inciples Pr and ticace r P of Lacrimal Surgery
Transcript of inciples Pr and ticace r P of Lacrimal Surgery
ISBN 978-81-322-2019-0 ISBN 978-81-322-2020-6 (eBook) DOI 10.1007/978-81-322-2020-6 Springer New Delhi Heidelberg New York Dordrecht London
Library of Congress Control Number: 2014952330
© Springer India 2015 This work is subject to copyright. All rights are reserved by the Publisher, whether the whole or part of the material is concerned, specifi cally the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfi lms or in any other physical way, and transmission or information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed. Exempted from this legal reservation are brief excerpts in connection with reviews or scholarly analysis or material supplied specifi cally for the purpose of being entered and executed on a computer system, for exclusive use by the purchaser of the work. Duplication of this publication or parts thereof is permitted only under the provisions of the Copyright Law of the Publisher's location, in its current version, and permission for use must always be obtained from Springer. Permissions for use may be obtained through RightsLink at the Copyright Clearance Center. Violations are liable to prosecution under the respective Copyright Law. The use of general descriptive names, registered names, trademarks, service marks, etc. in this publication does not imply, even in the absence of a specifi c statement, that such names are exempt from the relevant protective laws and regulations and therefore free for general use. While the advice and information in this book are believed to be true and accurate at the date of publication, neither the authors nor the editors nor the publisher can accept any legal responsibility for any errors or omissions that may be made. The publisher makes no warranty, express or implied, with respect to the material contained herein.
Printed on acid-free paper
Springer is part of Springer Science+Business Media (www.springer.com)
Editor Mohammad Javed Ali, MS, FRCS, FRCGP Dacryology Service L.V. Prasad Eye Institute Hyderabad India
Dedicated to my family – Dawood Ali, Qaiser Yasmeen, Farhana Baig, Majid Ali, Rehana Ali, Hafsa Javed, Nabiha Khan, and Jibran Ali
Dedicated to all my mentors and all my patients
vii
Over the last 25 years, the lacrimal system has received increasing interest both from the oculoplastic and sinus surgeons. Traditionally, the lacrimal sys-tem has been approached through a medial canthal external incision. In the best hands of trained Oculoplastic surgeons, this technique has excellent results. The revival in interest in approaches to the lacrimal system has been driven by the development of the endoscope and increasingly better digital camera systems that allow the anatomy to be both magnifi ed and displayed in crisp detail facilitating delicate and precise surgery. This move in lacrimal surgery mirrors the general surgical move from incisions to minimally inva-sive surgery with the endoscope playing the central role in this surgical evolvement. The interest in the endoscopic techniques has increased espe-cially among oculoplastic surgeons, as the results with this technique are now at least equivocal and in some publications better than the traditional external techniques.
This book provides an extraordinarily comprehensive reference, starting with historical perspectives, anatomy, and assessment and then going through the many and varied external approaches before moving to an extensive guide on the endoscopic approaches. Finally, an overview of quality of life in lacri-mal disorders is provided. The list of contributors is impressive as is their expertise in the chapters which they provide. Worthy additions to the text are a number of chapters on controversial topics in lacrimal surgery, such as the role of mitomycin C, whether the lacrimal system should be routinely intu-bated after DCR surgery, and the management of common canaliculus strictures.
This text is wide ranging and extensive and covers established knowledge, new ideas, and controversies presented by high-quality contributors with insight and experience and as recognized experts in the fi eld. This book would be a worthy addition to the library of any surgeon interested in lacrimal surgery, allowing them to delve quickly into chapters for valuable insights as well as having it as a major reference text resource. This book is the most valuable contribution to our literature, and the editor and contributing authors are to be congratulated.
Adelaide , SA , Australia Peter-John Wormald
Foreword
ix
Lacrimal Surgery: Glorious Past, Exciting Present Era, and the Audacity of Hope for a Brilliant Future
Do not fear to be eccentric in opinion, for every opinion now accepted was once eccentric. – Bertrand Russell (1872–1970)
The evolution of lacrimal disorders and their management amply exemplifi es the above stated quote of the twentieth-century British philosopher Bertrand Russell. Lacrimal surgeries has been a subject of discussion in antiquity with the earliest documented reference being a lacrimal sac incision in the “Code of Hammurabi” in 2250 BC [1]. The past which appears glorious today had once travelled through many rough terrains in ancient times nurtured by the Egyptians (Ebers Papyrus – 1500 BC), the Greeks (Hippocrates and Celcus – 25 BC), and the Romans (Galen – 200 AD) [1, 2]. The Arabians chipped in between with their contributions from Ibn Sina and Al Razi in the medieval times. The Modern Dacryology was given impetus with the hallmark anatomical works of Giovanni Morgagni (1682–1771) and Johann Zinn (1727–1759) and equally by the infl uential lacrimal treatises by Percival Pott (1714–1788) and Johann Schmidt (1759–1809) [3].
