Lp 14 digestive system 2009
-
Upload
kirstyn-soderberg -
Category
Documents
-
view
161 -
download
0
description
Transcript of Lp 14 digestive system 2009

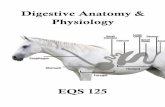
Digestive System
VTT 235/245 Anatomy & Pathology Lab

Introduction
The digestive system consists of: **A tube that runs from the mouth to
the anus. Accessory digestive organs that aid in
the process of digestion and absorption of nutrients.
The accessory organs are: Salivary glands The liver The pancreas

Functions
Prehension (grasping of food) Mastication Chemical digestion Absorption of nutrients and water Elimination of wastes

Oral Cavity
Mechanical digestion- chewing, breaking food down into smaller particles to increase the surface area available for exposure to enzymes involved in chemical digestion.

Oral Cavity…
Digestive enzymes are proteins that promote (catalyze) the chemical reactions that split complex food molecules into simpler compounds.
The addition of saliva helps moisten, soften, and shape food into a form that is more easily swallowed.
Salivary amylase breaks down amylose, a sugar component of starch.
Lipase, an enzyme that digests lipids (fats) can also be found in the saliva of some species.

Oral Cavity…
The salivary glands are controlled by the autonomic nervous system.
Stimulation of the parasympathetic division results in increased salivation.

Peristalsis
The contents of the digestive tract are moved and mixed by two types of smooth muscle contractions: Peristaltic- move contents along the
digestive tract. They consist of circular muscle contractions
that propel contents.
Segmental- cause back-and-forth mixing movements.


Esophagus
A muscular tube that extends from the pharynx to the stomach.
Its function is to conduct swallowed material to the stomach.
The esophagus enters the stomach at the cardia. Made of smooth muscle, Which helps with peristalsis.

Gastroesophageal Reflux & Esophagitis
Inflammation of the esophageal wall most often associated with contact of irritants with the mucosa of the esophagus.
Acids, alkalis, drugs, toxins, and hot materials can produce lesions of varying severity.
Once inflammatory damage occurs, lower esophageal sphincter function becomes abnormal, perpetuating the problem.

Megaesophagus Esophageal paralysis or
hypomotility. A dilation of the esophagus Due to a vascular ring anomaly or
an unknown cause May be secondary to systemic
disease (hypothyroidism) Primary sign- regurgitation
(begins at weaning if congenital)

Esophageal Obstruction
Bones and small toys commonly enlodge at the thoracic inlet, cardiac base, or distal esophagus.
The degree of damage to the esophagus depends on: The size of the object The shape The time spent in contact with the
mucosal lining

Spirocera lupi
Can cause neoplasia of the esophagus.

Stomach…
Divisions- Cardia- the area
immediately surrounding the opening from the esophagus. Associated with the
cardiac sphincter.
Fundus- the section that forms a blind pouch that expands as more food is swallowed.

Stomach…
Divisions- Body- also a distensible
section in the “middle” of the stomach.
***Pylorus- the distal part of the stomach that grinds up swallowed food and regulates hydrochloric acid (HCl). **The glands of the pylorus
contain endocrine cells called G cells which secrete the hormone gastrin.

Stomach…
The body & fundus are both rich in glands containing 3 key cells- Parietal cells- which produce HCl. Chief cells- which produce
pepsinogen. Mucous cells- which produce
protective mucus.
Mucous- adjective Mucus- noun

Stomach…
Inside the stomach, multiple folds called rugae can be observed.

Gastric Motility
Swallowing of food stimulates vigorous mixing, grinding, and propulsive contractions that move food toward the pylorus.
The smooth muscle in the wall of the stomach responds to several hormones, peptides, and nervous system controls. Stimulation of the vagus nerve causes the
fundus to relax (so it can fill), while increasing the contractions in the body and pylorus for mixing and peristaltic movements.

