribute to decision-making, and that change is
easier when staff are involved and given a say. As one service manager explained, the approach is to sit
down with staff, to explain the situation to them and to involve them in planning for the future. This
contrasts with the approach 10 years ago when ‘those decisions would be made and then you’d just tell
the staff the good or bad news.’ Wendy Lyon emphasised the importance of early engagement; ‘the
earlier they talk to staff the better. If they talk to us, we may well have solutions to the problems. We’re
the ones doing the work.’
In addition to service change, staff are also encouraged to contribute towards innovation at Oxleas. One
employee in the Adult Learning Disability team explained how there is a bottom-up approach to
innovation, with managers ‘encouraging the grass-roots to come up with suggestions for how we can
do things better.’ Suggestions are investigated and are often adopted, helping employees feel valued
and encouraging them to offer more suggestions. As another employee from the Recovery and Assertive
Outreach Team explained, ‘you’re always thinking; what else can I come up with, what ideas can I come
up with. That really motivates people – wanting to do more.’
Again, the impact of this is clear in the staff survey. Oxleas scores higher than trust type average in
terms of how both managers and senior leaders involve staff in decision-making. Oxleas also scores
highest in the country for mental health and learning difficulties trust in terms of the extent to which
staff feel able to contribute to improvements at work.
Progression and Development
Speaking to employees at Oxleas, there is a strong sense that there are opportunities for progression.
This is important given the wealth of evidence that links perceptions of opportunities for development
and advancement to employee engagement.
The Chief Executive himself started as a Healthcare Assistant and there is a focus on providing
opportunities for staff to develop their careers and advance. One Service Manager explained that she
had progressed from a junior role to her current position; ‘people want to learn and move up the ladder
and there is that opportunity for people to advance.’ Another explained that she had staff who had gone
all the way from basic skills training to studying Masters Degrees ‘there’s a real sense that you have a
career structure here.’
The Future
There is a recognition across the trust that there will continue to be significant changes over the next
few years, and that this will pose a challenge to employees. Senior leaders at the trust understand this
could potentially impact on levels of engagement but they are focused on ensuring this does not
happen. As Simon Hart explained; ‘if staff understand what the situation facing the organisation is, they
can see that management are doing absolutely everything in their power to do the right thing, there’s a
5
transparency of approach that will support a genuine belief that they’re being asked to participate in
finding solutions; that is the only way we will be able to keep the same level of staff engagement as we
have now.’
Key Lessons:
Senior leaders play an important role in employee engagement through setting the tone and
modelling the culture. They must to stay in touch with frontline employees;
Line managers also play a big role in engaging their teams and need to be supported to do so.
A strong partnership relationship with the trade unions – based on trust and meaningful
involvement – can help lay the foundations for good employee engagement.
Employees have immense and often under-utilised potential for innovation. Engaging
effectively can help unlock this innovation in order to improve services.
Giving employees opportunities for training and progression builds a sense of loyalty and
engagement.
This case study was conducted by Joe Dromey, Head of Policy and Research at the IPA in February
2014. We’d like to thank all of the staff who took the time out to speak to us. It formed part of a wider
project looking at employee engagement in the NHS. You can see the full report here.
Board of Directors – Public Date December 18 2014 TSS Lessons Learnt
Version 1.0
Author: Leigh Howlett Department: Commercial
Page 1 of 4 Date produced: Retention period: 30 years
Report To: Board of Directors – Public
Meeting Date: December 18 2014
Title of Report: Trust Service Strategy Lesson Learnt
Action Sought: For Debate
Estimated time: 15 minutes
Author: Leigh Howlett, Commercial Director
Director: Leigh Howlett, Commercial Director
Executive Summary:
The Trust Service Strategy (TSS) has closed as a programme of work.
This report is an overview of the key lessons learnt themes from TSS overall, which are:
Leadership
Planning & Data
Workforce
Communication & Engagement
Finance, Estates and ICT Support
The Trust Board acknowledges mistakes were made in the TSS programme overall, recognises the impact on some staff this has had and has been open in its apology. However, it is equally important to note that some of the changes have been positive and successful new services have been created. The hard work and commitment of our staff which has gone into the multiple TSS work streams is a credit to them, the Trust and local mental health services.
The Board intends to learn from this and ensure future change programmes, which are essential to the future of the Trust, mental health services and the NHS, are implemented in a more proactive, transparent and consistent manner.
The approach change from this point forwards will include:
The establishment of a Programme Management Office (PMO) function led by a single Executive Director
External expertise is only obtained when that particular skill set is not available with the Trust, with transfer of these skills to existing staff being an explicit requirement
Training for all staff on Project Lite and Lean
The HR processes to support change is overhauled
Communication of, and engagement in, any change should begin before decisions or choices are made. For staff this will include full support of Annexe X.
Date: 18 December 2014
M Item: 14.172 ii
Board of Directors – Public Date December 18 2014 TSS Lessons Learnt
Version 1.0
Author: Leigh Howlett Department: Commercial
Page 2 of 4 Date produced: Retention period: 30 years
1.0 Report contents
1.1 The Trust Service Strategy (TSS) was a four year change programme (2012 – 2016) which aimed to reduce costs by 20% (circa £40m) over the life of the strategy, as well as redesign services to meet the changing, and future, needs for mental health services. At the time it was a forward thinking proposal given the financial crisis the Trust could foresee coming and indeed has been realised and now affects the NHS as a whole.
1.2 However, the Board has agreed the TSS programme is now closed, ahead of its planned completion date of 2016, as it has reached a point where it no longer meets organisational needs and a different approach to organisational change is required. That said, it is important to note that much hard work has gone into the multiple TSS work streams and the commitment of our staff is a credit to them, the Trust and local mental health services.
1.3 Many TSS work streams undertook specific lessons learnt workshops with staff after go live of their project. However, this report is not an in-depth review of each of these, nor does it comment on the respective merits or otherwise of the changes, instead it provides an overview of the lessons learnt themes from TSS as a programme of change and outlines how the Trust will approach change from this point forward.
1.4 The Trust Board acknowledges mistakes were made in the planning and delivery of TSS, recognising the impact on some staff this has had and has been open in its apology to those affected.
1.5 The Board is also clear that while there are issues within some services as a result of TSS, and these are now being revisited, it is equally important to note that many of the changes have been positive and successful new services have been created.
1.6 The Board intends to learn from this and ensure future change programmes, which are essential to the future of the Trust, mental health services and the NHS, are implemented in a more proactive, transparent and consistent manner.
2.0 Key Themes from Lessons Learnt
2.1 The following are an amalgam of feedback from lessons learnt workshops, discussions with staff, service users, carers and external partners. It may appear a negative review as, by their nature; lessons learnt exercises can often be considered as such.
2.2 The commitment, enthusiasm and resilience of many of our staff were exemplary and their equal keenness to see future change programmes learn from the following to ensure success is to be commended.
2.2 Leadership
There was a common consensus to a lack of ownership at every level. Managers were unsure which executive was leading, managers and clinicians were each unsure of who was responsible for which aspect of design or delivery. Project roles were not defined.
TSS was billed as a clinician led project yet many report feeling they were not involved post initial discussions and as a result feel little ownership to the end product.
2.3 Planning & Data
The programme did not have a defined start with clear leadership and as such due to the lack of a programme overview, many of the work streams had competing priorities at every level. A key example of this was trying to develop care packages at the same time as the workforce changes where one clearly comes before the other. As such, at implementation phase, many outcomes did not match the intended plan.
The population health needs, service usage and patient flow data to support TSS in terms of a rationale for change, was either considered not to be robust or not evident. The
Board of Directors – Public Date December 18 2014 TSS Lessons Learnt
Version 1.0
Author: Leigh Howlett Department: Commercial
Page 3 of 4 Date produced: Retention period: 30 years
clinical change case was reported to be more about efficiency and money with no benchmarking or analytical review of health trends evident.
Staff felt that much time was spent talking about TSS and then final decisions and plans were rushed through without adequate time to consider all factors. Staff and stakeholders also consider that, at the time of merger when TSS was not fully defined, an opportunity was missed to consider the benefits of planning Norfolk and Suffolk services together.
Timeliness of planning overall was considered to be a major challenge. TSS was billed as a five year strategy and yet all the major changes were over within a year to eighteen months. As the overall strategic planning was not in place, alterations to services were made without adequate consideration of the impact elsewhere; this has been particularly evident in the community services in Norfolk. The financial imperative was cited as the reason for HR and business processes being, in the views of the staff, unnecessarily rushed.
2.4 Workforce
The supporting HR processes had a mixed review and, like many change process, was impacted on by the experience of the manager and the HR support they received. While standard templates and processes were available, the use of these was not consistent.
Of particular concern was the handling of voluntary redundancy. This one factor has caused the biggest damage to staff morale. In addition, the different approach to the medical workforce (and in particular the transition money spend on locums) was the other significant area of dissatisfaction amongst staff at all levels.
The workforce data was not considered to be robust enough to truly enable effective change. Banding data, length of service and skill sets were not adequately recorded to support the significant change required for many services. Again, much of the outcome from this was dependent on the managers’ knowledge and experience as opposed to hard data.
2.5 Communication & Engagement
Though TSS had a dedicated communication lead, a single set of key messages to be used by every manager or work stream lead as the principles for change, were not delivered. This was mainly due to the lack of overall control / oversight whereby each work stream was acting independently and therefore the overall goal of TSS was lost.
It was universally agreed that engagement was inconsistent and, like many of the workforce factors, entirely dependent on the experience and knowledge of the manager/clinician involved rather than an agreed format and style.
In addition, though external engagement events were held, service users, carers and stakeholders report they did not feel this was robust or adequate for them to fully understand the changes.
2.6 Finance, Estates & ICT Support
The TSS programme was considered by many staff to be financially driven however the data on which this was derived, combined with the poor workforce data and, more importantly, service outcome and usage, was considered to be less than robust once change was underway.
The estate and ICT changes required for some work streams to be successful were not considered in adequate detail ahead of implementation. The estates and ICT teams were not effectively engaged at the beginning of the process and as such issues remain, such as IDTs not being in the right location, ongoing a year post go-live.
Board of Directors – Public Date December 18 2014 TSS Lessons Learnt
Version 1.0
Author: Leigh Howlett Department: Commercial
Page 4 of 4 Date produced: Retention period: 30 years
The ICT kit required for team moves and base changes were often an afterthought which caused a great deal of disruption to clinical and ICT business as usual services and unnecessary stress to staff.
3.0 Conclusions
3.1 The Trust Board has acknowledged that lesson must be learnt and a change in the way change is managed is required. The following are considered the key actions:
o The establishment of a Programme Management Office (PMO) to oversee all organisational change to include dedicated corporate support functions led by a single Executive Director
o The Trust should supplement its own staff with external expertise where it is clear that a particular skill set or knowledge is not available with the Trust. Ideally as part of this, the external support should provide some transfer of these skills to existing staff
o Training for all staff on Project Lite and Lean should be rolled out from the New Year. This will allow staff to understand their roles in how to deliver change effectively and efficiently
o HR processes are re-evaluated to ensure a consistent approach. This includes the criteria that voluntary redundancy should not be offered as a first choice and all staff, clinical and non-clinical, are treated equally
o All change plans should be clear on their intended outcomes, drivers and principles, focussing on how benefits will be realised and not on benefit mapping
o The PMO should provide / support the rationale and evidence to support the need for change
o The timescale for change should be challenging but realistic to allow for the organisational design piece to be robust, this in turn will facilitate an easier, quicker transition phase
o Communication of, and engagement in, any change should begin before decisions or choices are made. For staff this will include full support of Annexe X.
4.0 Recommendations
4.1 The Board is asked to consider, and accept, this report and its conclusions.
Leigh Howlett
Commercial Director
December 18 2014
BoD public - 18.12.14 Board reporting template
Version 0.1
Author: Robert Nesbitt Department: Corporate
Page 1 of 2 Date produced: 08.12.14 Retention period: 30 years
Report To: Board of Directors – Public
Meeting Date: 18th December 2014
Title of Report: Board report format refresh
Action Sought: For Debate
Estimated time: 5 minutes
Author: Robert Nesbitt
Executive: Robert Nesbitt (Trust Secretary)
Executive Summary:
The Foresight Partnership board evaluation action plan recommended that the board report format be reviewed with a particular focus on “narrative, analysis, improvement actions and trajectory to ‘green’”. This paper refreshes the template provided to all authors of papers, and proposes that the Trust Secretary provide individual feedback to authors after each board in order to improve the quality of reports.
