Lab 11: PULMONARY VENTILATION - slccphys.com
Transcript of Lab 11: PULMONARY VENTILATION - slccphys.com

Page 11.1
Lab 11: PULMONARY VENTILATION
Objectives At the conclusion of this activity, the student will be able to:
1. Understand the ventilation volumes and capacities. 2. Experience a hands-on use of instruments used to determine ventilation volumes. 3. Understand and demonstrate the factors that control respiratory patterns. 4. Demonstrate that breathing can affect cardiac function.
This lab consists of 4 activities, measuring respiratory air volumes with a spirometer under different conditions, and measuring the impact of breathing on heart rate.
ACTIVITY 1. Breathing in a Resting Volunteer ACTIVITY 2. Breathing Immediately After ACTIVITY 3. Increasing the Length of the Airways ACTIVITY 4. Breathing and Cardiac Function
BACKGROUND AND REFERENCES Respiration is the process by which the body obtains and utilizes oxygen, and produces and eliminates carbon dioxide. It can be divided into 5 stages:
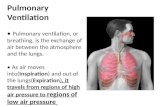
• Pulmonary ventilation, which is the movement of gases between the lungs and the environment. This will be studied in this chapter.
• Pulmonary gas exchange, which is the movement of gases between the lungs and the blood stream.
• Gas transport, which is the movement of gases within the blood stream. • Tissue/blood gas exchange, which is the movement of gases between the
bloodstream and the tissues. • Cellular respiration, which is the consumption of oxygen and the production of
carbon dioxide by cells and organelles.
The respiratory system enables the exchange of O2 and CO2 between the atmosphere, the body, and the cells, thus enabling the intake of O2 into the body for aerobic respiration and the release of CO2 for regulation of body fluid pH. In this exercise, we will examine ventilation of the lungs to enable the exchange of air between the alveoli and the atmosphere. The amount of air contained in the lungs during ventilation can change considerably depending on what muscles are driving air flow and how forcefully they contract. The different amounts of air drawn into or out of the lungs by contracting different groups of muscles are called primary lung volumes. Different combinations of the primary lung volumes, in turn provide us with lung capacities, which define either how much air is present in the lungs or how much air can be moved by the lungs under specific situations. In this lab, you will be measuring and calculating lung volumes and capacities at rest, after exercise, and after artificially increasing the length of the airways. You will also explore the effect of breathing on heart rate.

Page 11.2
The human respiratory system consists of a series of tubes that branch and terminate as clusters of small membranous air sacs called alveoli. During pulmonary gas exchange, oxygen and carbon dioxide cross between the alveoli and the capillaries by diffusion through the respiratory membranes. The respiratory membrane is two cell layers thick—the epithelial cells of the alveoli and the epithelial cells of the capillary. Factors that influence diffusion of the gases include surface area, diffusion distance, and concentration gradient. The total area of the alveoli is about the size of a tennis court, and their thin walls provide a short diffusion distance. A high concentration gradient is insured by (1) movement of blood with low oxygen and high carbon dioxide levels to the lungs and (2) pulmonary ventilation (breathing), which maintains a high level of oxygen and a low level of carbon dioxide in the alveolar air. Thus, the alveoli and associated blood supply are well-suited for the diffusion of oxygen into the blood from the alveoli and carbon dioxide into the air in the alveoli from the blood.
Ventilation of the human lung is produced by muscular contraction. The resulting change in thoracic volume is conveyed to the elastic lungs by the fluid-filled pleural cavity. Inspiration is achieved by a contraction of the diaphragm and the external intercostal muscles, both of which increase the volume of the thoracic cavity. In the resting individual, expiration is usually passive since muscle relaxation and the elasticity of the lungs allow a decrease in thoracic volume.
The ventilation volume and ventilation rate are controlled by the respiratory control center, which is located in the medulla oblongata of the brain. The center insures that the exchange of oxygen and carbon dioxide at the lungs takes place at a rate that matches the body's requirements. Respiratory control is a dynamic process, since the body's requirements change over time. This is the subject of the first activity, which examines breathing in a volunteer at rest and immediately after exercise. The respiratory control center in the medulla is responsible for matching the amount of O2 used by and CO2 produced at the tissues, with the amount of O2 taken up and CO2 discharged at the lungs.
Checkpoint: 1. What is the overall function of respiration?
2. What specific process happens at the respiratory membrane?