Gastric Secretions
Pepsinogen is secreted by chief cells and is a precursor for the enzyme pepsin.
The proteins broken down by pepsin form chains of amino acids (polypeptides & peptides).
The presence of peptides in the pylorus stimulates the G cells to release more gastrin, which stimulates more HCl and pepsinogen release.

Gastric Secretions… Once the pepsin moves from the acidic pH
of the stomach to the more alkaline pH of the duodenum, it is inactivated by the change in pH and stops functioning.
The mucus produced by the gastric glands provides a protective coating of the stomach.
Mucins are complex molecules produced by the goblet cells in the gastric glands and are the main constituents of the coating.
Bicarbonate ion is also secreted onto the surface making it more alkaline.

Gastric Secretions…
The parietal cells in the gastric glands secrete hydrogen and chloride ions separately into the stomach.
Once these ions are secreted, they combine to produce the HCl that accounts for the stomach’s acidic pH.
The parietal cells have 3 receptors that regulate acid production.

Gastric Secretions…
These receptors are for: Gastrin Acetylcholine Histamine
Stimulation of all receptors results in the optimum amount of hydrogen and chloride secretion.

Gastric Secretions…
When the pH of the stomach contents drops below 3, gastrin release is inhibited.
When gastrin is inhibited, hydrogen and chloride production is terminated, and HCl production declines.
Selectively blocking any one of these receptors decreases the production of stomach acid. This is the way antacid drugs work.

Mechanism of Vomiting
Vomiting occurs due to the stimulation of the emetic center in the brain. Visual, vestibular, toxins…
Color and content of the vomit can assist in a diagnosis. Flecks of blood- recent hemorrhage in the
esophagus or stomach. Coffee grounds- digested blood Yellow-green- bile

Acute Gastritis
Causes include: Diet- spoiled food, change in diet, food allergy, or
food intolerance. Infection- bacterial, viral, or parasitic. Toxins- chemicals, plants, drugs, or organ failure.
Ingestion of foreign objects may also result in gastritis.
Once the mucosa is damaged, inflammation occurs and clinical symptoms develop.

Gastric Ulcers
Commonly a result of drug therapy. NSAID’s
Aspirin, ibuprofen…
Disruption of the normal gastric mucosal barrier, resulting in ulceration.

GDV
Diet and exercise have been indicated in the development of GDV.
As the stomach fills with air, food, and/or fluid, the outflow tracts become occluded.
Further distension results in a simple dilation (air-filled stomach), or the air-filled stomach may twist along its longitudinal axis (volvulus).

GDV…
The pylorus usually passes under the stomach.
The enlarged stomach presses against the diaphragm, making breathing difficult and blocking venous return.
The spleen may also be involved.

GDV

Pyloric Stenosis
Hypertrophy of circular smooth muscle fibers of the pyloric sphincter
This causes an obstructive narrowing and projectile vomiting

Hemorrhagic Gastroenteritis- (HGE) Acute onset of bloody diarrhea
Malabsorption Syndrome- the small intestine is unable to deliver nutrients to the circulation (EPI)
Pathology…

Small Intestine
Function:Digestion and absorption

Small Intestine
Where the majority of nutrients are absorbed into the bloodstream.
Divided into 3 segments- Duodenum- first short section leaving
the stomach. Jejunum- longest portion, makes up the
majority of the small intestine. Ileum- enters the colon at the ileocecal
sphincter.

Small Intestine…
Ileocecal sphincter- regulates movement of materials from the small intestine to the colon.
The parasympathetic nervous system provides stimulation for small intestinal motility, secretions, & blood flow.

Structure
The mucosa is adapted to provide a large surface area for absorbing nutrients through folds in the intestinal wall and millions of villi.
Each villus contains thousands of microvilli called the brush boarder.
These cells have many digestive enzymes and carrier molecules embedded in their cell membrane for digestion and absorption of nutrients, vitamins, and minerals.



