Last Update: 4/5/2004 Division of Tuberculosis Control Virginia Department of Health Richmond,...
-
Upload
shawn-carson -
Category
Documents
-
view
216 -
download
2
Transcript of Last Update: 4/5/2004 Division of Tuberculosis Control Virginia Department of Health Richmond,...
Last Update: 4/5/2004
Division of Tuberculosis Control
Virginia Department of Health
Richmond, Virginia
Tuberculosis Infection & Disease: Fundamentals for the General Public
Picture of tuberculosis bacteria under the microscope
Last Update: 4/5/2004
Table of Contents
1. Introduction2. Role of the Public Health Department
and the Virginia Tuberculosis Control Laws
3. Tuberculosis Transmission and Pathogenesis
4. Epidemiology of Tuberculosis in Virginia5. Screening for Tuberculosis Infection6. Evaluating for LTBI and TB Disease7. Treatment of LTBI and TB Disease8. Infection Control Guidelines
Last Update: 4/5/2004
Tuberculosis (TB): A Disease ofPublic Health Significance
Potentially fatal disease transmitted by droplet nuclei after close contact with a person who has infectious, TB diseaseLong, multidrug treatment regimens increase potential risk of nonadherenceSerious impact on community if TB treatment is improper and/or inadequateDisproportionate impact on persons with inadequate access to health care
Last Update: 4/5/2004
Current TB Challenges in Virginia
Increasing proportion of TB patients born outside the US 48 different countries of origin in 2003 At least 20 primary languages, other
than English, spoken in 2003
High incidence of drug-resistant TB cases21 deaths from TB in 2003 TB is a curable disease
Last Update: 4/5/2004
The Public Health Department
Is a recognized expert in TB control for the local community
Is a resource for the latest on testing and treatment standards
Has access to medical experts at CDC for consultation on complicated TB cases
Last Update: 4/5/2004
Health Department’s Role in Community TB Control
Provides follow-up care to persons diagnosed with TB
Has ultimate responsibility for TB control in Virginia
Has authority to legally enforce the VA Health Code Requires compliance to TB treatment
See Guidebook for the 2001 TB Control Laws www.vdh.state.va.us/epi/tb/guidebook.htm
Assists in interjurisdictional referrals for patients who move residences
Last Update: 4/5/2004
VA Division of TB Control (DTC)Role of the Central Office in Richmond
Mission of the DTC Provide leadership in overcoming
barriers to protect the people of Virginia from tuberculosis
Objectives of the DTC Detect all cases of TB disease Treat all cases of active TB disease Complete treatment of all cases of
active TB disease and their infected contacts
Last Update: 4/5/2004
Virginia TB Control Laws: Key Points
Require reporting of TB disease
Require treatment and adherence to TB treatment
Allow isolation of infectious TB disease patients who refuse TB treatment and/or put the public at risk for TB infection
Last Update: 4/5/2004
How TB is Transmitted
TB is caused by a bacteria, Mycobacterium tuberculosis (tubercle bacillus)
TB transmission occurs when a person with active, infectious TB disease coughs, sneezes, laughs, sings, etc. TB spreads through the air by inhaled
droplet nuclei TB needs prolonged contact for transmission
Last Update: 4/5/2004
Factors That Determine TB Transmission
Infectiousness of the person with TB disease The more infectious a person, the more likely the TB will
be transmitted to others who are in close contact with this individual
Environment in which exposure to TB occurs Room size and ventilation -- Transmission of TB is likely
to occur in rooms that are small and with poor ventilation
Length of time spent with the infectious TB patient The longer the time spent with an infectious TB patient,
the more likely TB transmission will occur
Virulence (strength) of the TB bacteria The stronger the TB bacteria, the more likely the
transmission of TB infection will occur
Last Update: 4/5/2004
Pathogenesis of TB
TB occurs most commonly in lungs (85% of the time), but can occur in other parts of the body
A person with TB infection and a normal immune system has a 10% chance of developing active TB disease in his/her lifetime This risk is greatest within the first 2
years after acquiring TB infection
Last Update: 4/5/2004
Common Sites in the Body Where TB Disease May Occur
Pulmonary (Lungs) -- (85% of the time)Extrapulmonary (outside the lungs) Pleura (lining of the lungs) Central nervous system Lymphatic system Genitourinary systems Bones and joints Multiple sites in the body
Last Update: 4/5/2004
TB Infection or Latent TB Infection (LTBI)
Occurs when TB bacteria are in the body, but are inactiveDoes not have any clinical symptoms of active TB disease Is not infectious to othersProduces a “positive” reaction to the TB Skin TestPresents a normal chest X-ray
Last Update: 4/5/2004
Active TB Disease
Occurs when the inactive TB bacteria in the body (LTBI) become active
May be infectious
Has clinical symptoms (see next slide)
Last Update: 4/5/2004
Symptoms of Active TB Disease
Prolonged cough(may produce sputum)*Chest pain*Hemoptysis*FeverChills
*Symptoms commonly seen in cases of pulmonary (lung) TB
Night sweatsFatigueLoss of appetiteWeight loss orfailure to gain weight
Last Update: 4/5/2004
TB Infection (LTBI) vs. Active TB Disease
TB Infection Pulmonary (Lung) TB Disease
Tubercle bacilli in body Tubercle bacilli in body
Tuberculin skin test reaction usually positive
Tuberculin skin test reaction usually positive
Chest X-ray usually normal Chest X-ray usually abnormal
Sputum smear & culture negative
Sputum smear & culture positive
Asymptomatic Often infectious before treatment
Not a case of TB (Reportable only in children < 4 years of age)
A case of TB (Reportable)
Treated with 1 drug Treated with multiple drugs
Last Update: 4/5/2004
Persons at Higher Risk forBecoming Infected with TB
Close contacts of persons known or suspected to have active, infectious TB diseaseForeign-born persons from areas in the world where TB is commonResidents and employees of high-risk congregate settingsHealth care workers (HCWs) who serve high-risk clients
(Continued on next slide)
Last Update: 4/5/2004
Persons at Higher Risk for Becoming Infected with TB (continued)
Medically underserved, low-income populations
High-risk racial or ethnic minority populations
Children exposed to adults in high-risk categories
Persons who inject illicit drugs
Last Update: 4/5/2004
Once Infected with TB, Factors That Would Increase the Risk for Developing TB Disease
These high-risk persons should be tested for TB infection, and if positive, treated.
