Histopathology of the rheumatoid lesion
-
Upload
michael-bromley -
Category
Documents
-
view
220 -
download
2
Transcript of Histopathology of the rheumatoid lesion

HISTOPATHOLOGY OF THE RHEUMATOID LESION
Identification of Cell Types at Sites of Cartilage Erosion
MICHAEL BROMLEY and DAVID E. WOOLLEY
Histochemical and ultrastructural techniques were used to examine the cartilage-pannus junction of 49 rheumatoid joints. Whereas 24 showed relatively acellular, fibrous pannus tissue, 25 demonstrated “cel- lular” junctions with different cell types at sites of erosion. Macrophages and fibroblasts were commonly observed as majority cell types in most specimens, but others showed mast cells, polymorphonuclear leuko- cytes, dendritic, or plasma cells as the predominant cell type. Some showed local accumulations of different cell types at sites along each junction. Our findings show that the cellular composition at sites of cartilage erosion varies greatly and suggest that cells are subject to turnover and interchange.
Extensive proteolytic degradation of articular cartilage is a characteristic feature of joint destruction in rheumatoid arthritis. This process is generally irre- versible and is commonly associatcd with invasive, hypertrophied synovium. Histologic observations have shown that the early rheumatoid lesion is charac- terized by a proliferation of synovial lining cells with subscquent neovascularization and infiltration by lym-
-- ~
From the University Department of Medicine, University Hospital of South Manchester. West Didsbury. Manchester. United Kingdom.
Supported by grants from the Arthritis and Rheumatism Council.
Michael Bromley. BSc, MSc: Research Associate of the Arthritis and Rheumatism Council; David E. Woolley, PhD: Univer- sity Senior Research Fellow, University Hospital of South Man- Chester.
Address reprint requests to David E. Woolley. PhD. De- partment of Medicine, University Hospital of South Manchester. Manchester. M20 8LR, United Kingdom.
Submitted for publication January 24, 1984; accepted in revised form April 3. 1984.
phocytes, macrophages, fibroblasts, and plasma cells (1-4). The importance of this soft pannus tissue in cartilage erosion has been recognized by several re- searchers, especially from in vitro studies which have shown it to be a source of matrix-degrading enzymes
Immunolocalization studies have demonstrated the enzyme collagenase at the cartilage-pannus junc- tions of several rheumatoid specimens, but relatively little immunoreactive enzyme was associated with the chondrocytes or pannus tissue remote from the junc- tion (8,9). Such observations have provided direct evidence that collagenase participates in cartilage ero- sion and suggest that the physiologic conditions of the cartilage-pannus junction are very different from those of adjacent tissues, possibly reflecting the type and distribution of specific cells (8,9). Similar findings have been reported for the immunolocalization of neutrophil elastase in rheumatoid tissue (10). Histolog- ic studies of cartilage-pannus junctions have demon- strated mainly fibroblast and macrophage-like cells (1 1-15). polyrnorphonuclear ncutrophils (16,17), and “immature mesenchymoid cells” (4,ItT); as judged by their morphologic appearance. Most ultrastructural studies have been limited to relatively few specimens. In this study on 49 rheumatoid joints, we have at- tempted to identify the cells at sites of cartilage erosion using specific histochemical staining tech- niques.
(5-8).
MATERIALS AND METHODS Preparation of swimens. Specimens of cartilage-
pannus junction were obtained during therapeutic arthro- tomy procedures on knee joints of patients with classic, seropositive rheumatoid arthritis. Each specimen was fixed
Arthritis and Rheumatism, Vol. 27, No. 8 (August 1984)

858 BROMLEY AND WOOLLEY
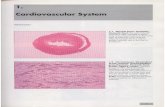
Figure 1. a, Photomicrograph of a fibrous cartilage-pannus junction stained with methylene blue-azure 11. b. Photomicrograph of a cellular cartilage-pannus junction stained with methylene blue-azure 11; cm = cartilage matrix; fp = fibrous pannus; c p = cellular pannus. Bars represent 50 wm.
for 2 hours in 1% formaldehyde and 0.25% glutaraldehyde in 0. IM sodium cacodylate buffer (pH 7.4) and rinsed in 0.15M sodium cacodylate (pH 7.4) prior to acetone dehydration. The specimens were infiltrated overnight in JB-4 solution A (Polysciences, Warrington, PA) and finally embedded in thc complete JB-4 mixture (20 ml NO.15 gm initiator 0.7 ml B). All steps were carried out at 4°C. Sections 2.5 pm thick were cut on an LKB Historange microtome, floated on water, and dried on glass coverslips at 30°C.