Page 11.3
Lung ventilation can be influenced by many factors, including emotion, speech, disease and the body's position relative to gravity. In the last two activities you will examine other factors that influence breathing as well as the effect of breathing on cardiac function.
ACTIVITIES 1 & 2. Breathing Parameters at Rest and After Exercise The amount of air that moves in or out of the lungs during any one normal breathing cycle is called the tidal volume (TV). After normal inspiration, it is possible to breathe in additional air--this is called the inspiratory reserve volume (IRV). Similarly, after a normal expiration, it is possible to exhale additional air from the lungs--this is the expiratory reserve volume (ERV). Even if the expiratory reserve volume is fully expelled from the lungs, there is still a volume of air in the lungs, called the residual volume (RV), that cannot be exhaled. The residual volume has a very low oxygen and a high carbon dioxide concentration. But the residual volume is necessary to allow continuous diffusion of gases between the alveoli and the capillaries between breaths. Upon inhalation, fresh air mixes with stale air from the residual volume to create air in the alveoli that has gas concentrations that facilitate the diffusion of oxygen into and carbon dioxide out of the capillaries. The total amount of air that can be moved in one breath is the Vital Capacity (VC). The basic equation for vital capacity is (VC = TV + IRV + ERV) The respiration center in the medulla insures that gas exchange at the lung matches the requirements of the body. During times of increased demand, the tidal volume can be increased, using some of the reserve lung volumes to bring more fresh air into the body. In addition, the rate of breathing and the rate of air movement in and out of the lungs can be adjusted. In this lab you will measure these parameters in a volunteer at rest and immediately after exercise, when the body's demands for oxygen have been elevated.
Checkpoint: 1. What are the two stages of ventilation?
2. What specific brain area controls ventilation rate and ventilation volume?

Page 11.4
Definitions: Pulmonary functions are described by the following respiratory volume definitions.
- Tidal Volume (TV): The volume of air inspired (or expired) during normal relaxed ventilation (Average = 500 ml in males and 400 ml in females). 10-20% of the vital capacity.
- - Inspiratory Reserve Volume (IRV): The volume of air that may be forcibly inspired above
the normal inspired tidal volume (Average = 3,100 ml). 60-70% of the vital capacity. - - Expiratory Reserve Volume (ERV): The volume of air that may be forcibly expelled
following normal expired tidal volume (Average = 1,200 ml). 25% of the vital capacity.
- - Vital Capacity (VC): The volume of air expired from maximal inspiration to maximal
expiration or the volume of air inspired from maximal expiration to maximal inspiration. VC = IRV + TV + ERV
- - Residual Volume (RV): The volume of air remaining in the lungs following maximal forceful
expiration (Average = 1,200 ml). - - Total Lung Capacity (Volume) (TLC): The sum of the inspiratory reserve volume, tidal
volume, expiratory reserve volume and residual volume (Average = 6,000 ml). TLC = IRV + TV + ERV + RV or TLC = VC + RV
- Functional Residual Capacity (FRC): The amount of air left in the lung after a normal expiration. FRC = RV + ERV or FRC = TLC – RV
Checkpoint: Give the physiological name and abbreviation for each of these:
• The amount of air that moves in or out of the lungs during any one normal breathing cycle:
_______________________________
• The additional air that can be breathed in after normal inspiration: _______________________________
• The amount of additional air that can be breathed out after normal expiration: _______________________________
• The amount of additional air that CANNOT be exhaled out of the lungs:
_______________________________ By definition, which is larger, Tidal Volume or Vital Capacity?