1.0 The current template and reporting issues
1.1 The current template (appendix 1) includes guidance to authors on how to write a board report. However, the quality of reports that come to board is variable.
The main themes are:
Reports are sometimes too long with information copied and pasted from other papers without sufficient regard for the needs of the board.
Reports sometimes have too much data and insufficient analysis.
It is sometimes hard to discern a clear narrative that not only describes the key issues succinctly, but also sets out the causes and the significance for quality.
There is sometimes a focus on processes and activities at the expense of assurance as to when and how the issue will be addressed or, if this assurance cannot be given, what the risks the board needs to consider.
1.2 The timescale for board reporting mean that directors often rely on leads within their areas to draft board reports, and these arrive in time for printing and posting but not in time for re-writing. It is therefore important that the authors understand
Date: 18th
Dec 2014
N Item: 14.172iii
BoD public - 18.12.14 Board reporting template
Version 0.1
Author: Robert Nesbitt Department: Corporate
Page 2 of 2 Date produced: 08.12.14 Retention period: 30 years
how well their papers meet the board’s needs. At present there is no formal way for authors to receive feedback on their reports.
2.0 Revised template and feedback arrangements
2.1 The current template will be revised to include the following guidance for authors
“Ensure that your paper is succinctly written and clearly identifies the key messages for the board. If your paper includes data it must a. be essential for the board’s deliberation and b. accompanied by an analysis which explains what the data says, why it is significant, what the causes are, and what the proposals are to address any deficiencies.
2.3 “Any performance or quality problems identified in your report must either include an action plan that is in sufficient detail to provide assurance that it is achievable, or a narrative that explains why the plan might fall short and what the risk consequences are. Action plans must be SMART with trajectories that show the milestones to ‘green’.
2.4 “The board is there to assist in making difficult decisions and there is no expectation that every problem must be accompanied by a solution. Such an approach can lead to defensiveness. It is better to provide an option appraisal setting out the relative merits and risks for each option and to ask the board use its skills and experience to make a decision. However, if you are taking this approach the matter must have already been discussed at the executive team meeting and there must be a comprehensive report to the board to enable the final decision.
2.5 It is proposed that Trust Secretary provides feedback via email to authors on the quality of their reports after each board meeting for 6 months (Jan to June 2015) and that the board then uses development time to reflect on whether the quality of reports has sufficiently improved.
3.0 Recommendations
3.1 That the board approves changes to the report template and agrees for the above feedback system to be put into place.
Robert Nesbitt Trust Secretary 08.12.14
Background Papers / Information Appendix 1 – Current board template.
Name of meeting - Date of mtg <Name of doc>
Version 0.1
Author: Department:
Page 1 of 3 Date produced: Retention period: 30 years
Report To: Name of meeting
eg: Board of Directors – Public or Private
Meeting Date:
Title of Report:
Action Sought: For Approval / For Debate / For Information <-(no other option here)
Estimated time:
Author: Name (in full): Job title
Director: Name (in full): Job title
Executive Summary:
Remove sections in blue before sending. The purpose of the executive summary is to orientate the reader to the main points and priority issues, not to simply repeat the content of the main report. For approval papers:
What are the key points for the Board to consider?
What decisions need to be made?
Where in the paper can the information be found on which to base the decision? For debate papers:
Why is does the Board need to debate this matter?
What considerations need to be taken into account?
What should the Board have achieved at the end of this debate? For information papers:
Why is it essential that this information paper needs to come to the Board? (if this is not clear, then it should not come)
What are the headline messages?
What will happen next?
Date: DO NOT DELETE
Item:
Name of meeting - Date of mtg <Name of doc>
Version 0.1
Author: Department:
Page 2 of 3 Date produced: Retention period: 30 years
Notes for main report: Use succinct summaries and analysis which set out the implications of information and do not load the report with raw data; just give sufficient for the board to make a decision. Make sure that you include qualitative and quantitative analysis where appropriate to aid decision making. ALWAYS complete 1.0, 5.0 and 6.0. Complete 2.0, 3.0 and 4.0 if appropriate. Please use colour in your reports only when absolutely necessary: this will save on
printing costs and time Give abbreviations in full the first time they are used Give dates in full – include the year
1.0 Report contents
1.1 Para 1
1.2 Para 2
1.3
2.0 Financial implications (including workforce effects)
2.1
2.2
3.0 Quality implications
3.1
3.2
4.0 Equality implications / summary of consultation
4.1
4.2
5.0 Risks / mitigation in relation to the Trust objectives (Consider implications for internal and external communications and implications for the Board Assurance Framework)
5.1
Name of meeting - Date of mtg <Name of doc>
Version 0.1
Author: Department:
Page 3 of 3 Date produced: Retention period: 30 years
5.2
6.0 Recommendations
6.1
6.2
Name Title of Author Date of Paper
Background Papers / Information Give details of any background papers / information
Board of Directors – Public 18
th December 2014, Green Light
Toolkit implementation – Learning Disability Strategy
Version 1.0
Author: Jane Sayer Department: Trust Management
Report To: Board of Directors – Public
Meeting Date: 18th December 2014
Title of Report: Learning Disability Service Strategy
Green Light Toolkit Implementation: Learning Disability Strategy
Action Sought: For Approval
Estimated time: 10 minutes
Author: Jane Sayer, Director of Nursing, Quality and Patient Safety
Director: Jane Sayer, Director of Nursing, Quality and Patient Safety
Executive Summary:
This is a report on progress by the Trust to provide modernised services for people with a learning disability and mental health problem in Suffolk, with an update on proposals currently being considered by Clinical Commissioning Groups. The report also gives an update on the Trust’s work to provide accessible, effective and caring services for people with a learning disability who need to use mental health services across the Trust. This is a group that has not always received good services nationally, and who have particular vulnerabilities and needs. The Trust has previously delivered a good overview and action planning process, but this has been less robust since Trust merger. With the assistance of the National Development Team for inclusion (NDTi), a small group of staff have been working on immediate priorities for action, and planning longer-term strategy development. Results from the Green Light Toolkit self-audit are now available, and the action plan delivery is in progress, and due for review again in January 2015.
1.0 Report contents
2.0 The Trust continues to work with Commissioners in Suffolk on plans to re-focus care for people with learning disabilities and mental health problems to community-based care.
3.0 Plans are in place to establish a baseline of performance, and set priorities for immediate action. The Green Light Toolkit audit was conducted in November 2014, and highlights areas for improvement. Plans are also in place for development of a co-produced learning disability strategy for mental health services in Norfolk and Suffolk.
2.0 Suffolk Learning Disability Service Strategy
Date: 18 December 2014
P Item: 14.173 ii
Board of Directors – Public 18
th December 2014, Green Light
Toolkit implementation – Learning Disability Strategy
Version 1.0
Author: Jane Sayer Department: Trust Management
2.1 Background
In April 2013 Suffolk CCG's issued a revised specification for the provision of Learning Disability services in Suffolk. Key elements of this specification included: a reduction in the number of inpatient beds and no further use of out of area placements. Commissioners indicated they wished to work with NSFT to co-create new services and invited the Trust to develop proposals to meet the new specification. In October 2013 NSFT submitted, as requested, a detailed capacity and capability assessment together with an outline model. Commissioners did not respond to this submission until Spring 2014, but following meetings expressed an interest in moving forward with NSFT’s proposal. They also asked the Trust to provide a high level action plan and detailed costings. These were submitted to commissioners in June 2014. The Trust has been in discussion with the CCGs from this point, and the remit has been the redesign of services for people with Learning Disabilities including the development of an all age pathway for children, adolescents and adults. The implementation of the Suffolk Learning Disability Service Redesign Pilot is subject to discussion with the Health Overview and Scrutiny Committee.
2.2 Current Provision
The current core LD service in Suffolk comprises:
Inpatient Services, Walker Close, Ipswich. Twelve Assessment and Treatment beds (six male, six female) commissioned by Suffolk CCGs.
Lothingland, 7 Airey Close - four beds (male) for step down and recovery typically for service users returning from low secure or locked rehab provision. Three of these beds are commissioned by Suffolk CCGs and one by Great Yarmouth and Waveney CCG.
Lothingland, 6 Airey Close - four beds (two male, two female) for young people under 18. Again three beds are commissioned by Suffolk and one by Great Yarmouth and Waveney.
Community. In Suffolk there are five neurodevelopmental pathways , one within each of the Integrated Delivery Teams. In Waveney there is a CAMHS LD service to young people and their families. This team works closely with the wider children, families and young peoples services. There is no equivalent team in the rest of Suffolk although the function is delivered as far as possible by two dedicated posts.
In summary, the current community service model is Monday to Friday 9-5 with no out of hours cover. There are limited alternatives to admission when residential placements breakdown as housing needs are often complex and there is a poorly developed supported housing market with long lead times. Community based in-reach into residential settings is limited and, therefore, there is a low threshold for admission. Once a residential placement breaks down finding a suitable alternative is difficult and leads to delayed transfers of care with extended length of stays of up to 6/12 months
Board of Directors – Public 18
th December 2014, Green Light
Toolkit implementation – Learning Disability Strategy
Version 1.0
Author: Jane Sayer Department: Trust Management
2.3 Future Plans
In essence NSFT's proposals seek to provide a more community based service for people with a learning disability and one which works much more closely with primary care. In line with one of the key Winterbourne View recommendations, the model also seeks to ensure people who need a service get that service as close to home as possible. The main proposals for the pilot include:
Link workers in Primary Care to work within G.P. Practices.
Dedicated Learning Disability pathway within IDTs for all ages.
24/7 Home Treatment Team to offer an alternative to inpatient admission.
Smaller Inpatient service, with reduced bed numbers
Positive Behaviour Approach to focus on working with people with challenging behaviours.
Work in partnership with other providers to provide time away from home beds.
All age service redesign of the neuro-developmental disability team.
Funded within existing financial envelope
2.4 Milestones for Delivery
There are no firm dates associated with the planned pilot yet, as further discussions with the HOSC are happening in December 2014. However, the following outline plan is proposed: January – March 2015:
Internal staff engagement including care pathway review,
Carer and service user engagement
External stakeholder engagement
Begin implementation of bed reduction plan
April – June 2015:
Primary Care linkworkers in place
July – December 2015:
Staff training and redeployment where necessary
Current cohort of service users discharged to appropriate accommodation
3.0 Learning Disability Strategy
3.1 Background In the last thirteen years, the drive to improve access to mainstream services for people with a learning disability has strengthened. Valuing People (2001) set out a vision for moving from specialist, poorly resourced and often discriminatory provision to mainstream and high quality provision in the areas of employment, housing and healthcare. A number of reports have highlighted the poor healthcare services that people with learning disabilities receive, and the dreadful
Board of Directors – Public 18
th December 2014, Green Light
Toolkit implementation – Learning Disability Strategy
Version 1.0
Author: Jane Sayer Department: Trust Management
consequences of this. Death by Indifference (2007) told the story of people who died prematurely from conditions that were treatable but undetected, and the Ombudsman Report of 2009, Six Lives, set out expectations for the transformation of services to prevent such tragedies. Although most of these have occurred in primary and acute care, mental health services also need to improve their access to services and treatment of people with learning disabilities. The revised Green Light Toolkit (2013) provides a service improvement framework for mental health services. The Trust has previously developed and delivered actions in response to these issues, but the latest plans are from 2011, and this priority seems to have lost its impetus since the Trust merger in 2012.
3.2 Progress to date
The National Development Team for inclusion (NDTi) is now working with the Trust to improve immediate service provision for people with learning disabilities in mainstream services, and then to work on a co-produced strategy for the medium-term. Following two meetings with a small team of staff in September and October 2014, the actions described in Appendix 1 are in progress, and the GLTK team is due to meet again in January 2015 to review outcomes to date.