For electron microscopy, the specimens were fixed for 3 hours in 1.5% glutaraldchyde buffered with O.IM sodium cacodylatc (pH 7.4) and 3 mM MgCI2, followed by 1.5 hours postfixation in 1% osmium tetroxidc. Epon 812 sections were stained with uranyl acetate and lead citratc and examined on an AEI Corinth electron microscope.
Enzyme histochemistry. JB-4 sections of each speci- men were stained as follows: Chloracetate esternse (CAE). The incubation medium comprised 2 mg Naphthol AS-D chloracetate (Sigma, St. Louis, MO) in 0.5 ml dimethyl formamide which was added to 9.5 ml 0.067M phosphate buffer (pH 7.4) and 0.05 ml hexazotized new fuchsin. Sec- tions were incubated with medium for 90 minutes at 37°C (19).
Naplrrhyl acetate esterase ( N A E ) . The incubation medium contained 10 mg a-naphthyl acetate (Sigma) in 0.5 ml ethylene glycol monomethyl ether (EGMME) which was added to 9.5 ml 0.067M phosphate buffer (pH 6.3) and 0.05 ml hexazotized pararosaniline. Sections were incubated for 2 hours at 37°C (19).
Aminocaproate esterase (ACE). The incubation me-
dium contained 2 mg Naphthol AS aminocaproate in 1 .O ml EGMME which was added to 0.067M phosphate buffer (pH 7.4) and 0.05 ml hexazotized new fuchsin. Sections were incubated for 90 minutes at 37°C (20).
All sections were counterstained briefly in 0.25% azure II,0.25% methylene blue in 0.25% borax; micrographs were taken on a Vickers M41 photoplan microscope using Kodak Panatomic X film and a green filter.
Cell identification, Macrophagic cells were identified as NAE-positive cells with macrophagic morphology. Whereas NAE staining of macrophages was usually intense, a few fibroblasts were weakly positive, and T lymphocytes demonstrated an obvious punctate pattern of staining. Mast cells were positive for CAE and ACE, and their characteris- tic granules were confirmed by electron microscopy (21). Polymorphonuclear leukocytes (PMNs) were recognized by their positive reaction for CAE and nuclear morphology, and were differentiated from mast cells by their lack of ACE staining. Other cell types were identified morphologically and included fibroblastic, dendritic, and plasma cells. Each junction was classified by the predominant cell type within 2-3 cell diameters of the cartilage front.
RESULTS Forty-nine specimens of cartilage-pannus junc-
tion were examined. Whereas 24 of these showed relatively acellular, fibrous pannus overlying a smooth cartilage surface, 25 specimens demonstrated cellular

CELLS IN CARTILAGE EROSION 859
Figure 2. a, Photomicrograph of a cartilage-pannus junction stained for a-naphthyl acetate esterase, showing positive macro- phagic cclls in close contact with cartilage matrix. Counterstained with methylene blue-azure 11. Bar represents 40 pm. b, Photomicro- graph of a cartilage-pannus junction showing mast cells with charac- teristic granular inclusions. Section stained with methylene blue- azure 11. Adjacent sections stained for chloracetate esterase (CAE) and aminocaproate esterase confirmed identification of mast cells. Bar represents 20 Fm. c, Photomicrograph of a cartilage-pannus junction showing polymorphonuclear leukocytes and characteristic nuclei. Section stained with methylene blue-azure 11. Adjacent sections showed same cells positive for CAE‘. Bar represents 20 pm.
junctions with pockets of cells penetrating the carti- lage matrix (Figure 1). Using histochemical techniques with light microscopy, and morphologic studies with electron microscopy, specific cell types, such as mac- rophages, mast cells, polymorphonuclear leukocytes, fibroblasts, and lymphocytes were identified. Since we were primarily interested in the types of cell at the cartilage-pannus junction, we made a careful analysis of the cells within approximately 2-3 cell diameters of the cartilage front. Although all specimens showed a mixed population of cells at the junction, in most cases it was possible to identify one predominant type (Figures 2 and 3).
