Leaders Update on central system cytopathology. I ... · Updateoncentral nervoussystem...
Transcript of Leaders Update on central system cytopathology. I ... · Updateoncentral nervoussystem...
JT Clin Pathol 1994;47:573-578
Leaders
Update on central nervous system cytopathology.I. Cerebrospinal fluid
J E Bell
IntroductionExamination of cerebrospinal fluid providesextremely useful diagnostic information inmany diseases of the central nervous system.In particular, analysis of cytological appear-ances may help to confirm or refute the pres-ence of inflammatory or neoplastic processesin the subarachnoid compartment. This arti-cle explores some of the issues, both practicaland theoretical, which influence the efficacyof this investigation and highlights the dilem-mas and methodological pitfalls which mayinterfere with diagnostic accuracy.
NeuropathologyLaboratory,UniversityDepartment ofPathology, WesternGeneral Hospital,Edinburgh EH4 2XUJ E BellCorrespondence to:Dr J E BellAccepted for publication29 March 1994
Normal physiology of cerebrospinal fluidCerebrospinal fluid (CSF) is produced withinthe ventricular system of the brain by secre-tion from choroid plexuses at a rate of about500 ml a day.' The CSF circulates throughthe ventricular system, escaping through theforamina of the roof of the fourth ventricleinto the subarachnoid space, before beingreabsorbed under normal circumstancesthrough the arachnoid granulations into thevenous sinuses of the dura mater.' The spinaland cranial subarachnoid spaces are in conti-nuity unless there is obstruction at the fora-men magnum. The central canal of the spinalcord, although patent during developmentand in early life, is frequently occluded inlater life and may not contain CSF.CSF is normally crystal clear and colour-
less, and should contain no more than 5 x 106cells per litre in samples aspirated from thelumbar cistern.' These cells are predomi-nantly lymphocytes. Normal CSF containsglucose at a level approximately two thirds ofthat in blood but the protein content is verylow. The table lists normal CSF valuestogether with abnormal findings which areindicative of various pathological conditions.In adult life the protein content of lumbarCSF is somewhat higher than that of ventric-
ular CSF.' Fetal CSF is comparatively rich inprotein.2
Indications for cytological examinationofCSFCSF is usually submitted for cytologicalexamination to confirm, or help to exclude, adiagnosis of infective, inflammatory, or neo-plastic processes in the subarachnoid com-partment. Samples are sometimes submittedto the laboratory following other proceduressuch as a myelogram, administration ofintrathecal drugs, or in dementia of earlyonset. In these circumstances negative CSFcytology can be reassuring. Certain features,such as a higher than normal openingintrathecal pressure, or raised protein concen-trations, or cell counts, are frequently predic-tive of abnormal CSF cytology.3
Samples of CSF are usually obtained fromthe lumbar subarachnoid space and onlyrarely nowadays from the cisterna magna.Ventricular samples can be obtained duringoperation, during positioning of a CSF accessdevice, or during or after placement of a ven-
ii 4
S _
W.
'p
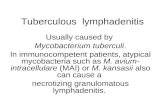
CSFfindings in central nervous system infections and inflammations
Infection Protein Glucose Cells
Normal 0 1-0 45 g/l 2 5-4 mmol/l <5 x 106/1 lymphocytesBacterial Raised: 0-5-5 g/l Reduced: 0-2-0 mmol/A Many polymorphsTuberculous Raised: 0-5-2 g/l Reduced: Polymorphs early,
1-2-2-0 mmol/l lymphocytes laterViral Slightly raised Normal Polymorphs early,
0 5-1-5 g/l lymphocytes laterMultiple sclerosis Oligoclonal IgG Normal Lymphocytes
on electrophoresisFigure 1 Ventnicular sample ofCSF containsmacrophage-like cells and a cytologically benign clump ofcels probably derivedfrom choroid plexus (Giemsa).