Motility
Has peristaltic waves, which mix the intestinal contents and slow their movement through the length of the intestine.
The churning motion brings digested material into contact with the surface for absorption.
Slowing the movement also allows enough time to contact with the intestinal wall long enough to be absorbed.
Peristaltic movements are stimulated by reflexes to dilation.

Structure…
Goblet cells are also present. They produce mucus that helps
protect the intestinal mucosa from the flow of ingestion as it passes over the intestinal lining.

Digestion
Electrolytes and vitamins can be absorbed intact into the small intestine wall while carbohydrates, proteins and fats must be chemically digested.
Chemical digestion has 2 steps- By enzymes in the lumen of the intestine. By enzymes associated with the brush
boarder.

Mechanism of Diarrhea
Osmotic- or poor absorption of contents. Dietary overload, maldigestion or malabsorption
Secretory- hyper secretion of the valley portion of the villi. More secretion than absorption. Ex. Parvo, bacterial
Abnormal Motility- abnormal transit time, usually a hypomotility. Hypomotility allows for bacterial overgrowth and
rotting ingesta. Yummy!

Small vs. Large Intestine Diarrhea
Signs Small Intestine Large Intestine
Frequency Normal to
Volume Large Small
Urgency Absent Present
Straining Absent Present
Mucus Presence Absent Present
Blood Presence Coffee grounds Very red
Vomiting Present Absent
Weight Loss Present Absent

Small Intestine Pathology… Enteritis
Inflammation of the small intestine. Can be infectious or inflammatory. The diarrhea usually contains digested blood.
Volvulus- Rotation of the bowel.
Perforations- Penetration of the small intestine wall. Causes: ulcers, foreign bodies, necrosis IIº to
obstruction, herniation or external penetration. This causes painful peritonitis!

Parvo
Parvo virus affects the lining of the small intestine.
It invades/wipes out the simple columnar tissue which exposes blood vessels causing “bloody diarrhea”.
The intestinal response is to become inflamed- Increased peristaltic activity- cramps Propels chyme through rapidly- diarrhea!

Intussusception
The cause is usually idiopathic but can be the result of: Parasite infection Foreign bodies Infections Neoplasia

Intussusception…
The telescoping of the proximal intestine into the distal intestine.
It produces a partial to complete blockage and compromises blood supply to the segments causing bowel necrosis.

Mesentery Mesentery- Clear, suspends the intestines from the
roof of the abdomen. Prevents intestine entanglement Supplies blood to the intestines (small & large)
Omentum- Part of the mesentery. Helps prevent a torsion. Attached at the greater curvature of the
stomach.

Large Intestine
Water absorption and bacterial digestion

Anatomy Review
“Colon” Ascending Transverse Descending

Colitis Acute-
Sudden onset of inflammation of the colon.
Often in dogs. Frequent defecation,
small amounts. Causes: garbage
ingestion, stress, parasites:
Trichuris, Coccidia Bacteria: Salmonella
All cause a change in motility!
Chronic- Long-term, non-specific
inflammation of the colon.
Causes include: idiopathic, FIV+, FIP+
Signs include: diarrhea with slow, progressive weight loss.

Megacolon
An abnormally dilated colon or segment of the colon.
Seen frequently in cats. The presenting symptom is straining to
defecate. These cats are usually dehydrated and
may be vomiting. The cause of this disorder has been
thought to involve a defect in the neurostimulation mechanism that promotes colon evacuation.

Megacolon…
Other causes include: Hypothyroidism Pelvic deformities
Severe prolonged colon distension for any reason can disrupt normal motility and result in megacolon.

Constipation
True constipation is uncommon. The presence of foreign objects,
tumors, pelvic injury, anal sac abscesses, urinary obstruction, and dehydration can result in the failure to pass feces.

Inflammatory Bowel Disease (IBD)-
A group of GI diseases characterized by similar signs with unknown causes.
Diagnosis is made when an excessive number of inflammatory cells are found in mucosal samples of the GI system.
Colonic inflammation disrupts mucosal integrity and results in decreased absorption of sodium and water.
Inflammation also results in hypermotility, resulting in more frequent defecation.