Table I provides an indication of the frcquen- cies of the predominant cell types in the 25 cellular junctions. Macrophage- and fibroblast-type junctions were observed in a majority of the specimcns; 3 were classified as mast cell junctions and 2 as polymorpho- nuclear leukocyte junctions. Plasma cells and dendrit- ic cells each represented the majority cell type at the junction of I specimen. Two other specimens rc- mained “unclassified” because they contained a mixed population of cells in roughly equal proportions. Three specimens were each classified under 2 head- ings (thus making a total of 28 in Table 1); 1 contained a preponderance of PMNs or macrophages at different sites along the junction, while the others had similar distributions of mast cells and fibroblasts or macro- phages and fibroblasts.
Figure 2a shows an example of a macrophagic junction with NAE-positive cells in close contact with cartilage. Mast cells containing metachromatic gran- ules and PMNs at sites of cartilage erosion are shown in Figures 2b and c, respectively. Degranulated mast cells were difficult to identify, but scattered granules were obscrved occasionally along the cartilagepan- nus junction of a few specimens (data not shown). The presence of polymorphonuclear leukocytes was usual- ly associated with a relatively thin pannus tissue.
Figure 3a shows a fibroblast-typc junction with cells negative for NAE, CAE, and ACE staining, but exhibiting a typical bipolar morphology. Dendritic cells, with long, branched cytoplasmic processes pen- etrating into the cartilage matrix, are shown in Figure 3b. Such cells strikingly resembled the synovial den- dritic cells that have been shown to elaborate collage- nase in vitro (22). Figure 3c shows the junction which contained predominantly plasma cells, identified by their characteristic nuclear staining.
Figure 4 illustrates a specimen that was classi- fied as being both macrophagic and polymorphonucle-

860 BROMLEY AND WOOLLEY
DISCUSSiON Of the 49 rheumatoid joints examined, 25 had
clearly defined cellular cartilagc-pannus junctions and 24 showed a fibrous pannus with very few cells at the cartilage interface. These relatively “acellular,” f i - brous junctions usually showed a smooth cartilage surface, suggesting a nonerosive or quiescent phase, in contrast to the irregular cartilage fronts commonly observed in cellular junctions. Previous ultrastructural studies of the cartilage-pannus interface havc reported macrophagic and fibroblastic cells, designated mor- phologically as synovial types A and B, respectively
Since hypertrophic rheumatoid synovial tissue contains a variety of inflammatory and tissue cells ( I - 3), such studies describing only typc A and B cclls seemed an oversimplification for such a heterogeneous tissue. Using both histochemical esterase staining techniques for mast cells, macrophagcs, and polymor- phonuclear leukocytes, and electron microscopic stud- ies, we have attempted to identify more preciscly the cell types at cartilage-pannus junctions. The dual problems of sectioning hard tissue and retaining en- zyme activity for histochemical reactions werc over- come by using a methacrylate-based embedding mcdi- um (JB-4, Polysciences) (23,24).
The junctions examined broadly resembled the 3 types described by Kobayashi and Ziff ( 1 1 ) . In agreement with the findings of others ( 1 1-15), macro- phages and fibroblasts were idcntificd in almost all the cellular junctions in our study, and represented the majority ccll type in most specimens. Mohr and col- leagues (16,17) have suggestcd that about 25% of cartilage-pannus junctions contain polymorphonuclear leukocytes, an observation that has not been con- firmed by most other studies. Sincc those investigators used naphthol-ASD-chloracetate esterase staining to identify PMNs, it is possible that mast cells, which are also positive for CAE, may have contributed to their numbers.
Although we did not find such a high incidence
( 1 1-13).
