History of neurosurgery at University of Toronto: the St ... · Currently, neurosurgery is an...
Transcript of History of neurosurgery at University of Toronto: the St ... · Currently, neurosurgery is an...

HISTORICAL VIGNETTEJ Neurosurg 127:1417–1425, 2017
For more than 90 years, the Division of Neurosurgery at the University of Toronto has been training and educating neurosurgeons from all over the world.3
Currently, neurosurgery is an established specialty in 4 teaching hospitals affiliated with the University of Toronto (St. Michael’s Hospital, Sunnybrook Health Sciences Cen-tre, Toronto Western Hospital, and the Hospital for Sick Children). Each hospital embraces a rich history of surgi-cal expertise and provides diverse patient encounters for residents and fellows.15,25
In this report, we describe the history of neurosurgery at St. Michael’s Hospital and highlight the founders’ roles in restructuring the division. No physician was appointed at St. Michael’s Hospital unless he or she held a university position; thus, all appointments were joint hospital/univer-sity jobs, and promotion in academic rank was according to the university criteria. All significant leadership roles in the Department of Surgery are on 5-year appointments, which can be renewed once. This constant renewal and modernization of leadership is a key factor in the success
of both the University of Toronto and St. Michael’s Hos-pital program. We hope that this historical perspective of our leadership and program can act as a guide for develop-ing programs around the world.
MethodsWe conducted a literature review using MEDLINE,
Embase, Science Direct, and Google Scholar. We also searched St. Michael’s Hospital and City of Toronto ar-chives to extract related published articles, books, and his-torical reports and pictures. To further verify the content, emeritus faculty from St. Michael’s Hospital reviewed the manuscript.
The St. Michael’s Story: the Sisters of St. Joseph
In the 19th century, an unanticipated influx of im-migrants to Toronto generated a critical strain on public health and financial and educational resources. The streets
ABBREVIATIONS aSAH = aneurysmal subarachnoid hemorrhage.SUBMITTED May 1, 2016. ACCEPTED September 22, 2016.INCLUDE WHEN CITING Published online January 27, 2017; DOI: 10.3171/2016.9.JNS161119.
History of neurosurgery at University of Toronto: the St. Michael’s storyNaif M. Alotaibi, MD,1,2 Daipayan Guha, MD,1,2 Christopher S. Ahuja, MD,1,2 Julian Spears, MD,1 Paul J. Muller, MD,1 William S. Tucker, MD,1 Alan R. Hudson, MB,1 and R. Loch Macdonald, MD, PhD1–3
1Division of Neurosurgery, Department of Surgery, and 2Institute of Medical Science, University of Toronto; and 3Division of Neurosurgery, St. Michael’s Hospital, Labatt Family Centre of Excellence in Brain Injury and Trauma Research, Keenan Research Centre for Biomedical Science, and the Li Ka Shing Knowledge Institute of St. Michael’s Hospital, Department of Surgery, University of Toronto, Ontario, Canada
In this paper, the authors describe the history of neurosurgery at St. Michael’s Hospital, University of Toronto. St. Mi-chael’s has long been regarded as one of the top teaching and research hospitals in Canada. A detailed literature review of published and unpublished works was performed to formulate a succinct but in-depth review of its development, successes, and challenges. This fascinating 125-year history serves as a reminder of the importance of their institution’s origins, and the authors hope that it will be a useful guide for developing programs around the world.https://thejns.org/doi/abs/10.3171/2016.9.JNS161119KEY WORDS neurosurgery; history; St. Michael’s Hospital; University of Toronto
©AANS, 2017 J Neurosurg Volume 127 • December 2017 1417
Unauthenticated | Downloaded 06/15/20 06:31 AM UTC