Page 11.5
A visual representation of these terms is presented in Figure 1. The amounts given for the various volumes and capacities are those for a young, average male. Actual values will vary from subject to subject with the values for females usually being about 25% less than those for males. Notice that the values called “capacities” can be obtained by adding two or more volumes together.
6000 ml
2800 ml
2300 ml
1200 ml
Spirometry to Measure Breathing Volumes
A spirometer is a device used to measure lung volumes. A wet spirometer, so named because water is used to form a low friction seal between a bell float chamber and the environmental air, can be used for this purpose. A simple dry spirometer is often used in a clinic or hospital to assess a patient’s respiratory function after surgery. We will be using a mouthpiece that measures air flow per time. This measurement is then converted to volumes and recorded by a computer program (IWorx). A Sanborn respirometer can be used to assess these values and also to determine oxygen consumption by an individual. Take the time to look at each of these instruments in the lab and to understand how each works. Figure 2 shows these three types of instruments.
The volumes presented in Figure 1 are average numbers for young, healthy males. These values can vary greatly and are affected by the ventilation habits of the subject and the position of the subject during measurement. Heavy breathing due to exercise usually decreases the IRV and increases the TV. The residual volume cannot be emptied from the lung of a healthy individual and thus cannot be measured directly with a spirometer.
Many breathing disorders can be detected by noting abnormalities in the volumes and capacities that we will be measuring in this lab activity. For example, a low Vital Capacity may indicate a loss of distensible lung tissue which could be caused by disorders such as pneumonia, pulmonary restrictions, bronchiogenic carcinoma, or pulmonary congestion. Emphysema will cause the TV and FRC to increase and the IRV to decrease.
IRV
IRC TV VC
ERV
FRC
RV RV
Figure 1. A spirogram of lung volumes and capacities

Page 11.6
We will also be measuring the Forced Expiratory Volume (FEV1) in these activities. This is a measurement of the rate of airflow. The rate of air flow is most dramatically affected by changes in the conductive zone of the respiratory system. The subject inhales completely and then exhales as forcefully and rapidly as possible while the FEV is measured. The FEV is usually expressed as the percent of the VC expelled per unit of time. The percent of the VC expelled at one second is the FEV1 and this value should be 75-85% of the VC for a normal young adult. The FEV2 should be 94% of the VC and the FEV3 should be about 97% of the VC. The FEV test can indicate obstructive respiratory problems such as asthma. If the VC is normal and the FEV is below normal, the subject may have an airway obstruction or restriction.
Checkpoint: Why would asthma decrease a person’s FEV1?

Page 11.7
A. B. C. D.
ACTIVITIES 3 & 4. Increasing the Length of the Airways and Breathing and Cardiac Function. During these two activities, we will investigate the impact of increasing the length of the airways on the measured volumes and assess the impact of breathing on cardiac function. For many people, heart rate is different at different phases of the breathing cycle. Also, when you take a deep breath, and hold it, the extra air held in your lungs puts pressure on large blood vessels. This decreases blood flow to the heart, which affects the heart rate. Because the heart rate changes, the brain reacts through negative feedback.
All students will perform this activity using the IWorx computer program. Students will work in groups of 2-5 students.
Equipment Required
• PC Computer • iWorx unit, and USB or serial
cable SP-304 Spirometer • FH-300 Spirometer flow head and plastic
tubes PT-104 Pulse plethysmograph • Needle and thread • Nose clips, mouthpieces,
filters 18-24” tubes
Figure 2. Various instruments used to measure lung volumes and oxygen consumption.
A. wet spirometer, B. dry spirometer, C. flow mouthpiece used by the IWorx System D. Sanborn respirometer

Page 11.8
Equipment Setup
1. Connect the iWorx unit to the computer. 2. Firmly push the two air flow tubes onto the two outlets on the flow head. 3. Firmly push the other ends of the two air flow tubes onto the two outlets on the SP
304 spirometer unit. 4. Plug the DIN connector of the spirometer into Channel 4 (Figure 3).
Figure 3. The Spirometer connection to the iWorx214 unit. Note that the airflow tubes arise from the top of the flowhead. Keep these airflow tubes upright.
Start the Software
1. Click the Windows Start menu, move the cursor to Programs and then to the iWorx folder and select LabScribe; or click on the LabScribe icon on the Desktop
2. When the program opens, select Load Group from the Settings menu. 3. When the dialog box appears, select IPLMV3.iws. or SLCCphysiology.iws. (Ask your
lab instructor which to use). Click Load. 4. Click on the Settings menu again and select the Breathing-Rest-Exercise settings file. 5. After a short time, LabScribe will appear on the computer screen as configured by
the Breathing- Rest-Exercise settings.
Before Starting the Measurements 1. The spirometer will monitor breathing from a volunteer. It is important that the
volunteer is healthy and has no history of respiratory or cardiovascular problems. 2. The two outlets on the flow head should always be in the upright position to avoid
problems with condensation developing in the airflow tubes (see Figure 3 for this upright position). Have a member of the group help hold the white tube connected to the flow head to avoid bending the tube (which greatly affects measurement). Also, avoid holding the black box that the tube is connected to. Heating of this box will adversely affect the results.
Keep tube outlets Pointed upward