Figure 3. a, Photomicrograph of fibroblastic cells at the cartilage- pannus junction. Stained with methylene blue-azure 11. Bar repre- sents 20 pm. b, Photomicrograph showing dendritic cells at the cartilage-pannus junction. Stained with methylenc blue-azure 11. Bar represents 10 pm. c. Photomicrograph of plasma cells at the cartilage-pannus junction. Stained with methylene blue-azure 11. Bar represents 40 pm.
ar. Each of thesc cell types was in the majority at different regions of the cartilagc-pannus junction. This observation demonstrates that even within one speci- men, differcnt distributions of cells may be found at sites of cartilage erosion.
Table 1. Classification of cartilage-pannus junctions according to predominant cell type’
Macrophagic Fibroblastic Mast cells Polymorphonuclear leukocytes Plasma cells Dendritic Unclassified
* n = 2 5 ; 3 specimens were each classified under 2 headings.

CELLS IN CARTILAGE EROSION 86 1
Figure 4. a , Low-power photomicrograph of a cartilage-pannus junction stained with methylene blue-azure 11. Arrow with b delineates macrophages (shown at higher magnification in Figure 4b). Arrow with c delineates polymorphonuclear leukocytes (shown at higher magnification in Figure 4c). Bar represents 100 pm. b, Photomicrograph of cartilage-pinnus junction region labeled b in Figure 4a. Section stained for (I- naphthyl acetate esterase showing macrophages (darkly stained) and fibroblasts. Counterstained with rnethylene blue-azure 11. Bar represents 10 pm. c. Photomicrograph of cartilage-pannus junction region labeled c in Figure 4a. Polymorphonuclear leukocyres at the cartilage interface. Stained with methylene blue- azure 11. Bar represents 10 prn.
of PMNs, we can confirm that PMNs can be seen apparently penetrating the cartilage matrix. The 2 polymorphonuclear junctions found in this study were usually associated with a relatively thin pannus tissue, perhaps suggesting an early phase of cartilage degrada- tion and pannus formation. All but 2 of our specimens were derived from knee joints: thus, our observations may not necessarily reflect the histopathology of other,
more distal, smaller joints such as those investigated by Mohr and coworkers (16,17).
The recognition of mast cells at sites of cartilage erosion is particularly interesting since these cells have the potential to degrade cartilage by the produc- tion of proteoglycan-degrading enzymes (25) and to participate in inflammatory reactions. The 3 mast cell junctions observed represented local accumulations of

862 BROMLEY AND WOOLLEY
such cells, in contrast to their random distribution (about 2-3% of all cells) in pannus tissue remote from the junction (Bromley M: unpublished data). The potential of mast cells to regulate microenvironmental conditions (26), their role in autoimmune reactions and chronic inflammation (27), and the recent demonstra- tion that chondrocytes have surface histamine H-2 receptors (28) suggest that they may play an important role in the mechanism of cartilage degradation.
The majority of our specimens came from pa- tients in advanced stages of disease; it is possible that the cellular composition described may be different from that of early erosive lesions. Fassbender (4,18) has recently described immature mesenchymal cells as being responsible for cartilage erosion in very early rheumatoid disease, and mast cells and PMNs were the first to appear in very early stages of rat adjuvant arthritis (29). However, our observations of collage- nase at thc cartilage-pannus interface in joints from patients with advanced rheumatoid disease suggest that cartilage erosion is not limited to the early stages of disease activity (8,9).
Small blood vessels were occasionally observed close to the junction, but they were rarely found to penetrate the cartilage matrix. No lymphocytes were observed at sites close to the cartilage, but these cells were very conspicuous in the pannus tissue remote from the junction, as described by othcrs (30,31). Some studies have suggested that chondrocytcs par- ticipate in cartilage degradation, as judged by loss of pericellular proteoglycan and collagen (12,32). We have observed this phenomenon in 20-30% of speci- mens (especially marked in relation to mast cell junc- tions), but the remaindcr showed normal chondrocyte appearances even close to the erosive lesion.