N. M. Alotaibi et al.
J Neurosurg Volume 127 • December 20171418
were laden with desperately poor and ill patients. Armand-François-Marie de Charbonnel, Bishop of Toronto (1850–1860), asked the Sisters of St. Joseph (a Roman Catholic religious congregation of women that originated in 1650 in France) to start working on instituting charitable hospi-tals, schools, boarding homes, and orphanages.54 In 1885, the Sisters created a boarding house for working women, Notre Dame des Anges, at 32 Bond Street. To address the further need for care of the poor in the south of Toronto, the Sisters founded St. Michael’s Hospital in 1892, with Mother de Chantal as its first superior (Fig. 1). It is thought that it was her idea to establish a hospital.38
A strong supporter of the Sisters’ initiative was Robert J. Dwyer (Fig. 2). Dwyer graduated from the University of Toronto in the year that St. Michael’s was founded and was one of the few physicians at the time to hold mem-bership in the Royal Colleges of Physicians of the United Kingdom. He became St. Michael’s first house surgeon, a role that he fulfilled passionately. Dwyer was well known for his exemplary clinical and teaching skills, as described
in an obituary letter in the Canadian Journal of Medicine and Surgery in 1920: “The deceased was a great teacher … not only by reason of his gift of imparting knowledge, but for his ability to communicate his penetrative diagnos-tic acumen.”57
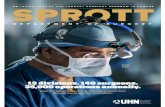
On July 1, 1892, St. Michael’s Hospital opened its doors with only 26 beds, 6 physicians, and 4 nurses. Within a few years, a dedicated emergency department was created, and the hospital officially started accepting medical stu-dents for training. By 1912, St. Michael’s boasted a 300-bed capacity and 5 operating suites. An official reciprocal agreement with the faculty of medicine at the University of Toronto was penned in 1920, which endures today.38 St. Michael’s is currently the only Level 1 adult trauma center in downtown Toronto, with 463 acute adult inpatient beds, 20 operating rooms, and more than 1600 nurses (Fig. 3). Li Ka Shing Knowledge Institute of St. Michael’s opened in 2011 and forms the hub for leading researchers and edu-cators at St. Michael’s.4,38
The Early YearsThere is evidence that neurosurgical procedures were
being performed at St. Michael’s before the development of specialized neurosurgical services at the hospital and
FIG. 1. The Sisters of St. Joseph of Toronto founded St. Michael’s Hos-pital in 1892. Mother de Chantal served as its first superior. Copyright St. Michael’s Hospital Archives. Published with permission.
FIG. 2. Robert J. Dwyer (1867–1920), the first house surgeon at St. Michael’s Hospital. Copyright St. Michael’s Hospital Archives. Published with permission.
Unauthenticated | Downloaded 06/15/20 06:31 AM UTC

History of neurosurgery: St. Michael’s
J Neurosurg Volume 127 • December 2017 1419
during the same time when Kenneth G. McKenzie (Can-ada’s first neurosurgeon) was practicing and training resi-dents at Toronto General Hospital. The earliest published neurosurgical work at St. Michael’s dates back to 1938 when David Pratt published a case report on pineal tumor surgery.45 Pratt used an occipital-transtentorial approach that, at the time, was used only by a few skilled neurosur-geons in the world. This report is credited as one of the first successful surgeries for pineal tumors in the world.27 Pratt also published his clinical experiences with brain ab-scesses and ventriculitis.44
Pratt graduated from the University of Toronto in 1926 and was a recipient of the Ellen Mickle Scholarship, which funded his studies in Freiburg, Germany. He joined St. Michael’s surgical staff in 1927 and subsequently was cer-tified by the Royal College and the American College of Surgeons.38 The surgeon-in-chief at the time, George Wil-son, described Pratt (Fig. 4) in an annual report as some-one who “always wears striped trousers, short coat, wing collar and bow-tie.”53
It is unclear whether Pratt had any working relation-ship with McKenzie at that time or even where he learned his neurosurgical techniques. He was also not mentioned in any of the previous historical works on the history of neurosurgery in Toronto and Canada.8,15,17,40,55
The First Neurosurgeon at St. Michael’s Hospital
W. Keith Welsh graduated from the University of To-ronto with honors in 1926 and trained under the mentor-ship of Norman Shenstone, one of the fathers of thoracic surgery in Canada.11 In 1947, he became chief of the De-partment of Surgery and began developing dedicated divi-sions for plastic surgery, orthopedic surgery, and neuro-surgery. One of his achievements was assigning energetic young doctors to lead these divisions. In 1954, Welsh ap-pointed William J. Horsey as the first head of the Division of Neurosurgery. Within a few years, Horsey was able to establish the first dedicated operating room for neurosur-gery and a combined nursing unit for neurosurgical and orthopedic patients.17,38
Horsey was an outstanding student and received a scholarship to enroll in medical school at the University of Toronto. He graduated in 1944 with the Cody Silver
FIG. 4. Rare portrait of David W. Pratt, the first surgeon to perform neu-rosurgical procedures at St. Michael’s Hospital. Copyright St. Michael’s Hospital Archives. Published with permission.
FIG. 3. St. Michael’s Hospital in 1892 (left) and the current building (right). Copyright St. Michael’s Hospital Archives. Published with permission.
Unauthenticated | Downloaded 06/15/20 06:31 AM UTC

N. M. Alotaibi et al.
J Neurosurg Volume 127 • December 20171420
Medal and Chappell Prize for best surgical student. After he finished his surgical internship at St. Michael’s Hospi-tal, he joined the Royal Canadian Army. After discharge in 1946, he worked in the Department of Anatomy at the University of Toronto as a teaching assistant, followed by a year of neurosurgical research at Johns Hopkins Hospi-tal in Baltimore. Horsey returned to Toronto as a resident in neurosurgery under the direction of Harry Botterell, mentor to Toronto’s greatest neurosurgeons (William Lougheed, Ross Fleming, Ron Tasker, and Harold J. Hoff-man). Horsey became the first of 6 chief residents under Botterell (Fig. 5).16,17
Horsey performed further training in neurosurgery across Europe, including Queen Square in London, Eng-land. In July 1954, he was chosen to be the first head of the Division of Neurosurgery at St. Michael’s Hospital in To-ronto (Table 1). Most Canadian historians concur that he established that division to become a major neurosurgical center in Canada for clinical care and education. He was the only neurosurgical staff for 6 years, performing surgi-cal cases (including aneurysm cases) with the aid of the operating room nurse Mary Allen and interns only. Mary Allen was Horsey’s right hand for many years. He built the service single-handedly until Stanley W. Schatz (second neurosurgeon at St. Michael’s Hospital) arrived in 1961 to take some of the surgical load. Both were very similar in their thinking and took teaching responsibilities seriously.