“Men love to wonder and that is the seed of science,” said the famous nineteenth-century American poet Ralph Waldo Emerson. Lacrimal surgeries have undergone a sea change in the last two centuries. The original Woolhouse technique (1724) of dacryocystectomy underwent numerous changes in tech-niques and approaches to the present age but with progressively lesser indica-tions. The external dacryocystorhinostomy (DCR) had a steeper evolution for obvious reasons from the times when Addeo Toti (1904) fi rst described it to the current-day practice with various incisions and lacrimal sac implants [4, 5]. With the introduction of rigid endoscopy and better view, endonasal dac-ryocystorhinostomy showed a steep resurgence into the practice (McDonough −1989) [6], more than a century after its original description (Caldwell – 1893) [7] failed to gain wider acceptance. Endocanalicular laser DCR, how-ever, till the present date has failed to gain widespread acceptance despite numerous modifi cations since its introduction to dacryology by Levin and Stormogipson in 1992 [8, 9]. Likewise was the journey of trans-conjunctival DCR (CDCR), which evolved into endoscopic and lesser invasive approaches along with numerous Jones tube modifi cations [10, 11]. Balloon dacryoplasty
Prol ogue
x
has evolved mostly in terms of indications rather than instrumentation or techniques [12, 13].
The present era of lacrimal practice is exciting and, at the same time, challenging. State-of-the-art equipment and mechanisms, including high- defi nition endoscopic systems, diagnostic and therapeutic dacryoendoscopy, and higher resolution yet safer imaging, are increasingly contributing toward our understanding of the disorders as well as developing minimally invasive surgical options. Many debates today are centered on the approaches to a DCR, ostium size, mitomycin C, and intubation. The recent most meta- analyses have been able to shed much needed light into these areas highlight-ing their clinical implications [14, 15]. The PEDIG studies have helped greatly in the management of congenital nasolacrimal duct obstructions in terms of clinical decision making and outcomes [16, 17]. There is an increas-ing focus on canalicular and nasolacrimal duct recanalizations under dacryo-endoscopic guidance in an effort to avoid a DCR [18]. Although this mode appears promising, skepticism is very well justifi ed at this stage. The present era is also seeing many attempts to standardize the nomenclatures [19], drug dosage [20], introduction of newer terminologies [21], and paradigm shifts in the understanding of lacrimal anatomy [22, 23]. The armamentarium of a lacrimal surgeon today is more well equipped than any other time, and this very fact brings in more responsibility on us than any other time, to take this forward in every possible way into the future!
The audacity of hope and optimism points toward a brighter future for the patients of tomorrow with lacrimal disorders. However, despite some of the advances highlighted, we still have a long way to go in our understanding and treatment of lacrimal disorders. This would require work on two different fronts with concurrent amalgamation. The fi rst front should be science related, and let the second be related to the surgeon. On the science frontier, the need of the hour is to demystify the etiopathogenesis of lacrimal disor-ders, primarily that of primary acquired nasolacrimal duct obstruction, or PANDO. It would be inappropriate to continue managing lacrimal disorders mechanically without simultaneous efforts to unravel the elusive etiopatho-genesis. The key to this, I believe, lies with the basic sciences. Embryonic studies to look for regulatory proteins infl uencing lacrimal primordium and sub-adjacent mesenchyme of surface ectoderm during Carnegie stages of development may hold promising clues to understanding of congenital lacri-mal disorders. Cytochemical analysis for infl ammatory mediators in tears of patients with PANDO and, if the culprits are zeroed in on, the search to phar-macologically block them or their receptors in the lacrimal system may have prophylactic value early on in the disease. Lacrimal immunology work on lacrimal drainage-associated lymphoid tissue (LDALT), its derangements [24], and how differently it behaves from the rest of the immune system should be carried forward to its logical conclusions, as this may have great bearing on our understanding of lacrimal physiology. Other avenues of poten-tial research in the near future include lacrimal system stem cell characteriza-tion on similar lines as that of lacrimal gland [25], drug-coated stents, and electron microscopic inter- and intracellular changes in lacrimal disorders.