Although macrophages and fibroblasts repre- sented the predominant cells in 76% of the cellular junctions, the observation of mast cells, PMNs, and others suggests that the cells of the rheumatoid lesion are subject to turnover and interchange. This is partic- ularly well-demonstrated in Figure 4, where PMNs and macrophages are each shown to be locally concentrat- ed at different micro-foci of the same junction. More- over, we believe that cartilage erosion may represent a transient, discontinuous process occurring in local regions along the cartilage-pannus junction (8,9), and it is probably determined at any one time by specific cell types and their reaction to microenvironmental conditions. Although our studies suggest that the cellular composition of the rheumatoid lesion is sub- ject to change, we do not know the sequence of
cellular events, or the relative time that each cell type occupies the junctional region.
ACKNOWLEDGMENTS We thank Rosaleen Walker for excellent technical
assistance, and Drs. H. Bertfield, H. Williams, and W. Fisher, consultant orthopedic surgeons, for the supply of specimens. We also thank Professor L. T. Yam for his gift of Naphthol AS aminocaproate. Professor J. Evanson for his reading of the manuscript, and Mrs. K. Hale for its prepara- tion.
REFERENCES
1. Kulka JP, Bocking D, Ropes MW, Bauer W: Early joint lesions of rheumatoid arthritis. Arch Pathol Lab Med 59:129-150, 1955
2. Ball J : Pathological aspccts of rheumatoid arthritis, Early Synovectomy in Rheumatoid Arthritis. Edited by W Hijmons, WD Paul, H Herschel. Amsterdam, Ex- cerpta Medica Foundation, 1969, p 23
3. Gardner DL: Pathology of rheumatoid arthritis. Cope- man's Textbook of the Khcumatic Diseases. Fifth edi- tion. Edited by JT Scott. London, Churchill Living- stone, 1978, pp 273-317
4. Fassbender HG: Histomorphological basis of articular cartilage destruGtion in rheumatoid arthritis. Coll Relat Res 3:141-155, 1983
5. Evanson JIM, Jeffrey J J . Krane SM: Studies on collage- nase from rheumatoid synovium in tissue culture. J Clin Invest 47:2639-2651, 1968
6 . Krane SM: Heberden oration 1980: aspects of the cell biology of the rheumatoid synovial lesion. A n n Rheum Dis 40:433-448, 1981
7. Dingle J?': Hcberden oration 1978: recent studies on the control of joint damage: the contribution of the Strangeways Research Laboratory. Ann Rheum Dis 38:201-214, 1979
8. Woolley DE, Crossley MJ, Evanson JM: Collagenase at sites of cartilage erosion in the rheumatoid joint. Arthri- tis Rheum 20:1231-1239, 1977
9. Woolley DE, Tetlow LC, Evanson JM: Collagenase immunolocalisation studies of rheumatoid and malignant tissues, Collagenase in Normal and Pathological Con- nective Tissues. Edited by DE Woolley, JM Evanson. Chichester, UK, John Wiley and Sons, 1980, pp 105-125
10. Menninger H, Putzier R, Mohr W, Wessinghage D, Tillman K: Granulocyte elastase at the site of cartilage erosion by rheumatoid synovial tissue. Z Rheumatol
11. Kobayashi I , Ziff M: Electron microscopic studies of the 39~145-156, 1980

CELLS IN CARTILAGE EROSION 863
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
cartilage-pannus junction in rheumatoid arthritis. Arthri- tis Rheum 18:475-483, 1975 Muirden KD: Electron microscopic studies of the syno- vial-cartilage junction in rheumatoid arthritis. Eur J Rheumatol Inflamm 5:30-38, 1982 Shiozawa S, Shiozawa K, Fujita T: Morphologic obser- vations in the early phase of the cartilage-pannus junc- tion: light and electron microscopic studies of active cellular pannus. Arthritis Rheum 26:472-478, 1983 Mills K: Pathology of the knee joint in rheumatoid arthritis: a contribution to the understanding of synovec- tomy. J Bone Joint Surg 52B:746-756, 1970 Tateishi H: Ultrastructure of synovio-cartilage junction rheumatoid arthritis. Kobe J Med Sci 1951-56, 1973 Mohr W, Menninger H: Polymorphonuclear granulo- cytes at the pannus-cartilage joint in rheumatoid arthri- tis (letter). Arthritis Rheum 23: 1413-1414, 1980 Mohr W, Wessinghage D: The relationship between polymorphonuclear granulocytes and cartilage destruc- tion in rheumatoid arthritis. Z Rhcumatol 37:81-86, 1978 Fassbender HG, Simmling-Annefeld M: The potential aggressiveness of synovial tissue in rheumatoid arthritis. J Pathol 139:399-406, 1983 Yam LT, Li CY, Crosby WH: Cytochemical identifica- tion of rnonocytes and granulocytes. Am J Clin Pathol