573
on June 5, 2020 by guest. Protected by copyright.
http://jcp.bmj.com
/J C
lin Pathol: first published as 10.1136/jcp.47.7.573 on 1 July 1994. D
ownloaded from
Bell
triculo-peritoneal shunt. Ventricular samplesare noticeably more cellular than lumbarsamples and may contain small fragments ofbrain or choroid plexus tissue4 (fig 1).Cisternal samples are more likely than lumbarsamples to be positive in cases of neoplasticspread in CSF.5 It follows that knowledge ofthe source of the sample, as well as the clini-cal history, is important for interpretation ofCSF findings. It should be noted that CSFsamples obtained after death, even from thelumbar subarachnoid space, are hypercellularcompared with samples obtained during life,due to shedding of cells.6 This also occurs in"respirator brain," where fragments of cere-bellum can be found in lumbar CSF samples:this may cause diagnostic confusion.7 Theseshed cells should not be interpreted necessar-ily as evidence of inflammation or of otherclinically relevant antemortem pathologicalprocesses.
It is appropriate to request repeat CSFsamples in diagnostically difficult cases orwhen the sample has been unsatisfactory, orto chart progress of certain diseases includingsubarachnoid disease in leukaemia and pri-mary brain neoplasms.8
Preparation of samplesIt is important to ensure that CSF samplesreach the laboratory as soon as possible afterthe lumbar puncture because cells in CSFdeteriorate rapidly.9 The accompanyingrequest form should contain sufficient clinicaldetail to ensure that the sample does not posea high risk to the laboratory staff, and to assistin interpretation of the findings. Volume,colour, and clarity of the specimen should benoted at the time of receipt. A cell countshould be performed using standard countingchambers into which a drop of CSF stainedwith toluidine blue is introduced unless thesample is in the high risk category.
Cytological examination should be under-taken concurrently with glucose and proteinestimations, and antibody titres if appropri-ate, all in the same sample of CSF. Of all thepossible methods for transferring cells fromCSF samples on to slides, most laboratoriesnow use a cytospin apparatus,4 such as theShandon cytocentrifuge, which is efficient interms of cell yield.10 To prepare cytospins, 0-2mm3 of CSF is placed in balanced wells andspun for five minutes at 600 rpm. If the origi-nal sample exceeds 1 ml, it is pre-concen-trated by centrifugation at 2000 rpm for fiveminutes. The cytospin preparations are airdried and fixed in methanol for 10 minutesbefore staining. Routine stains includeGiemsa, Papanicolaou, and haematoxylin andeosin.
Examination of routinely stained cytospinsmay reveal abnormalities which suggest thatfurther cytospins should be prepared for addi-tional stains, and if these are to includeimmunocytochemical procedures, the sparecytospins should be fixed in cold acetone forfive minutes. Additional routine stainsinclude Gram, Ziehl Neelsen, periodic acid
Schiff, Perls's and Masson Fontana. Immuno-cytochemical or immunofluorescence studieshelp to identify cellular subpopulations.9Antibodies of interest include epithelial mark-ers (cytokeratin, epithelial membrane anti-gen) lymphoid and macrophage markers(leucocyte common antigen, panel of T andB cell markers, and PGM1) and neuroecto-dermal markers (glial fibrillary acidic protein,PGP 9'5, and S100 protein). S100 protein isalso a marker for melanoma cells. An anti-body to placental alkaline phosphatase mayassist in the identification of germ celltumours. Double immunofluorescence pre-parations can be considered when onlylimited numbers of cytospin preparations areavailable.
Cytology findings in CSF samplesHAEMORRHAGEIn a so-called traumatic tap peripheral bloodcan be introduced into CSF during aspirationof the sample. In this case the sample willappear blood-stained but on settling the CSFsupernatant fluid is clear. Genuine subarach-noid haemorrhage may be marked by xan-thochromia of the supernatant fluid, andspectroscopy can be used to detect haemoglo-bin and bilirubin. In either case red bloodcells, together with an appropriate number ofmixed white cells, are present in the sampleon cytological examination. Pigment-ladenmacrophages which prove positive with aPerls's Prussian Blue reaction provide evi-dence of previous haemorrhage (fig 2).
ACUTE INFLAMMATORY INFILTRATEThe infiltrate is characterised by the presenceof polymorphs without an accompanyingappropriate number of red blood cells.
*
Figure 2 Two macrophages showing pigmented inclusionsin the cytoplasm, from a patient with previoussubarachnoid haemorrhage (haematoxylin and eosin).