Page 11.9
3. Turbulence in the flow head will produce a noisy signal. To reduce turbulence, the subject should place their lips around the outside of the opening of the flowhead, or its mouthpiece, or its bacterial filter.
4. Use a clip to prevent air from entering or leaving the nose as the subject is breathing. air that passes through the nose is not included in the volume measurements and causes errors in these values.
5. The settings file, Breathing-Rest-Exercise, programmed LabScribe to display the Airflow of the spirometer on Channel 4, and the Volume on Channel 5. The settings file activates an algorithm designed specifically to convert the airflow data of the iWorx SP-304 spirometer to volume data.
6. Right click on the Volume Channel (CH 5). Select Spirometry and be sure that the Volume option is checked. If it is not checked, select it now.
7. Allow the SP-304 to warm up for 10 minutes before recording for the first time. Do not hold the spirometer amplifier in your hand; the heat of your hand will alter the volumes recorded.
8. Determine which opening of the flowhead should be used to make the deflection on the Airflow channel (CH 4) go up as the subject inhales.
9. Open the Window menu in the LabScribe software, and select Preview. A window displaying the signal coming into Channel 1 of the iWorx unit appears. Click on the arrows above the display to change the channel being viewed in the display to the Airflow channel. Watch the display as the subject inhales. To increase the size of the trace, click AutoScale. The trace on the display should go up as the subject inhales. If the trace goes down during inhalation, breathe through the other end of the flowhead or reverse the airflow tubes on the outlets of the flowhead.

Page 11.10
ACTIVITY 1: Breathing in a Resting Volunteer Objective: To measure breathing parameters in a resting individual. Procedure
1. The subject should sit quietly and become accustomed to breathing through the spirometer. They should be breathing normally before any recordings are made. Remember to hold the flowhead so that the outlets are on top.
2. Have the subject remove the flowhead from their mouth. They should hold it at the same level as their mouth, but in a position that prevents their breath or any other airflow from moving through the flowhead. Note: The LabScribe software will zero the Volume channel during the first five seconds of recording. No air should be moving through the flow head during this time.
3. Click Start. Type "Resting" in the comment line to the right of the Mark button. After waiting five seconds for the Volume channel to zero, have the subject place the flowhead in their mouth and begin breathing. Press the Enter key on the keyboard. Click the AutoScale buttons for the Air Flow (CH 4) and Volume (CH 5) channels. Notice the slowly moving wave on the Volume channel. Record 5 breaths, which normally takes about 30 seconds. During this time, the Volume channel may automatically reset itself to zero; which it will do every 30 seconds after the recording begins.
4. Type "Maximum" on the comment line. Press the Enter key on the keyboard as the subject inhales as much as possible. As quickly as possible after reaching their maximum inhalation volume, the subject should exhale as quickly and as completely as possible.
5. The volunteer should return to normal breathing through the spirometer. 6. Click Stop to halt recording.

