Lymphatic tissue. Components of lymphoid system Lymph and lymph nodes Lymph – fluid scavenged...
-
Upload
bryan-marshall -
Category
Documents
-
view
245 -
download
2
Transcript of Lymphatic tissue. Components of lymphoid system Lymph and lymph nodes Lymph – fluid scavenged...
Components of lymphoid system
Lymph and lymph nodes Lymph – fluid scavenged from the intersitium Collected in thin walled lymphatic vessels Returned to general circulation Contains leukocytes Filtered through small specialized organs (lymph
nodes)
Lymph
Capillaries lose 2-4 L of fluid and plasma protein
Lymphatic system absorbs excess fluid and returns it to the bloodstream Makes sure circulatory system has enough blood
to work properly Decreases edema
Lymph– Clear colorless fluid—like plasma Less proteins Has bacteria, virus, cell debris Lipid content high Lymphocytes content high Many in capillary bed
Lymphatic vessels Take fluid from tissue back to the bloodstream—veins Usually along side of vein Similar to vein (low pressure, use SK muscle and
respiratory pump to help flow, valves also)
Lymphoid Cells
The two main varieties are T cells and B cells Both types originate from stem cells in bone
marrow T cells – cell mediated immunity B cells – humoral/ antibody mediated immunity Small and large lymphocytes in peripheral blood Large are the activated B lymphocytes Antigen – anything the body perceives as foreign
Bacteria and their toxins; viruses Mismatched RBCs or cancer cells
Lymphocytes T cells
Manage the immune response Attack and destroy foreign cells
B cells Produce plasma cells, which
secrete antibodies Plasma cells are derived from
activated B lymphocytes that have left the blood stream and taken up residence in connective tissue. SPOKE wheel appearance
Antibodies immobilize antigens
Other Lymphoid Cells
Macrophages – phagocytize foreign substances and help activate T cells
Dendritic cells – spiny-looking cells with functions similar to macrophages
Reticular cells – fibroblast like cells that produce a stroma, or network, that supports other cell types in lymphoid organs
Lymphoid Tissue Lymphatic follicles
(nodules)
Solid, spherical bodies consisting of tightly packed reticular elements and cells
Have a germinal center composed of dendritic and B cells
Found in isolation and as part of larger lymphoid organs
Introduction Lymphoid system consists of cells, tissues
& organs that contain aggregates of lymphocytes.
The lymphoid organs are:
1. Primary lymphoid organs – bone marrow & thymus
2. Secondary lymphoid organs – lymph nodes, spleen, tonsils, Peyer’s patches, MALT (mucosa associated lymphoid tissue)
Lymphoid Organs
Central
ThymusBone marrow
SpleenLymphoid nodesSolitary nodulesTonsilsAppendixPeyer’s patches
Peripheral
Origin and main differentiation
Proliferation and additional differentiationImmune response
Thymus
A bilobed organ that secrets hormones (thymosin and thymopoietin) that cause T lymphocytes to become immunocompetent
The size of the thymus varies with age In infants, it is found in the inferior neck and extends
into the mediastinum where it partially overlies the heart
It increases in size and is most active during childhood It stops growing during adolescence and then
gradually atrophies
Thymus The thymus differs from other lymphoid organs in important
ways It functions strictly in T lymphocyte maturation It does not directly fight antigens
Function: production of immunocompetent T lymphocytes production of mature but naïve T cells for peripheral
tissues and circulation immunological self-tolerance regulation of T cell maturation, proliferation and function
via secretion of hormones
Internal Anatomy of the Thymus Thymic lobes contain an
outer cortex and inner medulla
The cortex contains densely packed lymphocytes and scattered macrophages
The medulla contains fewer lymphocytes and thymic (Hassall’s) corpuscles
Thymic Cortex Consists of proliferating
lymphocytes dispersed among macrophages & epithelial reticular cells.
These epithelial cells/ reticular cells form the support structure for the developing T cells but also play an important role in isolating the T cells from foreign anitgens during their development
They are of endodermal origin & do not secrete reticular fibers.
Epithelial Reticular Cells
Endodermally derived. Stellate eosinophilic cells with an oval nucleus. Joined to adjacent reticular cells by desmosomes. Enclose the developing lymphocytes within them. Help in the formation of a blood-thymus barrier - prevents
antigenic stimulation of the lymphocytes & allows for proper differentiation.
Secrete various hormones (thymulin, thymopoietin, thymosin & thymic humoral factor) that regulate T cell differentiation.