574
on June 5, 2020 by guest. Protected by copyright.
http://jcp.bmj.com
/J C
lin Pathol: first published as 10.1136/jcp.47.7.573 on 1 July 1994. D
ownloaded from
Update on central nervous system cytopathology I
Although bacterial infection is the most usualcause, early viral, tuberculous, and fungalinfections also provoke an initial polymor-phonuclear leucocyte reaction.9 An acuteinflammatory infiltrate in the subarachnoidspace is occasionally due to necrotisingprocesses in the brain or spinal cord such assurfacing infarcts or malignant tumours.Other conditions associated with polymorphinfiltration include epilepsy and reactions tointrathecal drugs, while CSF eosinophiliamay be a response to drugs, or shunt proce-dures, or to metastatic disease in the lepto-meninges.9 Infecting organisms, particularlyGram positive bacteria, or fungi such asCryptococcus sp, may sometimes be identifiedin the CSF by special stains. However, bacte-rial and viral agents are more likely to becharacterised accurately by microbiologicalinvestigation, which also forms the basis forappropriate drug treatment.
CHRONIC INFIAMMATORY INFILTRATEThis is characterised by lymphocytes andusually macrophages (fig 3). In active chronicinflammation plasmacytoid cells may be pre-sent (fig 4). Typically, this type of infiltrate isseen in the active stages of viral and tubercu-lous infections, and should prompt microbio-logical investigation of the sample if theclinical history is appropriate and if this hasnot already been undertaken. However, infec-tive causes are rarer in Western practice thannon-infective inflammatory causes. Small butclinically important numbers of CSF lympho-cytes are often seen in the active phases ofmultiple sclerosis, and occasionally resultsimply from irritation of the leptomeninges-for example, by a prolapsed disc. Reactiveand infective lymphoid infiltrates arepolyclonal and include mixed B and T cells,
S~~~~~~A L
identified by immunocytochemical staining ofspare cytospin preparations.9A summary of the CSF findings in infective
and inflammatory conditions is shown in thetable.
NEOPLASTIC INFILTRATIONMalignant cells can be shed into the CSFfrom primary tumours of the central nervoussystem (CNS), particularly medulloblas-tomas, ependymomas, pineal tumours, pri-mary CNS lymphomas and less commonlyfrom gliomas (fig 5). Although primarytumours rarely metastasise outwith the CNS,they have a capacity for seeding through thesubarachnoid space." Subarachnoid spreadmay also complicate recurrence of a previ-ously treated intrinsic CNS tumour.
Malignant cells can also be present in theCSF as a result of metastatic spread fromtumours arising in other systems, includingcarcinoma (fig 6), melanoma, non-CNS lym-phoma and sarcoma.4 Tumours of the breast,lung, and prostate tend to spread in the sub-arachnoid compartment and melanomas alsofrequently metastasise here.9 Cranial andspinal nerves may be invaded by collectionsof metastatic tumour cells, particularly bylymphoma. Occasionally the primary tumouris occult and meningeal disease is the firstclinical indication of disease. Analysis of CSFcytology, particularly by immunocytochemi-cal investigation, may suggest possible pri-mary sites. Routine follow up of cases ofleukaemia may reveal blast cells in the CSF,the presence of which would prompt appro-priate CNS directed treatment.
Highly atypical or frankly malignant cellscan be present in cytospin preparations ofCSF either singly (fig 6) or in clumps (fig 7),and their nature and origin is further defin-
S
0
....
08
Figure 3 Chronic inflammatory infiltrate in CSFshowing lymphocytes and a macrophage (top left)(haematoxylin and eosin).
SFigure 4 Chronic inflammatory infiltrate in CSFshowing plasmacytoid cells (centre) in addition tolymphocytes (haematoxylin and eosin).
575
on June 5, 2020 by guest. Protected by copyright.
http://jcp.bmj.com
/J C
lin Pathol: first published as 10.1136/jcp.47.7.573 on 1 July 1994. D
ownloaded from
576
a
Figure 5 Clump ofglioma cells in specimen oflumbarCSF aspirated 10 days after biopsy of the primary tumour(haematoxylin and eosin).
able by immunocytochemical techniques (figs8 and 9). If there is insufficient CSF in theoriginal sample for more detailed studies arepeat sample should be requested. Malig-nant CSF cellular infiltrates are very fre-quently accompanied by a raised CSF proteinconcentration.