HIV infectionSubstance abuseRecent TB infectionLow body weight (10% or more below the ideal)
Diabetes mellitusSilicosisProlonged corticosteroid therapyOther immunosuppressive therapyEnd-stage renal diseaseCancer of the head or neck
Last Update: 4/5/2004
TB and HIV Coinfection: A Concern
For persons infected with TB, HIV positive status is the strongest risk factor for developing active TB disease
In persons who are HIV positive and have TB infection, the chances of developing TB disease increases from 10% in a lifetime to 7% to 10% each year!
Last Update: 4/5/2004
What is Epidemiology?
Epidemiology is the study of the distribution and determinants of disease in human populations
Epidemiological data tell us: who in the population is most at risk for
developing TB disease what risk factors these individuals possess where TB disease is most prevalent how to best protect the public from the
spread of TB disease
Last Update: 4/5/2004
Epidemiology & Surveillance
Epidemiology guides the efforts of the Virginia Division of TB Control and health departments Epidemiology helps determine which
persons to screen for TB
Surveillance is an epidemiological method where there is an on-going systematic collection of disease data to obtain a thorough understanding and analysis of disease patterns
Last Update: 4/5/2004
TB Cases Reported in Virginia, 1992-2003
See Notes pages for an explanation of this graph. [In the menu bar, click “View,” then “Notes Pages.”]
332 in 2003
Last Update: 4/5/2004
Percent of TB Cases by Age and Sex inVirginia, 2003
See Notes Pages for an explanation of the graph.
0
10
20
30
40
50
60
70
Num
ber of
Cas
es
0-14 15-24 25-44 45-64 65+
Age Group in Years
Male
Female
Last Update: 4/5/2004
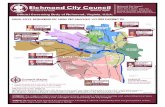
Percent of TB Cases in Virginia, by Region2002 and 2003
Black30%
White19%
Asian/Pacific Islander
32%
Hispanic19%
Hispanic22%
Asian/Pacific Islander
32% White20%
Black28%
20032002
Last Update: 4/5/2004
Goal of Screening for LTBI
Find persons with LTBI who would benefit from treatment to prevent the development of TB disease
Find persons with TB disease who would benefit from treatment
[Persons at no risk for TB infection should not be tested for TB]
Last Update: 4/5/2004
Mantoux Tuberculin Skin Test (TST)
A test for TB infection only Preferred test for TB infection
Clinician performs procedure An injection
Interpretation of TST result (positive, negative) based on: Size of the induration (swelling) and Person’s risk factors for TB
Last Update: 4/5/2004
Persons Who Have Had the BCG Vaccine
Persons born outside the US, and in a country where TB is common may have received the Bacille Calmette-Guerin (BCG) vaccine one or more times
These persons can still receive the TB skin test
Persons who had the BCG vaccine and have a positive TB skin test should be treated for TB infection
Last Update: 4/5/2004
Steps in Evaluating forLTBI and TB Disease
Health care worker will perform the following when evaluating persons for LTBI or TB disease: Assess risk for TB infection, and if
necessary…Administer TB Skin TestRefer persons for Chest x-rayCollect sputum and/or other specimen
to determine presence of TB
Last Update: 4/5/2004
What is the Purpose of a Chest X-Ray?
Chest x-rays… Are needed if the TB skin test is
positive, or if a patient has symptoms of TB disease
Help determine if LTBI has progressed to TB disease in persons who have a positive TB skin test
Check for lung abnormalities in persons with symptoms of TB disease
Last Update: 4/5/2004
What is the Bacteriology Process?
