J LIVER FUNCTION TESTS Surveynatal period with respect to liver function tests have been summarized...
Transcript of J LIVER FUNCTION TESTS Surveynatal period with respect to liver function tests have been summarized...
255
J
LIVER FUNCTION TESTSA Survey of Some Recent Work
By E. KAWERAU, M.B., M.Sc.(Dub.), A.R.I.C.Senior Lecturer in Chemical Pathology, St. Mary's Hospital, London, W.2.
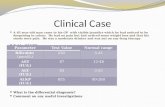
TABLE I
Alternate orTest Indication Supplementary
Procedure
Plasma alkaline phosphataseTotal serum bilirubin To assess the degree DuodenalTotal serum cholesterol of biliary obstruction intubationUrine bilirubin
Direct bilirubin percentage LIVER
fBromsulphalein clearance BIOPSY\ Plasma cholinesterase level Specific tests of
Galactose tolerance parenchymatous\ Benzoic acid detoxication liver damagePlasma prothrombin levelUrinary urobilinogen
Flocculation Tests:( fThymol turbidity
\Cephalin-cholesterol Non-specific tests SERUM PROTEIN' Thymol iflocculation of parenchymatous IONOPHORESIS(B) Zinc sulphate turbidity liver damage (on filter paper)
Gamma flocculation
For the last 30 years an evaluation of liverfunction has been attempted by various chemicaland physiological tests. Many of these are nowobsolete and reference to them is omitted. In re-cent years an interim study has been undertakenby a variety of new methods of investigation,notably electrophoresis, which have materiallyassisted in the diagnosis and treatment of liverdisorders. For the purpose of this survey, there-fore, only work of recent date is included.Much information is contained in the excellent
reviews ofthis subject that have appeared in the lastthree years; in particular the paper by Popper andSchaffner (1950), the Ciba Foundation Sym-posium on Liver Disease (Sherlock and Wolsten-holme, 1951), the survey of cirrhosis by Sherlock(this journal, 1950) and the infective hepatitis re-port of the Medical Research Council (No. 273,I951). The difficulties encountered in the neo-natal period with respect to liver function testshave been summarized by Harris (1952). In ad-dition, a number of important contributions havebeen made to our knowledge of the behaviour of
the serum protein fractions in liver disease, inparticular the elctrophoretic studies of Popper etal. (I95I), Franklin et al. (I95i), Ricketts andSterling (1949, I951) and Wuhrmann et al. (1950).
It is not without significance that during thesame period at least three papers have appearedwith the sole object of pointing out the pitfalls(Kramer, 950) and misuses of liver function tests.At the same time the number of new tests is in-creasing every year. The biochemist has no easytask as he has to decide which of the many testsmean precisely the same thing and are thereforeredundant, as unnecessary laboratory investiga-tions have often resulted in confusion rather thanincreased clarity in diagnosis. Should we havesix, nine or 20 simultaneous tests of liver function?With the ever widening circle of suspected liverdamage (e.g. infectious mononucleosis) a restric-tion of tests becomes necessary unless especialfacilities for these investigations are provided.Table i is an attempt to classify approximatelyequivalent tests. In the writer's opinion testsgrouped together in a bracket though different in
copyright. on A
pril 5, 2020 by guest. Protected by
http://pmj.bm
j.com/
Postgrad M
ed J: first published as 10.1136/pgmj.29.331.255 on 1 M
ay 1953. Dow
nloaded from
POSTGRADUATE MEDICAL JOURNAL
character have approximately the same clinicalvalue, in other words only one from each groupneed to be done in any particular investigation.Biliary Obstruction
It is not sufficient to assess the extent of biliaryobstruction alone as in every case of jaundicehepatocellular damage may be present as well.The pure form of extrahepatic obstruction is atleast four times less common than intrahepaticobstruction with concomitant cell pathology.Severe parenchymatous liver damage is a strongcontraindication to any form of surgical inter-vention including needle biopsy. Hence, a com-plete investigation has to be made in every case.
Total serum bilirubin and the direct reactingbilirubin percentage. The amount of bilirubindiazotizing within one, ten or 15 minutes in thevan den Bergh reaction is measured quantitatively.This direct (or prompt) reacting bilirubin is in-dependent of the concentration of circulating bili-rubin and when expressed as a percentage of thetotal gives more useful information than theformer vague designations ' direct,' ' biphasic'and 'indirect' van den Bergh reaction. Thedirect reacting bilirubin (Na-bilirubinate) reachesthe highest levels in complete extrahepatic obstruc-tion. Incomplete extrahepatic obstruction andobstruction arising from acute or chronic in-flammatory liver disease gives rise to high ormoderate increases in total bilirubin of which halfor more is of the fast diazotizing form. There ismuch overlapping of results, and an estimation ofthe direct reacting bilirubin percentage is of littleuse in the differential diagnosis ofjaundice whetherhaemolytic, obstructive or viral in origin (Klatskinand Drill, 1950). All that one can say is thatwhen the ratio of the direct reacting bilirubin tothe total bilirubin is less than 40, obstructivejaundice can be excluded (Gray, I947).The position is different where a diagnosis has
been established or where the aim is to differentiateextrahepatic obstruction from some other intra-abdominal condition, e.g. pancreatitis. Here posi-tive not negative findings lead in diagnosis andprognosis. Schalm (1952), using as criterion ahigh io minute direct reacting bilirubin per-centage, has shown that this may be used to con-firm an attack of cholelithiasis in the absence ofvisible jaundice and bilirubinuria.Whether one postulates a renal threshold for
bilirubin (Neye, 1952) or not (Watson, 1946,I95I; Pollock, I951) the direct reacting bilirubinalways appears early in the urine where it can beidentified by the sensitive Harrison-Fouchet orHunter reaction. These urine tests are usefulbefore frank jaundice develops and during con-valescence.