Prologue
xi
On the second front, the lacrimal surgeon should not only focus on evidence- based practice but also constantly endeavor to explore avenues to generate evidence. The research potential needs to be unlocked, and aca-demic institutes should strive toward protecting and rearing the endangered species of “clinician-scientists” rather than pure clinicians. The need of the hour is also to cross-specialize where it matters! The lacrimal drainage sys-tem has a long course within the nasal cavity, and it is obvious that a good lacrimal work cannot be done without a good anatomical and surgical knowl-edge of the nose. Although the resurgence of EENT (eye, ear, nose, and throat) specialists may not be desirable due to explosion in the knowledge and vast nature of each subject, the benefi ts of limited cross-specialization cannot be overemphasized. Cross-specialization also opens up the surgeon to at least some ideas of one specialty that when appropriately extrapolated to the other may have benefi cial results. Basic sciences are the key to the future; hence, a very good understanding of the fundamentals of the lacrimal system up to the molecular level would greatly help the lacrimal surgeon in dealing with the disorders both in the lab and the clinic. Efforts should be made on the part of the lacrimal surgeon to perform focused clinical and research work with an emphasis on translational values. The challenge of the future is to set audacious goals and strive hard to achieve them. “We” as lacrimal surgeons need to remind ourselves frequently of our equally important responsibility to advance medicine and hand it over in a better shape to the next generation and probably beyond them. Are we doing enough on these fronts? If not, let us change that from today!
There is a single light of science, and to brighten it anywhere is to brighten it every-where. — Isaac Asimov (1920–1992)
Hyderabad , India Mohammad Javed Ali , MS, FRCS, FRCGP
References
1. Hirschberg J. The renaissance of ophthalmology in 18th century. In: Hirschberg J, editor. The history of ophthalmology, Vol 1. Amsterdam: Wayenborg publications; 1984. p. 11.
2. Hirschberg J. The renaissance of ophthalmology in 18th century. In: Hirschberg J, editor. The history of ophthalmology, Vol 3. Amsterdam: Wayenborg publications; 1984. p. 250–5.
3. Albert DM. Ophthalmic plastics surgery. In: Albert DM, Edwards DD, editors. The his-tory of ophthalmology. Cambridge: Blackwell Science; 1996. P. 235–54.
4. Ekinci M, Cagatay HH, Oba ME, et al. The long term follow-up results of external dac-ryocystorhinostomy skin incision scar with ‘W’ incision. Orbit. 2013;32:349–55.
5. De Castro DK, Santiago YM, Cunningham M, et al. A modifi ed lacrimal sac implant for high risk dacyrocystorhinostomy. Ophthal Plast Reconstr Surg. 2013;29:367–72.
6. McDonogh M, Meiring JH. Endoscopic transnasal dacryocystorhinostomy. J Laryngol Otol. 1989;103:585–7.
7. Caldwell GW. Two new operations for the obstruction of the nasal duct with preservation of the canaliculi. Am J Ophthalmol. 1893;10:189.
8. Levin PS, Stormogipson DJ. Endocanalicular laser assisted DCR. An anatomic study. Arch Ophthalmol. 1992;110:1488–90.
9. Henson RD, Cruz HL, Henson RG Jr, et al. Post operative application of mitomycin C in endocanalicular laser DCR. Ophthal Plast Reconstr Surg. 2012;28:192–5.
Prologue
xii
10. Jones LT. Conjunctivodacryocystorhinostomy. Am J Ophthalmol. 1965;59:773–83. 11. Ali MJ, Honavar SG, Naik M. Endoscopically guided minimally invasive bypass tube
intubation without DCR: evaluation of drainage and objective outcomes assessment. Minim Invasive Ther Allied Technol. 2013;22:104–9.
12. Becker BB, Berry FD. Balloon catheter dilatation in lacrimal surgery. Ophthalmic Surg. 1989;20:193–8.
13. Ali MJ, Naik MN, Honavar SG. Balloon dacryoplasty: ushering the new and routine era in minimally invasive lacrimal surgeries. Int Ophthalmol. 2013;33:203–10.
14. Feng YF, Yu JG, Shi JL, et al. A meta-analysis of primary external dacryocystorhinos-tomy with and without mitomycin C. Ophthalmic Epidemiol. 2012;19:364–70.