Page 11.11
Data analysis for normal breathing
1. While still in the main window, scroll the data until the beginning of the first breathing cycle appears on the Main window. Adjust the Display Time (Figure 4) so that two complete breathing cycles appear on the window. As you do the data analysis, you will be gathering data to fill in Table 1 in the Data Sheet.
2. Click the 2-Cursor icon (Figure 4), so that two blue vertical lines appear over the recording window.
3. Drag the blue cursor lines left and right so that the two complete breathing cycles are located between the two blue lines.
4. Click the Analysis icon (Figure 4) to open the window.
Figure 4. The LabScribe toolbar.
Measuring the Breathing Parameters
1. Display only the Volume (CH 5) by clicking and deselecting all the other channels in Display Channel list, on the left side of the Analysis window. Select Title, V2-V1, T2-T1, max_dv/dt, and min_dv/dt from the Table Functions list.
2. Use the mouse to click and drag the cursors over each of the five breathing cycles to measure the following parameters. For each parameter, you will have 5 measurements, one for each breath. You will then find the average of these 5 measurements.
3. This data can be entered into the Journal by either typing the titles and values directly or by using the right-click menu. Place the cursors to take measurements; then, select Add Title to Journal or Add Data to Journal from the right click menu to add the measurements to the Journal.
You will enter this information, and information from subsequent measurements, into Table 1 of your Data Sheet, to have a central place to see your data regarding breathing.

Page 11.12
A. Tidal Volume (TV): the amplitude of the breathing cycle. Place the one cursor at the
trough (low point) prior to the inhalation, and the second cursor to the peak of the cycle. The value, V2-V1, is the Tidal Volume (Figure 5.)
Figure 5. The Volume displayed in the Analysis window; an upward deflection represents inspiration. The cursors are positioned on the trough and the peak of the signal to measure the tidal volume (V2-V1).
B. Period: the duration of each breathing cycle. The duration can be measured either
between peaks or troughs. The value T2-T1 is the Period (Figure 6).
Figure 6. The Volume displayed in the Analysis window; an upward deflection represents inspiration. The cursors are positioned on the peaks of successive signals to measure the time interval or period (T2-T1).

Page 11.13
C. Maximum Inspiratory Flow: the maximum rate of air movement during inhalation. Place the cursors on either side of the steepest portion of the volume curve recorded during inhalation. The value, max dv/dt, is the Maximum Inspiratory Flow rate (Figure 7).
Figure 7. The Volume displayed in the Analysis window. The cursors are positioned on the steepest part of the inhalation slope to represent Maximum Inspiratory Flow rate (max dv/dt).
D. Maximum Expiratory Flow: the maximum rate of air movement during exhalation. Place the cursors on either side of the steepest portion of the volume curve recorded during exhalation. The value, min dv/dt, is the Maximum Expiratory Flow rate. Min dv/dt is used since the exhalation curve has a downward or negative slope.

Page 11.14
Data analysis for maximum breathing
1. Scroll the data in the Analysis window until the "Maximum" breathing cycle appears in the window. Adjust the Display Time (Figure 4) so the complete cycle appears on the window, from the normal tidal volume (or baseline) before the maximum inhalation to the flat line after the subject has completely expelled all the air from their lungs. Your data may look something like Figure 8.
2. Click the 2-Cursor icon (Figure 4), so that two blue vertical lines appear over the Analysis window. Select Title, V2-V1,T2-T1, max_dv/dt, and min_dv/dt from the Table Functions list.
3. Drag the blue cursor lines left and right to measure; Tidal Volume (TV), Inspiratory Reserve (IR), Expiratory Reserve (ER), and the Vital Capacity (VC) (Figure 8). Also, measure maximum rates for inspiratory and expiratory flows.
Figure 8. The Volume displayed in the Analysis window; an upward deflection represents inspiration. The trace shows a normal breathing cycle (left) and then a forced inspiration and expiration (right); labels show tidal volume (TV), inspiratory reserve volume (IR), expiratory reserve volume (ER), vital capacity (VC), and Forced Expiratory Volume at 1 Second (FEV(1)).
4. Place a cursor on the point in the maximum volume trace where the maximum inspiratory volume is reached. Use the T2-T1 function to place the second cursor at a point that is one second after the position of the first cursor. The V2-V1 value for these two cursors equals the Forced Expiratory Volume at 1 Second or FEV(1)
Checkpoint: Record your resting data in the Data Tables. After measuring the subject's breathing parameters, record your data in the ‘resting column of Table 1 in your Data Sheet. Which measurements do you predict with change after exercise and why?