3.2.1 Green Light Toolkit audit One of the first priorities for the Trust has been to re-audit services using the 2013 version of the Green Light Toolkit (GLKT). The audit tool in Appendix 2 was used. The audit rates services against basic, better and best standards, using a four point scale for each item of assessment. This audit was done relatively quickly to give us a baseline, so was conducted through self-assessment, largely by Matrons. The following services provided a self-assessment:
Secure Services: Inpatient.
Secure Services: Criminal Justice Mental health and Liaison.
Secure Services: Community Mental health Team.
Central Locality: Norfolk child Families and Young Peoples service EI.
Central Locality: Norfolk child Families and Young Peoples service Youth.
Central Locality: Norfolk child Families and Young Peoples service Under 14’s.
Central Locality: Community services.
Central locality: Older Peoples service Hammerton Court.
Central locality: Older Peoples service Sandringham Ward.
Central locality: Older Peoples service Blickling Ward.
Gt Yarmouth and Waveney Locality: Submitted for all services.
Gt Yarmouth and Waveney Locality: LD CAMHS service
West Norfolk: Submitted for all services.
West Suffolk: Adult Acute.
West Suffolk: Adult Community.
East Suffolk: Acute services.
Board of Directors – Public 18
th December 2014, Green Light
Toolkit implementation – Learning Disability Strategy
Version 1.0
Author: Jane Sayer Department: Trust Management
The audit findings are displayed collectively for the Trust in Appendix 3, against nationally benchmarked data collected by NDTi. Notably, the Trust performed relatively well in the following areas:
Assessment
People needing personal care
Psychological therapies
Working together
Buildings and environments
Monitoring
The main areas for improvement are:
Physical health
Personalisation
Research
Health and care records and care plans
Commissioning
Checking services
These findings will now be considered alongside the current action plans for areas to prioritise. We will also review what supports teams to do this well so we can learn from them and spread good practice
3.2.2 Other areas of progress The Modern Matron for Learning Disability Services will be supporting the Director of Nursing and Quality, working as a GLTK lead for the organisation two days a month from January 2015. The 2015 PLACE audits will include a learning disability perspective – we hope to engage a service user to be part of the inspection team. Work on accessible information in underway, including links with pharmacy to ensure that medication information is accessible.
3.3 Strategy Development
The actions above will contribute to the development of a Trust strategy for the provision of mental health services for people with learning disabilities. NDTi will assist with the production of the strategy, initially engaging potential coproduction partners. Because the work covers both Norfolk and Suffolk we have agreed that it would be most sensible to spend a day in Norfolk having a meeting with people with learning disabilities followed by a meeting with family carers – repeated the following day in Suffolk. The point of these meeting is to share the principles of coproduction, what the Trust wants to do and engage people in getting involved in the coproduction group.
Board of Directors – Public 18
th December 2014, Green Light
Toolkit implementation – Learning Disability Strategy
Version 1.0
Author: Jane Sayer Department: Trust Management
The intention was to do these meeting in late October or early November, but the timescale slipped with preparation for the CQC visit. We have identified the following participants – local Mencaps, local MINDS, Suffolk User forum, Open Doors, ACE, Better Lives, Age UK, and Inclusion East, and are intending to hold meetings in February 2105. Further work will then continue to produce a strategy with meaningful and measureable outcomes, and it is anticipated that this work should be completed by the end of Summer 2015.
4.0 Risks / Mitigation in Relation to the Trust Objectives (Implications for Board Assurance Framework)
4.1 Healthcare services that meet the needs of people with learning disabilities are likely to be universally high quality, responsive and caring. It is essential that services we provide can be measured against the requirements of the Green Light Toolkit with positive outcomes, and that we can consistently meet the Monitor requirements on Access to Healthcare for people with learning disabilities.
5.0 Recommendations
5.1 The Board of Directors is asked to note and approve the contents of this report, particularly in relation to part 12 of the action plan.
Jane Sayer Director of Nursing and Quality 8th December 2014
Background Papers / Information Appendix 1: GLTK working group action plan Appendix 2: GLTK audit results Appendix 3: GLTK audit
Board of Directors – Public 18
th December 2014, Green Light
Toolkit implementation – Learning Disability Strategy
Version 1.0
Author: Jane Sayer Department: Trust Management
Appendix 1: Green Light Toolkit Action Plan, Meeting held 7th October 2014 Topic Sponsor and Priority Delivery
team Suggested milestones
1. Engage people using services and relatives
Bring together people using services and family members who have experience of the GLTK agenda. Invite people via advocacy organisations and user led organisations, such as Equal Lives, Norfolk People First, Suffolk Family Carers, Better Lives, Impact, ACE, Age UK and other agencies and mental health organisations. Coordinate this with Topic 2 below.
Is there any evidence that services are being personalised, or are services still dictating the content of support packages and offering standardised and limited options, rather than promoting unique solutions invented by the person or their informal community?
Sponsor: Jane Sayer. Priority: to begin before CQC visit but continue afterwards
Jude Wells, NDTi
To start work in Jan 2015.
An undertaking has been given from Ian and Jane as senior figures in the Trust that the messages from this exercise will be treated with respect
Set dates for one day of meetings in Norfolk and one in Suffolk
Win one member of each of the named groups to support the success of the project
Good turnout at meetings, constructive discussion and a detailed record
NDTi to provide a report which will (i) show how feedback from people using services and relatives links with strategy, and (ii) can be shared with all stakeholders
2. Audit GLTK progress to date
GLTK Audit Tools – nothing done to date, so start with inpatient first and do community later.
Sponsored by Jane Sayer and promoted by modern matrons. Peter to send the 3 audits as Word documents.
Decide whether to do the Basic Audit or all three.
Board of Directors – Public 18
th December 2014, Green Light
Toolkit implementation – Learning Disability Strategy
Version 1.0
Author: Jane Sayer Department: Trust Management
Topic Sponsor and Priority Delivery team
Suggested milestones
3. Advocacy services
Identify commissioned advocacy services working in mental health, learning disability and autism. Liaise with Topic 1 to prevent duplication.
Talk to them about their experience of supporting GLTK people. Get numbers if possible.
Once the systems have been reformed so that ‘GLTK people’ are recognised, check the number of times IMHAs have been requested through Mental Health Act offices.
Short term priority Ruth Turner Sue Bridges David Oakley
Advocacy is provided by Powr (secure mental health services do not expect to see referrals who also have LD), Impact provides LD advocacy, Voicability has both LD and MH skills. Some facilities are seeing advocacy organisations coming into their building and delivering presentations to service user meetings.
Design interview proforma (drawing on here and here and here) and approach to aggregating findings
Share out interview duties
Complete interviews within a month
Produce summary of key messages and recommendations within a further fortnight.
Feedback from Advocacy organisations has indicated that they Recovery College and Service User Forums are not making reasonable adjustments – action this.
Board of Directors – Public 18
th December 2014, Green Light
Toolkit implementation – Learning Disability Strategy
Version 1.0
Author: Jane Sayer Department: Trust Management
Topic Sponsor and Priority Delivery team
Suggested milestones
4. Links and champions - within and between teams and organisations
Identify a liaison person for mental health, learning disability and autism services by locality and service line. Find out why the previous network of champions disappeared and learn the lessons for a sustainable approach.
Locate, celebrate and disseminate good practice where it already exists in the Trust, with a particular focus on low-effort, high-impact solutions in the short term and big wins in the long term. Engage with the Trust Communications team and build a strategy for sharing progress on GLTK with all relevant stakeholders
Regain membership of Health Forum (part of LD Partnership Board) which is chaired by the Commissioner in order to seek tools and good practice
Build links with other local allies – seldom heard groups (including BAME and LGBT), social care provision, specialist services for women, Healthwatch, Health and Wellbeing Boards, Partnership Boards
Improve linkages and access to inclusive opportunities in the community beyond services via employment, further education, sports and leisure activities alongside the general public.
Sponsored by Julia Ankrah, Andrew Scott. Short term priority.
Ruth Pillar Markhu Wood
Decide where such champions should be located so that the numbers are not too great and yet people are close enough to the frontline and can prioritise GLTK work – so the network of GLTK champions is efficient and effective.
This idea is supported by Jane and Ian - each MH, LD and ASD service to be required to nominate a liaison person to advise the other teams.
Identify a Trustwide GLTK Coordinator to provide leadership, vision and coordination.
Once the network is established within the Trust, do a similar exercise with local allies – partnership board, seldom heard groups etc, asking each of them to nominate a link person
Write explanation and role description so people know what they are being asked to do
Circulate names and contact details to all.
Convene initial meeting to (i) share this action plan and win support for it, (ii) locate examples of good GLTK practice, (iii) harvest additional ideas for improvement. PB willing to facilitate this.
Board of Directors – Public 18
th December 2014, Green Light
Toolkit implementation – Learning Disability Strategy
Version 1.0
Author: Jane Sayer Department: Trust Management
Topic Sponsor and Priority Delivery team
Suggested milestones
5. Accessible information
Focus on appointment letters and service information leaflets, then consider referral documents and CPA forms (which are inaccessible to many people using services and dominated by service needs rather than personal recovery)
Rewrite Handy Charts so they help more learning disabled people to make an informed choice about medication
Collect and share some examples of personalised documents, such as plain English summary of a care review meeting. Work with
SALT experts to check, discard and improve where necessary
Support the Pharmacy service to produce accessible information about medication
Work with Governance colleagues to ensure that good examples of easy to understand information are not hidden or delayed but can be identified, spread and adopted at pace and scale.
Engage with the Communications team to get the message out
Sponsored by Julia Ankrah, Ruth Taylor and Ruth Pillar. Short term priority
Julia Ankrah Heidi McKay
Jane and Ian to secure support for the project from Governance and other gatekeepers who could block adoption of new documents for legal, procedural or other reasons
Select target documents in collaboration with these gatekeepers
Collect examples of personalised and plain English documents
Identify team to quality check and suggest improvements
Quality checkers to define acceptable standards
Link with Pharmacy
Create a dissemination strategy that enables good examples to be shared and spread and adoption to be tracked
Board of Directors – Public 18
th December 2014, Green Light
Toolkit implementation – Learning Disability Strategy
Version 1.0
Author: Jane Sayer Department: Trust Management
Topic Sponsor and Priority Delivery team
Suggested milestones
6. Staff skills audit
Find people with dual qualifications or specialist knowledge and experience by updating and repeating the previous audit of staff skills led by Paul Johnson, Talent Manager
Share findings, so that staff know who to ask for advice
This will begin to identify the specialists across the service, some of whom will become champions for the GLTK agenda.
Consider whether we can ask mental health staff (i) is learning disability and autism your business? (ii) Do you have the skills to do this well? (iii) Is your environment suited to this work?
Sponsored by Andrew Scott, Ruth Taylor and Ruth Pillar. Short term priority
Paul Johnson Ian Young Lauren Coates
Task 3 above is a priority and will gain more rapid progress than this task, so it will be tackled later rather than straight away.
Check out whether it would be possible to use the online staff directory to share details of staff GLTK skills
Locate previous audit and update for current needs – autism, personalisation, safeguarding etc.
Obtain advice from research colleagues to ensure survey questions are well designed and meaningful.
Decide whether to ask wider questions as discussed in column 1. Agree a questionnaire within a fortnight.
Distribute to staff and ask for completion within a further fortnight. Use Surveymonkey to speed distribution, collection of results and aggregation of results.
Communications plan for sharing contact details of experts identified through the audit
Board of Directors – Public 18
th December 2014, Green Light
Toolkit implementation – Learning Disability Strategy
Version 1.0
Author: Jane Sayer Department: Trust Management
Topic Sponsor and Priority Delivery team
Suggested milestones
7. Crisis response
Consider the services respond to GLTK people in crisis – at Accident and Emergency and other front door services. Are people with comorbidities being properly identified? Can anything be done to reduce the number of people who have to leave their neighbourhood and personal community in order to receive a service?
An extension of this is to consider the people who are referred out of the Trust’s area entirely. The number of people who are funded for out of area placements is too high.
This discussion will arise during the CQC inspection, but any serious work to address the causes will need a medium and long term solution.
This topic was raised in the meeting in August 2014 but it was agreed in today’s meeting that it was not a priority issue. The Psychiatric Liaison Service and general preparation for the CQC visit may consider these issues elsewhere.
8. In-patient units – physical environment
Particular focus on physical environment, signage, aids and adaptations, sensory stimuli, wayfinding etc.