Yam LT, Yam CF, Li CY: Eosinophilia in systemic mastocytosis. Am J Clin Pathol 73:48-54, 1980 Caulfield JP, Lewis RA, Hein A, Austen KF: Secretion in dissociated human pulmonary mast cclls. J Cell Biol
Woolley DE, Brinckerhoff CE, Mainardi CL, Vater CA, Evanson JM, Harris ED: Collagenase production by rheumatoid synovial cells: morphological and irnrnuno-
55~283-290, 1970
85:299-312, 1980
histochemical studies of the dendritic cell. Ann Rheum Dis 38:262-270, 1979
23. Ruddell CL: Embedding media for 1-2 micron section- ing 2 hydroxyethyl methacrylate combined with 2-bu- toxyethanol. Stain Techno1 42:253-255, 1%7
24. Beckstead JH, Bainton DF: Enzyme histochemistry on bone marrow biopsies: reactions useful in the differential diagnosis of leukemia and lymphoma applied to 2- micron plastic sections. Blood 55:38&394. 1980
25. Bromley M, Fisher WD. Woolley DE: Mast cells at sites of cartilage erosion in the rheumatoid joint. Ann Rheum Dis 43:76-79, 1984
26. Lewis RA, Austen KF: Mediation of local homeostasis and inflammation by leukotrienes and other mast cell- dependent compounds. Nature 293: 103-108, 1981
27. Austen KF: Biologic implications of the structural and functional characteristics of the chemical mediators of immediate-type hypersensitivity. Harvey Lect Series
28. Taylor DJ, Yoffe JR, Woolley DE: Histamine Hz recep- tors on foetal-bovine articular chondrocytes. Biochem J
29. Gryfe A, Sanders PM. Gardner DL: The mast cell in early rat adjuvant arthritis. Ann Rheum Dis 30:24-30, 1971
30. Kobayashi I, Ziff M: Electron microscopic studies of lymphoid cells in the rheumatoid synovial membrane. Arthritis Rheum 16:471-486. 1973
31. Ziff M: Relation of cellular infiltration of rheumatoid synovial membrane to its immune response. Arthritis Rheum 17:313-319, 1974
32. Mitchell NS, Shepard N: Changes in proteoglycan and collagen in cartilage in rheumatoid arthritis. J Bone Joint Surg 60A:349-354, 1978
73:93-161, 1979
2 125 17-520, I983
Brandt and Gay Win Carol Nachrnan Prize
ARA members Dr. Kenneth D. Brandt, Professor and Chief of the Rheumatology Division, Indiana University School of Medicine, Indianapolis and Dr. Renate E. Gay, Research Associate Professor of Medicine, Division of Clinical Immunology and Rheumatology, Department of Medicine, University of Alabama in Birmingham, have been awarded the 1984 Carol Nachman Prize for Rheumatology. Both researchers established for the first time a comprehensive testing system which investigates the direct effects of antirheumatic drugs on the major target organ of joint cartilage. Their work was entitled “New Basic Research and Testing-Systems for the Comprehensive Evaluation of the Effects of Antirheumatic Drugs on Articular Cartilage.” Drs. Brandt and Gay have developed a two-step test system which involves studies on the effect of nonsteroidal antiinflammatory (antirheumatic) drugs on the proteoglycan and collagen metabolism of normal and osteoarthritic cartilage in vitro, as well as in an in vivo dog model. The Carol Nachman Prize of about $30,000.00 was awarded on May 11, 1984 in Wiesbaden, West Germany. Previous winners from the United States are Dr. Morris Ziff of Dallas, Texas and Drs. Steffen Gay, Edward J. Miller, and William J. Koopman, all of the University of Alabama in Birmingham.