After the retirement of Keith Welsh, Horsey became surgeon-in-chief in 1968, and, at that point, almost ev-eryone in the hospital knew him. He was available to residents and students as seen in one of the intern’s diary notes about him:26
Always available, he roamed the halls of the hospital smoking his pipe. He loved the emergency department and frequently would appear unannounced. A couple of suggestions and a little humor and he would be on his way. His rapier wit was subtle and funny but occasionally made the recipient feel more than a little foolish. He enjoyed a good party and no annual Christmas party would have been complete without him leading the entire assembly in a Gay Gordon.
Horsey was appointed full professor at the University of Toronto and was also appointed chairman of the medi-cal advisory board at St. Michael’s Hospital, a position he held for many years. He was probably one of the first neurosurgeons to introduce the operating microscope for lumbar discectomy as well as the anterior approach to the cervical spine in Ontario or even Canada.17,21
After his retirement in 1989, Horsey was recognized for his major influences on clinical research with the es-tablishment of the Horsey Prize for best resident research presentation given yearly at the Botterell lectureship at the University of Toronto (Supplementary Table 1). Horsey died in 2002.
The Hudson YearsAlan Hudson attended medical school in Cape Town,
South Africa. After graduating in 1960, he joined Groote Schuur Hospital in Cape Town as a general surgery resi-dent to Professor J. H. Louw, a pioneer in pediatric surgery for congenital small-bowel disorders.28 Hudson subse-quently undertook research training under E. Bruce Hen-drick in 1962 at the Hospital for Sick Children, assessing the epidemiology of traumatic brain injury in children.20
Interestingly, in 1964 Hudson applied to Toronto for further training in general surgery and was surprised that he was offered a training position in neurosurgery for which he never applied. Hudson started his neurosurgi-cal training at St. Michael’s Hospital under the mentorship of Horsey and Schatz. During this time (1965–1968), the St. Michael’s Hospital resident was on call all year and responsible for all encephalograms, ventriculograms, and angiograms until the arrival of a specialized neuroradi-ologist (C. Gonzolves), who decreased the residents’ du-ties over these investigations. Every ward was headed by a nun in religious habit. The nuns were very supportive of the residents, with whom they shared the vocational focus of caring for the patients. There was no question that the nuns created the spirit at St. Michael’s Hospital, and all residents were welcomed, regardless of creed or color.
Hudson was awarded the McLaughlin Fellowship to pursue further training in peripheral nerve science with Professor G. Weddell at University of Oxford.22 He was then appointed as neurosurgery faculty at St. Michael’s in 1970 (Fig. 6). The 3 neurosurgeons (Hudson, Horsey, and Schatz) relied enormously on the nurses to monitor their critical patients on the mezzanine floor (4 M) while they were in the operating room. Consequently, they designed a large neurosurgical ICU in the center of the new ward
FIG. 5. Portrait of W. J. Horsey, the first head of the Division of Neuro-surgery at St. Michael’s Hospital (left) and a picture of him during his last operative spine case in 1989 (right). Copyright St. Michael’s Hospi-tal Archives. Published with permission.
TABLE 1. Heads of the Division of Neurosurgery at St. Michael’s Hospital (1954–2016)
Year Appointed Neurosurgeon
1954 William J. Horsey1977 Alan Hudson1983 Paul Muller 1993 William Tucker2000 Richard Moulton2007 R. Loch Macdonald2015 Julian Spears
Unauthenticated | Downloaded 06/15/20 06:31 AM UTC

History of neurosurgery: St. Michael’s
J Neurosurg Volume 127 • December 2017 1421
on Victoria Street to support nurses’ exchanges between ward and ICU at any time. Hudson became head of the Division of Neurosurgery in 1977. He established the first dedicated neurosurgical ICU and was able to increase the neurosurgery bed capacity to 41 beds. Furthermore, the neurosurgery service officially received approval for elec-tive operating time. The division also fostered strong, col-laborative relationships with leaders from the Divisions of Neurology (Henry Berry and Joseph Marotta) and Pathol-ogy (Juan M. Bilbao) and organized the first ever city-wide multidisciplinary brain tumor program.