Blood Thymus barrier Prevents premature exposure of lymphocytes to
antigen (to inhibit tolerance). The integrity of the space within the epithelial cell
framework is extremely important because it prevents the premature stimulation of T cells by antigens
Non-fenestrated endothelium with occluding junctions (major component of the barrier) Endothelium Thick basal lamina Pericytes Macrophages Type I epithelioreticular cells
Thymic Cortex
Contains maturing lymphocytes, macrophages & reticular cells.
Many lymphocytes die by apoptosis & are removed by macrophages.
Outer cortex is populated by immature lymphocytes & as they mature they migrate to the deeper part of the cortex.
Maturation of T cell in thymus • First T cell has to
acquire markers CD4 and CD8
• Cell without marker is destroyed
Epithelio reticular cell
(RE)
MHC I
MHC II
RE cell teaches the immature T cell to recognize the MHC markers
Some identify MHC I and some MHC II
T cell who don’t learn to identify either are destroyed
Immature T cell
CD4 CD8
Immature T cell
CD4 CD8
MHC I
Immature T cell
CD4 CD8
MHC II
MEDULLA
CORTEX
T cells that recognize MHC I are destroyed or they lose CD4 from their surface
CD4 +ve
T cell
CD8 +ve
T cell
Thymic Medulla
Hassall’s corpuscles concentrically arranged, flattened epithelial reticular cells that become filled with keratin filaments, degenerate & may become calcified.
They appear in the fetus & their number gradually increases after birth.
QUESTION
The production of new T lymphocytes in the thymus occurs in which of the following regions?
A. Superficial cortex
B. Corticomedullary junction
C. Thymic nodules
D. Deep medulla
E. Thymic corpuscles
Lymph Node
A filter: purifies lymph before return to venous circulation
Removes: debris pathogens 99% of antigens
Initiation of immune response Activation & proliferation of lymphocytes
Function of lymph nodes
filter debris and microorganisms via phagocytosis by fixed macrophages
facilitate the interaction between antigen presenting cells and circulating lymphocytes to initiate an immune response
B lymphocytes: activation and proliferation; plasma cell formation and antibody production in response to antigens
T lymphocytes: activation to become T helper and T cytotoxic cells
Lymphnode structure
Afferent vessels – convey lymph towards the node
Efferent vessels – drain lymph away from the node at the hilum
Capsule Trabeculae Reticular tissue
Structure of a Lymph Node (Cortex) Superficial cortex: The cortex contains follicles with
germinal centers, heavy with dividing B cells
Dendritic cells nearly encapsulate the follicles
Deep cortex houses T cells in transit
T cells circulate continuously among the blood, lymph nodes, and lymphatic stream
Lymphoid follicle
Germinal Center (GC) - contains pale-staining cells. The open, pale-staining nature of the nuclei of these cells indicate that they are B lymphocytes undergoing active proliferation.
Other cells include: Follicular dendritic cells that present antigen to the B cells Macrophages that engulfed dead B cells that have died by apotosis
Lymphoid follicle cortex
Germinal center - Functional aspects: resting B cells enter the lymph node parenchyma though the high
endothelial venules and if they encounter an antigen with which they can react, they then enter the cycle of blast transformation to produce clones of plasma cells and B memory cells.
This production of clones occurs in the germinal centers of lymphoid follicles.
Mantle zone (corona) – The germinal center is surrounded by a ring of darker-staining cells. The
condensed nature of their nuclei indicates that these are resting B cells. Also present in the mantle zone are T helper cells, macrophages and dendritic cells.
Paracortical zone / deep cortex Paracortical zone - deeper regions of the cortex contain primarily T
lymphocytes that do not form into follicles. T lymphocytes (helper and cytotoxic/suppresor) arrive through the circulation, enter the
lymph node parenchyma through the high endothelial venules and take up residence in the paracortical zone.
If activated, the T lymphocytes undergo active proliferation to produce expanded clones of activated T lymphocytes.
Functional aspects: T lymphocytes that arrive at the lymph node via the arterial blood stream gain access to the
parenchyma of the lymph node through the wall of the high endothelial venules located in the paracortical zone.
These blood vessels contain endothelial cells that are expressing specific lymphocyte binding molecules called addressins.
These surface molecules are available to bind to lymphocytes that recognize them, the lymphoctyes bind to the surface of the endothelium, then cross the vessel wall and enter the lymph node parenchyma.
Homing of lymphocytes
A process by which lymphocytes return to lymph node by crossing walls of blood vessels, High endothelial venules- present in lymph nodes.