Utilise previous findings from PLACE audits, CCG visits, CQC
Develop a new audit framework to focus on GLTK aspects, use it to help inpatient services build an action plan for improvement and insert the most important monitoring items into local PLACE audits for ongoing use
Sponsored by Jane Sayer. Short term priority.
Jane Sayer
Jane has reviewed evidence from previous CQC assessments, done numerous checks and considered the value of the PLACE Audits in relation to the GLTK work.
Identify units who will be audited with the new framework and win support from their managers, so that findings and recommendations result in action. Set visit dates early, and find auditors and design audit framework afterwards
Liaise with coordinators of PLACE audits to establish that key items can be usefully added that will help to address the GLTK agenda
Identify audit teams – including people using services and carers – to conduct these GLTK PLACE audits
Board of Directors – Public 18
th December 2014, Green Light
Toolkit implementation – Learning Disability Strategy
Version 1.0
Author: Jane Sayer Department: Trust Management
Topic Sponsor and Priority Delivery team
Suggested milestones
9. Informatics
Ensure the Lorenzo client database is fit for GLTK. Model outputs (trends that will drive management action) before the final sign-off of the data fields
Develop the ability to count the number of GLTK people in each part of the service, aggregate across service lines, compare with population profiles and uncover patterns so that action can be quickly taken to improve the service response. This is particularly important for GLTK people who are not using learning disability services.
Form a group with a clear agenda, meeting dates and information feed who will be able to receive trend and exception reports, recommend action and report to the GLTK Champions and Senior Management.
Sponsor: Julia Ankrah Long term priority
Long term priority, so no milestones set at this stage (need to start very soon, but not overstock the agenda at this point in time)
Heidi has attended a meeting in relation to this workstream and found out that there is provision for easy read formats in the new system.
Today’s meeting included some time spent on considering the outputs of an informatics system that would allow the GLTK Steering Group under Jane’s leadership to track progress (the ‘6 Graphs’ challenge).
10. Train staff
Review relevance and uptake of the e-learning package on learning disability awareness that was co-produced by a learning disabled person, a carer and a staff member some years ago.
People using services and their relatives to co-present training sessions
Sponsored by Julia Ankrah. Long term priority
Long term priority – see above
The e-learning training package has been reviewed by Julia. 300 people have used it in the last year, but it is out of date. Agreed to carry out a quick fix by amending organisation names etc so that it appears more up to date, whilst developing a longer term approach to having it replaced.
Board of Directors – Public 18
th December 2014, Green Light
Toolkit implementation – Learning Disability Strategy
Version 1.0
Author: Jane Sayer Department: Trust Management
Topic Sponsor and Priority Delivery team
Suggested milestones
11. Safeguarding – review data from LD services
Define the most significant risks to people using learning disability services and how the Trust is responding.
Review the past 6-12 months records of incidents and near misses, look for lessons and make service improvements accordingly.
Within this work, consider how people with mental health issues fare.
Sponsored by Andrew Scott. Priority for overall CQC agenda, within which the GLTK is one component. So GLTK group need to be partners, but not lead on this.
Andrew Scott
Ownership of this issue sits outside the GLTK group. However, clarify GLTK issues within the wider safeguarding Topic within the CQC purview
Andrew has obtained details of safeguarding incidents in LD services in the past 12 months. Nearly 600 reports were generated, so the suggestion that they be reviewed would mean a much larger project than can be undertaken at this time. Normal reporting mechanisms seek patterns and learning points.
Board of Directors – Public 18
th December 2014, Green Light
Toolkit implementation – Learning Disability Strategy
Version 1.0
Author: Jane Sayer Department: Trust Management
Topic Sponsor and Priority Delivery team
Suggested milestones
12. Strategic Leadership a. Obtain commitment from Trust Board and Senior
Management Team, along with a reporting framework to ensure that staff time and resources are available and the GLTK agenda is given due priority and wide support.
b. Identify, appreciate and build on good work that has been done in the past. Collate previous reports, resources and tools and use them as an historic benchmark where possible to avoid reinventing the wheel.
c. Identify all the relevant guidance documents that should shape the work
d. Assert core principles of service delivery – person-centred care rather than diagnoses of exclusion and capacity-building to help non-specialists develop their competence and confidence through internal consultancy support across teams, collaborative work where needed in response to co-morbidity.
e. Honest inquiry to find out if we do what we say in local service information leaflets, relevant policy documents etc. and take action as appropriate.
f. Clarify the requirements of commissioners whilst robustly indicating our view of best practice.
g. Section 75 transfers and other organisational changes – anticipate and mitigate adverse consequences for GLTK group
10a-10c are short term priorities.
Jane Sayer
Set programme of dates for the GLTK Steering Group to meet and oversee these developments. Take regular reports on all the Topics identified here from each of the Delivery Teams. Identify chair and membership.
Jane has written a paper and submitted it to the Trust Board to gain senior support for this action plan and agree reporting arrangements that are agile and responsive. NED member of the GLTK Project Group with delegated authority to approve and/or routine reporting to Board?
Ransack the archive to show that this agenda is not new to the Trust – look for places where we can build on old work. Put out a call for documents and place them in an intranet shared workspace.
Create newsletter or regular GLTK item in generic news briefings so that everyone gets frequent updates on GLTK progress in the Trust.
Refresh the relationship with commissioners.
Appendix 2: Green Light Toolkit Audit
Basic
Audit In the garage, not yet started
D
On the journey, but stuck at Red
C
Ready for more – Amber
B
Continuous progress – Green
A
Sco
re
Physical
Health 1D. We are doing nothing locally to correct for the health inequalities suffered by people with a combination of autism, LD and MH needs
1C. There is some understanding that people with autism or LD may have specific health needs, but no clear plan to address this
1B. Specific actions are taken by MH services to help people with autism or LD engage with routine health screening in primary care
1A. In addition to supporting people to access routine health screening our local MH service is taking action to encourage healthy lifestyles and people with autism and LD are engaged
Eligibility and
Access 2D. Autism or LD is used as a diagnosis of exclusion to shut people out of MH services
2C. Some people with autism or LD may receive support from MH services, but this is not part of a deliberate and systematic approach
2B. Eligibility criteria include a clear expectation that MH services should serve people with autism or LD, but they may not actually be doing so
2A. People with autism or LD are found in all parts of the MH service
Secure
Settings 3D. Local people with autism or LD in addition to a MH issue are inappropriately placed in prisons or secure settings rather than a more suitable setting
3C. There is a prison diversion scheme that responds to offenders who have MH in addition to LD or autism
3B. Prisoners and people in secure MH settings can get access to MH, LD and autism expertise when needed
3A. Targeted work addresses offending and challenging behaviour in a manner that is relevant and effective for people with any combination of MH, autism and LD needs
Safeguarding 4D. We have no evidence to demonstrate the safety record of MH services in relation to people with autism or LD
4C. The MH service tracking system for untoward incidents includes a specific facility for tracking incidents involving people with autism or LD
4B. There is evidence that the MH service is learning and changing its practice in response to local incidents involving people with autism or LD
4A. Frontline MH staff report feeling supported when raising safeguarding concerns – they feel that they work in a healthy learning culture rather than a blame culture
Assessment 5D. Some people benefit from a detailed assessment of how autism, LD and MH issues affect them, but we can’t obtain that assessment round here
5C. Screening for autism or learning disability takes place for people with MH issues who need it
5B. Detailed assessments for autism, LD and challenging behaviour can be obtained for people who need them who are currently using MH services
5A. There is a systematic and proportionate approach to the use of screening and full assessment. Results have a positive effect on what happens to the person afterwards
Board of Directors – Public 18
th December 2014, Green Light
Toolkit implementation – Learning Disability Strategy
Version 1.0
Author: Jane Sayer Department: Trust Management
Equalities 6D. We can’t find any Reasonable Adjustments that have been made in anticipation of people with autism or LD using mainstream MH services.
6C. A couple of things have been done, but they do not really affect common practice in MH services.
6B. Some specific good practices in relation to autism or LD are used throughout the MH service, but weaknesses remain
6A. Reasonable Adjustments made in MH services are routinely identified, adopted where needed and recorded to show their impact on people with autism and LD
Personalisation 7D. There are such a lot of practical and ethical difficulties with personalisation in our local area that we haven’t really considered it for people with autism or LD alongside a MH problem.
7C. A few people with autism or LD alongside MH issues are in receipt of a personal budget or direct payment
7B. A combination of universal community facilities, telecare and bespoke arrangements has been tried out for a few people with a MH issue alongside autism or LD
7A. People with autism or LD alongside a MH need are most likely to receive a bespoke service unlike anyone else’s that avoids institutional responses, but is rather designed around their circumstances and uses universal community facilities wherever possible
Staff attitude
and values 8D. Staff in MH services do not believe they should treat people with autism or LD
8C. Some mental health staff recognise the value of their service supporting people with LD or autism, perhaps through receiving awareness training in LD and autism
8B. All staff are encouraged to take a positive approach in this area, perhaps by local champions for LD and autism in MH services who have sustained input into development and training programmes
8A. Attitudes and values are demonstrated in practice – there is evidence that MH staff have improved their practice in response to the needs of people with autism and LD
Accessible
Information 9D. No easy read materials can be found when visiting MH services
9C. Some easy read or audio materials are available, perhaps on the organisation’s website, but there is no evidence that they are being used
9B. Easy read and audio materials are available in patient areas and cover medication, the Mental Health Act, local services, complaints procedures, and advice on how to get help
9A. Staff utilise these resources and adapt their communication to the person rather than just relying on the leaflet
Board of Directors – Public 18
th December 2014, Green Light
Toolkit implementation – Learning Disability Strategy
Version 1.0
Author: Jane Sayer Department: Trust Management
Better
Audit In the garage, not yet started
D
On the journey, but stuck at Red
C
Ready for more – Amber
B
Continuous progress – Green
A
Sco
re
Research 10D. Commissioners and lead clinicians have made no use of research evidence in relation to the combination of autism, LD and MH
10C. Research evidence is informing how MH services are arranged and delivered to people with autism or LD
10B. Standardised tools and evidence-informed interventions are in use locally to help people with autism or LD in addition to a MH issue
10A. Local MH staff are generating new research evidence on this topic
Health and
care records
and care plans
11D. There are no adjustments made to health and care records or care plan proformas in our mainstream MH service to accommodate people with autism or LD
11C. Copies of accessible care plans and care records are available on request
11B. When a person with autism or LD is identified in the MH service, they are routinely given an accessible copy of their care plan
11A. People have a copy of their care plan which they have co- produced and recorded in a format that they understand (e.g. photographs as well as writing)
Local plans 12 D. There is no reference to people who have a combination of autism, LD and MH needs in the mental health section of population needs mapping, the Joint Strategic Needs Assessment, the local Health and Wellbeing strategy or commissioning plans for MH services
12C. National data is used to highlight the need for MH services to respond to people with autism or LD, but there is no local data. General statements assert the principle of fair access for people with autism and LD in MH services
12B. The principle of fair access for people with autism and LD to MH services is converted into specific local actions
12A. The local plans show clear links between national data, local data capture, planning for service developments and improvements to outcomes
How
specialist
services relate
to local
provision
13D. Most of the local people who need intensive support are in secure settings far from home
13C. Mental health services play a part in some people with overlapping needs returning to live in the local area, we know who is still living out of area and plans are
13B. An increasing number of people with the most complex MH needs in addition to LD or autism are supported in the local area through personalised
13A. In addition, specialist services (e.g. secure settings or people with specialist skills in working with people who have overlapping needs) routinely help
Board of Directors – Public 18
th December 2014, Green Light
Toolkit implementation – Learning Disability Strategy
Version 1.0
Author: Jane Sayer Department: Trust Management
in place to bring them back wherever possible.
arrangements that include support from mental health services
their colleagues in mainstream MH services to develop their skills
Skilled
workforce 14D. Our MH service has limited effectiveness with people who have autism or LD because we lack crucial skills
14C. It is clear through Job Descriptions, programmes of compulsory training and other signals that MH staff should provide a service to people with autism and LD
14B. Appropriate policy and procedure documents in MH services have some embedded reference to people with autism and LD using the services
14A. MH staff have access to support in working with people who have autism or LD, perhaps through training or a local Community of Practice that identifies challenges and raises standards
People
needing
personal care
15D. It’s a problem every time someone arrives in MH services and needs help with personal care
15C. Additional help is brought in to support the person as needed
15B. Our staff team are flexible and help people who need it with eating, using the toilet or personal care, such as cutting finger nails
15A. Our MH staff team learn about best practice in personal care and change their behaviour in response so that everyone needing our MH service can benefit, including those with autism or LD
User
involvement
in governance
of the service
16D. No sign of effort being made by the people responsible for management and governance of the MH service to engage people with autism or LD
.