Dilemmas and pitfalls in CSFexaminationThe diagnostic dilemmas are of two main
Figure 7 Clump of malignant cells in lumbar CSFfroma patient with a primary tumour in the lung(haematoxylin and eosin).
Figure 6 Carcinoma cels in lumbar CSFfrom a patientwith a primary tumour in the breast (haematoxylin andeosin).
types. First, the presence of atypical cells (fig10), which are abnormal but not clearlymalignant, is always worrisome, and theirinterpretation should be undertaken with cau-tion. The diagnostic problem arises whencells such as this are seen in very small num-bers. Their presence should prompt a requestfor a repeat specimen.9 The problem is partic-ularly acute when there is no history to sug-gest that the patient has a tumour. Thepresence of clumps of cells, or of mitotic
Figure 8 Malignant cells in CSF are positive forcytokeratin confirming their epithelial nature. Small non-malignant cells in the sample are negative for cytokeratin(top right) (immunocytochemistry).
Bell
JML
on June 5, 2020 by guest. Protected by copyright.
http://jcp.bmj.com
/J C
lin Pathol: first published as 10.1136/jcp.47.7.573 on 1 July 1994. D
ownloaded from
Update on central nervous system cytopathology I
Figure 9 Smallmalignant cells in CSF arepositive for vimentin(negative ceUs are also seenin this preparation) in apatient with a paraspinalEwing's sarcoma(immunocytochemistry).
figures, should not be taken as indisputable
evidence of malignancy, as both occur in
non-neoplastic conditions. Clumps of cells
may be found in cellular samples aspiratedfrom ventricular cavities and occasionally in
lumbar CSF.4 The cytological architecture is
helpful in this context as the morphology of
small choroid plexus fragments (fig 1), or
even of cartilaginous fragments, is usually suf-
ficiently characteristic to exclude the suspi-
cion of malignancy. Mitotic figures are seen
occasionally reactive inflammatory infil-
trates, particularly in macrophage-like cells.
Cells may assume quite bizarre appearances
in florid reactive processes and these may be
sufficient to raise the suspicion of malig-
Figure 10 Severalmononuclear cells are seenin this CSF. cytospinpreparation from a 45 yearold woman withrelapsinglremitting brainstem disturbance, thoughtto be due to demyelination.Proteinaceous debrissurrounds scattered cells,the largest of which has anirregular nucleus withvariable chromatindensity. The appearancesare suspicious but notdiagnostic of malignancy,(haematoxylin and eosin).
nancy. Atypical cells may be present in suchsmall numbers as to give uninformative sparecytospin preparations, in which caseimmunocytochemical studies will be unhelp-ful. Lumbar puncture may have to berepeated and the timing of this is likely to beinfluenced by the clinical progress of thepatient.A second major dilemma lies in the
difficulty of distinguishing between reactiveand neoplastic lymphocytic infiltrates.49Cytological appearances of the cells may behelpful-monomorphic and lymphoblasticinfiltrates suggest neoplasia whereas reactiveinfiltrates are usually of mixed cellularity. Thepresence of plasma cells is also helpful inpointing to a reactive rather than a neoplasticinfiltrate as plasmacytoid lymphomas are veryrare in the CNS.9 Immunocytochemical stud-ies show that reactive infiltrates are composedof mixed T and B cells. Primary CNS lym-phomas should show monoclonality, mostbeing of B cell type.9 Difficulties arise becauseprimary B cell lymphomas are frequentlyaccompanied by a T cell reaction: interpreta-tion of immunocytochemical findings shouldbe undertaken only with full knowledge of theclinical and radiological findings. If samplesare inadequate for full immunocytochemicalstudies, a repeat sample must be requested.