Lymph node architecture
• HEV – specializedPost-capillary venules.
• Cuboidal endothelium
• Concentrates lymph
• Receptors for antigenprimed lymphocytes
*HEV- High endothelial venules
Structure of a Lymph Node (Medulla) Medullary cords extend from the cortex and contain B cells, T cells,
and plasma cells The medullary cords are composed of plasma cells producing antibodies, their
precursors, macrophages and T helper cells. The most prominent cell in the cord is the precursor to plasma cells or
immunoblasts that came from the germinal centers of the lymphoid follicles in the cortex of the node.
In the medullary cords, the plasma cells undergo final maturation and secrete antibodies into the lymph that is collected by efferent lymphatic vessels in the node and eventually carried to the general circulation. Plasma cells may also get into the general circulation in this manner
The medullary sinuses are composed primarily of reticular fibers (RF) providing the support framework, reticular cells (fibroblast-like cells that secrete the reticulin) (RC)
and macrophages.
Structure of a Lymph Node (Medulla)
Lymphatic Disorders: Elephantiasis: parasite, roundworm
Lives in lymph nodes Prevents fluid flow back to circulatory system Chronic edema (fluid swelling) Leads to thickening of skin
Autoimmune diseases Failure of self tolerance Immune system fails to recognize self antigens from foreign ones
and attacks body’s own tissuese.g Lupus
Young women more impacted usually Autoimmune disease against DNA
Part of the circulatory system with secondary immune system function
Functions Reserve blood storage Removal of aged cells Immune-surveillance (hematogenous exposure
to antigens) Filters particulates from the blood (secondary to
hepatic filter)
Spleen
Structure of the Spleen
Fibrous capsule Trabeculae that extend inward and contains lymphocytes,
macrophages, and huge numbers of erythrocytes Two distinct areas of the spleen are:
White pulp : area containing mostly lymphocytes suspended on reticular fibers and involved in immune functions
Red pulp : remaining splenic tissue concerned with disposing of worn-out RBCs and bloodborne pathogens
Spleen – Capsule Collagenous connective tissue
Smooth muscle (most prominent in ruminants and horses) Allows contraction of the spleen
Large network of septa/trabeculae Septa are framework through
which vessels reach interior of spleen
Delicate reticular stroma
White Pulp – lymphiod Tissue
Periarteriolar lymphoid tissue (PALS) Central artery coated by
sheath of lymphocytes Forms nodular lymphoid
tissue Has germinal centers Supported by a fine
specialized stroma
White pulp
The white pulp of the spleen is characterized by a parenchyma that consists of two types of lymphocytes, i.e., B cells and T cells located in two different areas of the spleen.
B cells are located in the lymphoid follicles scattered throughout the organ. In younger animals, a germinal center can be seen as seen in lymph nodes. In fact, this type of white pulp functions much in the manner that lymphoid follicles of lymph nodes function, i.e., initiation of immune responses by B cells to foreign antigens in the blood. T cells are located around the central arteries and form a kind of sheath. This site is called the periarteriolar lymphoid sheath.
In the micrograph above, white pulp of the spleen is seen in both locations: (1) a lymphoid follicle, outlined by the dashed line and (2) the PALS located around the central artery in which T cells are found. The lymphoid follicle has a pale-staining germinal center (GC) in which B cells are proliferating. Note the presence of a mantle zone (ManZ) that contains small lymphocytes and an outer marginal zone that contains larger lymphocytes that are less densely packed than cells in the mantle zone. Outside the marginal zone is the red pulp.
In the micrograph above, white pulp of the spleen is seen in both locations: (1) a lymphoid follicle, outlined by the dashed line and (2) the PALS located around the central artery in which T cells are found. The lymphoid follicle has a pale-staining germinal center (GC) in which B cells are proliferating. Note the presence of a mantle zone (ManZ) that contains small lymphocytes and an outer marginal zone that contains larger lymphocytes that are less densely packed than cells in the mantle zone. Outside the marginal zone is the red pulp.
Splenic follicle
Same structure as cortical follicle in lymph node. Germinal center Mantle zone Marginal zone
Form adjacent to PALS.
Splenic Cords and Sinuses
Make up the red pulp Venous sinuses
Lined by phagocytic endothelial cells Contain circulating blood
Cords are all the tissue inbetween Contain RBCs, macrophages, lymphocytes, occasional
neutrophils Site where filtering function occurs High number of nuclei compared to the sinuses
Red pulp
The red pulp of the spleen is characterized by a parenchyma (PN) that consists of macrophages of the sheathed capillaries as well as other macrophages and blood cells. Occupied by numerous venous sinuses (VS).