Hudson was the first neurosurgeon to establish St. Mi-chael’s and Toronto on the world stage as a center of excel-lence for peripheral nerve surgery and science. His labora-tory had many distinguished visitors, including Sir Sydney Sunderland. Hudson is remembered by the Canadian me-dia as the first surgeon in the world to have successfully performed a sciatic nerve allotransplant.35 He also became chairman of the Division of Neurosurgery at the University of Toronto and the first chairman who brought the annual meetings of the World Federation of Neurosurgical Societ-ies, American Association of Neurological Surgeons, Con-gress of Neurological Surgeons, and Society of Neurologi-cal Surgeons to convene in Toronto. Following his term as chairman in 1989, Dr. Hudson was first appointed surgeon-in-chief, followed by appointments as president and chief executive officer of The Toronto Hospital. The institution expanded during his term to include the Toronto Western and Princess Margaret Hospitals and to become known as the University Health Network. The Alan and Susan Hud-son Chair in Neuro-Oncology has been established at the University Health Network, as has the Hudson Teaching Award given annually at the William S. Keith Lectureship for the best resident and faculty teacher in the Division of Neurosurgery (Supplementary Table 2).
Era of SubspecializationStan Schatz decided to leave St. Michael’s Hospital in
1973 and spent the remainder of his career in Hamilton, Ontario. This led to the recruitment of William S. Tucker and Paul J. Muller, both graduates of the University of Toronto. They followed Alan Hudson and became divi-sion heads in 1983 (Muller) and 1993 (Tucker). Their main focus was initiating a neurosurgical subspecialty practice at St. Michael’s. They recruited faculty in neurotrauma (Richard Moulton), complex skull base and pituitary
(Harley Smyth, Michael Cusimano), and spine (Richard Perrin) and strengthened the operative abilities of the divi-sion (Fig. 7, Supplementary Table 3). Muller focused on intrinsic brain tumors, while Tucker focused on complex aneurysms and carotid surgeries. It was the first time for significant diversification of experiences for residents at St. Michael’s.
Bill Tucker was also the first head of the trauma ser-vice and trauma team leader at St. Michael’s Hospital, a largely medical role that was present in only few centers in North America. Based on a 1984 annual hospital re-port, trauma at St. Michael’s was one of busiest services in Ontario, with 151 admissions for polytrauma with injury severity scores greater than 16, and 61 cases that required craniotomy.
The development of a trauma and neurosurgery ICU combining the disciplines of neurosurgery, general sur-gery, and orthopedics into a cohesive unit was a very suc-cessful step of this era. From its early years in 1985, 1986, and 1987, the unit served 778, 828, and 846 neurosurgical patients, respectively. To this day, the trauma and neuro-surgery ICU serves hundreds of critically ill patients every year.
William S. TuckerBill Tucker joined the neurosurgical faculty in 1977. He
received his training in Toronto from 1969 to 1975. Follow-ing his Royal College certification in neurosurgery, he went to the University of Colorado for basic science research un-der the mentorship of Wolff M. Kirsch. Tucker served as the residency program director in Toronto for many years and also was Toronto’s site coordinator for major interna-tional studies that involved the natural history of intracra-nial aneurysms.24 He was also the first head of the trauma
FIG. 6. Portrait of Alan Hudson (left) and him working at the peripheral nerve laboratory with his research partner Daniel Hunter (right). Copy-right St. Michael’s Hospital Archives. Published with permission.
FIG. 7. Portraits of the neurosurgeons contributing to subspecialization of neurosurgery at St. Michael’s Hospital: Bill Tucker (A), Paul Muller (B), Harley Smyth (C), Richard Perrin (D), Richard Moulton (E), and Michael Cusimano (F). Copyright St. Michael’s Hospital Archives. Published with permission.
Unauthenticated | Downloaded 06/15/20 06:31 AM UTC

N. M. Alotaibi et al.
J Neurosurg Volume 127 • December 20171422
service at St. Michael’s Hospital. He was appointed presi-dent of the Canadian Medical Protective Association from 2007 to 2010 and retired from St. Michael’s Hospital and the University of Toronto in 2010 as professor emeritus.
Paul MullerPaul Muller finished his undergraduate studies in To-
ronto and graduated from the Faculty of Medicine at the University of Toronto in 1969. Muller entered the neuro-surgical training program in Toronto in 1970. Following his clinical training, he undertook graduate studies at the Institute of Medical Sciences in Toronto and received his master’s degree on the topic of experimental neurooncolo-gy; he was awarded the most prestigious Canadian neuro-surgical award named the K. G. McKenzie Prize for basic neuroscience research. His research field was focused on photodynamic therapy for patients with malignant glio-mas.56 Dr. Muller continued a very active and busy prac-tice until his retirement in 2013. He is currently professor emeritus in the Department of Surgery at the University of Toronto.