Preventable pitfalls in CSF cytopathologi-cal diagnosis include inadequate clinicaldetails and delay in transport to the labora-tory, causing deterioration in cellular preser-vation, which specifically interferes withimmunocytochemical staining properties.9Artefacts of preparation, such as cellular dis-ruption, may be caused by excessive cytospinspeeds. Discrepancies in appearance betweendifferent cytospin preparations from an indi-vidual sample may result from insufficientmixing of the original fluid or from unbal-anced cytospin wells.The differences between CSF samples
from different sites have already been men-tioned. If a ventriculoperitoneal shunt is insitu fluid obtained from the lower end of theshunt may be extremely cellular, containingclumps of bizarre-looking cells, probably ofperitoneal origin, in which mitoses are notunusual. Paediatric CSF samples, especiallyfrom premature babies with intraventricularhaemorrhage sometimes contain clusters ofgerminal matrix cells whose primitive appear-ance is suggestive of neoplasia to the inexperi-enced observer.
Examnation ofhigh risk samplesCertain categories of CSF samples may rep-resent a particular hazard to laboratory staff.Most of these are infections in AdvisoryCommittee on Dangerous Pathogens cate-gory 3, but Creutzfeldt-Jakob disease (cate-gory 2) is also a particular case.'2 Samplestaken from patients with known or suspectedHIV infection, tuberculosis, or hepatitis B,and from possible cases of Creutzfeldt-Jakobdisease should be treated as "high risk".
High risk samples of CSF should be trans-
577
AML
qg:.40im;L
ANh6.
W:
on June 5, 2020 by guest. Protected by copyright.
http://jcp.bmj.com
/J C
lin Pathol: first published as 10.1136/jcp.47.7.573 on 1 July 1994. D
ownloaded from
578
ported to, and handled in, a containmentlevel three laboratory. The cell count is gen-erally omitted. In preparing cytospins fromsuch a sample, consideration should be givento the infective agents which are likely to bepresent. For instance, if Ctyptococcus infectionis suspected in a patient with AIDS, a sampleof CSF may be mixed with India ink whichwill clearly outline, and leave unstained, thesmall spores of Ctyptococcus. In possibletuberculous meningitis cytospin preparationsshould be analysed for acid and alcohol fastbacilli4 after ensuring that a sample has beensubmitted for bacteriological examination. InHIV infection the CSF may contain viralantigen in the pre-symptomatic stages of ill-ness. Small but clinically important numbersof lymphocytes may be detected in CSFbefore the onset of AIDS. Further examina-tion shows that these are T lymphocytes andthat very few B cells are present in the pre-AIDS subarachnoid infiltrate."3 On progres-sion to AIDS, the T cell infiltrate largelydisappears from the subarachnoid space, butadditional opportunistic infections, such asCryptococcus sp, may be accompanied by apolymorph response. An additional finding inAIDS may be the presence of primary B celllymphoma infiltrate. It is the presence of HIVitself in CSF, rather than that of opportunis-tic agents, which represents a hazard to labo-ratory staff. Of the full range of possibleinfections in immunocompromised patients(not just AIDS cases) few, apart fromCryptococcus, are readily identifiable in cyto-logical examination of CSF.9As CSF shows no apparent abnormalities
in Creutzfeldt-Jakob disease it is questionablewhether lumbar puncture has any value inlikely cases. CSF from patients with sus-pected Creutzfeldt-Jakob disease should behandled in a category 3 containment labora-tory using disposable equipment where possi-ble. All instruments and disposable itemsused in the lumbar puncture procedureshould be destroyed by incineration.Laboratory equipment can be decontami-nated by immersion in solutions containing20 000 ppm chlorine (14 Presept tabletsfreshly dissolved in 1000 ml of water), or 2 Nsodium hydroxide solution, or by steam auto-claving at 134°C for 18 minutes (porous loadautoclave). It is preferable to dispose ofequipment that has been contaminated withCreutzfeldt-Jakob disease agent. There is asyet no validated clinical test which wouldconfirm or exclude the presence ofCreutzfeldt-Jakob disease in life.
