Infected nonunion2
-
Upload
orthoprince -
Category
Health & Medicine
-
view
1.367 -
download
3
description
Transcript of Infected nonunion2

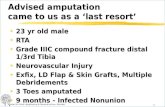
INFECTED NONUNION

NON UNIONA state in which healing process comes to a
halt as judged by clinical & x-ray evidence, beyond the stipulated period of healing for a particular bone due to mechanical or biological failure , with a gap being filled with fibrous or dense fibro cartilaginous tissue requiring a change in treatment.

INFECTED NONUNIONThat state existing after considerable time
[6-8 months] has elapsed, when there is no evidence that fracture will unite and infection still persists. Therefore other method of treatment to be done to achieve union and eradicate infection.

PROBLEMSMultiple sinusesOsteomyelitisBone and soft tissue lossDisuse OsteoporosisAdjacent joint stiffnessComplex deformitiesLimb length inequalitiesMulti-drug resistant polybacterial
infections

Tibia – most common siteOpen fracture with infection – most
common causeInfection following ORIF of closed #.

PATHOGENESISINOCULATIONVirulence of microbeSuboptimal condition of the local
environmentSystemic compromise of the host.

Infection perse doesn’t cause nonunionOM thrombosis of blood vessel of
haversian canals bone sclerosis and dead bone.
Butterfly fragments become sequestrii, isolated & devitalized by pus & infection granulation tissue.

Infection granulation tissue Osteolysis gaps nonunion.
Osteolysis occurs around the implants loosening instability of fixation nonunion.
Infection causes nonunion earlier than non-infected pts.

BIOFILMKey for the development & persistence of
inf.Aggregation of microbes enclosed with in
an extracelluar polysaccharide matrix [glycocalyx] that adheres to the surface of the implants or devitalized bone.
59% of orthopaedic biomaterial related infections +ve findings.

Protects the organism from antibiotics and host defense mechanism.
Allows the infection to exist in sub clinical state and recur.
Implants promotes biofilm, infection would persist.

MICROBIOLOGYStaphylococcus aureas most common,
[alone or in combination in 65-70%].Pseudomonas aeroginosa [20-37%]Commonly polymicrobial [32-70%].Atypical mycobacterium & fungi in
immunocompromised pts.

CLASSIFICATIONInfected nonunion comes under Cierney
type IV chronic osteomyelitis ie; there unstable before and after debridement.

ROSEN et al [AO manual]Infected non-draining nonunionInfected draining nonunion.

Infected nondraining nonunion Quiescent ( dry, nondraining for at least 3
months) Needs one stage treatment.Active ( non draining but abscess & fever). Needs two stage treatment.

Infected draining nonunionI STAGE: By pass bone grafting [fibular
protibia, posteromedial femur or humerus grafting.
II STAGE: By pass has become solid radical debridement & open/closed irrigation & antibiotics.
III STAGE: cancellous B.G, muscle or skin pedicle flap,

G.S KULKARNI classificationSeverity of infectionApposition of fragmentsPresence or absence of deformity.

TYPE I: fragments in apposition with mild infection and with or with out implant, stable implant insitu with mild infection.
TYPE II: Fragments in apposition with severe infection with large or small wound.
TYPE III: Severe infection with a gap or deformity or shortening.
3A defect with loss of full circumference 3B defect in > 1/3 of cortex 3C infected nonunion with deformity.

CLINICAL EVALUATIONPain, erythema, swelling, draining sinuses,
abnormal mobility.No Fever Infection is clinically silent. High index of suspicion esp in atrophic
nonunion.0.2-1.6% chronic draining sinuses S.C.CSuspect when change in pain / discharge.

INVESTIGATIONElevated ESR & CRP,Normal WBC.X RAY: 1] Quality of bone 2] Type of implant 3] Fracture healing status 4] Angular alignment.

Areas suspicious of infectionBone resorptionSequestrum & involucrumPeriosteal & endosteal new bone formationCortical irregularities.

DisadvantagesDue to distorted anatomy due to traumaPhysiological reaction of bone to injury.Presence of implants.Can't reliably differentiate between septic
and aseptic changesSerial x rays, sensitivity-14%, specificity-
70% in diagnosing active infection.

C.T SCANBetter cortical bone detailsSequestrumSubtle cortical erosionBest detail of bone structure for planning.No artifact with implants.

MRIHighly sensitive modality. 98% sensitivity,
75% specificity.Gadolinium enhanced MRI: allows
discrimination of active infection from artifacts and fibro-vascular scar.
Demonstrate sinus tracts, differentiate bone & soft tissue inf, extent of bone involvement.

NUCLEAR IMAGING STUDIES Tc-99 M high sensitivity but low
specificity15%Ga-67 more specific.Indium 111 labeled WBC scan: sensitivity
83%, specificity 86%.Labor intensive, increase radiation dose, 24
hr delay, low resolution image, in-vitro label.

IMMUNOSCINTIGRAPHYInj of radiolabelled murine monoclonal anti-
granulocyte AB that binds WBC antigen.Sensitivity: 93%, specificity: 89%.In-vivo labeling.

CULTUREGold standardPrior antibiotic treatment and improper
handling of specimens preclude the growth.Multiple intra-op specimens: sinus tract,
purulent fluid, soft tissue, curetted bone, bed of the involved bone.
Different micro enviroments.