Inflammatory Bowel Disease (IBD)…
Signs include: Diarrhea with little weight loss. frequency of defecation and fecal
volume.

Rectum & Anus
Rectum- the part of the colon running through the anal cavity.
Anus- Anal sphincter- a muscular ring that
controls the passage of feces out of the body.
What type of muscle? Smooth!

Anatomy
Perianal Glands- sebacous glands located in the skin, encircling the anus.
Anal Glands- located in the submucosa, at the anocutaneous junction. Where are the ducts?

Anal Gland Impaction
Retention of anal sac secretions If left untreated, they may abscess Anal sac rupture is secondary to
obstructions

Perianal Adenoma
Usually in intact male dogs. Bengin, hormone dependant tumor
that arises from the perianal gland. Which hormone? Testosterone

Perianal Fistulae
Multiple ulcerative, smelly draining tracts surrounding the anus
Caused by dogs with a low tail carriage and/or a broad tail base (which retains fecal film) ex. GSD

Hepatic Anatomy

The Liver
The largest gland in the body. A digestive gland of substantial
importance in metabolism.

The Liver…
Functions: Detoxification of drugs and toxins. Formation and secretion of bile. Metabolism of carbohydrates and fats. Plasma protein production. Urea formation.

Anatomy
The liver consists of six lobes. HEPATOCYTES.


Blood Supply
The liver has a unique venous system referred to as the Hepatic Portal System, which receives both oxygenated and deoxygenated blood.
All products of digestion are filtered through the liver and approximately 80% of the blood that flows into the liver enters through the portal vein and originates from the stomach and intestines.

Blood Supply…
The hepatocytes are nourished by this blood which is rich in nutrients but not in oxygen.
As blood enters the lobules, it flows across the hepatocytes and filters into the central vein.
The blood then travels from the central vein into the hepatic vein and eventually the caudal vena cava.

Blood Supply…
As the blood is filtered through the liver, it passes through Kupffer cells, which help remove bacteria.
The hepatic artery supplies the remaining 20% of blood to the liver. This blood, which is rich in both oxygen
and nutrients, supports the high metabolic activity of the hepatocytes.


Hepatocytes
The hepatocytes also secrete hormones and bile, a green digestive hormone liquid.
The bile is carried through channels to the gallbladder where it is stored and the common bile duct, which leads to the duodenum, where bile is released.

Physiology

Bile
Bile plays an important role in digestion, and bile production is one of the main functions of the liver.
Bile consists primarily of bile salts, water, and bile pigments such as bilirubin.
One of the most important functions of bile is to emulsify fat so it can be broken down by digestive enzymes in the gut.

Carbohydrate Metabolism
In a process called glycolysis, the liver metabolizes carbs by converting excess glucose into glycogen for storage.
The process is reversed when energy is needed.
The entire cycle is known as glycogenolysis and is under the influence of the hormone glucagon.

Deamination
Amino acids are broken down by the removal of an amino group.
The discarded amino group is converted into ammonia and then into urea or uric acid, which is excreted through renal filtration. Animals with liver failure may have
increased levels of ammonia.

Synthesis
The liver synthesizes both alpha and beta globulins, which transport lipids and fat-soluble vitamins throughout the body.
Prothrombin is one of the most important alpha globulins produced by the liver.

Pathology
Cirrhosis- scarring of the liver, which is replaced with connective tissue. 70% of the liver can be destroyed before problems occur.
Jaundice- A build-up of bilirubin in the body.
Hepatitis- inflammation of the liver causing damage to the hepatocytes.
Cholecystitis- inflammation of the gallbladder.

Infectious Canine Hepatitis
Caused by Canine Adenovirus I and has long been recognized as a cause of hepatic necrosis in dogs.
Infection occurs via the oronasal route.
Viral replication occurs in the tonsils and lymph nodes.