Future trends in CSF diagnosisThe number of problem cases in which it ishard to achieve a firm diagnosis followingexamination of CSF suggests that there is stillroom for progress in diagnostic procedures.'4Immunocytochemical techniques have helpedto refine diagnosis and to separate specificcellular subpopulations in CSF. This helps todistinguish intrinsic from metastatic tumoursin the subarachnoid space and to pinpoint the
possible origin of metastatic tumour cells.Progress will probably be made in in situhybridisation techniques identifying host orviral DNA products within cells, and in PCRtechniques which amplify DNA fragments ofinterest. If major progress were to be made inCSF based diagnosis of conditions such asAlzheimer's disease and Creutzfeldt-Jakobdisease, it would be unlikely to be based incytopathology as CSF is generally acellular inthese diseases.
Several recent surveys have questioned thewisdom of routinely analysing cytopathologyappearances in all CSF samples. It has beensuggested that if the cell count and CSF pro-tein are within normal limits and if there is norelevant clinical history, then the likelihood offinding important pathology by further inves-tigation of CSF samples is very low indeed." 15Such case selection might reduce the work-load in very busy laboratories. However, itmight also be argued that it is proper toextract as much information as possible froma CSF sample and negative results may havesome value in this context. It is difficult toascertain the number of cases in which majorpathology is missed when CSF is reported asnormal but several studies have shown thatthe number of false negative results is likely tobe low.49 '5 These matters are open to debateand may be influenced by local practice,especially at a time when cost effectiveness ofhospital procedures is under close scrutiny."
My thanks are due to Mr W Shade and the skilled technicalstaff of the Edinburgh Neuropathology Laboratory, to Dr JWIronside for helpful discussion, and to Miss A Boyd for typingthe manuscript.
1 Davson H, Welch K, Segal MB. The physiology and patho-physiology of the cerebrospinal fluid. Edinburgh: ChurchillLivingstone, 1987.
2 Bell JE, Fryer AA, Collins M, et al. Developmental profileof plasma proteins in human fetal cerebrospinal fluidand blood. NeuropatholAppl Neurobiol 1991;17:441-56.
3 Hayward RA, Shapiro MF, Oye RK. Laboratory testing ofcerebrospinal fluid. Lancet 1987;1: 1-4.
4 Bigner SH. Cerebrospinal fluid (CSF) cytology: currentstatus and diagnostic applications. J7 Neuropathol ExpNeurol 1992;51:235-45.
5 Rogers LR, Duchesneau PM, Nunez C. Comparison ofcisternal and lumbar CSF examination in lepto-meningeal metastases. Neurology 1992;42:1239-41.
6 Platt MS, McLure S, Clarke R, et al. Postmortem CSFpleocytosis. Am J7 Forens Med Pathol 1989;10:209-12.
7 Norenberg MD, Bruce-Gregorios J. Nervous system man-ifestations of systemic disease. In: Davis RL, RobertsonDM, eds. Textbook of neuropathology. Second Edn.Baltimore: Williams and Wilkins, 1991:461-534.
8 Bigner SH, Johnston WW. Cytopathology of the centralnervous system. New York: Masson Publishing, 1983.
9 Walts AE. Cerebrospinal fluid cytology. Diagn Cytopathol1992;8:394-408.
10 Seyfert S, Kabbeck-Kupijai D, Marx P, Kossmehl G.Cerebrospinal fluid cell preparation methods: an evalua-tion. Acta Cytol 1992;36:927-31.
11 Russell DS, Rubinstein U. Pathology of tumours of the ner-vous system. London: Edward Arnold, 1989.
12 Advisory Committee on Dangerous Pathogens. Categori-sation of pathogens according to hazard and categories ofcontainment. Second Edn. London: HMSO: 1990.
13 Bell JE, Busutill A, Ironside JW, et al. Human immuno-deficiency virus and the brain: Investigation of virusload and neuropathologic changes in pre-AIDS subjects.JInfect Dis 1993;16:818-24.
14 Andrews JM, Schumann GB. Laboratory processing ofcerebrospinal fluid specimens. Diagn Cytopathol 1990;6:139-43.
15 Fairbanks VF, Folger WN. Cost containment, qualityassurance, and physician microscopy of cerebrospinalfluid with normal cell counts. Am J Clin Pathol 1990;94:67-72.
Bell
on June 5, 2020 by guest. Protected by copyright.
http://jcp.bmj.com
/J C
lin Pathol: first published as 10.1136/jcp.47.7.573 on 1 July 1994. D
ownloaded from