Total serum cholesterol. In progressive portalcirrhosis and hepatic insufficiency cholesterolvalues are normal or low, but in biliary cirrhosisand extrahepatic obstruction values are generallyhigh. It is a useful confirmatory test especiallywhen obstruction occurs in early infancy. Inadults a high serum cholesterol value should beinterpreted with care even in the presence ofjaundice as numerous other conditions may causea rise in serum cholesterol, e.g. hypothyroidism.
Alkaline phosphatase. It is a normal functionof the polygonal cells of the liver to excrete serumalkaline phosphatase through the bile channels(LaVeen et al., I950). Obstruction of thesepassages causes failure of excretion of the enzymeand correspondingly high levels in the blbod, theamount being roughly proportional to the degreeof obstruction. Hence, moderate elevations areseen in hepatitis and very high values in extra-hepatic obstruction.Freeman (1951) has shown in dogs that common
bile duct obstruction gives rise to a much higheralkaline phosphatase concentration in the bloodthan total hepatectomy. This has been interpretedto mean that the liver cells themselves synthesizethe enzyme and add a contribution to the serum.It must be remembered, however, that Sherlockand Walshe (I947) in their very searching studydid not find any histological evidence to supportthis suggestion, though they admit that histo-logical studies of material from cases of obstruc-tive jaundice can yield little information on thispoint.At present, therefore, it does not seem un-
reasonable to assume that serum alkaline phos-phatase is of multiple origin, the major contribu-tions being derived from the tissues that mostactively secrete it, notably bone, 'intestines, thekidneys and liver.A dual function on part of the liver cells (secre-
tion and excretion) would fit the clinical evidencebest. In infective hepatitis we deal with a partialfailure of both mechanisms. The observed en-zyme rise in the serum representing the balancebetween the enzyme lowering effect of hepato-.cellular failure on the one hand and the enzymeraising effect of intrahepatic obstruction on theother. In extrahepatic obstruction the excretorymechanism may fail completely whereas thesecretory mechanism since it is mainly non-hepatic remains undisturbed.
Twenty-five King-Armstrong units of alkalinephosphatase have been taken as the dividing linebetween obstructive and non-obstructive jaundice.Baker (I95ib), in conformity with other workers,found that in infective hepatitis the serum alkalinephosphatase values were below 30 units. Inbiliary obstruction he found that cases of malig-
256 May I953copyright.
on April 5, 2020 by guest. P
rotected byhttp://pm
j.bmj.com
/P
ostgrad Med J: first published as 10.1136/pgm
j.29.331.255 on 1 May 1953. D
ownloaded from
KAWERAU: Liver Function Tests
nant obstruction gave more consistently highvalues than cases of mechanical obstruction. Thisis in agreement with the observations by Ricketts(1951) who found that even cases of metastaticcarcinoma with practically normal liver functiontests had a raised serum alkaline phosphatasethough there was no direct evidence of obstruction.Many forms of bone disease, e.g. rickets, Paget's
disease, malignancy, etc., may give rise to a highserum alkaline phosphatase level and these con-ditions should be excluded before the test is con-sidered in the differential diagnosis of liver disease.
Damage to Liver Cells. Specific TestsMany of the metabolic functions of the liver
have been made the basis of a function test. Allthese tests are handicapped from the start as theyrely on either single or serial estimations of theplasma concentration of a liver metabolite. Thespecificity of the test is thereby reduced as theplasma level of liver metabolites is controlledapart from factors regulating circulatory volumeand the metabolic activity of other organs, bydiverse hormonal influences. It is not surprising,therefore, that relatively uncommon substances tothe liver like galactose and complete strangers likebromsulphalein have yielded more reliable evidenceof liver dysfunction than tests employing glucose,fructose or benzoic acid.Much work has been done with these more
specific tests for parenchymatous liver damage, butit has not always been realized that these testsmust be performed under standard conditions.Previous dietary regimen, recumbency whilst thetest is being done, size of the test dose, whetherthe patient is afebrile or not and other factorsaffect the reproducibility of results (Kramer, I950).Under comparable conditions repeat tests showgood agreement (Mendeloff et al., I949).
The direct reacting bilirubin percentage. Livercells transform indirect bilirubin into the directform and excrete the latter. This mechanism be-comes deranged when the parenchyma is affectedand the direct reacting bilirubin accumulates in theblood. This increase apparently occurs at theexpense of the indirect bilirubin fraction as thechange takes place before there is'a significant risein total bilirubin. In infective hepatitis the directreacting bilirubin increases early and reaches apeak value during the pre-icteric stage of the ill-ness. An estimation of this fraction is therefore amost valuable test in the early diagnosis of thedisease (Pollock, 1945, 1951). Similarly, the testmay be employed during convalescence from in-fective hepatitis, when a persistently high directreacting fraction in spite of a normal total bilirubinlevel indicates continuous activity of the patho-logical process (Schaffner et al., I950).