Patients provide specimen (sputum or other)Laboratories: Prepare a smear of the specimen to assess the
presence of the tubercle bacilli Guides in making a presumptive diagnosis of TB
Culture (grow) the specimen for presence of TB bacteria
Positive culture confirms diagnosis of TB disease If culture is positive, further tests are done to
determine the susceptibility/resistance to TB drugs
Helps clinicians choose correct drugs for patient
Last Update: 4/5/2004
Basic Principles of TB Treatment
Goals of treatment for TB disease are: Provide the safest, most effective
therapy in the shortest possible time Give multiple drugs to which the TB
bacteria are susceptible Ensure patient adherence to therapy
Last Update: 4/5/2004
Treatment of LTBI
Treating LTBI prevents the development of TB disease, especially for persons at high risk for developing TB disease if infected with TB
Usual medication regimen for treating TB infection Isoniazid (INH) for 9 months is optimal
6 months of INH is acceptable Rifampin for 4 months is alternative in
certain circumstances
Last Update: 4/5/2004
Medications for TB Disease
Usual medication regimen Minimum of 6 months of therapy, sometimes
longer Initial 4 drug therapy standard, and they are:
Isoniazid (INH) Rifampin Pyrazinamide (PZA) Ethambutol
Medications may need to be changed if the TB is drug resistant to any medication listed above
Last Update: 4/5/2004
Treatment of Extrapulmonary TB Disease
In most cases, extrapulmonary TB is treated with same regimens as those used for pulmonary (lung) TB
A minimum of 12 months of treatment is recommended for bone and joint TB, miliary TB, or TB meningitis in children
Last Update: 4/5/2004
Treatment of Multidrug-Resistant (MDR) TB Disease
MDR presents difficult treatment problems
Treatment must be tailored to each patient and the strain of the patient’s TB bacteria
Use of directly observed therapy (DOT) is mandatory in treating persons with MDR-TB
Last Update: 4/5/2004
Causes of Drug Resistance
Physician prescribes an inappropriate drug regimen
Patients do not take their TB medications exactly as instructed
Infection with a TB bacteria that is already drug-resistant
Last Update: 4/5/2004
Monitoring of Treatment
Patients will be monitored for adverse reactions to the TB therapy Clinicians will conduct baseline tests to
assess a patient’s health at the start of therapy
Patients will be seen at least monthly to:Assess the response to medicationsAssess the adverse reactions to
medicines
Last Update: 4/5/2004
Directly Observed Therapy (DOT)
A health care worker watches a TB patient swallow each dose of the prescribed drugs
DOT is recommended for all persons who have TB disease
The health care worker will conduct DOT at a time and place convenient for each patient who has TB disease
Last Update: 4/5/2004
Benefits of DOT
DOT allows for the rapid identification of problems patients may experience with the TB medicines Health care workers can intervene
earlier to resolve any reactions to medication
[Health care workers are routinely checking on patients’ progress]
Last Update: 4/5/2004
Infectiousness of TB Patients
Persons with active TB disease of the lungs and throat are considered infectious if they: Are coughing Are undergoing cough-inducing or
aerosol-generating procedures Have sputum smears positive for acid-fast
bacilli and are not receiving therapy Have just started TB therapy Have poor clinical response to therapy
Last Update: 4/5/2004
Infectiousness of TB Patients (continued)
The infectiousness is directly related to the: number of tubercle bacilli the TB patient
releases into the air clinical characteristics of the patient’s
TB disease patient’s response to therapy
Infectiousness declines rapidly after adequate treatment is started
Last Update: 4/5/2004
When are Persons with TB Disease Considered Non-Infectious?
Patients with TB disease are considered non-infectious if they meet all of the following criteria: They are on adequate therapy for at
least 2 weeks They have had a significant positive
clinical response to therapy They have had 3 consecutive negative
specimen smear results
Last Update: 4/5/2004
How to Protect Yourself FromTB Infection
When in close contact with a person with infectious TB disease: Wear a mask Open windows in rooms Get screened for TB at your local
health department Learn more about TB infection and
disease from your local health department
Last Update: 4/5/2004
How to Protect Others From TB If You Have Infectious TB Disease
Eliminate contact with others if you are infectiousIf close contact with others is inevitable, make sure that you always:
Wear a mask Open windows in rooms Cover your mouth and nose with hands
when sneezing, speaking, coughing, singing, etc.
Encourage persons who spend a great deal of time with you to be screened for TB infection
Last Update: 4/5/2004
For More Information…
Virginia Department of Health Division of TB Control1500 East Main St, Room 119, Richmond, VA 23218804-786-6251 (Telephone); 804-371-0248 (Fax)http://www.vdh.state.va.us/epi/tb
Local Health Departmentshttp://www.vdh.state.va.us/LHD/LocalHealthDistricts.asp
Centers for Disease Control and PreventionDivision of TB Eliminationhttp://www.cdc.gov/nchstp/tb/default.htm