Richard MoultonRichard Moulton graduated from the medical school
at University of Calgary in 1979. He then received his training in neurosurgery from 1979 to 1984. Because of his strong interest in neurotrauma, he went to the Medi-cal College of Virginia to be trained under the supervision of Professor Anthony B. Marmarou.37 Moulton joined the neurosurgery staff at St. Michael’s in 1986. He also served as the next division head after Bill Tucker. Moulton fur-ther characterized the role of neurosurgery in brain injury management that inspired many residents and fellows to pursue careers in neurotrauma. In 2004, Dr. Moulton left St. Michael’s to become the chairman of neurosurgery at University of Ottawa, where he continues to work as a fac-ulty member.
The Surgeon-Scientist GenerationR. Loch Macdonald was recruited in 2007 to become
the next division head. In this period, neurosurgery at St. Michael’s underwent a reorganization of its clinical and ba-sic science research into dedicated subdivisions, linking re-lated teams of neurosurgeons, neurologists, interventional neuroradiologists, and intensivists into an integrated neu-roscience research group. Macdonald and his faculty (Fig. 8, Supplementary Table 4) supported the infrastructural advancement of St. Michael’s by acquiring the latest op-erative and research technology including image guidance, endovascular devices, and laboratory equipment. He also continued the classic Horsey tradition of hosting neurosur-gery rounds every week to highlight important educational points for residents, fellows, and medical students. The an-nual number of operative cases reached record highs dur-ing Macdonald’s term as division head.
The Division of Neurosurgery also became one of the world’s leading centers in aneurysmal subarachnoid hem-orrhage (aSAH) treatment and research with the establish-ment of the new neurovascular center. The center includes a multidisciplinary team from radiology (Tom Marotta, Walter Montanera, Dipanka Sarma, and Aditya Bharatha)
and neurosurgery (Julian Spears and R. Loch Macdonald). The team also established the first Acute Carotid Clinic in Canada (http://carotid.ca/) to allocate rapid detection and triaging of patients with symptomatic carotid steno-sis. This collaborative team meets weekly in the Marotta Clinic, named in honor of Joe Marotta’s contributions in neurology and medicine at St. Michael’s Hospital, to dis-cuss decisions on complex neurovascular conditions that require input from many areas. The division is currently the home for the world’s largest international aSAH data registry.29 In 2016, Jefferson Wilson was recruited as a neurosurgeon-scientist to join the current collaborative spine team from orthopedics (Henry Ahn) and neurosur-gery (Howard Ginsberg).
R. Loch MacdonaldLoch Macdonald obtained his medical degree from the
University of British Columbia, after which he completed a PhD program in experimental surgery at the University of Alberta in Edmonton under the mentorship of Bryce Weir.31 He subsequently undertook his neurosurgical training at the University of Toronto. Following a clini-cal fellowship in open vascular surgery in Toronto, he was recruited to the University of Chicago Medical Center in
FIG. 8. Portraits of the surgeon-scientist generation at St. Michael’s Hospital: R. Loch Macdonald (A), Julian Spears (B), Howard Ginsberg (C), and Sunit Das (D). Copyright St. Michael’s Hospital Archives. Pub-lished with permission.
Unauthenticated | Downloaded 06/15/20 06:31 AM UTC

History of neurosurgery: St. Michael’s
J Neurosurg Volume 127 • December 2017 1423
1993 as an assistant professor. He directed the University of Chicago neurosurgery residency program from 2000 to 2003. In 2007, Macdonald was recruited to Toronto as head of neurosurgery at St. Michael’s Hospital, as well as full professor in the Department of Surgery at the Uni-versity of Toronto. He held the Keenan Endowed Chair at St. Michael’s Hospital until 2016. His productive research program focuses on the basic mechanisms of vasospasm in subarachnoid hemorrhage, on which he is a world expert. He has published numerous clinical papers that studied risk factors and outcomes of aSAH and vasospasm30 and is highly active in maintaining the Subarachnoid Hemor-rhage International Trialists (SAHIT) repository.29
Academic and Educational Contributions of St. Michael’s
The University of Toronto and St. Michael’s Hospital have a lengthy record of distinction in Canadian research and education. One of the most important accomplish-ments was the division’s participation in the Arthur and Sonia Labatt Brain Tumor Research Centre project for identification of human brain tumor initiating cells, which led to a landmark paper in Nature.52 Horsey described the earliest surgical experience for early anterior operation in acute injuries of the cervical spine and a novel modified drill guide for anterior cervical fusion.5,21 Hudson pub-lished extensively in basic science research investigating the pathophysiology of peripheral nerve injury, regenera-tion, and allotransplantation.23,33,35 His laboratory gradu-ated many prominent fellows with interests in peripheral nerve surgery and neurosurgery. Among these are Susan E. Mackinnon,32–35 a plastic surgeon who went on to a bril-liant career in the United States and made significant con-tributions to women in surgery in North America;36,39 Ab-hijit “Ab” Guha,14,47 a Toronto-trained neurosurgeon and innovative brain tumor researcher (Dr. Guha died in 2011); and Fred Gentili,18,19 a world-renowned skull base surgeon at the Toronto Western Hospital.