16C. People with autism or LD and MH difficulties and their relatives are kept informed about service changes
16B. People with autism or LD and their relatives provide feedback on the quality of MH services
16A. People with autism or LD and their relatives are involved in assessing population need and designing MH services – perhaps via a Partnership Board or similar arrangement
Psychological
therapies 17D. Psychological therapies are not available in primary care or MH services for people with autism or LD
17C. People with LD or autism are offered longer and more numerous psychological therapy sessions at suitable times
17B. MH psychological therapy services have made adjustments to their clinical interventions (i.e. the content of sessions rather than just their duration) so that people with autism or LD benefit from
17A. In addition, a specialist practitioner or team provides advice to the mainstream service and offers psychological therapies to people with autism or LD who struggle to benefit from the usual
Board of Directors – Public 18
th December 2014, Green Light
Toolkit implementation – Learning Disability Strategy
Version 1.0
Author: Jane Sayer Department: Trust Management
them
provision
Working
together 18D. Conflict, silo working and boundary disputes between teams and organisations mean staff don’t know people outside their own service
18C. A few staff working in MH services know and work with their colleagues in LD and autism services
18B. Most of the time, people who need expertise from two or more services receive it without undue delay or coordination difficulties
18A. There is an effective dispute resolution process that helps with the interface between MH, LD and autism services, including joint working and transition between services
Best
Audit In the garage, not yet started
D
On the journey, but stuck at Red
C
Ready for more – Amber
B
Continuous progress – Green
A
Sco
re
Advocacy 19D. Local advocacy services for people with MH issues do not work with people with autism or LD
19C. Local advocacy services for people with MH issues are willing and eager to work with people with autism or LD to improve their experience of mainstream MH services
19B. A programme for training and ongoing support is in use to ensure advocacy workers are effective with people who have autism or LD in addition to MH difficulties
19A. The advocacy service presents a regular report to the MH commissioner to show their activities and impact in relation to people with autism or LD who use MH services.
Commissionin
g 20D. Mental health and LD services are commissioned separately and MH commissioning does not address the needs of people who also have autism or LD. No account is taken of information collected for the Joint Strategic Needs Assessment
20C. The MH commissioning plan includes people who have autism or LD in addition to MH issues
20B. Clear outcomes are defined in MH services for people with autism or LD, perhaps with incentives for services that achieve them. Outcomes are linked to population needs and the plans made by our local Health and Wellbeing Board.
20A. Gaps are identified and this intelligence is used to develop the market and make improvements to the overall pattern of service delivery
Buildings and 21D. People with autism or LD are 21C. There is a general 21B. There are places and times 21A. Environments have been
Board of Directors – Public 18
th December 2014, Green Light
Toolkit implementation – Learning Disability Strategy
Version 1.0
Author: Jane Sayer Department: Trust Management
environments expected to use the same facilities in the same way as everyone else without adjustment
recognition that people with autism or LD may be adversely affected by some physical or social environments
where people can be quiet and away from others
signs, to provide effective help with wayfinding or booking appointment times
Leadership 22D. We don’t know who is interested in improving MH services for people with autism or LD
22C. We know who the self-appointed champions are
22B. Leadership on this topic is identified and can relate to all teams and levels of the organisation
22A. Identified champions promote creative problem solving amongst all staff – ‘distributed leadership’ is promoted.
Family and
friends 23D. Family and friends of people with MH needs in addition to LD or autism are rarely given information about MH services or the support they may be entitled to in their own right.
23C. Family and friends of people with autism or LD are asked about their experience of MH services and these are collated to look for shared themes
23B. Family and friends of people with autism or LD report positive experience of MH services
23A. Family and friends of people with autism or LD receive targeted support from the MH service, perhaps through a carers support group or training opportunities
Employment
support 24D. People with a combination of autism, LD and MH issues rely on ordinary employment services, such as Jobcentre Plus
.
24C. Specialist MH employment support (such as job coaching, IAPT and IPS services) are available to people with autism or LD with the goal of getting and keeping open employment
24B. Five or more people with autism or LD have been supported by MH employment support agencies to get or keep a job in the last 12 months
24A. We have identified specific interventions that work with people who have a combination of autism, LD and MH needs to help them obtain and retain paid open employment
Checking
services 25D. No specific action has been taken to focus on how people with LD or autism get on in MH services.
25C. MH care pathways have been reviewed to ensure that people with autism or LD receive the support they need
25B. People with autism or LD and their family carers are involved in checking the quality of MH services
25A. The effectiveness of reasonable adjustments made in our MH services for people with autism and LD is routinely reported to the Board and Monitor
Board of Directors – Public 18
th December 2014, Green Light
Toolkit implementation – Learning Disability Strategy
Version 1.0
Author: Jane Sayer Department: Trust Management
Monitoring 26D. We have no local data on the number of people with autism or LD using MH services
26C. Some data collection has been done regarding MH service users who have autism or LD, but this has not become a regular routine and the data may be of poor quality or may not have been analysed
26B. Data is routinely collected via the electronic care record system. Some comparisons have been drawn with other data sets (e.g. census, national prevalence or regional benchmarks)
26A. Data is routinely collected and analysed. Unwarranted variations in access and outcomes for people with autism and LD using MH services are routinely identified and services are amended in response
Challenging
Behaviour 27D. Incidents of behaviour that challenge, self-harm and suicide are dealt with as they arise
27C. The MH crisis support team and anyone else responding to untoward incidents within the MH service has received training in autism and LD
27B. The MH service’s response to challenging behaviour and self-harm has been adjusted to accommodate people with LD or autism.
27A. When the person needs some help from external agencies, such as the police or Accident and Emergency department, our MH service help them to respond well to people who have any combination of autism, LD and MH issues.
people lives communities
B
C
D
A
Basic Audit Better Audit Best Audit
Red = your group Blue = national
November 2014
Green Light 2013: Audit Scores
Board of Directors – Public December 19 2014 PLACE Update
Version 1.0
Author: Leigh Howlett Department: Commercial
Page 1 of 3 Date produced: Retention period: 30 years
Report To: Board of Directors – Public
Meeting Date: December 18 2014
Title of Report: Patient Led Assessment Of The Care Environment (PLACE) 2013/14
Action Sought: For Information
Estimated time: 10 minutes
Author: Leigh Howlett, Commercial Director
Director: Leigh Howlett, Commercial Director
Executive Summary:
The purpose of this report is to provide the Board with a summary of PLACE results for 2014 and provide a comparison against the 2013 results and national benchmark. When benchmarked nationally against the other 49 mental health Trusts the Trust performed as follows:
Criteria NSFT Score
National Score
Mental Health National Benchmark
Cleanliness 99.63% 97.75% 10th
Food 91.57% 85.42% 20th
Privacy & Dignity 89.22% 88.90% 28th
Condition Appearance & Maintenance
97.56% 88.78% 6th
It should be noted that, due to changes in the assessment methodology and scoring for the Food and Privacy & Dignity sections comparison between 2013/14 is not directly comparable. All the individual unit scores are contained with the report. The above is reflected across all units with the exception of Wedgwood which scored poorly at the time of assessment. The result was unexpected and due to major building works being underway at the time which impacted on the environment and quality of dining experience, however, the food satisfaction at ward level score remained high (93.46%).
Date: 18 December 2014
Q Item: 17.173 iii
Board of Directors – Public December 19 2014 PLACE Update
Version 1.0
Author: Leigh Howlett Department: Commercial
Page 2 of 3 Date produced: Retention period: 30 years
1.0 Report contents
1.1 In previous years, the patient environment was subject to annual inspection under the Patient Environment Assessment Team (PEAT) process, in 2013, this was replaced by the Patient Led Assessment of the Care Environment (PLACE).
1.2 The purpose of this report is to provide the Board with a summary of PLACE results for 2014 and provide a comparison against the 2013 results and, where possible, national benchmark.
1.3 It is important to note that due to changes in the assessment methodology and scoring, the 2014 results for Food and Hydration and Privacy Dignity and Wellbeing are not considered to be directly comparable with 2013.
2.0 PLACE Assessment Aim & Criteria
2.1 The aim of PLACE assessments is to provide a snapshot of how the Trust is performing against a range of non-clinical activities which impact on the patient experience of care, these are made up of the following.
Cleanliness: covers all items commonly found in healthcare premises including patient equipment; baths, toilets and showers; furniture; floors and other fixtures and fittings.
The Condition, Appearance and Maintenance of healthcare premises: includes the above items as well as a range of other aspects of the general environment including décor, tidiness, signage, lighting (including access to natural light), linen, access to car parking (excluding the costs of car parking), waste management and the external appearance of buildings and the tidiness and maintenance of the grounds.
The extent to which the environment supports the delivery of care with Privacy and Dignity: includes infrastructural/organisational aspects such as provision of outdoor/recreation areas, changing and waiting facilities, access to television, radio, computers and telephones; and practical aspects such as appropriate separation of sleeping and bathroom/toilet facilities for single sex use, bedside curtains being sufficient in size to create a private space around beds and ensuring patients are appropriately dressed to protect their dignity.
The quality and availability of food and drink: includes a range of questions relating to the organisational aspects of the catering service (e.g. choice, 24-hour availability, meal times, and access to menus) as well as an assessment of the food service at ward level and the taste and temperature of food.
2.2 Although the basic assessment process is common to all our units, the precise areas undertaken in any particular site will vary according to size, service provision, and the precise services on offer. The results for NSFT for 2014 are shown in Appendix 1 of this report.
2.3 The scores for cleanliness were above the 2013 national average for all sites assessed except Northgate and St Clements which both showed a slight deterioration. Both sites receive regular visits from the Quality Assurance department within the facilities team and improvement has been seen with no complaints from service users or staff.
Board of Directors – Public December 19 2014 PLACE Update
Version 1.0
Author: Leigh Howlett Department: Commercial
Page 3 of 3 Date produced: Retention period: 30 years
2.4 The scores for food were above the 2013 national average for all sites assessed with the exception of Wedgwood. The food offering across all sites, except Wedgwood, is sourced from the same supplier and is part of a new contract introduced in early 2014. This is encouraging and work continues with the suppliers to ensure standards are maintained and improved further for longer stay units such as the Norvic.
3.5 The food at Wedgwood is, unlike all other sites, fresh cook and provided by the PFI partner Grosvenor. Previous scores and satisfaction rates have been high for this unit overall. A detailed review of the Wedgwood scores showed a service user satisfaction rate from the wards of 93.46% which is significantly above average and the overall poor score was a result of service users’ poorer dining experience given the major building works underway at the time. Whilst this work has completed on one ward, the overall unit refurbishment is scheduled for completion in January 2015. The Trust remains vigilant in working with Grosvenor to ensure the more important service user satisfaction score remains high.
3.6 The scores for privacy, dignity and wellbeing are above the 2013 national average for all sites assessed except the Norvic which is slightly below. Due to the changes in scoring and assessment, an initial review of the results indicated that the criteria for provision of televisions and radios was amended and this had a small adverse impact on the score along with provision of internet access to patients (which has a full roll out plan in place).
3.7 The Board are asked to note that no material breaches (e.g. single sex accommodation) associated with Privacy, Dignity and Well-being were noted during the PLACE assessments in 2014.
3.8 The scores for condition, appearance and maintenance were above the 2013 national average for all sites assessed except Wedgwood which was due to the extensive refurbishment programme being undertaken. An improvement for all other sites was recorded for the 2014 results which is an excellent achievement given the reduction in revenue spend over the reporting period.
3.0 Risks / mitigation in relation to the Trust objectives (implications for Board Assurance Framework)
5.1 PLACE results will be published and used as a component of assessing provider organisations ability to deliver safe and effective services and will directly contribute to informing targeted improvements to quality of the patient environment.