The bromsulphalein test. This is considered thebest general screening test. It will reveal the im-maturity of liver function during the neonatalperiod (Mollison and Cutbush, 1949), detectparenchymatous liver damage in cases of latentcirrhosis (Ricketts and Kirsner, 1951) and hepatitiswithout jaundice and show a positive correlationwith liver disease arising from focal lesions, e.g.cysts, metastatic nodules, etc. (Ricketts, 195 ).The test should always be performed in suspectedmalignancy as when positive it is a strong contra-indication to surgical intervention (Magath, 1951).The usual test dose is 5 mg. per kg. of body
weight. This large amount has been objected toby Lorber and Shay (I951) on the grounds that itgives rise to a marked entero-hepatic circulation ofthe dye, which interferes with the interpretation ofresults. Owen (195I), however, could not detectany evidence of an entero-hepatic circulation afterintroducing bromsulphalein into the stomach orduodenum and only the 5 mg. dose imposes asufficient load on the liver to make the testclinically reliable. The liver clearance rate forbromsulphalein is approximately the same as forbilirubin (Cantarow et al., 1948).The results can be expressed either as the
amount of dye retained, for which calculation aplasma volume of 50 ml. per kg. is assumed, orthey can be given as the clearance rate employingthe method of Goodman (I952), which is basedon the formulas developed by Lewis (1950).The test bears a good relationship to morpho-
logical changes in the liver except during the re-covery period when the test may remain unalteredfor years despite steady clinical improvement(Patek, 1950).
The detoxication tests. Quick's hippuric acidtest has often been criticized, but newer detoxica-tion tests employing p-aminobenzoic acid (Deissand Cohen, 1950) orp-hydroxyphenylpyruvic acid(Felix et al., I951) do not present a material ad-vance from the clinical point of view, howeverinteresting the biochemical findings. The generaltrend in parenchymatous liver disease is forglycine and sulphuric acid conjugation to fail andto become replaced by the glycuronic acid mechan-ism (Hartmann, I951). In response to thestandard test dose of benzoic acid, therefore,hippuric acid excretion is diminished with acorresponding increase in the excretion of benzoyl-glycuronide (Snapper et al., I951). As the kidneysalso take part in hippuric acid synthesis the testhas to be interpreted with care. Its main value isin the evaluation of liver function when jaundicerenders other tests unsuitable and in prognosis.Where the test is employed routinely throughoutthe course of the illness it serves as a reliable index
May 1953 257
copyright. on A
pril 5, 2020 by guest. Protected by
http://pmj.bm
j.com/
Postgrad M
ed J: first published as 10.1136/pgmj.29.331.255 on 1 M
ay 1953. Dow
nloaded from
POSTGRADUATE MEDICAL JOURNAL
to the rate of recovery. It is valueless as a meansof differential diagnosis (Peters et al., I950).
The galactose tolerance and index tests. Theblood galactose level is less affected by hormonalinfluences than the blood glucose level as is seenfrom the absence of the physiological Staub-Traugott phenomenon (Lauchenauer, 1950). Boththe intravenous and oral tests yield reliable results,though abnormal findings should not be inter-preted on a quantitative basis, i.e. the test lacksprognostic significance. In differential diagnosisit is only of value when cases of uncomplicatedearly extrahepatic obstruction are considered asthere is a considerable overlapping of results be-tween the hepatitis, cirrhosis and late obstructivegroup of conditions. As this test has a betterphysiological basis than the bromsulphalein test ithas been employed preferentially in testing drugssuspected of hepatotoxic action (Bostr6m andGardell, 1950).
The plasma prothrombin level in response tovitamin K. This test though not a very sensitiveone gives a fair quantitative indication of parenchy-matous damage; a level 15 per cent. below normalbeing considered slight damage and 25 per cent.below normal severe damage. The results areaffected to some extent by the method of estima-tion, some authors having declared Quick's originalmethod unsuitable for the purpose (Perlick, 1951).Positive findings alone are useful. The main valueof the test is to the surgeon who will be unwise tooperate when faced with an unfavourable labora-tory report. The test is not sensitive enough toreveal the extent of parenchymatous damage in in-fective hepatitis, at least 50 per cent. of the casesgiving a normal response (Gottlebe, 1950).
Theplasma cholinesterase level. The protagonistsof this comparatively new test are uniformly inagreement with its value in liver disease (Alcalde,1950; Wilson et al., 1952). It is, they say, thebest means of testing the liver's ability to synthesizeprotein. A low level of plasma cholinesteraseindicates parenchymatous damage, provided myas-thenia gravis has been excluded from the diagnosis.The test is of greatest value in the chronic case,especially in portal cirrhosis. The plasma enzymelevel is low during the active stage of infectivehepatitis and during a relapse. Normal values areencountered in cholangiohepatitis unless infectionsupervenes. In extrahepatic obstruction the lowvalues are not seen until the obstruction has per-sisted for at least two months. The test is valuableboth from a diagnostic and prognostic view andwith the simplified technique for measuring theenzyme that was introduced by Michel (1949)deserves greater popularity in the future and mightwell replace some of the less specific flocculationtests.