In addition to his work as a site director for multiple large international vascular trials, Bill Tucker was the first Canadian neurosurgeon to show the value of reoperation for glioblastoma and the possible association between Chlamydia pneumonia and atherosclerosis of the carotid artery.9,13 Paul Muller published more than 20 articles on photodynamic therapy for gliomas,41–43,56 which resulted in Toronto being listed as having one of the major research groups on this topic, as mentioned in a recent review.46 In the present era of St. Michael’s Hospital, with the recruit-ment of exceptional translational researchers, the division continued to publish new insights on multiple neurosurgi-cal topics. Loch Macdonald and Tom Schweizer, a neuro-scientist at St. Michael’s Hospital, collaborated together to publish a series of peer-reviewed publications and a full comprehensive book for the cognitive and neurobehavioral effects of stroke and aSAH.1,2,6,7,50,51 Michael Cusimano’s work with Kalman T. Kovacs, a legendary pathologist and worldwide expert on pituitary disease, is another example of a highly productive collaborative team at St. Michael’s Hospital. Together, they published 48 scientific articles in-volving both in vitro and in vivo investigations for benign and aggressive complex pituitary tumors.10,12,48,49
All University of Toronto neurosurgical residents are part of the Gallie Program. The Gallie Program is an in-tegrated residency program in the diverse specialties of surgery. At each hospital, the division head of neurosur-gery directs that hospital’s neurosurgical unit and its re-lated role in neurosurgical education for fellows, residents, and students. Over the years, St. Michael’s division heads and faculty have influenced many residents and fellows in their surgical training. The division hosts 3 weekly grand rounds to discuss cases and clinical decisions in general neurosurgery, neurooncology, and cerebrovascular sur-gery. Furthermore, the division organizes city-wide rounds featuring prominent visiting professors from all over the world, including visits from Hans Peter Richter, Hanno Millesi, Giuseppe Lanzino, Henry Marsh, Christopher M. Wallace, and David G. Kline. Lastly, St. Michael’s Hos-pital provides 4 well-established fellowship programs in cerebrovascular (including endovascular), skull base, and spinal surgery, as well as surgical education.
The FutureThe prospective objectives of the Division of Neuro-
surgery at St. Michael’s Hospital are to continue its world-leading care for patients and to sustain the high-quality research in aSAH, neurotrauma, brain tumors, clinical epidemiology, and clinical trials design. It is anticipated that, in 2019, the hospital will finish major redevelopment projects that will include new operating rooms with state-of-the-art medical imaging equipment.
AcknowledgmentsWe thank Ms. Teruko Kishibe, archivist, St. Michael’s Hospital
Archives, for facilitating access to the archives of the Division of Neurosurgery. We dedicate this work to St. Michael’s neurosurgery nurses, nursing practitioners, and secretaries for their hard work in taking care of our patients for all the past years.
References 1. Al-Khindi T, Macdonald RL, Schweizer TA: Cognitive and
functional outcome after aneurysmal subarachnoid hemor-rhage. Stroke 41:e519–e536, 2010
2. Al-Khindi T, Macdonald RL, Schweizer TA: Decision-mak-ing deficits persist after aneurysmal subarachnoid hemor-rhage. Neuropsychology 28:68–74, 2014
3. Alexander E Jr: Kenneth George McKenzie, Canada’s first neurosurgeon. J Neurosurg 41:1–9, 1974
4. Bell CM, Brener SS, Gunraj N, Huo C, Bierman AS, Scales DC, et al: Association of ICU or hospital admission with unintentional discontinuation of medications for chronic dis-eases. JAMA 306:840–847, 2011
5. Berry H, Horsey WJ: A modified drill guide for the anterior cervical fusion (Cloward) procedure. Technical note. J Neu-rosurg 52:284–285, 1980
6. Bonares MJ, de Oliveira Manoel AL, Macdonald RL, Sch-weizer TA: Behavioral profile of unruptured intracranial aneurysms: a systematic review. Ann Clin Transl Neurol 1:220–232, 2014
7. Bonares MJ, Egeto P, de Oliveira Manoel AL, Vesely KA, Macdonald RL, Schweizer TA: Unruptured intracranial aneurysm treatment effects on cognitive function: a meta-analysis. J Neurosurg 124:784–790, 2016
Unauthenticated | Downloaded 06/15/20 06:31 AM UTC