4.0 Recommendations
6.1 The PLACE scores for 2014 provide evidence of an estate that is clean and maintained to a high standard and where patients are provided with food which in most cases is above the 2013 national average benchmark and the Board is asked to note this report.
Leigh Howlett Commercial Director December 18 2014
SITE
2013
PLACE
2014
PLACE
NATIONAL
AVERAGE
LOCAL
VARIANCE
2013 >14
VARIANCE
NATIONAL
AVERAGE
Hellesdon Hospital
CLEANLINESS 98.73 99.11 97.25
FOOD** 96.45 95.15 88.79 N/A
PRIVACY, DIGNITY AND WELLBEING** 93.07 91.12 87.73 N/A
CONDITION APPEARANCE AND MAINTENANCE 92.86 99.03 91.97
Carlton Court
CLEANLINESS 99.48 99.48 97.25
FOOD** 97.18 96.20 88.79 N/A
PRIVACY, DIGNITY AND WELLBEING** 95.17 92.06 87.73 N/A
CONDITION APPEARANCE AND MAINTENANCE 97.50 99.62 91.97
Norvic Clinic
CLEANLINESS 98.94 99.66 97.25
FOOD** 96.38 93.77 88.79 N/A
PRIVACY, DIGNITY AND WELLBEING** 97.57 95.11 87.73 N/A
CONDITION APPEARANCE AND MAINTENANCE 97.83 99.72 91.97
Fermoy Unit
CLEANLINESS 97.46 99.03 97.25
FOOD** 96.83 90.00 88.79 N/A
PRIVACY, DIGNITY AND WELLBEING** 89.14 81.67 87.73 N/A
CONDITION APPEARANCE AND MAINTENANCE 83.33 98.36 91.97
Julian Hospital
CLEANLINESS 99.14 99.95 97.25
FOOD** 96.34 93.50 88.79 N/A
PRIVACY, DIGNITY AND WELLBEING** 92.66 91.83 87.73 N/A
CONDITION APPEARANCE AND MAINTENANCE 95.38 99.35 91.97
Wedgwood
CLEANLINESS 99.48 99.94 97.25
FOOD** 97.88 86.70 88.79 N/A
PRIVACY, DIGNITY AND WELLBEING** 93.68 85.85 87.73 N/A
CONDITION APPEARANCE AND MAINTENANCE 96.25 90.35 91.97
St. Clements Hospital
CLEANLINESS 99.44 99.33 97.25
FOOD** 97.31 86.37 88.79 N/A
PRIVACY, DIGNITY AND WELLBEING** 97.58 73.61 87.73 N/A
CONDITION APPEARANCE AND MAINTENANCE 90.91 92.16 91.97
Woodlands
CLEANLINESS 99.25 99.95 97.25
FOOD** 96.21 87.05 88.79 N/A
PRIVACY, DIGNITY AND WELLBEING** 97.22 86.86 87.73 N/A
CONDITION APPEARANCE AND MAINTENANCE 89.84 97.76 91.97
Northgate Hospital
CLEANLINESS 99.63 99.06 97.25
FOOD** 96.77 95.06 88.79 N/A
PRIVACY, DIGNITY AND WELLBEING** 94.71 87.38 87.73 N/A
CONDITION APPEARANCE AND MAINTENANCE 94.74 99.18 91.97
Name of meeting - Board of Directors -Pvt 18 December 2014
Version 1.0
Author: Robert Nesbitt Department: Corporate
Page 1 of 3 Date produced: 10 December 2014 Retention period: 30 years
Report To: Board of Directors – Public
Meeting Date: 18th December 2014
Title of Report: Audit and Risk Committee Chair’s Report
Action Sought: For Information
Estimated time: 5 mins
Author: Robert Nesbitt (Trust Secretary)
Director: John Brierley (Non-Executive Director)
Executive Summary
The Audit and Risk Committee met on 10th December 2014. This report highlights the issues that need to be brought to the attention to the Board of Directors.
1.0 External Audit draft plan and fees
The committee received KPMG’s draft external audit plan which sets out the objectives, methodology and scope for their work. As a result of a change in audit standards (ISA 610) EA will no longer be able to directly rely on Internal Audit’s work (although IA’s reports can still be used to inform KPMG’s understanding of the Trust as a whole). In addition to the two standard risk areas that apply to all Trusts (management override of controls and fraud risk), KPMG have identified a range of risks specific to NSFT including delivery of CIP, valuation of property and equipment, and IT systems. The risks associated with the Monitor investigation and the CQC inspection report may impact on audit plan and this will be kept under review. The scope will also cover the Quality Report and Charitable funds. The key KPMG links will remain Stephanie Beavis and Gary McLeod. The fees are, as agreed, £64.4k for core audit and £3.5k for charitable funds (excluding VAT). The final plan will be presented to the next meeting of the Committee. I have agreed to meet with the external auditors and the Director of Finance to discuss current issues.
2.0 Internal Audit reports and overall assessment
IA reported on two completed reports (non-medical clinical supervision and consultant appraisals and job planning).
2.1 The non-medical clinical supervision report outcome was ‘insufficient assurance’. This was partly because the policy was not clear and this led to confusion as to the definition of clinical supervision and its relationship to management supervision.
Date: 18 December 2014
R Item: 14.173 iv
Name of meeting - Board of Directors -Pvt 18 December 2014
Version 1.0
Author: Robert Nesbitt Department: Corporate
Page 2 of 3 Date produced: 10 December 2014 Retention period: 30 years
Practice was also very variable across the Trust. This is an issue that Dr Jane Sayer (Director of Nursing) has already identified and there is a working group which will report to Service Governance Committee in January 2015.
2.2 The consultant appraisal and job planning report outcome was ‘requires
improvement’. Again, the policy and practice in this area was unclear and as well as improving the coordination of appraisals and job planning with the register of interests it was recommended that job plan objectives should be expressed in a way that they could be measured. Dr Bohdan Solomka will take forward these recommendations.
2.3 A draft report on Remote Access- 3rd Party Support is also likely to give an opinion
of ’insufficient assurance’. 2.4 IA asked the committee to note that given the number of report outcomes so far
this year which have concluded that there has been ‘insufficient assurance’ or ‘requires improvement’ the IA opinion on the Trust is more likely to be one of ‘limited assurance’ overall.
2.5 The Committee noted the outstanding actions and progress since the last meeting.
This will be kept under review and Internal Audit will continue to remind the relevant managers.
3.0 Ligature risks The committee received a report on ligature risks and noted action to manage
these issues. Although not grounds for complacency, benchmarking with other MH Trusts shows that we have lower ligature incident levels in the context of being a high incident reporting Trust. On the Risk Register, ligature risks show as ‘12’ which the committee reviewed and considered a reasonable assessment.
4.0 Service Governance Committee Chair’s report Dr Peter Jefferys’ report highlighted a range of issues where actions have been
identified as required but where they have not been consistently implemented. This represents a significant risk to quality and safety and highlights the need for the board to insist that these issues are addressed as an imperative. The Committee believe the Board needs to consider how the governance issues raised by the Service Governance Committee are considered and how and what action is agreed. This should be addressed as part of the review of committee terms of reference and delegations to be concluded in readiness for implementation for the next financial year.
5.0 Risk Register The committee reviewed the risk register and proposed a number of amendments
and additions including the Monitor investigation and physical health. It was also suggested some of the financial related risks eg CIPs need to be higher and the bed pressure risk should be reviewed and probably increased as should the risk in
Name of meeting - Board of Directors -Pvt 18 December 2014
Version 1.0
Author: Robert Nesbitt Department: Corporate
Page 3 of 3 Date produced: 10 December 2014 Retention period: 30 years
relation to Mandatory Training. Some of the action and review dates have also been passed without update although this may be a timing issue.
6.0 Legal claims
The committee reviewed and noted the legal claims report and the potential benefits of having our in-house lawyer.
7.0 Accounts receivable The committee received the accounts receivable position. There are significant
sums outstanding in relation to a disputed S.75 payment and payments for Compass Norwich and Belton (a project that supports young people excluded from mainstream education). Actions are underway to resolve these disputes which will be monitored. The process which agreed these contracts and/ or SLAs needs to be reviewed to ensure no misunderstanding in the future for similar arrangements.
8.0 Monitor code of governance (section E remuneration) The committee reviewed and approved the stocktake of the Trust against the
code, and agreed to refer one matter (related to secondments) to the Remuneration Committee for further clarification.
9.0 Salary over-payments / Writing off of old debts The committee heard with concern, and concurred with this view, that there has
been an increase in salary overpayments largely due to management deficiencies in not completing P4 forms in a timely or accurate manner. The finance team have put into place a range of measures to address this problem. Every effort is made to recover overpayments but where there is a case for writing off such debt this has been delegated to the Director of Finance, with reporting to the A&RC continuing.
10.0 Business conduct policy It was agreed that, following some further amendments, the A&RC Chair would
take delegated action to approve the policy rather than delay release until the next meeting.
11.0 Confidential Matters One item was taken with restricted attendance on the Register of Business
Interests. The Internal Audit which reported on this item is now closed and action is continuing in respect of potential legal and disciplinary matters by the Medical Director, the Trust Secretary and the in-house lawyer.
John Brierley – Committee Chair.
Name of meeting - Board of Directors 18 December 2014
Version 0.1
Author: Graham Creelman Department: Corporate
Page 1 of 2 Date produced: 09 December 2014 Retention period: 30 years
Report To: Board of Directors – Public
Meeting Date: 18 December 2014
Title of Report: Communications Committee Chair’s Report
Action Sought: For Information
Estimated time:
Author: Graham Creelman (Non-Executive Director)
Director: Graham Creelman (Non-Executive Director)
Chair’s Report, Communications Committee, 9th December 2014 These are the key items to report from this meeting: Communications outcomes for November This main body of this report is prepared from data available before circulation of the Monitor letter and our response to staff. However the year-on-year summary information in Appendix A does incorporate analysis of media coverage of the Monitor announcement and our response. I’m pleased to say that this showed no unusual spike in negative coverage and only modest neutral coverage. This is a huge tribute both to the content of our response, the resilience of the communication strategy and the capacity of the team. Before the Monitor announcement is taken into account, there was a small increase in negative month-on-month coverage. This can be attributed to the activities of one BBC on-line journalist, and action has been taken to help him understand the issues facing the Trust, and mental health services in general. Overall, the coverage position moved from net positive to net neutral Across the month, including the Monitor letter, the Campaign had been quite balanced and more restrained in their activities. Across the year, negative coverage has been falling since June.
Since writing this report on 09 December 2014 there has been significant front page and inside coverage in the EDP of 10 December 2014 of Trust issues, specifically the financial position and out of area placements. Thought damaging, this material is balanced and fairly neutral in the way it treats the Trust – highlighting mental health services in crisis rather than ‘trust failing again’. We will not be responding on matters of fact but it is deeply disappointing that some of the stories are once again based on leaked documents as was the case with the recent press release from Chloe Smith MP Norwich North.
Media overview November was difficult overall, with considerable work in preparing our reaction to two suicides, a murder/suicide and a murder.