Page 11.15
ACTIVITY 2: Breathing Immediately After Exercise Objective: To measure breathing parameters after exercise.
Procedure
1. For this exercise, use the same subject whose resting breathing parameters have already been measured. Attach a clean flowhead to the spirometer.
2. The volunteer should exercise to sufficiently elevate breathing rate, but with minimal class disruption. Running up and down flights of stairs is a good method.
3. The volunteer should immediately sit down after concluding exercise. Click Start. Type "After Exercise" on the comment line to the right of the Mark button.
4. After waiting five seconds for the Volume channel to zero, have the subject place the flowhead in their mouth and begin breathing. Press the Enter key on the keyboard. Record five complete breathing cycles. Click the AutoScale buttons for the Air Flow (CH 4) and Volume (CH 5) channels.
Checkpoint: Data analysis
1. Use the mean duration of the breathing cycles to calculate breathing rate:
Breathing Rate (Breaths/minute) = 60seconds/minute) mean duration (seconds/breath)
2. Multiply the mean tidal volume by the breathing rate to calculate the volume of air passing in and out of the resting subject's lungs each minute. This value is the minute ventilation.
3. Determine the ratio of FEV(1) to VC. Normally, FEV(1) is compared to the Forced Ventilatory Capacity (FVC) which equals the Predicted Vital Capacity; but, for our purposes will use the actual Vital Capacity (VC). FEV(1)/FVC is an indicator of the severity of pulmonary impairment due to obstructions; any value greater than 65% is considered normal.

Page 11.16
5. Type "Maximum" on the comment line. Press the Enter key on the keyboard as the subject inhales as much as possible. As quickly as possible after reaching their maximum inhalation volume, the subject should exhale as quickly and as completely as possible.
6. The volunteer should breathe through the spirometer until the volunteer returns to normal breathing.
7. Click Stop to halt recording.
Other Factors that Affect Breathing Patterns
ACTIVITY 3: Increasing the Length of the Airways Objective: To study any changes in breathing patterns when the volunteer breathes through a plastic tube. Procedure
1. Click on the Settings menu again and select the Breathing - Other Factors settings file. 2. Employ a subject whose breathing parameters at rest have been recorded. The subject
should sit in a chair, be relaxed, and accustomed to breathing through the spirometer. Remember to hold the flowhead so that the outlets are on top.
3. Have the subject remove the flowhead from their mouth. Place a 18-24" length of plastic tubing, about the same diameter as the opening of the flowhead, on the end used as the mouthpiece. The flowhead and the tubing should be held at the same level as the subject's mouth, but in a position that prevents their breath or any other airflow from moving through the flowhead.
Checkpoint: Record your after exercise data in the Data Tables. After measuring the subject's breathing parameters immediately after exercise using the same techniques used in Exercise 1, determine Tidal Volume, Breath Duration, Maximum Inspiratory Flow, and Maximum Expiratory Flow from the Volume and record your measurements and calculations in the ‘after exercise’ column of Table 1. Upon observation, which measurements appear to be significantly different after exercise than at rest?

Page 11.17
The LabScribe software will zero the Volume channel during the first five seconds of recording. No air should be moving through the flow head during this time.
4. Click Start. Type "Breathing through a Tube" in the comment line to the right of the Mark button. After waiting five seconds for the Volume channel to zero, have the subject place the end of the tube in their mouth and begin breathing. Press the Enter key on the keyboard. Click the AutoScale buttons for the Air Flow (CH 4) and Volume (CH 5) channels. Record 10 breaths, which normally takes about 1 minute. During this time, the Volume channel may automatically reset itself to zero; which it will do every 30 seconds after the recording begins.
5. Click Stop to halt recording.
Checkpoint: Record your ‘with tubing’ data in the Data Tables. After measuring the subject's breathing parameters with tubing using the same techniques used in Exercise 1 and 2, determine Tidal Volume, Breath Duration, Maximum Inspiratory Flow, and Maximum Expiratory Flow from the Volume and record your measurements and calculations record your measurements in the ‘with tubing’ column of Table 1. Which measurements look to be significantly different with tubing than than at rest? After exercise? Why do you think these measurements differ?