15. Feng YF, Cai JQ, Zhang JY, et al. A meta-analysis of primary dacryocystorhinostomy wit h and without silicone intubation. Can J Ophthalmol. 2011;46:521–7.
16. Repka MX, Chandler DL, Holmes JM, et al. Balloon catheter dilatation and nasolacri-mal duct intubation for treatment of nasolacrimal duct obstruction in after failed prob-ing. Arch Ophthalmol. 2009;127:633–9.
17. Repka MX, Chandler DL, Bremer DL, et al. Repeat probing for treatment of persistent nasolacrimal duct obstruction. J AAPOS. 2009;13:306–7.
18. Javate RM, Pamintuan FG, Cruz RT Jr. Effi cacy of endoscopic lacrimal duct recanaliza-tion using microendoscope. Ophthal Plast Reconstr Surg. 2010;26:330–3.
19. Ali MJ, Mohapatra S, Mulay K, et al. Incomplete punctal canalization: the external and internal punctal membranes. Outcomes of membranotomy and adjunctive procedures. Br J Ophthalmol 2013;97:92–95.
20. Ali MJ, Mariappan I, Maddileti S, et al. Mitomycin C in dacyrocystorhinostomy: the search for the right concentration and duration – a fundamental study on human nasal mucosa fi broblasts. Ophthal Plast Reconstr Surg. 2013;29:469–74.
21. Ali MJ, Naik MN. Canalicular wall dysgenesis: the clinical profi le of canalicular apla-sia and hypoplasia, associated systemic and lacrimal anomalies, and clinical implica-tions. Ophthal Plast Reconstr Surg. 2013;29:464–8.
22. Park J, Takahasi Y, Nakano T, et al. The orientation of the lacrimal fossa to the bony nasolacrimal canal: an anatomical study. Ophthal Plast Reconstr Surg. 2012;28:463–8.
23. Kakizaki H, Ichinose A, Takahashi Y, et al. Anatomical relationship of Horner’s muscle origin and posterior lacrimal crest. Ophthal Plast Reconstr Surg. 2012;28:66–8.
24. Ali MJ, Mulay K, Pujari A, et al. Derangements of lacrimal drainage associated lym-phoid tissue (LDALT) in human chronic dacryocystitis. Ocul Immunol Infl amm. 2013;21:417–23.
25. Tiwari S, Ali MJ, Balla MM, et al. Establishing human lacrimal gland cultures with secretory function. PLoS One. 2012;7:e29458.
Prologue
xiii
1 Lacrimal Disorders and Surgery: Historical Perspectives. . . . 1 Mohammad Javed Ali
2 Embryology of the Lacrimal Drainage System . . . . . . . . . . . . . 9 Mohammad Javed Ali and Hirohiko Kakizaki
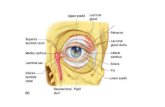
3 Anatomy, Physiology, and Immunology of the Lacrimal System . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 17 Hirohiko Kakizaki
4 Paradigm Shifts in the Lacrimal Anatomy . . . . . . . . . . . . . . . . 35 Hirohiko Kakizaki
5 The Sinonasal Anatomy: Endoscopic Lacrimal and Orbital Perspectives . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 41 Hirohiko Kakizaki
6 Evaluation of Epiphora . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 61 Sima Das
7 Setup for Nasal Endoscopy and Endoscopic Surgery. . . . . . . . 75 Hesham Saleh and Natasha Choudhury
8 Nasal Endoscopic Evaluation . . . . . . . . . . . . . . . . . . . . . . . . . . . 81 Hesham Saleh and Natasha Choudhury
9 Dacryoendoscopic Examination of the Lacrimal System . . . . . 87 Mohammad Javed Ali
10 Imaging Modalities for Lacrimal Disorders . . . . . . . . . . . . . . . 93 Lakshmi Mahesh and Mohammad Javed Ali
11 Disorders of the Upper Lacrimal System . . . . . . . . . . . . . . . . . 103 Mohammad Javed Ali
12 Congenital Nasolacrimal Duct Obstruction . . . . . . . . . . . . . . . 117 Saurabh Kamal , Mohammad Javed Ali , Vinod Gauba and Qasim Qasem
13 Primary Acquired Nasolacrimal Duct Obstruction (PANDO) and Secondary Acquired Lacrimal Duct Obstructions (SALDO) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 133 Saurabh Kamal and Mohammad Javed Ali