N. M. Alotaibi et al.
J Neurosurg Volume 127 • December 20171424
8. Botterell EH: Dr. Kenneth George McKenzie. An apprecia-tion. Can Med Assoc J 91:880–881, 1964
9. Chiu B, Viira E, Tucker W, Fong IW: Chlamydia pneumoni-ae, cytomegalovirus, and herpes simplex virus in atheroscle-rosis of the carotid artery. Circulation 96:2144–2148, 1997
10. Cusimano MD, Kan P, Nassiri F, Anderson J, Goguen J, Vanek I, et al: Outcomes of surgically treated giant pituitary tumours. Can J Neurol Sci 39:446–457, 2012
11. Deslauriers J, Pearson FG, Nelems B: Evolution of thoracic surgery in Canada. Can Respir J 22:72, 2015
12. Di Ieva A, Rotondo F, Syro LV, Cusimano MD, Kovacs K: Aggressive pituitary adenomas—diagnosis and emerging treatments. Nat Rev Endocrinol 10:423–435, 2014
13. Dirks P, Bernstein M, Muller PJ, Tucker WS: The value of reoperation for recurrent glioblastoma. Can J Surg 36:271–275, 1993
14. Feldkamp MM, Gentili F, Hudson AR, Guha A: A persistent median artery causing carpal tunnel syndrome in a patient with chronic renal failure: case report. Neurosurgery 37:140–143, 1995
15. Findlay JM: Neurosurgery at the Toronto General Hospital, 1924–1990: part 2. Can J Neurol Sci 21:278–284, 1994
16. Findlay JM: William M. Lougheed and the development of vascular neurosurgery at the Toronto General Hospital. Can J Neurol Sci 20:337–340, 1993
17. Findlay JM, Tucker WS: William John Horsey, M.D., F.R.C.S.C. Neurosurgeon to St. Michael’s Hospital, Toronto. Can J Neurol Sci 20:254–255, 1993
18. Gentili F, Hudson AR, Hunter D: Clinical and experimental aspects of injection injuries of peripheral nerves. Can J Neu-rol Sci 7:143–151, 1980
19. Gentili F, Hudson AR, Kline D, Hunter D: Early changes following injection injury of peripheral nerves. Can J Surg 23:177–182, 1980
20. Hendrick EB, Harwood-Hash DC, Hudson AR: Head injuries in children: a survey of 4465 consecutive cases at the hospital for sick children, Toronto, Canada. Clin Neurosurg 11:46–65, 1964
21. Horsey WJ, Tucker WS, Hudson AR, Schatz SW: Experience with early anterior operation in acute injuries of the cervical spine. Paraplegia 15:110–122, 1977
22. Hudson A, Morris J, Weddell G: An electron microscopic study of regenervation in sutured rat sciatic nerves. Surg Fo-rum 21:451–453, 1970
23. Hudson AR, Hunter D, Kline DG, Bratton BR: Histological studies of experimental interfascicular graft repairs. J Neu-rosurg 51:333–340, 1979
24. International Study of Unruptured Intracranial Aneurysms Investigators: Unruptured intracranial aneurysms—risk of rupture and risks of surgical intervention. N Engl J Med 339:1725–1733, 1998
25. Jea A, Al-Otibi M, Rutka JT, Drake JM, Dirks PB, Kulkarni AV, et al: The history of neurosurgery at the Hospital for Sick Children in Toronto. Neurosurgery 61:612–625, 2007
26. Kopplin PA: On Call in the Heart of the City: 100 Years of Resident and Intern Life. Toronto: Warwick, 1993
27. Kunicki A: Operative experiences in 8 cases of pineal tumor. J Neurosurg 17:815–823, 1960
28. Louw JH, Barnard CN: Congenital intestinal atresia; obser-vations on its origin. Lancet 269:1065–1067, 1955
29. Macdonald RL, Cusimano MD, Etminan N, Hanggi D, Hasan D, Ilodigwe D, et al: Subarachnoid Hemorrhage Interna-tional Trialists data repository (SAHIT). World Neurosurg 79:418–422, 2013
30. Macdonald RL, Higashida RT, Keller E, Mayer SA, Moly-neux A, Raabe A, et al: Clazosentan, an endothelin receptor antagonist, in patients with aneurysmal subarachnoid haem-orrhage undergoing surgical clipping: a randomised, double-blind, placebo-controlled phase 3 trial (CONSCIOUS-2). Lancet Neurol 10:618–625, 2011
31. Macdonald RL, Weir BK: A review of hemoglobin and the pathogenesis of cerebral vasospasm. Stroke 22:971–982, 1991
32. Mackinnon SE, Dellon AL, Hudson AR, Hunter DA: Chronic human nerve compression—a histological assessment. Neu-ropathol Appl Neurobiol 12:547–565, 1986
33. Mackinnon SE, Dellon AL, Hudson AR, Hunter DA: Chronic nerve compression—an experimental model in the rat. Ann Plast Surg 13:112–120, 1984
34. Mackinnon SE, Dellon AL, Hudson AR, Hunter DA: A primate model for chronic nerve compression. J Reconstr Microsurg 1:185–195, 1985
35. Mackinnon SE, Hudson AR: Clinical application of periph-eral nerve transplantation. Plast Reconstr Surg 90:695–699, 1992