Urinary urobilinogen excretion. Baumgirtel(1950) maintains that bilirubin is reduced tostercobilin in the gut and not to urobilinogen andhe does not believe in an enterohepatic circulationof urobilinogen. His ideas though gaining groundon the Continent have not been accepted here orin America, where Watson has refuted Baum-girtel's claims (see Ciba Symposium, p. 221).Healthy liver cells re-oxidize urobilinogen tobilirubin.An interruption of the enterohepatic circulation
of urobilinogen may be due either to biliary ob-struction or a hepato-cellular' block,' the formerbeing associated with a total lack of urinary uro-bilinogen and the latter with an augmented bloodlevel and renal excretion of this substance. Thepeak of urobilinogen excretion is in the earlyafternoon (Suavely and Unglaub, I952), hencespecimens for routine testing should be collectedat this time.
In infective hepatitis urinary urobilinogen ex-cretion is increased in the pre-icteric stage andwhen jaundice is on the decline, but fails at theheight of jaundice on account of intrahepatic ob-struction. This gives rise to the characteristiccamel's back curve in serial excretion studies.Obstruction from stone is rarely complete, hencesome urobilinogen can be detected in the urine;in malignant obstruction, however, the test isusually quite negative (Baker, 195 a). This dis-tinctive behaviour is of considerable diagnosticimportance to the surgeon. In progressive andactive cirrhosis parenchymatous damage blocks thepath and the amount of urobilinogen found in theurine is an indication of the severity of the damage.Non-specific Tests
These tests depend on alterations in the serumprotein fractions and they are called non-specificbecause as F. Wuhrmann has rightly pointed out(Ciba Symposium, p. 72), 'all disease withoutexception decreases serum albumin and simul-taneously increases the globulin, never the con-trary.' The liver, however, plays the dominantrole in plasma protein synthesis and manufacturesexclusively all the albumin, prothrombin, alpha-globulin and some enzyme proteins (Roberts andWhite, I949). Isotope studies in the rat haveshown that most of the fibrinogen and 80 per cent.of the remaining globulins are also synthesized bythe liver (Miller et al., I95I).We have several methods for studying the
serum protein fractions but only two will be dis-cussed here. First, the flocculation tests whichdepend less on quantitative than qualitativealterations of the proteins, and secondly the iono-phoretic method (electrophoresis) which princip-ally measures quantitative alterations but may
May 1953258copyright.
on April 5, 2020 by guest. P
rotected byhttp://pm
j.bmj.com
/P
ostgrad Med J: first published as 10.1136/pgm
j.29.331.255 on 1 May 1953. D
ownloaded from
KAWERAU: Liver Function Tests
detect qualitative changes when they are pro-nounced. The two methods, therefore, are tosome extent complementary to each other.
The flocculation tests. The literature is too vastto be reviewed here in detail, and for recent dis-cussions of this topic the reader is referred tothe papers by Sophian and Connolly (1952), Kihnet al. (I95I), Popper et al. (I95I), Popper andSchaffner (1950) and Maclagan (I948; CibaSymposium, 195 ).
Sufficient data have accumulated since theintroduction of most of the flocculation tests toput us into a position to do some rigorous pruning.It is the writer's considered opinion that for onereason or another that cannot be discussed herein detail we can now afford to discard the followingas liver function tests: The formol gel andTakata-Ara reactions, the Weltmann coagulationband, the colloidal gold and colloidal silver re-actions and probably the cephalin-cholesterol andcadmium sulphate reactions. The remainder ofthe flocculation tests can be divided into twogroups: (A) the hypersensitive and (B) the sen-sitive group (see Table i). To the former belongthe thymol turbidity and cephalin-cholesteroltests and to the latter the gamma flocculation,thymol flocculation and zinc sulphate tests.Group (A) tests will detect a minimal amount
of liver damage but owing to their high sensitivitylack specificity and are less useful in differentialdiagnosis. Hence, when the aim is to differentiatebetween infective hepatitis and extrahepatic ob-struction, group (B) tests give more reliable in-formation.
In a positive flocculation test visible colloidaggregates are formed. This is due to a re-duction in serum albumin and a simultaneous in-crease in the gamma (and beta) globulins. Apositive flocculation test can be reversed by additionof sufficient albumin which is said to exert a pro-tective action on the colloid system. The magni-tude of the thymol reaction depends in addition onthe amount of serum lipid; it is a more complexreaction.
It is not always realized that the tests in group(A) and the thymol flocculation test must be per-formed under standard conditions, i.e. blood froma fasting patient must be used and heparin mustnot be used as the anticoagulant. The laboratoryreagents should be standardized (Kibrick et al.,1952) when possible.