Date: 18 December 2014
S Item: 14.173 v
Name of meeting - Board of Directors 18 December 2014
Version 0.1
Author: Graham Creelman Department: Corporate
Page 2 of 2 Date produced: 09 December 2014 Retention period: 30 years
We issued seven proactive stories, and three reactive statements. Our Facebook profile is difficult to read, but it is interesting that the most popular Facebook post was a joint one from the UEA School of Pharmacy and the Trust about research into the importance of renal monitoring of people taking lithium (770 people reached.) This may tell us that people want hard, useful information from our Facebook presence rather than fluffier stuff. Our Twitter feed was down month-on-month, but October was very strong. The most popular tweet was a feel-good piece about the benefits of art as therapy. Again, this may be a helpful pointer towards what the Tweetosphere is looking for. There is steady growth in visits to our LinkedIn Channel which is important as this has a largely professional and engaged “readership.” Our YouTube channel (http://www.youtube.com/NSFTVChannel) is doing well, despite little promotion of new content. In the blogging arena, plans are well advanced for an official launch of the Youth Blog in January or February, and this area is very active with a Youth Blog Council set up. There has been no progress on the Dementia Blogger outreach pilot. Our external web-site shows strong growth again, with users up 18% on the 14% growth of last month. Page views are up, but the duration of visits and pages per session continue to shorten. This is not necessarily negative, as it is likely that, as people get familiar with the site, they log on to access specifically what they are looking for and then leave. Intranet access increased by circa 5% month on month, following a steep growth of circa 30% the previous month. The more interactive, responsive nature of the site is probably driving this continuing growth in engagement. The Lorenzo pages reached a milestone of over 2k new and unique users which indicates staff are looking for the information as set out in the regular weekly e-newsletter. Internal communications These proved to be pleasingly robust over the Monitor announcements and our internal response to the Foresight report. Informal feedback says that our comms were clean and clear over the Monitor announcement and staff felt informed about the Trust’s position. There was some cynicism that the tone of some announcements tended to blame those no longer with us, and to absolve the current leadership of any culpability! I think a clear message to us all is that we, the leadership in its widest sense, will be being watched very carefully. Having pledged a new start, better communication, consultation and training, we must ensure that the inevitable CIP cuts are properly contextualised and explained well in advance or creditability will be lost. Graham Creelman Non Executive Director 09 December 2014
mnews
pos/neg 11-2013 12-2013 01-2014 02-2014 03-2014 04-2014 05-2014 06-2014 07-2014 08-2014 09-2014 10-2014 11-2014 12-2014
negative - Norfolk and Suffolk NHS Foundation Trust || UK Press Coverage8.01 0.8 2.94 1.07 3.07 4.14 2.67 5.07 4.01 0.4 2.54 0.27 1.34 0.8
neutral - Norfolk and Suffolk NHS Foundation Trust || UK Press Coverage2.67 0 1.2 1.07 1.6 4.01 3.87 1.87 1.47 1.74 1.6 1.87 3.07 2.67
positive - Norfolk and Suffolk NHS Foundation Trust || UK Press Coverage1.34 0.53 0.53 1.34 2.67 2.67 2.14 2.14 6.54 4.01 4.41 2.67 2.67 0.53
Sum 12.02 1.33 4.67 3.48 7.34 10.82 8.68 9.08 12.02 6.15 8.55 4.81 7.08 4
0
1
2
3
4
5
6
7
8
9
11-2013 12-2013 01-2014 02-2014 03-2014 04-2014 05-2014 06-2014 07-2014 08-2014 09-2014
(%)
month
Norfolk and Suffolk NHS Foundation Trust || UK Press Coverage
negative - Norfolk and Suffolk NHS Foundation Trust || UK Press Coverage
neutral - Norfolk and Suffolk NHS Foundation Trust || UK Press Coverage
positive - Norfolk and Suffolk NHS Foundation Trust || UK Press Coverage
Page 1
Name of meeting - OD & W 11 December 2014
Version 0.1
Author: Brian Parrott Department: Corporate
Page 1 of 2 Date produced: Retention period: 30 years
Report To: Board of Directors – Public
Meeting Date: 11 December 2014
Title of Report: Operational Development and Workforce Committee Report
Action Sought: For Information
Estimated time:
Author: Brian Parrott (Non Executive Director)
Director: Gary Page (Chair)
Chair’s Report of OD & W Committee, 11 December 2014 Meeting chaired by Gary Page with OD&WC Chair, Brian Parrott, contributing fully from stationery train stuck between Stowmarket and Diss. Well attended meeting, including Trust Chief Executive, but except for absence of any operational management representation from Norfolk and Waveney – a concern given the priority to matters of operational staff engagement & morale. Main points of discussion / actions:
1. From last meeting Discussion 1:1 between Medical Director & Clinical NED had taken place, a note of actions required in relation to medical staff recruitment processes was now with Sarah Ball and Bohdan Solomka who agreed to progress. Will advise Committee Chair & Trust Chair if remains problematic.
2. Current Workforce Priorities
With the departure of Jane Marshall-Robb and the imminent (January) departure of Kate Coplestone, Brian Parrott had asked Kate Coplestone and Sarah Ball jointly to prepare a short paper on ‘Summary of Current Workforce Priorities’ for the Committee, and potentially also all NEDs for information. Discussion of this paper including, both Trust Chair and Chief Exec, focused on the 5 most important:
1. Staff engagement 2. Recruitment / temporary staffing 3. Appraisals 4. Sickness 5. Statutory and mandatory training:
With clear metrics produced showing reliable evidence of what progress we are making over coming months. It is important also that these metrics are all available at a 5 x Locality/3 x Specialist or Corporate service so that all can see what progress is being made. The Committee Chair has requested that the paper be made available to the whole Board as an appendix to this Chair’s report.
Date: 18 December 2014
T Item: 14.173 vii
Name of meeting - OD & W 11 December 2014
Version 0.1
Author: Brian Parrott Department: Corporate
Page 2 of 2 Date produced: Retention period: 30 years
3. Workforce Management Information Some improved performance across key indicators, including in relation to ‘5 most important’ (above) but Committee is watching, scrutinizing & encouraging. Noted that national staff survey response level had risen from 31% to 35%. .
4. Staff Engagement As above, plus noted that Locality Managers will be invited in succession to future OD&WC meetings to ‘bring their staff engagement and wider workforce plans to life and provide more detailed assurance about plans, progress and challenges.’ Chair proposes beginning with West Norfolk and West Suffolk.
5. Statutory & Mandatory training Concerns continue in number of areas – important practice training expectations not being met, variable across localities/services, even if for some understandable. Suffolk CCGs have requested a focus on safeguarding, mental capacity act and deprivation of liberties safeguards; Norfolk CCGs sought assurance that templates for access & assessment, community and crisis resolution/home treatment are set correctly. Important for Leigh Howlett and Jane Sayer in new roles to take fresh training overview – priorities, proportionality etc.
6. Equalities and Diversity The committee received an update report on progress against equality delivery system objectives. Both Ravi Seenan and Robert Nesbitt attended. Several good initiatives with partners across the Trust. Concerns about absence of some identified equality leads required and evidence of training not done. Discussion not just about maximizing training completion (measured) with the actual impact it has and what changes in behaviour and culture as a result (not measured). It was agreed that Equality and Diversity training should be more than a one off event. Leigh and Robert to discuss options and bring back to Committee. It was also agreed that BME Staff from the Norvic would be invited to present to the Board given recent concerns expressed.
7. Performance Appraisals Very substantial progress particularly in some localities/services (90-100%). To be applauded. Others still at 50-60% need improvement. The Committee & Trust Board will need to have early 2015 discussions about what to do with pay increments where appraisals have not been completed. It is a risk area for the Trust, including in relation to staff engagement. Important item for first 2015 Committee.
8. East of England Deanery Visit Visit took place on 5 November – no surprises to Trust or critical concerns for immediate action. Agreed Committee will discuss medical workforce issues in full at next meeting, including with Dr Stephen Jones, Core Programme Director.
Brian Parrott Gary Page NED and OD & W Committee Chair Trust Chair and Chair of
meeting
Board of Directors – Public 18Dec2014 RemToS Chair’s report
Version 1.0 Author: Robert Nesbitt Department: Corporate
Page 1 of 2 Date produced: 08Dec2014 Retention period: 30 years
Report To: Board of Directors – public
Meeting Date: 18th December 2014
Title of Report: Remuneration and Terms of Service Committee Chair’s report, and joint meeting of RemToS and Nominations Committee Chair’s report
Action Sought: For information (RemToS ToR for approval)
Estimated time: 5 minutes
Author: Robert Nesbitt: Trust Secretary
Director: Gary Page: Chair
Executive Summary:
The Remuneration and Terms of Service Committee (RemToS) met on 01.12.14 and considered the Clinical Excellence Awards, the Director of Operations (Suffolk) appointment and its Terms of Reference. This meeting was then followed by the annual joint meeting between the RemToS and Nominations committee which considered the Foresight Partnership external board evaluation. This report summarises the key points and decisions.
1.0 RemToS committee meeting 01.12.14
1.1 The committee reviewed the recommendations for the clinical excellence awards which are a nationally mandated requirement. The quality of applications was good and the recommendations were approved.
1.2 The committee noted the extensive stakeholder involvement in the recruitment process for the Director of Operations for Suffolk and formally appointed Alison Armstrong who will start in January 2015.
1.3 An updated set of terms of reference were agreed by the committee and are presented now for approval by the Board.
2.0 Annual Joint RemToS / Remuneration committee meeting 01.12.14
2.1 The joint meeting considered the Foresight Partnership external board evaluation. Monitor’s code of governance requires that FTs periodically engage an external provider to ensure that there is an independent view of the board of directors’ performance. It was recognised that whilst service user and carer governors were
Date: 18th
December 2014
U Item: 14.173viii
Board of Directors – Public 18Dec2014 RemToS Chair’s report
Version 1.0 Author: Robert Nesbitt Department: Corporate
Page 2 of 2 Date produced: 08Dec2014 Retention period: 30 years
invited to participate in the focus groups it would have been preferable for a wider range of service users and carers to be involved in the process.
2.2 As Foresight Partnership were unable to attend the joint meeting, a telephone conference call had taken place with those members of the Nominations Committee who were available. This provided a briefing for governors on the evaluation outcomes.
2.3 The Foresight report listed six priority areas and the joint committee meeting reviewed the action plan. It was noted that the membership of the board had changed somewhat since the evaluation earlier this year. Consideration will be given to inviting Foresight Partnership back in approximately six months to assess progress on the priority areas.
3.0 Recommendations
3.1 That the Board of Directors notes the above points and approves the revised RemToS terms of reference.
Robert Nesbitt Trust Secretary 08.12.14
Appendix 1 – RemToS revised Terms of Reference
Terms of Reference 14Mar08: Reviewed 7Sept09, Reviewed 27Jan2011. Reviewed 03Dec2012. Approved by BoD 22Dec2012, Approved BoD 15Jan2014 Page 1 of 6
Remuneration & Terms of Service Committee (RemToS)
Terms of Reference
1.0 Authority
1.1 The RemToS committee is constituted as a standing committee of the Trust’s board of directors.
1.2 The RemToS committee is authorised to act within its terms of reference in order to identify and appoint candidates for all executive director positions, and to determine their remuneration and terms of service.
1.3 The RemToS committee is authorised by the board of directors to instruct professional advisors and to request the attendance of individuals from outside the Trust with relevant skills and expertise in order to exercise its functions.
1.4 The RemToS committee is authorised to obtain such internal information it needs to fulfil its functions. All members of staff are directed to cooperate with any such request made by the RemToS committee.
1.5 When appointing the chief executive, the committee shall be the committee described in Schedule 7, 17(3) of the NHS Act (2006) (the Act). When appointing other executive directors the committee shall be the committee described in Schedule 7,17(4) of the Act.
2.0 Supporting Principles
2.1 Where Executive Directors or Senior Managers are involved in advising the Remuneration & Terms of Service Committee, care must be taken to avoid conflict of interests.
2.2 The Remuneration & Terms of Service Committee will work with the Board of Governors (Nominations Committee) in evaluating the skills, knowledge and experience of the whole Board and regularly review the structure, size and composition of the whole Board. At least annually a joint meeting will be held between the Remuneration and Terms of Service Committee and the Nominations Committee.
2.3 In all its work the RemToS committee will adhere to relevant laws, regulations and Trust policies, and will take into account best practice.
3.0 Appointments role
3.1 The RemToS committee will regularly review the structure, size and composition (skills, knowledge, experience and diversity) of the board, acting on the output of the board evaluation process as appropriate and making recommendations to the board of directors or board of governors, as applicable, as to any changes.
3.2 The RemToS committee will consider and make plans for succession planning for the chief executive and other executive directors, taking into account the challenges and
Date: 18 Dec 2014
U Item: 14.173viii App 1
Terms of Reference 14Mar08: Reviewed 7Sept09, Reviewed 27Jan2011. Reviewed 03Dec2012, Reviewed 16Dec2013, Reviewed 01Dec2014 Page 2 of 6
opportunities facing the organisation and the balance of skills and expertise needed on the board for the future.
3.3 The RemToS committee will keep the leadership needs of the Trust under review at executive level to ensure the continued ability of the Trust to operate effectively in the health and social care economy.