Infectious Canine Hepatitis…
Signs include: Petechial hemorrhages Lethargy Fever >103°F Depression Pale MM Abdominal pain Anorexia Bloody diarrhea Hepatomegaly

Feline Hepatic Lipidosis
“Fatty Liver Disease” Severe accumulation of fat in the liver Secondary to diabetes mellitus in obese
cats, malnutrition, drugs, toxins, or idiopathic.
Complete anorexia in obese cats CBC- non-regenerative anemia, stress
neutrophilia, lymphopenia. ALP (20x normal), ALT (10x normal),
hyperbilirubinemia, hypoalbuminemia, bile acids.

Hepatic Lipidosis
Signs- Hepatoencephalopathy V/D Icterus Sporadic vomiting Anorexia Obesity Melena (black, tarry stools)

Portosystemic Shunts Portal Systemic
Shunts The blood by-passes
the liver due to a congenital defect or acquired by chronic hepatitis.
This leaves the blood unfiltered as it returns to the heart.
Ammonium biurate crystals in the urine can be an indicator.

Shunts Causes:
Congenital- a vascular anomaly
Acquired- IIº to chronic active hepatitis or serosis, (portal vein non-functional)
Signs: CNS-
hepatoencephalopathy d/t ammonia build-up in the brain.

Shunts
Signs- Anorexia Depression Ataxia Head-pressing Circling, pacing,
blindness Seizures Hypersalivation

Pancreas: Anatomy Review

Pancreatic Function
An endocrine and exocrine gland. The primary organ supplying digestive
enzymes. Helps regulate glucose levels. 4 Secretions-
Sodium bicarbonate Trypsin Amylase Lipase

Pancreatic Function
No secretion: starvation due to nutrients not digested.
Oversecretion: over digestion, autodigestion of the pancreas.

Anatomy
Located along the greater curvature of the stomach.
Venous drainage of the pancreas to the portal vein, (filtered by the liver), and then returned to circulation. Hepatitis is common with acute
pancreatitis.


Pancreatic Anatomy… Pancreatic secretions
pass from secreting cells in the pancreas into small ducts.
The small ducts ultimately unite to form the ducts that carry secretions to the small intestine.
The pancreas is made up of small clusters of glandular epithelial cells.

Pancreatic Anatomy… About 99% of the cells are arranged in
clusters called acini and constitute the exocrine portion of the organ.
The cells within the acini secrete a mixture of fluid and digestive enzymes called pancreatic juice.
The remaining 1% of cells are organized into clusters called pancreatic islets.
They form the endocrine portion of the pancreas that secrete the hormones insulin and glucagon.

Pancreatitis
Inflammation of the pancreas. May be acute or chronic. Develops when digestive enzymes are
activated within the gland, resulting in autodigestion.
Once autodigestion develops, the gland becomes inflamed, resulting in tissue damage, multisystemic involvement, and often death.
More prevalent in obese animals.

Pancreatitis…
Diets high in fat may predispose animals to the disease.
Most commonly a post-holiday disease. Feeding scraps from turkey, ham, or
roast drastically increases an animal’s dietary fat, resulting in acute signs of the disease.

Pancreatitis…
Clinical signs- Depression Anorexia Vomiting Dehydration Abdominal pain

Exocrine Pancreatic Insufficiency (EPI)
Develops with a progressive loss of acinar cells followed by inadequate production of digestive enzymes.
Clinical signs may not develop until 85%-90% of the secretory ability has been lost.
Lack of normal secretions affects the mucosal lining of the small intestine and decreases its absorptive power.
Disruption of the normal acinar structure may affect insulin production, leading to glucose intolerance.

Exocrine Pancreatic Insufficiency & EPI…
Clinical signs- Mild to marked weight loss Polyphagia, copraphagia Diarrhea, fatty stool Flatulence