Fatty metamorphosis of the liver and fibroustissue infiltration unaccompanied by infection orinflammatory reaction do not give rise to positiveflocculation tests (Moyer and Wurl, I95 ; Ricketts,I951). A general mesenchymal reaction withincreased activity and proliferation of the Kupffercells must take place before flocculation tests be-
come positive, and such a reaction is not exclusiveto liver disease. This explains on the one hand thenegative tests obtained in biliary cirrhosis, portalcirrhosis without symptoms (Baker, 195Ia), Banti'sdisease (Nussey, I949) and focal lesions of theliver; and on the other, the so-called false positivereactions that may be witnessed in myelomatosis,Kala-azar, rheumatoid arthritis, etc. Kupffercells also proliferate in biliary obstruction but theyare devoid of cytoplasmic basophilic granules,which suggests that the loading with regurgitatedbiliary products (lecithin) suppresses their specificactivity (Popper, Ciba Symposium, 1951), and inconsequence tht flocculation tests remain negative.A false negative flocculation reaction may alsooccur when there is a great increase in the alpha-one-globulin as it appears to be able to exert aprotective influence on the test similar to albumin(Seitz, I950).
In summing up one may say that to follow thecourse of acute infective hepatitis a test of group(A) is best. The latter should be substituted byone of the tests of group (B) during convalescenceas they more clearly indicate smouldering activity,a slow rise in gamma globulins and the transitionto cirrhosis.Serum protein ionophoresis. For clinical pur-
poses the classical Tiselius method has been super-seded by the filter paper method which is bestknown in this country from the work of Flynn andde Mayo (I95 ). Filter paper ionophoresis is nowused routinely in some laboratories for the separateestimation of the serum protein fractions: Paralleldeterminations by the two methods have shownthat the filter paper method gives basically thesame results as the classical method (K6iw et al.,1952), except for the beta-globulin, for which atruer value is obtained by the paper method. Itseems profitable, therefore, to review as briefly aspossible what has been learned from the classicalmethod as most of this knowledge can be applieddirectly to the interpretation of results obtained bythe paper method.A good ionophoretic separation shows us at
least six distinct fractions, which in order of speedof movement read as follow: albumin, alpha-one-globulin, alpha-two-globulin,. beta-globulin,gamma-one-globulin and gamma-two-globulin.Some pathological sera may show a double betafraction. The early hopes that individual patternsmight be detected for the various liver diseaseshave not been fulfilled; nevertheless, information ofconsiderable value can be derived from thefractionation. It enables us to determine cor-rectly the albumin:gamma-globulin ratio, which isdifficult to obtain by the single stage salting-outprocedure as the latter method precipitates thealpha-one-globulin with the albumin fraction. A
May I953 259copyright.
on April 5, 2020 by guest. P
rotected byhttp://pm
j.bmj.com
/P
ostgrad Med J: first published as 10.1136/pgm
j.29.331.255 on 1 May 1953. D
ownloaded from
POSTGRADUATE MEDICAL JOURNAL
true albumin: gamma-globulin ratio has consider-able diagnostic and prognostic value (Popper etal., I951), whereas the ordinary albumin:globulinratio is of little value in liver disease (Rafsky et al.,1950; Baker, 1951; Sophian and Connolly, 1952).The failure of the crude albumin:globulin ratio islargely due to the erratic behaviour of both thealpha-globulins as also to the fact that the betafraction is increased in obstructive jaundice aswell as in toxic and infective hepatitis (Popper etal., I951).The range of normal values for the individual
protein fractions is quoted from the paper ofPopper, Bean, de la Huerga, Franklin, Tsumagari,Routh and Steigmann (I95I).Albumin: In normal people this should be above 3.8
per cent., though in old age the normal limit is some-what lower (Rafsky et al., 1952). Albumin diminishesrapidly in acute infective hepatitis and keeps at a levelabove 3.5 per cent. only in the mildest cases. Thelowest values are seen in portal cirrhosis with sym'ptoms,though in portal cirrhosis without symptoms and inbiliary cirrhosis where the lesions are often well com-pensated by regeneration, normal or borderline valuesare frequently encountered. A. J. Patek (1950) hasshown that in dealing with liver failure the effect oftreatment is better reflected in the serum albumin levelthan in the bromsulphalein test and serves as a, reliableguide to prognosis.
Alpha-globulins: The normal range is 0.7 to x.5 percent. with the alpha-two fraction being slightly more thandouble the alpha-one-globulin. These two fractions areraised in a great number of miscellaneous conditionsand therefore without significance in liver disease.
Beta-globulir-: The normal range is o.5 to I.o percent., though at present it is not certain whether thesefigures are also true for the paper ionophoresis method.Sudan III staining lipid moves with the beta-globulinfraction (Kunkel and Slater, 1952) and in pathologicalsera both are usually found increased together when thebeta fraction is raised. They are raised early in viralhepatitis, almost in proportion to the severity of theillness. Such a relationship is not found in toxic hepatitisor cirrhosis. Some striking elevations are seen in biliarycirrhosis when the classical method is used (lipid plusbeta-globulin) (Nicola, Wuhrmann and Wunderly,I950). According to Popper et al. (I95I), the beta-globulins are elevated in portal cirrhosis and more so inthe jaundiced than the non-jaundiced patient, thoughMartin (1949) reports low or normal values in thesecases.
Fibrinogen: Fibrinogen is difficult to determine by theelectrophoretic method as it travels at the same speedas the gamma-one-globulin (Franklin et al., 1951).Fibrinogen is decreased in liver failure and increasedin portal cirrhosis.