Contents
xiv
14 Functional Obstructions of the Lacrimal System . . . . . . . . . . . 143 Mohammad Javed Ali
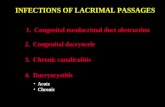
15 Infections of the Lacrimal Drainage System . . . . . . . . . . . . . . . 149 Aditi Watve and Mohammad Javed Ali
16 Lacrimal Trauma and Its Management. . . . . . . . . . . . . . . . . . . 159 Gangadhara Sundar
17 Primary External Dacryocystorhinostomy . . . . . . . . . . . . . . . . 171 Mohammad Javed Ali
18 Endoscopic-Guided Single Self- Linking of Stents . . . . . . . . . . 177 Mohammad Javed Ali
19 Aesthetic External DCR: The Subciliary Approach. . . . . . . . . 183 Milind N. Naik
20 Aesthetic External DCR: The Transconjunctival Approach . . . . . . . . . . . . . . . . . . . . . . . . 189 Pelin Kaynak
21 Primary Endoscopic Dacryocystorhinostomy . . . . . . . . . . . . . . 195 Kelvin Kam-Lung Chong
22 Ultrasonic Endoscopic Dacryocystorhinostomy . . . . . . . . . . . . 203 Mohammad Javed Ali
23 Non-endoscopic Endonasal Dacryocystorhinostomy . . . . . . . . 213 Suryasnata Rath , Samir Mahapatra and Peter J. Dolman
24 Primary Endocanalicular Laser Dacryocystorhinostomy . . . . 219 Raoul Paolo D. Henson
25 5- and 9-mm Balloon-Assisted Dacryocystorhinostomy. . . . . . 231 David I. Silbert and Noelle S. Matta
26 Revising a Failed Dacryocystorhinostomy. . . . . . . . . . . . . . . . . 245 Emmy Lee , Hunter Yuen and Mohammad Javed Ali
27 Conjunctivodacryocystorhinostomy: Indications, Techniques, and Complications . . . . . . . . . . . . . . . 257 Mohammad Javed Ali
28 Adjunctive Endonasal Procedures with Dacryocystorhinostomy . . . . . . . . . . . . . . . . . . . . . . . . . . . 267 Joseph Brunworth , Alkis James Psaltis and Peter-John Wormald
29 Evaluation of a DCR Ostium and DOS Scoring . . . . . . . . . . . . 279 Mohammad Javed Ali , Alkis James Psaltis and Peter-John Wormald
30 Intubation in Lacrimal Surgery: Devices and Techniques. . . . 289 Tarjani Vivek Dave and Mohammad Javed Ali
Contents
xv
31 Pediatric and Adult Balloon Dacryoplasty . . . . . . . . . . . . . . . . 303 David I. Silbert and Noelle S. Matta
32 Dacryoendoscopic Guided Canalicular and Nasolacrimal Duct Recanalization . . . . . . . . . . . . . . . . . . . 309 Mohammad Javed Ali
33 Tumors of the Lacrimal Drainage System . . . . . . . . . . . . . . . . . 319 Gangadhara Sundar
34 Dacryocystectomy: Indications and Techniques . . . . . . . . . . . . 327 Mohammad Javed Ali
35 Debates in Dacryology: The Ostium Dilemma . . . . . . . . . . . . . 335 Andrea Zarkovic , Edwin C. Figueira , Simon N. Madge , Marcus M. Marcet and Dinesh Selva
36 Debates in Dacryology: The Mitomycin-C Dilemma . . . . . . . . 341 Yi-fan Feng
37 Debates in Dacryology: The Intubation Dilemma . . . . . . . . . . 347 Edwin C. Figueira , Andrea Zarkovic , Simon N. Madge , Marcus M. Marcet and Dinesh Selva
38 The Great Debate: External Versus Endonasal Dacryocystorhinostomy . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 351 Andre Litwin and Raman Malhotra
39 Quality of Life in Lacrimal Disorders and Patient Satisfaction Following Management . . . . . . . . . . . . . . . . . . . . . 359 Mohammad Javed Ali
40 Future Directions in Lacrimal Disorders and Their Management . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 363 Mohammad Javed Ali
Contents
xvii
Mohammad Javed Ali , MS, FRCS, FRCGP Dacryology Service , L.V. Prasad Eye Institute , Hyderabad , India
Contributors
xviii
Peter-John Wormald , FRACS Department of Otolaryngology, Head Neck Surgery , University of Adelaide , Adelaide , SA , Australia