Sinuses are very open and can be easily traversed by blood cells. Their lining consists of long endothelial cells (arrows) oriented along the longitudinal axis of the vessel.
Large spaces occur between adjacent endothelial cells and the underlying basement membrane is discontinuous, thus blood cells can easily pass between the endothelial cells and gain access to the bloodstream on the venous side.
Few fibroblasts responsible for producing the reticulin fibers; special stains are required to visualize the reticular network.
Splenic Macrophages
Part of the MPS (macrophage phagocytic system)
Primary function is removal of “senescent” cells
Some are also antigen presenting cells (dendritic cells)
Lymphoid Tissue (Unencapsulated)
Diffuse lymphatic tissue
Scattered reticular tissue in every body organ Larger collections in the lamina propria of mucous
membranes and lymphoid organs Mucosal associated lymphoid tissue (MALT) Gut-associated (GALT) Bronchial-associated (BALT)
Tonsils
Simplest lymphoid organs; form a ring of lymphatic tissue around the pharynx
Location of the tonsils Palatine tonsils – either side of the posterior end of the oral
cavity Lingual tonsils – lie at the base of the tongue Pharyngeal tonsil – posterior wall of the nasopharynx Tubal tonsils – surround the openings of the auditory tubes
into the pharynx
Tonsils
Lymphoid tissue of tonsils contains follicles with germinal centers
Tonsil masses are not fully encapsulated Epithelial tissue overlying tonsil masses invaginates,
forming blind-ended crypts Crypts trap and destroy
Aggregates of Lymphoid Follicles
Peyer’s patches – isolated clusters of lymphoid tissue, Found in the wall of the distal portion of the small intestine
(Ileum) Similar structures are found in the appendix
Appendix: Destroy bacteria, preventing them from breaching the
intestinal wall Generate “memory” lymphocytes for long-term immunity
MALT
MALT – mucosa-associated lymphatic tissue is composed of: Peyer’s patches, tonsils, and the appendix
(digestive tract) Lymphoid nodules in the walls of the bronchi
(respiratory tract)
MALT protects the digestive and respiratory systems from foreign matter
Types of MALT and Functional aspects: larger aggregates function much like lymph nodes
smaller, scattered MALT are mostly T lymphocytes but also have B cells and plasma cells - mostly IgA in the intestines and respiratory tract to protect against pathogens that may gain access to underlying tissues - IgG and IgM secreted into lamina propria to counteract pathogens that have gained access to connective tissue - IgE secreted into lamina propria; mediates the release of histamine from mast cells
single lymphocytes found within the lamina epithelial are mostly T lymphocytes
MALT is drained by efferent lymphatic's but there are no afferent lymphatic's
lymphocytes exposed in MALT regions go through regional lymph nodes then return to the MALT region after activation
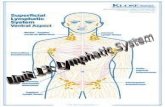
Organs of the Lymphatic System Thymus
Houses developing lymphocytes Secretes hormones that regulate lymphocyte activity Shrinks with age
Lymph nodes Concentrated near ear, mandible, neck, armpit, breasts, trachea, aorta, iliac crest, groin Filter lymph, cleanse foreign matter Remove impurities from fluid before return to blood
Spleen Many RBC, lymphocytes, macrophages Produces blood cells Blood reservoir Destroys old and bad RBC Filter like lymph nodes If removed, functions taken over by liver and bone marrow
Tonsils Deal with ingested, foreign, inhaled pathogens Many lymphocytes in tonsils
Q 2
Macrophages are directly involved in immune responses in which ofthe following ways?a. Production of IL-2b. Presentation of antigenc. Specific killing of tumor cellsd. Production of antibodiese. Inactivation of helper T cells
Q 3The mechanism for lymphocyte circulation from the lymphoid compartmentin the region marked with the asterisk to the blood involveswhich of the following?
A. Homing receptors on lymphocytes that recognize vascular addressins on high endothelial venule cellsB. Lymphocyte binding to endothelial integrins followed by passage through endothelial cells lining the high endothelial postcapillary venulesC. Lymphocyte passage through the zonulae occludentes by diapedesis after dissolution of the junctions by proteolytic enzyme releaseD. Lymphocyte passage from the efferent lymphatic vessel to the thoracic duct and subsequently the venous systemE. Passage of lymphocytes through the discontinuous sinusoidal wall into the blood
This organ, shown at low magnification (A) and high magnification (B) is which of the following?
Q 4