Gamma-globulin: Values above 1.25 per cent. shouldbe considered with suspicion though upper normalvalues of I.44 per cent. are occasionally seen. Thegamma-one fraction was shown by Deutsch et al. (1946)to possess antibody properties; it is normally present inserum. In the ionophoresis diagram it shows up as aplateau rather than a peak. Gamma-one globulin israised a little in infective hepatitis and grossly in cirr-hosis where it may reach values of 6 per cent. or more.Values over 6 per cent. are usually only encountered infatal cases of hepatic failure (Viollier, Ciba Symposium,195I). The gamma-one plateau when raised tends to
overlap with the gamma-two fraction, hence mostauthors only quote total gamma-globulin values.The gamma-globulins are greatly augmented in the
serum during the first three months of life and thisfact accounts for the false positive flocculation tests en-countered during this period (Longsworth et al., I945;Moore et al., 1949).
In summing up one may say that not everypeak in the ionophoresis diagram has always thesame interpretation but that some diseases tend tobe associated with a similar pattern from case tocase (e.g. progressive portal cirrhosis with symp-toms). The clinician should look at the diagramas well as consider the result in percentage orabsolute figures, as the same figure may equallyresult from a tall peak as from a wide plateau,e.g. the tall gamma-globulin peak of multiplemyelomatosis and the broad gamma plateau ofcirrhosis. The ionophoretic serum protein frac-tionation is of especial value in the chronic casewhen repeated flocculation tests and other in-vestigations over a period of time have remainedunaltered or given equivocal results. In thesecases serial serum protein analysis by ionophoresisare the best guide to prognosis.With the wider application of filter paper iono-
phoresis, no doubt more data of critical value willemerge, but even now the opinion has been voicedthat flocculation tests can be dispensed with whenone uses this method (Grassmann, Hannig andKnedel, I95I). This opinion is not shared byMaclagan (Ciba Symposium, I95I) but space for-bids a full discussion of this controversy.
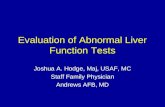
SummaryThe question of how many tests one should use
remains unanswered. Without a careful clinicalhistory and thorough physical examination testsare misleading. At the onset of the illness theproblem is usually one of deciding whether thepatient and his complaint should be treated medic-ally or surgically. For this purpose Popper andSchaffner (1950) have suggested a scheme which isset out in Table 2. Following this initial classifica-tion no further rules can be laid down as anyadditional investigation will depend on the exactnature of the illness and the kind of informationone is anxious to obtain.There are several ancillary methods of in-
vestigating liver disease that cannot be discussedhere in full. The various forms of liver biopsymay be most helpful and for a discussion of theirvalue the reader is referred to the above-mentionedpaper by Popper and Schaffner, the papers byMoyer and Wurl (195I) and Schiff (I95 ). Liverbiopsy is not an infallible guide to diagnosis, prog-nosis or treatment and it is not an absolutely safemethod. The blood picture may also assist in the
260 May 1953copyright.
on April 5, 2020 by guest. P
rotected byhttp://pm
j.bmj.com
/P
ostgrad Med J: first published as 10.1136/pgm
j.29.331.255 on 1 May 1953. D
ownloaded from
May I953 KAWERAU: Liver Function Tests 26
TABLE 2
(AFTER POPPER AND SCHAFFNER)Routine Investigation Interpretation of Results
(i) (A) positive and (B) negativeMEDICAL
(A) Do TWO different tests Exception: A palpable mass is present orfor liver cell damage urinary urobilinogen fluctuates on con-
secutive examinations.(ii) (A) positive and (B) positive
and with abnoxmal with normalflocculation tests flocculation tests
(B) ONE test for obstruc- MEDICAL SURGICALtion to the flow of bile (primary hepatitis(See Table I) with some degree of
obstruction)Exception: Exception:
purulent hepatitis few cases of toxicor cases with pal- hepatitis (arsenic)pable abdominal
mass(iii) (A) negative and (B) positive
SURGICALException: Rarely, when a toxic factor is dis-
covered, or when a history of precedinginfective hepatitis speaks for cholangioliticcirrhosis.
diagnosis. Macrocytic anaemia being common inliver disease on account of the role the liver playsin haemopoiesis. For a detailed account of thechanges in erythrocyte structure that accompanymacrocytic anaemia of liver disease, the reader isreferred to the careful work of Larsen (1948). Thechanges in the white cell picture in infectivehepatitis are discussed by Miles (Medical ResearchCouncil Report, p. 84).ConclusionNo single system of tests will meet all require-
ments. The puzzling case with negative liverfunction tests that does not reveal a tell-tale storyuntil he comes under the classifying eyes of themorbid anatomist, will recur again and again. Butthis does not mean that the tests are unreliable.The evidence merely points to the imperfection ofour knowledge of the basis of most of the tests weemploy. It is hoped that the newer methods maythrow fresh light on this perplexing problem andmake our understanding more complete for thesake of the patient.