Joseph Brunworth , MD Department of Otolaryngology , University of Adelaide , Adelaide , SA , Australia
Contributors
xix
Kelvin Kam-Lung Chong , MD Ophthalmic Plastics Surgery , Chinese University of Hong Kong , Sha Tin, New Territories , Hong Kong
Natasha Choudhury , FRCS (ORL-HNS) Department of Otolaryngology, Charing Cross Hospital , London , UK
Contributors
xx
Sima Das , MS Ophthalmic Plastics Sugery , Schroff Eye Hospital , Delhi , India
Tarjani Vivek Dave , DNB, FLVPEI Ophthalmic Plastics Surgery , L.V. Prasad Eye Institute , Hyderabad , India
Contributors
xxi
Peter J. Dolman , MD, FRCSC Ophthalmic Plastics Surgery , University of British Columbia , Vancouver , BC , Canada
Yi-fan Feng , MD, PhD Department of Ophthalmology , Zhongshan Hospital and Fudan University , Shanghai , China
Contributors
xxii
Edwin C. Figueira , FRANZCO Ophthalmic Plastics Surgery , Royal Adelaide Hospital , Adelaide , SA , Australia
Vinod Gauba , FRCS Ophthalmic Plastics Surgery , Imperial Healthcare Institute , Dubai , UAE
Contributors
xxiii
Raoul Paolo D. Henson , MD Ophthalmic Plastics Surgery , Makati Medical Center , Makati City , Philippines
Hirohiko Kakizaki , MD, PhD Department of Ophthalmology , Aichi Medical University , Aichi , Japan
Contributors
xxiv
Saurabh Kamal , MD Ophthalmic Plastics Surgery , L.V. Prasad Eye Institute , Hyderabad , India
Pelin Kaynak , MD Ophthalmic Plastics Surgery , Beyoglu Eye Research and Training Hospital , Istanbul , Turkey
Contributors
xxv
Emmy Lee , FRCS Department of Ophthalmology , Chinese University of Hong Kong , Shatin, New Territories , Hong Kong
Andre Litwin , FRCS Oculoplastic Surgery , Queen Victoria NHS Trust , London , UK
Contributors
xxvi
Simon N. Madge , FRCOphth Department of Ophthalmology , Wye Valley Trust, NHS , Hereford , UK
Samir Mahapatra , MS Ophthalmic Plastics Surgery , L.V. Prasad Eye Institute , Vishakapatnam , India
Contributors
xxvii
Lakshmi Mahesh , MS Department of Ophthalmology , Manipal Hospital , Bangalore , India
Raman Malhotra , FRCS Oculoplastic Surgery , Cadogan Clinic and Queen Victorial NHS Trust , London , UK
Contributors
xxviii
Marcus M. Marcet , MD Department of Ophthalmology , University of Hong Kong , Cyberport , Hong Kong
Noelle S. Matta , CO, CRC, COT Department of Pediatric Ophthalmology, Family Eye Group , Lancaster , PA , USA
Contributors
xxix
Milind N. Naik , MD Ophthalmic Plastics Surgery , L.V.Prasad Eye Institute , Hyderabad , India
Alkis James Psaltis , FRACS Department of Otolaryngology, Head Neck Surgery , University of Adelaide , Adelaide , SA , Australia
Contributors
xxx
Qasim Qasem , MD Pediatric Ophthalmology , Imperial Healthcare Institute , Dubai , UAE
Suryasnata Rath , MS, FRCS Ophthalmic Plastics Surgery , L.V. Prasad Eye Institute , Bhubaneswar , India
Contributors
xxxi
Hesham Saleh , FRCS, FRCS (ORL-HNS) Department of Otolaryngology , Charing Cross Hospital and Imperial College , London , UK
Dinesh Selva , FRANZCO Ophthalmology and Visual Sciences , University of Adelaide , Adelaide , SA , Australia
Contributors
xxxii
David I. Silbert , MD, FAAP Department of Pediatric Ophthalmology, Family Eye Group , Lancaster , PA , USA
Gangadhara Sundar , DO, FRCSEd, FAMS Orbit and Oculofacial Surgery , National University of Singapore , Singapore , Singapore
Contributors
xxxiii
Aditi Watve , MD Ophthalmic Plastics Surgery , L.V. Prasad Eye Institute , Hyderabad , India
Hunter Yuen , MRCS Department of Ophthalmology , Chinese University of Hong Kong , Shatin, New Territories , Hong Kong
Contributors