36. Mackinnon SE, Mizgala CL, McNeill IY, Walters BC, Fer-ris LE: Women surgeons: career and lifestyle comparisons among surgical subspecialties. Plast Reconstr Surg 95:321–329, 1995
37. Maset AL, Marmarou A, Ward JD, Choi S, Lutz HA, Brooks D, et al: Pressure-volume index in head injury. J Neurosurg 67:832–840, 1987
38. McDonald I: For the Least of My Brethren: A Centenary History of St. Michael’s Hospital. Toronto: Dundurn Press, 1992
39. Mizgala CL, Mackinnon SE, Walters BC, Ferris LE, McNeill IY, Knighton T: Women surgeons. Results of the Canadian Population Study. Ann Surg 218:37–46, 1993
40. Morley TP: Biographical sketch of Kenneth G. McKenzie (1892–1964). J Neurosurg 93:518–525, 2000
41. Muller PJ, Wilson BC: Photodynamic therapy for malignant newly diagnosed supratentorial gliomas. J Clin Laser Med Surg 14:263–270, 1996
42. Muller PJ, Wilson BC: Photodynamic therapy for recurrent supratentorial gliomas. Semin Surg Oncol 11:346–354, 1995
43. Muller PJ, Wilson BC: Photodynamic therapy of malignant primary brain tumours: clinical effects, post-operative ICP, and light penetration of the brain. Photochem Photobiol 46:929–935, 1987
44. Pratt DW: Acute suppurative ventriculitis secondary to brain abscess with recovery. Can Med Assoc J 55:128–131, 1946
45. Pratt DW, Brooks EF: Successful excision of a tumour of the pineal gland. Can Med Assoc J 39:240–243, 1938
46. Quirk BJ, Brandal G, Donlon S, Vera JC, Mang TS, Foy AB, et al: Photodynamic therapy (PDT) for malignant brain tumors—where do we stand? Photodiagn Photodyn Ther 12:530–544, 2015
47. Rutka JT: In memoriam, Dr. Abhijit Guha, 1957–2011. Neuro Oncol 14:3–5, 2012
48. Salehi F, Kovacs K, Cusimano MD, Horvath E, Bell CD, Rotondo F, et al: Immunohistochemical expression of nestin in adenohypophysial vessels during development of pituitary infarction. J Neurosurg 108:118–123, 2008
49. Salehi F, Kovacs K, Scheithauer BW, Lloyd RV, Cusimano M: Pituitary tumor-transforming gene in endocrine and other neoplasms: a review and update. Endocr Relat Cancer 15:721–743, 2008
50. Schweizer TA, Al-Khindi T, Macdonald RL: Mini-Mental State Examination versus Montreal Cognitive Assessment: rapid assessment tools for cognitive and functional outcome after aneurysmal subarachnoid hemorrhage. J Neurol Sci 316:137–140, 2012
51. Schweizer TA, Macdonald L: The Behavioral Consequenc-es of Stroke. New York: Springer, 2013
52. Singh SK, Hawkins C, Clarke ID, Squire JA, Bayani J, Hide T, et al: Identification of human brain tumour initiating cells. Nature 432:396–401, 2004
53. St. Michael’s Archives: St. Michael’s Hospital Medical Staff Report for 1922–1952, Document number: H-3 (135). Toronto: St. Michael’s Hospital, 1952
Unauthenticated | Downloaded 06/15/20 06:31 AM UTC

History of neurosurgery: St. Michael’s
J Neurosurg Volume 127 • December 2017 1425
54. Stelter GA, Artibise AFJ: The Canadian City. Essays in Ur-ban and Social History. Ottawa: Carleton University Press, 1984
55. Weir B: A history of neurosurgery in Canada. Can J Neurol Sci 38:203–219, 2011
56. Yang VX, Muller PJ, Herman P, Wilson BC: A multispectral fluorescence imaging system: design and initial clinical tests in intra-operative Photofrin-photodynamic therapy of brain tumors. Lasers Surg Med 32:224–232, 2003
57. Young WA (ed): Robert Dwyer. Can J Med Surg 47:173–175, 1920
DisclosuresDr. Macdonald reports that he receives grant support from the Physicians Services Incorporated Foundation, the Brain Aneurysm Foundation, the Canadian Institutes for Health Research, and the Heart and Stroke Foundation of Canada, and is chief scientific officer of Edge Therapeutics, Inc.
Author ContributionsConception and design: Macdonald, Alotaibi. Acquisition of data: Alotaibi. Analysis and interpretation of data: Alotaibi, Guha. Drafting the article: Alotaibi, Guha, Ahuja, Tucker, Hudson. Criti-cally revising the article: Macdonald, Spears, Muller, Tucker, Hudson. Reviewed submitted version of manuscript: all authors. Study supervision: Macdonald.
Supplemental Information Online-Only ContentSupplemental material is available with the online version of the article.
Supplementary Tables 1–4. https://thejns.org/doi/suppl/ 10.3171/2016.9.JNS161119.
CorrespondenceR. Loch Macdonald, Division of Neurosurgery, St. Michael’s Hos-pital, University of Toronto, 30 Bond St., Toronto, ON M5B 1W8, Canada. email: [email protected].
Unauthenticated | Downloaded 06/15/20 06:31 AM UTC