BIBLIOGRAPHYALCALDE, J. M. O. (1950), J. Lab. din. Med., 36, 39I.BAKER, J. P. (I95sa), Guy's Hosp. Gazette, o00, 238.BAKER, J. P. (195gb), Ibid., 0oo, 342.BAUMGARTEL, T. (I950), Dtsch. Arch. klin. Med., x97, I39.BOSTROM, H, and GARDELL, S. (I950), Acta physiol. Scand.,
20, 313.CANTAROW, A., WIRTS, C. W., SNAPE, W. J., and MILLER,
L. L. (1948), Amer. J. Physiol., IS4, 21 .
DEISS, W. P., and COHEN, P. P. (I95), J. clin. Invest., 29, I014.DEUTSCH, H. F., ALBERTY, R. A., and GOSBING, L. J.
(I946), J. biol. Chem., x6s, 21.
FELIX, K., LEONHARDI, G, and VON GLASENAPP, I. (1951),Hoppe-Seyl. Z., 287, I33.
FRANKLIN, M., BEAN, W. B., PAUL, W. D., ROUTH, J. I.,DE LA HUERGA, J., and POPPER, H. (x95xa), .. din. Invest.,30, 718.
FRANKLIN, M., BEAN, W. B., PAUL, W. D., ROUTH, J. I.,DE LA HUERGA, J., and POPPER, H. (i95ib), Ibid., 30, 729.
FREEMAN, S. (x95I), Amer. J. Physiol., 164, 792.FLYNN, F. V., and DE MAYO, P. (I95I), Lancet, ii, 235.GOODMAN, R. D. (1952), .. Lab. clin. Med., 40, 531.GOTTLEBE, P. (g95o), Dtsch. Arch. klin. Med., I97, 397.GRASSMANN, W., HANNIG, K., and KNEDEL, M. (I95),
Dtsch. med. Wschr., 76, 333.GRAY, C. H (I947), Quart. J. Med., I6, 135.HARRIS, R. C. (I952), Bull. N.Y. Acad. Med., 28, 721.HARTMANN, F. (I95I), Z. klin. Med., 147, 55I.' Infective Hepatitis,' Medical Research Council Special Report
Series No. 273 (1951), by MAcCALLUM, F. O., McFARLAN,A. M., MILES, J. A. R., POLLOCK, M. R., and WILSON, C.
KIBRICK, A. C. (1952), Am. J. clin. Path., 22, I88.KIHN, L., HANUSCH, A., and DOLITZSCHER, E. (1951), Z.
ges. Inn. Med., 6, o02.KLATSKIN, G, and DRILL, V. A. (i950),.. din. Invest., 29, 660.KOIW, E, WALLENIUS, G., and GRONWALL, A. (1952),
Scand. .. din. Lab. Invest., 4, 47.KRMER, P. (1950), Med. Clinics, North America, 34, 1459.KUNKEL, H. G, and SLATER, R. J. (1952), . ldin. Invest., 31,
677.LARSEN, G (1948), Acta med. Scand., Suppt. 220 (Oslo). -
LAUCHENAUER, C. (195o), Gastroenterologia (Basel), 75, 193.LEVEEN, H. H., TALBOT, L. J., RESTUCCIA, M., and BAR-
BERIO, J. R. (I950), 7. Lab. din. Med., 36, 192.LEWIS, A. E. (I950), Amer. .7 Physiol., 163, 54.LONGSWORTH, L. G., CURTIS, R. M., PEMBROKE, JR.,
R. H. (I945), J. din. Invest., 24, 46.LORBER, S. H., and SHAY, H. (i95I), Amer. .. Med. Sc., 221,
II4.MACLAGAN, N. F. (1948), Brit. med. .7, ii, 892.MACLAGAN, N. F. (I951), in 'Liver Disease,' Ciba Foundation
Symposium, J. & A. Churchill, London.MAGATH, T B. (I95 ), Ibid.MARTIN, N. H. (I949), Brit. J. exp. Path., 30, 23I.MENDELOFF, A. I., KRAMER, P., INGELFINGER, F. J.,
and BRADLEY, S. E. (I949), Gastroenterology, 13, 222.MICHEL, H. 0. (I949), . Lab. clin. Med., 34, 1564.MILES, J. A. R. (I95I), in' Infective Hepatitis,' see above.
copyright. on A
pril 5, 2020 by guest. Protected by
http://pmj.bm
j.com/
Postgrad M
ed J: first published as 10.1136/pgmj.29.331.255 on 1 M
ay 1953. Dow
nloaded from
262 POSTGRADUATE MEDICAL JOURNAL May 1953MILLER, L. L., BLY, C. G., WATSON, M. L., and BALE,W. F. (I9SI), . exp. Med., 94, 431.MOLLISON, P. L., and CUTBUSH, M. (1949), Arch. Dis.