3.4 The RemToS committee is responsible for identifying and appointing candidates to fill posts within its remit.
3.5 When a vacancy arises, the RemToS committee will evaluated the requirements of the board and prepare or update a job description and person specification setting out the requirements for the appointment.
3.6 The RemToS committee may use recruitment consultants to facilitate the search for suitable candidates but will always advertise the vacancy publicly.
3.7 Throughout the recruitment process candidates will be considered on their merits against objective criteria derived from the needs of the Trust.
3.8 Should an executive director candidate have significant commitments, these will be disclosed to the RemToS committee before appointment, and any changes will be reported to the board of directors as they arise.
3.9 Should an executive director candidate have any past, current or known future business interests that may give rise to a conflict of interest (or a perception of a conflict of interest) then these will be disclosed to the RemToS committee before an appointment is made. Any changes to interests will be reported to the board of directors as they arise.
3.10 In the case of any matter related to an executive director being suspended, or having their service terminated, then the RemToS committee will consider this matter, subject to any legal provision and the individual’s employment contract.
4.0 Remuneration role
4.1 The RemToS committee will establish a remuneration policy in respect of executive directors, and any senior managers on locally determined pay below board level, and keep this under review. As part of this policy the committee will consult with the chief executive over proposals related to the remuneration of other executive directors.
4.2 The scope of the remuneration policy will include:
Salary, including performance related pay or bonus payments if applicable,
Provision for other benefits including pensions and cars,
Allowances
Payable expenses
Compensation payments
4.3 An underlying principle of this policy will be to establish sufficient levels of remuneration so as to attract and motivate executive directors of the required quality to lead the Trust, without paying more than is necessary for this purpose, and at a level affordable for the organisation. In doing so, the RemToS committee will draw on national guidance and market benchmarking analysis in any determination of executive director pay (and any senior managers on locally determined pay). The RemToS committee will ensure that no director or senior manager on locally determined pay
Terms of Reference 14Mar08: Reviewed 7Sept09, Reviewed 27Jan2011. Reviewed 03Dec2012, Reviewed 16Dec2013, Reviewed 01Dec2014 Page 3 of 6
receives an increase in remuneration where the Trust or the individuals’ performance does not justify such an increase. The RemToS committee will take into account and be sensitive to the pay and conditions of staff in the wider Trust in setting the remuneration policy and in making specific decisions based upon it.
4.4 The RemToS committee will monitor and assess the performance appraisal of individual executive directors and consider this information when reviewing changes to remuneration packages.
4.5 The RemToS committee will oversee contractual arrangements for executive directors (including termination payments) so as to avoid rewarding poor performance.
5.0 Membership and Quoracy
5.1 The RemToS committee shall consist of the Chair of the Board of Directors and all Non-Executive Directors. The Trust Chair will chair the committee.
5.2 The chief executive shall be a member of the RemToS committee for the purpose of appointing executive directors (other than the chief executive).
5.3 Four members of the RemToS committee, including the Chair, shall constitute a quorum.
5.4 Only members of the RemToS committee have a right to attend meetings.
5.4 The composition of the Remuneration & Terms of Service Committee shall be recorded in the Annual Report.
6.0 Attendance
6.1 The Chief Executive is invited to all meetings.
6.2 The Director of OD and WF, or other managers may be asked to attend.
6.3 The RemToS committee may invite representatives of the Nominations Committee to attend meetings.
6.4 Any member of the committee, including the Trust Secretary, will be required to leave the committee when their own remuneration or terms of service are the subject of discussion.
7.0 Secretariat support
7.1 The Trust Secretary, or their nominated deputy, shall be responsible for minuting meetings and providing administrative support to the RemToS committee.
7.2 The Trust Secretary will arrange with HR for the completion of payroll documentation following decisions made by the RemToS committee.
8.0 Reporting
8.1 The Chair will report to the board of directors following each meeting.
8.2 Minutes of the RemToS committee shall normally be reserved to members of the Committee.
8.3 The RemToS committee will ensure that disclosure of executive director remuneration is included in the Trust’s Annual Report in line with reporting requirements.
Terms of Reference 14Mar08: Reviewed 7Sept09, Reviewed 27Jan2011. Reviewed 03Dec2012, Reviewed 16Dec2013, Reviewed 01Dec2014 Page 4 of 6
9.0 Frequency of meeting
9.1 The RemToS committee will meet at least two times a year. Meetings may be called as required.
10 Review
10.1 These Terms of Reference shall be reviewed annually, unless otherwise required.
10.2 The performance of the RemToS committee will be reviewed as part of the annual board performance review process, taking into account these Terms of Reference.
Robert Nesbitt
17.11.14
Terms of Reference 14Mar08: Reviewed 7Sept09, Reviewed 27Jan2011. Reviewed 03Dec2012, Reviewed 16Dec2013, Reviewed 01Dec2014 Page 5 of 6
Appendix I Extract from the Monitor NHS Foundation Trust Code of Governance (March 2010) E. Director remuneration E.1 The level and make-up of remuneration Main principle Levels of remuneration should be sufficient to attract, retain and motivate directors of the quality required to run the NHS foundation trust successfully, but an NHS foundation trust should avoid paying more than is necessary for this purpose. Supporting principles The remuneration committee should decide if a proportion of executive directors’ remuneration should be
structured so as to link reward to corporate and individual performance. The remuneration committee should judge where to position its NHS foundation trust relative to other NHS foundation trusts and comparable organisations. Such comparisons, however, should be used with caution in view of the risk of an upward ratchet of remuneration levels with no corresponding improvement in performance.
The remuneration committee should also be sensitive to pay and employment conditions elsewhere in the NHS foundation trust, especially when determining annual salary increases.
Code provisions Remuneration policy E.1.1 Any performance-related elements of the remuneration of executive directors should be designed to align
their interests with those of patients, service users and taxpayers and to give these directors keen incentives to perform at the highest levels. In designing schemes of performance-related remuneration, the remuneration committee should follow the following provisions:
(i) The remuneration committee should consider whether the directors should be eligible for annual bonuses. If so, performance conditions should be relevant, stretching and designed to match the long term interests of the public and patients.
(ii) Payouts or grants under all incentive schemes should be subject to challenging performance criteria reflecting the objectives of the NHS foundation trust. Consideration should be given to criteria which reflect the performance of the NHS foundation trust relative to a group of comparator trusts in some key indicators, and the taking of independent and expert advice where appropriate.
(iii) Performance criteria and any upper limits for annual bonuses and incentive schemes should be set and disclosed.
(iv) The remuneration committee should consider the pension consequences and associated costs to the NHS foundation trust of basic salary increases and any other changes in pensionable remuneration, especially for directors close to retirement. In general, only basic salary should be pensionable.
E.1.2 Levels of remuneration for the chairman and other non-executive directors should reflect the time
commitment and responsibilities of their roles. E.1.3 Where an NHS foundation trust releases an executive director, for example to serve as a non-executive
director elsewhere, the remuneration disclosures of the annual report should include a statement on whether or not the director will retain such earnings.
Service contracts and compensation E.1.4 The remuneration committee should carefully consider what compensation commitments (including
pension contributions and all other elements) their directors’ terms of appointment would give rise to in the event of early termination. The aim should be to avoid rewarding poor performance. In an early termination, compensation should be reduced to reflect a departing director’s obligation to mitigate loss.
Terms of Reference 14Mar08: Reviewed 7Sept09, Reviewed 27Jan2011. Reviewed 03Dec2012, Reviewed 16Dec2013, Reviewed 01Dec2014 Page 6 of 6
E.2 Procedure Main principle There should be a formal and transparent procedure for developing policy on executive remuneration and for fixing the remuneration packages of individual directors. No director should be involved in deciding his or her own remuneration. Supporting principles The remuneration committee should consult the chairman and/or chief executive about its proposals
relating to the remuneration of other executive directors.
The remuneration committee should also be responsible for appointing any independent consultants in respect of executive director remuneration.
Where executive directors or senior management are involved in advising or supporting the remuneration committee, care should be taken to recognize and avoid conflicts of interest.
Code provisions E.2.1 The board of directors must establish a remuneration committee composed of non- executive directors
which should include at least three independent non-executive directors. The remuneration committee should make available its terms of reference, explaining its role and the authority delegated to it by the board of directors. Where remuneration consultants are appointed, a statement should be made available of whether they have any other connection with the NHS foundation trust.
E.2.2 The remuneration committee should have delegated responsibility for setting remuneration for all
executive directors, including pension rights and any compensation payments. The committee should also recommend and monitor the level and structure of remuneration for senior management. The definition of senior management for this purpose should be determined by the board but should normally include the first layer of management below board level.
E.2.3 The board of governors is responsible for setting the remuneration of non-executive directors and the
chairman. The board of governors should consult external professional advisers to market-test the remuneration levels of the chairman and other non-executives at least once every three years and when they intend to make a material change to the remuneration of a non-executive.
Name of meeting - Public Board of Directors 18.12.14 Chair of Charitable Funds Committee Report
Version 0.1
Author: Graham Creelman Department: Corporate
Page 1 of 2 Date produced: 09 December 2014 Retention period: 30 years
Report To: Board of Directors – Public
Meeting Date: 18 December 2014
Title of Report: Charitable Funds Committee Report (08 December 2014)
Action Sought: For information
Estimated time:
Author: Graham Creelman (Non-Executive Director)
Director: Graham Creelman (Non-Executive Director)
Chair’s report, Charitable funds. Monday 8th December, Ipswich Executive Summary: Key Points: Beccles Hospital Fund There was disappointing news that it is not possible for the Trust to return the Beccles hospital fund to either GY and W CCG or to Health East, the social enterprise which was the old PCT’s provider arm. The Beccles fund is administered by the Trust on behalf of the old PCT. It has proved impossible in the past for the committee to approve proposals to use the fund (£1.25million) because of revenue implications which were unacceptable to the commissioners. The NSFT board agreed at its last meeting that it would be appropriate to return the fund to the CCG/Health East as they were closer to the needs of the hospital, and might be better able to find innovative solutions. Kate Gill, of Great Yarmouth and Waveney CCG, reported that she had been advised by their auditors that the CCG could not hold these legacy moneys, and that the CCG thought it inappropriate that money should go to Health East to administer. This view was echoed by the NSFT lawyer, Maeve Heaney, who reported that it was not possible to transfer the money to Health East, as it was not an NHS body, and transfers of funds like these to non-NHS bodies were forbidden by NHS England. In the light of this stalemate, the committee decided to invite representatives of the hospital to attend future charitable guns meetings to discuss non-revenue possibilities, and the Sue Whiffen and I would visit the hospital in January to explain the situation.
Date: 18 December 2014
V Item: 14.173 ix.
Name of meeting - Public Board of Directors 18.12.14 Chair of Charitable Funds Committee Report
Version 0.1
Author: Graham Creelman Department: Corporate
Page 2 of 2 Date produced: 09 December 2014 Retention period: 30 years
Recharging of Administrative Costs for legacy funds This has been partially accomplished, but a representative of Ipswich and East Suffolk CCG, Roger Holt, reported that his board had not agreed to the request,as applications for the funds would come from employees of Serco for their community patients. It was agreed that Kathy Walsh would speak to Roger outside of the meeting to discuss possible ways forward. Fund quarterly income and expenditure Total expenditure for second quarter of 2014 was £35,962, slightly less than the previous quarter. Requests remain steady for Norfolk and Suffolk, although there has been little overall movement in income and expenditure Total balance of all funds on 30th September was £1,793,054, of which 74% (the Beccles hospital bequest) is attributable to Great Yarmouth and Waveney CCG, as successors to the PCT. Annual Accounts The committee agreed to recommend approval of the annual accounts to the Trustee, subject to some non-material amendments. Release of small funds The committee passed a resolution to release into general funds two small restricted funds the purpose of which were now unclear. The Charity Commission have told us that, in fit ire, we do not need their permission to free up funds of under £10,000 the original intention of which is either unclear or no longer valid. This ruling will now be applied to other such small funds we hold. South Suffolk Club House Included among charitable funds is £10,000 for the South Suffolk Club House project. This is a scheme to help those with mental health issues back into employment. The Club House no longer exists, and there have been no recent request to use the fund. It was agreed that the £10,000 should be absorbed into general unrestricted funds, with a note to those still concerned with the original intention that they were free to apply at any time for help from general funds. Graham Creelman