PRINCIPLESPrompt diagnosis and aggressive RxInfection control with surgical debridement
and specific antibiotics.# stabilisation Soft tissue coverageRestoration of bone defects.

GOALS
(1) the infected tissues must be resected to live margins;
(2) the methods must address previous fixation failures and structural deficiencies;
(3) the patient must have the potential to heal, survive treatment, and benefit from treatment; and
(4) the prognosis for success must be reasonable and the methods within the capabilities of the medical team

METHODSConventional or classic methodActive or modern method Pulsed electromagnetic fieldsIlizarov method.

CONVENTIONAL METHODTo convert an infected and draining
nonunion in to one that has not drained for several months and then to promote bone healing by bone grafting.
More time consuming.Stiffness of adjacent joints.Reconstructive procedures should be
delayed until at least 6 months after all signs of infections have disappeared.

POSTEROLATERAL GRAFTINGTo avoid the active draining sinuses and
poor skin in the anterior aspect.Posterior aspect of the tibia is roughened
superior and inferior to nonunion.Entire area is covered with graft.Nonunion site is not exposed.


ACTIVE METHODTo obtain bony union early and thus
shorten the period of convalescence.To preserve the motion in adjacent jts.Restoration of bony continuity- I step.Bone union takes priority over infection.Nonunion exposed through old scars and
sinuses.

The ends of the fragments are decorticated subperiosteally osteoperiosteal flaps.
All devitalized and infected bone and soft tissue were removed.
Fragments aligned and stabilised ext.fix.If necessary a second decortication with or
with out B.G carried out.


ILIZAROV METHODTo eliminate infection and to achieve union
vascularity must be increased.By corticotomy and circular ext. fix.To remove necrotic and infected segments
before osteosynthesis.For hypertrophic nonunion with minimal
infection & no sequestrated bone compression.

Monofocal compressionCompression increases repair callus and
vascularity.Infection spontaneously eliminated.For infected hypertrophic nonunion with
deformity.


Segmental bone transportEliminates need for B.G.Simultaneous restoration of bony defectElimination of limb shortnessCorrection of deformityImprovement in local soft tissue.Increase in local blood circulationElimination of infection.

TYPES OF BONE TRANSPORT3 TYPES.Differs in the way that the bone fragments
are transfixed to the frame and in how they are transported to the intended site

EXTERNAL TRANSPORT For combined bone loss replacement with
correction of deformity and lengthening of the limb
INTERNAL TRANSPORT: For bone loss replacement without
deformity correction or limb lengthening.

B.T OVER A NAIL
Herzenberg et.alAt the end of the bone transport
interlocking was done.Ilizarov fixator can be removed at an early
stage .Avoid complications of the ring fixator.

HARMONS GRAFTINGBone grafting on the interosseous
membrane to obtain a long synostosis with fibula, spanning the tibial defect.
C.I in proximal defects.

HARMONS POSTEROLATERAL GRAFT

Free vascularised bone transfer Rib, fibula, iliac crest.Isolation of a segment of contra lateral
fibula with attached nutrient artery and vein.
Length of graft should be 4 cm longer than defect to allow 2 cm overlap at the proximal and distal ends.

VASCULARISED FIBULAR GRAFT



DEFORMITY CORRECTIONComplex deformity consists of : shortening,
rotation, angulation & translation.Generally length must be reestabilised
before other deformities being corrected.

ANTIBIOTIC BEADS

Polymethyl methacrylate powder is mixed with antibiotic powder beads.
Aminoglycosides common choice. broad spectrum heat stability low allergenicity.

BEAD POUCH TECHNIQUE
Occupy dead space and prevents haematoma or scar tissue.
Free flap placed over the beads contour much better.
High local conc. Antibiotic.Minimizes systemic toxicity.Seals the wound from external
environment with semi permeable barrier prevents secondary inf.

IMPLANT REMOVAL

CLOSED SUCTION IRRIGATION
Used when there is a large potential space or cavity after closure.
Abandoned due to risk of secondary contamination.

PRIMARY CLOSUREWhen all the infected tissue has been
removed, wound is alive, dead space has been addressed and the antibiotic is pathogen specific.

Electrical and electromagnetic stimulationBone growth stimulators used along with
cast immobilization and weight bearing.Either invasive or semi-invasive.

Gap tissues progressively calcify and are invaded by vessels from the flanking bone margins, producing a picture very similar to that of normal endochondral ossification.
The electrical fields do not stimulate osteogenesis directly, but rather appear to modify fibrochondrocyte function so that any soft-tissue impediment to bridging by bone is eliminated.


PAPINEAU PROCEDURE
Open bone grafting tech, done to control infection.
Infected nonunion with large cavity or bone defect & inadequate soft tissue coverage & inability to close skin directly.

PAPINEAU TECH1) granulation tissue markedly resists infection, 2) Autogenous cancellous bone grafts are rapidly
revascularized and are resistant to infection, 3) the infected area is completely excised, 4) adequate drainage is provided, 5) adequate immobilization is provided, 6) antibiotics are used for prolonged periods.

Stage I: Radical debridementStage II: bone graftingStage III: skin coverage.

PAPINEAU TECH

Amputation
Any one or all of the following1) Extensive bone defect 2) Poor soft tissue cover3) Neurovascular compromise4) Anticipated poor outcome after
treatment.5) Severe Pt co morbidities.