Childh., 24, 7.MOORE, D. H., Du PAU, R. M., and BUXTON, C. L. (x949),Amer. 7. Obst. Gyn., 57, 312.MOYER, J. H., and WURL, O. A. (I951), Amer. 7. Med. Sc., 221,28.NEYE, K. (I952), Dtsch. med. 7., 3, I77.NICOLA, P., WUHRMANN, F., and WUNDERLY, C. (1950),Minerva med., 41, 3.NUSSEY, A. M. (1949), Brit. med. J., ii, 414.OWEN, C. A., JUN. (I95s), .. Lab. cin. Med., 38, 583.PATEK, A. J., JUN. (1950), Advan. Int. Med., 4* 329.PERLICK, E. (I951), Z. ges. exp. Med., Ix6, 540.PETERS, G., and HARMANCI, N. A. (1950), Dtsch. med. Wschr.,
75, 252.POLLOCK, M. R. (1945), Lancet, ii, 626.POLLOCK, M. R. (I95I), in ' Infective Hepatitis,' see above.POPPER, H., and SCHAFFNER, F. (1950), Advan. Int. Med., 4,
357 (395 references).POPPER, H., BEAN, W. B., DE LA HUERGA, J., FRANKLIN,M., TSUMAGARI, Y., ROUTH, J. I., and STEIGMANN,
F. (I95S), Gastroenterology, 17, 138.POPPER, H. (195g), in 'Liver Disease,' Ciba Foundation Sym-
posium, J. A. Churchill, London.RAFSKY, H. A., WEINGARTEN, M., KRIEGER, C. I., STERN,
K. G., and NEWMAN, B. (I950), Gastroenterology, 14, 29.RAFSKY, H. A., BRILL, A. A., STERN, K. G., and COREY,
H. (1952), Amer. 7. med. Sc., 224, 522.RICKETTS, W. E. (I95g), Ibid., 221, 287.RICKETTS, W. E., and STERLING, K. (1x9S), Ibid., 221, 38.
RICKETTS, W. E., and STERLING, K. (1949), J. din. Invest.,28, 1477.
RICKETTS, W. E., and KIRSNER, J. B. (I95S), Gastroenterology.,x7, 184.
ROBERTS, S., and WHITE, A. (1949), J. biol. Chem., io8, 5o5.SCHAFFNER, F., POPPER, H., and STEIGMANN, F. (1950),Amer. J. med. Sc., 219, 307.SCHALM, L. (1952), Lancet, ii, 1153.SCHIFF, L. (I95I), Ann. intern. Med., 34, 948.SEITZ, W. (1950), Med. Monatschr., 4, 241.SHERLOCK, S. (1950), Postgr. med. J., 26, 472.SHERLOCK, S., and WALSHE, V. (I947), J. Path. Bact., 59, 615.SNAPPER, I., ROBINSON, B. D., and ROSENTHAL, D. J.(i95i), J. Mt. Sinai Hosp., 18, 203.SOPHIAN, L. H., and CONNOLLY, V. J. (1952), Amer. J. Digest.Dis., 19, 44.STERLING, K., and RICKETTS, W. E. (I949), 7. din. Invest.,28, 1469.SUAVELY, J. R., and UNGLAUB, W. G. (1952), Med. Clin.
North Amer., 36, 393.VIOLLIER, G. (x95S), in 'Liver Disease,' Ciba Foundation
Symposium, J. & A. Churchill, London.WATSON, C. J. (1946), Blood, I, 99.WATSON, C. J. (I951), in 'Liver Disease,' Ciba Foundation
Symposium, J. & A. Churchill, London.WILSON, A., CALVERT, R. J., GEOHEGAN, H. (1952), J.clin. Invest., 3I, 8I5.WUHRMANN, F. (195), in 'Liver Disease,' Ciba Foundation
Symposium, J. & A. Churchill, London.WUHRMANN, F., WUNDERLY, C., and DE NICOLA, P. (I950),Klin. Wschr., 28, 667.
YSOLITARY AND INFIRM OLD PEOPLEBy Miss C. L. REEVE, B.A., F.S.H.M.
Secretary and Housing Manager, Rowe Housing Trust and Aub-ey Trust
The experience on which I base the views ex-pressed in this article comes from my work as aHousing Manager for two housing associationsin North Kensington. Much of their propertyconsists of old houses which can be let off in singlerooms, and these are often occupied by elderlypeople (for the most part women) who in otherdistricts might have to live with relations orfriends. If one of these old people becomes ill,but is not bad enough for hospital and there areno relations living near, a distressing situationarises which worries doctors as well as neighboursand social workers.Our first attempt to meet this kind of hardship
was to convert two connecting houses into a hostelwhere 28 old people could be fed and looked afterwhen they could no longer manage for themselves.This type of hostel is called Part III accommoda-tion, and under the National Assistance Act themajor part of the maintenance cost is met by thewelfare authority if it considers the old personin need of care and attention. We provide a
Matron and an Assistant Matron who, though notqualified nurses, have had nursing experience, andwe look after the old people until they die unlessthey become so ill that they need hospital care.It is as difficult to get old people into hospital froma hostel as it is from their homes, but it is possibleto arrange direct exchanges if there are people inthe hospital ready for hostel life at the time whenthere is a serious illness in the house.At this hostel the old people go out as they like,
help in the house if they are able, bring some oftheir own furniture if they want and generally lookon it as their permanent home. They share bed-rooms for the most part without difficulty, but ifwe were taking professional people it would beessential to have single bedrooms.The fact that the hostel is run by people they
know and in a district they know makes the movewhen it comes less worrying for old people thanit would be. I cannot stress too strongly what apity it is that, under present legislation, differentauthorities are responsible for old people at
copyright. on A
pril 5, 2020 by guest. Protected by
http://pmj.bm
j.com/
Postgrad M
ed J: first published as 10.1136/pgmj.29.331.255 on 1 M
ay 1953. Dow
nloaded from