Page 11.18
ACTIVITY 4: Breathing and Cardiac Function Objective: To study changes in heart rate during breathing. Background For many people, heart rate is different at different phases of the breathing cycle. Also, when you take a deep breath, and hold it, the extra air held in your lungs puts pressure on large blood vessels. This decreases blood flow to the heart, which affects the heart rate. Because the heart rate changes, the brain reacts through negative feedback. Procedure
1. Plug the DIN connector on the end of the plethysmograph cable into Channel 3. 2. Place the plethysmograph on the volar surface (where the fingerprints are located) of the
distal segment of the middle finger, and wrap the Velcro strap around the end of the finger to attach the unit firmly in place (Figure 9).
3. As with measuring resting breathing in Activity 1, the subject should be relaxed and accustomed to breathing through the spirometer.
4. Have the subject remove the flowhead from their mouth. They should hold it at the same level as their mouth, but in a position that prevents their breath or any other airflow from moving through the flowhead.
The LabScribe software will zero the Volume channel during the first five seconds of recording. No air should be moving through the flow head during this time.
Figure 9. Attach the spirometer and plethysmograph to the iWorx/214 unit.

Page 11.19
5. Click Start. Type "Resting" in the comment line to the right of the Mark button. After waiting five seconds for the Volume channel to zero, have the subject place the flowhead in their mouth and begin breathing. Press the Enter key on the keyboard. Click the AutoScale buttons for the Pulse (CH 3) and the Air Flow (CH 4) channels.
6. Then, click the AutoScale buttons for the Heart Rate (CH 2) and the Volume (CH 5). channels. During this time, the Volume channel may automatically reset itself to zero; which it will do every 30 seconds after the recording begins. Record about 10 normal breath cycles.
7. Type "Deep Breathing" on the comment line. Ask the subject to breathe slowly and deeply. Press the Enter key on the keyboard. Record about 10 complete breathing cycles.
8. Click Stop to halt recording. Record your data: 9. Scroll the data until the beginning of the first resting breath cycle appears on the Main
window. Adjust the Display Time (Figure 4) so that five complete breath cycles appear on the window. Click the AutoScale buttons on the Heart Rate, Pulse, and Volume channels.
10. Click the 2-Cursor icon (Figure 4), so that two blue vertical lines appear over the recording window.
Figure 10. Heart Rate (upper trace), Pulse (middle trace), and lung Volume (lower trace) during slow, deep breathing. An upward deflection on the Volume channel indicates inhalation; Heart Rate is a computed function of the Pulse.
11. Drag the blue cursor lines left and right so that three complete breath cycles are located between the two blue lines.
12. Click the Analysis icon (Figure 4) to open the Analysis window.

Page 11.20
13. Display the Heart Rate (CH 2) and Volume (CH 5) by clicking and deselecting all the other channels in Display Channel list, on the left side of the Analysis window. Select Title, Value1, Value2, Time1, Time2, V2-V1, T2-T1 from the Table Functions list. Select Heart Rate from the Value from Ch list.
14. Use the mouse to click and drag the cursors over each of the three breathing cycles to measure the following parameters.
a. Heart rate at the beginning of inspiration. b. Heart rate at the end of inspiration. c. 2 or 3 evenly spaced heart rates taken between the beginning and end of
inspiration. d. 2 or 3 evenly spaced heart rates taken between the beginning and end of expiration.
Additional Experiments Try the following experiments to further examine the link between breathing and heart rate:
1. (Optional)To examine the effects of gravity, repeat the deep breathing experiment with the subject lying on their back. Are the effects on heart rate as pronounced?
2. Have the volunteer breathe out and then go through the motions to breathe in but close the mouth and nose--i.e. lower the diaphragm and raise the ribs to inflate the thorax, but do not allow any air into the lungs. This will produce a negative pressure in the thoracic cavity. What is the effect on heart rate?
3. Have the volunteer breathe in and then hold their breath as long as they can (this is the Valsalva maneuver). Record breathing and finger pulse during apnea (breath holding) and during recovery.
Checkpoint:. Record the measurements from number 14 (above) in Table 2 of your Data Sheet and answer the following questions.
1. Did you see any major changes in heart rate? 2. Were the changes during inspiration or expiration? 3. If you noticed changes, can you describe the reason for the changes in heart
rate?